Abstract
Exercise is an efficacious intervention for mental and physical health, but few studies have identified the additive benefits of exercise prescriptions for those undergoing empirically-supported psychosocial treatment. Behavioral activation (BA) involves completing activities to improve mood, an ideal format for exercise augmentation. The purpose of this study was to examine the credibility and exploratory effect size estimates of augmenting BA with exercise.
Thirty-one sedentary, depressed patients were randomized to receive nine sessions of BA+exercise or BA+stretching over 12 weeks. Monthly assessments of depression, quality of life, distress intolerance (DI), perceived stress, and exercise were conducted.
Results demonstrated strong credibility and completion rates of BA+exercise, comparable to other PA interventions. Randomization did not contribute to differential exercise between conditions; all participants engaged in more exercise over time. Similarly, all participants significantly improved on all outcomes over time. Condition differences emerged for DI and perceived stress; the exercise condition evidenced greater improvements over time. Participants who engaged in more exercise also evidenced greater and faster declines in depression.
BA may be a useful strategy for improving depression and increasing exercise. Additional explicit exercise prescriptions may not be necessary to improve depression but may be helpful for DI and stress.
Clinical Trials Registry (clinicaltrials.gov): NCT02176408, “Efficacy of Adjunctive Exercise for the Behavioral Treatment of Major Depression”
Keywords: depression, behavioral activation, exercise, physical activity, distress intolerance
Introduction
Repeated meta-analyses support the efficacy of exercise interventions for major depression, with findings of moderate to large effect sizes relative to control conditions (Kvam, Kleppe, Nordhus, & Hovland, 2016; Schuch et al., 2016; Stathopoulou, Powers, Berry, Smits, & Otto, 2006), but there are some indications these effect sizes may be somewhat inflated due to risk of bias in some studies (Cooney et al., 2013). In addition, there is reliable evidence that exercise interventions significantly reduce stress anxiety symptoms, and anxiety sensitivity/distress intolerance, although fewer of these trials target outpatients in mental health clinics (Jacquart et al., 2019; LeBouthillier and Asmundson, 2017; Stubbs et al., 2017). The success of these interventions encourages further investigation of ways in which PA can be used to augment existing treatments.
Combining exercise with behavioral activation (BA)--an empirically-supported treatment aimed at engaging patients in rewarding, adaptive activities through activity scheduling (Cuijpers, van Straten, & Warmerdam, 2007)-- may provide a useful context for introducing exercise into more-standard clinical practice. BA has been shown to enhance overall well-being (Mazzucchelli, Kane, & Rees, 2010) and reduce depression symptoms with similar effect sizes to both cognitive therapy and antidepressant medication (Dimidjian et al., 2006; Richards et al., 2016). Accordingly, the integration of exercise into BA may provide a useful way to add efficacy to an established treatment, as has been observed in the initial study of the addition of exercise to exposure therapy for anxiety-related disorders (Merom et al., 2008; Powers et al., 2015).
Initial studies of the combined use of BA and exercise have investigated web-delivered, self-help interventions, with initial findings supporting both the feasibility and efficacy of this strategy for improving both major depressive disorder (Pentecost et al., 2015) and elevated depression symptoms (Lambert et al., 2018). To our knowledge, the only published trial of the in-person combination of BA and exercise was a 6-month pilot trial consisting of 29 patients with comorbid MDD and Type 2 diabetes, in which behavioral activation plus a group exercise intervention significantly lowered depression scores over time relative to an enhanced usual care control condition (Schneider et al., 2016).
The current study was designed to further examine the pairing of BA and exercise for improvement of depressed mood and overall functioning in the unique setting of the combination of in-person, individual treatment, with incorporation of strategies to enhance adherence and remove barriers for exercise. Our goal for this study was to establish the credibility of a combination in-person treatment with effect size estimates complemented by traditional significance testing to characterize response to this combined intervention for future investigations. We hypothesized that the intervention would be credible and acceptable based on engagement and dropout rates and credibility ratings. Further, we hypothesized that depressed individuals receiving BA plus exercise would engage in more exercise and be less depressed following the 12-week intervention than those in a BA plus stretching active control. In addition, we hypothesized that distress intolerance and perceived stress would be reduced significantly in the exercise condition.
Material and Methods
Participants
Depressed, sedentary adults were recruited from the community through internet advertisements, flyers, and referrals from clinics to participate in a randomized, controlled clinical trial (clinicaltrials.gov identifier: NCT02176408; “Efficacy of Adjunctive Exercise for the Behavioral Treatment of Major Depression”). Interested participants were screened over the phone, and if preliminary eligibility requirements were met, were scheduled for an in-person diagnostic and medical evaluation. Inclusion criteria were the following: (1) males or females ages 18-65; (2) current principal diagnosis of MDD or persistent depressive disorder (PDD) with a current major depressive episode as determined by the Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown and Barlow, 2014); and (3) sedentary (moderate-intensity exercise less than two days per week for at least 30 minutes each time for at least three months, matching other trials in the field, e.g., Swift et al., 2012; Trivedi, Greer, Grannemann, Chambliss, & Jordan, 2006) as assessed on phone screen and at screening visit.
