Abstract
A large number of older adults have physical and/or cognitive challenges and require help to manage everyday activities. Many older adults receive care from a spouse. Over the long term, this has adverse consequences for caregiver health and well-being. Less is known about the outcomes associated with the early transition to becoming a spousal caregiver. Nor is it clear how mild cognitive decline worsens caregiver outcomes. The present study uses dyadic data from 588 couples in the National Social Life, Health and Aging Project to compare mental and social well-being in marital partners who became a spousal caregiver versus those who remained non-caregivers or became caregivers for someone other than a spouse between 2010 and 2015. Cognitive ability was assessed using a validated version of the Montreal Cognitive Assessment. Moderated Actor-Partner Independence Models revealed that becoming a caregiver was associated with an increase in perceived stress in both men and women, and an increase in anxiety among men. Partners’ cognitive limitations moderated, in a dose-dependent fashion, the association between becoming a caregiver and changes in well-being. Specifically, becoming a caregiver was associated with increased support from friends for wives at lower levels of husband’s cognitive ability, and with increased anxiety for husbands at lower levels of wife’s cognitive ability. Associations were independent of demographic characteristics and physical limitations. We discuss the value of using population-based samples to study the transition to caregiving and implications for interventions during the early transition to a caregiving role for even modestly cognitively impaired partners.
Keywords: spousal caregiving, cognitive ability, mental health, social relationships, actor-partner model
By the age of 80, about 38% of older adults require help with self-care, mobility, and household tasks. That figure increases with increasing age such that a majority (76%) require assistance by age 90 (Freedman & Spillman, 2014). Also, spousal caregiving becomes more prevalent with age; 9% of 50–64 year-old, 24% of 65–74 year-old, and 46% of 75+ year-old caregivers are estimated to care for a spouse/partner (NAC & AARP, 2015), a role that disrupts established patterns of interaction between partners and has consequences for the caregiver’s physical and mental health and well-being (Schulz & Eden, 2016). Caregiver burden may differ as a function of the type of impairments in the person requiring care, with greater burden observed among spouses caring for a partner with a cognitive than with a physical impairment (Gibbons et al., 2014), and greatest burden observed for those caring for someone with both physical and cognitive impairments (Tooth et al., 2008). Caregiver burden, in turn, worsens quality of life and increases risk for depression, anxiety, and worsening health (Cheng, 2017). This has been shown for caregivers providing care to adults with frank dementia, but caregivers often provide care for many years preceding more advanced cognitive impairment in the care recipient. Extant research falls short in assessing whether mild symptoms of cognitive decline affect caregiving consequences during the early transition to a caregiving role. The present study uses dyadic data from the National Social Life, Health and Aging Project (NSHAP) to compare mental health and social relationships in marital partners who did versus did not experience a transition to providing care for their spouse over a 5-year interval from 2010 to 2015. Our objectives are to shed light on the unique consequences that ensue after a transition specifically to spousal caregiving (over and above any concurrent caregiving responsibilities for other individuals), whether spousal caregiver consequences are dependent on the cognitive level of their care recipient, and whether husband and wife caregivers differ in this regard. Findings may be informative in targeting interventions to best support the health of spousal caregivers during the early stages of caregiving.
Background
Conceptual Model
The stress process model provides the conceptual framework guiding the present study of caregiver outcomes (Pearlin, Mullan, Semple, & Skaff, 1990). In the context of spousal caregiving for partners with dementia, Pearlin’s stress process model of caregiving holds that the ongoing stress of managing a spouse’s cognitive limitations and behavioral challenges (i.e., the primary stressors) places caregivers under a physical, mental, and emotional burden that can cause secondary stressors (family conflicts, economic problems, restricted social life) and intra-psychic strains (loss of control, challenges to self-esteem and mastery). In turn, primary and secondary stress and strain result in adverse physical and mental health outcomes, including depression, anxiety, and perceived stress. Coping processes (acceptance and adaptation, meaning-making) and social support are posited to mediate or moderate the effect of stress; the availability and use of social supports, for example, can speed the recovery from stress and diminish the severity and prevalence of adverse outcomes (Seeher et al., 2014; Pearlin et al., 1990).
Extant Research: Review and Limitations
The health effects associated with caregiving have been well-documented (Schulz & Sherwood, 2008), but this research has been limited in several ways. First, most research to date has been cross-sectional, comparing caregivers with non-caregivers at a given time. In one study of caregiving transitions, those who became caregivers tended to be older and had lower income at baseline than those who remained non-caregivers (Burton, Zdaniuk, Schulz, Jackson, & Hirsch, 2003), however, and such pre-existing differences obfuscate comparisons of health between caregivers and non-caregivers. Second, studies that have taken a longitudinal approach to examine the transition to caregiving have found adverse outcomes for those who became caregivers, but these studies have not considered the interaction of physical and cognitive needs in the care recipient on the caregiving burden (Burton, et al., 2003; Schulz & Beach, 1999). Research explicitly examining the moderating effect of care recipients’ cognitive limitations on caregiver outcomes is completely lacking.
Third, studies that have examined the health consequences of caregiving for a spouse with cognitive limitations have centered on caring for a person with moderate to advanced dementia (Braun, Scholz, Bailey, Perren, Hornung, & Martin, 2009; Pinquart & Sorensen, 2003). However, even early stages of cognitive decline can adversely affect the mental health of the caregiving spouse. For example, in their cross-sectional study of 106 care partners (primarily spouses) of community residents recently diagnosed with mild cognitive impairment (MCI), Blieszner & Roberto (2010) found that caregiving responsibilities were associated with greater depression even before the onset of significant behavioral changes in the cognitively impaired partner. Spouses have been shown to reliably detect subtle (i.e., pre-clinical) deficits in partners’ cognitive functioning across the whole range of cognitive ability (Nosheny et al., 2018) and this awareness could affect their own well-being (e.g., anxiety).
Finally, research on caregiver outcomes has been limited primarily to small convenience and clinical samples (e.g., recruited in frailty and dementia clinics, hospital outpatient departments) and have not included probability samples of the population. As shown in a meta-analysis, results from these studies differ from those few studies that have used probability samples (Pinquart & Sorensen, 2003). A characteristic of studies using convenience or clinical samples is the absence of a non-caregiver group against which to compare caregivers. In a systematic literature review of caregiver outcomes among those caring for a person diagnosed with mild cognitive impairment, only 10 relevant quantitative studies were identified, and these studies did not compare outcomes for caregivers relative to non-caregivers. Outcomes were compared between caregivers and the general population using estimates derived from independent sources. Depressive symptoms were elevated and depression was more prevalent than rates reported in the general population, although somewhat less than in dementia caregivers (Seeher et al., 2014). Other outcomes (anxiety, burden, stress) also differed between caregivers and the general population, but were examined in only single studies so no pooled results were possible. One subsequent study found significantly greater burden among MCI caregivers than an informant control group (Paradise et al., 2015).
Taken in combination, these studies reveal adverse effects for MCI caregivers. Cognitive limitations may have adverse effects on caregiver outcomes across the continuum of cognitive ability, and Pearlin’s stress process model allows the consideration of the impact of cognitive ability across the spectrum, without respect for artificial boundaries.
In sum, longitudinal follow-up studies in representative population-based samples are needed to capture normative changes in older adult dyads as they newly adapt to a spousal caregiving role while considering the moderating effects of cognitive impairment.
Caregiver Outcomes
Depression is frequently assessed in caregiving research, but other mental health outcomes, such as anxiety and loneliness, have not been explored as extensively. In qualitative research, focus group interviews have revealed that caregivers of those with mild cognitive impairment most frequently raise issues around social well-being (e.g., change in social roles; need for social support) when discussing “important aspects of health-related quality of life,” followed in frequency by mental health concerns (e.g., anger, anxiety, need for patience) (Carlozzi et al., 2018). One study showed that co-resident caregivers of individuals with dementia are less likely to seek social support (Snyder et al., 2015), but we are not aware of any longitudinal research that examines whether caregivers perceive or experience increased social support after the transition to caregiving. Other studies have found no changes in caregivers’ social activity following the transition to caregiving (Queen, Butner, Berg, & Smith, 2017), and no changes in loneliness with the onset of informal caregiving, although caregivers attained regular contact with a larger number of individuals than non-caregivers (Hajek & König, 2018). Researchers have called for greater attention to a range of outcomes among caregivers (Paradise et al., 2015; Seeher et al., 2014), in part to better target interventions that could be delivered earlier in the caregiving “career” and thus reduce or prevent the development of more consequential symptoms and reactions later in the course of the care recipient’s declining cognitive ability.
Gender differences in caregiver outcomes.
