Abstract
Stigma and judgment by health workers toward people living with HIV (PLHIV) and key populations can undermine the uptake of HIV services. In 2014, we recruited health workers delivering HIV services from 21 urban communities in South Africa and Zambia participating in the first year of the HPTN 071 (PopART) cluster-randomized trial. We analyzed self-reported levels of stigma and judgment toward (1) PLHIV, (2) women who sell sex, (3) men who have sex with men (MSM), and (4) young women who become pregnant before marriage. Using logistic regression, we compared responses between three health worker cadres and explored risk factors for stigmatizing attitudes. Highest levels of stigma and judgment were in relation to women who sell sex and MSM, especially in Zambia. Heath workers did not generally think that clients should be denied services, although this was reported slightly more commonly by community health workers. Higher education levels were associated with lower judgmental beliefs, whereas higher perceptions of coworker stigmatizing behaviors toward PLHIV and each key population were associated with holding judgmental beliefs. Training experience was not associated with judgmental attitudes for any of the key populations. Our findings confirm a high prevalence of judgmental attitudes toward key population groups but lower levels in relation to PLHIV, among all cadres of health workers in both countries. Planning and implementing targeted stigma reduction interventions within health settings are critical to meet the needs of vulnerable populations that face more stigmatizing attitudes from health workers.
Keywords: HIV, stigma, health care, key populations, judgmental attitudes
Introduction
Recent successes in the treatment and management of HIV have led to declines in global HIV incidence.1 Despite this, the global HIV burden remains high, and the target of reducing incidence to fewer than 500,000 new infections by 2020 is challenging.2 An ambitious cluster randomized trial, HPTN 071 (PopART), reduced incidence in urban communities by 30% through a door-to-door HIV combination prevention approach.3 In understanding who was harder to reach through this approach, and how this might contribute to HIV incidence, it is important to consider the role of key populations, including men who have sex with men (MSM), adolescent girls and young women, and female sex workers, who are disproportionately affected by HIV.2,4 Negative attitudes and beliefs about these populations by health workers could have adverse effects on the uptake of HIV services and thereby influence HIV prevention and care.
Stigma is “the co-occurrence of labelling, stereotyping, separation, status loss, and discrimination in a context in which power is exercised.”5 Moral judgment is a common manifestation of HIV stigma.6 Stigma can act as a barrier to HIV testing and uptake of treatment,7–10 and stigma among health workers may affect service delivery.11–14 Perceived or anticipated stigma can reduce demand for services. Some clients, including key populations, may avoid accessing HIV services due to fear of being stigmatized by health workers who may talk badly about them or reveal their HIV status to others without their permission.15,16 Stronger antidiscrimination policies within health settings have been called for.17
Stigma among health workers may hinder HIV control efforts based on a universal test-and-treat (UTT) approach.18–20 In this model, HIV incidence reductions are achieved by increasing levels of diagnosis among those infected with HIV, starting treatment among those who are diagnosed as early as possible, and successfully maintaining viral suppression among those who initiate treatment.20,21 Delivering these services will involve lay and trained health workers in both facility and community settings. However, health practitioners delivering an intervention based on these principles in South Africa found that community members sometimes refrained from accessing testing due to fear of being seen entering a health facility, or fear of status disclosure by health workers after being tested.19
Fear of “being seen” was linked to demarcated HIV services, visibility and orientation of HIV service structures, particular items and distinctive client flow in the 21 health facilities that were situated in the 21 South African and Zambian communities that were part of the HPTN 071 (PopART) trial.22 Home, community-based or self-testing may overcome such health facility stigma barriers, but stigma may still act as a barrier to members of key populations.23 Indeed, stigma may affect already marginalized and disempowered populations more so than others.5 Female sex workers living with HIV in Zimbabwe reported experiencing more stigma in relation to their work than in relation to their HIV status, although their experience of discrimination by health workers was relatively low.23
Intersectional stigma has also been described among MSM in Swaziland.24 It is important to understand how layered or intersectional stigma persists among key populations. Failing to understand and address them may mean that the stigma that these populations experience, and the adverse effects of these experiences, may be underestimated and therefore be more likely to persist.
A growing body of literature seeks to understand how stigma might influence health seeking practices, and how stigma among health workers might influence these behaviors in various contexts.25–27 We set out to explore stigma and judgment toward both people living with HIV (PLHIV) and key population groups reported by health workers delivering HIV services in the 21 urban South African and Zambian communities taking part in the HPTN 071 (PopART) trial.28,29 During the first year of the study, we compared levels of stigma and judgment toward different population groups, and between different cadres of health workers, and identified risk factors for stigmatizing attitudes.
Methods
Setting
The HPTN 071 (PopART) trial was a three-arm cluster randomized trial evaluating the effectiveness of the PopART combination HIV prevention intervention package in reducing HIV incidence. The trial was implemented in 21 study communities (7 matched triplets), 12 in Zambia and 9 in the Western Cape province, South Africa.29 In the two treatment arms (A and B), a new cadre of community-based health workers (CHWs) known as community HIV care providers (CHiPs) were locally recruited to carry out door-to-door HIV testing and referral services. In all arms, health facility- and existing CHWs received training on the PopART intervention.
Study population
From August 2014 to May 2015, data collection took place at enrollment to an open cohort study of CHiPs (arms A and B only), and health facility staff (HFS) and CHWs (in all trial arms). By this time, the HPTN 071 (PopART) trial had been running for 8–18 months depending on the study communities.30 Inclusion criteria for all cadres were that they had to be at least 18 years of age and able to provide informed consent for participation. All CHiPs were automatically considered eligible for the study upon recruitment to the PopART intervention team. The procedure for the selection of CHiPs is described in detail elsewhere.29 All staff at health facilities were eligible, including doctors, nurses, laboratory technicians, cleaners, and security guards. CHWs who primarily worked in the field but were part of community HIV services and worked on a weekly basis were also eligible. For this analysis, we included 1557 participants across all three cadres of health workers who responded “yes” when asked “Do you directly provide HIV-related services to clients?” This was the enrollment survey in a cohort study that stretched from 2014 to 2018.28
Data collection procedures
After providing informed consent, participants completed a self-administered questionnaire on an electronic data collection device. Data were anonymized and participants were given a unique study identification number. We asked questions about sociodemographic characteristics, experience at the facility in which they work, training, job stress, experiences providing care, and stigma, including questions about their own beliefs as well as about their perceptions of the behaviors of coworkers.
Stigma measurement
The survey presented to health workers the same four statements about judgments toward four groups of people: PLHIV, “women who sell sex,” MSM, and young women who become pregnant before marriage. We used the broad terminology “women who sell sex” in question wording following local consultation. Participants were asked to respond to the statements using a 4-point Likert scale (strongly agree, agree, disagree, strongly disagree). We used standardized questions from the Nyblade et al. tool for assessing HIV stigma and discrimination in health facilities that was validated in six countries.31
Two statements related solely to judgmental attitudes that may be held by participants: “I would be ashamed if someone (a man, a woman, a young woman) in my family was (living with HIV, had sex with men, sold sex, became pregnant before marriage)” and, “(PLHIV, MSM, women who sell sex, or young women who become pregnant before marriage) engage in irresponsible behaviors.” Two statements further linked these attitudes to aspects of health service provision: “Other people deserve access to health services more than (PLHIV, MSM, women who sell sex, or young women who become pregnant before marriage)”; and, “If I had a choice, I would prefer not to provide services to (PLHIV, MSM, women who sell sex, or young women who become pregnant before marriage).”
Data analysis
First, we enumerated the eligible population and described details of nonparticipation and nonresponse. Second, for participants included in the analysis, we described sociodemographics and job-related characteristics across the three cadres of health workers and the two countries. Third, we analyzed the levels of judgmental attitudes toward each of the different population groups within each country, and compared these between the health worker cadres adjusting for age, sex, and study triplet to reflect the cluster randomized trial design of the study. Fourth, we pooled the data and used logistic regression to explore individual risk factors associated with each of the items in turn, adjusting for age, sex, cadre of health worker, and triplet.