Psychiatric exclusion criteria included current or past psychotic disorders, bipolar disorder (1, II, or unspecified), schizoaffective disorder, anorexia, bulimia, alcohol or drug dependence within the last three months, or high suicide risk as evaluated by the Columbia Suicide Severity Rating Scale (C-SSRS; Posner, Oquendo, Gould, Stanley, & Davies, 2007; endorsing yes to items 4 or 5) and Beck Depression Inventory-II (Beck, Steer, & Brown, 1996) suicide item (≥ score of 2).
Medical exclusion criteria included risk for exercise engagement according to Physical Activity Readiness Questionnaire (PAR-Q) in accordance with guidelines set forth by the American College of Sports Medicine (ACSM) as well as assessment by the study physician. Other exclusion criteria included individuals who have participated in CBT for a mood disorder within three months of baseline, those simultaneously participating in another psychosocial treatment (other than supportive therapy) or those taking psychotrophic medications (unless at eight weeks of stable dosage) as well as women who were currently pregnant, planned to be pregnant in the next year, or currently breastfeeding.
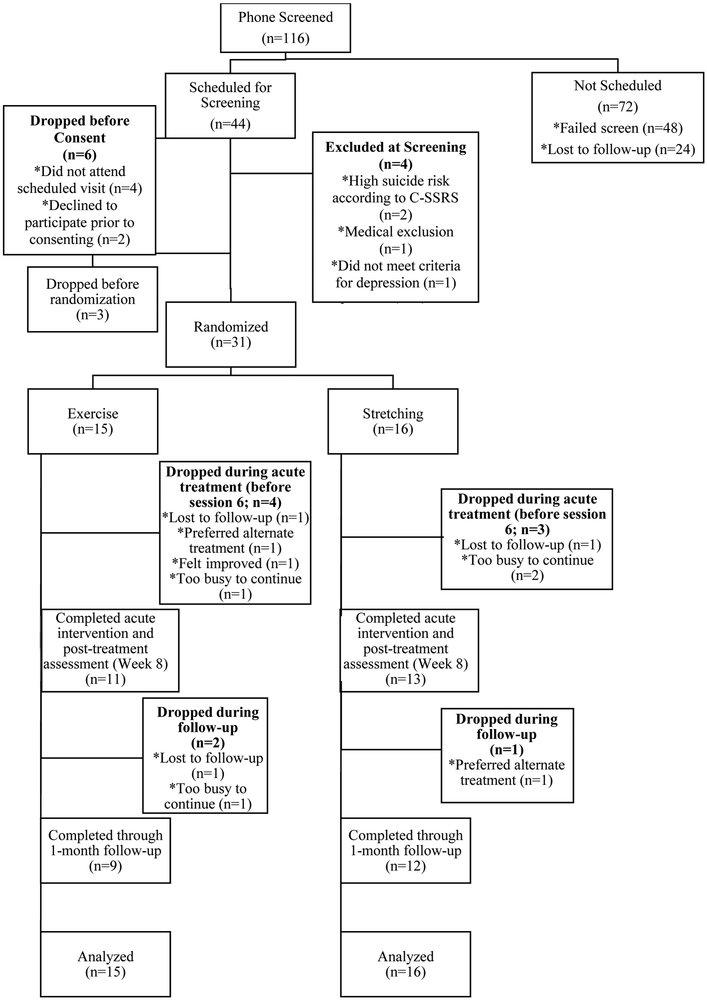
Participants were enrolled in the study at Boston University between July 2014 and April 2016 and all follow-up assessments were completed by August 2016. All study procedures were approved by the Institutional Review Board. A total of 38 individuals were enrolled in the study and 34 met inclusion criteria. Thirty-one individuals were randomized to either exercise (n=15) or stretching (n=16) augmentation, with randomization occurring immediately prior to participation in Week 1 of treatment, in a parallel design with a 1:1 allocation ratio. No block assignments were used in randomization. The first author generated random allocation sequence, enrolled participants, and assigned participants to intervention strictly following allocation sequence. All independent evaluators were blind to randomization assignment as they did not take part in delivering treatment or random assignments. Figure 1 summarizes participant flow throughout the study. Informed consent was obtained from all participants before the start of study procedures.
Figure 1.
CONSORT diagram
Assessments
Assessments were completed at baseline and weeks 4, 8, and 12 (endpoint) of treatment and at week 16 (1-month follow-up).
Outcome expectancy and credibility was assessed by the Credibility-Expectations Questionnaire (CEQ; Devilly and Borkovec, 2000), which was administered following the completion of the first treatment session and focused on credibility and expected outcome of the exercise or stretching augmentation strategy.
Independent evaluators, Master’s level clinicians, administered the Montgomery-Asberg Depression Rating Scale (MADRS; Montgomery and Asberg, 1979), a 10-item measure of depression severity with strong validity and inter-rater reliability and an α of 0.75 in the context of the present study. All independent evaluators were trained by the first author until reliability was established (>80% agreement on items) and were blind to condition.
Self-reported depression, functional impairment, quality of life, distress intolerance, and perceived stress were assessed by the Beck Depression Inventory-II (Beck, et al., 1996; α = 0.87), the Work and Social Adjustment Scale (WSAS; Mundt, Marks, Shear, & Greist, 2002; α = 0.77), the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q; Endicott, Nee, Harrison, & Blumenthal, 1993; α = 0.82), the Distress Intolerance Index (DII; McHugh and Otto, 2012; α = 0.90), and the Perceived Stress Scale (PSS; Cohen and Williamson, 1988; α = 0.78), respectively.