Among spousal caregivers of a partner with dementia, wives are consistently observed to experience greater caregiver burden than husbands. Some studies have shown that women spend more time caregiving than men (Calasanti, 2010), and are more likely than men to ignore their own health when in a caregiving role (Solomi & Casiday, 2016). Data from the Netherlands’ Older Persons and Informal Caregivers Survey indicate that caregiving wives experience greater burden than husbands in part because they carry the weight of more secondary stressors such as relational and financial problems and difficulties completing their daily activities because of the demands of caregiving (Swinkels, van Tilburg, Verbakel, & Broese Van Groenou, 2017). Greater burden has been shown to contribute to gender differences in the health consequences of caregiving, including differences in behavioral and psychosocial consequences (Swinkels et al., 2017). A study of 65 caregivers of a spouse with dementia (20 men, 45 women) found that wives, relative to husbands, were more heavily burdened by the caregiver role, reported worse physical and mental health, had significantly more depressive symptoms, and practiced fewer health-promoting behaviors (Gibbons et al., 2014). Engagement in most types of leisure activities, including visiting friends, was low and did not differ in frequency between husbands and wives. Male and female caregivers were equally likely to take advantage of formal and informal help and services, and were equally satisfied with the supports and services they accessed, but wives received significantly fewer hours of help than husbands. On the other hand, a Finnish study of 335 dyads of dementia patients and their spousal caregivers found that, even though wives with dementia had more severe disease than husbands, husband caregivers experienced less burden than wife caregivers (Pöysti et al., 2012).
A review of 18 studies of well-being outcomes experienced by older-adult spousal caregivers revealed that wife caregivers experienced greater depression, anxiety, stress, and loneliness than husband caregivers (Lavela & Ather, 2010). Most of the studies in the review centered on care for a spouse with a dementia and did not distinguish outcomes from those associated with care for a physically impaired or a more modestly cognitively impaired partner. Another study showed a larger association in wives than husbands between depression and caregiving for a spouse with physical impairments. Wives were also more likely than husbands to be caring for a spouse who was concurrently experiencing severe cognitive impairment (Sugiura, Ito, Kutsumi, & Mikami, 2009), suggesting that the additional burden of spousal cognitive limitations may help to explain the more negative outcomes experienced by wife than husband caregivers. Physical frailty and cognitive decline frequently co-occur in older age (Artero, Touchon, & Ritchie, 2001). It is not currently known whether cognitive decline adds to the negative consequences of caring for a spouse with concurrent physical impairment, and whether wife caregivers, relative to husband caregivers, experience greater negative consequences from caring for a spouse with lower levels of cognitive ability.
Actor-Partner Effects in a Caregiving and Receiving Dyad
The theoretical framework of spousal interrelations (Hoppmann & Gerstorf, 2009) posits that partners in a marriage exert dynamic and mutual effects on each other into old age, which in the context of caregiving suggests that characteristics of the care recipient may affect the caregivers’ health and well-being (and vice versa). Dyadic-level analyses, as operationalized in actor-partner interdependence models (APIM), are able to provide estimates of the simultaneous impacts of one member of the dyad on the other member’s outcomes. The relevance of this approach to caregiving is evident in cross-sectional research showing that husbands’ physical impairment is associated with wives’ lower marital support and higher marital strain, and husbands’ cognitive limitations are associated with wives’ greater support from friends and family (Wong & Hsieh, 2017). Using data from older adults enrolled in the Cardiovascular Health Study, Monin et al. (2018) conducted a longitudinal dyadic path analysis and found cross-partner associations such that one spouse’s depressive symptoms predicted a decrease in the partner’s cognitive ability over time, but a spouse’s cognitive ability did not predict a change in the partner’s depressive symptoms over time. Neither of these studies focused on caregiving, however.
A dyadic approach can be useful in determining not only direct effects of partners on each other, but also in estimating the buffering effects of a care recipient’s characteristics on caregiver outcomes elicited by the caregiving experience (Braun et al., 2009). It is the latter approach that allows us to examine whether the care recipient’s degree of cognitive ability moderates the association between caregiving and well-being.
The Present Study.
The present study seeks to fill the previously identified gaps in the caregiving literature. First, we examine outcomes associated with the transition to spousal caregiving by following a nationally representative sample of older adult dyads over five years. At study onset, neither partner is providing care to the other (but may provide care to someone else). Over the 5-year period, some start providing care to their spouse (or to another adult). We compare outcomes for those who do and do not become spousal caregivers, regardless of whether they also become caregivers for someone other than a spouse. Second, we test the impact of care recipients’ cognitive ability on caregiver well-being across the full range of cognitive functioning. We adjust for physical impairments to assess the unique moderating influence of care recipient’s cognitive ability on caregiver well-being in those who transition versus do not transition into a spousal caregiver role. Throughout, we include a wide range of outcomes, and examine whether men and women are affected differently by the transition to caregiving and by their spouse’s cognitive limitations.
We hypothesize that (1) transitioning to a spousal caregiver role (predictor variable) will decrease the caregiver’s well-being (dependent variable), (2) caregiving wives will experience greater declines in well-being than caregiving husbands, and (3) the impact on caregiver well-being will increase as the spousal cognitive limitations increase (moderator). Prior literature suggests that the transition to caregiving will be associated with an increase in perceived stress (an indicator of caregiver burden; Pearlin et al., 1990) and an increase in depressive symptoms. Given the paucity of research on the transition to caregiving in a population-based sample, we make no specific hypotheses regarding our other indicators of well-being.
Method
Sample
This study uses dyadic data from the National Social Life, Health and Aging Project (NSHAP). NSHAP is an ongoing panel study of health and aging in a nationally representative sample of older adults aged 57–85 years at study onset in 2005–06 (Wave 1). NSHAP conducts follow-up surveys every five years (2010–11, Wave 2; 2015–16, Wave 3). Data are collected by the National Opinion Research Center (NORC) at the University of Chicago. Interviews are conducted in the home by trained interviewers using Computer Assisted Personal Interviewing (CAPI) along with a leave-behind questionnaire (LBQ) that respondents complete and mail back. The LBQ was completed and returned by 87% of the sample in Wave 2 (2010–11) and 85% of sample in Wave 3 (2015–16). This study was approved by the Institutional Review Boards of NORC and the University of Chicago. All respondents provided written, informed consent.
In 2010 (Wave 2), NSHAP added co-resident spouses and partners of the respondents to the sample, yielding a subsample of 955 couples (O’Muircheartaigh, English, Pedlow, & Kwok, 2014). In Wave 3 (2015), due to the dropout of one or both members of the couple, 334 of the 955 couples exit the dyadic subsample, and thus 621 couples have longitudinal dyadic data from Wave 2 to Wave 3. To account for bias due to dropout, this study uses inverse probability weighting adjustment to reweight the remaining couples.
Further, this study is interested in couples who were not yet caregivers in Wave 2, and therefore excluded couples who were already caregivers in Wave 2 (N=32). In addition, given our interest in gender differences within a couple, one homosexual couple was excluded. These restrictions yielded an analytic sample of 588 heterosexual couples. We refer to partners as husband and wife, but 3.7% of couples (n=22) were co-resident but not married.
Measures
Four mental health variables constitute the first set of outcomes in this study: depression, loneliness, anxiety, and perceived stress. The latter three measures were assessed in the LBQ; depressive symptoms were assessed in the in-person interview. The measure descriptions and scoring instructions have been documented previously (Payne et al., 2014), and are summarized below. The second set of outcomes concern social activities and social support as described below; all were assessed in the LBQ.
Mental health outcomes.
Depressive symptoms.
NSHAP uses items derived from the CES-D, a validated tool designed to detect risk for clinical depression (Radloff, 1977). The items ask about the frequency of 11 symptoms during the past week, which are coded as “rarely or none of the time” (0), “some of the time” (1), and “much or most of the time” (2). Scores are summed to produce a total score (“CES-D”) that ranges from 0 to 22. In the analytical sample, the Cronbach’s alpha for the 11 items is 0.78 in Wave 2 and Wave 3.
Loneliness.
A validated 3-item version of the UCLA Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, 2004) was used. Response categories were coded as “hardly ever or never” (0), “some of the time” (1) or “often” (2), and summed to yield a loneliness score (“UCLA-R”) ranging from 0–6. The Cronbach’s alpha for the 3 items is 0.79 in Wave 2 and Wave 3.
Anxiety.
NSHAP uses 7 items from the Hospital Anxiety and Depression Scale’s Anxiety Subscale (HADS-A) (Zigmond & Snaith, 1983) regarding symptoms experienced during the past week. The 4-point response scale includes “rarely or none of the time” (0), “some of the time” (1), “occasionally” (2), and “much or most of the time” (3). Scores are summed to produce a total score (“HADs”) that ranges from 0 to 21. The Cronbach’s alpha for the 7 items is 0.75 in Wave 2 and 0.71 in Wave 3.
Perceived stress.
NSHAP uses a validated 4-item version of the Perceived Stress scale developed by Cohen & Williamson (1988) regarding experiences during the past week. Response categories are equivalent to those for the depressive symptom scale, and are summed to yield a perceived stress score (“PSS”) ranging from 0–8. The Cronbach’s alpha is 0.52 in Wave 2 and 0.59 in Wave 3.
Social activities and social support outcomes.
Religious service attendance.
