Abstract
Suicide is a leading cause of adolescent death. Recent data support the efficacy of cognitive-behavioral treatments with strong family components for reducing suicide risk; however, not all youth benefit from current interventions. Identifying predictors of treatment response can inform treatment selection and optimize benefits. This study examines predictors of response to a DBT-informed cognitive-behavioral family treatment (SAFETY), among 50 youth with recent suicide attempts/self-harm. Youth and parents were assessed at baseline and post-treatment. Results indicated medium to large effect sizes for SAFETY on youth suicidal behavior (SB; defined as suicide attempts, aborted attempts, and planning), depression, hopelessness, social adjustment, and parental depression. Classification tree analysis, with a correct classification rate of 93.3%, and follow-up logistic analyses indicated that 35% of youths reporting active SB at baseline reported active SB at post-treatment, whereas post-treatment SB was rare among youths whose active suicidality had resolved by the baseline assessment (5%). Among youths reporting baseline SB, those endorsing sleep problems were more likely to report post-treatment SB (53%) versus those without sleep problems (0%). These findings highlight the potential value of personalized treatment approaches based on pre-treatment characteristics and the significance of baseline SB and sleep problems for predicting treatment response.
INTRODUCTION
In the United States, suicide is the second leading cause of death in adolescents and young adults, with rates rising from 1999 to 2014 (Curtin, Warner, & Hedegaard, 2016). This alarming increase in deaths paired with even higher rates of non-fatal suicide attempts (SAs) and non-suicidal self-injury (NSSI) in youth (CDC, 2015) underscore the pressing need for empirically supported treatments for adolescent suicidality and self-harm (SH).
Despite limited evidence on effective treatments for suicidality and SH in youth, recent data support the efficacy of cognitive-behavioral treatments with strong family components for reducing SA risk (Ougrin, Tranah, Stahl, Moran, & Asarnow, 2015; Iyengar et al., 2018). Integrated cognitive-behavioral therapy (I-CBT; Esposito-Smythers, Spirito, Kahler, Hunt, & Monti, 2011) for adolescents with comorbid suicidality and substance abuse, was associated with a lower SA rate compared to treatment as usual (TAU). SAFETY, a DBT-informed cognitive-behavioral family treatment, has also been shown to reduce SA risk over time and lower rates of SAs, compared to TAU (Asarnow, Hughes, Babeva, & Sugar, 2017). Both I-CBT and SAFETY use a two-therapist model, with one therapist working with youth and the other with parent/family. Both treatments were also associated with significantly fewer suicide-related/psychiatric ED visits and hospitalizations, relative to TAU. Dialectical behavior therapy (DBT) was shown to be superior to active comparator conditions in reducing SH (SAs and NSSI) in two independent studies with adolescents (Mehlum et al., 2014; McCauley et al., 2018), and in reducing SAs in one study (McCauley et al., 2018). Other treatments have been shown to reduce overall SH, suicidal ideation (SI), and overall suicidality in randomized controlled trials (RCTs) and non-randomized trials (Ougrin et al., 2015; Iyengar et al., 2018).
Given that not all youth benefit from current interventions for adolescent SH, identifying predictors of treatment response is important for both: 1) refining existing treatments; and 2) personalizing treatment, such that youths and families are matched to intervention strategies that are most likely to yield strong benefits. To date, however, minimal research has focused on understanding predictors of response to treatments for SH. Indeed, to our knowledge, there are no published studies on predictors of treatment response to skills-based interventions for suicidality/SH or to interventions with a family focus. However, some trials have evaluated predictors in depressed, suicidal adolescents. Collectively, these studies document that both youth (depression, current and past suicidality, substance use) and parental characteristics/family factors (parental functioning, conflict, lack of cohesion) are likely to simultaneously influence the outcomes of youth with suicidality receiving psychosocial and/or medication treatments. Specifically, results of the Treatment of Adolescent Suicide Attempters (TASA) study, a non-randomized trial where youths received CBT, medication, or both, indicate that suicidal events (SAs or SI requiring emergency referral) were predicted by a range of variables with the most parsimonious set of predictors being family income, history of sexual abuse, and lower lethality of previous attempts (Brent et al., 2009). In the Treatment of Resistant Depression in Adolescents (TORDIA), where almost half of youth reported SH at baseline (47.4%), the strongest predictors of time to SAs during the 24 weeks of treatment were history of NSSI and self-reported hopelessness (Asarnow et al., 2011). Finally, in a trial evaluating multi-systemic therapy (MST) for youths with SH presenting for emergency psychiatric hospitalization, predictors of response, defined as SH during the one-year follow-up period, included: female gender, youth depression, caregiver distress, caregiver history of psychiatric hospitalization, and parental control (Huey et al., 2005). None of these studies showed evidence that treatment type affected observed predictive relationships.
Less well-studied possible predictors of response to treatments for suicidality/SH are sleep problems, which have been identified as potential warning signs of acute suicide death risk and are documented predictors of SAs in adolescents (Goldstein, Bridge, & Brent, 2008; Wong & Bower, 2012), with affect dysregulation a likely mediator of the association between sleep and suicidality (Ward-Ciesielski, Winer, Drapeau, & Nadorff, 2018). Sleep difficulties are also associated with problems in attention, memory, and learning (Beebe, Field, Miller, Miller, & LeBlond, 2017). This suggests that difficulty sleeping may hinder the ability to benefit from skills-based treatments such as SAFETY, where a putative treatment mechanism is skill acquisition.
The current study focuses on treatment response among youths receiving the SAFETY treatment. We report outcomes across both phases of our treatment development process, hypothesizing that treatment effects observed in reducing youth SB, depression, and hopelessness; and improvements in youth social functioning would be in the medium-to-large range in both the first and second-phase samples, and the full combined sample. Next, we examined baseline predictors of treatment response. In this sample of youths selected for the presence of recent SAs or SH, treatment response was defined as the absence of active SB (SAs, aborted SAs, planning) at post-treatment. Potential predictors were selected based on the prior literature and included sociodemographic, clinical, and family/environmental variables. Because no prior studies have evaluated baseline predictors of family-based skills training interventions for youths with suicidality/SH, we limited a priori predictions and tested the hypotheses that SB at end of treatment would be predicted by baseline: 1) levels of suicidal behavior; and 2) sleep problems.