Exercise and stretching were assessed via the 7-Day Physical Activity Recall (PAR; Blair et al., 1985), an interviewer-administered, timeline follow-back measure of amount of minutes of vigorous and moderate intensity exercise and stretching, which has been shown to be sensitive to change in studies of moderate-intensity activity (Dunn, Andersen, & Jakicic, 1998). Metabolic equivalents (METs) were calculated for both vigorous- and moderate-intensity exercise.
Interventions
Participants were randomized to receive either an exercise or stretching augmentation in addition to nine sessions of brief BA.
Behavioral activation
All participants received standard BA based on a modified version of the manualized treatment by Lejuez and colleagues (2011). Treatment was delivered by the first author (KLS) and 2 other doctoral graduate student clinicians in 60-minute weekly in-person, individual sessions over a 6-week period followed by 3 biweekly booster sessions. Sessions were audiotaped and reviewed in weekly supervision meetings with BA-trained clinicians. The first six sessions focused on the following topics: psychoeducation about depression with introduction to activity monitoring; identification of values and activities within several life areas; ranking activities in order of difficulty; scheduling activities; discussion of the role of social support in aiding with completion of activities; and relapse prevention. The concept of activity scheduling, introduced in Session 4, was practiced throughout the remainder of the treatment. Within activity scheduling, participants in both conditions were encouraged and required to identify activities outside of exercise or stretching to schedule. Exercise and stretching scheduling was specific to the subsequent half-hour augmentation sessions (described below). The biweekly booster sessions reviewed each of these concepts.
Exercise and stretching augmentations
Sessions dedicated to the exercise/stretching augmentation occurred immediately following each of the first six weekly BA sessions for 30 minutes each. Both interventions were provided by the same therapist providing BA. Sessions included providing rationale for the program, introducing new strategies to enhance adherence/reduce barriers adapted from Otto & Smits (2011), and/or reviewing the previous week’s progress. Participants were encouraged to perform a total of 150 minutes of moderate-intensity aerobic exercise (600 METs) or light stretching (including light yoga poses, but not intense forms of yoga) per week. Participants chose the type of exercise/stretching and set their own schedule for the week with guidance from the therapist. For the exercise condition, procedures to aid the enjoyment as outlined in Otto & Smits (2011), were provided. To match this guidance, participants in the stretching condition were provided with a 50-minute DVD of stretching techniques. Homework compliance for amount of exercise/stretching completed was rated by the study therapist at weeks 2-6, 8, 10, and 12 based on the coding system developed by Busch and colleagues (2010).
Statistical analysis
A sample size of 32 patients completing all 5 outcome assessments (i.e., MADRS) was determined to provide adequate power (80%) to detect effects at a medium effect size (d=0.50), conservatively estimated below the large effect size (d=1.42) for Stathopoulou et al. (2006), using a repeated measures ANOVA. Demographic and clinical differences between conditions at baseline were assessed via χ2 analyses or t-tests. Comparison of dropout rates by treatment condition was performed using a χ2 test. Logistic regressions predicting dropout based on credibility and expectancy were separately examined for the overall sample and including treatment condition as a covariate. Homework completion condition differences were examined in a linear regression. The random effects of treatment condition and time were examined on all randomized participants using a mixed-effects linear regression model with restricted maximum likelihood (REML) estimation methods and an unstructured variance-covariance matrix where all follow-up assessments (including 1-month follow-up) were entered as repeated dependent variables. Means and standard deviations are reported. All analyses were conducted using SPSS Version 24.0.
Results
Participant baseline characteristics
The randomized sample was 77% female with a mean age of 34.2 (±13.4) years. Fifty-eight percent of the sample was White, 23% was Asian, 6% was African American, and 13% designated race as other. Seven percent identified themselves as Hispanic/Latino(a). The majority of the sample (58%) had completed college, with another 36% completing some college. Primary diagnosis was MDD for 65% of the sample and PDD for the other 35%, with baseline depression severity at a moderate level (MADRS: M=26.1, SD=8.0). Seven individuals had co-principal diagnoses of either GAD (n=4; 13%) or social anxiety disorder (n=3; 10%) and several participants had secondary diagnoses (average number of diagnoses=2.6±1.3). Chi-square and t-tests did not reveal significant differences between conditions on demographic or clinical characteristics (all p>0.09); see Table 1 for study baseline clinical characteristics.
Table 1.
Clinical severity and exercise characteristics of the randomized sample at baseline assessment.
