Abstract
Introduction
Although there is increased public concern about low testosterone levels in aging men, the diagnosis and treatment of hypogonadism in this growing population is controversial.
Aim
To document the current practices of endocrinologists and urologists in the management of older men with low testosterone in Israel.
Methods
A 20-question survey of the management of hypogonadism was sent to members of the Israel Endocrine Society and the Israeli Urology Association
Main Outcome Measures
Participants were interviewed about their practice in diagnostic workup, prescription habits and monitoring of testosterone therapy.
Results
The response rate was low (range 8–12%). Significant differences were found between members of the 2 professional associations. Overall, endocrinologists take a more conservative approach to the diagnosis and initial workup, modes of treatment, and to concerns about the safety of testosterone therapy. A divergence from the published clinical guidelines was also noted in some aspects of the clinical practices in both groups.
Clinical Implications
Significant variances in the diagnosis and treatment approach of hypogonadism between endocrinologists and urologists, as well as divergences from clinical guidelines, may lead to misuse of testosterone therapy.
Strengths & Limitations
This is the first study undertaken in Israel among urologists and endocrinologists of this increasingly recognized health issue. In our country, these 2 groups of physicians comprise nearly all of the testosterone treatment providers. The limitation of this study is linked to bias of all surveys based on subjective reporting, the fact that it was performed in only 1 country, and that we did not control for the specific assay used to measure testosterone levels.
Conclusions
These findings highlight the need for the implementation of coordinated guidelines to facilitate the appropriate diagnosis and treatment of men who can benefit from testosterone therapy and to minimize the risks of this therapy.
Ishay A, Tzemah S, Nitzan R, et al. Testosterone Management in Aging Males: Surveying Clinical Practices of Urologists and Endocrinologists in Israel. Sex Med 2019;7:409–417.
Key Words: Survey, Clinical Practice, Testosterone Management
Introduction
Classical hypogonadism caused by hypothalamic-pituitary disorder or testicular failure is a well-defined condition associated with obvious low testosterone levels that require testosterone (T) replacement therapy. In these patients, the response to T therapy is generally excellent.1 By contrast, age-related decline in testosterone (referred to as age-related hypogonadism or late-onset hypogonadism) is a vaguer syndrome. This is due, first, to the fact that testosterone levels are often only mildly decreased, in contrast to young men with hypogonadism and, second, because the symptoms of androgen deficiency in the elderly may be non-specific and overlap comorbidities.
Numerous conditions are associated with hypogonadism, including obesity, metabolic syndrome, diabetes mellitus, and chronic lung disease. It is well established that, in men, the serum total testosterone (TT) gradually declines with age.2, 3 Due to the age-related increase of the sex hormone–binding globulin (SHBG), the decline in free T is even more pronounced in the elderly. The decreased levels of the bioavailable T (bT) in the elderly is also partially explained by the increase in SHBG with age.4 The declining levels of hormones associated with aging can manifest in a variety of signs and symptoms, including sexual dysfunction, depressive symptoms, mood changes, weakness and functional decline, loss of muscle mass and strength, and osteoporosis.
The prevalence of testosterone deficiency syndrome may vary between 2.1–5.7% in men aged 49–79.5 The rate and the magnitude of the drop in T may be greater in patients with comorbidities, obesity, or medications and could be due to functional suppression of the hypothalamic–pituitary–testicular axis.6, 7, 8 Given the increased life expectancy worldwide, the number of men with testosterone deficiency syndrome will continue to increase and represent an important public health concern.
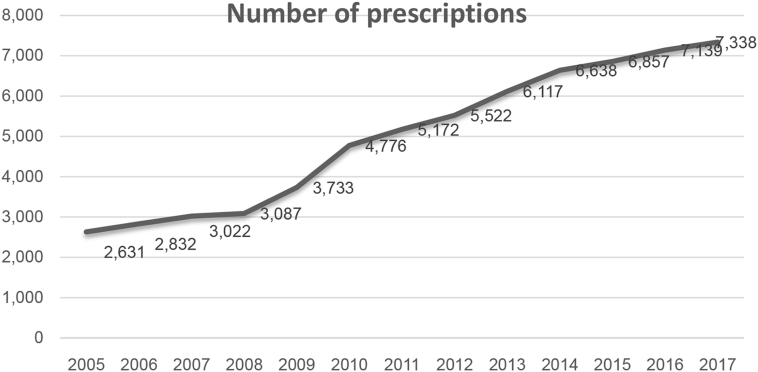
Data available from Clalit Health Services, a not-for-profit health maintenance organization covering more than half of the Israeli population (4,460,965 members) show that there has been an increase of approximately 300% in testosterone prescriptions between 2005–2017 (Figure 1). However, there is considerable controversy regarding whether the age-associated decrease in testosterone levels has any clinical significance and, therefore, should be treated with testosterone supplementation.
Figure 1.
Testosterone prescriptions trend in Israel (2005–2017).
