Abstract
Objective:
There exists considerable individual variability in the development and progression of pathological stress reactions after experiencing trauma, as well as in individuals’ response to psychological interventions. Yet until recently, such individual differences had not been considered when evaluating the efficacy of therapeutic interventions for post-traumatic stress disorder (PTSD). This systematic review aims to examine the emerging literature on this subject and, specifically, to identify trajectories and predictors of psychotherapeutic response in adults with PTSD.
Method:
Four databases were searched using specific keywords without date or language restrictions. For each study, independent reviewers systematically evaluated whether it met eligibility criteria and assessed risk of bias. For included studies, reviewers completed data extraction using standard formats. Those examining how subgroups of adults respond to therapy for clinical PTSD using trajectory modeling were deemed eligible. Demographic, PTSD, clinical, and trauma-related factors associated to particular trajectories were also examined.
Results:
Of the 1,727 papers identified, 11 were included in this analysis. Of these studies, six focused on military-related traumas and five on civilian ones. Although studies found between two and five trajectories, most supported a three-trajectory model of response categorized as responders, nonresponders, and subclinical participants. Over 22 predictors of treatment trajectories were examined. Comorbid depression, anxiety, and alcohol abuse were the strongest predictors of poor therapeutic response. Age, combat exposure, social support, and hyperarousal were moderate predictors.
Conclusion:
This review provides valuable insight into the treatment of PTSD, as it supports the heterogeneous trajectories of psychotherapeutic responses and provides avenues for the development of interventions that consider individual-level factors in treatment response.
Keywords: post-traumatic stress disorder, psychotherapy, trajectory, response, review
Abstract
Objectif :
Il existe une variabilité individuelle considérable dans le développement et la progression des réactions pathologiques au stress après l’expérience d’un traumatisme, de même que dans la réponse des personnes aux interventions psychologiques. Et pourtant, jusqu’à récemment, ces différences individuelles n’étaient pas prises en compte dans l’évaluation de l’efficacité des interventions thérapeutiques pour le trouble de stress post-traumatique. Cette revue systématique vise à examiner la littérature émergente à ce sujet, et spécifiquement, à identifier les trajectoires et les prédicteurs de la réponse psychothérapeutique des adultes souffrant du trouble de stress post-traumatique (TSPT).
Méthode :
Une recherche a été menée dans quatre bases de données à l’aide de mots clés spécifiques sans restriction de date ou de langue. Pour chaque étude, des réviseurs indépendants ont évalué systématiquement si elle satisfaisait aux critères d’admissibilité et ont évalué le risque de biais. Pour les études incluses, les réviseurs ont procédé à l’extraction de données à l’aide de formats standards. Celles qui examinaient comment les sous-groupes d’adultes répondaient à la thérapie pour le TSPT clinique à l’aide d’un modèle de trajectoire étaient jugées admissibles. Les facteurs démographiques, du TSPT, cliniques et liés au traumatisme associés à des trajectoires particulières ont été aussi examinés.
Résultats :
Sur les 1 727 articles identifiés, 11 ont été inclus dans cette analyse. Sur ces études, six portaient sur des traumatismes liés aux militaires et cinq, sur des civils. Même si les études ont observé de deux à cinq trajectoires, la plupart soutenaient un modèle à trois trajectoires de réponses réparties comme répondeurs, non-répondeurs et participants sous-cliniques. Plus de 22 prédicteurs de trajectoires de traitement ont été examinés. La dépression comorbide, l’anxiété et l’abus d’alcool étaient les prédicteurs les plus forts d’une mauvaise réponse thérapeutique. L’âge, l’exposition au combat, le soutien social et l’hyperexcitation étaient des prédicteurs modérés.
Conclusion :
Cette revue offre une information valable sur le traitement du TSPT, car elle confirme les trajectoires hétérogènes des réponses psychothérapeutiques et offre des avenues pour le développement d’interventions qui tiennent compte des facteurs de niveau individuel de la réponse au traitement.
