Abstract
Objectives
Identifying the issues and concerns that matter most to burns survivors can be challenging. For a number of reasons, but mainly relating to patient empowerment, some of the most pressing concerns patients may have during a clinical encounter may not naturally be the focal point of that encounter. The Patient Concerns Inventory (PCI) is a tried and tested concept initially developed in the field of head and neck cancer that empowers patients during a clinical encounter through provision of a list of prompts that allows patients to self-report concerns prior to consultation. The aim of this study was to develop a PCI for adult burns patients.
Design
Content for the PCI was generated from three sources: burns health-related quality of life tools, thematic analysis of one-to-one interviews with 12 adult burns patients and 17 multidisciplinary team (MDT) members. Content was refined using a Delphi consensus technique, with patients and staff members, using SurveyMonkey.
Setting
Within outpatient secondary care.
Participants
Twelve adult burns patients and MDT members from two regional burns centres.
Results
A total of 111 individual items were generated from the three sources. The Delphi process refined the total number of items to 58. The main emergent domains were physical and functional well-being (18 items), psychological, emotional and spiritual well-being (22 items), social care and social well-being (7 items) and treatment-related concerns (11 items).
Conclusions
The Adult Burns Patient Concerns Inventory is a 58-item, holistic prompt list, designed to be used in the outpatient clinic. It offers a new tool in burn care to improve communication between healthcare professionals and patients, empowering them to identify their most pressing concerns and hence deliver a more focused and targeted patient-centred clinical encounter.
Keywords: burns, patient concerns inventory, health-related quality of life/patient-centred care
Strengths and limitations of this study.
The Patient Concerns Inventory (PCI) offers a new tool in burn care to improve communication between healthcare professionals and patients.
The Adult Burns Patient Concerns Inventory has been developed in accordance with international standards on health-related quality of life tool development.
Content within the PCI may not capture concerns unique to patients from other cultures, age groups or those with other types of burns.
Further work is required to determine the efficacy of the tool in the clinical setting.
Introduction
Globally, burns are the fourth most common form of trauma after road traffic accidents, falls and interpersonal violence.1 In 2008, WHO estimated that 195 000 people died from fire-related injuries, a decrease of almost 40% in relation to 2004.1 2 The decline in mortality has been attributed to improved knowledge of the pathophysiological response to injury and progress in intensive care, nutrition, surgical techniques and infection control.3 Consequently, more patients are surviving major burn injuries and require long-term support and rehabilitation.
The need for a holistic approach to burn care is essential if the many issues that a patient may encounter such as physical symptoms, psychological issues and reduced physical function are to be fully addressed.4 5 In the time-restricted outpatient setting, identifying the issues and concerns that matter most to patients can be challenging. Furthermore, it is often difficult to identify patients that ‘suffer in silence’ and some concerns, for example, the impact of burn injuries on sexual relationships, may be potentially embarrassing or difficult for both the patient and healthcare professional to discuss unless there is some mechanism or prompt to facilitate this.6 7 The stress and anxiety associated with attending clinic appointments, often involving extensive journeys, may also cause patients to forget to raise important issues during the consultation.
An open, communicative relationship helps patients understand their health condition, improving satisfaction, improving health outcomes and reducing patient stress.8 9 Improvements in patient-professional communication have been most notable in oncology where the concept of Holistic Needs Assessment (HNA) has become an integral aspect of care.10 Rogers et al developed and piloted a Patient Concerns Inventory (PCI) to assess the needs of patient with head and neck cancer.11 The PCI, is a prompt list containing potential concerns, that patients may wish to discuss with their healthcare professional. It is completed prior to consultation, and enables the clinician to focus the discussion around the individual’s needs. The PCI has since been validated in rheumatology,12 neuro-oncology13 and breast cancer14 and is associated with greater patient satisfaction, and service efficiency.11 13 15 16
The aim of this study was to develop a PCI for adult burns patients.
Methods
The study comprised three distinct stages. First, content for the PCI was generated from three sources: burns-specific health-related quality of life (HRQoL) tools, one-to-one interviews with burns patients and focus groups with multidisciplinary care teams (MDT) from two regional burns centres. Following this stage, items were refined using a Delphi process. The final stage of PCI development was to group items into discrete domains.
The need for both patient and professional involvement in the development of patient-focused tools is extensively documented within the literature. It is argued that such an approach is essential to ensure the tool adequately reflects the needs of the target population17–19 and this approach was therefore adopted from the outset.
Content generation
HRQoL tools
A systematic search of MEDLINE, the Cochrane library, Embase and PsycInfo was undertaken in June 2017 to identify HRQoL tools psychometrically validated for an adult burn population (≥18). Grey literature was searched using Google Scholar and OpenGrey. The detailed search strategy is outlined in online supplementary appendix 1.
bmjopen-2019-032785supp001.pdf (126.9KB, pdf)
Relevant items were extracted from the HRQoL measures by JAGG and independently verified by SS.
One-to-one patient interviews
Participants were recruited from two regional burn centres in the UK: The Welsh Centre for Burns & Plastic Surgery, Swansea and The Mersey Burns Centre, Liverpool, using the following eligibility criteria: participants aged 18 years or above, with a burn injury and actively receiving treatment. Participants unable to speak English or unable to provide informed consent were excluded.
A purposive sampling strategy was used to select participants representative of the wider burns population based on: age (18–30, 31–50, 50–65, >65 years), gender, mechanism of burn (scald, flame, contact, electrical and chemical), severity of burn (0%–15% total body surface area (TBSA), >15% TBSA) and time following injury (<6 months since injury, 6 months−1 year, >1 year).