Several guidelines from different professional societies have addressed the problem of diagnosis and management of hypogonadism in adult men.9, 10, 11, 12, 13 In Israel, testosterone replacement therapy is nearly always recommended by endocrinologists and urologists. Previous surveys assessed clinical routine practices among endocrinologists, urologists, and general practitioners.9, 10, 11, 12, 13, 14, 15, 16 But no study was intended to compare the practice patterns between endocrinologists and urologists. The objective of this study is to document and compare the current clinical practice in management of low T in elderly men between endocrinologists and urologists in Israel.
Material and Methods
Survey Design and Implementation
During June–October 2017, an electronic questionnaire was sent by e-mail, using the web-based Survey Monkey tool (Palo Alto, California), to 198 endocrinologists, members of the Israeli Endocrine Society, and to 270 urologists, members of the Israeli Urology Association. The members of the 2 professional associations were contacted, irrespective of their mode and domain of clinical practice. Reminder e-mails were sent 2 and 4 weeks after the first invitation. After consideration, our institutional review board decided that the study does not pose any risk. Therefore, the trial was exempt from registration as a clinical trial. A 20-question survey was designed by the authors to be completed in 10–15 minutes. The questionnaire included demographic inquiries about sex, specialty, seniority, and experience with testosterone therapy of the responders. Most of the survey was comprised of questions about the diagnostic workup and treatment of a hypothetical 64-year-old male patient with suspected androgen deficiency (Table 1). The complete survey is available in the supplementary material in the electronic version of this article.
Table 1.
Index case
| A 64-year-old man presents with decreased libido, reduced erectile function, tiredness, and mild irritability. He has well-controlled hypertension and asymptomatic stable ischemic heart disease for which he had a previous coronary stent 5 years ago. Current medications include an angiotensin II receptor blocker, a statin, and low-dose aspirin. There are no other significant comorbidities. He fathered 4 children in his twenties and thirties. On physical examination, his body mass index is 31.2 kg/m2, body hair is normally, male pattern, distributed. Testes are 20 mL bilaterally, and there is no gynecomastia or muscle atrophy. The prostate is slightly enlarged but not suspicious. He and his wife are bothered by these symptoms and seek your advice about testosterone therapy. |
Statistical Analysis
Categorical factors were reported using frequency tables. The categorical factors consist of a set of demographic data about the respondents (sex, specialty, seniority, and experience with testosterone therapy) and data about the diagnostic workup and treatment of the hypothetical case patient. To analyze the differences between the 2 professional association groups (endocrinologists and urologists) by each of the categorical variables, a series of χ2 tests were conducted or Fisher's exact tests when the assumptions of the parametric χ2 test were not met. To test whether the groups differed by their resistance to start T therapy, a non-parametric Mann–Whitney U test was conducted. We computed 2-tailed P values, where P < .05 is considered a statistically significant result. Statistical analyses were performed using the SAS software package, version 9.4 (SAS Institute, Cary, NC, USA).
Results
Demographics of the Respondents
The response rate was 12% (24 of 198) for the Israeli Endocrine Society members and 8% (40 of 270) for the members of Israeli Urology Association. 90% of the urologists and 100% of the endocrinologists answered all 20 questions. Women accounted for 67% of the endocrinologists' respondents, compared with only 8% of the urologists' respondents. Of the urologists' respondents 64% had ≥10 years’ experience as practitioners compared with 54% of the endocrinologists. The participants’ experience with testosterone therapy (number of patients who initiated T therapy per year) is shown in Table 2.
Table 2.
Experience of respondents in initiating testosterone therapy
| No. of patients yearly | Endocrinologists (n = 24) | Urologists (n = 36) |
|---|---|---|
| 0–12 | 7 (29%) | 12 (33%) |
| 12–24 | 11 (46%) | 9 (25%) |
| ≥25 | 6 (25%) | 15 (42%) |
Responses to the Survey Questionnaire