| Exercise Baseline N=15 Mean (SD) |
Week 12 N=9 |
Week 16 N=9 |
Stretching Baseline N=16 Mean (SD) |
Week 12 N=12 |
Week 16 N=12 |
|
|---|---|---|---|---|---|---|
| MADRS | 24.7 (8.1) | 12.9 (6.8) | 11.2 (7.5) | 27.3 (8.0) | 17.5 (10.0) | 16.0 (9.5) |
| BDI-II | 26.4 (10.9) | 11.2 (9.9) | 8.7 (9.5) | 26.7 (9.5) | 12.1 (10.5) | 13.2 (9.6) |
| WSAS | 24.8 (8.6) | 15.1 (13.2) | 10.7 (10.5) | 23.8 (7.6) | 17.1 (12.0) | 16.5 (12.5) |
| Q-LES-Q | 39.3 (7.6) | 48.8 (8.6) | 53.9 (9.0) | 39.7 (8.6) | 48.4 (11.0) | 45.5 (10.6) |
| DII | 17.4 (10.4) | 12.3 (8.9) | 5.6 (6.3) | 20.2 (7.3) | 13.9 (10.7) | 15.5 (12.5) |
| PSS | 25.1 (5.4) | 19.3 (6.6) | 13.7 (6.1) | 25.3 (6.2) | 21.3 (8.2) | 19.3 (7.2) |
| METs* | 279.5 (371.7) | 836.9 (586.8) | 752.9 (447.6) | 391 (414.7) | 644.7 (539.5) | 530.0 (515.0) |
| Stretching minutes | 8.0 (23.3) | 8.9 (20.3) | 2.5 (7.1) | 10.4 (15.2) | 84.9 (74.1) | 31.0 (53.5) |
Note. p values derived from χ2 tests for race and education and t-tests for all other comparisons. MADRS=Montgomery-Asberg Depression Rating Scale, BDI-II=Beck Depression Inventory-II, WSAS=Work and Social Adjustment Scale, Q-LES-Q=Quality of Life Enjoyment Questionnaire, DII=Distress Intolerance Index, PSS Perceived Stress Scale, METs=metabolic equivalents,
METs are calculated for combined vigorous & moderate intensity activity (self-reported for week prior to baseline).
Intervention credibility
Overall, patients reported high levels of both credibility (M=27.1 ±4.7, range from 18 to 35; questionnaire range from 4 to 36) and expectancy (M=12.6 ±3.1, range 6 to 18; questionnaire range from 2 to 18) for the effects of the randomized treatment on their depression symptoms. Proportions of individuals reporting 5 or higher (somewhat agree or above) were 96.9% (n=30) for the intervention’s logicality, 87.2% (n=27) for how successful the intervention would be in treating depression, and 100% were recommend this intervention to a friend. There were no differences between the exercise and stretching conditions on ratings of credibility of the intervention as assessed by the CEQ (t(29)= −0.79, p=0.44, d 0.29, Mean difference= −1.85, 95% CI: −6.7 to 3.0).
Acceptability, treatment completion, and dropout
To determine acceptability, we examined willingness to engage in the trial. These rates were determined by percentage of qualified individuals based on the phone screen who chose to sign consent and participate in the study. Two participants (5%) who attended the screening visit declined to participate prior to consenting. Another three participants (7.5%) discontinued participation following screening and/or baseline study visits. A total of 77.5% of participants who attended the in-person screening visit chose to enroll in the study through randomization.
Overall, participants completed an average of 6.9 (±3) sessions. As shown in Figure 1, six participants (4 during treatment and 2 during follow-up, 40% total) in the exercise condition and four (3 during treatment and 1 during follow-up, 25% total) in the stretching condition dropped out during the study. These dropout rates were not significantly different from each other (χ2(1)=0.78, p=0.37, d=0.32). Neither baseline credibility (Odds Ratio: Exp(B)=0.93, p=0.42) nor expectancy (Odds Ratio: Exp(B)=0.85, p=0.22) ratings significantly predicted dropouts in either of the randomized conditions or overall. Overall, 68% of sample completed the entire study including 1-month follow-up.
Homework completion
On average, participants had a homework completion rate of 77.1% (±15.8). Homework completion did not differ by condition (t(25)=1.15, p=0.26, d=0.44, Mean difference=6.95, 95% CI = −5.6 to 19.4).
Exercise and stretching outcomes
Evaluation of the effect of the randomized intervention conditions on exercise based on the PAR revealed no significant differences between the conditions on exercise completion over time (condition by time interaction: F(4, 21)=0.73, p=0.58, d=0.30); condition main effect: (F(1, 22)=0.78, p=0.39, d=0.31). See Supplemental Materials Figure 1 for more information. A significant effect for time indicated that participants, regardless of condition, performed more METs of vigorous- and moderate-intensity exercise over the course of the study at a level approaching a large effect size (F(4, 21)=4.66, p=0.008, d=0.76).
In contrast to the exercise data, a significant condition by time interaction (F(4, 23)=8.10, p<0.001, d=1.01) was found for the stretching measure, whereby the stretching condition completed more stretching over time than the exercise condition.
Effects of intervention on depression, functioning, and quality of life
In a mixed-effects linear regression model, there was a significant main effect of time for all participants (F(4, 21)=11.3, p<0.001, d=1.19), at a large effect size, for the MADRS (see Supplemental Materials Figure 2). There was no significant main effect of condition (F(1, 29)=0.88, p=0.36, d=0.33) or condition by time interaction (F(4, 21)=0.99, p=0.44, d=0.35). The small to moderate, non-significant effects in the direction of more improvement in the exercise condition versus the stretching condition over time.
When examining a mixed-effects linear regression, there was no significant condition by time interaction effect or main effect of condition for the BDI-II, Q-LES-Q, and WSAS (see Supplemental Materials Figures 3-5). However, patients significantly improved in all of these measures over time (BDI-II: F(4, 18)=10.77, p<0.001, d=1.16; Q-LES-Q: F(4, 20)=8.9, p<0.001, d=1.06; WSAS: F(4, 20)=6.1, p=0.004, d=0.87), with effect sizes in the large range.
