Abstract
Background
Sepsis occurs when an infection is complicated by organ failure. Sepsis may be complicated by impaired corticosteroid metabolism. Thus, providing corticosteroids may benefit patients. The original review was published in 2004 and was updated in 2010 and 2015 prior to this update.
Objectives
To examine the effects of corticosteroids on death in children and adults with sepsis.
Search methods
We searched CENTRAL, MEDLINE, Embase, LILACS, ClinicalTrials.gov, ISRCTN, and the WHO Clinical Trials Search Portal, on 25 July 2019. In addition, we conducted reference checking and citation searching, and contacted study authors, to identify additional studies as needed.
Selection criteria
We included randomized controlled trials (RCTs) of corticosteroids versus placebo or usual care (antimicrobials, fluid replacement, and vasopressor therapy as needed) in children and adults with sepsis. We also included RCTs of continuous infusion versus intermittent bolus of corticosteroids.
Data collection and analysis
All review authors screened and selected studies for inclusion. One review author extracted data, which was checked by the others, and by the lead author of the primary study when possible. We obtained unpublished data from the authors of some trials. We assessed the methodological quality of trials and applied GRADE to assess the certainty of evidence. Review authors did not contribute to assessment of eligibility and risk of bias, nor to data extraction, for trials they had participated in.
Main results
We included 61 trials (12,192 participants), of which six included only children, two included children and adults, and the remaining trials included only adults. Nine studies are ongoing and will be considered in future versions of this review. We judged 19 trials as being at low risk of bias.
Corticosteroids versus placebo or usual care
Compared to placebo or usual care, corticosteroids probably slightly reduce 28‐day mortality (risk ratio (RR) 0.91, 95% confidence interval (CI) 0.84 to 0.99; 11,233 participants; 50 studies; moderate‐certainty evidence). Corticosteroids may result in little to no difference in long‐term mortality (RR 0.97, 95% CI 0.91 to 1.03; 6236 participants; 7 studies; low‐certainty evidence) and probably slightly reduce hospital mortality (RR 0.90, 95% CI 0.82 to 0.99; 8183 participants; 26 trials; moderate‐certainty evidence). Corticosteroids reduced length of intensive care unit (ICU) stay for all participants (mean difference (MD) ‐1.07 days, 95% CI ‐1.95 to ‐0.19; 7612 participants; 21 studies; high‐certainty evidence) and resulted in a large reduction in length of hospital stay for all participants (MD ‐1.63 days, 95% CI ‐2.93 to ‐0.33; 8795 participants; 22 studies; high‐certainty evidence). Corticosteroids increase the risk of muscle weakness (RR 1.21, 95% CI 1.01 to 1.44; 6145 participants; 6 studies; high‐certainty evidence). Corticosteroids probably do not increase the risk of superinfection (RR 1.06, 95% CI 0.95 to 1.19; 5356 participants; 25 studies; moderate‐certainty evidence). Corticosteroids increase the risk of hypernatraemia (high‐certainty evidence) and probably increase the risk of hyperglycaemia (moderate‐certainty evidence). Moderate‐certainty evidence shows that there is probably little or no difference in gastroduodenal bleeding, stroke, or cardiac events, and low‐certainty evidence suggests that corticosteroids may result in little to no difference in neuropsychiatric events.
Continuous infusion of corticosteroids versus intermittent bolus
We are uncertain about the effects of continuous infusion of corticosteroids compared with intermittent bolus administration. Three studies reported data for this comparison, and the certainty of evidence for all outcomes was very low.
Authors' conclusions
Moderate‐certainty evidence indicates that corticosteroids probably reduce 28‐day and hospital mortality among patients with sepsis. Corticosteroids result in large reductions in ICU and hospital length of stay (high‐certainty evidence). There may be little or no difference in the risk of major complications; however, corticosteroids increase the risk of muscle weakness and hypernatraemia, and probably increase the risk of hyperglycaemia. The effects of continuous versus intermittent bolus administration of corticosteroids are uncertain.
Plain language summary
Corticosteroids for treating sepsis
Review question
We reviewed the evidence on the effect on death of using corticosteroids in children and adults with sepsis.
Background
Sepsis is present when an infection is complicated by organ failure. People develop rapid breathing, hypotension (low blood pressure), and mental confusion. Sepsis can interfere with the effectiveness of the body’s corticosteroids, which serve as a key defence against infection. Corticosteroids have been given for decades to people with infection resulting from various causes.
Search date
The evidence provided in this review is current to July 2019.
Study characteristics
This review included 61 trials (12,192 participants). Fifty‐eight trials compared corticosteroids to no corticosteroids (placebo or usual care in 48 and nine trials, respectively); three trials also compared continuous versus bolus administration of corticosteroids.
Study funding sources
Three trials were funded by a drug company, 27 by public organizations or through charitable funding, and six by both a drug company and public organizations or charitable funding; 25 did not declare the source of funding.
Key results
We have analysed the following two comparisons.
• Corticosteroids versus placebo/usual care.
Corticosteroids probably reduce the risk of death at 28 days by 9% (50 trials; 11,233 participants), with consistent treatment effects between children and adults. They also probably slightly reduce the risk of dying in hospital. There may be little or no effect of corticosteroids on risk of dying over the long term (longer than three months), but these results are less certain. Corticosteroids result in a large reduction in length of stay in the intensive care unit (ICU) and in hospital. Corticosteroids increase the risk of muscle weakness and hypernatraemia. They probably increase the risk of hyperglycaemia. They probably do not increase the risk of superinfection. There may be little or no effect of corticosteroids on risk of gastroduodenal bleeding, neuropsychiatric events, stroke, or cardiac events.
• Continuous infusion versus intermittent boluses of corticosteroids.
We are uncertain about the effects of continuous infusion of corticosteroids compared with intermittent bolus administration. Three studies reported data for this comparison, and the certainty of evidence for all outcomes was very low.
Certainty of evidence
• Corticosteroids versus placebo/usual care
We judged the certainty of evidence for 28‐day mortality as moderate due to some inconsistency related to differences among study populations, types of corticosteroids and how they were given, and use of additional interventions.
• Continuous infusion versus intermittent boluses of corticosteroids
We judged the certainty of evidence for 28‐day mortality as very low due to inconsistency and imprecision.
Summary of findings
Summary of findings for the main comparison. Corticosteroids compared to placebo or usual care for treating sepsis.
| Corticosteroids compared to placebo or usual care for treating sepsis | ||||||
| Patient or population: children and adults with sepsis Setting: hospitalised patients; trials were performed in numerous countries from the 5 continents Intervention: corticosteroids Comparison: placebo or usual care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo or usual care | Risk with corticosteroids | |||||
| 28‐Day all‐cause mortalitya | Study population | RR 0.91 (0.84 to 0.99) | 11233 (50 RCTs) | ⊕⊕⊕⊝ Moderateb | Corticosteroids probably slightly reduce 28‐day all‐cause mortality | |
| 264 per 1000 | 240 per 1000 (222 to 261) | |||||
| Long‐term mortalityc | Study population | RR 0.97 (0.91 to 1.03) | 6236 (7 RCTs) | ⊕⊕⊝⊝ Lowb,d | Corticosteroids may result in little to no difference in long‐term mortality | |
| 386 per 1000 | 374 per 1000 (351 to 397) | |||||
| Hospital mortality | Study population | RR 0.90 (0.82 to 0.99) | 8183 (26 RCTs) | ⊕⊕⊕⊝ Moderateb | Corticosteroids probably slightly reduce hospital mortality | |
| 323 per 1000 | 291 per 1000 (265 to 320) | |||||
| Length of intensive care unit stay for all participants in days | Mean length of intensive care unit stay for all participants was 14 days | MD 1.07 lower (1.95 lower to 0.19 lower) | ‐ | 7612 (21 RCTs) | ⊕⊕⊕⊕ Highb,e | Corticosteroids reduced length of intensive care unit stay for all participants |
| Length of hospital stay for all participants in days | Mean length of hospital stay for all participants was 21 days | MD 1.63 lower (2.93 lower to 0.33 lower) | ‐ | 8795 (22 RCTs) | ⊕⊕⊕⊕ Highb,e | Corticosteroids result in a large reduction in length of hospital stay for all participants |
| Number of participants with adverse events ‐ superinfection (up to longest follow‐up) | Study population | RR 1.06 (0.95 to 1.19) | 5356 (25 RCTs) | ⊕⊕⊕⊕ Moderated | Corticosteroids probably do not increase the number of participants with adverse events ‐ superinfection | |
| 169 per 1000 | 180 per 1000 (161 to 202) | |||||
| Number of participants with adverse events ‐ muscle weakness (up to longest follow‐up) | Study population | RR 1.21 (1.01 to 1.44) | 6145 (6 RCTs) | ⊕⊕⊕⊕ High | Corticosteroids increase the number of participants with adverse events ‐ muscle weakness | |
| 56 per 1000 | 68 per 1000 (57 to 81) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; RCT: randomized controlled trial; RR: risk ratio. The unit of measure for length of stay is days. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aSensitivity analysis based on trials judged as being at low risk of bias showed an RR for dying at 28 days of 0.91 (95% CI 0.84 to 0.98; P = 0.01; 7896 participants; 17 studies; I² = 0%).
bDowngraded one level for inconsistency; there was significant statistical heterogeneity.
cLong‐term mortality was recorded up to six months for three trials (Annane 2018; Keh 2016; Venkatesh 2018), and up to one year for four trials (Annane 2002; Briegel 1999; Meduri 2007; Sprung 2008).
dLarge 95% confidence interval overlapping the neutrality line.
eUpgraded one level due to large size effects.
Background
Description of the condition
Sepsis occurs when the host response to an infection is dysregulated (Singer 2016). The dysregulated host response is usually defined by the presence of a sequential organ failure assessment (SOFA) score of 2 or higher (Singer 2016; Vincent 1996). Septic shock is a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with greater risk of mortality than is sepsis alone. Patients with septic shock can be clinically identified by a vasopressor requirement to maintain mean arterial pressure of 65 mmHg or greater and serum lactate levels greater than 2 mmol/L (> 18 mg/dL) in the absence of hypovolaemia. The dysregulated response may result in systemic inflammation and organ damage, or in immune paresis and secondary infection (van der Poll 2017). In 2017, the World Health Organization estimated that around 31 million people develop sepsis each year, and about 10 million die (WHO 2018). According to a recent retrospective cohort study of adult patients admitted to 409 academic, community, and federal hospitals in the USA from 2009 to 2014, sepsis was present in 6% of adult hospitalizations (Rhee 2017). Another study of electronic health records from 27 academic hospitals in the USA reported an annual incidence of septic shock of about 19 per 1000 hospitalizations in 2014 (Kadri 2017). People with sepsis usually die from hypotension or progressive multiple organ failure (Angus 2013; Annane 2003; Annane 2005; Parrillo 1993). There is no current diagnostic test for sepsis. Its standard management includes control of the source of infection with antibiotics and surgery whenever needed, as well as control of tissue oxygenation with fluid replacement, oxygen with or without respiratory support, and vasopressors whenever needed (Rhodes 2017). No specific interventions are yet available to control immune responses to invading pathogens (Rhodes 2017). The financial burden of sepsis on the healthcare system has been calculated to be > 24 billion USD, representing 6.2% of total hospital costs in 2013 (WHO 2018). Studies in Europe and Canada estimated the daily costs of hospital care for a septic patient in 2000 to be between EUR 710 and EUR 1033 (equivalent to about USD 645 and USD 939, respectively) (WHO 2018).
Description of the intervention
Corticosteroids include the natural steroid hormones produced by adrenocortical cells and a broad variety of synthetic analogues. These substances have various effects that may be grossly classified into glucocorticoid and mineralocorticoid effects. Glucocorticoid effects include mainly regulation of carbohydrate, lipid, and protein metabolism, as well as regulation of inflammation. Mineralocorticoid effects include mainly regulation of electrolyte and water metabolism. At molecular levels, glucocorticoids have non‐genomic and genomic effects (Annane 2017a; Cain 2017). Rapid (within minutes) non‐genomic effects of glucocorticoids include a decrease in platelet aggregation, in cell adhesion, and in intracellular phosphotyrosine kinases, and they include an increase in annexin 1 externalization (Lowenberg 2005). These effects may result from the interaction of glucocorticoids with specific membrane sites (Norman 2004). Glucocorticoids have indirect genomic effects, called trans‐repression (Rhen 2005). These occur within a few hours following exposure of cells to glucocorticoids. They result from the physical interaction between the monomeric glucocorticoid‐glucocorticoid receptor (G‐GR)α complex and various nuclear transcription factors, such as nuclear factor (NF)‐κB and activator protein (AP)‐1. Subsequently, these nuclear transcription factors are sequestrated in the cytosol and cannot enter the nucleus, preventing the expression of genes encoding for most if not all pro‐inflammatory mediators. Glucocorticoids also have direct genomic effects, called transactivation. They require only a few days of cell exposure to glucocorticoids. Indeed, conformational changes (i.e. dimerization of the G‐GRα complex) are needed before this complex can migrate to the nucleus to interact with glucocorticoid‐responsive elements, that is, parts of genes encoding for regulators of termination of inflammation. Then, key anti‐inflammatory factors are up‐regulated, leading to phagocytosis, chemokinesis, and anti‐oxidative processes. The net effect of glucocorticoids involves reprogramming rather than inhibiting immune cell function (Erschen 2007). Glucocorticoids induce specific activated anti‐inflammatory monocyte subtypes that migrate quickly to inflamed tissues (Varga 2008). They prolong survival of this subtype of monocyte via A3 adenosine receptor‐triggered anti‐apoptotic effects (Barczyk 2010). Overall, these molecular mechanisms of action of glucocorticoids are appropriate for counteracting the uncontrolled inflammation that may characterize sepsis.
How the intervention might work
Researchers have explored the biological mechanisms of sepsis to investigate potential interventions. Corticosteroids have been a topic of particular focus because of their influence on the immune response (Cain 2017). In sepsis, the hypothalamic‐pituitary gland hormonal pathway to the adrenal glands stimulates corticosteroid production (Annane 2017a; Chrousos 1995; Cooper 2003; Heming 2018). These hormones affect inflammation through the production of white blood cells, cytokines (proteins that influence the immune response), and nitric oxide. In sepsis, cytokines may suppress adrenocorticotropin hormone synthesis (Annane 2017a; Polito 2011; Sharshar 2003), along with the cortisol response to exogenous adrenocorticotropin hormone (Annane 2017a; Hotta 1986; Jaattela 1991). Likewise, sepsis may be associated with alterations in scavenger receptor B1‐mediated cholesterol delivery (Cai 2008). This causes poor adrenal activity in almost half of patients (Annane 2000; Lipiner 2007; Marik 2008; Rothwell 1991), as well as possible resistance of body tissues to corticosteroids due to fewer corticosteroid receptors or receptors with lower affinity (Barnes 1995; Huang 1987; Meduri 1998a; Molijn 1995). Alteration of corticosteroid receptor numbers and in binding capacity may be related at least in part to nitric oxide (Duma 2004; Galigniana 1999). Recent work suggests that immune cells ‐ not steroid‐secreting cells ‐ are key regulators of the interaction between the immune system and the adrenals (Kanczkowski 2013). In addition, acute illness such as sepsis may be associated with decreased cortisol clearance from plasma (Boonen 2013; Melby 1958), likely resulting from altered hepatic and renal inactivation of cortisol (Boonen 2013). Early studies showed that a pharmacological dose of corticosteroids prolonged survival among animals with sepsis (Fabian 1982). More recent studies in rodents have demonstrated that lower doses of corticosteroids, for example, 0.1 mg/kg of dexamethasone, improved haemodynamic and organ function, favourably modulated the inflammatory response, and prolonged survival (di Villa Bianca 2003; Heller 2003; Tsao 2004; Vachharajani 2006). Protective effects of these glucocorticoids against sepsis may be mediated in part by the endothelial glucocorticoid receptor (Goodwin 2013). In healthy volunteers challenged with endotoxin, a low dose of corticosteroids, for example, 10 mg of prednisolone, blocked the release of pro‐inflammatory cytokines, prevented endothelial cell and neutrophil activation, and inhibited the acute phase response without altering coagulation and fibrinolysis balance (de Kruif 2007). Studies in patients with septic shock have shown that a short course of corticosteroids may result in a rebound in the systemic inflammatory response (Briegel 1994; Keh 2003). In addition, it is now recognized that increased pro‐inflammatory cytokine release can be sustained for longer than a week in patients with sepsis (Kellum 2007). Likewise, the timing of initiation of corticosteroids may be an important factor in the response to treatment. Indeed, in observational studies, short‐term mortality increased with delayed initiation of hydrocortisone (Katsenos 2014; Park 2012). For these reasons, we would anticipate that corticosteroid treatment is beneficial for patients with sepsis, and that differences in dose, timing, or duration of corticosteroid treatment may differentially affect patient response to treatment. Finally, several authors have argued that in patients with sepsis, hydrocortisone should be given as a continuous infusion rather than as intermittent boluses to reduce the risk of metabolic complications (Rhodes 2017). In sepsis trials, continuous infusion of hydrocortisone was variably associated with better outcomes or worse outcomes than intermittent intravenous boluses (Loisa 2007; Tilouche 2019).
Why it is important to do this review
Initially, researchers used high doses of corticosteroids, usually given as a single bolus, in an attempt to block potential bursts in pro‐inflammatory cytokines. Two systematic reviews and meta‐analyses of trials of corticosteroids in sepsis or in septic shock included 10 ‐ Lefering 1995 ‐ and nine ‐ Cronin 1995 ‐ randomized controlled trials (RCTs), respectively. These systematic reviews showed no significant effect on relative risk of death, gastrointestinal bleeding, or superinfection associated with the use of corticosteroids.
Subsequently, most clinicians will not recommend the use of high doses of corticosteroids in sepsis (Annane 2017b; Rhodes 2017). The potential benefits of a lower dose (≤ 400 mg hydrocortisone or equivalent per day) and a longer duration at full dose (≥ 3 days) of treatment have been investigated in numerous RCTs over the past three decades (Annane 2017b; Lamontagne 2018; Rochwerg 2018). In the past two years, clinical practice guidelines about corticosteroid use in sepsis have been released by at least five entities (Annane 2017b; Lamontagne 2018; Nishida 2018; Rhodes 2017; Tavaré 2017). All but one of the guidelines ‐ Lamontagne 2018 ‐ recommended against the use of corticosteroids in sepsis, except in patients with septic shock and a poor response to fluid replacement and vasopressor therapy. Some guidelines suggested that corticosteroids should be given as a continuous infusion rather than in intermittent boluses (Annane 2017b; Rhodes 2017). In the year 2018, five different systematic reviews and meta‐analyses addressed the effects of corticosteroids in sepsis (Allen 2018; Fang 2018; Ni 2018; Rochwerg 2018; Rygard 2018). The number of included trials was different in all reviews and ranged from 14 to 42. The risk ratio of death in the short term varied from 0.91 to 0.96, and the upper limit of the 95% confidence interval (CI) varied from 0.98 to 1.03. Another systematic review and meta‐analysis of one randomized trial and 17 observational studies examined the risk of acquired muscle weakness associated with exposure to corticosteroids in patients in the intensive care unit (ICU) (Yang 2018). This review found an odds ratio for acquired muscle weakness of 1.84 (95% CI 1.26 to 2.67) with corticosteroids compared to control.
Therefore, we aim to systematically review the effects of corticosteroids in children and adults with sepsis.
Objectives
To examine the effects of corticosteroids on death in children and adults with sepsis.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) with no methodological restrictions. We excluded quasi‐randomized trials (i.e. trials assigning patients to treatment arms based on systematic methods, such as alternation, assignment based on date of birth, case record number, and date of presentation).
Types of participants
We included children and adults with sepsis as defined by the Sepsis 3 criteria ‐ Singer 2016 ‐ or by the following criteria (ACCP/SCCM 1992; Vincent 2013).
Suspected or documented infection defined as culture or Gram stain of blood, sputum, urine, or normally sterile body fluid that is positive for a pathogenic micro‐organism; or a focus of infection identified by visual inspection (e.g. ruptured bowel with the presence of free air or bowel contents in the abdomen found at the time of surgery; wound with purulent drainage).
At least two symptoms of a systemic inflammatory response syndrome, such as fever (body temperature > 38°C) or hypothermia (< 36°C), tachycardia (> 90 beats per minute), tachypnoea (> 20 breaths per minute), or hyperventilation (arterial carbon dioxide tension (PaCO₂) < 32 mmHg), and abnormal white blood cell count (> 12,000 cells/mL or < 4000 cells/mL) or more than 10% immature band of neutrophils.
At least one sign of organ dysfunction, that is, metabolic acidosis, arterial hypoxaemia (arterial oxygen tension (PaO₂):fractional inspired oxygen (FiO₂) < 250 mmHg), oliguria (< 30 mL/h for ≥ 3 hours), coagulopathy, or encephalopathy.
Septic shock is defined by the presence of sepsis and of hypotension (persisting systolic arterial pressure < 90 mmHg) that is refractory to fluid resuscitation and requires vasopressor support (i.e. > 5 µg/kg of body weight per minute of dopamine or any dose of epinephrine or norepinephrine).
We included data from trials of community‐acquired pneumonia or acute respiratory distress syndrome (ARDS) when separate data were available for participants with sepsis, or when contact with study authors resulted in provision of the data.
Types of interventions
Corticosteroids versus placebo/usual care
Intervention
Systemic treatment was provided as any type of corticosteroid preparation (e.g. cortisone, hydrocortisone, methylprednisolone, betamethasone, dexamethasone).
Low‐dose corticosteroid treatment was defined by a total dose per day of 400 mg or less of hydrocortisone (or equivalent); otherwise, the dose of corticosteroid would be considered high. A long course for the intervention was defined by a full‐dose treatment duration of three or more days; otherwise, treatment was considered as a short course.
Control
Standard therapy was provided, which may have included antibiotics, fluid replacement, inotropic or vasopressor therapy, mechanical ventilation, or renal replacement therapy, or placebo.
Continuous infusion versus bolus administration of corticosteroids
Intervention
Continuous infusion was defined by intravenous infusion of corticosteroids with or without an initial loading dose.
Control
Bolus administration was defined by intermittent intravenous injections with duration less than 30 minutes.
Types of outcome measures
Primary outcomes
28‐Day all‐cause mortality
Indeed, this was the primary outcome measure in most of the RCTs on sepsis conducted since 1992 (Annane 2009b). Most studies performed before 1992 looked at 14‐day or hospital mortality rates. We used these data to compute the pooled analysis for 28‐day mortality, unless we could obtain actual 28‐day mortality rates from primary study authors.
Secondary outcomes
90‐Day all‐cause mortality
This was the primary outcome in the two most recent and largest trials on corticosteroids for sepsis.
Long‐term (longest available follow‐up beyond three months) all‐cause mortality
ICU all‐cause mortality
Hospital all‐cause mortality
In‐ICU and in‐hospital mortality outcomes provide the location of death, which adds context to the primary outcome.
Number of participants with shock reversal (as defined by stable haemodynamic status ≥ 24 hours after withdrawal of vasopressor therapy) at day seven and at day 28
Number of organs affected and severity of organ dysfunction at day seven, in individual patients, as measured by the SOFA score (Vincent 1996). This score scales from 0 (normal function) to 4 (most severe) the dysfunction of six organ systems (Respiration, Coagulation, Liver, Cardiovascular, Central nervous system, Renal). It ranges from 0 (no organ failure) to 24 (most severe organ dysfunction)
Length of stay in the ICU (for all participants and for survivors only). This outcome is expressed in mean (standard deviation (SD)) number of days, and is calculated by the difference between dates of ICU discharge and ICU admission, with first and last days of ICU stays counted as full ICU days regardless of the time of admission and time of discharge
Length of hospital stay (for all participants and for survivors only). This outcome is expressed in mean (SD) number of days, and is calculated by the difference between dates of hospital discharge and hospital admission, with first and last days of hospital stays counted as full hospital days regardless of time of admission and time of discharge
Adverse events (i.e. gastrointestinal bleeding, superinfection, hyperglycaemia, hypernatraemia, muscle weakness, neuropsychiatric events, stroke, cardiac events, or any other adverse effects or complications of corticosteroid treatment). Each adverse event is expressed as the number (%) of patients with at least one episode of this event, as defined in individual studies, except for hyperglycaemia and hypernatraemia. Whenever possible, hyperglycaemia was defined by values > 180 mg/dL, and hypernatraemia by values > 149 mmol/L.
Search methods for identification of studies
We attempted to identify all relevant studies regardless of language or publication status (e.g. published, unpublished, in press, in progress).
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2019 Issue 7), in the Cochrane Library, using the search terms 'sepsis', 'septic shock', 'steroids', and 'corticosteroids' (for the detailed search strategy, see Appendix 1).
We also searched (to 25 July 2019) MEDLINE ALL (Ovid SP), Embase (Ovid SP), and Latin American Caribbean Health Sciences Literature (LILACS), using the topic search terms in combination with the search strategy for identifying trials developed by Cochrane (Higgins 2011). (For detailed search strategies, see Appendix 2 (MEDLINE), Appendix 3 (Embase), and Appendix 4 (LILACS).)
Finally, we searched for ongoing RCTs (to 25 July 2019) at ClinicalTrials.gov, International Standard Randomized Controlled Trials Number (ISRCTN), and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP), using the search terms 'septic shock', 'sepsis', steroids', 'corticosteroids', 'adrenal cortex hormones', and 'glucocorticoids'.
Searching other resources
We checked the reference lists and citations of all trials and relevant systematic reviews identified by the electronic searches, and we contacted study authors to request additional published or unpublished data. We also searched the proceedings of annual meetings of major critical care medicine symposia, that is, Society of Critical Care Medicine, American Thoracic Society, International Symposium on Intensive Care and Emergency Medicine, American College of Chest Physicians, and European Society of Intensive Care Medicine (1998 to 2019).
Data collection and analysis
Selection of studies
All review authors checked the titles and abstracts identified during the search. All review authors examined, in full, any trial that potentially met the inclusion criteria. We decided which trials met the inclusion criteria. We resolved disagreements between review authors by discussion until we reached consensus. Review authors did not contribute to the decision for inclusion of trials in which they had participated.
One review author (DA) contacted study authors for clarification, when necessary.
Data extraction and management
One review author (DA) drew up a standard data extraction form, and four other review authors (PEB, JB, DK, YK) amended and validated the design of the form before data abstraction. Review authors (DA, PEB, JB, DK, RP, BR) independently extracted data, except those from trials in which they had participated.
One review author (DA) systematically contacted the authors of trials to request missing data when possible.
One review author (DA) and one member of this author’s research staff independently extracted and entered data into the computer. All review authors checked the accuracy of data entered against the original articles.
Assessment of risk of bias in included studies
We assessed risk of bias within individual trials as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We considered the following domains: selection bias, performance bias, detection bias, attrition bias, reporting bias, and any other bias. We judged selection bias on the basis of how the random sequence was generated, and how allocation was concealed. We judged performance bias and detection bias on the basis of who was blinded and how, among participants, caregivers, pharmacists, data collectors, outcome assessors, and data analysts (Devereaux 2001). In judging attrition bias, we considered how many participants were lost to follow‐up or were not included in analyses (and the reasons why). When available, we compared outcomes reported in trial protocols versus actual results reported, to identify potential selective reporting bias. We resolved disagreements between review authors by discussion until we reached consensus.
One review author (DA) contacted study authors for clarification, when necessary.
We assessed, independently and in duplicate (two of DA, BR, or RP), for each outcome of individual studies using a modified Cochrane risk of bias tool (Guyatt 2013), which classifies risk of bias as "low", "probably low", "probably high", or "high" for each of the following domains: sequence generation, allocation sequence concealment, blinding, selective outcome reporting, and other bias. We rated the overall risk of bias as the highest risk attributed to any criterion.
Review authors did not contribute to the assessment of risk of bias of any trial in which they had participated.
Measures of treatment effect
We performed intention‐to‐treat (ITT) analyses. We performed all statistical calculations using Review Manager 2014 or Stata 2015, as appropriate
We calculated a weighted treatment effect across trials. We expressed results as risk ratios (RRs) with 95% confidence intervals (CIs) for dichotomous outcomes, and as mean differences (MDs, 95% CIs) for continuous outcomes
Unit of analysis issues
In this review, we used data from trials in which the unit of randomization was the individual, and in which parallel groups were designed. For events that may occur repeatedly, such as receiving vasopressor therapy or staying in the ICU, we used only the first occurrence of the event.
When trials included more than two arms (e.g. comparing vs control two different corticosteroids or two different modes of administration of the same corticosteroid), we pooled data from the experimental arms for comparison of steroids versus control.
Dealing with missing data
We systematically tried to contact primary authors of original trials to obtain missing information and unpublished data. We obtained additional data from primary authors of 28 trials, including access to individual patient data for 16 trials (Appendix 5). This information is provided for each trial in the notes section of Characteristics of included studies.
For the primary outcome of this review (28‐day all‐cause mortality), we systematically contacted trial authors when needed to obtain data for participants who dropped out. When trials did not report 28‐day all‐cause mortality, and contact with trial authors failed to yield actual 28‐day mortality rates, we used available mortality data closest to 28 days.
When trials reported length of stay in the ICU or in hospital only as median and interquartile ratio (IQR), and when contact with trial authors failed to elicit means and SDs, we did not include these trials in the analysis.
Assessment of heterogeneity
We considered that evidence for significant heterogeneity was present when I² > 30%.
Assessment of reporting biases
We sought evidence of publication bias by using the funnel plot method. We used Stata 2015 to prepare a contour‐enhanced funnel plot (Peters 2008). This graphical analysis used the standard error of the log of the RR. We plotted contours illustrating the statistical significance of study effect estimates by using a two‐tailed test.
Data synthesis
We considered methods based on the random‐effects model for all analyses, except when we found no evidence for significant heterogeneity in the results (i.e. I² ≤ 30%). Indeed, we suspected that we would observe heterogeneity across studies, as they were conducted over a wide period of time (almost half a century between first and last trials) and the rationale on which studies were designed varied greatly over time, with marked differences in treatment strategies and in populations between studies conducted before and after the early 1990s.
Subgroup analysis and investigation of heterogeneity
To identify potential sources of heterogeneity, we sought, a priori, to conduct a subgroup analysis based on 'dose and duration', that is, a long course (≥ 3 days at full dose) of low‐dose (≤ 400 mg/d) hydrocortisone or equivalent. This subgroup analysis allowed evaluation of a strategy based on developments in our understanding of the role of corticosteroids in host response to sepsis, as tested in trials performed after 1992. Older trials used most often a short course (one to four bolus doses within 24 hours) of high‐dose corticosteroids (> 400 mg of hydrocortisone or equivalent), and trials conducted after 1992 used most often low‐dose corticosteroids at full dose over a longer period (≥ 3 days).
We also conducted a subgroup analysis based on the type of corticosteroids, the method of corticosteroid administration, intravenous bolus versus continuous infusion, and termination without versus with tapering off. To further explore the putative interaction between corticosteroid dose and duration and the magnitude of effect, we considered performing a meta‐regression analysis using 28‐day all‐cause mortality as the dependent variable, and dosage and duration of corticosteroids as predictors. We performed meta‐regression analyses using Stata 2015. We also tested, a priori, the interaction between baseline severity of illness and magnitude of effect in a meta‐regression analysis using mortality rates in controls as predictors. Finally, we conducted a subgroup analysis based on targeted population, sepsis, only septic shock, sepsis with ARDS, community‐acquired pneumonia, and sepsis with critical illness‐related corticosteroid insufficiency (Annane 2017a).
-
We assessed the validity of subgroup analyses on the basis of the following criteria.
Subgroup comparisons within rather than between studies.
