Abstract
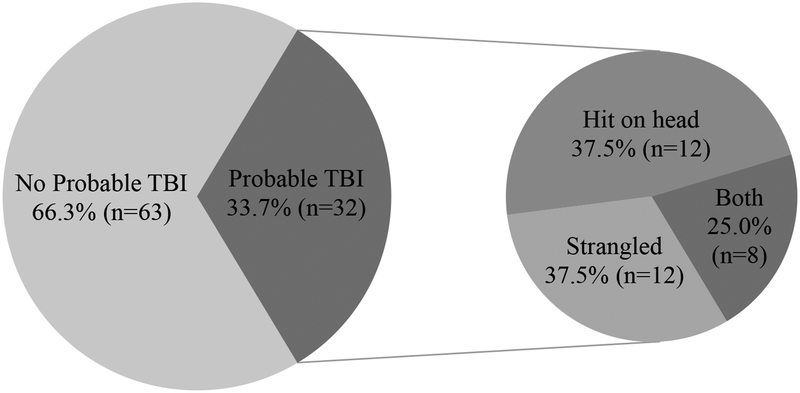
Severe intimate partner violence (IPV) including loss of consciousness from head injuries and/or strangulation can result in traumatic brain injury (TBI), a brain pathology characterized by altered brain function, cognitive impairment, and mental health disorders, including depression and posttraumatic stress disorder (PTSD). This study examines the prevalence of probable TBI (defined as loss of consciousness from a blow to the head and/or strangulation) and its association with comorbid PTSD and depression among Black women, who experience both higher rates of IPV and greater mental health burden than White and Latina women. Data come from a retrospective cohort study of 95 Black women with abuse history including IPV, forced sex, and childhood maltreatment. About one-third of women (n=32) had probable TBI. Among them, 38% (n=12) were hit on the head, 38% (n=12) were strangled to unconsciousness, and 25% (n=8) were strangled and hit on the head. Women with IPV history and probable TBI had significantly greater odds of various physical injuries including those that required medical care compared to other abused women. Probable TBI significantly increased comorbid PTSD and depression by 8.93 points (SE=3.40), after controlling for past violence (F(4, 90)=3.67, p<.01). Findings from this study reinforce the need to screen women who lost unconsciousness due to IPV for TBI and facilitate referrals to IPV interventions and mental health treatment.
Keywords: intimate partner violence, domestic violence, physical abuse, sexual abuse, depression, posttraumatic stress disorder, strangulation, unconscious
Intimate partner violence (IPV), the physical and/or sexual violence, stalking, and/or psychological aggression inflicted by a current or former intimate partner (Breiding, Basile, Smith, Black & Mahendra, 2015), is a pervasive public health concern. IPV can lead to long-lasting physical and mental health consequences. Physical IPV, the use of intentional physical force, can result in injuries, disability, and even death (Breiding et al., 2015). In fact, physical IPV is a leading cause of death for women under age 44 (Campbell, Webster, and Glass, 2009; [Centers for Disease Control and Prevention CDC, 2018]; Petrosky et al., 2017). Nearly 1 in 4 women in the United States (US) experience physical IPV at some point in their lifetime. Black women experience higher rates of physical IPV and intimate partner homicide compared to White and Latina women (Black et al., 2011; Smith et al., 2018), and therefore, experience greater mental health burden from violence (Stockman, Hayashi, & Campbell, 2015).
Physical IPV that results in the loss of consciousness from head injuries and/or non-fatal strangulation can cause neurological changes indicative of traumatic brain injury (TBI)—a brain pathology characterized by an alteration in brain function, cognitive impairment, and mental health disorders. Symptoms of TBI can include neurologic deficits, loss of consciousness, decreased level of consciousness, changes in mental state, and/or memory loss (CDC, 2016; Langlois, Rutland-Brown, & Wald, 2006). In the last decade, TBI rates have increased to nearly 2.5 million, due in part, to public recognition in athletic and military populations, as well as improved TBI screening methods (National Center for Injury Prevention and Control [NCIPC], 2003; Pervez, 2018). However, the literature on the contribution of IPV to TBI is scant. The prevalence of TBI in women with histories of abuse by an intimate partner is likely substantial, but needs further exploration (Valera & Kucyi, 2017). Despite the dearth in the literature, one study of 537 abused Black women sampled from health care sites found that 49% experienced symptoms consistent with TBI (i.e., probable TBI) from head injuries and/or strangulation due to physical IPV (Campbell et al, 2018).
What is Traumatic Brain Injury?
TBI is a disruption of the brain’s normal functioning after a blunt or penetrating head injury (Savitsky, Givon, Rozenfeld, Radomislensky, & Peleg, 2016). Asphyxia by strangulation (“choking”)—external pressure to the neck that closes off blood vessels and/or air passages, depriving the brain of oxygen (cerebral hypoxia)—is another trauma that can result in TBI (Sauvageau & Boghossian, 2010). Even mild oxygen deprivation, with no loss of consciousness can result in mild TBI (Murray, Lundgren, Olson, & Hunnicutt, 2016). Seizures, coma, and brain death may occur in prolonged hypoxia (National Institute of Neurological Disorders and Stroke [NINDS], 2018). Multiple head injuries sustained throughout childhood, adolescence, and young adulthood have a cumulative effect and can increase vulnerability to chronic traumatic encephalopathy (CTE), a progressive neurodegenerative brain disorder from repetitive TBIs (Laurer et al., 2001; Stern et al., 2011; McKee et al., 2009).
TBI is formally diagnosed via a brain scan (i.e., MRI, CAT scan, PET scan), but neuropsychological testing (i.e., Glasgow Coma Scale) can suggest probable TBI and help clarify the extent of neurocognitive damage (Chung & Khan, 2013; Rimel, Jane, & Edlich, 1979; Teasdale & Jannett, 1974). Gender disparity in diagnosis and recovery of TBI means that women (and their providers) may be less aware of TBI risks, symptoms, and effects (Banks, 2007). For instance, the frequency and severity of reported TBI symptomatology (e.g., higher rates of abnormal CT results, headaches, dizziness, memory problems, difficulty concentrating, etc. relative to men) differ between men and women (Alston, Jones, & Curtin, 2012; Colantonio, Harris, Ratcliff, Chase, & Ellis, 2010; Munivenkatappa et al, 2016). One study suggested that women had twice the concussion rate (a type of mild TBI) as men. Furthermore, women’s TBI severity was greater than men’s, as demonstrated by their higher three-month post-concussion injury scores (Laskowski, Creed, & Raghupathi, 2015). In another study, women also experienced higher mortality rates from brain injuries than did men (Munivenkatappa, Agrawal, Shukla, Kumaraswamy, & Devi, 2016).