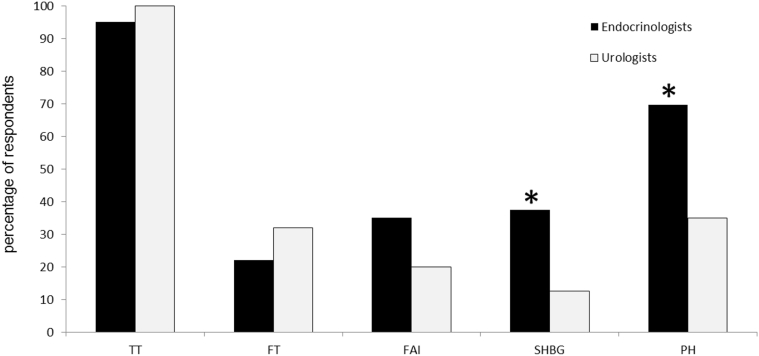
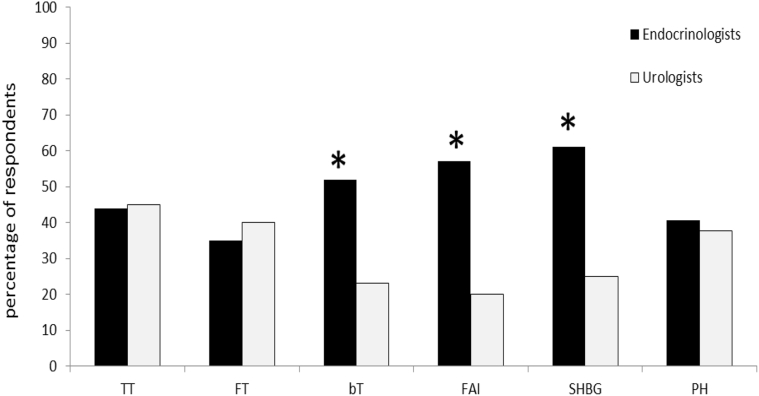
Initial Workup. Initial biochemical testing required by the participants is shown in (Figure 2). Total T was the initial blood test required by most (98.4%) participants. However, whereas 70% of the endocrinologists included measurement of pituitary hormones levels in their initial assessment, only 35% of urologists required these additional measurements (P = .03). In addition, 37.5% of endocrinologists ordered a measurement of the SHBG level (vs 12.5% of urologists, P = .01). When asked about conditions required for blood testosterone sampling, most respondents specifically required morning testing (90% of endocrinologists and 75% of urologists, P = NS), but only 29% of endocrinologists and 10% of urologists (P = .04) would order for fasting sampling. 48% of urologists and 58% of endocrinologists (P = NS) were aware of the importance to test testosterone levels at a safe distance from any acute disease. Overall when analyzed by seniority, younger physicians were more informed of this point than their older colleagues (73% vs 33%, P = .02). Figure 3 shows the additional tests the participants would send, assuming that the initial TT level was borderline or low. It should be noted that only 44% and 45% of the endocrinologists and urologists, respectively, will ask for a repeat TT measurement, but significantly more endocrinologists, compared with urologists, will require other androgen testing: free androgen index, SHBG, or bT (P = .004, .007, and .003, respectively) . In contrast to the hormone tests required at the beginning (Figure 2), at this step, a similar number of endocrinologists and urologists will obtain pituitary hormone (PH) level measurements (Figure 3).
Figure 2.
Initial laboratory measurements requested by all participants. FAI = free androgen index; FSH = follicle- stimulating hormone; FT = free testosterone; LH = luteinizing hormone; PH = pituitary hormones; PRL = Prolactin; SHBG = sex hormone–binding globulin; TT = total testosterone.
Figure 3.
Approach to patient with initial low total testosterone level. bT = bioavailable testosterone; FAI = free androgen index; FSH = follicle-stimulating hormone; FT = free testosterone; LH = luteinizing hormone; PH = pituitary hormones; PRL = prolactin; SHBG = sex hormone binding globulin; TT = total testosterone.
Additional Testing in Patients With Confirmed Low TT and Normal LH FSH Levels. At this stage 70% of endocrinologists require cortisol and FT4 levels, compared with 15% and 12.5% of urologists, respectively (P = .001). 29% of endocrinologists would perform pituitary imaging, compared with 15% of urologists (P = .2). 21% of endocrinologists also require laboratory iron studies, compared with 5% of urologists (P = .09).
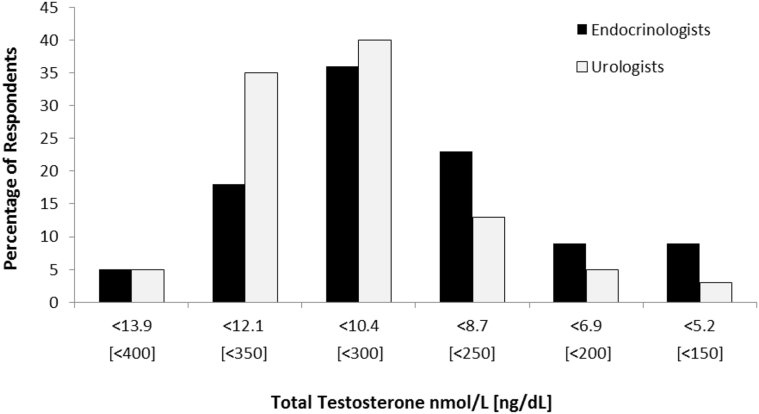
Threshold TT Levels for T Treatment. Assuming that the workup for a pathologic cause of secondary hypogonadism was negative, the participants were asked what would be the T threshold level below which they would offer T therapy. There were no statistically significant differences in the threshold value between the 2 professional groups of respondents (P = .16, Figure 4). But, interestingly, opinions vary when analyzed according to seniority and experience of physicians in T therapy, independent of their specialty: those with <15 years of practice would start T therapy with higher serum TT levels compared with those with professionals practicing >15 years (P = .02). Moreover, those physicians with solid experience in T therapy (treating >25 patients per year) will begin T therapy at higher TT levels compared with practitioners prescribing T less frequently (treating <12 patients per year, P = .03). It should be noted that the distribution of seniority and experience in T therapy between the 2 professional groups did not reveal any statistically significant differences (P = .4 and P = .2 for seniority and experience, respectively).
Figure 4.
Serum total testosterone threshold for testosterone therapy recommendation.
Additional Testing Before Initiating T Therapy. Before commencing with T therapy, 100% of the endocrinologists and 98% of the urologists would order PSA testing, 95% and 85% would obtain a complete blood cell count, respectively. However, only 60% of endocrinologists would perform a digital rectal examination (DRE), compared with 95% of urologists (P = .001). Inversely, only 21% of urologists would order a sleep study, compared with 67% of endocrinologists (P = .001).