Eligible participants were identified by clinic staff and provided with participant information sheets describing the study. Those willing to participate contacted JAGG who arranged a suitable time and date for the interview. Written informed consent was provided by all participants prior to interviews, which were conducted in a confidential space in the burns centre using a semi-structured interview format. Participants were asked to describe concerns and issues encountered during the course of their recovery; the initial acute inpatient treatment (where applicable), outpatient treatment and their concerns for the future (online supplementary appendix 2).
All interviews were conducted by JAGG. JAGG is a specialist registrar in Burns & Plastic Surgery and is a former burns survivor. Interviews were digitally audio-recorded and transcribed verbatim (JAGG). Data were analysed using a six-step inductive thematic approach20 supported by NVivo V.12 software. Data collection and analysis were concurrent to enable determination of data saturation, where additional interviews did not yield new information.21 Concerns described by participants were assigned unique codes and those deemed irrelevant to the PCI were excluded. Where possible, the wording of the codes was used in the language patients described their concerns. The codes that remained were the initial list of patient concerns. Coding was performed by JAGG and verified by SS who have extensive knowledge in qualitative analysis.
Multidisciplinary team
Staff were recruited from two regional burn centres in the UK: The Welsh Centre for Burns & Plastic Surgery, Swansea and The Mersey Burns Centre, Liverpool. The Welsh Centre for Burns & Plastic Surgery is the regional adult burns centre for the South West of the UK, covering a population of 10 million. The Mersey Burns Centre is a regional burns centre for the North West of the UK, covering a population of 4.5 million. Both services contain a dedicated burns MDT providing all aspects of burn care.
Staff were eligible if they were a dedicated member of the burns MDT and had been working in burn care for a minimum of 1 year. Informed consent was obtained from all staff participants. Items harvested in stage (a) were reviewed by members of the MDT who then added additional items. Concerns devised from patients in stage (b) were not shared with the MDT to enable comparison between groups.
Content refinement
Incorporating every concern identified would have been extensive, placing a high burden on patients and staff in terms of completion time and analysis, therefore not feasible in the confines of an outpatient clinic.19 21 Content reduction was therefore necessary at this stage to remove similar items and to achieve consensus on the final item list. Development of other versions of the PCI have confirmed that a checklist of 50–100 items is feasible in the outpatient setting.11–13 An item bank was compiled from the three aforementioned sources: HRQoL tools, patient interviews and the MDT. An online Delphi process using SurveyMonkey software22 was used to reduce and refine the item bank. To maintain stakeholder validity, both healthcare professionals and patients who participated in content generation were invited to take part. Participants were asked to select items for inclusion in the final PCI and to add additional items considered missing. Items with <60% selection rate were excluded from the final PCI. The survey was repeated and items with a 60% agreement were retained in the final list of concerns. This level of consensus has been shown to be effective in previous versions of the PCI.11–13
A secondary outcome of the Delphi study was to gain feedback on the wording of individual items on the PCI. Significant overlap was generated from the three sources of content development. All items generated, included those that had similar definitions (eg, energy and fatigue) were included in the Delphi. Participants were asked to review the wording of the items to ensure that the list was deemed comprehensive by the intended audience and to select the term they considered most appropriate.
Item domains
The purpose of this stage was to group similar aspects of health together to help patients focus on one topic at a time when completing the PCI. The final list of concerns were allocated to one of the four following domains:
Physical and functional well-being.
Psychological, spiritual and emotional well-being.
Social care and social well-being.
Treatment-related concerns.
These four domains feature on other versions of the PCI and are consistent with the domains of other general and disease-specific HRQoL measures.23 They were therefore deemed appropriate for the adult burns PCI. A further Delphi process, using SurveyMonkey, was used to allocate items to domains based on 60% consensus from MDT staff.
Patient and public involvement
A patient and public involvement session was hosted by the Katie Piper Foundation. This informal focus group highlighted the disparity between issues considered important by health professionals managing care and patients receiving care. Patient feedback was used to design the study and aid with patient recruitment.
Results
A diagram displaying an overview of the three stages of tool development alongside the number of concerns generated is shown in figure 1.
Figure 1.
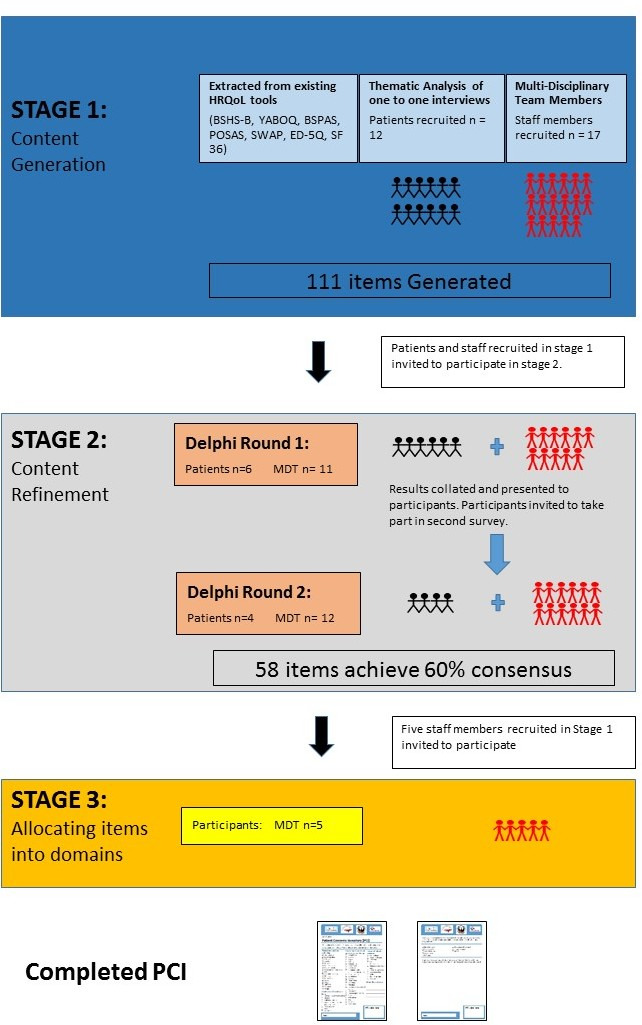
An overview of study design. BSPSAS, Burn-Specific Pain Anxiety Scale; BSHS-B, Burn-Specific Health Scale-Brief; EQ-5D, EuroQol-5D; HRQoL, health-related quality of life; PCI, Patient Concerns Inventory; MDT, multidisciplinary team; POSAS, Patient Observer Scar Assessment Scale; SF 36, 36-item Short-Form Health Survey; SWAP, Satisfaction With Appearance Scale; YABOQ, Young Adult Burn Outcome Questionnaire.