Traumatic Brain Injury as a Result of Intimate Partner Violence
Physical IPV, particularly in instances where the head and/or the neck are being hit, kicked, or slammed against something hard (“coup-contrecoup injuries”), or hypoxic/anoxic injury from strangulation, can cause TBI (Drew & Drew, 2004). Studies find that between 40% and 92% of IPV victims have sustained head injuries and nearly half have been strangled (Kwako et al., 2011; St. Ivany, Schminket, 2016). One study indicated that as much as 50% of IPV victims (N=890) who have been hit on the head and/or strangled are believed to have TBI (“probable TBI”) (Campbell et al., 2017). Since TBI is commonly underdiagnosed among women seeking medical treatment for IPV-related injuries, women may be unaware that they have (or had) a TBI, and clinicians may not adequately treat those patients (CDC, 2015; Banks, 2007). Furthermore, since choking is a consensual, erotic fetish for some individuals, its significance can be downplayed—even among women with abuse histories (Khan, 2016; Rehor, 2015). Nevertheless, non-fatal strangulation from an intimate partner is associated with a 7.5-fold increase in homicide risk (Zilkens et al., 2016).
IPV victims who experienced multiple head and/or neck injuries can suffer repetitive TBIs, placing them at higher risk for long-term injury (Strack et al., 2018). For instance, Smith et al. (2001) found that women with IPV history, sustaining between two and five non-fatal strangulation events have significantly more memory loss and tinnitus (ringing in the ear) than women strangled only once. Additionally, women who were strangled more than five times reported more frequent muscle spasms, tinnitus, dizziness, and weakness on one side of the body. This is a significant point as IPV victims rarely suffer one physically violent event. A systematic review of brain injuries among IPV victims showed that between 23 to 72% of victims have been hit on the head or strangled five or more times (Kwako et al., 2011). Furthermore, sustaining subsequent head injuries before full resolution of an index TBI—referred to as “second impact syndrome”—may increase negative health effects, including cerebral vascular congestion, intracranial pressure, and cerebral edema. Second impact syndrome is associated with prolonged symptoms and poor neurorecovery; severe cases result in CTE or death (Laskowski et al., 2015).
Mental Health Effects of IPV and TBI
Evidence suggests that abused women are more likely to experience TBI than men (Smith et al., 2018) and with potentially more serious health consequences (Patch, Anderson & Campbell, 2017). Both IPV and TBI can result in significant acute and long-term mental health consequences. The mental health effects of IPV and TBI manifest in similar symptoms, making it difficult to differentiate between the two issues. For instance, people with IPV history and those with TBI both experience disruptions in cognitive functioning, mood, emotions, and sleep (Archiniegas, Anderson, Topkoff & McAllister, 2005; Murray et al., 2016). IPV victims who survive severe physical violence—whether significant brain injury occurred or not— frequently report difficulty concentrating, anxiety, depression, (Campbell, 2002) and/or nightmares and hypervigilance associated with PTSD (Woods et al., 2008); these symptoms are also common effects of TBI (Murray et al., 2016). Even symptoms of mild TBI, which includes memory loss, decreased motor coordination, difficulty maintaining attention, and poor judgement (Silver, McAllister & Arciniegas, 2009) are similar to what is observed from IPV (Campbell, 2002). Thus, findings once attributed solely to IPV-related mental health disorders may in fact reflect brain injury (Kwako et al., 2011), particularly with cumulative head and/or strangulation injuries, which is common among victims of violence (Sabri et al., 2016). Evidence shows that repeated head trauma, such as head injuries sustained in childhood or adulthood have a cumulative effect (Guskiewicz et al., 2003; Kwako et al., 2011); this can further hinder efforts to isolate the cause of TBI-related mental health conditions. For instance, female veterans with IPV-related TBI reported higher levels of comorbid PTSD and depression symptoms than female veterans with an IPV-related head injury event but no TBI and female veterans with no IPV-related head injury event (Iverson & Pogoda, 2015).
Purpose of the Study
This study examines the relationship between IPV, injuries associated with probable TBI (i.e., becoming unconscious from being hit on the head and/or strangulation), and their effect on mental health disorders (i.e., comorbid depression and PTSD) among abused Black women. We focus on Black women because they have higher rates of physical IPV (Black et al., 2011) and the greater mental health burden (Stockman et al., 2015). The first aim is to describe the prevalence of probable TBI among abused Black women. The second aim is to examine the relationship between past experiences of violence and probable TBI. Finally, the third aim is to assess the effect of past violence and probable TBI on mental health disorders (i.e. comorbid depression and PTSD). Understanding the association between IPV, TBI, and their effect on mental health is critical in ensuring appropriate assessment, treatment/rehabilitation, and safety planning for abuse victims (Ackerman & Banks, 2003).
Methods
In the present study, the authors analyzed data on 116 Black women from The ESSENCE Project (R01HD077891), a retrospective cohort study examining the association between features of the built and social environment (e.g., neighborhood disorder, crime, poverty, racism, etc.), sexual assault, and HIV risk factors among Black women in Baltimore, Maryland. Cohorts were comprised of abused and non-abused women, however the current data includes abused women only. Data were collected from November 2016 to May 2018. The study design and procedures were approved by the institutional review boards of Johns Hopkins University and the University of California, San Diego.
Procedure
Black women recruited from two Baltimore City public health STD clinic were asked to participate in The ESSENCE Project. After providing informed consent, participants were screened for eligibility. To be eligible, participants had to self-report being biologically female, between ages 18–44, Black or African American, having sex with a man in the past 6 months, and having had at least two sexual partners in the past year or a high HIV risk sexual partner (i.e., used injection/non-injection drugs, has sex with men, been to prison, concurrent sex partner, had an STD, or was HIV-positive). Eligible women completed a 60 to 90-minute survey collected via audio computer-assisted self-interview. Participants received $35 ($10 for screening, $25 for survey), a transportation pass, and list of local community resources.
Measures
Probable TBI.