Choice of T Formulation and Target T Serum Levels. 40% of urologists and 60% of endocrinologists would use short-acting injectable T enanthate or cypionate as initial therapy, whereas 60% and 40%, respectively, will choose transdermal T gel formulation. For long-term therapy, 90% of urologists would prefer long-acting intramuscular T undecanoate, compared with only 60% of endocrinologists (P = .03). None of the urologists would choose injectable T enanthate or cypionate for long-term therapy in comparison to 12.5% of endocrinologists (P = .04). Apart of clinical improvement with T therapy, the participants were asked which serum T levels they would expect to reach with treatment. Whereas all endocrinologists aim to reach mean low–normal T levels, 24% of urologist aim to reach normal–high T levels (P = .01)
Approach in Presence of Clinical Variations of the Index Case. The participants were asked whether they refrained from starting T therapy if the hypothetical patient had some comorbidities as depicted in Table 3. Overall, endocrinologists were more likely to refrain from initiating T therapy. The most significant differences between the 2 groups were related to prostate health concerns. History of prostate cancer will prevent 58.3% of endocrinologists from initiating T therapy compared with 27.5% of urologists (P = .01). Even history of benign prostate hypertrophy (BPH) will prevent 25% of endocrinologists from starting T therapy, compared with 7.5% of urologists (P = .04)
Table 3.
Clinical situations which would prevent participants to start testosterone treatment
| Clinical situation | Endocrinologists would restrain from starting testosterone therapy (%) | Urologists would restrain from starting testosterone therapy (%) |
|---|---|---|
| The patient had an acute myocardial infarction 5 months ago that required coronary stenting. He now feels well without symptoms of angina or cardiac failure | 35 | 13 |
| The patient had radical prostatectomy 3 years ago for localized prostate cancer (T2cN0M0). The Gleason score at diagnostic was 7 (grade group 2). Since surgery the PSA level is undetectable. | 58.3 | 27.5 |
| The patient has benign prostate hypertrophy, confirmed by biopsy. His PSA level is 4.2. The disease severity as assessed by IPSS is 10 and the disease-specific quality of life score is 2 | 25 | 7.5 |
| The patient has moderate obstructive sleep apnea, BMI of 35.5 kg/m2 and does not tolerate CPAP oxygen therapy | 58.3 | 37.5 |
| The patient is smoking and has a hematocrit of >52% | 100 | 85 |
BMI = body mass index; CPAP = continuous positive airway pressure; IPSS = International Prostate Symptom Score; PSA = prostate-specific antigen.
Monitoring During T Treatment. Overall 68.5% of all participants will schedule the first follow-up visit after starting T therapy within 3 months, with no difference between the 2 groups of physicians. A similar percentage of endocrinologists and urologists would monitor PSA levels within 3 to 6 months of initiating therapy (68% vs 61%, respectively). However, 72.8% of urologists would perform DRE within 6–12 months of therapy, whereas rectal examination would be performed by only 32.4% of endocrinologists (P = .01). There was also a discrepancy regarding hematocrit monitoring. Whereas 86.3% of endocrinologists would annually perform hematocrit measurement, only 62.1% of urologists would do so (P = .04). When asked about scheduling T level measurement during T therapy, most of the respondents were aware of the importance of scheduling T level measurement with injectable testosterone enanthate formulation (90.5% of endocrinologists and 76.5% of the urologists), but less informed about scheduling T levels measurements with other testosterone formulations. Actually, most endocrinologists do not assign any importance to this point when using long-acting testosterone undecanoate, which is in contrast to urologists (66.7% vs 39.5%, respectively; P = .07). However, 53.3% of urologists assign importance to T level measurement timing when using transdermal testosterone gel, vs 16.7% of endocrinologists (P = .03).
Discussion
This study was designed to gauge the current knowledge and practice of endocrinologists and urologists on the management of low testosterone levels in older men. This is the first nationwide survey done on this topic in Israel. Overall this survey revealed significant differences between urologists’ and endocrinologists’ approaches regarding the initial workup and biochemical criteria for diagnosis, modes of treatment, as well as the attitude concerning the safety of T therapy.
A divergence from the clinical guidelines published by the respective professional societies was also noted in some aspects of management. The low response rate we obtain was in line with the response rates reported in similar surveys in Europe and North America.14, 15, 16 All participants agreed that the most specific symptoms of T deficiency are diminished sexual desire and erectile quality. Most of them (92% overall) were also aware that changes in mood concomitant with fatigue and depression may be manifestations of testosterone deficiency syndrome.
