Abstract
Background:
As robotic surgery becomes more ubiquitous, determining clinical benefit is necessary in order to justify the cost and time investment required to become proficient. We hypothesized that robotic cholecystectomy would be associated with improved clinical outcomes but also increased cost as compared with standard laparoscopic cholecystectomy.
Materials and methods:
All patients undergoing robotic or laparoscopic cholecystectomy at a single academic hospital between 2007-2017 were identified using an institutional clinical data repository. Patients were stratified by operative approach (robotic vs. laparoscopic) for comparison and propensity score-matched 1:10 based on relevant comorbidities and demographics. Categorical variables were analyzed by Chi-square test and continuous variables using Mann-Whitney U test.
Results:
3,255 patients underwent cholecystectomy during the study period. There were no differences in demographics or BMI, but greater rates of diabetes mellitus, hypertension, and gastroesophageal reflux disease were present in the laparoscopic group. After matching (n=106 robotic, n=1060 laparoscopic), there were no differences in preoperative comorbidities. Patients who underwent robotic cholecystectomy had lesser durations of stay (Robot: 0.1±0.7 vs. Lap: 0.8±1.9, p < 0.0001) and lesser 90-day readmission rates (Robot: 0% [0], Lap: 4.1% [43], p = 0.035); however, both operative and hospital costs were greater compared with laparoscopic cholecystectomy.
Conclusions:
Robotic cholecystectomy is associated with lesser duration of stay and lesser readmission rate within 90-days of the index operation, but also greater operative duration and hospital cost compared with laparoscopic cholecystectomy. Hospitals and surgeons need to consider the improved clinical outcomes but also the monetary and time investment required prior to pursuing robotic cholecystectomy.
Keywords: robotics, laparoscopy, cholecystectomy, cost, readmission
INTRODUCTION
Laparoscopic cholecystectomy is one of the most common operations performed in the United States, with over 400,000 ambulatory laparoscopic cholecystectomies performed in 2010.1 Since the 1990s, laparoscopic cholecystectomy has been considered the operative standard of care for gallstone disease.2,3 Recently, robotic surgery has gained increased popularity and applicability in general surgery, and may provide better outcomes than laparoscopic surgery in certain gastrointestinal procedures.4,5 Robotic cholecystectomy has been demonstrated to be a safe and efficacious procedure, however, there has been little clinical evidence to support its use over laparoscopic cholecystectomy.6–8
Proponents of robotic cholecystectomy cite technical advantages including three-dimensional view, enhanced instrument articulation, improved cosmetics with single port approach, ability for intraoperative fluorescence imaging of the biliary sysrem, and improved precision.9–12 Additionally, robotic cholecystectomy may be associated with leser rates of conversion to open procedure.13 Multiple studies have demonstrated the drawbacks of robotic cholecystectomy which include increased operative time and cost.8,9,13,14 Previous literature, however, has also demonstrated operative time to be similar between robotic and laparoscopic cholecystectomy.7 To date, there have been little data demonstrating improved clinical outcomes in patients undergoing robotic compared to laparoscopic cholecystectomy.
The purpose of this study was to determine if the use of robot assistance in laparoscopic cholecystectomy is justified by comparing outcomes between the two techniques. We hypothesized that robotic cholecystectomy would be associated with improved clinical outcomes but also increased cost as compared with standard laparoscopic cholecystectomy.
MATERIALS AND METHODS
Patient population
All patients undergoing robotic or laparoscopic cholecystectomy between 2007 and 2017 at a single academic medical center were captured using institutional data from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). Primarily, two acute care general surgeons performed the majority of cases, and both surgeons performed both laparoscopic and robotic cholecystectomies. Financial data were obtained from the institutional Clinical Data Repository. The Institutional Review Board at the University of Virginia approved waiver of consent for this study. Preoperative patient characteristics (age, sex, race, body mass index [BMI], and comorbid conditions), perioperative elements (operating room time and operative approach), 30 and 90-day postoperative outcomes, and inflation-adjusted hospital cost were analysed. We compared patients undergoing robotic-assisted cholecystectomy and laparoscopic cholecystectomy. The operative approach was at the discretion of the operating surgeon based on surgeon preference and preoperative characteristics of the patient. All patients requiring conversion to open were excluded from analysis, because cnversion represents a different patient population than elective cholecystectomy.
