Abstract
Background:
Pain is a common problem, especially in the first few years of breast cancer survivorship. Asian American breast cancer survivors reportedly have inadequate cancer pain management, subsequently reporting lower quality of life compared to other racial/ethnic groups. Technology-based programs could improve cancer pain management process. The purpose of this study was to examine the efficacy of a technology-based information and coaching/support program on cancer pain and its accompanying symptoms of Asian American breast cancer survivors.
Methods:
This study adopted a randomized pretest/posttest group design. The sample included 115 Asian American breast cancer survivors (control: 49, intervention: 66). The participants’ background features, pain (frequency and distress), accompanying symptom distress (global, physical, and psychological), and four theory-based mediators (attitude, self-efficacy, perceived barrier, and social influence) were measured using multiple instruments at three time points (pre-test, post-1-month, and post-3-months). This study took an intent-to-treat approach and conducted linear mixed-model growth curve analyses.
Results:
There were significant decreases in all outcome variables including pain and symptoms over time in both groups. There were greater decreases in physical symptom distress scores among the intervention group compared with the control group (p = 0.0229). The mediators as a whole significantly explained both groups’ overall decreases in general, physical, and psychological symptom distress scores at post-3-months and the intervention group’s greater decreases in general, physical, and psychological symptom distress scores at post-1-month.
Conclusions:
The technology-based program could help reduce cancer pain and its accompanying symptoms of Asian American breast cancer survivors.
Keywords: Technology, Pain, Symptom, Asian Americans, Breast Cancer, Survivors
Precis:
Technology-based programs could improve cancer pain management process. A technology-based program is effective in reducing cancer pain and accompanying symptoms among Asian American breast cancer survivors.
Introduction
The American Cancer Society estimates that, in 2019, there will be an estimated 268,600 new cases of invasive breast cancer, 62,930 new cases of breast carcinoma in situ, and 41,760 breast cancer deaths.1 Due to advances in early detection and treatment, these women represent nearly 44% of female cancer survivors in the U.S.1 These women usually have some combinations of surgery, radiation or chemotherapy, all of which can cause clinically significant chronic pain.2,3 Indeed, pain is a common problem, especially in the first few years of survivorship after treatment as well as during the diagnosis and treatment process.2 Furthermore, the prevalence of pain is much higher in breast cancer survivors compared with those with other types of cancer.2,4 Pain occurs in 25 to 60% of breast cancer survivors,5,6 and approximately 50% report moderate to severe pain.7 Chronic pain reportedly decreases the women’s quality of life and daily functioning, and increases their fatigue, depression, anxiety, and sleep disruption.8,9
Racial/ethnic minorities are reportedly high risk groups for inadequate pain and symptom management within breast cancer survivors. Racial/ethnic minority survivors, particularly underserved patients of lower socioeconomic status, are more likely to present with a later stage disease than non-minority patients, and their pain is more likely to be undertreated.10,11 Fisch et al.12 reported that the odds of a non-Hispanic White having inadequate pain management were about a half of those of a minority patient after adjusting for other explanatory variables (odds ratio, 0.51, p<0.01). Fu et al.13 reported that Hispanic women were more likely to have unmanaged pain-related symptoms than other racial/ethnic groups (p < 0.05). Anderson et al.14 reported that 28% of Hispanic and 31% of African American patients received analgesics that were insufficient to manage their pain. Wang et al.15 reported that Chinese breast cancer survivors were less likely to have their pain resolved because of cultural hesitance to ask help for pain.
Racial/ethnic minority breast cancer survivors shoulder unnecessary burden of pain because they rarely complain about pain, delay seeking help until pain becomes severe, and rarely ask or get necessary information and/or coaching/support due to their cultural values and beliefs and language barriers.16,17 These findings have supported a dire need for information and coaching/support for pain and symptom management in racial/ethnic minority breast cancer survivors.
In this study, the efficacy of a technology-based information and coaching/support program was examined on cancer pain and its accompanying symptoms of Asian American breast cancer survivors. Using the findings from previous studies,18–20 the program was developed with a focus on culturally unique aspects in cancer pain and symptom experience; the program was culturally tailored to Asian American women. The Bandura’s Theory of Behavioral Change21 was used to guide the development of the program and the study design. Four major concepts of the theory (women’s attitudes, self-efficacy, perceived barriers, and social influences) were considered in the program and study design (see the below for more information on the program). The hypotheses that were tested included:
Hypothesis 1. Those who use the study program and the American Cancer Society (ACS) website show significantly greater improvements than those who use only the ACS website in self-reported pain and accompanying symptoms from a pre-test (Time 0) to two follow-up time points (post-1-month [Time 1] and post-3-months [Time 2]).
Hypothesis 2. The theory-based variables (attitudes, self-efficacy, perceived barriers, and social influences) mediate the effect of the study program on self-reported pain and accompanying symptoms from Time 0 to Time 2.
Methods
The study used a randomized repeated measures pretest/posttest control group design. This was conducted as a sub-set of an ongoing intervention study to determine the impacts of a theory-driven, culturally tailored Technology-based Information and Coaching/support program on Asian American breast cancer survivors (TICAA). The Institutional Review Board of the institution that the authors were affiliated approved the parent study. The data were collected during the period between January 2017 and May 2018.
Samples and Settings
The participant recruitment was conducted through both online and offline communities/groups for Asian Americans such as churches, organizations, forums, healthcare centers, professional groups, and social media groups. The study was announced through contacting informal and formal leaders (e.g., website owners, pastors, etc.) and making study announcements in diverse groups of social media and community.
