Abstract
Background
The four approaches to hysterectomy for benign disease are abdominal hysterectomy (AH), vaginal hysterectomy (VH), laparoscopic hysterectomy (LH) and robotic‐assisted hysterectomy (RH).
Objectives
To assess the effectiveness and safety of different surgical approaches to hysterectomy for women with benign gynaecological conditions.
Search methods
We searched the following databases (from inception to 14 August 2014) using the Ovid platform: Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; EMBASE; Cumulative Index to Nursing and Allied Health Literature (CINAHL) and PsycINFO. We also searched relevant citation lists. We used both indexed and free‐text terms.
Selection criteria
We included randomised controlled trials (RCTs) in which clinical outcomes were compared between one surgical approach to hysterectomy and another.
Data collection and analysis
At least two review authors independently selected trials, assessed risk of bias and performed data extraction. Our primary outcomes were return to normal activities, satisfaction, quality of life, intraoperative visceral injury and major long‐term complications (i.e. fistula, pelvi‐abdominal pain, urinary dysfunction, bowel dysfunction, pelvic floor condition and sexual dysfunction).
Main results
We included 47 studies with 5102 women. The evidence for most comparisons was of low or moderate quality. The main limitations were poor reporting and imprecision.
Vaginal hysterectomy (VH) versus abdominal hysterectomy (AH) (nine RCTs, 762 women)
Return to normal activities was shorter in the VH group (mean difference (MD) ‐9.5 days, 95% confidence interval (CI) ‐12.6 to ‐6.4, three RCTs, 176 women, I2 = 75%, moderate quality evidence). There was no evidence of a difference between the groups for the other primary outcomes.
Laparoscopic hysterectomy (LH) versus AH (25 RCTs, 2983 women)
Return to normal activities was shorter in the LH group (MD ‐13.6 days, 95% CI ‐15.4 to ‐11.8; six RCTs, 520 women, I2 = 71%, low quality evidence), but there were more urinary tract injuries in the LH group (odds ratio (OR) 2.4, 95% CI 1.2 to 4.8, 13 RCTs, 2140 women, I2 = 0%, low quality evidence). There was no evidence of a difference between the groups for the other primary outcomes.
LH versus VH (16 RCTs, 1440 women)
There was no evidence of a difference between the groups for any primary outcomes.
Robotic‐assisted hysterectomy (RH) versus LH (two RCTs, 152 women)
There was no evidence of a difference between the groups for any primary outcomes. Neither of the studies reported satisfaction rates or quality of life.
Overall, the number of adverse events was low in the included studies.
Authors' conclusions
Among women undergoing hysterectomy for benign disease, VH appears to be superior to LH and AH, as it is associated with faster return to normal activities. When technically feasible, VH should be performed in preference to AH because of more rapid recovery and fewer febrile episodes postoperatively. Where VH is not possible, LH has some advantages over AH (including more rapid recovery and fewer febrile episodes and wound or abdominal wall infections), but these are offset by a longer operating time. No advantages of LH over VH could be found; LH had a longer operation time, and total laparoscopic hysterectomy (TLH) had more urinary tract injuries. Of the three subcategories of LH, there are more RCT data for laparoscopic‐assisted vaginal hysterectomy and LH than for TLH. Single‐port laparoscopic hysterectomy and RH should either be abandoned or further evaluated since there is a lack of evidence of any benefit over conventional LH. Overall, the evidence in this review has to be interpreted with caution as adverse event rates were low, resulting in low power for these comparisons. The surgical approach to hysterectomy should be discussed and decided in the light of the relative benefits and hazards. These benefits and hazards seem to be dependent on surgical expertise and this may influence the decision. In conclusion, when VH is not feasible, LH may avoid the need for AH, but LH is associated with more urinary tract injuries. There is no evidence that RH is of benefit in this population. Preferably, the surgical approach to hysterectomy should be decided by the woman in discussion with her surgeon.
Plain language summary
Surgical approach to hysterectomy for benign gynaecological diseases
Review question
Cochrane authors evaluated which is the most effective and safe surgery for hysterectomy in women with benign gynaecological disease.
Background
Hysterectomy for benign gynaecological disease, mostly abnormal uterine bleeding, prolapse or uterine fibroids, is one of the most frequent gynaecological procedures (30% of women by the age of 60; 590,000 procedures annually in the USA). It can be performed through several approaches. Abdominal hysterectomy involves removal of the uterus through an incision in the lower abdomen. Vaginal hysterectomy involves removal of the uterus via the vagina, without an abdominal incision. Laparoscopic hysterectomy involves 'keyhole surgery' through small incisions in the abdomen. The uterus may be removed vaginally or, after morcellation (cutting it up), through one of the small incisions. There are various types of laparoscopic hysterectomy, depending on the extent of the surgery performed laparoscopically compared to that performed vaginally. More recently, laparoscopic hysterectomy has been performed robotically. In robotic surgery, the operation is done by a robot, while the (human) surgeon steers the robot from a chair in the corner of the operating room. It is important to be well informed about the relative benefits and harms of each approach to make best informed choices for each woman needing hysterectomy for a benign disease.
Study characteristics
We analysed 47 randomised controlled trials (RCTs). A RCT is a type of study in which the people being studied are randomly allocated one or other of the different treatments being investigated. This type of study is usually the best way to evaluate whether a treatment is truly effective, i.e. truly helps the patient. A systematic review systematically summarises the available RCTs on a subject.
A total of 5102 women participated. Comparisons were vaginal versus abdominal hysterectomy (nine trials, 762 women), laparoscopic versus abdominal hysterectomy (25 trials, 2983 women), laparoscopic versus vaginal hysterectomy (16 trials, 1440 women) and laparoscopic versus robot‐assisted hysterectomy (two trials, 152 women); in addition there were studies in which three comparisons were made (four trials, 410 women). There were also studies included in which different types of laparoscopic hysterectomies were compared, including single‐port versus multi‐port (three trials, 203 women), total laparoscopic hysterectomy versus laparoscopic‐assisted vaginal hysterectomy (one trial, 101 women) and mini‐laparoscopic versus conventional laparoscopic hysterectomy (one trial, 76 women). The main outcomes were return to normal activities, satisfaction, quality of life and surgical complications.
Key results
We found that vaginal hysterectomy resulted in a quicker return to normal activities than abdominal hysterectomy. There was no evidence of a difference between them for our other main outcomes.
Laparoscopic hysterectomy also resulted in a quicker return to normal activities than abdominal hysterectomy. However, laparoscopic hysterectomies had a greater risk of damaging the bladder or ureter. There was no evidence of a difference between laparoscopic and vaginal hysterectomy or between laparoscopic and robot‐assisted hysterectomy for our main outcomes.
We conclude that vaginal hysterectomy should be performed whenever possible. Where vaginal hysterectomy is not possible, both a laparoscopic approach and abdominal hysterectomy have their pros and cons and these should be incorporated in the decision‐making process.
The evidence is current to August 2014.
Quality of the evidence
The evidence for most comparisons was of low or moderate quality. The main limitations were poor reporting of study methods and wide confidence intervals around the estimate of effect.
Summary of findings
Background
Description of the condition
Hysterectomy is the surgical removal of the uterus. It is the most frequently performed major gynaecological surgical procedure, with millions of procedures performed annually throughout the world (Garry 2005). Hysterectomy can be performed for benign and malignant indications. Approximately 90% of hysterectomies are performed for benign conditions, such as fibroids causing abnormal uterine bleeding (Flory 2005). Other indications include endometriosis/adenomyosis, dysmenorrhoea, dyspareunia and prolapse.
Abnormal menstrual bleeding affects women of all ages and is the most common gynaecological reason for referral to secondary care (Spencer 1999). There are a variety of potential causes for abnormal or heavy menstrual bleeding; these include the abovementioned fibroids, endometrial polyps of hyperplasia, adenomyosis, infectious diseases, (early) pregnancy complications or (pre)malignant conditions of the endometrium. However, in a large proportion of women no definitive diagnosis will be confirmed. Several more or less invasive therapies exist for heavy menstrual bleeding; oral contraceptives or the levonorgestrel‐releasing intrauterine system (LNG‐IUS) are often offered as a first‐line treatment when uterine abnormalities are ruled out. A recent review showed that the LNG‐IUS is the first‐line medical therapy for heavy menstrual bleeding, with combined hormonal contraceptives as second choice (Lethaby 2015). During the last decade, several new techniques for endometrial ablation have been developed. The effectiveness of these techniques has been described in another Cochrane review (Lethaby 2013). As a result of this variety of treatment options, a patient with heavy menstrual bleeding finds herself confronted with a wide range of possible medical and surgical interventions. Since hysterectomy is the only treatment that provides permanent symptom relief, a rather large proportion of women with the abovementioned conditions will eventually choose to have their uterus removed. This is demonstrated by the fact that rates of hysterectomy have declined less than expected with the introduction of new treatment modalities (Pynnä 2014).
Description of the intervention
Approaches to hysterectomy may be broadly categorised into four options: abdominal hysterectomy (AH); vaginal hysterectomy (VH); laparoscopic hysterectomy (LH) where at least some of the operation is conducted laparoscopically (Garry 1994), and robotic‐assisted hysterectomy (RH).
Abdominal hysterectomy: The AH has traditionally been the surgical approach for gynaecological malignancy, when other pelvic pathology is present such as endometriosis or adhesions, and in the context of an enlarged uterus. It remains the 'fallback option' if the uterus cannot be removed by another approach. Mini‐AH refers to an approach to hysterectomy where the abdominal incision does not exceed 7 cm (Sesti 2008a).
Vaginal hysterectomy: VH was originally used only for prolapse but has become more widely utilised for menstrual abnormalities such as dysfunctional uterine bleeding, when the uterus has a fairly normal size. Compared to AH, VH was (and still is) regarded as less invasive and seems to have the advantages of fewer blood transfusions, less febrile morbidity (fever) and less risk of injury to the ureter. However, the disadvantages are more bleeding complications and greater risk of bladder injury (Mäkinen 2013; Moen 2014a).
Laparoscopic hysterectomy: LH usually refers to a hysterectomy where at least part of the operation is undertaken laparoscopically (Garry 1994). This approach requires general laparoscopic surgical expertise. The proportion of hysterectomies performed by LH has gradually increased and, although the surgery tends to take longer, its proponents argue that the main advantages are the possibility of diagnosing and treating other pelvic diseases such as endometriosis, of carrying out adnexal surgery including the removal of the ovaries, the ability to secure thorough intraperitoneal haemostasis (direct laparoscopic vision enables careful sealing of bleeding vessels at the end of the procedure), and a more rapid recovery time from surgery compared to AH (Garry 1998). Three sub‐categorisations of LH have been described (Reich 2003), as follows:
Laparoscopic‐assisted vaginal hysterectomy (LAVH) is where part of the hysterectomy is performed by laparoscopic surgery and part vaginally, but the laparoscopic component of the operation does not involve division of the uterine vessels.
Laparoscopic hysterectomy (which we have abbreviated to LH(a)) is where the uterine vessels are ligated laparoscopically but part of the operation is performed vaginally.
Total laparoscopic hysterectomy (TLH) is where the entire operation (including suturing of the vaginal vault) is performed laparoscopically and there is no vaginal component except for the removal of the uterus. TLH requires the highest degree of laparoscopic surgical skills.
Single‐port laparoscopic hysterectomy and mini‐laparoscopic hysterectomy: In the last decade, single‐port laparoscopic hysterectomy (SP‐LH) and mini‐laparoscopic hysterectomy (mini‐LH, where the incisions do not exceed 3 mm, Ghezzi 2011) have been introduced into the endoscopic field.
Robotic‐assisted hysterectomy: RH has been performed since 1998. In this review RH is considered as a separate approach, which may have its own learning curve, surgical pitfalls and accompanying costs.
A total hysterectomy is the removal of the entire uterus including the cervix. When the cervix is not removed this is known as a subtotal or supracervical hysterectomy. Subtotal hysterectomies are most easily performed abdominally or laparoscopically, although it is possible to conserve the cervix in a VH or LAVH (Lethaby 2012).
The first reported elective hysterectomy was performed through a vaginal approach by Conrad Langenbeck in 1813. The first elective abdominal hysterectomy, a subtotal operation (where the cervix was conserved), was performed by Charles Clay in Manchester in 1863 (Sutton 1997). These approaches remained the only two options until the latter part of the 20th century. The first laparoscopic hysterectomy (LAVH) was reported by Harry Reich in 1989 (Reich 1989). He also reported the first total laparoscopic hysterectomy (TLH) in 1993. Robotic‐assisted hysterectomies have been performed since 1998.
Several patient factors may influence the surgeon's choice of approach to hysterectomy. For example, multiparous women with heavy menstrual bleeding who opt for hysterectomy may well be suitable for a vaginal approach. However, in the same case but with the suspicion of endometriosis based on dysmenorrhoea, dyspareunia or both, the surgeon will more likely be inclined to an abdominal or laparoscopic approach. With regards to enlarged myomatous uteri, surgeons' experience and skills will largely determine the surgical approach to hysterectomy.
In common with the overall hysterectomy rate, the proportion of hysterectomies currently being performed by different approaches varies markedly across countries, within countries, and even between individual surgeons working within the same unit. As mentioned, each gynaecologist will have different indications for the approach to hysterectomy for benign disease, based largely on their own array of surgical skills and the patient characteristics such as uterine size and descent, extra‐uterine pelvic pathology, previous pelvic surgery and other features such as obesity, nulliparity and the need for oophorectomy. Even though VH has been widely considered to be the operation of choice for abnormal uterine bleeding, the VALUE study has shown that, in 1995 in the UK, 67% of the hysterectomies performed for this indication were AH (Maresh 2002). Previous caesarean section, for example, is often considered to be a contraindication for VH. However, this is not supported by cumulative data from four studies indicating no significant difference in complication rates in hysterectomy patients following caesarean section (8 of 430 (1.86%) versus 11 of 1227 (0.89%), P value = 0.12) (Agostini 2005).
Mäkinen 2001 reported a prospective study on the learning curve in 10,110 hysterectomies for benign indications, of which 5875 were AH, 1801 were VH and 2434 were LH. As far as injuries to adjacent organs were concerned, the surgeons' experience significantly correlated inversely with the occurrence of urinary tract injuries in LH and the occurrence of bowel injuries in vaginal hysterectomy. In a following study the overall complication rates fell significantly in LH and markedly in VH over the course of 10 years (Mäkinen 2013). Encouraging vaginal surgery amongst gynaecologists has been shown to be an effective method of increasing VH rates (Mäkinen 2013; Moen 2014a). Finland had a VH rate as low as 7% in the 1980s. Following annual meetings on gynaecological surgery where vaginal and laparoscopic surgery were encouraged, and individual training provided, the VH rate increased to 44% in 2006 (Mäkinen 2013). In the same period of time, ureter injuries decreased, which represents an impressive national learning curve. In addition, the rate of LH increased (from 24% to 36%), with decreasing complication rates (Mäkinen 2013).
How the intervention might work
This review will focus on the benefits and harms of the different surgical approaches to hysterectomy for benign indications. From the patient's perspective, quality of life may well be the most important outcome, especially in surgery for benign indications. Consequently, we will choose patient‐reported outcome measures (PROMs) as primary outcomes. Injuries to adjacent organs are of concern in hysterectomy and their rates of occurrence differ with the various approaches to hysterectomy and surgical experience level (Brummer 2011; Mäkinen 2001; Mäkinen 2013). It is important to have adequate knowledge of the differences in adverse outcomes in several approaches to hysterectomy, in order to inform patients properly and to gain informed consent based on an adequate amount of data. Furthermore, operation times differ with the different approaches to hysterectomy. Longer operating times are even more likely with RH. In general it is presumed that the vaginal and laparoscopic approach will lead to a quicker recovery compared with open surgery, mainly because of less pain and quicker mobilisation due to smaller incisions.
In the current era of limited healthcare resources, the costs of surgery will likely play a more important role in decision making. Several studies have looked at the subject of the cost‐effectiveness of several types of hysterectomy (Bijen 2009; Pynnä 2014; Sarlos 2010; Tapper 2014). Overall, it is expected that VH will have the lowest costs, followed by AH and LH. Due to the high purchase costs and the use of expensive disposables, RH is likely to be the least cost‐effective. However, there is lack of well‐designed studies that also take societal costs (e.g. the costs of sick leave) into consideration.
Apart from the surgical approach to hysterectomy, other aspects of the surgical technique may have an effect on the outcome of surgery. Examples of this include total versus subtotal (where the cervix is not removed) hysterectomy (Lethaby 2012); Doderlein VH or LAVH versus standard VH or LAVH; techniques to support the vaginal vault; bilateral elective oophorectomy versus ovarian conservation (Orozco 2014); and other strategies used mainly by those conducting laparoscopic surgery with the aim of reducing the likelihood of complications, including the use of vaginal delineators, rectal probes and illuminated ureteric stents. These other aspects are not within the scope of this review (other than for assessing trial quality).
Why it is important to do this review
Since there are multiple approaches to hysterectomy, each with their procedure‐specific advantages and disadvantages, it is important to know which procedure is superior with respect to patient‐related outcomes. In general, randomised controlled trials (RCTs) deliver the highest quality of evidence. When the quality of RCTs of surgical interventions is sufficiently good, this yields information unrivalled in its quality compared to studies of other designs that assess surgical interventions. It was interesting to note that in 1998 there was not a single RCT comparing AH and VH (Garry 1998). The introduction of the newer approaches to hysterectomy (LH, SP‐LH and RH) has stimulated much greater interest in the scientific evaluation of all forms of hysterectomy. However, the more approaches exist, the more complex it becomes to decide on the best approach for each individual woman. This decision cannot be made without up‐to‐date evidence. Nor can it be made without knowing and respecting the informed preferences of patients. This review summarises the existing evidence presented in all published RCTs on benign conditions for hysterectomy. After finding and appraising the existing evidence, and integrating its inferences with clinical expertise, clinicians need to attempt a decision that reflects their patient's values and circumstances (Hoffmann 2014). This is an update of a Cochrane review first published in 2004, and previously updated in 2006, 2008 and 2009.
Objectives
To assess the effectiveness and safety of different surgical approaches to hysterectomy for women with benign gynaecological conditions.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), in which one surgical approach to hysterectomy was compared to another approach.
We excluded non‐randomised studies, as they are associated with a higher risk of bias.
Types of participants
Studies of women undergoing hysterectomy for benign disease (uterine fibroids, heavy menstrual bleeding, metrorrhagia of (suspicion of) adenomyosis) were eligible for inclusion. We excluded studies of women with gynaecological cancer. When trials included both women with benign and malignant disease, we requested from the authors a breakdown of data in order to include only women with benign disease. If this information was not forthcoming, we excluded the trial.
We defined dropouts as cases in which hysterectomy was cancelled after randomisation or randomised cases were excluded from analysis by the researchers. We did not regard loss to follow‐up as dropout.
Types of interventions
Surgical approaches to removal of the uterus, where at least one approach was compared with another, were eligible for inclusion. Approaches were as follows:
Abdominal hysterectomy (AH, including mini‐AH): AH involves removal of the uterus through an incision in the lower abdomen.
Vaginal hysterectomy (VH): VH involves removal of the uterus via the vagina, with no abdominal incision.
Laparoscopic hysterectomy (LH, including mini‐LH and single‐port (SP)‐LH): LH involves the use of laparoscopy to perform hysterectomy. We made the distinction between the subcategories of LH based on whether ligation of the uterine vessels was undertaken laparoscopically and whether suturing of the vaginal vault was undertaken vaginally (see Table 4) and this is further explained in the Background section. Thus we further subdivided LH in the analysis into LAVH, LH(a), TLH and non‐categorisable LH (where there is insufficient information or the types of LH are too heterogeneous to otherwise sub‐categorise). There are two other main classifications of LH available in the literature (Nezhat 1995; Richardson 1995) and these are summarised in Table 5 and Table 6, but we did not use these in the meta‐analysis. We defined SP‐LH as LH through one single port. Mini‐LH involves the approach to LH through ports not exceeding 3 mm.
Robotic hysterectomy (RH): RH involves a hysterectomy approach using a robotic system, allowing more ergonomic movements that are easier to perform and are more precise in filtering tremor. One surgeon is seated in a robot console and handles the laparoscope and two to three laparoscopic instruments. RH is generally performed in a similar fashion to a TLH with suturing of the vaginal vault via the robot.
1. Sub‐categorisation of laparoscopic hysterectomy.
| Type of LH | LH versus AH RCTs | LH versus VH RCTs | LH versus LH RCTs |
| LAVH | Ferrari 2000 | Agostini 2006 | Chen 2011 |
| Kunz 1996 | Ottosen 2000 | Roy 2011 | |
| Marana 1999 | Roy 2011 | Song 2013 | |
| Muzii 2007 | Roy 2012 | ||
| Ottosen 2000 | Sesti 2008(a) | ||
| Raju 1994b | Sesti 2008(b) | ||
| Sesti 2008(a) | |||
| Tsai 2003 | |||
| LH(a) | Ellstrom 1998 | Darai 2001 | |
| Falcone 1999 | Hwang 2002 | ||
| Harkki‐Siren 2000 | Soriano 2001 | ||
| Hwang 2002 | Summitt 1992 | ||
| Langebrekke 1998 | Zhu 2009 | ||
| Olsson 1996 | |||
| Persson 2006 | |||
| Schutz 2002 | |||
| Seracchioli 2002 | |||
| Summitt 1998 | |||
| Yuen 1998 | |||
| Zhu 2009 | |||
| TLH | Kluivers 2007 | Candiani 2009 | Ghezzi 2011 |
| Perino 1999 | Ghezzi 2010 | Jung 2011 | |
| Ribeiro 2003 | Morelli 2007 | Paraiso 2013 | |
| Ribeiro 2003 | Roy 2011 | ||
| Roy 2011 | Sarlos 2012 | ||
| Non‐categorisable LH | Garry 2004 | Garry 2004 | |
| Kongwattanakul 2012 | Richardson 1998 | ||
| Lumsden 2000 |
AH: abdominal hysterectomy LAVH: laparoscopic‐assisted vaginal hysterectomy LH: laparoscopic hysterectomy RCT: randomised controlled trial TLH: total laparoscopic hysterectomy VH: vaginal hysterectomy
2. Staging of laparoscopic hysterectomy ‐ Richardson 1995.
| Stage | Laparoscopic content |
| 0 | Laparoscopy done but no laparoscopic procedure before vaginal hysterectomy |
| 1 | Procedure includes laparoscopic adhesiolysis and/or excision of endometriosis |
| 2 | Either or both adnexa freed laparoscopically |
| 3 | Bladder dissected from the uterus laparoscopically |
| 4 | Uterine artery transected laparoscopically |
| 5 | Anterior and/or posterior colpotomy or entire uterus freed laparoscopically |
3. Steps of laparoscopic hysterectomy ‐ Nezhat 1995.
| Step | Laparoscopic content |
| 1 | Severing the round ligaments and dissection of the upper portion of the broad ligament |
| 2 | Severing the tubo‐uterine junction and the utero‐ovarian ligament if the adnexa are to be preserved, or severing the infundibulopelvic ligaments |
| 3 | Severing the uterine vessels |
| 4 | Preparation of the bladder flap |
| 5 | Severing the cardinal uterosacral ligaments complex |
| 6 | Performing anterior and posterior culdotomy and separation of the cervix |
| 7 | Closure of the vaginal cuff |
We thus excluded trials comparing, for example, different vessel sealing techniques within one approach.
Subtotal versus total hysterectomy is the scope of another Cochrane review (Lethaby 2012); we excluded trials making this comparison from the present review. We also excluded trials evaluating different surgical approaches to subtotal hysterectomy. However, if a minority of the women (less than 33%) had a subtotal hysterectomy and the comparison was made versus any of the three approaches outlined above then we included the trial.
Clinical data had to be reported in the included studies, thus excluding studies reporting only differences in laboratory results. If no relevant clinical outcomes were reported (i.e. not in the methods and results section), this was a criterion for exclusion.
Types of outcome measures
We assessed the following outcomes:
Primary outcomes
Return to normal activities
Satisfaction and quality of life
-
Intra‐operative visceral injury
Bladder injury
Ureter injury
Urinary tract (bladder or ureter) injury
Bowel injury
Vascular injury
-
Major long‐term complications
Fistula
Pelvi‐abdominal pain
Urinary dysfunction
Bowel dysfunction
Pelvic floor condition (prolapse)
Sexual dysfunction
Secondary outcomes
Operation time
Other intra‐operative complication
-
(Sequelae of) bleeding, including
Substantial bleeding
Transfusion
Pelvic haematoma
Unintended laparotomy for approaches not involving routine laparotomy
-
-
Short‐term outcomes and complications
Length of hospital stay
-
Infections
Vaginal cuff
Abdominal wall or wound
Urinary tract infection
Chest infection
Febrile episodes or unspecified infections
Thromboembolism
Unintended laparotomy for approaches not involving routine laparotomy
-
Short‐term outcomes and complications
Length of hospital stay
-
Infections
Vaginal cuff
Abdominal wall or wound
Urinary tract infection
Chest infection
Febrile episodes or unspecified infections
Thromboembolism
Postoperative ileus
Wound dehiscence
Costs
We sought data on the cost of treatment but we intended to describe these data qualitatively and not to include the information in the meta‐analysis since 'cost' could be defined differently in different studies depending upon whether studies incorporate the cost of sequelae. Different healthcare systems could produce markedly different results.
We used all types of outcome measures for meta‐analysis or described them in the review. This included composite outcome measures.
Search methods for identification of studies
We searched for all published and unpublished RCTs in August 2014, without language restriction and in consultation with the Cochrane Menstrual Disorders and Subfertility Group (MDSG) Trials Search Co‐ordinator.
Electronic searches
We will repeat the search for trials every two years and update the review if new trials are found. We searched the following electronic databases, trial registers and websites: the Cochrane Menstrual Disorders and Subfertility Group (MDSG) Specialised Register of Controlled Trials, the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, PsycINFO and CINAHL (Cumulative Index to Nursing and Allied Health Literature). We combined the MEDLINE search with the Cochrane highly sensitive search strategy for identifying randomised trials, which appears in the Cochrane Handbook for Systematic Reviews of Interventions (Version 5.1.0 chapter 6, 6.4.11) (Higgins 2011). We combined the EMBASE, PsycINFO and CINAHL searches with trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN) (http://www.sign.ac.uk/methodology/filters.html#random).
The appendices display detailed search strategies, as follows:
Cochrane MDSG Specialised Register (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL) in all fields (on Ovid platform July 2014) (Appendix 2);
Ovid MEDLINE(R) (1946 to 2014 week 32) (Appendix 3);
EMBASE (1980 to 2014 Week 32) (Appendix 4);
CINAHL (Appendix 5);
Biological Abstracts (1969 to August 2008, not included in searches beyond 2008) (Appendix 6);
PsycINFO (1806 to August Week 1 2014) (Appendix 7).
Other electronic sources of trials included:
-
trial registers for ongoing and registered trials:
DARE (Database of Abstracts of Reviews of Effects) on The Cochrane Library (http://onlinelibrary.wiley.com/o/cochrane/cochrane_cldare_articles_fs.html);
Web of Knowledge (http://wokinfo.com/);
OpenGrey (http://www.opengrey.eu/);
LILACS (Literaturo Latino Americana e do Ciências da Saúde) database (http://regional.bvsalud.org/php/index.php?lang=en);
PubMed; and
Google Scholar.
We searched the Clinical Trials Register, a registry of federally and privately funded US clinical trials, with the same keywords only for the initial Cochrane review in 2006 (Appendix 8).
Searching other resources
We searched the reference lists of articles retrieved by the search and contacted experts in the field to obtain additional data. We handsearched relevant journals and conference abstracts that are not covered in the MDSG register in liaison with the Trials Search Co‐ordinator.
Data collection and analysis
Selection of studies
Two review authors performed an initial screen of titles and abstracts retrieved by the search. We retrieved the full texts of all potentially eligible studies. Two review authors independently examined these full‐text articles for compliance with the inclusion criteria and selected studies eligible for inclusion in the review.
At least two of four review authors (ET, EC, AL, NJ) performed the selection of trials for inclusion in the initial Cochrane review (Johnson 2005b). Two different review authors (TN and KK) performed the selection of trials for the first update in 2009 (Nieboer 2009) and three review authors (JA, TN and KK) performed this for the current update.
We corresponded with study investigators as required, to clarify study eligibility. We resolved disagreements as to study eligibility by discussion or by referral to a third review author.
We documented the selection process with a PRISMA flow chart (Figure 1).
1.
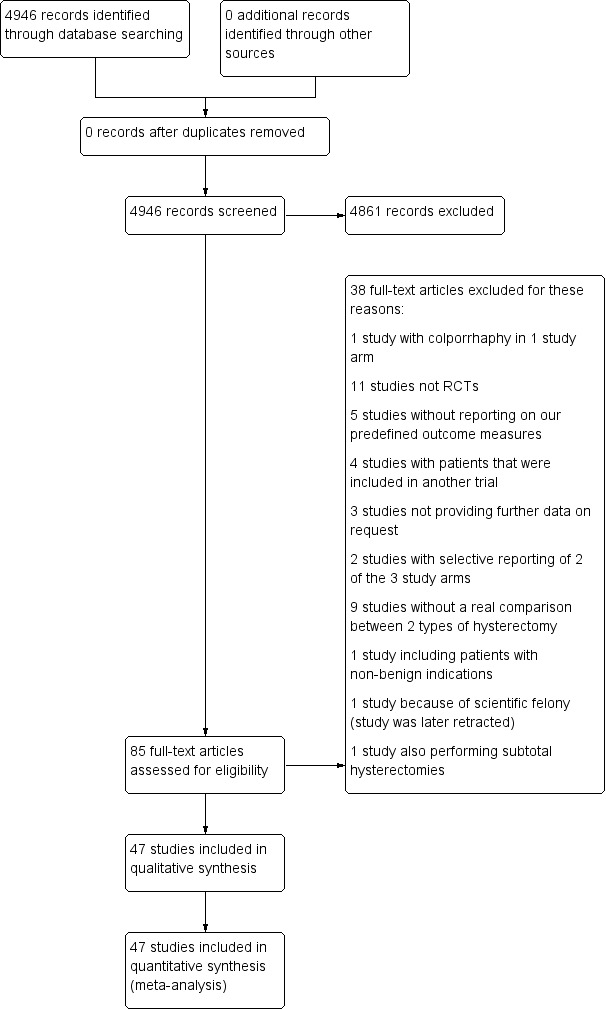
Study flow diagram.
We excluded trials from the review if they made comparisons other than those specified above. A selection of these trials is detailed in the table Characteristics of excluded studies. Classically we excluded studies if they did not report on differences in clinical outcomes, but did report laboratory results or different anaesthesia techniques or sealing techniques of vessels (e.g. electrosurgical bipolar vessel sealing) in hysterectomy patients. Trials are reported in the table Characteristics of excluded studies if there are other reasons for exclusion than those mentioned above.
Data extraction and management
Two review authors (at least two review authors from ET, EC, AL, NJ, TN, JA, KK) independently extracted data from eligible studies using a data extraction form designed and pilot‐tested by the authors. We resolved any disagreements by discussion or by referral to a third review author. Data extracted included study characteristics and outcome data (see data extraction table for details, Appendix 9). Where studies had multiple publications we collated multiple reports of the same study, so that each study rather than each report is the unit of interest in the review, and such studies have a single study ID with multiple references. We corresponded with study investigators for further data on methods, results or both, as required.
Assessment of risk of bias in included studies
Two review authors (at least two review authors from ET, AL, TN, JA and KK) independently assessed the included studies for risk of bias using the Cochrane 'Risk of bias' assessment tool (Higgins 2011) for: selection bias (random sequence generation and allocation concealment); performance bias (blinding of participants and personnel); detection bias (blinding of outcome assessors); attrition bias (incomplete outcome data); reporting bias (selective reporting); and other bias. We resolved disagreements by discussion or by referral to a third review author. We described all judgements fully and presented the conclusions in the 'Risk of bias' tables, which we incorporated into the interpretation of the review findings by means of sensitivity analyses (see below).
If randomisation and allocation concealment were not sufficiently reported, we labelled these as unclear or high risk of bias (depending on the extent of description and whether the method described was satisfactory).
If blinding was not performed or not reported, we judged this as high risk of bias.
We considered dropout rates and/or loss to follow‐up below 5% as low risk of bias. If dropouts or losses to follow‐up were not reported or were between 10% and 15%, we judged this as unclear risk of bias. If the dropouts or losses to follow‐up were substantial (i.e. more than 15%), we labelled this as high risk of bias.
If primary and/or secondary outcomes were not (pre)defined and/or a selection of outcomes was reported, we labelled this as unclear or high risk of bias.
Finally, we evaluated the studies included for any other potential bias, such as baseline data not comparable between groups or no description of surgeon experience. (Lack) of surgeon's experience could be particularly important when interpreting the results on, for instance, adverse events or operation time. This seems particularly important for the laparoscopic procedures, as studies have suggested that this technique has a specific learning curve. However, there is no clear‐cut consensus based on current evidence as to how many procedures a surgeon needs to perform (for all types of hysterectomies) to pass this learning curve. Therefore, if a study stated that a surgeon had sufficient experience (without mentioning a specific number) we did not consider this as a potential risk of bias. Depending on the extent of any other bias identified in the study, we judged this as unclear or high risk of bias. If three or more potential other biases were identified, we marked this as high risk of bias.
Measures of treatment effect
We performed statistical analysis in accordance with the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We analysed the data using an intention‐to‐treat model, where data were available.
We expressed dichotomous data as the numbers of events in the control and intervention groups of each study and calculated Mantel‐Haenszel odds ratios (OR) with 95% confidence intervals (95% CI). An increase in the odds of a particular outcome is displayed graphically in the meta‐analyses to the right of the centre line, and a decrease in the odds of an outcome is displayed graphically to the left of the centre line.
For continuous data (e.g. length of hospital stay), if all studies reported exactly the same outcomes, we calculated the mean difference (MD) between treatment groups. If similar outcomes were reported on different scales (e.g. change in haemoglobin), we calculated the standardised mean difference (SMD). We reversed the direction of effect of individual studies, if required, to ensure consistency across trials. We treated ordinal data (e.g. quality of life scores) as continuous data. We presented 95% CIs for all outcomes.
Where data to calculate ORs or MDs were not available, we utilised the most detailed numerical data available that facilitated similar analyses of included studies (e.g. test statistics, median and (interquartile) ranges, P values). We did not repeat or check values of skewness or kurtosis from the individual studies. We did not include outcome variables that were reported only graphically in the review. We compared the magnitude and direction of effect reported by studies with how they were presented in the review, taking account of legitimate differences.
Unit of analysis issues
The primary analysis was per woman randomised. We briefly summarised data that did not allow valid analysis (e.g. descriptive data) in additional tables and did not carry out meta‐analysis.
Dealing with missing data
We assessed the included studies for the number of women lost to follow‐up and exclusions from analysis after randomisation (dropouts). We did not impute missing variables for meta‐analysis.
Assessment of heterogeneity
We considered whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary. We assessed statistical heterogeneity by the measure of the I2 statistic. We took an I2 measurement greater than 50% to indicate substantial heterogeneity (Higgins 2003; Higgins 2011).
Where statistical heterogeneity (i.e. I2 > 50%) was apparent after pooling of data, we noted this and interpreted statistically significant results cautiously after further analysis using a random‐effects statistical model.
Assessment of reporting biases
In view of the difficulty of detecting and correcting for publication bias and other reporting biases, we aimed to minimise their potential impact by ensuring a comprehensive search for eligible studies and by being alert for duplication of data. If there were 10 or more studies in an analysis, we planned to use a funnel plot to explore the possibility of small study effects (a tendency for estimates of the intervention effect to be more beneficial in smaller studies).
Data synthesis
We stratified the analyses by the type of comparison and the subcategories within hysterectomy approaches.
We used a fixed‐effect model to calculate a pooled estimate of effect in meta‐analyses. If significant statistical heterogeneity was confirmed by the I2 statistic (I2 > 50%), we used a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We analysed the overall category laparoscopic hysterectomy (LH) and, where possible, the sub‐categorisation of LH (Table 4).
We took any statistical heterogeneity into account when interpreting the results, particularly if there was any variation in the direction of effect. Where there was substantial heterogeneity (I2 > 50%), we considered whether this was related to the subcategory of approach to hysterectomy.
Sensitivity analysis
We performed sensitivity analyses to examine the stability of the results in relation to the following factors.
Exclusion of trials that we judged as at unclear risk of bias with regard to adequate sequence generation in the 'Risk of bias' table.
Exclusion of trials comparing a surgical approach performed by one surgeon (or group of surgeons) with another surgical approach performed by a second (group of) surgeon(s).
The effect of analysing studies of LH subcategories compared to studies of LH pooled as an overall category.
Assessment of quality of evidence
We created Summary of findings tables and measured and reported the overall quality of the evidence for the primary outcomes (return to normal activities, urinary tract, bowel and vascular injuries, bleeding and unintended laparotomy) based on the GRADE criteria. We classified the quality of the evidence for each comparison as high, moderate, low or very low (Guyatt 2008).
Results
Description of studies
Results of the search
In our initial search, we identified 4946 articles. Of these, 85 articles were potentially eligible and we retrieved them in full text. We identified nine of these as published abstracts from conference proceedings. The data from two abstracts were published in RCTs included in this review (Cucinella 2000; Hahlin 1994), and we included two studies after additional information was received from the authors (Darai 2001; Miskry 2003). We excluded two studies because they proved not to be randomised studies (Møller 2001; Park 2003). For three studies no inclusion or exclusion decision could be made because insufficient information was available (and there was no response to our request for additional information on study design) (Davies 1998; Pabuccu 1996; Petrucco 1999).
We included 47 studies that met our inclusion criteria. We excluded 36 further studies from the review for reasons that are listed in the Characteristics of excluded studies table. We identified no additional studies through searching reference lists. See the study tables: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification and the PRISMA flow chart (Figure 1).
Where Olsson 1996 is mentioned in the review, we have used the data from Ellstrom 1998b where applicable. The eVALuate trial population was studied in two papers (Garry 2004; Sculpher 2004), and study quality was summarised under Garry 2004. There were two more studies on different outcomes and outcome measures from the same randomised study population: Persson 2006 and Persson 2008 were summarised under Persson 2006; and the long‐term follow‐up study by Nieboer 2012 was summarised under Kluivers 2007. Both Persson 2006 and Kluivers 2007 were already included in the 2009 update. One additional study was identified, which is awaiting classification (Sesti 2014).
Included studies
See Characteristics of included studies for an overview of the included studies.
Study design
All of the included trials had a parallel‐group design. Thirty‐seven of the trials were single‐centre studies (nine from Italy; two from Sweden; four from Taiwan; three from the USA; two each from the UK, Korea, China, India, Brazil, France and Germany; and one each from Finland, the Netherlands, Switzerland, Thailand and Hong Kong). Of the 10 multicentre trials, four trials recruited from two centres (Darai 2001 based in France; Langebrekke 1996 based in Norway; Miskry 2003 based in the UK; Paraiso 2013 based in the USA). Three trials recruited from three centres (Summitt 1998 based in the USA; Lumsden 2000 based in the UK; Muzii 2007 based in Italy). One trial from Italy recruited from four centres (Marana 1999); one Swedish trial recruited from five centres (Persson 2006); and a trial based in the UK with additional centres in South Africa (Garry 2004) recruited from 30 centres.
Participants
The 47 studies involved 5102 women.
The reported mean age of participants in the study groups ranged from 38 (Summitt 1992) to 55 years (Agostini 2006).
All of the included studies recruited women who needed a hysterectomy for benign causes; seven studies specifically included women who underwent hysterectomy for symptomatic uterine fibroids (Benassi 2002; Ferrari 2000; Hwang 2002; Long 2002; Ribeiro 2003; Sesti 2008a; Tsai 2003).
Vaginal hysterectomy (VH) versus abdominal hysterectomy (AH)
Benassi 2002 included women with symptomatic enlarged fibroid uteri. Silva Filho 2006 included women with myoma and a uterine size less than 300 cm3. Chakraborty 2011 and Miskry 2003 included women who needed hysterectomy for a benign condition.
Laparoscopic hysterectomy (LH) versus AH (including LH with bilateral salpingo‐oophorectomy (LH‐BSO) versus AH‐BSO, and LAVH versus minilaparotomy‐AH)
Fourteen of the 21 studies that compared LH with AH specifically included women who were scheduled for an abdominal hysterectomy or who had contraindications for a vaginal hysterectomy (Ellstrom 1998; Falcone 1999; Ferrari 2000; Harkki‐Siren 2000; Kluivers 2007; Kongwattanakul 2012; Lumsden 2000; Marana 1999; Muzii 2007; Olsson 1996; Seracchioli 2002; Summitt 1998; Tsai 2003; Yuen 1998).
LH (including all forms of LH) versus VH
Studies (n = 3) either included women if their uterine size was larger than a certain number (e.g. more than 280 g (Darai 2001; Soriano 2001) or between 300 g and 1500 g (Roy 2012)) or studies (n = 5) excluded women if their uterine size was greater than, for instance, 14 (Ghezzi 2010) or 16 weeks of pregnancy (Richardson 1995; Sesti 2008b; Summitt 1992). One study specifically included women with symptomatic or rapidly growing myoma (Sesti 2008b).
VH versus LH (vLH as it was called in the trial) and AH versus LH (aLH as it was called in the trial)
Garry 2004 included women scheduled for hysterectomy for non‐malignant conditions.
LH (including laparoscopic‐assisted vaginal hysterectomy (LAVH)) versus AH (including mini‐AH) versus VH
Four of the five trials specifically included women with uterine fibroids: e.g. leiomyomas of less than 15 cm (Ottosen 2000), leiomyomas of more than 8 cm and a maximum of three myomas (Hwang 2002), symptomatic myoma (Sesti 2008a), or any fibroid (Ribeiro 2003). The fifth study included women who were scheduled for hysterectomy with a uterine volume of 10 to 12 weeks of gestation and who had delivered at least one child (Zhu 2009).
Robotic‐assisted hysterectomy (RH) versus LH
Both Paraiso 2013 and Sarlos 2012 included patients who were scheduled for a hysterectomy for benign conditions. In Sarlos 2012, uterine weight had to be less than 500 g.
Single‐port laparoscopic hysterectomy (SP‐LH) versus LH
The three trials included women who had an indication for hysterectomy, no evidence of gynaecologic malignancy and an appropriate status for laparoscopic surgery (ASA 1 or 2) (Chen 2011; Jung 2011; Song 2013). Uterine size was also used as an exclusion criterion: more than 12 weeks gestation (Jung 2011); more than 20 weeks (Song 2013), and greater than 120 mm x 80 mm x 80 mm (Chen 2011).
LAVH versus total laparoscopic hysterectomy (TLH)
In Long 2002, women were included if they had contraindications for vaginal hysterectomy (a uterine weight greater than 280 g, previous pelvic surgery, pelvic inflammatory disease, need for adnexectomy, lack of uterine descent and limited vaginal access).
LAVH versus TLH versus VH
In Roy 2011, women were included if they had benign pathology of the uterus and medical therapy had failed.
LH versus mini‐LH
Ghezzi 2011 included women with benign gynaecological conditions requiring hysterectomy.
Interventions
Surgical procedures
VH versus AH (five trials)
Five trials compared VH with AH (Benassi 2002; Chakraborty 2011; Miskry 2003; Silva Filho 2006); one included a laparoscopic arm as well (Ottosen 2000). Hysterectomies were performed by standard technique for each route.
LH versus AH (21 trials)
Twenty‐one trials compared LH to AH (Ellstrom 1998; Falcone 1999; Ferrari 2000; Garry 2004; Harkki‐Siren 2000; Hwang 2002; Kluivers 2007; Kunz 1996; Langebrekke 1996; Lumsden 2000; Marana 1999; Muzii 2007; Perino 1999; Raju 1994; Ribeiro 2003; Seracchioli 2002; Sesti 2008a; Schutz 2002; Summitt 1998; Tsai 2003; Yuen 1998). These included four trials that randomised women to LH, AH and VH (Garry 2004; Hwang 2002; Ottosen 2000; Ribeiro 2003). Raju 1994 compared LH and bilateral salpingo‐oophorectomy (LH‐BSO) with AH‐BSO. Ellstrom 1998 stratified the two randomised groups (LH and AH) into total and subtotal hysterectomies. Muzii 2007 performed mini‐laparotomy for AH (with a moving surgical field or window using three separate retractors). Sesti 2008a compared LAVH and AH.
LH versus VH (10 trials)
Ten trials included a comparison of laparoscopic hysterectomy (LH) with vaginal hysterectomy (VH) (Agostini 2006; Candiani 2009; Darai 2001; Garry 2004; Ghezzi 2010; Richardson 1995; Roy 2012; Sesti 2008b; Soriano 2001; Summitt 1992), including four trials randomising women to LH, AH and VH and including the trial comparing TLH, LAVH and VH. Garry 2004 was a very large RCT comparing LH (called vLH in the trial) with VH and LH (called aLH in the trial) with AH; it was essentially two concurrent RCTs as part of the same study.
RH versus LH (two trials)
Paraiso 2013 and Sarlos 2012 compared conventional laparoscopic to robotically assisted hysterectomy.
SP‐LH versus LH (three trials)
Chen 2011 compared SP‐LAVH versus LAVH, whereas Jung 2011 and Song 2013 compared SP‐LH versus TLH.
LAVH versus TLH (one trial)
Long 2002 compared two types of laparoscopic hysterectomy, which was LAVH versus TLH.
LH versus mini‐LH (one trial)
Ghezzi 2011 compared two types of laparoscopic hysterectomy, which was mini‐LH versus LH.
LH subcategories
Although all the trials used variations of the terms 'laparoscopic‐assisted vaginal hysterectomy' (LAVH) or 'laparoscopic hysterectomy', their definition varied according to what stages of the hysterectomy were completed laparoscopically and the point at which the operation continued vaginally. We included all trials with hysterectomies that had some laparoscopic component in the overall LH category. Using the Richardson 1995 'Staging of laparoscopic hysterectomy' table (see Table 5) we were able to categorise 39 of the 45 included studies that involved LH according to the amount of laparoscopic content. We also subcategorised these trials involving LH as either LAVH, LH(a) or TLH, depending on the extent of the surgery performed either laparoscopically or vaginally (see Table 4). If any trial included women undergoing different Richardson LH stages in the LH arm, we arbitrarily categorised the stage firstly, as the stage to which the surgeons had intended to go; secondly, if that information was not available, to the LH stage that most women underwent surgery; or thirdly, to the most advanced LH stage that women underwent. According to Richardson staging, one trial involved stage zero LH (Ottosen 2000), four trials were stage two (Agostini 2006; Kunz 1996; Marana 1999; Raju 1994), nine trials were stage three (Chen 2011; Ferrari 2000; Muzii 2007; Roy 2011; Roy 2012; Sesti 2008a; Sesti 2008b; Song 2013; Tsai 2003), 10 trials were stage four where the uterine artery was transected laparoscopically (Darai 2001; Ellstrom 1998; Olsson 1996; Persson 2006; Schutz 2002; Soriano 2001; Summitt 1992; Summitt 1998; Yuen 1998; Zhu 2009), and 14 trials were stage five (Candiani 2009; Falcone 1999; Ghezzi 2010; Ghezzi 2011; Harkki‐Siren 2000; Hwang 2002; Jung 2011; Kluivers 2007; Langebrekke 1996; Paraiso 2013; Perino 1999; Ribeiro 2003; Sarlos 2012; Seracchioli 2002). For two trials we were unable to sub‐categorise the LH procedures and we described these as 'non‐categorisable LH' (Chakraborty 2011; Kongwattanakul 2012). Richardson 1995 had LHs of all stages from 0 to 5, and two trials did not stipulate the LH stages performed (Garry 2004; Lumsden 2000). In Long 2002, the LAVH treatment arm was a stage three whilst the TLH arm was a stage five.
Surgeons' experience
The surgeons' experience or level of training was reported in 33 of the trials. Eighteen of these trials specified that the same group of surgeons performed operations for both interventions (Benassi 2002; Candiani 2009; Chen 2011; Ghezzi 2010; Ghezzi 2011; Hwang 2002; Jung 2011; Kongwattanakul 2012; Lumsden 2000; Paraiso 2013; Roy 2011; Roy 2012; Sarlos 2012; Seracchioli 2002; Sesti 2008a; Sesti 2008b; Silva Filho 2006; Song 2013). In seven of these trials, the experience was specified in detail, e.g. in Candiani 2009 at least 50 of both procedures and in Jung 2011 at least 100 LH and 30 SP‐LH. In five trials, surgeons for one intervention were different to those performing the other intervention (Kluivers 2007; Langebrekke 1996; Long 2002; Olsson 1996; Raju 1994). In some trials the surgeons consisted only or partly of residents operating under supervision (e.g. Kluivers 2007; Ottosen 2000; Schutz 2002; Summitt 1998). In five trials specific information on surgical experience was lacking (Agostini 2006; Darai 2001; Falcone 1999; Perino 1999; Zhu 2009).
Outcomes
With respect to our primary outcomes, 16 studies reported on time needed to return to normal activities (Harkki‐Siren 2000; Hwang 2002; Langebrekke 1996; Miskry 2003; Olsson 1996; Ottosen 2000; Paraiso 2013; Persson 2006; Raju 1994; Richardson 1995; Roy 2011; Roy 2012; Sarlos 2012; Schutz 2002; Seracchioli 2002; Summitt 1998).
Two studies reported on satisfaction (Benassi 2002; Lumsden 2000), and seven studies reported on quality of life (Garry 2004; Kluivers 2007; Lumsden 2000; Olsson 1996; Persson 2006; Roy 2011; Silva Filho 2006). Song 2013 reported the cosmetic satisfaction after single‐port and multi‐port laparoscopic hysterectomy as primary outcome.