We restricted the analysis to health workers who had responded to all four questions about each key population. We hypothesized that stigma would be associated with sociodemographic variables and level of training: age, gender, and education level have all previously been associated with stigmatizing attitudes.32,33
We hypothesized that perceptions about the stigmatizing behavior of coworkers would also be associated with their own judgmental beliefs, as in other recent literature.34 This association might occur because health workers are more likely to hold stigmatizing attitudes if they think their coworkers share the same attitudes, or because health workers who hold stigmatizing attitudes think that others share their attitudes. We repeated this final stage of the analysis in relation to each of the four groups. We report the full findings for PLHIV in this article, and for women who sell sex, MSM, and young women who become pregnant before marriage in Supplementary Tables S1, S2, S3, S4, S5, S6, S7.
Ethics
The HPTN 071 (PopART) trial [Division of AIDS (DAIDS) number 11865 and Clinical Trials registration number NCT01900977] and the stigma ancillary study (DAIDS number HPTN071a) received Institutional Review Board approval from the London School of Hygiene and Tropical Medicine, LSHTM, the Health Research Ethics Committee, Stellenbosch University, and the Biomedical Research Ethics Committee at the University of Zambia. Written informed consent was sought and obtained from all participants for all aspects of the research.
Results
Recruitment of participants
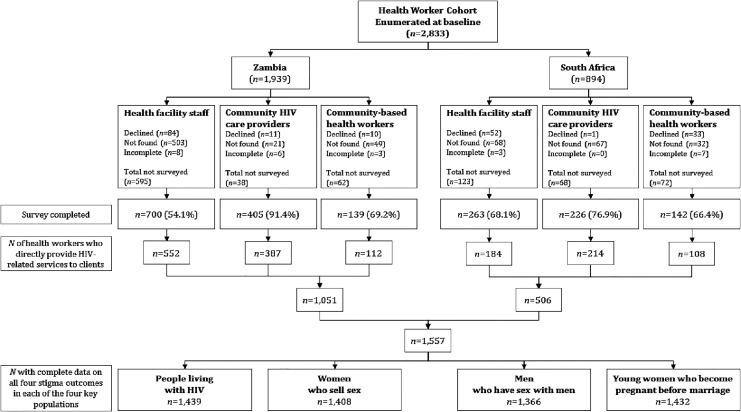
We enumerated 2833 eligible health workers (Fig. 1). The most important reason for not being included in the analysis was difficulty in locating respondents rather than refusal. Three hundred eighteen participants (HFS = 227, CHiPs = 30, and CHWs = 61) answered “no” to the question “Do you directly provide HIV-related services to clients” and so were excluded. Ultimately, 1557 health workers were included in the analysis (66% of the total number of eligible participants), including 736 HFS, 601 CHiPs, and 220 CHWs. The response rate was highest among the CHiP workers and lowest among HFS.
FIG. 1.
Participant flow diagram.
Description of study populations
Across all cadres, the majority of participants were women (73.1% for HFS; 69.6% for CHiPs; 86.8% for CHWs; Table 1). Just over half of HFS and CHWs were married (57.5% and 52.7%, respectively), while just over half of CHiPs were unmarried (54.4%). More HFS and CHWs were 44 years of age or older (34.0% and 39.5%, respectively), while more CHiPs were younger (e.g., 42.9% were aged 25–34 years). HFS, 65.4%, had completed further education beyond secondary school, while CHiPs had a higher education background compared with CHWs (44.6% and 11.4% had completed further education, respectively). More than 95% of CHWs lived in the community where they were working, but that proportion was lower among CHiPs (76.2%) and lowest among HFS (58.4%).
Table 1.
Sociodemographic and Behavioral Characteristics of 1557 Health Workers Who Provide HIV-Related Services by Country
| Cadre of health worker |
Country |
||||||
|---|---|---|---|---|---|---|---|
| HFS (n = 736), n (%) | CHiP (n = 601), n (%) | CHW (n = 220), n (%) | p | Zambia (n = 1051), n (%) | South Africa (n = 506), n (%) | p | |
| Cadre of health worker | <0.001 | ||||||
| HFS | 552 (52.5) | 184 (36.4) | |||||
| CHiP | 387 (36.8) | 214 (42.3) | |||||
| CHW | 112 (10.7) | 108 (21.3) | |||||
| Age group | <0.001 | <0.001 | |||||
| <25 years | 57 (7.7) | 58 (9.7) | 15 (6.8) | 69 (6.6) | 61 (12.1) | ||
| 25–34 years | 230 (31.3) | 258 (42.9) | 57 (25.9) | 322 (30.6) | 223 (44.1) | ||
| 35–44 years | 199 (27.0) | 142 (23.6) | 61 (27.7) | 267 (25.4) | 135 (26.7) | ||
| >44 year | 250 (34.0) | 143 (23.8) | 87 (39.5) | 393 (37.4) | 87 (17.2) | ||
| Sex | <0.001 | <0.001 | |||||
| Male | 198 (26.9) | 183 (30.4) | 29 (13.2) | 340 (32.4) | 70 (13.8) | ||
| Female | 538 (73.1) | 418 (69.6) | 191 (86.8) | 711 (67.6) | 436 (86.2) | ||
| Marital status | <0.001 | <0.001 | |||||
| Married | 423 (57.5) | 274 (45.6) | 116 (52.7) | 622 (59.2) | 191 (37.7) | ||
| Not married | 313 (42.5) | 327 (54.4) | 104 (47.3) | 429 (40.8) | 315 (62.3) | ||
| Education | <0.001 | <0.001 | |||||
| Did not complete secondary | 33 (4.5) | 9 (1.5) | 30 (13.6) | 64 (6.1) | 8 (1.6) | ||
| Completed secondary | 222 (30.2) | 324 (53.9) | 165 (75.0) | 400 (38.1) | 311 (61.5) | ||
| Furthera | 481 (65.4) | 268 (44.6) | 25 (11.4) | 587 (55.9) | 187 (37.0) | ||
| How important is religion to you | 0.221 | <0.001 | |||||
| Very important | 632 (85.9) | 522 (86.9) | 189 (85.9) | 965 (91.8) | 378 (74.7) | ||
| Important | 82 (11.1) | 68 (11.3) | 25 (11.4) | 73 (6.9) | 102 (20.2) | ||
| Somewhat important | 11 (1.5) | 6 (1.0) | 1 (0.5) | 5 (0.5) | 13 (2.6) | ||
| Not important | 10 (1.4) | 2 (0.3) | 5 (2.3) | 8 (0.8) | 9 (1.8) | ||
| Missing | 1 (0.1) | 3 (0.5) | 0 (0.0) | 0 (0.0) | 4 (0.8) | ||
| Do you live in this community | <0.001 | <0.001 | |||||
| No | 306 (41.6) | 143 (23.8) | 9 (4.1) | 340 (32.4) | 118 (23.3) | ||
| Yes | 430 (58.4) | 458 (76.2) | 211 (95.9) | 711 (67.6) | 388 (76.7) | ||
| Have you ever tested for HIV | 0.042 | 0.952 | |||||
| No | 16 (2.2) | 8 (1.3) | 8 (3.6) | 22 (2.1) | 10 (2.0) | ||
| Yes | 711 (96.6) | 592 (98.5) | 211 (95.9) | 1022 (97.2) | 492 (97.2) | ||
| Missing | 9 (1.2) | 1 (0.2) | 1 (0.5) | 7 (0.7) | 4 (0.8) | ||
| Please indicate the result of your last HIV test | <0.001 | <0.001 | |||||
| Negative | 549 (74.6) | 428 (71.2) | 132 (60.0) | 742 (70.6) | 367 (72.5) | ||
| Positive | 105 (14.3) | 117 (19.5) | 49 (22.3) | 214 (20.4) | 57 (11.3) | ||
| Undetermined | 3 (0.4) | 2 (0.3) | 4 (1.8) | 4 (0.4) | 5 (1.0) | ||
| Missing | 79 (10.7) | 54 (9.0) | 35 (15.9) | 91 (8.7) | 77 (15.2) | ||
| Did you ever receive training in infection control and universal precautions (including PEP and waste management)? | 0.003 | <0.001 | |||||
| No | 169 (23.0) | 135 (22.5) | 63 (28.6) | 258 (24.5) | 109 (21.5) | ||
| Yes | 532 (72.3) | 419 (69.7) | 134 (60.9) | 747 (71.1) | 338 (66.8) | ||
| Missing | 35 (4.8) | 47 (7.8) | 23 (10.5) | 46 (4.4) | 59 (11.7) | ||
| My coworkers sometimes treat PLHIV poorly when providing them with health services | 0.121 | <0.001 | |||||
| Strongly disagree | 265 (36.0) | 240 (39.9) | 73 (33.2) | 356 (33.9) | 222 (43.9) | ||
| Disagree | 333 (45.2) | 269 (44.8) | 101 (45.9) | 487 (46.3) | 216 (42.7) | ||
| Agree | 88 (12.0) | 58 (9.7) | 34 (15.5) | 151 (14.4) | 29 (5.7) | ||
| Strongly agree | 25 (3.4) | 13 (2.2) | 2 (0.9) | 30 (2.9) | 10 (2.0) | ||
| Missing | 25 (3.4) | 21 (3.5) | 10 (4.5) | 27 (2.6) | 29 (5.7) | ||
| My coworkers sometimes talk badly about people thought to be living with HIV | 0.322 | <0.001 | |||||
| Strongly disagree | 146 (19.8) | 135 (22.5) | 46 (20.9) | 185 (17.6) | 142 (28.1) | ||
| Disagree | 347 (47.1) | 270 (44.9) | 103 (46.8) | 472 (44.9) | 248 (49.0) | ||
| Agree | 177 (24.0) | 136 (22.6) | 43 (19.5) | 287 (27.3) | 69 (13.6) | ||
| Strongly agree | 54 (7.3) | 41 (6.8) | 23 (10.5) | 94 (8.9) | 24 (4.7) | ||
| Missing | 12 (1.6) | 19 (3.2) | 5 (2.3) | 13 (1.2) | 23 (4.5) | ||
Completed college/university or postgraduate studies.