The primary independent variable was probable TBI, which we defined probable TBI as either or both of the following two criterions: (1) becoming unconscious from a blow to the head, and/or (2) becoming unconscious from being choked (i.e., strangulation). The first criterion was measured using the single item above on the revised Conflict Tactics Scale-2 (CTS-2; Straus, Hambly, Boney-McCoy & Sugarman, 1996). The second criterion was measured from an item on the study’s screening survey (i.e., has your partner ever choked you until you became unconscious). Affirmative responses were classified as probable TBI (yes = 1; no = 0).
Past experiences of violence.
The control variables included past experiences of violence, which scored individually, since it was identified in the literature as independently associated with mental health disorders (Chapmen et al., 2004; Glover et al., 2010; Suliman, et al., 2009) and we sought to isolate past violence from TBI-related mental health effects. Past violence included: (1) childhood maltreatment, (2) types of lifetime IPV, and (3) history of non-intimate partner forced sex. Childhood maltreatment was measured with two items from the screening survey: (1) “As a child, did anyone physically abuse you (by physical abuse, we mean slapping, beating, kicking, choking, or threats with weapons)?” and (2) “As a child, did anyone sexually abuse you (by sexual abuse, we mean forcing or pressuring for sex or physically hurting the sexual parts of your body, including touching that made you uncomfortable)?”. Categories of childhood maltreatment included: (0) no childhood abuse, (1) childhood physical abuse only, (2) childhood sexual abuse only, and (3) both childhood physical and sexual abuse. Types of lifetime IPV was a summation of yes responses to any item in subscales of the CTS-2: (a) psychological aggression, (b) physical assault, and (c) injury from a partner (sexual violence was not included in the analysis because all participants were exposed to forced sex). Individual CTS-2 items, as well as categories of lifetime IPV (listed above), and a summation of types of lifetime IPV (range: 0 to 3) were analyzed. History of non-intimate partner forced sex was a dichotomous variable defined as someone who was not a current or former intimate partner ever using force (i.e., hitting, holding down, or using a weapon) or threats of force to make you have sex.
Mental health.
The primary dependent variable was mental health, specifically comorbid depression and PTSD. Depressive symptoms in the past week was measured using the 4-point, 10-item Center for Epidemiologic Studies Short Depression scale (CESD-10) (Andresen, Malmgren et al., 1994). Example items included, “feeling lonely,” “could not get going,” and “sleep was restless”. CESD-10 showed internal consistency in this sample (α=.88). PTSD symptoms in the past month was measured using the 4-point, 9-item National Stressful Events Survey PTSD Short Scale (NSESSS) (LeBeau, Mischel et al. 2014). Items included having a very negative emotional state and being super alert, on guard, or constantly on the lookout for danger. Items were summed (range: 0–36) and showed internal consistency in this sample (α=.91). The CESD-10 and NSESS were scored individually and then summed to create a composite variable representing comorbid PTSD and depression (range: 0–66).
Analysis
First, skewness and kurtosis tests of normality were conducted. Second, descriptive statistics were generated to compare sociodemographic characteristics of the sample using the dichotomized probable TBI measure. Third, bivariate associations between probable TBI and lifetime IPV types were assessed with Pearson’s chi-square tests for categorical variables and independent t-tests for continuous variables. Finally, a multiple linear regression was conducted to ascertain the independent effect of probable TBI on PTSD and depression (individually and comorbid), adjusting for past violence (i.e., lifetime history of non-intimate partner forced sex, types of lifetime IPV, and childhood maltreatment). Of 116 study participants, 18% (n=21) abstained from responding to some or all of the CTS-2 items or responded with “I don’t know.” These participants were subsequently excluded from the final regression analyses, resulting in a final sample size of 95. All statistical analyses were conducted using Stata (Version 15.1).
Results
Sample Description
Table 1 reports the sample demographics. The mean age among the 95 study participants was 28.8 (SD 7.34). Approximately 22% (n=21) of the sample did not complete high school, 30.5% (n=29) had a high school degree or GED equivalent, 25.3% (n=24) had some college or trade/vocational training, and 22.1% (n=21) completed college or graduate school. The majority of participants (64.2%, n=61) earned an annual income of less than $10,000. Half of the sample (50.5%, n=48) were currently employed. The majority of the sample (73.7%, n=70), reported receiving public assistance (e.g., housing, Medicaid, WIC, food stamps, and disability assistance, etc.). Approximately half of the sample (51.6%, n=49) had children. There were no significant demographic differences between women with abuse history with and without probable TBI except for the number of women who had children (χ2=11.5, p<0.05).
Table 1.
Demographic Characteristics of Black Women with Abuse History (N=95)
| Characteristic | Total Sample (N=95) | Women with no TBI (n=63) | Women with Probable TBI (n=32) | X2 |
|---|---|---|---|---|
| N(%) | n(%) | n(%) | ||
| Age | 5.56 | |||
| < 20 | 8(8.42) | 0(0) | 8(8.42) | |
| 20–29 | 50(52.6) | 33(34.7) | 17(17.9) | |
| 30–39 | 25(26.3) | 16(16.8) | 9(9.47) | |
| 40–49 | 12(12.6) | 6(6.32) | 6(6.32) | |
| Race | 9.54 | |||
| Black or African-American | 85(89.5) | 58(61.1) | 27(28.4) | |
| Black or African-Caribbean | 4(4.21) | 4(4.21) | 2(2.11) | |
| Black or African Born | 3(3.16) | 1(1.05) | 2(2.11) | |
| Mixed | 2(2.11) | 0(0) | 2(2.11) | |
| Other | 1(1.05) | 0(0) | 1(1.05) | |
| Education | 4.82 | |||
| > 9th grade, did not complete high school | 21(22.1) | 13(13.7) | 8(8.42) | |
| High school grad or GED | 29(30.5) | 22(23.2) | 7(7.37) | |
| Some trade/vocational school or college | 24(25.3) | 13(13.7) | 11(11.6) | |
| Completed college, trade/ vocational, or graduate school | 21(22.1) | 15(15.8) | 6(6.32) | |
| Income ($) | 2.31 | |||
| Less than 10,000 | 61(64.2) | 23(24.2) | 38(40.0) | |
| Between 10,000 – 19,000 | 17(17.9) | 5(5.26) | 12(12.6) | |
| Between 20,000 – 29,000 | 11(11.6) | 3(3.16) | 8(8.42) | |
| 30,000 or more | 6(6.32) | 1(1.05) | 5(5.26) | |
| Number of Children | 11.5* | |||
| No children | 46(48.4) | 34(54.0) | 12(12.6) | |
| 1 | 20(21.11) | 16(16.8) | 4(4.21) | |
| 2 | 15(15.8) | 5(5.26) | 10(10.5) | |
| 3 or more | 14(14.7) | 8(8.42) | 6(6.32) | |
| Currently Employed | 47(49.5) | 34(35.8) | 13(13.7) | 1.51 |
| Receiving Assistance1 | 70(73.7) | 44(46.3) | 26(27.4) | 1.42 |
Refers to assistance such as housing, Medicaid, WIC, food stamps, and disability assistance.