Data analysis
The primary outcomes for this study were operative time, duration of stay, 30 and 90-day readmission rate, and hospital cost. To account for differences in baseline comorbidities, patients were propensity score-matched 1:10 based on relevant comorbidities and demographics for comparison. We report preoperative factors between the groups in addition to intraoperative variables and postoperative outcomes. Inflation estimates of the Center for Medicare and Medicaid Services Inpatient Prospective Payment System (CMS-IPPS) were used to adjust cost to 2017 dollars to account for medical-specific inflation. Data were compared using Chi-square (χ2) test for categorical variables and Mann-Whitney U test for continuous variables. A p value < 0.05 was used for statistical significance. SAS version 9.4 (SAS Company, Cary NC) was used for all analyses.
RESULTS
A total of 3,255 patients were identified who underwent robotic or laparoscopic cholecystectomy between 2007 and 2017. Robotic-assisted approach was used in 3.3% (n = 106) of cases. There were no demographic differences in age, sex, race, and body mass index (BMI). Type II diabetes mellitus, hypertension, and gastroesophageal reflux disease were statistically significantly different between unmatched groups, with all three comorbidities being more common in the laparoscopic group (Table 1). A total of 1,066 patients (106 robotic, 1060 laparoscopic) were well-matched with no differences in prevalence of preoperative comorbidities, including type II diabetes mellitus, hypertension, chronic obstructive pulmonary disease, obstructive sleep apnea, gastroesophageal reflux disease, atrial fibrillation, chronic heart failure, and smoking status (Table 2). Median age (Robotic: 42 [30-56] vs. Laparoscopic: 43 [30-58] years, p = 0.8) and BMI (Robotic: 30.1 [26.5-36.4] vs. Laparoscopic: 30.2 [26.5-35.2]) were similar between groups. The most common comorbidities in the entire cohort were hypertension, type II diabetes mellitus, and tobacco use.
TABLE 1:
Unmatched demographics and comorbidities
| Robot (n=106) | Laparoscopic (n=3149) | p-value | |
|---|---|---|---|
| Demographics | |||
| Age (y) * | 41.5 [30-56] | 44 [30-57] | 0.7 |
| Female† | 71.7 (76) | 73.3 (2309) | 0.71 |
| White† | 75.5 (80) | 74.6 (2350) | 0.84 |
| BMI‡,* | 30.1 [26.5-36.4] | 30.9 [27-36.2] | 0.31 |
| Comorbidities† | |||
| Type II diabetes mellitus | 6.6 (7) | 13.8 (435) | 0.03 |
| COPD§ | 0 (0) | 2.9 (91) | 0.076 |
| OSA‖ | 2.8 (3) | 6.3 (198) | 0.15 |
| Hypertension | 10.4 (11) | 27 (851) | 0.0001 |
| GERD¶ | 4.7 (5) | 16.5 (520) | 0.0012 |
| Current smoker | 17 (18) | 23.3 (733) | 0.13 |
| CHF# | 0.9 (1) | 2.1 (66) | 0.41 |
| Atrial fibrillation | 0.9 (1) | 2 (64) | 0.43 |
Median [IQR], all such values
% (n), all such values
Body mass index
Chronic obstructive pulmonary disease
Obstructive sleep apnea
Gastroesophageal reflux disease
Congestive heart failure
TABLE 2:
Matched demographics and comorbidities
| Robotic (n=106) | Laparoscopic (n=1060) | p-value | |
|---|---|---|---|
| Demographics | |||
| Age (y) * | 41.5 [30-56] | 43 [30-58] | 0.77 |
| Female† | 71.7 (76) | 70.1 (747) | 0.79 |
| White† | 75.5 (80) | 76 (806) | 0.9 |
| BMI‡ | 30.1 [26.5-36.4] | 30.2 [26.5-35.2] | 0.95 |
| Comorbidities† | |||
| Type II diabetes mellitus | 6.6 (7) | 7.5 (79) | 0.75 |
| COPD§ | 0 (0) | 2.6 (27) | 0.1 |
| OSA‖ | 2.8 (3) | 3.1 (33) | 0.87 |
| Hypertension | 10.4 (11) | 10 (106) | 0.9 |
| GERD¶ | 4.7 (5) | 5 (53) | 0.9 |
| Current smoker | 17 (18) | 18.7 (198) | 0.67 |
| CHF# | 0.9 (1) | 1 (11) | 0.93 |
| Atrial fibrillation | 0.9 (1) | 1.2 (13) | 0.8 |
Median [IQR], all such values
% (n), all such values
Body mass index
Chronic obstructive pulmonary disease
Obstructive sleep apnea
Gastroesophageal reflux disease
Congestive heart failure
Operative duration (total time in the operating room) was greater for patients undergoing robotic-assisted cholecystectomy (Robot: 185 [175–195] vs. Lap: 160 [135–175] min, p < 0.0001, Figure 1). Patients who underwent robotic cholecystectomy had lesser durations of stay (Robot: 0.1±0.7 vs. Lap: 0.8±1.9, p < 0.0001) and lesser rates of 90-day readmission (Robot: 0% [0], Lap: 4.1% [43], p = 0.035, Table 3). Hospital cost (Robot: $6611 [$5484-8098] vs. Lap: $4930 [$4051-6865], p < 0.0001) was considerably more with robotic-assisted cholecystectomy (Figure 1).