CHiP, community HIV care provider; CHW, community-based health worker; HFS, health facility staff; PEP, postexposure prophylaxis; PLHIV, people living with HIV.
p-Values marked in bold indicate numbers that are significant on the 95% confidence limit.
Religion was more important to participants in Zambia (91.8%) than South Africa (74.7%). More than 95% of participants said they had ever received an HIV test. The self-reported proportion of health workers saying they had previously tested HIV positive was slightly higher among CHiPs and CHWs (19.5%, 117/601 and 22.3%, 49/220, respectively) compared with HFS (14.3%, 105/736). In Zambia, 8.7% (91/1051) of participants declined to answer this question, while in South Africa, 15.2% (77/506) did not answer the question. Zambian participants were more likely than South African participants to agree or strongly agree with the statement that their coworkers treat PLHIV poorly (17.3%, 181/1051 and 7.7%, 39/506, respectively; p < 0.001) or talk badly about them (36.2%, 381/1051 and 18.3%, 93/506, respectively; p < 0.001; Table 1).
Measures of stigma and judgment
In Zambia, 5.2% (52/1004) of respondents agreed with the statement “I would be ashamed if someone in my family had HIV.” Similarly, in South Africa, 5.5% (24/435) agreed. There was no strong evidence that levels of agreement with this statement differed by health worker cadre in either country (padj = 0.307 in Zambia, pm = 0.074 in South Africa; Table 2). A much larger proportion of health workers agreed with this statement in relation to women who sell sex in both countries. Agreement was higher in Zambia than in South Africa (81.3%, 815/1002 and 70.2%, 285/406, respectively) with little evidence of a difference between health worker cadres in either country (pm = 0.130 in Zambia, and pm = 0.344 in South Africa). Even higher proportions of health workers agreed to this statement in relation to MSM in Zambia (88.1%, 856/972), whereas in South Africa agreement was lower (53.0%, 209/394).
Table 2.
Logistic Regression Describing Health Workers' Personal Attitudes Toward People Living with HIV and Key Populations by Country
| PLHIV (n = 1439) |
Women who sell sex (n = 1408) |
MSM (n = 1366) |
Young women who become pregnant before marriage (n = 1432) |
|||||
|---|---|---|---|---|---|---|---|---|
| n/N (%) | aORs (95% CIs)* | n/N (%) | aORs (95% CIs)* | n/N (%) | aORs (95% CIs)* | n/N (%) | aORs (95% CIs)* | |
| I would be ashamed if someone in my family was (key population) | ||||||||
| Zambia | ||||||||
| HFS | 32/528 (6.1) | 1 [0.307]† | 437/523 (83.6) | 1 [0.130]† | 451/500 (90.2) | 1 [0.052]† | 257/517 (49.7) | 1 [0.005]† |
| CHiP | 13/373 (3.5) | 0.57 (0.30–1.10) | 299/373 (80.2) | 0.83 (0.58–1.19) | 314/366 (85.8) | 0.71 (0.46–1.08) | 191/371 (51.5) | 0.97 (0.73–1.28) |
| CHW | 7/103 (6.8) | 1.62 (0.72–3.67) | 79/106 (74.5) | 0.61 (0.36–1.03) | 91/106 (85.8) | 0.67 (0.35–1.30) | 69/108 (63.9) | 1.32 (0.85–2.07) |
| South Africa | ||||||||
| HFS | 8/159 (5) | 1 [0.074]† | 108/153 (70.6) | 1 [0.344]† | 75/147 (51) | 1 [0.287]† | 36/162 (22.2) | 1 [<0.001]† |
| CHiP | 6/181 (3.3) | 0.55 (0.18–1.66) | 119/162 (73.5) | 1.27 (0.79–2.05) | 83/157 (52.9) | 0.96 (0.62–1.48) | 58/178 (32.6) | 2.10 (1.28–3.46) |
| CHW | 10/95 (10.5) | 2.58 (1.01–6.57) | 58/91 (63.7) | 0.89 (0.52–1.51) | 51/90 (56.7) | 1.20 (0.72–1.99) | 42/96 (43.8) | 3.07 (1.78–5.31) |
| (Key population) engage in irresponsible behaviors | ||||||||
| Zambia | ||||||||
| HFS | 152/528 (28.8) | 1 [<0.001]† | 432/523 (82.6) | 1 [0.001]† | 387/500 (77.4) | 1 [0.170]† | 237/517 (45.8) | 1 [<0.001]† |
| CHiP | 105/373 (28.2) | 0.96 (0.71–1.31) | 302/373 (81) | 0.92 (0.64–1.32) | 287/366 (78.4) | 0.98 (0.70–1.38) | 203/371 (54.7) | 1.33 (1.01–1.75) |
| CHW | 40/103 (38.8) | 1.45 (0.91–2.32) | 88/106 (83) | 1.13 (0.62–2.05) | 87/106 (82.1) | 1.10 (0.62–1.95) | 73/108 (67.6) | 2.15 (1.36–3.40) |
| South Africa | ||||||||
| HFS | 47/159 (29.6) | 1 [<0.001]† | 92/153 (60.1) | 1 [0.049]† | 79/147 (53.7) | 1 [0.010]† | 63/162 (38.9) | 1 [0.366]† |
| CHiP | 36/181 (19.9) | 0.67 (0.40–1.13) | 93/162 (57.4) | 0.94 (0.59–1.50) | 67/157 (42.7) | 0.80 (0.51–1.28) | 60/178 (33.7) | 0.86 (0.54–1.35) |
| CHW | 31/95 (32.6) | 1.44 (0.83–2.51) | 55/91 (60.4) | 0.93 (0.55–1.59) | 43/90 (47.8) | 0.80 (0.47–1.35) | 37/96 (38.5) | 1.09 (0.65–1.82) |
| Other people deserve access to health services more than (key population) | ||||||||
| Zambia | ||||||||
| HFS | 90/528 (17) | 1 [0.020]† | 61/523 (11.7) | 1 [0.018]† | 68/500 (13.6) | 1 [0.017]† | 76/517 (14.7) | 1 [0.088]† |
| CHiP | 91/373 (24.4) | 1.64 (1.17–2.31) | 69/373 (18.5) | 1.78 (1.21–2.62) | 64/366 (17.5) | 1.38 (0.94–2.03) | 61/371 (16.4) | 1.16 (0.79–1.70) |
| CHW | 30/103 (29.1) | 2.23 (1.35–3.70) | 22/106 (20.8) | 2.04 (1.16–3.60) | 28/106 (26.4) | 2.42 (1.42–4.13) | 27/108 (25) | 1.95 (1.15–3.33) |
| South Africa | ||||||||
| HFS | 22/159 (13.8) | 1 [0.001]† | 14/153 (9.2) | 1 [0.002]† | 15/147 (10.2) | 1 [0.106]† | 20/162 (12.3) | 1 [0.020]† |
| CHiP | 51/181 (28.2) | 2.71 (1.53–4.82) | 27/162 (16.7) | 2.52 (1.26–5.04) | 27/157 (17.2) | 2.18 (1.09–4.32) | 36/178 (20.2) | 1.75 (0.97–3.15) |
| CHW | 32/95 (33.7) | 3.54 (1.90–6.58) | 25/91 (27.5) | 3.88 (1.90–7.92) | 20/90 (22.2) | 2.90 (1.40–5.97) | 23/96 (24) | 2.46 (1.30–4.64) |
| If I had a choice, I would prefer not to provide services to (key population) | ||||||||