Note: p<.05
Aim 1: Prevalence of Probable TBI Among Black Women with Abuse History
Of the 95 women, 33.7% (n=32) were identified as having probable TBI, of which 37.5% (n=12) were hit on the head, 37.5% (n=12) were strangled to unconsciousness, and 25.0% (n=8) were strangled and hit on the head in the past year (results not shown). Figure 1 shows the overlap between these categories. Of the 32 women who were identified as having probable TBI, 28.1% (n=9) lost consciousness multiple times, and thus may have sustained multiple TBIs.
Figure 1.
Proportion of Patterns of Violence Resulting in Probable TBI Among Black Women
Aim 2: The Relationship Between Past Experiences of Violence and Probable TBI
Table 2 reports the relationship between past experiences of violence and probable TBI. About three in four women (77.9%, n=74) experienced at least one form of childhood maltreatment (i.e., physical abuse, sexual abuse, or both). Among those women, 19.0% (n=18) reported physical abuse only, 17.9% (n=17) reported sexual abuse only, and 41.1% (n=39) reported both physical and sexual child maltreatment. Pearson’s chi-square test of association indicated that childhood maltreatment was significantly associated with probable TBI (χ2=10.4, p<.05). Just over half of the sample (55.8%, n=53) experienced non-partner forced sex. There was no significant association between probable TBI and non-partner forced sex experience. All participants experienced some form of lifetime IPV with psychological abuse being most prevalent, followed by physical IPV, and injury. Pearson’s chi-square test of association revealed that types of lifetime IPV was significantly associated with probable TBI (χ2=18.7, p<.001).
Table 2.
Past Violence between Black Women with and without Probable TBI (N=95)
| Characteristic | Total Sample (N=95) | Women without TBI (n=63) | Women with Probable TBI (n=32) | X2 |
|---|---|---|---|---|
| N(%) | n(%) | n(%) | ||
| Childhood Abuse | 10.4* | |||
| No childhood maltreatment | 21(22.1) | 16(25.4) | 5(15.6) | |
| Childhood physical abuse only | 18(18.9) | 10(15.9) | 8(25.0) | |
| Childhood sexual abuse only | 17(17.9) | 16(25.4) | 1(3.12) | |
| Both childhood physical and sexual abuse | 39(41.1) | 21(33.3) | 18(56.3) | |
| Types of Lifetime IPV | - | - | - | 18.7*** |
| Psychological IPV | 75(78.9) | 46(73.0) | 29(90.6) | |
| Physical IPV | 57(60) | 32(50.8) | 25(78.1) | |
| Injury from partner | 47(49.5) | 22(34.9) | 25(78.1) | |
| Non-partner forced sex | 53(55.8) | 31(49.2) | 22(68.8) | 3.29** |
Note: p<.05;
p<.01;
p<.001
Although all 95 participants were abused by an intimate partner, women classified as having probable TBI had significantly greater odds of experiencing psychological IPV (OR=3.57, 95% CI: 0.90–20.4, p<0.05), physical IPV (OR=3.45, 95% CI: 1.21–10.8, p<0.05), and receiving an injury from an intimate partner (OR=6.66, 95% CI: 2.29–20.8, p<.001).
Aim 3: The Effect of Past Violence and TBI on Mental Health Outcomes
The average depression score among the entire sample was 13.5 (SD=7.06). The CESD-10 cut off score of > or = 10 indicates significant depressive symptoms (Andresen, Malmgren et al., 1994). Women identified as having probable TBI had depression scores 2.65 points higher than women without probable TBI (average score of 15.3 (SD=7.09) vs. 12.6 (SD=6.95), respectively), though this difference was not statistically significant. PTSD scores among the entire sample was 19.5 (SD=10.1). The NSESSS cut off score of > or = 24 indicates significant PTSD symptoms (LeBeau, Mischel et al. 2014). Women identified as having probable TBI scored an average of 7.76 points higher on the PTSD scale that women without probable TBI (average score of 24.8 (SD=8.08) vs. 16.9 (SD=9.95), respectively), which was statistically significant (95% CI: −11.7– −4.17, p<.001). Comorbid depression and PTSD in the entire sample was 33.1 (SD=15.1). Women identified as having a probable TBI had an average of 10.6 points higher compared to women without probable TBI (average comorbid score of 40.1 (SD=13.3) vs. 29.5 (SD=14.8), respectively), which was statistically significant (95% CI: −16.6–4.61, p<0.001).
Table 3 shows the multivariate regression results. In the unadjusted regression model (1a) for depression only (F(1, 93)=3.04, p<.10), probable TBI increased the CESD depression score by 2.64 (SE=1.52, p<0.10). In the adjusted model (1b) that controlled for past violence, TBI was not significantly associated with depression symptomatology. With regard to PTSD only, in the unadjusted regression model (2a) (F(1, 93)=15.3, p<.001) showed that probable TBI increased PTSD symptoms by 7.96 (SE=2.03, p<0.001). In the adjusted model for PTSD only (2b) controlling for past experiences of violence (F(4, 90)=4.51, p<.005), TBI was independently associated with an increase in number of PTSD symptoms by 7.16 (SE=2.23, p<0.005).
Table 3.