Twenty‐three studies reported on intra‐operative visceral injury (Benassi 2002; Chakraborty 2011; Darai 2001; Garry 2004; Jung 2011; Kluivers 2007; Kongwattanakul 2012; Langebrekke 1996; Long 2002; Lumsden 2000; Marana 1999; Olsson 1996; Ottosen 2000; Perino 1999; Persson 2006; Raju 1994; Ribeiro 2003; Richardson 1995; Roy 2011; Sarlos 2012; Summitt 1992; Summitt 1998; Tsai 2003).
Six studies reported on major long‐term complications (Long 2002; Lumsden 2000; Olsson 1996; Ottosen 2000; Perino 1999; Summitt 1992).
. Forty‐five trials assessed the length of postoperative hospital stay and 10 included an analysis of costs. An assessment of quality of life was reported in 11 trials; four trials included sexual activity or body image in the analysis (Candiani 2009; Garry 2004; Long 2002; Song 2013).
Most of the trials assessed the operation times and intra or postoperative complications. Lumsden 2000 and Garry 2004 split the complications into major and minor. Ellstrom 1998 reported on the difference in erythrocyte volume fraction. Febrile morbidity was measured in 13 trials, pulmonary function in one trial (Ellstrom 1998), and 12 trials reported any operations that were converted to abdominal surgery (Darai 2001; Garry 2004; Kluivers 2007; Marana 1999; Muzii 2007; Ottosen 2000; Persson 2006; Richardson 1995; Seracchioli 2002; Soriano 2001; Summitt 1992; Summitt 1998).
Excluded studies
See Characteristics of excluded studies for an overview of the excluded studies, including the reasons why they were excluded from the review.
Risk of bias in included studies
An overview of the risk of bias is provided in Figure 2 and Figure 3. Two studies fulfilled all criteria for adequate management of risk of bias (Ghezzi 2011; Miskry 2003). Several studies fulfilled all criteria, except one (Candiani 2009; Garry 2004; Ottosen 2000; Paraiso 2013; Schutz 2002; Sesti 2008a; Song 2013). Three studies met none of the criteria for adequate management of risk of bias (Long 2002, LH versus LAVH; Roy 2011, TLH versus LAVH versus VH; Roy 2012, LH versus VH; and Zhu 2009, AH versus LH versus VH).
2.
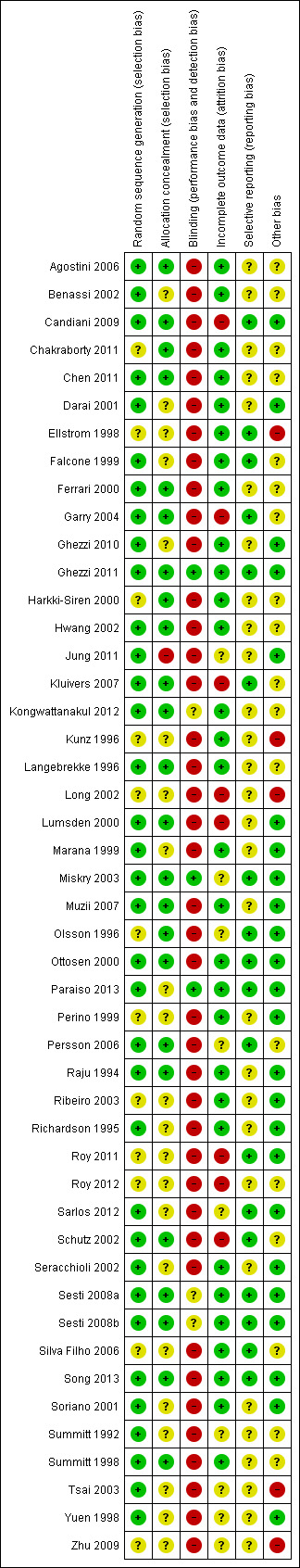
'Risk of bias' summary: review authors' judgements about each methodological quality item for each included study.
3.
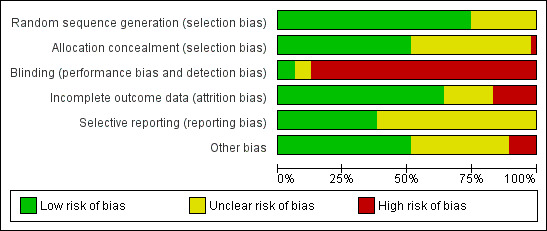
'Risk of bias' graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Allocation
Sequence generation
Seventeen studies randomised using a computer (Agostini 2006; Candiani 2009; Chen 2011; Ferrari 2000; Garry 2004; Ghezzi 2010; Ghezzi 2011; Hwang 2002; Miskry 2003; Muzii 2007; Ottosen 2000; Raju 1994; Schutz 2002; Sesti 2008a; Sesti 2008b; Song 2013; Summitt 1998). Langebrekke 1996 and Richardson 1995 used a table of random digits for randomisation. Ten trials used a computer‐generated randomisation code (Benassi 2002; Darai 2001; Falcone 1999; Lumsden 2000; Marana 1999; Seracchioli 2002; Soriano 2001; Summitt 1992; Roy 2012; Tsai 2003; Yuen 1998); one performed randomisation through a computer‐generated randomisation schedule with random block sizes (Paraiso 2013). Eleven trials did not report the randomisation method (Chakraborty 2011; Ellstrom 1998; Harkki‐Siren 2000; Jung 2011; Kunz 1996; Long 2002; Olsson 1996; Perino 1999; Ribeiro 2003; Roy 2011; Zhu 2009). Overall, we considered 35 studies to have low risk of bias and 12 studies to have unclear risk of bias.
Allocation concealment
Twenty studies used sealed, opaque envelopes (Agostini 2006; Candiani 2009; Chen 2011; Ferrari 2000; Ghezzi 2010; Ghezzi 2011; Harkki‐Siren 2000; Hwang 2002; Kluivers 2007; Langebrekke 1996; Miskry 2003; Muzii 2007; Olsson 1996; Ottosen 2000; Persson 2006; Raju 1994; Sesti 2008a; Sesti 2008b; Song 2013; Summitt 1998). For instance, Persson 2006 numbered the envelopes according to a random list, and Kluivers 2007 sealed the envelopes after which they were shuffled and numbered by a third party. Two trials used a telephone (Garry 2004; Schutz 2002). Twenty trials did not report whether allocation was concealed (Benassi 2002; Chakraborty 2011; Darai 2001; Ellstrom 1998; Falcone 1999; Jung 2011; Kunz 1996; Long 2002; Lumsden 2000; Marana 1999; Paraiso 2013; Perino 1999; Ribeiro 2003; Roy 2011; Seracchioli 2002; Soriano 2001; Summitt 1992; Roy 2012; Tsai 2003; Yuen 1998; Zhu 2009). We identified no studies as having high risk of bias; in 21 studies it was unclear and 26 studies had low risk of bias.
Blinding
One trial reported sham abdominal dressings until discharge from hospital after VH (Miskry 2003). Another trial comparing mini‐LH and LH covered the incisions with the same size of plasters (Ghezzi 2011). Paraiso 2013 reported blinding of patients for the intervention. In Kongwattanakul 2012 and Sesti 2008a, the researchers were blinded. One trial reported blinding of the interviewer one month after surgery (Silva Filho 2006). All other trials included in this review did not apply any blinding of participants, clinicians or researchers, resulting in high risk of performance and detection bias. Overall, three studies had low risk of bias, three unclear risk of bias and 41 studies high risk of bias.
Incomplete outcome data
We considered attrition bias low in 32 trials, unclear in seven trials and high in eight trials.
Dropouts
Twenty‐eight trials reported no dropouts. Nineteen trials reported dropouts, with the dropout rate ranging from 1.7% to 20%. Table 7 lists the trials that reported dropouts with the dropout circumstances. In five trials the dropouts were excluded from the data analysis (Long 2002; Lumsden 2000; Persson 2006; Summitt 1998; Yuen 1998), whereas the other three either included the data in the analysis where possible (Falcone 1999; Kluivers 2007; Paraiso 2013; Sarlos 2012), or performed a sensitivity analysis for the missing data (Garry 2004). Three trials had women withdraw pre‐operatively: Falcone 1999 (4 out of 48), Garry 2004 (34 out of 1380) and Persson 2006 (1 out of 119). In the Lumsden 2000 study, seven women withdrew pre‐operatively and case records were not available for three more. Two and one women respectively refused their assigned procedure in the Summitt 1998 and Kluivers 2007 studies; in the Yuen 1998 study, four women declined their assigned operation and a further two women refused to participate postoperatively. In the Long 2002 trial, excluded post‐randomisation were: three women undergoing conversion to laparotomy, seven with incomplete records and three with combined procedures. A further 53 were excluded because they did not have indications of uterine fibroids or adenomyosis. In the Persson 2006 trial, five patients allocated to AH and one to LH withdrew after giving informed consent prior to the operation or withdrew in the postoperative period before the five‐week follow‐up. In the Paraiso 2013 trial, six patients dropped out before the intervention was performed after randomisation. These were analysed in the allocated intervention arm.
4. Studies reporting dropouts.
| Trial | No. dropouts | Details |
| Chen 2011 | 2 | Excluded from analysis postoperatively, because they underwent accessory adnexal surgery |
| Falcone 1999 | 4 (1 LH; 3 AH) | Withdrew pre‐operatively |
| Garry 2004 | 34 (23 LH (11 aLH; 12 vLH); 6 AH; 5 VH) | Withdrew pre‐operatively |
| Long 2002 | 13 | 3 laparotomy conversions were excluded from analysis; 7 incomplete records; 3 combined procedures that were excluded post‐randomisation |
| Lumsden 2000 | 10 | 10 dropouts were not analysed. 7 women did not attend surgery and 3 records were not available |
| Kluivers 2007 | 1 | Refused assignment procedure |
| Lumsden 2000 | 10 | 7 withdrew pre‐operatively; 3 case records not available |
| Paraiso 2013 | 6 | 6 withdrew after randomisation but before the intervention was performed |
| Persson 2006 | 6 | 5 allocated to AH and 1 to LH withdrew after informed consent prior to the operation or withdrew in the postoperative period before the 5‐week follow‐up |
| Roy 2011 | 9 | 5 excluded because they needed adenectomy during surgery and 4 excluded from all analyses because they did not show up for follow‐up after intervention |
| Roy 2012 | 1 | 1 LH patient excluded from analysis due to conversion |
| Sarlos 2012 | 5 | After randomisation 5 did not complete the study and were excluded from the analysis |
| Song 2013 | 1 | 1 lost to follow‐up because of dissatisfaction with hospital care |
| Summitt 1998 | 2 | Refused assignment procedure |
| Yuen 1998 | 6 | 4 declined operation; 2 refused to participate postoperatively |
AH: abdominal hysterectomy aLH: laparoscopic cases in the abdominal arm of the eVALuate trial LH: laparoscopic hysterectomy VH: vaginal hysterectomy vLH: laparoscopic cases in the vaginal arm of the eVALuate trial
Loss to follow‐up
In eight trials the follow‐up period was not specified (and considered an unclear risk of bias), the number analysed in the follow‐up period was not reported, or the loss to follow‐up was between 5% to 10% of the patient population (Persson 2006; Sarlos 2012; Summitt 1992; Tsai 2003; Yuen 1998; Zhu 2009). Seven studies lost more than 10% of their patient population in the follow‐up period (Candiani 2009; Kluivers 2007; Long 2002; Lumsden 2000; Roy 2011; Roy 2012; Schutz 2002).
Intention‐to‐treat
Twenty‐eight trials reported no dropouts. Of the 19 RCTs reporting dropouts, seven reported analysis by intention‐to‐treat (ITT), defined as all randomised women reported upon according to their group of randomised allocation (Falcone 1999; Garry 2004; Kluivers 2007; Paraiso 2013; Persson 2006; Sarlos 2012; Sesti 2008a). The remaining RCTs reporting dropouts did not report ITT analysis of all randomised women. One further trial that had no dropouts did not analyse by ITT but according to the treatment received, which was different to the assigned treatment in two cases: the operation was converted from LH to AH and these women were analysed in the AH group (Tsai 2003).
Selective reporting
In 29 studies insufficient information was available to determine whether primary or secondary outcomes had been predefined. These studies had therefore an unclear risk of reporting bias. Eighteen studies had low risk of bias. We considered no studies to have a high risk of bias.
Other potential sources of bias
We judged the risk of potential other bias as follows: low risk of bias in 24 studies, unclear risk of bias in 17 studies and high risk of bias (three or more other potential sources of bias) in six studies.
Differences in baseline characteristics
In three studies, baseline characteristics between intervention groups were not comparable (Chakraborty 2011; Hwang 2002), or baseline characteristics were not reported (Kongwattanakul 2012). In Kluivers 2007, the AH group had more residents as a first surgeon than the other two groups. In the other studies no other bias could be identified. In the Long 2002 trial, women were randomised to treatment groups before a large number (i.e. 66) of the women were excluded. Therefore, the women in each treatment group may not have been a true representation of the original randomised groups.
Surgeon's experience
The surgeon's experience or level of training was reported in 30 of the trials and was not considered as a potential source of bias. In the remaining 17 studies the surgeon's experience was not reported or specified or varied substantially between groups. The studies by Benassi 2002, Chakraborty 2011, Chen 2011, Ellstrom 1998, Ferrari 2000, Hwang 2002, Kunz 1996 and Tsai 2003 did not report or specify the surgeon's experience for the interventions evaluated. In five trials, surgeons for one intervention were different to those performing the other intervention: Olsson 1996 (LH carried out by two out of five senior registrar grade surgeons trained in LH, AH carried out by two out of 10 senior registrar grade surgeons trained in AH); Langebrekke 1996 (LH performed exclusively by the two authors, AH performed by any skilled gynaecologist in the department); Raju 1994 (LAVH performed by one of the authors, AH by one of the authors or a senior registrar grade surgeon); Kluivers 2007 (LH was performed or supervised (resident 39%) by three out of 10 experienced gynaecologists (at least 100 LHs), AH performed or supervised by all 10 gynaecologists); and Long 2002 (one surgeon performed all LAVH, another performed all TLH). Residents were the first surgeon in 39% of LH and 88% of AH. In Agostini 2006, the five surgeons were experienced in vaginal surgery but laparoscopic experience was not reported. In Ottosen 2000, 15 gynaecological surgeons with assistants performed the operations; their experience varied and there were cases of residents performing operations under supervision. In Schutz 2002, 71% of LH were performed by the attending physician and 29% by a resident under supervision, and 40% of AH were performed by the attending physician and 60% by the resident under supervision. One trial used only gynaecological residents to perform all the operations with the assistance of the attending physician (Summitt 1998). It is unlikely that any of the latter three trials used the same group of surgeons for both intervention groups. In three other trials it was unclear if the surgeons performing the operations were different: Darai 2001 (all experienced in laparoscopic and vaginal surgery but no mention of who performed each intervention); Perino 1999 (LH by team of three laparoscopic surgeons with experience of more than 100 LHs, no details provided for AH arm); and Falcone 1999 (one of the senior authors performed all the LH operations with the assistance of a pelvic surgery fellow or resident, but no mention of the AH group). In four of the trials, surgeons of all grades and experience carried out the operations. In Garry 2004, each surgeon recruited to the trial had to have performed 25 of each procedure, however cases could be used for teaching if the main assistant was the designated surgeon.
Source of funding
Three studies received funding from pharmaceutical or surgical instrumentation companies: Falcone 1999 received part of the funding from Ethicon Endosurgery Inc; Harkki‐Siren 2000 received a part of its funding from the Research Foundation of the Orion Corporation; Summitt 1998 received all of its funding from US Surgical Corporation, USA.
Other bias
If a trial lacked information, such as a description of one of the interventions or details on the inclusion or exclusion criteria, we considered this a possible source of other bias.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. Vaginal hysterectomy versus abdominal hysterectomy for benign gynaecological disease.
| Vaginal hysterectomy versus abdominal hysterectomy for benign gynaecological disease | ||||||
| Patient or population: patients with benign gynaecological disease Settings: hospital Intervention: vaginal versus abdominal hysterectomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Abdominal hysterectomy | Vaginal hysterectomy | |||||
| Return to normal activities (days) | The mean return to normal activities (days) in the AH group was 42.7 days | The mean return to normal activities (days) in the VH group was 9.5 lower (12.6 to 6.4 lower) | — | 176 (3 studies) | ⊕⊕⊕⊝ moderate1 | — |
| Urinary tract (bladder or ureter) injury | 0 per 1000 | 0 per 1000 (0 to 0) | OR 3.09 (0.48 to 19.97) | 439 (4 studies) | ⊕⊕⊕⊝ moderate2,3 | There were no urinary tract injuries in one study |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AH: abdominal hysterectomy; CI: confidence interval; OR: odds ratio; VH: vaginal hysterectomy | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1There was a large difference in return to normal activities between the different studies; the analysis had high heterogeneity (I2 = 75%) but consistent direction of effect. 2In 2 studies there was doubt about the method used for random sequence generation. 3There were only three events altogether, all in the VH arms.
Summary of findings 2. Laparoscopic hysterectomy versus abdominal hysterectomy for benign gynaecological disease.
| Laparoscopic hysterectomy versus abdominal hysterectomy for benign gynaecological disease | ||||||
| Patient or population: patients with benign gynaecological disease Settings: hospital Intervention: laparoscopic versus abdominal hysterectomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Abdominal hysterectomy | Laparoscopic hysterectomy | |||||
| Return to normal activities (days) | The mean return to normal activities (days) in the AH group was 36.3 days | The mean return to normal activities (days) in the LH group was 13.6 lower (15.4 to 11.8 lower) | — | 520 (6 studies) | ⊕⊕⊝⊝ low1,2 | — |
| Urinary tract (bladder or ureter) injury | 10 per 1000 | 24 per 1000 (12 to 46) | OR 2.44 (1.24 to 4.80) | 2140 (13 studies) | ⊕⊕⊝⊝ low1,3 | — |
| Bowel injury | 7 per 1000 | 1 per 1000 (0 to 11) | OR 0.21 (0.03 to 1.33) | 1175 (4 studies) | ⊕⊕⊕⊝ moderate3 | — |
| Vascular injury | 9 per 1000 | 16 per 1000 (5 to 51) | OR 1.76 (0.52 to 5.87) | 956 (2 studies) | ⊕⊕⊕⊝ moderate3 | — |
| Bleeding | 16 per 1000 | 6 per 1000 (2 to 19) | OR 0.45 (0.15 to 1.37) | 1266 (5 studies) | ⊕⊕⊝⊝ low3,4 | — |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AH: abdominal hysterectomy; CI: confidence interval; LH: laparoscopic hysterectomy; OR: odds ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1In some studies there was doubt about the method used for random sequence generation or allocation of patients. Furthermore, one study did not perform an intention‐to‐treat analysis. 2There was a large difference in return to normal activities between the different studies; the analysis had moderate heterogeneity (I2 = 48%) but consistent direction of effect. 3Wide confidence intervals crossing the line of no effect. 4In some studies there was doubt about the method used for random sequence generation or allocation of participants.
Summary of findings 3. Laparoscopic hysterectomy versus vaginal hysterectomy for benign gynaecological disease.
| Laparoscopic hysterectomy versus vaginal hysterectomy for benign gynaecological disease | ||||||
| Patient or population: patients with benign gynaecological disease Settings: hospital Intervention: laparoscopic versus vaginal hysterectomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Vaginal hysterectomy | Laparoscopic hysterectomy | |||||
| Return to normal activities (days) | The mean return to normal activities (days) in the VH group was 25.2 days | The mean return to normal activities (days) in the LH group was 1.1 lower (4.2 lower to 2.1 higher) | — | 140 (2 studies) | ⊕⊕⊕⊝ moderate1 | — |
| Urinary tract (bladder or ureter) injury | 16 per 1000 | 16 per 1000 (6 to 42) | OR 1.0 (0.36 to 2.75) | 865 (7 studies) | ⊕⊕⊝⊝ low2,3 | — |
| Vascular injury | 12 per 1000 | 18 per 1000 (6 to 58) | OR 1.58 (0.48 to 5.27) | 745 (5 studies) | ⊕⊕⊝⊝ low3,4 | — |
| Bleeding | 29 per 1000 | 25 per 1000 (9 to 70) | OR 2.45 (0.38 to 15.78) | 644 (3 studies) | ⊕⊕⊝⊝ low3,5 | — |
| Unintended laparotomy | 24 per 1000 | 37 per 1000 (19 to 73) | OR 1.55 (0.76 to 3.15) | 1160 (10 studies) | ⊕⊕⊝⊝ low2,3 | — |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; LH: laparoscopic hysterectomy; OR: odds ratio; VH: vaginal hysterectomy | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Wide confidence intervals crossing the line of no effect. 2In some studies there was doubt about the method used for random sequence generation or allocation of patients. 3Wide confidence intervals crossing the line of no effect. 4In one study it was unclear how participants were allocated to their study group. 5In two studies it was unclear how participants were randomised and allocated.
1 Vaginal hysterectomy (VH) versus abdominal hysterectomy (AH)
Primary outcomes
1.1 Return to normal activities
For vaginal versus abdominal hysterectomy, patients returned to normal activities sooner after VH (mean difference (MD) ‐12.33, 95% confidence interval (CI) ‐19.89 to ‐4.77; three randomised controlled trials (RCTs), 176 women, I2 = 75%, moderate quality evidence) (Figure 4; Analysis 1.1).
4.
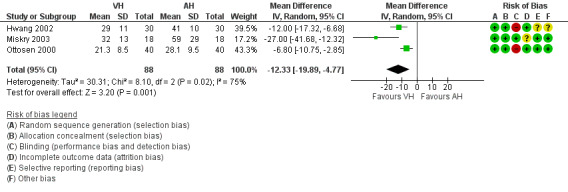
Forest plot of comparison: 1 VH versus AH, outcome: 1.1 Return to normal activities (days).
1.1. Analysis.
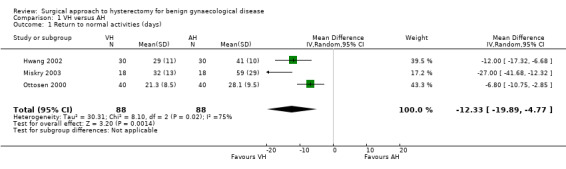
Comparison 1 VH versus AH, Outcome 1 Return to normal activities (days).
1.2 Satisfaction and quality of life
There was no evidence of a difference in patient satisfaction between vaginal and abdominal hysterectomy, although the point estimate clearly favoured VH (odds ratio (OR) 2.69, 95% CI 0.50 to 14.42, one RCT, 119 women, I2 = n/a, moderate quality evidence) (Analysis 1.2).
1.2. Analysis.
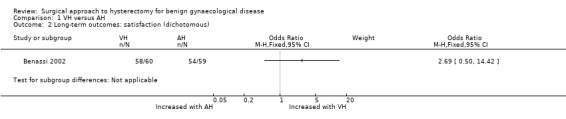
Comparison 1 VH versus AH, Outcome 2 Long‐term outcomes: satisfaction (dichotomous).
Silva Filho 2006 found better quality of life after vaginal hysterectomy, compared to abdominal hysterectomy, in the SF‐36 subscales for functional capacity (means VH versus AH: 95 versus 73), physical aspects (means VH versus AH: 100 versus 38), and pain (means VH versus AH: 84 versus 51). Additionally, a higher rate of patients who underwent vaginal hysterectomy would choose the same treatment again (Analysis 1.8).
1.8. Analysis.
Comparison 1 VH versus AH, Outcome 8 All outcomes, descriptive data.
| All outcomes, descriptive data | ||||
|---|---|---|---|---|
| Study | VH | AH | Comments | |
| Quality of life (descriptive data) | ||||
| Silva Filho 2006 | Questionnaire SF‐36. Only data from functional capacity, physical aspect and pain are presented. A high score is a better quality of life | n = 30 1 month after surgery, response rate 100% | n = 30 1 month after surgery, response rate 100% | Functional capacity: VH mean = 95, IQ‐range = 75 to 100. AH mean = 72.5, IQ‐range = 55 to 90
Physical aspect: VH mean = 100, IQ‐range = 25 to 100. AH mean = 37.5, IQ‐range = 0 to 100
Pain: VH mean = 84, IQ‐range = 59.2 to 100. AH mean = 51, IQ‐range = 41 to 65. A higher rate of patients in VH would choose the same therapeutic modality (90 % versus 65.5 %, P value = 0.021) |
| Operation time (descriptive data) | ||||
| Hwang 2002 | With 2nd procedure: median = 93 range = 80 to 110 n = 3 Without 2nd procedure: median = 74 range = 40 to 120 n = 27 | With 2nd procedure: median = 117 range = 90 to 190 n = 8 Without 2nd procedure: median = 98 range = 85 to 150 n = 22 | Not tested separately | |
| Miskry 2003 | Mean 68.8 (range 30 to 180) mins n = 18 | Mean 68.2 (range 45 to 174) mins n = 18 | — | |
| Ribeiro 2003 | Mean 78 mins n = 20 | Mean 109 mins n = 20 | No measure of spread stated | |
| Length of hospital stay (descriptive data) | ||||
| Hwang 2002 | n = 30 median = 4.7 days range (3 to 7) | n = 30 median = 5 days range (4 to 8) | Not tested separately | |
| Ribeiro 2003 | n = 20 All went home on second postoperative day | n = 20 All went home on third postoperative day | — | |
1.3 Intra‐operative visceral injury
There were three times as many urinary tract injuries after vaginal versus abdominal hysterectomy, although there was no evidence of a difference (OR 3.09, 95% CI 0.48 to 19.97, four RCTs, 439 women, I2 = 0%, moderate quality evidence) (Analysis 1.3). No ureter, bowel or vascular injuries occurred in either group.
1.3. Analysis.
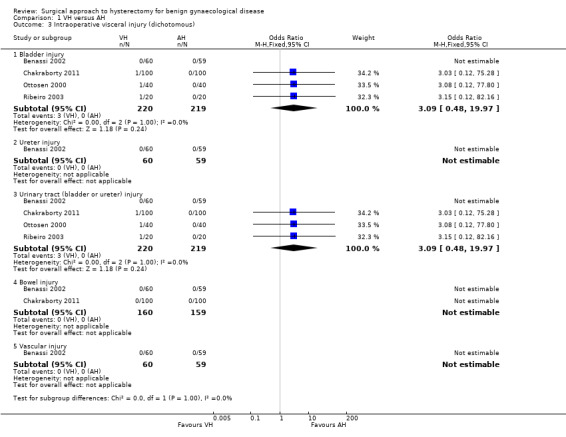
Comparison 1 VH versus AH, Outcome 3 Intraoperative visceral injury (dichotomous).
1.4 Major long‐term complications
No urinary dysfunction occurred in either group (OR n/a, one RCT, 80 women) (Analysis 1.4).
1.4. Analysis.
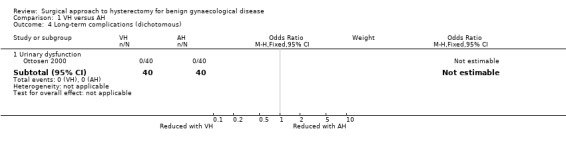
Comparison 1 VH versus AH, Outcome 4 Long‐term complications (dichotomous).
Fistula formation, pelvic‐abdominal pain, bowel dysfunction, pelvic floor condition (prolapse) and sexual dysfunction were not studied.
Secondary outcomes
1.5 Operation time
Four trials showed evidence of a difference: three in favour of vaginal hysterectomy, one in favour of abdominal hysterectomy (four RCTs, 359 women) (Analysis 1.5). The direction of the treatment effect differed amongst studies, therefore we did not pool the results.
1.5. Analysis.
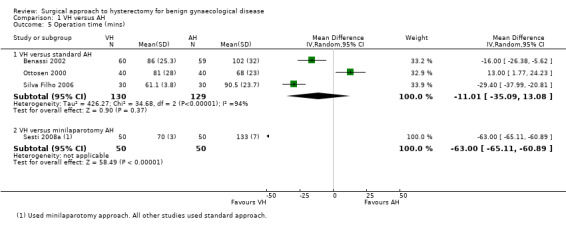
Comparison 1 VH versus AH, Outcome 5 Operation time (mins).
Three trials reported descriptive data on operation times for this comparison. The trial by Hwang 2002 reported data as a median and range and found a shorter median operating time for VH (74 minutes, range 40 to 120) versus AH (98 minutes, range 85 to 150). Miskry 2003 reported mean and range (VH 68.8 minutes (30 to 180) versus AH 68.2 minutes (45 to 174), whereas Ribeiro 2003 reported mean only (VH 78 minutes versus AH 109 minutes) (Analysis 1.8).
1.6 Intra‐operative complications (other than visceral injury)
There was no evidence of a difference between the groups in the need for blood transfusion (OR 0.82, 95% CI 0.34 to 1.96, five RCTs, 495 women, I2 = 19%) and occurrence of pelvic haematoma (OR 0.99, 95% CI 0.34 to 2.89, five RCT, 535 women, I2 = 0%) (Analysis 1.6).
1.6. Analysis.
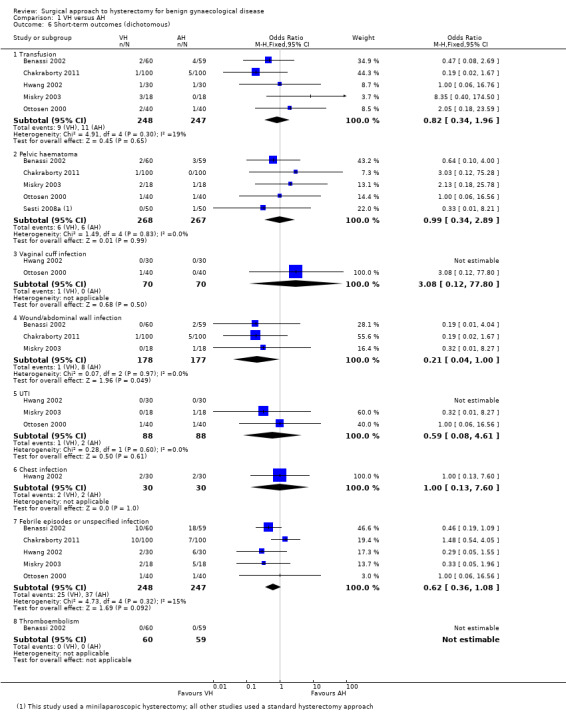
Comparison 1 VH versus AH, Outcome 6 Short‐term outcomes (dichotomous).
Substantial bleedings were not studied for this comparison.
Unintended laparotomy was not compared in meta‐analysis because AH involves routine laparotomy.
1.7 Short‐term outcomes and complications
Hospital stay was shorter in vaginal hysterectomy compared to standard abdominal hysterectomy (MD ‐1.07, 95% CI ‐1.22 to ‐0.92; four RCTs; 295 women; I2 = 0%) as well as compared to minilaparotomy AH (MD ‐2.10, 95% CI ‐2.19 to ‐2.01; one RCT; 100 women; I2 = n/a) (Analysis 1.7).
1.7. Analysis.
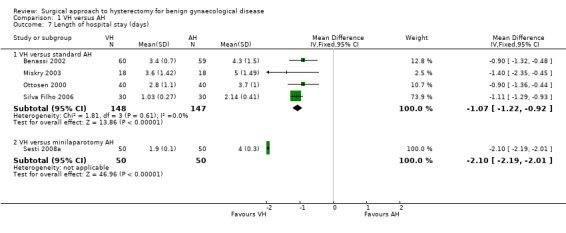
Comparison 1 VH versus AH, Outcome 7 Length of hospital stay (days).
Wound/abdominal wall infection (OR 0.21, 95% CI 0.04 to 1.00, three RCTs, 355 women, I2 = 0%), urinary tract infection (OR 0.59, 95% CI 0.08 to 4.61, three RCTs, 176 women, I2 = 0%) and febrile episodes or unspecified infections (OR 0.62, 95% CI 0.36 to 1.08, five RCTs, 495 women, I2 = 15%) all occurred less after VH than after AH, but there was no evidence of a difference. The number of women included in studies that reported on chest infection (OR 1.00, 95% CI 0.13 to 7.60, one RCT, 60 women, I2 = n/a) or low backache (OR 0.57, 95% CI 0.20 to 1.65, one RCT, 200 women, I2 = n/a) were too low to make meaningful comparisons. There were no thromboembolisms in either group (one RCT, 119 women) (Analysis 1.6).
No data on perioperative mortality, postoperative ileus and wound dehiscence were reported for this comparison.
1.8 Cost
No studies reported this outcome in this comparison.
2 Laparoscopic hysterectomy (LH) versus abdominal hysterectomy (AH)
Primary outcomes
2.1 Return to normal activities
Return to normal activities was quicker after laparoscopic‐assisted vaginal hysterectomy (LAVH) than after AH (MD ‐8.40, 95% CI ‐12.15 to ‐4.65; one RCT; 80 women; I2 = n/a) and was quicker after LH than after AH (MD ‐15.17, 95% CI ‐17.21 to ‐13.14; five RCTs; 440 women; I2 = 48%) (Analysis 2.1). One study reported only the mean days and did not find evidence of a difference (Schutz 2002). For three additional RCTs the data could not be pooled. Median duration of return to normal activities was shorter for LH in these three trials (Langebrekke 1996; Persson 2006; Raju 1994) (Figure 5; Analysis 2.1)
2.1. Analysis.
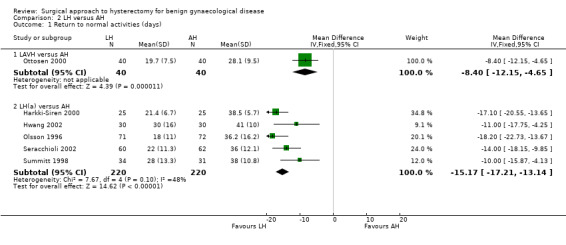
Comparison 2 LH versus AH, Outcome 1 Return to normal activities (days).
5.
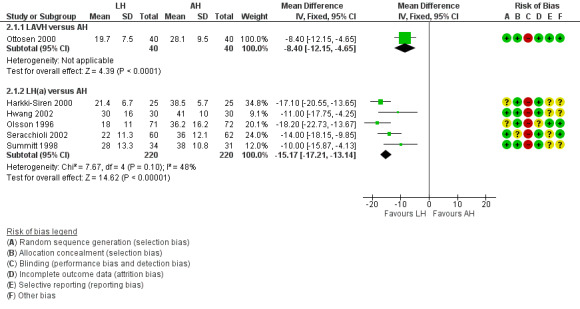
Forest plot of comparison: 2 LH versus AH, outcome: 2.1 Return to normal activities (days).
2.2 Satisfaction and quality of life
There was no evidence of a difference in patient satisfaction between LH and AH (OR 0.65, 95% CI 0.32 to 1.30, one RCT, 166 women, I2 = n/a, low quality evidence) (Lumsden 2000) (Analysis 2.2).
2.2. Analysis.
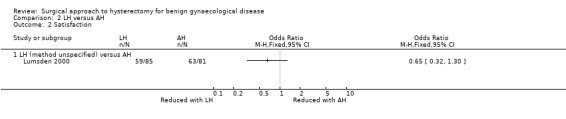
Comparison 2 LH versus AH, Outcome 2 Satisfaction.
For LH versus AH, Garry 2004 demonstrated that quality of life (measured by the SF12 scoring system) was better for LH at six weeks; body image was improved for LH versus AH at six weeks, but not at four and 12 months; and sexual frequency was higher at six weeks following LH. Kluivers 2007 found a treatment effect favouring LH in the RAND‐36 scale for vitality in the first 12 weeks postoperatively. In the long‐term follow‐up (four years) of Kluivers 2007, Nieboer 2012 found that the total RAND‐36 score favoured LH, as well as the RAND‐36 sub‐scale scores for vitality, physical functioning and social functioning. Lumsden 2000 used the EuroQol 5D thermometer, and there was no evidence of a difference at one month, six months or a year after surgery. Olsson 1996 asked the patients six to eight weeks after surgery whether the duration of postoperative hospital stay had been adequate and 9% (LH) versus 17% (AH) of patients reported that the stay had been too short. Persson 2006 applied four psychometric tests, but there was no evidence of a difference between the interventions in the first six months after surgery (Analysis 2.24).
2.24. Analysis.
Comparison 2 LH versus AH, Outcome 24 Long‐term outcomes: quality of life (descriptive data).
| Long‐term outcomes: quality of life (descriptive data) | ||||
|---|---|---|---|---|
| Study | Description | LH | AH | Comments |
| Garry 2004 | Questionnaire assessment of sexual activity, body image (BIS) and health status (SF‐12) before and after surgery (6 weeks, 4 months and 1 year) SF‐12 scores: difference at each time point (high score = better quality of life). Body Image Scale: difference at each time point (low score = a better body image) | SF scores PHYSICAL COMPONENT SUMMARY (PCS‐12) Baseline (n = 447) Mean = 44.9, SD = 11.7 6 weeks (n = 301) Mean = 46.8, SD = 10.1 4 months (n = 304) Mean = 52.6, SD = 8.6 1 year (n = 330) Mean = 53.6, SD = 8.4 MENTAL COMPONENT SUMMARY (MCS‐12) Baseline (n = 447 Mean = 45.8, SD = 11.7 6 weeks (n = 301) Mean = 50, SD = 11.4 4 months (n = 304) Mean = 50.9, SD = 10.5 1 year (n = 330) Mean = 50.7, SD = 10.7 Body Image Scale Baseline (n = 540) Mean = 8.8, SD = 8.1 6 weeks (n = 357) Mean = 3.7, SD = 4.9 4 months (n = 346) Mean = 3.3, SD = 4.9 1 year (n = 387) Mean = 3.4, SD = 5.2 | SF scores PHYSICAL COMPONENT SUMMARY (PCS‐12) Baseline (n = 221) Mean = 45.6, SD = 11.5 6 weeks (n = 148) Mean = 41.7, SD = 9.7 4 months (n = 134) Mean = 51.6, SD = 8.6 1 year (n = 148) Mean = 52.7, SD = 9.3 MENTAL COMPONENT SUMMARY (MCS‐12) Baseline (n = 221) Mean = 45.3, SD = 11.3 6 weeks (n = 148) Mean = 51.9, SD = 10.8 4 months (n = 134) Mean = 51.8, SD = 9.5 1 year (n = 148) Mean = 51.9, SD = 10.2 Body Image Scale Baseline (n = 270) Mean = 9, SD = 7.9 6 weeks (n = 172) Mean = 5.2, SD = 5.9 4 months (n = 159) Mean = 4.4, SD = 6.3 1 year (n = 168) Mean = 4.1, SD = 5.7 | SF scores PCS‐12 Baseline: difference CI = 0.6 (‐1.2 to 2.5) 6 weeks: difference CI = ‐5.1 (‐7.1 to ‐3.2). P value < 0.0001 4 months: difference CI = ‐1.0 (‐2.8 to 0.7). P value = 0.25 1 year = difference in CI = ‐0.9 (‐2.5 to 0.8). P value = 0.32 MCS‐12 Baseline: difference in CI = ‐0.5 (‐2.4 to 1.4) 6 weeks: difference in CI = 1.8 (‐0.4 to 4). P value = 0.11 4 months: difference in CI = 0.8 (‐1.3 to 2.9). P value = 0.44 1 year: difference in CI = 1.1 (‐0.9 to 3.2) P value = 0.27 Body Image Scale Baseline: difference in CI = 0.2 (‐0.9 to 1.4) 6 weeks: difference in CI = 1.5 (0.5 to 2.4). P value = 0.005 4 months: difference in CI = 1.1 (0.06 to 2.1). P value = 0.06 1 year: difference in CI = 0.7 (‐0.2 to 1.7). P value = 0.13 Both aLH and AH groups had improvements in the Physical and Mental components of SF12 and Body Image Scale. These were maintained and improved at 12 months. Significant difference in PCS‐12 at 6 weeks between aLH and AH and highly significant differences in BIS at 6 weeks, but this difference did not persist at 4 and 12 months |
| Kluivers 2007 | Questionnaire RAND‐36. A high score is a better quality of life. Statistical analysis with use of linear mixed model to evaluate the differences between 2 and 12 weeks while accounting for baseline value In Nieboer 2012, the same patients were evaluated with use of the same questionnaire 4 years after surgery |
n = 27 at baseline
n = 27, 26, 26, 25 and 22 at 1, 2, 4, 6 and 12 weeks respectively n = 23 at 4 years |
n = 32 at baseline
n = 32, 32, 32, 31, 30 and 30 at 1, 2, 4, 6 and 12 weeks respectively n = 26 at 4 years |
Difference (95%CI) in favour of LH (the score range on subscales is 100, score range on total RAND‐36 scales is 800) over the first 12 weeks:
Physical functioning 7.8 (‐0.3; 15.9)
Social functioning 7.0 (‐1.8; 15.7)
Role physical 1.7 (‐7.7; 11.1)
Role emotional 1.5 (‐13.4; 16.5)
Mental health 3.6 (‐2.8; 9.9)
Vitality 12.0 (4.7; 19.3)
Bodily pain 8.4 (‐0.1; 17.4)
General health 0.0 (‐8.1; 8.1)
Total RAND‐36 49.6 (‐5.1; 104.2)
Only the difference in the subscale vitality was statistically significant Analysis over 4 years follow up after surgery: Total RAND‐36 scores overall mean difference 50.4 points (95% confidence interval 1.0 –99.7) in favour of LH. Statistically significant higher scores were also found on the domains physical role functioning, social role functioning and vitality |
| Lumsden 2000 | EuroQol Health Questionnaire used to measure women's evaluation of their health state post surgery (1, 6 and 12 months after surgery). Use of a visual analogue thermometer (0 is worst imaginable health state and 100 is best imaginable health state). | 1 month (post‐op minus pre‐op): n = 74. Mean = 7, SD = 24.1. Median = 10, range (‐50 to 50) 6 months: n = 62. Mean = 11.3, SD = 23.9. Median = 15, range (‐50 to 60) 1 year: n = 43. Mean = 12.6, SD = 25. Median = 14, range (‐40 to 73) |
1 month: n = 76. Mean = 6.8, SD = 19.2. Median = 8, range (‐50 to 60). 6 months: n = 61. Mean = 14.9, SD = 16.7 Median = 15, range (‐20 to 60) 1 year: n = 47. Mean = 15.9, SD = 21. Median = 15, range (‐40 to 60) | Mean difference: 1 month: ‐1.6 (‐7.2 to 6.9) 6 months: 3.7 (‐3.7 to 11). 1 year: 4.9 (‐6.7 to 12.8) No evidence of a significant differences at 1 month, 6 months or 1 year after surgery |
| Olsson 1996 | 6 to 8 weeks after surgery participants were asked in an anonymous questionnaire if they considered the duration of their post‐operative stay adequate | 9% of women in the LAVH group considered their time in hospital following surgery to be too short | 17% of women in the AH group considered their time in hospital following surgery to be too short | — |
| Persson 2006 | Questionnaires: Psychological General Wellbeing (PGWI), Women Health Questionnaire (WHQ), Spielberger Trait Anxiety Inventory (STAI) and Beck's Depression Inventory (BDI)
A higher score in the PGWB shows a higher degree of wellbeing, whereas in the WHQ, STAI, BDI a higher score shows the more undesirable outcomes. Assessment at baseline, and 5 weeks and 6 months postoperatively. Statistical analysis with the use of ANOVA for repeated measurements Persson 2008 analysed wellbeing on a 0 to 100 VAS and stress coping ability |
n = 63 PGWB: Baseline: mean = 96.7, SD = 17.9. 5 weeks: mean = 100.4, SD = 16.7. 6 months: mean = 104.7, SD = 18.5 WHQ: Baseline: mean = 64.9, SD = 13.9. 5 weeks: mean = 54.6, SD = 12.8. 6 months: mean = 55.0, SD = 14.4. STAI: Baseline: mean = 35.6, SD = 9.1. 5 weeks: mean = 32.7, SD = 8.7. 6 months: mean = 33.6, SD = 10.2. BDI: Baseline: mean = 6.6, SD = 5.8. 5 weeks: mean = 4.6, SD = 5.5. 6 months: mean = 5.3, SD = 6.8 | n = 56 PGWB: Baseline: mean = 96.5, SD = 16.5. 5 weeks: mean = 102.1, SD = 16.4. 6 months: mean = 106.1, SD = 16.0 WHQ: Baseline: mean = 63.9, SD = 18.2. 5 weeks: mean = 54.3, SD = 17.1. 6 months: mean = 54.2, SD = 17.2. STAI: Baseline: mean = 34.7, SD = 10.1. 5 weeks: mean = 31.7, SD = 10.6. 6 months: mean = 31.7, SD = 9.2. BDI: Baseline: mean = 6.9, SD = 6.1. 5 weeks: mean = 5.0, SD = 6.5. 6 months: mean = 4.0, SD = 5.2 | Main effect between groups: PGWB P value = 0.719, WHQ P value = 0.800, STAI P value = 0.418, BDI P value = 0.788. Main effect over time: PGWB P value < 0.0001, WHQ P value < 0.0001, STAI P value = 0.0002, BDI P value = 0.0002
Interaction: PGWB P value = 0.772, WHQ P value = 0.953, STAI P value = 0.762, BDI P value = 0.223 In Persson 2008: No significant difference was found in the day‐by‐day recovery of the general wellbeing between the operating methods. Stress coping ability did significantly influence the day‐by‐day recovery of general wellbeing |
2.3 Intra‐operative visceral injury
Although there was no proof of a difference in intra‐operative visceral injury, most point estimates indicated more harm after LH, i.e. bladder injury (OR 1.89, 95% CI 0.91 to 3.90, 12 RCTs, 2038 women, I2 = 0%) (Analysis 2.3), ureter injury (OR 3.46, 95% CI 0.94 to 12.71, seven RCTs, 1417 women, I2 = 0%) (Analysis 2.4), and vascular injury (OR 1.76, 95% CI 0.52 to 5.87, two RCTs, 956 women, I2 = 0%) (Analysis 2.7); with the exception of bowel injury (OR 0.21, 95% CI 0.03 to 1.33, four RCTs, 1175 women, I2 = 0%) (Analysis 2.6).
2.3. Analysis.
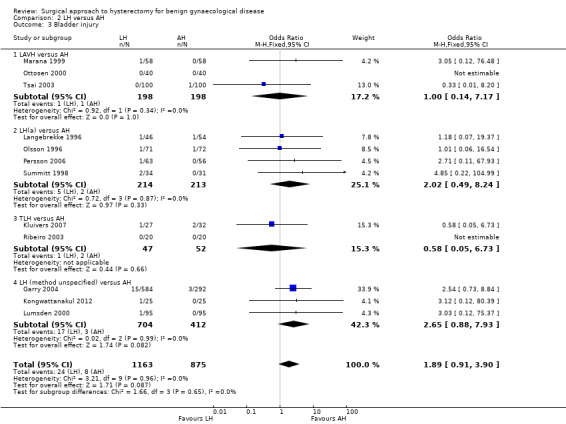
Comparison 2 LH versus AH, Outcome 3 Bladder injury.
2.4. Analysis.
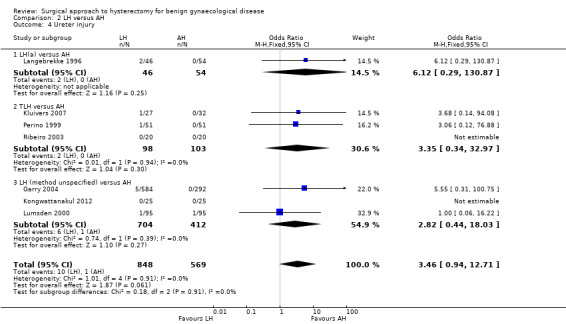
Comparison 2 LH versus AH, Outcome 4 Ureter injury.
2.7. Analysis.
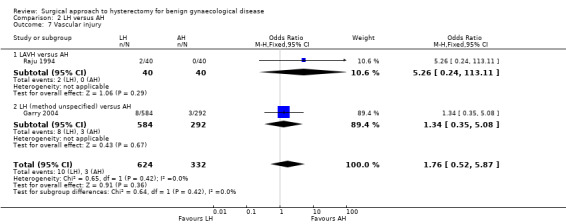
Comparison 2 LH versus AH, Outcome 7 Vascular injury.
2.6. Analysis.
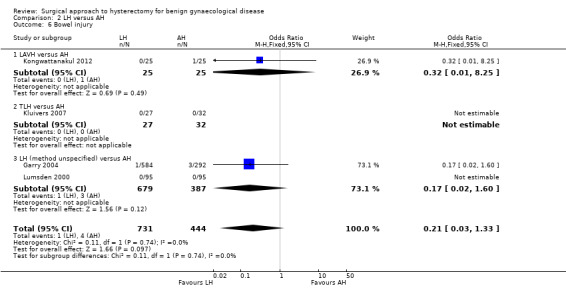
Comparison 2 LH versus AH, Outcome 6 Bowel injury.
When we pooled bladder and ureter injuries as 'urinary tract injury', there was evidence of a difference (OR 2.44, 95% CI 1.24 to 4.80, 13 RCTs, 2140 women, I2 = 0%, low quality evidence) (Analysis 2.5).
2.5. Analysis.
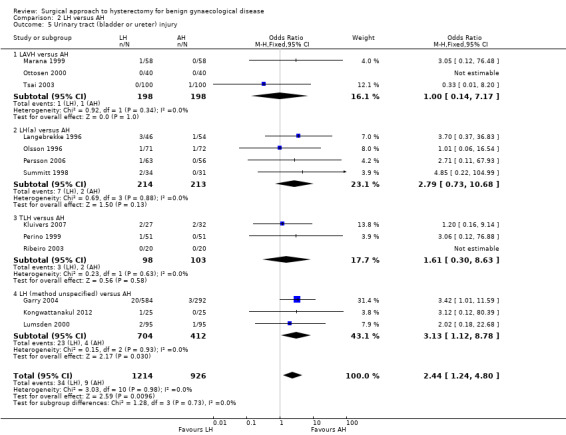
Comparison 2 LH versus AH, Outcome 5 Urinary tract (bladder or ureter) injury.