| Zambia | ||||||||
| HFS | 37/528 (7) | 1 [0.492]† | 39/523 (7.5) | 1 [0.123]† | 53/500 (10.6) | 1 [0.165]† | 27/517 (5.2) | 1 [0.210]† |
| CHiP | 20/373 (5.4) | 0.84 (0.48–1.48) | 24/373 (6.4) | 0.95 (0.55–1.63) | 33/366 (9) | 0.90 (0.56–1.43) | 9/371 (2.4) | 0.45 (0.20–0.98) |
| CHW | 7/103 (6.8) | 1.06 (0.45–2.50) | 17/106 (16) | 2.51 (1.27–4.95) | 20/106 (18.9) | 2.01 (1.08–3.73) | 8/108 (7.4) | 1.41 (0.57–3.48) |
| South Africa | ||||||||
| HFS | 4/159 (2.5) | 1 [<0.001]† | 11/153 (7.2) | 1 [0.004]† | 9/147 (6.1) | 1 [0.128]† | 10/162 (6.2) | 1 [0.014]† |
| CHiP | 8/181 (4.4) | 1.27 (0.38–4.23) | 11/162 (6.8) | 0.92 (0.39–2.15) | 11/157 (7) | 1.02 (0.42–2.47) | 11/178 (6.2) | 1.09 (0.45–2.63) |
| CHW | 13/95 (13.7) | 8.74 (2.85–26.77) | 16/91 (17.6) | 2.90 (1.29–6.49) | 15/90 (16.7) | 3.38 (1.46–7.83) | 12/96 (12.5) | 2.90 (1.23–6.84) |
HFS is the reference category with overall padj value of the model presented in brackets.
Adjusted for sex, age, and triplet.
pm Value for model.
aOR, adjusted odds ratio; CIs, confidence intervals; CHiP, community HIV care provider; CHW, community-based health worker; HFS, health facility staff; MSM, men who have sex with men; PLHIV, people living with HIV.
p-Values marked in bold indicate numbers that are significant on the 95% confidence limit.
There was some evidence for a difference in judgmental attitudes toward MSM between health worker cadres in Zambia, with CHiPs and CHWs being less likely to agree compared with HFS (pm = 0.052), but not in South Africa (padj = 0.287). In Zambia, 48.4% (517/1068) of respondents agreed that they would be ashamed if a young woman in their family became pregnant before marriage with nonsignificant differences observed between cadres despite the model being statistically significant (padj = 0.005). In South Africa, 31.2% (136/436) agreed with this statement with CHiPs being two times [adjusted odds ratio (aOR) = 2.10, 95% confidence interval (CI): 1.28–3.46] and CHWs being three times (aOR = 3.07, 95% CI: 1.78–5.31) more likely to agree compared with HFS (padj < 0.001).
Patterns of responses to the second statement, “[Key population members] engage in irresponsible behaviors,” were similar to the “ashamed” statement with two exceptions. First, more participants agreed with this statement in relation to PLHIV (29.6%, 297/1004 and 26.2%, 114/435 in Zambia and South Africa, respectively), whereas fewer participants agreed in relation to MSM (76.4%, 761/996 and 29.6%, 129/436, respectively). Second, CHiPs were 1.33 times and CHWs were two times more likely, compared with HFS, to agree with the “irresponsible” statement in relation to young women who become pregnant before marriage in Zambia (aOR = 1.33, 95% CI: 1.01–1.75 and aOR = 2.15, 95% CI: 1.36–3.40, respectively; Table 2). Although most models fit the data well (p < 0.05 in all cases, but Zambia for MSM and South Africa for young women who become pregnant before marriage), no evidence of a difference in this statement between cadres was observed (Table 2).
In Zambia, 21.0% (221/1004) of respondents reported that: “Other people deserve access to services more than PLHIV,” compared with 24.1% (105/435) in South Africa. Slightly lower proportions of health workers reported this sentiment in relation to women who sell sex (15.3%, 152/996 and 15.1%, 66/436), MSM (16.1%, 160/996 and 14.2%, 62/436), and young women who become pregnant before marriage (16.5%, 164/996 and 18.1%, 79/436) in Zambia and South Africa, respectively. In relation to all of the key population groups, CHWs were the most likely to report this sentiment [aORs (95% CI)] compared with HFS, varying from 1.95 (1.15–3.33) to 3.88 (1.90–7.92; Table 2).
Finally, in relation to the final statement “If I had a choice, I would prefer not to provide services to (key population group),” a lower proportion reported this in both countries, by each health worker cadre, and in relation to each key population group than for all previous statements. The only exception was PLHIV, where proportions were similar when compared with the “ashamed” statement. In both countries, CHWs were once again the most likely to report this sentiment [aORs (95% CI) varying from 1.06 (0.45–2.50) to 8.74 (2.85–26.77)] in comparison with HFS (Table 2).
Risk factors
Sociodemographic factors, HIV testing, HIV status, and training experience were generally not significantly associated with judgmental attitudes toward PLHIV, with a few exceptions (Tables 3 and 4). Perceptions of coworkers' stigmatizing behaviors were significantly related to all four judgmental attitudes (Table 4). Female health workers were less likely to hold judgmental attitudes, and this was statistically significant in relation to the “irresponsible” statement (aOR = 0.45, 95% CI: 0.35–0.59; Table 3). Health workers who were more educated were least likely to agree with three of the statements about PLHIV (this was statistically significant with respect to the “ashamed” statement (aOR = 0.31, 95% CI: 0.10–0.94; Table 3) and yet more likely to hold stigmatizing and judgmental attitudes in relation to the “irresponsible” and “ashamed” statements for key populations. However, they were also less likely to hold such attitudes toward key populations in relation to the other two statements (not providing services and deserving access).
Table 3.