One item asked how frequently respondents attend religious services (“RSA”). Response categories range from 0–4, where 0=not at all, 1=one or more times a year, 2=two or three times a month, 3=once a week, and 4=more than once a week.
Social engagement.
Social engagement was derived from three items asking how frequently the respondents participate in volunteer work, socialize with friends or relatives, and attend meetings of organized groups in the past 12 months. Ordinal response categories for each item ranged from 0 to 6, with 6 indicating the highest level of frequency. Thus the composite social engagement score (“SE”) ranges from 0 to 18. The Cronbach’s alpha for the 3 items is 0.65 in Wave 2 and 0.66 in Wave 3.
Social support.
NSHAP uses social support items originally introduced in the 2002 Health and Retirement Study. In this study, we assess social support from two sources - family and friends, using the same two items- (1) how often can you open up to, and (2) how often can you rely on... your family/friends. Response categories range from 0–3, with 3 indicating the highest level of support. Responses are averaged across the two items. The Cronbach’s alpha for the family support items (“FamSp”) is 0.65 in Wave 2 and 0.70 Wave 3; the Cronbach’s alpha for the friend support items (“FrndSp”) is 0.77 in Wave 2 and 0.73 in Wave 3.
Predictor Variable.
Caregiving.
The key predictor variable in this study is becoming a spousal caregiver by Wave 3. A change in caregiver status is dummy-coded, where 0 represents those who remained non-caregivers over the time period under study, and 1 represents respondents who became spousal caregivers. The variable is based on information from two items in the LBQ. The first item asks, “Are you currently assisting an adult who needs help with day to day activities because of age or disability?”, and the answers are either Yes or No. If the respondent answers “Yes,” the second item asks “What is this person’s relationship to you?” If the answer is “Yes” to the first item and “Spouse” for the second item, the respondent is coded as a spousal caregiver. If the respondent answers “No” to the first item or answers “Yes’ but identifies a non-spousal relationship (e.g., child, grandchild) with the care recipient, the respondent is coded as a non-caregiver. The non-caregiving group includes 41 women (9.3% of the non-caregiving women) and 27 men (5.9% of the non-caregiving men) who care for someone other than a spouse. Effects reported here are for those who became spousal caregivers and are therefore conservative estimates because the comparison group includes some who also become caregivers but for someone other than a spouse.
Moderator.
Cognitive ability.
This study uses the survey-adapted Montreal Cognitive Assessment (MoCA-SA) to measure cognitive ability. The development and validation of the measure have been described previously (Kotwal et al., 2016; Shega et al., 2014). The calculated MoCA-SA score ranges from 8 to 30, with larger values indicating a higher level of cognitive ability. Because we believe that Wave 3 caregiving outcomes are moderated by cognitive ability, we employ the Wave 3 MoCA-SA score as our covariate. For the analysis, we subtracted the gender-specific mean MoCA-SA (23.45 for wives and 22.41 for husbands) from the raw score to allow the effect of caregiving to represent the omnibus effect at the gender-specific average MoCA-SA score. This study also calculates the change in MoCA-SA from Wave 2 to Wave 3 by subtracting the Wave 2 MoCA-SA score from the Wave 3 MoCA-SA score. We did this to hold constant the “trajectory” of cognitive ability over time.
Control variables.
Functional limitations.
Functional limitations refer to the number of difficulties the respondent has with Activities of Daily Living (ADLs; for detail, see Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). Specifically, this study considers 6 ADLs, which includes walking across the room, dressing, bathing, eating, getting in and or of bed, and using the toilet. The difficulty with each of the activities is coded as either 1 (any difficulty) or 0 (no difficulty). Responses to the six ADLs are summed and functional limitations thus range from 0 to 6. Changes in functional limitations from Wave 2 to Wave 3 are calculated by subtracting Wave 2 functional limitations from Wave 3 functional limitations.
Comorbidity index.
Respondent’s health status in Wave 2 was assessed by asking about chronic health conditions. The NSHAP Comorbidity Index is based on the method developed by Vasilopoulos et al. (Vasilopoulos, Kotwal, Huisingh-Scheetz, Waite, McClintock, & Dale, 2014), and sums the number of chronic conditions endorsed by the respondent. Number of conditions were defined by 5 ordinal categories: 0, 1, 2, 3, or 4 or more.
Demographic covariates.
This study selected demographic covariates based on the potential confounding associations between caregiving and mental health or social activities and support that have been observed in the literature. The selected covariates included household income in Wave 2 (less than $25,000; $25,000<50,000, $50,000<100,000, or $100,000 and more), race (Black, Hispanic, or White and “other” race/ethnicities), education (less than high school, high school or equivalent, some college, or Bachelor’s degree or more), age in years (less than 65, 65–74, 75–84, or 85 and older). Household income was reported separately by each partner, and there was occasional inconsistency in the reported household income. In these circumstances, the household income reported by the husband was used as the household income for both partners. When only one of the partners reported household income, that value was used as the household income for both partners regardless of who reported the income. We conducted sensitivity tests and determined that results were not substantively altered if we used the wife’s reported household income or the household income reported by the partner with better cognitive functioning instead of the husband’s report. Results are included in supplementary material (Supplementary Tables 2 and 3, respectively).
Analytic Strategy
The current study addresses the research question by using a Moderated Actor-Partner Interdependence Model (MAPIM). This is a modification of the Actor-Partner Interdependence Model (APIM) detailed by Kenny et al. (Kenny, Kashy, & Cook, 2006; see also Wong & Hsieh, 2017; Hsieh & Hawkley, 2018). We use path analysis with observed variables rather than a latent variable approach.
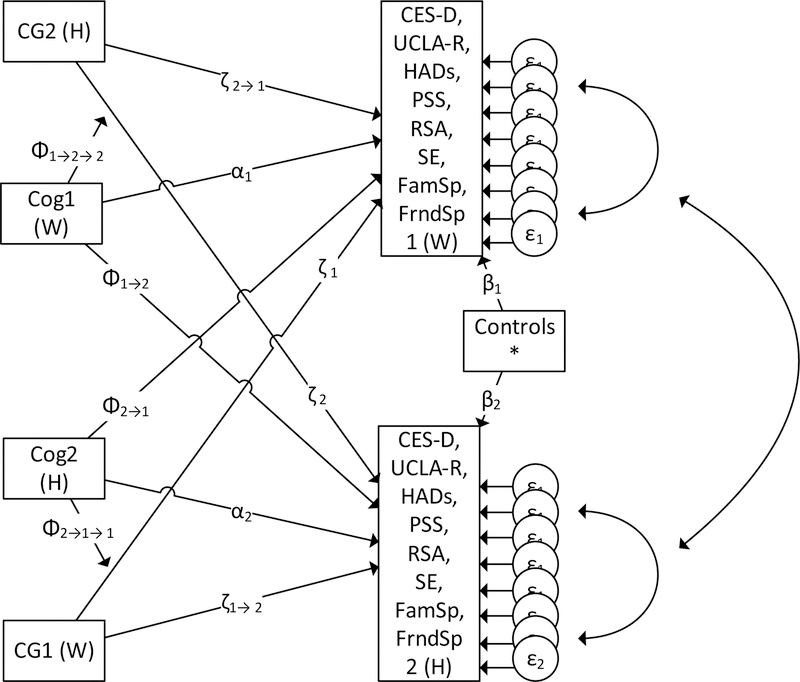
The focus of our paper is in how outcomes associated with transitioning to a spousal caregiver role are moderated by the partner’s cognitive ability while adjusting for their partner’s physical ability. Figure 1 presents our moderated actor partner interdependence model (MAPIM). In this model, we introduce a variable, CG, which represents change in caregiving status between waves. This variable enters the MAPIM model in three ways. For each actor (1 and 2), the moderator CG has a direct association with the actor’s set of outcomes (CES-D, UCLA-R, HADs, PSS, RSA, SE, FamSp, and FrndSp), through the paths noted as ζ1 for actor 1 and ζ2 for actor 2 (a path is estimated for each outcome). There is also a main partner path of the moderator (i.e., cognitive ability, Cog), noted as ζ1 →2 for the partner effect of actor 1 to 2, and likewise the converse partner path of ζ2 →1 (again, a path is estimated for each outcome). Our interest is in how the partner’s cognitive ability (Cog), alters the association between the actor’s caregiving status (CG), and the actor’s set of outcomes. We denote these moderation effects as the partner effects ϕ1→2→2 to represent how actor 1’s cognitive ability (Cog) influences the association between actor 2’s caregiving status (CG) and actor 2’s set of outcomes. To aid in the interpretation of the coefficients, the MoCA-SA scores were centered (demeaned) on the sample average. This allows the other path coefficients to be interpreted in isolation as the value for an average MoCA-SA. The path ϕ2→1→1 has a similar meaning. Paths are estimated for each outcome. To detail the effects in terms of the variables, we posit that the association between i caring for j and the well-being of i is
Figure 1:
Moderated Actor Partner Interdependence Model
Notes. Variable definitions: H: Husband; W: Wife. CG: caregiving status change, Cog: Cognitive ability as measured by the MoCA-SA. CES-D: Depression, UCLA-R: Loneliness, HADs: Anxiety, PSS: Perceived stress, RSA: Religious service attendance, SE: social engagement, FamSp: Family support, and FrndSp: Friend support. Controls* include measures of functional limitations in Wave 3 and change from Wave 2, comorbidity index in Wave 3 and change from Wave 2, change in cognitive ability from Wave 2, and indicators for household income categories, race categories, education categories, and age categories.
