Abstract
Community Health Advisors (CHAs) contribute to health promotion program effectiveness, but their role in faith-based programs is understudied, and little is known about their role performance or satisfaction. In a dissemination and implementation study, 19 CHAs were trained to provide healthy eating (HE) and physical activity (PA) program training to church committees. Of these, 17 CHAs trained 347 attendees from 115 churches. Thirteen CHAs remained for the 12-month period and provided telephone-based technical assistance (TA) to churches. To evaluate their experiences and satisfaction, CHAs completed questionnaires at baseline and 12 months. Staff observers and church committee members evaluated CHAs’ effectiveness as trainers. There were no significant changes in the CHAs’ own body mass index, physical activity, fruit and vegetable intake, or self-rated health but significant increases in their perceived knowledge of PA (p=0.01) and HE (p=0.02). CHAs reported high agreement regarding the quality of their training for the role and moderate volunteer satisfaction on average but thought that the time required of them was somewhat more than expected, though they were interested in volunteering for a future, similar role. Church committee members agreed with CHAs’ effectiveness as trainers and the helpfulness of the TA calls. Staff observers rated CHAs’ as having covered 87.8% of church training content and agreed that, on average, the CHAs were effective trainers. Assessing CHAs’ availability, clear communication about the time requirements, and over-recruitment to offset attrition and decrease the workload may be needed to improve retention and support satisfaction.
Keywords: Community health advisors, faith-based, dissemination and implementation, physical activity, healthy eating
Background
Dissemination and implementation (D&I) research helps to bridge the gap between research findings and widespread uptake of evidence-based programs in the community [1]. A D&I study was conducted of an evidence-based healthy eating (HE) and physical activity (PA) program originally tested in African American churches [2,3]. The goal was to discover factors that affect how the evidence-based program was adopted and scaled up for broad dissemination. The faith-based program focuses on preparing and supporting church committees to create a church environment to support congregants’ HE and PA and to tailor program components to meet the congregation’s needs.
During the original effectiveness study [2,3], university-based staff persons provided training and technical assistance (TA) to support church committee members’ program implementation; however, during Phase 1 of the D&I study, a group-randomized trial conducted with multiple denominations in a single, SC county [4], the researchers trained Community Health Advisors (CHAs) to provide the church training and TA. During Phase 2, the focus for this paper, a statewide, quasi-experimental study was conducted in partnership with one faith denomination, which implemented the CHA-delivered training and TA on a larger scale.
Community Health Advisors have played a central role in health promotion and disease prevention for decades [5], and evidence supports the feasibility of CHA involvement and their contributions to positive program outcomes [6–12]. From rigorous reviews, the Community Preventive Services Task Force found evidence of program effectiveness and cost-effectiveness for engaging community health workers (including CHAs) in cardiovascular and diabetes prevention and control [13,14]. Nevertheless, little description exists in the literature regarding the CHAs’ successful implementation and performance of their responsibilities, satisfaction, or the match between their expectations and experiences [6].
Objectives
The objectives of this study were to describe the CHAs’ training, responsibilities, and retention; characteristics, perceptions, and behaviors; impressions of their training and experiences in the program and volunteer satisfaction; and effectiveness as trainers and providers of technical assistance.
Methods
Setting and recruitment
For Phase 2 of the D&I study, the researchers partnered with the South Carolina Conference of the United Methodist Church to recruit CHAs through advertisements in church publications and websites, mailings and emails to pastors, emails to lay leaders, and presentations at district level and statewide pastors’ meetings and lay leader events. Interested individuals completed a form describing their training or experiences related to health, HE, and PA. Two staff persons conducted telephone interviews addressing the individuals’ interest, experiences, comfort level, and self-rated strengths and limitations related to being a CHA, conducting HE and PA programs, working with churches, and conducting training, teaching, or public speaking; their ability to travel for trainings, their schedule flexibility for delivering TA calls and training; and their commitment duration for the CHA position. With the applicant’s permission, the staff person sent the applicant’s pastor a review form and a CHA position description and requested the pastors’ rating of his/her confidence that the applicant possessed the requirements and skills. The review form also allowed the pastor to write other relevant comments. Based on the applicant interviews and the pastors’ ratings, staff persons reached consensus on which applicants to invite to participate.
Community Health Advisors’ training, role, and responsibilities
A paper describing the Phase 1 CHA training, including its content and evaluation, along with CHA roles and responsibilities, has been described in detail [15]. The same approach was applied in Phase 2 with a larger group of CHAs. Because of the larger number of CHAs, we also added a self-administered questionnaire that they completed before and after their participation (described below). The CHA training included online self-paced, narrated material; a day-long, in-person training session; telephone-based training regarding record-keeping responsibilities; three “booster” sessions through conference calls to problem-solve and reinforce CHAs’ skills and three newsletters over 12 months; and telephone- and email-based support as needed. Staff persons observed the CHAs co-deliver at least one church training session and provided informal, constructive feedback by email or phone, including general tips gleaned from across all the sessions and tips specific to each CHA’s observed session(s).