Hypothesis preceding the analysis.
One of very few hypotheses.
Large and consistent differences across studies.
External evidence supporting the results (Guyatt 2008b).
When subgroup analyses met these criteria and were found to be statistically significant, we applied GRADE criteria to evaluate the certainty of evidence (GRADEpro GDT 2015; Guyatt 2008a).
Sensitivity analysis
We conducted sensitivity analyses based on generation of allocation sequence, concealment of allocation, and blinding, and for trials judged at low risk of bias.
'Summary of findings' table and GRADE
For assessment of the overall certainty of evidence for each outcome that included pooled data from RCTs only, we downgraded the evidence from "high certainty" by one level for serious (or by two for very serious) study limitations (according to risk of bias evaluation), indirectness of evidence, serious inconsistency (i.e. when I² > 30%), imprecision of effect estimates (large 95% confidence intervals or small treatment effects), or potential publication bias.
We exported data from Review Manager 5 to GRADEpro GDT 2015 to create 'Summary of findings' tables. We included the following patient‐centred outcomes in the 'Summary of findings' tables.
28‐Day all‐cause mortality.
In‐hospital all‐cause mortality.
Long‐term (longest follow‐up beyond three months) all‐cause mortality.
Length of stay in the ICU.
Length of hospital stay.
Number of participants with superinfection up to longest follow‐up.
Number of participants with muscle weakness up to longest follow‐up.
Results
Description of studies
Results of the search
Our search results are detailed in Figure 1.
1.
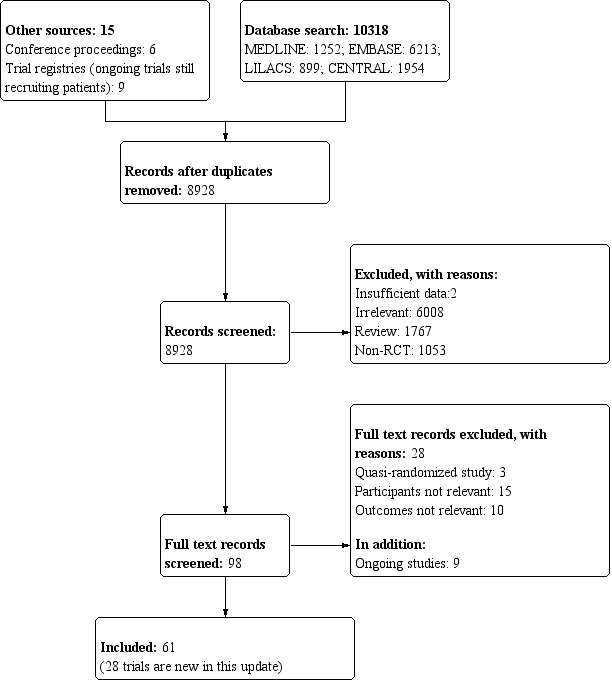
Study flow diagram.
The search strategy yielded 98 trials that evaluated corticosteroids in sepsis, of which we excluded 28 trials (see Characteristics of excluded studies). Nine trials are still ongoing (see Characteristics of ongoing studies).
Included studies
Since the last update in 2015 (see Published notes), we have included 28 additional trials for a total of 61 trials (n = 12,192 participants); we have described these below (see Characteristics of included studies).
Source of information
In addition to data extracted from these publications, we obtained unpublished information from 28 trials by contacting the primary authors (Appendix 5). We did not contact the authors of 10 trials, mainly because of the absence of contact details (Characteristics of included studies). For the remaining trials, contact with study authors did not lead to the provision of additional information (Characteristics of included studies).
Trial centres
Twenty trials were multi‐centre trials (i.e. > 2 centres) (Characteristics of included studies). Twenty‐four trials were conducted in Europe, 11 in North America, 12 in Asia, five in the Middle East, five in Africa, and one in Latin America, and three multi‐national trials were conducted in North America and Africa (Slusher 1996), in Europe and the Middle East (Sprung 2008), and in Australia, New Zealand, Europe, and the Middle East (Venkatesh 2018) (Characteristics of included studies).
Age of participants
Two trials enrolled both children and adults (CSG 1963; McHardy 1972). Six trials included only children (El‐Nawawy 2017; Menon 2017; Nagy 2013; Slusher 1996; Tagaro 2017; Valoor 2009). All of the remaining trials included only adults.
Description of participants
Eleven trials included both participants with sepsis and individuals with septic shock. Four trials included participants with sepsis without shock (Fernández‐Serrano 2011; Keh 2016; Rinaldi 2006; Sabry 2011). Fifteen trials targeted participants with community‐acquired pneumonia‐related sepsis. Five trials focused on participants with ARDS and sepsis (Liu 2012; Meduri 2007; Rezk 2013; Tongyoo 2016; Zhou 2015). The remaining trials focused on participants with septic shock treated by a vasopressor. Three trials included only participants with septic shock and adrenal insufficiency as defined by a cortisol increment less than 9 µg/dL after a corticotropin bolus (Aboab 2008; Huh 2007; Tandan 2005). In 18 trials, investigators systematically performed a short corticotropin test at baseline.
Control
Comparison of corticosteroids versus placebo or usual care
Nine studies did not use a placebo and compared corticosteroid therapy versus usual care, that is, antibiotics, fluid resuscitation, and vasopressor when needed (El Ghamrawy 2006; Hu 2009; Huang 2014; Li 2016; McHardy 1972; Mirea 2014; Rinaldi 2006; Sui 2013; Zhou 2015). In one study, only one centre used a placebo (Sprung 1984). One trial that compared hydrocortisone versus hydrocortisone plus fludrocortisone did not use a placebo of fludrocortisone for technical reasons (Annane 2010). Another trial compared duration of hydrocortisone treatment (i.e. 3 days vs 7 days) and did not use a placebo (Huh 2007). The remaining trials compared corticosteroid therapy to placebo.
Comparison of continuous infusion versus intermittent intravenous boluses of corticosteroids
Three trials compared continuous infusion versus bolus administration of hydrocortisone (Hyvernat 2016; Loisa 2007; Tilouche 2019). One trial had three parallel arms including continuous infusion of 200 mg hydrocortisone daily for seven days, intravenous bolus of 50 mg hydrocortisone every six hours for seven days, and usual care (Mirea 2014).
Corticosteroid dose and treatment course
Thirty‐seven trials tested the effects of a long‐course (three or more days at full dose) of low‐dose hydrocortisone. In one trial (Huh 2007), investigators compared hydrocortisone 50 mg intravenously every six hours when given for three days versus seven days. One trial had three parallel groups including continuous infusion of 200 mg hydrocortisone per day for seven days, intravenous bolus of 50 mg hydrocortisone every six hours for seven days, and usual care (Mirea 2014). In three trials, investigators compared continuous infusion versus intermittent intravenous boluses of hydrocortisone (Hyvernat 2016; Loisa 2007; Tilouche 2019). Another trial compared seven‐day treatment with hydrocortisone versus seven‐day treatment with the combination of hydrocortisone plus fludrocortisone (Annane 2010). One trial compared a short course (two days at full dose) of low‐dose intravenous hydrocortisone (300 mg on day one and 250 mg on day two) versus placebo (CSG 1963). Another study used a cross‐over design to compare a three‐day course of low‐dose hydrocortisone versus placebo (Keh 2003).
Five trials tested the effects of a long course of low‐dose prednisone or prednisolone (Blum 2015; McHardy 1972; Snijders 2010; Yildiz 2002; Yildiz 2011).
Two trials tested the effects of a long course of low‐dose dexamethasone (Cicarelli 2007; Meijvis 2011). Two trials tested the effects of a short course (two days at full dose) of low‐dose dexamethasone (Slusher 1996; Tagaro 2017).
Eight studies tested the effects of a long course of low‐dose intravenous methylprednisolone (Fernández‐Serrano 2011; Li 2016; Meduri 2007; Nagy 2013; Rezk 2013; Sui 2013; Torres 2015; Zhou 2015).
Five trials tested the effects of a short course of a large dose of methylprednisolone (Bone 1987; Luce 1988; Schumer 1976; Sprung 1984; VASSCSG 1987), and two tested the effects of a large dose of dexamethasone (Schumer 1976; Sprung 1984).
One trial did not report the type of corticosteroids given (Kurungundla 2008).
Outcomes
Overall, data from 52 trials was used to inform 28‐day mortality rates. One trial (Mirea 2014) provided data for both comparison of corticosteroids versus placebo or usual care and comparison of continuous infusion versus bolus administration of corticosteroids. Two trials ( Hyvernat 2016;Tilouche 2019) provided data for the comparison of continuous infusion versus bolus administration of corticosteroids. Fifty trials were used in the comparison of corticosteroids versus placebo or usual care. Of these trials, 29 explicitly reported on 28‐day mortality and contact with the primary author of three additional trials led to recording of 28‐day mortality rates (Meduri 2007; Rinaldi 2006; Sprung 1984). Thus, actual 28‐day mortality rates were computed for 32 trials. For 18 additional trials, 28‐day mortality rates were extrapolated from hospital mortality rates (Aboab 2008, El Ghamrawy 2006,Fernández‐Serrano 2011, Luce 1988, McHardy 1972, Menon 2017,Nafae 2013, Schumer 1976, Slusher 1996, Torres 2015), ICU mortality rates (Hu 2009, Sabry 2011), 14‐day mortality rates (Bone 1987, VASSCSG 1987), and short term mortality rates (Kurungundla 2008, Mirea 2014, Nagy 2013, Rezk 2013).
Sixteen trials explicitly reported ICU mortality rates, and the primary authors of three additional trials reported this outcome (Chawla 1999; Rinaldi 2006; Torres 2015).
Hospital mortality rates were available for 26 trials.
Mortality rates at 90 days and in the long term were reported for seven trials.
Rates of shock reversal at day seven and at day 28 were reported in 16 and 13 trials, respectively.
Ten trials reported the numbers of dysfunctional organs, that is, SOFA scores, at day seven.
Twenty‐one trials reported length of ICU stay, and 22 reported on length of hospital stay.
Excluded studies
We excluded 28 trials (see Characteristics of excluded studies for details).
Ongoing studies
From trial registries, we identified nine additional RCTs of corticosteroids for sepsis (see Characteristics of ongoing studies). These trials are still recruiting patients, and we will follow the status of these trials to include them in a future update of the review whenever data become publicly available.
Studies awaiting classification
We found no studies awaiting classification
Risk of bias in included studies
We reported the detailed methodological quality of individual trials in the 'Risk of bias' tables in Figure 2 and Appendix 6.
2.
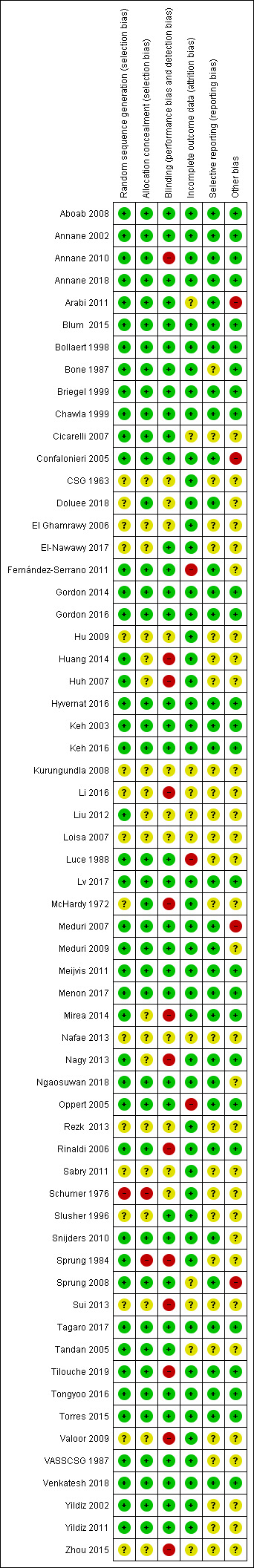
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
We judged 19 trials as being at low risk of bias, that is, we assessed them as having low risk of bias for the five domains (allocation, blinding, incomplete data, selective reporting, and other potential sources of bias).
Allocation
Random sequence generation
In one trial, the method of generation of allocation sequence was based on a card system (Schumer 1976); we judged this trial to be at high risk of selection bias. For 16 trials, the method was unclear. We judged the remaining trials to have low risk of bias.
Allocation concealment
We judged the method used for allocation concealment to be at low risk of bias in all but 10 trials. One trial assigned treatment using unsealed envelopes (Schumer 1976). In another trial, investigators enrolling participants at one of the two participating centres could have foreseen the upcoming assignment, as the local ethical committee refused to accept concealed allocation (Sprung 1984). In 20 trials, study authors did not report the method used for allocation concealment.
Blinding
Blinding of participants and personnel
For 13 trials, we judged the method used for blinding of participants and personnel as having high risk of bias. Twelve trials used open‐label treatments. For one trial (Sprung 1984), the local ethical committee at one of the two centres did not permit double‐blind allocation and administration of treatment. Therefore, blinding was not possible for 40 of the 59 participants included in the trial.
Eleven additional trials did not report the method used to ensure blinding.
For the remaining trials, blinding of participants and personnel was deemed appropriate. We judged these trials to be at low risk of bias for this domain.
Blinding of outcomes assessors
In 12 trials, outcome assessors were not blinded to study treatments. We judged these trials to be at high risk of detection bias.
Twelve trials did not report any information that could be used to judge the risk of detection bias.
For the remaining trials, blinding of outcomes assessors was deemed appropriate. We judged these trials to be at low risk of bias for this domain.
Incomplete outcome data
Twenty‐eight trials explicitly provided the numbers of and reasons for withdrawals or losses to follow‐up.
Nineteen trials explicitly reported the use of intention‐to‐treat analysis (as the primary analysis) and the numbers of, and reasons for, non‐adherence to the protocol. One trial reported only use of intention‐to‐treat analysis (Luce 1988). The remaining trials provided no information about these criteria. However, the number of analysed participants matched the number of randomly assigned participants, except for 16 trials. One trial did not include one of 191 participants in the placebo group in the mortality analysis (Bone 1987). In four trials (Annane 2002; Lv 2017; Sprung 2008; Tongyoo 2016), participants withdrew their consent, and study authors did not include in the analyses one of 300, two of 120, one of 500, and nine of 206 randomly assigned participants, respectively. For two trials, contact with the primary author allowed us to obtain information on participants who were dropped out from the analysis (Oppert 2005; Rinaldi 2006). In the first study, seven randomly assigned participants (five in the corticosteroid group and two in the placebo group) were not analysed (Oppert 2005). Four of these participants (two in the corticosteroid group and two in the placebo group) were discharged alive from the ICU and then were lost to follow‐up. The three remaining participants (in the corticosteroid group) died: two before receiving hydrocortisone, and the last at study day 17. In the second study, 12 of 52 participants dropped out of the study: six in the control group and six in the corticosteroid group (Rinaldi 2006). Nine participants (four in the control group) were excluded, as they developed renal failure. Two control participants died in the ICU at day five and at day seven, respectively. Three of the corticosteroid‐treated participants died, at days 5, 6, and 28, respectively. Three other participants (two in the control group) were excluded, as they developed septic shock. All died at days 3, 5, and 6, respectively.
Two trials gave additional open‐label corticosteroids to some participants (Gordon 2014; Snijders 2010). In the first trial, five (23.3%) participants in the placebo arm were given rescue corticosteroids for treatment of life‐threatening hypotension and were considered as cross‐overs (Gordon 2014). In the second trial, 37 (17.4%) participants did not complete the full course of study treatment as a consequence of premature death of 10 participants, consent withdrawal for five participants, post‐randomization exclusion for eight participants, and additional open‐label corticosteroid treatment for 14 participants (Snijders 2010). In seven trials, from 4% to 20% were withdrawn from the primary analysis for various reasons that were explained in the trial report (Blum 2015; Fernández‐Serrano 2011; Keh 2016; Gordon 2016; Menon 2017; Tilouche 2019; Venkatesh 2018).
Selective reporting
For 34 trials, we could rule out selective reporting bias after contact with authors, full access to trial protocols, or access to individual participant data. We judged these trials to be at low risk of bias for this domain.
Seventeen trials were published before it was mandatory to register trials in an open access repository, and we have had no access to trial protocols. We judged these trials as having unclear risk of selective reporting bias. For the remaining trials, we could not obtain access to protocols, we could not find trials on an open access registry, and our attempts to contact trial authors failed.
Other potential sources of bias
One trial recruited only 500 of the 800 expected participants, mainly as the result of loss of equipoise among investigators (Sprung 2008). Another trial was halted prematurely for futility after enrolment of 75 of 150 foreseen participants (Arabi 2011).
No trials used the Sepsis 3 definition as all were designed before publication of the new definition for sepsis (Singer 2016). Thirty trials provided an explicit definition of sepsis (as defined in the Methods section of this review). Seven trials provided a definition of septic shock without referring to the need for vasopressor agents (Bone 1987; Luce 1988; Rinaldi 2006; Schumer 1976; Slusher 1996; VASSCSG 1987; Yildiz 2002). One study did not explicitly provide the definition used for sepsis (CSG 1963). Eleven trials explicitly defined sepsis due to community‐acquired pneumonia. Two trials randomly assigned participants on the basis of the presence of ARDS, and data provided in these papers confirmed the presence of sepsis (Liu 2012; Rezk 2013). In another trial on early ARDS, contact with the primary author confirmed that explicit definitions of sepsis were used (Meduri 2007).
Effects of interventions
See: Table 1
We did not pool the data from one trial that included both children and adults (CSG 1963), one cross‐over trial (Keh 2003), one trial that compared two durations of hydrocortisone treatment (Huh 2007), and one trial that compared hydrocortisone versus the combination of hydrocortisone plus fludrocortisone (Annane 2010).
In this update, we introduced a new comparison (i.e. continuous infusion vs intermittent boluses of steroids).
Corticosteroids versus placebo or usual care
We have summarized the main results in Table 1.
Primary outcome
28‐Day all‐cause mortality
Data for 28‐day mortality were available for 32 trials. In addition, we used data on 14‐day mortality (two trials), hospital mortality (10 trials), or ICU mortality (2 trials), or data on short‐term mortality (four trials). Thus, we computed data from 50 trials that accounted for 11,233 participants. In the treated group, 1388 of 5667 participants died by day 28 compared with 1469 of 5566 participants in the control group. Some heterogeneity was evident in the results (Chi² test = 68.06; P = 0.03; I² = 29%). The risk ratio (RR) of dying at 28 days was 0.91 (95% confidence interval (CI) 0.84 to 0.99; P = 0.04; random‐effects model; Analysis 1.1). We downgraded the certainty of evidence for this outcome from high to moderate for inconsistency (significant heterogeneity across trial results).
1.1. Analysis.
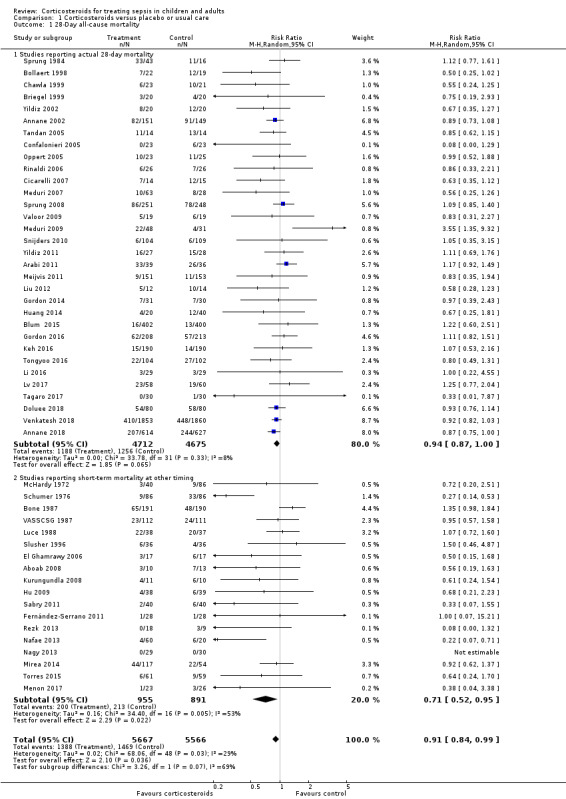
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 1 28‐Day all‐cause mortality.
Differences in methodological quality across trials may have accounted for observed heterogeneity in the results. A sensitivity analysis based on trials judged as being at low risk of bias showed an RR for dying at 28 days of 0.91 (95% CI 0.84 to 0.98; P = 0.01; 7896 participants; 17 studies; I² = 0%; Analysis 1.2).
1.2. Analysis.
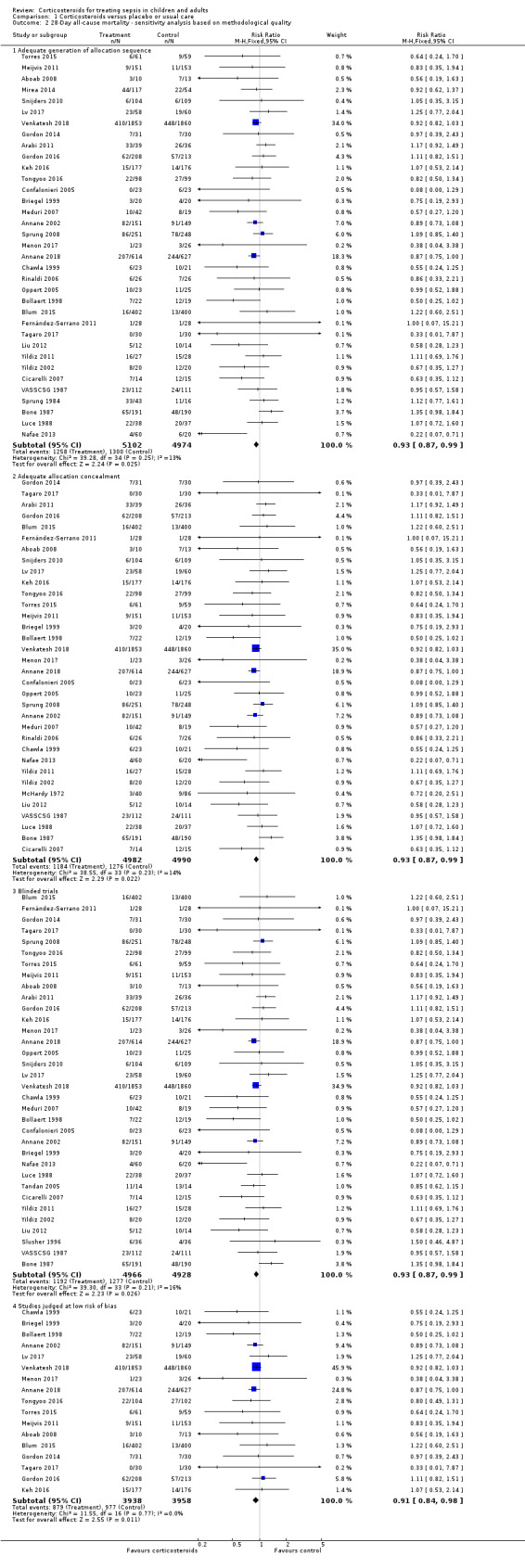
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 2 28‐Day all‐cause mortality ‐ sensitivity analysis based on methodological quality.
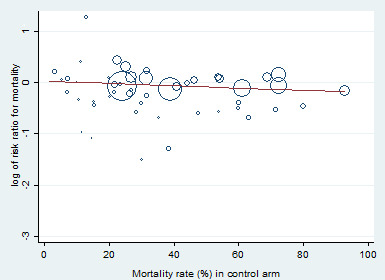
Heterogeneity across trials also may have been the result of different therapeutic regimens. Subgroup analyses based on types of corticosteroids did not suggest that this may influence the response to treatment (test for subgroup differences: Chi² = 1.48; df = 3; P = 0.69; I² = 0%; Analysis 1.3). Likewise there was no evidence that dose/duration (test for subgroup differences: Chi² = 0.29; df = 1; P = 0.59; I² = 0%; Analysis 1.4) or mode (continuous vs intermittent bolus) of corticosteroid administration (test for subgroup differences: Chi² = 0.41; df = 1; P = 0.52; I² = 0%; Analysis 1.5) influences the response to treatment. Meta‐regression analyses showed no evidence of interaction between the RR for dying at 28 days and the dose given at day 1 (P = 0.14; Figure 3), total dose (P = 0.12; Figure 4), or duration of treatment (P = 0.86). One trial of a large dose of corticosteroids was a statistical outlier and was excluded from the meta‐regression analysis (Schumer 1976).
1.3. Analysis.
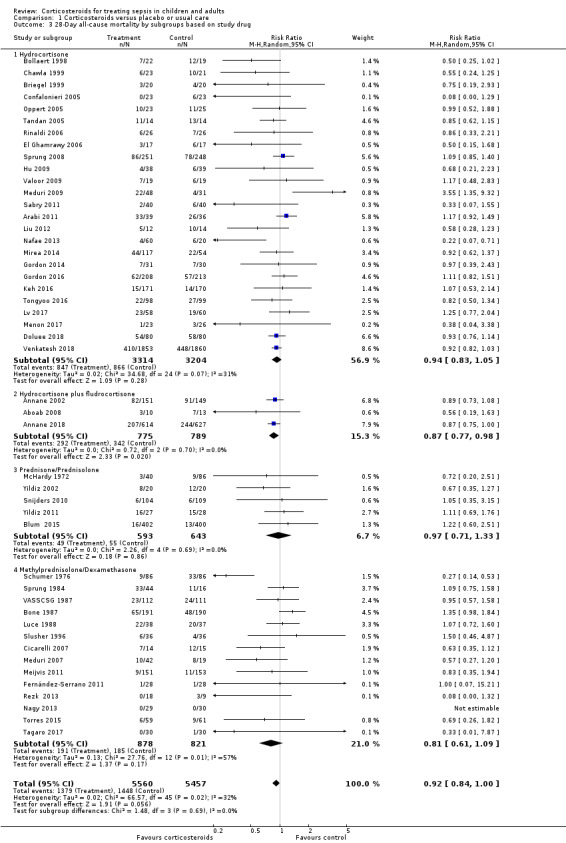
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 3 28‐Day all‐cause mortality by subgroups based on study drug.
1.4. Analysis.
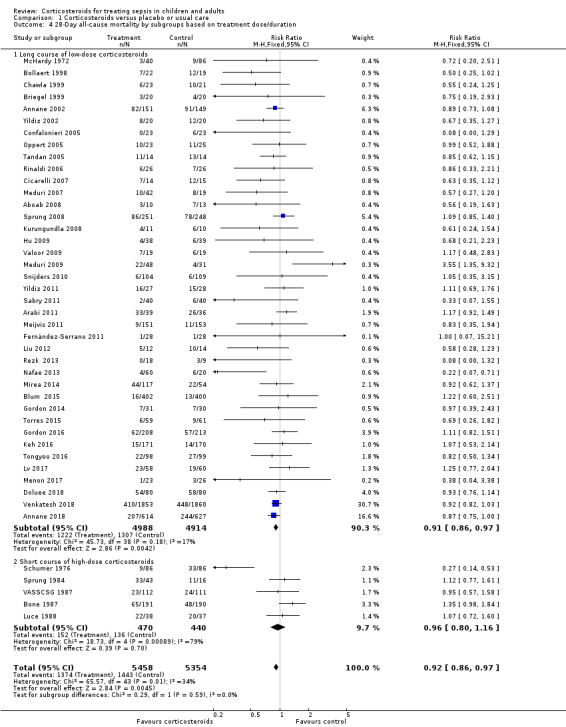
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 4 28‐Day all‐cause mortality by subgroups based on treatment dose/duration.
1.5. Analysis.
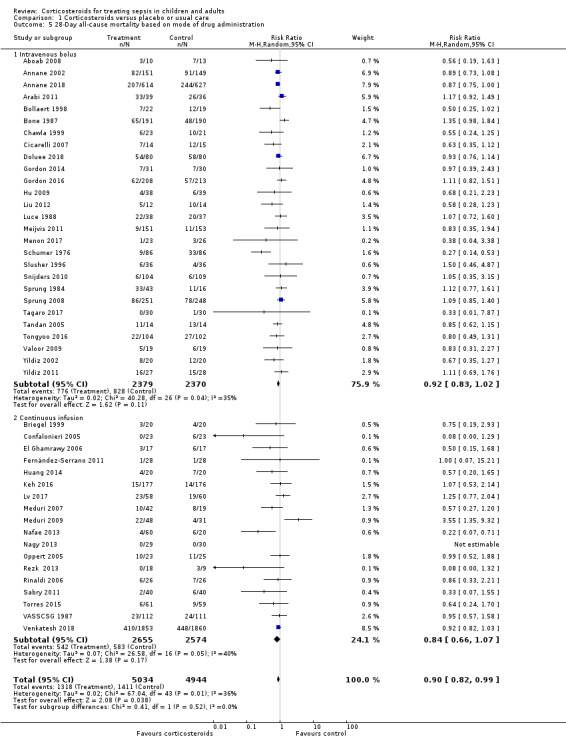
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 5 28‐Day all‐cause mortality based on mode of drug administration.
3.
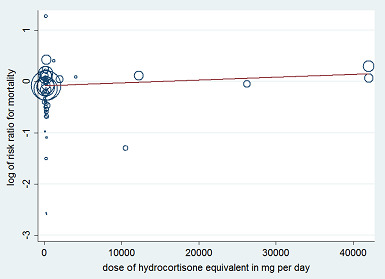
Figure represents the results from meta‐regression of log of risk ratio of dying and the dose of corticosteroids given at day 1 and expressed as equivalent milligrams of hydrocortisone. Estimates from each study are represented by circles. Circle sizes depend on the precision of each estimate (the inverse of its within‐study variance), which is the weight given to each study in the fixed‐effect model.
Meta‐regression included 53 trials.
REML estimate of between‐study variance: tau² = .008551. % residual variation due to heterogeneity: I² res = 28.86%. Proportion of between‐study variance explained: Adj R² = 43.76%.
4.
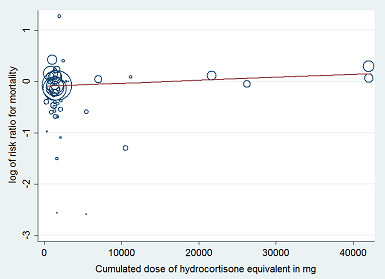
Figure represents results from meta‐regression of log of risk ratio of dying and log of cumulated dose of corticosteroids expressed as equivalent milligrams of hydrocortisone. Estimates from each study are represented by circles. Circle sizes depend on the precision of each estimate (the inverse of its within‐study variance), which is the weight given to each study in the fixed‐effect model.
Meta‐regression included 53 trials.
REML estimate of between‐study variance: tau² = .008628. % residual variation due to heterogeneity: I² res = 28.68%. Proportion of between‐study variance explained: Adj R² = 43.25%.
By contrast, trials in which corticosteroids were not tapered off found an RR of dying at 28 days of 0.87 (95% CI 0.78 to 0.98; 8770 participants; 30 studies; I² = 42%; random‐effects model) in favour of corticosteroids, whereas trials in which corticosteroids were tapered off found no evidence of mortality differences between groups (RR 1.04, 95% CI 0.92 to 1.18; P = 0.54; 2136 participants; 17 studies; I² = 0%) (test for subgroup differences: Chi² = 3.94; df = 1; P = 0.05; I² = 74.6%; Analysis 1.6).