The Association Between Sociodemographic Characteristics of Health Workers and Four Stigma Outcomes for People Living with HIV
| Variable | Categories | I would be ashamed if someone in my family was a person living with HIV |
PLHIV engage in irresponsible behaviors |
If I had a choice, I would prefer not to provide services to PLHIV |
Other people deserve access to health services more than PLHIV |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n/N (%)* | aOR (95% CIs)† | pw‡ | n/N (%)* | aOR (95% CIs)† | pw‡ | n/N (%)* | aOR (95% CIs)† | pw‡ | n/N (%)* | aOR (95% CIs)† | pw‡ | ||
| Sex | Male | 25/386 (6.5) | 1 | 0.082 | 150/386 (38.9) | 1 | <0.001 | 29/386 (7.5) | 1 | 0.074 | 88/386 (22.8) | 1 | 0.330 |
| Female | 51/1053 (4.8) | 0.63 (0.37–1.06) | 261/1053 (24.8) | 0.45 (0.35–0.59) | 60/1053 (5.7) | 0.64 (0.39–1.04) | 228/1053 (21.7) | 0.86 (0.64–1.16) | |||||
| Age | <25 years | 7/117 (6.0) | 1 | 0.594 | 34/117 (29.1) | 1 | <0.001 | 9/117 (7.7) | 1 | 0.170 | 30/117 (25.6) | 1 | 0.437 |
| 25–34 years | 24/490 (4.9) | 0.80 (0.33–1.92) | 115/490 (23.5) | 0.71 (0.45–1.13) | 21/490 (4.3) | 0.54 (0.24–1.22) | 99/490 (20.2) | 0.74 (0.46–1.20) | |||||
| 35–44 years | 16/376 (4.3) | 0.66 (0.26–1.67) | 101/376 (26.9) | 0.87 (0.54–1.40) | 23/376 (6.1) | 0.78 (0.35–1.75) | 84/376 (22.3) | 0.89 (0.54–1.45) | |||||
| >44 year | 29/456 (6.4) | 1 (0.42–2.39) | 161/456 (35.3) | 1.35 (0.85–2.13) | 36/456 (7.9) | 1 (0.46–2.19) | 103/456 (22.6) | 0.94 (0.57–1.52) | |||||
| Education | Did not complete secondary | 5/64 (7.8) | 1 | <0.001 | 22/64 (34.4) | 1 | 0.188 | 7/64 (10.9) | 1 | 0.065 | 12/64 (18.8) | 1 | 0.106 |
| Completed secondary | 51/650 (7.8) | 1.16 (0.43–3.17) | 204/650 (31.4) | 1.02 (0.58–1.81) | 51/650 (7.8) | 0.88 (0.37–2.12) | 174/650 (26.8) | 1.55 (0.79–3.07) | |||||
| Further | 20/725 (2.8) | 0.31 (0.10–0.94) | 185/725 (25.5) | 0.80 (0.44–1.44) | 31/725 (4.3) | 0.49 (0.19–1.25) | 130/725 (17.9) | 1.18 (0.59–2.39) | |||||
| Marital status | Married | 42/752 (5.6) | 1 | 0.886 | 231/752 (30.7) | 1 | 0.488 | 56/752 (7.4) | 1 | 0.094 | 165/752 (21.9) | 1 | 0.516 |
| Not married | 34/687 (4.9) | 0.96 (0.58–1.61) | 180/687 (26.2) | 0.91 (0.70–1.18) | 33/687 (4.8) | 0.65 (0.40–1.07) | 151/687 (22.0) | 0.91 (0.69–1.20) | |||||
| Religion | Very important | 65/1245 (5.2) | 1 | 0.726 | 354/1245 (28.4) | 1 | 0.618 | 74/1245 (5.9) | 0.482 | 276/1245 (22.2) | 1 | 0.308 | |
| Important | 8/160 (5.0) | 0.94 (0.43–2.04) | 47/160 (29.4) | 1.12 (0.76–1.64) | 12/160 (7.5) | 1.41 (0.73–2.73) | 31/160 (19.4) | 0.85 (0.55–1.30) | |||||
| Somewhat important | 2/17 (11.8) | 2.44 (0.50–11.75) | 3/17 (17.6) | 0.48 (0.13–1.79) | 2/17 (11.8) | 2.71 (0.56–13.06) | 6/17 (35.3) | 2.14 (0.77–6.00) | |||||
| Not important | 1/15 (6.7) | 0.87 (0.11–7.01) | 6/15 (40.0) | 1.29 (0.44–3.80) | 1/15 (6.7) | 0.85 (0.10–6.82) | 2/15 (13.3) | 0.51 (0.11–2.34) | |||||
| Missing | 0/2 (0.0) | 1/2 (50.0) | 0/2 (0.0) | 1/2 (50.0) | |||||||||
| Ever tested | No | 4/29 (13.8) | 1 | 0.093 | 13/29 (44.8) | 1 | 0.109 | 4/29 (13.8) | 1 | 0.162 | 12/29 (41.4) | 1 | 0.020 |
| Yes | 72/1403 (5.1) | 0.39 (0.13–1.17) | 396/1403 (28.2) | 0.54 (0.25–1.15) | 85/1403 (6.1) | 0.46 (0.15–1.37) | 303/1403 (21.6) | 0.40 (0.19–0.87) | |||||
| Missing | 0/7 (0.0) | 2/7 (28.6) | 0/7 (0.0) | 1/7 (14.3) | |||||||||
| HIV status | Negative | 47/1029 (4.6) | 1 | 0.077 | 294/1029 (28.6) | 1 | 0.575 | 58/1029 (5.6) | 1 | 0.204 | 225/1029 (21.9) | 1 | 0.302 |
| Positive | 17/257 (6.6) | 1.75 (0.94–3.24) | 81/257 (31.5) | 1.10 (0.80–1.51) | 20/257 (7.8) | 1.44 (0.82–2.53) | 53/257 (20.6) | 0.83 (0.58–1.18) | |||||
| Undetermined | 0/8 (0.0) | 2/8 (25.0) | 0/8 (0.0) | 2/8 (25.0) | |||||||||
| Missing | 12/145 (8.3) | 34/145 (23.4) | 11/145 (7.6) | 36/145 (24.8) | |||||||||
Proportion of health workers responding strongly agree or agree.
The aOR for sex is adjusted for age group, cadre of health worker, and triplet; the aOR for age group is adjusted for sex, cadre of health worker, and triplet; the aOR for all other predictor variables is adjusted for sex, age group, cadre of health worker, and triplet.
A p value of <0.05 indicates that the predictor creates a statistically significant improvement in the fit of the model.
aOR, adjusted odds ratio; CIs, confidence intervals; n, number of individuals reporting the four types of stigma within groups; N, total number of individuals within groups; PLHIV, people living with HIV; pw, p value of the Wald test.
p-Values marked in bold indicate numbers that are significant on the 95% confidence limit.
Table 4.