2.4 Major long‐term complications Comparisons of long‐term complications were either underpowered (fistula formation (OR 3.07, 95% CI 0.32 to 29.96, two RCTs, 245 women, I2 = 0%, low quality evidence) (Analysis 2.8) and urinary dysfunction (OR 0.94, 95% CI 0.48 to 1.84, two RCTs, 246 women, I2 = 0%, low quality evidence) (Analysis 2.9)) or were lacking (pelvi‐abdominal pain, bowel dysfunction, pelvic floor condition (prolapse), sexual dysfunction).
2.8. Analysis.
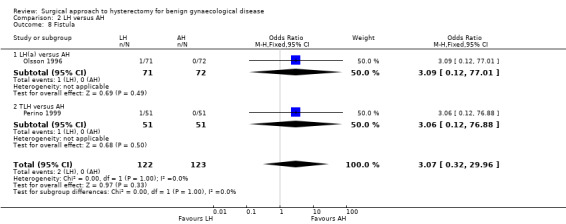
Comparison 2 LH versus AH, Outcome 8 Fistula.
2.9. Analysis.
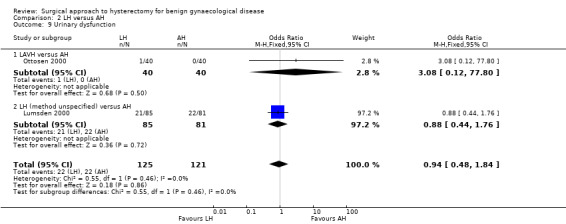
Comparison 2 LH versus AH, Outcome 9 Urinary dysfunction.
Secondary outcomes
2.5 Operation time
There was no evidence of a difference in operation time between LAVH versus AH (MD 0.27, 95% CI ‐23.39 to 23.93; four RCTs; 466 women; I2 = 96%) (Analysis 2.10). Other subcategories of laparoscopic hysterectomy (LH(a) and total laparoscopic hysterectomy (TLH)) took longer than abdominal hysterectomies (LH(a) versus AH: MD 33.45, 95% CI 14.82 to 52.08; five RCTs, 420 women, I2 = 90% (Analysis 2.10); TLH versus AH: MD 28.74, 95% CI 2.64 to 54.85; two RCTs, 161 women, I2 = 87%) (Analysis 2.10). Operation time was eight minutes shorter in LAVH compared to mini‐AH (MD ‐8.00 minutes, 95% CI ‐10.56 to ‐5.44, one RCT, 100 women, I2 = n/a, moderate quality evidence) (Analysis 2.10). These analyses used a random effects model. We considered clinical and methodological differences between the studies that might account for the high heterogeneity; training and experience of surgeons may play a role.
2.10. Analysis.
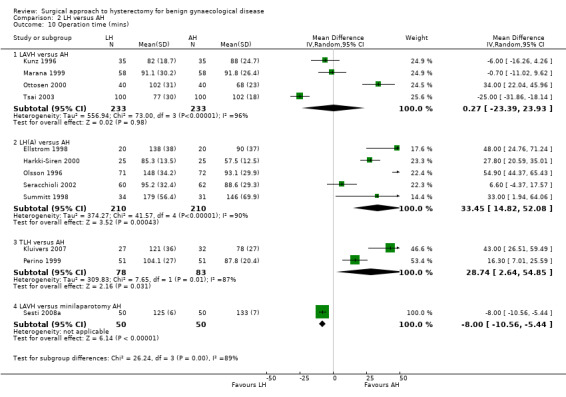
Comparison 2 LH versus AH, Outcome 10 Operation time (mins).
Eleven additional trials could not be pooled because of the descriptive format in which the data were presented. Except for Yuen 1998, all trials showed that abdominal hysterectomy had a shorter median operation time (Falcone 1999; Ferrari 2000; Garry 2004, Hwang 2002; Langebrekke 1996; Muzii 2007; Persson 2006; Raju 1994, Ribeiro 2003; Schutz 2002) (Analysis 2.25).
2.25. Analysis.
Comparison 2 LH versus AH, Outcome 25 Operation time (descriptive data).
| Operation time (descriptive data) | |||
|---|---|---|---|
| Study | LH | AH | Comments |
| Falcone 1999 | n = 23 median = 180 mins range (139 to 225) | n = 21 median = 130 mins range (97 to 155) | LH(a) vs AH Wilcoxon rank‐sum test P value < 0.001 |
| Ferrari 2000 | n = 31 median = 135 mins range (115 to 173) | n = 31 median = 120 mins range (98 to 123) | LAVH vs AH P value = 0.001 Calculated from the first incision to closure of all wounds |
| Garry 2004 | n = 584 median = 84 mins range(10 to 325) | n = 292 median = 50 mins range (19 to 155) | non‐categorisable LH vs AH Calculated from first incision to last suture |
| Hwang 2002 | With 2nd procedure n = 13 median = 119 range (80 to 165) Without 2nd procedure n = 17 median = 109 mins range (85 to 175) | With 2nd procedure n = 8 median = 117 mins range (90 to 190) Without 2nd procedure n = 22 Median = 98 Range (85 to 150) | LH(a) vs AH Not tested separately |
| Langebrekke 1996 | n = 46 median = 100 mins range (50 to 153) | n = 54 median = 60.5 mins range (22 to 105) | LH(a) vs AH |
| Muzii 2007 | n = 40 median = 86 mins range (60 to 120) |
n = 41 median = 58 mins range (45 to 75) |
LAVH vs minilaparotomy AH |
| Persson 2006 | n = 63 median = 99 mins range (50 to 190) | n = 56 median = 64 mins range (35 to 150) | LH(a) vs AH P value < 0.0001 (students t test) |
| Raju 1994 | n = 40 median = 100 mins range (61‐180) | n = 40 median = 57 mins range (25 to 151) | LAVH vs AH P value < 0.0001 Mann‐Whitney U test Calculated from first incision to time all wounds were closed, dressed and urinary catheter inserted |
| Ribeiro 2003 | n = 20 Mean 119 mins (no measure of spread reported) | n = 20 Mean 109 mins (no measure of spread reported) | TLH vs AH |
| Schutz 2002 | n = 28 median = 133 mins range (120 to 160) | n = 20 median = 132 mins range (121 to 145) | LH(a) vs AH |
| Yuen 1998 | n = 20 median = 95 mins range (79 to 143) | n = 24 median = 105 mins range (86 to 120) | LH(a) vs AH Calculated from first surgical incision to time of last suture |
2.6 Intra‐operative complications (other than visceral injury)
There was no evidence of a difference in the number of women with substantial bleeding between laparoscopic and abdominal hysterectomy (OR 0.45, 95% CI 0.15 to 1.37, five RCTs, 1266 women, I2 = 0%) (Analysis 2.11).
2.11. Analysis.
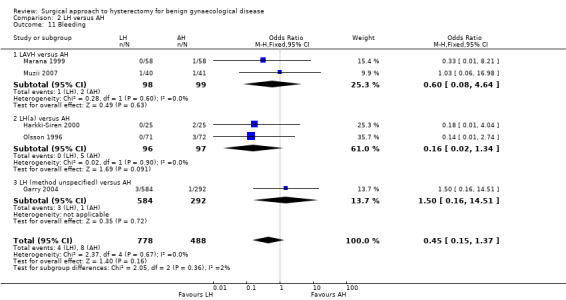
Comparison 2 LH versus AH, Outcome 11 Bleeding.
Overall, laparoscopic versus abdominal hysterectomy did not show evidence of a difference in the need for blood transfusions (OR 0.58, 95% CI 0.30 to 1.10, 20 RCTs, 2638 women, I2 = 32%, moderate quality evidence) (Analysis 2.12). Pelvic haematomas occurred less after laparoscopic hysterectomy, but again there was no evidence of a difference (OR 0.75, 95% CI 0.38 to 1.47, eight RCTs, 782 women, I2 = 0%, low quality evidence) (Analysis 2.13).
2.12. Analysis.
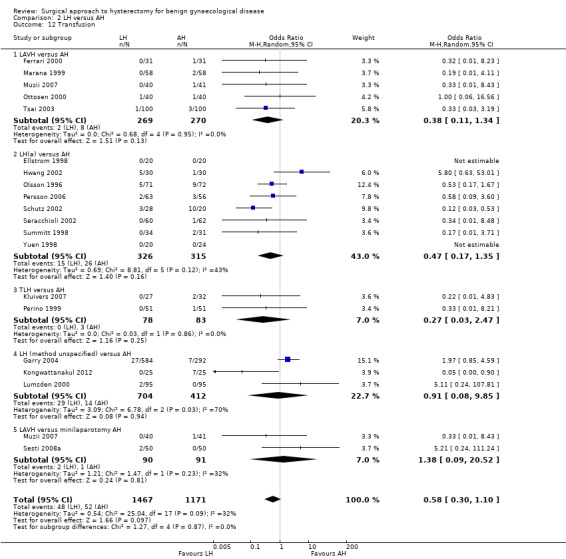
Comparison 2 LH versus AH, Outcome 12 Transfusion.
2.13. Analysis.
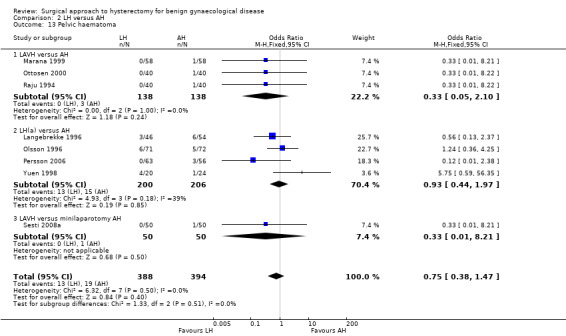
Comparison 2 LH versus AH, Outcome 13 Pelvic haematoma.
Unintended laparotomy was not compared in meta‐analysis because AH involves routine laparotomy. In two trials there was no proof of a difference in unintended conventional laparotomies between the interventions (OR 0.49, 95% CI 0.08 to 2.82, two RCTs, 181 women, I2 = n/a) (Analysis 2.14).
2.14. Analysis.
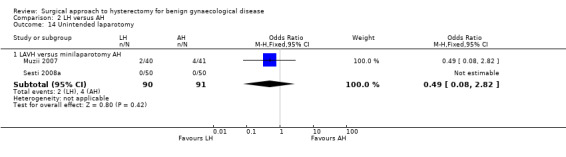
Comparison 2 LH versus AH, Outcome 14 Unintended laparotomy.
2.7 Short‐term outcomes and complications
Hospital stay was generally shorter in LH compared to AH: LAVH versus AH (MD ‐2.64, 95% CI ‐4.16 to ‐1.12; four RCTs, 466 women, I2 = 97%), LH(a) versus AH (MD ‐1.82, 95% CI ‐2.34 to ‐1.31; four RCTs, 380 women, I2 = 70%), TLH versus AH (MD ‐2.53, 95% CI ‐5.08 to 0.01; two RCTs, 161 women, I2 = 95%) and LAVH versus minilaparotomy AH (MD ‐1.10, 95% CI ‐1.20 to ‐1.00; one RCT, 100 women, I2 = n/a) (Analysis 2.15). These analyses used a random effects model. We considered clinical and methodological differences between the studies that might account for the high heterogeneity; training and experience of surgeons may play a role.
2.15. Analysis.
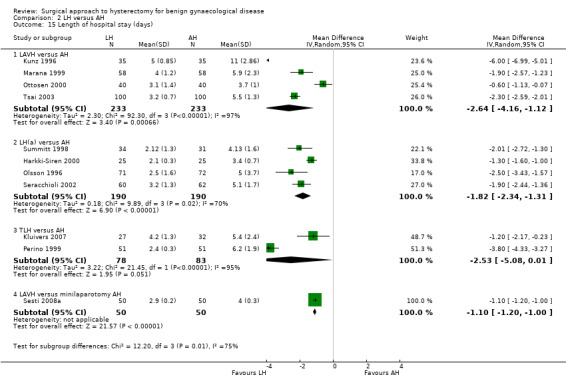
Comparison 2 LH versus AH, Outcome 15 Length of hospital stay (days).
Data from 11 trials on hospital stay could not be included in the meta‐analysis, because of the presentation of median numbers instead of means. In all of these trials, median duration of hospital stay was shorter. There was evidence of a difference, proving hospital stay was shorter for laparoscopic hysterectomy, in six trials (Falcone 1999; Ferrari 2000; Langebrekke 1996; Persson 2006; Raju 1994; Yuen 1998), whereas in one study there was no evidence of a difference (Muzii 2007). In the other four trials no statistical testing was applied (Analysis 2.26).
2.26. Analysis.
Comparison 2 LH versus AH, Outcome 26 Length of hospital stay (descriptive data).
| Length of hospital stay (descriptive data) | |||
|---|---|---|---|
| Study | LH | AH | Comments |
| Falcone 1999 | n = 23 median = 1.5 days range (1.0 to 2.3) | n = 21 median = 2.5 days range (1.5 to 2.5) | P value = 0.038 Wilcoxon rank‐sum test |
| Ferrari 2000 | n = 31 median = 3.8 days range (3.8 to 4.0) | n = 31 median = 5.8 days range (5.3 to 6.3) | P value < 0.001 |
| Garry 2004 | n = 584 median = 3 days range (1 to 36) | n = 292 median = 4 days range (1 to 36) | — |
| Hwang 2002 | n = 30 median = 4.7 days range (3 to 7) | n = 30 median = 5 days range (4 to 8) | Not tested separately |
| Langebrekke 1996 | n = 46 median = 2 days range (0 to 5) | n = 54 median = 5 days range (3 to 12) | P value < 0.001 Wilcoxon rank‐sum test |
| Muzii 2007 | n = 40 median = 2 days range (1 to 3) |
n = 41 median = 3 days range = (1 to 5) |
P value = 0.53 |
| Persson 2006 | n = 63 median = 2 days range (1 to 11) | n = 56 median = 3 days range (2 to 7) | P value = 0.0006 In the same population (described in Persson 2008), duration of sick leave was associated with the occurrence of postoperative complications but not with stress‐coping ability |
| Raju 1994 | n = 40 median = 3.5 days range (1 to 6) | n = 40 median = 6 days range (3 to 13) | P value < 0.0001 Mann‐Whitney U test |
| Ribeiro 2003 | n = 20 all home on day 2 | n = 20 all home on day 3 | — |
| Schutz 2002 | n = 28 median = 6.5 days range (5 to 7) | n = 20 median = 10 days range (8.25 to 11) | — |
| Yuen 1998 | n = 20 median = 4 days range (4 to 5) | n = 24 median = 6 days range (5 to 9) | P value < 0.001 Mann‐Whitney U test |
There were fewer wound or abdominal wall infections in laparoscopic hysterectomy (OR 0.29, 95% CI 0.12 to 0.71; six RCTs, 611 women, I2 = 5%, low quality evidence) (Analysis 2.17) and fewer febrile episodes or unspecified infections for the comparisons LAVH versus AH (OR 0.25, 95% CI 0.09 to 0.73; four RCTs, 339 women, I2 = 0%) and LH(a) versus AH (OR 0.55, 95% CI 0.33 to 0.90; seven RCTs, 572 women, I2 = 47%) (Analysis 2.20).
2.17. Analysis.
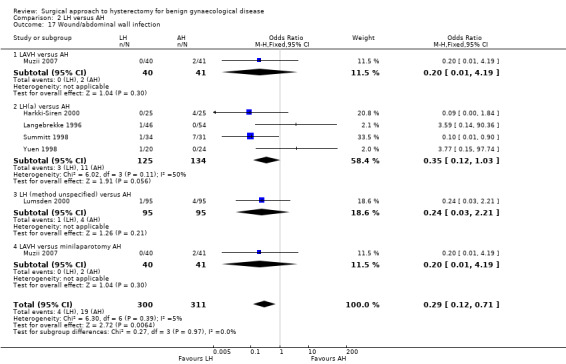
Comparison 2 LH versus AH, Outcome 17 Wound/abdominal wall infection.
2.20. Analysis.
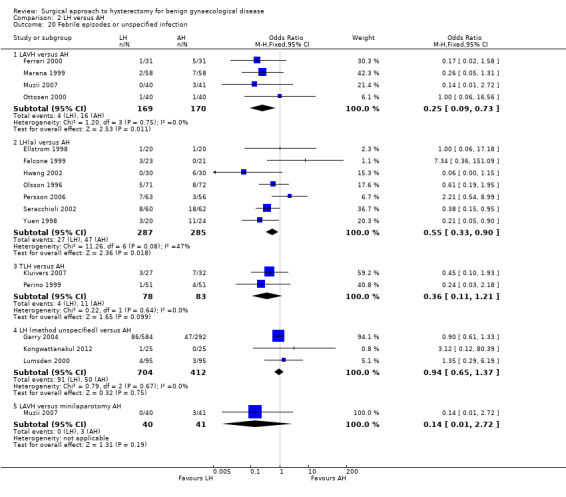
Comparison 2 LH versus AH, Outcome 20 Febrile episodes or unspecified infection.
There was no evidence of a difference in the occurrence of vaginal cuff infection (OR 1.43, 95% CI 0.67 to 3.04, nine RCTs, 852 women, I2 = 0%, low quality evidence) (Analysis 2.16), urinary tract infections (OR 1.04, 95% CI 0.54 to 2.00, eight RCTs, 659 women, I2 = 0%, low quality evidence) (Analysis 2.18), chest infection (OR 0.31, 95% CI 0.07 to 1.35, three RCTs, 294 women, I2 = 17%, low quality evidence) (Analysis 2.19), and thromboembolic events (OR 0.89, 95% CI 0.23 to 3.39, three RCTs, 1125 women, I2 = 0%, low quality evidence) (Analysis 2.21).
2.16. Analysis.
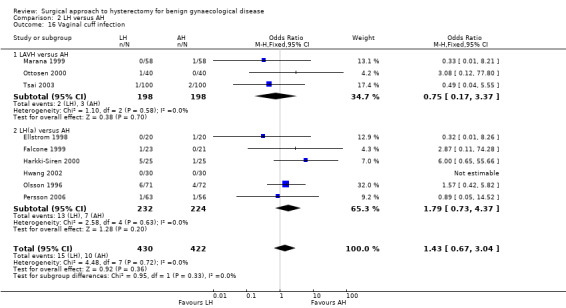
Comparison 2 LH versus AH, Outcome 16 Vaginal cuff infection.
2.18. Analysis.
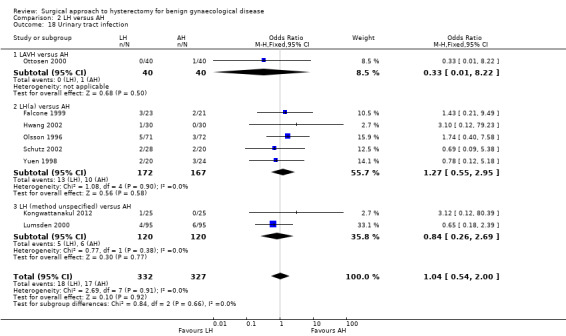
Comparison 2 LH versus AH, Outcome 18 Urinary tract infection.
2.19. Analysis.
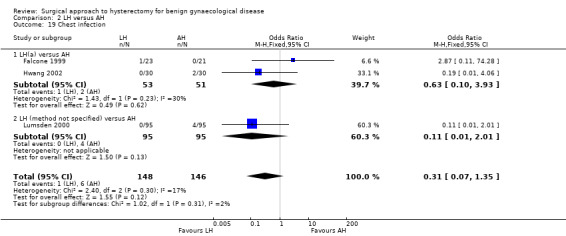
Comparison 2 LH versus AH, Outcome 19 Chest infection.
2.21. Analysis.
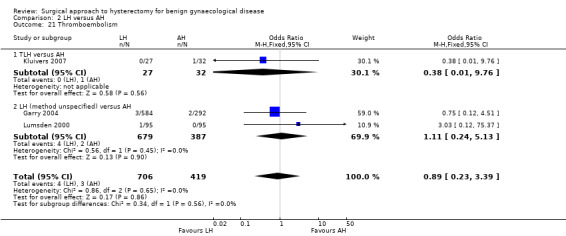
Comparison 2 LH versus AH, Outcome 21 Thromboembolism.
With regard to the subcategory LAVH versus mini‐LH, no evidence of a difference was found for wound or abdominal wall infections (OR 0.20, 95% CI 0.01 to 4.19, one RCT, 81 women, I2 = n/a, low quality evidence) (Analysis 2.17), febrile episodes or unspecified infection (OR 0.14, 95% 0.01 to 2.72, one RCT, 81 women, I2 = n/a, low quality evidence) (Analysis 2.20). Other infections (vaginal cuff, urinary tract or chest infection) were not evaluated for this comparison. No evidence of a difference was found for wound dehiscence (OR 3.15, 95% CI 0.12 to 79.69, one RCT, 81 women, I2 = n/a, low quality evidence) (Analysis 2.22). Thromboembolism and perioperative mortality were not evaluated for this comparison.
2.22. Analysis.
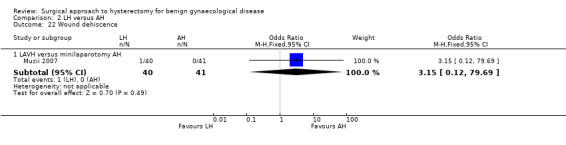
Comparison 2 LH versus AH, Outcome 22 Wound dehiscence.
Also the occurrence of wound dehiscence showed no evidence of a difference (OR 3.15, 95% CI 0.12 to 79.69, one RCT, 81 women, I2 = n/a, low quality evidence) (Analysis 2.22).
There were no reports on perioperative mortality for this comparison.
2.8 Cost
There was no evidence of a difference in the overall cost, but only six RCTs examined comparative cost in any detail (Ellstrom 1998; Garry 2004 (as published in Sculpher 2004); Falcone 1999; Lumsden 2000; Raju 1994; Summitt 1998).
3 Laparoscopic hysterectomy (LH) versus vaginal hysterectomy (VH)
Primary outcomes
3.1 Return to normal activities
Women undergoing laparoscopic hysterectomy returned to work one day earlier than women undergoing VH, but the time to return to normal activities showed no evidence of a difference (MD ‐1.07, 95% CI ‐4.21 to 2.06, two RCTs, 140 women, I2 = 0%, low quality evidence) (Figure 6; Analysis 3.1).
6.
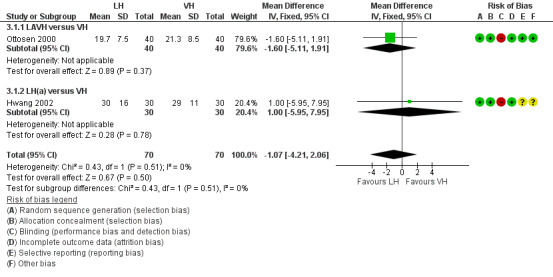
Forest plot of comparison: 3 LH versus VH, outcome: 3.1 Return to normal activities (days).
3.1. Analysis.

Comparison 3 LH versus VH, Outcome 1 Return to normal activities (days).
Data from three RCTs could not be included in the meta‐analysis because of their descriptive nature (Richardson 1995; Roy 2011; Roy 2012). These three trials did not show evidence of a difference in return to normal activities between LH and VH either (Analysis 3.21).
3.21. Analysis.
Comparison 3 LH versus VH, Outcome 21 Return to normal activities (descriptive data).
| Return to normal activities (descriptive data) | |||
|---|---|---|---|
| Study | LH | VH | Comments |
| Richardson 1995 | n = 22 mean = 23.1 days range (7 to 56) | n = 23 mean = 22.2 range (7 to 56) | |
| Roy 2011 | TLH: n = 30 median = 15 days min‐max = 7 to 30 days LAVH: n = 30 median = 20 days min‐max = 8 to 40 days |
n = 30 median = 14 days min‐max = 7 to 25 days |
P value = 0.7 |
| Roy 2012 | n = 10 median = 20 days min‐max = 10 to 30 days |
n = 10 median = 16 days min‐max = 12 to 24 days |
P value = 0.05 |
3.2 Satisfaction and quality of life
Roy 2011 showed that six months after surgery, patients were more satisfied after total laparoscopic hysterectomy and vaginal hysterectomy than those who underwent laparoscopic‐assisted vaginal hysterectomy (P value = 0.003). The satisfaction rate was similar between patients undergoing total laparoscopic hysterectomy and non‐descent vaginal hysterectomy (Analysis 3.22). The descriptive character of these data means that these could not be included in the meta‐analysis.
3.22. Analysis.
Comparison 3 LH versus VH, Outcome 22 Long‐term outcomes: quality of life (descriptive data).
| Long‐term outcomes: quality of life (descriptive data) | ||||
|---|---|---|---|---|
| Study | Description | LH | VH | Comment |
| Roy 2011 | Patient satisfaction was evaluated using HRQOL (Health Related Quality Of Life) questionnaire and SF‐12 (12‐item Short Form health survey) and follow‐up visits in outpatient clinic were done at 1, 3 and 6 months | TLH: n = 30 LAVH: n = 30 |
n = 30 | After 6 months of surgery, there was significant higher satisfaction rate among patients who underwent TLH and NDVH (non‐descent vaginal hysterectomy) than those who underwent LAVH (P value = 0.003). The satisfaction was similar between the TLH and NDVH group |
3.3 Intra‐operative visceral injury
There was no evidence of a difference in bladder injury (OR 0.91, 95% CI 0.32 to 2.56, seven RCTs, 895 women, I2 = 0%, low quality evidence) (Analysis 3.3), ureter injury (OR 1.51, 95% CI 0.06 to 37.18, two RCTs, 594 women, I2 = n/a, low quality evidence) (Analysis 3.2), urinary tract injury (OR 1.00, 95% CI 0.36 to 2.75, seven RCTs, 895 women, I2 = 0%, low quality evidence) (Analysis 3.4), and vascular injury (OR 1.58, 95% CI 0.48 to 5.27, four RCTs, 685 women, I2 = 0%, low quality evidence) (Analysis 3.6), but the power to detect a difference is low due to the numbers and low event rates. In the studies from Garry 2004 and Roy 2011 bowel injury did not occur.
3.3. Analysis.
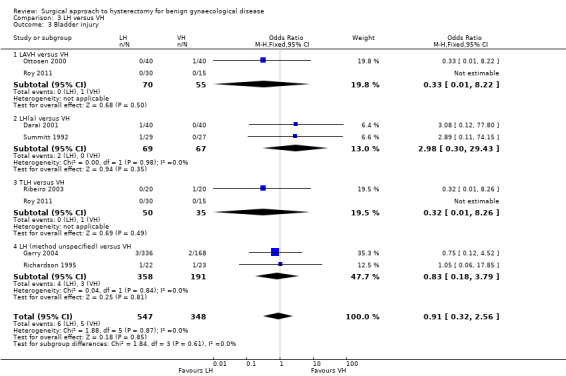
Comparison 3 LH versus VH, Outcome 3 Bladder injury.
3.2. Analysis.
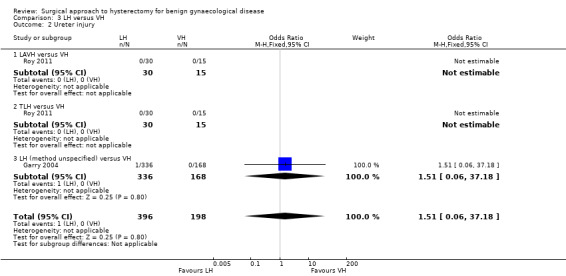
Comparison 3 LH versus VH, Outcome 2 Ureter injury.
3.4. Analysis.
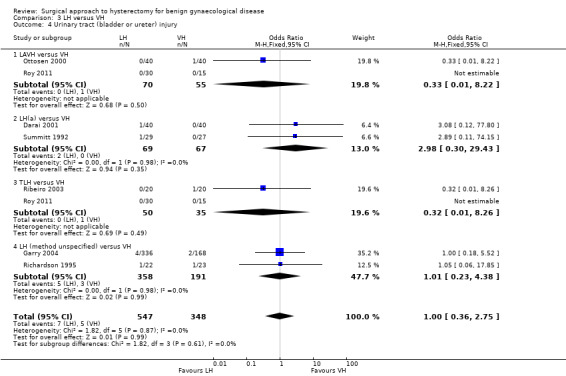
Comparison 3 LH versus VH, Outcome 4 Urinary tract (bladder or ureter) injury.
3.6. Analysis.
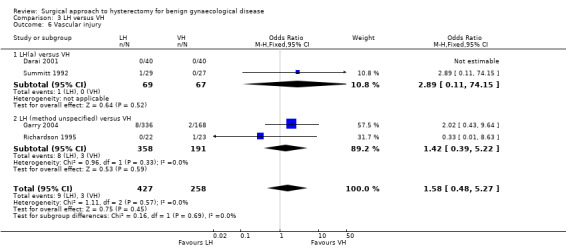
Comparison 3 LH versus VH, Outcome 6 Vascular injury.
3.4 Major long‐term complications
Also, there was no evidence of a difference in the following long‐term complications: fistula formation (OR 0.30, 95% CI 0.01 to 7.67, one RCT, 56 women, I2 = n/a, low quality evidence) (Analysis 3.7), and urinary dysfunction (OR 3.08, 95% CI 0.12 to 77.80, one RCT, 80 women, I2 = n/a, low quality evidence) (Analysis 3.8). Pelvi‐abdominal pain, bowel dysfunction, pelvic floor condition (prolapse) and sexual dysfunction were not studied for this comparison.
3.7. Analysis.
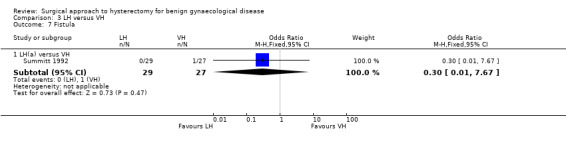
Comparison 3 LH versus VH, Outcome 7 Fistula.
3.8. Analysis.
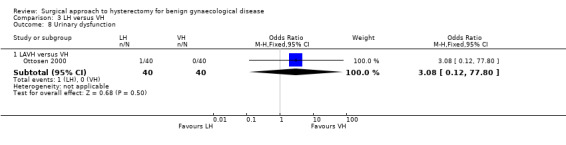
Comparison 3 LH versus VH, Outcome 8 Urinary dysfunction.
Secondary outcomes
3.5 Operation time
All subcategories of laparoscopic hysterectomy showed a longer operation time than vaginal hysterectomy. For LAVH versus VH: MD 33.60, 95% CI 20.13 to 47.07, 5 RCTs, 377 women, I2 = 98%. For LH(a) versus VH: MD 53.58, 95% CI 43.67 to 63.49, 3 RCTs, 213 women, I2 = 0%. For TLH versus VH: MD 17.30, 95% CI 3.34 to 31.26, 1 RCT, 60 women. These analyses used a random effects model. We considered clinical and methodological differences between the studies that might account for the high heterogeneity in the LAVH versus VH subgroup only; training and experience of surgeons may play a role but we were unable to explain why heterogeneity was not present in the LH(a) versus VH subgroup. (Analysis 3.9)
3.9. Analysis.
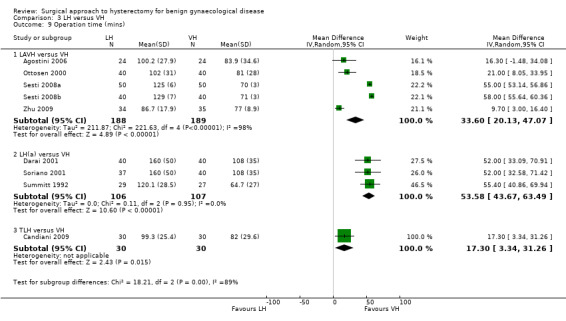
Comparison 3 LH versus VH, Outcome 9 Operation time (mins).
In the operation time analysis, four studies could not be pooled (Hwang 2002; Ribeiro 2003; Richardson 1995; Roy 2012). These studies all found longer operation times in laparoscopic hysterectomy with a statistical test result reported in two studies, of which one showed evidence of a difference (Hwang 2002) and one did not (Roy 2012) (Analysis 3.23).
3.23. Analysis.
Comparison 3 LH versus VH, Outcome 23 Operation time (descriptive data).
| Operation time (descriptive data) | |||
|---|---|---|---|
| Study | LH | VH | Comments |
| Hwang 2002 | With 2nd proc: n = 13 Median = 119 Range (80 to 165) Without 2nd proc: n = 17 Median = 109 Range (85 to 175) | With 2nd proc: n = 3 Median = 93 Range (80 to 110) Without 2nd proc: n = 27 Median = 74 Range (40 to 120) | Kruskal Wallis test: P value = 0.12 P value < 0.001 |
| Ribeiro 2003 | n = 20 mean 119 mins (no measure of spread) | n = 20 mean 78 mins (no measure of spread) | — |
| Richardson 1995 | n = 22 mean = 131.4 mins range (76 to 180) | n = 23 mean = 76.7 mins range (35 to 150) | Some of these cases include oophorectomies. Oophorectomy (mean): LH 129.7 mins, VH 95.3 mins; no oophorectomy (mean): LH 132.7 mins, VH 64.7 mins |
| Roy 2012 | n = 10 median = 90 mins min‐max = 60 to 165 mins |
n = 10 median = 75 min‐max = 40 to 105 |
Not statistically significant |
3.6 Intra‐operative complications (other than visceral injury)
There was no evidence of a difference in other intra‐operative complications between laparoscopic and vaginal hysterectomy: substantial bleeding (OR 1.55, 95% CI 0.24 to 10.09, three RCTs, 614 women, I2 = 0%, low quality evidence) (Analysis 3.10), , the number of transfusions (OR 1.60, 95% CI 0.80 to 3.18, eight RCTs, 1039 women, I2 = 0%, low quality evidence) (Analysis 3.11), pelvic haematoma (OR 1.21, 95% CI 0.36 to 4.03, four RCTs, 308 women, I2 = 0%, moderate quality evidence) (Analysis 3.12) and unintended laparotomies (OR 1.55, 95% CI 0.76 to 3.15, 10 RCTs, 1160 women, I2 = 5%, moderate quality evidence) (Analysis 3.13).
3.10. Analysis.
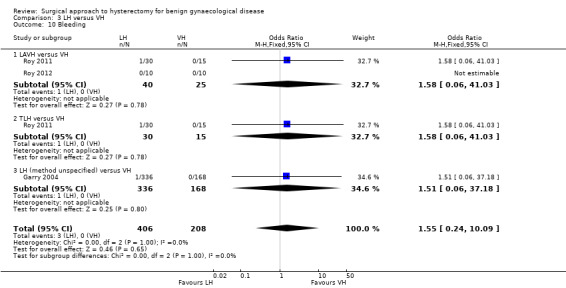
Comparison 3 LH versus VH, Outcome 10 Bleeding.
3.11. Analysis.
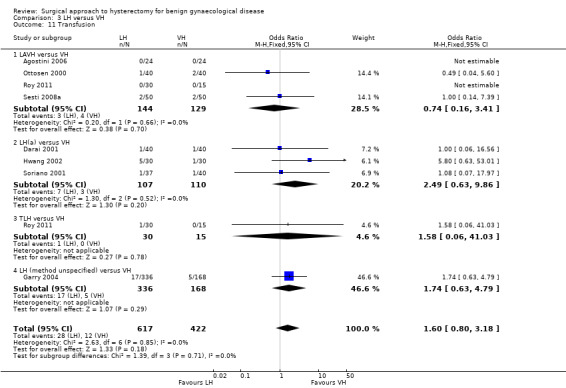
Comparison 3 LH versus VH, Outcome 11 Transfusion.
3.12. Analysis.
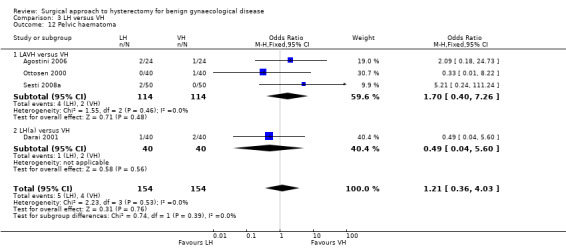
Comparison 3 LH versus VH, Outcome 12 Pelvic haematoma.
3.13. Analysis.
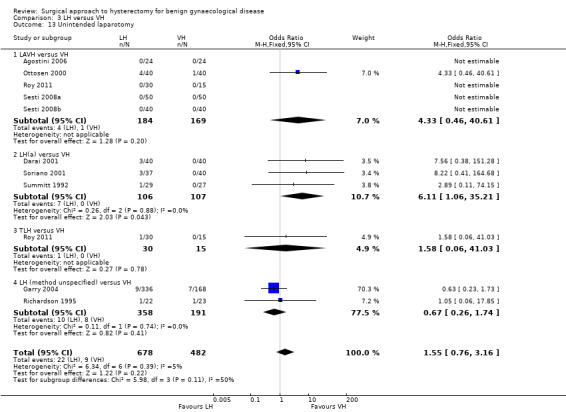
Comparison 3 LH versus VH, Outcome 13 Unintended laparotomy.
3.7 Short‐term outcomes and complications
Hospital stay was one day shorter after vaginal hysterectomy (MD 0.99 days, 95% CI 0.94 to 1.03, seven RCTs, 525 women, I2 = 67%, moderate quality evidence) (Analysis 3.20). There was no evidence of a difference in short‐term outcomes between laparoscopic and vaginal hysterectomy, i.e. occurrence of pelvic haematoma (OR 1.21, 95% CI 0.36 to 4.03, four RCTs, 308 women, I2 = 0%, low quality evidence) (Analysis 3.12), vaginal cuff infection (OR 0.98, 95% CI 0.22 to 4.39, four RCTs, 276 women, I2 = 0%, low quality evidence) (Analysis 3.14), wound/abdominal wall infection (OR 2.88, 95% CI 0.31 to 27.06, two RCTs, 170 women, I2 = 0%, low quality evidence) (Analysis 3.15), urinary tract infection (OR 1.66, 95% CI 0.40 to 6.82, three RCTs, 230 women, I2 = 0%, low quality evidence) (Analysis 3.16), chest infection (OR 0.19, 95% CI 0.01 to 4.06, one RCT, 60 women, low quality evidence) (Analysis 3.17), febrile episodes or unspecified infection (OR 0.80, 95% CI 0.51 to 1.24, nine RCTs, 1074 women, I2 = 0%, low quality evidence) (Analysis 3.18), and thromboembolic events (OR 1.00, 95% CI 0.15 to 6.67, two RCTs, 564 women, I2 = 0%, low quality evidence) (Analysis 3.19), but again confidence intervals were wide.
3.20. Analysis.
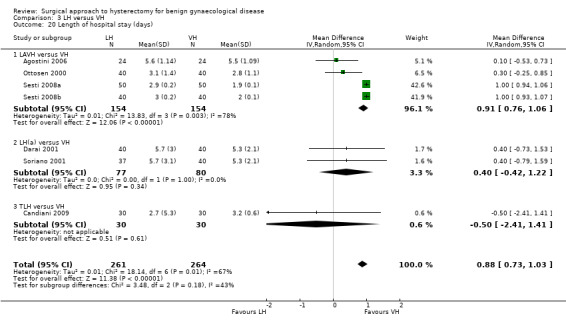
Comparison 3 LH versus VH, Outcome 20 Length of hospital stay (days).
3.14. Analysis.
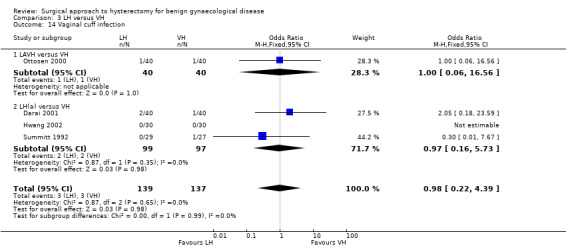
Comparison 3 LH versus VH, Outcome 14 Vaginal cuff infection.
3.15. Analysis.
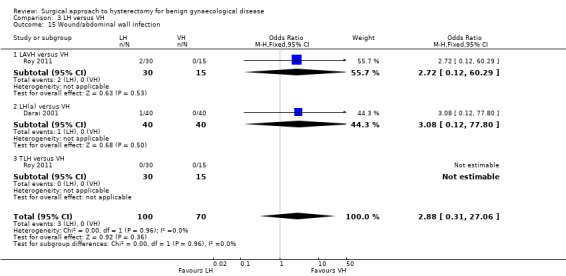
Comparison 3 LH versus VH, Outcome 15 Wound/abdominal wall infection.
3.16. Analysis.
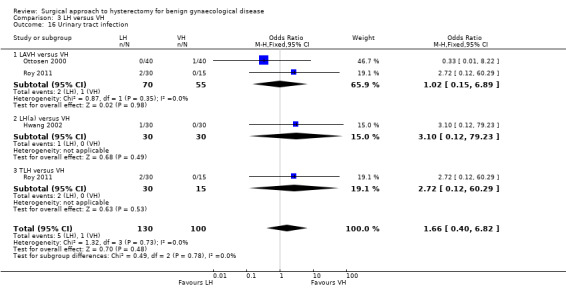
Comparison 3 LH versus VH, Outcome 16 Urinary tract infection.
3.17. Analysis.
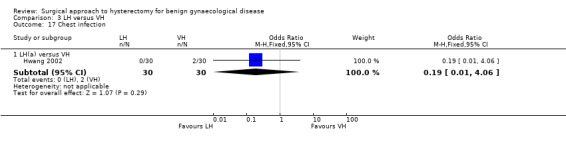
Comparison 3 LH versus VH, Outcome 17 Chest infection.
3.18. Analysis.
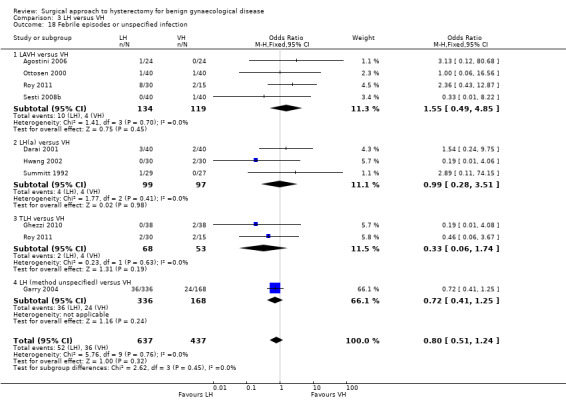
Comparison 3 LH versus VH, Outcome 18 Febrile episodes or unspecified infection.
3.19. Analysis.
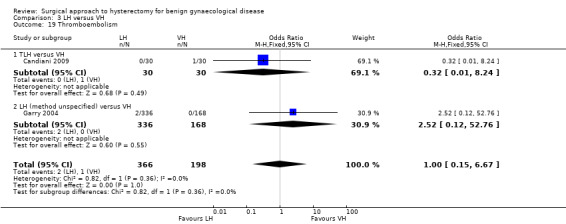
Comparison 3 LH versus VH, Outcome 19 Thromboembolism.
Four studies reported on differences in hospital stay, which could not be pooled in the meta‐analysis because of the descriptive format of the presented data (Hwang 2002; Richardson 1995; Roy 2011; Roy 2012). Two studies performed statistical testing but did not find evidence of a difference (Roy 2011; Roy 2012).
3.8 Cost
Laparoscopic hysterectomy costs an average of GBP 401 more than vaginal hysterectomy (95% CI GBP 271 to GBP 542; Garry 2004 as published in Sculpher 2004). The mean total hospital cost was higher for LH than for VH (Summitt 1992).
4 Robotic‐assisted hysterectomy (RH) versus laparoscopic hysterectomy (LH)
Primary outcomes
4.1 Return to normal activities
One small RCT evaluated return to normal activities between robotic‐assisted and laparoscopic hysterectomy. It showed a difference of two days favouring the robotic‐assisted hysterectomy, but there was no conclusive evidence of a difference (MD 2.4 days, 95% CI ‐8.5 to 3.7 days, one RCT, 100 women, I2 = n/a, moderate quality evidence) (Figure 7; Analysis 4.1).
7.
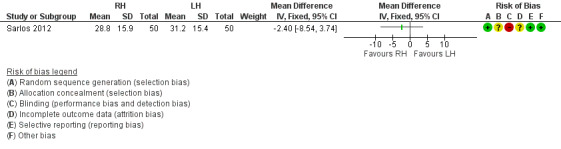
Forest plot of comparison: 4 RH versus LH, outcome: 4.1 Return to normal activities (days).
4.1. Analysis.
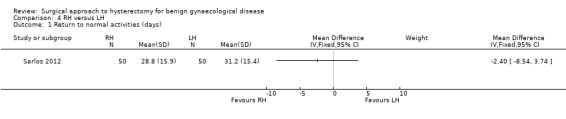
Comparison 4 RH versus LH, Outcome 1 Return to normal activities (days).
Data on return to normal baseline activities from the Paraiso 2013 study could not be pooled in the meta‐analysis, but there was no evidence of a difference between robotic‐assisted and laparoscopic hysterectomy.
4.2 Satisfaction and quality of life
These outcomes were not reported in studies comparing robotic‐assisted and laparoscopic hysterectomy.
4.3 Intra‐operative visceral injury The one RCT comparing these interventions was underpowered regarding ureter injury (OR 0.33, 95% CI 0.0 to 8.21, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 4.2) and vascular injury (OR 1.00, 95% CI 0.06 to 16.44, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 4.2).
4.2. Analysis.
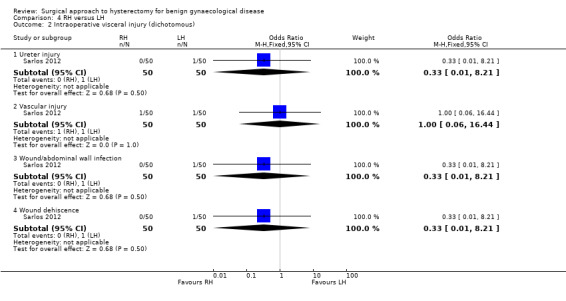
Comparison 4 RH versus LH, Outcome 2 Intraoperative visceral injury (dichotomous).
4.4 Major long‐term complications
Fistula formation, pelvi‐abdominal pain, urinary dysfunction, bowel dysfunction, pelvic floor condition (prolapse) and sexual dysfunction were not reported in studies comparing robotic‐assisted and laparoscopic hysterectomy.
Secondary outcomes
4.5 Operation time
Robotic‐assisted hysterectomy took 32 minutes longer than laparoscopic hysterectomy, which showed evidence of a difference (MD 32.42 minutes, 95% CI 22.67 to 42.18, two RCTs, 152 women, I2 = 58%, moderate quality evidence) (Analysis 4.3).
4.3. Analysis.
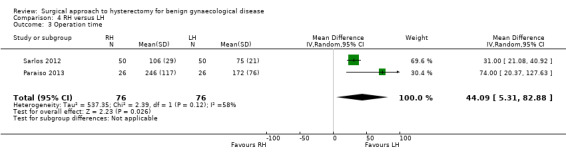
Comparison 4 RH versus LH, Outcome 3 Operation time.
4.6 Intra‐operative complications (other than visceral injury)
No evidence of a difference was found between robotic‐assisted and laparoscopic hysterectomy regarding the need for transfusion (OR 2.08, 95% CI 0.18 to 24.51, one RCT, 52 women, I2 = n/a, low quality evidence) (Analysis 4.4). Sequelae of bleeding, drop in haemoglobin/haematocrit, pelvic haematoma or unintended laparotomy were not studied for this comparison.
4.4. Analysis.

Comparison 4 RH versus LH, Outcome 4 Transfusion.
4.7 Short‐term outcomes and complications
No evidence of a difference between robotic‐assisted and laparoscopic hysterectomy was found for wound/abdominal wall infection (OR 0.33, 95% CI 0.01 to 8.21, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 4.2) and wound dehiscence (OR 0.33, 95% CI 0.01 to 8.21, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 4.2). Length of hospital stay, other infections (urinary tract infection, chest infection, febrile episodes or unspecified infections), thromboembolism, perioperative mortality were not studied for this comparison.
4.8 Cost
Cost was not studied in studies comparing robotic‐assisted and laparoscopic hysterectomy.
5. Single‐port laparoscopic hysterectomy subcategory (SP‐LH) versus laparoscopic hysterectomy (LH) subcategories
Primary outcomes
5.1 Return to normal activities
No studies compared this outcome for this comparison.
5.2 Satisfaction and quality of life
No studies compared this outcome for this comparison.
5.3 Intra‐operative visceral injury
No evidence of a difference was found between total laparoscopic hysterectomy and single‐port total laparoscopic hysterectomy for bladder injury (OR 3.51, 95% CI 0.14 to 89.42, one RCT, 64 women, I2 = n/a, moderate quality evidence) (Analysis 5.1). Ureter, urinary tract, bowel and vascular injury were not reported in studies comparing SP‐LH and LH.
5.1. Analysis.
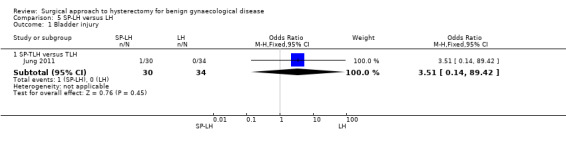
Comparison 5 SP‐LH versus LH, Outcome 1 Bladder injury.
5.4 Major long‐term complications
No studies compared this outcome for this comparison.
Secondary outcomes
5.5 Operation time
No evidence of a difference in operation time between SP‐LH and LH was found (MD 1.95 minutes, 95% CI ‐7.03 to 10.93, two RCTs, 164 women, I2 = 57%, moderate quality evidence) (Analysis 5.2).