67% of urologists would consider anemia as a feature of male hypogonadism compared with 91% of endocrinologists (P = .08). All endocrinologist and 72% of the urologists acknowledge that osteoporosis may be a manifestation of male hypogonadism and would assess bone mineral density within the first year after diagnosis. This is in contrast to results of a previous worldwide survey in which only 38.1% of respondents were aware of the importance of skeletal health and performed bone densitometry measurement in patients with overt hypogonadism.15
Almost all respondents (98.4%) would measure TT level as initial blood test, and most of them are aware of the diurnal variation of testosterone levels and would ask for a morning sample. Only 29% of endocrinologists and 10% of urologists would request a fasting sample, even though there is increased evidence that food intake or glucose load may blunt testosterone levels.17, 18 This is contrary to the current guidelines of the European Association of Urologists and the Endocrine Society, which recommend measuring testosterone levels after an overnight fast.10, 11, 12 However, previous recommendations of the Endocrine Society, the International Society for the Study of the Aging Male1, 11 and the American Urological Association13 did not recommend explicitly that testosterone blood testing be performed in a fasting state. This may partly explain the few participants who were aware of this point. Nearly half of the endocrinologists and more than half of the urologists were unaware that acute illnesses may cause a transient decrease in testosterone concentrations and that it is not recommended to perform testing for testosterone deficiency around and during acute disease.1, 10, 19
Although the current guidelines underline the importance of confirming a borderline-low testosterone level, more than half of the participants did not comply with this recommendation. Inversely, a significantly higher proportion of endocrinologists than urologists (Figure 2) will include this in their first laboratory testing set, measurements of SHBG, gonadotropins and prolactin levels, although this is not a recommendation for an initial diagnosis in men with suspected testosterone deficiency.10, 13
Actually, SHBG and free testosterone (FT) measurements are recommended in initial laboratory tests only if there are comorbidities that may alter SHBG levels and consequently TT levels.10 Moreover, FT measurements performed under reliable standardized conditions are not routinely available in Israel. Direct immunometric assays to measure FT levels are more available but less accurate than the gold standard equilibrium dialysis method.10, 20
Algorithms based on TT, albumin, and SHBG levels may be used to assess FT concentration.21, 22, 23 When low testosterone was confirmed, there was a large difference between the 2 study groups in the degree to which the participants would broaden their investigation of the index case. Similar proportions of endocrinologists and urologists would require a measurement of PRL levels (74% and 79%, respectively), although >75% of urologists were unaware of the relevance of FT4 and cortisol measurements in contrast to only 30% of endocrinologists. 80% of urologists and 71% of endocrinologists would not perform imaging of the pituitary of the index case, which is in accordance with the guidelines that recommend performing pituitary magnetic resonance imaging only when severe secondary hypogonadism; panhypopituitarism; pathologic hyperprolactinemia; or symptoms or signs of acromegaly, Cushing syndrome, or tumor mass effect are present.1
We did not find a significant difference between the 2 interviewed groups in the threshold T level below which they would recommend T therapy. However, urologists were more inclined to offer treatment at a higher threshold: 35% of urologists would start androgen therapy at T levels <12.1 nmol/L, compared with only 18% of endocrinologists (Figure 4). This may be a reflection of the lack of agreement in the published guidelines. The International Society for the Study of the Aging Male and the European Association of Urologists (EUA) recommend a level of 12.1 nmol/L,11, 12 whereas the guidelines of the Endocrine Society recommend a level of 9.2 nmol/L.10
A recent position paper released in August 2018 by a committee including members of the IES, the IUA and the Israeli Society of Sexual Medicine (ILSSM) recommends a level of 10.5 nmol/L.19 The available options of treating male hypogonadism in Israel are short- or long-acting injectable testosterone and transdermal gel. Short-acting preparations are generally preferred for initiating therapy because they are easier to discontinue if needed.24
This survey shows that more urologists than endocrinologists would use newer formulations as an initial therapy (60% vs 40%, respectively for T gel), as well as for long-term therapy (90% vs 60%, respectively for T undecanoate, P = .03). The urologists are also prone to reach higher target T levels than endocrinologists (P = .01). These findings reflect a more conservative approach to T therapy among endocrinologists. Although almost all (99%) respondents will monitor PSA levels during T therapy, only 60% of endocrinologists and 95% of urologists would perform a DRE. This contradicts standards from the Endocrine Society, International Society for the Study of the Aging Male , European Association of Urologists, and ILSSM, which clearly state that men >40 years of age should undergo a physical examination before starting and during testosterone treatment.10, 11, 12, 19
The significantly high percentage of endocrinologists who do not perform DRE may be probably explained by the nature of the professional specialty and by the fact that many endocrinologists are relying on the urologists' assessment with respect to prostate safety. Most respondents are aware of the importance of scheduling T levels measurements midway between injections of T enanthate,1, 10 but they seem to be less informed about scheduling T measurements with newer formulations. Actually, only 33.3% of endocrinologists (in contrast to 60.5% of urologists) are aware that it is recommended for testosterone undecanoate to measure serum T levels at the end of the dosing interval, just before the next injection and aim to achieve base levels in low–mid range.10 Inversely, the timing of T measurement with transdermal testosterone gel is less critical, after the patient has been receiving treatment for ≥1 week.10
In this survey, endocrinologists are more aware about this point (83.3% vs 46.7% of urologists; P = .03). The divergent results we found among endocrinologist and urologists in monitoring testosterone levels are partly the consequence of the experience acquired by each group with a specific formulation but also reflect a lack of knowledge of the pharmacokinetic properties of the different T formulations.