Content generation
HRQoL tools
The search identified seven HRQoL tools. Five were disease specific; the Burn-Specific Health Scale-Brief,24 the Young Adult Burn Outcome Questionnaire,25 Burn Specific Pain Anxiety Scale,26 the Patient Observer Scar Assessment Scale,27 the Satisfaction With Appearance Scale.28 Two were generic: EuroQol-5D29and SF 36.30 Forty-nine items were harvested from the seven measures (online supplementary appendix 3).
One-to-one interviews
Twelve face-to-face interviews lasting for average of 46 min (20–85 min) were conducted between August and September 2018. Saturation was determined as interviews number 11 and 12 did not lead to the emergence of any new codes. This was independently assessed by SS.
Population demographics are shown in table 1.
Table 1.
Patient demographics
| Patients, N | 12 |
| Age (years), mean (SD), range | 47.9 (12.3), 28–60 |
| Male, N | 7 |
| Female, N | 5 |
| White British | 12 |
| Years since injury, mean (SD), range | 13.3 (23.1), 0.1–53 |
| Percentage TBSA, mean (SD), range | 24 (29.4), 1–80 |
| Aetiology | |
| Contact burn, N | 2 |
| Chemical burn, N | 1 |
| Electrical burn, N | 1 |
| Flame burn, N | 5 |
| Flash burn, N | 2 |
| Scald burn, N | 1 |
| Contractures, N | 4 |
| Presence of scarring, N | 9 |
| Type of scarring | |
| Pigmented, N | 5 |
| Hypertrophic, N | 6 |
| Location of scarring | |
| Head and neck, N | 5 |
| Upper limb, N | 7 |
| Lower limb, N | 4 |
| Torso, N | 6 |
| Surgical intervention, N | 7 |
N, Number; SD, Standard Deviation; TBSA, total body surface area.
A total of 97 individual codes were generated from the 12 interviews. Following removal of 40 duplicate and similar items, 57 concerns remained. Where possible, the wording of the concerns and issues outlined in the Items Generated section reflected the language used by the patients interviewed.
Items generated
Physical concerns relating to wounds and scars
All 12 participants expressed concerns about potential scarring, although only 9 had developed scars. When specifically probed about the physical appearance of scars, patients did not focus on specific features, such as the colour or texture; they were more concerned with overall appearance and the impact of scarring on other aspects of physical health and well-being, such as mobility. The following concerns were identified in relation to wounds and scars.
Pain was an overriding concern for all participants, at multiple time points of their recovery.
I don’t remember what normal felt like…it sounds really stupid to say but a year has gone and I don’t know what it’s like to not be in pain. (Participant 8)
Nerve (neuropathic) pain was described separately by three patients and therefore considered a separate concern. The wording of ‘nerve pain’ was selected as this was the common language that patients described their symptoms.
Mobility was a concern raised by eight participants, such as an inability to perform routine day-to-day activities, arising from movement restriction, pain or skin sensitivity.
The initial part from laying down to sitting up to getting off the bed was really hard across the back (Patient had burn wounds to the back). It was so painful, it was really hard. (Participant 11)
Hand function was a concern expressed by all six participants that had injuries to the hand and upper limb. For one builder, this issue severely limited his ability to work:
I still can’t grip with this one, (Lifts dominant left hand) that’s my grip (attempts to grip the investigators pen with limited success). But it’s like stupid things, like I can’t hold a nail. I hold a nail and me arm shakes. I can’t hold a screw. (Participant 8)
Skin strength was a concern for five participants. For one participant, a self-employed mechanic, it had a substantial impact on his work:
I’ve noticed a few times now that when I cut my hands on something, when you’re working, it opens the skin up quite easily. Whereas before it may have caused a scratch, now it’s a big problem. (Participant 2)
Scar tightness was a concern for all nine participants that had scarring. For six patients, this was related to mobility limitation and captured above, but for three participants, scar tightness was associated with discomfort rather mobility issues.
The groin is quite tight. It’s like I’ve got a pair of knickers on that are four sizes too small. (Participant 7)
Scar tightness was also a concern for patients with abdominal scarring during pregnancy.
Weight gain was a concern for four patients, arising from reduced mobility and excessive calorie intake. The excess weight increased participant’s dissatisfaction with their appearance and increased scar tightness resulting in additional discomfort.
Skin sensitivity was a concern for most of the interviewees, including itching during wound healing (four participants), scar sensitivity (six participants) and heat sensitivity (five participants).