5.2. Analysis.
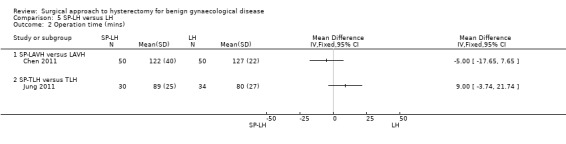
Comparison 5 SP‐LH versus LH, Outcome 2 Operation time (mins).
Data from Song 2013 on operation time could not be pooled, but also did not show evidence of a difference (LAVH median = 92 minutes; SP‐LAVH median = 95 minutes, P value = 0.47) (Analysis 5.9).
5.9. Analysis.
Comparison 5 SP‐LH versus LH, Outcome 9 Operation time (descriptive data).
| Operation time (descriptive data) | |||
|---|---|---|---|
| Study | SP‐LH | Conventional LH | Comments |
| Song 2013 | n = 20 SP‐LAVH Mean = 92 min Range 57 to 220 min |
n = 19 LAVH Mean = 95 min Range 70 to 154 min |
P value = 0.47 |
5.6 Intra‐operative complications (other than visceral injury)
No evidence of a difference between the groups was found for the following outcomes: , transfusion (OR 1.37, 95% CI 0.30 to 6.26, three RCTs, 203 women, I2 = 0%, low quality evidence) (Analysis 5.3), pelvic haematoma (OR 3.06, 95% CI 0.12 to 76.95, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 5.4).
5.3. Analysis.
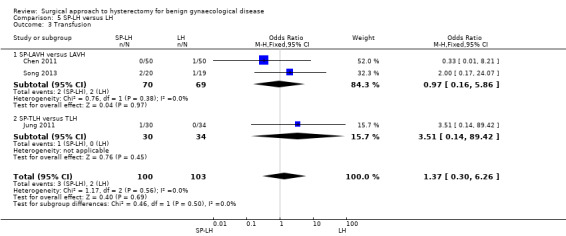
Comparison 5 SP‐LH versus LH, Outcome 3 Transfusion.
5.4. Analysis.
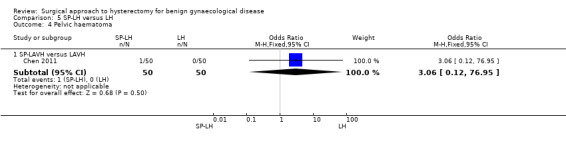
Comparison 5 SP‐LH versus LH, Outcome 4 Pelvic haematoma.
Numbers of bleeding and unintended laparotomy were not evaluated for this comparison.
5.7 Short‐term outcomes and complications
No evidence of a difference in hospital stay was found between TLH and SP‐TLH (MD ‐0.20, 95% CI ‐0.49 to 0.09, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 5.8).
5.8. Analysis.
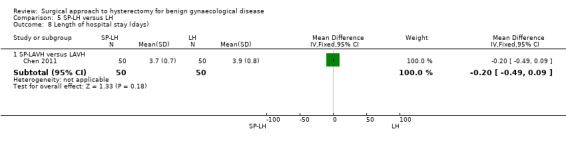
Comparison 5 SP‐LH versus LH, Outcome 8 Length of hospital stay (days).
Further data on hospital stay from two RCTs on SP‐TLH versus TLH could not be pooled, but both did not show evidence of a difference (Song 2013: median TLH 3 days versus median SP‐TLH 3 days, P value = 0.95 and Jung 2011: TLH median 3 days versus SP‐TLH 3.4 days, P value = 0.075, Analysis 5.10).
5.10. Analysis.
Comparison 5 SP‐LH versus LH, Outcome 10 Length of hospital stay (descriptive data).
| Length of hospital stay (descriptive data) | |||
|---|---|---|---|
| Study | SP‐LH | LAVH | Comments |
| Jung 2011 | n = 30 SP‐TLH Median postoperative hospital stay = 3.4 days Range 3.0 to 4.3 days |
n = 34 TLH Median postoperative hospital stay = 3.0 days Range 3.0 to 3.0 days |
P value = 0.075 |
| Song 2013 | n = 20 SP‐LAVH Mean = 3 days Range 2 to 4 days |
n = 19 LAVH Mean = 3 days Range 2 to 4 days |
P value = 0.95 |
No evidence of a difference was found for wound/abdominal wall infection between TLH and SP‐TLH (OR 0.33, 95% CI 0.01 to 8.21, one RCT, 100 women, I2 = n/a, low quality evidence) (Analysis 5.5). More febrile episodes or unspecified infections occurred in the SP‐TLH group than in the TLH group (OR 4.87, 95% CI 0.93 to 25.62, one RCT, 64 women, I2 = n/a, moderate quality evidence) (Analysis 5.6).
5.5. Analysis.

Comparison 5 SP‐LH versus LH, Outcome 5 Wound/abdominal wall infection.
5.6. Analysis.
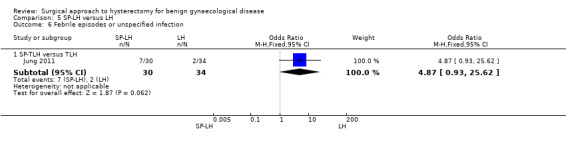
Comparison 5 SP‐LH versus LH, Outcome 6 Febrile episodes or unspecified infection.
No evidence of a difference in postoperative ileus occurrence was found (OR 2.36, 95% CI 0.20 to 27.39, one RCT, 64 women, I2 = n/a, moderate quality evidence) (Analysis 5.7).
5.7. Analysis.
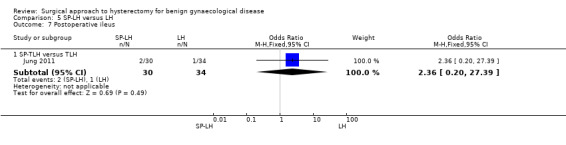
Comparison 5 SP‐LH versus LH, Outcome 7 Postoperative ileus.
Other infections, i.e. vaginal cuff, urinary tract or chest infection, were not reported.
Thromboembolism, perioperative mortality or wound dehiscence were not studied.
5.8 Cost
Cost was not studied for this comparison.
6. Total laparoscopic hysterectomy (TLH) versus laparoscopic‐assisted vaginal hysterectomy (LAVH)
Primary outcomes
6.1 Return to normal activities
No studies compared TLH and LAVH for this outcome.
6.2 Satisfaction and quality of life
No studies compared TLH and LAVH for this outcome.
6.3 Intra‐operative visceral injury
There was no evidence of a difference in injury to bladder (OR 0.72, 95% CI 0.06 to 8.27, two RCTs, 161 women, I2 = n/a, low quality evidence) (Analysis 6.1), ureter (OR 3.03, 95% CI 0.27 to 34.52, two RCTs, 161 women, I2 = n/a, low quality evidence) (Analysis 6.1), urinary tract (OR 1.50, 95% CI 0.29 to 7.83, two RCTs, 161 women, I2 = n/a, low quality evidence) (Analysis 6.1), or vascular injury (OR 1.48, 95% CI 0.09 to 24.27, one RCT, 101 women, I2 = n/a, low quality evidence) (Analysis 6.1) for the comparison TLH versus LAVH. No bowel injuries occurred in either group.
6.1. Analysis.
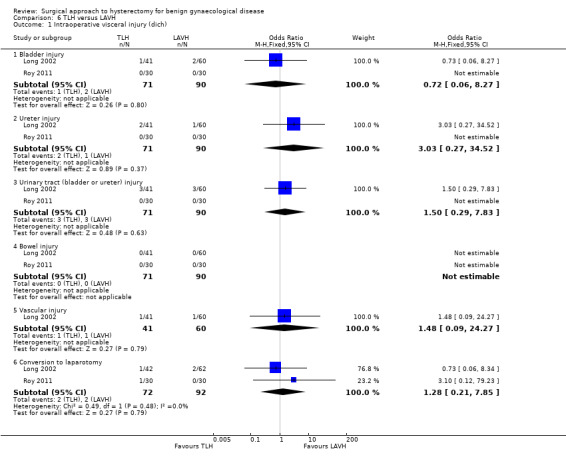
Comparison 6 TLH versus LAVH, Outcome 1 Intraoperative visceral injury (dich).
6.4 Major long‐term complications
No evidence of a difference was found in the following long‐term complications: dyspareunia (OR 2.64, 95% CI 0.59 to 11.72, one RCT, 101 women, I2 = n/a, low quality evidence) (Analysis 6.2) or failure to orgasm (OR 0.84, 95% CI 0.38 to 1.86, one RCT, 101 women, I2 = n/a, low quality evidence, Analysis 6.2). Other major long‐term complications (i.e. fistula formation, pelvi‐abdominal pain, urinary dysfunction, bowel dysfunction, pelvic floor condition) were not studied for this comparison.
6.2. Analysis.
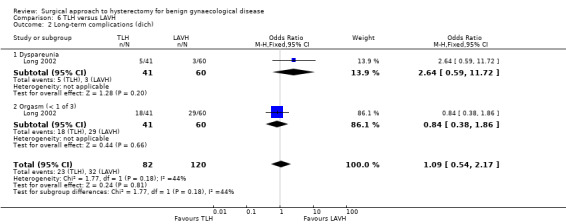
Comparison 6 TLH versus LAVH, Outcome 2 Long‐term complications (dich).
Secondary outcomes
6.5 Operation time
LAVH had a shorter operation time than TLH (MD ‐23.3 minutes, 95% CI ‐10.0 to ‐40.6; one RCT, 101 women, I2 = n/a, low quality evidence) (Analysis 6.3).
6.3. Analysis.
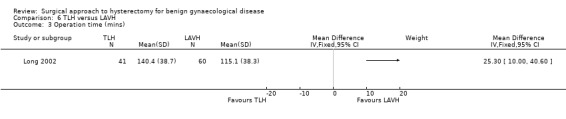
Comparison 6 TLH versus LAVH, Outcome 3 Operation time (mins).
6.6 Intra‐operative complications (other than visceral injury)
There was no evidence of a difference in the number of unintended laparotomies (OR 1.28, 95% CI 0.21 to 7.85, two RCTs, 104 women, I2 = 0%, low quality evidence) (Analysis 6.1).
6.7 Short‐term outcomes and complications
There was no evidence of a difference in hospital stay for TLH versus LAVH (MD 0.00, 95% CI ‐0.45 to 0.45, one RCT, 101 women, I2 = n/a, low quality evidence) (Analysis 6.5). No evidence of difference was found between TLH and LAVH for vaginal cuff infection (OR 0.28, 95% CI 0.03 to 2.45, one RCT, 101 women, I2 = n/a, low quality evidence) (Analysis 6.4), abdominal wall/wound infection (OR 0.19, 95% CI 0.01 to 4.06, one RCT, 60 women, I2 = n/a, low quality evidence) (Analysis 6.4), urinary tract infection (OR 1.00, 95% CI 0.13 to 7.60, one RCT, 60 women, I2 = n/a, low quality evidence) (Analysis 6.4) and febrile episodes (OR 0.50, 95% CI 0.17 to 1.48, two RCTs, 161 women, I2 = 66%, low quality evidence) (Analysis 6.4). There was no evidence of a difference in the number of patients that needed transfusion between TLH and LAVH (OR 1.04, 95% CI 0.24 to 4.43, two RCTs, 161 women, I2 = 0%, low quality evidence) (Analysis 6.4).
6.5. Analysis.
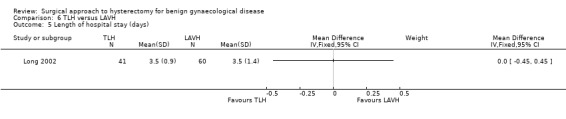
Comparison 6 TLH versus LAVH, Outcome 5 Length of hospital stay (days).
6.4. Analysis.
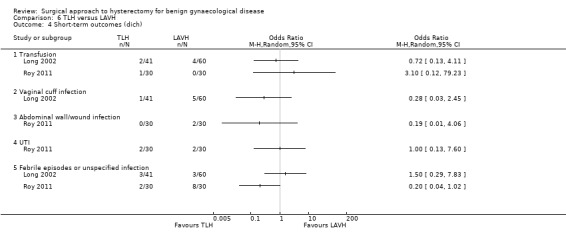
Comparison 6 TLH versus LAVH, Outcome 4 Short‐term outcomes (dich).
Other short‐term outcomes (thromboembolism, perioperative mortality, postoperative ileus or wound dehiscence) were not reported in the studies included in this review.
6.8 Cost
Cost was not studied for this comparison.
7. Mini‐laparoscopic hysterectomy (mini‐LH) versus total laparoscopic hysterectomy (TLH)
Primary outcomes
7.1 Return to normal activities
No studies compared mini‐laparoscopic hysterectomy and total laparoscopic hysterectomy for this outcome.
7.2 Satisfaction and quality of life
No studies compared mini‐laparoscopic hysterectomy and total laparoscopic hysterectomy for these outcomes.
7.3 Intra‐operative visceral injury
No studies compared mini‐laparoscopic hysterectomy and total laparoscopic hysterectomy for these outcomes.
7.4 Major long‐term complications
No studies compared mini‐laparoscopic hysterectomy and total laparoscopic hysterectomy for these outcomes.
Secondary outcomes
7.5 Operation time
Data on operation time could not be included in the meta‐analysis, but showed no evidence of a difference between mini‐laparoscopic hysterectomy and total laparoscopic hysterectomy (median mini‐LH 58 minutes; median TLH 60 minutes; one RCT, 66 women, low quality evidence) (Analysis 7.1).
7.1. Analysis.
Comparison 7 Mini‐LH versus TLH, Outcome 1 Operation time (descriptive data).
| Operation time (descriptive data) | |||
|---|---|---|---|
| Study | Mini‐TLH | Conventional TLH | Comments |
| Ghezzi 2011 | n = 38 Median = 58 mins Range: 30 to 135 mins |
n = 38 Median = 60 mins Range: 30 to 155 mins |
P value = 0.55 |
7.6 Intra‐operative complications (other than visceral injury)
. Bleeding, transfusion, pelvic haematoma or unintended laparotomy were not studied for this comparison.
7.7 Short‐term outcomes and complications
Women undergoing mini‐laparoscopic hysterectomy and total laparoscopic hysterectomy both had a median hospital stay of one day (one RCT, 66 women) (Analysis 7.2). The effect of these procedures on vaginal cuff, abdominal wall/wound, urinary tract or chest infections, or febrile episodes, were not studied.
7.2. Analysis.
Comparison 7 Mini‐LH versus TLH, Outcome 2 Length of hospital stay (descriptive data).
| Length of hospital stay (descriptive data) | |||
|---|---|---|---|
| Study | mini‐TLH | Conventional TLH | Comment |
| Ghezzi 2011 | n = 38 Median = 1 day Range: 0 to 2 |
n = 38 Median = 1 day Range: 1 to 2 |
P value = 0.73 |
7.8 Cost
Cost was not studied for this comparison.
Sensitivity analyses
Exclusion of trials susceptible to inadequate sequence generation during the randomisation process
Exclusion of seven trials with unclear or detrimental sequence generation (Ellstrom 1998; Kunz 1996; Long 2002; Olsson 1996; Perino 1999; Ribeiro 2003; Silva Filho 2006) altered the results as follows: bleeding and transfusion in LH versus VH were no longer significantly different; and transfusion in LH(a) versus AH was no longer significantly different.
Exclusion of trials susceptible to 'surgeon effect'
Exclusion of the four trials in which surgeons for one intervention were unequivocally different to those performing the other intervention did not alter the statistical significance of any meta‐analysis results (Kluivers 2007; Langebrekke 1996; Olsson 1996; Raju 1994).
Discussion
Summary of main results
Regarding the primary outcomes of this review, vaginal hysterectomy proved to be the superior procedure since it was associated with the quickest return to normal activities and earliest discharge from hospital. Furthermore, vaginal hysterectomy had the shortest operation time compared to both laparoscopic and abdominal hysterectomy. Vaginal hysterectomy proved to be superior to laparoscopic hysterectomy regarding substantial bleeding, use of oral pain tablets on day two and hospital costs. Laparoscopic hysterectomy offered a number of statistically significant advantages over abdominal hysterectomy; among these were quicker return to normal activities, less postoperative pain, earlier discharge from hospital and improved quality of life in the first months and at four years after surgery; the cost was more urinary tract injuries and longer operating time. Single‐port laparoscopic hysterectomy showed no significant advantages over conventional laparoscopic hysterectomy, besides better cosmetic outcomes. Robotic‐assisted hysterectomy offered no significant advantages over laparoscopic hysterectomy; however operation time was significantly longer. In conclusion, it seems that whenever vaginal hysterectomy is possible, it should be the preferred route over other approaches. However, uncertainty remains about the safety of these procedures based on the low number of adverse events in this review. LH appeared to result in better long‐term quality of life compared to AH; this is an important finding for the counselling of patients.
Urinary tract damage, in particular ureteric injury, remains the major concern related to the laparoscopic approach (Garry 2004; Garry 1995; Mäkinen 2013). However, this meta‐analysis of randomised controlled trials (RCTs) was underpowered to detect a clinically significant increase in the incidence of bladder and ureter damage as separate entities from a laparoscopic approach. Many of the data for an increased incidence of urinary tract injury have come from non‐randomised studies. Only large case series usually have the power to detect such rare complications, but RCTs remain the least biased way to assess the benefits and harms of an intervention. When we pooled bladder and ureter injuries in our meta‐analysis under a single category 'urinary tract injury', we detected a significant increase in urinary tract injury for LH versus AH.
Overall completeness and applicability of evidence
It is particularly difficult to address the issues surrounding effectiveness and complications in surgical procedures where the skill base of surgeons is not only variable, but differs also regarding surgeon experience of 'traditional' operations and laparoscopic operations. This is likely to be especially relevant to the rates at which complications, such as ureteric damage, occur. Hysterectomy outcomes tend to improve the more experience a surgeon gains in a particular technique (Mäkinen 2013). In contrast to exclusive assessment of numbers of performed operations, others have put emphasis on an intrinsic skills factor of each surgeon, which can only be monitored over time and in relation to the surgical case mix (Twijnstra 2012). There is no good way to assess the individual risk of rare complications per surgeon beyond the learning curve, but continuous monitoring of, for example, the CUSUM score, a tool to assess physicians’ clinical competence, may help us forward in this respect.
The number of studies in the review was too low and the description of surgical skills was not specific enough to assess learning curve effects for the different routes of hysterectomy in a subgroup analysis. This is not just a hysterectomy issue but pervades many aspects of surgical therapy and surgical innovations. It does not apply to the same extent where drug therapy interventions are being studied, in which the efficacy is much less dependent on the skill of the investigator providing the treatment. Much of the Cochrane methodology has been developed based on the medical model of intervention.
Regarding the overall applicability of the evidence, it must be noted that most studies in this review had specific inclusion criteria. For example, studies including vaginal hysterectomy in one treatment arm had different exclusion criteria, ranging from a uterine size more than 14 or more than 16 weeks of gestational age, pelvic organ prolapse, chronic pelvic pain and a (subjectively assessed) narrow vagina. The same matter is relevant for laparoscopic and abdominal hysterectomy. These specific inclusion and exclusion criteria make it more or less difficult to extrapolate the findings to everyday practice, where one is confronted with patients that often have more than one problem or have a surgical history that surpasses that of most included patients in the studies in this review.
Until the 1990s, the vast majority of hysterectomies were performed abdominally (Reich 2003; Vessey 1992), and routes of hysterectomy still vary widely per centre and country. In some countries there is a tendency to perform fewer abdominal hysterectomies in favour of other routes (Brummer 2008; Mäkinen 2013; Moen 2014a; Spilsbury 2006). In the current state of gynaecological practice and training, gynaecologists tend to become best trained in abdominal hysterectomy techniques, but there is huge variation in their learning curve position in relation to vaginal and laparoscopic hysterectomy techniques (Moen 2014b). Numbers of hysterectomies are overall decreasing with the introduction of more uterus‐preserving techniques in benign gynaecology (e.g. ablation techniques, Mirena intrauterine device (IUD)). For example, in the Netherlands, subspecialty has already been introduced in gynaecology training, which implies that not all gynaecologists will be able to self dependently perform a hysterectomy at the end of their training. The expected advantage is that the trainees who decide for a surgical profile will become better trained in hysterectomy.
In clinical practice as well as in the trials included in this review, vaginal hysterectomy will be mostly performed under optimum conditions only, whereas abdominal hysterectomy remains the default intervention for all more difficult cases. Each gynaecologist (as has been the case since abdominal hysterectomy became the alternative to vaginal hysterectomy, in 1863) will have his or her own indications for the choice of approach to hysterectomy for benign disease. These choices may be influenced to some extent by the results from scientific evidence (for example this review) but the decisions will also be largely based on their own array of surgical skills and the patient characteristics. Whether there will be more of a consensus in the future than there has been to date, regarding these indications for route of hysterectomy, is less certain. To reach this consensus, however, should probably not be the ultimate goal since the prudent decision for one approach to hysterectomy over the other may be very justified and may lead to better outcomes after all.
Patient‐reported outcome measures (PROMs) are increasingly recognised as important outcomes for medical interventions. PROMs (e.g. quality of life, patient experiences) can show the impact of surgery and complications on patients' lives, and thus can be a leading argument in the discussion about the best way to perform a hysterectomy (Dawson 2010). For instance, speed of recovery is determined by the avoidance of an abdominal procedure: abdominal hysterectomy is associated with lengthier recovery than all other approaches to hysterectomy. Only a few studies in the meta‐analysis have used quality of life as an outcome measure and only one study reported the long‐term (four years) effect on quality of life. However, the quality of life data do not lend themselves easily to meta‐analysis (due to the use of diverse tools, time frames and statistical analysis). The available data indicate that the laparoscopic and vaginal procedures performed better or equally compared with abdominal hysterectomy as far as quality of life in the first weeks after the procedure was concerned. Laparoscopic hysterectomy performed better after four years. In the decision as to the approach to hysterectomy, the advantage of better quality of life should be offset against the disadvantages. Meta‐analysis of PROMs, such as quality of life, would benefit from the use of well‐validated instruments applied in a standardised manner in future studies.
One concern is the statistical heterogeneity of the trials included in this review. The heterogeneity in such outcomes as operating time, even when the 'traditional' hysterectomy vaginal versus abdominal techniques are compared, directly relates to the fact that some surgeons are better trained in and thus perform faster either type of hysterectomy. This heterogeneity might be expected to be even more apparent when laparoscopic hysterectomy is compared with either abdominal or vaginal hysterectomy. Sculpher et al have analysed learning curve in the eVALuate trial (Sculpher 2004). The conclusion was that after completing the mandatory 25 cases to qualify for participation in the study, there was no surgical learning curve demonstrated, neither in seniority and experience nor related to the place in the timeline of the study.
Another point of discussion relates to the inclusion and exclusion criteria in several studies. Particularly the studies including an abdominal hysterectomy arm excluded women who were not eligible for the less invasive approaches to hysterectomy. This results in an abdominal hysterectomy population that is not representing the entire abdominal hysterectomy population in our clinical practice, but a population of only those women who were eligible for vaginal or laparoscopic hysterectomy as well.
Furthermore, studies typically do not address the same outcomes. This makes it difficult to draw clinically relevant conclusions. Increasingly it has been recognised that a standardised collection of core outcomes is needed. This resulted in the CROWN (CoRe Outcomes in WomeN's health) initiative, in which the Cochrane Menstrual Disorders and Subfertility Group also participates (Khan 2014). With respect to this review, it would be worth the effort to develop a core set of outcomes for the evaluation of hysterectomy.
Quality of the evidence
The quality of the evidence for the comparisons included in this review is mainly graded as low or moderate, resulting in uncertainty regarding the effects on primary and secondary outcomes between the different approaches to hysterectomy (Table 1; Table 2; Table 3). Limitations in the evidence included imprecision of results and inadequate reporting of study methods (e.g. randomisation and allocation procedure, no predefined primary and secondary outcomes). The 'Summary of findings' tables show the quality of evidence for our primary outcomes for the three main comparisons. With regard to abdominal versus vaginal hysterectomy there was a large difference in return to normal activities between the different studies, although all results were in favour of vaginal hysterectomy. In two studies, studying urinary tract injury, there was doubt about the method used for random sequence generation. With regard to laparoscopic versus abdominal hysterectomy doubt existed about the method used for random sequence generation or allocation of patients. There was a large difference in return to normal activities between the different studies, although all results were in favour of laparoscopic hysterectomy. Furthermore, there were wide confidence intervals crossing the line of no effect present.
Also, with regard to the comparison between laparoscopic and vaginal hysterectomy wide confidence intervals crossing the line of no effect were present. In some studies, studying urinary tract injury and unintended laparotomy, there was doubt about the method used for random sequence generation or allocation of patients. In some trials, studying complications, it was unclear how participants were randomised and allocated to their study group.
The majority of trials had unblinded participants, mostly imputed to the nature of the intervention (e.g. vaginal hysterectomy resulting in no abdominal scar in contrast with abdominal hysterectomy). However, as for example Miskry 2003 and Paraiso 2013 showed, sham abdominal dressings could be applied to blinded participants. This is particularly beneficial for unbiased patient‐reported outcomes, such as postoperative pain, satisfaction or quality of life. Trials studying short‐term outcomes in short follow‐up periods, had minimal missing data. However, importantly, some of the trials evaluating long‐term outcomes, such as quality of life (e.g. Garry 2004), had significant numbers lost to follow‐up. Therefore, the outcomes of these studies have to be interpreted with caution. An important reason for the low quality of evidence was imprecision of results, particularly resulting from the low number of adverse events in terms of intraoperative and major long‐term complications per study. This is important to take into account when interpreting the results regarding the safety of each type of hysterectomy.
Most outcomes for the comparisons between laparoscopic and abdominal hysterectomy, as well as laparoscopic and vaginal hysterectomy, are based on the large trial by Garry 2004, with a moderate risk of bias and most importantly a high rate of incomplete outcome data. Garry 2004 performed the largest trial (n = 1380) and used major complications as the primary outcome. The recruitment target was met in the laparoscopic versus abdominal hysterectomy arm but not in the laparoscopic versus vaginal hysterectomy arm. With regard to the comparison between vaginal and abdominal hysterectomy, the conclusions are based on six trials with comparable sample sizes and low risk of bias. The sensitivity analysis has led to some changes in statistical significance in various variables on bleeding and blood loss. Complication rates, operation times and recovery times did not change with the exclusion of trials with more detrimental trial quality.
In conclusion, further research is at least likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Potential biases in the review process
We used a rigorous process to identify all relevant studies, but we excluded grey literature. Some attempts to contact authors of studies lacking sufficient data to include them in this review were not successful. Four so‐called multi‐arm trials have been included in the review (Hwang 2002; Ottosen 2000; Ribeiro 2003; Sesti 2008a), where data have been used twice in different comparisons. There is not an agreed approach to this problem. Since no large effects of correlation and non‐independence of data are expected on the resulting conclusions, we took no special measures in the review to address this issue. Similar correlation between the two trials and inter‐dependence of data might be present in the study by Garry 2004, where the surgeon, and not randomisation, made the decision in which trial a patient was included. We followed procedures to reduce other potential bias in the review process.
Agreements and disagreements with other studies or reviews
Several other reviews and studies have evaluated different approaches to hysterectomy. Kovac 2014 reported that the evidence demonstrated that, in general, vaginal hysterectomy is associated with better outcomes and has fewer complications than laparoscopic or abdominal hysterectomy. This is also the conclusion from the Committee on Gynecologic Practice of the American College of Obstetrics & Gynecology (ACOG 2009). Furthermore, it is mentioned that laparoscopic hysterectomy is an alternative to abdominal hysterectomy for those women for whom a vaginal hysterectomy is not indicated or feasible. Overall, this is in accordance with the conclusions from this review. Pynnä 2014 performed a systematic review of studies that have investigated the cost‐effectiveness of hysterectomy for benign gynaecological disease. They concluded that the cost‐effectiveness of hysterectomy has been surprisingly poorly studied and that conclusions are difficult to draw due to the different study designs, indications, follow‐up times and quality of life instruments used. Laparoscopic hysterectomy seemed to be the least cost‐effective in their review, although further data from original patient cohorts with long‐term follow‐up are needed. However, they did not include any studies with robot‐assisted hysterectomy and not all studies included cost derived from sick leave. Smorgick 2014 studied he benefits and challenges of robotic‐assisted hysterectomy. Conforming with our review, they found that recent studies comparing robotic and laparoscopic hysterectomy for benign indications have not demonstrated a clear advantage for either approach in terms of complications, blood loss and hospital stay. The higher cost of robotic hysterectomy remains a significant disadvantage of this approach, although the total cost may decrease with increasing surgeon experience (via shorter operative time) and may be offset in some circumstances by reduced hospital stay and cost of complications compared with abdominal hysterectomy. It is expected that when more robotic consoles enter the market, prices will drop and cost‐effectiveness may move into the direction of that in laparoscopic hysterectomy. Furthermore, better ergonomic circumstances in robotic‐assisted hysterectomy will likely have the benefit of fewer physical complaints in laparoscopic surgeons and, consequently, less cost regarding surgeons absenteeism.
Authors' conclusions
Implications for practice.
Among women undergoing hysterectomy for benign disease, vaginal hysterectomy appears to be superior to laparoscopic and abdominal hysterectomy, as it is associated with a speedier return to normal activities. When technically feasible, vaginal hysterectomy should be performed in preference to abdominal hysterectomy because of more rapid recovery and fewer febrile episodes postoperatively. Where vaginal hysterectomy is not possible, laparoscopic hysterectomy has some advantages over abdominal hysterectomy (including less operative blood loss, more rapid recovery, fewer febrile episodes, and fewer wound or abdominal wall infections) but these are offset by a longer operating time. No advantages of laparoscopic over vaginal hysterectomy could be found; laparoscopic hysterectomy had a longer operation time, and total laparoscopic hysterectomy had more urinary tract injuries. Of the three subcategories of laparoscopic hysterectomy, there are more randomised controlled trial (RCT) data for laparoscopic‐assisted vaginal hysterectomy and LH(a) than for total laparoscopic hysterectomy. The surgical approach to hysterectomy should be decided by the woman in discussion with her surgeon in light of the relative benefits and hazards. These benefits and hazards seem to be dependent on surgical expertise and this may influence the decision. Single‐port laparoscopic and robotic‐assisted hysterectomy should be either abandoned or further evaluated since there is a lack of evidence of any benefit over conventional laparoscopic hysterectomy. However, this has to be interpreted with caution as adverse event rates were low, resulting in low power for these outcomes.
Implications for research.
The concept of evidence‐based gynaecological surgery has been challenged based on the many pitfalls in being able to successfully undertake RCTs to assess surgical interventions (Johnson 2009), however our extensive systematic review of surgical approaches to hysterectomy shows the concept of evidence‐based gynaecological surgery to be alive and well. When the quality of RCTs of surgical interventions is sufficiently good, this yields information unrivalled in its quality compared to studies of other designs that assess surgical interventions. There is no longer any excuse not to undertake high quality trials of surgical interventions.
The enhanced evidence on short‐term outcomes and adverse events generated by this meta‐analysis would benefit from large study populations, with surgeons well beyond their learning curve. Since laparoscopic hysterectomy was introduced 20 years ago and adequate training programmes are available, studies undertaken during the learning curve will not be helpful for making choices in current clinical practice. We also recommend that future trials should stratify allocation by surgeon, so that there is a balance of procedures performed by each surgeon in both arms. It should, however, be noted that outcomes for patients treated by the same surgeon will be correlated, and that failure to account for this will lead to incorrect inferences in the individual studies.
More high quality research would be welcome regarding the long‐term effects of the different approaches to hysterectomy, such as pelvic organ dysfunction.
The various subcategories of laparoscopic hysterectomy may be further evaluated against each other. For example, whether total laparoscopic hysterectomy has any benefits or harms in comparison to other forms of laparoscopic hysterectomy (including LH(a) and laparoscopic‐assisted vaginal hysterectomy). The increase in the rate of ureteric injury resulting from laparoscopic hysterectomy, suggested by very large observational studies, remains to be conclusively proven by RCT data. We strongly encourage trial authors to report their laparoscopic approach to hysterectomy according to our defined subcategories: laparoscopic‐assisted vaginal, LH(a), total laparoscopic and subtotal laparoscopic hysterectomy (Table 4). This should minimise the confusion that has prevailed in the first published literature on laparoscopic hysterectomy. Single‐port laparoscopic and robotic‐assisted hysterectomy should be performed in clinical trials only, since there is lack of evidence of any benefit over conventional laparoscopic hysterectomy. The claimed superior ergonomics of robotic hysterectomy has not been shown to give rise to enhanced patients outcomes.
Although it is important that RCTs should have the same surgeon (or group of surgeons) carrying out each of the approaches being compared, different levels of expertise with each approach means that such RCTs are always likely to be statistically heterogeneous when considered for pooling in meta‐analyses.
There is an absence of data for long‐term outcomes in RCTs comparing surgical approaches to hysterectomy. RCTs should aim to report long‐term outcomes, including urinary, bowel and sexual function, along with occurrence of fistulae. Quality of life or other PROMs may be regarded as key outcomes in trials on approaches to hysterectomy for benign disease to capture the patient's perspective. To enable meta‐analysis of quality of life data, well‐validated instruments should be applied in a standardised manner.
What's new
| Date | Event | Description |
|---|---|---|
| 20 October 2014 | New citation required and conclusions have changed | This review has been updated. We have included 17 new studies (Candiani 2009; Chakraborty 2011; Chen 2011; Ghezzi 2010; Ghezzi 2011; Jung 2011; Kongwattanakul 2012; Paraiso 2013; Roy 2011; Roy 2012; Sarlos 2012; Sesti 2008a; Sesti 2008b; Song 2013; Nieboer 2012; Persson 2006; Zhu 2009). Some of the conclusions have changed. We have included three new types of intervention in the review; these have emerged as new approaches to hysterectomy in randomised controlled trials, i.e. robot‐assisted hysterectomy, mini laparoscopic hysterectomy and single‐port laparoscopic hysterectomy. We have excluded Drahonovsky 2006 and Morelli 2007 in this update of the review |
| 20 October 2014 | New search has been performed | The addition of new studies has led to a change in the conclusions of this review. |
History
Protocol first published: Issue 2, 2002 Review first published: Issue 1, 2005
| Date | Event | Description |
|---|---|---|
| 12 February 2009 | New citation required and conclusions have changed | New authors: Theodoor E Nieboer, Sabine van Voorst, Ben Willem J Mol, Kirsten B Kluivers. Seven new studies were included. The following comparisons became statistically significant in the update: a shorter operation time in LAVH compared to TLH; more substantial bleeding in LH compared to VH; more febrile episodes or unspecified infections in TLH compared to LAVH; higher score on subscale vitality after LH compared to AH; higher satisfaction in VH compared to AH. New comparison: TLH versus LAVH. |
| 9 June 2008 | Amended | Converted to new review format. |
| 5 February 2008 | New citation required and conclusions have changed | Substantive amendment. |
Acknowledgements
We thank the trial authors for their tremendous effort, and the editors and external peer reviewers of this work.
We thank David Barlow, who was involved in the accomplishment of the protocol and the first review, for all his work.
We thank Sebastian Franik for his contributions to the 'Summary of findings' tables.
We thank Mrs Anne Lethaby, Auckland who commented on the protocol, assisted with selection of trials, data extraction, and data entry in the first review, and has contributed to all previous versions.
We thank the following people for their contributions to previous versions of this review: Jane Clarke, the former Managing Editor of Cochrane Menstrual Disorders and Subfertility Group, New Zealand; Sabine van Voorst, the Netherlands; Elisabeth Curr, New Zealand.
Appendices
Appendix 1. MDSG search
MDSG Specialised Register SS for NJ473 11.11.10
Keywords CONTAINS "Hysterectomy" or Title CONTAINS "Hysterectomy"
AND
Keywords CONTAINS "Hysterectomy,abdominal" or "Hysterectomy, Vaginal" or "hysterectomy ‐laparoscopic" or "hysterectomy, laparoscopically assisted vaginal" or "Hysterectomy, subtotal" or "hysterectomy techniques" or "laparoscopic assisted vaginal hysterectomy" or "laparoscopic hysterectomy" or "LAVH" or Title CONTAINS "Hysterectomy,abdominal" or "Hysterectomy, Vaginal" or "hysterectomy ‐laparoscopic" or "hysterectomy, laparoscopically assisted vaginal" or "Hysterectomy, subtotal" or "hysterectomy techniques" or "laparoscopic assisted vaginal hysterectomy" or "laparoscopic hysterectomy" or "LAVH" or "TVH" or "TLH" or "vaginal hysterectomy"or "abdominal hysterectomy"or "abdominal myomectomy"or"laparoscopic"or"laparoscopic procedure"or"laparoscopic surgical treatment"or"laparoscopically assisted hysterectomy"or"laparoscopically assisted vaginal hysterectomy"or"laparoscopy"or "laparotomy"or"mini‐laparoscopy"or "mini‐laparotomy"or "abdominal hysterectomy"
Appendix 2. CENTRAL search
Cochrane Central Register of Controlled Trials (CENTRAL) in all fields (on Ovid platform)
1. Hysterectomy 2. Abdominal 3. Vaginal 4. Laparoscopic assisted 5. Laparo‐vaginal 6. Laparoscopic 7. 1 and 2 or 3 or 4 or 5 or 6
Appendix 3. MEDLINE search
Ovid MEDLINE(R) (1946 to 2014 week 32)
Search strategy:
1 exp HYSTERECTOMY/ (24605) 2 hysterectom$.tw. (26883) 3 1 or 2 (37348) 4 abdom$.tw. (253636) 5 vaginal$.tw. (74351) 6 (lap$ adj assist$).tw. (3843) 7 (lap$ adj5 vaginal$).tw. (1692) 8 LAVH.tw. (324) 9 LVH.tw. (3897) 10 (Ah or Vh or Lh).tw. (62452) 11 TLH.tw. (309) 12 exp Laparoscopy/ (69937) 13 Laparoscop$.tw. (84412) 14 route$.tw. (121604) 15 technique$.tw. (1094816) 16 approach$.tw. (1056843) 17 exp Laparotomy/ (15750) 18 laparotom$.tw. (38835) 19 minilaparotom$.tw. (927) 20 or/4‐19 (2520921) 21 3 and 20 (16470) 22 randomized controlled trial.pt. (385723) 23 controlled clinical trial.pt. (89662) 24 randomized.ab. (305899) 25 placebo.tw. (162963) 26 clinical trials as topic.sh. (172008) 27 randomly.ab. (220260) 28 trial.ti. (131972) 29 (crossover or cross‐over or cross over).tw. (62251) 30 or/22‐29 (950838) 31 exp animals/ not humans.sh. (3994784) 32 30 not 31 (876347) 33 21 and 32 (1715) 34 2014$.ed. (619882) 35 2014$.dp. (613080) 36 34 or 35 (1063755) 37 33 and 36 (106)
Appendix 4. EMBASE search
EMBASE (1980 to 2014 Week 32)
1 Controlled study/ or randomised controlled trial/ 2 double blind procedure/ 3 single blind procedure/ 4 crossover procedure/ 5 drug comparison/ 6 placebo/ 7 random$.ti,ab,hw,tn,mf. 8 latin square.ti,ab,hw,tn,mf. 9 crossover.ti,ab,hw,tn,mf. 10 cross‐over.ti,ab,hw,tn,mf. 11 placebo$.ti,ab,hw,tn,mf. 12 ((doubl$ or singl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).ti,ab,hw,tn,mf. 13 (comparative adj5 trial$).ti,ab,hw,tn,mf. 14 (clinical adj5 trial$).ti,ab,hw,tn,mf. 15 or/1‐14 16 nonhuman/ 17 animal/ not (human/ and animal/) 18 or/16‐17 19 15 not 18 20 exp HYSTERECTOMY/ 21 hysterectom$.tw. 22 20 or 21 23 abdom$.tw. 24 vaginal$.tw. 25 (Lap$ adj Assist$).tw. 26 (Lap$ adj Vaginal$).tw. 27 LAVH.tw. 28 LH.tw. 29 or/23‐28 30 exp Surgical Technique/ 31 route$.tw. 32 technique$.tw. 33 approach$.tw. 34 or/30‐33 35 22 and 29 36 34 and 35 37 19 and 36
Appendix 5. CINAHL search
CINAHL search strategy for NJ473 28.01.14
# Query Results
S38 S22 AND S36
S37 S22 AND S36
S36 S23 OR S24 or S25 or S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35
S35 TX allocat* random*
S34 (MH "Quantitative Studies")
S33 (MH "Placebos")
S32 TX placebo*
S31 TX random* allocat*
S30 (MH "Random Assignment")
S29 TX randomi* control* trial*
S28 TX ( (singl* n1 blind*) or (singl* n1 mask*) ) or TX ( (doubl* n1 blind*) or (doubl* n1 mask*) ) or TX ( (tripl* n1 blind*) or (tripl* n1 mask*) ) or TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
S27 TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
S26 TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
S25 TX clinic* n1 trial*
S24 PT Clinical trial
S23 (MH "Clinical Trials+")
S22 S3 AND S21
S21 S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20
S20 TX minilaparotom*
S19 TX laparotom*
S18 (MM "Laparotomy")
S17 TX approach*
S16 TX technique*
S15 TX route*
S14 TX Laparoscop*
S13 (MM "Laparoscopy")
S12 TX TLH
S11 TX (Ah or Vh or Lh)
S10 TX LVH
S9 TX LAVH
S8 TX (lap* N2 vagina*)
S7 TX (lap* N2 assist*)
S6 TX vagina*
S5 (MM "Hysterectomy, Vaginal")
S4 TX abdomin*
S3 S1 OR S2
S2 TX Hysterectom*
S1 (MH "Hysterectomy+")
Appendix 6. Biological abstracts search
Biological Abstracts (1969 to August 2008, not included in searches beyond 2008)
1 exp HYSTERECTOMY/ (0) 2 hysterectom$.tw. (10663) 3 1 or 2 (10663) 4 abdom$.tw. (149794) 5 vaginal$.tw. (31662) 6 (lap$ adj assist$).tw. (691) 7 (lap$ adj5 vaginal$).tw. (540) 8 LAVH.tw. (71) 9 LVH.tw. (1654) 10 Laparoscop$.tw. (16487) 11 route$.tw. (373620) 12 technique$.tw. (3259392) 13 approach$.tw. (354093) 14 laparo$.tw. (29111) 15 or/4‐14 (3796162) 16 3 and 15 (7312) 17 limit 16 to yr="2007 ‐ 2008" (529) 18 from 17 keep 1‐529 (529)
Appendix 7. PsycINFO search
PsycINFO <1806 to August Week 1 2014>
Search strategy:
1 exp Hysterectomy/ (384) 2 hysterectom$.tw. (677) 3 or/1‐2 (698) 4 abdom$.tw. (4874) 5 vaginal$.tw. (3769) 6 (lap$ adj assist$).tw. (6) 7 (lap$ adj5 vaginal$).tw. (10) 8 LAVH.tw. (2) 9 LVH.tw. (23) 10 Laparoscop$.tw. (304) 11 route$.tw. (11033) 12 technique$.tw. (151513) 13 approach$.tw. (369519) 14 or/4‐13 (509044) 15 3 and 14 (149) 16 limit 15 to yr="2014 ‐Current" (2)
Appendix 8. Clinical Trials Register
1. Hysterectomy 2. Abdominal 3. Vaginal 4. Laparoscopic assisted 5. Laparo‐vaginal 6. Laparoscopic 7. 1 and 2 or 3 or 4 or 5 or 6
Appendix 9. Data extraction
-
Trial characteristics
-
Method of randomisation, in order of preference, as follows:
third party randomisation, for example by pharmacy, computer, or telephone;
true randomisation by carer, for example by opaque numbered envelope or register;
not stated.
-
Study design:
blinding;
duration of follow‐up;
type of follow‐up.
-
Size of study:
number of women recruited;
number of women randomised;
number of women excluded;
number of women withdrawn and lost to follow‐up;
number of women analysed.
-
Study setting:
single centre or multicentre;
location;
timing and duration;
source of funding stated or not.
-
Analyses:
whether a power calculation was performed and adhered to;
whether 'intention‐to‐treat' analysis was performed by authors, was possible from the data but not performed by authors, not possible or uncertain.
-
Criteria for hysterectomy:
indications specified;
data broken down by indications for hysterectomy.
-
-
Characteristics of the study participants
-
Baseline characteristics:
age;
parity;
indication for hysterectomy;
investigative work up, for example pelvic ultrasound scan, endometrial sampling;
previous treatments;
exclusion criteria.
-
Treatment characteristics:
pre‐operative preparation, for example pre‐operative medical treatment;
level of training of surgeons.