METHODS
Participants and Procedures
Participants included 50 youths receiving the SAFETY intervention drawn from two previously published trials: 1) all 30 participants from an initial open trial (Asarnow et al., 2015); and 2) all 20 participants receiving SAFETY in a small RCT (Asarnow et al., 2017; 22 participants receiving the comparator treatment were excluded). Youths were recruited through: the ED (n=20); inpatient/partial hospitalization programs (n=18); and outpatient programs (n=12). Inclusion criteria were: age 11–18 years; an SA within 3 months of presentation (defined as an intentional self-injury with some intent to die) or NSSI as the primary problem and ≥ 3 NSSI episodes, one of which occurred within 3 months of presentation. Youth with repetitive SH but no SAs were included in the RCT sample given evidence that NSSI, separately from past SAs, is a strong predictor of future SAs (Asarnow et al., 2011; Wilkinson et al., 2011). Exclusion criteria were: no contact information for follow-up; unstable family living situation (e.g., planning out-of-home placement); and other symptoms/factors interfering with participation (e.g., psychosis).
Participants provided written informed consent/assent according to local IRB regulations. Detailed descriptions of methods are provided elsewhere (Asarnow et al., 2015; 2017), consequently we provide a brief overview focusing on measures used in this study.
The SAFETY Treatment
SAFETY (Asarnow et al., 2015), a time-limited, DBT-informed cognitive-behavioral treatment, is designed to address challenges in treating adolescents with SA/SH. In line with the Interpersonal–Psychological Theory of Suicidal Behavior (Joiner, 2005), SAFETY is a family-centered treatment. It specifically targets adolescents’ perceptions of burdensomeness and social alienation by including work with parents and the family together to strengthen support and feelings of connection. SAFETY utilizes a two-therapist model, with one therapist working with parent(s)/caregiver(s), and the other therapist with youth. Each therapeutic contact typically consists of simultaneous individual work with youth and parent(s), followed by joint family session time to practice skills and address identified issues. Due to the heterogeneity in pathways to SAs/SH, SAFETY is guided by a detailed cognitive-behavioral fit analysis (CBFA) which identifies: 1) the chain of triggering events; 2) proximal cognitive, behavioral, emotional, and environmental processes/reactions leading to the target SA/SH; 3) potential protective processes; and 4) consequences of the SA/SH. Treatment targets are thoughtfully and collaboratively chosen based on risk and protective processes identified through the CBFA and addressed using selected treatment modules such as: helpful thoughts; problem-solving; emotion regulation, active listening/validation; creating a “hope box” (containing reminders of reasons for living/cues for the safety plan), and a family album. Treatment is also generally organized around a SAFETY pyramid encompassing: 1) SAFE SETTINGS – restricting access to lethal means and attending to risk and protective factors across settings (home, school, peers, community); 2) increasing time spent with SAFE PEOPLE; 3) encouraging SAFE ACTIVITIES AND ACTIONS; 4) SAFE THOUGHTS; and 5) SAFE STRESS REACTIONS. This results in an individually-tailored yet principle-guided approach addressing the unique strengths and challenges of each youth/family, while also maintaining core features across participants. Lastly, because treatment benefits often diminish over time and 12 weeks may be too short to address the full needs of high suicide-risk patients, a critical intervention component is linkage to follow-up care as needed at end of treatment. [For a more detailed description of SAFETY, please see Asarnow et al., 2015, 2017; & Hughes et al., in press].
Assessment
Baseline and post-treatment assessments were conducted with adolescents and their primary caretaking parent, typically mothers (80%). Assessors were naive to treatment condition.
Measures.
Suicidal Ideation & Behavior.
Suicidality during the month prior to the assessment was assessed using the 17-item self-report Harkavy Asnis Suicide Survey (HASS; Harkavy-Friedman & Asnis, 1989). HASS items are rated on a 5-point Likert scale ranging from 0 (never) to 4 (most or all of the time). The SB scale, used as the primary outcome for this study, includes two items assessing SA behavior (SAs and aborted SAs) plus a suicide planning item previously shown to be the strongest predictor of SAs among the HASS items, correctly identifying 84% of youths with SAs or aborted SAs (Asarnow, McArthur, Hughes, & Berk, 2012). Additionally, the HASS yields a total score (0 to 68) and scores for Passive Suicidal Ideation (PSI) and Active Suicidal Behavior and Ideation (ASBI). Because the distribution of the HASS items is highly skewed, as in prior work, scores on the HASS SB Scale were dichotomized, with any non-zero score indicative of suicidal behavior (Asarnow et al., 2012). Internal consistency for all HASS scales was high: Total Score α = 0.94; SB scale α = 0.76; Passive SI α = 0.93; ASBI α = 0.83.
Clinical, Family/Environmental, & Socio-Demographic Variables.
Depressive disorders were assessed using the Diagnostic Interview Schedule for Children & Adolescents (NIMH DISC-IV), a computerized interviewer-administered structured diagnostic interview with adequate inter-rater and test-retest reliability (Shaffer et al., 2000). The Center for Epidemiological Studies-Depression Scale (CES-D; Radloff, 1977) assessed youth and parent depressive symptoms. Youth and parent hopelessness was measured with the Beck Hopelessness Scale (BHS; Beck & Steer, 1988). The 4-item Primary Care PTSD screen (PC-PTSD; Prins et al., 2003) assessed youth PTSD symptoms, with ≥ three items endorsed considered a positive screen. Youth externalizing and internalizing symptoms as well as overall functioning were assessed using the Achenbach Youth Self-Report (YSR) and parent-completed Child Behavior Checklist (CBCL) measures (Achenbach & Rescorla, 2001). Sleep problems were assessed through self-report using YSR item #100. The Social Adjustment Scale-Self Report for Youth (SAS-SR; Weissman, Orvaschel, & Padian, 1980) assessed overall social functioning based on four areas – at school; with peers; with family; and during spare time. The Conflict Behavior Questionnaire – Adolescent Version (CBQ; Robin & Foster, 1989) assessed youth-reported parent-child conflict. Youth report was used to assess age, gender, race, Hispanic/Latino identification, ethnicity, and sexual preference. Income was reported by parents.
Primary Outcome Measure:
The primary study outcome was the dichotomized HASS SB scale indicating the presence versus absence of SAs, aborted SAs, and SA planning at end of treatment.
Statistical Analysis.