Epidemiological studies indicate that exposure to events that involve a threat to safety, life, or integrity and that have the potential to induce distress, also termed traumatic events, is very common.1 Indeed, in Canada, about 75.9% of the population will be exposed to at least one traumatic event in their lifetime.2 Furthermore, the prevalence of such events can substantially vary,1 as individuals in different parts of the world might be exposed to a wide range of traumatic events (e.g., natural disasters, experiences of war and combat). For instance, in Canada, the most common traumatic events are the sudden unexpected death of a loved one, witnessing death or serious injury, being sexually molested, and being involved in a life-threatening vehicle accident.2 While traumatic events can lead to several psychopathologies, studies suggest that traumatic exposure is most frequently associated to post-traumatic stress disorder (PTSD).3 PTSD is characterized by intrusive memories or flashbacks of the trauma, avoidance of its reminders, negative thoughts and mood, as well as alterations in reactivity after exposure to a traumatic event.4 In over 80% of cases, this debilitating disorder also co-occurs with at least one other condition, such as depression, substance abuse, affective disorders, physical chronic illness, inability to work, and higher rates of attempted suicide.2,5,6
Not all individuals exposed to a traumatic event will react the same way and most will never develop PTSD. In fact, four patterns of adaptation to such events have been described7: resilience, recovery from initial dysfunction, delayed onset dysfunction, and chronic dysfunction. Mirroring these trajectories, Santiago and colleague’s8 systematic review of PTSD prevalence, and trajectories found that among individuals exposed to intentional traumatic events, on average, 41.1% meet PTSD diagnosis criteria at one point in time. Indeed, on average, 18.5% had PTSD but recovered after 3 months, 18.3% showed a chronic PTSD trajectory, and 4.3% had a delayed expression of PTSD after 3 months. Equally important, a meta-analysis9 showed that, without treatment, few recover spontaneously from PTSD, such that follow-up studies did not report higher long-term remission rates (range 10 to 204 months). These results suggest that, for the vast majority, the simple passage of time is not sufficient for PTSD recovery and highlight the importance for effective treatments.
Fortunately, several trauma-focused psychotherapies (e.g., trauma-focused cognitive behavioral therapy, eye movement desensitization, and reprocessing) have been empirically tested using randomized controlled clinical trials and have received strong support from extensive meta-analyses.10,11 However, as there is heterogeneity in the natural evolution of trauma reactions,7 such variability also exists in individuals’ response to psychotherapy. Kelly and colleagues12 found that 39.2% of participants in their sample experienced a rapid and significant reduction in PTSD symptoms while receiving a 7- to 12-week-long Cognitive Behavioral Therapy (CBT). In fact, between Weeks 2 and 5 of therapy, they reported a minimum reduction of 12 points on the Posttraumatic Stress Diagnostic Scale (PDS) that was maintained for at least two subsequent sessions. This suggests that subgroups of participants may respond distinctly to therapy. Furthermore, although these empirically supported treatments are effective for a substantial portion of individuals with PTSD, the considerable nonresponse (often over 50%) and dropout rates (up to 54%) reported by meta-analytic studies suggest that they are not effective for all patients.13
This variability in treatment response prompted an interest in the search for predictors and moderators associated with better response to psychotherapy. Some researchers have identified clinical factors as predictors, such as comorbidity.14 For example, in a sample of 134 Vietnam veterans with combat-related PTSD, Forbes et al.14 found that posttreatment symptoms were significantly associated with baseline depression, anger, and alcohol use, independently from baseline PTSD severity. While certain predictors have been documented, the literature on trauma-related variables remains mixed. For instance, some studies have found the amount of time passed since the traumatic event, the lifetime exposure to traumatic events, and the type of trauma to be significantly related to treatment outcome,15 but others have failed to replicate these results.16 Findings regarding demographic factors have been similarly equivocal: No association between sex, marital status, or education level and treatment outcome have been consistently reported.15–18 With regard to age, some studies suggest that younger individuals are at a greater risk of dropping out of treatment.19–21 These inconsistent results regarding predictors currently provide limited therapeutic use in improving treatment response.