-
-
Interventions
Approach to hysterectomy, percentage of patients having subtotal hysterectomy
Subcategory in case of LH (i.e. LAVH, LH(a) and TLH)
Use of technique to support the vaginal vault
Proportion undergoing bilateral elective oophorectomy versus ovarian conservation
Other strategies to reduce the likelihood of complications
Absence of co‐interventions in treatment and control groups
If the trial compared a surgical approach performed by one (group of) surgeon(s) with another surgical approach performed by a second (group of) surgeon(s)
-
Outcomes
Primary outcomes:
1. Return to normal activities
2. Satisfaction and quality of life
3. Intra‐operative visceral injury: bladder injury, ureter injury, urinary tract (bladder or ureter) injury, bowel injury, vascular injury
4. Major long‐term complications: fistula, pelvi‐abdominal pain, urinary dysfunction, bowel dysfunction, pelvic floor condition (prolapse), sexual dysfunction
Secondary outcomes:
5. Operation time
6. Other intra‐operative complication: estimated blood loss, (sequelae of) bleeding, including substantial bleeding, haemoglobin or haematocrit drop, transfusion, pelvic haematoma, unintended laparotomy for approaches not involving routine laparotomy
7. Short‐term outcomes and complications: length of hospital stay, infections: vaginal cuff, abdominal wall or wound, urinary tract infection, chest infection, febrile episodes or unspecified infections, thromboembolism, perioperative mortality, postoperative ileus, wound dehiscence, pain scales and pain relief
8. Costs
Data and analyses
Comparison 1. VH versus AH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Return to normal activities (days) | 3 | 176 | Mean Difference (IV, Random, 95% CI) | ‐12.33 [‐19.89, ‐4.77] |
| 2 Long‐term outcomes: satisfaction (dichotomous) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Intraoperative visceral injury (dichotomous) | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Bladder injury | 4 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.48, 19.97] |
| 3.2 Ureter injury | 1 | 119 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 Urinary tract (bladder or ureter) injury | 4 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.48, 19.97] |
| 3.4 Bowel injury | 2 | 319 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.5 Vascular injury | 1 | 119 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Long‐term complications (dichotomous) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Urinary dysfunction | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Operation time (mins) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 VH versus standard AH | 3 | 259 | Mean Difference (IV, Random, 95% CI) | ‐11.01 [‐35.09, 13.08] |
| 5.2 VH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐63.0 [‐65.11, ‐60.89] |
| 6 Short‐term outcomes (dichotomous) | 6 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Transfusion | 5 | 495 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.34, 1.96] |
| 6.2 Pelvic haematoma | 5 | 535 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.34, 2.89] |
| 6.3 Vaginal cuff infection | 2 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 6.4 Wound/abdominal wall infection | 3 | 355 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.04, 1.00] |
| 6.5 UTI | 3 | 176 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.08, 4.61] |
| 6.6 Chest infection | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 6.7 Febrile episodes or unspecified infection | 5 | 495 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.36, 1.08] |
| 6.8 Thromboembolism | 1 | 119 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Length of hospital stay (days) | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 VH versus standard AH | 4 | 295 | Mean Difference (IV, Fixed, 95% CI) | ‐1.07 [‐1.22, ‐0.92] |
| 7.2 VH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐2.1 [‐2.19, ‐2.01] |
| 8 All outcomes, descriptive data | Other data | No numeric data | ||
| 8.1 Quality of life (descriptive data) | Other data | No numeric data | ||
| 8.2 Operation time (descriptive data) | Other data | No numeric data | ||
| 8.3 Length of hospital stay (descriptive data) | Other data | No numeric data |
Comparison 2. LH versus AH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Return to normal activities (days) | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 LAVH versus AH | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐8.40 [‐12.15, ‐4.65] |
| 1.2 LH(a) versus AH | 5 | 440 | Mean Difference (IV, Fixed, 95% CI) | ‐15.17 [‐17.21, ‐13.14] |
| 2 Satisfaction | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 LH (method unspecified) versus AH | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Bladder injury | 12 | 2038 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.91, 3.90] |
| 3.1 LAVH versus AH | 3 | 396 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 7.17] |
| 3.2 LH(a) versus AH | 4 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.49, 8.24] |
| 3.3 TLH versus AH | 2 | 99 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.05, 6.73] |
| 3.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.65 [0.88, 7.93] |
| 4 Ureter injury | 7 | 1417 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.46 [0.94, 12.71] |
| 4.1 LH(a) versus AH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 6.12 [0.29, 130.87] |
| 4.2 TLH versus AH | 3 | 201 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.35 [0.34, 32.97] |
| 4.3 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.82 [0.44, 18.03] |
| 5 Urinary tract (bladder or ureter) injury | 13 | 2140 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [1.24, 4.80] |
| 5.1 LAVH versus AH | 3 | 396 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 7.17] |
| 5.2 LH(a) versus AH | 4 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.79 [0.73, 10.68] |
| 5.3 TLH versus AH | 3 | 201 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [0.30, 8.63] |
| 5.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.13 [1.12, 8.78] |
| 6 Bowel injury | 4 | 1175 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.03, 1.33] |
| 6.1 LAVH versus AH | 1 | 50 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.25] |
| 6.2 TLH versus AH | 1 | 59 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 LH (method unspecified) versus AH | 2 | 1066 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.60] |
| 7 Vascular injury | 2 | 956 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.76 [0.52, 5.87] |
| 7.1 LAVH versus AH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.26 [0.24, 113.11] |
| 7.2 LH (method unspecified) versus AH | 1 | 876 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.35, 5.08] |
| 8 Fistula | 2 | 245 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.32, 29.96] |
| 8.1 LH(a) versus AH | 1 | 143 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.12, 77.01] |
| 8.2 TLH versus AH | 1 | 102 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.06 [0.12, 76.88] |
| 9 Urinary dysfunction | 2 | 246 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.48, 1.84] |
| 9.1 LAVH versus AH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 9.2 LH (method unspecified) versus AH | 1 | 166 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.44, 1.76] |
| 10 Operation time (mins) | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 LAVH versus AH | 4 | 466 | Mean Difference (IV, Random, 95% CI) | 0.27 [‐23.39, 23.93] |
| 10.2 LH(A) versus AH | 5 | 420 | Mean Difference (IV, Random, 95% CI) | 33.45 [14.82, 52.08] |
| 10.3 TLH versus AH | 2 | 161 | Mean Difference (IV, Random, 95% CI) | 28.74 [2.64, 54.85] |
| 10.4 LAVH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐8.0 [‐10.56, ‐5.44] |
| 11 Bleeding | 5 | 1266 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.15, 1.37] |
| 11.1 LAVH versus AH | 2 | 197 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.08, 4.64] |
| 11.2 LH(a) versus AH | 2 | 193 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.34] |
| 11.3 LH (method unspecified) versus AH | 1 | 876 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.16, 14.51] |
| 12 Transfusion | 19 | 2638 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.30, 1.10] |
| 12.1 LAVH versus AH | 5 | 539 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.11, 1.34] |
| 12.2 LH(a) versus AH | 8 | 641 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.17, 1.35] |
| 12.3 TLH versus AH | 2 | 161 | Odds Ratio (M‐H, Random, 95% CI) | 0.27 [0.03, 2.47] |
| 12.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.08, 9.85] |
| 12.5 LAVH versus minilaparotomy AH | 2 | 181 | Odds Ratio (M‐H, Random, 95% CI) | 1.38 [0.09, 20.52] |
| 13 Pelvic haematoma | 8 | 782 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.38, 1.47] |
| 13.1 LAVH versus AH | 3 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.05, 2.10] |
| 13.2 LH(a) versus AH | 4 | 406 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.97] |
| 13.3 LAVH versus minilaparotomy AH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 14 Unintended laparotomy | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 LAVH versus minilaparotomy AH | 2 | 181 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.08, 2.82] |
| 15 Length of hospital stay (days) | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 LAVH versus AH | 4 | 466 | Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐4.16, ‐1.12] |
| 15.2 LH(a) versus AH | 4 | 380 | Mean Difference (IV, Random, 95% CI) | ‐1.82 [‐2.34, ‐1.31] |
| 15.3 TLH versus AH | 2 | 161 | Mean Difference (IV, Random, 95% CI) | ‐2.53 [‐5.08, 0.01] |
| 15.4 LAVH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐1.1 [‐1.20, ‐1.00] |
| 16 Vaginal cuff infection | 9 | 852 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.67, 3.04] |
| 16.1 LAVH versus AH | 3 | 396 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.37] |
| 16.2 LH(a) versus AH | 6 | 456 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.73, 4.37] |
| 17 Wound/abdominal wall infection | 6 | 611 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.12, 0.71] |
| 17.1 LAVH versus AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.19] |
| 17.2 LH(a) versus AH | 4 | 259 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.12, 1.03] |
| 17.3 LH (method unspecified) versus AH | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.03, 2.21] |
| 17.4 LAVH versus minilaparotomy AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.19] |
| 18 Urinary tract infection | 8 | 659 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.54, 2.00] |
| 18.1 LAVH versus AH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.22] |
| 18.2 LH(a) versus AH | 5 | 339 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.55, 2.95] |
| 18.3 LH (method unspecified) versus AH | 2 | 240 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.26, 2.69] |
| 19 Chest infection | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.07, 1.35] |
| 19.1 LH(a) versus AH | 2 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.10, 3.93] |
| 19.2 LH (method not specified) versus AH | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 2.01] |
| 20 Febrile episodes or unspecified infection | 16 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 LAVH versus AH | 4 | 339 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.09, 0.73] |
| 20.2 LH(a) versus AH | 7 | 572 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.33, 0.90] |
| 20.3 TLH versus AH | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.11, 1.21] |
| 20.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.65, 1.37] |
| 20.5 LAVH versus minilaparotomy AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.72] |
| 21 Thromboembolism | 3 | 1125 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.23, 3.39] |
| 21.1 TLH versus AH | 1 | 59 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.01, 9.76] |
| 21.2 LH (method unspecified) versus AH | 2 | 1066 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.24, 5.13] |
| 22 Wound dehiscence | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 LAVH versus minilaparotomy AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.15 [0.12, 79.69] |
| 23 Return to normal activities (descriptive data) | Other data | No numeric data | ||
| 24 Long‐term outcomes: quality of life (descriptive data) | Other data | No numeric data | ||
| 25 Operation time (descriptive data) | Other data | No numeric data | ||
| 26 Length of hospital stay (descriptive data) | Other data | No numeric data | ||
| 27 Pain relief (descriptive data) | Other data | No numeric data | ||
| 27.1 Pain scales | Other data | No numeric data | ||
| 27.2 Postoperative analgesics | Other data | No numeric data | ||
| 27.3 Recovery from pain (days) | Other data | No numeric data | ||
| 28 Cost (descriptive data) | Other data | No numeric data |
2.23. Analysis.
Comparison 2 LH versus AH, Outcome 23 Return to normal activities (descriptive data).
| Return to normal activities (descriptive data) | |||
|---|---|---|---|
| Study | LH | AH | Comments |
| Langebrekke 1996 | n = 46 median = 19.5 days range (0 to 140) | n = 54 median = 36.5 days range (23 to 259) | P value < 0.001 Wilcoxon rank‐sum test |
| Persson 2006 | n = 63 median = 26 days range (3 to 86) | n = 56 median = 33.5 days range (14 to 61) | P value = 0.0081 |
| Raju 1994 | n = 40 median = 21 days range = (7 to 35) | n = 40 median = 42 days range (21 to 67) | P value < 0.0001 Mann‐Whitney U test |
| Schutz 2002 | n = 28 median = 42 days | n = 20 median = 42 days | — |
2.27. Analysis.
Comparison 2 LH versus AH, Outcome 27 Pain relief (descriptive data).
| Pain relief (descriptive data) | ||||
|---|---|---|---|---|
| Study | Description | LH | AH | Conclusions |
| Pain scales | ||||
| Ellstrom 1998 | Pain during rest and when coughing. 100 mm visual analogue scale, endpoints 'no pain' and 'worst pain possible'. Day 0, Day 1 (10am and 6pm) and Day 2 | n = 40 DAY 0 (8pm). At rest: mean = 22, SD = 16. Coughing: mean = 29, SD = 20 DAY 1 (10am). At rest: mean = 17, SD = 16. Coughing: mean = 32, SD = 19. P value < 0.05 DAY 1 (6pm). At rest: mean = 24, SD = 20. Coughing: mean = 31, SD = 25 DAY 2 (10am). At rest: mean = 10, SD = 10. Coughing: mean = 15, SD = 14. P value < 0.01 | n = 40 DAY 0 (8pm). At rest: mean = 36, SD = 26. Coughing: mean = 48, SD = 30 DAY 1 (10am). At rest: mean = 30, SD = 24. Coughing: mean = 53, SD = 30. P value < 0.05 DAY 1 (6pm). At rest: mean = 28, SD = 24. Coughing: mean = 52, SD = 28 DAY 2 (10am). At rest: mean = 20, SD = 22. Coughing: mean = 47, SD = 31 P value < 0.01 | Lower pain score following LAVH compared to AH at 10am on 1st and 2nd day when coughing (P value < 0.05 and P value < 0.01 respectively). No significant difference with the pain scores at rest |
| Falcone 1999 | Weekly visual analogue scales for pain (from "no pain" to "most severe pain". Reported in graph form | n = 22 Data portrayed in graph | n = 20 Data portrayed in graph | No significant difference in change over time (group by time interaction) between groups. No difference in mean pain scores over the postoperative interval (P value = 0.38). The number of weeks before a pain score of less than 1 was recorded was not significantly different between the 2 groups (P value = 0.95) |
| Garry 2004 | Daily diary using a visual analogue scale, scored on day 0 (operation day), and days 2, 7 and 21. Analysis of covariance used to adjust pain scores over days 0 to 6 by the number of days that opiates were used | VH: n = 168 vLH: n = 336 Adjusted means: 3.1 VH and 3.5 vLH, mean difference of ‐0.3 (CI ‐0.7, 0.002), P value = 0.07) | AH: n = 292 aLH: n = 584 Adjusted means: 3.9 AH and 3.5 aLH, mean difference of 0.4 CI (0.09, 0.7, P value = 0.01) | A higher proportion of AH participants used opiates than aLH. AH is more painful than aLH and LH has a tendency to be less painful than vLH |
| Marana 1999 | 10‐point visual analogue scale. Evaluation of pain on postoperative days 1, 2 and 3 | n = 58 DAY 0: mean = 40, SD = 1.2, P value < 0.001 DAY 1: mean = 5.2, SD = 2.6, P value < 0.05 DAY 2: mean = 2.3, SD = 2.3, P value < 0.001 DAY 3: mean 1.3, SD = 1.6, P value < 0.005 | n = 58 DAY 0: mean = 5.9, SD = 2.3, P value < 0.001 DAY 1: mean = 6.3, SD = 1.6, P value < 0.05 DAY 2: mean = 4.4, SD = 1.9, P value < 0.001 DAY 3: mean = 2.8, SD = 2.3, P value < 0.005 | Significant difference between 2 groups at 3 evaluations. Lower pain score following LAVH compared to AH |
| Muzii 2007 | VAS scores (no further description) Postoperative day 1 and 2 |
n = 40 Day 1 median = 2.8 Range (0 to 6) Day 2 median = 0.8 Range (0 to 3.7) |
n = 41 Day 1 median = 4.4 Range (2 to 6.2) Day 2 median = 2.9 Range (2 to 5.5) |
Day 1 P value < 0.05 Day 2 P value < 0.05 |
| Olsson 1996 | Visual analogue scale (range 0 to 7), 2 days after surgery | n = 71 Median = 3.6, P value < 0.05 | n = 72 Median = 4.2, P value < 0.05 | Postoperative pain 2 days after surgery was significantly less following LAVH compared to AH |
| Perino 1999 | 10‐point visual analogue scale, 0 = no pain to 10 = maximum pain. Assessed pain for 3 days after surgery | n = 51 DAY 1: mean = 4.1, SD = 1.2. DAY 2: mean = 2.3, SD = 1.6. DAY 3: mean 1.0, SD = 0.7. P value < 0.001 | n = 51 DAY 1: mean = 6.9, SD = 1.8. DAY 2: mean = 5.4, SD = 1.3. DAY 3: mean = 3.1, SD = 0.9. P value < 0.001 | Participants who underwent LH had less intense postoperative pain than those in the AH group |
| Schutz 2002 | 10‐point visual analogue scale on days 1, 3 and 5. Pain index on 4th postoperative day (WHO scale) | n = 28 Pain index: median = 0 (0 to 1.75), P value < 0.05 | n = 20 Pain index: median = 5 (4 to 6), P value < 0.05 | Pain index was 0 on postoperative day 4 in the LH group and 5 in the AH group, LH was significantly less painful than AH |
| Postoperative analgesics | ||||
| Falcone 1999 | Length of time PCA pump was required (hours) and number of narcotic (oxycodone) or acetaminophen pills used in the hospital and after discharge was recorded | n = 23 PCA: Median = 22.1 hours, range (15.9 to 23.5), P value < 0.001 Number of narcotics (in hospital): median = 6, range (2.0 to 9.0), P value = 0.21. After discharge: median = 19.5, range(2 to 26), P value = 0.28. Number of non‐narcotics (in hospital): median = 0, range (0 to 4), P value = 0.36. After discharge: median = 11, range (2 to 31), P value = 0.71 | n = 21 PCA: Median = 36.7 hours, range (26.2 to 45), P value < 0.001 Number of narcotics (in hospital): Median = 8.5, range (4 to 10), P value = 0.21. After discharge: Median = 8, range (0 to 23.5), P value = 0.28 Number of non‐narcotics (in hospital): Median = 0, range (0 to 3.5), P value = 0.004. After discharge: median = 13.5, range (1 to 66), P value = 0.71 | Participants in the LH group required less PCA time |
| Ferrari 2000 | Analgesic requirement recorded daily for 3 groups (number who require analgesia for more than 24 hours after surgery): 1) Whole series of participants 2) Participants with uteri weighing under 500 g and 3) uteri weighing greater than 500 g | Group 1: n = 31 Median = 7, n% = 23, P value < 0.001 Group 2: n = 20. Median = 1, n% = 5, P value = 0.0001 Group 3: n = 11). Median = 6, n% = 55 | Group 1: n = 31. Median = 24, n% = 77, P value < 0.001. Group 2: n = 21. Median = 16, n% = 76, P value = 0.0001 Group 3: n = 10. Median = 8, n% = 80 | LAVH was associated with a significantly lower administration of analgesics after the first 24 postoperative hours. Group 2, uteri weighing less than 500 g, LAVH was associated with less analgesic administration |
| Kluivers 2007 | Number of participants receiving opioids during the first 3 days after surgery were recorded | n = 27 Use of opioids: 10 | n = 32 Use of opioids: 22 | Less women in LH versus AH group required opioids (P value < 0.01) |
| Langebrekke 1996 | Number of participants receiving analgesics (parenterally, oral and rectal analgesics) during the hospital stay and 5 days postoperatively | n = 46 Data portrayed as bar chart | n = 54 Data portrayed as bar chart | The need for both kinds of analgesics was reduced in the LH group |
| Raju 1994 | Duration of postoperative analgesia (days) | n = 40 Median = 6.6 days, range (0 to 23). P value < 0.0001 | n = 40 Median = 13.3 days, range (2 to 38) P value < 0.0001 | Participants in the LAVH group required fewer days of analgesia than participants in the AH group |
| Summitt 1998 | Use of intramuscular narcotics and oral pain medication | n = 34 26 of the 34 participants required IM narcotics on the day of surgery, P value = 0.018 | n = 31 30 of the 31 participants required IM narcotics on the day of surgery, P value = 0.18 | A statistically greater number of patients in the AH group required IM narcotics on the day of surgery compared to those in the LH group |
| Recovery from pain (days) | ||||
| Raju 1994 | Number of days until participants are free from pain | n = 40 Median = 13 days, range (6 to 34). P value < 0.0001 | n = 40 Median = 26 days, range (10 to 46) P value < 0.0001 | Participants who had LAVH recovered from pain quicker than those who had AH |
2.28. Analysis.
Comparison 2 LH versus AH, Outcome 28 Cost (descriptive data).
| Cost (descriptive data) | ||||
|---|---|---|---|---|
| Study | Description | LH | AH | Comments |
| Ellstrom 1998 | Analysis of cost over a period of 12 weeks, starting on the day the participant entered the hospital. Direct costs (hospital costs) and indirect costs (loss of production value) were analysed separately. Units of currency = Swedish crowns (SEK) | n = 38 Direct costs (average) = SEK 23,169 Indirect costs (average) = SEK 10,314 | n = 38 Direct costs (average) = SEK22,780. Indirect costs (average) = SEK20,743. | The change in costs between LH and AH are negligible as approximately 50% of hospital costs are fixed costs |
| Falcone 1999 | Hospital costs (amount a provider must pay for goods and services) were assessed through the hospital accounting system. The direct and indirect costs were calculated for each patient from 3 different components: operating room costs, anaesthesia costs and ward costs | n = 24 Difference in medians (LH‐AH): total hospital costs = USD 277 (CI ‐163 to 1097), P value = 0.21 | n = 24 (see LH) | Total hospital costs were not significantly higher in the LH group than the AH group |
| Lumsden 2000 | Single set of unit costs applied to each unit of resource to provide a NHS cost for each woman. 1997/98 prices | n = 95 Total cost (operation, inpatient stay and readmissions): median = GBP 2112, mean = GBP 2479 Cost excluding disposables: median = GBP 1740, mean = GBP 2173 | n = 95 Total cost: median = £1667, mean = £1832. Cost excluding disposables: median = £1667, mean = £1832 | AH had significantly lower total costs than LH, resulting principally from the difference in operation costs. When the cost of disposable equipment was removed, the difference was non‐significant |
| Raju 1994 | Cost analysis of each type of procedure on the major points of difference between either operation: cost of disposable consumables and the comparative costs of postoperative lengths of stay in hospital | n = 40 Cost of operation (average) = GBP 225. Cost of mean length of stay including operation time and cost of disposable instruments = GBP 1260 | n = 40 Cost of operation (average) = GBP 30. Cost of mean length of stay including operation time and cost of disposable instruments = GBP 1750 | — |
| Summitt 1998 | Hospital charges for both groups | n = 34 Mean = USD 8161, SD = 3600, range (3061 to 23,591). P value > 0.05 | n = 31 Mean = USD 6974, SD = 2843, range (3183 to 16,086). P value > 0.05 | Lack of a statistical difference in total hospital charges |
Comparison 3. LH versus VH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Return to normal activities (days) | 2 | 140 | Mean Difference (IV, Fixed, 95% CI) | ‐1.07 [‐4.21, 2.06] |
| 1.1 LAVH versus VH | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [‐5.11, 1.91] |
| 1.2 LH(a) versus VH | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐5.95, 7.95] |
| 2 Ureter injury | 2 | 594 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.06, 37.18] |
| 2.1 LAVH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.06, 37.18] |
| 3 Bladder injury | 7 | 895 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.32, 2.56] |
| 3.1 LAVH versus VH | 2 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.22] |
| 3.2 LH(a) versus VH | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.98 [0.30, 29.43] |
| 3.3 TLH versus VH | 2 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 3.4 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.18, 3.79] |
| 4 Urinary tract (bladder or ureter) injury | 7 | 895 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.36, 2.75] |
| 4.1 LAVH versus VH | 2 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.22] |
| 4.2 LH(a) versus VH | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.98 [0.30, 29.43] |
| 4.3 TLH versus VH | 2 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 4.4 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.23, 4.38] |
| 5 Bowel injury | 2 | 639 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 LAVH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 TLH versus VH | 1 | 90 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Vascular injury | 4 | 685 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.48, 5.27] |
| 6.1 LH(a) versus VH | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.89 [0.11, 74.15] |
| 6.2 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.39, 5.22] |
| 7 Fistula | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 LH(a) versus VH | 1 | 56 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.01, 7.67] |
| 8 Urinary dysfunction | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 LAVH versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 9 Operation time (mins) | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 LAVH versus VH | 5 | 377 | Mean Difference (IV, Random, 95% CI) | 33.60 [20.13, 47.07] |
| 9.2 LH(a) versus VH | 3 | 213 | Mean Difference (IV, Random, 95% CI) | 53.58 [43.67, 63.49] |
| 9.3 TLH versus VH | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 17.30 [3.34, 31.26] |
| 10 Bleeding | 3 | 614 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.24, 10.09] |
| 10.1 LAVH versus VH | 2 | 65 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 10.2 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 10.3 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.06, 37.18] |
| 11 Transfusion | 8 | 1039 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.80, 3.18] |
| 11.1 LAVH versus VH | 4 | 273 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.16, 3.41] |
| 11.2 LH(a) versus VH | 3 | 217 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.49 [0.63, 9.86] |
| 11.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 11.4 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.63, 4.79] |
| 12 Pelvic haematoma | 4 | 308 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.36, 4.03] |
| 12.1 LAVH versus VH | 3 | 228 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.40, 7.26] |
| 12.2 LH(a) versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.04, 5.60] |
| 13 Unintended laparotomy | 10 | 1160 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.76, 3.16] |
| 13.1 LAVH versus VH | 5 | 353 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.33 [0.46, 40.61] |
| 13.2 LH(a) versus VH | 3 | 213 | Odds Ratio (M‐H, Fixed, 95% CI) | 6.11 [1.06, 35.21] |
| 13.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 13.4 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.26, 1.74] |
| 14 Vaginal cuff infection | 4 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.22, 4.39] |
| 14.1 LAVH versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 16.56] |
| 14.2 LH(a) versus VH | 3 | 196 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.16, 5.73] |
| 15 Wound/abdominal wall infection | 2 | 170 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.88 [0.31, 27.06] |
| 15.1 LAVH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.72 [0.12, 60.29] |
| 15.2 LH(a) versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 15.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Urinary tract infection | 3 | 230 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.40, 6.82] |
| 16.1 LAVH versus VH | 2 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.15, 6.89] |
| 16.2 LH(a) versus VH | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.10 [0.12, 79.23] |
| 16.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.72 [0.12, 60.29] |
| 17 Chest infection | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 LH(a) versus VH | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 4.06] |
| 18 Febrile episodes or unspecified infection | 9 | 1074 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.51, 1.24] |
| 18.1 LAVH versus VH | 4 | 253 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.49, 4.85] |
| 18.2 LH(a) versus VH | 3 | 196 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.28, 3.51] |
| 18.3 TLH versus VH | 2 | 121 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.06, 1.74] |
| 18.4 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.41, 1.25] |
| 19 Thromboembolism | 2 | 564 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.15, 6.67] |
| 19.1 TLH versus VH | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.24] |
| 19.2 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.52 [0.12, 52.76] |
| 20 Length of hospital stay (days) | 7 | 525 | Mean Difference (IV, Random, 95% CI) | 0.88 [0.73, 1.03] |
| 20.1 LAVH versus VH | 4 | 308 | Mean Difference (IV, Random, 95% CI) | 0.91 [0.76, 1.06] |
| 20.2 LH(a) versus VH | 2 | 157 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.42, 1.22] |
| 20.3 TLH versus VH | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐2.41, 1.41] |
| 21 Return to normal activities (descriptive data) | Other data | No numeric data | ||
| 22 Long‐term outcomes: quality of life (descriptive data) | Other data | No numeric data | ||
| 23 Operation time (descriptive data) | Other data | No numeric data | ||
| 24 Length of hospital stay (descriptive data) | Other data | No numeric data | ||
| 25 Pain relief (descriptive data) | Other data | No numeric data | ||
| 25.1 Pain scales | Other data | No numeric data | ||
| 25.2 Postoperative analgesics | Other data | No numeric data | ||
| 26 Cost (descriptive data) | Other data | No numeric data |
3.5. Analysis.
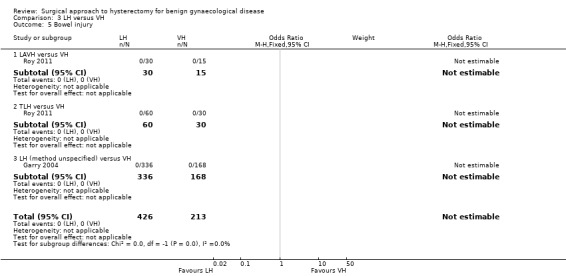
Comparison 3 LH versus VH, Outcome 5 Bowel injury.
3.24. Analysis.
Comparison 3 LH versus VH, Outcome 24 Length of hospital stay (descriptive data).
| Length of hospital stay (descriptive data) | |||
|---|---|---|---|
| Study | LH | VH | Comments |
| Hwang 2002 | n = 30 median = 4.7 days range (3 to 7) | n = 30 median = 4.7 days range (3 to 7) | Not tested separately |
| Richardson 1995 | n = 22 mean = 3.2 days range (2 to 7) | n = 23 mean = 3.3 days range (1 to 18) | — |
| Roy 2011 | TLH: n = 30 median = 2 days min‐max = 2 to 12 days LAVH: n = 30 median = 3 days min‐max = 4 days |
VH: n = 30 median = 2 days min‐max = 1 to 4 days |
P value = 0.15 |
| Roy 2012 | n = 10 median = 3 days min‐max = 2 to 4 days |
n = 10 median = 2 days min‐max = 2 to 4 days |
Not statistically significant |
3.25. Analysis.
Comparison 3 LH versus VH, Outcome 25 Pain relief (descriptive data).
| Pain relief (descriptive data) | ||||
|---|---|---|---|---|
| Study | Description | LH | VH | Conclusion |
| Pain scales | ||||
| Ghezzi 2010 | VAS pain scores at several times post surgery | n = 41 VAS score after 1 h: mean = 4.7, SD = 2.6 VAS score after 3 h: mean = 3.2, SD = 2.5 VAS score after 8 h: mean = 2.1, SD = 2.2 VAS score after 24 h: mean = 1.8, SD = 1.7 |
n = 41 VAS score after 1 h: mean = 7.8, SD = 1.7 VAS score after 3 h: mean = 6.6, SD = 2.0 VAS score after 8 h: mean = 5.3, SD = 2.1 VAS score after 24 h: mean = 3.6, SD = 2.6 |
P value < 0.0001 P value < 0.0001 P value < 0.0001 P value = 0.001 |
| Sesti 2008b | VAS pain 24 hours post surgery | 6 patients (15%) reported absence of pain 24 hours post surgery | 20 patients (50%) reported absence of pain (VAS = 0) 24 hours post surgery | Patients undergoing LAVH had more postoperative pain compared with patients undergoing VH |
| Postoperative analgesics | ||||
| Ghezzi 2010 | The need for additional use of analgesics after the operation | n = 41 7 (17.1%) |
n = 41 32 (78.0%) |
P value < 0.0001 |
| Richardson 1995 | The number of postoperative opoid injections and the number of days analgesia was required was recorded | n = 22 Opoid injections: mean = 2.3, range (0 to 8) Analgesia required: mean = 2.9 days, range (0 to 20) | n = 23 Opoid injections: mean = 2.6, range (0 to 15) Analgesia required: mean = 2.6 days, range (1 to 17) | The number of opoid injections and analgesia requirements were similar in each group |
| Soriano 2001 | Total consumption of paracetamol, NSAID and subcutaneous opoid | n = 37 Paracetamol: mean = 11.1 g, SD = 5.6 NSAID:mean = 137 mg, SD = 148 Opoid: mean 6.8 mg, SD = 13.7 | n = 40 Paracetamol: mean = 10.1 g, SD = 6.7 NSAID: mean = 137 mg, SD = 155 Opoid: mean = 8.7 mg, SD = 15.7 | No significant difference in the total consumption of paracetamol, NSAID and subcutaneous opoid between the 2 groups |
| Summitt 1992 | Pain control was assessed by documenting the intramuscular narcotic use on the day of surgery and the number of pain tablets used on the day of surgery and the first 2 postoperative days | n = 28 Number of oral pain tablets. Day of surgery: mean = 3.13, SD = 2.1, range(0 to 9). P value = NS Postop Day 1: mean = 3.67, SD = 2.5, range (1 to 10). P value = NS Postop Day 2: mean = 2.71, SD = 2.9, range (0 to 12). P value = 0.27 Number of participants requiring IM narcotics within the first 6 hours after surgery: 9 | n = 27 Number of oral pain tablets. Day of surgery: mean = 3.82, SD = 1.8, range (0 to 7). P value = NS Postop Day 1: mean = 3.61, SD = 2.3, range (0 to 10). P value = NS Postop Day 2: mean = 1.57, SD = 1.5, range (0 to 5). P value = 0.27 Number of participants requiring IM narcotics within the first 6 hours after surgery: 8 | — |
3.26. Analysis.
Comparison 3 LH versus VH, Outcome 26 Cost (descriptive data).
| Cost (descriptive data) | |||
|---|---|---|---|
| Study | Description | LH | VH |
| Summitt 1992 | Mean total hospital charge when surgery was performed on an outpatient basis. Charges consisted of: operating room fee, operating room time, anaesthesia time, charges for disposable staples, scissors, graspers and a charge for recovery in the ambulatory surgery unit, including laboratory fees | n = 29 Mean = USD 7905, SD = 501, range (7197 to 8289), P value = 0.035 | n = 27 Mean = USD 4891, SD = 355, range (4311 to 5247), P value = 0.035 |
Comparison 4. RH versus LH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Return to normal activities (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Intraoperative visceral injury (dichotomous) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Ureter injury | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 2.2 Vascular injury | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 16.44] |
| 2.3 Wound/abdominal wall infection | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 2.4 Wound dehiscence | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 3 Operation time | 2 | 152 | Mean Difference (IV, Random, 95% CI) | 44.09 [5.31, 82.88] |
| 4 Transfusion | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Return to normal activities (descriptive data) | Other data | No numeric data |
4.5. Analysis.
Comparison 4 RH versus LH, Outcome 5 Return to normal activities (descriptive data).
| Return to normal activities (descriptive data) | ||||
|---|---|---|---|---|
| Study | Description | RH | LH | Comment |
| Paraiso 2013 | Percentage to return to normal baseline activities at 1, 2, 3, 4, 5 and 6 weeks postoperatively |
1 week (n = 17): 22% 2 weeks (n = 17): 46% 3 weeks (n = 17): 54% 4 weeks (n = 17): 60% 5 weeks (n = 17): 66% 6 weeks (n = 16): 72% |
1 week (n = 19): 29% 2 weeks (n = 19): 46% 3 weeks (n = 18): 58% 4 weeks (n = 18): 64% 5 weeks (n = 17): 73% 6 weeks (n = 17): 82% |
P value (overall) = 0.25 |
Comparison 5. SP‐LH versus LH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Bladder injury | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.51 [0.14, 89.42] |
| 2 Operation time (mins) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 SP‐LAVH versus LAVH | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 SP‐TLH versus TLH | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Transfusion | 3 | 203 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.30, 6.26] |
| 3.1 SP‐LAVH versus LAVH | 2 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.16, 5.86] |
| 3.2 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.51 [0.14, 89.42] |
| 4 Pelvic haematoma | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 SP‐LAVH versus LAVH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.06 [0.12, 76.95] |
| 5 Wound/abdominal wall infection | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 SP‐LAVH versus LAVH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 6 Febrile episodes or unspecified infection | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.87 [0.93, 25.62] |
| 7 Postoperative ileus | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.36 [0.20, 27.39] |
| 8 Length of hospital stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 SP‐LAVH versus LAVH | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.49, 0.09] |
| 9 Operation time (descriptive data) | Other data | No numeric data | ||
| 10 Length of hospital stay (descriptive data) | Other data | No numeric data |
Comparison 6. TLH versus LAVH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intraoperative visceral injury (dich) | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Bladder injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.06, 8.27] |
| 1.2 Ureter injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.03 [0.27, 34.52] |
| 1.3 Urinary tract (bladder or ureter) injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.29, 7.83] |
| 1.4 Bowel injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.5 Vascular injury | 1 | 101 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.09, 24.27] |
| 1.6 Conversion to laparotomy | 2 | 164 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.21, 7.85] |
| 2 Long‐term complications (dich) | 1 | 202 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.54, 2.17] |
| 2.1 Dyspareunia | 1 | 101 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.64 [0.59, 11.72] |
| 2.2 Orgasm (< 1 of 3) | 1 | 101 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.38, 1.86] |
| 3 Operation time (mins) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4 Short‐term outcomes (dich) | 2 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Transfusion | 2 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Vaginal cuff infection | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Abdominal wall/wound infection | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 UTI | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Febrile episodes or unspecified infection | 2 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Comparison 7. Mini‐LH versus TLH.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Operation time (descriptive data) | Other data | No numeric data | ||
| 2 Length of hospital stay (descriptive data) | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Agostini 2006.
| Methods | Single‐centre study, parallel‐group design Duration: April 2002 to February 2004 (1 year, 10 months) Randomisation: computer‐generated allocation list Allocation concealment: numbered, sealed, opaque envelopes Blinding: no Number of women eligible and randomised = 48 Dropouts: there were no dropouts or conversions Follow‐up: women were followed up until 1 month after surgery. No loss to follow‐up Power calculation for sample size: yes. 24 patients per group were necessary to detect a difference in complications between the 2 groups of 35% or more (25% versus 60% in VHO and LAVHO respectively) with 80% power and a significance level of 0.05 Analysis by intention‐to‐treat: yes (no conversions) |
|
| Participants | 48 women with a mean age of 55 years in the VHO group and 53 years in the LAVHO group Inclusion criteria: women with benign disease, older than 45 years, uterine size below halfway pubis and umbilicus Exclusion criteria: virgin patient, contraindication pneumoperitoneum, adnexal mass | |
| Interventions |
VHO versus LAVHO
VHO: standard VH technique with removal of ovaries and tubes as described by Ballard, or an endo loop in case needed
LAVHO: laparoscopic dissection of suspensory ligaments and round ligaments, followed by vaginal hysterectomy. Laparoscopy at the end of the procedure
Both groups received prophylactic antibiotic treatment (Cefoxitin IV)
GA for both VHO and LAVHO Surgeons: 5 different surgeons carried out both procedures Surgeon experience: surgeons experienced in vaginal surgery |
|
| Outcomes | Primary outcome: complications (blood loss more than 500 ml, blood transfusion, haematoma, postoperative fever) Secondary outcomes: operative time; hospital stay | |
| Notes | France University Hospital of Marseille Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocation list |
| Allocation concealment (selection bias) | Low risk | Numbered, sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No clear primary outcome was defined |
| Other bias | Unclear risk | Surgeons' experience with laparoscopic procedures not reported |
Benassi 2002.
| Methods | Single‐centre study, parallel‐group design Duration: June 1997 to December 2000 (2 years, 6 months) Randomisation: computer‐selected randomisation Allocation concealment: not clearly described Blinding: no Number of women randomised = 119. No dropouts reported Follow‐up: no loss to follow‐up No power calculation reported |
|
| Participants | 119 women with a mean age of 47 years for the AH group and 48 years for the VH group Inclusion criteria: women with symptomatic enlarged uteri (200 ml to 1300 ml) Exclusion criteria: prolapse, uterine or adnexal neoplasia, pelvic inflammation, vaginal stenosis, previous pelvic or vaginal procedures, hormonal treatment in the 6 months prior to surgery | |
| Interventions |
AH versus VH
AH and VH performed according to Novak technique
Peri‐menopausal patients also underwent bilateral oophorectomy
Antibiotic treatment: both groups received prophylactic antibiotic treatment (cefotaxime 2 g IV) and anticoagulant therapy with enoxaparin 2000 IU
General anaesthetic for AH; spinal anaesthetic for VH Surgeons: the same surgeons carried out the surgery. Experience not reported |
|
| Outcomes | Operative time; operative complications (injury to major vessel, ureter, bladder and bowel); drop in haemoglobin; postoperative complications; hospital stay No clear primary or secondary outcomes |
|
| Notes | Italy University Hospital of Parma Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐selected randomisation |
| Allocation concealment (selection bias) | Unclear risk | Patients were randomly allocated, not clearly described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not (pre)defined |
| Other bias | Unclear risk | No other bias identified. Surgeons' experience not reported |
Candiani 2009.
| Methods | Single‐centre study, parallel‐group design Duration: April 2004 to April 2006 (2 years) Randomisation: computer‐generated Allocation concealment: sealed, opaque envelopes Blinding: no Number of women eligible = 95. Number of patients randomised = 60 Follow‐up: in the 12‐month follow‐up, 7 patients in LH and 6 in VH were lost to follow‐up. There were no conversions Power calculation was performed for sample size: 30 patients per group were necessary to detect a difference of more than 25% in discharge at day 2 (less than 5% versus more than 30% in VH and LH, respectively) with 80% power and a significance level of 0.05 Analysis by intention‐to‐treat: yes (no conversions) |
|
| Participants | 60 women with a mean age of 49 years in the LH group and 51 in the VH group Inclusion criteria: women with an indication for vaginal hysterectomy for benign pathology Exclusion criteria: uterine volume greater than 300 ml, previous surgery for pelvic inflammatory disease or endometriosis, suspicion of malignancy, the presence of an ovarian cyst greater than 4 cm and a vaginal prolapse higher than first degree |
|
| Interventions |
LH versus VH LH: total laparoscopic hysterectomy including the laparoscopic closure of the vaginal cuff and its suspension to the uterosacral ligaments VH: following Heaney's technique Antibiotic treatment: prophylactic antibiotic treatment (type not mentioned) at the beginning of the surgery and repeated 12 hours later Type of anaesthesia (in VH): not mentioned Surgeons' experience: all the procedures were performed by 2 skilled surgeons for each group; only surgeons who had performed at least 50 procedures were involved |
|
| Outcomes |
Primary outcome: hospital stay (with fixed parameters to discharge patients) Secondary outcomes: pain (as measured by VAS and analgesic request), blood loss and execution of adnexectomy if preoperatively planned |
|
| Notes | Italy San Paolo Hospital, University School of Medicine (Milan) Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocation list |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes based on a computer‐generated allocation list |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout and loss to follow‐up mentioned; no conversions. 10% lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Primary endpoint was clearly stated |
| Other bias | Low risk | No other bias identified |
Chakraborty 2011.
| Methods | Single‐centre study, parallel‐group design Duration: June 2006 to May 2008 (2 years) Randomisation: computer‐generated random numbers Allocation concealment: envelopes Blinding: no Number of women randomised = 200. No dropouts reported. No conversions mentioned Follow‐up: duration of follow‐up not mentioned. No loss to follow‐up Power calculation for sample size: not reported Analysis by intention‐to‐treat: not reported |
|
| Participants | 200 women; age only mentioned in groups and not in means Inclusion criteria: women scheduled for hysterectomy for benign disease without uterine decent and a uterine size < 14 weeks gestational age Exclusion criteria: primary diagnosis related to cancer, pelvic endometriosis, adnexal pathology, multiple abdominal scar from previous surgery and prolapse |
|
| Interventions |
VH versus AH VH: non‐descent vaginal hysterectomy. The surgical technique is not described either for VH or for AH Use of prophylactic antibiotic treatment not reported Surgeons' experience not mentioned |
|
| Outcomes | Length of hospital stay, operating time, intra and postoperative blood transfusion, minor and major complications | |
| Notes | India Hospital New Raipur (Dabur Park) Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Computer‐generated random numbers were used for randomisation. While assigning groups to envelopes, if the computer‐generated random number was odd, the assigned group was A (non‐descent vaginal hysterectomy). If the random number was even, the envelope was assigned to group B: abdominal hysterectomy |
| Allocation concealment (selection bias) | Low risk | Simple random allocation of study participants to 2 surgical procedure groups was done by using envelopes numbered from 001 to 200. While assigning groups to envelopes, if the computer‐generated random number was odd, the assigned group was A (non‐descent vaginal hysterectomy) for the first (001 numbered) envelope. A card with Group‐A: ND vaginal hysterectomy written over it was put inside the envelope. The next envelope was then taken and next random number was checked. If the random number was even, the envelope was assigned to group B: abdominal hysterectomy. A card with Group‐B: abdominal hysterectomy written over it was put inside the envelope no 002. Similarly cards with group‐A/B written over them were put inside sequentially numbered envelopes by matching with odd/even random numbers as generated by computer. 1st patient for the clinical trial was allocated to the group assigned to the envelope no‐001, 2nd patient was allotted to the group assigned to the envelope no.002. In this way 200 participants were allocated into 2 intervention groups and eventually the numbers in 2 groups were 100 in group A and 100 in group B |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Unclear risk | The distribution in age and parity between the groups is somewhat skewed. Surgeon's experience not reported |
Chen 2011.
| Methods | Single‐centre study Duration: September 2009 to June 2010 Randomisation: computerised balanced method (1:1). Random numbers were computer‐generated Allocation concealment: random numbers were inserted in numbered, sealed and opaque envelopes. A single envelope was opened by the surgeon when the patient was hospitalised Blinding: no Number of women: assessed for eligibility = 118, randomised = 102 Follow‐up: single‐port LAVH ‐ no loss to follow‐up or dropout; multiple‐port LAVH ‐ 2 excluded from analysis, 0 lost to follow‐up ‐ 2 discontinued intervention Power calculation for sample size: yes, based on previous study of 24‐hour pain scores, they used 2.5 +/‐ 0.7 compared with 3.5 +/‐ 0.8 (mean and SD) and 1.9 +/‐ 1.4 compared with 2.8 +/‐ 1.4 for single‐port LAVH and multi‐port LAVH, as the primary criterion to calculate a minimum sample size of 45 patients for each group |
|
| Participants | n = 102 Inclusion criteria: women, age 30 to 79 years, and an ASA classification of I or II Exclusion criteria: if disease was malignant, if they needed additional adnexal surgery (n = 13) or unwilling to participate (n = 3) |
|
| Interventions |
Single‐port LAVH versus multi‐port LAVH Single‐port LAVH: A 1.5 cm horizontal intra‐umbilical skin incision, a 1.5 cm to 2 cm rectus fasciotomy to open the peritoneal cavity, insertion small wound extractor. The wrist of surgical glove fixed to outer ring of wound extractor. A 12 mm trocar was inserted through a small hole made in one of the fingertip areas of the glove and advanced into the abdominal cavity. An additional hole for the accessory channel was made in another fingertip of the glove and one 5 mm trocar was inserted Multi‐port LAVH: 4 ports, one 12 mm port inserted umbilically, the other 5 mm ports in lateral abdominal wall and suprapubic. 0 degree rigid 10 mm scope Surgeons: all procedures were performed by a single surgeon, assisted by another surgeon, at a single institute Antibiotics: perioperative antibiotic treatment not reported Postoperative assessment performed by 2 independent investigators |
|
| Outcomes | Postoperative pain (at 12, 24 and 48 hours, VAS) Operative time, additional procedures, blood loss, transfusion requirements, postoperative hospital stay |
|
| Notes | Taiwan Taipei Veterans General Hospital, Taipei Funding reported, i.e. Taipei Veterans General Hospital, Taipei and Yen‐Tjing‐Ling Medical Foundation, Taiwan |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated numbers |
| Allocation concealment (selection bias) | Low risk | Numbered, sealed and opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts and loss to follow‐up reported. No loss to follow‐up. 2 discontinued multi‐port LAVH |
| Selective reporting (reporting bias) | Unclear risk | No primary outcome defined. Insufficient information available |
| Other bias | Unclear risk | Surgeons reported, but experience unclear. Analysis according to intention‐to‐treat not mentioned |
Darai 2001.
| Methods | Multicentre study (n = 2), parallel‐group design Duration: January to December 1999 (1 year) Randomisation: pre‐determined computer‐generated randomisation code Allocation concealment: not reported Blinding: no Number of women randomised = 80. No dropouts reported. 3 LAVH converted to AH Follow‐up: 6 to 8 weeks after surgery. No loss to follow‐up reported Power calculation to estimate sample size: yes, 35 women required for each surgery arm (assuming that the incidence of complications in women who had LH(a) was 10% and there was an increase of complication rate to 40%), with an alpha (type I error) of 0.05 and a beta (type II error) of 0.2 |
|
| Participants | 80 women with a mean age of 50 years for the LH(a) group and 49 years for the VH group Inclusion criteria: women scheduled for abdominal hysterectomy for benign disease with traditional contraindications for VH, including uterine size larger than 280 g and one or more of the following: previous pelvic surgery, history of pelvic inflammatory disease (PID), moderate or severe endometriosis, concomitant adnexal masses, indication for adnexectomy and nulliparity without uterine descent Exclusion criteria: anaesthetic contraindications for laparoscopic surgery; suspicious adnexal mass on ultrasound; ovarian blood flow and tumour markers; vaginal narrowed to less than 2 fingers wide; immobile uterus with no descent and no lateral mobilisation |
|
| Interventions |
VH versus LH (LH(a))
LH(a) arm (considered LH type IV): included coagulation and sectioning of the round ligament, utero‐ovarian ligaments with fallopian tubes when ovaries were conserved, and the infundibulopelvic ligaments when ovaries were removed; opening of the bladder flap and bladder dissection, uterosacral ligaments, base of cardinal ligaments and uterine vessels. Vaginal phases included circular incision of the vagina and, when necessary, wedge morcellation, coring or bivalving. Peritoneal closure and closure of the vaginal vault concluded the vaginal phase, at which time the pelvis and abdomen were re‐evaluated through the laparoscope to be sure of haemostasis and for pelvic lavage
VH arm: according to modified Heaney technique Antibiotics: both groups received prophylactic antibiotic treatment (cefazolin 2 g IV) at the beginning and anticoagulant therapy with low molecular weight heparin the evening before the operation Surgeons: surgeons experienced in laparoscopic and vaginal surgery completed all the operations |
|
| Outcomes | Intra‐operative and postoperative complications; febrile morbidity; analgesia requirement; postoperative hospital stay; conversion to laparotomy; uterine size and weight | |
| Notes | France 2 hospitals in Paris Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pre‐determined computer‐generated randomisation code |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts, 3 procedures converted. No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available. Primary outcome not clearly defined in paper |
| Other bias | Low risk | No other bias identified |
Ellstrom 1998.
| Methods | Single‐centre study, parallel‐group design Duration: not reported Randomisation: method not stated Allocation concealment not reported Blinding: no Number of women randomised = 40. No dropouts reported Follow‐up: assessment of pain, nausea and vomiting, 8 pm day of surgery, 10 am and 6 pm first day and 10 am second postoperative day. Pulmonary function assessed pre‐operatively and 10 am, first and second day. Time of anaesthesia, surgery, per and postoperative complications and difference in erythrocyte volume fraction (EVF) before and 2 days after surgery. No loss to follow‐up Power calculation for sample size: not reported |
|
| Participants | 40 women with a mean age of 46 years (LH(a) group) and 48 years (AH group) Inclusion criteria: scheduled for abdominal hysterectomy for benign disorders; maximum width of uterus, measured by transvaginal ultrasound, less than 11 cm. American Society of Anaesthesiologists (ASA) Grade 1 Exclusion criteria: not reported | |
| Interventions | AH versus LH (LH(a)). Both groups stratified to total and subtotal hysterectomies LH(a) arm: total hysterectomy (n = 14) and laparoscopic subtotal hysterectomy (n = 6). The laparoscopic part of the total hysterectomy was finished when the uterine artery and parts of the sacrouterine ligaments were transected. The operation was then continued vaginally Second‐generation cephalosporin and metronidazole were given intravenously during the operation and by oral administration for 2 days after surgery. With the subtotal hysterectomy, morcellation was carried out after transection of the uterine arteries using a mechanical or an electrical morcellator. The cervical canal was desiccated with bipolar cautery AH arm: total hysterectomy (n = 14) and subtotal hysterectomy (n = 6). With the abdominal hysterectomies, standard surgical techniques were used. A lower midline or Pfannenstiel incision was made. The type of incision was left to the individual surgeon and patient to decide Anaesthesia: both groups received standardised anaesthesia; flunitrazepam (1 mg) was given as pre‐medication approximately 2 hours before surgery. Anaesthesia was induced with propofol (1.5 to 2.5 mg per kg body weight). Morphine (100 uG per kg body weight) was given for perioperative analgesia. Neuromuscular block was achieved with vecuronium (0.1 mg per kg body weight). Suxamethonium (1.0 mg per kg body weight) was administrated for optimal intubation. Anaesthesia was maintained with isoflurane in oxygen/air. Morphine was postoperatively self administered by the patients by programmable infusion pump containing morphine 1.0 mg/ml. Additional analgesic medication was restricted to paracetamol. Patients with nausea were given 10 mg metoclopramide Surgeon experience: not reported | |
| Outcomes | Primary: postoperative pain, pulmonary function Secondary: time of anaesthesia, time of surgery, per and postoperative complications, difference in erythrocyte volume fraction (EVF) | |
| Notes | Sweden University Hospital of Sahlgrenska Funding: Goteborg Medical Society Fund, Swedish Medical Research Council |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Primary outcome clearly defined |
| Other bias | High risk | Analysis according to intention‐to‐treat unclear; no exclusion criteria reported. No sample size calculation performed. Surgeon's experience not reported |
Falcone 1999.
| Methods | Single‐centre study, parallel‐group design Duration: September 1995 to February 1997 (1 year, 6 months) Randomisation: assigned according to a computer‐generated randomisation schedule with random block sizes Allocation concealment: All patients were told of their assignment before surgery Blinding: no Number of women randomised = 48, number analysed = 44 Dropout: 4 withdrew before surgery (3 AH group and 1 LH group) Follow‐up: daily diary for 6 weeks, recording symptoms, lifestyle impact, life events, medication. In each arm, 1 patient refused to keep a diary Power calculation for sample size: yes, 22 patients per group were necessary to detect a difference of 30 minutes or more in surgical time between the 2 groups with 90% power and a significance level of 0.05 Analysis by intention‐to‐treat: yes |
|
| Participants | 44 women with a mean age of 42.8 years (LH group) and 43.8 years (AH group) Inclusion criteria: scheduled for abdominal hysterectomy for benign disease Exclusion criteria: pelvic mass size greater than 2 cm below the umbilicus; concomitant incontinence or pelvic reconstructive procedures required | |
| Interventions |
AH versus LH
LH arm: 3 10 mm trocar sites ‐ 1 umbilical and 1 in each lower quadrant lateral to inferior epigastric artery 6 cm to 8 cm above pubic rami. Uterine arteries occluded laparoscopically with electrocautery. Cardinal ligaments cut laparoscopically. If the uterus had minimal descent, uterosacral ligaments were also cut laparoscopically. Vagina incised either laparoscopically or vaginally, depending on the ease that this could be achieved. Either anterior or posterior fornix, depending on access. Surgery then completed vaginally. Vaginal cuff closed vaginally Surgeons: performed by senior author with assistance from pelvic surgery fellow or resident Postoperative pain relief was given to patients intravenously AH arm: procedure not reported |
|
| Outcomes | Operative time; blood loss; length of hospital stay; uterine weight; intra‐operative complications; postoperative pain; return to work/normal activities and hospital costs per patient | |
| Notes | USA Cleveland Clinic Foundation, Ohio Funding by Ethicon Endosurgery and the Minimally Invasive Center of the Cleveland Clinic Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule with random block sizes |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 patients withdrew before surgery and data were included where possible. In each arm 1 patient was lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | No reporting bias identified |
| Other bias | Unclear risk | Funding from pharmaceutical or surgical instrumentation company. Surgeon's experience unclear |
Ferrari 2000.