When I got the slightest touch, I would just have to move. (Participant 6)
Physical concerns not related to scars
Concerns about other aspects of physical function included sleep deprivation (seven participants), loss of appetite (four participants) and fatigue during the initial recovery stage (six participants) and lack of energy (four participants).
It’s a different tired to when you’re not getting sleep. (Participant 2)
Body image
Physical appearance and body image was an important concern for all participants.
I still want nice normal skin. I want to look in a mirror and not see this burned flesh that stays with me all the time. (Participant 7)
As a direct consequence of scarring, nine participants described anxiety associated with acceptance by society. Five participants described a lack of confidence and low self-esteem following the injury.
I just felt like nothing. I’m now very happy with my life but it (the injury) made me feel ugly and worthless. (Participant 7)
Comments from others were of great concern throughout the recovery process for all twelve participants. Three patients reported bullying and another described discrimination in the workplace owing to scarring.
If I were to walk into a pub with you I would be the topic of conversation because I‘m different. I see that and I feel that. (Participant 5)
Coping strategies
Coping with the psychological sequelae of the injury was a concern for seven of the participants. Coping mechanisms such as increased alcohol consumption and smoking were concerns for two participants and avoidance of reminders were described by seven participants. For some, this impacted on daily functioning.
The stove is still a no go for me. I’m back in the kitchen doing butties and things like that but putting things on the stove I’m still a bit shaky. (Participant 6)
Fear for the future and anger were other negative coping strategies described by participants.
I get angry now when I talk about it because I used to get a bit sad and a bit feeling down but I can’t now, I just get…. It’s like a rage that comes over me. No, I can’t work it out. (Participant 4)
Mental health
Anxiety was encountered by five participants, causing considerable repercussions.
I’m suffering a lot from panic attacks, anxiety, really, really badly. There’s mornings now where I have to really argue with myself to actually wake up and go to work. (Participant 8)
Depression was experienced by five participants and low mood by eight.
It would change my mood. It would bring me down and I’m not a person that’s down. (Participant 2)
Participants described low mood to avoid the perceived stigma associated with mental health conditions. One participant described the impact of appropriate terminology:
If you say that people need help with their well-being and their full recovery, which means physical and mental in every sense, emotional and so on, that is better than implying that people must have mental health problems because they’ve been through a trauma. That would draw in a wider set of people who (wanted or needed) some kind of mental health support. (Participant 9)
Dependence on others and guilt were described by seven and six patients, respectively. Guilt was experienced mostly by patients who, witnessed other survivors with more severe injuries.
I felt ashamed and embarrassed and horrible and dirty and guilty because I’m alive really. (Participant 7)
Post-traumatic stress disorder symptomology
Seven participants suffered flashbacks of the injury event.
I would have the odd flashback. I try not to think about it … as they were really bad. (Participant 2)
Six participants described broad concerns and issues relating to their psychological and emotional well-being that could not be defined by any of the above themes. The term psychological trauma was used as the code. One patient who was assaulted, developed depression and post-traumatic stress disorder (PTSD):
I’ve had to stop thinking about it, because the more I was trying to think about why they did it, I was getting nowhere, … but when I look at my arm sometimes, (the scar) it just triggers it again. (Participant 8)
Social well-being
All 12 participants were concerned about the impact of the injury on their intimate, personal and social relationships. Four participants raised specific concerns about intimacy.
Intimacy is awkward, you know… we still have a loving relationship but it’s not what it was before the accident. It was quite hard to come to terms with. (Participant 4)
All participants were concerned about the impact of their injury on family members. Concerns related to the psychological trauma experienced by members of the family who witnessed the trauma:
My son was screaming, I mean he must have seen me on fire. (Participant 1)
Both physical and psychological aspects of the injury prevented six participants from continuing their regular hobbies and interests. Returning to work and education following the injury were concerns raised by 10 participants. The financial implications of the injury were far reaching and perceived as an issue for six patients. For one participant, it was perceived as the most difficult aspect of the injury.
Financial that’s been…. If I’m honest with you, I’ve found that worse than the pain. (Participant 8)
Treatment-related concerns
All 12 participants expressed concerns about good communication with the clinical team in relation to their treatment. Communication was perceived as poor when patients did not feel that their needs were identified or addressed, leading to significant distress.
Some went ‘don’t you worry we’re doing what we can’ kind of thing. So what are you doing? What is the plan? I kind of got the impression that had we not pushed, they wouldn’t have explained. (Participant 9)
On the other hand, excellent communication inspired greater confidence in the competence of healthcare professionals. In instances where treatment options were not available for particular issues, patients appreciated honesty.
As an adult now, he’s helped me understand. It’s like he can do little bits to tidy me up. I think that I don’t want to accept it. He can’t get rid of it all but he can make me better. So I feel valued as a person not like the other consultants. It can do a lot of damage. It really can. (Participant 7)
In the early stages of recovery, patients had numerous concerns relating to wound care and infection.
Well with the wound healing, what it was was the infection. Because of the smell I was constantly worrying that the work they (healthcare professionals) had done was wasted and that I would be back (in hospital) getting something else done. (Participant 6)
Once wounds had healed, the majority of concerns related to scar treatment options, notably pressure garments, splints, reconstruction and camouflage.
Four participants raised numerous concerns about the primary care (general practitioner) team’s knowledge of burns injuries.
I felt quite vulnerable because they didn’t have the (specialist) knowledge. I don’t think there is a lot of knowledge (about) burns, I really don’t. (Participant 12)
An aspect of care that four participants felt was missing was support for family members, especially parents of young children. For one participant, who was assaulted, this was a significant concern.