First, we report data pre- and post the SAFETY intervention for a core set of suicidality, depression, and social functioning variables using standard descriptive statistics (Kraemer, Mintz, Noda, Tinklenberg, & Yesavge, 2006). Effect sizes are reported using Cohen’s d, calculated as the mean change from baseline to end of treatment divided by the pooled estimate of the standard deviation. Values of 0.30, 0.50, and 0.80 are considered small, medium, and large respectively (Cohen, 1988). Second, we use a classification tree analysis to identify those variables that separate: (a) treatment responders and non-responders, operationalized as those with presence versus absence of SB on the HASS-SB scale at the post-treatment assessment. Classification trees use binary recursive partitioning to identify the predictors that best separate subjects into subgroups that are homogenous with respect to a categorical outcome variable (Brieman, Friedman, Stone, & Olshen, 1984). The first split identifies the predictor and cut-off value that best divides the full sample space, or parent node, into two subregions, or daughter nodes, that are as pure as possible in terms of the outcome (in this case, presence of SB) for the corresponding subjects, thus improving the classification error rate. For continuous predictors, the algorithm looks at all possible thresholds for dividing the data space on high versus low values. For categorical predictors, the algorithm considers all possible divisions of the variable values into two groups. This splitting process is repeated for each daughter nodes until predictive accuracy cannot be further improved or nodes become too small. Each of the resulting terminal nodes is labeled according to the most common outcome value of the subjects it contains. Individuals (both new subjects and those in the original data set) are then classified according to the terminal node associated with their covariate values. Cross-validated error rates (calculated by sequentially excluding subsets of the data, re-growing the tree, and then classifying the held-out subjects to get an unbiased estimate of the prediction accuracy for new subjects) are used to evaluate the stability of the resulting trees. Recursive partitioning methods are particularly useful for identifying complex interactions among predictors in a data-driven manner; handle multicollinearity, missing data, and large pools of potential covariates well; are invariant to transformations or distributional properties of the predictor variables; and provide easily interpretable clinical decision-making rules. These advantages make classification trees an attractive alternative to logistic regression and have led to these methods gaining popularity in the health sciences (Zhang & Singer, 1999).
The variable pool for the classification tree analysis was selected from the main domains suggested by prior research, eliminating redundant variables. It included: demographic factors (age, gender, Caucasian vs. racial/ethnic minority status, income, heterosexual vs. other); baseline SB status; clinical measures (depression, hopelessness, PTSD, clinically significant elevation on the YSR and CBCL internalizing, externalizing, and total behavior problem scales); self-reported sleep problems (YSR); youth self-reported stress; and family characteristics (parental depression, family conflict, parent hopelessness).
To further evaluate the significance of the predictors identified by the classification tree algorithm and to obtain effect size estimates on the odds ratio scale, we fit follow-up logistic regression models corresponding to the successive splits in our tree model. Specifically, we used Firth regression, a penalized method, which minimizes overfitting in small samples. Analyses were conducted using STATA v15 (StataCorp, 2017), except for the classification tree analysis, which was conducted using the package rpart (Therneau & Atkinson, 2012) in the R software environment (R Core Team, 2011).
RESULTS
Baseline participant characteristics are presented in Table 1. As expected, youths were predominantly female (90.0%), with a mean age of 15.19 years (SD 1.62 years, range 11.92 to 17.75). The ethnic and racial makeup of the sample was diverse, with 30.0% endorsing Hispanic/Latino ethnicity, and 50.0% endorsing other than White/Caucasian race. Twenty-two percent endorsed non-heterosexual/questioning orientation. Families varied in income levels, with 50.0% reporting annual incomes ≥ $75,000. Most (98.0%) had health insurance. History of foster home placement was rare (2.0%). At baseline, 78.0% of the sample reported SAs within the past 3 months, while 22.0% reported only NSSI during the past 3 months. Lifetime SAs were reported by 84.0% of the sample, with 62.0% reporting multiple lifetime SAs (range: 2–6). Over half of youths, 56.0%, reported both lifetime SAs and NSSI. Sixty percent (60.0%) of youth had recent histories of hospitalization (past 3-months), and 60.0% had past 3-month ED visits. Most youths (64.0%) had mental health treatment within the prior 6-months. At baseline, 38.0% of youths met past-year criteria for major depressive disorder on the DISC-IV (youth-report), 64.0% met DISC criteria for either major depression or intermediate major depression (sub-syndromal but significant symptoms associated with impairment in functioning), and 68.0% reported severe current depressive symptoms on the CES-D (Total Score ≥ 24). As expected, youths presented with a range of symptoms/problems, with 32.0% screening positive for PTSD. Clinically elevated levels of externalizing behavior problems were identified in over a third of youths (42.0% youth YSR; 34.0% parent CBCL). Parental depression was common, with clinically elevated levels reported in 62.0% of the sample. Youths in phase 1 and 2 were similar with the only statistically significant between-group differences stemming from the broader study inclusion criteria in phase 2, specifically: phase 1 youths were significantly more likely than phase 2 youths to present with recent SAs (past 3-months) (Fischer’s Exact Test, p<0.001) and lifetime SA histories (Fischer’s Exact Test, p=0.005), whereas phase 2 youths were more likely to report recent NSSI (Fischer’s Exact Test, p=0.042).
Table 1.
Description of Sample at Baseline: Comparison of Demographic & Other Characteristics Across Phase
| Total SAFETY (n=50) | SAFETY Ph1(n=30) | SAFETY Ph2 (n=20) | |
|---|---|---|---|
| Demographic Characteristics | |||
| Age in years, Mean (SD) Age, years | 15.19±1.62 | 15.47±1.36 | 14.76±1.91 |
| Female sex | 45 (90.0%) | 27(90.0%) | 18 (90.0%) |
| Non-heterosexual Orientation | 11 (22.0%) | 6 (20.0%) | 5 (25.0%) |
| Non-Caucasian (Racial/Ethnic Minority) | 25 (50.0%) | 19 (63.3%) | 6 (30.0%) |
| Hispanic/Latino | 15 (30.0%) | 11 (36.7%) | 4 (20.0%) |
| Family annual income | |||
| Less than $29,999 | 5 (10.0%) | 3 (10.0%) | 2 (10.0%) |
| $30,000 to $74,999 | 17 (34.0%) | 9 (30.0%) | 8 (40.0%) |
| $75,000 or more | 25 (50.0%) | 16 (53.3%) | 9 (45.0%) |
| Youth Clinical Variables | |||
| SA/NSSI Status - Past 3 mos | |||
| SA only | 22 (44.0%) | 17 (56.7%) | 5 (25.0%) |
| NSSI only | 11 (22.0%) | 1 (3.3%) | 10 (50.0%) |
| SA + NSSI | 17 (34.0%) | 12 (40.0%) | 5 (25.0%) |
| SA/NSSI Status - Lifetime | |||
| SA only | 14 (28.0%) | 11 (36.7%) | 3 (15.0%) |
| NSSI only | 8 (16.0%) | 1 (3.3%) | 7 (35.0%) |
| SA + NSSI | 28 (56.0%) | 18 (60.0%) | 10 (50.0%) |
| Youth, Major Depressive Disorder (DISC) | 19 (38.0%) | 11 (36.7%) | 8 (40.0%) |
| CES-D in severe range (CES-D ≥ 24) | 34 (68.0%) | 20 (66.7%) | 14 (70.0%) |
| PTSD, # symptoms | 1.64±1.50 | 1.72±1.41 | 1.50±1.65 |
| YSR Internalizing Behavior, Clinical Range | 30 (60.0%) | 17 (56.7%) | 13 (65.0%) |
| YSR Externalizing Behavior, Clinical Range | 21 (42.0%) | 14 (46.7%) | 7 (35.0%) |
| YSR Total Problems, Clinical Range | 29 (58.0%) | 17 (56.7%) | 12 (60.0%) |
| CBCL Internalizing Behavior, Clinical Range | 27 (54.0%) | 14 (46.7%) | 13 (65.0%) |
| CBCL Externalizing Behavior, Clinical Range | 17 (34.0%) | 12 (40.0%) | 5 (25.0%) |
| CBCL Total Problems, Clinical Range | 29 (58.0%) | 17 (56.7%) | 12 (60.0%) |
| Service Use Variables (Parent-report) | |||
| Medication treatment in last 6 mos | 18 (36.0%) | 9 (30.0%) | 9 (45.0%) |
| Mental Health treatment in last 6 mos | 32 (64.0%) | 16 (53.3%) | 16 (80.0%) |
| Family & Environmental Variables | |||
| Parent CES-D, Clinical Range ≥16 | 31 (62.0%) | 17 (56.7%) | 13 (65.0%) |
| Number of life stresses (Past 6 mos) | 4.24±2.20 | 4.30±2.28 | 4.15±2.13 |
| Conflict Behavior Questionnaire | 8.11±5.87 | 9.07±6.26 | 6.71±5.08 |
Data are presented as Mean±SD for continuous variables, N (%) for dichotomous variables, missing data results in variation in N across variables.