Estimation of associations.
The associations are estimated using a single structural equation model (SEM) that includes all outcomes. We also estimate variances for each outcome and all possible covariances (symbolized as the arrows on the right of Figure 1). Our models also include demographic controls, a comorbidity index, and change scores measuring the change in functional limitations and cognitive ability from Wave 2 to Wave 3. The change scores are included to capture the extent of between-wave declines and hold them constant.
Survey estimation and non-response.
NSHAP used multi-stage probabilistic sampling techniques to obtain a nationally representative sample (O’Muircheartaigh, Eckman, & Smith, 2009). Thus, in order to retain the representativeness of the sample, we employed the couple weights to account for unequal selection probability as well as setting the household (each with two observations) as the primary sampling unit (Lohr, 2009). The weights were adjusted for between-wave non-response using a probability model that predicted the likelihood of response. We then used the predicted probabilities from that model to redistribute the survey weight from non-respondents to respondents. The household income variable was missing data for 16.6% of the cases, and we represented these values by creating an income category that we labeled “missing.” The value of the coefficient for this category of income is relatively meaningless since it represents an unknown range of household incomes, but including the category preserves these respondents and the other data they provided. This ensured that we maximized use of all available data before relying on full information maximum likelihood (FIML) in our SEM models. By using FIML, this study retains all 588 eligible couples in the statistical analyses.
Computing interaction effects and other comparison tests.
Our models include moderated effects whereby the conditional effect of caregiving (CG) is dependent on the value of partner cognition (COG), that is
where CGiCogj is the product term (interaction) used to estimate the moderated effect. We used Stata 15 to estimate our models and compute the conditional slopes, or values of the slope at specific values of the moderator. Conditional slopes are essentially linear combinations of the model coefficients (the main effect, ζi, plus the moderating effect times the value of the moderator, Cogjϕj→i→i). Thus, we took advantage of Stata’s “lincom” command to compute and test linear combinations of the resulting coefficients from the model.1 This allowed us to determine whether the conditional slope, f(CGi→j), was statistically significant at specific values of the moderator, Cogj. Output from the “lincom” command produces results equivalent to Aiken and West’s (1991) centering technique to test interactions in a regression model,2 and also easily permits calculation of slopes at different levels of the moderator. In our case, we obtain the slopes (i.e., association) between spousal caregiving status (yes vs. no) and outcomes at different levels of spouse’s cognitive ability.
Gender differences.
As all paths were estimated from a single model, we again utilized the linear combination procedure in Stata (“lincom”) to test whether the differences in the coefficients, namely , were statistically different than 0.3 Thus, we test the gender differences of both the main and moderating effects. Supplementary Table 5 details the differences in the coefficients, their standard errors, and statistical tests.
Results
Descriptive Statistics by Gender
Table 1 presents the descriptive statistics for the analyzed couples by gender. Degrees of freedom (df’s) are 587 for all comparisons. Relative to men (husbands), women (wives) had significantly higher levels of depressive symptoms (t = −2.15, p = 0.032), greater social engagement (t = −2.73, p = 0.007), and more support from family (t = −2.89, p = 0.004) and friends (t = −2.59, p = 0.01) at baseline (Wave 2).
Table 1.
Weighted Descriptive Statistics by Gender (Wife/Husband).
| Variable | Mean (SD)/proportion | |
|---|---|---|
| Wife |
Husband |
|
| Outcome in Wave 2 | ||
| Depression (CES-D) * | 4.24 (3.98) | 3.59 (3.76) |
| Loneliness (UCLA-R) | 0.88 (1.39) | 0.71 (1.16) |
| Anxiety (HADs) | 5.85 (3.04) | 5.42 (3.06) |
| Stress (PSS) | 3.93 (1.67) | 4.15 (1.53) |
| Religious Service Attendance | 2.60 (1.73) | 2.34 (1.80) |
| Social engagement ** | 9.79 (4.14) | 8.92 (4.23) |
| Family Support *** | 2.52 (0.61) | 2.15 (0.78) |
| Friend Support *** | 2.20 (0.79) | 1.86 (0.81) |
| Outcome in Wave 3 | ||
| Depression (CES-D) ** | 4.95 (4.23) | 4.05 (3.71) |
| Loneliness (UCLA-R) * | 0.86 (1.29) | 0.65 (1.13) |
| Anxiety (HADs) | 5.84 (3.05) | 5.41 (2.94) |
| Stress (PSS) | 4.11 (1.55) | 4.00 (1.68) |
| Religious Service Attendance | 2.53 (1.74) | 2.37 (1.80) |
| Social engagement * | 9.73 (4.30) | 8.99 (4.15) |
| Family Support *** | 2.53 (0.57) | 2.26 (0.67) |
| Friend Support *** | 2.11 (0.73) | 1.84 (0.73) |
| Independent Variables | ||
| Became spousal caregiver by W3 | ||
| (%) | ||
| Yes | 10.4 | 9.4 |
| No | 89.6 | 90.6 |
| Covariates | ||
| MoCA-SA in Wave 3 ** | 23.57 (4.28) | 22.58 (4.27) |
| Change in MoCA-SA (W3-W2) | −0.67 (3.03) | −0.41 (3.11) |
| Functional limitations in Wave 3 | 0.47 (1.10) | 0.53 (1.11) |
| Change in functional limitations (W3-W2) | 0.09 (0.92) | 0.22 (1.18) |
| Household income (%) | ||
| Less than $25,000 | 12.4 | ---- |
| $25,000 <= $50,000 | 25.5 | ---- |
| >$50,000 <=$100,000 | 40.1 | ---- |
| > $100,000 | 5.4 | ---- |
| Missing | 16.6 | ---- |
| Race (%) | ||
| White and other | 86.6 | 85.6 |
| Black | 6.8 | 6.9 |
| Hispanic | 6.6 | 7.5 |
| Education (%) | ||
| Less than high school | 11.0 | 13.7 |
| High school or equivalent | 22.4 | 24.6 |
| Some college | 41.2 | 27.3 |
| Bachelor’s degree or more | 25.3 | 34.4 |
| Age in years (%) *** | ||
| <= 64 | 41.2 | 22.8 |
| 65–74 | 43.7 | 49.8 |
| 75–84 | 14.6 | 25.1 |
| >= 85 | 0.6 | 2.3 |
| Comorbidity index (%) *** | ||
| 0 | 13.5 | 7.8 |
| 1 | 22.3 | 27.6 |
| 2 | 21.0 | 24.3 |
| 3 | 14.2 | 21.0 |
| 4 and higher | 29.0 | 19.7 |
| N (unweighted) | 588 | 588 |
Note. MoCA-SA: Montreal Cognitive Assessment – Survey Adapted.
Women and men are compared using t-tests for continuous variables, and chi-square tests for categorical variables.
p < 0.05,
p < 0.01,
p < 0.001 (two-tailed tests).
In Wave 3, women had significantly higher MoCA-SA scores than men (t = −3.08, p = 0.002). However, the number of functional limitations was not significantly different between women and men. A somewhat higher proportion of women (10.4%) compared to men (9.4%) reported becoming caregivers for their partners, but a chi-square test indicated no significant association between caregiving and gender.
Descriptive Statistics by Gender & Caregiving Status
Analyses by gender and Wave 3 caregiving status were conducted to test for pre-existing differences in these groups prior to adopting a spousal caregiving role (i.e., in Wave 2) (see Table 2). These results revealed that men who went on to become spousal caregivers reported significantly more depressive symptoms in Wave 2 than their counterparts who did not become spousal caregivers. Women who went on to become caregivers did not differ from their non-caregiving counterparts in Wave 2 outcomes. In addition, the demographics of those who became caregivers differed from those who remained non-caregivers. Specifically, White women were under-represented in the caregiving group (84%) relative to the continuous non-caregiving group of wives (89%). Relative to the continuous non-caregiving group of husbands, men under age 65 were under-represented (11% vs. 25.5%) and men with a greater comorbidity burden (4 or more chronic conditions) were over-represented in the caregiving group (65.5% vs. 25%).
Table 2.