There’s been no support offered for my kids. Even if it’s just to talk to somebody… (Participant 8)
Multidisciplinary team
Data collection was performed between September and October 2018. Seventeen members of the clinical teams from the two centres contributed to item generation, which identified 54 potential concerns. Composition of the MDT is shown in table 2, with the list of concerns displayed in online supplementary appendix 4. The wording of items were devised by each staff member.
Table 2.
Multidisciplinary team members
| Professional | Number |
| Consultant Burns Surgeon | 3 |
| Consultant Anaesthetist | 2 |
| Consultant Clinical Psychologist | 3 |
| Physiotherapist | 3 |
| Occupational Therapist | 2 |
| Staff Nurse | 4 |
Content generation: variation between sources
While specific wording of concerns varied between the literature, patients and MDT sources, there was significant overlap and consistency in the content of the four domains (online supplementary appendix 5). There were also differences between the sources, with each contributing unique concerns, reinforcing the validity and importance of capturing multiple professional and patient perspectives during content generation.
For the physical and functional well-being domain, the concerns identified were largely consistent across all three sources. However, there were a few exceptions. Skin strength and dental health were concerns unique to patients. Dry skin, contractures and specific scar characteristics (shape, size and texture) were identified in the HRQoL tools and by members of the MDT, but not during the patient interviews.
For the psychological, emotional and spiritual well-being domain, acceptance by society was a concern only raised by patients. Hypervigilance/increased awareness of danger was not identified in the HRQoL tools. Change of personality was a concern identified by a member of the MDT, but this concern was not raised by patients.
For the social care and social well-being domain, concerns about driving were only raised by patients whereas religion, and responses by friends and family were identified by the MDT and HRQoL tools.
For the treatment-related concerns domain, medication and the management of infection were concerns raised only by patients.
Content refinement
After removal of duplicate items, a total of 111 individual concerns, generated from the literature, patient interviews and the MDT were incorporated in the Delphi survey. Nine of the 12 (75%) patients that participated in the one-to-one interviews participated in the survey. Seventeen members of the MDT’s at the two sites participated in the Delphi survey.
Fifty-eight items achieved a 60% consensus agreement following the two rounds of the Delphi survey and were retained for the inventory.
Grouping items in domains
Five staff members independently allocated the final 58 concerns into one of the following four domains, which were previously identified from other versions of the PCI: physical and functional well-being (18 concerns); psychological, spiritual and emotional well-being (22 concerns); social care and social well-being (7 concerns); treatment-related concerns (11 concerns). Categorisation of the final 58 concerns is shown in the Adult Burns Patients Concerns Inventory (online supplemental appendix 6).
bmjopen-2019-032785supp002.pptx (50.8KB, pptx)
Discussion
The Adult Burns Patient Concerns Inventory is a 58-item prompt list that empowers patients to raise issues that are of greatest concern to them, which facilitates care providers to focus on these patient priorities. This study has captured the most important concerns experienced during recovery as perceived by patients and healthcare professionals, providing a tool that has shown to improve communication between patients and healthcare professionals in other healthcare settings, and has similar potential in the context of burn care.
In addition to the development of a new tool, this study has identified a number of other key findings. There was substantial overlap between the concerns raised by staff and patients. However, there were also notable differences. Staff raised issues and selected items that were more clinically driven, whereas patients raised and selected issues that had an influence on their daily lives. Each source of content provided unique issues. Skin strength, infection, medication, dental health, acceptance and driving were concerns unique to the patient participants. On the other hand, scar characteristics, religion, personality, dry skin, contractures, friend’s response and family’s response were unique to HRQoL tools and the MDT. The importance of capturing concerns from both sides of the clinical consultation are demonstrated in the final PCI; five of these concerns appear on the PCI. This study has demonstrated that burns patients experience a wide range of concerns relating to their physical and functional well-being. Concerns raised by the majority of patients such as pain, itch, sleep and increased sensitivity are well described in the literature.4 31–36 Concerns that were less prevalent however, are not well described. Dental health, for instance, a concern for two individuals, is absent in the burns literature.
All patients raised concerns about scarring that impacted on all four domains of the PCI. The physical appearance of scars, such as colour and texture, were considered important during development of the POSAS HRQoL tool27 and therefore included during content generation, but patients in our study were more concerned about the overall appearance and functional limitations associated with scarring, and scar features were not retained during the Delphi exercise. This is consistent with findings from the PEGASUS qualitative study where patients also focused on the general appearance of scars.37 Our findings may indicate that the detailed characteristics of scars may be important when assessing the efficacy of clinical interventions, but are not of specific concern to patients. Scar characteristics were however deemed important in a study, performed by Kool et al. 38 The mixed method study aimed to determine a hierarchical structure of HRQoL domains identified from a cohort of adult burns patients. The differences in these findings could be attributed to a different study population or the sample size in this present study. The discrepancies highlight the heterogeneity of concerns within the adult burns population and the need to hear each patient’s voice.
The psychological, emotional and spiritual well-being domain contains more items than any other in the PCI. Many patients described these concerns as having greater and longer lasting impact than any other aspect of their injury and the central theme related to body image. Persistent psychological symptoms, such as flashbacks and fear avoidance, relating to the injury event were also prevalent. Patients in this study were not assessed for PTSD but their psychological concerns may align with the symptomatic profile of PTSD, which emphasises cognitive features such as the negative appraisal of traumatic events and its central role in the maintenance of psychological distress.39 40 Many patients described their scarring as a constant reminder of their injury, which supports the growing evidence that appearance distress and PTSD symptomology are interlinked in patients with visible disfigurement.41 Psychological interventions aimed at addressing PTSD symptoms therefore need to simultaneously identify and address concerns relating to body image.