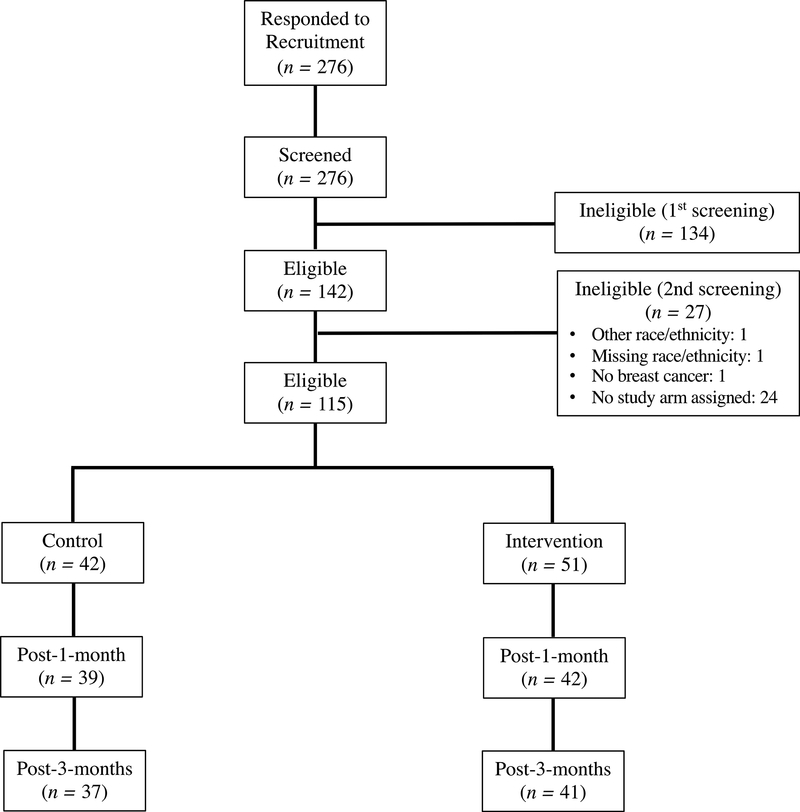
The women were included if they (a) self-identified as Chinese, Korean, or Japanese; (b) were aged 21 years and older; (c) had a diagnosis of breast cancer within the last 5 years; (d) were able to read and write English, Mandarin Chinese (traditional or simplified), Korean, or Japanese; and (e) had access to the Internet using computers or mobile devices. Of 276 screened, 115 were eligible for taking part in the study and became the analytic sample. Of 115, however, only 93 participants completed the pre-test questionnaire. The retention rates among the control group were: 92.9% at post 1-month (n = 39) and 88.1% at post 3-months (n = 37). Those among the intervention group were: 82.4% at post 1-month (n = 42) and 80.4% at post 3-months (n = 41; Figure 1). However, no one actually withdrew from the study.
Figure 1.
Participant flow diagram
When the necessary sample size was calculated using the G*Power 3.1.9.2 software,22 the results showed that 21 participants would be needed with an assumed effect size of 0.8023(the difference in pain and accompanying symptom scores), 80% of power, and an alpha level of 0.10. Thus, the total number of participants (n = 115) in the analysis was adequate to test the hypotheses.
The Technology-Based Information and Coaching/Support Program
The TICAA included online educational modules, online resources, and group and individual (one-to-one) coaching that were culturally tailored (e.g., Chinese RN interventionists for culturally appropriate coaching sessions for Chinese participants). Specifically, the TICAA intervention included: (a) 15 online educational modules provided in five different languages (English, Mandarin Chinese [traditional and simplified], Korean, or Japanese) with general and culture-specific content such as herbal medicine and acupuncture; (b) periodically updated online resources from credible sources in the U.S. and participants’ countries of origin; (c) group and one-to-one coaching by interventionists with a professional (e.g., medical, nursing, or public health) degree and/or license who were from the same ethnic and cultural background with the participants. Group coaching took place in the form of an online forum on the project website where participants could ask questions to interventionists or share information/experience with peer survivors. The one-to-one coaching continued for 12 weeks for each participant via diverse channels, including chatting on the project website, texting, phone calls, or emails. When scheduling individual coaching sessions, the participants could select the channel of communication as they wanted. The information and coaching were to make changes in the women’s attitudes, self-efficacy, perceived barriers, and social influences related to breast cancer and pain and symptom management. The literature supports that coaching24 and information25 could effectively alter health behaviors through modifying attitudes, self-efficacy, perceived barriers, and social influences. More details on the intervention can be found elsewhere.26
Instruments
Multiple instruments were used to assess the participants’ background characteristics, pain and accompanying symptom distress, attitudes, self-efficacy, perceived barriers, and social influences. In this study, 95 of 115 (82.6%) eligible participants were non-English speakers and used languages other than English. At the development stage, all the instruments were forward- and back-translated into Chinese (traditional and simplified), Korean, and Japanese when translated versions of the instruments were not available in these languages by original authors of the instruments.
Background characteristics.
Multiple questions were used to assess women’s sociodemographic and health characteristics including age, sub-ethnicity (Chinese, Korean, or Japanese), educational attainment, religion, marital status, employment, income sufficiency, access to health care, Asians in the neighborhood, type of residential area, U.S.-born, the length of U.S. residence, acculturation, cancer type, cancer stage (Stage I-IV or don’t know), perceived health status, the use of medication, cancer pain management, and cancer-related symptom management. The acculturation level was measured by the Suinn-Lew Asian Self-identity Acculturation Scale (a five-point Likert scale in the areas of food, music, customs, close friends, and language). The instrument’s standardized Cronbach’s alpha was 0.87 in this study.
Pain and accompanying symptom distress.
The Memorial Symptom Assessment Scale-Short Form (MSAS-SF)27 was used to measure cancer pain and its accompanying symptoms. The MSAS-SF assesses the symptom distress associated with 26 physical symptoms (including pain) and the frequency of 4 psychological symptoms during the past 7 days. The distress of each symptom is rated on a 5-point Likert scale (0.8 = “not at all,” 1.6 = “a little bit,” 2.4 = “somewhat,” 3.2 = “quite a bit,” 4.0 = “very much”). If the symptom is not present, a value of zero is assigned. The frequency of psychological symptoms is rated from 1 to 4 (1 = “rarely,” to 4 = “almost constantly”). Each sub-scale’s standardized Cronbach’s alpha was 0.78 (global distress index), 0.75 (physical symptom distress), and 0.77 (psychological symptom distress) in this study.
Attitudes.