| Methods | Single‐centre study, parallel‐group design Duration: 24 months Randomisation: computer‐generated randomisation numbers Allocation concealment: sealed opaque envelopes Blinding: no Number of women randomised = 62. No dropouts reported. With 3 women in the LAVH group, the procedure was converted to a AH. In all cases the decision was made during the laparoscopic part of the procedure Follow‐up: women were followed up until discharge from hospital. Postoperatively, temperature and analgesic requirement were recorded daily. No loss to follow‐up Power calculation for sample size: no |
|
| Participants | 62 women aged from 43 to 50 years Inclusion criteria: symptomatic uterine fibroids Exclusion criteria: history of severe pelvic disease; lack of uterine accessibility and mobility or a sonographically estimated uterine volume > 1500 ml (abdominal hysterectomy). Women without a history of severe pelvic disease, with an accessible and mobile uterus and a sonographically estimated uterine volume < 500 ml, underwent a vaginal hysterectomy | |
| Interventions | AH versus LH (LAVH) LAVH arm: visualisation of the pelvis and upper abdomen, the treatment of adhesions or endometriosis when present, and the completion of the upper part of the hysterectomy. Round ligaments, tubes and utero‐ovarian ligaments were desiccated and transected when the adnexa were to be preserved, while the round and infundibulopelvic ligaments were desiccated and transected when the adnexa were to be removed. The broad ligaments were dissected to their lower margin. When the bladder was stretched over the anterior aspect of the uterus due to previous surgery, the bladder flap was developed laparoscopically. The vaginal part of the hysterectomy included colpoceliotomy an bilateral ligation and transection of utero‐sacral ligaments, uterine vessels and cardinal ligaments; cervical amputation, corporal hemisection, myomectomy and uterine morcellation were performed when necessary AH arm: performed according to a standard technique Surgeon experience: not reported | |
| Outcomes | Operating time; blood loss; complications; febrile morbidity; analgesic administration and hospital stay | |
| Notes | Italy San Paolo Biomedical Sciences Institute, University of Milan Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation numbers |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not predefined |
| Other bias | Unclear risk | Surgeon's experience unclear. Power calculation for sample size not performed |
Garry 2004.
| Methods | Multicentre study (n = 30), parallel‐group design Duration: November 1996 to September 2000 (4 years) Randomisation: 2:1 imbalance randomisation method. Allocation to abdominal or vaginal trial by surgeon. Randomisation to conventional or laparoscopic approach was performed with a computer‐generated program and allocation was advised by telephone call to the central North Yorkshire Clinical Trials unit. Allocation concealment: Blinding: no Number of women randomised: 1380 ‐ Abdominal trial: 876 (AH: 292, aLH: 584) ‐ Vaginal trial: 504 (VH: 168, vLH: 336) ‐ Number of patients that withdrew/dropped out pre‐operatively: AH:6, aLH: 11,VH: 5, vLH: 12 Follow‐up: 6 weeks, 4 months and 1 year. In the abdominal trial: AH arm ‐ 6 weeks n = 17, 4 months n = 104, 1 year n = 104; LH arm ‐ 6 weeks n = 29, 4 months n = 166, 1 year n = 166. In the vaginal trial: VH arm ‐ 6 weeks n = 10, 4 months n = 55, 1 year n = 55; LH arm ‐ 6 weeks n = 27, 4 months n = 110, 1 year n = 118 Power calculation to estimate sample size: yes. The sample size for the abdominal trial was calculated on the basis of 9% of AH having major complications. In order to detect a reduction in complication rate of 50%, a sample size of 450 in each arm was required using 80% power and a 2‐sided type 1 error rate of 5% Results were confirmed using a per‐protocol analysis |
|
| Participants | 1380 women with a mean age of 41 years Inclusion criteria: women who needed hysterectomy for non‐malignant conditions Exclusion criteria: confirmed or suspected malignant disease of any part of the genital tract; 2nd or 3rd degree uterine prolapse; a uterine mass greater than the size of a 12‐week pregnancy; any associated medical illness precluding laparoscopic surgery; a requirement for bladder or other pelvic support surgery and patient refusal of consent for the trial | |
| Interventions | 4 arms: VH, LH in the vaginal trial (vLH); AH and LH in the abdominal trial(aLH) Surgical procedures were not reported Surgeons recruited had to have performed at least 25 of each type of procedure, however cases could be used for teaching if the main assistant was the designated surgeon. Surgeons of all grades and experience participated | |
| Outcomes |
Primary outcomes: major complications (major haemorrhage, bowel injury, ureteric injury, bladder injury, pulmonary embolus, anaesthesia problems, unintended laparotomy, wound dehiscence, haematoma) Secondary outcomes: minor complications (major haemorrhage, anaesthesia problems, pyrexia, infection, haematoma, DVT); blood loss; pain; analgesia requirement; sexual activity; body image; health status; length of surgery; length of hospital stay |
|
| Notes | UK (28 centres) and South Africa (2 centres) Funding: National Health Service Research and Development Health Technology Assessment Programme, UK |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised with use of a computer‐generated program |
| Allocation concealment (selection bias) | Low risk | Telephone inquiry |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 17 patients in each trial dropped out before surgery and sensitivity analysis was performed. Particularly in the AH arm and LH arms loss to follow‐up was high (> 15%) Quality of life outcome at baseline reported in 76% of women |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes well defined |
| Other bias | Unclear risk | Surgical procedures not reported. Surgeons of all grades and experience participated |
Ghezzi 2010.
| Methods | Single‐centre Duration: February 2009 to September 2009 (7 months) Randomisation: computer‐generated list Allocation concealment: treatment allocation was concealed until the day of surgery Blinding: no Number of women: 123 women eligible, of which 82 randomised: 41 randomised to LH and 41 randomised to VH. No dropout Follow‐up: no loss to follow‐up Power calculation to estimate sample size: yes, based on mean VAS pain score after VH reported by Candiani et al (2011). With an alpha error of 5% and a power of 95%, at least 40 patients in each group needed to detect a 50% decrease in the mean postoperative pain on day 0 in patients with LH Intention‐to‐treat analysis: not reported |
|
| Participants | 82 women with a mean age of 48 years in both groups Inclusion criteria: indication for hysterectomy for a supposed benign gynaecological condition Exclusion criteria: uterine volume > 14 weeks of gestation, suspicion of malignancy, concomitant presence of large adnexal masses (diameter > 4 cm) and pelvic organ prolapse > stage 1 according to POP‐Q classification. Chronic pelvic pain and endometriosis or PID were excluded |
|
| Interventions |
TLH versus VH TLH: intrauterine manipulator inserted. 5 mm scope umbilical site. 3 5 mm ancillary trocars inserted, 1 suprapubically and 2 laterally. Coagulation and dissection of round ligaments and infundibulopelvic ligaments. Broad ligament opened to uterovesical fold, caudal reflection of bladder. Uterine arteries, cardinal ligaments and uterosacral ligaments coagulated and transected. Colpotomy with monopolar hook. Uterus extracted vaginally. Vaginal cuff closure with single layer sutures VH: performed according to a standardised technique Surgeons: surgical team and their experience were not reported Antibiotic and antithrombotic prophylaxis administered postoperatively |
|
| Outcomes |
Primary outcome: postoperative pain (VAS at 1, 3, 8 and 24 hours after procedure) Secondary outcome: operative time |
|
| Notes | Varese, Italy Del Ponte Hospital, University of Insubria Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation with use of a computer‐generated list |
| Allocation concealment (selection bias) | Unclear risk | Concealed until day of surgery. Method of concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout and loss to follow‐up reported. Low numbers |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not clearly defined in methods of study |
| Other bias | Low risk | Surgical experience reported |
Ghezzi 2011.
| Methods | Single‐centre Duration: October 2009 to May 2010 (7 months) Randomisation: block randomisation, computer‐generated list, with block size of 28 Allocation concealment: the surgeon was notified of the allocation on the day of the procedure Blinding: patients and research assistants were blinded to group randomisation Number of women: 112 patients eligible of which 76 randomised. 38 allocated to each group. Randomised = 76; analysed = 76. No dropouts Follow‐up: no loss to follow‐up Power calculation for sample size: yes, a reduction in pain intensity of 2 points on the VAS would be regarded as clinically significant. With alpha = 0.05 and beta = 0.20, a sample size of 38 women per group would be required to detect a reduction in the mean pain score at 1 hour after surgery from 4.7 to 2.7 Intention‐to‐treat analysis: not reported |
|
| Participants | 76 patients with a mean age of 46 and 47 years for each group Inclusion criteria: women with benign gynaecological conditions requiring hysterectomy Exclusion criteria: pelvic organ prolapse > grade I. Severe cardiopulmonary disease if anaesthesiology team decided that laparoscopy was contraindicated |
|
| Interventions |
LH versus mini‐LH Same surgical technique was used for both LH and mini‐LH. LH was a standardised technique. Only difference is that in mini‐ LH all ports were 3 mm or smaller Surgeons: same surgical team skilled in advanced laparoscopy Patients underwent a standardised anaesthesia protocol |
|
| Outcomes |
Primary outcome: postoperative pain (VAS 1, 3, 8 and 24 hours postoperative) Secondary outcomes: operative parameters, volume in inflated CO2 |
|
| Notes | Varese, Italy Del Ponte Hospital, University of Insubria Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation: block‐randomisation, computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Allocation concealment described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Patients and research assistants were blinded to group randomisation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout and loss to follow‐up reported, low numbers |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes defined |
| Other bias | Low risk | No other bias identified |
Harkki‐Siren 2000.
| Methods | Single‐centre study, parallel‐group design with no blinding Duration: March to September 1997 (6 months) Randomisation: patients were randomly allocated Allocation concealment: sequentially numbered, opaque and sealed envelopes Blinding: no Number of women randomised = 50. No dropouts reported. Tissue trauma analysis for 18 uncomplicated hysterectomies in both groups were included Follow‐up: first follow‐up visit was scheduled 4 weeks after the operation and then followed up until complete recovery. No loss to follow‐up Power calculation for sample size: yes, 21 women in each group would be needed for 90% study power and for differentiation of 10 mg/L (standard deviation) between the means of C‐reactive protein (CRP) concentration when type I error is 5%. For 80% study power, 15 women in each group needed |
|
| Participants | 50 women with a mean age of 47 years (LH(a) group) and 48 years (AH group) Inclusion criteria: scheduled for AH for benign reasons Exclusion criteria: major medical diseases; BMI above 32 kg/m2; size of uterus larger than of 14 weeks of pregnancy or uterine width greater than 10 cm by transvaginal ultrasonography; severe adhesions or endometriosis; prolapse and any other contraindications for laparoscopy | |
| Interventions | AH versus LH (LH(a)) LH(a) arm: a 5 mm trocar was inserted suprapubically. Pelvis was inspected and ureters located. The uterosacral ligaments were coagulated with bipolar electrocoagulation and cut with unipolar scissors, as were the infundibulopelvic vessels and ligaments (if adnexa were to be removed) or the round ligaments, fallopian tubes and utero‐ovarian ligaments (adnexa not removed). The vesical peritoneum was opened with scissors and the bladder pulled down. Uterine vessels were prepared free and divided. The anterior fornix of the vagina was opened laparoscopically with monopolar scissors, the uterus was removed vaginally and the vagina was closed with resorbable suture AH arm: operated on in a standard manner through a lower midline or Pfannenstiel incision. Diathermy was used only for haemostasis and peritoneal closure was performed All women received 500 mg metronidazole intravenously at the beginning of anaesthesia and operations were performed under GA with endotracheal intubation in both groups. The bladder was drained with a Foley catheter in all women. A drain was left from the perineal cavity in both groups Surgeon experience: not reported | |
| Outcomes | Operating time; anaesthetic time; blood loss; haemoglobin change; hospital stay; sick leave and complications | |
| Notes | Finland Jorvi Hospital, Espoo Funding: The Clinical Research Institution of Helsinki University Central Hospital and Jorvi Hospital, The Finnish Medical Foundation and The Research Foundation of Orion Corporation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were randomly allocated. Method not clearly described |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered and sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Unclear risk | Tissue trauma reported in uncomplicated surgeries only Funding from pharmaceutical or surgical instrumentation company |
Hwang 2002.
| Methods | Single‐centre study, parallel‐group design Duration: June 1999 to May 2001 (2 years) Randomisation: sealed envelopes containing computer‐generated block randomisation numbers, block size of 10 Blinding: no Number of women randomised = 90. No dropouts reported Follow‐up: 6 weeks after surgery Power calculation to estimate sample size: yes. Power of analysis was 80% at alpha = 0.05. Result of power calculation not reported |
|
| Participants | 90 women with a mean age of 45.1 years Inclusion criteria: scheduled for hysterectomy for uterine fibroids; myoma diameter larger than 8 cm and second myoma less than 5 cm or 2 myomata, both at least 6 cm in diameter but less than 8 cm (maximum number of fibroids was 3) Exclusion criteria: indications of adenomyosis; uterine prolapse; chronic pelvic pain; dysfunctional uterine bleeding; cervical dysplasia; pelvic inflammatory disease | |
| Interventions |
AH versus VH versus LH (LH(a))
AH arm: abdomen opened by vertical midline or Pfannenstiel skin incision. Uterus removed by extrafascial technique and vaginal cuff closed with continuous interrupted suture followed by re‐peritonealisation
VH arm: patients in Trendelenburg tilt position and given vasopressin injection. Anterior circumferential incision of the cervix and posterior V‐shape incision. Anterior peritoneal cavity opened and cul‐de‐sac of Douglas entered. After uterine artery ligation, volume reducing techniques were performed vaginally. Peritoneum closed and uterosacral ligaments and vaginal vault sutured.
LH(a) arm: 10 mm trocar inserted into umbilical position, one 5 mm trocar in each lower quadrant and another inserted suprapubically. Uterosacral ligament incision and round and broad ligaments were excised. Anterior colpotomy was performed after ligation of the bilateral uterine artery. The rest of the hysterectomy was completed vaginally. The uterus was removed vaginally by volume reducing techniques and the vaginal cuff was closed All operations performed under general anaesthesia by second author, with the assistance of the other authors. Standardised postoperative protocol of 2 doses of IV meperidine 50 mg every 4 hours for pain control followed by acetaminophen 325 mg every 6 hours Prophylactic antibiotics (cephalosporin 1.0 g every 8 hours (3 doses/day) combined with aminoglycoside 80 mg every 12 hours (2 doses/day), were administered to all for 1 day after surgery Surgeons' experience: 1 surgeon performed all procedures and had much experience |
|
| Outcomes | Operating time; hospital stay; intra‐operative blood loss; complications; postoperative tenderness score; return to work; antibiotics used | |
| Notes | Taiwan Shin Kong Wu Ho‐Su Memorial Medical Centre, Taipei Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation numbers |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts. No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Uterine weight in AH group was significantly higher than in VH and LAVH group |
Jung 2011.
| Methods | Single‐centre Duration: October 2009 to March 2010 (5 months) Randomisation: based on computer‐generated random sampling numbers Allocation concealment: not described Blinding: no Number of women randomised = 68. 34 in TLH arm analysed. 30 in SP‐LH arm analysed: 4 converted procedures excluded from analysis Follow‐up: no loss to follow‐up Power calculation for sample size: yes, a difference of 0.8 in the VAS score was considered clinically relevant. The number of cases needed per group was 34 Intention‐to‐treat analysis not applied |
|
| Participants | Mean age was 48 years Inclusion criteria: age >/ = 20 years, no evidence of gynaecologic malignancy, normal cervical cytology or histology, appropriate medical status for laparoscopic surgery (ASA 1 or 2), adequate uterus size for vaginal removal (</ = 12 weeks) Exclusion criteria: uterine size larger than 12 weeks, history of pelvic radiation therapy, suspicion of gynaecologic cancer, more than 3 prior laparotomies, treated for gastrointestinal or gynaecologic malignancy |
|
| Interventions |
SP‐TLH versus 4‐port/conventional TLH Conventional TLH: 4 5 mm trocars were placed. A 5 mm port for the laparoscope inserted through the umbilicus. 2 5 mm ports were placed in the left lower quadrant of the abdomen and one in the right lower quadrant SP‐TLH: a 1.2 cm vertical intra‐umbilical skin incision was made and a 1.5 cm rectus fasciotomy was performed for entrance to the peritoneal cavity. A single 3‐channel port was used. After introduction in both arms the procedure was performed similarly. Utero‐ovarian ligaments and round ligaments and broad ligaments were sequentially ligated and dissected. The vesico‐uterine peritoneal fold was opened and the bladder mobilised. The uterine vessels were sealed and dissected. The uterus was removed vaginally; some had to be morcellated. The vaginal vault was sutured laparoscopically or transvaginally, depending on the surgeon's decision Surgeons' experience: all procedures performed by 3 skilled surgeons. Surgical experience: at least 100 LH and 30 SP‐LH |
|
| Outcomes |
Primary: postoperative pain (VAS) and need of analgesics Secondary: operative time, intra and postoperative complications, postoperative hospital stay, haemoglobin |
|
| Notes | Korea Gangnam Medical Center, Seoul Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation: based on computer‐generated random sampling numbers |
| Allocation concealment (selection bias) | High risk | Allocation concealment not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up, 4 converted procedures in SP arm excluded from analysis |
| Selective reporting (reporting bias) | Unclear risk | Converted procedures not analysed; primary and secondary outcomes predefined |
| Other bias | Low risk | No other bias identified |
Kluivers 2007.
| Methods | Single‐centre study, parallel‐group design Duration: August 2002 to January 2005 (2 years, 6 months) Randomisation: randomly allocated Allocation concealment: sealed, opaque envelopes Blinding: no Number of women eligible = 88, and randomised = 59 Dropouts: in the LH group, 1 woman refused the allocated procedure and an AH was performed. There were 2 intra‐operative conversions to AH. There were 2 patients with re interventions (laparotomy) in the AH group Follow‐up: women were followed up until 3 months after surgery. At 12 weeks the follow‐up was complete in 81% of the LH group and 94% of the AH group Power calculation for sample size: yes, 28 patients per group were necessary to detect a difference between the 2 groups of 15 units or more on each of the 8 RAND‐36 subscales with standard deviation 20 units and 80% power with a significance level of 0.05 Analysis was by intention‐to‐treat |
|
| Participants | 59 women with a mean age of 46 years in both groups Inclusion criteria: women with benign disease in whom VH was not possible and LH was feasible Exclusion criteria: suspicion of malignancy, a previous lower midline incision, the need for simultaneous procedures like prolapse repair, inability to speak Dutch | |
| Interventions |
TAH versus TLH
AH: was performed according to the extrafascial technique (clamps and suture ligation) LH: intentional TLH procedures, using the Storz uterine manipulator type Clemont Ferrand, and a 4‐port technique with bipolar coagulation and scissors. Opening the bladder flap and colpotomy (with the use of monopolar coagulation) were performed laparoscopically, as well as laparoscopic extracorporeal suturing of the vagina Antibiotic treatment: both groups received prophylactic antibiotic treatment (amoxicillin clavulanate 2.2 g IV) and anticoagulant therapy Anaesthesia: general anaesthesia for both AH and LH Surgeons: 10 different surgeons carried out AH, of whom 3 surgeons also carried out LH; (supervising) surgeons had performed at least 100 procedures |
|
| Outcomes | Primary: quality of life (questionnaire RAND‐36) Secondary: operative time; blood loss; operative complications (injury to adjacent organs, haemorrhage, anaesthesia problems); conversions to AH, LAVH, LH(a) or subtotal hysterectomy; haemoglobin decrease; postoperative complications; hospital stay; use of opioids and antiemetics | |
| Notes | The Netherlands Maxima Medical Centre, Veldhoven No funding |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly allocated |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes shuffled and sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1 refused assigned procedure and was analysed in assigned treatment group. Loss to follow‐up was almost 20% in LH group; in AH group 6% |
| Selective reporting (reporting bias) | Low risk | Primary outcomes predefined and accordingly reported |
| Other bias | Unclear risk | Different group of surgeons for different procedures. More residents as first surgeon in AH |
Kongwattanakul 2012.
| Methods | Single‐centre. Stratified, open, randomised, controlled, parallel‐group trial Duration: April 2010 to March 2011 (1 year) Randomisation: computer‐generated list. Stratified random sampling. Group 1: uterus </ = 12 weeks of gestation (n = 32); Group 2: uterus > 12 to 16 weeks of gestation (n = 11); Group 3: history of abdominal surgery (n = 7) Allocation concealment: sealed, opaque, numbered envelopes Blinding: researcher blinded; patients not blinded Number of women: after randomisation: LAVH 25 (group 1 = 16; group 2 = 6; group 3 = 3); AH 25 (group 1 = 16; group 2 = 5; group 3 = 4) Follow‐up: until discharge from the hospital. No loss to follow‐up Power calculation for sample size: yes, it was calculated from the population mean from a sample size determination as per WHO Health Studies. A power calculation verified that no more that 24 patients were needed in each group Analysis by intention‐to‐treat: not reported |
|
| Participants | 50 women Inclusion criteria: indication for hysterectomy because of benign disease. Uterus </ = 16 weeks Exclusion criteria: cardiopulmonary disease, cardiac arrhythmias, history of ischaemic heart disease, other medical risks |
|
| Interventions |
LAVH versus AH Surgical techniques not reported Surgeons: 2 surgeons who performed both procedures at least 30 times Preoperatively antibiotic prophylaxis cefotaxime 1 g |
|
| Outcomes | Intraoperative blood loss, duration of operation, intraoperative and early postoperative complications, conversion rate, pain, duration of hospital stay | |
| Notes | Thailand Srinagarind Hospital, Khon Kaen Funding: grant support by the Faculty of Medicine of Khon Kaen University |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by means of a computer‐generated list of random numbers |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque, numbered envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of researcher; patients not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up reported, conversion rate reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Unclear risk | Not reported if 3 groups are comparable on basic characteristics; power calculation unclear |
Kunz 1996.
| Methods | Single‐centre study, parallel‐group design Duration: November 1993 to February 1995 (1 year, 4 months) Randomisation: method not reported Allocation concealment: not reported Blinding: no Number of women randomised = 70, number analysed = 70. No dropouts Follow‐up: until discharge from the hospital. No loss to follow‐up No power calculation for sample size was reported |
|
| Participants | 70 women with a mean age of 43 (LAVH group) and 48 years (AH group) Inclusion criteria: scheduled for hysterectomy for non‐malignant diseases Exclusion criteria: not reported | |
| Interventions |
AH versus LH (LAVH)
LAVH arm: a curette was inserted into the uterus and the laparoscopic video camera was introduced. 2 5 mm trocars were inserted. Division of the adnexopexy from the uterus or the infundibulopelvic ligaments and round ligaments was accomplished with tissue tension, bipolar coagulation and the use of hook scissors. Transverse incision on the anterior fold of the broad ligaments bilaterally and transection of the visceral peritoneum at the bladder resection. Separation of the posterior fold of the broad ligaments, uterine arteries are skeletonised and demonstrated close to the uterus (2 cm). The hysterectomy was continued vaginally. The cervix was circumcised and the vaginal skin is reflected. Reflection of the bladder and the anterior peritoneum is demonstrated. The pouch of Douglas is entered and the sacrouterine ligaments are clamped and ligated. Uterine arteries are clamped and ligated bilaterally and the uterus extracted vaginally. The sacrouterine ligaments are fixed together and the vagina is closed in interrupted sutures AH arm: the abdominal hysterectomies followed a common technique (Ober and Meinrenken 1964) Antibiotics: both groups received peri‐operative antibiotic prophylaxis with 2 g of cephalosporin (Ceftriaxon), 15 minutes prior to the operation Both groups had a pre and postoperative vaginal ultrasound scan. Pre and postoperative blood tests and measured CRP postoperatively (day 1 and 3) Postoperative analgesia was piritramid (22 mg ampoule), pentazocin (30 mg ampoule) and tramadol hydrochloride (100 mg orally) |
|
| Outcomes | Operating time, pain relief, size of uterus, haemoglobin change, stay in hospital and complications | |
| Notes | Germany Hospital in Stuttgart Funding not reported Paper in German language. Translation was commissioned |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | High risk | No exclusion criteria; no power calculation for sample size. Surgeons' experience unclear |
Langebrekke 1996.
| Methods | Multicentre study (n = 2), parallel‐group design Duration: not reported Randomisation: a table of random digits, numbered 1 to 100 Allocation concealment: sealed envelopes Blinding: no Number of women randomised = 100, number analysed = 100. No dropouts or conversions Follow‐up: until women returned to work/normal activities. No loss to follow‐up No power calculation for sample size was reported |
|
| Participants | 100 women. The age of the women was not reported Inclusion criteria: women with indications for elective hysterectomy Exclusion criteria: proven or suspected malignancies in the pelvic area, suspected intra‐abdominal adhesions; uterus enlarged beyond the size of a 12‐week size pregnancy; serious cardiopulmonary disease; previous colporrhapy | |
| Interventions |
AH versus LH (LH(a))
LH(a) arm: a 10 mm laparoscope was inserted through the umbilicus and a general inspection of the entire pelvic cavity was performed. 2 5 mm trocars were introduced into the iliac fossae. A 12 mm trocar was placed in the midline 4 cm below the umbilicus in cases where the automatic stapler endo‐GIA was used. Bipolar diathermy or GIA were used to divide the ligaments. With unipolar scissors, the vesicouterine perineal fold was cut and the bladder mobilised. The uterine arteries were coagulated with bipolar diathermy. The vagina was opened laparoscopically with unipolar scissors and the uterus removed vaginally. The vagina was closed with resorbable sutures from below, the sutures including the cardinal ligaments. All operations performed exclusively by 2 of the authors AH arm: according to standard techniques. Abdomen was entered via a Pfannenstiel incision. The entire abdominal cavity was palpated and the pelvis inspected. The uterine ligaments were clamped and ligated. The bladder peritoneum was opened and the bladder was mobilised away from the cervix and upper anterior vaginal wall. Uterine vessels were clamped, cut and ligated. The vagina was closed with resorbable sutures. Performed by any skilled gynaecologist in the department Antibiotics: cephalosporin (2 g IV) and low molecular heparin (injected subcutaneously) was given to both groups postoperatively Surgeons: different group of surgeons for different procedures |
|
| Outcomes | Operation time; hospital stay; time elapsed before resuming work; postoperative pain; complications and blood loss | |
| Notes | Norway (2 centres) Aker University Hospital, Oslo, and Akershus central Hospital, Oslo Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random digits |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | Unclear risk | Different group of surgeons for different procedures |
Long 2002.
| Methods |
Duration: November 1999 to December 2000 (1 year, 1 month) Randomisation: randomly assigned to treatment groups. Method not stated Allocation concealment not reported Single‐centre study, parallel‐group design with no blinding Number of women randomised = 167. Number of dropouts = 13. Number of women analysed = 101 (women excluded if hysterectomy performed for reasons other than uterine fibroids of adenomyosis) Follow‐up: until discharged from hospital. No loss to follow‐up reported Power calculation for sample size: no Intention‐to‐treat analysis: no |
|
| Participants | 101 women with a mean age of 45.9 (LAVH group) and 45.5 (TLH group) Inclusion criteria: indications of uterine fibroids of adenomyosis and contraindications for VH ‐ uterine weight > 280 g, previous pelvic surgery, history of PID, need for adnexectomy, lack of uterine descent and limited vaginal access Criteria for choosing laparoscopic hysterectomy was based on the uterine volume, less than that of a 16‐week pregnancy (700 g) Exclusion criteria: suitable for a vaginal hysterectomy and the uterine volume was greater than a 16‐week pregnancy | |
| Interventions |
LAVH versus TLH (a comparison of 2 LH techniques)
LAVH arm: if the ovaries were to be conserved, the fallopian tubes, round and utero‐ovarian ligament was resected with bipolar forceps and scissors. For adnexectomy, mesosalpinx, round and infundibulopelvic ligament were resected. Laparoscopic dissection of the bladder flap, resection of the broad ligaments, anterior and posterior colpotomies were performed. Proceeded vaginally ‐ clamping, transecting and suture ligating of uterine vessels, cardinal and uterosacral ligaments. Closure of peritoneum and vaginal vault anchored to the cardinal‐uterosacral ligament complex after removing uterus TLH arm: same manner as the LAVH procedure above the uterine artery level. After dissection of the bladder flap and resection of the broad ligament, the uterine artery was coagulated by bipolar electrocoagulator and separated from the uterine sidewall by scissors. Bilateral desiccation and transection of the cardinal‐uterosacral ligament complex. Circular colpotomy was performed close to the cervix and uterus was removed through the vagina All operations performed under GA Surgeons: by the same gynaecologist for each procedure (LAVH by one surgeon and TLH by another) Postoperative analgesia included lysine aspirin which was administered intravenously Antibiotic prophylaxis IV cefazolin 1 g administered pre and postoperatively |
|
| Outcomes | Operation time, blood loss, hospital stay, cost, complications and sexual symptoms | |
| Notes | Taiwan Kaohsiung Municipal Hsiao Kang Hospital Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13 dropouts (excluded from analysis after randomisation because of conversions to AH (n = 3), incomplete records (n = 7) or combined surgical procedures (n = 3)). No further loss to follow‐up reported |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | High risk | Analysis not according to intention‐to‐treat. Different surgeons for different procedures Women were randomised to treatment groups before a large number (i.e. 66) of the women were excluded. Therefore, the women in each treatment group may not have been a true representation of the original randomised groups |
Lumsden 2000.
| Methods | Multicentre (n = 3) study, parallel‐group design Duration: 2 years Randomisation: performed by the research nurse using a computer‐generated schedule Allocation concealment: by third party (research nurse) Number of women randomised = 200, number analysed = 190. Dropouts: 7 did not attend for operation and the case records were not available for a further 3 women Follow‐up: women asked to keep a diary of recovery 'milestones' and reviewed by the research nurse 4 weeks after surgery. EuroQol Health Questionnaire completed at 1, 6 and 12 months after surgery. The response rate for the patient questionnaire was 87% and that for EuroQol was 78%, 64% and 47% at 1, 6 and 12 months, respectively Power calculation for sample size: yes; 120 patients per arm allowed an 80% chance of detecting a 15% difference in complication rates at a 5% level using a 2‐sided test Analysis was stated as by intention‐to‐treat (8 women did not have LAVH as randomised but were analysed in the LAVH group) |
|
| Participants | 190 women with a mean age of 42.7 years (AH group) and 41.1 (LH group) Inclusion criteria: scheduled for AH for benign gynaecological disease and they were not suitable for VH because of a uterine size in excess of 14 weeks or a requirement for oophorectomy Exclusion criteria: suitable for VH | |
| Interventions |
AH versus LH. Operation procedures not reported Surgeons: performed by 5 consultant gynaecologists who have undertaken a minimum of 50 LH procedures |
|
| Outcomes | Length of operation; length of hospital stay; admission to ITU; readmissions; women requiring additional surgery; blood transfusions; complications (major and minor); patient‐reported outcomes; costs and change in health status | |
| Notes | Scotland 3 hospitals in Glasgow Funding: Scottish Home and Health Department, Scotland |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | By third party (research nurse) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10 dropouts were not analysed. 7 women did not attend surgery and 3 records were not available (< 10%) Loss to follow‐up: at 12 months only 47% of patients filled out the questionnaire |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Low risk | No other bias identified |
Marana 1999.
| Methods | Multicentre study (n = 4), parallel‐group design Duration: October 1995 to November 1996 (1 year, 1 month) Randomisation: computer‐generated sequence Allocation concealment: not reported Blinding: no Number of women randomised 116, number analysed 116. No dropouts Follow‐up: until patient left hospital. Postoperative follow‐up included evaluation of pain on postoperative days 1, 2 and 3, length of postoperative hospital stay and evaluation of postoperative complications. No loss to follow‐up Power calculation for sample size: yes. The sample size was selected to detect a difference of 25% in total complication rates with a power of 80% at the 5% level of significance, given a complication rate in the control group of 42% |
|
| Participants | 116 women with a mean age of 49 years Inclusion criteria: scheduled for AH for benign disease and had one or more of the following contraindications to VH: uterine size > 280 g and an upper limit of 16 weeks gestation (700 g); previous pelvic surgery; history of pelvic inflammatory disease; moderate or severe endometriosis; concomitant adnexal mass or indication for adnexectomy; and nulliparity with lack of uterine descent and limited vaginal access Exclusion criteria: suitable for VH | |
| Interventions |
AH versus LH (LAVH)
LAVH arm: 10 mm laparoscope introduced through the umbilicus, and 3 accessory 5 mm reusable trocars were introduced suprapubically. The pelvis and upper abdomen were then accurately evaluated, and endometriotic lesions, adhesions or ovarian cysts, when present, were treated appropriately. When the ovaries were to be conserved, bipolar forceps and scissors were used to resect the round and uteroovarian ligaments with the fallopian tubes
For adnexectomy, bipolar forceps and scissors were used to resect the round and infundibulopelvic ligaments, mesosalpinx, and mesovarium. Opening of the bladder flap was performed at the laparoscopic phase, whereas bladder dissection was performed during the vaginal phase. Laparoscopic haemostasis was achieved using exclusively bipolar electrocoagulation. The vaginal phase included circular incision of the vagina; bladder dissection to the laparoscopically opened bladder flap; entry in the posterior cul‐de‐sac; and clamping, transecting, and suture ligating of uterosacral ligaments, base of cardinal ligaments, and uterine vessels. Where necessary, wedge morcellation, coring or bivalving was performed. Peritoneal closure with pedicles exteriorised and closure of vaginal vault anchored to the uterosacral and cardinal ligaments concluded the vaginal phase AH arm: performed according to the technique described by Mattingly and Thompson Surgeon experience: not reported Antibiotic prophylaxis: all received intravenous piperacillin 2 g administered 30 minutes before surgery Postoperative medication consisted of the administration of ketorolac by intramuscular injection or by mouth every 6 hours for the first 24 hours |
|
| Outcomes | Blood loss; postoperative fever; postoperative pain; length of postoperative hospital stay; postoperative complications; haemoglobin reduction and intra‐operative conversion to abdominal surgery | |
| Notes | Italy 4 university hospitals Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Low risk | No other bias identified |
Miskry 2003.
| Methods | 2‐centre study, parallel‐group design Duration of trial not stated Randomisation: computer‐generated in blocks of 10 Allocation concealment: sequentially numbered, sealed, opaque envelopes, opened by nursing staff immediately prior to surgery Blinding: double‐blind until discharge from hospital, maintained by a sham opaque lower abdominal dressing (unless pyrexia or other complication necessitated direct inspection of the abdomen) and vaginal staining with methylene blue in cases undergoing VH Number of women randomised = 36, number analysed = 36. No dropouts Follow‐up: follow‐up at 6 weeks and 6 months with completion of SF‐6 Short Form general health survey. Loss to follow‐up not clearly described Power calculation for sample size: yes; 36 women required for 80% power to show a 2‐day difference in hospital stay at P = 0.05 |
|
| Participants | 36 women with a mean age of 42 years Inclusion criteria: scheduled for elective hysterectomy Exclusion criteria: genital tract malignancy; adnexal pathology; uterine size > 14 weeks; need for concurrent procedure (e.g. vaginal repair, colposuspension); reduced uterine mobility on VE; inadequate vaginal access | |
| Interventions |
AH versus VH
Total hysterectomy performed by standard technique for each route. Low transverse incision, closed with subcuticular absorbable suture, for AH; Heaney technique for VH. In all cases, concurrent oophorectomy performed if indicated; peritoneal and vaginal vault closed Surgeons: performed by most senior surgeon available All GA plus caudal block for one VH case Antibiotic prophylaxis co‐amoxiclav 1.2 g at induction of anaesthesia. Thromboprophylaxis heparin 5000 units at induction and twice daily until mobile |
|
| Outcomes | Primary outcome: duration of hospital stay Secondary outcomes: analgesic requirements; complications; return to normal function | |
| Notes | UK Royal Free and North Middlesex Hospitals Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by computer |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Sham abdominal dressing until discharge |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts; loss to follow‐up not clearly described |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes were adequately reported |
| Other bias | Low risk | No other bias identified |
Muzii 2007.
| Methods | Multicentre study, parallel‐group design Duration: January 2005 to December 2005 (1 year) Randomisation: computer‐generated allocation list; in operating room Allocation concealment: numbered, sealed opaque envelopes Blinding: no Number of women eligible: 86. Number of women randomised = 81. There were no dropouts. Conversions to AH: 2 in LAVH group and 4 in minilaparotomy group Follow‐up: women were followed up until discharge. No loss to follow‐up Power calculation was performed for sample size. Actual sample size was necessary to detect a difference in complications between the 2 groups of 30% (complication rate 42% in control group) with 80% power with a significance level of 0.05 Intention‐to‐treat analysis was possible from data but not performed by authors on all outcomes |
|
| Participants | 81 women with a mean age of 49 years in the LAVH group and 48 years in the minilaparotomy group Inclusion criteria: benign disease: myoma and/or abnormal uterine bleeding with and without adnexal masses. Contraindication for vaginal hysterectomy Exclusion criteria: uterine size greater than 700 g on ultrasound, previous midline incision, absolute contraindication to laparoscopy |
|
| Interventions |
LAVH versus minilaparotomy LAVH: 4‐port technique, laparoscopic dissection with bipolar forceps and scissors of either round and utero‐ovarian ligaments or infundibulo‐pelvic ligaments. Opening bladder flap, followed by vaginal hysterectomy. Uterosacral/cardinal ligament complex was anchored vaginally to vaginal vault. Laparoscopy at the end of the procedure Minilaparotomy: Trendelenburg position, 4 cm to 9 cm transverse incision, moving operative window with 3 retractors. Ligaments cut after electrocoagulation, whereas vascular pedicles clamped, ligated and cut. Vaginal vault abdominally closed with running suture and suspension to uterosacral/cardinal ligament complex Surgeons: experience not reported Prophylactic antibiotic treatment: first or second‐generation cephalosporin IV GA for both LAVH and mini‐laparotomy |
|
| Outcomes |
Primary outcome: overall complications Secondary outcomes: operative time; conversions; haemoglobin drop (day 1); VAS pain (day 1 and 2); time to return bowel function; hospital stay |
|
| Notes | Italy 3 university hospitals in Rome Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Numbered, sealed, opaque envelopes in operating room |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Low risk | No other bias identified |
Olsson 1996.
| Methods | Single‐centre, parallel‐group design Duration: not reported Randomisation: 1:1 ratio. Method not reported Allocation concealment: sealed, opaque envelopes Blinding: no Number of women randomised = 143, number analysed = 143. No dropouts Follow‐up: 4 to 6 weeks after surgery, all patients returned for a gynaecological examination including vaginal ultrasound. 6 to 8 weeks after surgery patients were asked to complete an anonymous questionnaire if they considered the duration of their postoperative hospital stay and sick leave to have been adequate. In a subgroup of patients (TLH: n = 38; AH: n = 38), postoperative health status and quality of life were self assessed prospectively 1, 3 and 12 weeks after surgery using "The Medical Outcome Trust 36‐item Short‐Form Health Survey questionnaire". Loss to follow‐up not described Power calculation for sample size: yes; assuming a complication probability of 40% for AH, the power of predicting a difference in complication rate was at least 80% at the 5% level, 2‐sided test, provided that the probability of complications following LH(a) is at most 18% and at least 64% when 70 patients are included in each group |
|
| Participants | 143 women with median age 48 years Inclusion criteria: scheduled for AH for benign disorders, with a maximum uterine width of less than 11 cm and not considered suitable for VH Exclusion criteria: suitable for VH (adnexa are not to be removed; no suspicion of endometriosis or post‐inflammatory disorders, when uterine size is normal, or in the case of uterovaginal prolapse, less than the size of an 8‐week pregnancy) | |
| Interventions |
AH versus LH (LH(a))
LH(a) arm: all patients were prescribed a second‐generation cephalosporin as well as metronidazole intravenously during the operation and by oral administration for 2 days after surgery. Ureters were identified, where this was difficult, the ureters were dissected free down to the level of the uterine arteries. If the adnexa were to be removed, the infundibulopelvic ligaments were transected by diathermal cautery and monopolar scissors. If the adnexa were to be conserved the utero‐ovarian pedicles were transected on both sides, using the same instruments. The round ligaments and the upper portion of the broad ligaments were divided using monopolar scissors and the bladder was dissected to the level just below the vaginal cuff. The posterior part of the broad ligaments were divided by scissors close to the uterus, down to the upper part of the uterosacral ligaments, which were then transected. The uterine arteries were transected close to the uterus after bipolar coagulation. The upper portion of the cardinal ligaments were divided close to the uterus, after which an incision was made into the anterior fornix of the vagina. The vaginal phase: vaginal epithelium surrounding the cervix was transected as well as any residual tissue from the cardinal and uterosacral ligaments. The transected ligaments were ligated together and incorporated into the vaginal wall AH arm: antibiotics were not routinely prescribed in this group of patients. They underwent either a lower midline or Pfannenstiel incision. If the adnexa were to be removed, the infundibulopelvic ligaments were clamped, transected and ligated. In cases where the adnexa were not to be removed, the utero‐ovarian pedicles were transected and ligated. The anterior broad ligaments were divided down to the vesico‐vaginal junction and the bladder reflected to just below the vaginal cuff. The uterine vessels were divided close to the uterus. Following division of the cardinal and uterosacral ligaments, the uterus was excised. The vaginal cuff was closed with interrupted sutures and the peritoneal layers closed and attached to the top of vagina Surgeons: 2 out of 5 surgeons of senior registrar grade and specifically trained in LH(a). 2 out of 10 surgeons of senior registrar grade trained in AH |
|
| Outcomes | Operating time (minutes); complications; postoperative pain relief; convalescence (sick leave); hospital stay; quality of life; economic analysis (cost) | |
| Notes | Sweden University Hospital of Sahlgrenska Funding: Goteborg Medical Society Fund, Swedish Medical Research Council |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts; loss to follow‐up unknown |
| Selective reporting (reporting bias) | Low risk | Primary outcomes clearly defined and reported |
| Other bias | Low risk | No other bias identified |
Ottosen 2000.
| Methods | Single‐centre study, parallel‐group design Duration: January 1996 to May 1998 (2 years, 5 months) Randomisation: computer‐generated numbers. Randomly allocated to one of 3 operating methods in 4 blocks of 30 to ensure a balanced number of patients throughout study period. Interim analysis done after 25 patients were randomised to each group Allocation concealment: sealed, opaque envelopes prepared by and successively opened by the research nurse Blinding: no Number of women randomised = 120, number analysed = 120. No dropouts Follow‐up: 2 weeks postoperatively in outpatient clinic for examination to detect complications and evaluate need for further sick leave. No loss to follow‐up Power calculation for sample size: yes; sample size based on reported hospital stay for vaginal and abdominal hysterectomy of 2.3 and 4 days, respectively. If 1.5 is the SD for hospital stay, 40 women were randomised to achieve a power of 80% at alpha = 0.05 Intention‐to‐treat analysis: yes |
|
| Participants | 120 women with a mean age of 47 years (AH group), 49 years (VH group) and 48 years (LAVH group) Inclusion criteria: scheduled for hysterectomy for anticipated benign causes. Inclusion: menorrhagia, leiomyomas < 15 cm in diameter, dysplasia, endometrial atypia and pain Exclusion criteria: ovarian pathology, uterus larger than 16 weeks of gestational size, previously known dense adhesions, narrow vagina or obvious inaccessible uterus | |
| Interventions |
AH versus VH versus LH (LAVH) ‐ 3 treatment arms
LAVH arm: the laparoscopic part was minimised. Trocars were left in place and after closing the vaginal wall the surgeon returned to laparoscopic view to confirm haemostasis. The surgery was performed under GA in 109/120 cases, spinal block in 3/120 or in combination with epidural block in 8/120 cases AH arm: the abdomen was opened and closed in different ways according to surgeon preference. The uterus was removed by extrafascial technique and the vagina closed and covered by peritoneum VH arm: the vault was injected with 20 ml of mepivacain/adrenalin before incision in order to minimise bleeding. The peritoneal folds were opened and ligaments and uterine vessels were divided. If at this time the uterine size did not allow easy exteriorisation, bisecting, coring, morcellation, enucleation or combinations of these volume‐reducing techniques were performed. The peritoneum was closed, followed by suturing of the sacrouterine ligaments and vaginal vault Surgeons: 1 of 15 gynaecological surgeons, experience varied and in some cases residents performed under supervision Antibiotics: all patients had at least 1 dose of prophylactic antibiotic peri‐operatively: cefuroxime 1.5 g intravenously and metronidazole 1 g rectally. A daily dose of exoxaparin 20 mg subcutaneously was given as thrombotic prophylaxis through the hospital stay |
|
| Outcomes | Duration of surgery, duration of anaesthesia, stay in hospital, recovery time, peri‐operative blood loss and complications | |
| Notes | Sweden Hospital of Helsingborg Funding: Thelma Zoegas Foundation and the Stig and Ragna Gorthons Foundation, Sweden |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by computer |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Primary outcome defined |
| Other bias | Low risk | No other bias; no differences between the 3 groups regarding patients' characteristics. Surgeons' experience varied |
Paraiso 2013.
| Methods | Multicentre study (2 institutions) Duration: June 2007 to March 2011 (45 months) Randomisation: stratified by surgeon and uterine size (> or </= 12 weeks). Participants were assigned randomly according to a computer‐generated randomisation schedule with random block sizes Allocation concealment: not described Blinding: yes; patients were blinded to their assessment Number of women: randomised = 75 women. In both arms 6 cases dropped out before the intervention was performed Follow‐up: no loss to follow‐up Power calculation for sample size: yes, 23 participants per arm were needed to detect a difference of >/= 30 minutes in operating time between conventional versus robotic‐assisted TLH with 90% power and a significance level of 0.05 Intention‐to‐treat analysis applied (converted procedures analysed in original allocated arm) |
|
| Participants | 53 women with a mean age of 45.6 and 43.8 respectively Inclusion criteria: >/= 18 years old, hysterectomy for benign conditions Exclusion criteria: suspected malignancy, medical illness that precluded laparoscopy, inability to give informed consent, morbid obesity (BMI > 44), or need for concomitant bowel resection |
|
| Interventions | TLH and robotic‐assisted TLH Conventional: 4 ports Robotic‐assisted: performed with the Da Vinci Surgical System with an umbilical port for laparoscopic camera, one 10/12 mm port placed in the right of left subcostal area lateral to the rectus for suture introduction, 2 8 mm robotic ports placed in the bilateral lower quadrants and one 5 mm port 8 cm inferior to right or left subcostal margin The technique to perform the hysterectomy was performed in both arms in a standard fashion, with the entirety of the hysterectomy performed laparoscopically Surgeons: 5 experienced laparoscopists: 75 to 400 LH and at least 20 RH |
|
| Outcomes |
Primary outcomes: total case time from incision to closure Secondary outcomes: intra‐ and postoperative complications, the impact of surgery on daily living and narcotic use for 6 weeks |
|
| Notes | USA
Cleveland Clinic Supported by a grant from the Cleveland Clinic Center for Surgical Innovation, Teaching and Education |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was stratified by surgeon and uterine size (> or </= 12 weeks). Participants were assigned randomly according to a computer‐generated randomisation schedule with random block sizes |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Patients blinded to their assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. In both arms 6 cases dropped out before the intervention was performed |
| Selective reporting (reporting bias) | Low risk | No reporting bias identified |
| Other bias | Low risk | No other bias. Stratified by surgeon and uterine size |
Perino 1999.
| Methods | Single‐centre study, parallel‐group design Duration: January 1997 to 30 September 1998 (1 year, 9 months) Randomisation: method not stated and allocation concealment not reported Allocation concealment: not reported Blinding: no Number of women randomised = 102, number analysed = 102. No dropouts Follow‐up: until women were discharged from hospital. Postoperative pain was assessed 3 days after surgery. No loss to follow‐up Power calculation for sample size: no |
|
| Participants | 102 women with a mean age of 48 years Inclusion criteria: scheduled for hysterectomy for benign diseases Exclusion criteria: not stated | |
| Interventions |
AH versus LH (TLH)
TLH arm: after a CO2 pneumoperitoneum was created, a 10 mm trocar was placed in the umbilical site to introduce the laparoscope and the camera. 3 ancillary 5 m trocars were placed suprapubically. After an abdominal inspection, lysis of any adhesions was performed, the uterus was then mobilised. After bipolar coagulation, the round ligament was sectioned at 3 cm from the uterus. The areolar tissue of the broad ligament was then dissected and its posterior fold fenestrated at an avascular area above the uterine vessels. The infundibulo‐pelvic ligament vessels were coagulated and cut using bipolar forceps and scissors under direct visualisation of the pelvic ureter. Once the uterine ligaments were sectioned, the operation continued centrally in a downward direction. If the adnexae were not to be removed, the utero‐ovarian ligament was coagulated and sectioned proximal to the ovaries. The vesico‐uterine peritoneal fold was opened by scissors and a bladder dissection from the low uterine segment down to the upper part of the vagina was performed. The utero‐sacral ligaments were then coagulated and sectioned. The uterine artery was skeletonised and then coagulated with bipolar forceps and cut with scissors. Incision and coagulation of the cardinal ligaments to expose the vaginal fornices, separated from the stump of the uterine artery. Circular colpotomy was then performed and the uterus was removed from the vagina. The vaginal vault was then sutured laparoscopically or vaginally
AH arm: performed according to the technique described for benign disease (Mattingly and Thompson) Intravenous pain relief was given postoperatively Surgeons: all operations performed by the same team of 3 surgeons with experience of 100+ TLH procedures |
|
| Outcomes | Operating time; blood loss; postoperative pain; postoperative decrease in haemoglobin; complications and duration of postoperative hospital stay | |
| Notes | Italy Gynaecologic University Hospital of Palermo Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | Low risk | No power calculation reported, no other bias identified |
Persson 2006.