Until recently, rather than examining symptom change over time, most studies have assessed the effectiveness of treatments by simply comparing pretreatment and posttreatment scores in symptom severity and effect sizes. Consequently, in order to better understand differential responding to psychotherapy among individuals with PTSD, an emerging number of researchers have focused on understanding the diverse patterns of response to psychotherapy for PTSD and on the factors associated to these responses.13,22 Generally speaking, a trajectory represents the course of an outcome over time. Several trajectory analysis methods have been developed to identify trajectories of therapeutic response: group-based trajectory models,23 growth mixture models,24 or latent class analysis.25 These models assign individuals to subgroups based on latent common patterns of outcome evolution, such as PTSD symptom severity. Post hoc analyses are then conducted to compare characteristics and outcomes of individuals classified into different trajectories. In this review, variables that may explain differential responses or predict assignment to a particular group are referred to as trajectory predictors. By isolating predictors of nonresponse that may be addressed during treatment, trajectory and predictor identification are interesting avenues by which to individualize psychotherapy, thereby increasing its efficacy.22
The current study is the first systematic review to examine the literature on heterogeneous response trajectories to therapy for adults with PTSD. The first objective of this study was to evaluate the number and type of trajectories that best described responses to psychotherapy across studies. The second objective was to identify factors that distinguish assignment to the treatment response and nonresponse trajectories. This review is essential to gain insight on the different types of responses to therapy and to optimize treatments accordingly.
Methods
Search Strategy and Study Selection
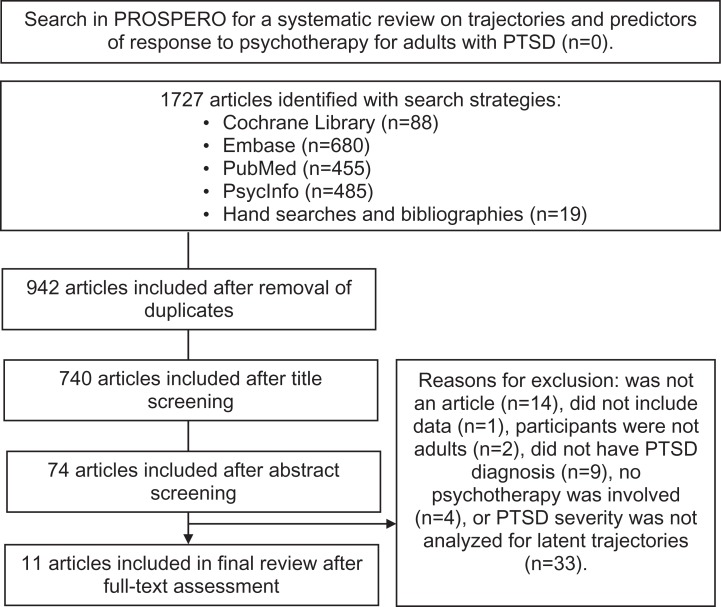
This systematic review was conducted following the Preferred Reporting for Systematic Review and Meta-Analyses (PRISMA) guidelines. The review protocol was registered in Prospero (2018; CRD42018090975). The systematic search of literature was conducted in February 2018 using specific keywords in four databases with no date, publication type, or language restrictions: The Cochrane Library, EMBASE, PsycINFO, and PubMed. Using the “All Text” field, the keyword search strategy entered was the following: (PTSD OR “posttraumatic stress disorder” OR “post-traumatic stress disorder”) AND (psychotherap* OR therapy OR therapies OR intervention OR psychological) AND (“group-based” OR “latent class” OR “growth mixture” OR trajector*). Three additional search strategies were utilized to ensure that all relevant article titles and unpublished studies were found. First, searches were performed in Google Scholar to identify potential dissertations and reports. Second, titles in identified articles’ references lists were hand searched. Third, seen as authors of the identified articles have published work in this field, they were contacted about unpublished empirical research, but none were identified. From the objective and Population, Intervention, Comparison, Outcome (PICO) components, four criteria were established to determine eligibility of articles: (1) all participants had to meet PTSD diagnosis or a clinical level of PTSD symptomatology (above the clinical score suggested as indicative of a probable PTSD diagnosis), according to a validated measure or diagnosis method; (2) all participants had to be 18 years or older at baseline; (3) a group of participants had to have received psychotherapy for PTSD; and (4) severity of PTSD across time points had to be analyzed for trajectories (e.g., growth mixture modeling, latent class growth analysis). After the removal of duplicate studies, all titles and abstracts obtained were independently analyzed by two reviewers, and studies that clearly did not match inclusion criteria were excluded. The remaining articles were revised in their entirety. Reviewers’ ratings on the four inclusion criteria were then compared, and when discrepancies were observed, they were discussed until a consensus could be reached. When necessary, a third reviewer was consulted to resolve disagreements and achieve consensus (see Figure 1).