Multivariate Regression Model Examining Effect of Past Violence and TBI on Mental Health Outcomes (N=95)
| Model | β | SE | 95% CI | p |
|---|---|---|---|---|
| 1a: Depression only | ||||
| Probable TBI | 2.64 | 1.52 | ‒0.37–5.66 | 0.09 |
| Past IPV | 1.16 | 0.62 | ‒0.06–2.39 | 0.06 |
| Childhood maltreatment | 0.52 | 0.61 | ‒0.68–1.72 | 0.39 |
| Non-partner forced sex | 0.52 | 1.47 | ‒2.40–3.43 | 0.73 |
| 1b: Depression only, adjusted for past violence | ||||
| Probable TBI | 1.77 | 1.67 | ‒1.54–5.08 | 0.29 |
| Past IPV | 0.87 | 0.67 | ‒0.46–2.20 | 0.20 |
| Childhood maltreatment | 0.35 | 0.62 | ‒0.89–1.59 | 0.57 |
| Non-partner forced sex | ‒0.05 | 1.78 | ‒3.06–2.97 | 0.98 |
| 2a: PTSD only | ||||
| Probable TBI | 7.96 | 2.03 | 3.92–12.0 | 0.000 |
| Past IPV | 2.16 | 0.87 | 0.44–3.88 | 0.014 |
| Childhood maltreatment | 0.92 | 0.86 | ‒0.79–2.63 | 0.29 |
| Non-partner forced sex | ‒0.10 | 2.09 | ‒4.25–4.04 | 0.96 |
| 2b: PTSD only, adjusted for past violence | ||||
| Probable TBI | 7.16 | 2.23 | 2.73–11.6 | 0.002 |
| Past IPV | 1.07 | 0.89 | ‒0.71–2.84 | 0.24 |
| Childhood maltreatment | 0.63 | 0.83 | ‒1.03–2.28 | 0.45 |
| Non-partner forced sex | ‒1.79 | 2.03 | ‒5.82–2.23 | 0.38 |
| 3a: Comorbid PTSD and depression | ||||
| Probable TBI | 10.6 | 3.11 | 4.43–16.8 | 0.001 |
| Past IPV | 3.33 | 1.30 | 0.75–5.90 | 0.012 |
| Childhood maltreatment | 1.44 | 1.29 | ‒1.12–4.00 | 0.27 |
| Non-partner forced sex | 0.41 | 3.14 | ‒5.81–6.64 | 0.90 |
| 3b: Comorbid PTSD and depression, adjusted for past violence | ||||
| Probable TBI | 8.93 | 3.40 | 2.18–15.7 | 0.010 |
| Past IPV | 1.94 | 1.36 | ‒0.77–4.64 | 0.16 |
| Childhood maltreatment | 0.98 | 1.27 | ‒1.54–3.51 | 0.44 |
| Non-partner forced sex | ‒1.84 | 3.09 | ‒7.98–4.31 | 0.55 |
Note: SE = Standard error; CI = Confidence Interval; past violence includes lifetime history of non-intimate partner forced sex, types of lifetime IPV, and childhood maltreatment
Finally, in the unadjusted model (3a) for comorbid PTSD and depression (F(1, 93)=11.7, p<.005), probable TBI increased comorbid PTSD and depression by 10.6 (SE=3.11, p<.005). In the adjusted model (F(4, 90)=3.67, p<.01) (3b) that controlled for past violence, probable TBI independently increased the cumulative number of symptoms by 8.93 (SE=3.40, p<.05).
Discussion
The present study estimated the prevalence of probable TBI among a sample of Black women with abuse history from community health clinics (i.e., not from domestic violence service organizations nor women who had sought help from the police department), and investigated the associations between probable TBI, past IPV experience, and comorbid PTSD and depression. We found three key results that carry public health implications for TBI screening among women with histories of abuse.
First, TBI from physical IPV was prevalent with about one-third of the sample (33.7%) sustaining injuries associated with probable TBI. This is a comparable, or somewhat smaller proportion, than that found in the scant literature on IPV-related TBI from both head injuries and strangulation. One study, which used a convenience sample of 99 women with severe IPV, found that about 75% of the women experienced at least one TBI and 50% had experienced multiple TBIs (Valera & Berenbaum, 2003). Another study using less stringent criteria for TBI than the present study (i.e., injuries to head and face &/or strangulation but not necessarily to unconsciousness) found a 50% prevalence among 537 African American women with abuse histories, sampled from primary health care settings, with 7% reporting a head injury with loss of consciousness, 31% reporting any head injury, and 36% reporting strangulation but not necessarily with unconsciousness, and the overlap of the prior two categories not reported (Campbell et al, 2018). Iverson and Pagoda (2015) surveyed 179 female veterans and found 19% reported experiencing one or more acts of physical IPV to the head, neck or face that resulted in loss of consciousness, alternations in consciousness, posttraumatic amnesia, concussion or head injury (IPV-related strangulation was not assessed). The high prevalence of IPV-related probable TBI is alarming and calls for changes in the healthcare system to improve screening for TBI among girls and women with histories of abuse (Ackerman & Banks, 2003).
Non-fatal strangulation, the most common mechanism of probable TBI in the present sample, was particularly alarming given strangulation is associated with a 6-fold increased odds of experiencing attempted homicide and a 7-fold increased odds of homicide compared to women with abuse histories who have never been strangled (Glass et al, 2008). This finding carries strong implications for the need to screen for strangulation among women in abusive relationships to better understand the prevalence of TBI and to intervene in order to prevent intimate partner homicide. TBI among women with histories of abuse often underdiagnosed or overlooked (Banks, 2007). Enhanced screening for TBI-related symptoms may improve our understanding of the prevalence and health repercussions for TBI among women with histories of abuse (Hux, Schneider & Bennett, 2009), and prevent future incidents of violence or lethality.
Second, women classified as experiencing probable TBI also experienced more overall violence than women with histories of abuse without probable TBI. Physical, sexual, and psychological IPV were significantly and strongly associated with probable TBI. This finding supports the literature that states women who have repetitive head injury could have increased vulnerability to TBI. Additionally, women with probable TBI experienced physical violence in which they reported injuries that require medical attention, presenting an important opportunity for screening and intervention from medical care providers. Further, significant associations were found between probable TBI and forced sex and childhood maltreatment (i.e., physical abuse, sexual abuse, or both). This is particularly important, as it is common for women with experiences of IPV to have histories of childhood maltreatment (Chapmen et al., 2004; Glover et al., 2010; Suliman, et al., 2009) and there is a strong likelihood that those women have experienced previous TBIs as girls and young women. Cumulative TBI has been linked to more severe and long-lasting TBI symptoms (Guskiewicz et al., 2003), therefore, may increase risk and severity of PTSD and depression.
Lastly, probable TBI was associated with increased psychological abuse and independently increased comorbid PTSD and depression symptoms, even after controlling for past violence. Strangulation is a physical abuse tactic, but has implicit psychological effects signaling that the abuser has the capacity to take the victims life (Training Institute for Strangulation Prevention, 2017). Future prospective studies are needed to tease out the mental health sequelae of IPV and TBI, as the effects often overlap (Kwako et al., 2011).