Weighted Descriptive Statistics by Gender and Wave 3 Caregiving Status.
| Variable | Mean (SD)/proportion | |||
|---|---|---|---|---|
| Wives | Husbands | |||
| Non- and non- spousal caregivers |
Spousal caregivers |
Non- and non- spousal caregivers |
Spousal caregivers |
|
| N (unweighted) | 439 | 44 | 458 | 39 |
| Outcome in Wave 2 | ||||
| Depression (CES-D) | 3.94 (3.73) | 4.96 (3.87) | 3.24 (3.48) | 5.27 (4.54)* |
| Loneliness (UCLA-R) | 0.89 (1.40) | 0.89 (1.48) | 0.64 (1.10) | 1.02 (1.12) |
| Anxiety (HADs) | 5.87 (3.02) | 6.47 (3.65) | 5.29 (3.00) | 5.09 (2.42) |
| Stress (PSS) | 4.04 (1.57) | 3.54 (1.82) | 4.11 (1.52) | 4.04 (1.47) |
| Religious Service Attendance | 2.66 (1.73) | 2.22 (1.80) | 2.34 (1.79) | 2.38 (2.06) |
| Social engagement | 10.10 (4.05) | 8.74 (4.12) | 9.13 (4.02) | 9.44 (5.78) |
| Family Support | 2.53 (0.62) | 2.63 (0.56) | 2.18 (0.76) | 2.17 (0.71) |
| Friend Support | 2.23 (0.78) | 2.36 (0.64) | 1.87 (0.80) | 1.81 (0.78) |
| Outcome in Wave 3 | ||||
| Depression (CES-D) | 4.72 (4.09) | 5.51 (4.08) | 3.74 (3.58) | 5.05 (3.92) |
| Loneliness (UCLA-R) | 0.78 (1.27) | 1.27 (1.30) | 0.62 (1.10) | 0.70 (0.94) |
| Anxiety (HADs) | 5.66 (2.94) | 7.20 (3.42) * | 5.27 (2.87) | 6.16 (3.37) |
| Stress (PSS) | 4.04 (1.52) | 4.74 (1.62) * | 3.92 (1.70) | 4.86 (1.66)* |
| Religious Service Attendance | 2.56 (1.76) | 2.18 (1.69) | 2.35 (1.78) | 2.31 (1.84) |
| Social engagement | 9.97 (4.31) | 8.78 (3.95) | 9.21 (4.00) | 9.25 (4.73) |
| Family Support | 2.53 (0.56) | 2.54 (0.52) | 2.27 (0.65) | 2.31 (0.70) |
| Friend Support | 2.10 (0.72) | 2.27 (0.62) | 1.87 (0.72) | 1.64 (0.71) |
| Covariates | ||||
| MoCA-SA in Wave 3 | 24.07 (3.97) | 23.12 (4.08) | 23.06 (4.18) | 21.30 (3.79)* |
| Change in MoCA-SA (W3-W2) | −0.47 (3.02) | −0.54 (2.96) | −0.30 (2.98) | −1.01 (3.20)* |
| Functional limitations in Wave 3 | 0.46 (1.10) | 0.45 (1.12) | 0.40 (0.94) | 1.04 (1.42)* |
| Change in functional limitations (W3-W2) | 0.10 (0.91) | −0.16 (0.86) | 0.13 (1.06) | 0.62 (1.25)* |
| Household income (%) | ||||
| Less than $25,000 | 10.0 | 7.9 | 9.7 | 22.3 |
| $25,000<= $50,000 | 25.2 | 25.7 | 22.7 | 24.0 |
| >$50,000<=$100,000 | 42.0 | 43.0 | 43.9 | 30.5 |
| > $100,000 | 4.6 | 6.6 | 5.5 | 4.4 |
| Missing | 18.1 | 16.8 | 18.3 | 19.0 |
| Race (%) | * | |||
| White and others | 88.9 | 83.8 | 87.1 | 81.3 |
| Black | 5.4 | 16.2 | 5.8 | 10.1 |
| Hispanic | 5.7 | 0.0 | 7.1 | 8.6 |
| Education (%) | ||||
| Less than high school | 6.9 | 14.5 | 11.7 | 21.0 |
| High school or equivalent | 20.2 | 34.4 | 21.9 | 11.9 |
| Some college | 45.1 | 31.1 | 29.0 | 21.8 |
| Bachelor’s degree or more | 6.9 | 14.5 | 37.4 | 45.3 |
| Age in years (%) | * | |||
| <= 64 | 44.0 | 34.1 | 25.5 | 11.0 |
| 65–74 | 42.7 | 46.6 | 49.8 | 50.5 |
| 75–84 | 12.9 | 19.4 | 24.1 | 33.1 |
| >= 85 | 0.4 | 0.0 | 0.6 | 5.4 |
| Comorbidity Index (%) | *** | |||
| 0 | 6.3 | 13.6 | 14.9 | 1.9 |
| 1 | 28.7 | 14.4 | 22.8 | 12.0 |
| 2 | 25.1 | 19.6 | 22.6 | 9.9 |
| 3 | 19.6 | 35.5 | 14.8 | 10.8 |
| 4 and higher | 20.3 | 16.9 | 25.0 | 65.5 |
Note. MoCA-SA: Montreal Cognitive Assessment – Survey Adapted.
Caregivers and non-caregivers are compared, within gender, using t-tests for continuous variables, and chi-square tests for categorical variables.
p < 0.05,
p < 0.01,
p < 0.001 (two-tailed tests).
Correlations Among Key Variables and Across Waves by Gender.
Correlations among the predictor, moderating, and dependent variables between husbands and wives in Wave 3 are presented in Supplementary Table 1a. As expected, husbands’ and wives’ levels of the well-being and social activity measures were significantly correlated, with the exception of perceived stress at r=0.08 (p = .056). Spouses’ MoCA scores were also correlated (r=.39, p < .001), but spousal caregiving status was not significantly correlated between husbands and wives (r=−0.06, p = .167).
Correlations among the predictor, moderating, and dependent variables across waves were estimated separately for husbands and wives and are presented in Supplementary Tables 1b and 1c, respectively. For both husbands and wives, levels of well-being and social activity were reliably correlated over time, but social activity measures (religious service attendance and social engagement) were more corrected over time than the well-being measures. One exception was perceived stress, a measure that was not significantly correlated across waves for husbands (r=0.08, p = .052) but was correlated for wives (r=0.17, p < .001).
Actor-Partner Effects of Caregiving
Table 3 presents the analytical results of the key paths presented in Figure 1, namely, ζi,ϕj→i, and ϕj→i→i, , and , which constitute the effects of becoming a caregiver for an average MoCA-SA, the effect of partners’ deviation from the average MoCA-SA, and the moderating effect of caregiving based on the partners’ deviation from the average MoCA-SA, respectively. Specific effects can be computed as , where Cogj is the centered MoCA-SA score for the partner.
Table 3.
SEM regressions of mental health, social activity, and social support on MoCA, caregiving, and MoCA-by-caregiving interactions showing standardized coefficients (SEs).
| Outcome Variable | Depression | Loneliness | Anxiety | Stress | Religious Service Attendance |
Social Engagement |
Family Support |
Friend Support |
|---|---|---|---|---|---|---|---|---|
| Wife (Actor 1) | ||||||||
| Wife becomes caregiver for husband (ζ1) | 0.031 (0.183) |
0.238 (0.162) |
0.296 (0.282) |
0.557** (0.206) |
−0.002 (0.131) |
0.046 (0.134) |
0.090 (0.176) |
0.081 (0.155) |
| Husband’s MoCA-SA
(ϕ 2→1) |
−0.021 (0.015) |
0.0006 (0.017) |
0.039* (0.018) |
0.009 (0.019) |
−0.018† (0.010) |
0.009 (0.013) |
0.0031† (0.016) |
0.0016 (0.015) |
| Husband’s MoCA-SA × Wife
becomes caregiver for husband (ϕ 2→1→1) |
0.031 (0.033) |
−0.046 (0.037) |
−0.054 (0.051) |
−0.033 (0.052) |
0.016 (0.021) |
−0.023 (0.021) |
0.040 (0.034) |
−0.090** (0.031) |
| Husband (Actor 2) | ||||||||
| Husband becomes caregiver for wife (ζ2 | −0.354† (0.182) |
−0.215 (0.205) |
0.518* (0.247) |
0.487* (0.240) |
0.028 (0.125) |
−0.174 (0.157) |
0.170 (0.197) |
−0.313 (0.195) |
| Wife’s MoCA-SA (ϕ1→2) | −0.006 (0.015) |
−0.014* (0.018) |
−0.017 (0.017) |
0.018 (0.017) |
0.003 (0.010) |
0.000 (0.013) |
0.015 (0.016) |
0.007 (0.016) |
| Wife’s MoCA-SA × Husband becomes caregiver for Wife (ϕ1→2→2) | 0.006 (0.038) |
0.087 (0.059) |
−0.198*** (0.059) |
−0.052 (0.050) |
−0.009 (0.040) |
−0.044 (0.045) |
0.096 (0.062) |
0.036 (0.039) |
Note. MoCA-SA: Montreal Cognitive Assessment – Survey Adapted. Covariates included in all models. The outcome variables have been standardized so that the coefficient can be interpreted in standard deviation units. The complete table including the coefficients for all the variables can be found in supplementary materials.
p < 0.1,
p < 0.05,
p < 0.01,
p < 0.001 (two-tailed tests).