Trained CHAs then provided a day-long training session(s) to church program committees and a year of monthly telephone-based TA to pastors (four calls) and church program coordinators (eight calls) to support program implementation. TA calls followed a structured, flexible script to provide active listening and feedback, goal-setting, problem-solving, and discussion of challenges and successes. The CHAs tracked TA completion and content in an online data entry system. They received reimbursement for travel costs to training and modest compensation for participation as a CHA. Retention strategies were the aforementioned newsletters; a monthly gift card drawing for timely data entry; an increase in the CHA stipend, along with a more appealing distribution schedule; recognition by name via an article in the South Carolina United Methodist Church’s newspaper; handwritten thank-you and holiday cards; and program-related resource guides.
Evaluation measures and methods
Community Health Advisors’ Characteristics, Perceptions, and Behaviors
Before their training, the CHAs completed a baseline self-administered questionnaire with sociodemographic characteristics and relevant professional background and experience in HE and PA and in teaching or leading training or public speaking; personal interest and experience with HE and PA behaviors (1–4: none to a lot); perceived level of knowledge of HE and PA (1–5: very low to very high); self-rated health (1–5: poor to excellent); and height and weight. Body mass index was computed as weight in kilograms divided by height in meters2.
HE was measured as cups per day of fruit and vegetables (F&V). The questionnaire showed a list of 1-cup examples to assist CHAs in reporting their cups of fruit and 100% fruit juice and cups of vegetables and 100% vegetable juice per day. This measure was sensitive to change in other faith-based studies [16, 17]. Three items based on the original six items in the 2009 Behavioral Risk Factor Surveillance System physical activity module assessed moderate to vigorous intensity physical activity (MVPA). The only change was the combining of moderate and vigorous intensity activities for each question (i.e., whether activity was done, days/week, and duration/day). Consistent with the 2008 Physical Activity Guidelines for Americans, and based on minutes/week of MVPA, CHAs were categorized as inactive (<10 minutes/week of PA), underactive (10–149 minutes/week), or regularly active (≥150 minutes/week).
Community Health Advisors’ Evaluation of their Training and Program Experiences
At the end of the CHA training session, CHAs rated the training regarding ease of application, role clarity, confidence in needed skills, comfort in contacting university staff, and program materials and resources. They also rated the training’s pace and replied to open-ended questions regarding most and least liked training aspects and suggested improvements.
Additionally, the CHAs completed an online post-program questionnaire at 12 months that repeated the baseline perceptions, health-related, and behavioral questions, and added questions about their preparation for and satisfaction with the CHA experience.
Based on items from the Volunteer Satisfaction Index, which has established validity and reliability [19], we created 21 items that assessed the CHAs’ satisfaction, modifying items to create program specificity. We also created new questions that addressed the CHAs’ interest in a similar role in the future and a comparison of their actual versus expected time commitment for fulfilling their CHA responsibilities. The CHAs rated the helpfulness of the booster calls and suggested changes. Additional open-ended questions addressed how well the CHAs’ training prepared them and any suggested changes. The CHAs also reported if they attempted to make any changes to their own HE or PA behavior and their levels of success in making these behavioral changes.
Community Health Advisors’ Performance and Effectiveness
Coverage of the Church Training Curriculum
Eight research faculty and staff persons who were familiar with the program and the training curriculum observed the CHAs as they delivered 13 of the 22 church committee training sessions, with the goal of observing each CHA at least once; however, because a staff person participated in the training delivery during four of these sessions, evaluations from those sessions were omitted. The eight observers observed 1–2 sessions each and completed a checklist to rate whether the CHAs who co-delivered the nine sessions had, as a pair, completely, partially, or not covered each of 69 topics and learning activities.
Effectiveness as Trainers
In addition to rating completion of topics and learning activities, the staff observers evaluated each CHA separately on sticking to the allotted time slot (1–4: none of the time to most or all of the time) and indicated agreement (1–4: strongly disagree to strongly agree) regarding the CHAs’ preparation and organization, appropriate eye contact, confidence, enthusiasm and engagement, encouragement and elicitation of participants’ responses and participation, appropriate and respectful interaction with participants, and reliance on reading from their notes or PowerPoint slides.
The church committee members, including pastors, program coordinators, and other members, completed an evaluation form immediately after their training session. Four items assessed each CHA’s effectiveness (1–4: strongly disagree to strongly agree) regarding how well the CHA kept the training interesting, was an effective teacher, appeared to have a good understanding of the material, and was effective in answering questions about the material. They also rated the pace of the presentation as too slow, just right, or too fast.
Ratings of Technical Assistance
At 12 months, pastors and church program coordinators responded to interviews for overall program evaluation. They rated how helpful the monthly calls from the CHA were for carrying out the program in their church (1 to 4: not at all helpful to very helpful) and how they described the length of the monthly calls (1 to 3: too long, just about right, or too short).
Data Analysis
We computed percentages, means, and standard deviations for descriptive purposes and calculated paired t-tests to compare CHAs’ characteristics, perceptions, and behaviors at baseline and 12 months.