FIGURE 1:
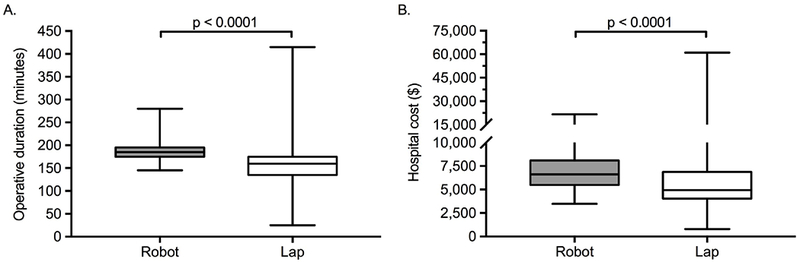
Matched outcomes
A. Operative duration (total time in the operating room) for robotic and laparoscopic cholecystectomies (Robot: 185 [175–195] vs. Lap: 160 [135–175] min, p < 0.0001). B. Hospital cost per case for robotic and laparoscopic cholecystectomies (Robot: $6611 [$5484-8098] vs. Lap: $4930 [$4051-6865], p < 0.0001). Median [interquartile range], all such values.
TABLE 3:
Matched outcomes
| Robotic (n=106) | Laparoscopic (n=1060) | p-value | |
|---|---|---|---|
| Duration of stay (days) | 0 [0-0]* | 0 [0-1] | <0.0001 |
| 30-day readmission† | 0 (0) | 2.6 (27) | 0.096 |
| 90-day readmission† | 0 (0) | 4.1 (43) | 0.035 |
Median [IQR], all such values
% (n), all such values
DISCUSSION
The present study compared outcomes after robotic-assisted and laparoscopic cholecystectomy to determine if there were benefits to performing this operation with robotic-assist. Both operative duration was greater and hospital cost were greater in robotic-assisted cholecystectomy, but hospital duration of stay and 90-day related readmission rates were less in robotic-assisted cholecystectomy; 30-day readmission rates were similar between both groups.
Robotic-assisted operations have become common in certain gastrointestinal procedures, including colorectal surgery.4,5,15,16 The robot has been reported to provide improvement in visualization, dexterity, and instrumentation in minimal accesssurgery.9,10 While robotic surgery has been utilized by many institutions as a marketing tool to increase their local market share, the support for its use in many procedures has not been justified by clinical data. Subsequently, surgeons have begun to use the robot to perform cholecystectomy with outcomes comparable to the more typical laparoscopic approach, however there has been minimal evidence to suggest improved clinical outcomes.6–8
As with any new technology, there is a substantial learning curve associated with efficiently operating the robot assistant.10,17 Additionally, there is a time and monetary investment required to become proficient in the robot. Consequently, it is important to determine whether there are clinical benefits with using the technology.
The present study found that robotic-assisted cholecystectomy takes a greater timeer and is associated with greater hospital charges and cost; but robotic-assisted cholecystectomy also has some improved clinical outcomes compared to laparoscopic repairs. A prospective 1: 1 case-matched study of 50 consecutive patients undergoing robotic cholecystectomy by Breitenstein et al. also found that overall hospital cost to be substantially greater compared to laparoscopic cholecystectomy with no difference in complication rate.8 This observation was supported in a single-center, retrospective review comparing 140 patients undergoing robotic cholecystectomy and 97 patients undergoing laparoscopic cholecystectomy by Strosberg et al. who found the robotic approach to be associated with greater operative time and greater cost; but robotic cholecystectomy was also associated with a lesser rate of conversion to open procedure.13
The present study did not obtain data for specific postoperative complications or whether readmissions were related or unrelated to the index operation. Ayloo et al. , however, demonstrated in a single-center, retrospective review of 326 patients undergoing cholecystectomy (147 laparoscopic and 179 robotic) no difference in complication rate between groups. Interestingly, this study also reported no difference in operative time, attributed to advanced surgeon experience and the high numbers of robotic procedures leading to shorter docking times.7 The learning curve of robotic surgery inevitably contributes to some of the increased operative time in the present study, and all operations had resident involvement.