Notes: Phase 1 sample includes only youth in open trial (N=30); previous publication (Asarnow et al.,2015) included 5 youths from RCT resulting in N=35.
CBCL/YSR: Clinical range defined as T >64 for broadband scales.
Participation in the post-treatment assessment was high (90%). Four of the five assessment non-responders had dropped out of treatment. Assessment responders were similar to non-responders on baseline measures, with the exception of higher scores on parent-reported internalizing, externalizing, and total problems (as measured by the CBCL). These variables were not associated with baseline suicidality for the entire sample (n=50) or with suicidality at post-treatment for the assessment completers (n=45), suggesting that our findings should not be biased by differential non-response related to the outcomes of interest. To be conservative, these measures were included in the variable pool for the tree-based analysis in case they were important for subsets of the target population.
SAFETY Treatment Received.
Youths received a mean of 9.34 sessions (SD 4.09), with a median of 10 sessions. Parents attended a mean of 8.18 sessions (SD 4.12), and a mean of 8.92 family sessions (SD 3.80) were conducted. Mean number of sessions was similar in Phases 1 and 2 for youth [M1=8.34, SD1 4.76; M2=9.90, SD2 2.95; t(47)=1.38, p=.18], parent [M1=7.69, SD1 4.56; M2=7.85, SD2 3.48; t(47)=0.13, p=.90], and family sessions [M1=8.31, SD1 4.34; M2=9.05, SD2 2.98; t(47)=0.72, p=.48].
Outcomes/Effect Sizes
At follow-up, statistically significant improvements were seen on measures of SB and SI, youth depression and hopelessness, youth social adjustment, and parent depression and hopelessness (see Table 2). Effect sizes were in the medium-to-large range, both overall and in the two subsamples, with the exception of the HASS PSI scale which declined significantly only in the combined and phase 2 samples. In addition to decreases in the mean scores, the variance of the HASS and CES-D scores tended to decrease at follow-up, suggesting that youth became more homogenous in their scores on these measures with fewer youths showing high levels of symptoms.
Table 2.
SAFETY Outcomes: Effect Sizes Across Phase
| Phase 1 (N=26) | Phase 2 (N=19) | Total Sample (N=45) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Paired Mean Difference | p value | Cohen’s d | Paired Mean Difference | p value | Cohen’s d | Paired Mean Difference | p value | Cohen’s d | |
| HASS Scores | |||||||||
| SB | 1.35 (2.91) | .027 | .59 | 1.26 (1.94) | .011 | .92 | 1.31 (2.52) | .001 | .66 |
| ASB | 2.19 (4.80) | .028 | .57 | 2.89 (3.67) | .003 | 1.05 | 2.49 (4.32) | .000 | .73 |
| PSI | 2.62 (8.06) | .111 | .25 | 11.42 (11.59) | .000 | 1.46 | 6.33 (10.54) | .000 | .65 |
| TOTAL | 4.45 (12.29) | .077 | .32 | 14.32 (14.66) | .000 | 1.43 | 8.62 (14.07) | .000 | .68 |
| Youth CES-D | 14.53 (10.49) | .000 | 1.24 | 17.00 (13.61) | .000 | 1.55 | 15.59 (11.85) | .000 | 1.38 |
| Youth BHS | 4.67 (5.05) | .000 | .91 | 6.42 (6.40) | .000 | 1.00 | 5.41 (5.66) | .000 | 1.00 |
| Parent CES-D | 6.29 (11.05) | .010 | .60 | 9.47 (10.70) | .002 | .96 | 7.65 (10.89) | .000 | .76 |
| Parent BHS | .99 (3.89) | .26 | .23 | 1.49 (3.58) | .087 | .38 | 1.23 (3.71) | .043 | .30 |
| SAS Scales | |||||||||
| Total (No school) | 9.46 (8.93) | .000 | 1.23 | 11.14 (10.49) | .000 | 1.20 | 10.17 (9.54) | .000 | 1.22 |
| School | 3.27 (4.23) | .002 | .79 | 3.67 (6.37) | .026 | .85 | 3.45 (5.23) | .000 | 0.82 |
| Peer | 3.92 (4.18) | .000 | .98 | 5.74 (5.87) | .000 | 1.00 | 4.69 (4.99) | .000 | 0.98 |
| Family | 2.38 (4.61) | .014 | .68 | 3.58 (4.79) | .004 | .81 | 2.89 (4.67) | .000 | 0.79 |
| Spare Time | .81 (1.63) | .018 | .49 | .26 (2.00) | .573 | .15 | .58 (1.79) | .036 | 0.34 |
Predicting Treatment Response: Suicidal Behavior
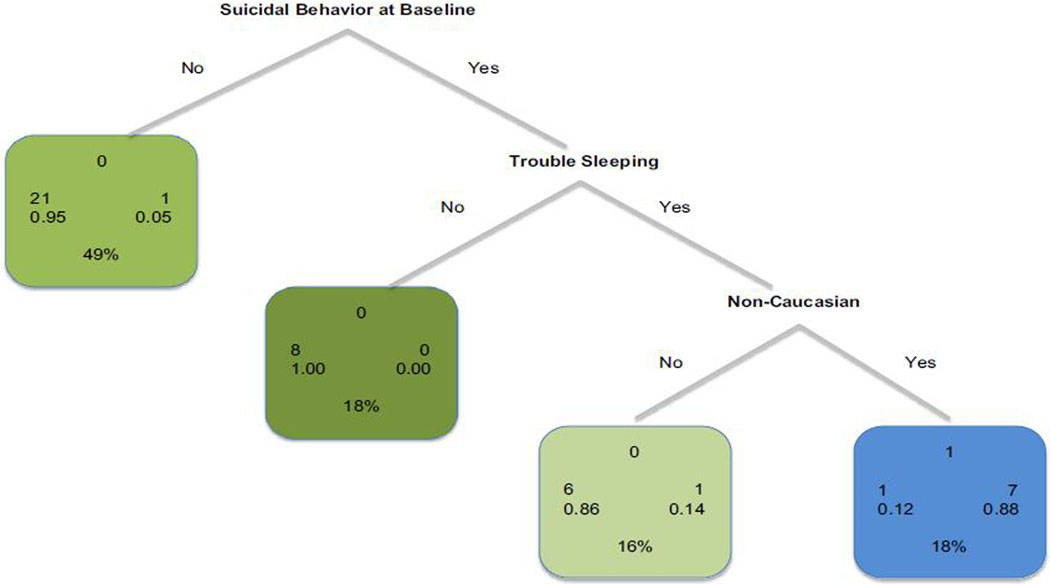