Results
Screening and Retention of the Community Health Advisors
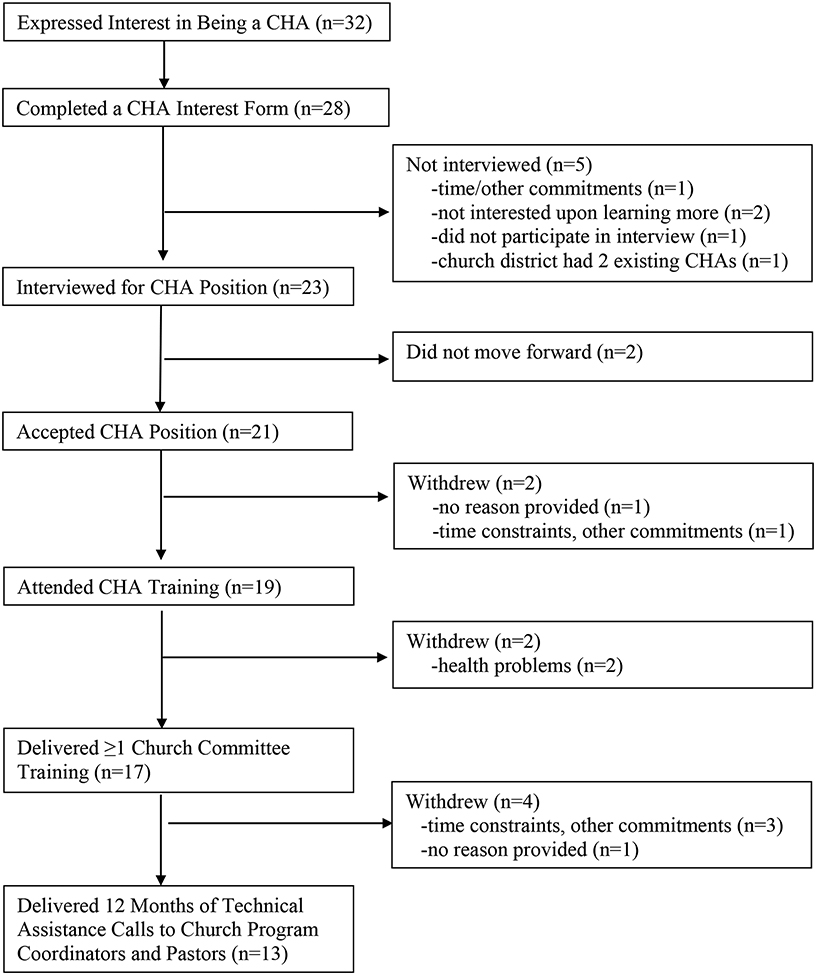
As shown in Table 1, of the 32 people who initially expressed an interest, 23 (71.9%) completed the CHA interview screening process, and 21 were offered and accepted the CHA position (65.6% of those who expressed interest). Of these, two withdrew before completing CHA training. An additional two dropped out before delivering any training; therefore, 17 of 21 CHAs who accepted the position provided training to church committees (81%). Four withdrew after providing church training and some TA (one month’s TA, n=2; three months’ TA, n=1) or no TA (n=1), leaving 13 of the original 21 (62%) who provided both the church training and the full 12 months of TA. Because of the CHA withdrawals, university staff persons and a CHA from the Phase 1 study assisted in providing TA. University staff persons were excluded from the analysis of TA call attempts and completion.
Table 1.
Recruitment and Retention of Community Health Advisors
Community Health Advisors’ Characteristics
Table 2 shows characteristics of the retained 13 CHAs. The majority were women, college educated, employed, married, trained in a health-related field, and in excellent or very good self-rated health. Half self-identified as Black or African American. Their mean years of church membership was 31.5 (SD=19.7). Their employment settings included health care (n=5), ministry (n=3), health/fitness (n=2), the private sector (n=2), and education (n=1). In describing their interests and experiences with HE and PA, the CHAs described their own behavioral change efforts, challenges, and successes and their own and/or a family members’ health-related challenges. Means for their self-rated levels of relevant background and experience (1, none to 4, a lot) were the following: for PA, mean=2.5, SD=1.1; HE, mean=2.8, SD=1.0; and teaching, training, or speaking, mean=3.6, SD=0.7. At baseline and 12 months, seven CHAs (54%) reported they had led or co-led health promotion efforts at their churches, with the predominant topics of HE and PA.
Table 2.
Characteristics of Community Health Advisors in a Faith-Based Healthy Eating and Physical Activity Study (n=13)
| Characteristic | n | % |
|---|---|---|
| Degree or certificate in a health-related field (yes) | 8 | 61.5 |
| Self-rated health status | ||
| Excellent or very good | 10 | 76.9 |
| Good | 3 | 23.1 |
| Fair or poor | 0 | 0.0 |
| Employment | ||
| Full-time (32 or more hours per week) | 7 | 53.8 |
| Part-time (Less than 32 hours per week) | 4 | 30.8 |
| Not employed | 2 | 15.4 |
| Gender (women) | 12 | 92.3 |
| Education | ||
| College graduate (Bachelor’s or higher) | 10 | 76.9 |
| Some college (1 year to 3 years) | 2 | 14.3 |
| High school graduate | 1 | 7.1 |
| Race | ||
| Black or African American | 7 | 53.8 |
| White | 5 | 38.5 |
| Missing | 1 | 7.7 |
| Marital Status | ||
| Married or living with a partner | 9 | 69.2 |
| All others | 4 | 30.8 |
| Mean | SD | |
| Age, years | 54.2 | 10.4 |
Note. Community Health Advisors who delivered church training and 12 months of technical assistance.