The sub-scale of attitudes from the Questions on Attitudes, Subjective Norm, Perceived Behavioral Control, and Behavioral Intention (QASPB) was used to assess one’s attitudes toward breast cancer survivorship and her management of pain and accompanying symptoms.28 The attitude sub-scale was comprised of six items on a 6-point Likert scale (−3 = “dull” to 3 = “interesting”). The standardized Cronbach’s alpha of the attitude sub-scale was 0.96 in this study.
Self-Efficacy.
The Cancer Behavior Inventory (CBI) was adopted to rate how confident women feel about managing stress and changes related to cancer and its treatment. In this study, only six of the 14 original items were used as the summary score of each individual (on a 9-point Likert scale; 1 = “not at all confident” to 9 = “totally confident”). The standardized Cronbach’s alpha of the modified CBI was 0.92 in this study.
Perceived barriers.
The QASPB’ subscale on perceived barriers was used to assess one’s perceived barriers to breast cancer survivorship and management of pain and accompanying symptoms. The sub-scale included 16 items on a 4-point Likert scale (1 = “never” to 4 = “always”) asking how frequent each problem kept a woman from managing her issues/concerns related to breast cancer. The standardized Cronbach’s alpha of the perceived barriers sub-scale was 0.91 in this study.
Social influences.
Three instruments were used to capture one’s social influences on breast cancer survivorship and her management of pain and accompanying symptoms. First, this study adopted the QASPB’ sub-scale on social influences.28 The sub-scale included three items on a 7-point Likert scale (1= “disagree” to 7 = “agree”). Second, the Personal Resource Questionnaire (PRQ-2000) was used to measure one’s perceived level of social support. The PRQ-2000 had 15 items on a 7-point Likert scale, which reflected five dimensions: provision for attachment/intimacy, social integration, opportunity for nurturing behavior, reassurance of worth, and the availability of informational, emotional, and material help. Lastly, the Perceived Isolation Scale (PIS) was used to measure one’s perceived interactions or social isolation. The PIS had six items of social support and three items of interactions/loneliness, all of which were evaluated on a 3-point Likert scale. The standardized Cronbach’s alpha was 0.89, 0.93, and 0.85 for the social influences sub-scale, the PRQ-2000, and the PIS, respectively.
Data Collection Procedures
The participants were asked to choose their preferred language for the project website (English, Mandarin Chinese [traditional and simplified], Korean, or Japanese). When potential participants came to the project website, they were asked to click the ‘I agree to participate’ button to participate in the study (after reviewing the informed consent in their selected languages). When they agreed, they were checked with the inclusion criteria, and only those meeting the inclusion criteria were connected to the online questionnaire for the pre-test. When they completed the pre-test questionnaire, the participants were asked to register for the study through the project website. During the registration process, the participants, through an automated random number generator on the project website, were randomly assigned to two groups (control and intervention). The participants could change their IDs and passwords once they logged in the project website. The participants were asked to print out the electronic instruction sheet for their records.
The participants in both groups were given a web-link to the American Cancer Society (ACS) website on breast cancer survivorship including pain and symptom management, and asked to use the website at their convenience. The information on the ACS website is available in 13 different languages, including Chinese and Korean. During the three-month intervention period, the intervention group was asked to use both the TICAA program and the ACS website, whereas the control group was asked to use only the ACS website. As part of the TICAA program, the intervention group received weekly group or individual coaching by culturally-matched nurse interventionists. The intervention group was also asked to use the online resources housed on the project website (general and culture-specific resources). Then, all participants were requested to complete the second and third questionnaires at the end of the first and the third months. During the time, the participants were asked to keep their usual searches for information through their usual sources of information. The participants also received biweekly reminders and thank you emails by research staff.
Data Analysis
All analyses were performed using the SAS, version 9.4 (SAS Institute, Cary, NC). Statistical significance was determined at an alpha level of 0.05. The outcome variables that were not normally distributed were square-root transformed. However, when the skewness of the outcome variables was not corrected despite various transformations, those variables were analyzed by Friedman’s two-way nonparametric ANOVA. The data analysis in this study took an intention-to-treat approach; hence, missing fields remained as missing without substitution.
First, the participants’ background characteristics at the pre-test were examined using descriptive statistics (e.g., percentage or mean and standard deviation). Also, their features at the pre-test were compared between the study groups using chi-square tests and t-tests, respectively, for categorical and continuous variables. Next, the intervention effects were evaluated using a linear mixed-model growth cure analysis using the SAS/STAT PROC MIXED.29 The modeling was based upon the maximum likelihood estimation, the unstructured covariance structure, and the Kenward-Roger degree of freedom method. Of note, this degree of freedom method is known to improve model performance when a model, like ones in this study, is an unbalanced design, assumes complex covariance structures, and needs to adjust for the bias from a small sample size.30 In this study, two models were built for each outcome: Model 1 included group (control and intervention), time (Time 0, Time 1, and Time 2), and group × time interaction terms. Model 2 added the four domains of mediators (attitudes, self-efficacy, barriers, and social influence) to Model 1 in order to test the hypothesis if such mediators account for the changes in outcomes by group and time. In all models, random intercepts and the pre-determined covariates were controlled. Despite significant time effects in some outcomes, a random slope was not modeled because the current sample size was small and a random slope could add too much complexity to individual models.
Result
Background Characteristics
Table 1 illustrates the participants’ sociodemographic and health characteristics at the pre-test. The average age was about 51.11 ± 11.41 years. Approximately 50% of the participants were Chinese. Over 50% of the participants had a religion, and 63% were married. The participants tended to be highly educated; about 58% were college graduates or with an advanced degree. About 39% were employed, and 50% considered their income sufficient. About 87% of the participants were living in urban areas; 78% were living in neighborhoods where many Asians were populated. Also, approximately 88% of the participants were foreign-born, and they had lived in the U.S. for 16.53 ± 10.30 years on average. The mean acculturation score was 18.16 ± 3.59 (possible range: 5–25). About 89% of the participants had access to health care, 78% had invasive breast cancer, and about 77% were diagnosed with stage I or stage II breast cancer. Only 46% perceived their health status positively (good, very good, or excellent). About 82% were taking medications; about 48% and 65% were managing their cancer pain and cancer-related symptoms, respectively. No differences were observed in these characteristics between control and intervention groups, which supported successful randomization.