Inter-correlations between predictors included in the classification tree variable pool are presented in Table 3. The model that emerged from the SB classification tree analysis (Figure 1) had 3 nodes, an overall correct classification rate of 93.3%, and a relative error rate of 0.33. Among youths reporting no baseline SB, post-treatment SB was rare, 5% (1/22). In contrast, SB was more common among youths with baseline SB; 35% (8/23) of youths with baseline SB continued to report SB at post-treatment. Within the group of youths reporting baseline SB, those endorsing sleep problems (YSR Q100>0) were more likely to report SB at follow-up, 53% (8/15), while none of the youths (0/8) without sleep problems reported SB at post-treatment. Among youths with baseline SB and sleep problems, those endorsing racial/ethnic minority status (i.e., any race/ethnicity other than Caucasian including Hispanic, African-American, American-Indian/Alaskan native, Asian) were more likely to report SB at follow-up [88% (7/8)], as compared to Caucasian youths [14% (1/7)].
Table 3.
Correlations among Predictor Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | |||||||||||||||||||||||
| 1. Age | |||||||||||||||||||||||
| 2. Caucasian (Yes/No) | .06 | ||||||||||||||||||||||
| 3. Sexual Preference | .06 | −.03 | |||||||||||||||||||||
| 4. Income | −.04 | .25 | .22 | ||||||||||||||||||||
| Youth-Report Measures | |||||||||||||||||||||||
| 5. Sleep Problems (YSR item 100) | −.04 | .05 | −.29* | .07 | |||||||||||||||||||
| 6. Hopelessness Total Score | .18 | .15 | −.16 | .03 | .57** | ||||||||||||||||||
| 7. CBQ Total Score | .29* | −.07 | −.22 | .06 | −.11 | .09 | |||||||||||||||||
| 8. CESD ≥ 24 | .08 | −.03 | .00 | −.02 | .26 | .43** | .09 | ||||||||||||||||
| 9. DUSI Total Score | .40* | −.22 | −.10 | −.20 | .18 | .19 | .13 | −.05 | |||||||||||||||
| 10. YSR Externalizing, Clinical Range | .19 | .04 | −.16 | −.03 | .11 | .12 | .28 | .13 | .39** | ||||||||||||||
| 11. YSR Internalizing, Clinical Range | .27 | .00 | −.21 | −.11 | .45** | .67** | .09 | .44 | .30* | .12 | |||||||||||||
| 12. YSR Total Problems, Clinical Range | .11 | −.04 | −.36 | −.26 | .45** | .56** | .08 | .23 | .38* | .48 | .63 | ||||||||||||
| 13. PTSD Screen Total Score | .13 | .12 | −.17 | −.18 | .39** | .34* | −.08 | .24 | .23 | .28 | .21 | .20 | |||||||||||
| 14. SAS-SR Total Score (without school) | −.01 | .01 | −.14 | −.06 | .30* | .15 | .29* | .31* | .33* | .38** | .49** | .61** | .36* | ||||||||||
| 15. SAS-SR School Subscale | −.10 | .07 | .09 | .12 | .20 | .51** | .16 | .33* | −.03 | .18 | .36* | .40** | −.11 | .46** | |||||||||
| 16. SAS-SR Peer Subscale | −.01 | .00 | −.08 | .08 | .42** | .40** | .04 | .41** | .21 | .18 | .51** | .58** | .25 | .85** | .43* | ||||||||
| 17. SAS-SR Family Subscale | .25 | −.01 | −.30* | −.09 | .07 | .52** | .52** | .02 | .33* | .40** | .28 | .45** | .33* | .71** | .23 | .35* | |||||||
| 18. Stress Total Score | .44** | −.09 | .10 | .06 | .00 | .09 | .14 | .08 | .18 | .28 | .18 | .08 | .22 | .30* | .09 | .17 | .44** | ||||||
| Parent-Report Measures | |||||||||||||||||||||||
| 19. Parent Hopelessness Total Score | −.08 | −.09 | −.11 | −.17 | −.11 | .15 | −.17 | .15 | −.03 | −.02 | .01 | .17 | .10 | −.12 | .13 | −.01 | −.07 | .05 | |||||
| 20. Parent CESD ≥ 16 | −.04 | −.01 | −.18 | −.32 | .16 | .11 | −.12 | .28 | −.12 | .04 | .06 | .20 | .11 | .00 | −.03 | .15 | .03 | .01 | .46** | ||||
| 21. CBCL Internalizing, Clinical Range | −.27 | .04 | .03 | −.09 | .27 | .36** | −.16 | .09 | .03 | −.03 | .23 | .35 | .09 | .11 | .37* | .26 | −.10 | −.21 | .45** | .14 | |||
| 22. CBCL Externalizing, Clinical Range | −.02 | −.13 | .05 | −.05 | −.07 | −.22 | .25 | .11 | .15 | .42 | −.02 | .01 | −.03 | −.01 | .16 | −.07 | −.06 | −.06 | −.19 | −.18 | .15 | ||
| 23. CBCL Total Problems, Clinical Range | −.06 | −.04 | .10 | .09 | .17 | .08 | −.09 | .05 | .20 | .23 | −.03 | .18 | .06 | .08 | .35* | .19 | −.06 | .00 | .28 | .11 | .68 | .35 |
Notes:
p < .05;
p < .01
Figure 1.
