Abstract
This study uses South Korean administrative database data to assess changes in incidence of postthyroidectomy hypoparathyroidism during a period of fluctuations in thyroid cancer screening and surgery between 2007 and 2016.
In 1999, the South Korean government initiated a national cancer screening program, which led to increased high-resolution ultrasonography screening for thyroid cancer. Consequently, thyroid cancer incidence increased from 7.2 per 100 000 population in 1999 to 68.7 per 100 000 population in 2011,1,2 and most patients received surgery. However, many screen-detected cancers were small and likely indolent. Concerns about overdiagnosis were raised beginning in 2012, and ultrasonographic screening was discouraged in 2014, leading to decreased incidence of thyroid cancer and thyroidectomies.3,4 We assessed the changes in incidence rates of postoperative hypoparathyroidism, a complication of thyroidectomy, between 2007 and 2016.
Methods
We used the South Korean National Health Insurance Sharing Service Database, an administrative database based on health insurance claims from the entire population of South Korea, to calculate the change in incidence of thyroid cancer, total and partial thyroidectomies, and postoperative hypoparathyroidism per 100 000 between 2007 and 2016. Definitions of partial and total thyroidectomies were adopted from a previous report5; partial thyroidectomies are less likely to result in hypoparathyroidism. Data on incidence of postoperative hypoparathyroidism and thyroid cancer were age-standardized to the South Korean standard population of 2000. The operational definition of postoperative hypoparathyroidism was modified from a previous report.6 The following conditions had to be satisfied, in the corresponding year but not in the previous 3 years, to meet the definition of permanent postoperative hypoparathyroidism: (1) thyroidectomy prior to first active vitamin D prescription; (2) thyroid cancer before first active vitamin D prescription or diagnostic code for hypoparathyroidism after thyroidectomy; and (3) at least three 90-day prescriptions for active vitamin D. The incident date of hypoparathyroidism was defined as the first date of active vitamin D prescription. The operational definition was validated through a separate retrospective chart review at a single medical center, in which we queried electronic medical records to identify cases of postsurgical hypoparathyroidism between 2010 and 2018 and verified the results by manual chart review. Sixty-five of 81 cases (81.5%) identified by electronic medical record were confirmed to have hypoparathyroidism, suggesting an acceptable positive predictive value for the operational definition.
We calculated 95% confidence intervals for incidences using SAS software, version 9.4 (SAS Institute Inc). The Gachon University Gil Medical Center institutional review board approved this study with a waiver of informed consent.
Results
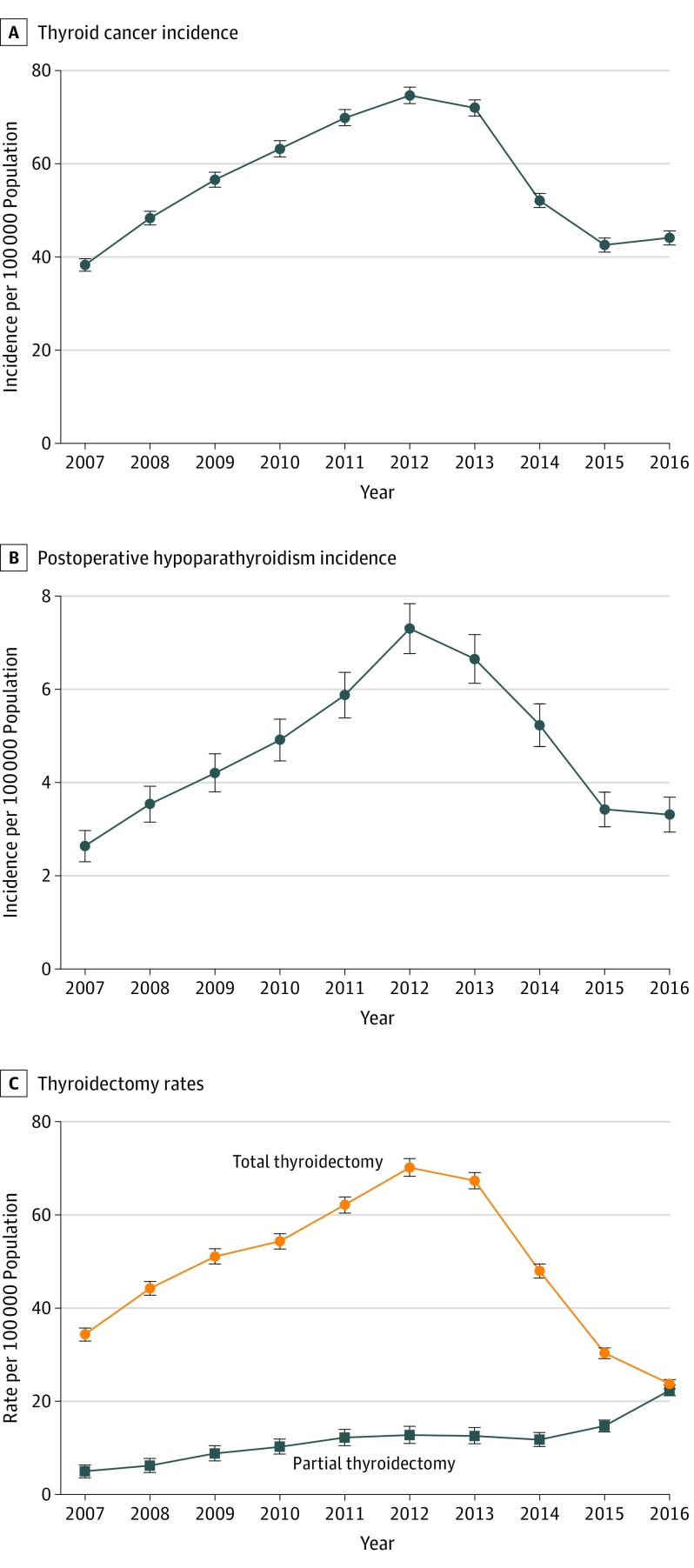