Stigma associated with mental health disorders is associated with poor self-esteem, self-confidence and reluctance to seek care.42 43 Patients in our study were also concerned about the negative connotations and potential stigmatisation associated with mental health support. Further work is required to identify patient friendly terminology for psychological support and to address the stigma associated with mental health disorders in the burns population.
Concerns identified for the domain of social care and social well-being were more consistent across the three sources used for content generation compared with the other PCI domains. The importance of social support for improving outcomes for burn survivors is well established,44 45 but less is known about the impact on families. All patients were concerned about significant psychological distress observed in spouses, family and friends, following the burn trauma, many of whom had witnessed the injury. This is consistent with evidence from one study that reported clinical anxiety, depression or PTSD-related symptoms in 77% of spouses and 56% of close relatives immediately following injury.44 However, the study did not include long-term follow-up of relatives, therefore the long-term trajectory of psychological distress in relatives and its relationship to the long-term psychological state of the patient remain unclear. Psychological support for family members was the only aspect of care that patients felt was missing. Further research is needed on the prevalence of mental health conditions in family members and its impact on survivor recovery. Treatment-related concerns tended to focus on burden, such as the number of appointments, number of operations, the number of prescribed medicines and their side effects, the impact of treatment on the family (such as childcare), time off work and the financial cost of attending appointments. The majority of patients accepted the necessity of treatment for their recovery. However, patients with extensive injuries were concerned about the impact of treatment in delaying reintegration into society. This is consistent with the significant impact of treatment burden reported in a recent qualitative study,37 but further research is required to explore this in further detail.
There is significant overlap with the findings of this study and those reported by Kool et al indicating the validity of the findings.38 The study identified two key distinctions in HRQoL, resilience and vulnerability. Vulnerability included five domains: psychological, economic, social, physical and intimate/sexual. Resilience incorporated positive coping and social sharing.
Similar to our study, functional limitations and issues with scarring were the predominant aspects of the physical domain. Likewise, negative emotions, body perception and trauma-related symptoms, cognitive problems were central to the psychological domain. Social aspects such as intimacy, finance and work were also predominant. Unique issues such as medication, their side effects and aspects relating to treatment burden were also considered important by participants. As described above, discrepancies between the two studies were observed with the physical characteristics with scarring, which indicate the importance of assessing the needs of patients on an individual basis.
The greatest potential limitation of this study, and similar HNA and HRQoL tools, is representativeness of the sampled patient population.19 While the purposive sampling strategy aimed to capture the underlying population, it did not cover the full demographic or clinical spectrum. Notably, all of the participants were white British, non-English speaking patients were excluded and the age range did not include younger (under 28) and older (over 60) patients. In addition, less common injuries such as frostbite were not included in the injury profile. It is therefore possible that the PCI does not capture concerns unique to patients from other cultures, age groups or those with other types of burns. Once feasibility and acceptability of the Adult Burn Patient Concerns Inventory has been established, further validation work will help to establish its relevance for other populations not included in this study—and perhaps a version ‘two-point-zero’ in years hence along similar lines to the progression of other patient-centric tools including POSAS.27
A further limitation of the Adult Burn Patient Concerns Inventory is the use of single words (eg, itch) or short phrases (eg, loss of functioning). While this facilitates inclusion of a broad range of concerns without overburdening patients, the selected terms may not fully encapsulate the specifics of the issue that the patient wishes to talk about. However, the addition of a free text option allows patients to raise additional concerns and this information could be used to further refine the content.
The next stage of validation for the Adult Burn Patient Concerns Inventory is to determine the feasibility and acceptability of the tool in a clinical setting and to optimise the mode of administration, for example, paper and pencil, portable devices such as smartphones and internet-based platforms.11 46 Once feasibility has been established, a comparative study is required to determine whether the PCI improves patient/consultant communication and clinical outcomes compared with standard practice.
Conclusions
We have developed the Adult Patient Concerns Inventory for Burns (PCI-B). Through this process, we believe burns survivors will be empowered to guide clinicians towards their most pressing needs, and to better navigate the numerous potential problems they encounter. The PCI-B as published in this paper can be freely used and re-branded so long as the content is not altered and the acknowledgements are retained.
Supplementary Material
Acknowledgments
The authors would like to thank all patients and staff from the Mersey Regional Burns Centre, Whiston Hospital and subsequently The Welsh Centre for Burns and Plastic Surgery, Morriston Hospital for their participation in the study. The authors would like to thank Miss Bethan Hughes, RuthAnn Fanstone and Ezinna Rospigliosi of the Katie Piper Foundation for their invaluable input into the early stages of the PCI development. The authors would also like to thank the Katie Piper Foundation for part-funding the study.
Footnotes
Correction notice: This article has been corrected since it was published. Supplementary file has been updated.
Contributors: JAGG: designed the study, conducted and analysed the literature review, patient interviews and the Delphi process. JAGG also wrote the early draft of the manuscript. JY: contributed relevant clinical evidence (Burns Surgery) and assisted with patient recruitment. LB: contributed relevant clinical evidence (Burns Nursing) and assisted with patient recruitment. JE: contributed relevant clinical evidence (Burns Occupational Therapy) and assisted with patient recruitment. SS: assisted JAGG with study design, independently conducted data analysis and assisted with supervised manuscript preparation. SNR: conceived the initial PCI and provided extensive support for study design. KS: conceived the idea of a Burns-PCI and presented the idea, encouraged JAGG to investigate the presented idea, applied for and acquired funding for this research and contributed relevant clinical evidence (Burns Surgery). The majority of patients involved in the study were under the care of KS, who afforded access to and assisted with patient recruitment, supervised manuscript preparation and editing, responses to peer-review comments and final proof-reading of the manuscript. All authors discussed the results, provided a critical appraisal and contributed to the final manuscript. All authors discussed the results, provided a critical appraisal and contributed to the final manuscript.