Classification Tree Predicting Suicidal Behavior at Post-Treatment.
Consistent with results of the classification tree, penalized likelihood (firth) logistic regression analyses examining baseline predictors of post-treatment SB indicated a significantly higher odds of SB at post-treatment among youths with baseline SB, OR=7.86 (95% CI: 1.23 – 50.22), p=.03. Of note, the confidence interval is wide due to the small sample size and the low rates of past-month SB at the end of treatment. Indeed, 21 out of 22 (95.5%) youths reporting no past-month baseline SB continued to report no SB at post-treatment. This makes the exact estimate of the odds ratio somewhat unstable, although the difference in rates between the groups is striking even given the sample sizes. To complement the results of the tree-based analysis, penalized likelihood logistic analyses predicting treatment response were conducted within the subgroup of 23 youths who reported SB at the baseline assessment. Results indicated that presence of sleep problems was associated with higher odds of SB at post-treatment (OR = 3.57, 95% CI: 1.06–12.00, p =.04). Racial/ethnic minority status was also significantly associated with increased odds of SB, with a significant effect for non-Caucasian identification (OR = 10.00, 95% CI: 1.25–71.43, p =.03) as well as for Hispanic ethnicity (OR = 8.49, 95% CI: 1.27–56.84, p =.03).
As a sensitivity/stability analysis, we explored the cross-validated error rate, which provides an estimate of the predictive accuracy of the obtained tree for new subjects. If the splits represent real predictive improvement, then the cross-validated error rate should go down. Due to the small sample size, however, the cross-validated estimate of the error rate associated with each split was itself somewhat variable. In the majority of the classification tree model runs, the cross-validation error improved from the root node to the final node in the tree. These results are compelling because the selected variables were the ones that were a priori expected to be the most important, and the estimated effects derived from the logistic regression analyses based on the tree are clinically meaningful, with unadjusted p values reaching alpha <.05.
DISCUSSION
This study provides data from two samples indicating medium-to-large effect sizes for the SAFETY treatment on measures of youth SB, depression, hopelessness, and social adjustment in the domains of school, home, and with peers, as well as a large effect size for parental depression. These effect sizes, observed in two independent samples, support the benefits of SAFETY, although future research is needed to evaluate these effect sizes relative to comparator conditions.
The main objective of this study was to examine predictors of response to SAFETY, a DBT-informed cognitive-behavioral family treatment. Development of evidence-based algorithms to help determine which adolescents are most likely to benefit from specific treatments is crucial for more effectively matching patients to interventions. It is also key for personalizing treatment approaches by modifying/supplementing them to better address the needs of the heterogeneous group of youths with suicidality and/or SH. As predicted, we found that even in this group of adolescents presenting with recent SAs/SH, nearly all (21 of 22; 95.5%) youths whose active suicidality had resolved by the point of the baseline assessment continued to report no active SB following the 3-month SAFETY treatment period. Taken together with the relatively low rate of SB at the end of SAFETY treatment, RCT data on rates of recurrent SAs in treatment as usual (e.g., 33% at 3 months; Asarnow et al., 2017), and the relatively high SB risk observed with diverse interventions (Ougrin et al., 2015), our findings suggest that SAFETY may have offered some protection from SB recurrence. However, youths with rapid remission of SB may have remained stable with other treatments or with no treatment.
As a next step in our algorithm, among teens who reported baseline SB, those suffering from sleep problems were significantly more likely to report SB at post-treatment. These findings point to sleep problems as a predictor of inadequate treatment response among youths presenting with baseline SB and add to an emerging literature pointing to weaker CBT treatment effects among youths with sleep problems (e.g., Zalta et al., 2013). Our results are also consistent with the view that sleep problems can adversely influence learning and memory thereby impeding the efficacy of skills-based treatments like SAFETY where the presumed treatment mechanism is learning new coping behaviors (Beebe et al., 2017). It is important to note causality was not tested, i.e., disrupted sleep may be a marker of poor treatment response, without having caused poor treatment response. At baseline, sleep problems were associated with other clinical variables such as PTSD symptoms, internalizing symptoms, and social adjustment problems. In other words, those reporting more sleep problems in our sample were also reporting more PTSD and internalizing symptoms as well as more social difficulties, which may have contributed to poorer treatment outcome in conjunction with or separately from sleep problems. Nevertheless, disruptions in sleep have been found to predict a variety of adverse mental health outcomes, including suicidality and SH (Wong, Brower, & Zucker, 2011); emotional lability and impulsivity (Gruber et al., 2009); depression (Sivertsen et al., 2014); and substance abuse (Johnson & Breslau, 2001). Other research also documents that sleep problems may be a proximal indicator of short-term or “imminent” risk for fatal and nonfatal SAs (Goldstein, Bridge, & Brent, 2008). Lastly, existing pilot research shows that sleep, improved through intervention, is associated with better depression treatment outcomes in adolescents (Clarke et al., 2016). If replicated, our findings that sleep problems may be a marker (or mechanism) of increased SA risk and poor treatment response have important clinical implications in terms of directly addressing sleeping difficulties when treating suicidality. Future research is needed to determine whether sleep is a modifiable risk factor in youths with severe suicide/SH risk, the impact of improved sleep on subsequent SA risk, and mechanisms contributing to observed intervention impacts.
Among youths with baseline SB and self-reported sleep problems, racial/ethnic minority youth, most of whom were Hispanic/Latino (5/8, 62.5%), experienced poorer treatment outcome compared to their Caucasian counterparts. This was an unanticipated finding needing cautious interpretation, although it is in line with studies that demonstrate more positive CBT treatment effects for Caucasian youth (e.g., Rohde, Seeley, Kaufman, Clarke, & Stice, 2006). While our results do not rule out the possibility that racial/ethnic minority status in general (rather than Hispanic ethnicity in particular) contributed to poorer outcome, our finding that this subgroup of Hispanic girls had higher SB rates post-treatment merits note in view of national surveillance data indicating that Hispanic females have the highest rate of SAs in the adolescent age range (CDC, 2015). The mixed findings in the field related to the effects of race/ethnicity on youth treatment outcome (Huey & Polo, 2008), in conjunction with our finding that racial/ethnic minority status predicted outcome only among youths with baseline SB, highlight the need for further research to clarify the impact of racial/ethnic minority status on the emergence and progression of youth suicidality and to develop optimal care strategies to address the needs of diverse racial/ethnic and cultural groups.