Figure 1.
Preferred Reporting for Systematic Review and Meta-Analyses flowchart of the search process for articles investigating trajectories and predictors of response to psychotherapy for adults with post-traumatic stress disorder.
Data Extraction
Using a standard form and method, two reviewers double-extracted the following data from each study: study design, sample size, sample characteristics, type of trauma, time since target traumatic event, symptoms assessed, and characteristics of psychotherapy. Relevant results were also extracted, such as the number and characteristics of trajectories and findings related to predictors. Any divergences in extracted data were discussed and verified until consensus was reached.
Risk of Bias Assessment
The risk of bias was assessed using the Downs and Black Inventory (DBI).26 This validated 27-item scale is designed to provide an overall quality score for randomized and nonrandomized studies by assessing quality of reporting, external validity, internal validity related to methodological biases, as well as the distribution of confounding variables and the statistical power. For this review, 2 items were removed: Item 14 about the subjects being blind to the treatment they receive and Item 27 about power. These 2 items were removed because they were not well suited for the type of intervention and analysis included in this review. Apart from a single item, a score of 1 is given for all items where “yes” is endorsed and a score of 0 for items where “no” or “unable to determine” are endorsed. For the item assessing “whether the distribution of confounding variables in each group of subjects is sufficiently described” (Item 5), a score of 2 is given for responding “yes,” of one for responding “partially,” and of 0 for responding “no.” Therefore, the overall quality score could range from 0 to 26 points. The DBI has satisfying psychometric properties: internal consistency of .89, interrater reliability of .75, and criterion validity between .86 and .90.26 Interrater reliability for the DBI was calculated with mean percent agreement between the reviewers,27 and any discrepancies were discussed until agreement was reached.
Trajectory Analysis and Predictor Identification
To allow comparison of PTSD severity trajectories from the different studies and their associated predictors, trajectories were first compiled and analyzed according to their severity scores at different time points. Trajectories were reclassified into three categories as follows: (1) responders, where the preintervention score was above clinical PTSD cutoff score and the postintervention score was below clinical PTSD cutoff score; (2) nonresponders, where the pre- and postintervention scores were both above clinical PTSD cutoff; or (3) subclinical participants, where the trajectory was neither “responders” or “nonresponders” as preintervention score was below clinical PTSD cutoff score. Reclassification was reviewed to make sure trajectories were all accounted for. Probable PTSD diagnosis cutoff values were used to reclassify trajectories because they were the only scores available from self-report measures used in studies to assess significant clinical change over time. A three-step procedure was followed during reclassification of trajectories. First, PTSD symptom severity was computed at pre- and postintervention for each trajectory across all studies. Exceptionally, for two studies,28,29 no scores were available immediately after treatment. For these studies, the first posttreatment data available, corresponding to 6 months after baseline, were used as postintervention scores. In addition, while some authors kindly provided missing data upon request, the exact scores were still missing from four studies. Scores for these studies were estimated using the smallest scales available in the graphic depiction of results.