Funding: This work was supported by The Katie Piper Foundation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Due to the sensitive nature of the study and to prevent the risk of patient identification, data from the study will not be made available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the Health Research Authority North West—Greater Manchester Central Research Ethics Committee 17/NW/0297 IRAS ID 214597 in May 2017 prior to the commencement of the study.
References
- 1.World Health Organisation . Global burden of disease. Switzerland: World Health Organization Press, 2004: 1–160. [Google Scholar]
- 2.Who | burns. World Health Organization; 2017. [Google Scholar]
- 3.Gibson JAG, Spencer S, Rogers SN, et al. Formulating a patient concerns inventory specific to adult burns patients: learning from the PCI concept in other specialties. Scars Burn Heal 2018;4. 10.1177/2059513118763382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stavrou D, Weissman O, Tessone A, et al. Health related quality of life in burn patients--a review of the literature. Burns 2014;40:788–96. 10.1016/j.burns.2013.11.014 [DOI] [PubMed] [Google Scholar]
- 5.Van Loey NEE, Van Son MJM. Psychopathology and psychological problems in patients with burn scars: epidemiology and management. Am J Clin Dermatol 2003;4:245–72. 10.2165/00128071-200304040-00004 [DOI] [PubMed] [Google Scholar]
- 6.Connell KM, Phillips M, Coates R, et al. Sexuality, body image and relationships following burns: analysis of BSHS-B outcome measures. Burns 2014;40:1329–37. 10.1016/j.burns.2014.01.006 [DOI] [PubMed] [Google Scholar]
- 7.Piccolo MS, Gragnani A, Daher RP, et al. Burn sexuality questionnaire: Brazilian translation, validation and cultural adaptation. Burns 2013;39:942–9. 10.1016/j.burns.2012.10.012 [DOI] [PubMed] [Google Scholar]
- 8.Greenfield S, Kaplan SH, Ware JE, et al. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med 1988;3:448–57. 10.1007/bf02595921 [DOI] [PubMed] [Google Scholar]
- 9.Griffin SJ, Kinmonth A-L, Veltman MWM, et al. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med 2004;2:595–608. 10.1370/afm.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coulter A, Collins A. Making shared decision making a reality: no decision about me, without me. London: The King's Fund, 2011. [Google Scholar]
- 11.Rogers SN, El-Sheikha J, Lowe D. The development of a patients concerns inventory (PCI) to help reveal patients concerns in the head and neck clinic. Oral Oncol 2009;45:555–61. 10.1016/j.oraloncology.2008.09.004 [DOI] [PubMed] [Google Scholar]
- 12.Ahmed A, Rogers S, Bruce H, et al. THU0332 Development of a Rheumatology-Specific Patient Concerns Inventory (PCI) and its Use in the Rheumatology Outpatient Clinic Setting. Ann Rheum Dis 2015;74:315.3–6. 10.1136/annrheumdis-2015-eular.5947 [DOI] [PubMed] [Google Scholar]
- 13.Rooney AG, Netten A, McNamara S, et al. Assessment of a brain-tumour-specific patient concerns inventory in the neuro-oncology clinic. Support Care Cancer 2014;22:1059–69. 10.1007/s00520-013-2058-2 [DOI] [PubMed] [Google Scholar]
- 14.Kanatas A, Lowe D, Velikova G, et al. Issues patients would like to discuss at their review consultation in breast cancer clinics--a cross-sectional survey. Tumori 2014;100:568–79. 10.1177/1660.18184 [DOI] [PubMed] [Google Scholar]
- 15.Ahmed AE, Lowe D, Kirton JA, et al. Development of a Rheumatology-specific patient concerns inventory and its use in the rheumatology outpatient clinic setting. J Rheumatol 2016;43:779–87. 10.3899/jrheum.150068 [DOI] [PubMed] [Google Scholar]
- 16.Ghazali N, Roe B, Lowe D, et al. Patients concerns inventory highlights perceived needs and concerns in head and neck cancer survivors and its impact on health-related quality of life. Br J Oral Maxillofac Surg 2015;53:371–9. 10.1016/j.bjoms.2015.01.022 [DOI] [PubMed] [Google Scholar]
- 17.Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res 2002;11:193–205. 10.1023/a:1015291021312 [DOI] [PubMed] [Google Scholar]
- 18.Cano SJ, Browne JP, Lamping DL. Patient-Based measures of outcome in plastic surgery: current approaches and future directions. Br J Plast Surg 2004;57:1–11. 10.1016/j.bjps.2003.08.008 [DOI] [PubMed] [Google Scholar]
- 19.Cano SJ, Hobart JC. The problem with health measurement. Patient Prefer Adherence 2011;5:279–90. 10.2147/PPA.S14399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 21.Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res 2009;18:1263–78. 10.1007/s11136-009-9540-9 [DOI] [PubMed] [Google Scholar]
- 22.SurveyMonkey . SurveyMonkey n.d. Available: www.surveymonkey.com [Accessed 19 Sep 2016].