| Methods | Multicentre study, parallel‐group design Duration: October 1996 to May 2003 (5 years, 6 months) Randomisation: block randomisation (according random table) Allocation concealment: sealed, opaque envelopes Number of women eligible = 1360, and randomised = 125. 1 dropout: withdrew before consent. In the LH group, there were 3 intra‐operative conversions to AH Follow‐up: women were followed up until 6 months after surgery. 5 lost to follow‐up: in the LH group 1 woman withdrew consent before the 5 weeks follow‐up, and 4 women withdrew consent before the 5 weeks follow‐up Power calculation for sample size: 60 patients per group were necessary to detect a difference between the 2 groups of 10 units or more on the PGWB with 90% power, a significance level of 0.05 and a dropout rate of 20% Analysis was byintention‐to‐treat |
|
| Participants | 119 women with a mean age of 44 years in both groups Inclusion criteria: women with benign disease, LH was feasible, fluent in Swedish Exclusion criteria: genital tract malignancy, pre‐operative GnRH analogues, postmenopausal women without HRT, psychiatric disorders | |
| Interventions | AH versus LH(a) AH: performed by Pfannenstiel incision and according to the extrafascial technique LH were LH(a) procedures: with a 3‐port technique. Parametrium and uterine artery were sealed laparoscopically with bipolar coagulation or stapling. Cardinal and uterosacral ligaments as well as suturing of vaginal cuff vaginally. In both procedures the vaginal cuff was anchored to the uterosacral ligaments without peritonealisation Antibiotics: both groups received prophylactic antibiotic treatment (cefuroxime 1.5 g and metronidazole 1 g IV) Surgeon experience: (supervising) surgeons were skilled and experienced | |
| Outcomes | Primary outcome: psychological well being (questionnaires PGWB) Secondary outcomes: questionnaires WHQ, STAI, BDI; operative time; complications, conversions to AH; hospital stay; return to normal activities | |
| Notes | Sweden 2 county hospitals, 2 central hospitals and 1 university hospital in the southeast Funding: grants from the Medical Research Council of South East Sweden |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | According to random table |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 dropout after randomisation and 5 lost to follow‐up were not analysed (1 LH and 5 AH group), i.e. < 5%. It is not clear how many women were lost to follow‐up after 6 months |
| Selective reporting (reporting bias) | Low risk | Primary outcome predefined |
| Other bias | Unclear risk | Only 9% of eligible patients were randomised |
Raju 1994.
| Methods | Single‐centre study, parallel‐group design Duration: March 1992 to October 1993 (1 year, 8 months) Randomisation: containing computer‐generated block randomisation numbers. Block size of 10 Allocation concealment: sealed envelopes Blinding: no Number of women randomised = 80, number analysed = 80. No dropouts Follow‐up: 6 weeks after surgery and until women return to work. No loss to follow‐up Power calculation for sample size: yes, 40 patients in each arm were estimated to detect a 25% difference in morbidity between the groups, with a power of 90% at the 5% level |
|
| Participants | 80 women with a mean age of 46 years Inclusion criteria: scheduled for hysterectomy and bilateral oophorectomy for benign conditions Exclusion criteria: morbid obesity, uterus larger than 14 weeks gestation size or uterovaginal prolapse | |
| Interventions |
AH + BSO versus LH (LAVH) + BSO
LAVH + BSO arm: 5.5 mm flap‐valved trocars were inserted enabling the insertion of laparoscopic instruments. 12 mm trocar and cannula were introduced suprapubically in the midline 3 cm above the upper border of the symphysis pubis as a port for the use of the Autosuture Multifire Endo GIA 30 stapling device.The cervix was grasped with a vulsellum and a broad‐ended blunt uterine curette was inserted to manipulate the uterus from the perineal end. Any adhesions between the uterus or adnexae to adjacent structures were divided with scissors after diathermy coagulation. Both round ligaments were treated with diathermy and cut with scissors approximately 3 cm from the internal inguinal ring whilst holding the ligament with a grasping forceps. The peritoneum of the anterior leaf of the broad ligament was dissected from the divided round ligament back towards the infundibulo‐pelvic ligament thus opening the tissue space between the 2 folds of broad ligament. The posterior leaf of the broad ligament was then pierced with endoshears to make a window, a safe distance above the ureter which had been previously identified. The ovarian pedicle was then sized for thickness of tissue by means of a GIA endo gauge inserted through the midline suprapubic incision. The correct size of endo stapling clamp was selected. The ovarian pedicle was clamped and cut with the appropriate GIA endo stapling device, placed from the upper border of the infundibulo‐pelvic ligament and with the jaws of the stapler passing well through the peritoneal window in the broad ligament. By using this technique each ovarian pedicle required only one firing of the GIA stapler to divide it. Finally the uterovesical fold of the peritoneum was divided with scissors and sometimes the uterosacral ligaments were divided after diathermy coagulation. The uterus, tubes and both ovaries were then removed vaginally after circumcising the cervix and opening the pouch of Douglas to allow ligation and division of the cardinal ligaments and uterine vessels as in a traditional vaginal hysterectomy. The vaginal vault was anchored to the cardinal ligaments and closed with interrupted sutures
AH+BSO arm: procedures were performed using a standard technique
Operations were performed by one of the authors or by another surgeon of senior registrar grade Surgeons: operations performed by one of the authors. Experience unknown Premedication: temazepam 20 mg, 2 hours before operation. GA induced with thiopentone and maintained with enflurane and nitrous oxide. Under anaesthesia a bolus intravenous injection of amoxicillin clavulanate (Augmentin) 1.2 g was given. Antibiotic therapy continued for 7 days postoperatively |
|
| Outcomes | Operating time, blood loss, haemoglobin change, hospital stay, postoperative analgesia, complications, recovery time (subjective assessment of patient's general well being and return to normal activity) and cost | |
| Notes | UK St Thomas's Hospital, London Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by computer |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available |
| Other bias | Low risk | No other bias reported. Surgeon's experience unknown, but all surgeries performed by 1 surgeon |
Ribeiro 2003.
| Methods | Single‐centre study, parallel‐group design Duration: not reported Randomisation: method not stated Allocation concealment: not reported Blinding: no Number of women randomised = 60, number analysed = 60. No dropouts Follow‐up: routinely up to 6 days. No loss to follow‐up Power calculation for sample size: no |
|
| Participants | 60 women with an overall mean age of 42.3 years (range 34 to 76 years) Inclusion criteria: benign uterine disease: myoma n = 41; adenomyosis n = 19 Exclusion criteria: uterine volume greater than 400 ml; use of any anti‐inflammatory medication during preceding 3 months; diabetes mellitus; coagulation disorders; autoimmune diseases | |
| Interventions |
AH versus VH versus LH (TLH)
AH: by Thompson and Warshaw technique VH: by Heaney's technique LH (TLH): 10 mm laparoscope inserted at umbilicus, 2 5 mm secondary ports for laparoscopic instruments. Uterine mobiliser with blunt tip used to antevert uterus and delineate vaginal fornices. Round ligaments divided with monopolar forceps and vesico‐uterine fold divided with scissors and bladder mobilised until anterior vagina identified. Utero‐ovarian ligament and fallopian tube pedicles desiccated with bipolar forceps, then scissors division of broad ligament peritoneum. Uterine artery grasped, elevated and bipolar coagulated. Cardinal and uterosacral ligaments divided with monopolar forceps. Vagina entered posteriorly near cervico‐vaginal junction. 4 cm vaginal delineator outlined circumferentially the cervico‐vaginal junction and prevented loss of pneumoperitoneum. Monopolar forceps completed the circumferential culdotomy. Uterus removed vaginally (after morcellation if necessary). Laparoscopic vaginal vault interrupted suturing and suspended by suture attachment to uterosacral/cardinal pedicles, sutures being tied extracorporally Surgeon experience: not reported Antibiotic and thrombo prophylaxis not specified |
|
| Outcomes | Operative time; pre and postoperative haemoglobin; complications | |
| Notes | Brazil Sao Paulo University School of Medicine Hospital Funding: Foundation of Research Support from Sao Paulo State |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not clearly defined |
| Other bias | Low risk | No other bias identified |
Richardson 1995.
| Methods | Single‐centre study, parallel‐group design Duration: not reported Randomisation: random numbers table Allocation concealment: not reported Blinding: no Number of women randomised = 45, number analysed = 45. No dropouts Follow‐up: 6 to 8 weeks after surgery, women completed a questionnaire on their recovery. All kept a prospective diary of their recovery for 6 weeks. No loss to follow‐up Power calculation for sample size: no |
|
| Participants | 45 women with a mean age of 41 years (LH group) and 45 years (VH group) Inclusion criteria: contraindications for vaginal surgery according to traditional criteria (absence of vaginal prolapse, nulliparity, uterine enlargement, previous pelvic surgery endometriosis and need for oophorectomy) Exclusion criteria: uterine size greater than the equivalent of 16 weeks' gestation, endometrial carcinoma, adnexal masses, known dense pelvic adhesions, or moderate/severe endometriosis | |
| Interventions |
VH versus LH
LH arm: the laparoscope was inserted sub‐umbilical incision, and usually 2 5 mm secondary portals were used for the laparoscopic instruments. Surgery was performed under the guidance of the image generated by a Supercam 9050 PB video chip camera attached to a 30 degree forward oblique laparoscope. The principal method of haemostasis was bipolar electrosurgical desiccation but Endo‐GIA 30 linear staplers were used in 8 women. In 1 woman VH was done after diagnostic laparoscopy (stage 0 VH) and in 2 VH was carried out after laparoscopic adhesiolysis had made this possible (stage 1 LH). When the ovaries were conserved, bipolar diathermy was used medially to desiccate the round and ovarian ligaments, and the fallopian tube. The approach to the ovarian pedicle during oophorectomy depended on whether the uterine vessels were to be divided laparoscopically or vaginally. If divided vaginally, the ovarian vessels were coagulated and divided but not the round ligaments. Dissection then proceeded towards the uterine origin of the round ligament, after which the hysterectomy was completed vaginally (stage 2 LH) or after laparoscopic mobilisation of the bladder (stage 3 LH). If the uterine vessels were treated laparoscopically (stage 4 LH), the round ligaments were always divided, together with the ovarian vessels and fallopian tubes, and the dissection continued to the level of the uterine arteries which were then desiccated and cut close to the uterus. Laparoscopic dissection only continued further than the uterine artery in 3 cases (stage 5 LH), all other procedures being completed vaginally VH arm: modified Heaney approach Surgeon experience: not reported |
|
| Outcomes | Operating time; analgesia required; hospital stay; recovery time and postoperative complications | |
| Notes | UK Royal Free Hospital, London Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined; insufficient information available |
| Other bias | Low risk | No other bias identified |
Roy 2011.
| Methods |
Duration: April 2007 to June 2009 (2 years, 1 month) Randomisation and allocation: not reported Blinding: no. Randomisation was revealed to the surgeon before induction of anaesthesia Follow‐up: at 1, 3 and 6 months. 9 patients were lost to follow‐up and were not analysed and reported because they needed adenectomy or did not return for follow‐up Power calculation for sample size: yes was calculated using operative time as a primary outcome. With a type I error of 0.05 and a power of 80%, a sample size of 30 women in each arm was required No intention‐to‐treat analysis |
|
| Participants | 90 women with a mean age of 41.9 in the TLH group, 43.4 in the LAVH group and 43.7 in the NDVH group Inclusion: benign pathology of uterus and not amenable to or failed medical therapy Exclusion: malignancy, PID, uterovaginal descent greater that first degree. Patients with contraindication for laparoscopy |
|
| Interventions |
TLH versus LAVH versus non‐descent VH (NDVH) TLH: 4 ports were made. A 10 mm umbilical port for laparoscope, 2 ports of 5 mm, 1 extra 10 mm port. All pedicles were coagulated and transected laparoscopically. Adnexa were preserved. The uterus was cut at the vault laparoscopically. Uterus was delivered vaginally and vault was sutured laparoscopically LAVH: the laparoscopic part included coagulation and transection of round ligament, ovarian ligament and medial end of tube followed by dissection of bladder peritoneum. The procedure was then completed vaginally: uterosacrale ligaments, cardinal ligaments and uterine vessels were ligated and transected. The uterus was extracted vaginally. Vaginal cuff sutured NDVH: incision was made in cervico‐vesical junction anteriorly. Bladder was pushed anteriorly and pouch of Douglas opened posteriorly. Uterosacral ligaments, Mackenrodt ligament, uterine vessels followed by round and ovarian ligament were clamped, transected. In cases of large uteri, bisection of the specimen or myomectomy was done. Vaginal cuff was sutured Surgeons: all procedures were performed by the same surgeon. Experience not reported |
|
| Outcomes | Intra‐ and postoperative parameters Primary outcomes: total duration of surgery and blood loss Secondary outcomes: postoperative pain, febrile morbidity, infection, total duration of hospital stay, satisfaction (HRQOL and SF‐12) and sexual dysfunction (self developed questionnaire) |
|
| Notes | India All India institute, New Delhi Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Randomisation was revealed to surgeon just before induction of anaesthesia. Blinding of patients or researchers not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No dropouts. Loss to follow‐up reported (n = 9; i.e. 10%) |
| Selective reporting (reporting bias) | Low risk | Patients who also underwent adnexal removal were excluded to minimise bias |
| Other bias | Low risk | No other bias identified |
Roy 2012.
| Methods | Single tertiary centre Duration: April 2008 to June 2010 (2 years, 1 month) Randomisation: computer‐based Allocation procedure: not reported Number of patients randomised = 23, number of patients analysed = 20. 3 dropouts: serum interleukin level could not be processed in 1 patient from each group; 1 patient had conversion to mini‐laparotomy Blinding: not reported Analysis by intention‐to‐treat: no; 1 conversion in the LAVH group was taken out of analysis and was not further reported Follow‐up: no loss to follow‐up Power calculation for sample size: to detect a difference of 1 standard deviation between interleukin level of the 2 groups of hysterectomy for a uterine size >/= 12 weeks, with type 1 error of 0.01 and a power of 80%, we calculated that 10 women needed to be operated in each group |
|
| Participants | 20 women with a mean age of 41.6 years in the LAVH group and 43 years in the NDVH group Inclusion criteria: women with benign pathology of uterus who had estimated uterine weight between 300 g and 1500 g and were planned for hysterectomy Exclusion criteria: genital malignancy, acute pelvic inflammatory disease, utero‐vaginal descent greater than first degree and any contraindications for laparoscopy |
|
| Interventions | Laparoscopic‐assisted vaginal hysterectomy (LAVH) versus non‐descent vaginal hysterectomy (NDVH) LAVH: 4 ports were made. A 10 mm port was placed at umbilicus for laparoscope. 3 other ports were placed in the lowed abdomen. The laparoscopic part included coagulation and transection of round ligament and transection of bladder peritoneum. When preservation of adnexa was needed, the fallopian tube and ovarian ligament were coagulated and transected. In cases where salpingo‐oophorectomy was needed, the infundibulopelvic ligament was isolated, coagulated and transected. The procedure was completed vaginally. The anterior and posterior cul‐de‐sac were opened. The cardinal ligaments, uterosacral ligaments and the uterine vessels were ligated and transected. The uterus was extracted vaginally. Vaginal cuff was closed NDVH: incision was made in cervico‐vesical junction anteriorly. Bladder was pushed anteriorly and pouch of Douglas opened posteriorly. The uterosacral ligaments, cardinal ligaments, uterine vessels followed by round and ovarian ligaments were clamped, cut and ligated. After clamping uterine arteries, uterus was bisected and myomectomy done to reduce the bulk of the uterus. Vaginal cuff was closed Surgeons: all procedures performed by the same surgeon. Experience not reported Antibiotic and thrombo prophylaxis not specified |
|
| Outcomes |
Primary: venous blood levels of IL‐6 preoperatively and 3, 24 and 72 hours after surgery Secondary: blood loss, operating time, postoperative analgesia requirement, hospital stay and morbidity |
|
| Notes | India All India institute, New Delhi Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation: computer‐based, but not further specified |
| Allocation concealment (selection bias) | Unclear risk | Allocation procedure not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts: n = 3, i.e. 15%. No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Since the study focused mainly on tissue trauma, 1 patient who underwent a conversion to mini‐laparotomy was excluded from the final analysis |
| Other bias | Unclear risk | Analysis by intention‐to‐treat: not reported |
Sarlos 2012.
| Methods | Single‐centre Duration: 2008 to 2011 (3 years) Randomisation: the randomisation scheme was generated by using the website www.randomization.com Allocation concealment: not reported Blinding: patients could not be blinded because the robot surgery took place in another building Number of women: 100 patients randomised; 95 completed the study Follow‐up: loss to follow‐up not described Power calculation for sample size: not performed Analysis by intention‐to‐treat |
|
| Participants | 95 patients with a mean age of 45.8 years in the conventional group and 46.3 years in the robot‐assisted group Inclusion criteria: indication for hysterectomy because of benign lesions if vaginal hysterectomy was expected to be difficult because of myomas or nulliparity. Uterus weight less than 500 g Exclusion criteria: not reported |
|
| Interventions | Robot‐assisted LH versus conventional LH RALH: a 3‐armed daVinci standard surgical robot was used cLH: a 10 mm optical port and 3 5 mm working trocars were used Both procedures performed according the same standard operating procedure Antibiotic prophylaxis: cefazoline 2 g Surgeons: 2 senior gynaecologists experienced in laparoscopic surgery, performing at least 50 laparoscopic LH and 30 RH per year. The surgical team consisted of a console surgeon, a bedside assistant and a surgical nurse No conversions to laparotomy |
|
| Outcomes | Primary outcomes: surgical outcome (time to hospital discharge) and quality of life | |
| Notes | Switzerland Cantonal Hospital, Aarau Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation scheme was generated by using the website www.randomization.com |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Patients could not be blinded because the robot surgery took place in another building |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropout. Follow‐up not described |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes predefined and reported as such |
| Other bias | Low risk | No other bias identified |
Schutz 2002.
| Methods | Single‐centre study, parallel‐group design Duration: August 1995 to December 1997 (2 years, 4 months) Randomisation: computer‐generated randomisation list Allocation concealment: concealment by telephone inquiry Blinding: no Number of women randomised = 48, number analysed = 48. No dropouts Follow‐up: following discharge from hospital the women received a self administered questionnaire to evaluate their recuperation over a period of 12 months. 35 women (72.9%) answered the questionnaire, 20 of 28 (71.4%) in the LAVH group and 15 of 20 (75%) in the AH group Power calculation for sample size: yes |
|
| Participants | 48 women with median age of 48 years Inclusion criteria: sonographically estimated uterine weight > 200 g and patient has no preference for either surgical technique Exclusion criteria: not stated | |
| Interventions | AH versus LH (LH(a)) LH(a) arm: either type I or II procedure. Type I: the laparoscopic part included coagulation and transection of the round ligament and transection of the bladder peritoneum. If the adnexa was desired, the fallopian tube and the ovarian ligament were coagulated and transected. Where salpingo‐oophorectomy was needed, the infundibulo‐pelvic ligament was isolated, coagulated and transected following visualisation of the ureter. Type II: the uterine artery was identified at its origin when branching off the internal iliac artery. The identification was made coming from either the internal umbilical ligament or the pararectal fossa. Prior to coagulation of the uterine artery, the ureter was identified and pushed medially. After coagulation, it was left to the discretion of the surgeon to transect the uterine artery. The uterus was mobilised by pulling on the transected round ligaments and no intrauterine probes were applied for mobilisation of the uterus 71.4% operations performed by attending physician, 28.6% by resident assisted by physician AH arm: followed the standard extrafascial technique. A Balfour retractor was used and the skin incision was stapled Surgeons: 40% performed by physician and 60% by resident assisted by physician | |
| Outcomes |
Primary outcome: length of stay in hospital Secondary outcomes: operating time; postoperative pain; blood loss and recovery time until return to full work activity |
|
| Notes | Germany Friedrich Schiller University, Jena Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Telephone inquiry |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No dropouts; loss to follow‐up: 75% and 78% (i.e. > 15% loss to follow‐up), respectively, answered the questionnaire after 12 months |
| Selective reporting (reporting bias) | Low risk | No reporting bias identified |
| Other bias | Unclear risk | Surgeons' experience was not clear |
Seracchioli 2002.
| Methods | Single‐centre study, parallel‐group design Duration: January 1997 to January 2001 (4 years) Randomisation: computer‐generated randomisation unknown to the surgeons Allocation concealment: not mentioned Blinding: no Number of women randomised = 122, 122 analysed. No dropouts reported Follow‐up: telephone interviews 2 months after discharge to determine the number of days before going back to normal activities. No loss to follow‐up Power calculation for sample size: no |
|
| Participants | 122 women with a mean age of 46.3 (LH(a) group) and 47.3 (AH group) Inclusion criteria: eligible for AH due to a large uterus (> 14 weeks) caused by myomas. Uterine weight > 300 g, determined by a pelvic examination and transvaginal ultrasonography Exclusion criteria: uterus projecting above the transverse umbilical line and with other pelvic pathologies (prolapse, pelvic floor relaxation, stress incontinence and adnexal masses). Medical conditions that require hospital monitoring, e.g. diabetes, heart disease, if they had undergone previous abdominal surgery requiring longitudinal laparotomy or contraindications to operative laparoscopy | |
| Interventions | AH versus LH (LH(a)) LH(a) arm: 10 mm cannula placed in the umbilical site to introduce the laparoscope and camera. 2 5 mm suprapubic access routes were inserted lateral to deep inferior epigastric arteries. A third cannula was inserted between the umbilicus and xiphoid. Round ligaments, fallopian tubes and utero‐ovarian ligaments (or infundibulopelvic ligaments if the ovaries were to be removed) were coagulated and sectioned. Uterine peritoneal fold was opened with scissors, dissecting the bladder off the lower uterine segment and cervix. Incision of the fornix, extended laterally, stopping close to uterine vessels. Uterine pedicles skeletonised, coagulated and sectioned. Parametrial tissues were coagulated and sectioned so the uterus is free to be removed vaginally. Vaginal vault was sutured vaginally with the cardinal‐uterosacral ligaments Antibiotic prophylaxis: ampicillin 2 g Surgeons: all surgical procedures were performed by the same investigators under GA. Experience not reported | |
| Outcomes | Operating time, laparo‐conversions, blood loss, haemoglobin drop, fever, transfusions, hospital stay and convalescence | |
| Notes | Italy S Orsola Hospital, University of Bologna Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Allocation reported as "unknown to surgeons" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | Low risk | No other bias identified |
Sesti 2008a.
| Methods | Single‐centre study, 3 parallel‐groups Duration: May 2005 to September 2007 (2 years, 4 months) Randomisation: computer‐generated list Allocation concealment: serially numbered, opaque, sealed envelopes Blinding: patients were not blinded. Those performing the surgical procedures did not know which patients had been included in the study and those assessing the outcomes were blinded to the group assignment Number of women eligible 189, number of women randomised 150. There were no dropouts Follow‐up: no loss to follow‐up Power calculation for sample size: yes, 36 patients in each group were necessary to detect a difference of more than 24 hours in discharge time with an alpha error level of 5% and a beta error of 80% Analysis was by intention‐to‐treat (no conversions) |
|
| Participants | 50 women in the VH group (mean age 47.8 years) 50 women in the LAVH group (mean age 49.0 years) 50 women in the mini‐laparotomy (mini‐LPT) group (mean age 47.7 years) Inclusion criteria: symptomatic or rapidly growing myomas, age less than 55 years and uterine size greater than or equal to 12 weeks of gestation Exclusion criteria: nulliparous women, uterine size greater than or equal to 16 weeks, previous uterine surgery and suspicion of malignant gynaecological disease |
|
| Interventions |
VH versus LAVH versus mini‐LPT VH: as described by Dargent in 2004. If the uterine size did not allow easy exteriorisation, bisecting, coring, morcellation, enucleation of myomas or combinations of these volume‐reducing techniques were performed LAVH: type ID (dissection up to but not including uterine arteries plus anterior structures, and posterior culdotomy) according to the AAGL Classification System for Laparoscopic Hysterectomy Mini‐LPT: performed using a 4 cm to 7 cm suprapubic incision. The subcutaneous fat and the abdominal fascia were transversely opened 2 cm above the skin incision. The abdominal muscle and the parietal peritoneum were longitudinally opened on the midline Antibiotics: all patients received intraoperative prophylactic antibiotic therapy (ampicillin sodium/sulbactam sodium combination 2 g). Intravenous pain relief was given postoperatively Surgeons: all procedures were performed by 2 equally skilled and experienced surgeons using identical techniques |
|
| Outcomes |
Primary outcome: difference in hospital discharge time (measured in hours) among the 3 procedures Secondary outcomes: operating time, blood loss, paralytic ileus time, intraoperative complications, febrile morbidity, intensity of postoperative pain and early postoperative complications |
|
| Notes | Italy Tor Vergata University Hospital, Rome Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Those assessing the outcomes were blinded to the group assignment; patients were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes (pre)defined and accordingly reported |
| Other bias | Low risk | Procedures were performed by 2 equally skilled and experienced surgeons using identical techniques |
Sesti 2008b.
| Methods | Single‐centre study, parallel‐group design Duration: April 2003 to June 2005 (2 years, 2 months) Randomisation: numbered, sealed, opaque envelopes based on a computer‐generated list Blinding: those who performed surgical procedures did not know which patients undergoing surgery had been included in the study. Those assessing the outcomes were blinded to the group assignments Number of women eligible = 89; 9 women refused to participate and 80 patients were included (40 in each group). There were no conversions or dropouts Follow‐up: women were followed up until 30 days after surgery. No loss to follow‐up Power calculation for sample size: yes, at least 26 patients in each group were necessary to detect a difference of more than 24 hours in discharge time with a significance level of 0.05% and a power of 80% |
|
| Participants | 80 women with a mean age of 49 years in the VH group and 48 years in the LAVH group Inclusion criteria: symptomatic or rapidly growing myomas, age < 55 years, uterine size at least 12 weeks gestation Exclusion criteria: nulliparous women, uterine size greater than 16 weeks gestation, previous uterine surgery, suspicion of malignant gynaecological disease |
|
| Interventions |
VH versus LAVH VH: as described by Dargent in 2004. If the uterine size did not allow easy exteriorisation, bisecting, coring, morcellation, enucleation of myomas or combinations of these volume‐reducing techniques were performed LAVH: type ID (dissection up to but not including uterine arteries plus anterior structures and posterior culdotomy) according to the AAGL Classification System for Laparoscopic Hysterectomy Antibiotics: patients in both groups received prophylactic antibiotic therapy by an ampicillin sodium/sulbactam sodium combination Type of anaesthesia not mentioned for VH Surgeons: all procedures performed by the same 2 surgeons using the same technique. Surgeon experience not mentioned |
|
| Outcomes |
Primary outcomes: discharge time as measured in hours after surgery. The patients were discharged from the hospital when they were tolerant of a normal diet, able to dress themselves, fully mobile, apyrexial and not requiring analgesics Secondary outcomes: differences in operation time, blood loss, paralytic ileus time, febrile morbidity (body temperature 38°C in 2 consecutive measurements 4 hours apart), intensity of pain, early postoperative complications (any unfavourable episode occurring within 30 days after surgery requiring readmission, blood transfusion or repeat surgery) |
|
| Notes | Italy Tor Vergata University Hospital Research funds by the Italian Ministry of Education |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Numbered, sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Those assessing the outcomes were blinded to the group assignments; patients not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes (pre)defined and accordingly reported |
| Other bias | Low risk | No other bias identified |
Silva Filho 2006.
| Methods | Parallel‐group design Duration: July 2004 to January 2005 (6 months) Randomisation: not reported Blinding: not reported Number of women randomised = 60. There were no dropouts. There were no conversions to AH in the VH group Follow‐up: women were followed up until 1 month after surgery. The return rate of the questionnaires at 1 month was 100% Power calculation for sample size: no Analysis was by intention‐to‐treat |
|
| Participants | 60 women. Mean age 45 years in both groups Inclusion criteria: women with myoma and uterine size < 300 cm3 Exclusion criteria: uterine prolapse, need for associated procedures, suspicion of extrauterine disease | |
| Interventions | VH and TAH Procedures were performed according to the modified Richardson's and Heaney's technique. Bisection and morcellation if needed in VH Antibiotics: both groups received prophylactic antibiotic treatment (cefalotin 1 g IV) and anticoagulant therapy Epidural anaesthesia for both VH and TAH Surgeon experience: surgeons reported as experienced in both procedures | |
| Outcomes | Primary outcome: quality of life (questionnaire SF‐36) Secondary outcomes: operative time; conversions to AH; hospital stay | |
| Notes | Brazil It is unclear from which hospital(s) the women were recruited Funding not reported The subscales and score ranges of the questionnaire SF‐36 are not in agreement with the international standard |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding of patients not reported. The interviewer at 1 month after surgery was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No reporting bias identified |
| Other bias | Unclear risk | The subscales and score ranges of the questionnaire SF‐36 were not in agreement with the international standard |
Song 2013.
| Methods | Single‐centre Duration: January 2010 to January 2011 (12 months) Randomisation: patients were randomly assigned 1:1 with the use of a computer‐generated schedule to undergo LESS LAVH or multi‐port LAVH. Randomisation was performed in permuted blocks of 4 with random variation of the blocking number Allocation procedure: a research nurse prepared all numbered, opaque, sealed envelopes Blinding: not reported Number of women 40 women randomised, 39 women analysed. 1 SP‐LH procedure converted Follow‐up: 1 woman assigned to multi‐port was lost to follow‐up Power calculation for sample size: yes, on the basis of the difference in primary outcome. Assuming a standard deviation of 2 points for the BIS or CS score, allowing 5% dropout rate, they estimated that 20 patients would be needed per group |
|
| Participants | 39 women with a mean age of 44.6 and 43.5 respectively Inclusion criteria: patients who had an indication for hysterectomy, no evidence of gynaecologic malignancy, appropriate medical status for laparoscopic surgery (ASA 1 or 2) Exclusion criteria: age </= 18 years, uterine size > 20 weeks, recent diagnosis of cancer, inability to understand and provide written informed consent |
|
| Interventions |
SP‐LH versus conventional multi‐port LAVH Multi‐port: after the primary 12 mm trocar was placed at the umbilicus, a 5 mm trocar was placed in each lower quadrant, lateral to the inferior epigastric artery Surgeons: all procedures by a single surgeon with experience of more than 500 LH and 200 SP‐LH |
|
| Outcomes |
Primary outcomes: cosmetic satisfaction 1, 4 and 24 weeks after surgery Secondary outcomes: operative time, perioperative complications and postoperative hospital stay |
|
| Notes | Korea Samsung Medical Center, Seoul Supported by grant CRS 110‐09‐1 from Samsung Medical Center |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned 1:1 with the use of a computer‐generated schedule to undergo LESS LAVH or multi‐port LAVH. Randomisation was performed in permuted blocks of 4 with random variation of the blocking number |
| Allocation concealment (selection bias) | Low risk | A research nurse prepared all numbered, opaque, sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up/conversions reported (< 5%) |
| Selective reporting (reporting bias) | Low risk | No reporting bias |
| Other bias | Low risk | No other bias identified |
Soriano 2001.
| Methods | Single‐centre study, parallel‐group design Duration: January 1999 to December 1999 (1 year) Randomisation: pre‐determined computer‐generated randomisation code Blinding: no Number of women randomised = 80, number analysed = 80. No reported dropouts Follow‐up: until women were discharged from hospital Power calculation to estimate sample size: yes. Assumed that the incidence of complications in patients undergoing LH(a) is 10% and there will be an increase of complication rate to 40%, with alpha (type I error) of 0.05 and beta (type II error) of 0.2. It was planned to recruit at least 35 women to each arm |
|
| Participants | 80 women with a mean age of 49 years Inclusion criteria: women referred for hysterectomy due to benign pathology. Uterine size larger than 280 g and one or more of the following: previous pelvic surgery, history of pelvic inflammatory disease, moderate or severe endometriosis, concomitant adnexal masses or indication for adnexectomy Exclusion criteria: suspicious adnexal mass, anaesthetic contra‐indications for laparoscopic surgery. Women with contra‐indications to acetaminophen, or to nonsteroidal antiinflammatory drugs and those whose pain evaluation was judged unreliable due to neurological disease, or treatment by steroids, NSAIDs or opioids prior to surgery | |
| Interventions | VH versus LH (LH(a)) LH(a) arm (LH type IV): after induction of pneumoperitoneum and insertion of the video laparoscope, 3 suprapubic trocars were introduced for the ancillary instruments. The pelvis and the upper abdomen were evaluated and endo metric lesions, adhesion or ovarian cysts, when present, were treated. When the ovaries were to be conserved, bipolar forceps and scissors were used to resect the round ligament and the uteroovarian ligaments with the fallopian tubes. For adnexectomy, bipolar forceps and scissors were used to resect the round and infundibulopelvic ligaments, mesosalpinx and mesovarium. The laparoscopy included opening the bladder flap and bladder dissection, coagulating and transecting the uterosacral ligaments, base of cardinal ligaments and uterine vessels. Laparoscopic haemostasis was achieved using exclusively bipolar electrocoagulation. The vaginal phases included only circular incision of the vagina and wedge morcellation, coring or bivalving was performed. Peritoneal closure and closure of the vaginal vault concluded the vaginal phase VH arm: performed using the modified Heaney procedure. When necessary, wedge morcellation, coring or bivalving was performed Surgeon experience: not reported Prophylactic antibiotic: cefazoline 2 g IV and low molecular heparin the evening before the operation. Intravenous pain relief was given postoperatively | |
| Outcomes | Uterine weight; operative time; haemoglobin drop; postoperative complications; blood loss; pain relief and hospital stay | |
| Notes | France Hopital Hotel‐Dieu, Paris Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation code |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts; no loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not clearly defined; insufficient information available |
| Other bias | Low risk | Surgeons' experience not specified. No other possible bias identified |
Summitt 1992.
| Methods | Single‐centre study, parallel‐group design Duration: June 1991 to February 1992 (9 months) Randomisation: computer‐generated randomisation numbers Blinding: no Number of women randomised = 56, number analysed = 56. One operation was unsuccessful therefore for certain outcomes only 55 were analysed Follow‐up: postoperative follow‐up consisted of a telephone call by the attending surgeon on the evening of surgery and the first 2 postoperative days. Patients were then seen 1 and 6 weeks postoperatively in the outpatient clinic Power calculation for sample size: not reported Analysis not by intention‐to‐treat (conversion excluded from analysis) |
|
| Participants | 56 women with a mean age of 38 years
Inclusion criteria: 1) age 18 to 65 years; 2) no significant medical illness that required prolonged postoperative monitoring or care; 3) a telephone in working order; 4) a support person who could assist the patient for the first 48 hours after surgery and 5) an understanding of all postoperative instructions
Criteria for VH: 1) uterine size no larger than 16 gestational weeks; 2) the presence of uterine mobility; 3) a pubic arch of at least 90 degrees. Factors that did not influence the decision to proceed vaginally include: 1) a preoperative diagnosis of pelvic pain; 2) the need for oophorectomy, or 3) a history of previous pelvic surgery Exclusion criteria: 1) A concomitant anterior or posterior colporrhaphy was required; 2) cervical conisation was performed within the previous 48 hours; and 3) additional antibiotic prophylaxis was required for valvular heart disease. They were also excluded if they had absolute contraindications to laparoscopy, such as 1) any condition that could not tolerate anaesthesia, 2) severe bleeding disorder, 3) acute peritonitis of the upper abdomen and uterine myomata or 4) a pelvic mass larger than 16 gestational weeks in size |
|
| Interventions |
VH versus LH (LH(a))
LH(a) arm: 3 12 mm trocars were used, one placed infra‐umbilically and one placed in each lower quadrant approximately 6 cm to 8 cm above the pubic rami, lateral to the inferior epigastric arteries. A Hulka tenaculum was used to manipulate the uterus. The bladder flap was developed by incising the vesicouterine fold of peritoneum and dissecting the bladder below the cervix. The ureters were then identified and mobilised using linear incisions in the medial leaf of the broad ligament, midway between the uterosacral ligaments and infundibulopelvic vessels
The Multifire EndoGIA disposable surgical stapler was used to staple‐ligate and cut all uterine pedicles, each consisting of the round ligament, fallopian tubes and utero‐ovarian ligament, were cut. If the ovaries were to be removed, the stapler was instead placed outside the tube and ovary, encompassing the infundibulopelvic ligament. The uterine arteries were next staple‐ligated and cut bilaterally. If possible, the stapling device was also used to ligate and cut the cardinal ligaments. Otherwise, stapling of uterine pedicles ended and the anterior vaginal fornix was entered with unipolar cautery, incising over a moistened sponge distending the anterior vagina. The remainder of the hysterectomy was completed vaginally
Surgeons: performed by a team of 3 surgeons (2 attending faculty and a senior gynaecology resident) VH arm: anaesthesiologist's choice of general or regional anaesthesia. A modified Heaney technique was performed using O‐coated polyglycolic acid suture for all pedicles. The vaginal cuff was closed in all cases Surgeons: performed by a gynaecology resident with attending faculty member All received pre‐operative antibiotic prophylaxis (cefazolin 2 g) intravenously. If allergic to penicillin, 200 mg dose of doxycycline intravenously was used |
|
| Outcomes | Operating time, blood loss, anaesthesia time, intra‐operative complications, febrile morbidity, pain relief and costs | |
| Notes | USA Gynecology clinic, University of Tennessee, Memphis Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts, loss to follow‐up not reported |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | Unclear risk | No intention‐to‐treat analysis, no power calculation. Procedures performed by different group of surgeons |
Summitt 1998.
| Methods | Multicentre study (n = 3), parallel‐group design Duration: not reported Randomisation: computer‐generated randomisation list Allocation procedure: each surgical assignment placed in consecutive sealed envelopes and opened by an independent person (study secretary) Blinding: no Number of women randomised = 67, number analysed = 65. 2 women who were randomised refused their assigned procedure and they were removed from the study and their random numbers discarded Follow‐up: 2 and 6 weeks postoperatively in the outpatient office. No loss to follow‐up Power calculation to estimate sample size: not reported Analysis said to be by intention‐to‐treat, but 2 randomised women were not analysed |
|
| Participants | 65 women with a mean age of 38.3 (LH(a) group) and 41.5 (AH group)
Inclusion criteria: scheduled for AH for benign diseases. Indications for AH: 1) documented visual diagnosis of pelvic endometriosis; 2) documented pelvic adhesions; 3) 3 or more previous laparotomies; 4) uterine leiomyomata 12 to 18 gestational weeks in size; 5) previous tuboovarian abscess or 2 documented episodes of pelvic inflammatory disease requiring IV antibiotic therapy; 6) adnexal mass in the presence of an indication for hysterectomy; and 7) indicated hysterectomy with lack of mobility and unfavourable vaginal introitus. The following inclusion criteria were met: 1) age at least 18 years, 2) a working telephone in the home, 3) an available support person in the home for 48 hours after surgery, and 4) an understanding of the postoperative instructions Exclusion criteria: concomitant colporrhaphy, urethropexy, vaginal vault suspension or a non‐gynaecologic major operation required. Medical conditions requiring in‐hospital monitoring or if they had known cervical or endometrial cancer. Candidates were also excluded if they had absolute contraindications to operative laparoscopy, including: 1) uterine leiomyomas or pelvic masses greater than 18 gestational weeks in size, 2) conditions making them intolerant to anaesthesia, 3) severe bleeding disorders, 4) acute periodontitis of the upper abdomen with severe distension, or 5) a midline abdominal hernia |
|
| Interventions |
AH versus LH (LH(a)) LH(a) arm: 3 12 mm trocars were used, one placed infra umbilically and one placed in each lower quadrant approximately 6 cm to 8 cm above the pubic rami, lateral to the inferior epigastric arteries. A Hulka tenaculum was used to manipulate the uterus. The bladder flap was developed by incising the vesicouterine fold of peritoneum and dissecting the bladder below the cervix. The ureters were then identified and mobilised using linear incisions in the medial leaf of the broad ligament, midway between the uterosacral ligaments and infundibulopelvic vessels The Multifire EndoGIA disposable surgical stapler was used to staple‐ligate and cut all uterine pedicles, each consisting of the round ligament, fallopian tubes and utero‐ovarian ligament, were cut. If the ovaries were to be removed, the stapler was instead placed outside the tube and ovary, encompassing the infundibulopelvic ligament. The uterine arteries were next staple‐ligated and cut bilaterally. If possible, the stapling device was also used to ligate and cut the cardinal ligaments. Otherwise, stapling of uterine pedicles ended and the anterior vaginal fornix was entered with unipolar cautery, incising over a moistened sponge distending the anterior vagina. The remainder of the hysterectomy was completed vaginally AH arm: modified Richardson technique Surgeon experience: not reported All received pre‐operative antibiotic prophylaxis (cefazolin 2 g) intravenously. If allergic to penicillin, 200 mg dose of doxycycline intravenously was used |
|
| Outcomes | Operating time; blood loss; intra‐operative and postoperative complications; hospital stay; febrile morbidity; requirement for analgesia; recovery time; conversion to abdominal hysterectomy and costs | |
| Notes | USA University of Tennessee, Memphis; Bowman Gray School of medicine, Winston‐Salem, North Carolina; University of North Carolina, Chapel Hill Funding: US Surgical Corporation, Norwalk, Connecticut USA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 women refused assigned procedure and were excluded from analysis No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | Unclear risk | Analysis not according to intention‐to‐treat
Surgeons' experience not reported Funding from pharmaceutical or surgical instrumentation company |
Tsai 2003.
| Methods | Single‐centre study, parallel‐group design Duration: August 1997 to March 1999 (1 year, 6 months) Randomisation: computer‐generated random number sequence Allocation procedure: not reported Blinding: no Number of women randomised = 200, number analysed = 200 Follow‐up: duration not specified Not analysed on intention‐to‐treat basis ‐ 2 LAVHs converted to AH analysed as AH No power calculation for sample size reported |
|
| Participants | 200 women with a mean age of 46.9 years (AH) and 46.7 years (LAVH) Inclusion criteria: good mobility of an enlarged uterus on bimanual pelvic examination Exclusion criteria: upper uterine margin higher than midpoint between symphysis pubis and umbilicus; pre‐existing cardiopulmonary dysfunction or poorly controlled systemic disease; cervical malignancy on colposcopy; indication for conventional VH | |
| Interventions | AH versus LH (LAVH)
AH technique: not specified
LAVH: under GA. Uterine manipulator applied and pneumoperitoneum established. 2 trocar puncture sites, 12 mm umbilically and 2 mm right lower quadrant. 2 mm minilaparoscope allowed inspection and treatment of endometriosis lesions or adhesions through umbilical port. Multifire EndoGIA stapler resection of round and utero‐ovarian ligaments (or bipolar forceps applied to round ligaments if large myoma present). Vaginal phase included insertion of 10 mm laparoscope after division of the vesicouterine fold and peritoneal entry (the LETS technique). Then standard VH technique, including clamping, transection and suture ligation of uterosacral, cardinal and uterine pedicles, followed by peritoneal closure, then laparoscopic re‐evaluation and lavage after haemostasis if necessary
Antibiotic and thrombo prophylaxis not specified Surgeons' experience: 2 attending doctors performed all hysterectomies, each with an experience of more than 50 laparoscopic procedures |
|
| Outcomes | Operating time; complications; duration of hospital stay | |
| Notes | Taiwan University and municipal hospital in Kaohsuing Funding not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts, loss to follow‐up unclear. Follow‐up period not specified |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined |
| Other bias | High risk | Analysis not according to intention‐to‐treat (with 2 conversions from LH to AH). No power calculation reported. Surgeons' experience not reported. AH technique not reported |
Yuen 1998.
| Methods | Single‐centre study, parallel‐group design Duration: January 1996 to June 1996 (6 months) Randomisation: computer‐generated sequence of random numbers Blinding: no Number of women randomised = 50, number analysed = 44. 4 declined the operation Follow‐up: until discharge from hospital. 2 refused to participate postoperatively No power calculation for sample size Analysis by intention‐to‐treat was reported |
|
| Participants | 44 women with a median age of 44 (LH(a) group) and 43 (AH group) Inclusion criteria: no major medical diseases requiring hysterectomy for benign disorders Exclusion criteria: suitable for VH or a uterus larger than 16 weeks' gravid size | |
| Interventions |
AH versus LH (LH(a))
LH(a) arm: performed with the use of 3 ports and bipolar desiccation for hemostasis. The laparoscopic part of the operation stopped after securing the uterine arteries, and the remainder of the operation was performed vaginally
AH arm: performed in the standard manner through a Pfannenstiel or lower midline incision Surgeon experience: not reported |
|
| Outcomes | Operation time; blood loss; postoperative stay and postoperative complications | |
| Notes | Hong Kong Chinese University Funding: direct grant for research from the Chinese University of Hong Kong |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4 dropouts were not analysed (4 declined the operation) and 2 lost to follow‐up (refused to participate postoperatively). This is 5% to 10% of the sample |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not defined. Dropouts were not analysed |
| Other bias | Low risk | No other bias identified |
Zhu 2009.