Table 1.
Characteristics of the participants by group at the pre-test (N = 115).
| Control | Intervention | Total | χ2 | P-Value | |
|---|---|---|---|---|---|
| Characteristics | (n = 49) | (n = 66) | (n = 115) | or ta | |
| Age (mean ± SD) | 50.50 ± 12.94 | 51.63 ± 10.05 | 51.11 ± 11.41 | −0.48 | 0.63 |
| Subethnicity (%) | |||||
| Chinese | 53.06 | 42.42 | 46.96 | 1.29 | 0.53 |
| Korean | 32.65 | 39.39 | 36.52 | ||
| Japanese | 14.29 | 18.18 | 16.52 | ||
| Religion (%) | |||||
| No | 40.43 | 44.64 | 42.72 | 0.19 | 0.67 |
| Yes | 59.57 | 55.36 | 57.28 | ||
| Marital status (%) | |||||
| Single, never partnered | 6.38 | 9.09 | 7.84 | 7.67 | 0.10 |
| Married | 68.09 | 58.18 | 62.75 | ||
| Partnered, permanent relationship | 6.38 | 3.64 | 4.90 | ||
| Divorced/separated/no longer partnered | 12.77 | 29.09 | 21.57 | ||
| Widowed | 6.38 | 0.00 | 2.94 | ||
| Education (%) | |||||
| Junior high school/graduated | 4.26 | 3.57 | 3.88 | 1.52 | 0.82 |
| High school/graduated | 17.02 | 25.00 | 21.36 | ||
| Partial college | 17.02 | 16.07 | 16.50 | ||
| College/graduated | 36.17 | 37.50 | 36.89 | ||
| Graduate degree | 25.53 | 17.86 | 21.36 | ||
| Employment (%) | |||||
| No | 57.89 | 63.64 | 60.98 | 0.28 | 0.60 |
| Yes | 42.11 | 36.36 | 39.02 | ||
| Income sufficiency (%) | |||||
| Totally insufficient | 11.36 | 24.07 | 18.37 | 3.85 | 0.28 |
| Very hard to pay for basics | 34.09 | 29.63 | 31.63 | ||
| Somewhat hard to pay for basics | 38.64 | 38.89 | 38.78 | ||
| Not hard to pay for basics | 15.91 | 7.41 | 11.22 | ||
| Residence type (%) | |||||
| Urban | 84.09 | 88.89 | 86.73 | 1.15 | 0.56 |
| Rural | 13.64 | 7.41 | 10.20 | ||
| Other | 2.27 | 3.70 | 3.06 | ||
| Asians in the neighborhood (%) | |||||
| No | 18.18 | 25.93 | 22.45 | 0.84 | 0.36 |
| Yes | 81.82 | 74.07 | 77.55 | ||
| U.S.-born (%) | |||||
| No | 88.37 | 87.27 | 87.76 | 0.03 | 0.87 |
| Yes | 11.63 | 12.73 | 12.24 | ||
| Length of U.S. residence (mean ± SD) | 16.41 ± 10.10 | 16.63 ± 10.60 | 16.53 ± 10.30 | −0.09 | 0.93 |
| Acculturation (mean ± SD) | 18.05 ± 3.60 | 18.26 ± 3.62 | 18.16 ± 3.59 | −0.32 | 0.75 |
| Access to health care (%) | |||||
| No | 6.52 | 14.55 | 10.89 | 1.66 | 0.20 |
| Yes | 93.48 | 85.45 | 89.11 | ||
| Type of breast cancer (%) | |||||
| Invasive | 74.36 | 80.77 | 78.02 | 0.53 | 0.46 |
| Non-invasive (in situ) | 25.64 | 19.23 | 21.98 | ||
| Stage of breast cancer (%) | |||||
| Stage I | 32.56 | 34.55 | 33.67 | 0.35 | 0.99 |
| Stage II | 41.86 | 43.64 | 42.86 | ||
| Stage III | 11.63 | 9.09 | 10.20 | ||
| Stage IV | 4.65 | 5.45 | 5.10 | ||
| Don’t know | 9.30 | 7.27 | 8.16 | ||
| Perceived health status (%) | |||||
| Excellent | 2.33 | 3.70 | 3.09 | 2.98 | 0.70 |
| Very good | 16.28 | 12.96 | 14.43 | ||
| Good | 27.91 | 29.63 | 28.87 | ||
| Fair | 37.21 | 31.48 | 34.02 | ||
| Poor | 16.28 | 16.67 | 16.49 | ||
| Don’t know | 0.0 | 5.56 | 3.09 | ||
| Use of medication (%) | |||||
| No | 13.64 | 21.82 | 18.18 | 1.10 | 0.29 |
| Yes | 86.36 | 78.18 | 81.82 | ||
| Cancer pain management (%) | |||||
| No | 57.89 | 47.27 | 51.61 | 1.02 | 0.31 |
| Yes | 42.11 | 52.73 | 48.39 | ||
| Symptom management (%) | |||||
| No | 41.03 | 31.48 | 35.48 | 0.90 | 0.34 |
| Yes | 58.97 | 68.52 | 64.52 |
Chi-square or t-value was presented for categorical or continuous variables, respectively.
Table 2 presents group differences in the outcomes and mediators at the pre-test. There were no significant differentials in pain (frequency and distress), accompanying symptoms (distress), and four mediators (attitudes, self-efficacy, barriers, and social influences) between the control and intervention groups, which also supported successful randomization.
Table 2.