Second, a cutoff score indicative of probable PTSD diagnosis was established for each PTSD symptom severity tool used in this review. Since most studies did not provide such scores, probable PTSD diagnosis cutoff scores were established according to the scientific literature. Seven studies used the Posttraumatic Stress Disorder Checklist (PCL), the PCL Military Version, or the PCL Specific Trauma Version. For these studies, a recommended cutoff score for clinical PTSD of 50 was used for military populations and of 44 for civilian and specific trauma-exposed populations.30,31 Three studies used the PDS or, its former version, the self-report PTSD Symptom Scale-SR).32 A cutoff score of 17 was used for these tools,33 which suggests moderately severe PTSD symptoms.34 One study29 used the Harvard Trauma Questionnaire and identified a cutoff score of 40 which is equivalent to the mean cutoff score of 2.5 consistently used in other studies.35 Finally, Rosenkranz and Muller’s study36 used the Trauma Symptom Checklist- 40. After an extensive search of literature, no cutoff score was found for this tool. As recommended in a review by Jacobson and Truax,37 to be considered a probable cutoff score, the sample’s posttreatment mean score had to be lower than half the difference between the pretreatment sample group’s mean and the normative group’s mean (M posttreatment − ((M pretreatment − M normative sample)/2 = cutoff score). Third, with the mean baseline and postintervention PTSD scores, as well as the probable PTSD cutoff scores, the trajectories were reclassified. Finally, all selected studies were reviewed to identify any factor that had been investigated by at least two studies and which could potentially distinguish subgroups of participants across each trajectory. For studies with more than one reclassified trajectory of the same type (e.g., two responder groups), comparisons of trajectory and associated predictors were combined (see Table 1). Three nonresponder trajectories were impossible to combine in Phelps et al.’s38 comparisons of guilt (see Table 1) since they had discordant results: Two nonresponder groups (NR1 and NR3) had significantly higher levels of guilt than the subclinical group while the third nonresponder (NR2) group had lower levels of guilt than this subclinical group. For this reason, all original trajectories were kept.
Table 1.
Predictors of Trajectories Examined in Each Study.
| First Author | Allan | Clapp | Currier | Elliott | Fletcher | Galovski | Phelps | Rosenkranz | Schumm | Stein | Taylor |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Types of Trajectories | RE, NR | RE, NR | NR, SB | NR, SB | RE, NR, SB | RE, NR | RE, NR, SB | RE, NR | RE, NR | RE, NR | NR |
| Demographic baseline predictors | |||||||||||
| Age | ns | NR < SB* | ns | RE < SB* | RE < NR* | ns | RE < NR* | ns | |||
| Ethnicity | ns | ns | ns | RE > NR* (%White) | ns | ||||||
| Sex | ns | RE > NR* (%female) | ns | ||||||||
| Marital status | RE > NR*** (%married) | ns | ns | ns | ns | ||||||
| Education | ns | ns | |||||||||
| PTSD and trauma-related baseline predictors | |||||||||||
| PTSD severity | ns | ns | NR > SB *** | ns | RE < NR *** | RE < NR* | ns | ||||
| Reexperiencing | RE < NR** | RE < NR * | ns | ns | |||||||
| NR > SB** | |||||||||||
| Hyperarousal | RE < NR* | RE < NR * | RE < NR*** | ns | |||||||
| NR > SB** | |||||||||||
| Avoidance | RE < NR* | RE < NR * | ns | ns | |||||||
| NR > SB** | |||||||||||
| Dissociation | ns | RE < NR *** | ns | ||||||||
| Numbing | ns | NR1 > NR2* | |||||||||
| Anger | NR > SB*** | ns | ns | NR1 > NR2* | |||||||
| Guilt | RE > NR* | ns | |||||||||
| RE > SB*** | |||||||||||
| NR1 > SB*** | ns | ||||||||||
| NR2 < SB* | |||||||||||
| NR3 > SB*** | |||||||||||
| Time since trauma | RE > NR* | ns | |||||||||
| RE > SB* | |||||||||||
| Combat exposure | NR < SB*** | NR > SB*** | RE < NR* | ||||||||
| Sexual abuse | RE < NR *** | ns | |||||||||
| Other clinical baseline predictors | |||||||||||
| Depression symptoms | ns | ns | NR > SB*** | RE < NR** RE > SB** NR > SB*** |
RE < NR *** | RE < NR* | NR1 > NR2* | ||||
| MDD diagnosis | RE < NR*** | NR1 > NR2*** | |||||||||
| Anxiety symptoms | RE < NR* | NR > SB *** | RE < NR *** | ||||||||
| PD diagnosis | ns | ns | |||||||||
| Alcohol use or abuse | NR > SB** | NR > SB*** | |||||||||
| Social support | ns | RE > NR** RE < SB* NR < SB*** |
ns | ||||||||
Note. RE = responders; NR = nonresponders; SB = subclinical; ns = nonstatistically significative; MDD = major depression disorder. PD = panic disorder. PTSD = post-traumatic stress disorder. *P > 0.05. **P > 0.01. ***P > 0.001.