To our knowledge, SAFETY, which includes a strong family focus, is currently the only intervention for youth suicidality/SH demonstrating reductions in parental depression. This was an unanticipated positive finding, as parental depression is not a direct SAFETY treatment target. Consistent with prior work demonstrating that low family social support and feelings of burdensomeness predict suicidality in youth (e.g., Joiner et al., 2009; Opperman, Czyz, Gipson, & King, 2015), individual parent and family sessions focused on skills to strengthen supportive communication and the parent-child relationship (e.g., listening skills, validation, “thanks notes”). While it is possible that simply participating in individual sessions led to improvements in parental depressive symptoms, it is also possible that skills acquisition contributed to the observed improvement, particularly as the intervention model brought youth and parents together to practice skills and enhance support. The goal of active parental participation in the intervention was to increase parental protective actions, to promote feelings of family connection and belonging, and to increase the likelihood that youths turn to their parents at times of acute distress and/or when experiencing suicidal urges. Thus, increases in rewarding family interactions, improved family cohesion, or reduced parental stress due to improvements in youth suicidality may have all contributed to reduced depression in parents. While these hypothesized pathways leading to decreases in parental depression need to be investigated by future research, the demonstrated reductions are encouraging in terms of supporting youth well-being over time, as parental depression has been found to be associated with poorer youth functioning (Beardslee, Versage, & Gladstone, 1998).
Our results must be considered within the context of study limitations. Albeit diverse, the sample was relatively small and drawn from a single site, underscoring the importance of replication of our findings, including the obtained classification tree, with independent, larger, and even more diverse samples. Relatedly, our sample was predominantly female. Given known gender differences in suicide (i.e., females are more likely to attempt suicide, while males experience higher suicide mortality; WHO, 2016), future research on the SAFETY treatment program would benefit from the inclusion of a larger number of male youth, given their higher risk of suicide death. The present results focused on treatment benefits at post-treatment and were based on a within-subject design. Future work is needed to clarify the sustainability of treatment effects and whether the observed predictors are specific to SAFETY or are more general predictors of treatment response across a range of treatments. Additionally, while our results suggest mechanisms through which SAFETY led to treatment benefits, our study design did not allow for direct assessment of mediators or mechanisms of treatment action. Future work is needed to determine whether treatment mechanisms vary across youths and families, as might be expected in this intervention which was designed to address the heterogeneity in the population of suicidal and self-harming youths by targeting the unique proximal risk and protective processes identified for each youth and family. Consistent with other results indicating the strongest benefits for interventions including family treatment components for suicidal and self-harming adolescents (Ougrin et al., 2015; Iyengar et al., 2018), our finding of large treatment effects in reducing parental depression suggest the importance of further work exploring whether reduced parental depression is an important SAFETY treatment mechanism. An alternative hypothesis is that reducing parental depression through any approach (medication, psychotherapy) is sufficient for achieving reductions in adolescent SB. Finally, the study used a self-report measure of sleep quality. Our results suggest the value of more extensive sleep evaluations to supplement subjective assessments with more objective measures, such as actigraphy and sleep diaries, as well as directly targeting sleep difficulties to evaluate whether improvements in sleep lead to improved treatment outcomes in suicidal/self-harming adolescents (Kazdin, 2007).
In conclusion, identifying treatments for reducing SA-risk has been elusive, and SAFETY is one of only three treatments that have been shown in RCTs to reduce SAs in youths (Asarnow et al., 2017; Esposito-Smythers et al., 2011, McCauley et al., 2018). Our results demonstrating medium-to-large effects across our phase 1 and phase 2 samples strengthen confidence in the range of observed treatment effects and highlight the potential value of developing personalized approaches that use baseline characteristics to inform treatment strategies. Finally, our findings indicating that sleep problems are associated with reduced benefits of the SAFETY treatment, a skills-based CBT-oriented treatment, suggest the value of evaluating and addressing sleep problems when deciding upon a treatment strategy.
Acknowledgments
Research reported in this publication was supported by grants from the National Institute of Mental Health, R34 MH078082 and American Foundation for Suicide Prevention (AFSP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or AFSP. We thank the youths, families, staff, and colleagues who made this project possible, including Gabrielle Carlson, Donald Guthrie, and Mark Rappaport who served on our Data Safety & Management Board and Michele Berk who was a member of the original treatment development team.
Contributor Information
Kalina N. Babeva, Semel Institute for Neuroscience and Human Behavior, Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA 90095.
Alexandra M. Klomhaus, Fielding School of Public Health, Department of Biostatistics, University of California, Los Angeles, Los Angeles, CA 90095.
Catherine A. Sugar, Fielding School of Public Health, Department of Biostatistics, University of California, Los Angeles, Los Angeles, CA 90095.
Olivia Fitzpatrick, Semel Institute for Neuroscience and Human Behavior, Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA 90095.
Joan R. Asarnow, David Geffen School of Medicine, Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA 90095.
References
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Asarnow JR, McArthur D, Hughes JL, Barbery V, & Berk M (2012). Suicide Attempt Risk in Youths: Utility of the Harkavy-Asnis Suicide Scale for Monitoring Risk Levels. Suicide Life Threatening Behavior, 42(6), 684–698. doi: 10.1111/j.1943-278X.2012.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Berk M, Hughes JL, & Anderson NL (2015). The SAFETY Program: A Treatment-Development Trial of a Cognitive-Behavioral Family Treatment for Adolescent Suicide Attempters. Journal of Clinical Child & Adolescent Psychology, 44(1), 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Hughes JL, Babeva KN, & Sugar CA (2017). Cognitive-behavioral family treatment for suicide attempt prevention: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 56(6), 506–14. doi: 10.1016/j.jaac.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, … Brent DA (2011). Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. Journal of the American Academy of Child and Adolescent Psychiatry, 50(8), 772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, & Gladstone TRG (1998). Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent, 37(11), 1134–1141. [DOI] [PubMed] [Google Scholar]
- Beck AT, & Steer RA (1988). BHS, Beck hopelessness scale: Manual. San Antonio, Texas: Psychological Corp; Harcourt Brace Jovanovich. [Google Scholar]
- Beebe DW, Field J, Milller MM, Miller LE, & LeBlond E (2017). Impact of multi-night experimentally induced short sleep on adolescent performance in a simulated classroom. Sleep, 40(2). doi: 10.1093/sleep/zsw035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiman L, Friedman JH, Olshen RA, & Stone CJ (1984). Classification regression trees. Belmont, CA: Wadsworth. [Google Scholar]
- Brent D, Greenhill L, Compton S, Emslie G, Wells K, Walkup J, … Turner JB (2009). The Treatment of Adolescent Suicide Attempters (TASA) Study: Predictors of suicidal events in an open treatment trial. Journal of the American Academy of Child and Adolescent Psychiatry, 48(10), 987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2015). Youth Risk Behavior Survey Data. Available from: www.cdc.gov/yrbs. Accessed on December 22, 2017.