Gender differences in the associations between caregiving and well-being were insignificant for every outcome (see Supplementary Table 5) and are not presented individually. Husbands and wives did not differ in the moderating effect of spouse’s cognitive ability on most caregiver outcomes (Supplementary Table 5); results are presented individually for outcomes with significant associations.
Mental Health, Social Activities and Social Support.
Depressive symptoms.
As shown in Table 3, associations between caregiving and depressive symptoms were not significant for caregiving wives, regardless of their husbands’ MoCA-SA scores. On the other hand, a negative association between caregiving and depressive symptoms for caregiver husbands was large (see Table 3) but failed to achieve statistical significance (β = −0.354, p<0.1) at wives’ average MoCA-SA scores (i.e., after controlling for wives’ MoCA-SA scores). Wive’s MoCA-SA score did not moderate the effect of husband’s caregiving on his depressive symptom score (β = 0.006, n.s.).
Loneliness.
No associations were observed between caregiving and loneliness for either husbands or wives at average levels of their partners’ MoCA-SA scores. Nor did the spouse’s cognitive ability moderate the effect of caregiving on loneliness for either husbands or wives.
Anxiety.
For husbands, a significant positive association was observed between caregiving and anxiety at wives’ average MoCA-SA score (β = 0.518, p = .036). The moderation effect was also significant, where the impact of caregiving on the husband’s anxiety decreased at higher levels of the wife’s MoCA-SA (β = −0.198, p<0.001). For instance, at a wife’s average MoCA-SA score of 24, the husband’s caregiving was only weakly and insignificantly related to changes in his anxiety (β = 0.30, SE=0.23, p=0.18). However, when the wife’s cognitive ability was below average, the effect of caregiving was significant. For example, when the wife’s MoCA-SA score was 20, the husband’s caregiving was associated with a 1.2 standard deviation increase in his anxiety (SE=0.36, p < 0.001). Table 4 presents the association of husband’s caregiving with anxiety as a function of the wife’s MoCA-SA. We did not observe a caregiving association with anxiety for wives, nor was the moderation effect significant. The gender difference in the moderation effect was sizeable (β = 0.144, SE=0.078), but only approached statistical significance (p=0.065) (see Supplementary Table 5).
Table 4.
Predicted Change in Husbands’ Anxiety Associated With Moving Into a Caregiving Role by Wive’s MoCA-SA score.
| Predicted Effect on Husband’s Anxiety | |||
|---|---|---|---|
| Wife’s MoCA-SA | Effect (SD units) |
Standard Error |
p |
| 20 (mean – 1 SD) | 1.16 | 0.36 | <0.001 |
| 24 (mean) | 0.30 | 0.23 | 0.18 |
| 28 (mean + 1 SD) | −0.56 | 0.28 | 0.05 |
Note. MoCA-SA: Montreal Cognitive Assessment – Survey Adapted.
SD: Standard Deviation.
Perceived Stress.
For both wives and husbands, caregiving was associated with sizeable increases in perceived stress; changes in perceived stress between waves were about half a standard deviation greater in the caregiving than the non-caregiving groups of wives (β = 0.557, p<0.001) and husbands (β = 0.487, p<0.001). These associations did not differ significantly between men and women. Also, these effects were not moderated by the partner’s MoCA-SA score.
Social activities.
Caregiving was not associated with changes in religious service attendance or social engagement, nor did cognitive limitations moderate associations of caregiving with these outcomes.
Social support.
Caregiving was not associated with changes in family or friend support for husbands or wives at average levels of the spouse’s MoCA-SA score. However, the association between caregiving and the wife’s friend support varied with the husband’s cognitive ability (β = −0.090, p < 0.01). As shown in Table 5, if the husband MoCA-SA score was 19, an indicator of low cognitive ability, providing care for the husband was associated with increase of wife’s (caregiver) friend support by, on average, 0.38 standard deviations (SE=0.16, p=0.02). Providing care for a husband with average cognitive ability, however, exerted no significant effects. For example, if the husband had a MoCA-SA score of 23, caregiving was not significantly related to wife’s friend support (β = 0.08, SE=0.16, p=0.6). The moderating effect was not evident for husband’s friend support as the wife’s cognitive ability declined, and the difference between husbands and wives in this effect was significant, β = −0.126, SE=0.051, p < .014 (see Supplementary Table 5).
Table 5.
Predicted Change in Wives’ Friend Support Associated With Moving Into a Caregiving Role by Husbands’ MoCA-SA Score.
| Predicted Effect on Wife’ Friend Support | |||
|---|---|---|---|
| Husband’s MoCA-SA | Effect (SD units) |
Standard Error |
p |
| 19 (mean – 1 SD) | 0.38 | 0.16 | 0.02 |
| 23 (mean) | 0.08 | 0.16 | 0.6 |
| 27 (mean + 1 SD) | −0.22 | 0.22 | 0.33 |
Note. MoCA-SA: Montreal Cognitive Assessment – Survey Adapted.
SD: Standard Deviation.
Covariates.
Associations between well-being and all covariates are provided in Supplementary Table 5. Notably, functional limitations were also associated with outcomes independent of the associations seen with cognitive ability. For wives and husbands, an increase in their number of functional limitations was associated with an increase in their own depressive symptoms, and for husbands, an increase in their wife’s functional limitations was independently associated with more depressive symptoms. That is, there is a self (actor) and a spouse (partner) effect of increased functional limitations on husbands’ depressive symptoms. In addition, a decrease in social activity was evident for wives with more functional limitations; husbands’ functional limitations were generally not associated with social activity.
Sensitivity Analysis.
The non-caregiving group included some who became caregivers for someone other than a spouse (N=68). We repeated the MAPIM excluding these individuals and found that results were substantively unchanged (see Supplementary Table 6). Two additional effects were observed. First, wives who transition into spousal caregiving are lonelier than non-caregivers, and second, husbands report greater family support at higher levels of wives’ cognitive functioning.
Discussion
In this study, we sought to better understand how the early transition to spousal caregiving among older adult couples was related to changes in caregiver well-being, and whether the cognitive limitations in the cared-for spouse modified the associations in a nationally-representative sample. We employed a novel analytic strategy that extends the typical actor-partner interdependence model. Specifically, APIM sets up an interdependent system, and we introduced a “shock” variable (i.e., becoming a caregiver) and examined how its impact is affected by key system variables (e.g., cognitive ability). Our use of a nationally representative sample provides normative data not inferable from clinical and convenience samples that have typically been used in caregiving research (Pinquart & Sorensen, 2003).Whereas prior research has typically conducted cross-sectional comparisons of caregivers and non-caregivers, we compared new spousal caregiver dyads to those who never provided care and to those who provided care to another person. As hypothesized, we found that becoming a caregiver was associated with a decrease in well-being. For instance, in comparison to married people who did not experience a transition to spousal caregiving, wives and husbands who became spousal caregivers reported significantly greater perceived stress, an indicator of caregiver burden (Pearlin et al., 1990). In addition, for husbands, the transition to the caregiver role was associated with significantly more anxiety. Contrary to our hypothesis, the effects of caregiving on well-being did not differ by gender. Differences between husbands and wives were large (0.2 – 0.4 SDs) for some outcomes (e.g., depression, loneliness, anxiety, social engagement, friend support), suggesting that our sample of new caregivers was likely too small to produce precise estimates that would allow us to detect significant differences. Additional research and larger samples of caregivers are needed to examine gender differences in well-being and their potential sources. Because men and women may adjust to caregiving differently, a more comprehensive set of outcomes may need to be included to detect aspects of well-being that are differentially affected in husbands and wives during early phases of spousal caregiving.
Also contrary to our hypothesis, depressive symptoms did not increase significantly more in those who became caregivers than those who remained non-caregivers. Given the consistency with which depressive symptoms have been associated with caregiving in the literature, our inability to detect this association may result from our study design. We included a heterogeneous group of care recipients; some required help due to physical limitations, others cognitive limitations, and still others had both deficits. It is possible that caring for someone with physical limitations was more or less likely to elicit depression than caring for a spouse with cognitive limitations.
Changes in social activity and religious service attendance over the 5-year interval did not differ significantly between those who did versus did not become caregivers, at least not at average levels of cognitive ability. This is consistent with prior research (Queen et al., 2013), but is likely a phenomenon restricted to the early caregiving period. As mobility declines, and especially as cognition declines, social activity becomes more difficult for both the patient and the spousal caregiver. More frequent follow-up assessments over a longer period are necessary to better understand how caregivers and their spouses modify their social lives as limitations increase, and whether changes in social activity are reflected in levels of loneliness and depression, for example.