Results
The database search identified 1,708 articles, and an additional 19 articles were identified in reference lists and in Google Scholar (total of 1,727 articles). As illustrated in the PRISMA flowchart (Figure 1), 942 articles were assessed after removal of duplicates: 202 were eliminated after title screening, 666 after abstract analysis, and 62 after full-text analysis. Therefore, reviewers identified 11 studies that met full inclusion criteria. All 11 articles were written in English.
As seen in Table 2, of the 11 studies, none were published prior to 2001,39 and all originated from high-income countries. Most studies used archival data analysis (n = 6)28,29,38,40–42 or randomized controlled trials (n = 3).43–45 The two remaining studies used a waitlist comparison design (n = 1)36 and a single group with repeated measures design (n = 1).39 The mean analytic sample size was 662 participants (SD = 916.33) and ranged from 45 to 2,686 participants. Mean age varied between samples from 33.6 to 55.9 years. Six samples were mostly male (over 80% male), two were mostly female (over 80% female), two were mixed (64% and 68% female), and one study did not report the sex distribution of their sample. In terms of ethnicity, six studies reported ethnically diverse samples (i.e., no ethnic group accounted for more than 65% of sample). Nevertheless, participants in three samples identified predominantly as Caucasian (i.e., over 85% Caucasian), and two samples did not report ethnicity. Nearly all studies excluded participants who had active psychosis, suicidality, or substance abuse (drug or alcohol). Most evaluated comorbid conditions (i.e., mood, anxiety, personality, and substance or alcohol abuse) and reported comorbidity rates of their sample. Given that it was an inclusion criterion for this review, all studies reported clinical levels of PTSD in participants. They also reported a variety of index traumatic events. Information regarding psychotherapy type (see Table 2), content, modality, and duration likewise varied.
Table 2.
Summary of Studies Examining Post-Traumatic Stress Disorder Symptom Trajectories in Response to Psychotherapy.
| First Author (Year, Country) | Analytic N | DBI Total Score | % of DBI Items “Unable to Determine” | Age | Sex Ratio | Ethnicity | Diagnosis Criteria | Type of Clinical Population | Type of Psychotherapy | |
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | |||||||||
| Allan (2017, USA) | 231 | 20 | 12 | 45.7 | 14.9 | 94.4% ♂ | 50.6% White; 47.2% Black | DSM IV TR | Military | Behavioral activation and therapeutic exposure |
| Clapp (2016, USA) | 109 | 14 | 24 | 47.9 | 15.3 | 81.7% ♂ | 39.4% Black; 55% White/Non-Hispanic | DSM IV | Military | PE |
| Currier (2014, USA) | 805 | 13 | 24 | 51.53 | 8.0 | 89.1% ♂ | 59.5% Caucasian; 16.6% African American; 14.7% Latino; 2.2% Asian American; 1.9% Native American; 5.1% Other | DSM IV | Military | Group cognitive behavioral intervention |
| Elliott (2005, Australia) | 2219 | 14 | 28 | — | — | 100% ♂ | — | DSM IV | Military | Inpatient or outpatient group cognitive behavioral intervention |
| Fletcher (2017, Denmark) | 439 | 11 | 24 | 36.5 | 10.8 | 85.8% ♀ | 100% Caucasian | DSM IV TR | Civilian; victims of CSA | Personalized psychotherapy (includes cognitive, psychodynamic, and behavioral treatments) |
| Galovski (2016, USA) | 69 | 17 | 16 | 39.8 | 11.7 | — | 51% Black; 42% White; 7% Latino | DSM IV | Civilian; victims of interpersonal violence | Cognitive processing therapy |
| Phelps (2018, Australia) | 2686 | 16 | 16 | 55.9 | 10.5 | 98.8% ♂ | — | DSM IV | Military | Individual and group therapy |
| Rosenkranz (2011, Canada) | 161 | 16 | 16 | 42.9 | 9.2 | 64% ♀ | 91.9% European-Canadian, 4.5% Aboriginal, 1.8% African/Caribbean-Canadian, 0.9% Other | DSM IV | Civilian; adult survivors of CSA | Psychotherapy based on Bloom’s Sanctuary model |
| Schumm (2013, USA) | 205 | 15 | 12 | 42.3 | 14.4 | 89% ♂ | 81% White | DSM IV TR | Military | Cognitive processing therapy |
| Stein (2012, USA) | 313 | 19 | 16 | 33.6 | 11.3 | 100% ♀ | 65% Caucasian, 31% African American | DSM IV | Civilian; female victims of interpersonal violence | Cognitive processing therapy or PE or cognitive therapy or written accounts |
| Taylor (2001, Canada) | 45 | 16 | 16 | 35.6 | 10.3 | 68% ♀ | 86% White; 10% Asian; 4% Other | DSM IV | Civilian; victims of a road accident | Group cognitive behavioral therapy |
Note. CSA = childhood sexual abuse; DBI = Downs & Black Inventory; ♀ = female; ♂=male; — = not mentioned; # = number; PE = prolonged exposure.