- 23.Griffiths C, Guest E, White P, et al. A systematic review of patient-reported outcome measures used in adult burn research. J Burn Care Res 2017;38:e521–45. 10.1097/BCR.0000000000000474 [DOI] [PubMed] [Google Scholar]
- 24.Kildal M, Andersson G, Fugl-Meyer AR, et al. Development of a brief version of the burn specific health scale (BSHS-B). J Trauma 2001;51:740–6. 10.1097/00005373-200110000-00020 [DOI] [PubMed] [Google Scholar]
- 25.Ryan CM, Schneider JC, Kazis LE, et al. Benchmarks for multidimensional recovery after burn injury in young adults: the development, validation, and testing of the American burn Association/Shriners hospitals for children young adult burn outcome questionnaire. J Burn Care Res 2013;34:e121–42. 10.1097/BCR.0b013e31827e7ecf [DOI] [PubMed] [Google Scholar]
- 26.Taal LA, Faber AW. The burn specific pain anxiety scale: introduction of a reliable and valid measure. Burns 1997;23:147–50. 10.1016/S0305-4179(96)00117-9 [DOI] [PubMed] [Google Scholar]
- 27.Draaijers LJ, Tempelman FRH, Botman YAM, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg 2004;113:1960–5. 10.1097/01.PRS.0000122207.28773.56 [DOI] [PubMed] [Google Scholar]
- 28.Lawrence JW, Heinberg LJ, Roca R, et al. Development and validation of the satisfaction with appearance scale: assessing body image among burn-injured patients. Psychol Assess 1998;10:64–70. 10.1037/1040-3590.10.1.64 [DOI] [Google Scholar]
- 29.EuroQol Group . EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208. 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 30.Ware JE, Sherbourne CD. The mos 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 31.Anzarut A, Chen M, Shankowsky H, et al. Quality-Of-Life and outcome predictors following massive burn injury. Plast Reconstr Surg 2005;116:791–7. 10.1097/01.prs.0000176257.22583.4b [DOI] [PubMed] [Google Scholar]
- 32.Pan R, Egberts MR, Nascimento LC, et al. Health-Related Quality of Life in adolescent survivors of burns: Agreement on self-reported and mothers’ and fathers’ perspectives. Burns 2015;41:1107–13. 10.1016/j.burns.2014.12.011 [DOI] [PubMed] [Google Scholar]
- 33.Laarhoven A, Ulrich D, Wilder-Smith O, et al. Psychophysiological processing of itch in patients with chronic Post-burn itch: an exploratory study. Acta Derm Venereol 2016;96:613–8. 10.2340/00015555-2323 [DOI] [PubMed] [Google Scholar]
- 34.Van Loey NEE, Bremer M, Faber AW, et al. Itching following burns: epidemiology and predictors. Br J Dermatol 2008;158:95–100. 10.1111/j.1365-2133.2007.08278.x [DOI] [PubMed] [Google Scholar]
- 35.Van Loey NE, Faber AW, Taal LA. Do burn patients need burn specific multidisciplinary outpatient aftercare: research results. Burns 2001;27:103–10. 10.1016/S0305-4179(00)00099-1 [DOI] [PubMed] [Google Scholar]
- 36.van Loey NE, van Beeck EF, Faber BW, et al. Health-Related quality of life after burns: a prospective multicenter cohort study with 18 months follow-up. J Trauma Acute Care Surg 2012;72:513–20. 10.1097/ta.0b013e3182199072 [DOI] [PubMed] [Google Scholar]
- 37.Jones LL, Calvert M, Moiemen N, et al. Outcomes important to burns patients during scar management and how they compare to the concepts captured in burn-specific patient reported outcome measures. Burns 2017;43:1682–92. 10.1016/j.burns.2017.09.004 [DOI] [PubMed] [Google Scholar]
- 38.Kool MB, Geenen R, Egberts MR, et al. Patients’ perspectives on quality of life after burn. Burns 2017;43:747–56. 10.1016/j.burns.2016.11.016 [DOI] [PubMed] [Google Scholar]
- 39.Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clin Psychol Rev 2003;23:339–76. 10.1016/S0272-7358(03)00033-3 [DOI] [PubMed] [Google Scholar]
- 40.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther 2000;38:319–45. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- 41.Macleod R, Shepherd L, Thompson AR. Posttraumatic stress symptomatology and appearance distress following burn injury: an interpretative phenomenological analysis. Health Psychol 2016;35:1197–204. 10.1037/hea0000391 [DOI] [PubMed] [Google Scholar]
- 42.Sartorius N. Stigma and mental health. The Lancet 2007;370:810–1. 10.1016/S0140-6736(07)61245-8 [DOI] [PubMed] [Google Scholar]
- 43.Corrigan P. How stigma interferes with mental health care. Am Psychol 2004;59:614–25. 10.1037/0003-066X.59.7.614 [DOI] [PubMed] [Google Scholar]
- 44.Bond S, Gourlay C, Desjardins A, et al. Anxiety, depression and PTSD-related symptoms in spouses and close relatives of burn survivors: when the supporter needs to be supported. Burns 2017;43:592–601. 10.1016/j.burns.2016.09.025 [DOI] [PubMed] [Google Scholar]
- 45.Badger K, Royse D. Helping others heal: burn survivors and peer support. Soc Work Health Care 2010;49:1–18. 10.1080/00981380903157963 [DOI] [PubMed] [Google Scholar]
- 46.Rogers SN, Lowe D. An evaluation of the head and neck cancer patient concerns inventory across the Merseyside and Cheshire network. Br J Oral Maxillofac Surg 2014;52:615–23. 10.1016/j.bjoms.2014.04.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-032785supp001.pdf (126.9KB, pdf)
bmjopen-2019-032785supp002.pptx (50.8KB, pptx)
Data Availability Statement
Due to the sensitive nature of the study and to prevent the risk of patient identification, data from the study will not be made available.