- Clarke G, McGlinchey EL, Hein K, Gullion CM, Dickerson JF, Leo MC, Harvey AG (2016). Cognitive-behavioral treatment of insomnia and depression in adolescents: A pilot randomized trial. Behavior Research Therapy, 69, 111–118. doi: 10.1016/j.brat.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Curtin SC, Warner M, & Hedegaard H (2016). Increase in suicide in the United States, 1999–2014 NCHS data brief, no 241. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, & Monti P (2011). Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized trial. Journal of Consulting and Clinical Psychology, 79(6), 728–39. doi: 10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Bridge JA, & Brent DA (2008). Sleep disturbance preceding completed suicide in adolescents. Journal of Consulting and Clinical Psychology, 76(1), 84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R, Cassoff J, Frenette S, Wiebe S, & Carrier J (2012). Impact of Sleep Extension and Restriction on Children’s Emotional Lability and Impulsivity. Pediatrics, 130(5). doi: 10.1542/peds.2012-0564. [DOI] [PubMed] [Google Scholar]
- Harkavy-Friedman JM, & Asnis GM (1989). Assessment of suicidal behavior: A new instrument. Psychiatric Annals, 19(7), 382–387. [Google Scholar]
- Huey SJ Jr., Henggeler SW, Rowland MD, Halliday-Boykins CA, Cunningham PB, & Pickrel SG (2005). Predictors of treatment response for suicidal youth referred for emergency psychiatric hospitalization. Journal of Clinical Child & Adolescent Psychology, 34(3), 582–589. doi: 10.1207/s15374424jccp3403_13. [DOI] [PubMed] [Google Scholar]
- Huey SJ Jr., & Polo AJ. (2008). Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child & Adolescent Psychology, 37(1), 262–301. doi: 10.1080/15374410701820174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JL, Babeva KN, Asarnow JR (in press, 2019). The SAFETY Program: A Youth and Family Centered Cognitive-Behavioral Intervention Informed by Dialectical Behavior Therapy In Berk MS (Ed.), Evidence-Based Treatment Approaches for Suicidal Adolescents: Translating Science into Practice. Washington DC: American Psychiatric Association Press. [Google Scholar]
- Iyengar U, Snowden N, Asarnow JR, Moran P, Tranah T, Ougrin D (2018). A Further Look at Therapeutic Interventions for Suicide Attempts and Self-Harm in Adolescents: An Updated Systematic Review of Randomized Controlled Trials. Frontiers in Psychiatry, 9: 583. doi: 10.3389/fpsyt.2018.00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE (2005). Why people die by suicide. Cambridge, MA: Harvard University Press. [Google Scholar]
- Joiner TE Jr., Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, & Rudd MD (2009). Main predictions of the interpersonal–psychological theory of suicidal behavior: Empirical tests in two samples of young adults. Journal of Abnormal Psychology, 118(3), 634–646. doi: 10.1037/a0016500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EO, & Breslau N (2001). Sleep problems and substance use in adolescence. Drug and Alcohol Dependence, 64(1), 1–7. doi: 10.1016/S0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- Kazdin A (2007). Mediators and Mechanisms of Change in Psychotherapy Research. Annual Review of Clinical Psychology, 3, 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, & Yesavge JA (2006). Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry, 63, 484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, … Linehan MM (2018). Efficacy of Dialectical Behavior Therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry, 75(8), 777–785. doi: 10.1001/jamapsychiatry.2018.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehlum L, Tormoen AJ, Ramberg M, Haga E, Diep LM, … Groholt B (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(10):1082–1091. [DOI] [PubMed] [Google Scholar]
- Opperman K, Czyz EK, Gipson PY, & King CA (2015). Connectedness and Perceived Burdensomeness among Adolescents at Elevated Suicide Risk: An Examination of the Interpersonal Theory of Suicidal Behavior. Archives of Suicide Research : Official Journal of the International Academy for Suicide Research, 19(3), 385–400. doi: 10.1080/13811118.2014.957451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, Moran P, & Asarnow JR (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 54(2), 97–107. doi: 10.1016/j.jaac.2014.10.009. [DOI] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, … F. D, Sheikh JI, (2003). The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics (PDF). Primary Care Psychiatry, 9, 9–14. doi: 10.1185/135525703125002360. [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- R Core Team (2014). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: Retrieved from: http://www.R-project.org/. [Google Scholar]
- Robin AL & Foster SL (1989). Negotiating parent-adolescent conflict: A behavioral-family systems approach. New York: Guilford Press. [Google Scholar]
- Rohde P, Seeley JR, Kaufman NK, Clarke GN, & Stice E (2006). Predicting time to recovery among depressed adolescents treated in two psychosocial group interventions. Journal of Consulting and Clinical Psychology, 74(1), 80–88. doi: 10.1037/0022-006X.74.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Harvey AG, Lunderbold AJ, & Hysing M (2014). Sleep problems and depression in adolescence: Results from a large population-based study of Norwegian adolescents aged 16–18 years. European Child and Adolescent Psychiatry, 23(8), 681–689. doi: 10.1007/s00787-013-0502-y. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- Therneau TM, & Atkinson EJ (2011). rpart: Recursive Partitioning. R package version 3.1–51. Retrieved from: http://CRAN.R-project.org/package=rpart.
- Ward-Ciesielski EF, Winer ES, Drapeau CW, & Nadorff MR (2018). Examining components of emotion regulation in relation to sleep problems and suicide risk. Journal of Affective Disorders, 241, 41–48. doi: 10.1016/j.jad.2018.07.065. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Orvaschel H, & Padian N (1980). Children’s symptom and social functioning self-report scales. Comparison of mothers’ and children’s reports. Journal of Nervous Mental Disorders, 168(2), 736–740. [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, & Goodyer I (2011). Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). American Journal of Psychiatry, 168(5), 495–501. [DOI] [PubMed] [Google Scholar]
- Wong MM & Brower KJ (2012). The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. Journal of Psychiatric Research, 46(7), 953–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, & Zucker RA (2011). Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. Journal of Psychiatric Research, 45(4), 505–511. doi: 10.1016/j.jpsychires.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2016). Suicide rate estimates, age-standardized, estimates by country. Available from: http://apps.who.int/gho/data/node.main.MHSUICIDEASDR?lang=en. Accessed on October 1, 2018.
- Zalta AK, Dowd S, Rosenfield D, Smits JAJ, Otto MW, Simon NM, … Pollack MH (2013). Sleep quality predicts treatment outcome in CBT for social anxiety disorder: Sleep quality and CBT for social anxiety. Depression and Anxiety, 30(11), 1114–1120. doi: 10.1002/da.22170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang HP & Singer B (1999). Recursive Partitioning in the Health Science. New York: Springer. [Google Scholar]