Implications for Practice
Results reinforce the critical need for healthcare professionals to assess women for IPV, to inquire about recent and/or past injuries resulting in unconsciousness (i.e., strangulation, hit on the head), and to screen women with histories of IPV for TBI-related neurological disorders and facilitate linkage to mental health treatment. Among the 28.1% (n=9) of women who reported lost consciousness multiple times is concerning, as this underscores the need for healthcare systems to prudently assess for IPV, as well as screen quickly for TBI among women with histories of IPV (e.g. using the screen for DV related TBI developed by the VA (Iverson et. Al, 2017) in order to ensure the women receive the psychological and neurological referrals needed that will assess for cognitive function alterations. If there has been recent TBI, either from head injury and/or strangulation, emergency care is immediately needed (see emergency protocols at www.strangulationinstitute.org). Referring and providing interventions that specifically address historical or recent IPV would be beneficial to the women, as such programs have been show to improve women’s mental health sequelae. Specifically, self-care engagement and self-efficacy have been identified as internal resources for managing abusive relationships (Sabri et al., 2016).
Limitations
There are limitations to this study. First, the study is retrospective, therefore we cannot ascertain whether the mental health outcomes observed were due to the physical IPV injuries, probable TBI, or some other confounding effect. Second, the parent study’s eligibility criteria sought to examine Black women at risk for HIV who experienced forced sex (i.e., multiple male sex partners and/or partners with multiple HIV risk behaviors); thus, the sample is not representative of all abused women, nor all Black women. Another limitation relates to the variability in accepted definitions and diagnosis of TBI. The present study classified women who were hit on the head and/or strangled to unconsciousness as experiencing probable TBI; however, some definitions of TBI (Crowe et al., 2018; Leo & McCrea, 2016; Savitsky, Givon, Rozenfeld, Radomislensky, & Peleg, 2016) define is as a result of head injuries only. Relatedly, this study relied on self-reported IPV and loss of consciousness, which are subject to recall bias. Relatedly, we measured depression in the past week, PTSD in the past month, and controlled for lifetime PTSD, which may have introduced error and are subject to recall bias. Finally, we were only able to infer probable TBI, and did not specifically screen for nor test for TBI. While assessments such as the Glasgow Coma Scale (Teasdale & Jennett, 1974) are available, brain scans ante- and post-mortem are the most definitive (Panzer, Covaliav, Augat, & Peschel, 2017) diagnostic methods, and were not feasible in the present study. Additionally, we did not measure neurological symptoms associated with TBI. Despite these limitations, the results are compelling and call for further studies examining the prevalence of IPV and TBI to further understand this phenomenon.
Conclusion
In conclusion, the present study demonstrated that a significant proportion of abused Black women who sustained probable TBI injuries had a greater likelihood of experiencing comorbid PTSD and depression. These findings reinforce the critical need for healthcare professionals to assess for IPV, screen for TBI-related neurological disorders and injuries including recent and/or past unconsciousness, and facilitate linkage to IPV interventions and mental health treatment.
Acknowledgements:
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD077891-J.K. Stockman, J.C. Campbell, A.N. Cimino, K. Tsuyuki), the National Institute on Minority Health and Health Disparities (L60MD003701-J.K. Stockman; L60MD011184-K. Tsuyuki), and the National Institute of Alcohol Abuse and Alcoholism (K01AA025009-K. Tsuyuki). This research was also supported by the Center for AIDS Research (CFAR) at Johns Hopkins University (P30AI094189- A.N. Cimino) and University of California, San Diego (P30AI036214), an NIH-funded program which is supported by the following NIH Institutes and Centers: NIAID, NCI, NIMH, NIDA, NICHD, NHLB, NIA, NIGMS, and NIDDK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the paper.
Contributor Information
Andrea N. Cimino, Johns Hopkins University School of Nursing, Baltimore, MD, USA;.
Grace Yi, Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD, USA;.
Michelle Patch, Johns Hopkins University School of Nursing, Baltimore, MD, USA;.
Yasmin Alter, US Army’s Sexual Harassment and Assault Response and Prevention (SHARP) Program;.
Jacquelyn C. Campbell, Johns Hopkins University School of Nursing, Department of Community Public Health, Baltimore, MD, USA;.
Kristin K. Gundersen, University of California San Diego, Division of Infectious Diseases and Global Public Health, Department of Medicine La Jolla, CA, USA;.
Judy T. Tang, University of California San Diego, Division of Infectious Diseases and Global Public Health, Department of Medicine La Jolla, CA, USA;.
Kiyomi Tsuyuki, University of California San Diego, Division of Infectious Diseases and Global Public Health, Department of Medicine La Jolla, CA, USA;.
Jamila K. Stockman, Vice Chief University of California San Diego, Division of Infectious Diseases and Global Public Health, Department of Medicine La Jolla, CA, USA.