1.6. Analysis.
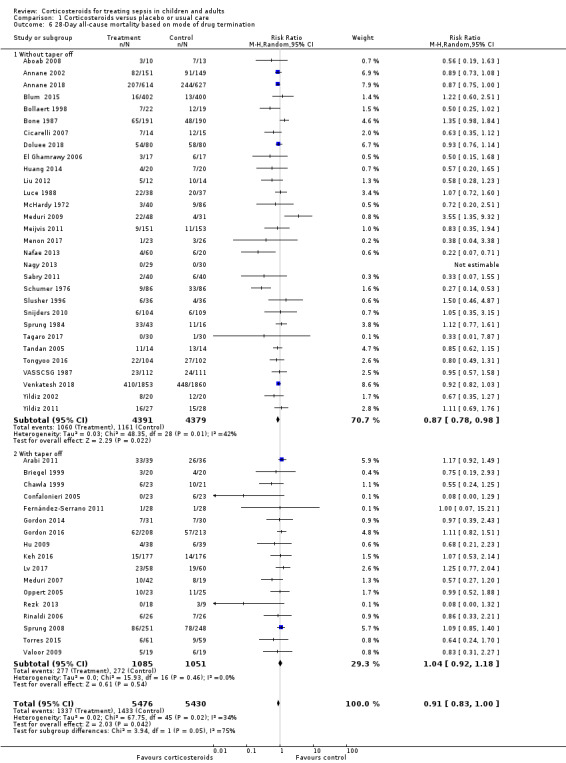
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 6 28‐Day all‐cause mortality based on mode of drug termination.
Heterogeneity across trials may have resulted from factors related to participants. There was no evidence of differences in response to treatment between children and adults (test for subgroup differences: Chi² = 0.29; df = 1; P = 0.62; I² = 0%; Analysis 1.7). Subgroup analysis based on targeted populations showed non‐significant subgroup differences (test for subgroup differences: Chi² = 7.60; df = 3; P = 0.06; I² = 60.5%; Analysis 1.8). In studies of heterogeneous populations of participants with sepsis, the RR for dying at 28 days was 1.17 (95% CI 0.98 to 1.39; P = 0.09; 1358 participants; 10 studies; I² = 25%; fixed‐effect model). In studies of only participants with septic shock, the RR for dying at 28 days was 0.91 (95% CI 0.83 to 1.00; P = 0.06; 7428 participants; 23 studies; I² = 32%; random‐effects model). In studies of participants with sepsis and ARDS, the RR was 0.66 (95% CI 0.46 to 0.94; P = 0.02; 411 participants; 4 studies; I² = 8%; fixed‐effect model), and in studies of participants with sepsis and community‐acquired pneumonia, the RR was 0.69 (95% CI 0.50 to 0.96; P = 0.03; 2038 participants; 13 studies; I² = 0%; fixed‐effect model). Likewise, meta‐regression showed no evidence of interaction between the RR of dying at 28 days and severity of illness as assessed by crude mortality in the control arm (P = 0.29; Figure 5). Subgroup analysis of participants with adrenal insufficiency showed no heterogeneity in the results. Investigators reported 251 deaths among 525 participants in the treated group and 291 deaths among 554 in the placebo group. The RR for dying was 0.92 (95% CI 0.82 to 1.03; P = 0.16; 1079 participants; 12 studies; I² = 0%; fixed‐effect model; Analysis 1.9).
1.7. Analysis.
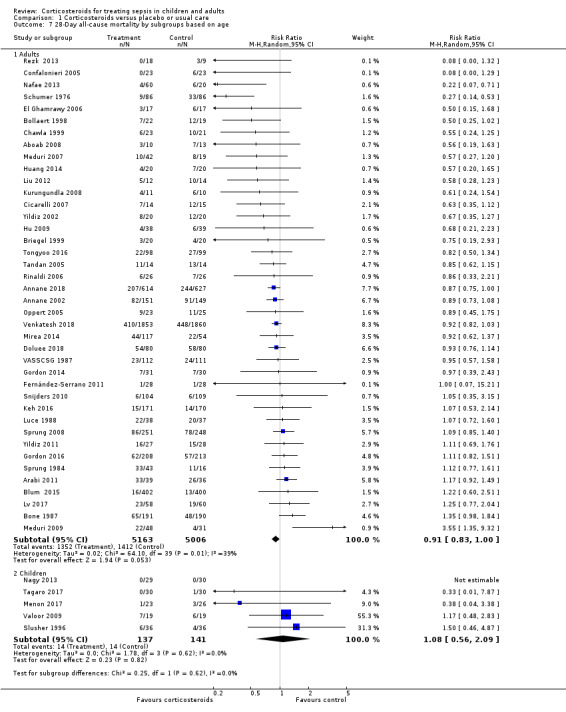
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 7 28‐Day all‐cause mortality by subgroups based on age.
1.8. Analysis.
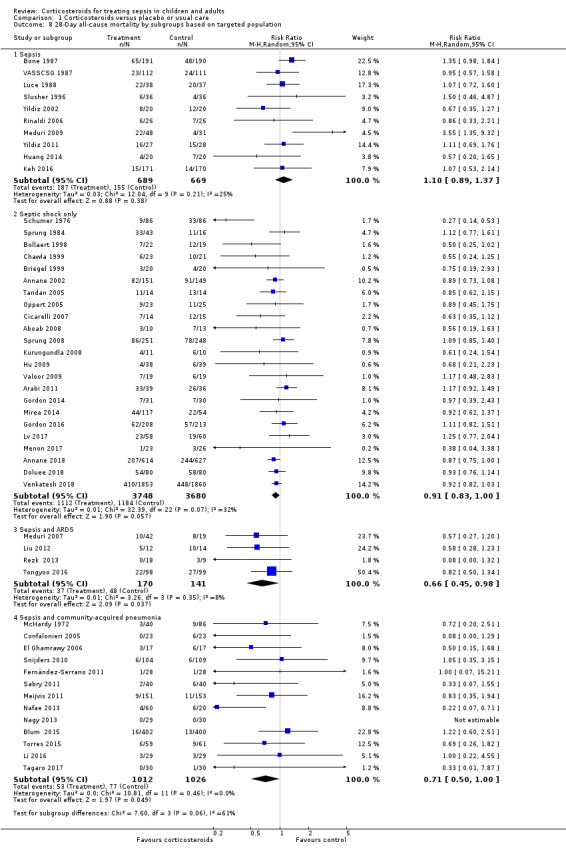
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 8 28‐Day all‐cause mortality by subgroups based on targeted population.
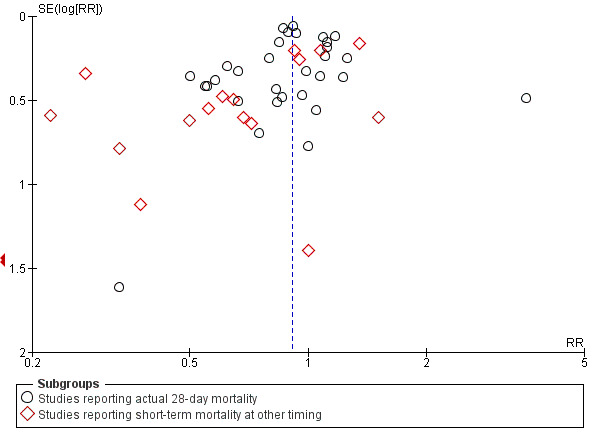
5.
Meta‐regression of the log of the risk ratio for 28‐day mortality against actual mortality at 28 days in the control arm.
1.9. Analysis.
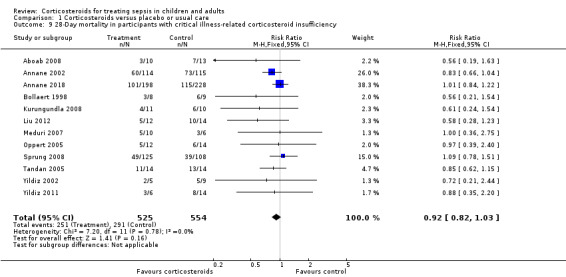
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 9 28‐Day mortality in participants with critical illness‐related corticosteroid insufficiency.
Funnel plot analysis, including all trials, suggested some asymmetry (Figure 6). Contour‐enhanced funnel plot analysis including trials of a long course of low‐dose corticosteroids suggested no significant asymmetry (Figure 7).
6.
Funnel plot of comparison: 1 Steroids vs control, outcome: 1.1 28‐Day all‐cause mortality.
7.
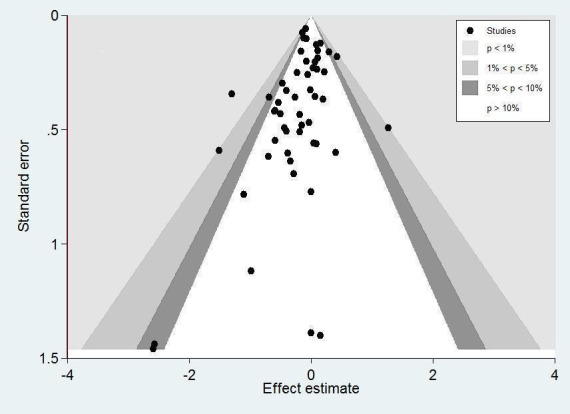
Contour‐enhanced funnel plot.
Log of risk ratio for 28‐day mortality is plotted against its standard error.
In one trial comparing hydrocortisone alone versus hydrocortisone plus fludrocortisone, the hazard ratio of death was 0.94 (95% CI 0.73 to 1.21; Annane 2010).
Secondary outcomes
90‐Day all‐cause mortality
We could extract data on 90‐day mortality from seven trials. A total of 961 of 2975 participants in the treated group and 1026 of 2959 in the control group died within 90 days. The RR of dying within 90 days was 0.93 (95% CI 0.87 to 1.00; P = 0.05; 5934 participants; 7 studies; I² = 0%; fixed‐effect model; Analysis 1.10) in favour of the corticosteroid group. This was based on moderate‐certainty evidence (lowered for imprecision).
1.10. Analysis.
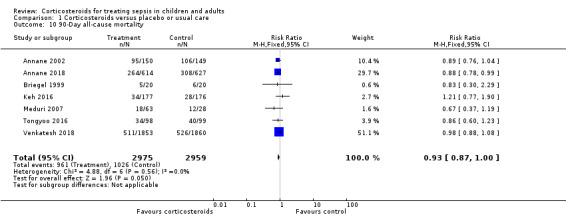
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 10 90‐Day all‐cause mortality.
Long‐term mortality
We could extract data on mortality beyond three months for seven trials. The RR of dying was 0.97 (95% CI 0.91 to 1.03; P = 0.29; 6236 participants; 7 studies; I² = 28%; Analysis 1.11). We downgraded the certainty of evidence to low owing to inconsistency in results and imprecision.
1.11. Analysis.
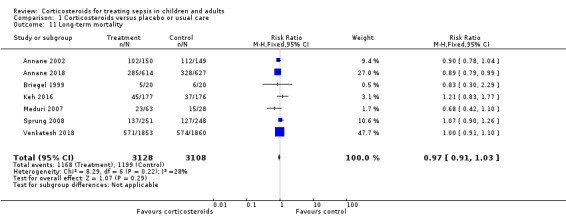
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 11 Long‐term mortality.
Intensive care unit (ICU) mortality
Data were available from 18 trials, accounting for 7267 participants. All of these trials investigated a long course of low‐dose corticosteroids. A total of 908 of 3636 participants in the treated group and 1015 of 3631 participants in the control group died in the ICU. There was little heterogeneity in the results (Chi² = 19.18; df = 17; P = 0.32; I² = 11%). The RR for dying in the ICU was 0.89 (95% CI 0.83 to 0.96; fixed ‐effect model; Analysis 1.12). This was based on high‐certainty evidence.
1.12. Analysis.
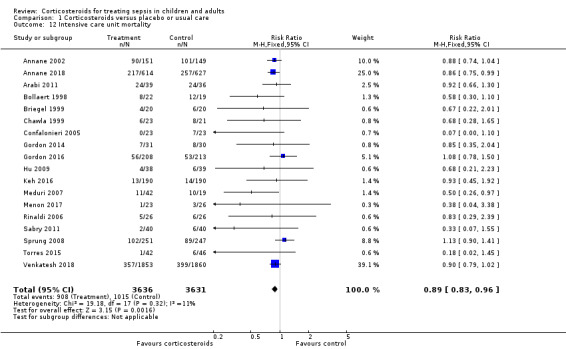
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 12 Intensive care unit mortality.
Hospital mortality
We could extract data on hospital mortality from 26 trials that accounted for 8183 participants. A total of 1223 of 4109 participants in the treated group compared with 1315 of 4074 in the control group died in hospital. Heterogeneity in the results was significant (Chi² = 39.58; df = 25; P = 0.03; I² = 37%). The RR for dying in hospital was 0.90 (95% CI 0.82 to 0.99; P = 0.03; random‐effects model; Analysis 1.13). We downgraded the certainty of evidence for this outcome from high to moderate for inconsistency.
1.13. Analysis.
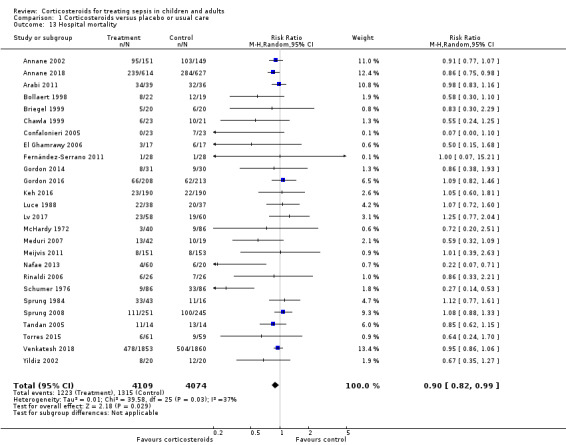
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 13 Hospital mortality.
Number of participants with shock reversal (as defined by stable haemodynamic status ≥ 24 hours after withdrawal of vasopressor therapy) at day 7
We could extract data from 16 trials that accounted for 6711 participants. A total of 2642 of 3361 participants in the treated group and 2168 of 3350 in the control group had shock reversed at day 7. Significant heterogeneity was evident in the results (Chi² = 43.87; df = 15; P = 0.0001; I² = 66%). The RR for having shock reversed at day 7 was 1.23 (95% CI 1.13 to 1.34; P < 0.0001; random‐effects model) in favour of the corticosteroid group (Analysis 1.14). This was based on moderate‐certainty evidence (lowered for inconsistency).
1.14. Analysis.
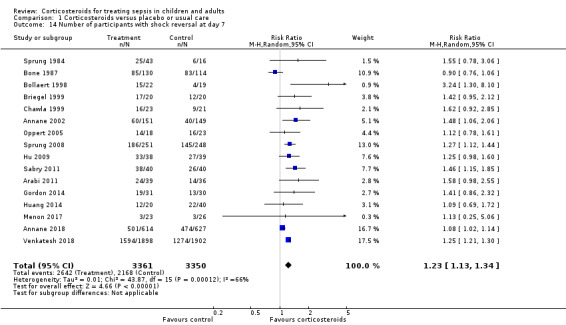
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 14 Number of participants with shock reversal at day 7.
Sensitivity analysis excluding the two trials that evaluated a short course of high‐dose corticosteroids did not reduce heterogeneity in the results (RR 1.26, 95% CI 1.16 to 1.37; 6408 participants; 16 studies; I² = 59%) (Bone 1987; Sprung 1984).
In one cross‐over trial, hydrocortisone was given for three days at a dose of 240 mg per day (Keh 2003). Although this trial could not provide information on shock reversal at day 7, investigators showed that at day 3, fewer hydrocortisone patients than placebo‐treated patients required norepinephrine treatment (6/20 vs 14/20; P = 0.025).
Number of participants with shock reversal (as defined by stable haemodynamic status ≥ 24 hours after withdrawal of vasopressor therapy) at day 28
We could extract data from 13 trials, accounting for 6753 participants. A total of 2767 of 3382 participants in the treated group had shock reversed at day 28, as did 2629 of 3397 in the placebo group. No heterogeneity was evident in the results (I² = 0%). The RR for having shock reversed was 1.06 (95% CI 1.03 to 1.08; P < 0.00001) in favour of the corticosteroid group (Analysis 1.15). This was based on high‐certainty evidence.
1.15. Analysis.
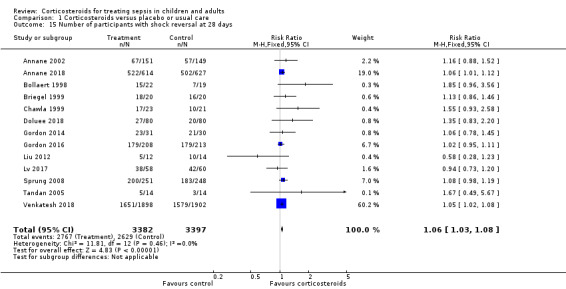
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 15 Number of participants with shock reversal at 28 days.
Number of organs affected and severity of organ dysfunction at day 7, as measured by the sequential organ failure assessment (SOFA) score
Ten studies (2157 participants) reported the SOFA score at seven days post randomization. The mean difference (MD) in the SOFA score at day 7 was ‐1.37 (95% CI ‐1.84 to ‐0.90; P < 0.00001; random‐effects model) in favour of corticosteroids. Moderate heterogeneity across studies was noted (Chi² = 17.03; df = 9; P = 0.05; I² = 47%; Analysis 1.16). This was based on moderate‐certainty evidence (lowered for inconsistency).
1.16. Analysis.
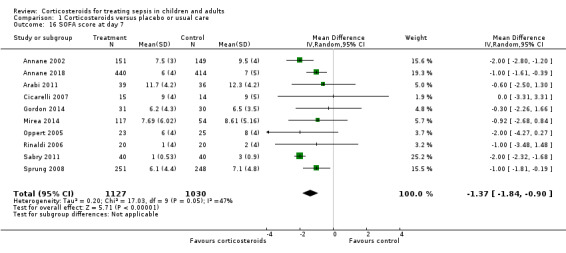
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 16 SOFA score at day 7.
In one study (Briegel 1999), corticosteroid treatment was associated with a non‐significant (P = 0.18) trend toward earlier resolution of organ dysfunction.
Length of stay in the intensive care unit
For all participants
In 21 trials (7612 participants), the MD for ICU length of stay for all participants was ‐1.07 days (95% CI ‐1.95 to ‐0.19; P = 0.02; random‐effects model) in favour of the corticosteroid group, with some heterogeneity evident across studies (Chi² = 31.49; df = 20; P = 0.05; I² = 36%; Analysis 1.17). We judged the certainty of evidence for this outcome as high. There was some heterogeneity in the results. However, the treatment effect was large.
1.17. Analysis.
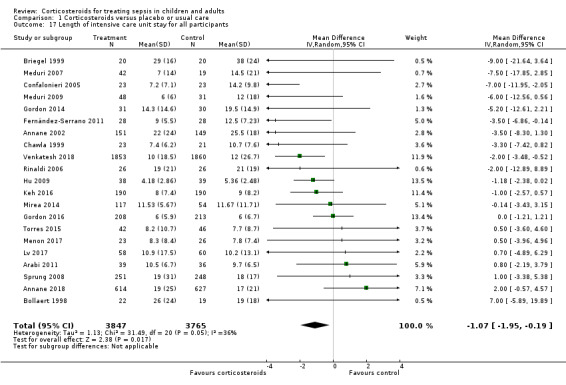
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 17 Length of intensive care unit stay for all participants.
For survivors only
We could extract data from 10 trials on 778 ICU survivors. The MD for ICU length of stay among these survivors was ‐2.19 days (95% CI ‐3.93 to ‐0.46; P = 0.01; fixed‐effect model). No heterogeneity was evident across studies (Chi² test = 8.63; P= 0.47; I² = 0%; Analysis 1.18).
1.18. Analysis.
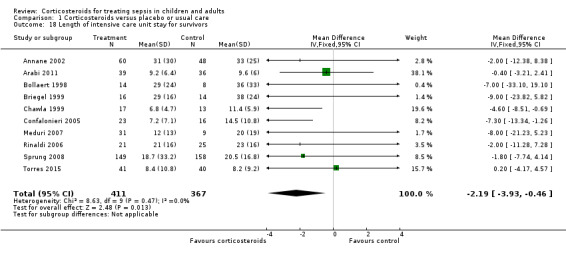
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 18 Length of intensive care unit stay for survivors.
Length of hospital stay
For all participants
From 22 trials (8795 participants), we could extract data on all participants. We noted heterogeneity in the results (heterogeneity: Chi² = 51.44; df = 201; P = 0.0002; I² = 59%). The MD for length of hospital stay for all participants was ‐1.63 days (95% CI ‐2.93 to ‐0.33 ; P = 0.01; random‐effects model; Analysis 1.19). We judged the certainty of evidence for this outcome as high. There was some heterogeneity in the results. However, the treatment effect was large.
1.19. Analysis.
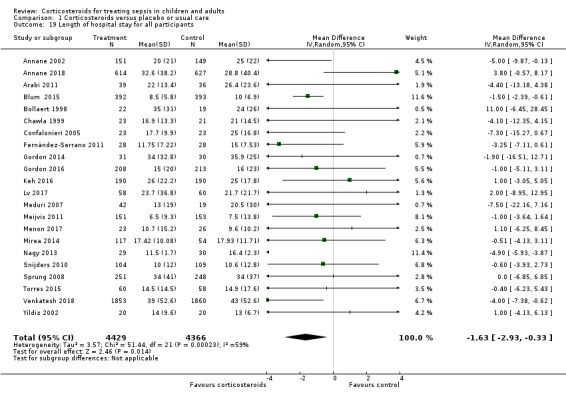
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 19 Length of hospital stay for all participants.
For survivors only
We could extract data for hospital survivors from nine studies (710 participants). We noted some heterogeneity in the results (I² = 43%). No evidence suggested a difference between the two groups (MD ‐4.11 days, 95% CI ‐8.50 to 0.28; P = 0.07; random‐effects model; Analysis 1.20).
1.20. Analysis.
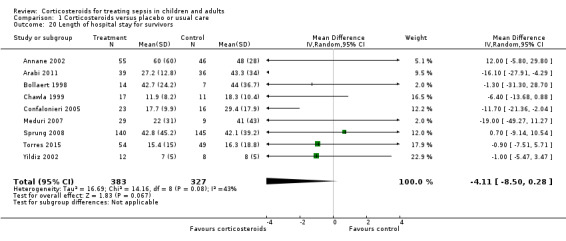
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 20 Length of hospital stay for survivors.
Adverse events
Gastroduodenal bleeding
We could extract data from 25 trials (5171 participants). A total of 131 of 2607 participants in the treated group and 120 of 2564 in the control group had an episode of gastroduodenal bleeding. We noted no heterogeneity in the results (I² = 0%). The RR for having gastroduodenal bleeding was 1.07 (95% CI 0.85 to 1.35; P = 0.55; fixed‐effect model; Analysis 1.21). We judged this to be based on moderate‐certainty evidence (lowered due to imprecision).
1.21. Analysis.
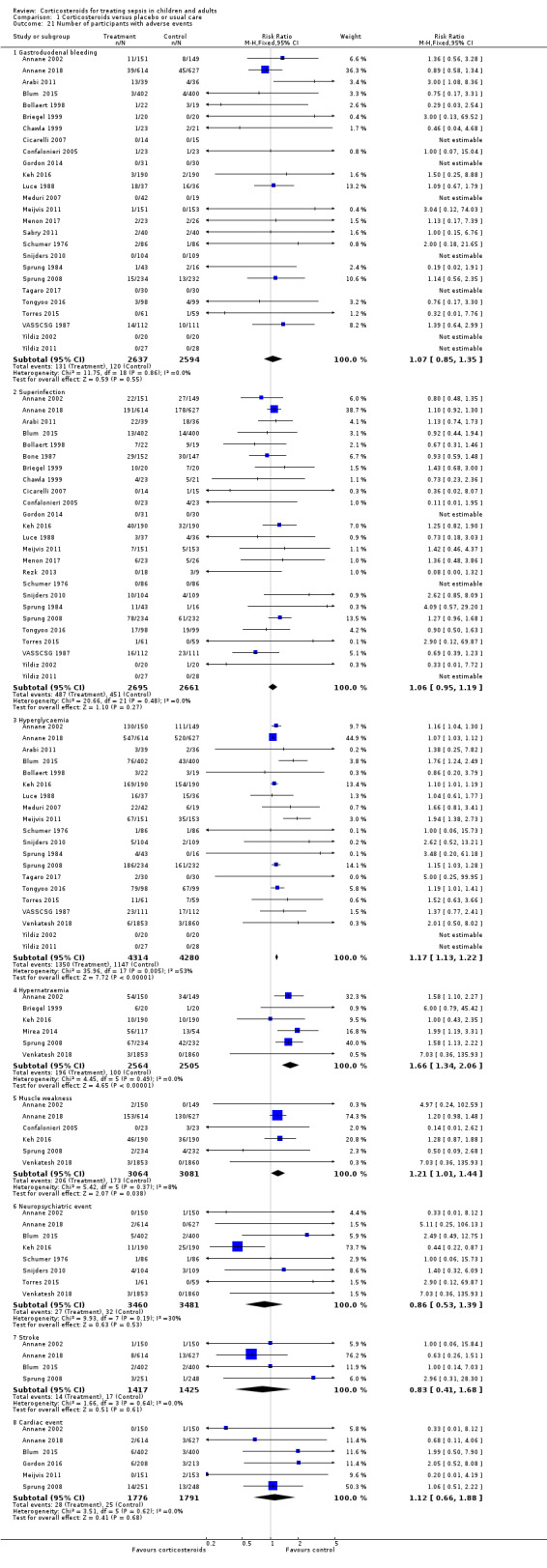
Comparison 1 Corticosteroids versus placebo or usual care, Outcome 21 Number of participants with adverse events.
Superinfection
We could extract data from 25 trials (5356 participants). A total of 487 of 2695 participants in the treated group and 451 of 2661 participants in the control group had an episode of nosocomial infection. We noted no heterogeneity in the results (Chi² = 20.66; df = 21; P = 0.48; I² = 0%). The RR for superinfection was 1.06 (95% CI 0.95 to 1.19; P = 0.27; fixed‐effect model; Analysis 1.21). We judged the certainty of evidence as moderate for this outcome (lowered for imprecision).
Hyperglycaemia
The number of participants who presented with hyperglycaemia was reported for 20 trials (8594 participants). There was heterogeneity in the results (Chi² = 35.96; df = 17; P = 0.005; I² = 53%). The RR for hyperglycaemia was 1.20 (95% CI 1.10 to 1.31; P < 0.00001; random‐effects model; Analysis 1.21). This was based on moderate‐certainty evidence (lowered for inconsistency).
One trial comparing tight glucose control versus standard care found no benefit in normalizing blood glucose levels among corticosteroid‐treated septic shock participants (Annane 2010).
Hypernatraemia
The number of participants who presented with hypernatraemia was reported for six trials (5069 participants). We noted no heterogeneity in the results (Chi² = 4.45; df = 5; P = 0.49; I² = 0%). The RR for hypernatraemia was 1.66 (95% CI 1.34 to 2.06; P < 0.00001; fixed‐effect model; Analysis 1.21). This was based on high‐certainty evidence.
Muscle weakness
The number of participants who presented with muscle weakness was reported for six trials (6145 participants). There was little to no heterogeneity in the results (Chi² = 5.42; df = 5; P = 0.37; I² = 8%). The RR for muscle weakness was 1.21 (95% CI 1.01 to 1.44; P = 0.04; fixed‐effect model; Analysis 1.21) in favour of the control group. We judged the certainty of evidence as high for this outcome.
Neuropsychiatric events
The number of participants who presented with neuropsychiatric events was reported for eight trials (6941 participants). There was some heterogeneity in the results (Chi² = 9.93; df = 7; P = 0.19; I² = 30%). The RR for neuropsychiatric events was 1.15 (95% CI 0.52 to 2.57; P = 0.73; random‐effects model; Analysis 1.21). This was based on low‐certainty evidence (lowered for imprecision and inconsistency).
Stroke
The number of participants who presented with stroke was reported for four trials (2842 participants). There was no heterogeneity in the results (Chi² = 1.66; df = 3; P = 0.64; I² = 0%). The RR for stroke was 0.83 (95% CI 0.41 to 1.68; P = 0.73; fixed‐effect model; Analysis 1.21). This was based on moderate‐certainty evidence (lowered for imprecision).
Cardiac events
The number of participants who presented with cardiac events was reported for six trials (3567 participants). There was no heterogeneity in the results (Chi² = 3.51; df = 5; P = 0.62; I² = 0%). The RR for acute coronary events was 1.12 (95% CI 0.66 to 1.88; P = 0.68; fixed‐effect model; Analysis 1.21). This was based on moderate‐certainty evidence (lowered for imprecision).
Continuous infusion versus intermittent bolus of corticosteroids
We have summarized the main results in Table 2.
1. Continuous infusion compared to bolus administration of corticosteroids for children and adults with sepsis.
| Continuous infusion compared to bolus administration of corticosteroids for children and adults with sepsis | ||||||
| Patient or population: children and adults with sepsis Setting: hospitalized patients; trials were performed in France, Tunisia, Romania, and Finland Intervention: continuous infusion Comparison: bolus administration of corticosteroids | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with bolus administration of corticosteroids | Risk with continuous infusion | |||||
| 28‐Day all‐cause mortality | Study population | RR 1.03 (0.81 to 1.31) | 310 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,b | Evidence is very uncertain about the effect of continuous infusion on 28‐day all‐cause mortality | |
| 444 per 1000 | 457 per 1000 (359 to 581) | |||||
| Long‐term mortalityc | Study population | RR 1.36 (1.02 to 1.81) | 70 (1 RCT) | ⊕⊝⊝⊝ Very lowd,e,f | Evidence is very uncertain about the effect of continuous infusion on long‐term mortality | |
| 636 per 1000 | 865 per 1000 (649 to 1000) | |||||
| Hospital mortality | Study population | RR 0.95 (0.72 to 1.25) | 240 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,g | Evidence is very uncertain about the effect of continuous infusion on hospital mortality | |
| 458 per 1000 | 435 per 1000 (329 to 572) | |||||
| Length of intensive care unit stay for all participants in days | Mean length of intensive care unit stay for all participants was 13 days | MD 1.05 lower (4.54 lower to 2.45 higher) | ‐ | 310 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,b,h | Evidence is very uncertain about the effect of continuous infusion on length of intensive care unit stay for all participants |
| Length of hospital stay for all participants in days | Mean length of hospital stay for all participants was 17 days | MD 0.01 higher (5.05 lower to 5.07 higher) | ‐ | 310 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,b,h | Evidence is very uncertain about the effect of continuous infusion on length of hospital stay for all participants |
| Number of participants with adverse events ‐ superinfection (up to longest follow‐up) | Study population | RR 1.12 (0.37 to 3.33) | 193 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,h | Evidence is very uncertain about the effect of continuous infusion on number of participants with adverse events ‐ superinfection | |
| 204 per 1000 | 229 per 1000 (76 to 680) | |||||
| Number of participants with adverse events ‐ muscle weakness (up to longest follow‐up) | Study population | RR 0.89 (0.13 to 5.98) | 70 (1 RCT) | ⊕⊕⊝⊝ Lowd,e | Evidence suggests that continuous infusion may result in little to no difference in the number of participants with adverse events ‐ muscle weakness | |
| 61 per 1000 | 54 per 1000 (8 to 362) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; MD: mean difference; RCT: randomized controlled trial; RR: risk ratio. The unit of measure for length of stay is days. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level as only one of the four trials was judged as having low risk of bias.
bDowngraded one level as trials were small and the 95% confidence interval was large.
dDowngraded one level as the only trial reporting this outcome was open‐labelled and at high risk of performance bias.
eDowngraded one level as only one trial reported this outcome.
fDowngraded one level as the observed increase in risk of dying in the long term is not consistent with treatment effects on 28‐day mortality.
gDowngraded one level as results show some heterogeneity.
hDowngraded two levels as heterogeneity in the results is strong.
cLong‐term mortality was assessed up to six months.