Community Health Advisors’ Perceptions and Behaviors
The CHAs (n=13) had small, statistically significant increases in their perceived knowledge of PA and HE from baseline to 12 months. For knowledge about PA, exercise, or fitness, the mean was 3.5 (SD=0.66) at baseline and 4.0 (SD=0.81) at 12 months (t=3.2, df=12, p=0.01). The mean for perceived knowledge of HE was 3.7 (SD=0.75) at baseline and 4.1 (SD=0.64) at 12 months (t=2.74, df=12, p=0.02)
At 12 months, 12 of the 13 affirmed that they had tried to make changes in their own HE or PA behaviors. Changes attempted were increasing PA (n=6), F&V intake (n=6), or whole grains (n=1); reducing sodium (n=6) or carbohydrates (n=1); replacing soft drinks with water (n=2); and other behavioral changes (n=4) (label reading, making healthier choices, diet monitoring, joining a weight loss program). They described themselves as very successful (n=2), successful (n=5), moderately successful (n=4), or “not where I want to be” (n=1) in their attempts to change.
At baseline, no CHAs reported being inactive, three reported being underactive, and nine reported accumulating ≥150 minutes of MVPA weekly. At 12 months, there were two, four, and seven CHAs, respectively, at each PA level. A Fisher’s exact test comparing baseline and 12-month PA levels was not significant (p=.49). The mean combined daily F&V intake was 5.7 cups (SD=1.4, 4–8 cups) at baseline and 4.9 cups at 12 months (SD=1.6, 3–8 cups). A paired t-test between baseline and 12-month F&V intake was not significant (t=1.45, df=12, p=.17).
The mean BMI (kg/m2) at baseline was 29.8 (SD=6.5, 20.6–40.8), and at 12 months, it was 29.4 (SD=6.9, 20.3–44.3), which are BMI values classified as overweight [20]. A paired t-test of baseline and 12-month BMI was not significant (t=0.86, df=12, p=.41). The mean for self-rated health of 3.8/5.0 did not change from baseline to 12 months.
Community Health Advisors’ Evaluation of their Training and Experiences
Seventeen of the 19 CHAs who attended the CHA training completed an evaluation immediately after the training. As shown in Table 3, the CHAs had very positive impressions of their training, with a grand mean of 3.8/4.0 for the five items. While the majority felt the training’s pace was just right, a substantial minority thought it was too fast.
Table 3.
Community Health Advisors’ (CHA) Evaluation of Their Training and Experiences
| In-Person CHA Training (n=17)1 (1, Strongly disagree to 4, Strongly agree) | Mean | SD |
|---|---|---|
| What I learned in today’s training can easily be applied when I train [program name] committees. | 3.8 | 0.4 |
| My role and tasks needed to carry out training with [program name] committees are clear. | 3.7 | 0.5 |
| I am confident that I have the skills needed to do [program name] committee training. | 3.6 | 0.5 |
| I feel comfortable contacting the university staff as needed following today’s training | 3.9 | 0.3 |
| I will use the materials/resources given to me today. | 3.9 | 0.2 |
| The information in this training was provided at an appropriate pace.2 (too slow, just right, too fast) | Just right % | Too fast % |
| 56.3 | 43.8 | |
| CHA Experiences (n=13)3 | Mean | SD |
| How would you describe the amount of time it took to complete the Community Health Advisor work compared to what you expected? (1, A lot more time than expected to 5, A lot less time than expected) | 1.9 | 0.9 |
| The booster calls were helpful to me in my Community Health Advisor work. (1, Strongly disagree to 5, Strongly agree) | 4.1 | 0.6 |
| Based on my experience as a Community Health Advisor, I would be interested in volunteering in a similar role if there were future opportunities. (1, Strong disagree to 5 Strongly agree) | 3.5 | 1.4 |
| We mailed you three Newsletters – “[Program name] Quarterly Connection.” How much of each newsletter did you read? (most or all, some, none) | Most or all % | Some % |
| 53.8 | 46.2 |
Note. Percentages may not sum to 100 because of rounding.
Questionnaire administered immediately following CHA training sessions to the 17 CHAs who participated in training.
16 respondents, 1 missing
Online questionnaire administered at 12 months to the 13 retained CHAs.
Aspects of the training CHAs liked best were the organization, clarity, and thoroughness of the material; the presenters’ positive qualities of focus, friendliness, ease of manner, and clear delivery; the informal, small-group format; tips, how-to information, and scripts; activities such as physical activity breaks and role playing; and continuing support for training delivery to the churches. Aspects they liked least were the long day or the inclusion of too much material for the time. Two noted no problems and complimented the training, and eight CHAs had no comments about anything they disliked. There were few suggestions for improvements. Two CHAs suggested more time for the session. One suggested that the session begin with a prayer to emphasize the program’s faith aspect (Note: this omission was an oversight in the first training session and was added to the subsequent trainings).
In the 12-month questionnaire, the CHAs thought that the time required of them on average was somewhat more than expected. Key activities such as reaching people to schedule and complete the calls, delivering the TA calls, and data entry to track call completion required more time than expected; however, on average, the CHAs agreed that they would be interested in volunteering for a similar role in the future (see Table 3).