References
- Ackerman RJ, & Banks ME (2003). Assessment, treatment, and rehabilitation for interpersonal violence victims: Women sustaining head injuries. Women & Therapy, 26, 343–363. [Google Scholar]
- Alston M, Jones J, & Curtin M (2012). Women and traumatic brain injury: “It’s not visible damage”. Australian Social Work, 65(1), 39–53. Doi: 10.1080/0312407X.2011.594898 [DOI] [Google Scholar]
- Anderson JC, Stockman JK, Sabri B, Campbell DW, & Campbell JC (2015). Injury outcomes in African American and African Caribbean women: The role of intimate partner violence. Journal of Emergency Nursing, 41(1), 36–42. Doi: 10.1016/j.jen.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, & Patrick DL (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American journal of preventive medicine, 10(2), 77–84. [PubMed] [Google Scholar]
- Arciniegas DB, Anderson CA, Topkoff J, & McAllister TW (2005). Mild traumatic brain injury: a neuropsychiatric approach to diagnosis, evaluation, and treatment. Neuropsychiatric disease and treatment, 1(4), 311–327. [PMC free article] [PubMed] [Google Scholar]
- Banks ME (2007). Overlooked but critical: Traumatic brain injury as a consequence of interpersonal violence. Trauma, Violence, & Abuse, 8(3), 290–298. Doi: 10.1177/1524838007303503 [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Chen J, & Stevens MR (2011). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Breiding MJ, Basile KC, Smith SG, Black MC, Mahendra RR (2015). Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 2.0. Atlanta (GA): National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Campbell J (2002). Health consequences of intimate partner violence. Lancet, 359, 1331–1336. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Anderson JC, McFadgion A, Gill J, Zink E, Patch M….& Campbell D (2018). The effects of intimate partner violence and probable traumatic brain injury on central nervous system symptoms. Journal of Women’s Health, 27(6), 761–767. Doi: 10.1089/jwh.2016.6311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC, Webster DW, & Glass N (2009). The danger assessment: validation of a lethality risk assessment instrument for intimate partner femicide. Journal of interpersonal violence, 24(4), 653–674. Doi: 10.1177/0886260508317180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (2018). Leading Causes of Death in Females, 2015 (current listing). Accessed July 29, 2018 at https://www.cdc.gov/women/lcod/2015/all-females/index.htm [Google Scholar]
- CDC. (2016). Basic information about traumatic brain injury and concussion. National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention; Atlanta, GA: Accessed July 29, 2018 at https://www.cdc.gov/traumaticbraininjury/basics.html. [Google Scholar]
- CDC. (2015). Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention; Atlanta, GA. [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of affective disorders, 82(2), 217–225. Doi: 10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- Chung P, & Khan F (2013). Traumatic brain injury (TBI): Overview of diagnosis and treatment. Journal of Neurology & Neurophysiology, 5(1), 182–92. [Google Scholar]
- Colantonio A, Harris JE, Ratcliff G, Chase S, & Ellis K (2010). Gender differences in self reported long term outcomes following moderate to severe traumatic brain injury. BMC neurology, 10(1), 102 Doi: 10.1186/1471-2377-10-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe LM, Hearps S, Anderson V, Borland ML, Phillips N, Kochar A, … & Neutze J (2018). Investigating the variability in mild traumatic brain injury definitions: a prospective cohort study. Archives of physical medicine and rehabilitation. Doi: 10.1016/j.apmr.2017.12.026 [DOI] [PubMed] [Google Scholar]
- Drew LB, & Drew WE (2004). The contrecoup-coup phenomenon. Neurocritical care, 1(3), 385–390. Doi: 10.1385/NCC:1:3:385 [DOI] [PubMed] [Google Scholar]
- Glass N, Laughon K, Campbell J, Block CR, Hanson G, Sharps PW, & Taliaferro E (2008). Non-fatal strangulation is an important risk factor for homicide of women. The Journal of emergency medicine, 35(3), 329–335. Doi: 10.1016/j.jemermed.2007.02.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover DA, Loeb TB, Carmona JV, Sciolla A, Zhang M, Myers HF, & Wyatt GE (2010). Childhood sexual abuse severity and disclosure predict posttraumatic stress symptoms and biomarkers in ethnic minority women. Journal of Trauma & Dissociation, 11(2), 152–173. Doi: 10.1080/15299730903502920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guskiewicz KM, McCrea M, Marshall SW, Cantu RC, Randolph C, Barr W, … Kelly JP (2003). Cumulative effects associated with recurrent concussion in collegiate football players. Journal of the American Medical Association, 290, 2549–2555. [DOI] [PubMed] [Google Scholar]
- Hux K, Schneider T, & Bennett K (2009). Screening for traumatic brain injury. Brain Injury, 23(1), 8–14. [DOI] [PubMed] [Google Scholar]
- Khan Ummni (2016). Take my breath away: Competing contexts between domestic violence, kink and the criminal justice system in R. vs. J.A. Oñati Socio-Legal Series, 6(6). [Google Scholar]
- Kwako LE, Glass N, Campbell J, Melvin KC, Barr T & Gill JM (2011). Traumatic brain injury in intimate partner violence: A critical review of outcomes and mechanisms. Trauma Violence Abuse, 12(3), 115–126. Doi: 10.1177/1524838011404251. [DOI] [PubMed] [Google Scholar]
- Iverson KM, & Pogoda TK (2015). Traumatic brain injury among women veterans: An invisible wound of intimate partner violence. Medical Care, 53(4 Suppl 1), S112–119. Doi: 10.1097/MLR.0000000000000263. [DOI] [PubMed] [Google Scholar]
- Iverson KM, Dardis CM, & Pogoda TK (2017). Traumatic brain injury and PTSD symptoms as a consequence of intimate partner violence. Comprehensive Psychiatry, 74, 80–87. Doi: 10.1016/j.comppsych.2017.01.007. [DOI] [PubMed] [Google Scholar]
- Kwako LE, Glass N, Campbell J, Melvin KC, Barr T, & Gill JM (2011). Traumatic brain injury in intimate partner violence: A critical review of outcomes and mechanisms. Trauma, Violence, & Abuse, 12(3), 115–126. Doi: 10.1177/1524838011404251 [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, & Wald MM (2006). The epidemiology and impact of traumatic brain injury: a brief overview. The Journal of head trauma rehabilitation, 21(5), 375–378. [DOI] [PubMed] [Google Scholar]
- Laskowski RA, Creed JA, & Raghupathi R (2015). Chapter 4: Pathophysiology of Mild TBI Implications for Altered Signaling Pathways In Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Boca Raton, FL: Taylor & Francis. [PubMed] [Google Scholar]
- Laurer HL, Bareyre FM, Lee VM, Trojanowski JQ, Longhi L, Hoover R, & McIntosh TK (2001). Mild head injury increasing the brain’s vulnerability to a second concussive impact. Journal of neurosurgery, 95(5), 859–870. [DOI] [PubMed] [Google Scholar]
- LeBeau R, Mischel E, Resnick H, Kilpatrick D, Friedman M, & Craske M (2014). Dimensional assessment of posttraumatic stress disorder in DSM-5. Psychiatry research, 218(1–2), 143–147. Doi: 10.1016/j.psychres.2014.03.032 [DOI] [PubMed] [Google Scholar]