Primary outcome
28‐Day all‐cause mortality
Data for 28‐day mortality were available for three trials accounting for 310 participants. There was no heterogeneity in the results (Chi² = 1.94; df = 2; P = 0.38; I² = 0%). A total of 73 of 159 participants in the continuous infusion group and 67 of 151 participants in the intermittent bolus group died at 28 days. The RR of dying at 28 days was 1.03 (95% CI 0.81 to 1.31; P = 0.82; fixed‐effect model; Analysis 2.1) in favour of the intermittent bolus group. We downgraded the certainty of evidence to very low due to high risk of bias in all except one trial and due to imprecision.
2.1. Analysis.
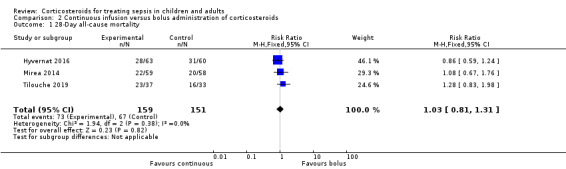
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 1 28‐Day all‐cause mortality.
Secondary outcomes
90‐Day all‐cause mortality
Data for 90‐day mortality were available for only one trial (Hyvernat 2016). This trial provided no evidence of a difference between groups for 90‐day all‐cause mortality (RR 0.87, 95% CI 0.61 to 1.22; Analysis 2.2). We judged this to be very low‐certainty evidence (with very high risk of bias and imprecision).
2.2. Analysis.
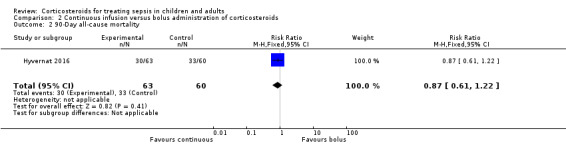
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 2 90‐Day all‐cause mortality.
Long‐term mortality
In one trial that reported mortality at one year, the RR of dying was 1.36 (95% CI 1.02 to 1.81; 70 participants; Analysis 2.3) (Tilouche 2019). We downgraded the certainty of evidence to very low owing to the fact that data were available from only one small trial that was at high risk of performance and detection bias.
2.3. Analysis.
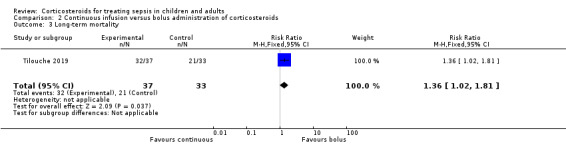
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 3 Long‐term mortality.
Intensive care unit mortality
We could extract data from four trials. We found no evidence of a difference between the two groups (RR 1.02, 95% CI 0.80 to 1.29; 358 participants; I² = 0%; fixed‐effect model; Analysis 2.4). This was based on very low‐certainty evidence (with very high risk of bias and imprecision).
2.4. Analysis.
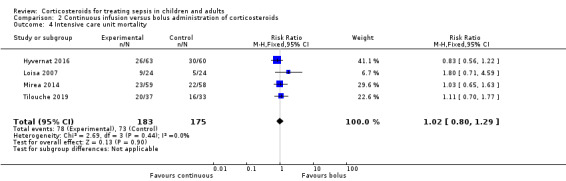
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 4 Intensive care unit mortality.
In‐hospital mortality
We could extract data from two trials. We found no evidence of a difference between the two groups (RR 0.95, 95% CI 0.72 to 1.25; P = 0.70; 240 participants; 4 studies; I² = 0%; fixed‐effect model; Analysis 2.5). We downgraded the certainty of evidence to very low owing to imprecision and risk of bias in one study.
2.5. Analysis.
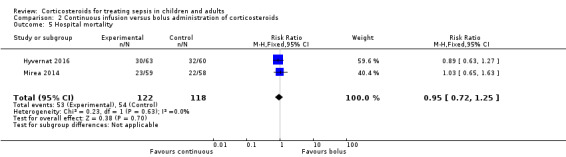
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 5 Hospital mortality.
Number of participants with shock reversal (as defined by stable haemodynamic status ≥ 24 hours after withdrawal of vasopressor therapy) at day 7
We could extract data about shock reversal from four trials (358 participants). The results showed heterogeneity (Chi² = 10.09; df = 3; P = 0.02; I² = 70%). A total of 104 of 183 participants in the continuous infusion group and 118 of 175 participants in the intermittent bolus group had shock reversal. The RR of shock reversal was 0.80 (95% CI 0.59 to 1.10; P = 0.17; random‐effects model; Analysis 2.6). This was based on very low‐certainty evidence (due to risk of bias, imprecision, and inconsistency).
2.6. Analysis.
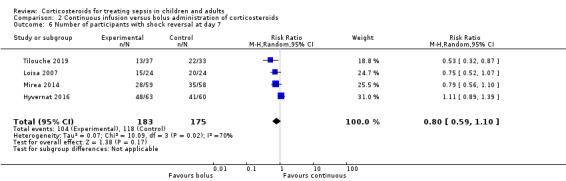
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 6 Number of participants with shock reversal at day 7.
Number of participants with shock reversal (as defined by stable haemodynamic status ≥ 24 hours after withdrawal of vasopressor therapy) at 28 days
Data were available from one trial (Tilouche 2019). The RR of having shock reversed by 28 days was 0.78 (95% CI 0.45 to 1.34; 70 participants; Analysis 2.7). This was based on very low‐certainty evidence (due to risk of bias and very severe imprecision).
2.7. Analysis.
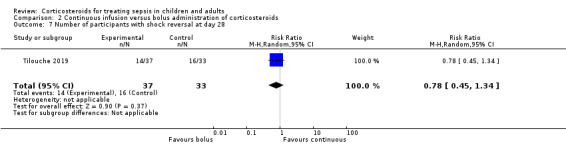
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 7 Number of participants with shock reversal at day 28.
Number of organs affected and severity of organ dysfunction at day 7, as measured by the sequential organ failure assessment (SOFA) score
The SOFA score at day 7 was available for three trials. The mean difference between groups for the SOFA score was 1.00 (95% CI ‐0.25 to 2.26; 260 participants; I² = 7%; fixed‐effect model; Analysis 2.8). This was based on very low‐certainty evidence (due to risk of bias and very severe imprecision).
2.8. Analysis.
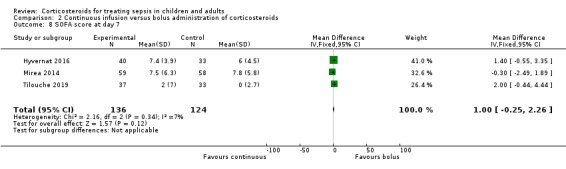
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 8 SOFA score at day 7.
Length of stay in the intensive care unit
For all participants
We could extract data about length of stay in the ICU for three trials. We found no evidence of a difference between groups (MD ‐1.05 days, 95% CI ‐4.54 to 2.45; P = .56; 310 participants; I² = 67%; random‐effects model; Analysis 2.9). We downgraded the certainty of evidence to very low owing to inconsistency, imprecision, and high risk of bias in two studies.
2.9. Analysis.
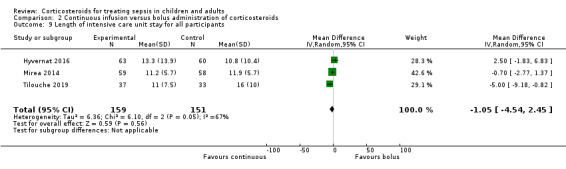
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 9 Length of intensive care unit stay for all participants.
For survivors only
No trial provided data for length of ICU stay among survivors only.
Length of stay in the hospital
For all participants
We could extract data about length of stay in the hospital from three trials. We found no evidence of a difference between groups (MD 0.01 days, 95% CI ‐5.05 to 5.07; P = 1.00; 310 participants; I² = 70%; random‐effects model; Analysis 2.10). We downgraded the certainty of evidence to very low owing to inconsistency, imprecision, and high risk of bias in two studies.
2.10. Analysis.
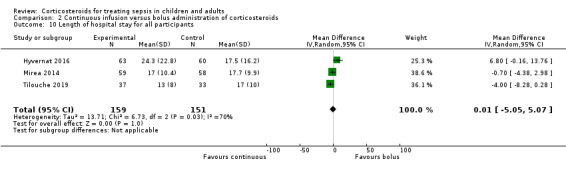
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 10 Length of hospital stay for all participants.
For survivors only
No trial provided data for length of hospital stay among survivors only.
Adverse events
Gastroduodenal bleeding
Data from two trials suggest no evidence of a difference between groups in the risk of gastroduodenal bleeding (RR 0.79, 95% CI 0.10 to 6.37; P = 0.83; 193 participants; I² = 67%; random‐effects model; Analysis 2.11). This was based on very low‐certainty evidence (due to risk of bias, inconsistency, and very severe imprecision).
2.11. Analysis.
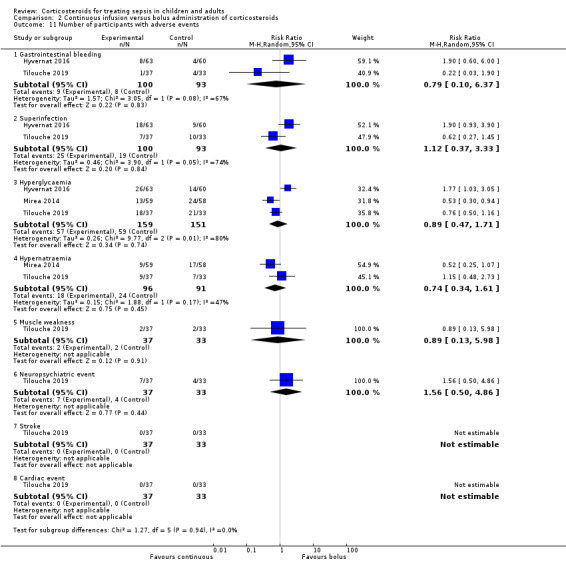
Comparison 2 Continuous infusion versus bolus administration of corticosteroids, Outcome 11 Number of participants with adverse events.
Superinfection
Data from two trials suggest no evidence of a difference between groups in the risk of superinfection (RR 1.12, 95% CI 0.37 to 3.33; P = 0.84; 193 participants; I² = 74%; random‐effects model; Analysis 2.11). We downgraded the certainty of evidence to very low owing to inconsistency, imprecision, and high risk of bias in one of the studies.
Hyperglycaemia
Data from three trials suggest no evidence of a difference between groups in the number of patients with at least one episode of hyperglycaemia (RR 0.89, 95% CI 0.47 to 1.71; P = 0.74; 310 participants; I² = 80%; random‐effects model; Analysis 2.11). This was based on very low‐certainty evidence (due to risk of bias, inconsistency, and imprecision).
Two trials reported mean blood glucose levels. One trial found slightly lower mean blood glucose levels in the continuous infusion group when compared to the intermittent boluses group (6.4 ± 0.7 mmol/L vs 6.2 ± 0.7; P = 0.04) (Loisa 2007). Another trial found no statistically significant difference between these groups (9.± 2.5 mmol/L vs 8.5 ± 6.0; P = 0.55) (Hyvernat 2016). In addition, three trials found that managing hyperglycaemia required higher doses of insulin in continuous infusion versus bolus administration. The MDs for insulin dose were 12.92 (95% CI ‐15.43 to 41.27) (Hyvernat 2016), ‐5.00 (95% CI ‐28.50 to 18.50) (Loisa 2007), and 7.57 (95% CI 4.07 to 11.07) (Tilouche 2019).
Hypernatremia
Data from two trials suggest no evidence of a difference between groups (RR 0.74, 95% CI 0.34 to 1.61; P = 0.45; 187 participants; I² = 47%; random‐effects model; Analysis 2.11). This was based on very low‐certainty evidence (due to risk of bias, inconsistency, and imprecision).
Muscle weakness
Only one trial reported data about muscle weakness (Tilouche 2019). This trial provided no evidence of a difference in this outcome between groups (RR 0.89, 95% CI 0.13 to 5.98). We downgraded the certainty of evidence to very low as this outcome was available from only one trial that was at high risk of performance and detection bias.
Neuropsychiatric events
Only one trial reported data about neuropsychiatric events (Tilouche 2019). This trial provided no evidence of a difference in this outcome between groups (RR 1.56, 95% CI 0.50 to 4.86). This was based on very low‐certainty evidence (due to risk of bias, inconsistency, and very severe imprecision).
Stroke
One trial reported that this outcome did not occur during patient follow‐up (Tilouche 2019). The other trials did not report information about this outcome.
Cardiac events
One trial reported that this outcome did not occur during patient follow‐up (Analysis 2.11) (Tilouche 2019). The other trials did not report information about this outcome.
Discussion
Summary of main results
Effects of corticosteroids on mortality
Overall, this review suggests that in sepsis, corticosteroids reduce all‐cause mortality at 28 days and at 90 days, as well as mortality at intensive care unit (ICU) and hospital discharge. For these outcomes, results show some heterogeneity.
Sensitivity analysis based on trials judged as being at low risk of bias found a significant reduction in 28‐day all‐cause mortality with corticosteroids.
Subgroup analysis based on the specific study drug used did not find significant subgroup differences, although treatment effects on 28‐day mortality might be greater with the combination of hydrocortisone and fludrocortisone. Only one trial directly compared hydrocortisone alone to hydrocortisone and fludrocortisone and found a non‐statistically significant 3% absolute reduction in in‐hospital mortality in favour of the combination (Annane 2010). Meta‐regression and subgroup analyses based on treatment modalities show that dose and duration did not influence response to corticosteroids. Nevertheless, most trials published in the past two decades provided a long course (> 72 hours at full dose) of low‐dose (< 400 mg per day of hydrocortisone equivalent) corticosteroids. Researchers provided no evidence of subgroup differences based on continuous infusion versus intermittent bolus administration of corticosteroids. Likewise, trials that directly compared continuous infusion versus intermittent bolus of corticosteroids reported no evidence of a difference between groups in mortality at 28 days, at 90 days, in the long term, and at ICU and hospital discharge. Subgroup analysis based on modalities for stopping corticosteroids suggests that survival benefit from corticosteroids was greater without versus with tapering off.
Subgroup analyses based on factors related to participants suggest that age (children vs adults) did not influence patients' response to corticosteroids. Patients with septic shock, those with acute respiratory distress syndrome (ARDS), and those with community‐acquired pneumonia may be more likely to derive a survival benefit from corticosteroids than patients with less severe sepsis, although subgroup differences were barely statistically significant. Analysis of trials including patients with critical illness‐related corticosteroid insufficiency (CIRCI) did not show a significant reduction in the risk of death at 28 days. However, studies did not use the same definition for adrenal insufficiency. Additional studies are needed to determine the best diagnostic tool for CIRCI (Annane 2017b).
Effects of corticosteroids on morbidity outcomes
The beneficial effects of corticosteroids on mortality may be related to favourable effects of this treatment on the duration of shock. Indeed, this review shows that treatment with corticosteroids resulted in a substantial reduction in shock duration, with fewer patients remaining on vasopressor therapy by day 7 and by day 28. Treatment with corticosteroids may attenuate the severity of inflammation (Confalonieri 2005; Keh 2003; Mikami 2007; Oppert 2005; Rinaldi 2006), as well as the intensity and duration of organ system failure (Briegel 1999; Confalonieri 2005; Keh 2003; Oppert 2005; Sprung 2008), as shown in this review by a marked decrease in sequential organ failure assessment (SOFA) score at day 7. In addition, subsequent to favourable effects on cardiovascular and other organ functions, corticosteroid therapy resulted in substantial shortening of ICU and hospital length of stay.
These favourable effects of corticosteroids on sepsis‐related morbidity were not influenced by modalities of treatment administration, as was found in trials that directly compared continuous infusion versus intermittent boluses of corticosteroids.
Tolerance of corticosteroids
Finally, this review also found no evidence of an effect of corticosteroids on rates of gastroduodenal bleeding or superinfection, nor on the proportion of patients with neuropsychiatric events, stroke, or cardiac events. Corticosteroids were associated with increased risk for developing hyperglycaemia and hypernatraemia, and for developing acquired muscle weakness.
Evidence from four trials that compared continuous infusion versus intermittent bolus of corticosteroids does not show significant differences in rates of hyperglycaemia, mean blood glucose levels, or the need for higher insulin doses when corticosteroids were administered as continuous infusion. One trial including 509 corticosteroid‐treated patients with septic shock reported no benefit for normalizing blood glucose levels (Annane 2010). The rates of any other serious adverse events were not significantly different between continuous infusion and intermittent bolus administration of corticosteroids.
Overall completeness and applicability of evidence
We identified 61 trials addressing the question of corticosteroids versus control for sepsis. These trials accounted for a large population (i.e. 12,192 participants). Most of the eligible trials contributed to the primary outcome for this review. In addition, four trials provided information on direct comparison of continuous infusion versus intermittent bolus administration of corticosteroids. We found no evidence of publication bias.
Owing to the large number of trials, and to the large size of some individual trials, we could investigate all foreseen outcomes. We found mild heterogeneity in results for the primary outcome, which we explored through sensitivity analyses, subgroup analyses, and meta‐regression analyses. Although subgroup analyses represent a between‐study ‐ not a within‐study ‐ hypothesis, we thought its validity was acceptable according to proposed criteria (Guyatt 2008b). First, we defined the hypothesis for an interaction between practical modalities of administration and effects of corticosteroids on mortality a priori. Second, we conducted subgroup analyses based on only two factors (i.e. modalities of drug administration and population). Third, findings show that the treatment effect was consistent in terms of 28‐day, ICU, hospital, 90‐day, and long‐term mortality (risk ratios (RRs) 0.91, 0.89, 0.90, 0.93, and 0.97, respectively). Fourth, strong external evidence supports these results. Experimental and human studies have shown that a dose of 400 mg or less of hydrocortisone or equivalent can reverse the systemic inflammatory response, endothelial activation, and coagulation disorders secondary to infection (Annane 2005; Heming 2018), thus arguing against the use of higher doses. Moreover, at these low doses, corticosteroids have been shown to improve rather than suppress innate immunity in patients with septic shock (Kaufman 2008). It is now established that sepsis results in a sustained pro‐inflammatory state, arguing against a short course of treatment (Angus 2013; Kellum 2007; van der Poll 2017).
Review authors noted some variation in the routine use of corticosteroids in sepsis. A survey of 542 US critical care physicians found that 83% do not routinely use corticosteroids in adults with sepsis, contrasting with 81% reporting common use of corticosteroids for septic shock (Bruno 2012). The findings of this review suggest that treatment effects on mortality may be greater in sepsis with versus without shock. Roughly one out of three respondents to the survey believed that corticosteroids reduce mortality in septic shock, whereas 27% did not and 45% were unsure. Hydrocortisone was the most common corticosteroid prescribed (93%), with a median dosage of 200 mg/d and administration via intermittent intravenous injection.
Quality of the evidence
We judged the certainty of evidence for 28‐day mortality as moderate rather than high because of some inconsistency across trials that was related in part to differences in study populations and to differences in the types of corticosteroids used and the ways in which corticosteroids were given.
Potential biases in the review process
For this review, we performed a comprehensive search of the literature with no restriction on language, so we can assume that the risk of missing important trials was very limited. Slight asymmetry in the funnel plot for the primary outcome of this review may suggest some publication bias. However, potential sources of an asymmetrical funnel plot also include selection biases, poor methodological quality of smaller studies, true heterogeneity, artefacts, and chance (Egger 1997). Visual inspection of the funnel plot suggests a small‐study effect (i.e. among small studies, the positive ones are more likely to be published). Nevertheless, our thorough search strategy and the need to enrol studies in public clinical trial registries may have decreased the risk of missing any randomized controlled trials. True heterogeneity seems to be a more plausible explanation for the observed asymmetrical funnel plot. Indeed, the effects of corticosteroids on mortality may be proportionate to the basal risk of death, and the two large trials that did not find survival benefit ‐ Sprung 2008 and Venkatesh 2018 ‐ included patients at lower risk of death than was seen in the two large trials that found a survival benefit ‐ Annane 2002 and Annane 2018. Finally, the asymmetrical funnel plot may have been due to chance.
One trial used a cross‐over design (Keh 2003), and we could obtain none of the foreseen outcomes for this review. This trial concluded that prolonged treatment with a low dose of hydrocortisone improved haemodynamic and immune outcomes. Another trial compared three days versus seven days of hydrocortisone therapy and provided no evidence of differences in outcomes between patients treated for three days or seven days (Huh 2007). However, this trial had some limitations, including lack of blinding and small sample size. We considered that pooling the results of remaining trials in a meta‐analysis was acceptable.
Three trials were published only as an abstract (Chawla 1999; Mirea 2014; Tandan 2005). Nevertheless, the primary investigators for these studies provided sufficient unpublished data for review authors to compute the primary outcome and several secondary outcomes for this review, allowing us to include these trials in the meta‐analysis. Both published and unpublished data were available for 28 trials (Appendix 5), and the primary author for each trial validated the data extraction form. For four studies, contact with the primary investigator yielded no additional data (Luce 1988; Meijvis 2011; Rezk 2013; Snijders 2010).
We chose to convert outcome measures that correspond to censored data into dichotomous variables, that is, the proportion of participants with a particular event after one week and after four weeks, or at ICU or hospital discharge.
Agreements and disagreements with other studies or reviews
Findings in this review that a short course of high‐dose corticosteroids provides no benefit for patients with sepsis are in line with reports from previous systematic reviews (Cronin 1995; Lefering 1995), as well as with current international guidelines (Annane 2017b; Rhodes 2017).
We found scarce data that could not allow conclusions on the effects of corticosteroids in children with sepsis, in keeping with a recent systematic review (Menon 2013). Nevertheless, we found no evidence of a difference in response to corticosteroids between children and adults.
The beneficial effects of corticosteroids on shock reversal in patients with septic shock are consistent across recent systematic reviews (Allen 2018; Fang 2018; Kalil 2011; Moran 2010; Ni 2018; Rochwerg 2018; Rygard 2018; Sherwin 2012). The survival benefit derived from corticosteroids for patients with sepsis was suggested by some previous authors (Allen 2018; Fang 2018; Moran 2010; Ni 2018; Rochwerg 2018), but not by others (Table 3) (Kalil 2011; Rygard 2018; Sherwin 2012). Nevertheless, this systematic review included trials that were not included in previous systematic reviews, as they were published only recently or were published in a non‐English language. The current review included non‐published information for a large number of trials after contact was made with original study authors, resulting in inclusion of qualitatively and quantitatively better data than were provided previously.
2. Recent systematic reviews about the use of corticosteroids in sepsis.
| Author | Number of trials | Primary outcome | No of patients | Estimate | 95% CI |
| Ni 2018 | 19 | 28‐Day mortality | 7035 | Sepsis: RR = 0.91 Septic shock: RR = 0.92 |
0.85 to 0.98 0.85 to 0.99 |
| Allen 2018 | 6 | Not stated | 5689 | Only qualitative assessment | Only qualitative assessment |
| Rochwerg 2018 | 42 | 28‐ to 31‐day mortality | 10,194 | RR = 0.93 | 0.84 to 1.03 |
| Rygard 2018 | 22 | Short‐term mortality | 7297 | RR = 0.96 | 0.91 to 1.02 |
| Fang 2018 | 37 | 28‐Day mortality | 9564 | RR = 0.90 | 0.82 to 0.98 |
A recent network meta‐analysis suggests that hydrocortisone was more likely than methylprednisolone to achieve shock reversal (Gibbison 2017).
Authors' conclusions
Implications for practice.
Moderate‐certainty evidence indicates that corticosteroids probably reduce 28‐day, 90‐day, and hospital mortality among patients with sepsis. Corticosteroids result in a large reduction in ICU and hospital length of stay (high‐certainty evidence). There may be little or no difference in the risk of major complications; however, corticosteroids increase the risk of muscle weakness and hypernatraemia (high‐certainty evidence), and probably increase the risk of hyperglycaemia (moderate‐certainty evidence). The effects of continuous versus intermittent bolus administration of corticosteroids are uncertain.
Implications for research.
The criteria for critical illness‐related corticosteroid insufficiency in septic shock remain to be defined.
Subgroup analyses suggest that additional studies are needed to address these topics related to the use of corticosteroids in patients with sepsis.
The role of a long course of low‐dose corticosteroids for treatment of septic shock in children.
The role of a long course of low‐dose corticosteroids for treatment of patients with sepsis without shock, or with a mild form of septic shock; patients with ARDS; and patients with sepsis related to community‐acquired pneumonia.
The role of mineralocorticoid replacement.
Optimal timing of initiation of treatment.
Optimal dose and duration of hydrocortisone (or equivalent).
Optimal modality to administer treatment that is continuous versus intermittent bolus.
Optimal modality to stop treatment with or without taper off.
The role of a long course of low‐dose corticosteroids for treatment of sepsis caused by different types of infections.
Long‐term neuromuscular effects of steroids.
Feedback
Feedback, 9 May 2013
Summary
Annane et al in their systematic review of corticosteroids for treating severe sepsis and septic shock concluded “a long course of low dose corticosteroids reduced mortality without inducing major complications” (Annane 2004; updated 2010). This was based on a subgroup analysis, as all doses/durations of corticosteroids for septic shock did not show a benefit in reduction of mortality.
Given that the two largest trials have contradicting results (Annane 2002; Sprung 2008), we were interested in looking into these trials. Upon our review, we feel that the risk of bias assessment for these trials has not adequately addressed the issue of incomplete data. In one trial (Sprung 2008), authors used a per‐protocol analysis for their adverse event data; this was subsequently used in this review. Neither the trial nor the review addresses the reasons for this approach. Using per‐protocol data is not the preferred method of outcome reporting, as it does not allow for preservation of randomization. Section 14.6.1 of the Cochrane Handbook for Systematic Reviews of Interventions specifically asks whether any patients were excluded in reporting of adverse events. Participants who experience unfavourable adverse events may drop out of the trial. When the per‐protocol analysis is used, adverse effect results may therefore be biased in favour of steroids. The same scenario can be applied for the placebo group.
In another trial (Annane 2002), we are concerned with the way data were collected and reported for adverse events. Events are reported as being “possibly related to steroids” and “possibly related to vasopressors”. We are unsure as to how one would know whether or not an adverse event was related to the intervention. Neither the review nor the trial specifically outlines the adjusting procedure for determining whether or not adverse events were due to steroids. Patients in the intensive care unit have many risk factors for infection ‐ GI bleeding, psychiatric disorders (e.g. delirium) ‐ therefore it seems inappropriate to try to ascertain whether or not the event was secondary to steroids. Section 14.6.1 of the Cochrane Handbook for Systematic Reviews of Interventions explains how clinical trials may have a well‐designed method for collecting data for the primary outcome, but in fact may take a retrospective, unblinded approach to collecting adverse event data. An extension of the CONSORT statement for harm also echoes this, recommending that clinical trials should explicitly define how data for adverse events were defined, collected, and analysed (Ioannidis 2004). As Annane 2002 was a randomized controlled trial, adverse events would not require assessment of whether or not they were thought to be due to treatment. Randomization should take care of confounding factors and thus should be able to show differences (if they truly exist) in adverse events. In our opinion, preference should be given to all‐cause adverse events for this reason. Last, we note that in Analysis 1.12 for "superinfection", the percentage of participants with an event was used instead of the actual number of events in Annane 2002. For example, the number of events for the treatment arm should have been "22", but "15" was used instead. Given that these issues on selective reporting ‐ Annane 2002 ‐ and incomplete data surrounding the two largest trials of this review have not been adequately addressed in the risk of bias assessments, we find it difficult to conclude at this time on the safety profile of corticosteroid use in treating severe sepsis and septic shock. We look forward to hearing your response to our concerns.
Reply
We are grateful to Dr. Harbin and colleagues for their comments on the Cochrane review on corticosteroids for severe sepsis and septic shock.
Dr. Harbin and colleagues questioned the validity of the concluding statement of this review that corticotherapy was overall well tolerated apart from inducing hyperglycaemia and hypernatraemia. Indeed, they pointed out that Sprung and colleagues reported serious adverse events as per‐protocol (Sprung 2008). In fact, in this trial, data for adverse events were reported only for 466 of 499 patients. We have now reported this information in the risk of bias table in a revised version of the review.
Annane and colleagues reported in their main paper the number of participants with any serious adverse events in each treatment arm as per intent‐to‐treat analysis (Annane 2002). All serious adverse events that were observed were reported in each treatment group. Serious adverse events were further classified according to what was known about complications of corticosteroids or catecholamines. For example, all superinfections, gastroduodenal bleeding, metabolic disorders, and psychiatric disorders that occurred at any time from randomization were reported and further classified in a blinded manner as possibly related to corticosteroids. Thus, no manipulation of data occurred. All serious adverse events were carefully scrutinized and reported in the manuscript, and additional unpublished information (i.e. raw data) was available during preparation of the Cochrane review.
Finally, Dr. Harbin and colleagues highlighted an error in numbers used for Analysis 1.12 (number of participants with superinfection) that is now corrected in the revised version of the review. This modification did not significantly alter the direction and the magnitude of the pooled estimate for evaluation of serious adverse events. Thus, we believe that the conclusion statement ‐ that treatment with corticosteroids in patients with sepsis or septic shock is well tolerated apart from metabolic disorders ‐ is still valid.
Contributors
Megan Harbin, BSc Pharm Asal Taheri, BSc Pharm Wan‐Yun Polinna Tsai, BSc Pharm Gloria Su, BSc Pharm Aaron M Tejani, BSc Pharm, PharmD
Reply:
Djillali Annane
Feedback, 9 November 2017
Summary
Annane and colleagues, in their systematic review (Annane 2015), concluded that “a long course of low dose corticosteroids reduced mortality without inducing major complications”. This was based on a subgroup analysis, analysis of outcome 1.4, so we pursued it in greater detail. Upon our review, we found that the forest plot was created using a fixed‐effect model. However, the largest trial ‐ Sprung 2008 ‐ carried only 21.5% weight, and the second largest trial ‐ Annane 2002 ‐ was allotted a larger weight of 25.1%. Although we acknowledge that given that I² was 16%, a fixed‐effect model was chosen, we felt that because these two trials had conflicting results, suggesting clinical heterogeneity, a random‐effects model would have been a more conservative and more appropriate approach in this scenario. We took the initiative to re‐create the forest plot using a random‐effects model, and we found that the treatment effect became not statistically significant. This suggests that perhaps the conclusion is not as simple as “a long course of low dose corticosteroids reduced mortality” in severe sepsis and septic shock.
Furthermore, when we reviewed Table 1, we noticed that footnote “a” states that the certainty of evidence for the primary outcome was downgraded due to “1 of the 2 largest trials [showing] no survival benefit”. We feel that this sentence implies that the other largest trial did show a survival benefit, and may mislead the readers to believe so. However, both of the largest trials did not show a statistical benefit for corticosteroids compared to placebo for mortality benefits in sepsis and septic shock (Annane 2002; Sprung 2008). One trial simply showed that there was no increase in mortality, but did not show a reduction in mortality.
Based on our findings, we feel that there could be an alternative interpretation of the results of these trials. This review includes studies from 1976 to 2015, and when we look at studies published before 2002, the studies as a group show a more convincing trend toward mortality benefit with corticosteroids. In contrast, studies published after 2002 show more conflicting results. This may suggest that medical therapy today is better for treating sepsis and hence the benefits from corticosteroids are not as apparent as was previously thought. In contrast to the conclusion stated by the review authors, we feel that this review presents inconclusive evidence for mortality benefit with corticosteroid use in septic patients. We look forward to your response.