Hospital cost was greater for robotic-assisted cholecystectomy. There was also a much larger variability seen in operative duration and hospital cost in the laparoscopic cohort compared to the robotic cohort. Because pre-operative diagnosis was not captured in the data, it is likely that more patients who were being treated for acute cholecystitis and operated on a more urgent basis underwent laparoscopic cholecystectomy instead of robotic cholecystectomy due to robot staffing and resource availability. Patients with acute cholecystitis are more likely to require a difficult dissection, and if so, likely contributed to the occasional greater operating times and hospital cost seen. Without the time required to position and set up the robot, a straightforward laparoscopic cholecystectomy can also require much less time than a robotic cholecystectomy. Both of these factors likely contributed to the greater variability seen in the laparoscopic cohort. As robotic surgery is more widely adopted and performed routinely, costs will decrease over time. To justify the use of costlier technology, a clinical benefit should be present. The present study demonstrated no readmissions at 90 days for patients undergoing robotic cholecystectomy, with 43 patients (4.1%) readmitted by 90 days who underwent laparoscopic cholecystectomy. This finding may be a result of improved technique and dissection with the robotic assistant, allowing for decreased postoperative complications, but there may be other hidden factors explaining this as well.
The present study and its findings are limited by the retrospective nature of the study, the single-institution design with two surgeons performing the majority of operations, and the lack of long-term follow up data, quality-of-life data, and data on rate of postoperative complications . Considering that postoperative morbidities and mortalities after cholecystectomy are rare, detecting any statistically significant differences would be difficult with a randomized controlled trial, let alone the retrospective, single-institution experience described here. Additionally, although patients were matched based on their demographics and comorbidities, preoperative diagnosis was not captured in these data, which leaves considerable room for selection bias. Patients in the laparoscopic cohort had a greater duration of stay, which may be attributable to a variety of factors, including the need to stay overnight, especially if the procedure finished in the evening and/or the patient lived far away. A considerable proportion of our institution’s patient population is rural and frequently require multiple hours to drive home, which will often push an evening discharge to the next morning; mhowever, because pre-operative diagnosis was not captured in these data, there is the possibility more patients in the laparoscopic cohort were treated for acute cholecystitis, which would make them more likely to be observed overnight post-operatively. Only 3.4% of patients during the study period underwent robotic cholecystectomy, likely reflective of the limited availability of the robot, properly-trained staff, and/or resources. Use of the robot for cholecystectomy was relatively new to the institution in 2007, and thus used infrequently . Despite this, we present a fairly large cohort of propensity-matched cholecystectomies over a 10-year period, with greater costs and greater operative times, yet lesserer durations of stay and lesser 90-day readmission rates in patients undergoing robotic cholecystectomy.
This is one of the first studies to suggest that a robotic approach to cholecystectomy may provide improved outcomes for patients. Greater operative duration was demonstrated, but as surgeons, residents, and operating room staff continue to use the robot and become more efficient, operative times should decrease. Hospital costs were considerably greater for robotic-assisted cholecystectomy, however this could be offset when one considers the added cost of the greater number of readmissions seen in the laparoscopic group. This work serves to contribute to the increasing body of work suggesting that robotic-assisted cholecystectomy can be justified on clinical grounds, and the disadvantages of increased operative time and cost—have the potential to improve with time. While robotic surgery has an established place in surgical oncology4,5, this study helps to further support the use of robotic-assistance in non-cancer-related, minimally-invasive surgery. Despite these findings, until large dataset analyses or randomized controlled trials can be completed, surgeon comfort level, hospital cost, and patient preference should dictate whether cholecystectomy is approached robotically or laparoscopically.