Group differences in the outcomes and mediators at the pre-test (N = 115).
| Control | Intervention | Total | χ2 or t | P-Value | |
|---|---|---|---|---|---|
| Variable | (n = 49) | (n = 66) | (n = 115) | ||
| Outcomes | |||||
| Pain | |||||
| Frequency (%) | 30.61 | 22.73 | 26.09 | 0.91 | 0.34 |
| Frequency (mean ± SD) | 0.31 ± 0.47 | 0.23 ± 0.42 | 0.26 ± 0.44 | 0.95 | 0.35 |
| Distress (mean ± SD) | 0.78 ± 1.30 | 0.62 ± 1.23 | 0.69 ± 1.26 | 0.70 | 0.49 |
| Accompanying symptom distress | |||||
| Global distressa (mean ± SD) | 0.60 ± 0.40 | 0.50 ± 0.43 | 0.55 ± 0.42 | 1.25 | 0.21 |
| Physical distressa (mean ± SD) | 0.53 ± 0.36 | 0.45 ± 0.43 | 0.48 ± 0.40 | 1.03 | 0.31 |
| Psychological distressa (mean ± SD) | 0.55 ± 0.44 | 0.55 ± 0.46 | 0.55 ± 0.45 | 0.03 | 0.97 |
| Mediators | |||||
| Attitudes (mean ± SD) | −2.73 ± 12.36 | 1.21 ± 11.51 | −0.50 ± 11.98 | −1.57 | 0.12 |
| Self-efficacy (mean ± SD) | 77.70 ± 20.94 | 81.98 ± 22.62 | 80.08 ± 21.88 | −0.96 | 0.34 |
| Barriers (mean ± SD) | 29.61 ± 9.14 | 31.96 ± 9.86 | 30.91 ± 9.57 | −1.17 | 0.24 |
| Social influences (mean ± SD) | |||||
| Social influences | 16.98 ± 4.70 | 16.96 ± 3.84 | 16.97 ± 4.22 | 0.02 | 0.99 |
| Perceived social support | 5.41 ± 0.14 | 5.22 ± 1.10 | 5.30 ± 1.02 | 0.87 | 0.39 |
| Perceived isolation | 1.66 ± 0.40 | 1.80 ± 0.50 | 1.74 ± 0.46 | −1.42 | 0.16 |
Note.
The distress of pain and accompanying symptoms was measured by the Memorial Symptom Assessment Scale-Short Form (MSAS-SF). As the mediators, attitudes and perceived barriers, self-efficacy, social influences, perceived social support, and perceived isolation were measured by the modified Questions on Attitudes, Self-Efficacy, Perceived Barriers, and Social Influences (QASPS), Cancer Behavior Inventory (CBI), QASPS’ social influences subscale, Personal Resource Questionnaire (PRQ-2000), and Perceived Isolation Scale (PIS).
Square-root transformation was performed due to the data’s positive skewness.
The Effects on Cancer Pain and Accompanying Symptoms (Hypothesis 1)
Table 3 shows changes in the outcome variables and mediators by group and time. When individual variations were considered, the control group was more likely than the intervention group to experience global, physical, and psychological symptoms at the pre-test. Both groups showed significant decreases in all the outcome variables (i.e., the frequencies and distress scores of pain, the distress scores of global, physical, and psychological symptoms) over time. There were greater decreases in physical and psychological symptom distress scores in the intervention group than in the control group particularly over the first month (βGxT1 = −0.22, p = 0.0062 for physical symptom distress and βGxT1 = −0.18, p = 0.0319 for psychological symptom distress).
Table 3.
Changes in the outcomes and mediators by group and time (N = 115).
| Groups | Control | Intervention | P-Valuesa | ||||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 49) | (n = 66) | Group | Time | Group* Time | |||||
| Mb | SE | M | SE | ||||||
| Pain frequencyc | |||||||||
| T0 | 2.07 | 0.10 | 2.07 | 0.09 | 1.0000 | 0.0499* | 0.9719 | ||
| T1 | 1.99 | 0.10 | 2.00 | 0.09 | |||||
| T2 | 1.94 | 0.10 | 1.93 | 0.09 | |||||
| Pain distressc | |||||||||
| T0 | 2.10 | 0.12 | 2.04 | 0.12 | 1.0000 | 0.0367* | 0.6504 | ||
| T1 | 2.03 | 0.12 | 2.02 | 0.12 | |||||
| T2 | 1.87 | 0.12 | 1.93 | 0.12 | |||||
| Global symptom distressd | |||||||||
| T0 | 0.74 | 0.12 | 0.59 | 0.11 | 0.0024** | 0.0021** | 0.1207 | ||
| T1 | 0.75 | 0.12 | 0.44 | 0.11 | |||||
| T2 | 0.62 | 0.12 | 0.43 | 0.11 | |||||
| Physical symptom distressd | |||||||||
| T0 | 0.63 | 0.11 | 0.51 | 0.11 | 0.0007** | 0.0003** | 0.0229* | ||
| T1 | 0.65 | 0.11 | 0.31 | 0.11 | |||||
| T2 | 0.53 | 0.11 | 0.28 | 0.11 | |||||
| Psychological symptom distressd | |||||||||
| T0 | 0.71 | 0.12 | 0.67 | 0.11 | 0.0580† | <.0001*** | 0.0967† | ||
| T1 | 0.65 | 0.12 | 0.44 | 0.11 | |||||
| T2 | 0.58 | 0.12 | 0.43 | 0.11 | |||||
| Attitudesc | |||||||||
| T0 | 1.71 | 0.26 | 1.71 | 0.24 | 0.8930 | 0.4146 | 0.9616 | ||
| T1 | 1.91 | 0.26 | 1.84 | 0.25 | |||||
| T2 | 1.87 | 0.27 | 1.88 | 0.25 | |||||
| Self-efficacy | |||||||||
| T0 | 86.94 | 5.82 | 94.38 | 5.49 | 0.0102* | 0.0015** | 0.3692 | ||
| T1 | 92.07 | 5.88 | 99.94 | 5.57 | |||||
| T2 | 90.85 | 5.93 | 103.08 | 5.60 | |||||
| Barriers | |||||||||
| T0 | 33.82 | 2.37 | 32.74 | 2.28 | 0.0100* | 0.1596 | 0.0161* | ||
| T1 | 33.51 | 2.40 | 29.65 | 2.29 | |||||
| T2 | 35.49 | 2.41 | 29.19 | 2.33 | |||||
| Social influencec | |||||||||
| T0 | 1.86 | 0.22 | 1.86 | 0.21 | 0.5904 | 0.7866 | 0.0386* | ||
| T1 | 2.03 | 0.23 | 1.62 | 0.21 | |||||
| T2 | 1.67 | 0.23 | 1.88 | 0.22 | |||||
| Perceived social supporte | |||||||||
| T0 | 27.66 | 3.13 | 26.59 | 3.01 | 0.9286 | 0.0724† | 0.6585 | ||
| T1 | 25.63 | 3.14 | 26.12 | 3.02 | |||||
| T2 | 27.87 | 3.17 | 27.94 | 3.05 | |||||
| Perceived isolationd | |||||||||
| T0 | 1.33 | 0.05 | 1.35 | 0.05 | 0.6875 | 0.0213* | 0.8983 | ||
| T1 | 1.31 | 0.05 | 1.32 | 0.05 | |||||
| T2 | 1.29 | 0.05 | 1.30 | 0.05 | |||||
Note.