Reply
The planned analysis was to use a fixed‐effect model unless heterogeneity across trials could be suspected (i.e. squared I statistic > 30%). We weighted studies by the amount of information they contribute (more specifically, by the inverse variances of their effect estimates). It is also important to highlight that CORTICUS ‐ Sprung 2008 ‐ was terminated prematurely (after 500 participants were recruited out of 800 expected) owing to low recruitment rate and loss of equipoise among investigators. Changing from fixed‐ to random‐effects models did not change the magnitude nor the direction of the point estimate (RR 0.87 vs 0.88) and slightly enlarged the 95% CI 0.78 to 0.97 versus 0.77 to 1.00. Thus, we do not believe that the conclusion from our systematic review was not supported by data analysis, and we disagree about over‐interpreting the data.
In the trial Annane 2002, the primary outcome was time to death in non‐responders to ACTH testing (modified intent‐to‐treat analysis). The primary analysis for the primary outcome in this trial showed a statistically significant increase in survival time (P = 0.02). The CORTICUS trial ‐ Sprung 2008 ‐ found no significant effect of treatment on mortality. Thus, we do not believe that we have misinterpreted (misreported) findings from the Annane 2002 or Sprung 2008 trial.
The pooled RR of dying from trials published before 2002 was 0.90 (95% CI 0.75 to 1.07). The pooled RR of dying from trials published from 2002 was 0.89 (95% CI 0.80 to 1.00). Thus, no evidence suggests that the effect of corticosteroids on mortality differed between trials published before 2002 versus those published since 2002. Finally, new trials have been published since the last update of this review, including Keh et al JAMA 2016; Bi et al PLoSOne 2016; Menon et al Ped CCM 2017; El Nawawy The Pediatric Infectious Disease Journal 2016; Qing‐quan Lv et al Am J Emerg Med 2017; and Tongyoo et al. Critical Care 2016; and two large trials are about to be published in the very next future (ADRENAl, n = 3800 and APROCCHSS, n = 1241). Thus, we believe that there is a need to update the review in light of these newly published studies.
Contributors
Summary
Candy Lee, Karen Ng, Shalini Singla, Marco Yeung
Pharmacy Residents
Lower Mainland Pharmacy Services, Pharmacy Association, Vancouver, Canada
We do not have any affiliation with or involvement in any organisation with a financial interest in the subject matter of my comment.
Reply
Djillali Annane
Department of Critical Care, Hyperbaric Medicine and Home Respiratory Unit Center for Neuromuscular Diseases; Raymond Poincaré Hospital (AP‐HP) Faculty of Health Sciences Simone Veil, University of Versailles SQY‐University of Paris Saclay 104 Boulevard Raymond Poincaré 92380 Garches France
What's new
| Date | Event | Description |
|---|---|---|
| 25 July 2019 | New search has been performed | We reran the search from October 2014 to 31 March 2019. The search was updated again 25 July 2019. |
| 25 July 2019 | New citation required but conclusions have not changed | A new search of the literature revealed 25 additional trials. Cumulative evidence from 48 trials including 11,114 patients confirmed the direction and magnitude of the point estimate for 28‐day mortality with narrow confidence interval limits. The review found evidence for a significant reduction in ICU and hospital mortality, and in ICU and hospital length of stay. The review now includes evidence for a reduction in mid‐term (90‐day) to long‐term (up to 1 year) mortality by corticosteroids. We made several changes to the Methods section.
|
History
Protocol first published: Issue 3, 2000 Review first published: Issue 1, 2004
| Date | Event | Description |
|---|---|---|
| 14 December 2018 | Amended | Editorial team changed to Cochrane Emergency and Critical Care |
| 4 May 2018 | Feedback has been incorporated | New Feedback and reply posted in review |
| 18 January 2016 | Amended | Typo corrected in plain language summary (it was made clear that corticosteroids decreased the number of organs that were not functioning properly (organ failure)) |
| 30 November 2015 | New citation required and conclusions have changed | A new search of the literature revealed 9 additional trials. Cumulated evidence from 33 trials confirmed the direction and the magnitude of the point estimate for 28‐day mortality with narrow confidence interval limits. Thus, this update suggests moderate evidence for reduced 28‐day mortality with corticosteroids in the primary analysis. Evidence also confirms significant interactions between the relative risk of dying at 28 days and treatment modalities (lower doses and longer durations yielded better chance of survival) and patient case mix (patients with septic shock, sepsis‐related acute respiratory distress syndrome (ARDS) or community‐acquired pneumonia may be more likely to benefit from corticosteroids). We decided to change the title to "Corticosteroids for treating sepsis" owing to recent changes in the definition of sepsis, suggesting that the term "severe sepsis" should be avoided. We made several changes to the Methods section.
Sensitivity analyses based on methodological quality are now restricted to the primary outcome. We used random‐effects models only in cases of heterogeneity with an I² statistic > 30%. Otherwise, we used fixed‐effect models. |
| 30 November 2015 | New search has been performed | We reran the search from October 2009 to October 2014 |
| 14 August 2013 | Feedback has been incorporated | Feedback was submitted and was responded to. An error in numbers used for Analysis 1.12 (number of participants with superinfection) has been corrected in the amended version of this review. 'Risk of bias' tables and 'Summary of findings' tables have also been amended. |
| 1 November 2010 | New search has been performed |
|
| 25 March 2008 | Amended | Converted to new review format. |
Notes
This review was initially developed within the Infectious Diseases Group and was transferred to the Anaesthesia Group in May 2005.
Update 2010
The review was updated in 2010 (Annane 2004). At that time, Cochrane updates did not earn a new citation unless they had new review authors or included a change to the conclusions. Review authors found 21 new trials in 2010. Of those 21 trials, they included nine randomized controlled trials in the 2010 update. Additional included studies did not change the conclusions of this review. Therefore the 2010 update did not earn a new citation.
Update 2015
The new search of the literature identified nine additional trials. Accumulated evidence from 33 trials confirmed the direction and magnitude of the point estimate for 28‐day mortality with narrow confidence interval limits. Thus, this update suggested moderate evidence for reduced 28‐day mortality with corticosteroids in the primary analysis and confirmed significant interactions between the relative risk of dying at 28 days and treatment modalities used (lower doses and longer duration yielded better chance of survival) and the patient case mix included (patients with septic shock, sepsis‐related ARDS, or community‐acquired pneumonia may be more likely to benefit from corticosteroids).
We decided to change the title to "Corticosteroids for treating sepsis" owing to recent changes in the definition of sepsis, suggesting that the term "severe sepsis" should be avoided.
We made several changes to the Methods section.
We excluded quasi‐randomized trials (three trials).
We changed the definition of "long course" from at least five days to at least three days. Indeed, and in keeping with the Surviving Sepsis Campaign recommendation, corticosteroids are often given at full dose until cessation of vasopressor therapy, which may occur sooner than five days. We changed the definition of "low dose" from 300 mg or less per day to 400 mg or less per day. Indeed, no consensus has been reached about what should be the optimal dose, and several RCTs testing so called "low‐dose" corticosteroids used variable doses up to 400 mg. According to findings from the meta‐regression analysis, changes in the definitions of "low dose" and "long course" might have had a negative impact on observed survival benefits of corticosteroids. Indeed, we found that both longer duration and lower dose were associated with better survival rates.
We incorporated information on how we used the GRADE system and how we selected outcomes for the 'Summary of findings' table.
Sensitivity analyses based on methodological quality are now restricted to the primary outcome.
Random‐effects models are used only in cases of heterogeneity, with I² statistic > 30%. Otherwise, fixed‐effect models are used.
Acknowledgements
We would like to thank Arash Afshari (Content Editor), Vibeke Horstmann (Statistical Editor), Neill Adhikari and Philipp Schuetz (Peer Reviewers), Jonathan Fuchs (Consumer Referee), Janne Vendt (Information Specialist), Jane Cracknell and Teo Quay (Managing Editors), and Harald Herkner (Co‐ordinating Editor), for help and editorial advice provided during preparation of the 2019 updated systematic review.
We would like to thank Harald Herkner (Content Editor), Jing Xie (Statistical Editor), Philipp Schuetz and Mirjam Christ‐Crain (Peer Reviewers), and Janet Wale (Consumer Editor) for help and editorial advice provided during preparation of the 2015 updated systematic review (Annane 2015).
We would like to thank Dr Y Arabi, Dr R De Gaudio, Dr A Gordon, Dr H Hyvernat, Dr L Liu, Dr GU Meduri, Dr SC Meijvis, Dr L Mirea, Dr M Oppert, Dr S Rinaldi, Dr C Sprung, Dr S Tandan, Dr N Tilouche, Dr S Tongyoo, Dr A Torres, and Dr O Yildiz for providing us with unpublished data. We also would like to thank Dr Bin Du (Medical ICU, Peking Union Medical College Hospital, Beijing 100730, China) and Dr E Azabou (University of Versailles SQY) for helping with abstraction of information from papers in the Chinese language.
We would like to thank Prof Harald Herkner (Content Editor); Marialena Trivella (Statistical Editor); Peter Minneci, Charles Natanson, Gordon Guyatt, and Matthias Briel (Peer Reviewers), and Karen Hovhannisyan (Trials Search Co‐ordinator) for help and editorial advice provided during preparation of the 2010 updated review (Annane 2004). (At that time, Cochrane updates did not earn a new citation unless they had new review authors or included a change in conclusions.)
Appendices
Appendix 1. Search strategy for CENTRAL
#1 MeSH descriptor: [Sepsis] explode all trees
#2 MeSH descriptor: [Shock, Septic] explode all trees
#3 MeSH descriptor: [Systemic Inflammatory Response Syndrome] explode all trees
#4 MeSH descriptor: [Central Nervous System Bacterial Infections] explode all trees and with qualifier(s): [blood ‐ BL, complications ‐ CO, drug therapy ‐ DT]
#5 MeSH descriptor: [Pneumonia] explode all trees
#6 MeSH descriptor: [Community‐Acquired Infections] explode all trees and with qualifier(s): [complications ‐ CO, drug therapy ‐ DT]
#7 MeSH descriptor: [Respiratory Distress Syndrome, Adult] explode all trees and with qualifier(s): [complications ‐ CO, drug therapy ‐ DT]
#8 MeSH descriptor: [Acute Lung Injury] explode all trees and with qualifier(s): [complications ‐ CO, drug therapy ‐ DT]
#9 sepsis or (septic* NEAR/3 shock*)
#10 (bacterem* or bacteraem* or pyrexia or septicaem* or septicem*)
#11 SIRS or (Inflammatory next Response next Syndrome*)
#12 bacteria* NEAR infect* NEAR (blood* or serum or invas* or severe or systemic)
#13 ((community next acquired) or severe) NEAR pneumonia
#14 (acute or adult) NEAR/2 (respiratory NEAR/2 distress)
#15 (acute or adult) NEAR/2 (lung NEAR/2 injury)
#16 ARDS
#17 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16
#18 MeSH descriptor: [Adrenal Cortex Hormones] explode all trees
#19 MeSH descriptor: [Hydrocortisone] explode all trees
#20 MeSH descriptor: [Cortisone] explode all trees
#21 MeSH descriptor: [Steroids] explode all trees
#22 corticosteroid* or steroid* or cortison* or hydrocortison*
#23 methylprednisolon* or (methyl next prednisolon*) or betamethason* or dexamethason* or glucocorticoid* or fludrocortison* or mineralocorticoid*
#24 #18 or #19 or #20 or #21 or #22 or #23
#25 #17 and #24
#26 #25 in Trials
Appendix 2. Search strategy for MEDLINE (Ovid SP)
1 exp Sepsis/
2 exp Shock, Septic/
3 Systemic Inflammatory Response Syndrome/
4 exp Bacteremia/
5 Bacterial Infections/bl, dt, co
6 Pneumonia/co, dt
7 Community‐Acquired Infections/co, dt
8 Respiratory Distress Syndrome, Adult/co, dt
9 Acute Lung Injury/co, dt
10 (sepsis or septic*).mp.
11 (bacter?em* or septic?em* or pyrexia).mp.
12 (SIRS or Inflammatory Response Syndrome*).mp.
13 (bacteria* adj6 infect* adj6 (blood* or serum or invas* or severe or systemic)).mp.
14 ((community‐acquired or severe) adj3 pneumonia).mp.
15 ((acute or adult) adj2 (respiratory adj2 distress)).mp.
16 ARDS.mp.
17 ((acute or adult) adj2 (lung adj2 injury)).mp.
18 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17
19 exp Adrenal Cortex Hormones/
20 exp Hydrocortisone/
21 (corticosteroid* or steroid* or cortison* or hydrocortison*).mp.
22 (methylprednisolon* or betamethason* or dexamethason* or glucocorticoid* or fludrocortison* or mineralocorticoid*).mp.
23 19 or 20 or 21 or 22
24 18 and 23
25 ((randomized controlled trial or controlled clinical trial).pt. or randomi?ed.ab. or placebo.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti.) not (animals not (humans and animals)).sh.
26 24 and 25
Appendix 3. Search strategy for Embase (Ovid SP)
1 exp sepsis/
2 exp septic shock/
3 pneumonia/co, dt [Complication, Drug Therapy]
4 adult respiratory distress syndrome/co, dt [Complication, Drug Therapy]
5 acute lung injury/co, dt [Complication, Drug Therapy]
6 systemic inflammatory response syndrome/co, dt [Complication, Drug Therapy]
7 community acquired infection/co, dt [Complication, Drug Therapy]
8 (sepsis or (septic* adj5 shock) or (bacter?em* or pyrexia or septic?em*) or (SIRS or Inflammatory Response Syndrome*)).mp.
9 (bacteria* adj2 infect* adj2 (blood* or serum or invas* or severe or systemic)).mp.
10 (((community‐acquired or severe) adj2 pneumonia) or ((acute or adult) adj1 (respiratory adj1 distress)) or ((acute or adult) adj1 (lung adj1 injury)) or ARDS).mp.
11 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10
12 steroid/
13 corticosteroid/
14 cortisone/
15 hydrocortisone/
16 (corticosteroid* or steroid* or cortison* or hydrocortison* or (methylprednisolon* or methyl prednisolon* or betamethason* or dexamethason* or glucocorticoid* or fludrocortison* or mineralocorticoid*)).mp.
17 12 or 13 or 14 or 15 or 16
18 11 and 17
19 ((placebo or randomized controlled trial).sh. or controlled study.ab. or random*.ti,ab. or trial*.ti,ab.) not (animal not human).sh.
20 18 and 19
Appendix 4. Search strategy for LILACS (via BIREME)
(sepsis OR septic$ OR SEPSIS OR SEPTIC OR SIRS OR "septic shock" OR "SEPTIC SHOCK/" OR SEPTICEMIA OR PNEUMONIA OR bact* OR "adult respiratory distress syndrome" OR "acute lung injury" OR "systemic inflammatory response syndrome" OR "bacterial infection" OR "community acquired infection" ) (corticosteroid* OR steroid* OR glucocorticoid* OR CORTCOSTEROID* OR GLUCOCORTICOID/ OR STEROID OR MINERALOCORTICOID OR cortison* OR hydrocortison* OR fludrocortison* OR betamethason* OR methylprednisolon* OR prednison* OR dexamethason*)
Appendix 5. Unpublished data obtained from trial authors
| Studies | Type of unpublished data provided by primary authors |
| Annane 2002 | Full access to individual data, details for randomization, and blinding procedures |
| Annane 2010 | Full access to individual data, details for randomization, and blinding procedures |
| Annane 2018 | Full access to individual data, details for randomization, and blinding procedures |
| Arabi 2011 | Full access to individual data |
| Bollaert 1998 | Full access to individual data, details for randomization, and blinding procedures. Additional information on adrenal function (data according to the review definition: delta cortisol ≤ 9 µg/dL). Additional information for ICU length of stay and adverse events |
| Briegel 1999 | Full access to individual data, details for randomization, and blinding procedures. Additional information for ICU length of stay and adverse events |
| Chawla 1999 | Details for randomization and blinding procedures. Additional information for mortality, shock reversal, and ICU length of stay and adverse events |
| Cicarelli 2007 | Details for randomization and blinding procedures |
| Confalonieri 2005 | Full access to individual data, details for randomization, and blinding procedures |
| Gordon 2014 | Full access to individual data, details for randomization, and blinding procedures |
| Gordon 2016 | Full access to individual data, details for randomization, and blinding procedures |
| Hyvernat 2016 | Full access to individual data, details for randomization, and blinding procedures |
| Keh 2003 | Details for randomization and blinding procedures. Additional information for adverse events |
| Keh 2016 | Full access to individual data, details for randomization, and blinding procedures |
| Liu 2012 | Full access to individual data, details for randomization, and blinding procedures |
| Meduri 2007 | Details for randomization and blinding procedures. Additional information for subgroups of patients with sepsis or septic shock on mortality, ICU and hospital length of stay, and adverse events |
| Meduri 2009 | Full access to individual data, details for randomization, and blinding procedures |
| Meijvis 2011 | Separate information for patients with sepsis |
| Mirea 2014 | Full access to individual data, details for randomization, and blinding procedures |
| Oppert 2005 | Details for randomization and blinding procedures. Additional information for mortality, for outcomes of patients randomized and not analysed, shock reversal, and adverse events |
| Rinaldi 2006 | Details for randomization and blinding procedures. Additional information for mortality, for outcomes of patients randomized and not analysed, and adverse events |
| Sprung 1984 | Additional information for 28‐day all‐cause mortality |
| Sprung 2008 | Full access to individual data, details for randomization, and blinding procedures |
| Tandan 2005 | Details for randomization and blinding procedures |
| Tilouche 2019 | Additional information for mortality data at 6 months and 1 year, number of patients with shock reversal at day 28, mean and SD value for SOFA score at day 7, number of patients with at least 1 episode of severe glycaemia > 180 mg/dL |
| Tongyoo 2016 | Full access to individual data, details for randomization, and blinding procedures |
| Torres 2015 | Details for randomization and blinding procedures. Additional information for mortality, shock reversal, SOFA, length of stay, and adverse events |
| Yildiz 2002 | Details for randomization and blinding procedures. Additional information for mortality, hospital length of stay, and adverse events |
Appendix 6. Methodological quality of studies
Data and analyses
Comparison 1. Corticosteroids versus placebo or usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 28‐Day all‐cause mortality | 50 | 11233 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.84, 0.99] |
| 1.1 Studies reporting actual 28‐day mortality | 32 | 9387 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.87, 1.00] |
| 1.2 Studies reporting short‐term mortality at other timing | 18 | 1846 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.52, 0.95] |
| 2 28‐Day all‐cause mortality ‐ sensitivity analysis based on methodological quality | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Adequate generation of allocation sequence | 35 | 10076 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.87, 0.99] |
| 2.2 Adequate allocation concealment | 34 | 9972 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.87, 0.99] |
| 2.3 Blinded trials | 34 | 9894 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.87, 0.99] |
| 2.4 Studies judged at low risk of bias | 17 | 7896 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.84, 0.98] |
| 3 28‐Day all‐cause mortality by subgroups based on study drug | 47 | 11017 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.84, 1.00] |
| 3.1 Hydrocortisone | 25 | 6518 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.83, 1.05] |
| 3.2 Hydrocortisone plus fludrocortisone | 3 | 1564 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.77, 0.98] |
| 3.3 Prednisone/Prednisolone | 5 | 1236 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.71, 1.33] |
| 3.4 Methylprednisolone/Dexamethasone | 14 | 1699 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.61, 1.09] |
| 4 28‐Day all‐cause mortality by subgroups based on treatment dose/duration | 44 | 10812 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.86, 0.97] |
| 4.1 Long course of low‐dose corticosteroids | 39 | 9902 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.86, 0.97] |
| 4.2 Short course of high‐dose corticosteroids | 5 | 910 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.80, 1.16] |
| 5 28‐Day all‐cause mortality based on mode of drug administration | 45 | 9978 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.82, 0.99] |
| 5.1 Intravenous bolus | 27 | 4749 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.83, 1.02] |
| 5.2 Continuous infusion | 18 | 5229 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.66, 1.07] |
| 6 28‐Day all‐cause mortality based on mode of drug termination | 47 | 10906 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.83, 1.00] |
| 6.1 Without taper off | 30 | 8770 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.78, 0.98] |
| 6.2 With taper off | 17 | 2136 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.92, 1.18] |
| 7 28‐Day all‐cause mortality by subgroups based on age | 45 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Adults | 40 | 10169 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.83, 1.00] |
| 7.2 Children | 5 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.56, 2.09] |
| 8 28‐Day all‐cause mortality by subgroups based on targeted population | 50 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Sepsis | 10 | 1358 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.89, 1.37] |
| 8.2 Septic shock only | 23 | 7428 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.83, 1.00] |
| 8.3 Sepsis and ARDS | 4 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.45, 0.98] |
| 8.4 Sepsis and community‐acquired pneumonia | 13 | 2038 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.50, 1.00] |
| 9 28‐Day mortality in participants with critical illness‐related corticosteroid insufficiency | 12 | 1079 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.82, 1.03] |
| 10 90‐Day all‐cause mortality | 7 | 5934 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.87, 1.00] |
| 11 Long‐term mortality | 7 | 6236 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.91, 1.03] |
| 12 Intensive care unit mortality | 18 | 7267 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.83, 0.96] |
| 13 Hospital mortality | 26 | 8183 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.82, 0.99] |
| 14 Number of participants with shock reversal at day 7 | 16 | 6711 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.13, 1.34] |
| 15 Number of participants with shock reversal at 28 days | 13 | 6779 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [1.03, 1.08] |
| 16 SOFA score at day 7 | 10 | 2157 | Mean Difference (IV, Random, 95% CI) | ‐1.37 [‐1.84, ‐0.90] |
| 17 Length of intensive care unit stay for all participants | 21 | 7612 | Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.95, ‐0.19] |
| 18 Length of intensive care unit stay for survivors | 10 | 778 | Mean Difference (IV, Fixed, 95% CI) | ‐2.19 [‐3.93, ‐0.46] |
| 19 Length of hospital stay for all participants | 22 | 8795 | Mean Difference (IV, Random, 95% CI) | ‐1.63 [‐2.93, ‐0.33] |
| 20 Length of hospital stay for survivors | 9 | 710 | Mean Difference (IV, Random, 95% CI) | ‐4.11 [‐8.50, 0.28] |
| 21 Number of participants with adverse events | 31 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 Gastroduodenal bleeding | 26 | 5231 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.85, 1.35] |
| 21.2 Superinfection | 25 | 5356 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.95, 1.19] |
| 21.3 Hyperglycaemia | 20 | 8594 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [1.13, 1.22] |
| 21.4 Hypernatraemia | 6 | 5069 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [1.34, 2.06] |
| 21.5 Muscle weakness | 6 | 6145 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.01, 1.44] |
| 21.6 Neuropsychiatric event | 8 | 6941 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.53, 1.39] |
| 21.7 Stroke | 4 | 2842 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.41, 1.68] |
| 21.8 Cardiac event | 6 | 3567 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.66, 1.88] |
Comparison 2. Continuous infusion versus bolus administration of corticosteroids.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 28‐Day all‐cause mortality | 3 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.81, 1.31] |
| 2 90‐Day all‐cause mortality | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.61, 1.22] |
| 3 Long‐term mortality | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [1.02, 1.81] |
| 4 Intensive care unit mortality | 4 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.80, 1.29] |
| 5 Hospital mortality | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.72, 1.25] |
| 6 Number of participants with shock reversal at day 7 | 4 | 358 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.59, 1.10] |
| 7 Number of participants with shock reversal at day 28 | 1 | 70 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.45, 1.34] |
| 8 SOFA score at day 7 | 3 | 260 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [‐0.25, 2.26] |
| 9 Length of intensive care unit stay for all participants | 3 | 310 | Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐4.54, 2.45] |
| 10 Length of hospital stay for all participants | 3 | 310 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐5.05, 5.07] |
| 11 Number of participants with adverse events | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Gastrointestinal bleeding | 2 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.10, 6.37] |
| 11.2 Superinfection | 2 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.37, 3.33] |
| 11.3 Hyperglycaemia | 3 | 310 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.47, 1.71] |
| 11.4 Hypernatraemia | 2 | 187 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.34, 1.61] |
| 11.5 Muscle weakness | 1 | 70 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.13, 5.98] |
| 11.6 Neuropsychiatric event | 1 | 70 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.50, 4.86] |
| 11.7 Stroke | 1 | 70 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.8 Cardiac event | 1 | 70 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aboab 2008.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 23) with septic shock and adrenal insufficiency as defined by a cortisol response to 250 µg synacthene (delta cortisol) ≤ 9 µg/dL Setting: intensive care unit Study location: France |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted study authors and they could not provide missing data Funding source: authors' institution (public source) Data were extracted by BR Risk of bias was assessed by EB and BR |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Annane 2002.
| Methods | Randomized controlled trial with 2 parallel groups 19 centres Dates study was conducted: from October 1995 to February 1999 |
|
| Participants | Adults (n = 300) with vasopressor‐ and ventilator‐dependent septic shock Stratification according to cortisol response to 250 µg synacthene for non‐responders (delta cortisol ≤ 9 µg/dL) and responders (> 9 µg/dL) Setting: intensive care unit Study location: France |
|
| Interventions |
Treatments have to be initiated within 8 hours from shock onset |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: French Ministry of Health Data were extracted by JB Risk of bias were assessed by RP and BR |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Annane 2010.
| Methods | Randomized controlled trial with 2 × 2 factorial design 11 centres Dates study was conducted: from July 2014 to October 2014 |
|
| Participants | Adults (n = 509) with vasopressor‐dependent septic shock Subgroups based on adrenal status assess by a 250‐µg ACTH test Setting: intensive care unit Study location: France |
|
| Interventions |
Treatments have to be initiated within 24 hours from shock onset |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: French Ministry of Health Data were extracted by EB Risk of bias was assessed by EB and BR |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization through a secured website |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Annane 2018.
| Methods | Randomized controlled trial with 2 × 2 factorial design 34 centres Dates study was conducted: from July 2014 to October 2014 |
|
| Participants | Adults (n = 1241) with vasopressor‐dependent septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study location: France |
|
| Interventions |
Treatments have to be initiated within 24 hours from shock onset |
|
| Outcomes |
Primary
Secondary
Safety outcomes included
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: French Ministry of Health Data were extracted by BR Risk of bias was assessed by BR and RP |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Arabi 2011.
| Methods | Randomized controlled trial 1 centre Dates study was conducted: from April 2004 to October 2007 |
|
| Participants | Adults (n = 75) with liver cirrhosis and septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study location: Saudi Arabia |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
Outcomes were also analysed in relation to adrenal insufficiency |
|
| Notes | We contacted authors and obtained access to individual patient data Funding source: King Abdulaziz City for Science and Technology |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Use of sealed envelopes by pharmacists |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Pharmacists: no Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unexplained discrepancy between reported K‐M curves and number of deaths at 28 days in placebo arm |
| Selective reporting (reporting bias) | Low risk | Access to unpublished data |
| Other bias | High risk | Trial terminated prematurely after enrolment of 75 participants; planned sample size was 150 |
Blum 2015.
| Methods | Multi‐centre. randomized, placebo‐controlled, 2‐parallel‐group study Dates study was conducted: from December 2009 to May 2014 |
|
| Participants | Adults (n = 800) patients hospitalized with community‐acquired pneumonia Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: emergency and medical wards Study location: Switzerland |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to trial protocol and some missing data Funding source: Swiss National Science Foundation, Viollier AG, Nora van Meeuwen Haefliger Stiftung, Julia und Gottfried Bangerter‐Rhyner Stiftung |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Low risk | Randomization was centralized Generator and executor of randomization were separated Variable block sizes of 4 to 6 |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Outcomes reported matched outcomes planned by trial protocol, which was publicly released before the end of the recruitment period |
| Other bias | Low risk | Contact with trial authors; access to trial protocol but could not identify areas of bias |
Bollaert 1998.
| Methods | Randomized controlled trial with 2 parallel groups 2 centres Dates the study was conducted: not reported |
|
| Participants | Adults (n = 41) with vasopressor‐ and ventilator‐dependent septic shock Stratification according to cortisol response to 250 µg synacthene for non‐responders (delta cortisol ≤ 6 µg/dL) and responders (> 6 µg/dL) Setting: intensive care unit Study location: France |
|
| Interventions |
Treatments have to be initiated after 48 hours or longer from shock onset |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: Nancy University Hospital. Data were extracted by DA Risk of bias was assessed by DA and EB |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Bone 1987.
| Methods | Randomized controlled trial with 2 parallel groups 19 centres Dates study was conducted: from November 1982 to December 1985 |
|
| Participants | Adults (n = 382) with sepsis (n = 234) or septic shock (n = 148) Setting: intensive care unit Study location: USA |
|
| Interventions |
Treatments have to be initiated 2 hours from time entry criteria were met |
|
| Outcomes |
Primary
|
|
| Notes | We did not contact study authors Funding source: Upjohn Company |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol to exclude reporting bias |
| Other bias | Low risk | No access to full data including screening log to exclude selection bias |
Briegel 1999.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from November 1993 to September 1996 |
|
| Participants | Adults (n = 40) with vasopressor‐ and ventilator‐dependent septic shock Setting: intensive care unit Study location: Germany |
|
| Interventions |
Treatments have to be initiated within 72 hours from shock onset |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: Friedrich‐Baur‐Stiftung, Germany, by departmental funds Data were extracted by DA Risk of bias was assessed by DA and EB |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Adequate randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Access to full data including screening log |
Chawla 1999.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 44) with vasopressor‐dependent septic shock Setting: intensive care unit Study location: USA |
|
| Interventions |
Treatments have to be initiated after 72 hours or longer from shock onset |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to trial protocol and some missing data Funding source: not declared Data were extracted by DA Risk of bias was assessed by DA and EB |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list was kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Access to full data including screening log |
Cicarelli 2007.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from November 2004 through December 2005 |
|
| Participants | Adults (n = 29) with vasopressor‐dependent septic shock Setting: intensive care unit Study location: Brazil |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted study authors and obtained information on study design but no additional unpublished data Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Lost to follow‐up: none; 3 participants were withdrawn after next of kin refused to consent |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol to rule out reporting bias |
| Other bias | Unclear risk | No access to data to rule out selection bias |
Confalonieri 2005.
| Methods | Randomized controlled trial with 2 parallel groups 6 centres Dates study was conducted: from July 2000 through March 2003 |
|
| Participants | Adults (n = 46) with severe community‐acquired pneumonia Setting: intensive care unit Study location: Italy |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: Assisi Foundation of Memphis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: 2 at 60 days after randomization, all in the placebo group |
| Selective reporting (reporting bias) | Low risk | Access to full data including screening log |
| Other bias | High risk | Study was stopped prematurely for apparent benefit; no sample size was defined a priori, but study authors used the triangular test as a stopping rule, analysing the primary outcome after each 20 participants |
CSG 1963.
| Methods | Randomized controlled trial with 2 parallel groups 5 centres |
|
| Participants | Adults (n = 194), and children (n = 135) with vasopressor‐dependent septic shock Setting: intensive care unit Study location: USA |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not given |
| Allocation concealment (selection bias) | Unclear risk | Not given |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants: yes Caregivers: yes Data collectors: unclear Outcome assessors: unclear Data analysts: unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol to exclude reporting bias |
| Other bias | Unclear risk | No access to data to exclude selection bias |
Doluee 2018.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from August 2014 to April 2015 |
|
| Participants | Adults (n = 160) that did not respond to vasopressor therapy for longer than 60 minutes Subgroup based on adrenal status as assessed by 250‐µg ACTH given intramuscularly Setting: intensive care unit Study location: Iran |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | Study authors contacted but did not reply Funding source: Mashhad University of Medical Sciences |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information was provided on method for generating the randomization list |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information was provided on who was blinded to study drug, albeit it is stated that hydrocortisone was compared to placebo (serum saline) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Reported outcomes in the publication matched those planned in the protocol as recorded in the Iranian Registry of Clinical Trials (https://en.irct.ir/trial/12131?revision=12131; accessed 7 April 2019) |
| Other bias | Unclear risk | No access to data to exclude selection bias |
El Ghamrawy 2006.