Acknowledgments
FUNDING/SUPPORT: This work was supported by The National Heart, Lung and Blood Institute [award numbers T32 HL007849 (JHM, RBH) and UM1 HL088925 (EJC)].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
COI/DISCLOSURE: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
REFERENCES
- 1.Hall MJ, Schwartzman A, Zhang J, Liu X (2017) Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report. 102:1–14 [PubMed] [Google Scholar]
- 2.Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW (1992) Laparoscopic Cholecystectomy The New “Gold Standard”? Arch Surg 127:917–921 [DOI] [PubMed] [Google Scholar]
- 3.Wilson RG, Macintyre IM, Nixon SJ, Saunders JH, Varma JS, King PM (1992) Laparoscopic cholecystectomy as a safe and effective treatment for severe acute cholecystitis. Br Med J 305:394–396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin S, Jiang H-G, Chen Z-H, Zhou S-Y, Liu X-SYJ-R (2011) Meta-analysis of robotic and laparoscopic surgery for treatment of rectal cancer. World J Gastroenterol 17:5214–5220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Altieri MS, Yang J, Telem DA, Zhu J, Halbert C, Talamini M, Pryor AD (2016) Robotic approaches may offer benefit in colorectal procedures, more controversial in other areas: a review of 168,248 cases. Surg Endosc 30:925–933 [DOI] [PubMed] [Google Scholar]
- 6.Baek NH, Li G, Kim JH, Hwang JC, Kim JH, Yoo BMKW (2015) Short-term surgical outcomes and experience with 925 patients undergoing robotic cholecystectomy during A 4-year period at a single institution. Hepatogastroenterology 62:573–576 [PubMed] [Google Scholar]
- 7.Ayloo S, Roh Y, Choudhury N (2014) Laparoscopic versus robot-assisted cholecystectomy: A retrospective cohort study. Int J Surg 12:1077–1081 [DOI] [PubMed] [Google Scholar]
- 8.Breitenstein S, Nocito A, Puhan M, Held U, Weber M, Clavien PA (2008) Roboticassisted versus laparoscopic cholecystectomy: Outcome and cost analyses of a casematched control study. Ann Surg 247:987–993 [DOI] [PubMed] [Google Scholar]
- 9.Zhou HX, Guo YH, Yu XF, Bao SY, Liu JL, Zhang Y, Ren YG (2006) Zeus robotassisted laparoscopic cholecystectomy in comparison with conventional laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int 5:115–118 [PubMed] [Google Scholar]
- 10.Vidovszky TJ, Smith W, Ghosh J, Ali MR (2006) Robotic Cholecystectomy: Learning Curve, Advantages, and Limitations. J Surg Res 36:172–178 [DOI] [PubMed] [Google Scholar]
- 11.Pietrabissa A, Pugliese L, Vinci A, Peri A, Tinozzi FP, Cavazzi E, Pellegrino E, Klersy C (2016) Short-term outcomes of single-site robotic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective, randomized, double-blind trial. Surg Endosc 30:3089–3097 [DOI] [PubMed] [Google Scholar]
- 12.Gangemi A, Danilkowicz R, Elli FE, Bianco F, Masrur M, Giulianotti PC (2017) Could ICG aided robotic cholecystectomy reduce the rate of open conversion reported with laparoscopic approach? A head to head comparison of the largest single institution studies. J Robot Surg 11(1):77–82. doi: 10.1007/s11701-016-0624-6 [DOI] [PubMed] [Google Scholar]
- 13.Strosberg DS, Nguyen MC, Muscarella P, Narula VK (2017) A retrospective comparison of robotic cholecystectomy versus laparoscopic cholecystectomy: operative outcomes and cost analysis. Surg Endosc Other Interv Tech 31:1436–1441 [DOI] [PubMed] [Google Scholar]
- 14.Rosemurgy A, Ryan C, Klein R, Sukharamwala P, Wood T, Ross S (2015) Does the cost of robotic cholecystectomy translate to a financial burden? Surg Endosc 29:2115–2120 [DOI] [PubMed] [Google Scholar]
- 15.Casillas MA, Leichtle SW, Wahl WL, Lampman RM, Welch KB, Wellock T, Madden EB, Cleary RK (2014) Improved perioperative and short-term outcomes of robotic versus conventional laparoscopic colorectal operations. Am J Surg 208:33–40 [DOI] [PubMed] [Google Scholar]
- 16.Lin S, Jiang H-G, Chen Z-H, Zhou S-Y, Liu X-S, Yu J-R (2011) Meta-analysis of robotic and laparoscopic surgery for treatment of rectal cancer. World J Gastroenterol 17:5214–5220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, Tomioka H, Mori K (2015) Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc. 29:1679–1685 [DOI] [PubMed] [Google Scholar]