Consistent with our hypothesis, the cognitive ability of care recipients moderated the association between caregiving and well-being in spousal caregivers. Moreover, the moderating effects of recipients’ cognitive ability added to the effects of recipients’ physical impairment on caregiver well-being. Gender differences appeared not in the direct effects of caregiving on outcomes but in the aspect of well-being that was susceptible to moderation by cognitive limitations. Specifically, whereas wives experienced a significant increase in support from friends at lower levels of spouses’ cognitive ability, husbands did not. This is consistent with research showing that husbands derive most of their support from wives, whereas wives get most of their support from friends and children (McLaughlin, Vagenas, Pahana, Begum, & Dobson, 2010). According to Pearlin’s stress process model, our data suggest that one of the reasons husbands experience poor well-being when caring for a cognitively impaired spouse is that they are losing or have lost their primary source of support and they lack a larger support network of friends that could help ameliorate the stress of caregiving. Social support has known benefits to caregiver well-being but if support is less easily accessed or less available at the very time that caregiving husbands most need it, they will not derive those benefits. This finding warrants additional research to determine whether providing some type of support helps caregiving husbands manage caregiving stress, particularly in the context of caring for a wife with cognitive limitations.
Gender differences also appeared in the direct effects of spousal cognitive ability. For those who had not become caregivers, lower levels of the wife’s cognitive ability were significantly and positively associated with the husband’s loneliness, whereas the husband’s cognitive ability was not associated with the wife’s loneliness. In the case of anxiety, spousal cognitive ability had a direct effect on anxiety in non-caregiving wives but not husbands. These data suggest that simply living with a partner with cognitive limitations is anxiety-provoking and/or loneliness-inducing. These findings support common wisdom; spousal cognitive decline is distressing even in the absence of caregiving responsibilities.
Implications & Limitations
We found that the moderating effects of cognitive limitations are dose dependent. Our use of a continuous measure of cognitive ability and a nationally representative sample of older adults reveals that caregiving begins to take its toll on well-being at fairly modest levels of the recipient’s cognitive limitations. The respondents in our sample of caregivers had transitioned to caregiving for a variety of spousal recipient needs (different types of physical, mental, or emotional needs), each of which may pose their own unique challenges, but our data indicate that increasingly severe declines in cognitive ability add to challenges imposed by physical impairments and have adverse health and social consequences for the caregiver. NSHAP does not obtain data on the nature of the care challenges posed by spouses with poor cognitive ability, however; spouses with poor cognitive ability who exhibit behavioral problems (e.g., disorientation, disruptive behavior, aggression) have been shown to be particularly difficult for caregivers, such that the effect on various aspects of caregiver well-being may be greater if the care recipient exhibits such behaviors (Cheng, 2017; Pinquart & Sorensen, 2003; Pozzebon, Douglas, & Ames, 2016). Additional research is needed to determine how different aspects of care recipients’ cognitive dysfunction affect caregiver outcomes, and how different types of formal and informal supports are best deployed to help caregivers manage their task.
NSHAP lacks information on duration of caregiving. Some outcomes (e.g., perceived stress - a “primary” stressor as per Pearlin’s model) may be affected soon after adoption of the caregiver role, whereas others may take longer to manifest (e.g., physical health). Our results collapse across months and up to 5 years of caregiving responsibilities in examining outcomes. A 5-year interval may not be an appropriate period to detect effects for some respondents who only recently transitioned to caregiving. For others, however, the transition happened up to 4 or 5 years earlier. We note that those who became spousal caregivers, relative to those who did not, differed in perceived stress and, in the case of women, anxiety at baseline. Other outcomes tended to exhibit the same pattern of differences, suggesting that well-being was affected before respondents declared themselves caregivers. Greater temporal resolution is needed to assess when spouses determine and declare that they are caregivers, and how long it takes for the challenge of caregiving to manifest in various mental health and social outcomes. In addition, we acknowledge that the perceived stress scale exhibited relatively low internal reliability in our sample (Cronbach’s alpha<0.6), a finding that has been documented previously (Payne et al., 2014), and indicates that more work is needed to understand how to improve the measurement of stress to reliably capture its diverse manifestations in this population.
Some husbands and wives may have been living with and ostensibly caring for a significantly cognitively and/or physically impaired spouse yet did not report that they were providing care, either because they relied on formal care for their spouse or because they have a higher threshold for defining themselves as caregivers. To the extent this was the case, some caregiving couples may have been misclassified as non-caregiving, and our results may underestimate the cost of caregiving for mental health and social relationships. Moreover, our study does not address individual differences in coping with and becoming habituated to the caregiver role, and how these differences manifest in temporal trajectories of well-being in older age spousal caregivers. These are topics for future research and may point to the most opportune times to intervene and reduce caregiver stress.
Our results may be subject to selection bias. For instance, men with a heavy comorbidity burden were disproportionately more likely to become spousal caregivers than healthier men. Older men were also disproportionately over-represented among men who became caregivers, and older men are more likely to experience a heavy load of chronic conditions. The fact that the most vulnerable men were more likely to become caregivers and that these vulnerabilities place individuals at risk of poor mental health and social relationships suggests that husbands’ outcomes may be attributable, in part, to differences that existed prior to assuming a caregiving role. We note also that attrition of couples between waves was often caused by the morbidity or mortality of one or both partners (results available upon request). Although we weighted the data to account for respondent drop-out, differential drop-out may nevertheless bias our results.
Finally, although we examined a wide range of caregiver outcomes, we did not consider possible positive outcomes. Spousal caregiving can have positive outcomes (Cunningham, Cunningham, & Roberson, 2018), including improving marital satisfaction and providing a sense of meaning and purpose. Positive outcomes may be independent of negative outcomes (e.g., caregivers can derive purpose from their role while they nevertheless feel anxious or lonely), but they may also attenuate the negative effects of partners’ cognitive limitations. Moreover, men and women may derive different benefits from the caregiving role. These issues require additional research.
Conclusion
Spousal caregiving is widely known to affect health and well-being, and effects may be exacerbated when the partner is cognitively impaired. We found that aspects of caregivers’ mental health and social relationships exhibit a dose-dependent worsening that begins at modest levels of spousal cognitive dysfunction and is independent of physical impairments that contribute to the need for care. This new knowledge about the transition to spousal caregiving in a nationally representative sample suggests that interventions to assist spouses should be considered even before the partner receives a diagnosis of MCI or dementia. Cognitive reframing of caregiver burden and support group interventions have proven effective in improving depression, anxiety, and perceived stress among dementia caregivers (Adelman, Tmanova, Delgado, Dion, & Lachs, 2014). Providing interventions to spousal caregivers of partners with even modest cognitive limitations may reduce the severity of caregiver consequences as cognition worsens and increases the caregiving burden. Notably, beneficial effects of interventions on psychosocial outcomes are evident even when the objective caregiving burden remains unchanged (Adelman et al., 2014). The growing proportion of older adults in US society will probably mean more physically and/or cognitive impaired older adults, along with a growing population of older adult spousal caregivers (Timonen, 2009). Risk for cognitive decline and impairment increases with age, as does the likelihood of becoming a spousal caregiver. Greater use should be made of population-based samples to better understand how the transition to the spousal caregiver role is experienced in rapidly aging societies.
Supplementary Material
Acknowledgments
This research was supported in part by grants from the National Institute on Aging and the National Institute of Health (R37-AG030481; R01-AG033903; R01-AG043538; R01-AG048511; R37-AG030481). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Again, like the moderation effects, these tests involve the coefficients, sampling variances of the coefficients (the square root of which is the standard error), and the sampling covariances.
Contributor Information
Louise Hawkley, Academic Research Centers, National Opinion Research Center (NORC) at the University of Chicago, Illinois.
Boyan Zheng, Academic Research Centers, NORC at the University of Chicago, Illinois.
E. C. Hedberg, Academic Research Centers, NORC at the University of Chicago, Illinois
Megan Huisingh-Scheetz, Department of Medicine, Section of Geriatrics and Palliative Medicine, University of Chicago, Illinois.
Linda Waite, Department of Sociology, University of Chicago, Illinois.