| Methods | Randomized trial on 2 parallel groups Single centre Dates study was conducted: not reported |
|
| Participants | Adults (n= 34) with severe community‐acquired pneumonia Setting: intensive care unit Study location: Saudi Arabia |
|
| Interventions | Hydrocortisone 200 mg intravenous bolus followed by infusion at 10 mg/h for 7 days | |
| Outcomes |
|
|
| Notes | Study authors contacted but did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information reported |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Insufficient information reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information reported |
| Other bias | Unclear risk | Insufficient information reported |
El‐Nawawy 2017.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Children (n = 96) aged 1 month to 4 years with septic shock Subgroups based on adrenal status assess by a 250‐µg ACTH test Setting: intensive care unit Study location: Egypt |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Study authors contacted but did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information was provided on the method used for generating the randomization list |
| Allocation concealment (selection bias) | Unclear risk | No information was provided on the method used for randomization concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol to exclude reporting bias |
| Other bias | Unclear risk | No access to data to exclude selection bias |
Fernández‐Serrano 2011.
| Methods | Randomized trial on 2 parallel groups Single centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 56) with severe community‐acquired pneumonia without shock and spontaneously breathing Setting: respiratory medicine department Study location: Spain |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | Study authors contacted but did not reply Funding source: Fondo de Investigaciones Sanitarias (FIS) and partial funding from ISCIII RTIC (Red Respira) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Low risk | Generator and executor of randomization were separated |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | > 10% of participants not analysed |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in the publication matched those planned in the protocol as released on ISRCTN registry |
| Other bias | Unclear risk | Insufficient information |
Gordon 2014.
| Methods | Randomized controlled trial with 2 parallel groups 4 centres Dates study was conducted: from October 2010 through March 2012 |
|
| Participants | Adults (n = 61) with septic shock on a maximal dose of vasopressin up to 0.06 U/min Setting: intensive care unit Study location: UK |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: National Institute for Health Research |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers prepared by an independent statistician |
| Allocation concealment (selection bias) | Low risk | Randomization done via an online system |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Hydrocortisone and its placebo presented in indiscernible forms |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Reported information matched published statistical plan |
| Other bias | Low risk | Accessed unpublished information to exclude other risk of bias |
Gordon 2016.
| Methods | Randomized controlled trial with 2 × 2 factorial design 18 centres Dates study was conducted: from February 2013 through May 2015 |
|
| Participants | Adults (n = 409) with septic shock requiring vasopressors despite fluid resuscitation within a maximum of 6 hours after onset of shock Setting: intensive care unit Study location: UK |
|
| Interventions |
Hydrocortisone or its placebo was started only when maximum dose for vasopressin or norepinephrine was reached to maintain the target mean arterial pressure of 65 to 75 mmHg |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: National Institute for Health Research |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Hu 2009.
| Methods | Randomized controlled trial 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 77) with septic shock Setting: intensive care unit Study location: China |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated in the manuscript |
| Allocation concealment (selection bias) | Unclear risk | Not stated in the manuscript |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated in the manuscript |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Huang 2014.
| Methods | Randomized controlled trial with 3 parallel groups Single centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 60) with sepsis Setting: intensive care unit Study location: China |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: yes Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Huh 2007.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from July 2005 through June 2006 |
|
| Participants | Adults (n = 82) with septic shock and adrenal insufficiency Setting: intensive care unit Study location: South Korea |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors, who did not reply Fundig source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Unclear risk | Not given |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No explicit information on plan analysis |
| Other bias | Unclear risk | No information |
Hyvernat 2016.
| Methods | Randomized controlled trial with 2 parallel groups 4 centres Dates study was conducted: from November 2008 through June 2010 |
|
| Participants | Adults (n = 120) with septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study location: France |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Fundng source: Association Niçoise de Réanimation Médicale |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | No evidence of other bias |
Keh 2003.
| Methods | Randomized controlled trial with cross‐over design 1 centre Dates study was conducted: from March 1997 through September 2000 |
|
| Participants | Adults (n = 40) with vasopressor‐dependent septic shock Setting: intensive care unit Study location: Germany |
|
| Interventions |
All participants received hydrocortisone for 3 days preceded or followed by placebo for 3 days |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding sources: Deutsche Forschungsgemeinschaft (expenses for analytes) and Pharmacia/Upjohn (expenses for patients’ insurance) Data were extracted by DA Risk of bias was assessed by DA and BR |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol |
| Other bias | Low risk | Full access to data including screening log |
Keh 2016.
| Methods | Randomized controlled trial with 2 parallel groups 34 centres Dates study was conducted: from January 2009 to August 2013 |
|
| Participants | Adults (n = 380) with severe sepsis who were not in septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study location: Germany |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding sources: Charité–Universitätsmedizin Berlin and grant from the German Federal Ministry of Education and Research Data were extracted by DA Risk of bias was assessed by DA and BR |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Kurungundla 2008.
| Methods | Randomized trial with 2 parallel groups Single centre |
|
| Participants | Adults (n = 21) with sepsis Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study location: USA |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted the study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not reported |
Li 2016.
| Methods | Randomized trial with 2 parallel groups Single centre Dates study was conducted: from May 2014 to February 2016 |
|
| Participants | Adults (n = 58) with community‐acquired pneumonia and septic shock Setting: intensive care unit Study location: China |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted the study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information reported |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol |
| Other bias | Unclear risk | Insufficient information reported |
Liu 2012.
| Methods | Randomized controlled trial with parallel groups 1 centre Dates the study was conducted: not reported |
|
| Participants | Adults (n = 26) with ARDS and sepsis, including septic shock (n = 12), and with critical illness‐associated corticosteroid insufficiency Setting: intensive care unit Study location: China |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted the study authors and obtained access to individual patient data Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Unclear risk | No explicit information in the manuscript |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No explicit information in the manuscript |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No explicit information in the manuscript |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Loisa 2007.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from July 2005 through April 2006 |
|
| Participants | Adults (n = 48) with septic shock Setting: intensive care unit Study location: Finland |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted the study authors, who did not reply Fuding source: Medical Research Fund of Tampere University Hospital and Medical Research Fund of Päijät‐Häme Central Hospital, Lahti |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated by study authors |
| Allocation concealment (selection bias) | Unclear risk | Not stated by study authors |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated by study authors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated by study authors |
| Selective reporting (reporting bias) | Unclear risk | Not stated by study authors |
| Other bias | Unclear risk | Not stated by study authors |
Luce 1988.
| Methods | Randomized controlled trial 1 centre |
|
| Participants | Adults (n = 75) with sepsis and septic shock Setting: intensive care unit Study location: USA |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and their data were no longer available Funding source: National Heart, Lung and Blood Institute, and Upjohn Company |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 out of 87 randomly assigned participants were not analysed, and follow‐up was not provided |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol |
| Other bias | Unclear risk | No access to data to exclude selection bias |
Lv 2017.
| Methods | Randomized controlled trial with parallel groups 1 centre Dates study was conducted: from September 2015 to September 2016 |
|
| Participants | Adults (n = 118) with septic shock that has developed within 6 hours before randomization Setting: intensive care unit Study location: China |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
McHardy 1972.
| Methods | Randomized trial on 4 parallel groups Single centre Dates study was conducted: not reported |
|
| Participants | Children age > 12 years and adults (n = 126) with severe community‐acquired pneumonia Setting: respiratory wards Study location: Scotland |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We did not contact study authors Funding source: anonymous gift to the Department of Respiratory Diseases, University of Edinburgh |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Meduri 2007.
| Methods | Randomized controlled trial (2:1 scheme) 5 centres Dates the study was conducted: from April 1997 through April 2002 |
|
| Participants | Adults (n = 91) with early ARDS (≤ 72 hours from diagnosis of ARDS); 61 (67%) had sepsis or septic shock, and the primary author provided separate data for these participants Stratification according to cortisol response to 250 µg synacthene for non‐responders (delta cortisol ≤ 9 µg/dL) and responders (> 9 µg/dL) Setting: intensive care unit Study location: USA |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | If participant failed to improve on LIS between day 7 and day 9, he/she received open‐label methylprednisolone at 2 mg/kg/d for unresolving ARDS We contacted study authors, who provided separate data for patients with sepsis Funding source: Baptist Memorial Health Care Foundation and the Assisi Foundation of Memphis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full access to data excluding any attrition bias |
| Selective reporting (reporting bias) | Low risk | Full access to data including screening log ‐ reported outcomes matched those planned in protocol |
| Other bias | High risk | Study was stopped prematurely for efficacy |
Meduri 2009.
| Methods | Randomized controlled trial with 2 parallel groups, stratified according to absence of shock and a multiple organ dysfunction score (MODS) < 3 (strata A), or presence of shock and MODS ≥ 3 (strata B) 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 80) with sepsis with or without septic shock Setting: intensive care unit Study location: USA |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | Study was published as an abstract only. We contacted study authors and obtained access to individual patient data Funding source: Baptist Memorial Health Care Foundation and Assisi Foundation of Memphis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full access to data excluding any attrition bias |
| Selective reporting (reporting bias) | Low risk | Study was stopped prematurely for efficacy |
| Other bias | Unclear risk | Full access to data including screening log Some imbalance in numbers allocated to hydrocortisone versus placebo |
Meijvis 2011.
| Methods | Randomized controlled trial with 2 parallel groups 2 centres Dates the study was conducted: from November 2007 to September 2010 |
|
| Participants | Adults (n = 304) with confirmed community‐acquired pneumonia Setting: emergency departments and medical wards Study location: The Netherlands |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained separate data for patients with sepsis Funding source: no funding source identified for this study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Pharmacist: no Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in the study protocol are reported in the final analysis |
| Other bias | Low risk | Full access to study protocol |
Menon 2017.
| Methods | Randomized controlled trial with 2 parallel groups 7 centres Dates study was conducted: from July 2014 through March 2016 |
|
| Participants | Children (n = 57) newborn to 17 years old inclusive with suspected septic shock on vasopressor therapy from 1 to 6 hours before randomization Setting: intensive care unit Study location: Canada |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: Canadian Institutes of Health Research (CIHR) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization through a secured website |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Access to study protocol with no evidence of other bias |
Mirea 2014.
| Methods | Randomized controlled trial with 3 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 171) with septic shock Setting: intensive care unit Study location: Romania |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol and to raw data of individual patients excluding reporting bias |
| Other bias | Low risk | Full access to raw data of individual patients including screening log |
Nafae 2013.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 80) with severe community‐acquired pneumonia Setting: chest department, respiratory, intensive care unit, general medicine department, and general medicine intensive care unit Study location: Egypt |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information reported |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Insufficient information reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information reported |
| Other bias | Unclear risk | Insufficient information reported |
Nagy 2013.
| Methods | Randomized controlled trial performed on 2 parallel groups Single centre Dates study was conducted: from June 2007 through September 2009 |
|
| Participants | Children (n = 59) with severe community‐acquired pneumonia Setting: Department of Paediatric Medical Health Study location: Hungary |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: New Hungary Development Plan, co‐financed by the European Social Fund and the European Regional Development Fund |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence of random numbers for parallel groups was computer generated without block randomization |
| Allocation concealment (selection bias) | Unclear risk | No information given on how people were blinded to randomization list |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: unclear Data analysts: unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reported outcomes matched outcomes released on EudraCT registry |
| Other bias | Low risk | No evidence of other source of bias. Trial was completed with planned number of participants |
Ngaosuwan 2018.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates the study was conducted: from October 2014 to October 2016 |
|
| Participants | Adults (n = 80) with septic shock Setting: intensive care unit Study location: Thailand |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted study authors, who did not provide additional information Funding source: Srinakharinwirot University |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Reported outcomes in publication matched planned outcomes as released on clinicaltrial.gov registry |
| Other bias | Unclear risk | Study authors did not reply, and we could not access full protocol |
Oppert 2005.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 40) with vasopressor‐dependent septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study location: Germany |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained details for randomization and blinding procedures, along with additional information for mortality, for outcomes of participants randomized and not analysed, for shock reversal, and for adverse events Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7 of 48 randomly assigned participants were not analysed: 5 in the corticosteroid group and 2 in the placebo group. 4 of these 7 participants were lost to follow‐up, and 3 died (all in the steroid group) |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data including screening log |
Rezk 2013.
| Methods | Randomized controlled trial (2:1 scheme) with 2 parallel groups 1 centre Dates study was conducted: from October 2011 through October 2012 |
|
| Participants | Adults (n = 27) with ARDS and hospital‐ or community‐acquired pneumonia Setting: intensive care unit Study location: Egypt |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors, who did not provide additional information Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No explicit information in the manuscript |
| Allocation concealment (selection bias) | Unclear risk | No explicit information in the manuscript |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No explicit information in the manuscript |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Rinaldi 2006.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: not reported |
|
| Participants | Adults (n = 40) with sepsis and not receiving vasopressor support Setting: intensive care unit Study location: Italy |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained details for randomization and blinding procedures, along with additional information for mortality, for outcomes of participants randomized and not analysed, and for adverse events Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12 of 52 participants dropped out of the study: 6 in the control group and 6 in the corticosteroid group; contact with the primary author permitted completion of follow‐up for all 12 participants |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding any reporting bias |
| Other bias | Low risk | Full access to data including screening log |
Sabry 2011.
| Methods | Randomized controlled trial 3 centres Dates the study was conducted:from July 2010 through January 2011 |
|
| Participants | Adults (n = 80) admitted to ICU with community‐acquired pneumonia and sepsis Setting: intensive care unit Study location: Egypt |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors, who did not provide additional information Funding source: authors' institution (public) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information in the manuscript |
| Allocation concealment (selection bias) | Unclear risk | No information in the manuscript |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information in the manuscript |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information in the manuscript |
| Other bias | Unclear risk | No information in the manuscript |
Schumer 1976.
| Methods | Randomized controlled trial with 3 parallel groups 1 centre Dates the study was conducted: from 1967 through 1975 |
|
| Participants | Adults (n = 172) with septic shock with positive blood culture Setting: surgical department Study location: USA |
|
| Interventions |
Treatments might have been repeated once after 4 hours and had to be initiated at the time of diagnosis |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomized card system |
| Allocation concealment (selection bias) | High risk | Unsealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants: yes Caregivers: unclear Data collectors: unclear Outcome assessors: unclear Data analysts: unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol |
| Other bias | Unclear risk | No data to exclude selection bias |
Slusher 1996.
| Methods | Randomized controlled trial 2 centres Dates the study was conducted: from September 1991 through October 1992 |
|
| Participants | African children (n = 72; 1 to 16 years of age) with sepsis or septic shock Setting: 2 rural hospitals in Africa Study location: USA, Kenya, and Nigeria |
|
| Interventions |
Treatments had to be initiated 5 to 10 minutes before first dose of antibiotic |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: Roche Pharmaceuticals donated ceftriaxone and provided partial financial support for the study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not given |
| Allocation concealment (selection bias) | Unclear risk | Unclear; not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol |
| Other bias | Unclear risk | No data to exclude selection bias |
Snijders 2010.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates the study was conducted: from August 2005 through July 2008 |
|
| Participants | Adults (n = 213) with severe community‐acquired pneumonia Setting: medical wards Study location: The Netherlands |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and did not obtain additional information Funding source: unrestricted grant by Astra Zeneca |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Pharmacist: no Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in study protocol are reported in final analysis |
| Other bias | Unclear risk | No access to full protocol |
Sprung 1984.
| Methods | Randomized controlled trial with 3 parallel groups 2 centres Dates the study was conducted: from August 1979 to February 1982 |
|
| Participants | Adults (n = 59) with vasopressor‐dependent septic shock Setting: intensive care unit Study location: USA |
|
| Interventions |
Treatments might have been repeated once after 4 hours if shock persisted, and they had to be initiated at time of diagnosis |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained additional data (i.e. 28‐day all‐cause mortality) Funding source: Veterans Administration and Upjohn Company |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | High risk | At 1 centre, not clear how randomization list was kept confidential |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: yes at 1 centre, no at the other Caregivers: yes at 1 centre, no at the other Data collectors: yes at 1 centre, no at the other Outcome assessors: yes at 1 centre, no at the other Data analysts: unclear University of Miami Research Committee did not allow study to be performed in a double‐blind manner, nor for participants to receive placebo |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol |
| Other bias | Unclear risk | No data to exclude selection bias |
Sprung 2008.
| Methods | Randomized controlled trial with 2 parallel groups 52 centres Dates the study was conducted: from March 2002 to November 2005 |
|
| Participants | Adults (n = 499) with septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit Study locations: Europe and Israel |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding sources: contract (QLK2‐CT‐2000‐00589) from the European Commission, the European Society of Intensive Care Medicine, the European Critical Care Research Network, the International Sepsis Forum, and the Gorham Foundation. Roche Diagnostics provided the Elecsys cortisol immunoassay Data were extracted by EB Risk of bias was assessed by EB and BR |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Lost to follow‐up: none; 1 participant withdrew his consent Data for serious adverse events reported for only 466 of 499 participants, and analysis of these outcomes performed per‐protocol, not by intent‐to‐treat |
| Selective reporting (reporting bias) | Low risk | Access to study protocol and to raw data of individual participants to confirm absence of reporting bias |
| Other bias | High risk | Only 500 participants included; expected sample size 800 participants |
Sui 2013.
| Methods | Randomized controlled trial with 2 parallel groups Single centre Dates the study was conducted: not reported |
|
| Participants | Adults (n = 60) with severe community‐acquired pneumonia Setting: medical wards Study location: China |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information reported |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information reported |
| Other bias | Unclear risk | Insufficient information reported |
Tagaro 2017.
| Methods | Randomized trial performed on 2 parallel groups 9 centres Dates the study was conducted: 1 January 2011, and 31 May 2015 |
|
| Participants | Children (n = 60), ranging in age from 1 month to 14 years, with community‐acquired pneumonia and pleural effusion Setting: intensive care unit Study location: Spain |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | Source of funding: Spanish Ministry of Health and Sociedad de Pediatría de Madrid y Castilla La Mancha. Kern Pharma, Inc, Barcelona, Spain, supplied the drugs (dexamethasone and saline) and randomization. We did not contact trial authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme performed by manufacturer of the study drug (Kern Pharma, Barcelona, Spain) |
| Allocation concealment (selection bias) | Low risk | Use of prepackaged boxes provided by manufacturer of the study drug (Kern Pharma, Barcelona, Spain). The boxes were numbered consecutively for each hospital, severity stratum, and patient, according to the randomization scheme. They contained 15 transparent ampoules of dexamethasone or placebo, which were indiscernible from each other |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | No difference between planned outcomes as released on ClinicalTrial.gov registry and reported outcomes in the main publication |
| Other bias | Low risk | No evidence for other bias ‐ trial was completed with planned sample size |
Tandan 2005.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates the study was conducted: not reported |
|
| Participants | Adults (n = 28) with septic shock and adrenal insufficiency Setting: intensive care unit Study location: India |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained information on study design but no additional data Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the local pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Lost to follow‐up: unknown; data reported only as an abstract with minimal information to allow accurate assessment of bias |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol; data reported only as an abstract with minimal information to allow accurate assessment of bias |
| Other bias | Unclear risk | Data reported only as an abstract with minimal information to allow accurate assessment of bias |
Tilouche 2019.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from April 2013 through June 2016 |
|
| Participants | Adults (n = 70) with septic shock Setting: intensive care unit Study location: Tunisia |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained additional information and unpublished data Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Reported outcomes matched those mentioned in trial protocol |
| Other bias | Low risk | No evidence for other risk of bias |
Tongyoo 2016.
| Methods | Randomized controlled trial with 2 parallel groups 1 centre Dates study was conducted: from December 2010 through December 2014 |
|
| Participants | Adults (n = 197) with septic shock and ARDS Setting: intensive care unit Study location: Thailand |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained access to individual patient data Funding source: Siriraj critical care research funding |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | Full access to data excluding selection bias |
Torres 2015.
| Methods | Randomized controlled trial with 2 parallel groups 3 centres Dates the study was conducted: from June 2004 through February 2012 |
|
| Participants | Adults (n = 61) with both severe CAP and high inflammatory response, defined as levels of C‐reactive protein > 15 mg/dL on admission Setting: intensive care unit Study location: Spain |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained details for randomization and blinding procedures, along with additional information for mortality, shock reversal, SOFA, length of stay, and adverse events Funding source: SEPAR, SOCAP, FUCAP, SGR‐2011, Fondo de Investigación Sanitaria, IDIBAPS, CIBERES |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to full protocol and unpublished information |
| Other bias | Low risk | Access to full protocol and unpublished information |
Valoor 2009.
| Methods | Randomized controlled trial on 2 parallel groups 1 centre Dates the study was conducted: not reported |
|
| Participants | Children (n = 38; 2 months to 12 years of age) with septic shock unresponsive to fluid therapy alone Setting: intensive care unit Study location: India |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No explicit information in the manuscript |
| Allocation concealment (selection bias) | Unclear risk | No explicit information in the manuscript |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
VASSCSG 1987.
| Methods | Randomized controlled trial 10 centres |
|
| Participants | Adults (n = 223) with sepsis or septic shock (n = 100) Setting: intensive care unit Study location: USA |
|
| Interventions |
Treatment had to be initiated within 2 hours |
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We did not contact study authors Funding source: Veterans Administration Cooperative Studies Program, Medical Research Service, Veterans Administration Central Office, Washington, DC |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol |
| Other bias | Unclear risk | No data to exclude selection bias |
Venkatesh 2018.
| Methods | Randomized controlled trial with 2 parallel groups 69 centres Dates the study was conducted: from March 2013 to April 2017 |
|
| Participants | Adults (n = 3800) with vasopressor‐ and ventilator‐dependent septic shock Setting: intensive care unit Study locations: Australia, Denmark, New Zeland, Saudi Arabia, UK |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and did not obtain additional data Funding source: National Health and Medical Research Council of Australia; Pfizer (which supplied hydrocortisone); Radpharm Scientific (which supplied placebo) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Low risk | Access to study protocol excluding reporting bias |
| Other bias | Low risk | No evidence for other bias |
Yildiz 2002.
| Methods | Randomized controlled trial 1 centre Dates study was conducted: May 1997 to April 1999 |
|
| Participants | Adults (n = 40) with sepsis (n = 14), severe sepsis (n = 17), and septic shock (n = 9) Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit and infectious disease department Study location: Turkey |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
|
|
| Notes | We contacted study authors and obtained details for randomization and blinding procedures, along with additional information for mortality, hospital length of stay, and adverse events Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme |
| Allocation concealment (selection bias) | Low risk | Randomization list kept confidential by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Other bias | Unclear risk | No data to exclude selection bias |
Yildiz 2011.
| Methods | Randomized controlled trial on 2 parallel groups 1 centre Dates the study was conducted: April 2005 and May 2008 |
|
| Participants | Adults (n = 55) with sepsis or septic shock Subgroups based on adrenal status assessed by a 250‐µg ACTH test Setting: intensive care unit and infectious disease department Study location: Turkey |
|
| Interventions |
|
|
| Outcomes |
Primary
Secondary
Outcomes were also assessed in relation to adrenal insufficiency |
|
| Notes | We contacted study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers used |
| Allocation concealment (selection bias) | Low risk | Randomization list kept by the pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Pharmacist: no Participants: yes Caregivers: yes Data collectors: yes Outcome assessors: yes Data analysts: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up: none |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Zhou 2015.
| Methods | Randomized controlled trial on 2 parallel groups 1 centre Dates the study was conducted: January 2008 to January 2013 |
|
| Participants | Adults (n = 46) with community‐acquired pneumonia and ARDS Setting: intensive care unit Study location: China |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | We contacted study authors, who did not reply Funding source: not declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Pharmacist: no Participants: no Caregivers: no Data collectors: no Outcome assessors: no Data analysts: no |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
ACTH: adrenocorticotrophin hormone.
AKIN: Acute Kidney Injury Network.
APACHE II: Acute Physiology and Chronic Health Evaluation II.
ARDS: acute respiratory distress syndrome.
CAP: community‐acquired pneumonia.
CRP: C‐reactive protein.
FiO₂: fractional inspired oxygen.
ICD‐10: International Classification of Disease ‐ version 10.
ICU: intensive care unit.
K‐M curves: Kaplan‐Meier curves.
LIS: Lung Injury Scale score.
MOD: multiple organ dysfunction.
PaO₂: arterial oxygen tension.
PELOD: paediatric logistic organ dysfunction score.
PICU: paediatric intensive care unit.
SaO₂: saturated oxygen.
SOFA: sequential organ failure assessment.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Asehnoune 2014 | This study has compared hydrocortisone plus fludrocortisone vs placebo in patients with traumatic brain injury and not in sepsis |
| Bernard 1987 | Mixed population of patients with refractory hypoxia; separate data on patients with sepsis not available |
| Cicarelli 2006 | Mixed population of critically ill patients; separate data on patients with sepsis not available |
| Hahn 1951 | Patients with acute streptococcal infection This trial investigated effects of hydrocortisone on fever, anti‐streptolysin titers, and onset of rheumatic fever. No data are reported for analysis of the various outcomes considered in this systematic review |
| Huang 2014a | This study has compared in adults with community‐acquired Mycoplasma pneumoniae pneumonia early (within 12 hours) vs late (at 72 hours) administration of methylprednisolone on clinical course |
| Huang 2015 | This study included severely burned patients without sepsis |
| Hughes 1984 | Only acute effects (within 1 hour) of methylprednisolone and/or naloxone on haemodynamic data were available; no data for any of the outcomes considered in this systematic review were reported |
| Kaufman 2008 | In this study, participants were randomly assigned to receive hydrocortisone or its placebo for 24 hours only. Then, treatment with open‐labelled hydrocortisone was given at physicians' discretion. This study was aimed at exploring effects of hydrocortisone on immune cell function |
| Klastersky 1971 | This study was not a randomized trial. Investigators did not describe how participants were allocated to experimental treatment |
| Lan 2015 | This study focused on methylprednisolone effects on cytokines levels in the bronchoalveolar lavage fluid in children with Mycoplasma pneumoniae pneumonia without providing information about outcomes relevant for this review |
| Lucas 1984 | This study was not a randomized trial. Participants were allocated to experimental treatment according to their hospital number |
| Luo 2014 | This study compared prednisolone as an adjunct therapy to antibiotics vs antibiotics alone in children with refractory Mycoplasma pneumoniae pneumonia. Researchers focused on short‐term improvement in clinical symptoms and on variations in serum ferritin and LDH levels. None of the outcomes relevant for this review were assessed in this study |
| Marik 1993 | This study compared effects of a short course (single bolus) of high‐dose (10 mg/kg) hydrocortisone given before antibiotics to adults with community‐acquired pneumonia. The trial focused on treatment effects on circulating levels of tumour necrosis factor and on short‐term clinical course without providing information about outcomes relevant for this review |
| McKee 1983 | Mixed population of critically ill patients; separate data on septic shock not available |
| Meduri 1998b | This trial included participants with late acute respiratory distress syndrome phase ‐ not those with sepsis |
| Mikami 2007 | This study included participants with community‐acquired pneumonia and explicitly excluded patients with sepsis, those needing admission to the intensive care unit, and those requiring mechanical ventilation |
| Newberry 2017 | This study assessed the effects of adjuvant prednisolone treatment in HIV‐exposed infants aged 2‐6 months. Thus study suggested that corticosteroids significantly reduced mortality at hospital discharge and at 6 months. |
| Peeters 2018 | This trial compared ACTH responses to 100 µg IV CRH and placebo in 3 cohorts of 40 matched patients in the acute (ICU‐day 3‐6), subacute (ICU‐day 7‐16) or prolonged phase (ICU‐day 17‐28) of critical illness, with 20 demographically matched healthy subjects. CRH or placebo was injected in random order on two consecutive days |
| Rogers 1970 | Study published only as an abstract; no contact with study authors was possible; incomplete information on primary and secondary outcomes |
| Roquilly 2011 | This study has assessed the effects of hydrocortisone on the onset of ventilator‐associated pneumonia in adults with multiple trauma and not in sepsis |
| Schwingshackl 2016 | This trial included children within 72 hours of onset of acute respiratory distress syndrome of various etiologies. Separate data on children with sepsis were not available. The trial focused on methylprednisolone effects on circulating levels of several cytokines without providing information on outcomes that are relevant for this review |
| Steinberg 2006 | This trial included participants with late acute respiratory distress syndrome phase ‐ not those with sepsis |
| Tam 2012 | This study assessed effects of oral prednisolone on viraemia in patients with dengue |
| Thompson 1976 | Study published only as an abstract; no contact with study authors was possible; incomplete information on primary and secondary outcomes |
| van Woensel 2003 | This study evaluated a short course (48 hours) of dexamethasone in children with viral pneumonia requiring mechanical ventilation. Viral pneumonia is a condition that is different in many aspects from bacterial sepsis |
| Venet 2015 | This study included severely burned patients without sepsis |
| Wagner 1955 | This study was not a randomized trial. Participants were allocated to experimental treatment according to hospital numbers |
| Weigelt 1985 | Mixed population of critically ill patients; separate data on septic shock not available |
LDH: lactate dehydrogenase.
Characteristics of ongoing studies [ordered by study ID]
NCT02517489.
| Trial name or title | Community‐acquired pneumonia: evaluation of corticosteroids (CAPE_COD) |
| Methods | Randomized double‐blind trial on 2 parallel groups |
| Participants | Adults (n = 1200), admitted to the ICU or intermediate care unit, with community‐acquired pneumonia |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | October 2015 |
| Contact information | Pierre‐François DEQUIN; pierre‐françois.dequin@univ‐tours.fr |
| Notes |
NCT02602210.
| Trial name or title | Supplemental corticosteroids in cirrhotic hypotensive patients with suspicion of sepsis (SCOTCH) |
| Methods | Randomized double‐blind trial on 2 parallel groups |
| Participants | Adults (n = 346), with liver cirrhosis and sepsis |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | January 2015 |
| Contact information | Philippe Meersseman, MD; philippe.meersseman@uzleuven.be |
| Notes |
NCT03258684.
| Trial name or title | Hydrocortisone, vitamin C, and thiamine for treatment of sepsis and septic shock (HYVCTTSSS) |
| Methods | Randomized trial on 2 parallel groups |
| Participants | Adults (n = 140) with sepsis or septic shock |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | September 2017 |
| Contact information | Yuping Liao |
| Notes |
NCT03333278.
| Trial name or title | The vitamin C, hydrocortisone, and thiamine in patients with septic shock trial (VITAMINS) |
| Methods | Multi‐centre, randomized, open‐label controlled trial |
| Participants | Adults (n = 216) with septic shock |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | May 2018 |
| Contact information | R Bellomo; rinaldo.bellomo@austin.org.au |
| Notes |
NCT03335124.
| Trial name or title | The effect of vitamin C, thiamine, and hydrocortisone on clinical course and outcome in patients with severe sepsis and septic shock |
| Methods | Randomized double‐blind placebo‐controlled trial |
| Participants | Adults (n = 30) with sepsis or septic shock |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | December 2018 |
| Contact information | S Stefanovic; sebastian.stefanovic@gmail.com |
| Notes |
NCT03389555.
| Trial name or title | Ascorbic acid, corticosteroids, and thiamine in sepsis (ACTS) trial |
| Methods | Randomized trial on parallel groups |
| Participants | n = 200 adults with septic shock |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | February 2018 |
| Contact information | Michael W Donnino, MD; mdonnino@bidmc.harvard.edu |
| Notes |
NCT03422159.
| Trial name or title | Metabolic resuscitation using ascorbic acid, thiamine, and glucocorticoids in sepsis (ORANGES) |
| Methods | Randomized double‐blind placebo‐controlled trial |
| Participants | Adults (n = 140) with sepsis or septic shock |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | February 2018 |
| Contact information | A Vassallo; Andrew.Vassallo@rwjbh.org |
| Notes |
NCT03509350.
| Trial name or title | Vitamin C, thiamine, and steroids in sepsis (VICTAS) |
| Methods | Multi‐centre, randomized, placebo‐controlled, double‐blind, adaptive clinical trial |
| Participants | Adults (n = 2000) with sepsis |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | August 2018 |
| Contact information | J Sevranski; jonathan.sevransky@emoryhealthcare.org |
| Notes |
NCT03592693.
| Trial name or title | Vitamin C, hydrocortisone, and thiamine for septic shock (CORVICTES) |
| Methods | Randomized, multicenter, parallel‐group, placebo‐controlled |
| Participants | Adults (n = 400) with septic shock |
| Interventions |
|
| Outcomes |
Primary
Secondary
|
| Starting date | September 2018 |
| Contact information | SD Mentzelopoulos; sdmentzelopoulos@yahoo.com |
| Notes |
AKI: acute kidney injury.
bCAM: brief confusion assessment method.