Based on cutoff of BDI-II < 10 (used in Chalder et al., 2012), 39% of the total sample (n=12) met criteria for being in recovery from depression symptoms at 1-month follow-up. Of the 19 trial completers, 11 (55%) met criteria for recovery at 1-month follow-up. Fisher Exact Tests indicated no significant differences in rates of recovery by treatment condition (p=0.71).
Effects of intervention on distress intolerance and perceived stress
For the DII and PSS, there were significant condition by time interactions on the order of medium to large effect sizes (F(4, 22)=3.9, p=0.016, d=0.70) and (F(4, 21)=2.8, p=0.049, d=0.60), respectively, whereby those in the exercise condition improved more in DII and PSS over time (See Supplemental Materials Figures 6 and 7). Additionally, for all participants, DII (F(4, 22)=4.9, p=0.008, d=0.78) and PSS (F(4, 21)=8.8, p=0.001, d=1.05) significantly improved over time. There were no significant main effects of treatment for either the DII or PSS. Multiple regression analyses are summarized in Table 2.
Table 2.
Results of Multiple Regression Analyses: Condition, Time, and Interaction Effects for Each Outcome Measure
| Outcome | Condition F(df) |
d | Time F(df) |
d | Interaction F(df) |
d |
|---|---|---|---|---|---|---|
| Clinician-rated Depression: MADRS | 0.88 (1, 29) | 0.33 | 11.30 (4, 21)*** | 1.19 | 0.99 (4, 21) | 0.35 |
| Self-reported Depression: BDI-II | 0.007 (1, 22) | 0.23 | 10.77 (4, 18)*** | 1.16 | 1.39 (4, 18) | 0.42 |
| Quality of Life: Q-LES-Q | 0.54 (1, 26) | 0.26 | 8.92 (4, 20)*** | 1.06 | 1.94 (4, 20) | 0.49 |
| Functional Impairment: WSAS | 0.08 (1, 29) | 0.10 | 6.08 (4, 20)** | 0.87 | 1.24 (4, 20) | 0.39 |
| Distress Intolerance: DII | 0.16 (1, 26) | 0.14 | 4.85 (4, 22)** | 0.78 | 3.89 (4, 22)* | 0.70 |
| Perceived Stress: PSS | 0.32 (1, 31) | 0.20 | 8.78 (4, 21)*** | 1.05 | 2.85 (4, 21)* | 0.60 |
| METs | 0.78 (1, 22) | 0.31 | 4.66 (4, 21)** | 0.76 | 0.73 (4, 21) | 0.30 |
| Stretching minutes | 20.67 (1, 27)*** | 1.61 | 5.06 (4, 23)** | 0.80 | 8.10 (4, 23)*** | 1.01 |
Note. MADRS=Montgomery-Asberg Depression Rating Scale, BDI-II=Beck Depression Inventory-II, Q-LES-Q=Quality of Life Enjoyment Satisfaction Questionnaire, WSAS=Work and Social Adjustment Scale, DII=Distress Intolerance Index, PSS=Perceived Stress Scale, METs=metabolic equivalents of moderate and vigorous intensity exercise. All regression analyses included time, condition, and group by condition interaction.
p < 0.05,
p < 0.01,
p < 0.001
Association between exercise and mood outcomes
Because both of the randomized intervention conditions significantly improved in exercise levels (with only a small-to-moderate effect size advantage for the exercise condition), we completed an ancillary analysis examining the association between the amount of exercise completed and treatment outcome. Exercise was linked to BDI-II outcomes. Specifically, a mixed effects model, revealed significant main effects of time (F(4, 25)=4.43, p=0.008, d=0.75) and METS of exercise (F(1, 65)=5.52, p=0.02, d=0.83) as well as a significant interaction effect (F(4, 28)=4.50, p=0.006, d=0.75). These effects indicated that those who engaged in more exercise received sharper declines in depression symptoms as assessed by the BDI-II over time. However, there was no main effect of METs of exercise or interaction effect on the MADRS.
Discussion
In this randomized clinical pilot trial, we examined the credibility and effect size estimates of the combination of in-person BA with an individualized program of moderate-intensity exercise. Participants found both the exercise and stretching augmentation strategies to be credible, with 87% or above of the sample indicating the interventions as logical and may be successful in treating depression symptoms with 100% indicating they would recommend them to a friend. Regarding dropout and study completion, results indicated that the intervention yielded a completion rate of 68%, similar to other studies of exercise (e.g., 53-75%; Chalder et al., 2012; Smits et al., 2016; Toups et al., 2011) and brief BA (e.g., 76-81%; Hopko et al., 2011; Moshier and Otto, 2017) as well as clinical trials of antidepressants (74%; Undurraga and Baldessarini, 2017). Accordingly, we found no evidence for a retention benefit of combining BA and exercise, but neither did we find a retention cost for this combined intervention relative to the broader standards in the field.