| Methods | Single‐centre Duration: 2004 to 2007 (3 years) Randomisation: not reported Allocation concealment: not reported Blinding: not reported Number of women: 101 women were randomised to 3 groups (34 LAVH, 35 TVH, 32 TAH). Dropouts not reported Follow‐up: duration not specified Power calculation for sample size: not reported |
|
| Participants | 69 women Inclusion criteria: patients of reproductive age and who had delivered at least 1 child. No adnexal disease, no gynaecological surgery history |
|
| Interventions |
TAH versus LAVH versus TVH TAH: performed utilising a standard technique LAVH: performed in a modified lithotomy position using a video‐monitor to record the laparoscopic part of the operation. A 10 mm scope was inserted subumbilically. Second and third entries were made suprapubically and on both sides. Round ligaments, tubes and utero‐ovarian ligaments were diathermy and cut. In some cases the adnexa were also removed and others were to be preserved. The uterovesical fold of the peritoneum was divided by scissors. The uterine artery and the partial cardinal and uterosacral ligament were diathermy and cut. The cervix was circumcised and the pouch of Douglas opened to allow ligation and division of the partial cardinal and uterosacral ligament, as in a traditional vaginal hysterectomy. No conversions Surgeons: 2 senior gynaecologists performed all operations |
|
| Outcomes | Operation time, blood loss, pain score (VAS), bowel recovery time, fever, postoperative morbidity, hospital stay | |
| Notes | China Peking Union Medical College hospital, Beijing Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropout not mentioned. From tables it seems that there was no loss to follow‐up, but follow‐up procedure was not specified |
| Selective reporting (reporting bias) | Unclear risk | Primary and secondary outcomes not defined |
| Other bias | High risk | Procedures really comparable as in 2 of the 3 groups salpingo‐oophorectomy was also performed. Pain score results must be interpreted with caution as different analgesics were used during the operation and postoperatively |
AAGL: American Association of Gynecologic Laparoscopists AH: abdominal hysterectomy aLH = laparoscopic cases in the abdominal arm of the eVALuate trial ASA: American Society of Anaesthesiologists BDI: Beck Depression Inventory BIS: Body Image Scale BMI: body mass index BSO: bilateral oophorectomy cLH: conventional laparoscopic hysterectomy CRP: C‐reactive protein CS: Cosmetic Scale DVT: deep vein thrombosis GA: general anaesthesia GIA: not an abbreviation; refers to a registered trademark (stapler device) HRQOL: health‐related quality of life HRT: hormone replacement therapy IL‐6: interleukin 6 ITU: intensive therapy unit IV: intravenous LAVH: laparoscopic‐assisted vaginal hysterectomy LAVHO: laparoscopy‐assisted vaginal hysterectomy with bilateral oophorectomy LH(a): hysterectomy where the procedure is done laparoscopically up to and including the uterine vessels and the remaining part vaginally NDVH: non‐descent vaginal hysterectomy NSAID: nonsteroidal anti‐inflammatory drug PGWB: Psychological General Well Being PID: pelvic inflammatory disease RALH: robot‐assisted laparoscopic hysterectomy SD: standard deviation SP: single‐port STAI: State‐Trait Anxiety Inventory TAH: Total Abdominal Hysterectomy TVH: Total Vaginal Hysterectomy TLH: total laparoscopic hysterectomy VAS: visual analogue scale VE: vaginal examination VH: vaginal hysterectomy VHO: vaginal hysterectomy with bilateral oophorectomy vLH: laparoscopic cases in the vaginal arm of the eVALuate trial WHO: World Health Organization WHQ: Women’s Health Questionnaire
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aka 2004 | Randomised trial comparing AH without colporrhaphy versus VH with colporrhaphy (n = 30). The complication profile for hysterectomy with colporrhaphy is different to hysterectomy without colporrhaphy. Inclusion of this trial and pooling for meta‐analysis would introduce undue clinical heterogeneity. Operation time was longer and hospital stay shorter in VH with colporrhaphy, compared with AH |
| Apoola 1998 | Non‐randomised comparison of VH and AH for women with moderately enlarged uterus. Women undergoing VH had less blood loss, a smaller haemoglobin drop and a shorter hospital stay |
| Atabekoglu 2004 | Randomised trial of LAVH versus AH (n = 46), but no intention‐to‐treat analysis. Authors did not measure any of our pre‐specified outcomes, focusing on tissue trauma (laboratory findings). There was one conversion to laparotomy in the laparoscopy group and a bladder lesions and a thrombophlebitis in the AH group. These patients were excluded from analysis. Lower CRP and CPK were found after LAVH |
| Cardone 2010 | Although presented as a randomised study, this was a comparison between a first sample of 100 patients treated with hysterectomy by laparotomy and a second sample of 100 patients treated with laparoscopic hysterectomy |
| Celik 2008 | There was not sufficient information available to decide that this was a randomised controlled study. Although in the discussion it was mentioned that this was a randomised study, this could not be confirmed in the description of the design of the study |
| Chapron 1999 | This study was not a randomised controlled study. Study assessed hysterectomy techniques and the rate of total laparoscopic hysterectomy (TLH) |
| Cucinella 2000 | Women included in another publication on the same outcome measures |
| Davies 1998 | There was not sufficient information available to decide that this was a randomised controlled study. No further data provided by author after request |
| Demir 2008 | Randomised trial of LH(a) (n = 15) versus TLH (n = 15) versus AH (n = 15) mainly focusing on tissue trauma by measuring IL‐6 and CRP. Lower values for both tissue trauma parameters were observed in LH(a) and TLH compared to AH 24 hours postoperatively |
| Drahonovsky 2006 | It appeared that only part of the collected data (i.e. 2 instead of 3 intervention groups) were reported in the study published in 2006, which was included in the 2009 update of this review. In a paper published in 2010, 3 intervention groups were reported, including the 2 described in the paper of 2006 and the missing third group. However, the study design (e.g. randomisation procedure) was insufficiently described to clarify this discrepancy. After requesting from the authors more information on the study design, we received too little information to assess the study for inclusion and exclusion criteria. Therefore, we excluded both papers from 2006 and 2010 from this review |
| Drahonovsky 2010 | See Drahonovsky 2006 |
| Dua 2012 | No comparison between routes of hysterectomy; women were randomised to have a drain or no drain after VH |
| Ellstrom 2003 | Randomised trial of TLH versus AH (n = 74), but did not measure any of our pre‐specified outcomes, focusing on psychological well being. No differences were found |
| Fanfani 2013 | This randomised controlled study was excluded because 40 out of 68 included patients had surgery for non‐benign indications. The data on the 28 patients with benign indications were not reported separately |
| Ghanbari 2009 | No comparison between different routes of hysterectomy; this randomised, double‐blind study compared 2 laparotomy techniques: transverse muscle‐cutting Maylard incision and the Pfannenstiel incision for AH |
| Hahlin 1994 | Women included in another publication on the same outcome measures |
| Holub 2000 | Randomised controlled trial (n = 70) but compared 2 variants of LAVH (described in the study as LAVH and VALH (vaginally assisted laparoscopic hysterectomy) respectively), rather than comparing LAVH with another surgical approach. In LAVH, the round ligament, upper broad ligament, infundibulopelvic or uteroovarian ligament, bladder pillars in preparation of the bladder flap were taken laparoscopically; the uterine vessels, cardinal‐uterosacral ligaments, anterior and posterior culdotomy and vaginal cuff closure were taken vaginally. In VALH, all steps were performed laparoscopically, other than taking the uterine vessels and vaginal cuff closure, which were performed vaginally. Operation time shorter for VALH (mean 81.33 versus 89.47 minutes, P value = 0.01), with no other significant differences in outcomes reported |
| Horng 2004 | Randomised controlled trial (n = 541) but compared 2 variants of colpotomy in LAVH (vaginal and laparoscopic approach), rather than comparing LAVH with another surgical approach. The vaginal approach was associated with significantly fewer urinary tract injuries as compared with the laparoscopic approach (9/274 and 1/267 respectively) |
| Howard 1993 | Not a randomised controlled study. Allocated to study groups based on the attending physician scheduled for the case. Intervention: laparoscopic hysterectomy (LH) versus abdominal hysterectomy (AH) |
| Kim 2010 | The study was excluded from the meta‐analysis because the primary outcome was on laboratory results and not on clinical data comparing routes of hysterectomy |
| Kucukozkan 2011 | No comparison between routes of hysterectomy; patient with large symptomatic myomas were randomised for an abdominal approach through minilaparotomy or midline incision |
| Lee 2011 | This study is a prospective case‐control study and not a RCT |
| Li 2012 | Not a true randomised trial; patients were assigned to receive single‐port TLH or conventional TLH according to the sequence of their admission |
| Long 2005 | Randomised controlled trial (n = 68) but compared 2 variants of LH(a) (with and without vaginal cuff suspension), rather than comparing LH(a) with another surgical approach. Less mobility of the bladder neck was found on ultrasound in LH(a) with suspension |
| Morelli 2007 | Case of scientific felony at Magna Graecia University of Catanzaro (via http://www.ncbi.nlm.nih.gov/pubmed/17923838) |
| Moustafa 2008 | No comparison between routes of hysterectomy; this randomised prospective study among women undergoing VH compared a closed vault technique with an open technique |
| Møller 2001 | This study was excluded from the review and meta‐analysis because this was not a randomised controlled study. Patients were allocated to study groups by the attending gynaecologist in a non‐randomised manner. Intervention: laparoscopic hysterectomy (LH) versus abdominal hysterectomy (AH) |
| Nezhat 1992 | Not a randomised controlled study, alternatively assigned to study groups. Intervention: laparoscopic hysterectomy (LH) versus abdominal hysterectomy (AH) |
| Oscarsson 2006 | Randomised trial comparing subtotal AH versus subtotal LH (n = 47). The complication profile for subtotal hysterectomy is different to total hysterectomy. Inclusion of this trial and pooling for meta‐analysis would introduce undue clinical heterogeneity. ASH was performed by Pfannenstiel incision and excision of the uterus in the cervical isthmus region after dissection of the uterine arteries LSH were performed by a 3‐port technique. Adnexal pedicles were dissected with bipolar coagulation and unipolar scissors. Uterine arteries were exposed prior to unipolar uterine dissection. Morcellation of the uterus with 20 mm automatic morcellator. Bipolar coagulation of the endocervical mucosa. Primary outcome: hospital stay Secondary outcomes: operation time, complications according to patient and physician, pain, pain medication, Foley catheter removal, return to fluid and food intake, return to normal activities and work, patient satisfaction Operation time was longer for subtotal LH, intra‐operative blood loss was higher for subtotal AH, VAS pain was higher for subtotal AH at 6 hours after surgery, return to work was sooner after subtotal LH. Other comparisons were not different |
| Pabuccu 1996 | No further data provided by author |
| Pan 2008 | Not a comparison of 2 different types of hysterectomy. In this study, 2 different techniques with regard to time point of coagulation of uterine vessels during LH(a) were compared |
| Park 2003 | This study was excluded in the review and meta‐analysis because this was not a randomised controlled study. Historical comparison of LAVH and TLH |
| Petrucco 1999 | No further data provided by author |
| Phipps 1993 | Not a truly randomised controlled study, allocated to study groups according to the last digit of their hospital record number by secretarial staff. Intervention: laparoscopic hysterectomy (LH) with bilateral salpingo‐oophorectomy (BSO) versus abdominal hysterectomy (AH) with BSO |
| Seow 2010 | No comparison between routes of hysterectomy; this randomised controlled study compared wound bleeding after injecting the colpotomy wound in LAVH with diluted vasopressin versus normal saline solution |
| Yue 2009 | The study was excluded from the meta‐analysis because the primary outcome was on laboratory results and not on clinical data comparing routes of hysterectomy |
AH: abdominal hysterectomy ASH: subtotal abdominal hysterectomy CPK: creatine phosphokinase CRP: C‐reactive protein IL‐6: interleukin 6 LAVH: laparoscopic‐assisted vaginal hysterectomy LH: laparoscopic hysterectomy LSH: subtotal laparoscopic hysterectomy RCT: randomised controlled trial TLH: total laparoscopic hysterectomy VALH: vaginally assisted laparoscopic hysterectomy VAS: visual analogue scale VH: vaginal hysterectomy
Characteristics of studies awaiting assessment [ordered by study ID]
Sesti 2014.
| Methods | Randomisation procedure was based on a computer‐generated list |
| Participants | 108 women requiring hysterectomy for enlarged myomatous uterus |
| Interventions | 3 treatment arms: TLH (n = 36); LAVH (n = 36); VH (n = 36) |
| Outcomes | The primary outcome was the discharge time comparison. The secondary outcomes were operating time, blood loss, paralytic ileus time, intraoperative complications, postoperative pain and early postoperative complications |
| Notes | Results: the mean discharge time was shorter after VH than after LAVH and TLH (P value = 0.001). Operating time significantly influenced the discharge time, considered as a dependent variable in general linear model analysis (P value = 0.006). In contrast, blood loss did not influence the discharge time (P value = 0.55). The mean operating time was significantly shorter in VH than in TLH and LAVH groups (P value = 0.000). The intraoperative blood loss was greater during LAVH than during TLH and VH (P value = 0.000). Paralytic ileus time was shorter after VH than after TLH and LAVH (P value = 0.000). No intraoperative complications or conversions to laparotomy occurred |
LAVH: laparoscopic‐assisted vaginal hysterectomy TLH: total laparoscopic hysterectomy VH: vaginal hysterectomy
Differences between protocol and review
Three new types of intervention have been included in the review, as they emerged as new approaches to hysterectomy in randomised controlled trials, i.e. robot‐assisted hysterectomy, mini laparoscopic hysterectomy and single‐port laparoscopic hysterectomy.
Haemoglobin or haematocrit drop has been removed from the list of secondary outcomes.
Contributions of authors
Johanna WM Aarts: selected trials and extracted data for the current update, data entry, wrote current update of the review. Theodoor E Nieboer: selected trials and extracted data for the current update, data entry, wrote current update of the review. Neil Johnson: conceptualised the first review, wrote the protocol and the review, having supervised the selection of trials and data extraction, and commented on the current update. Emma Tavender: trial selection, data extraction, trial quality assessment, data entry, wrote part of the description of studies and the methodological quality of included studies sections in the first review. Commented on the current update. Ray Garry: assisted with data extraction and interpretation, commented on the protocol and the current update. Ben Willem Mol: assisted with data extraction and interpretation, wrote the current update. Kirsten Kluivers: selected trials and extracted data for the current update, data entry, wrote and supervised the current update of the review.
Sources of support
Internal sources
No internal source of support, Other.
External sources
No external source of support, Other.
Declarations of interest
Ray Garry is the principal investigator in a UK‐based multicentre randomised trial comparing laparoscopic with both abdominal and vaginal hysterectomy (Garry 2004).
Neil Johnson is involved in fertility and endometriosis research with the University of Auckland, has a public hospital appointment at Auckland District Health Board, and has private appointments with private medical practice groups called Endometriosis Auckland and IVF Auckland (with whom he is a shareholder); Neil Johnson has accepted funding towards conference expenses and research meetings from the following industry sponsors within the last five years, none of these sums being greater than USD 5000: Organon, Serono, Schering and Device Technologies.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Agostini 2006 {published data only}
- Agostini A, Vejux N, Bretelle F, Collette E, Lapparent T, Cravello L, et al. Value of laparoscopic assistance for vaginal hysterectomy with prophylactic bilateral oophorectomy. American Journal of Obstetrics and Gynecology 2006;194(2):351‐4. [DOI] [PubMed] [Google Scholar]
Benassi 2002 {published data only}
- Benassi L, Rossi T, Kaihura CT, Ricci L, Bedocchi L, Galanti B. Abdominal or vaginal hysterectomy for enlarged uteri: a randomized clinical trial. American Journal of Obstetrics and Gynecology 2002;187:1561‐5. [DOI] [PubMed] [Google Scholar]
Candiani 2009 {published data only}
- Candiani M, Izzo S, Bulfoni A, Riparini J, Ronzoni S, Marconi A. Laparoscopic vs vaginal hysterectomy for benign pathology. American Journal of Obstetrics & Gynecology 2009;200(4):368.e1‐7. [DOI] [PubMed] [Google Scholar]
Chakraborty 2011 {published data only}
- Chakraborty S, Goswami S, Mukherjee P, Sau M. Hysterectomy..... Which route?. Journal of Obstetrics and Gynecology of India 2011;61(5):554‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2011 {published data only}
- Chen YJ, Wang PH, Ocampo EJ, Twu NF, Yen MS, Chao KC. Single‐port compared with conventional laparoscopic‐assisted vaginal hysterectomy. Obstetrics & Gynecology 2011;117(4):906‐12. [DOI] [PubMed] [Google Scholar]
Darai 2001 {published data only}
- Darai E, Kimtata P, Place C, Lecuru F. Vaginal hysterectomy versus laparoscopically assisted hysterectomy for enlarged uterus: a prospective randomized study. Gynaecological Endoscopy Supplement: 9th Congress of the European Society for Gynaecological Endoscopy. Paris, 2000:5.
- Darai E, Soriano D, Kimata P, Laplace C, Lecuru F. Vaginal hysterectomy for enlarged uteri, with or without laparoscopic assistance: randomized study. Obstetrics and Gynecology 2001;97(5):712‐6. [PubMed] [Google Scholar]
Ellstrom 1998 {published data only}
- Ellstrøm M, Olsen MF, Olsson J‐H, Nordberg G, Bengtsson A, Hahlin M. Pain and pulmonary function following laparoscopic and abdominal hysterectomy: a randomized study. Acta Obstetricia et Gynecologica Scandinavica 1998;77:923‐8. [PubMed] [Google Scholar]
Falcone 1999 {published data only}
- Falcone T, Paraiso MFR, Mascha E. Prospective randomized clinical trial of laparoscopically assisted vaginal hysterectomy versus total abdominal hysterectomy. American Journal of Obstetrics & Gynecology 1999;180:955‐62. [DOI] [PubMed] [Google Scholar]
Ferrari 2000 {published data only}
- Ferrari MM, Berlanda N, Mezzopane R, Ragusa G, Cavallo M, Pardi G. Identifying the indications for laparoscopically assisted vaginal hysterectomy: a prospective, randomised comparison with abdominal hysterectomy in patients with symptomatic uterine fibroids. British Journal of Obstetrics and Gynaecology 2000;107:620‐5. [DOI] [PubMed] [Google Scholar]
Garry 2004 {published data only}
- Garry R, Fountain J, Mason S, Napp V, Brown J, Hawe J, et al. The eVALuate study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ 2004;328(7432):129‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sculpher M, Manca A, Abbott J, Fountain J, Mason S, Garry R. Cost effectiveness analysis of laparoscopic hysterectomy compared with standard hysterectomy: results from a randomised trial. BMJ 2004;328(7432):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghezzi 2010 {published data only}
- Ghezzi F, Uccella S, Cromi A, Siesto G, Serati M, Bogani G, et al. Postoperative pain after laparoscopic and vaginal hysterectomy for benign gynecologic disease: a randomized trial. American Journal of Obstetrics and Gynecology 2010;203(2):e1‐8. [DOI] [PubMed] [Google Scholar]
Ghezzi 2011 {published data only}
- Ghezzi F, Cromi A, Siesto G, Uccella S, Boni L, Serati M, et al. Minilaparoscopic versus conventional laparoscopic hysterectomy: results of a randomized trial. Journal of Minimally Invasive Gynecology 2011;18(4):455‐61. [DOI] [PubMed] [Google Scholar]
Harkki‐Siren 2000 {published data only}
- Härkki‐Sirén P, Sjöberg J, Toivonen J, Tiitinen A. Clinical outcome and tissue trauma after laparoscopic and abdominal hysterectomy: a randomized controlled study. Acta Obstetricia et Gynecologica Scandinavica 2000;79:866‐71. [PubMed] [Google Scholar]
Hwang 2002 {published data only}
- Hwang J‐L, Seow K‐M, Tsai Y‐L, Huang L‐W, Hsieh B‐C, Lee C. Comparative study of vaginal, laparoscopically assisted vaginal and abdominal hysterectomies for uterine myoma larger than 6cm in diameter or uterus weighing at least 450g: a prospective randomized study. Acta Obstetricia et Gynecologica Scandinavica 2002;81:1132‐8. [DOI] [PubMed] [Google Scholar]
Jung 2011 {published data only}
- Jung YW, Lee M, Yim GW, Lee SH, Paek JH, Kwon HY, et al. A randomized prospective study of single‐port and four‐port approaches for hysterectomy in terms of postoperative pain. Surgical Endoscopy 2011;25(8):2462‐9. [DOI: 10.1007/s00464-010-1567-z] [DOI] [PubMed] [Google Scholar]
Kluivers 2007 {published data only}
- Kluivers KB, Hendriks JCM, Mol BWJ, Bongers MY, Bremer GL, Vet HCW, et al. Quality of life and surgical outcome after total laparoscopic hysterectomy versus total abdominal hysterectomy for benign disease: a randomized, controlled trial. Journal of Minimally Invasive Gynecology 2007;14(2):145‐52. [DOI] [PubMed] [Google Scholar]
- Nieboer TE, Hendriks JC, Bongers MY, Vierhout ME, Kluivers KB. Quality of life after laparoscopic and abdominal hysterectomy: a randomized controlled trial. Obstetrics & Gynecology 2012;119(1):85‐91. [DOI] [PubMed] [Google Scholar]
Kongwattanakul 2012 {published data only}
- Kongwattanakul K, Khampitak K. Comparison of laparoscopically assisted vaginal hysterectomy and abdominal hysterectomy: a randomized controlled trial. Journal of Minimally Invasive Gynecology 2012;19(1):89‐94. [DOI] [PubMed] [Google Scholar]
Kunz 1996 {published data only}
- Kunz G, Plath T, Leyendecker G. Comparison between laparoscopic assisted vaginal hysterectomy (LAVH) and abdominal hysterectomy. Geburtshilfe und Frauenheilkunde 1996;56:453‐7. [DOI] [PubMed] [Google Scholar]
Langebrekke 1996 {published data only}
- Langebrekke A, Eraker R, Nesheim BI, Urnes A, Busund B, Sponland G. Abdominal hysterectomy should not be considered as a primary method for uterine removal ‐ a prospective randomised study of 100 patients referred to hysterectomy. Acta Obstetrica et Gyanecologica Scandinavica 1996;75:404‐7. [DOI] [PubMed] [Google Scholar]
Long 2002 {published data only}
- Long CY, Fang JH, Chen WC, Su JH, Hsu SC. Comparison of total laparoscopic hysterectomy and laparoscopically assisted vaginal hysterectomy. Gynecologic and Obstetric Investigation 2002;53:214‐9. [DOI] [PubMed] [Google Scholar]
Lumsden 2000 {published data only}
- Lumsden MA, Twaddle S, Hawthorn R, Traynor I, Gilmore D, Davis J, et al. A randomised comparison and economic evaluation of laparoscopic‐assisted hysterectomy and abdominal hysterectomy. British Journal Obstetrics and Gynecology 2000;107:1386‐91. [DOI] [PubMed] [Google Scholar]
Marana 1999 {published data only}
- Marana R, Busacca M, Zupi E, Garcea N, Paparella P, Catalano GF. Laparoscopically assisted vaginal hysterectomy versus total abdominal hysterectomy: a prospective, randomized, multicenter study. American Journal of Obstetrics and Gynecology 1999;180:270‐5. [DOI] [PubMed] [Google Scholar]
Miskry 2003 {published data only}
- Miskry T. Randomised, prospective, double‐blind comparison of abdominal versus vaginal hysterectomy. XVI FIGO World Congress Abstract Book 3. Washington DC, 2000:44.
- Miskry T, Magos A. Randomized, prospective, double‐blind comparison of abdominal and vaginal hysterectomy in women without uterovaginal prolapse. Acta Obstetricia et Gynaecologica Scandinavica 2003;82:351‐8. [DOI] [PubMed] [Google Scholar]
Muzii 2007 {published data only}
- Muzii L, Basile S, Zupi E, Marconi D, Zullo MA, Manci N, et al. Laparoscopic‐assisted vaginal hysterectomy versus minilaparotomy hysterectomy: a prospective, randomized, multicenter study. Journal of Minimally Invasive Gynecology 2007;14(5):610‐5. [DOI] [PubMed] [Google Scholar]
Olsson 1996 {published data only}
- Olsson J‐H, Ellstrøm M, Hahlin M. A randomised prospective trial comparing laparoscopic and abdominal hysterectomy. British Journal of Obstetrics and Gynaecology 1996;103:345‐50. [DOI] [PubMed] [Google Scholar]
Ottosen 2000 {published data only}
- Ottosen C, Lingman G, Ottosen L. Three methods for hysterectomy: a randomised, prospective study of short term outcome. British Journal of Obstetrics and Gynaecology 2000;107:1380‐5. [DOI] [PubMed] [Google Scholar]
Paraiso 2013 {published data only}
- Paraiso MFR, Ridgeway B, Park AJ, Jelovsek JE, Barber MD, Falcone T, et al. A randomized trial comparing conventional and robotically assisted total laparoscopic hysterectomy. American Journal of Obstetrics & Gynecology 2013;208:e1‐7. [DOI] [PubMed] [Google Scholar]
Perino 1999 {published data only}
- Perino A, Cucinella G, Venezia R, Castelli A, Cittadini E. Total laparoscopic hysterectomy versus total abdominal hysterectomy: an assessment of the learning curve in a prospective randomized study. Human Reproduction 1999;14:2996‐9. [DOI] [PubMed] [Google Scholar]
Persson 2006 {published data only}
- Persson P, Kjolhede P. Factors associated with postoperative recovery after laparoscopic and abdominal hysterectomy. European Journal of Obstetrics & Gynecology and Reproductive Biology 2008;140:108‐13. [DOI] [PubMed] [Google Scholar]
- Persson P, Wijma K, Hammar M, Kjolhede P. Psychological well being after laparoscopic and abdominal hysterectomy ‐ a randomised controlled multicentre study. British Journal of Obstetrics and Gynecology 2006;113:1023‐30. [DOI] [PubMed] [Google Scholar]
Raju 1994 {published data only}
- Raju KS, Auld BJ. A randomised prospective study of laparoscopic vaginal hysterectomy versus abdominal hysterectomy each with bilateral salpingo‐oophorectomy. British Journal of Obstetrics & Gynaecology 1994;101:1068‐71. [DOI] [PubMed] [Google Scholar]
Ribeiro 2003 {published data only}
- Ribeiro SC, Ribeiro RM, Santos NC, Pinotti JA. A randomized study of total abdominal, vaginal and laparoscopic hysterectomy. International Journal of Gynecology and Obstetrics 2003;83:37‐43. [DOI] [PubMed] [Google Scholar]
Richardson 1995 {published data only}
- Richardson RE, Bournas N, Magos AL. Is laparoscopic hysterectomy a waste of time?. Lancet 1995;345:36‐41. [DOI] [PubMed] [Google Scholar]
Roy 2011 {published data only}
- Roy KK, Goyal M, Singla S, Sharma JB, Malhotra N, Kumar S. A prospective randomised study of total laparoscopic hysterectomy, laparoscopically assisted vaginal hysterectomy and non‐descent vaginal hysterectomy for the treatment of benign diseases of the uterus. Archives of Gynecology and Obstetrics 2011;284(4):907‐12. [DOI] [PubMed] [Google Scholar]
Roy 2012 {published data only}
- Roy KK, Subbaiah M, Singla S, Kumar S, Sharma JB, Mitra DK. Role of serum interleukin‐6 in comparing surgical stress after laparoscopic‐assisted vaginal hysterectomy and non‐descent vaginal hysterectomy for large uteri. Archives of Gynecology and Obstetrics 2012;285(3):671‐6. [DOI] [PubMed] [Google Scholar]
Sarlos 2012 {published data only}
- Sarlos D, Kots L, Stevanovic N, Felten S, Schär G. Robotic compared with conventional laparoscopic hysterectomy: a randomized controlled trial. Obstetrics & Gynecology 2012;120(3):604‐11. [DOI] [PubMed] [Google Scholar]
Schutz 2002 {published data only}
- Schutz K, Possover M, Merker A, Michels A, Schneider A. Prospective randomized comparison of laparoscopic‐assisted vaginal hysterectomy (LAVH) with abdominal hysterectomy (AH) for the treatment of the uterus weighing >200g. Surgical Endoscopy 2002;16:121‐5. [DOI] [PubMed] [Google Scholar]
Seracchioli 2002 {published data only}
- Seracchioli R, Venturoli S, Vianello F, Govoni F, Cantarelli M, Gualerzi B, et al. Total laparoscopic hysterectomy compared with abdominal hysterectomy in the presence of a large uterus. Journal of the American Association of Gynecologic Laparoscopists 2002;9(3):333‐8. [DOI] [PubMed] [Google Scholar]
Sesti 2008a {published data only}
- Sesti F, Calonzi F, Ruggeri V, Pietropoli A, Piccione E. A comparison of vaginal, laparoscopic‐assisted vaginal, and minilaparotomy hysterectomies for enlarged myomatous uteri. International Journal of Gynecology and Obstetrics 2008;103:227‐31. [DOI] [PubMed] [Google Scholar]
Sesti 2008b {published data only}
- Sesti F, Ruggeri V, Pietropolli A, Piccione E. Laparoscopically assisted vaginal hysterectomy versus vaginal hysterectomy for enlarged uterus. Journal of the Society of Laparoendoscopic Surgeons 2008;12:246‐51. [PMC free article] [PubMed] [Google Scholar]
Silva Filho 2006 {published data only}
- Silva‐Filho AL, Werneck RA, Magalhaes RS, Belo AV, Triginelli SA. Abdominal vs vaginal hysterectomy: a comparative study of postoperative quality of life and satisfaction. Archives of Gynecology and Obstetrics 2006;274(1):21‐4. [DOI] [PubMed] [Google Scholar]
Song 2013 {published data only}
- Song T, Cho J, Kim TJ, Kim IR, Hahm TS, Kim BG, et al. Cosmetic outcomes of laparoendoscopic single‐site hysterectomy compared with multi‐port surgery: randomized controlled trial. Journal of Minimally Invasive Gynecology 2013;20(4):460‐7. [DOI: 10.1016/j.jmig.2013.01.010] [DOI] [PubMed] [Google Scholar]
Soriano 2001 {published data only}
- Soriano D, Goldstein A, Lecuru F, Darai E. Recovery from vaginal hysterectomy compared with laparoscopy‐assisted hysterectomy: a prospective, randomized, multicenter study. Acta Obstetrica et Gynaecologica Scandinavica 2001;80:337‐41. [PubMed] [Google Scholar]
Summitt 1992 {published data only}
- Summitt RLJr, Stovall TG, Lipscomb GH, Ling FW. Randomized comparison of laparoscopy‐assisted vaginal hysterectomy with standard vaginal hysterectomy in an outpatient setting. Obstetrics and Gynecology 1992;80:895‐901. [PubMed] [Google Scholar]
Summitt 1998 {published data only}
- Summitt RLJr, Stovall TG, Steege JF, Lipscomb GH. A multicenter randomized comparison of laparoscopically assisted vaginal hysterectomy and abdominal hysterectomy in abdominal hysterectomy candidates. Obstetrics and Gynecology 1998;92:321‐6. [PubMed] [Google Scholar]
Tsai 2003 {published data only}
- Tsai EM, Chen HS, Long CY, Yang CH, Hsu SC, Wu CH, et al. Laparoscopically assisted vaginal hysterectomy versus total abdominal hysterectomy: a study of 100 cases on light‐endorsed transvaginal section. Gynecologic and Obstetric Investigation 2003;55:105‐9. [DOI] [PubMed] [Google Scholar]
Yuen 1998 {published data only}
- Yuen PM, Mak TWL, Yim SF, Ngan Kee WD, Lam CWK, Rogers MS, et al. Metabolic and inflammatory responses after laparoscopic and abdominal hysterectomy. American Journal of Obstetrics and Gynecology 1998;179:1‐5. [DOI] [PubMed] [Google Scholar]
Zhu 2009 {published data only}
- Zhu L, Lang JH, Liu CY, Shi HH, Sun ZJ, Fan R. Clinical assessment for three routes of hysterectomy. Chinese Medical Journal 2009;122(4):377‐80. [PubMed] [Google Scholar]
References to studies excluded from this review
Aka 2004 {published data only}
- Aka N, Köse G, Gönenc I, Api M. Tissue trauma after vaginal hysterectomy and colporrhaphy versus abdominal hysterectomy: a randomised controlled study. Australian and New Zealand Journal of Obstetrics and Gynaecology 2004;44:328‐31. [DOI] [PubMed] [Google Scholar]
Apoola 1998 {published data only}
- Apoola A, Hefni MA. Hysterectomy for moderately enlarged uterus: abdominal versus vaginal hysterectomy. Journal of Obstetrics and Gynaecology 1998;18:375‐6. [DOI] [PubMed] [Google Scholar]
Atabekoglu 2004 {published data only}
- Atabekoglu C, Sönmezer M, Güngör M, Aytaç R, Ortaç F, Unlü C. Tissue trauma in abdominal and laparoscopic‐assisted vaginal hysterectomy. Journal of the American Association Gynaecological Laparoscopists 2004;11(1):467‐72. [DOI] [PubMed] [Google Scholar]
Cardone 2010 {published data only}
- Cardone A, Zarcone R, Giardiello M. Comparison of 100 of hysterectomy laparoscopic against 100 cases hysterectomy laparotomy. Minerva Ginecologica 2010;62(3):171‐7. [PubMed] [Google Scholar]
Celik 2008 {published data only}
- Celik H, Gurates B, Yavuz A, Nurkalem C, Hanay F, Kavak B. The effect of hysterectomy and bilaterally salpingo‐oophorectomy on sexual function in post‐menopausal women. Maturitas 2008;61:358‐63. [DOI] [PubMed] [Google Scholar]
Chapron 1999 {published data only}
- Chapron C, Laforest L, Ansquer Y, Fauconnier A, Fernandez B, Breart G, et al. Hysterectomy techniques used for benign pathologies: results of a French multicentre study. Human Reproduction 1999;14(10):2464‐70. [DOI] [PubMed] [Google Scholar]
Cucinella 2000 {published data only (unpublished sought but not used)}
- Cucinella G, Gugliotta G, Adile B. Total laparoscopic hysterectomy versus total abdominal hysterectomy: a confront of 100 versus 101 cases in prospective randomized study. XVI FIGO World Congress Abstract Book 3. Washington DC. 2000:45.
Davies 1998 {published data only (unpublished sought but not used)}
- Davies A. Randomized controlled trial comparing oophorectomy at vaginal and laparoscopically assisted vaginal hysterectomy. In: British Journal of Obstetrics and Gynaecology, poster abstract 1998.
Demir 2008 {published data only}
- Demir A, Bige O, Saatli B, Solak A, Saygili U, Önvural A. Prospective comparison of tissue trauma after laparoscopic hysterectomy types with retroperitoneal lateral transsection of uterine vessels using ligasure and abdominal hysterectomy. Archives of Gynecology and Obstetrics 2008;277:325‐30. [DOI] [PubMed] [Google Scholar]
Drahonovsky 2006 {published data only}
- Drahonovsky J, Pan M, Baresova S, Kucera E, Feyereisl J. Clinical comparison of laparoscopy‐assisted vaginal hysterectomy (LAVH) and total laparoscopy hysterectomy (TLH) in women with benign disease of uterus ‐ a prospective randomized study [Klinické srovnání laparoskopicky asistované vaginální hysterektomie (LAVH) a totální laparoskopické hysterektomie (TLH) u zen s benigním onemocnemím delohy ‐ prospektivní randomizovaná studie]. Ceska Gynekologie 2006;71(6):431‐7. [PubMed] [Google Scholar]
Drahonovsky 2010 {published data only}
- Drahonovsky J, Haakova L, Otcenasek M, Krofta L, Kucera E, Feyereisl J. A prospective randomized comparison of vaginal hysterectomy, laparoscopically assisted vaginal hysterectomy, and total laparoscopic hysterectomy in women with benign uterine disease. European Journal of Obstetrics & Gynecology and Reproductive Biology 2010;148:172‐6. [DOI] [PubMed] [Google Scholar]
Dua 2012 {published data only}
- Dua A, Galimberti A, Subramaniam M, Popli G, Radley S. The effects of vault drainage on postoperative morbidity after vaginal hysterectomy for benign gynaecological disease: a randomised controlled trial. BJOG 2012;119(3):348‐53. [DOI] [PubMed] [Google Scholar]
Ellstrom 2003 {published data only}
- Ellstrom MA, Astrom M, Moller A, Olsson JH, Hahlin M. A randomized trial comparing changes in psychological well‐being and sexuality after laparoscopic and abdominal hysterectomy. Acta Obstetrica et Gynaecologica Scandinavica 2003;82:871‐5. [DOI] [PubMed] [Google Scholar]
Fanfani 2013 {published data only}
- Fanfani F, Fagotti A, Gagliardi ML, Monterossi G, Rossitto C, Costantini B, et al. Minilaparoscopic versus single‐port total hysterectomy: a randomized trial. Journal of Minimally Invasive Gynecology 2013;20(2):192‐7. [DOI] [PubMed] [Google Scholar]
Ghanbari 2009 {published data only}
- Ghanbari Z, Baratali BH, Foroughifar T, Pesikhani MD, Shariat M. Pfannenstiel versus Maylard incision for gynecologic surgery: a randomized, double‐blind controlled trial. Taiwanese Journal of Obstetrics & Gynecology 2009;48(2):120‐3. [DOI] [PubMed] [Google Scholar]
Hahlin 1994 {published data only}
- Hahlin M, Ellstrom M, Olsson JH. Laparoscopic hysterectomy. Further knowledge of advantages and disadvantages is necessary. Lakartidningen 1994;91:220‐2. [PubMed] [Google Scholar]
Holub 2000 {published data only}
- Holub Z, Jabor A, Kliment L, Voracek J, Lukac J. Comparison of two procedures for laparovaginal hysterectomy: a randomized trial. European Journal of Obstetrics and Gynecology 2000;90:31‐6. [DOI] [PubMed] [Google Scholar]
Horng 2004 {published data only}
- Horng SG, Huang KG, Lo TS, Soong YK. Bladder injury after LAVH: a prospective, randomized comparison of vaginal and laparoscopic approaches to colpotomy during LAVH. Journal of the American Association of Gynaecologic Laparoscopists 2004;11(1):42‐6. [DOI] [PubMed] [Google Scholar]
Howard 1993 {published data only}
- Howard FM, Sanchez R. A comparison of laparoscopically assisted vaginal hysterectomy and abdominal hysterectomy. Journal of Gynecologic Surgery 1993;9(2):83‐9. [DOI] [PubMed] [Google Scholar]
Kim 2010 {published data only}
- Kim TK, Yoon JR. Comparison of the neuroendocrine and inflammatory responses after laparoscopic and abdominal hysterectomy. Korean Journal of Anesthesiology 2010;59(4):265‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kucukozkan 2011 {published data only}
- Kucukozkan T, Ozkaya E, Ucar FO, Kara OF. Hysterectomy for large symptomatic myomas: minilaparotomy versus midline vertical incision. Archives of Gynecology and Obstetrics 2011;284(2):421‐5. [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee JH, Choi JS, Hong JH, Joo KJ, Kim BY. Does conventional or single port laparoscopically assisted vaginal hysterectomy affect female sexual function?. Acta Obstetricia et Gynecologica Scandinavica 2011;90(12):1410‐5. [DOI] [PubMed] [Google Scholar]
Li 2012 {published data only}
- Li M, Han Y, Feng YC. Single‐port laparoscopic hysterectomy versus conventional laparoscopic hysterectomy: a prospective randomized trial. Journal of International Medical Research 2012;40(2):701‐8. [DOI] [PubMed] [Google Scholar]
Long 2005 {published data only}
- Long CY, Liu CM, Wu TP, Hsu SC, Chang Y, Tsai EM. A randomized comparison of vesicourethral function after laparoscopic hysterectomy with and without vaginal cuff suspension. Journal of Minimally Invasive Gynecology 2005;12(2):137‐43. [DOI] [PubMed] [Google Scholar]
Morelli 2007 {published data only}
- Morelli M, Caruso M, Noia R, Chiodo D, Cosco C, Lucia E, et al. Total laparoscopic hysterectomy versus vaginal hysterectomy: a prospective randomized trial. Minerva Ginecologica 2007;59(2):99‐105. [PubMed] [Google Scholar]
Moustafa 2008 {published data only}
- Moustafa M, Elgonaid WE, Massouh H, Beynon WG. Evaluation of closure versus non‐closure of vaginal vault after vaginal hysterectomy. Journal of Obstetrics and Gynaecology 2008;28(8):791‐4. [DOI] [PubMed] [Google Scholar]
Møller 2001 {published data only}
- Moeller C, Kehlet H, Schouenborg L, Ottensen B, Friland S, Lund C. Fast track hysterectomy. XVI FIGO World Congress Abstract Book 3. Washington DC, 2000:46.
- Møller C, Kehlet H, Friland SG, Schouenborg LO, Lund C, Ottesen B. Fast track hysterectomy. European Journal of Obstetrics & Gynecology and Reproductive Biology 2001;98:18‐22. [DOI] [PubMed] [Google Scholar]
Nezhat 1992 {published data only}
- Nezhat F, Nezhat C, Gordon S, Wilkins E. Laparoscopic versus abdominal hysterectomy. Journal of Reproductive Medicine 1992;37(3):247‐50. [PubMed] [Google Scholar]
Oscarsson 2006 {published data only}
- Oscarsson U, Poromaa IS, Nussler E, Lofgren M. No difference in length of hospital stay between laparoscopic and abdominal supravaginal hysterectomy‐‐a preliminary study. Acta Obstetricia et Gynecologica Scandinavica 2006;85:682‐3. [DOI] [PubMed] [Google Scholar]
Pabuccu 1996 {published data only (unpublished sought but not used)}
- Pabuccu R, Atay V, Ergun A, Duru NK, Orhon E, Yenen MC. Laparoscopic assisted vaginal hysterectomy results. In: Human Reproduction: Abstracts of the 12th Annual Meeting of ESHRE. Maastricht 1996;11:235‐6. [Google Scholar]
Pan 2008 {published data only}
- Pan HS, Ko ML, Huang LW, Chang JZ, Hwang JL, Chen SC. Total laparoscopic hysterectomy (TLH) versus coagulation of uterine arteries (CUA) at their origin plus total laparoscopic hysterectomy (TLH) for the management of myoma and adenomyosis. Minimally Invasive Therapy 2008;17:318‐22. [DOI] [PubMed] [Google Scholar]
Park 2003 {published data only}
- Park NH, Kim JW, Seo CS, Kim SH, Song YS, Kang SB, et al. Comparison of two laparoscopic methods of hysterectomy. International Journal of Obstetrics and Gynecology 2003;83(Suppl 3):79. [Google Scholar]
Petrucco 1999 {published data only (unpublished sought but not used)}
- Petrucco OM, Luke C, Moss J, Healy D. Randomized prospective trial comparing laparoscopic assisted vaginal and abdominal hysterectomy. IX Annual Scientific Meeting of the Australian Gynaecological Endoscopic Society Abstracts. 1999:75.
Phipps 1993 {published data only}
- Phipps JH, John M, Nayak S. Comparison of laparoscopically assisted vaginal hysterectomy and bilateral salpingo‐ophorectomy with conventional abdominal hysterectomy and bilateral salpingo‐ophorectomy. British Journal of Obstetrics and Gynaecology 1993;100:698‐700. [DOI] [PubMed] [Google Scholar]
Seow 2010 {published data only}
- Seow KM, Lin YH, Hwang JL, Huang LW, Pan CP. A simple procedure to prevent chronic vaginal colpotomy wound bleeding after laparoscopically assisted vaginal hysterectomy. International Journal of Gynaecology and Obstetrics 2010;1091(1):49‐51. [DOI] [PubMed] [Google Scholar]
Yue 2009 {published data only}
- Yue Q, Ma R, Mao DW, Dong TJ, Sun L, Geng XX, et al. Effects of laparoscopically‐assisted vaginal hysterectomy compared with abdominal hysterectomy on immune function. Journal of International Medical Research 2009;37(3):855‐61. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Sesti 2014 {published data only}
- Sesti F, Cosi V, Calonzi F, Ruggeri V, Pietropolli A, Francesco L, et al. Randomized comparison of total laparoscopic, laparoscopically assisted vaginal and vaginal hysterectomies for myomatous uteri. Archives of Gynecology and Obstetrics 2014;290(3):485‐91. [DOI: 10.1007/s00404-014-3228-2] [DOI] [PubMed] [Google Scholar]
Additional references
ACOG 2009
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 444. Choosing the Route of Hysterectomy for Benign Disease. Obstetrics & Gynecology 2009;114(5):1156–8. [DOI] [PubMed] [Google Scholar]
Agostini 2005
- Agostini A, Vejux N, Colette E, Bretelle F, Cravello L, Blanc B. Risk of bladder injury during vaginal hysterectomy in women with a previous cesarean section. Journal of Reproductive Medicine 2005;50(12):940‐2. [PubMed] [Google Scholar]
Bijen 2009
- Bijen CB, Vermeulen KM, Mourits MJ, Bock GH. Costs and effects of abdominal versus laparoscopic hysterectomy: systematic review of controlled trials. PLoS One 2009;4(10):e7340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brummer 2008
- Brummer TH, Seppälä TT, Härkki PS. National learning curve for laparoscopic hysterectomy and trend in hysterectomy in Finland 2000‐2005. Human Reproduction 2008;23(4):840‐5. [DOI] [PubMed] [Google Scholar]
Brummer 2011
- Brummer TH, Jalkanen J, Fraser J, Heikkinen AM, Kauko M, Mäkinen J, et al. FINHYST, a prospective study of 5279 hysterectomies: complications and their risk factors. Human Reproduction 2011;26(7):1741‐51. [DOI] [PubMed] [Google Scholar]
Dawson 2010
- Dawson J, Doll H, Fitzpatrick R, Jenkinson C, Carr AJ. The routine use of patient reported outcome measures in healthcare settings. BMJ 2010;340:c186. [DOI] [PubMed] [Google Scholar]
Ellstrom 1998b
- Ellstrøm M, Ferraz‐Nunes J, Hahlin M, Olsson J‐H. A randomized trial with a cost‐consequence analysis after laparoscopic and abdominal hysterectomy. Obstetrics and Gynecology 1998;91:30‐4. [DOI] [PubMed] [Google Scholar]
Flory 2005
- Flory N, Bissonnette F, Binik YM. Psychosocial effects of hysterectomy: literature review. Journal of Psychosomatic Research 2005;59(3):117‐29. [DOI] [PubMed] [Google Scholar]
Garry 1994
- Garry R, Reich H, Liu CY. Laparoscopic hysterectomy ‐ definitions and indications. Gynaecological Endoscopy 1994;3:1‐3. [Google Scholar]
Garry 1995
- Garry R, Phillips G. How safe is the laparoscopic approach to hysterectomy?. Gynaecological Endoscopy 1995;4:77‐9. [Google Scholar]
Garry 1998
- Garry R. Towards evidence‐based hysterectomy. Gynaecological Endoscopy 1998;7:225‐33. [Google Scholar]
Garry 2005
- Garry R. Health economics of hysterectomy. Best Practice & Research. Clinical Obstetrics & Gynaecology 2005;19(3):451‐65. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist G, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. for the GRADE Working Group. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hoffmann 2014
- Hoffmann TC, Montori VM, Mar C. The connection between evidence‐based medicine and shared decision making. JAMA 2014;312(13):1295‐6. [DOI] [PubMed] [Google Scholar]
Johnson 2005b
- Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta‐analysis of randomised controlled trials. BMJ 2005;330(7506):1478‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2009
- Johnson NP. Gynaecological surgery from art and craft to science?. Australian and New Zealand Journal of Obstetrics and Gynaecology 2009;49:120‐3. [DOI] [PubMed] [Google Scholar]
Khan 2014
- Khan K. The CROWN initiative: Journal editors invite researchers to develop core outcomes in women's health. Journal of Obstetrics and Gynaecology 2014;34(7):553‐4. [DOI] [PubMed] [Google Scholar]
Kovac 2014
- Kovac SR. Route of hysterectomy: an evidence‐based approach. Clinical Obstetrics and Gynecology 2014;57(1):58‐71. [DOI] [PubMed] [Google Scholar]
Lethaby 2012
- Lethaby A, Ivanova V, Johnson NP. Total versus subtotal hysterectomy for benign gynaecological conditions. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD004993.pub3] [DOI] [PubMed] [Google Scholar]
Lethaby 2013
- Lethaby A, Penninx J, Hickey M, Garry R, Marjoribanks J. Endometrial resection and ablation techniques for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD001501.pub4] [DOI] [PubMed] [Google Scholar]
Lethaby 2015
- Lethaby A, Hussain M, Rishworth JR, Rees MC. Progesterone or progestogen‐releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 2015, Issue 4. [DOI: 10.1002/14651858.CD002126.pub3] [DOI] [PubMed] [Google Scholar]
Maresh 2002
- Maresh MJ, Metcalfe MA, McPherson K, Overton C, Hall V, Hargreaves J, et al. The VALUE national hysterectomy study: description of the patients and their surgery. BJOG 2002;109(3):302‐12. [DOI] [PubMed] [Google Scholar]
Moen 2014a
- Moen MD, Richter HE. Vaginal hysterectomy: the past, present and future. International Urogynecology Journal 2014;25(9):1161‐5. [DOI] [PubMed] [Google Scholar]
Moen 2014b
- Moen M, Walter A, Harmanli O, Cornella J, Nihira M, Gala R, Zimmerman C, Richter HE, Society of Gynecologic Surgeons Education Committee. Considerations to improve the evidence‐based use of vaginal hysterectomy in benign gynecology. Obstet Gynecol 2014;124(3):585‐588. [DOI] [PubMed] [Google Scholar]
Mäkinen 2001
- Mäkinen J, Johansson J, Tomás C, Tomás E, Heinonen PK, Laatikainen T, et al. Morbidity of 10 110 hysterectomies by type of approach. Human Reproduction 2001;16(7):1473‐8. [DOI] [PubMed] [Google Scholar]
Mäkinen 2013
- Mäkinen J, Brummer T, Jalkanen J, Heikkinen AM, Fraser J, Tomás E, et al. Ten years of progress‐‐improved hysterectomy outcomes in Finland 1996‐2006: a longitudinal observation study. BMJ Open 2013;3(10):e003169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nezhat 1995
- Nezhat C, Nezhat F, Admon D, Nezhat AA. Proposed classification of hysterectomies involving hysterectomy. Journal of the American Association of Gynecologic Laparoscopists 1995;2:427‐9. [DOI] [PubMed] [Google Scholar]
Orozco 2014
- Orozco LJ, Salazar A, Clarke J, Tristan M. Hysterectomy versus hysterectomy plus oophorectomy for premenopausal women. Cochrane Database of Systematic Reviews 2014, Issue 7. [DOI: 10.1002/14651858.CD005638.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pynnä 2014
- Pynnä K, Vuorela P, Lodenius L, Paavonen J, Roine RP, Räsänen P. Cost‐effectiveness of hysterectomy for benign gynecological conditions: a systematic review. Acta Obstetricia et Gynecologica Scandinavica 2014;93(3):225‐32. [DOI] [PubMed] [Google Scholar]
Reich 1989
- Reich H, Decaprio J, McGlynn F. Laparoscopic hysterectomy. Journal of Gynecological Surgery 1989;5:213‐6. [Google Scholar]
Reich 2003
- Reich H, Roberts L. Laparoscopic hysterectomy in current gynaecological practice. Reviews in Gynaecological Practice 2003;3:32‐40. [Google Scholar]
Sarlos 2010
- Sarlos D, Kots L, Stevanovic N, Schaer G. Robotic hysterectomy versus conventional laparoscopic hysterectomy: outcome and cost analyses of a matched case‐control study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2010;150(1):92‐6. [DOI] [PubMed] [Google Scholar]
Sculpher 2004
- Sculpher M, Manca A, Abbott J, Fountain J, Mason S, Garry R. Cost effectiveness analysis of laparoscopic hysterectomy compared with standard hysterectomy: results from a randomised trial. BMJ 2004;328(7432):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smorgick 2014
- Smorgick N, As‐Sanie S. The benefits and challenges of robotic‐assisted hysterectomy. Current Opinion in Obstetrics and Gynecology 2014;26(4):290‐4. [DOI] [PubMed] [Google Scholar]
Spencer 1999
- Spencer CP, Whitehead MI. Endometrial assessment re‐visited. BJOG 1999;106(7):623‐32. [DOI] [PubMed] [Google Scholar]
Spilsbury 2006
- Spilsbury K, Semmens JB, Hammond I, Bolck A. Persistent high rates of hysterectomy in Western Australia: a population based study of 83 000 procedures over 23 years. British Journal of Obstetrics and Gynaecology 2006;113(7):804‐9. [DOI] [PubMed] [Google Scholar]
Sutton 1997
- Sutton C. Hysterectomy: a historical perspective. Balliere's Clinical Obstetrics & Gynaecology 1997;11:1‐22. [DOI] [PubMed] [Google Scholar]
Tapper 2014
- Tapper AM, Hannola M, Zeitlin R, Isojärvi J, Sintonen H, Ikonen TS. A systematic review and cost analysis of robot‐assisted hysterectomy in malignant and benign conditions. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2014;177:1‐10. [DOI] [PubMed] [Google Scholar]
Twijnstra 2012
- Twijnstra AR, Blikkendaal MD, Zwet EW, Kesteren PJ, Kroon CD, Jansen FW. Predictors of successful surgical outcome in laparoscopic hysterectomy. Obstetrics and Gynecology 2012;119(4):700‐8. [DOI] [PubMed] [Google Scholar]
Vessey 1992
- Vessey MP, Villard‐Mackintosh I, McPherson K. The epidemiology of hysterectomy findings in a large cohort study. British Journal of Obstetrics and Gynaecology 1992;99:402‐7. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Johnson 2002
- Johnson N, Lethaby A, Farquhar C, Garry R, Barlow D. Surgical approaches to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews 2002, Issue 4. [DOI: 10.1002/14651858] [DOI] [Google Scholar]
Johnson 2005
- Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD003677.pub2] [DOI] [PubMed] [Google Scholar]
Johnson 2006
- Nieboer TE, Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD003677.pub3] [DOI] [PubMed] [Google Scholar]
Nieboer 2009
- Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD003677.pub4] [DOI] [PubMed] [Google Scholar]