The CHAs agreed that the booster calls were helpful (see Table 3); they stated that “everything was helpful [about the calls],” and “they … ran well and I liked the set agenda and time.” Suggestions were to make the calls more structured to encourage participation and invite CHAs to submit questions ahead of time. Note that before each call, we invited the CHAs to submit questions for the call, but some might have missed this invitation in the emails, which conveyed multiple points.
The majority read most or all of the three CHA newsletters, and all read at least some of them (see Table 3). Two CHAs described them as “fine,” or “somewhat insightful,” while the remainder were very positive, describing them as “useful,” “informative,” “relevant,” “supportive-added support for the role,” “very helpful,” “timely,” and “good information-reminder of goals or content,”
Table 4 presents the CHA’s satisfaction with their role as a volunteer. The item means indicate that the CHAs were “moderately satisfied” to “very satisfied” with their experiences. CHAs were especially satisfied with the support they received from university staff, acknowledgement from university staff, degree to which they felt they were a valued member of the program team, and availability of help from the university staff (means of 6.8–7.0). The grand mean was 6.2.
Table 4.
Community Health Advisors’ Volunteer Satisfaction (n=13)
| Volunteer Satisfaction (1, Very dissatisfied to 7, Very satisfied) | Mean | SD |
|---|---|---|
| The amount of information I received about the [program name’s] goals and objectives. | 6.5 | 1.2 |
| The support I received from the university staff. | 6.8 | 0.5 |
| The match between my expectations of the Community Health Advisor role and responsibilities and my actual experience. | 6.0 | 1.1 |
| How often the university staff acknowledged the work I do as a Community Health Advisor. | 6.9 | 0.3 |
| The amount of performance feedback that I received. | 6.6 | 0.5 |
| The degree to which I felt that I was a valued member of the [program name] team. | 6.8 | 0.3 |
| The availability of help from the university staff when I needed it. | 7.0 | 0.0 |
| The progress that I saw among churches in the [program name]. | 5.8 | 1.2 |
| The difference my work as a Community Health Advisor has made. | 6.1 | 1.0 |
| My ability to do the work of a Community Health Advisor as well as anyone else. | 6.1 | 1.2 |
| The opportunities I have had to learn new things. | 6.6 | 0.5 |
| The fit between my skills and the Community Health Advisor role. | 6.5 | 0.9 |
| How worthwhile my contribution was. | 6.5 | 0.9 |
| The amount of effort I put in as equaling the amount of change I influenced. | 5.6 | 1.4 |
| The amount of interaction I have had with other [program name name] Community Health Advisors. | 5.6 | 1.0 |
| My relationship with the other [program name] Community Health Advisors. | 5.1 | 1.2 |
| Extent to which the Community Health Advisor training prepared me to be a Community Health Advisor. | 6.5 | 0.9 |
| The quality of communication with church [program name] coordinators. | 6.0 | 1.2 |
| The quality of communication with [program name] pastors. | 5.4 | 1.7 |
Note. Online questionnaire administered at 12 months to the 13 retained CHAs.
Community Health Advisors’ Performance and Effectiveness
Delivery of Church committee training
Between April 1 and June 16, 2017, CHAs provided training to 347 church members from 115 churches (60 pastors, 106 program coordinators, and 181 other committee members). They presented 22 training sessions in 20 cities around the state. Attendance at each session ranged from 3 to 42 people representing 1 to 13 churches per training. Of the 22 sessions provided, the 17 CHAs co-delivered 17 sessions in pairs, while one CHA presented a session alone (the one training that included a single church). Scheduling the remaining four sessions necessitated pairing a CHA with a member of the university research team. Each CHA delivered one to five training sessions.
Coverage of the Church Training Curriculum
The goal of observing each CHA delivering church training at least once was met for 15 of the 17 CHAs. Observers’ ratings for two CHAs were not included in this analysis because staff persons participated in the training. The staff observers rated coverage of 69 content areas and learning activities across nine trainings and yielded a potential total of 621 ratings. Six ratings (1%) were missing. Of the 615 available ratings, 87.8% (n=540) rated the content or activity as completely covered, 7.1% (n=44) partially covered, and 5.0% (n=31) not covered at all.
Effectiveness as Trainers
As shown in Table 5, the staff observers of CHAs’ church training delivery provided ratings on seven items that described behaviors and attributes of effective trainers. The grand mean was 3.3.
Table 5.
Community Health Advisors’ Effectiveness as Trainers
| Observers’ Ratings1 | ||
|---|---|---|
| The Community Health Advisor … (1 Strongly disagree to 4 Strongly Agree) | Mean | SD |
| appeared prepared and organized. | 3.2 | 0.9 |
| made appropriate and regular eye contact with participants. | 3.1 | 1.1 |
| appeared confident in his/her role as trainer. | 3.6 | 0.7 |
| was enthusiastic and engaged when delivering training content and leading activities/discussions. | 3.5 | 0.9 |
| encouraged and solicited responses and participation from participants throughout the session. | 3.4 | 0.9 |
| interacted with participants appropriately and with respect (e.g., in answering questions, responding to comments, and general interactions). | 3.7 | 0.4 |
| tended to read from the slide notes or slides when delivering the training content.1 | 2.7 | 1.0 |
| Church Committee Training Attendees’ Ratings3 | ||
| The Community Health Advisor … (1 Strongly disagree to 4 Strongly Agree) | Mean | SD |
| kept the training interesting. | 3.3 | 0.6 |
| was an effective teacher. | 3.4 | 0.6 |
| appeared to have a good understanding of the material. | 3.5 | 0.5 |
| was effective in answering questions about the material. | 3.5 | 0.5 |
Means of eight observers’ ratings of 15 Community Health Advisors during nine of 22 co-delivered church training sessions (one observer observed two sessions); n=2 Community Health Advisors’ ratings missing.