However, despite the differential focus on stretching vs. exercise, we found that both treatment conditions significantly increased their exercise during the trial, with the advantage for the exercise condition showing only a non-significant, small-to-moderate effect size for greater exercise over time (d=0.30). The apparent effect of the treatment on depression reflected this finding for exercise in that both conditions achieved a significant overall improvement in mood, with a non-significant effect (d=0.35) of greater improvement in the exercise condition. We did find a significant link between the amount of exercise completed and our secondary measure of depression (the BDI-II), but this association was not significant for the MADRS, our primary measure. This may be due to the BDI-II’s greater hypothesized sensitivity in tracking changes related to psychotherapy (Demyttenaere and De Fruyt, 2003) and validates that the MADRS and BDI-II are complementary measures that each unique contribute to prediction of treatment outcome (Uher et al., 2012).
Participants in both treatment conditions also benefitted significantly in terms of decreased disability and improved quality of life. Furthermore, significant effects for condition were found for both DI and perceived stress: those assigned to the exercise condition exhibited sharper declines in DI and perceived stress over time than those in the stretching condition.
In sum, BA appears to be a richly suitable core intervention for the enhancement of exercise, enough so that depressed participants increased exercise in both the stretching and exercise conditions, and both conditions achieved clinical benefit. This is not typical for stretching control conditions (e.g., Dunn, Trivedi, Kampert, Clark, & Chambliss, 2005), again implicating BA as a potential exercise-enhancing core treatment component. Nonetheless, we found some indications of the differential focus on the exercise and stretching conditions: the exercise condition was associated with greater improvements in both DI and perceived stress, reflecting the rapid responsivity of these factors to exercise interventions (LeBouthillier and Asmundson, 2015; Smits et al., 2008).
In terms of limitations, the smaller scale of this pilot study allowed for evaluation of credibility, but had limited power to detect overall treatment differences particularly given higher levels of dropout than expected. The effect sizes obtained indicate that the combination of an exercise intervention with BA can enhance outcome beyond that for stretching augmentation of BA, on the order of small to medium effect sizes, with effects on DI and perceived stress achieving a moderate to large effect that could be detected by significance testing in this smaller pilot study. Given our findings, assessment of the degree to which BA alone has effects on exercise may reveal an important aspect of the mechanism of BA. Our study also had limited follow-up; greater effects of specific exercise assignments may be more evident over longer follow-up periods. Additionally, the lack of a waitlist (or no movement) control condition made it difficult to identify specific effects of exercise vs. possible regression to the mean. Finally, at baseline 30% of the sample (n=10) reported engaging in more exercise than the sedentary exclusion criteria; however, as noted in Supplementary Figure 1, exercise still increased on average over time in both conditions despite. Future studies may wish to include sedentary exclusion criteria at baseline as well, given that enrolling in an exercise study may enhance exercise engagement. Further, future research focusing on individuals with high DI or perceived stress may also reveal stronger benefits of exercise augmentation to BA given our preliminary findings.
Conclusions
This study adds to the growing literature of the efficacy of brief BA for improvement of depression symptoms and overall quality of life. In just 9 sessions offered over the course of 12 weeks, patients significantly reduced their depression symptoms, with 39% of the sample achieving remission. It also demonstrates feasibility and acceptability of an exercise augmentation strategy combined with BA, with suggestions that exercise may be useful for improving DI and perceived stress and may have additional effects on depression that may emerge in a well-powered study.
Supplementary Material
Supplemental Figure 1. Metabolic equivalents of moderate and vigorous intensity exercise by group over time
Supplemental Figure 2. Clinician-rated depression as assessed by the MADRS by group over time
Supplemental Figure 3. Self-reported depression as assessed by the BDI-II by group over time
Supplemental Figure 4. Quality of life as assessed by the Q-LES-Q by group over time
Supplemental Figure 5. Functional impairment as assessed by the WSAS by group over time
Supplemental Figure 6. Distress intolerance as assessed by the DII by group over time
Supplemental Figure 7. Perceived stress as assessed by the PSS by group over time
Acknowledgements:
We would like to acknowledge the contributions of M. Alexandra Kredlow and Josephine Lee for serving as study therapists; Elijah Patten, Leslie Unger, Stephen Lo, Emily Carl, Melanie Watkins, and Abraham Eastman for serving as independent evaluators; and Gabrielle Figueroa, Sarah Oppenheimer, Ani Keshishian, Daniel Reichling, and Benjamin Woodward for help with data entry.
Funding: This work was supported by a grant from the National Institute of Mental Health [F31 MH100773]. The funding source did not have any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
This work was completed as part of Kristin Szuhany’s doctoral thesis at Boston University.
Declaration of Interest Statement
In addition to Federal grant support, Dr. Otto receives royalties from multiple publishers (including royalties for books on exercise for mood). In addition, Dr. Otto received speaker support and is a member of the Scientific Advisory Board for Big Health. Dr. Szuhany declares no conflicts of interest.