The most common hindrance to T therapy is a history of prostate cancer. In our study, 72.5% of urologists respond that they would offer T therapy to men with history of a Gleason 7 disease after radical prostatectomy and no evidence of biochemical recurrence or metastatic disease. This result is comparable to the percentage (72%) reported in the same situation among members of the Sexual Medicine Society of North America,16 but it differs from a Canadian study in which 96% of urologists stated it will be safe to administer T after radical prostatectomy following prostate cancer.25 It is likely that the Canadian urologist would have responded differently if they had been asked in a more detailed fashion about the grade of the disease. Endocrinologists are more reluctant to prescribe T in such patients. Only 41.7% of the study endocrinologists would prescribe T, which is in line with 27.3% of a large international survey conducted among endocrinologists.15 Nevertheless, these results indicate a change in the old paradigm, among endocrinologists, of absolute contraindication of T therapy in any patient with prostate cancer. As a matter of fact, there are accumulating data supporting the safety of T therapy in a subset of patients with prostate cancer.9, 10, 26, 27, 28 In our survey, 92.5% of urologists and 75% of endocrinologists would prescribe testosterone in hypogonadal men with BPH. This reflects the trend of recent studies that showed that T therapy neither increases the risk of BPH nor worsens lower urinary tract symptoms,29, 30 as was previously thought.31 On the contrary, T therapy may improve lower urinary tract symptoms in hypogonadal men.32, 33
Our survey reveals that 65% of endocrinologists and 87% of urologists believe that testosterone therapy is safe to prescribe to patients who experienced a recent myocardial infarction. This result is in accordance with the percentage (71%) reported recently by members of the Sexual Medicine Society of North America,16 and contrasts with a previous international survey, in which 59.4% of endocrinologists considered a recent myocardial infarction a restricting factor for testosterone therapy.15 There has been significant controversy about the potential cardiovascular harm of testosterone replacement therapy, as reflected by discordant communications released by the Food and Drug Administration and the European Medicines Agency.34, 35 Several reports claimed higher rates of cardiovascular events in men receiving T therapy.36, 37, 38, 39 However, more-recent studies failed to show any association between testosterone therapy and major adverse cardiovascular events or even indicate a potentially cardioprotective effect.40, 41, 42 To date, there are insufficient data to establish a causal link between T therapy and major adverse cardiovascular events, despite the disturbing finding of a significantly increased coronary artery noncalcified plaque volume in 138 participants who receive testosterone.43
Study limitations and strengths
This study has several limitations. First, there is an inherent bias common to these kinds of studies because of the subjective nature of the reports by physicians. There may be discrepancies between the response reports and the actual clinical practice habits. A second drawback is the low response rate, which may reflect a biased participant base who are a priori interested in this topic. Another possible explanation is that members of the IES and IUA include medical trainees or basic scientists who don't usually prescribe testosterone. Third, the survey did not control for the specific assay method for TT measurement used in each local laboratory. Testosterone concentrations are commonly measured using radioimmunoassays, immunometric assays, or liquid chromatography–tandem mass spectrometry. There is considerable interassay and interlaboratory variability in TT and FT measurements. Standardized reference ranges for testosterone levels are critical to differentiate low from normal T levels and thus accurately diagnose hypogonadism.44 This study also harbors a number of strengths. This is the first study performed in Israel on this increasing globally recognized health issue. The study encompasses the practice of almost all the physicians who recommend testosterone therapy in Israel. This study opened the door for a joint initiative including members of the IES, the IUA, and the ILSSM focused on the publication of a position paper on management of male hypogonadism19
Conclusions
This survey uncovers significant differences between endocrinologists and urologists in Israel in various aspects of management of hypogonadism, which is a growing healthcare issue in aging men. The main divergences that stand out between the study groups originates mostly from the initial workup, the preferred use of testosterone preparations, and the approach to safety issues. They reflect a generally more conservative opinion among endocrinologists. These variations reveal the impact of each specialty and probably stem from conflicting guidelines that may affect physicians' beliefs and routine practices. The differences in clinical practices between endocrinologists and urologists highlighted in this study clearly indicate the need for shared and consistently updated guidelines.