T0 = pre-test, T1 = post-1-month, T2 = post-3-months, M = mean, SE = standard error.
The distress of pain and accompanying symptoms was measured by the Memorial Symptom Assessment Scale-Short Form (MSAS-SF). As the mediators, attitudes and perceived barriers, self-efficacy, social influences, perceived social support, and perceived isolation were measured by the modified Questions on Attitudes, Self-Efficacy, Perceived Barriers, and Social Influences (QASPS), Cancer Behavior Inventory (CBI), QASPS’ social influences subscale, Personal Resource Questionnaire (PRQ-2000), and Perceived Isolation Scale (PIS).
P-values for Group, Time, and Group*Time were estimated after controlling for age, subethnicity, educational attainment, marital status, income sufficiency, nativity, acculturation, cancer type, cancer stage, perceived health status, and random intercept.
Predicted means for each outcome by group and time.
The variable was still skewed after trying various modes of transformation. Thus, Friedman’s two-way nonparametric ANOVA was used to examine the hypothesis. By virtue of the nonparametric test, the predicted means were computed based on the ranks of outcome scores, not outcome scores per se.
Square-root transformation was performed due to the data’s positive skewness.
Power transformation (second power) was performed due to the data’s negative skewness.
p<.10,
p<.05,
p<.01,
p<.0001
There were meaningful changes in some mediators by group and time. Regardless of the group, the participants experienced positive changes over time in the scores of self-efficacy, perceived social support, and perceived isolation. There were significant increases in the scores of self-efficacy and perceived social support while there were significant decreases in their perceived isolation scores over time. More importantly, there were significant decreases in the perceived barriers scores in the intervention group, but not in the control group (βGxT2 = −3.55 p = 0.0033).
The Mediation of the Theory-Based Variables (Hypothesis 2)
Table 4 shows changes in the regression coefficients of the outcome variables after adjusting for the four domains of mediators. Mediating effects were considered as meaningful when the significant group, time, or their interactive effect in Model 1 lost its statistical significance in Model 2 when mediators were held constant. All the mediators as a whole significantly explained the overall decreases in general, physical, and psychological symptom distress over three months (regardless of the study group). The mediators accounted for the effect of TICAA on the accompanying symptoms especially over one month. In addition, the mediators had independent effects on the accompanying symptoms. Self-efficacy scores independently reduced the general and physical symptom distress scores. The perceived barrier scores independently increased the physical symptom distress scores. The perceived isolation scores independently increased the psychological symptom distress scores.
Table 4.
Regression coefficients of the outcomes (unadjusted and adjusted for the mediators) (N = 115).
| Model 1a | Model 2b | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Variables | Gc | Td | G*Tc | G | T | G*T | Attitude | Efficacy | Barrier | Influence | Perceived resource | Perceived isolation | ||
| Pain frequency | T0 | −0.01 | - | - | −0.01 | - | - | −0.002 | 0.002 | −0.000 | −0.003 | −0.001 | 0.014 | |
| T1 | −0.09 | 0.02 | −0.11 | 0.07 | ||||||||||
| T2 | −0.13 | 0.002 | −0.17† | −0.001 | ||||||||||
| Pain distress | T0 | −0.06 | - | - | −0.03 | - | - | −0.005 | −0.001 | −0.009 | 0.005 | −0.004 | 0.015 | |
| T1 | −0.07 | 0.05 | −0.09 | 0.07 | ||||||||||
| T2 | −0.24* | 0.13 | −0.24† | 0.10 | ||||||||||
| General symptom distress | T0 | −0.15† | - | - | −0.18* | - | - | 0.000 | −0.003* | 0.005 | 0.005 | 0.004 | 0.09 | |
| T1 | 0.01 | −0.16* | 0.05 | −0.06 | ||||||||||
| T2 | −0.12* | −0.04 | −0.06 | 0.08 | ||||||||||
| Physical symptom distress | T0 | −0.12 | - | - | −0.16† | - | - | |||||||
| T1 | 0.02 | −0.22** | 0.02 | −0.08 | 0.002 | −0.003† | 0.007† | 0.008 | −0.05 | −0.05 | ||||
| T2 | −0.10† | −0.13 | −0.05 | −0.05 | ||||||||||
| Psychological symptom distress | T0 | −0.04 | - | - | −0.13 | - | - | |||||||
| T1 | −0.05 | −0.18* | −0.03 | −0.08 | −0.004 | −0.002 | 0.004 | 0.004 | 0.007 | 0.13† | ||||
| T2 | −0.13* | −0.11 | −0.08 | 0.05 | ||||||||||
T0 = Time 0 (pre-test), T1 = Time 1 (post 1 month), T2 = Time 2 (post 3 months), G = group, T = time
Model 1 adjusted for the covariates, including age, sub-ethnicity, educational attainment, marital status, income, country of birth, acculturation, cancer type, cancer stage, and perceived health status in addition to a random intercept.
Model 2 adjusted for the covariates, a random intercept, and the theory-based mediators (attitude, efficacy, barrier, social influence, perceived social support, and perceived isolation).
Group and Group*Time effects were estimated for intervention group, relative to control group as a reference.