References
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II San Antonio. [Google Scholar]
- Blair SN, Haskell WL, Ho P, Paffenbarger RS Jr., Vranizan KM, Farquhar JW, & Wood PD (1985). Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol, 122(5), pp. 794–804. [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2014). Anxiety and related disorders interview schedule for DSM-5 (ADIS-5)–Adult version: New York, NY: Oxford University Press. [Google Scholar]
- Busch AM, Uebelacker LA, Kalibatseva Z, & Miller IW (2010). Measuring homework completion in behavioral activation. Behav Modif, 34(4), pp. 310–329. doi: 10.1177/0145445510373384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalder M, Wiles NJ, Campbell J, Hollinghurst SP, Searle A, Haase AM, … Lewis G (2012). A pragmatic randomised controlled trial to evaluate the cost-effectiveness of a physical activity intervention as a treatment for depression: the treating depression with physical activity (TREAD) trial. Health Technol Assess, 16(10), pp. 1–164, iii-iv. doi: 10.3310/hta16100 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Williamson G (1988). Perceived stress in a probability sample of the United States In Spacapan S & Oskamp S (Eds.), The social psychology of health: Claremont Symposium on Applied Social Psychology (pp. 31–67). Newbury Park, CA: Sage. [Google Scholar]
- Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, … Mead GE (2013). Exercise for depression. Cochrane Database Syst Rev(9), p Cd004366. doi: 10.1002/14651858.CD004366.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, & Warmerdam L (2007). Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev, 27(3), pp. 318–326. doi: 10.1016/j.cpr.2006.11.001 [DOI] [PubMed] [Google Scholar]
- Demyttenaere K, & De Fruyt J (2003). Getting what you ask for: on the selectivity of depression rating scales. Psychother Psychosom, 72(2), pp. 61–70. doi: 10.1159/000068690 [DOI] [PubMed] [Google Scholar]
- Devilly GJ, & Borkovec TD (2000). Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry, 31(2), pp. 73–86. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, … Jacobson NS (2006). Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol, 74(4), pp. 658–670. doi: 10.1037/0022-006x.74.4.658 [DOI] [PubMed] [Google Scholar]
- Dunn AL, Andersen RE, & Jakicic JM (1998). Lifestyle physical activity interventions. History, short- and long-term effects, and recommendations. Am J Prev Med, 15(4), pp. 398–412. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, & Chambliss HO (2005). Exercise treatment for depression: efficacy and dose response. Am J Prev Med, 28(1), pp. 1–8. doi: 10.1016/j.amepre.2004.09.003 [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, & Blumenthal R (1993). Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull, 29(2), pp. 321–326. [PubMed] [Google Scholar]
- Hopko DR, Armento ME, Robertson SM, Ryba MM, Carvalho JP, Colman LK, … Lejuez CW (2011). Brief behavioral activation and problem-solving therapy for depressed breast cancer patients: randomized trial. J Consult Clin Psychol, 79(6), pp. 834–849. doi: 10.1037/a0025450 [DOI] [PubMed] [Google Scholar]
- Jacquart J, Dutcher CD, Freeman SZ, Stein AT, Dinh M, Carl E, & Smits JA (2019). The effects of exercise on transdiagnostic treatment targets: A meta-analytic review. Behaviour research and therapy, 115, pp. 19–37. [DOI] [PubMed] [Google Scholar]
- Kvam S, Kleppe CL, Nordhus IH, & Hovland A (2016). Exercise as a treatment for depression: A meta-analysis. J Affect Disord, 202, pp. 67–86. doi: 10.1016/j.jad.2016.03.063 [DOI] [PubMed] [Google Scholar]
- Lambert JD, Greaves CJ, Farrand P, Price L, Haase AM, & Taylor AH (2018). Web-Based Intervention Using Behavioral Activation and Physical Activity for Adults With Depression (The eMotion Study): Pilot Randomized Controlled Trial. J Med Internet Res, 20(7), p e10112. doi: 10.2196/10112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBouthillier D, & Asmundson G (2017). The efficacy of aerobic exercise and resistance training as transdiagnostic interventions for anxiety-related disorders and constructs: A randomized controlled trial. J Anxiety Disord, 52, pp. 43–52. [DOI] [PubMed] [Google Scholar]
- LeBouthillier DM, & Asmundson GJ (2015). A Single Bout of Aerobic Exercise Reduces Anxiety Sensitivity But Not Intolerance of Uncertainty or Distress Tolerance: A Randomized Controlled Trial. Cogn Behav Ther, 44(4), pp. 252–263. doi: 10.1080/16506073.2015.1028094 [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, Acierno R, Daughters SB, & Pagoto SL (2011). Ten year revision of the brief behavioral activation treatment for depression: revised treatment manual. Behav Modif, 35(2), pp. 111–161. doi: 10.1177/0145445510390929 [DOI] [PubMed] [Google Scholar]
- Mazzucchelli TG, Kane RT, & Rees CS (2010). Behavioral activation interventions for well-being: A meta-analysis. J Posit Psychol, 5(2), pp. 105–121. doi: 10.1080/17439760903569154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, & Otto MW (2012). Refining the measurement of distress intolerance. Behav Ther, 43(3), pp. 641–651. doi: 10.1016/j.beth.2011.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merom D, Phongsavan P, Wagner R, Chey T, Marnane C, Steel Z, … Bauman A (2008). Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders--a pilot group randomized trial. J Anxiety Disord, 22(6), pp. 959–968. doi: 10.1016/j.janxdis.2007.09.010 [DOI] [PubMed] [Google Scholar]
- Montgomery SA, & Asberg M (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry, 134, pp. 382–389. [DOI] [PubMed] [Google Scholar]