Between 2007 and 2016, 29 063 cases of postoperative hypoparathyroidism were identified, including 1466 cases in 2007 and 2135 cases in 2016. Between 2007 and 2012, the incidence of thyroid cancer, total thyroidectomies, and postoperative hypoparathyroidism increased. Postoperative hypoparathyroidism increased from 2.6 (95% CI, 2.5-2.8) per 100 000 population in 2007 to 7.3 (95% CI, 7.1-7.5) per 100 000 population in 2012, an increase of 177% (Figure), and total thyroidectomies increased from 34.3 (95% CI, 33.7-34.8) per 100 000 population in 2007 to 70.1 (95% CI, 69.4-70.9) per 100 000 population in 2012, an increase of 104%. After 2012, the rate of thyroid cancer and total thyroidectomies decreased, the latter reaching 23.6 (95% CI, 23.2-24.0) per 100 000 population in 2016, and the incidence of postoperative hypoparathyroidism decreased to 3.3 (95% CI, 3.2-3.5) per 100 000 population. In contrast, the rate of partial thyroidectomies increased gradually between 2007 and 2016, comprising 18% of total thyroidectomies in 2012 (6369/35 307) and 94% in 2016 (11 365/12 066).
Figure. Incidence of Thyroid Cancer and Postoperative Hypoparathyroidism and Rates of Thyroid Cancer Surgeries in South Korea.
Error bars indicate 95% confidence intervals. A, The incidence of thyroid cancer per 100 000 population in 2007 was 38.3 (95% CI, 37.7-38.8) and in 2016 was 44.1 (95% CI, 43.5-44.7). B, The incidence of postoperative hypoparathyroidism per 100 000 population in 2007 was 2.6 (95% CI, 2.5-2.7) and in 2016 was 3.3 (95% CI, 3.2-3.5). C, The rate of total thyroidectomy per 100 000 population in 2007 was 34.8 (95% CI, 33.7-34.8) and in 2016 was 23.6 (95% CI, 23.2-24.0); the rate of partial thyroidectomy per 100 000 population in 2007 was 4.8 (95% CI, 4.3-5.4) and in 2016 was 22.2 (95% CI, 21.8-22.7).
Discussion
The incidence of postoperative hypoparathyroidism in South Korea increased and then decreased between 2007 and 2016 in parallel with trends in thyroid cancer diagnosis and treatment. The initial increase in the incidence of thyroid cancer might be linked to the initiation of a national cancer screening program, while the subsequent decrease may be related to concerns about overdiagnosis.3 The limitation of this study was that postoperative hypoparathyroidism might be underestimated because of use of administrative claims. Postoperative hypoparathyroidism is a rare but serious complication of thyroid surgery and an example of harm related to overdiagnosis and overtreatment.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”—screening and overdiagnosis. N Engl J Med. 2014;371(19):1765-1767. doi: 10.1056/NEJMp1409841 [DOI] [PubMed] [Google Scholar]
- 2.Korea Central Cancer Registry, National Cancer Center, Ministry of Health and Welfare Annual Report of Cancer Statistics in Korea in 2016 https://ncc.re.kr/main.ncc?uri=english/sub04_Statistics. Published December 2018. Accessed October 31, 2019.
- 3.Ahn HS, Welch HG. South Korea’s thyroid-cancer “epidemic”—turning the tide. N Engl J Med. 2015;373(24):2389-2390. doi: 10.1056/NEJMc1507622 [DOI] [PubMed] [Google Scholar]
- 4.Haugen BR, Alexander EK, Bible KC, et al. . 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133. doi: 10.1089/thy.2015.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sung M-W, Park B, An S-Y, Hah JH, Jung YH, Choi HG. Increasing thyroid cancer rate and the extent of thyroid surgery in Korea. PLoS One. 2014;9(12):e113464. doi: 10.1371/journal.pone.0113464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Underbjerg L, Sikjaer T, Mosekilde L, Rejnmark L. Cardiovascular and renal complications to postsurgical hypoparathyroidism: a Danish nationwide controlled historic follow-up study. J Bone Miner Res. 2013;28(11):2277-2285. doi: 10.1002/jbmr.1979 [DOI] [PubMed] [Google Scholar]