Lower ratings indicate better performance (i.e., not reading from notes or slides).
Means of 202 church committee training attendees with complete data provided 395 ratings of CHAs’ effectiveness during 18 training sessions on each of four items.
A total of 286 of 347 (82.4%) church committee training attendees completed a training evaluation immediately after the training session. Responses from the 72 attendees at four training sessions where research staff persons co-delivered the training were omitted from the analysis, resulting in a sample of 214 respondents, 212 of whom rated two CHAs and two of whom rated the one CHA who presented a solo session. Twelve respondents had incomplete data, resulting in a final total of 202 (70.6% of all 286 respondents, 94.4% of the final 214 respondents). As shown in Table 5, CHAs received favorable ratings on the four effectiveness items. The grand mean was 3.4. Among attendees who rated the training’s pace (n=195), 21.0% rated it too slow, 77.9% just right, and 1.0% too fast.
Completion of Technical Assistance Calls
Pastors and program coordinators from participating churches were offered TA calls even if they did not attend a church committee training The program offered one TA call in each of four months to pastors and one call in each of eight months to program coordinators. If each of the 108 churches received all 12 months of TA calls, a total of 1296 calls would have been delivered (864 coordinators and 432 pastors). After church withdrawals from the study or requests to skip or discontinue TA calls, the revised potential total was 1224 calls (811 to coordinators and 413 to pastors). An attempt to deliver TA could require one or more calls, which could result in completion or non-completion. On average, each completed TA call required 2.4 attempts, 2.3 for coordinators and 2.7 for pastors, with a range of 1–11 attempts for coordinators and 1–9 for pastors.
A total of 1200 of the 1224 calls were attempted. CHAs attempted 88.3% (n=1059) of them, while research staff persons attempted the remainder. The following results include call data from the 13 retained Phase 2 CHAs plus the one CHA from Phase 1 but exclude University staff persons. Overall, 97.9% of the 1082 TA calls assigned to the 14 CHAs were attempted at least once, and 71.9% were completed (71.8% for coordinators and 72.0% for pastors). Call duration was 18.1 minutes (SD=10.9) for program coordinators and 16.7 minutes (SD=10.2) for pastors, ranging from 2 to 67 minutes and 2 to 60 minutes, respectively.
Ratings of Technical Assistance
After TA had concluded, 78 pastors and 84 program coordinators completed a 12-month evaluation that included TA questions. Because staff persons rather than CHAs had provided some or all TA to 16 pastors, those pastors were omitted, along with one pastor with missing data, for a total of 61. Fifteen program coordinators were similarly omitted, for final totals of 61 pastors and 71 program coordinators. Pastors’ mean rating of the TA calls’ helpfulness was 3.1 (SD=0.8), and program coordinators’ mean was 3.2 (SD=0.7). Pastors felt the call length was too long (16.4%), just about right (80.3%), or too short (3.2%), while coordinators’ responses were 8.7%, 91.3%, and 0%, respectively.
Discussion
Overall, the CHAs were successful in covering the church training curriculum, and both staff and church committee members perceived them as effective trainers, even though there was variability in performance across CHAs. They had a high TA completion rate and expressed high satisfaction with their training and experiences. Areas with relatively lower satisfaction were the unexpected time commitment and the low interaction with other CHAs. The dispersion of CHAs across the state made face-to-face meetings impractical; however, social media may provide some degree of exchange in similar settings.
While CHAs’ health and behavior change was not a program goal, we examined these variables at baseline and 12 months (the program was implemented in 8 of 13 CHAs’ own churches). While there were no significant changes in self-rated health, BMI, MVPA, or F&V intake, there were small, significant increases in perceived knowledge about HE and PA.
Time constraints and a mismatch between expectations and the reality could have contributed to attrition and satisfaction level. Among the eight CHAs who dropped out after accepting the position, half named time constraints as reasons. Among the 13 CHAs who stayed the entire 12 months, 84.6% felt that the time required of them was a lot more or somewhat more than expected, noting the time to reach pastors and coordinators and complete TA calls. Nevertheless, the CHAs attempted nearly all of the assigned calls and completed 71.9%, while pastors and program coordinators rated the calls as helpful, and the majority perceived the call length as just about right.
By the end of 12 months, there was 61.9% retention among the 21 people who accepted the CHA position. High attrition among volunteer lay providers of evidence-based programs is not unusual [21–23] and may require some combination of over-recruitment to anticipate attrition, ongoing recruitment and training [22, 24], and ongoing professional support (we provided booster calls, newsletters, and individual telephone assistance as requested). These actions increase demands on personnel and financial resources [25]. In this study, because of CHA withdrawals, the investigators and research staff persons assisted the CHAs with training and TA delivery. Our findings suggest that specific assessment of CHA applicants’ available time for project tasks (per week, per month, etc.), clear communication about the time expectations, and over-recruitment both to offset attrition and spread the workload across more volunteers could help alleviate this issue while continuing to indicate appreciation of volunteers’ time. The CHAs’ work occurred as part of a research program and therefore included more data collection and tracking than would be typical. Research-related tasks likely increased the time demand in order to track TA provision, and thus time demands may be somewhat lower in community practice settings.