The Association Between Health Workers' Training, Perceptions of Coworker Attitudes, and Stigmatizing Attitudes with Four Stigma Outcomes for People Living with HIV
| |
|
I would be ashamed if someone in my family was a person living with HIV |
PLHIV engage in irresponsible behaviors |
If I had a choice, I would prefer not to provide services to a person living with HIV |
Other people deserve access to health services more than PLHIV |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Categories | n/N (%)* | aOR (95% CIs)† | pw‡ | n/N (%)* | aOR (95% CIs)† | pw‡ | n/N (%)* | aOR (95% CIs)† | pw‡ | n/N (%)* | aOR (95% CIs)† | pw‡ |
| Training on infection controla | No | 17/340 (5.0) | 1 | 0.640 | 94/340 (27.6) | 1 | 0.858 | 16/340 (4.7) | 1 | 0.156 | 68/340 (20.0) | 1 | 0.491 |
| Yes | 56/1019 (5.5) | 1.14 (0.65–2.02) | 293/1019 (28.8) | 1.03 (0.77–1.36) | 70/1019 (6.9) | 1.50 (0.86–2.65) | 219/1019 (21.5) | 1.12 (0.82–1.52) | |||||
| Missing | 3/80 (3.8) | 24/80 (30.0) | 3/80 (3.8) | 29/80 (36.3) | |||||||||
| My coworkers sometimes treat PLHIV poorlyb | Strongly disagree | 14/541 (2.6) | 1 | <0.001 | 114/541 (21.1) | 1 | <0.001 | 16/541 (3.0) | 1 | <0.001 | 90/541 (16.6) | 1 | <0.001 |
| Disagree | 35/658 (5.3) | 2.15 (1.14–4.07) | 209/658 (31.8) | 1.69 (1.28–2.21) | 40/658 (6.1) | 2.12 (1.16–3.85) | 148/658 (22.5) | 1.49 (1.10–2.00) | |||||
| Agree | 19/172 (11.0) | 4.64 (2.23–9.66) | 64/172 (37.2) | 1.96 (1.33–2.89) | 22/172 (12.8) | 4.57 (2.29–9.11) | 61/172 (35.5) | 2.97 (1.98–4.45) | |||||
| Strongly agree | 7/38 (18.4) | 8.00 (2.92–21.92) | 19/38 (50.0) | 3.16 (1.58–6.32) | 8/38 (21.1) | 8.38 (3.23–21.72) | 12/38 (31.6) | 2.78 (1.32–5.82) | |||||
| Missing | 1/30 (3.3) | 5/30 (16.7) | 3/30 (10.0) | 5/30 (16.7) | |||||||||
| My coworkers sometimes talk badly about PLHIVc | Strongly disagree | 10/297 (3.4) | 1 | <0.001 | 48/297 (16.2) | 1 | <0.001 | 7/297 (2.4) | 1 | <0.001 | 53/297 (17.8) | 1 | 0.007 |
| Disagree | 25/672 (3.7) | 1.15 (0.54–2.45) | 200/672 (29.8) | 2.16 (1.51–3.11) | 36/672 (5.4) | 2.49 (1.09–5.73) | 138/672 (20.5) | 1.26 (0.88–1.81) | |||||
| Agree | 24/339 (7.1) | 2.37 (1.10–5.13) | 109/339 (32.2) | 2.39 (1.60–3.56) | 30/339 (8.8) | 4.22 (1.80–9.89) | 89/339 (26.3) | 1.83 (1.23–2.72) | |||||
| Strongly agree | 17/114 (14.9) | 5.30 (2.29–12.24) | 51/114 (44.7) | 4.13 (2.50–6.82) | 16/114 (14.0) | 6.96 (2.72–17.78) | 32/114 (28.1) | 1.93 (1.15–3.26) | |||||
| Missing | 0/17 (0.0) | 3/17 (17.6) | 0/17 (0.0) | 4/17 (23.5) | |||||||||
Proportion of health workers responding strongly agree or agree.
Adjusted for sex, age, cadre of health worker, and triplet.
A p value of <0.05 indicates that the predictor creates a statistically significant improvement in the fit of the model.
Infection control and universal precautions (including postexposure prophylaxis and waste management).
My coworkers sometimes treat PLHIV poorly when providing them.
My coworkers sometimes talk badly about people thought to be living with HIV.
aOR, adjusted odds ratio; CIs, confidence intervals; n, number of individuals reporting the four types of stigma within groups; N, total number of individuals within groups; PLHIV, people living with HIV; pw, p value of the Wald test.
p-Values marked in bold indicate numbers that are significant on the 95% confidence limit.
Health workers who perceived that their coworkers either talked badly about their clients living with HIV or treated them poorly were more likely to hold judgmental and stigmatizing attitudes (p < 0.01 in all cases; Table 4). Specifically, health workers who strongly agreed with the statement that coworkers treat PHLIV poorly or talk badly about them were more likely to believe that “other people deserve access to health services more than PLHIV” (aOR = 1.93, 95% CI: 1.15–3.26) or would “prefer not to provide services to PLHIV” (aOR = 8.38, 95% CI: 3.23–21.72), respectively (Table 4). Across all key populations, perceptions about coworker stigmatizing behaviors were strongly associated with agreement with all four statements (Supplementary Table S1).
We found inconsistent patterns in relation to each of the other key populations for most of the risk factors we examined (Supplementary Tables S2, S3, S4, S5, S6, S7). We found no associations between age, marital status, HIV testing and status, and training experience and agreement with statements describing stigmatizing attitudes, with a few exceptions. Older health workers (44+) were more likely to agree that they would be ashamed if a young women in their family became pregnant before marriage (aOR = 1.85, 95% CI: 1.23–2.78; Supplementary Table S6). Older health workers were also more likely to agree that young women who become pregnant before marriage and MSM engage in irresponsible behaviors [aOR = 1.81, 95% CI: 1.11–2.94 (Supplementary Table S6) and aOR = 1.65, 95% CI: 1.09–2.49 (Supplementary Table S4), respectively]. Female health workers were less likely to hold judgmental attitudes in relation to the “irresponsible” statement for young women who become pregnant before marriage (aOR = 0.76, 95% CI: 0.64–0.91; Supplementary Table S6).
Health workers who tested for HIV were less likely to hold judgmental attitudes in relation to the “provision of services” statement for women who sell sex (aOR = 0.33, 95% CI: 0.12–0.91; Supplementary Table S2) and for young women who become pregnant before marriage (aOR = 0.29, 95% CI: 0.13–0.65; Supplementary Table S6), and for the “irresponsible” statement for MSM (aOR = 0.10, 95% CI: 0.01–0.81; Supplementary Table S4). Health workers who tested positive for HIV were less likely to hold judgmental attitudes in relation to the “irresponsible” statement for women who sell sex (aOR = 0.63, 95% CI: 0.42–0.95; Supplementary Table S2) and for the “provision of services” statement for young women who become pregnant before marriage (aOR = 0.54, 95% CI: 0.31–0.97; Supplementary Table S6). Health workers who reported that religion was somewhat important were more likely to report judgmental attitudes in relation to the “access” and “provision of services” statements for women who sell sex (aOR = 3.45, 95% CI: 1.21–9.84 and aOR = 5.63, 95% CI: 1.85–17.17, respectively; Supplementary Table S2).
Discussion
We found high levels of judgmental attitudes toward key population groups among 1557 health workers delivering HIV services in 21 urban communities in South Africa and Zambia and that these attitudes were more commonly and heavily targeted at women who sell sex, MSM, and adolescents who become pregnant before marriage than PLHIV. Health workers commonly agreed with statements linking key population groups to “being ashamed” and having “engaged in irresponsible behavior,” especially in relation to women who sell sex and MSM. Agreement was common, but less so, in relation to young women who get pregnant before marriage, but was relatively uncommon in relation to PLHIV. Fewer health workers reported that key populations did not “deserve access to health services as much as other people,” or stated that they “would prefer not to provide services” to key population groups. In relation to these statements, there were fewer differences between PLHIV and other groups; in other words, irrespective of social and health condition identity, key populations were considered to have a right to health care services by the majority of health workers. However, CHWs, including the CHiPS, employed by the HPTN071 (PopART) study, were more likely than HFS to report that “other people deserve access to health services more than the key population group.”
Education level and perceptions of coworker behaviors toward PLHIV and each of the key populations were associated with holding judgmental beliefs. More educated health workers were more likely not to link “shame” and “irresponsible behavior” with PLHIV, while linking both attributes with other key populations. Health workers who reported stigma among coworkers were more likely to report judgmental views toward PLHIV and key populations. We found inconsistent patterns of association between sex, age, religion, HIV status and testing, and judgmental and stigmatizing attitudes across the four key populations. Training experience was not associated with judgmental attitudes for any of the key populations.