CAM: confusion assessment method.
CDC: Centers for Diseases Control and Prevention.
CLIF: chronic liver failure consortium.
DCFD: delirium‐free and coma‐free days.
DIC: disseminated intravenous coagulopathy.
ED: emergency department.
G: gastric.
GI: gastrointestinal.
ICU: intensive care unit.
IL: interleukin.
IV: intravenous.
KDIGO: Kidney Disease: Improving Global Outcomes.
LOS: length of stay.
NaCl: sodium chloride.
PCT: procalcitonin.
RASS: Richmond Agitation‐Sedation Scale.
RRT: renal replacement therapy.
SOFA: sequential organ function assessment.
TNF: tumour necrosis factor.
VVFD: vasopressor‐ventilator‐free days.
Differences between protocol and review
Update 2019
We have made the following changes from the protocol.
We now include treatment effects on mortality at 90 days and in the long term (i.e. at longest follow‐up available beyond three months). Indeed, with the decline in sepsis‐related short‐term mortality observed in the past decade, more attention is given to mortality at longer term. The two most recent and largest trials of corticosteroids for septic shock had all‐cause mortality at 90 days as the primary outcome and followed up patients to six months.
We included the new Sepsis 3 definition in the selection of types of participants. For this update, we found no trial that used the Sepsis 3 definition, as all studies were designed before the new definition was available.
We added new adverse events (i.e. neuropsychiatric events, stroke, and cardiac events). Indeed, with more patients surviving in the short term, adverse events from treatment that may impact patients' long‐term outcomes have been given greater attention in sepsis trials. Such adverse events may include muscle weakness, neuropsychiatric events, stroke, and cardiac events, and we have added them to this review.
We added a subgroup analysis based on modes of administration of corticosteroids (i.e. continuous vs bolus administration, stopping with or without taper off). Indeed, over past decades, increasing use of corticosteroids for sepsis has raised new issues of controversy based on how corticosteroids are administered.
We conducted sensitivity analysis based on methodological quality by conducting an analysis of all studies judged to be at low risk of bias.
We introduced a new comparison that is a direct comparison of continuous infusion versus intermittent bolus of corticosteroids.
We modified the search strategy to increase its sensitivity by adding the search terms "pneumonia", "acute respiratory distress syndrome", and "acute lung injury".
Contributions of authors
Conceiving of the review: Djillali Annane (DA), Eric Bellissant (EB), Pierre Edouard Bollaert (PEB), Josef Briegel (JB), Didier Keh (DK), Yizhak Kupfer (YK), Romain Piracchio (RP), Bram Rochwerg (BR).
Co‐ordinating the review: DA.
Undertaking manual searches: DA, PEB, JB, DK, RP, BR.
Screening search results: DA, PEB, JB, DK, YK, RP, BR.
Organizing retrieval of papers: DA, PEB, JB, DK, YK, RP, BR.
Screening retrieved papers against inclusion criteria: DA, PEB, JB, DK, YK, RP, BR.
Appraising the quality of papers: DA, PEB, JB, DK, RP, BR, YK.
Abstracting data from papers: DA, RP, BR.
Writing to authors of papers to ask for additional information: DA.
Providing additional data about papers: DA, PEB, JB, DK, YK.
Obtaining and screening data on unpublished studies: DA, PEB, JB, DK, RP, BR, YK.
Managing data for the review: DA, EB, RP, BR.
Entering data into Review Manager (Review Manager 2014): DA.
Analysing RevMan statistical data: DA, EB, RP, BR.
Performing other statistical analyses not using RevMan: DA .
Performing double entry of data (data entered by person one: DA; data entered by person two: Laurenne Authelet).
Interpreting data: DA, EB, PEB, JB, DK, YK, RP, BR.
Making statistical inferences: EB.
Writing the review: DA, EB, PEB, JB, DK, YK, RP, BR.
Securing funding for the review: DA.
Performing previous work that served as the foundation of the present study: DA, EB, PEB, JB, DK, YK.
Serving as guarantor for the review (one review author): DA.
Taking responsibility for reading and checking the review before submission: DA.
Sources of support
Internal sources
Hopital Raymond Poincaré, Garches, France.
-
University of Versailles Saint Quentin en Yvelines, France.
Logistical support for literature search
External sources
Department for International Development, UK.
Declarations of interest
Djillali Annane is an author of the following studies included in this review: Aboab 2008; Annane 2002; Annane 2010; Annane 2018; Sprung 2008. He obtained funds from the French Minisitry of Health to conduct the following trials: Annane 2002; Annane 2010; and Annane 2018. He has been the chair of the international task force for elaborating 2017 guidelines for the diagnosis and treatment of critical illness‐related corticosteroid insufficiency.
Eric Bellissant is an author of the following studies included in this review: Annane 2002; Annane 2018.
Pierre Edouard Bollaert is an author of the following studies included in this review: Annane 2002; Bollaert 1998. He obtained public funds from the University of Nancy to conduct the trial (Bollaert 1998).
Josef Briegel is an author of the following studies included in this review: Briegel 1999; Keh 2016; Sprung 2008. He obtained public funds to conduct the trial (Briegel 1999). He contributed to the international task force for elaborating 2017 guidelines for the diagnosis and treatment of critical illness‐related corticosteroid insufficiency. He participated in the European Society of Intensive Care Medicine, the Deutsche interdisziplinäre Vereinigung Intensivmedizin, and the Deutsche Gesellschaft für Anästhesie und Intensivmedizin, and he has given lectures and talks on hydrocortisone treatment for septic shock.
Didier Keh is an author of the following studies included in this review: Keh 2003; Keh 2016; Sprung 2008. He obtained public funds from Charité–Universitätsmedizin Berlin and from the German Federal Ministry of Education and Research to conduct the following trials: Keh 2003; Keh 2016.
Yizhak Kupfer is an author of the following studies included in this review: Chawla 1999. He is a member of the Pfizer/BMS speakers' bureau for epixaban. This product has no relationship to steroids in sepsis. He obtained funds from his institution to conduct the trial (Chawla 1999).
Romain Pirracchio received funding for International Mobility from the Fulbright Foundation and from the Assistance Publique – Hôpitaux de Paris (APHP).
Bram Rochwerg is supported by McMaster University Department of Medicine early career research awards. He has contributed to the international task force for elaborating 2017 guidelines for the diagnosis and treatment of critical illness‐related corticosteroid insufficiency. He is a methodologist for American Thoracic Society, European Society of Intensive Care Medicine, and American Society of Haematology.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Aboab 2008 {published data only (unpublished sought but not used)}
- Aboab J, Polito A, Orlikowski D, Sharshar T, Castel M, Annane D. Hydrocortisone effects on cardiovascular variability in septic shock: a spectral analysis approach. Critical Care Medicine 2008;36(5):1481‐6. [PUBMED: 18434902] [DOI] [PubMed] [Google Scholar]
Annane 2002 {published and unpublished data}
- Annane D, Sebille V, Charpentier C, Bollaert PE, François B, Korach JM, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002;288(7):862‐71. [PUBMED: 12186604] [DOI] [PubMed] [Google Scholar]
Annane 2010 {published and unpublished data}
- COIITSS Study Investigators, Annane D, Cariou A, Maxime V, Azoulay E, D'honneur G, et al. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. JAMA 2010;303(4):341‐8. [PUBMED: 20103758] [DOI] [PubMed] [Google Scholar]
Annane 2018 {published and unpublished data}
- Annane D, Renault A, Brun‐Buisson C, Megarbane B, Quenot JP, Siami S, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. New England Journal of Medicine 2018;378(9):809‐18. [PUBMED: 29490185] [DOI] [PubMed] [Google Scholar]
Arabi 2011 {published and unpublished data}
- Arabi YM, Aljumah A, Dabbagh O, Tamim HM, Rishu AH, Al‐Abdulkareem A, et al. Low‐dose hydrocortisone in patients with cirrhosis and septic shock: a randomized controlled trial. Canadian Medical Association Journal 2010;182(18):1971‐7. [PUBMED: 21059778] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blum 2015 {published data only}
- Blum CA, Nigro N, Briel M, Schuetz P, Ullmer E, Suter‐Widmer I, et al. Adjunct prednisone therapy for patients with community‐acquired pneumonia: a multicentre, double‐blind, randomised, placebo‐controlled trial. Lancet 2015;385(9977):1511‐8. [PUBMED: 25608756] [DOI] [PubMed] [Google Scholar]
Bollaert 1998 {published and unpublished data}
- Bollaert PE, Charpentier C, Levy B, Debouverie M, Audibert G, Larcan A. Reversal of late septic shock with supraphysiologic doses of hydrocortisone. Critical Care Medicine 1998;26(4):645‐50. [PUBMED: 9559600] [DOI] [PubMed] [Google Scholar]
Bone 1987 {published data only}
- Bone RG, Fisher CJ, Clemmer TP, Slotman GJ, Metz CA, Balk RA. A controlled clinical trial of high‐dose methylprednisolone in the treatment of severe sepsis and septic shock. New England Journal of Medicine 1987;317(11):653‐8. [PUBMED: 3306374] [DOI] [PubMed] [Google Scholar]
Briegel 1999 {published and unpublished data}
- Briegel J, Forst H, Haller M, Schelling G, Kilger E, Kuprat G, et al. Stress doses of hydrocortisone reverse hyperdynamic septic shock: a prospective, randomized, double‐blind, single‐center study. Critical Care Medicine 1999;27(4):723‐32. [PUBMED: 10321661] [DOI] [PubMed] [Google Scholar]
Chawla 1999 {published and unpublished data}
- Chawla K, Kupfer Y, Tessler S. Hydrocortisone reverses refractory septic shock. Critical Care Medicine 1999;27(1):A33. [Google Scholar]
Cicarelli 2007 {published data only}
- Cicarelli DD, Vieira JE, Benseñor FE. Early dexamethasone treatment for septic shock patients: a prospective randomized clinical trial. Sao Paulo Medical Journal 2007;125(4):237‐41. [PUBMED: 17992396 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Confalonieri 2005 {published and unpublished data}
- Confalonieri M, Urbino R, Potena A, Piatella M, Parigi P, Giacomo P, et al. Hydrocortisone infusion for severe community acquired pneumonia: a preliminary randomized study. American Journal of Respiratory and Critical Care Medicine 2005;171(3):242‐8. [PUBMED: 15557131] [DOI] [PubMed] [Google Scholar]
CSG 1963 {published data only}
- Cooperative Study Group. The effectiveness of hydrocortisone in the management of severe infections. JAMA 1963;183(6):462‐5. [DOI: 10.1001/jama.1963.63700060029012] [DOI] [Google Scholar]
Doluee 2018 {published data only}
- Talebi Doluee M, Salehi M, Mahmoudi Gharaee A, Jalalyazdi M, Reihani H. The effect of physiologic dose of intravenous hydrocortisone in patients with refractory septic shock: a randomized control trial. Journal of Emergency Practice and Trauma 2018;4:29‐33. [DOI: 10.15171/JEPT.2017.25] [DOI] [Google Scholar]
El Ghamrawy 2006 {published data only}
- El‐Ghamraway AH, Shokeir MH, Esmat AA. Effects of low dose hydrocortisone in ICU patients with severe community acquired pneumonia. Egyptian Journal of Chest 2006;55:91‐9. [Google Scholar]
El‐Nawawy 2017 {published data only}
- El‐Nawawy A, Khater D, Omar H, Wali Y. Evaluation of early corticosteroid therapy in management of paediatric septic shock in paediatric intensive care patients: a randomized clinical study. Pediatric Infectious Disease Journal 2017;36(2):155‐9. [PUBMED: 27798546] [DOI] [PubMed] [Google Scholar]
Fernández‐Serrano 2011 {published data only}
- Fernández‐Serrano S, Dorca J, Garcia‐Vidal C, Fernández‐Sabé N, Carratalà J, Fernández‐Agüera A, et al. Effect of corticosteroids on the clinical course of community‐acquired pneumonia: a randomized controlled trial. Critical Care 2011;15(2):R96. [PUBMED: 21406101] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gordon 2014 {published and unpublished data}
- Gordon AC, Mason AJ, Perkins GD, Stotz M, Terblanche M, Ashby D, et al. The interaction of vasopressin and corticosteroids in septic shock: a pilot randomized controlled trial. Critical Care Medicine 2014;42(6):1325‐33. [PUBMED: 24557425] [DOI] [PubMed] [Google Scholar]
Gordon 2016 {published and unpublished data}
- Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, et al. Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA 2016;316(5):509‐18. [PUBMED: 27483065] [DOI] [PubMed] [Google Scholar]
Hu 2009 {published data only (unpublished sought but not used)}
- Hu B, Li JG, Liang H, Zhou Q, Yu Z, Li L, et al. The effect of low‐dose hydrocortisone on requirement of norepinephrine and lactate clearance in patients with refractory septic shock. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2009;21(9):529‐31. [PUBMED: 19751560] [PubMed] [Google Scholar]
Huang 2014 {published data only}
- Huang R, Zhang Z, Xu M, Chang X, Qiao Q, Wang L, et al. Effect of Sini decoction on function of hypothalamic‐pituitary‐adrenal axis in patients with sepsis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2014;26(3):184‐7. [PUBMED: 24598293] [DOI] [PubMed] [Google Scholar]
Huh 2007 {published data only}
- Huh JW, Lim CM, Koh Y, Hong SB. Effect of low doses of hydrocortisone in patient with septic shock and relative adrenal insufficiency: 3 days versus 7 days treatment. Critical Care Medicine 2006;34(12 suppl):A101. [Google Scholar]
Hyvernat 2016 {published and unpublished data}
- Hyvernat H, Barel R, Gentilhomme A, Césari‐Giordani JF, Freche A, Kaidomar M, et al. Effects of increasing hydrocortisone to 300 mg per day in the treatment of septic shock: a pilot study. Shock 2016;46:498‐505. [PUBMED: 27405061] [DOI] [PubMed] [Google Scholar]
Keh 2003 {published and unpublished data}
- Keh D, Boehnke T, Weber‐Cartens S, Schulz C, Ahlers O, Bercker S, et al. Immunologic and hemodynamic effects of "low‐dose" hydrocortisone in septic shock: a double‐blind, randomized, placebo‐controlled, crossover study. American Journal of Respiratory and Critical Care Medicine 2003;167(4):512‐20. [PUBMED: 12426230 ] [DOI] [PubMed] [Google Scholar]
Keh 2016 {published and unpublished data}
- Keh D, Trips E, Marx G, Wirtz SP, Abduljawwad E, Bercker S, et al. Effect of hydrocortisone on development of shock among patients with severe sepsis: the HYPRESS randomized clinical trial. JAMA 2016;316(17):1775‐85. [PUBMED: 27695824] [DOI] [PubMed] [Google Scholar]
Kurungundla 2008 {published data only (unpublished sought but not used)}
- Kurugundla N, Irugulapati L, Kilari D, Amchentsev A, Devakonda A, George L, et al. Effect of steroids in septic shock patients without relative adrenal insufficiency. American Thoracic Society 2008;116. [Google Scholar]
Li 2016 {published data only}
- Li G, Gu C, Zhang S, Lian R, Zhang G. Value of glucocorticoid steroids in the treatment of patients with severe community acquired pneumonia complicated with septic shock. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2016;28(9):780‐4. [DOI: 10.3760/cma.j.issn.2095-4352.2016.09.003] [DOI] [Google Scholar]
Liu 2012 {published and unpublished data}
- Liu L, Li J, Huang YZ, Liu SQ, Yang CS, Guo FM, et al. The effect of stress dose glucocorticoid on patients with acute respiratory distress syndrome combined with critical illness‐related corticosteroid insufficiency. Zhonghua Nei Ke Za Zhi 2012;51(8):599‐603. [PUBMED: 23158856] [PubMed] [Google Scholar]
Loisa 2007 {published data only}
- Loisa P, Parviainen I, Tenhunen J, Hovilehto S, Ruokonen E. Effect of mode of hydrocortisone administration on glycemic control in patients with septic shock: a prospective randomized trial. Critical Care 2007;11(1):R21. [PUBMED: 17306016] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luce 1988 {published and unpublished data}
- Luce JM, Montgomery AB, Marks JD, Turner J, Metz CA, Murray JF. Ineffectiveness of high‐dose methylprednisolone in preventing parenchymal lung injury and improving mortality in patients with septic shock. American Review of Respiratory Diseases 1988;138(1):62‐8. [PUBMED: 3202402 ] [DOI] [PubMed] [Google Scholar]
Lv 2017 {published and unpublished data}
- Lv QQ, Gu XH, Chen QH, Yu JQ, Zheng RQ. Early initiation of low‐dose hydrocortisone treatment for septic shock in adults: a randomized clinical trial. American Journal of Emergency Medicine 2017;35(12):1810‐4. [PUBMED: 28615145] [DOI] [PubMed] [Google Scholar]
McHardy 1972 {published data only}
- McHardy VU, Schonell ME. Ampicillin dosage and use of prednisolone in treatment of pneumonia: co‐operative controlled trial. BMJ 1972;4(5840):569‐73. [PUBMED: 4404939] [DOI] [PMC free article] [PubMed] [Google Scholar]
Meduri 2007 {published and unpublished data}
- Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest 2007;131(4):954‐63. [PUBMED: 17426195] [DOI] [PubMed] [Google Scholar]
Meduri 2009 {published data only (unpublished sought but not used)}
- Meduri GU, Golden E, Freire AX, Umberger R. Randomized clinical trial (RCT) evaluating the effects of low‐dose prolonged hydrocortisone infusion on resolution of MODS in severe sepsis. Chest 2009;136:154. [Google Scholar]
Meijvis 2011 {published data only}
- Meijvis SC, Hardeman H, Remmelts HH, Heijligenberg R, Rijkers GT, Velzen‐Blad H, et al. Dexamethasone and length of hospital stay in patients with community‐acquired pneumonia: a randomised, double‐blind, placebo‐controlled trial. Lancet 2011;377(9782):2023‐30. [PUBMED: 21636122] [DOI] [PubMed] [Google Scholar]
Menon 2017 {published data only}
- Menon K, McNally D, O'Hearn K, Acharya A, Wong HR, Lawson M, et al. A randomized controlled trial of corticosteroids in paediatric septic shock: a pilot feasibility study. Pediatric Critical Care Medicine 2017;18(6):505‐12. [PUBMED: 28406862] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mirea 2014 {published and unpublished data}
- Mirea L, Ungureanu R, Pavelescu D, Grintescu IC, Dumitrache C, Grintescu I, et al. Continuous administration of corticosteroids in septic shock can reduce risk of hypernatraemia. Critical Care 2014;18:S86. [Google Scholar]
Nafae 2013 {published data only}
- Nafae RM, Ragab MI, Amany FM, Rashed SB. Adjuvant role of corticosteroids in the treatment of community acquired pneumonia. Egyptian Journal of Chest Diseases and Tuberculosis 2013;62:439‐45. [Google Scholar]
Nagy 2013 {published data only}
- Nagy B, Gaspar I, Papp A, Bene Z, Nagy B Jr, Voko Z, et al. Efficacy of methylprednisolone in children with severe community acquired pneumonia. Pediatric Pulmonology 2013;48:168‐75. [PUBMED: 22588852] [DOI] [PubMed] [Google Scholar]
Ngaosuwan 2018 {published data only}
- Ngaosuwan K, Ounchokdee K, Chalermchai T. Clinical outcomes of minimized hydrocortisone dosage of 100mg/day on lower occurrence of hyperglycaemia in septic shock. Shock 2018;50(3):280‐5. [PUBMED: 29176402] [DOI] [PubMed] [Google Scholar]
Oppert 2005 {published and unpublished data}
- Oppert M, Schindler R, Husung C, Offerman K, Graef KJ, Boenisch O, et al. Low‐dose hydrocortisone improves shock reversal and reduces cytokine levels in early hyperdynamic septic shock. Critical Care Medicine 2005;33(11):2457‐64. [PUBMED: 16276166 ] [DOI] [PubMed] [Google Scholar]
Rezk 2013 {published data only}
- Rezk NA, Ibrahim AM. Effects of methyl prednisolone in early ARDS. Egyptian Journal of Chest Diseases and Tuberculosis 2013;62(1):167–72. [DOI: 10.1016/j.ejcdt.2013.02.013] [DOI] [Google Scholar]
Rinaldi 2006 {published data only}
- Rinaldi S, Adembri C, Grechi S, DeGaudio R. Low‐dose hydrocortisone during severe sepsis: effects on microalbuminemia. Critical Care Medicine 2006;34(9):2334‐9. [PUBMED: 16850006] [DOI] [PubMed] [Google Scholar]
Sabry 2011 {published data only}
- Sabry NA, El‐Din Omar E. Corticosteroids and ICU course of community acquired pneumonia in Egyptian settings. Pharmacology and Pharmacy 2011;2:73‐81. [Google Scholar]
Schumer 1976 {published data only}
- Schumer W. Steroids in the treatment of clinical septic shock. Annals of Surgery 1976;184(3):333‐41. [PUBMED: 786190 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Slusher 1996 {published data only}
- Slusher T, Gbadero D, Howard C, Lewinson L, Giroir B, Toro L, et al. Randomized, placebo‐controlled, double blinded trial of dexamethasone in African children with sepsis. Pediatric Infectious Diseases Journal 1996;15(7):579‐83. [PUBMED: 8823850] [DOI] [PubMed] [Google Scholar]
Snijders 2010 {published data only}
- Snijders D, Daniels JMA, Graaff CS, Werf TS, Boersma WG. Efficacy of corticosteroids in community‐acquired pneumonia – a randomized double blinded clinical trial. American Journal of Respiratory and Critical Care Medicine 2010;181(9):975‐82. [PUBMED: 20133929] [DOI] [PubMed] [Google Scholar]
Sprung 1984 {published and unpublished data}
- Sprung CL, Caralis PV, Marcial EH, Pierce M, Gelbard MA, Long WM, et al. The effects of high‐dose corticosteroids in patients with septic shock. A prospective, controlled study. New England Journal of Medicine 1984;311(18):1137‐43. [PUBMED: 6384785 ] [DOI] [PubMed] [Google Scholar]
Sprung 2008 {published and unpublished data}
- Sprung C, Annane D, Keh D, Moreno R, Singer M, Freivogel K, et al. Hydrocortisone therapy for patients with septic shock. New England Journal of Medicine 2008;358(2):111‐24. [PUBMED: 18184957] [DOI] [PubMed] [Google Scholar]
Sui 2013 {published data only}
- Sui DJ, Zhang W, Li WS, Zhao HX, Wang ZY. Clinical efficacy in the treatment of severe community acquired pneumonia and its impact on CRP. Chinese Journal of Integrative Medicine 2013;18:1171‐3. [Google Scholar]
Tagaro 2017 {published data only}
- Tagaro A, Otheo E, Baquero‐Artigao F, Navarro ML, Velasco R, Ruiz M, et al. Dexamethasone for parapneumonic pleural effusion: a randomized, double‐blind, clinical trial. Journal of Pediatrics 2017;185:117‐23. [PUBMED: 28363363] [DOI] [PubMed] [Google Scholar]
Tandan 2005 {unpublished data only}
- Tandan SM, Guleria R, Gupta N. Low dose steroids and adrenocortical insufficiency in septic shock: a double‐blind randomised controlled trial from India. Proceedings of the American Thoracic Society Meeting. 2005:A24.
Tilouche 2019 {published data only}
- Tilouche N, Jaoued O, Ben Sik Ali H, Gharbi R, Fekih Hassen M, Elatrous S. Comparison between continuous and intermittent administration of hydrocortisone during septic shock: a randomized controlled clinical trial. Shock 2019;52:481‐6. [DOI: 10.1097/SHK.0000000000001316.; PUBMED: 30628950] [DOI] [PubMed] [Google Scholar]
Tongyoo 2016 {published and unpublished data}
- Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, et al. Hydrocortisone treatment in early sepsis associated acute respiratory distress syndrome: results of a randomized controlled trial. Critical Care 2016;20(1):329. [PUBMED: 27741949] [DOI] [PMC free article] [PubMed] [Google Scholar]
Torres 2015 {published data only}
- Torres A, Sibila O, Ferrer M, Polverino E, Menendez R, Mensa J, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community‐acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA. 2015; Vol. 313, issue 7:677‐86. [PUBMED: 25688779] [DOI] [PubMed]
Valoor 2009 {published data only}
- Valoor HT, Singhi S, Jayashree M. Low‐dose hydrocortisone in paediatric septic shock: an exploratory study in a third world setting. Pediatric Critical Care Medicine 2009;10(1):121‐5. [PUBMED: 19057445] [DOI] [PubMed] [Google Scholar]
VASSCSG 1987 {published data only}
- Veterans Administration Systemic Sepsis Cooperative Study Group. Effect of high‐dose glucocorticoid therapy on mortality in patients with clinical signs of systemic sepsis. New England Journal of Medicine 1987;317(11):659‐65. [PUBMED: 2888017] [DOI] [PubMed] [Google Scholar]
Venkatesh 2018 {published data only (unpublished sought but not used)}
- Venkatesh B, Finfer S, Cohen J, Rajbhandari D, Arabi Y, Bellomo R, et al. Adjunctive glucocorticoid therapy in patients with septic shock. New England Journal of Medicine 2018;378:797–808. [DOI: 10.1056/NEJMoa1705835; PUBMED: 29347874] [DOI] [PubMed] [Google Scholar]
- Venkatesh B, Finfer S, Mybrugh J, Cohen J, Billot L. Long‐term outcomes of the ADRENAL trial [2018]. New England Journal of Medicine 2018;378(18):174‐5. [PUBMED: 29694789] [DOI] [PubMed] [Google Scholar]
Yildiz 2002 {published data only}
- Yildiz O, Doganay M, Aygen B, Guven M, Keleutimur F, Tutuu A. Physiological‐dose steroid therapy in sepsis. Critical Care 2002;6(3):251‐9. [PUBMED: 12133187] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yildiz 2011 {published data only}
- Yildiz O, Tanriverdi F, Simsek S, Aygen B, Kelestimur F. The effects of moderate‐dose steroid therapy in sepsis: a placebo‐controlled, randomized study. Journal of Research in Medical Sciences 2011;16(11):1410‐21. [PUBMED: 22973341] [PMC free article] [PubMed] [Google Scholar]
Zhou 2015 {published data only}
- Zhou M. Application value of glucocorticoid for comprehensive treatment of acute respiratory distress syndrome induced by serious community acquired pneumonia. Clinical Medicine and Engineering 2015;22:57‐8. [DOI: 10.3969/j.issn.1674-4659.2015.01.0057] [DOI] [Google Scholar]
References to studies excluded from this review
Asehnoune 2014 {published data only}
- Asehnoune K, Seguin P, Allary J, Feuillet F, Lasocki S, Cook F, et al. Hydrocortisone and fludrocortisone for prevention of hospital‐acquired pneumonia in patients with severe traumatic brain injury (Corti‐TC): a double‐blind, multicentre phase 3, randomised placebo‐controlled trial. The Lancet. Respiratory Medicine 2014;2:706‐16. [PUBMED: 25066331] [DOI] [PubMed] [Google Scholar]
Bernard 1987 {published data only}
- Bernard GR, Luce JM, Sprung CL, Rinaldo JE, Tate RM, Sibbald WJ, et al. High‐dose corticosteroids in patients with the adult respiratory distress syndrome. New England Journal of Medicine 1987;317:1565‐70. [PUBMED: 3317054] [DOI] [PubMed] [Google Scholar]
Cicarelli 2006 {published data only}
- Cicarelli DD, Bensenor FEM, Vieira JE. Effects of single dose of dexamethasone on patients with systemic inflammatory response. Sao Paulo Medical Journal 2006;124(2):90‐5. [PUBMED: 16878192 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hahn 1951 {published data only}
- Hahn EO, Houser HB, Rammelkamp CH, Denny FW, Wannamaker LW. Effect of cortisone on acute streptococcal infections and post‐streptococcal complications. Journal of Clinical Investigation 1951;30:274‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 2014a {published data only}
- Huang L, Gao X, Chen M. Early treatment with corticosteroids in patients with Mycoplasma pneumoniae pneumonia: a randomized clinical trial. Journal of Tropical Pediatrics 2014;64:338‐42. [PUBMED: 24710342] [DOI] [PubMed] [Google Scholar]
Huang 2015 {published data only}
- Huang G, Liang B, Liu G, Liu K, Ding Z. Low dose of glucocorticoid decreases the incidence of complications in severely burned patients by attenuating systemic inflammation. J Crit Care 2015;436:436.e7‐11. [DOI] [PubMed] [Google Scholar]
Hughes 1984 {published data only}
- Hughes GS Jr. Naloxone and methylprednisolone sodium succinate enhance sympathomedullary discharge in patients with septic shock. Life Sciences 1984;35(23):2319‐26. [PUBMED: 6390057] [DOI] [PubMed] [Google Scholar]
Kaufman 2008 {published and unpublished data}
- Kaufmann I, Briegel J, Schliephake F, Hoelzl A, Chouker A, Hummel T, et al. Stress doses of hydrocortisone in septic shock: beneficial effects on opsonization‐dependent neutrophil functions. Intensive Care Medicine 2008;34(2):344‐9. [PUBMED: 17906853 ] [DOI] [PubMed] [Google Scholar]
Klastersky 1971 {published data only}
- Klastersky J, Cappel R, Debusscher L. Effectiveness of betamethasone in management of severe infections. A double‐blind study. New England Journal of Medicine 1971;284(22):1248‐50. [PUBMED: 4929896] [DOI] [PubMed] [Google Scholar]
Lan 2015 {published data only}
- Lan Y, Yang D, Chen Z, Tang L, Xu Y, Cheng Y. Effectiveness of methylprednisolone in treatment of children with refractory Mycoplasma pneumoniae pneumonia and its relationship with bronchoalveolar lavage cytokine levels. Zhonghua Er Ke Za Zhi 2015;53:779‐83.. [PubMed] [Google Scholar]
Lucas 1984 {published data only}
- Lucas C, Ledgerwood A. The cardiopulmonary response to massive doses of steroids in patients with septic shock. Archives of Surgery 1984;119(5):537‐41. [PUBMED: 6712466 ] [DOI] [PubMed] [Google Scholar]
Luo 2014 {published data only}
- Luo Z, Luo J, Liu E, Xu X, Liu Y, Zeng F, et al. Effects of prednisolone on refractory Mycoplasma pneumoniae pneumonia in children. Pediatric Pulmonology 2014;49:377‐80. [PUBMED: 23401275] [DOI] [PubMed] [Google Scholar]
Marik 1993 {published data only}
- Marik P, Kraus P, Sribante J, Havlik I, Lipman J, Johnson DW. Hydrocortisone and tumour necrosis factor in severe community‐acquired pneumonia. A randomized controlled study. Chest 1993;104:389‐92. [PUBMED: 8339624] [DOI] [PubMed] [Google Scholar]
McKee 1983 {published data only}
- McKee JI, Finlay WE. Cortisol replacement in severely stressed patients. Lancet 1983;1(8322):484. [PUBMED: 6131207 ] [DOI] [PubMed] [Google Scholar]
Meduri 1998b {published and unpublished data}
- Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA 1998;280(2):159‐65. [PUBMED: 9669790] [DOI] [PubMed] [Google Scholar]
Mikami 2007 {published data only}
- Mikami K, Suzuki M, Kitagawa H, Kawakami M, Hirota N, Yamaguchi H, et al. Efficacy of corticosteroids in the treatment of community‐acquired pneumonia requiring hospitalization. Lung 2007;185(5):249‐55. [PUBMED: 17710485] [DOI] [PubMed] [Google Scholar]
Newberry 2017 {published data only}
- Newberry L, O'Hare B, Kennedy N, Selman A, Omar S, Dawson P, Stevenson K, Nishihara Y, Lissauer S, Molyneux E. Early use of corticosteroids in infants with a clinical diagnosis of Pneumocystis jiroveci pneumonia in Malawi: a double‐blind, randomised clinical trial. Paediatr Int Child Health. 2017;37:121‐128.. [DOI] [PubMed] [Google Scholar]
Peeters 2018 {published data only}
- Peeters B, Meersseman P, Vander Perre S, Wouters PJ, Debaveye Y, Langouche L, Berghe G. ACTH and cortisol responses to CRH in acute, subacute, and prolonged critical illness: a randomized, double‐blind, placebo‐controlled, crossover cohort study. Intensive Care Medicine 2018;44:2048‐58.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rogers 1970 {published data only}
- Rogers J. Large doses of steroids in septicaemic shock. British Journal of Urology 1970;42(6):742. [PUBMED: 4923652] [PubMed] [Google Scholar]
Roquilly 2011 {published data only}
- Roquilly A, Mahe PJ, Seguin P, Guitton C, Floch H, Tellier AC, et al. Hydrocortisone therapy for patients with multiple trauma: the randomized controlled HYPOLYTE study. JAMA 2011;305:1201‐9. [PUBMED: 21427372] [DOI] [PubMed] [Google Scholar]
Schwingshackl 2016 {published data only}
- Schwingshackl A, Kimura D, Rovnaghi CR, Saravia JS, Cormier SA, Teng B, et al. Regulation of inflammatory biomarkers by intravenous methylprednisolone in pediatric ARDS patients: results from a double‐blind, placebo‐controlled randomized pilot trial. Cytokine 2016;77:63‐71. [PUBMED: 26545141] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steinberg 2006 {published data only}
- Steinberg KP, Hudson LD, Goodman RB, Hough CL, Lanken PN, Hyzy R, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. New England Journal of Medicine 2006;354:1671‐84. [PUBMED: 16625008] [DOI] [PubMed] [Google Scholar]
Tam 2012 {published data only}
- Tam DT, Ngoc TV, Tien NT, Kieu NT, Thuy TT, Thanh LT, et al. Effects of short‐course oral corticosteroid therapy in early dengue infection in Vietnamese patients: a randomized, placebo‐controlled trial. Clinical Infectious Disease 2012;55(9):1216‐24. [PUBMED: 22865871] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 1976 {published data only}
- Thompson WL, Gurley HT, Lutz BA, Jackson DL, Kvols LK, Morris IA. Inefficacy of glucocorticoids in shock (double‐blind study). Clinical Research 1976;24:258A. [Google Scholar]
van Woensel 2003 {published data only}
- Woensel JB, Aalderen WM, Weerd W, Jansen NJ, Gestel JP, Markhorst DG, et al. Dexamethasone for treatment of patients mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus. Thorax 2003;58(5):383‐7. [PUBMED: 12728156] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venet 2015 {published data only}
- Venet F, Plassais J, Textoris J, Cazalis MA, Pachot A, Bertin‐Maghit M, et al. Low‐dose hydrocortisone reduces norepinephrine duration in severe burn patients: a randomized clinical trial. Critical Care 2015;19:21. [PUBMED: 25619170] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagner 1955 {published data only}
- Wagner HN, Bennett IL, Lasagna L, Cluff LE, Rosenthal MB, Mirick GS. The effect of hydrocortisone upon the course of pneumococcal pneumonia treated with penicillin. Bulletin of Johns Hopkins Hospital 1955;98(3):197‐215. [PUBMED: 13304518] [PubMed] [Google Scholar]
Weigelt 1985 {published data only}
- Weigelt JA, Norcross JF, Borman KR, Snyder WH 3rd. Early steroid therapy for respiratory failure. Archives of Surgery 1985;120(5):536‐40. [PUBMED: 3885915 ] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02517489 {published data only}
- NCT02517489. Community‐acquired pneumonia: evaluation of corticosteroids (CAPE COD) [Effects of low‐dose corticosteroids on survival of severe community‐acquired pneumonia]. https://clinicaltrials.gov/ct2/show/NCT02517489. First received 7 August 2015.