- Leo P, & McCrea M (2016). Chapter 1: Epidemiology In Translational Research in Traumatic Brain Injury. Boca Raton, FL: CRC Press/ Taylor & Francis. [Google Scholar]
- McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, … & Stern RA (2009). Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. Journal of Neuropathology & Experimental Neurology, 68(7), 709–735. Doi: 10.1097/NEN.0b013e3181a9d503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munivenkatappa A, Agrawal A, Shukla DP, Kumaraswamy D, & Devi BI (2016). Traumatic brain injury: Does gender influence outcomes? International journal of critical illness and injury science, 6(2), 70 Doi: 10.4103/2229-5151.183024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CE, Lundgren K, Olson LN, & Hunnicutt G (2016). Practice update: What professionals who are not brain injury specialists need to know about intimate partner violence-related traumatic brain injury. Trauma, Violence, & Abuse, 17(2), 298–305. Doi: 10.1177/1524838015584364 [DOI] [PubMed] [Google Scholar]
- National Center for Injury Prevention and Control. (2003). Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- National Institute of Neurological Disorders and Stroke. (2018). Cerebral Hypoxia Information Page. Retrieved from https://www.ninds.nih.gov/Disorders/All-Disorders/Cerebral-Hypoxia-Information-Page
- Panzer S, Covaliov L, Augat P, & Peschel O (2017). Traumatic brain injury: Comparison between autopsy and ante-mortem CT. Journal of forensic and legal medicine, 52, 62–69. Doi: 10.1016/j.jflm.2017.08.007 [DOI] [PubMed] [Google Scholar]
- Patch M, Anderson JC, & Campbell JC, (2017) Injuries of women surviving intimate partner strangulation and subsequent emergency health care seeking: An integrative evidence review. Journal of Emergency Nursing, S0099–1767(17), 30432–30434. Doi: 10.1016/j.jen.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pervez M, Kitagawa RS, & Chang TR (2018). Definition of traumatic brain injury, neurosurgery, trauma orthopedics, neuroimaging, psychology, and psychiatry in mild traumatic brain injury. Neuroimaging Clinics of North America, 28(1), 1–13. Doi: 10.1016/j.nic.2017.09.010. [DOI] [PubMed] [Google Scholar]
- Petrosky E, Blair JM, Betz CJ, Fowler KA, Jack SP, & Lyons BH (2017). Racial and ethnic differences in homicides of adult women and the role of intimate partner violence—United States, 2003–2014. MMWR. Morbidity and mortality weekly report, 66(28), 741 Doi: 10.15585/mmwr.mm6628a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehor JE (2015). Sensual, erotic, and sexual behaviors of women from the “kink” community. Archives of Sexual Behavior, 44(4), 825–836. Doi: 10.1007/s10508-015-0524-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimel RW, Jane JA, & Edlich RF (1979). An injury severity scale for comprehensive management of central nervous system trauma. Journal of the American College of Emergency Physicians, 8(2), 64–67. [DOI] [PubMed] [Google Scholar]
- Sabri B, Holliday CN, Alexander KA, Huerta J, Cimino A, Callwood GB, & Campbell JC (2016). Cumulative violence exposures: Black women’s responses and sources of strength. Social Work in Public Health, 31(3), 127–139. doi-org.ezp.welch.jhmi.edu/10.1080/19371918.2015.1087917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauvageau A, & Boghossian E (2010). Classification of asphyxia: The need for standardization. Journal of Forensic Science, 55(5), 1259–1267.. doi: 10.1111/j.1556-4029.2010.01459.x. [DOI] [PubMed] [Google Scholar]
- Savitsky B, Givon A, Rozenfeld M, Radomislensky I, & Peleg K (2016). Traumatic brain injury: It is all about definition. Brain injury, 30(10), 1194–1200. doi: 10.1080/02699052.2016.1187290 [DOI] [PubMed] [Google Scholar]
- Silver JM, McAllister TW, & Arciniegas DB (2009). Depression and cognitive complaints following mild traumatic brain injury. American Journal of Psychiatry, 166, 653–661. [DOI] [PubMed] [Google Scholar]
- Smith DJ Jr, Mills T, & Taliaferro EH (2001). Frequency and relationship of reported symptomology in victims of intimate partner violence: the effect of multiple strangulation attacks. The Journal of emergency medicine, 21(3), 323–329. doi: 10.1016/S0736-4679(01)00402-4 [DOI] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, Chen J (2018). The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, … & McKee AC(2011). Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PM & R, 3(10), S460–S467. doi: 10.1016/j.pmrj.2011.08.008 [DOI] [PubMed] [Google Scholar]
- Strack G, Gwinn C, Riviello R, Julien SS, Burke M, & Aceves Y (2018, March). “Do You Need a Paramedic?” The Role of Emergency Medical Services in Non-Fatal Strangulation Cases. Retrieved from https://www.familyjusticecenter.org/resources/paramedics-chapter/ [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of family issues, 17(3), 283–316. doi: 10.1177/019251396017003001. [DOI] [Google Scholar]
- Stockman JK, Hayashi H, & Campbell JC (2015). Intimate partner violence and its health impact on ethnic minority women. Journal of Women’s Health, 24(1), 62–79. doi: 10.1089/jwh.2014.4879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. Ivany A, & Schminkey D (2016). Intimate partner violence and traumatic brain injury: State of the science and next steps. Family & Community Health, 39(2), 129–137. doi: 10.1097/FCH.0000000000000094. [DOI] [PubMed] [Google Scholar]
- Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, & Seedat S (2009). Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive psychiatry, 50(2), 121–127. doi: 10.1016/j.comppsych.2008.06.006 [DOI] [PubMed] [Google Scholar]
- Teasdale G, & Jennett B (1974). Assessment of coma and impaired consciousness: a practical scale. The Lancet, 304(7872), 81–84. doi: 10.1016/S0140-6736(74)91639-0 [DOI] [PubMed] [Google Scholar]
- Training Institute on Strangulation Prevention (2017). Gwinn: Strangulation a step toward spousal murder. Retrieved from: https://www.strangulationtraininginstitute.com/gwinn-strangulation-step-toward-spousal-murder/ [Google Scholar]
- Valera EM, & Berenbaum H (2003). Brain injury in battered women. Journal of consulting and clinical psychology, 71(4), 797. [DOI] [PubMed] [Google Scholar]
- Valera E & Kucyi A (2017). Brain injury in women experiencing intimate partner-violence: Neural mechanistic evidence of an “invisible” trauma. Brain Imaging and Behavior, 11, 1664–1677. doi: 10.1007/s11682-016-9643-1. [DOI] [PubMed] [Google Scholar]
- Woods SJ, Hall RJ, Campbell JC, & Angott DM (2008). Physical health and posttraumatic stress disorder symptoms in women experiencing intimate partner violence. Journal of Midwifery & Women’s Health, 53, 538–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilkens RR, Phillips MA, Kelly MC, Mukhtar SA, Semmens JB, & Smith DA (2016). Non-fatal strangulation in sexual assault: A study of clinical and assault characteristics highlighting the role of intimate partner violence. Journal of forensic and legal medicine, 43, 1–7. [DOI] [PubMed] [Google Scholar]