Statement of Authorship
Category 1
-
(a)Conception and Design
- Avraham Ishay
-
(b)Acquisition of Data
- Avraham Ishay; Sharon Tzemah
-
(c)Analysis and Interpretation of Data
- Avraham Ishay; Sharon Tzemah; Ronit Nitzan; Ayellet Jehassi
Category 2
-
(a)Drafting the Article
- Avraham Ishay
-
(b)Revising It for Intellectual Content
- Avraham Ishay; Michael Cohen
Category 3
-
(a)Final Approval of the Completed Article
- Avraham Ishay; Sharon Tzemah; Ronit Nitzan; Ayellet Jehassi
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
Funding: None
References
- 1.Bhasin S., Cunningham G.R., Hayes F.J. Testosterone therapy in men with androgen deficiency syndromes: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536–2559. doi: 10.1210/jc.2009-2354. [DOI] [PubMed] [Google Scholar]
- 2.Wu F.C., Tajar A., Pye S.R. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: The European Male Aging Study. J Clin Endocrinol Metab. 2008;93:2737–2745. doi: 10.1210/jc.2007-1972. [DOI] [PubMed] [Google Scholar]
- 3.Feldman H.A., Longcope C., Derby C.A. Age trends in the level of serum testosterone and other hormones in middle-aged men: Longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab. 2002;87:589–598. doi: 10.1210/jcem.87.2.8201. [DOI] [PubMed] [Google Scholar]
- 4.Fabbri E., An Y., Gonzalez-Freire M. Bioavailable testosterone linearly declines over a wide age spectrum in men and women from the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. 2016;71:1202–1209. doi: 10.1093/gerona/glw021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu F.C., Tajar A., Beynon J.M. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123–135. doi: 10.1056/NEJMoa0911101. [DOI] [PubMed] [Google Scholar]
- 6.Basaria S. Testosterone therapy in older men with late-onset hypogonadism: A counter-rationale. Endocr Pract. 2013;19:853–863. doi: 10.4158/EP13318.RA. [DOI] [PubMed] [Google Scholar]
- 7.Grossmann M., Matsumoto A.M. A perspective on middle-aged and older men with functional hypogonadism: Focus on holistic management. J Clin Endocrinol Metab. 2017;102:1067–1075. doi: 10.1210/jc.2016-3580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Travison T.G., Araujo A.B., Kupelian V. The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. J Clin Endocrinol Metab. 2007;92:549–555. doi: 10.1210/jc.2006-1859. [DOI] [PubMed] [Google Scholar]
- 9.Dean J.D., McMahon C.G., Guay A.T. The International Society for Sexual Medicine's process of care for the assessment and management of testosterone deficiency in adult men. J Sex Med. 2015;12:1660–1686. doi: 10.1111/jsm.12952. [DOI] [PubMed] [Google Scholar]
- 10.Bhasin S., Brito J.P., Cunningham G.R. Testosterone therapy in men with hypogonadism: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2018;103:1715–1744. doi: 10.1210/jc.2018-00229. [DOI] [PubMed] [Google Scholar]
- 11.Lunenfeld B., Mskhalaya G., Zitzmann M. Recommendations on the diagnosis, treatment and monitoring of hypogonadism in men. Aging Male. 2015;18:5–15. doi: 10.3109/13685538.2015.1004049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Male hypogonadism guidelines. http://www.uroweb.org/guidelines/online-guidelines/ Available from: Accessed December 31, 2018.
- 13.Mulhall J.P., Trost L.W., Brannigan R.E. Evaluation and management of testosterone deficiency: AUA Guideline. J Urol. 2018;200:423–432. doi: 10.1016/j.juro.2018.03.115. [DOI] [PubMed] [Google Scholar]
- 14.Behre H.M., Christin-Maitre S., Morales A.M. Transversal European survey on testosterone deficiency diagnosis. Aging Male. 2012;15:69–77. doi: 10.3109/13685538.2012.655704. [DOI] [PubMed] [Google Scholar]
- 15.Grossmann M., Anawalt B.D., Wu F.C. Clinical practice patterns in the assessment and management of low testosterone in men: An international survey of endocrinologists. Clin Endocrinol. 2015;82:234–241. doi: 10.1111/cen.12594. [DOI] [PubMed] [Google Scholar]
- 16.Yafi F.A., Haney N.M., Anaissie J. Practice Patterns in the diagnosis and management of hypogonadism: A survey of Sexual Medicine Society of North America Members. Urology. 2017;106:87–95. doi: 10.1016/j.urology.2017.04.036. [DOI] [PubMed] [Google Scholar]
- 17.Caronia L.M., Dwyer A.A., Hayden D. Abrupt decrease in serum testosterone levels after an oral glucose load in men: Implications for screening for hypogonadism. Clin Endocrinol. 2013;78:291–296. doi: 10.1111/j.1365-2265.2012.04486.x. [DOI] [PubMed] [Google Scholar]
- 18.Lehtihet M., Arver S., Bartuseviciene I. S-testosterone decrease after a mixed meal in healthy men independent of SHBG and gonadotrophin levels. Andrologia. 2012;44:405–410. doi: 10.1111/j.1439-0272.2012.01296.x. [DOI] [PubMed] [Google Scholar]
- 19.Position paper on the management and treatment of men with sexual dysfunction and low testosterone. https://www.ima.org.il/userfiles/image/Ne114_tifkudMini.pdf Available at: Accessed August 31, 2018.