Time 0 is a reference.
p<.10,
p<.05,
p<.01
Discussion
The findings reported in this paper agree with the literature that technology-based coaching and support programs are effective in changing health behaviors, subsequently enhancing health outcomes including pain and symptoms.31,32 The literature is clear that technology-based interventions could be effective in improving health outcomes mainly due to easy access (e.g., no geographical or time restrictions) and in approaching isolated/marginalized people with stigmatized conditions and underserved populations.33–34 Moreover, the literature supports that marginalized groups such as racial/ethnic minorities value technology-based programs.33–34
Although the intervention group exhibited more favorable changes in some outcomes, both groups experienced positive changes in all outcomes of interest, which indicates the effectiveness of the attention control condition used in this study—the ACS website. The findings may suggest that a simple use of an informational website could also provide adequate support enough to improve pain and accompanying symptoms of Asian American breast cancer survivors. Nevertheless, the intervention group’s more considerable changes in physical and psychological symptom distress certainly support the need for technology-based coaching and support for Asian American breast cancer survivors. Indeed, the literature has been clear about the necessity of support for Asian American breast cancer survivors; the association of poor quality of life with fewer sources of information and coaching/support is higher for Asians than for Whites.35,36
The significant findings on the mediators’ influences on the intervention effect accord to the literature related to self-efficacy, perceived barriers, social influences, and attitudes. The existing studies strongly support that the survivorship experience of breast cancer patients largely depends on their attitudes toward breast cancer.37 Also, their self-efficacy (to adapt to breast cancer) and perceived barriers reportedly affect their survivorship experience.37,38 Furthermore, social influences including perceived social isolation are reported to affect their survivorship as well.37,38
The findings reported in this paper need careful interpretations because of the study’s limitations. First, the sample selection process and sample size were limited because the current study was a subset of an ongoing larger research project. Second, potential selection bias might be induced because the participants were a selected group of Asian American breast cancer survivors; they were included only when they had Internet access (using computers or mobile devices). Third, cancer pain was not measured using a dedicated instrument, but using a single item of the MSAS-SF (that was developed to assess physical and psychological symptom distress). Subsequently, pain intensity could not be measured. Moreover, because the MSAS-SF is based on a Likert scale, more sophisticated statistical analyses on the effects of the intervention on outcome variables could not be conducted. Fourth, dose-response relationships could not be determined due to a relatively small size of available samples with multiple intervention components, multiple data collection points, and multiple co-variates to consider. Finally, only self-reported data were collected and analyzed in the study.
Conclusions
Based on the findings, the following implications for future research and practice are proposed. First, future studies need a larger number of Asian American breast cancer survivors to replicate the current study and confirm the effects of a technology-based intervention on pain and symptom experience. Second, possible selection bias needs to be carefully identified and controlled in future research. Third, multiple and objective measures of pain and symptoms (e.g., biomarkers) need to be included in future research to minimize possible bias from self-reported data using a single instrument and to adequately determine the intervention effects on pain and symptoms.
Acknowledgements:
We greatly appreciate all the efforts made by the TICAA research team members and research participants.
Source of Funding:
This study was funded by the National Institutes of Health (NCI/NINR; 1R01CA203719).
Footnotes
Data Sharing and Data Accessibility: n/a
Conflict of Interest: The authors have no conflicts of interests to report.
References
- 1.American Cancer Society. Cancer Facts & Figures 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf.
- 2.Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32(16):1739–1747. doi: 10.1200/JCO.2013.52.4629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Satija A, Ahmed SM, Gupta R, et al. Breast cancer pain management - a review of current & novel therapies. Indian J Med Res. 2014;139:216–225. [PMC free article] [PubMed] [Google Scholar]
- 4.Stanton AL, Rowland JH, Ganz PA. Life after diagnosis and treatment of cancer in adulthood: contributions from psychosocial oncology research. Am Psychol. 2015;70(2):159–174. doi: 10.1037/a0037875 [DOI] [PubMed] [Google Scholar]
- 5.Peuckmann V, Ekholm O, Rasmussen NK, et al. Chronic pain and other sequelae in long-term breast cancer survivors: nationwide survey in Denmark. Eur J Pain Lond Engl. 2009;13(5):478–485. doi: 10.1016/j.ejpain.2008.05.015 [DOI] [PubMed] [Google Scholar]
- 6.Forsythe LP, Alfano CM, George SM, et al. Pain in long-term breast cancer survivors: the role of body mass index, physical activity, and sedentary behavior. Breast Cancer Res Treat. 2013;137(2):617–630. doi: 10.1007/s10549-012-2335-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loftus LS, Laronga C. Evaluating patients with chronic pain after breast cancer surgery: the search for relief. JAMA. 2009;302(18):2034–2035. doi: 10.1001/jama.2009.1642 [DOI] [PubMed] [Google Scholar]
- 8.Schou Bredal I, Smeby NA, Ottesen S, Warncke T, Schlichting E. Chronic pain in breast cancer survivors: comparison of psychosocial, surgical, and medical characteristics between survivors with and without pain. J Pain Symptom Manage. 2014;48(5):852–862. doi: 10.1016/j.jpainsymman.2013.12.239 [DOI] [PubMed] [Google Scholar]