- Moshier SJ, & Otto MW (2017). Behavioral activation treatment for major depression: A randomized trial of the efficacy of augmentation with cognitive control training. J Affect Disord, 210, pp. 265–268. doi: 10.1016/j.jad.2017.01.003 [DOI] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, Shear MK, & Greist JH (2002). The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry, 180, pp. 461–464. [DOI] [PubMed] [Google Scholar]
- Otto MW, & Smits JA (2011). Exercise for Mood and Anxiety: Proven Strategies for Overcoming Depression and Enhancing Well-Being New York, NY: Oxford University Press. [Google Scholar]
- Pentecost C, Farrand P, Greaves CJ, Taylor RS, Warren FC, Hillsdon M, … Evans PH (2015). Combining behavioural activation with physical activity promotion for adults with depression: findings of a parallel-group pilot randomised controlled trial (BAcPAc). Trials, 16(1), p 367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Oquendo MA, Gould M, Stanley B, & Davies M (2007). Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. American Journal of Psychiatry, 164(7), pp. 1035–1043. doi: 10.1176/ajp.2007.164.7.1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Medina JL, Burns S, Kauffman BY, Monfils M, Asmundson GJ, … Smits JA (2015). Exercise Augmentation of Exposure Therapy for PTSD: Rationale and Pilot Efficacy Data. Cogn Behav Ther, 44(4), pp. 314–327. doi: 10.1080/16506073.2015.1012740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, … Finning K (2016). Cost and Outcome of Behavioural Activation versus Cognitive Behavioural Therapy for Depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet, 388(10047), pp. 871–880. doi: 10.1016/s0140-6736(16)31140-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider KL, Panza E, Handschin B, Ma Y, Busch AM, Waring ME, … Pagoto SL (2016). Feasibility of Pairing Behavioral Activation With Exercise for Women With Type 2 Diabetes and Depression: The Get It Study Pilot Randomized Controlled Trial. Behav Ther, 47(2), pp. 198–212. doi: 10.1016/j.beth.2015.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch FB, Vancampfort D, Rosenbaum S, Richards J, Ward PB, & Stubbs B (2016). Exercise improves physical and psychological quality of life in people with depression: A meta-analysis including the evaluation of control group response. Psychiatry Res, 241, pp. 47–54. doi: 10.1016/j.psychres.2016.04.054 [DOI] [PubMed] [Google Scholar]
- Smits JA, Berry AC, Rosenfield D, Powers MB, Behar E, & Otto MW (2008). Reducing anxiety sensitivity with exercise. Depress Anxiety, 25(8), pp. 689–699. [DOI] [PubMed] [Google Scholar]
- Smits JA, Zvolensky MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, … Baird SO (2016). The Efficacy of Vigorous-Intensity Exercise as an Aid to Smoking Cessation in Adults With High Anxiety Sensitivity: A Randomized Controlled Trial. Psychosom Med, 78(3), pp. 354–364. doi: 10.1097/psy.0000000000000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stathopoulou G, Powers MB, Berry AC, Smits JA, & Otto MW (2006). Exercise interventions for mental health: a quantitative and qualitative review. Clinical psychology: Science and practice, 13(2), pp. 179–193. [Google Scholar]
- Stubbs B, Vancampfort D, Rosenbaum S, Firth J, Cosco T, Veronese N, … Schuch FB (2017). An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: A meta-analysis. Psychiatry Res, 249, pp. 102–108. doi: 10.1016/j.psychres.2016.12.020 [DOI] [PubMed] [Google Scholar]
- Swift DL, Johannsen NM, Myers VH, Earnest CP, Smits JA, Blair SN, & Church TS (2012). The effect of exercise training modality on serum brain derived neurotrophic factor levels in individuals with type 2 diabetes. PLoS One, 7(8), p e42785. doi: 10.1371/journal.pone.0042785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toups MS, Greer TL, Kurian BT, Grannemann BD, Carmody TJ, Huebinger R, … Trivedi MH (2011). Effects of serum Brain Derived Neurotrophic Factor on exercise augmentation treatment of depression. J Psychiatr Res, 45(10), pp. 1301–1306. doi: 10.1016/j.jpsychires.2011.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi MH, Greer TL, Grannemann BD, Chambliss HO, & Jordan AN (2006). Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract, 12(4), pp. 205–213. [DOI] [PubMed] [Google Scholar]
- Uher R, Perlis RH, Placentino A, Dernovsek MZ, Henigsberg N, Mors O, … Farmer A (2012). Self-report and clinician-rated measures of depression severity: can one replace the other? Depress Anxiety, 29(12), pp. 1043–1049. doi: 10.1002/da.21993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Undurraga J, & Baldessarini RJ (2017). Direct comparison of tricyclic and serotonin-reuptake inhibitor antidepressants in randomized head-to-head trials in acute major depression: Systematic review and meta-analysis. Journal of Psychopharmacology, 31(9), pp. 1184–1189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Metabolic equivalents of moderate and vigorous intensity exercise by group over time
Supplemental Figure 2. Clinician-rated depression as assessed by the MADRS by group over time
Supplemental Figure 3. Self-reported depression as assessed by the BDI-II by group over time
Supplemental Figure 4. Quality of life as assessed by the Q-LES-Q by group over time
Supplemental Figure 5. Functional impairment as assessed by the WSAS by group over time
Supplemental Figure 6. Distress intolerance as assessed by the DII by group over time
Supplemental Figure 7. Perceived stress as assessed by the PSS by group over time