- 20.Kacker R., Hornstein A., Morgentaler A. Free testosterone by direct and calculated measurement versus equilibrium dialysis in a clinical population. Aging Male. 2013;16:164–168. doi: 10.3109/13685538.2013.835800. [DOI] [PubMed] [Google Scholar]
- 21.Vermeulen A., Verdonck L., Kaufman J.M. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–3672. doi: 10.1210/jcem.84.10.6079. [DOI] [PubMed] [Google Scholar]
- 22.Zakharov M.N., Bhasin S., Travison T.G. A multi-step, dynamic allosteric model of testosterone's binding to sex hormone binding globulin. Mol Cell Endocrinol. 2015;399:190–200. doi: 10.1016/j.mce.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Sartorius G., Ly L.P., Sikaris K. Predictive accuracy and sources of variability in calculated free testosterone estimates. Ann Clin Biochem. 2009;46(Pt 2):137–143. doi: 10.1258/acb.2008.008171. [DOI] [PubMed] [Google Scholar]
- 24.Parsons J.K., Carter H.B., Platz E.A. Serum testosterone and the risk of prostate cancer: Potential implications for testosterone therapy. Cancer Epidemiol Biomarkers Prev. 2005;14:2257–2260. doi: 10.1158/1055-9965.EPI-04-0715. [DOI] [PubMed] [Google Scholar]
- 25.Millar A.C., Elterman D.S., Goldenberg L. A survey of Canadian urologists’ opinions and prescribing patterns of testosterone replacement therapy in men on active surveillance for low-risk prostate cancer. Can Urol Assoc J. 2016;10:181–184. doi: 10.5489/cuaj.3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baillargeon J., Kuo Y.F., Fang X. Long-term exposure to testosterone therapy and the risk of high grade prostate cancer. J Urol. 2015;194:1612–1616. doi: 10.1016/j.juro.2015.05.099. [DOI] [PubMed] [Google Scholar]
- 27.Khera M., Crawford D., Morales A. A new era of testosterone and prostate cancer: From physiology to clinical implications. Eur Urol. 2014;65:115–123. doi: 10.1016/j.eururo.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 28.Pastuszak A.W., Pearlman A.M., Lai W.S. Testosterone replacement therapy in patients with prostate cancer after radical prostatectomy. J Urol. 2013;190:639–644. doi: 10.1016/j.juro.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Debruyne F.M., Behre H.M., Roehrborn C.G. Testosterone treatment is not associated with increased risk of prostate cancer or worsening of lower urinary tract symptoms: Prostate health outcomes in the Registry of Hypogonadism in Men. BJU Int. 2017;119:216–224. doi: 10.1111/bju.13578. [DOI] [PubMed] [Google Scholar]
- 30.Kathrins M., Doersch K., Nimeh T. The relationship between testosterone-replacement therapy and lower urinary tract symptoms: A systematic review. Urology. 2016;88:22–32. doi: 10.1016/j.urology.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Wang C., Nieschlag E., Swerdloff R. Investigation, treatment and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA and ASA recommendations. Eur J Endocrinol. 2008;159:507–514. doi: 10.1530/EJE-08-0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim J.W., Oh M.M., Yoon C.Y. Nocturnal polyuria and decreased serum testosterone: Is there an association in men with lower urinary tract symptoms? Int J Urol. 2014;21:518–523. doi: 10.1111/iju.12345. [DOI] [PubMed] [Google Scholar]
- 33.Pearl J.A., Berhanu D., Francois N. Testosterone supplementation does not worsen lower urinary tract symptoms. J Urol. 2013;190:1828–1833. doi: 10.1016/j.juro.2013.05.111. [DOI] [PubMed] [Google Scholar]
- 34.Desroches B., Kohn T.P., Welliver C. Testosterone therapy in the new era of Food and Drug Administration oversight. Transl Androl Urol. 2016;5:207–212. doi: 10.21037/tau.2016.03.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.No consistent evidence of an increased risk of heart problems with testosterone medicines. https://www.ema.europa.eu/documents/press-release/no-consistent-evidence-increased-risk-heart-problems-testosterone-medicines_en.pdf Available at: Accessed November 21, 2014.
- 36.Finkle W.D., Greenland S., Ridgeway G.K. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PloS one. 2014;9 doi: 10.1371/journal.pone.0085805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu L., Freeman G., Cowling B.J. Testosterone therapy and cardiovascular events among men: A systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013;11:108. doi: 10.1186/1741-7015-11-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Basaria S., Coviello A.D., Travison T.G. Adverse events associated with testosterone administration. N Engl J Med. 2010;363:109–122. doi: 10.1056/NEJMoa1000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vigen R., O'Donnell C.I., Baron A.E. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310:1829–1836. doi: 10.1001/jama.2013.280386. [DOI] [PubMed] [Google Scholar]
- 40.Aversa A., Bruzziches R., Francomano D. Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: Results from a 24-month, randomized, double-blind, placebo-controlled study. J Sex Med. 2010;7:3495–3503. doi: 10.1111/j.1743-6109.2010.01931.x. [DOI] [PubMed] [Google Scholar]
- 41.Shores M.M., Smith N.L., Forsberg C.W. Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab. 2012;97:2050–2058. doi: 10.1210/jc.2011-2591. [DOI] [PubMed] [Google Scholar]
- 42.Corona G., Rastrelli G., Di Pasquale G. Testosterone and cardiovascular risk: Meta-analysis of interventional studies. J Sex Med. 2018;15:820–838. doi: 10.1016/j.jsxm.2018.04.641. [DOI] [PubMed] [Google Scholar]
- 43.Budoff M.J., Ellenberg S.S., Lewis C.E. Testosterone treatment and coronary artery plaque volume in older men with low testosterone. JAMA. 2017;317:708–716. doi: 10.1001/jama.2016.21043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Travison T.G., Vesper H.W., Orwoll E. Harmonized reference ranges for circulating testosterone levels in men of four cohort studies in the United States and Europe. J Clin Endocrinol Metab. 2017;102:1161–1173. doi: 10.1210/jc.2016-2935. [DOI] [PMC free article] [PubMed] [Google Scholar]