- 9.Denlinger CS, Ligibel JA, Are M, et al. Survivorship: pain version 1.2014. J Natl Compr Cancer Netw JNCCN. 2014;12(4):488–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tammemagi CM. Racial/ethnic disparities in breast and gynecologic cancer treatment and outcomes. Curr Opin Obstet Gynecol. 2007;19(1):31–36. doi: 10.1097/GCO.0b013e3280117cf8 [DOI] [PubMed] [Google Scholar]
- 11.Castel LD, Saville BR, Depuy V, Godley PA, Hartmann KE, Abernethy AP. Racial differences in pain during 1 year among women with metastatic breast cancer: a hazards analysis of interval-censored data. Cancer. 2008;112(1):162–170. doi: 10.1002/cncr.23133 [DOI] [PubMed] [Google Scholar]
- 12.Fisch MJ, Lee J-W, Weiss M, et al. Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung, or prostate cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30(16):1980–1988. doi: 10.1200/JCO.2011.39.2381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fu OS, Crew KD, Jacobson JS, et al. Ethnicity and persistent symptom burden in breast cancer survivors. J Cancer Surviv Res Pract. 2009;3(4):241–250. doi: 10.1007/s11764-009-0100-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson KO, Richman SP, Hurley J, et al. Cancer pain management among underserved minority outpatients: perceived needs and barriers to optimal control. Cancer. 2002;94(8):2295–2304. doi: 10.1002/cncr.10414 [DOI] [PubMed] [Google Scholar]
- 15.Wang JH, Adams I, Huang E, Ashing-Giwa K, Gomez SL, Allen L. Physical distress and cancer care experiences among Chinese-American and non-Hispanic White breast cancer survivors. Gynecol Oncol. 2012;124(3):383–388. doi: 10.1016/j.ygyno.2011.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kagawa-Singer M, Wellisch DK, Durvasula R. Impact of breast cancer on Asian American and Anglo American women. Cult Med Psychiatry. 1997;21(4):449–480. [DOI] [PubMed] [Google Scholar]
- 17.Okuyama T, Wang XS, Akechi T, et al. Adequacy of cancer pain management in a Japanese Cancer Hospital. Jpn J Clin Oncol. 2004;34(1):37–42. [DOI] [PubMed] [Google Scholar]
- 18.Im E-O, Lee SH, Liu Y, Lim H-J, Guevara E, Chee W. A national online forum on ethnic differences in cancer pain experience. Nurs Res. 2009;58(2):86–94. doi: 10.1097/NNR.0b013e31818fcea4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Im E-O, Liu Y, Kim YH, Chee W. Asian American cancer patients’ pain experience. Cancer Nurs. 2008;31(3):E17–23. doi: 10.1097/01.NCC.0000305730.95839.83 [DOI] [PubMed] [Google Scholar]
- 20.Im E-O. Online support of patients and survivors of cancer. Semin Oncol Nurs. 2011;27(3):229–236. doi: 10.1016/j.soncn.2011.04.008 [DOI] [PubMed] [Google Scholar]
- 21.Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 22.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- 23.Cohen J Statistical Power Analysis. Curr Dir Psychol Sci. 1992;1(3):98–101. doi: 10.1111/1467-8721.ep10768783 [DOI] [Google Scholar]
- 24.Kissane DW, Love A, Hatton A, et al. Effect of cognitive-existential group therapy on survival in early-stage breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2004;22(21):4255–4260. doi: 10.1200/JCO.2004.12.129 [DOI] [PubMed] [Google Scholar]
- 25.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med. 2002;22(4 Suppl):73–107. [DOI] [PubMed] [Google Scholar]
- 26.Im E-O, Kim S, Lee C, Chee E, Mao JJ, Chee W. Decreasing menopausal symptoms of Asian American breast cancer survivors through a technology-based information and coaching/support program. Menopause N Y N. 2019;26(4):373–382. doi: 10.1097/GME.0000000000001249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT. The memorial symptom assessment scale short form (MSAS-SF). Cancer. 2000;89(5):1162–1171. [DOI] [PubMed] [Google Scholar]
- 28.Armitage CJ. Can the theory of planned behavior predict the maintenance of physical activity? Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2005;24(3):235–245. doi: 10.1037/0278-6133.24.3.235 [DOI] [PubMed] [Google Scholar]
- 29.Littell RC, Milliken GA, Stroup WW, Wolfinger RD SAS System for Mixed Models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- 30.Bell B 433–2013: A Multilevel Model Primer Using SAS® PROC MIXED. 2013:19. [Google Scholar]
- 31.Col NF. Using Internet technologies to improve and simplify counseling about menopause: the WISDOM website. Maturitas. 2007;57(1):95–99. doi: 10.1016/j.maturitas.2007.02.020 [DOI] [PubMed] [Google Scholar]
- 32.Al-Zadjali M, Keller C, Larkey LK, Albertini L, Center for Healthy Outcomes in Aging. Evaluation of intervention research in weight reduction in post menopausal women. Geriatr Nurs N Y N. 2010;31(6):419–434. doi: 10.1016/j.gerinurse.2010.08.010 [DOI] [PubMed] [Google Scholar]
- 33.Pekmezi DW, Williams DM, Dunsiger S, et al. Feasibility of using computer-tailored and internet-based interventions to promote physical activity in underserved populations. Telemed J E-Health Off J Am Telemed Assoc. 2010;16(4):498–503. doi: 10.1089/tmj.2009.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoo J-S, Hwang A-R, Lee H-C, Kim C-J. Development and validation of a computerized exercise intervention program for patients with type 2 diabetes mellitus in Korea. Yonsei Med J. 2003;44(5):892–904. [DOI] [PubMed] [Google Scholar]
- 35.Chlebowski RT, Chen Z, Anderson GL, et al. Ethnicity and breast cancer: factors influencing differences in incidence and outcome. J Natl Cancer Inst. 2005;97(6):439–448. doi: 10.1093/jnci/dji064 [DOI] [PubMed] [Google Scholar]
- 36.Yi JK, Swartz MD, Reyes-Gibby CC. English proficiency, symptoms, and quality of life in Vietnamese- and Chinese-American breast cancer survivors. J Pain Symptom Manage. 2011;42(1):83–92. doi: 10.1016/j.jpainsymman.2010.09.014 [DOI] [PubMed] [Google Scholar]
- 37.van Uden-Kraan CF, Drossaert CHC, Taal E, Shaw BR, Seydel ER, van de Laar MAFJ. Empowering processes and outcomes of participation in online support groups for patients with breast cancer, arthritis, or fibromyalgia. Qual Health Res. 2008;18(3):405–417. doi: 10.1177/1049732307313429 [DOI] [PubMed] [Google Scholar]
- 38.Lieberman MA, Goldstein BA. Self-help on-line: an outcome evaluation of breast cancer bulletin boards. J Health Psychol. 2005;10(6):855–862. doi: 10.1177/1359105305057319 [DOI] [PubMed] [Google Scholar]