Ours was a large and novel study of stigma among health workers. We compared responses to questions about PLHIV and key population groups, and between different cadres of health workers involved in the delivery of HIV services. Our analyses, while robust, have some limitations. They are reflective of the inherent difficulties when assessing stigma, particularly in health facilities in high HIV prevalence settings where many health workers may be living with, or affected by, HIV in their personal lives. Health workers may misreport stigmatizing or judgmental views.31 Despite multiple efforts to contact every eligible health worker, our participant rates were quite low in some groups, reflecting the complexity of conducting this kind of research with health workers. It is difficult to compare the response rate of participants in our study to other similar studies because these studies used different populations (often only medical students, or only nurses), and sometimes did not report response rates.32,34–38
Some health workers opted not to answer questions about attitudes toward women who sell sex and MSM, perhaps reflecting discomfort or embarrassment with the wording of questions. Consequently, there may be some biases in our data, perhaps with fewer people holding stigmatizing attitudes choosing to respond. In Zambia, it is also illegal for MSM and anecdotally some participants reported that this made it hard to answer the questions comfortably. This raises questions about the contextual differences that may drive stigma in different countries and how they might have influenced our findings, and other similar studies measuring stigma toward PLHIV and key populations. The study was conducted in 21 purposively selected communities participating in the trial, and caution is warranted in considering how these results may be reflective of broader patterns of stigma. To truly understand the role that stigma plays in health worker interactions with PLHIV and key populations, it is necessary to understand why health worker attitudes are the way they are, which means understanding the mechanisms that drive their behaviors. There is a wide body of literature that seeks to understand such mechanisms through theoretical frameworks of the acceptability of interventions.39 Acceptability is the belief or consideration from those involved in the health care intervention that the intervention is appropriate, or good, based on their anticipated or experienced responses or reactions to the intervention.39 Understanding health workers within this intervention using a framework such as this one might help to uncover underlying social and contextual factors, which may be essential for developing appropriate and effective stigma reduction interventions.
Our study is limited in that it measures stigmatizing attitudes and beliefs against knowledge about HIV and key populations, as well as training on providing care. Other factors such as social and cultural norms and job satisfaction are not assessed in the present study, and these may heavily influence health workers (HW) feelings about the acceptability of the intervention, which in turn might influence the way they think about or treat clients.
We found that there were high levels of judgment toward key population groups, but lower levels in relation to PLHIV, among all cadres of health workers in both countries. This agrees with other literatures that seek to measure intersectional stigma.23,24 Agreement with statements about PLHIV was generally lower than previous literature has suggested.40 Our data may be consistent with reports that stigma toward PLHIV is reducing over time as testing and treatment expand. Normalization and increased tolerance of HIV in settings where UTT approaches are used have been reported.21
The HPTN 071 (PopART) intervention, being universal and implemented across whole communities, hopes to “avoid stigmatization, and should encourage community-wide support for HIV prevention and care.”29 Such interventions can help to reduce fear through increasing awareness about stigma and about PLHIV. Longitudinal cohort data from our study present a unique opportunity to track these dynamics.28 However, recent research from South Africa has indicated that normalization might not always occur.41 Stigma toward key population groups may be more resistant to change. Within our study, this was particularly notable in Zambian communities, and in relation to MSM. Zambia has a stronger moralizing culture than South Africa as noted in wider qualitative research,25 and pronounced prejudice toward MSM endorsed by law.42 This demonstrates a need for program and policy changes that specifically aim to address stigma toward key populations. These changes could happen at several levels, including at the policy level (i.e., national laws that protect lesbian, gay, bisexual, transgender, and queer (LGBTQ) populations against discrimination, and those that decriminalize sex work), community level (i.e., through mass sensitization campaigns and education), or at the organizational level (i.e., training on human rights and culturally competent care for key populations).
The stigma reduction framework outlined by Nyblade et al. suggests that increased awareness about stigmatizing behaviors toward PLHIV, reducing fear surrounding HIV, and understanding how to provide nonstigmatizing care to clients are fundamental for reducing stigma.43 This framework could be applied to key populations and scaled up to address the inherent stigmas that these populations face. Further, the main drivers of stigma and the mechanisms, which instigate stigmatizing behaviors from health workers, will be influenced by the social norms about key populations, as well as gender, and attitudes toward LGBTQ populations. A key goal for future research will be to understand how social and cultural norms such as these can be changed so that stigma does not persist in environments outside the health setting in different country contexts.
Anticipated stigma from health workers might act as a barrier to people accessing treatment and prevention services.8,44 We found that despite high levels of judgment, health workers were less likely to link this to whether PLHIV or key population groups deserve access to services, or whether they themselves would prefer not to provide such services. Nevertheless, 10–20% of participants did express these views in relation to key population groups. It will be important to consider over time whether the presence of judgmental attitudes acts as a barrier to PLHIV or other groups accessing services.
It was interesting that community health workers, who generally had lower levels of formal education than other groups, were more likely to agree that key population groups were less deserving of services than other health worker cadres. Interventions such as those in the HPTN 071 (PopART) study offered a chance to build on wider tolerance and empathy toward PLHIV and extend this to other key populations, and this may be an important consideration if the intervention were to be rolled out and/or replicated.35 A study of medical students in Malaysia found that clinical encounters with PLHIV were associated with higher knowledge about HIV and lower stigmatizing attitudes.36 Similar results were seen in a study of health care providers in Ethiopia.32 Nevertheless, anticipated negative perceptions from health workers can hinder a person's access to HIV services.11,12,45 Qualitative interviews with members of key population groups collected as part of our ongoing study will provide deeper insight into key population perceptions and experiences of how they are treated. The level of stigmatizing attitudes toward key populations may have hindered or lessened the effectiveness of the HPTN 071 (PopART) interventions.
For those PLHIV who know their status, intersecting stigma about living with HIV and being a member of a key population could undermine accessing key HIV treatment and prevention services. As such, members of key populations might not benefit from normalization of HIV among the wider public. We noted also that health workers' judgmental beliefs were associated with their perceptions of coworker behaviors, as in other studies.34,37 This might be because health workers are influenced by their peers, or because they believe peers hold the same beliefs as they do. Stigma reduction activities within health settings might work best when reaching all staff working in a health facility, and workplace-based antistigma campaigns might benefit from peer-led interventions and activities in an effort to facilitate a more tolerant environment.
Our findings highlight several factors within health settings, and based on HWs' previous interactions with PLHIV and key populations, but they do not interrogate the contextual or societal factors that might heavily contribute to HW attitudes, perceptions, and beliefs. To understand if and how stigma among HWs drives HIV testing and treatment, it is essential to understand the wider context in which they exist. This will be useful for the development of effective interventions to reduce stigma among this and other populations.
Supplementary Material
Contributor Information
Collaborators: on behalf of the HPTN 071 (PopART) Study Team
Author Disclosure Statement
No competing financial interests exist.
Funding Information
HPTN 071 (PopART) is sponsored by the National Institute of Allergy and Infectious Diseases (NIAID) under Cooperative Agreements UMq-AI068617 and UM1-AI068613, with funding from the US President's Emergency Plan for AIDS Relief (PEPFAR). Additional funding is provided by the International Initiative for Impact Evaluation (3ie) with support from the Bill and Melinda Gates Foundation, as well as by NIAID, the National Institute on Drug Abuse (NIDA), and the National Institute of Mental Health (NIMH), all part of NIH. The stigma ancillary study was funded by NIMH. Janet Seeley is part funded by the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement and is also part of the EDCTP2 programme supported by the European Union. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAID, NIMH, NIDA, PEPFAR, 3ie, or the Bill and Melinda Gates Foundation. S.K., T.P., A.S., and J.R.H. are members of the STRIVE consortium, which produces research on the structural drivers of HIV, including stigma. The STRIVE consortium is funded by UKaid from the Department for International Development (http://strive.lshtm.ac.uk). However, the views expressed do not necessarily reflect the department's official policies.