References
- Adelman RD, Tmanova LO, Delgado D, Dion S, & Lachs MS (2014). Caregiver burden: A clinical review. JAMA, 311 (10), 1052–1059. [DOI] [PubMed] [Google Scholar]
- Aiken LS, & West SG (1991). Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, California: Sage Publications, Inc. [Google Scholar]
- Artero S, Touchon J, & Ritchie K. (2001). Disability and mild cognitive impairment: A longitudinal population-based study. International Journal of Geriatric Psychiatry, 16, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Blieszner R, & Roberto KA (2010). Care partner responses to the onset of mild cognitive impairment. The Gerontologist, 50, 11–22. [DOI] [PubMed] [Google Scholar]
- Braun M, Scholz U, Bailey B, Perren S, Hornung R, & Martin M. (2009). Dementia caregiving in spousal relationships: A dyadic perspective. Aging and Mental Health, 13, 426–436. [DOI] [PubMed] [Google Scholar]
- Burton LC, Zdaniuk B, Schulz R, Jackson S, & Hirsch C. (2003). Transitions in spousal caregiving. The Gerontologist, 43, 230–241. [DOI] [PubMed] [Google Scholar]
- Calasanti T. (2010). Gender relations and applied research on aging. The Gerontologist, 50, 720–734. doi: 10.1093/geront/gnq085. [DOI] [PubMed] [Google Scholar]
- Cannuscio CC, Jones C, Kawachi I, Colditz GA, Berkman L, & Rimm E. (2002). Reverberations of family illness: A longitudinal assessment of informal caregiving and mental health status in the Nurses’ Health Study. American Journal of Public Health, 92, 1305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlozzi NE, Sherman CW, Angers K, Belanger MP, Austin AM, & Ryan KA (2018). Caring for an individual with mild cognitive impairment: A qualitative perspective of health-related quality of life from caregivers. Aging & Mental Health, 22, 1190–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng ST, (2017). Dementia caregiver burden: A research update and critical analysis. Current Psychiatry Reports, 19, 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, & Williamson G. (1988). Perceived stress in a probability sample of the U.S In Spacapam S & Oskamp S. (Eds.), The Social Psychology of Health: Claremont Symposium on Applied Social Psychology (pp. 31–67). Newbury Park, CA: Sage. [Google Scholar]
- Cunningham NA, Cunningham TR, Roberson JM (2018). Understanding and measuring the wellbeing of carers of people with dementia. Gerontologist. Advance access publication, doi: 10.1093/geront/gny018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedrich RJ (1982). In defense of multiplicative terms in multiple regression equations. American Journal of Political Science, 26, 797–833. [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, & Newcomer R. (2005). The longitudinal effects of early behavior problems in the dementia caregiving career. Psychology and Aging, 20, 100–116. [DOI] [PubMed] [Google Scholar]
- Gibbons C, Creese J, Tran M, Brazil K, Chambers L, Weaver B, & Bédard M. (2014). The psychological and health consequences of caring for a spouse with dementia: A critical comparison of husbands and wives. Journal of Women & Aging, 26, 3–21. [DOI] [PubMed] [Google Scholar]
- Hajek A & König H-H (2018). Impact of informal caregiving on loneliness and satisfaction with leisure-time activities. Findings of a population-based longitudinal study in Germany. Aging & Mental Health, DOI: 10.1080/13607863.2018.1506739. [DOI] [PubMed] [Google Scholar]
- Hoppmann C, & Gerstorf D. (2009). Spousal interrelations in old age - A mini-review. Gerontology, 55, 449–459. [DOI] [PubMed] [Google Scholar]
- Hsieh N, & Hawkley L. (2018). Loneliness in the older adult marriage: Associations with dyadic aversion, indifference, and ambivalence. Journal of Social and Personal Relationships, 35(10), 1319–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26, 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, & Jaffe MW (1963). Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. The Journal of the American Medical Association, 185, 914–919. doi: 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, & Cook WL (2006). The Analysis of Dyadic Data. New York: Guilford. [Google Scholar]
- Kotwal AA, Schumm LP, Kern DW, McClintock MK, Waite LJ, Shega JW, Huisingh-Scheetz M,J & Dale W. (2016). Evaluation of a brief survey instrument for assessing subtle differences in cognitive function among older adults. Alzheimer Disease & Associated Disorders, 29, 317–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavela SL, & Ather N. (2010). Psychological health in older adult spousal caregivers of older adults. Chronic Illness, 6, 67–80. [DOI] [PubMed] [Google Scholar]
- Lohr S. (2009). Sampling: Design and Analysis. Washington, DC: Nelson Education. [Google Scholar]
- McLaughlin D, Vagenas D, Pachana NA, Begum N, & Dobson A. (2010). Gender differences in social network size and satisfaction in adults in their 70s. Journal of Health Psychology, 15, 671–679. [DOI] [PubMed] [Google Scholar]
- Monin J, Doyle M, Van Ness PH, Schulz R, Marottoli RA,...& Kershaw T. (2018). Longitudinal associations between cognitive functioning and depressive symptoms among older adult spouses in the Cardiovascular Health Study. American Journal of Geriatric Psychiatry, 26, 1036–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NAC & AARP (2015). Caregiving in the U.S. 2015 - Focused Look at Caregivers of Adults Age 50+. National Alliance for Caregiving and the AARP Public Policy Institute; https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf. accessed June 27, 2019. [Google Scholar]
- Nosheny RL, Camacho MR, Insel PS, Flenniken D, Fockler J,.& Weiner MW (2018). Online study partner-reported cognitive decline in the Brain Health Registry. Alzheimer’s and Dementia, 4, 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Muircheartaigh C, Eckman S, & Smith S. (2009). Statistical design and estimation for the National Social Life, Health and Aging Project (NSHAP). Journals of Gerontology: Psychological Sciences and Social Sciences, 64, i 12–i 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Muircheartaigh C, English N, Pedlow S, & Kwok PK (2014). Sample design, sample augmentation, and estimation for Wave 2 of the NSHAP. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(Suppl_2), S15–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradise M, McCade D, Hickie IB, Diamond K, Lewis SJG, & Naismith SL (2015). Caregiver burden in mild cognitive impairment. Aging &Mental Health, 19, 72–78, doi: 10.1080/13607863.2014.915922. [DOI] [PubMed] [Google Scholar]
- Payne C, Hedberg EC, Kozloski M, Dale W, & McClintock MK (2014). Using and interpreting mental health measures in the National Social Life, Health, and Aging Project. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(Suppl_2), S99–S116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: an overview of concepts and their measures. Gerontologist, 30, 583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, & Sorensen S. (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. Journals of Gerontology: Psychological Sciences, 58B, P112–P128. [DOI] [PubMed] [Google Scholar]
- Pöysti MM, Laakkonen M-L, Strandberg T, Savikko N, Tilvis RS,... ,& Pitkälä KHY. (2012). Gender differences in dementia spousal caregiving. International Journal of Alzheimer’s Disease, Article ID 162960. doi: 10.1155/2012/162960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pozzebon M, Douglas J, & Ames D. (2016). Spouses’ experience of living with a partner diagnosed with a dementia: A synthesis of the qualitative research. International Psychogeriatrics, 28, 537–556. [DOI] [PubMed] [Google Scholar]
- Queen TL, Butner J, Berg CA, & Smith J. (2017). Activity engagement among older adult caregivers. Journals of Gerontology: Social Sciences. doi: 10.1093/geronb/gbx106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Schulz R, & Beach SR (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. Journal of the American Medical Association, 282, 2215–2219. [DOI] [PubMed] [Google Scholar]
- Schulz R, & Eden J, Eds. (2016). Older adults who need caregiving and the family caregivers who help them In Families Caring for an Aging America (pp. 43–72). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Schulz R, & Sherwood PR (2008). Physical and mental health effects of family caregiving. Journal of Social Work Education, 44, suppl. 3, 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeher K, Low L-F, Reppermund S, & Brodaty H. (2014). Predictors and outcomes for caregivers of people with mild cognitive impairment: A systematic literature review. Alzheimer ‘s & Dementia, 9, 346–355. [DOI] [PubMed] [Google Scholar]
- Shega JW, Sunkara PD, Kotwal A, Kern DW, Henning SL, McClintock MK, ... & Dale W. (2014). Measuring cognition: the Chicago Cognitive Function Measure in the National Social Life, Health and Aging Project, wave 2. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(Suppl_2), S166–S176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder CM, Fauth E, Wanzek J, Piercy KW, Norton MC, ... & Tschanz JT (2015) Dementia caregivers’ coping strategies and their relationship to health and well-being: the Cache County Study. Aging & Mental Health, 19:5, 390–399. DOI: 10.1080/13607863.2014.939610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomi VL, & Casiday RE (2017). In sickness and in health: The strains and gains of caring for a chronically ill or disabled spouse. Chronic Illness, 13, 75–87. [DOI] [PubMed] [Google Scholar]
- Sugiura K, Ito M, Kutsumi M, & Mikami H. (2009). Gender differences in spousal caregiving in Japan. Journals of Gerontology: Social Sciences, 64B, 147–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinkels J, Van Tilburg T, Verbakel E, & Broese van Groenou M. (2017). Explaining the gender gap in the caregiving burden of partner caregivers. Journals of Gerontology: Psychological Sciences & Social Sciences, Epub ahead of print, doi: 10.1093/geronb/gbx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timonen V. (2009). Toward an integrative theory of care: Formal and informal intersections In Mancini JA & Roberto KA (Eds.), Pathways of Human Development: Explorations of Change (pp. 307–326). Lanham, Maryland, US: Lexington Books. [Google Scholar]
- Tooth L, Russell A, Lucke J, Byrne G, Lee C, Wilson A, & Dobson A. (2008). Impact of cognitive and physical impairment on carer burden and quality of life. Quality of Life Research 17, 267–273. [DOI] [PubMed] [Google Scholar]
- Vasilopoulos T, Kotwal A, Huisingh-Scheetz MJ, Waite LJ, McClintock MK, & Dale W. (2014). Comorbidity and chronic conditions in the national social life, health and aging project (NSHAP), Wave 2. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(Suppl_2), S154–S165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong JS, & Hsieh N. (2017). Functional status, cognition, and social relationships in dyadic perspective. The Journals of Gerontology: Series B. Advance access publication. doi : 10.1093/geronb/gbx024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.