Conti et al [23] have noted that intensive management of and support to lay providers can reduce the expected savings from lay delivery of evidence-based programs; they found that volunteers with relatively less experience required more support and suggested that “This calls into question whether lay-led delivery models are suitable for scaling-up programs with limited resources,” and that “ … investing in common training and infrastructures for lay leader development could advance the quality and sustainability of real-world program delivery” [23p1].
This description and evaluation of CHAs’ characteristics, behaviors, perceptions, and performance has limitations. Findings are subject to the limitations of self-reported data, especially regarding health behaviors, and potential social desirability bias. Secondly, the small sample size prevents a comparison of characteristics, performance, past experience, and satisfaction between the CHAs who withdrew before the end of 12 months and those who were retained. Further, it prevents the exploration of an association between these same dimensions and the degree of success that churches attained in program implementation.
Faith-based settings have potential to reach large numbers of people who are part of a shared network, and volunteer service is part of faith-based culture, so these settings may be especially suited to lay delivery of health promotion and disease prevention programs; however, this remains an understudied question, and details of Community Health Advisors’ experiences, and volunteer satisfaction are sparse in the research and program evaluation literature. Despite limitations, this study contributes to the literature by describing successes and points of satisfaction, as well as challenges and areas for improvement in the participation of CHAs in upscaling an evidence-based program in a faith-based setting.
Acknowledgments
This work was supported by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion by Cooperative Agreement Number U48-DP-005000. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Department of Health and Human Services. The authors thank the South Carolina Conference of the United Methodist Church for their partnership and contributions to this research. The authors also appreciate the contributions of the faculty, staff, and students of the University of South Carolina Prevention Research Center.
Footnotes
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The University’s Institutional Review Board reviewed the faith-based healthy eating and exercise study and granted exempt status.
Human and Animal Rights and Informed Consent
The Institutional Review Board did not require written informed consent. Completion of questionnaires and interviews for program evaluation was voluntary. Verbal consent was documented, and interviewers provided participants a copy of the consent document.
Notes.
Among the four CHAs who did not deliver 12 months of technical assistance, one delivered no technical assistance calls, two delivered the first month of calls, and one delivered the first three months of calls. To provide adequate coverage after these four withdrew, one CHA from Phase 1 of the study, one graduate student assistant, and one research staff person assisted the remaining 13 CHAs to provide technical assistance calls.
Contributor Information
Patricia A. Sharpe, Arnold School of Public Health, Prevention Research Center, University of South Carolina, 921 Assembly Street, first floor, Columbia, SC 29208.
Sara Wilcox, Arnold School of Public Health, Prevention Research Center and Department of Exercise Science, University of South Carolina, 921 Assembly Street, first floor, Columbia, SC 29208.
Jessica Stucker, Arnold School of Public health, Prevention Research Center, University of South Carolina, 921 Assembly Street, first floor, Columbia, SC 29208.
Deborah Kinnard, Arnold School of Public health, Prevention Research Center, University of South Carolina, 921 Assembly Street, first floor, Columbia, SC 29208.
John Bernhart, Arnold School of Public health, Prevention Research Center and Department of Exercise Science, University of South Carolina, 921 Assembly Street, first floor, Columbia, SC 29208.
Reverend Katherine L. James, South Carolina Conference, The United Methodist Church, 4908 Colonial Drive, Columbia, SC 29203.