Supplementary Material
References
- 1. UNAIDS. Getting to Zero 2011–2015 Strategy Joint United Nations Programme on HIV/AIDS. Geneva, Switzerland: UNAIDS; 2010 [Google Scholar]
- 2. UNAIDS. The Gap Report. Geneva, Switzerland: UNAIDS; 2013 [Google Scholar]
- 3. Hayes RJ, Donnell D, Floyd S, et al. Effect of universal testing and treatment on HIV incidence—HPTN 071 (PopART). N Engl J Med 2019;381:207–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Infect Dis 2012;12:538–549 [DOI] [PubMed] [Google Scholar]
- 5. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol 2001;27:363–385 [Google Scholar]
- 6. Maughan-Brown B. Stigma rises despite antiretroviral roll-out: A longitudinal analysis in South Africa. Soc Sci Med 2010;70:368–374 [DOI] [PubMed] [Google Scholar]
- 7. Gari S. Doig-Acuña C, Smail T, Malungo JR, Martin-Hilber A, Merten S. Access to HIV/AIDS care: A systematic review of socio-cultural determinants in low and high income countries. BMC Health Serv Res 2013;13:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J Int AIDS Soc 2013;16(3 Suppl. 2):18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Musheke M, Ntalasha H, Gari S, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health 2013;13:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. UNAIDS. UNAIDS Guidance Note on HIV and Sex Work. Geneva, Switzerland: UNAIDS; 2012 [Google Scholar]
- 11. Letamo G. The discriminatory attitudes of health workers against people living with HIV. PLoS Med 2005;2:e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: What works? J Int AIDS Soc 2009;12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Reis RK, Galvao MT, Gir E. Challenges to an effective response for addressing stigma and discrimination related to HIV: From denial of rights to construction of support networks. J Int AIDS Soc 2013;16:18931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Uys L, Holzemer WL, Chirwa ML, et al. The development and validation of the HIV/AIDS Stigma Instrument-Nurse (HASI-N). AIDS care 2009;21:150–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alemu T, Biadgilign S, Deribe K, Escudero HR. Experience of stigma and discrimination and the implications for healthcare seeking behavior among people living with HIV/AIDS in resource-limited setting. Sahara J 2013;10:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mtetwa S, Busza J, Chidiya S, Mungofa S, Cowan F. “You are wasting our drugs”: Health service barriers to HIV treatment for sex workers in Zimbabwe. BMC Public Health 2013;13:698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Uys L, Chirwa M, Kohi T, et al. Evaluation of a health setting-based stigma intervention in five African countries. AIDS Patient Care STDS 2009;23:1059–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS 2008;22(Suppl. 2):S67–S79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moshabela M, Zuma T, Orne-Gliemann J, et al. “It is better to die”: Experiences of traditional health practitioners within the HIV treatment as prevention trial communities in rural South Africa (ANRS 12249 TasP trial). AIDS Care 2016;28(Suppl. 3):24–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reynolds LJ, Camlin CS, Ware NC, Seeley J. Exploring critical questions for the implementation of “universal test and treat” approaches to HIV prevention and care. AIDS Care 2016;28(Suppl. 3):1–6 [DOI] [PubMed] [Google Scholar]
- 21. Hayes R, Sabapathy K, Fidler S. Universal testing and treatment as an HIV prevention strategy: Research questions and methods. Curr HIV Res 2011;9:429–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bond V, Nomsenge S, Mwamba M, et al. “Being seen” at the clinic: Zambian and South African health worker reflections on the relationship between health facility spatial organisation and items and HIV stigma in 21 health facilities, the HPTN 071 (PopART) study. Health Place 2019;55:87–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hargreaves JR, Busza J, Mushati P, Fearon E, Cowan FM. Overlapping HIV and sex-work stigma among female sex workers recruited to 14 respondent-driven sampling surveys across Zimbabwe, 2013. AIDS Care 2017;29:675–685 [DOI] [PubMed] [Google Scholar]
- 24. Kennedy CE, Baral SD, Fielding-Miller R, et al. “They are human beings, they are Swazi”: Intersecting stigmas and the positive health, dignity and prevention needs of HIV-positive men who have sex with men in Swaziland. J Int AIDS Soc 2013;16(Suppl. 3):18749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bond V, Hoddinott G, Viljoen L, Simuyaba M, Musheke M, Seeley J. Good health and moral responsibility: Key concepts underlying the interpretation of treatment as prevention in South Africa and Zambia before rolling out universal HIV testing and treatment. AIDS Patient Care STDS 2016;30:425–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Geter A, Herron AR, Sutton MY. HIV-related stigma by healthcare providers in the United States: A systematic review. AIDS Patient Care STDS 2018;32:418–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Leserman J, Ironson G, O'Cleirigh C, Fordiani JM, Balbin E. Stressful life events and adherence in HIV. AIDS Patient Care STDS 2008;22:403–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hargreaves JR, Stangl A, Bond V, et al. HIV-related stigma and universal testing and treatment for HIV prevention and care: Design of an implementation science evaluation nested in the HPTN 071 (PopART) cluster-randomized trial in Zambia and South Africa. Health Policy Plan 2016;31:1342–1354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hayes R, Ayles H, Beyers N, et al. HPTN 071 (PopART): Rationale and design of a cluster-randomised trial of the population impact of an HIV combination prevention intervention including universal testing and treatment—A study protocol for a cluster randomised trial. Trials 2014;15:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shanaube K, Schaap A, Floyd S, et al. What works—Reaching universal HIV testing: Lessons from HPTN 071 (PopART) trial in Zambia. AIDS 2017;31:1555–1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nyblade L, Jain A, Benkirane M, et al. A brief, standardized tool for measuring HIV-related stigma among health facility staff: Results of field testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. J Int AIDS Soc 2013;16(3 Suppl. 2):18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Feyissa GT, Abebe L, Girma E, Woldie M. Stigma and discrimination against people living with HIV by healthcare providers, Southwest Ethiopia. BMC Public Health 2012;12:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hossain MB, Kippax S. Stigmatized attitudes toward people living with HIV in Bangladesh: Health care workers' perspectives. Asia Pac J Public Health 2011;23:171–182 [DOI] [PubMed] [Google Scholar]
- 34. Waluyo A, Culbert GJ, Levy J, Norr KF. Understanding HIV-related stigma among Indonesian nurses. J Assoc Nurses AIDS Care 2015;26:69–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chan KY, Stoové MA, Sringernyuang L, Reidpath DD. Stigmatization of AIDS patients: Disentangling Thai nursing students' attitudes towards HIV/AIDS, drug use, and commercial sex. AIDS Behav 2008;12:146–157 [DOI] [PubMed] [Google Scholar]
- 36. Chew BH, Cheong AT. Assessing HIV/AIDS knowledge and stigmatizing attitudes among medical students in Universiti Putra Malaysia. Med J Malaysia 2013;68:24–29 [PubMed] [Google Scholar]
- 37. Chirwa ML, Greeff M, Kohi TW, et al. HIV stigma and nurse job satisfaction in five African countries. J Assoc Nurses AIDS Care 2009;20:14–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jin H, Earnshaw VA, Wickersham JA, et al. An assessment of health-care students' attitudes toward patients with or at high risk for HIV: Implications for education and cultural competency. AIDS Care 2014;26:1223–1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. NZP+ and GNP+. People Living with HIV Stigma Index Zambia Country Assessment 2009. Lusaka: NZP+; 2011 [Google Scholar]
- 41. Orne-Gliemann J, Zuma T, Chikovore J, et al. Community perceptions of repeat HIV-testing: Experiences of the ANRS 12249 Treatment as Prevention trial in rural South Africa. AIDS Care 2016;28(Suppl. 3):14–23 [DOI] [PubMed] [Google Scholar]
- 42. Simpson A, Bond V. Narratives of Nationhood and HIV/AIDS: Reflections on Multidisciplinary Research on the HIV/AIDS Epidemic in Zambia over the Last 30 Years. J South Afr Stud 2014;40:1065–1089 [Google Scholar]
- 43. Nyblade L, Srinivasan K, Mazur A, et al. HIV stigma reduction for health facility staff: Development of a blended-learning intervention. Front Public Health 2018;6:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS 2007;21:584–592 [DOI] [PubMed] [Google Scholar]
- 45. Reis C, Heisler M, Amowitz LL, et al. Discriminatory attitudes and practices by health workers toward patients with HIV/AIDS in Nigeria. PLoS Med 2005;2:e246. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.