NCT02602210 {published data only}
- NCT02602210. Supplemental corticosteroids in cirrhotic hypotensive patients with suspicion of sepsis (SCOTCH) [Supplemental corticosteroids in cirrhotic hypotensive patients with suspicion of sepsis]. https://clinicaltrials.gov/ct2/show/NCT02602210. First received 11 November 2015.
NCT03258684 {published data only}
- NCT03258684. Hydrocortisone, vitamin C, and thiamine for the treatment of sepsis and septic shock (HYVCTTSSS) [Hydrocortisone, vitamin C, and thiamine for the treatment of sepsis and septic shock: a prospective study]. https://clinicaltrials.gov/ct2/show/NCT03258684. First received 23 August 2017.
NCT03333278 {published data only}
- NCT03333278. The vitamin C, hydrocortisone and thiamine in patients with septic shock trial (VITAMINS) [The vitamIn C, hydrocortisone and thiamine in patients with septic shock trial (VITAMINS trial) ‐ a prospective, feasibility, pilot, multi‐centre, randomised, open‐label controlled trial]. https://clinicaltrials.gov/ct2/show/NCT03333278. First received 6 November 2017.
NCT03335124 {published data only}
- NCT03335124. The effect of vitamin C, thiamine and hydrocortisone on clinical course and outcome in patients with severe sepsis and septic shock [A randomized, double blind, placebo‐controlled study to investigate the effects of vitamin C, hydrocortisone and thiamine on the outcome of patients with severe sepsis and septic shock]. https://clinicaltrials.gov/ct2/show/NCT03335124. First received 7 November 2017.
NCT03389555 {published data only}
- NCT03389555. Ascorbic acid, corticosteroids, and thiamine in sepsis (ACTS) trial [Ascorbic acid, hydrocortisone, and thiamine in sepsis and septic shock ‐ a randomized, double‐blind, placebo‐controlled trial]. https://clinicaltrials.gov/ct2/show/NCT03389555. First received 3 January 2018.
NCT03422159 {published data only}
- NCT03422159. Metabolic resuscitation using ascorbic acid, thiamine, and glucocorticoids in sepsis (ORANGES) [Outcomes of metabolic resuscitation using ascorbic acid, thiamine, and glucocorticoids in the early treatment of sepsis]. https://clinicaltrials.gov/ct2/show/NCT03422159. First received 5 February 2018.
NCT03509350 {published data only}
- NCT03509350. Vitamin C, thiamine, and steroids in sepsis (VICTAS) [A multi‐center, randomized, placebo‐controlled, double‐blind, adaptive clinical trial of vitamin C, thiamine and steroids as combination therapy in patients with sepsis]. https://clinicaltrials.gov/ct2/show/NCT03509350. First received 26 April 2018.
NCT03592693 {published data only}
- NCT03592693. Vitamin C, hydrocortisone and thiamine for septic shock (CORVICTES) [A randomized, double blind, placebo‐controlled trial to investigate the effect of vitamin C, hydrocortisone and thiamine on the outcome of patients with septic shock]. https://clinicaltrials.gov/ct2/show/NCT03592693. First received 19 July 2018.
Additional references
ACCP/SCCM 1992
- ACCP/SCCM Consensus Conference Panel. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Critical Care Medicine 1992;20(6):864‐74. [PUBMED: 1597042 ] [PubMed] [Google Scholar]
Allen 2018
- Allen JM, Feild C, Shoulders BR, Voils SA. Recent updates in the pharmacological management of sepsis and septic shock: a systematic review focused on fluid resuscitation, vasopressors, and corticosteroids. Annals of Pharmacotherapy 2018;53:385‐95. [DOI: 10.1177/1060028018812940; PUBMED: 30404539 ] [DOI] [PubMed] [Google Scholar]
Angus 2013
- Angus DC, Poll T. Severe sepsis and septic shock. New England Journal of Medicine 2013;369(21):840‐51. [PUBMED: 23984731] [DOI] [PubMed] [Google Scholar]
Annane 2000
- Annane D, Sébille V, Troché G, Raphael JC, Gajdos P, Bellissant E. A 3‐level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA 2000;283(8):1038‐45. [PUBMED: 10697064] [DOI] [PubMed] [Google Scholar]
Annane 2003
- Annane D, Aegerter P, Jars‐Guincestre MC, Guidet B, CUB‐Rea Network. Current epidemiology of septic shock: the CUB‐Réa Network. American Journal of Respiratory and Critical Care Medicine 2003;168(2):165‐72. [PUBMED: 12851245] [DOI] [PubMed] [Google Scholar]
Annane 2005
- Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet 2005;365(9453):63‐78. [PUBMED: 15639681] [DOI] [PubMed] [Google Scholar]
Annane 2009b
- Annane D. Improving clinical trials in the critically ill: unique challenge: sepsis. Critical Care Medicine 2009;37(1 Suppl):117‐28. [PUBMED: 19104211] [DOI] [PubMed] [Google Scholar]
Annane 2017a
- Annane D, Pastores SM, Arlt W, Balk RA, Beishuizen A, Briegel J, et al. Critical illness‐related corticosteroid insufficiency (CIRCI): a narrative review from a Multispecialty Task Force of the Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM). Intensive Care Medicine 2017;43(12):1781‐92. [PUBMED: 28940017] [DOI] [PubMed] [Google Scholar]
Annane 2017b
- Annane D, Pastores SM, Rochwerg B, Arlt W, Balk RA, Beishuizen A, et al. Guidelines for the diagnosis and management of critical illness‐related corticosteroid insufficiency (CIRCI) in critically ill patients (Part I): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Intensive Care Medicine 2017;43(12):1751‐63. [PUBMED: 28940011] [DOI] [PubMed] [Google Scholar]
Barczyk 2010
- Barczyk K, Ehrchen J, Tenbrock K, Ahlmann M, Kneidl J, Viemann D, et al. Glucocorticoids promote survival of anti‐inflammatory macrophages via stimulation of adenosine receptor A3. Blood 2010;116(3):446‐55. [PUBMED: 20460503] [DOI] [PubMed] [Google Scholar]
Barnes 1995
- Barnes PJ, Greening AP, Crompton GK. Glucocorticoid resistance in asthma. American Journal of Respiratory and Critical Care Medicine 1995;152(Suppl 6 Pt 2):125‐40. [PUBMED: 7489120] [DOI] [PubMed] [Google Scholar]
Boonen 2013
- Boonen E, Vervenne H, Meersseman P, Andrew R, Mortier L, Declercq PE, et al. Reduced cortisol metabolism during critical illness. New England Journal of Medicine 2013;388(16):1477‐88. [PUBMED: 23506003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Briegel 1994
- Briegel J, Kellermann W, Forst H, Haller M, Bittl M, Hoffmann GE, et al. Low‐dose hydrocortisone infusion attenuates the systemic inflammatory response syndrome. The Phospholipase A2 Study Group. Clinical Investigation 1994;72(10):782‐7. [PUBMED: 7865982] [DOI] [PubMed] [Google Scholar]
Bruno 2012
- Bruno JJ, Dee BM, Anderegg BA, Hernandez M, Pravinkumar SE. US practitioner opinions and prescribing practices regarding corticosteroid therapy for severe sepsis and septic shock. Journal of Critical Care 2012;27(4):351‐61. [PUBMED: 22341726] [DOI] [PubMed] [Google Scholar]
Cai 2008
- Cai L, Ji A, Beer FC, Tannock LR, Westhuyzen DR. SR‐BI protects against endotoxemia in mice through its roles in glucocorticoid production and hepatic clearance. Journal of Clinical Investigation 2008;118(1):364–75. [PUBMED: 18064300] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cain 2017
- Cain DW, Cidlowski JA. Immune regulation by glucocorticoids. Nature Reviews. Immunology 2017;17(4):233‐47. [PUBMED: 28192415] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chrousos 1995
- Chrousos GP. The hypothalamic‐pituitary‐adrenal axis and immune‐mediated inflammation. New England Journal of Medicine 1995;322(20):1351‐62. [PUBMED: 7715646] [DOI] [PubMed] [Google Scholar]
Cooper 2003
- Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. New England Journal of Medicine 2003;348(8):727‐34. [PUBMED: 12594318 ] [DOI] [PubMed] [Google Scholar]
Cronin 1995
- Cronin L, Cook DJ, Carlet J, Heyland DK, King D, Lansang MAD, et al. Corticosteroid treatment for sepsis: a critical appraisal and meta‐analysis of the literature. Critical Care Medicine 1995;23(8):1430‐9. [PUBMED: 7634816 ] [DOI] [PubMed] [Google Scholar]
de Kruif 2007
- Kruif MD, Lemaire LC, Giebelen IA, Zoelen MA, Pater JM, Pangaart PS, et al. Prednisolone dose‐dependently influences inflammation and coagulation during human endotoxemia. Journal of Immunology 2007;178(3):1845‐51. [PUBMED: 17237435] [DOI] [PubMed] [Google Scholar]
Devereaux 2001
- Devereaux PJ, Manns BJ, Ghali WA, Quan H, Lacchetti C, Montori VM, et al. Physician interpretations and textbook definitions of blinding terminology in randomized controlled trials. JAMA 2001;285(15):2000‐3. [PUBMED: 11308438 ] [DOI] [PubMed] [Google Scholar]
di Villa Bianca 2003
- Villa Bianca RE, Lippolis L, Autore G, Popolo A, Marzocco S, Sorrentino L, et al. Dexamethasone improves vascular hyporeactivity induced by LPS in vivo by modulating ATP‐sensitive potassium channel activity. British Journal of Pharmacology 2003;140(1):91–6. [PUBMED: 12967938] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duma 2004
- Duma D, Silva‐Santos JE, Assreuy J. Inhibition of glucocorticoid receptor binding by nitric oxide in endotoxemic rats. Critical Care Medicine 2004;32(11):2304–10. [PUBMED: 15640646] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [PUBMED: 9310563] [DOI] [PMC free article] [PubMed] [Google Scholar]
Erschen 2007
- Ehrchen J, Steinmüller L, Barczyk K, Tenbrock K, Nacken W, Eisenacher M, et al. Glucocorticoids induce differentiation of a specifically activated, anti‐inflammatory subtype of human monocytes. Blood 2007;109(3):1265‐74. [PUBMED: 17018861] [DOI] [PubMed] [Google Scholar]
Fabian 1982
- Fabian TC, Patterson R. Steroid therapy in septic shock. Survival studies in a laboratory model. American Surgeon 1982;48(12):614‐7. [PUBMED: 6760756] [PubMed] [Google Scholar]
Fang 2018
- Fang F, Zhang Y, Tang J, Lunsford LD, Li T, Tang R, et al. Association of corticosteroid treatment with outcomes in adult patients with sepsis: a systematic review and meta‐analysis. JAMA Internal Medicine 2019;179(2):213‐23. [DOI: 10.1001/jamainternmed.2018.5849; PUBMED: 30575845] [DOI] [PMC free article] [PubMed] [Google Scholar]
Galigniana 1999
- Galigniana MD, Piwien‐Pilipuk G, Assreuy J. Inhibition of glucocorticoid receptor binding by nitric oxide. Molecular Pharmacology 1999;55(2):317–23. [PUBMED: 9927624] [DOI] [PubMed] [Google Scholar]
Goodwin 2013
- Goodwin JE, Feng Y, Velazquez H, Sessa WC. Endothelial glucocorticoid receptor is required for protection against sepsis. Proceedings of the National Academy of Science 2013;110(1):306–11. [PUBMED: 23248291] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed 7 April 2019. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Guyatt 2008a
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [PUBMED: 18436948 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008b
- Guyatt GH, Wyer P, Ioannidis J. When to believe a subgroup analysis. In: Guyatt G, Rennie R, Meade M, Cook D editor(s). User’s Guides to the Medical Literature: A Manual for Evidence‐Based Clinical Practice. New York: McGraw‐Hill, 2008. [Google Scholar]
Guyatt 2013
- Guyatt GH, Busse J. Methods commentary: risk of bias in randomized trials 1. Evidence Partners 2013 (accessed 15 December 2018):http://distillercer.com/resources/methodological‐resources/risk‐of‐biascommentary/.
Heller 2003
- Heller AR, Heller SC, Borkenstein A, Stehr SN, Koch T. Modulation of host defence by hydrocortisone in stress doses during endotoxaemia. Intensive Care Medicine 2003;29(9):1456‐63. [PUBMED: 12879235 ] [DOI] [PubMed] [Google Scholar]
Heming 2018
- Heming N, Sivanandamoorthy S, Meng P, Bounab R, Annane D. Immune effects of corticosteroids in sepsis. Frontiers in Immunology 2018;9:1736. [DOI: 10.3389/fimmu.2018.01736; PUBMED: 30105022] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hotta 1986
- Hotta M, Baird A. Differential effects of transforming growth factor type beta on the growth and function of adrenocortical cells in vitro. Proceedings of the National Academy of Sciences of the United States of America 1986;83(20):7795‐9. [PUBMED: 3020557] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 1987
- Huang ZH, Gao H, Xu RB. Study on glucocorticoid receptors during intestinal ischemia shock and septic shock. Circulatory Shock 1987;23(1):27‐36. [PUBMED: 3690811] [PubMed] [Google Scholar]
Ioannidis 2004
- Ioannidis JPA. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Annals of Internal Medicine 2004;141(10):781‐8. [PUBMED: 15545678] [DOI] [PubMed] [Google Scholar]
Jaattela 1991
- Jaattela M, Ilvesmaki V, Voutilainen R, Stenman UH, Saksela E. Tumor necrosis factor as a potent inhibitor of adrenocorticotropin‐induced cortisol production and steroidogenic P450 enzyme gene expression in cultured human fetal adrenal cells. Endocrinology 1991;128(1):623‐9. [PUBMED: 1702707] [DOI] [PubMed] [Google Scholar]
Kadri 2017
- Kadri SS, Rhee C, Strich JR, Morales MK, Hohmann S, Menchaca J, et al. Estimating ten‐year trends in septic shock incidence and mortality in United States academic medical centers using clinical data. Chest 2017;151(2):278‐28. [PUBMED: 27452768] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kalil 2011
- Kalil AC, Sun J. Low‐dose steroids for septic shock and severe sepsis: the use of Bayesian statistics to resolve clinical trial controversies. Intensive Care Medicine 2011;37(3):420–9. [PUBMED: 21243334] [DOI] [PubMed] [Google Scholar]
Kanczkowski 2013
- Kanczkowski W, Alexaki VI, Tran N, Großklaus S, Zacharowski K, Martinez A, et al. Hypothalamo‐pituitary and immune‐dependent adrenal regulation during systemic inflammation. Proceedings of the National Academy of Science 2013;110(36):14801–6. [PUBMED: 23959899] [DOI] [PMC free article] [PubMed] [Google Scholar]
Katsenos 2014
- Katsenos CS, Antonopoulou AN, Apostolidou EN, Ioakeimidou A, Kalpakou GT, Papanikolaou MN, et al. on behalf of the Hellenic Sepsis Study Group. Early administration of hydrocortisone replacement after the advent of septic shock: impact on survival and immune response. Critical Care Medicine 2014;42(7):1651‐7. [PUBMED: 24674923] [DOI] [PubMed] [Google Scholar]
Kellum 2007
- Kellum JA, Kong L, Fink MP, Weissfeld LA, Yealy DM, Pinsky MR, et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Archives of Internal Medicine 2007;167(15):1655‐63. [PUBMED: 17698689] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lamontagne 2018
- Lamontagne F, Rochwerg B, Lytvyn L, Guyatt GH, Møller MH, Annane D, et al. Corticosteroid therapy for sepsis: a clinical practice guideline. BMJ 2018;362:k3284. [PUBMED: 30097460] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefering 1995
- Lefering R, Neugebauer EAM. Steroid controversy in sepsis and septic shock: a meta‐analysis. Critical Care Medicine 1995;23(7):1294‐303. [PUBMED: 7600840 ] [DOI] [PubMed] [Google Scholar]
Lipiner 2007
- Lipiner D, Sprung CL, Laterre PF, Weiss Y, Goodman SV, Vogeser M, et al. Adrenal function in sepsis: the retrospective CORTICUS cohort study. Critical Care Medicine 2007;35(4):1012‐8. [PUBMED: 17334243] [DOI] [PubMed] [Google Scholar]
Lowenberg 2005
- Lowenberg M, Tuynman J, Bilderbeek J, Gaber T, Buttgereit F, Deventer S, et al. Rapid immunosuppressive effects of glucocorticoids mediated through Lck and Fyn. Blood 2005;106(5):1703‐10. [PUBMED: 15899916] [DOI] [PubMed] [Google Scholar]
Marik 2008
- Marik PE, Pastores SM, Annane D, Meduri GU, Sprung CL, Arlt W, et al. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Critical Care Medicine 2008;36(6):1937–49. [PUBMED: 18496365] [DOI] [PubMed] [Google Scholar]
Meduri 1998a
- Meduri GU, Chrousos GP. Duration of glucocorticoid treatment and outcome in sepsis: is the right drug used the wrong way?. Chest 1998;114(2):355‐60. [PUBMED: 9726712] [DOI] [PubMed] [Google Scholar]
Melby 1958
- Melby JC, Spink WW. Comparative studies on adrenal cortical function and cortisol metabolism in healthy adults and in patients with shock due to infection. Journal of Clinical Investigation 1958;37(12):1791‐8. [PUBMED: 13611047] [DOI] [PMC free article] [PubMed] [Google Scholar]
Menon 2013
- Menon K, McNally D, Choong K, Sampson M. A systematic review and meta‐analysis on the effect of steroids in pediatric shock. Pediatric Critical Care Medicine 2013;14(5):474‐80. [PUBMED: 23867428] [DOI] [PubMed] [Google Scholar]
Molijn 1995
- Molijn GJ, Koper JW, Uffelen CJ, Jong FH, Brinkmann AO, Bruining HA, et al. Temperature‐induced down‐regulation of the glucocorticoid receptor in peripheral blood mononuclear leucocyte in patients with sepsis or septic shock. Clinical Endocrinology 1995;43(2):197‐203. [PUBMED: 7554315 ] [DOI] [PubMed] [Google Scholar]
Moran 2010
- Moran JL, Graham PL, Rockliff S, Bersten AD. Updating the evidence for the role of corticosteroids in severe sepsis and septic shock: a Bayesian meta‐analytic perspective. Critical Care 2010;14(4):R134. [PUBMED: 20626892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ni 2018
- Ni YN, Liu YM, Wang YW, Liang BM, Liang ZA. Can corticosteroids reduce the mortality of patients with severe sepsis? A systematic review and meta‐analysis. American Journal of Emergency Medicine 2018;S0735‐6757:30953‐7. [PUBMED: 30522935] [DOI] [PubMed] [Google Scholar]
Nishida 2018
- Nishida O, Ogura H, Egi M, Fujishima S, Hayashi Y, Iba T, et al. The Japanese clinical practice guidelines for management of sepsis and septic shock 2016 (J‐SSCG 2016). Acute Medicine and Surgery 2018;5:3‐89. [PUBMED: 29445505] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norman 2004
- Norman AW, Mizwicki MT, Norman DP. Steroid‐hormone rapid actions, membrane receptors, and a conformational ensemble model. Nature Reviews. Drug Discovery 2004;3(1):27‐41. [PUBMED: 14708019] [DOI] [PubMed] [Google Scholar]
Park 2012
- Park HY, Suh GY, Song JU, Yoo H, Jo IJ, Shin TG, et al. Early initiation of low‐dose corticosteroid therapy in the management of septic shock: a retrospective observational study. Critical Care 2012;16(1):R3. [PUBMED: 22226237] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parrillo 1993
- Parrillo JE. Pathogenic mechanisms of septic shock. New England Journal of Medicine 1993;328(20):1471‐7. [PUBMED: 8479467] [DOI] [PubMed] [Google Scholar]
Peters 2008
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour‐enhanced meta‐analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61(10):991‐6. [PUBMED: 18538991] [DOI] [PubMed] [Google Scholar]
Polito 2011
- Polito A, Sonneville R, Guidoux C, Barrett L, Viltart O, Mattot V, et al. Changes in CRH and ACTH synthesis during experimental and human septic shock. PLoS One 2011;6(11):e25905. [PUBMED: 22073145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rhee 2017
- Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, et al. CDC Prevention Epicenter Program. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009‐2014. JAMA 2017;318(13):1241‐9. [PUBMED: 28903154] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rhen 2005
- Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids: new mechanisms for old drugs. New England Journal of Medicine 2005;353(16):1711‐23. [PUBMED: 16236742] [DOI] [PubMed] [Google Scholar]
Rhodes 2017
- Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Medicine 2017;43(3):304‐77. [PUBMED: 28101605] [DOI] [PubMed] [Google Scholar]
Rochwerg 2018
- Rochwerg B, Oczkowski SJ, Siemieniuk RAC, Agoritsas T, Belley‐Cote E, D'Aragon F, et al. Corticosteroids in sepsis: an updated systematic review and meta‐analysis. Critical Care Medicine 2018;46(9):1411‐20. [PUBMED: 29979221] [DOI] [PubMed] [Google Scholar]
Rothwell 1991
- Rothwell PM, Udwadia ZF, Lawler PG. Cortisol response to corticotropin and survival in septic shock. Lancet 1991;337(8741):582‐3. [PUBMED: 1671944] [DOI] [PubMed] [Google Scholar]
Rygard 2018
- Rygård SL, Butler E, Granholm A, Møller MH, Cohen J, Finfer S, et al. Low‐dose corticosteroids for adult patients with septic shock: a systematic review with meta‐analysis and trial sequential analysis. Intensive Care Medicine 2018;44(7):1003‐16. [PUBMED: 29761216] [DOI] [PubMed] [Google Scholar]
Sharshar 2003
- Sharshar T, Gray F, Lorin de la Grandmaison G, Hopkinson NS, Ross E, Dorandeu A, et al. Apoptosis of neurons in cardiovascular autonomic centres triggered by inducible nitric oxide synthase after death from septic shock. Lancet 2003;362(9398):1799‐805. [PUBMED: 14654318] [DOI] [PubMed] [Google Scholar]
Sherwin 2012
- Sherwin RL, Garcia AJ, Bilkovski R. Do low‐dose corticosteroids improve mortality or shock reversal in patients with septic shock? A systematic review and position statement prepared for the American Academy of Emergency Medicine. Journal of Emergency Medicine 2012;43(1):7‐12. [PUBMED: 22221983] [DOI] [PubMed] [Google Scholar]
Singer 2016
- Singer M, Deutschman CS, Seymour CW, Shankar‐Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis‐3). JAMA 2016;315(8):801‐10. [PUBMED: 26903338] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stata 2015 [Computer program]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015.
Tavaré 2017
- Tavaré A, O’Flynn N. Recognition, diagnosis, and early management of sepsis: NICE guideline. British Journal of General Practice 2017;67(657):185‐6. [PUBMED: 28360070] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsao 2004
- Tsao CM, Ho ST, Chen A, Wang JJ, Li CY, Tsai SK, et al. Low‐dose dexamethasone ameliorates circulatory failure and renal dysfunction in conscious rats with endotoxemia. Shock 2004;21(5):484‐91. [PUBMED: 15087827] [DOI] [PubMed] [Google Scholar]
Vachharajani 2006
- Vachharajani V, Vital S, Russell J, Scott LK, Granger DN. Glucocorticoids inhibit the cerebral microvascular dysfunction associated with sepsis in obese mice. Microcirculation 2006;13(6):477‐87. [PUBMED: 16864414 ] [DOI] [PubMed] [Google Scholar]
van der Poll 2017
- Poll T, Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nature Reviews. Immunology 2017;17(7):407‐20. [PUBMED: 28436424] [DOI] [PubMed] [Google Scholar]
Varga 2008
- Varga G, Ehrchen J, Tsianakas A, Tenbrock K, Rattenholl A, Seeliger S, et al. Glucocorticoids induce an activated, anti‐inflammatory monocyte subset in mice that resembles myeloid‐derived suppressor cells. Journal of Leukocyte Biology 2008;84(3):644‐50. [PUBMED: 18611985] [DOI] [PubMed] [Google Scholar]
Vincent 1996
- Vincent JL, Moreno R, Takala J, Willatts S, Mendonça A, Bruining H, et al. The SOFA (Sepsis‐related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis‐Related Problems of the European Society of Intensive Care Medicine. Intensive Care Medicine 1996;22(7):707‐10. [PUBMED: 8844239] [DOI] [PubMed] [Google Scholar]
Vincent 2013
- Vincent JL, Opal SM, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet 2013;381(9868):774‐5. [PUBMED: 23472921] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2018
- WHO. Improving prevention, diagnosis and clinical management of sepsis. https://www.who.int/servicedeliverysafety/areas/sepsis/en/#.XAAf362Zqkk.mendeley. 2018. Accessed 29 November 2018.
Yang 2018
- Yang T, Li Z, Jiang L, Xi X. Corticosteroid use and intensive care unit‐acquired weakness: a systematic review and meta‐analysis. Critical Care 2018;22(1):187. [DOI: 10.1186/s13054-018-2111-0; PUBMED: 30075789] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Annane 2004
- Annane D, Bellissant E, Bollaert PE, Briegel J, Keh D, Kupfer Y. Corticosteroids for treating severe sepsis and septic shock. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD002243.pub2] [DOI] [PubMed] [Google Scholar]
Annane 2009
- Annane D, Bellissant E, Bollaert PE, Briegel J, Confalonieri M, Gaudio R, et al. Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. JAMA 2009;301:2362‐75. [PUBMED: 19509383 ] [DOI] [PubMed] [Google Scholar]
Annane 2015
- Annane D, Bellissant E, Bollaert PE, Briegel J, Keh D, Kupfer Y. Corticosteroids for treating sepsis. Cochrane Database of Systematic Reviews 2015, Issue 12. [DOI: 10.1002/14651858.CD002243.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gibbison 2017
- Gibbison B, López‐López JA, Higgins JP, Miller T, Angelini GD, Lightman SL, et al. Corticosteroids in septic shock: a systematic review and network meta‐analysis. Critical Care 2017;21:78. [PUBMED: 28351429] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rochwerg 2018a
- Rochwerg B, Oczkowski SJ, Siemieniuk RAC, Agoritsas T, Belley‐Cote E, D'Aragon F, et al. Corticosteroids in sepsis: an updated systematic review and meta‐analysis. Critical Care Medicine 2018;46:1411‐20. [PUBMED: 29979221] [DOI] [PubMed] [Google Scholar]