References
- 1.Tabak RG, Khoong EC, Chambers D, & Brownson RC (2012). Bridging research and practice: Models for dissemination and implementation research. American Journal of Preventive Medicine, 43(3), 337–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilcox S, Laken M, Parrott AW, Condrasky M, Saunders R, Addy CL et al. (2010). The Faith, Activity, and Nutrition (FAN) program: Design of a participatory research intervention to increase physical activity and improve dietary habits in African American churches. Contemporary Clincial Trials, 31, 323–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilcox S, Parrott A, Baruth M, Laken M, Condrasky M, Saunders R, et al. (2013). The Faith, Activity, and Nutrition program: A randomized controlled trial in African-American churches. American Journal of Preventive Medicine, 44, 122–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilcox S, Saunders RP, Kaczynski AT, Forthofer M, Sharpe PA, Goodwin C et al. (2018). A randomized dissemination and implementation study of the Faith, Activity, and Nutrition program: Countywide adoption, reach, and effectiveness. American Journal of Preventive Medicine, 54, 6, 776–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koch E (2000). Summary of the National Community Health Advisor Study, 1998: A Policy Research Project of The University of Arizona Summary by the Harrison Institute for Public Law, Georgetown University Lay Center. Washington, DC: for the Annie E. Casey Foundation; Retrieved from https://crh.arizona.edu/sites/default/files/pdf/publications/CAHsummaryALL.pdf March 4, 2019 [Google Scholar]
- 6.Fleury J, Keller C, Perez A, & Lee SM (2009). The role of lay health advisors in cardiovascular risk reduction: A review. American Journal of Community Psychology, 44, 28–42. [DOI] [PubMed] [Google Scholar]
- 7.Alcalay R, Alvarado M, Balcazar H, Newman E, & Huerta E (1999). Salud para su Corazon: A community-based Latino cardiovascular disease prevention and outreach model. Journal of Community Health, 24(5), 359–378. [DOI] [PubMed] [Google Scholar]
- 8.Cornell CE, Littleton MA, Greene PG, Pulley L, Brownstein JN, Sanderson BK et al. (2009). A community health advisor program to reduce cardiovascular risk among rural African-American women. Health Education Research, 24(4), 622–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hilfinger Messias DK, Parra-Medina D, Sharpe PA, Treviño L, Koskan AM, & Morales-Campos D (2013). Promotoras de Salud: Roles, responsibilities, and contributions in a multisite community-based randomized controlled trial. Hispanic Health Care International, 11(2), 62–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim S, Koniak-Griffin D, Flaskerud JH, & Guarnero PA (2004). The impact of lay health advisors on cardiovascular health promotion using a community-based participatory approach. Journal of Cardiovascular Nursing, 19(3), 192–199. [DOI] [PubMed] [Google Scholar]
- 11.Navarro AM, Rock CL, McNicholas LJ, Senn KL, & Moreno C (2000). Community-based education in nutrition and cancer: The Por La Vida Cuidandome curriculum. Journal of Cancer Education, 15, 168–172. [DOI] [PubMed] [Google Scholar]
- 12.Hunt CW, Grant JS, & Appel SJ (2011). An integrative review of community health advisors in Type 2 diabetes. Journal of Community Health, 36, 883–893. [DOI] [PubMed] [Google Scholar]
- 13.Community Preventive Services Task Force. Finding and Rationale Statement, Ratified March 2015. Cardiovascular Disease Prevention and Control: Interventions Engaging Community Health Workers. Retrieved March 4, 2019 from https://www.thecommunityguide.org/sites/default/files/assets/CVD-Community-Health-Workers_0.pdf [Google Scholar]
- 14.Community Preventive Services Task Force. Finding and Rationale Statement, Ratified August 2016. Diabetes Prevention: Interventions Engaging Community Health Workers. Retrieved March 4, 2019 from https://www.thecommunityguide.org/sites/default/files/assets/Diabetes-Prevention-Community-Health-Workers.pdf [Google Scholar]
- 15.Sharpe PA, Wilcox S, Kinnard D, Condrasky MD (2018). Community health advisors’ participation in a dissemination and implementation study of an evidence-based physical activity and healthy eating program in a faith-based setting. Journal of Community Health, 43(4), 694–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Resnicow K, Jackson A, Wang T, De AK, McCarty F, Dudley WN, et al. (2001). A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the Eat for Life trial. American Journal of Public Health, 91(10), 1686–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Resnicow K, Campbell MK, Carr C, McCarty F, Wang T, Periasamy S, et al. (2004). Body and soul. A dietary intervention conducted through African-American churches. American Journal of Preventive Medicine, 27(2), 97–105. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. 2009. Behavioral Risk Factor Surveillance System Survey Questionnaire. Retrieved April 4, 2019 from https://www.cdc.gov/brfss/questionnaires/pdf-ques/2009brfss.pdf
- 19.Galindo-Kuhn R, & Guzley RM (2001). The Volunteer Satisfaction Index: Construct definition, measurement, development, and validation. Journal of Social Service Research, 28(1), 45–68. [Google Scholar]
- 20.US Department of Health and Human Services. National Heart, Lung, and Blood Institute. Assessing Your Weight and Health Risk. Retrieved March 1, 2019 from https://www.nhlbi.nih.gov/health/educational/lose_wt/risk.htm
- 21.Lorig KR, Hurwicz ML, Sobel D, Hobbs M, & Ritter PL (2005). A national dissemination of an evidence-based self-management program: A process evaluation study. Patient Education and Counseling, 59(1), 69–79. [DOI] [PubMed] [Google Scholar]
- 22.Shelton RC, Dunston SK, Leoce N, Jandorf L, Thompson HS, Crookes DM et al. (2016). Predictors of activity level and retention among African American lay health advisors (LHAs) from The National Witness Project: Implications for the implementation and sustainability of community-based LHA programs from a longitudinal study. Implementation Science, 11, 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Conte KP, Held F, Piptone O, & Bowman S (2019, in press). The feasibility of recruiting and training lay leaders during real-world program delivery and scale-up: The case of Walk With Ease. Health Promotion Practice, published online April 11, 2019. [DOI] [PubMed] [Google Scholar]
- 24.Alam K, Tasneem S, & Oliveras E (2012). Retention of female volunteer community health workers in Dhaka urban slums: A case-control study. Health Policy and Planning, 27, 477–486. [DOI] [PubMed] [Google Scholar]
- 25.Nesbit R, Christensen RK, & Brudney JL (2018). The limits and possibilities of volunteering: A framework for explaining the scope of volunteer involvement in public and nonprofit organizations. Public Administration Review, 78, 502–513. [Google Scholar]