Quality Assessment
In this review, most studies were either randomized controlled trials, with strong internal validity, or archival data analysis. While archival data analysis designs typically have inherent downfalls such as nonrandomization and less control for confounding variables, they provide additional external validity. Together, these studies provide information from both naturalistic and research settings. The quality of these studies, as assessed by the DBI, ranged from 12 to 21 of 26 possible points (see Table 2), with a mean score of 16.45, suggesting moderate quality. However, when considering other relevant factors, such as sample size and proportion of items on the DBI that remained unanswered, the quality of these studies varied from fair to good. In fact, sample sizes were mostly very large, which represent an important methodological strength. Furthermore, due to a lack of information in the articles, 22.2% of item responses were marked as “unable to determine” and were thus assigned a score of 0, which consequently skews quality scores. All four studies that received a score of 15 or under (see Table 2) had rather large sample sizes (109, 439, 805, and 2,219 participants) and the highest rates of items marked as “unable to determine” (between 24.0% and 28.0%). Therefore, even though they obtained a score of moderate on the DBI, these studies were considered to be of fair quality. The remaining studies received scores over 15 and were deemed of good quality. The percentage of agreement between raters on the DBI was 83.0%, which is higher but consistent with the 75% agreement found in the validation study.26
Trajectory Analysis
Using different modeling procedures (see methodology column in Table 3), between two and five trajectories were found in all studies. Reclassification of trajectories was conducted using the mean baseline and postintervention PTSD symptom severity scores for each subgroup’s trajectory, as well as the established cutoff score for probable PTSD for each measure (see Table 3). A total of 34 trajectories were reclassified: 13 as responders, 17 as nonresponders, and 4 as subclinical trajectories. Eight studies of the 12 had at least one responder and one nonresponder trajectory. Three studies did not include a group that could be considered as responder.
Table 3.
Details of Trajectory Analysis and Reclassification for Each Study.
| First Author (year) | Methodology | Assessments | Type of Clinical Population | # of Trajectories | PTSD Severity | Trajectory | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Cutoff Score | Av. at Baseline | Av. at Postintervention | Original Name | % | Reclassified Name | Summed % | |||||
| Allan (2017) | Growth mixture modeling | Baseline, session 2, 4, 6, 8, and postintervention | Military | 3 | PCL-M | >50 | 55.70 | 35.19 | Responders | 15.15 | Responders | 17.75 |
| 63.92 | 24.00 | Immediate responders | 2.60 | Responders | ||||||||
| 58.11 | 52.35 | Nonresponders | 82.25 | Nonresponders | 82.25 | |||||||
| Clapp (2016) | Latent profile analysis | Baseline, at discretion of clinician and postintervention | Military | 3 | PCL-M | >50 | 63.25 | 28.30 | Rapid responder | 18.30 | Responders | 58.70 |
| 62.09 | 39.52 | Linear responder | 40.40 | Responders | ||||||||
| 62.60 | 53.07 | Delayed responder | 41.30 | Nonresponders | 41.30 | |||||||
| Currier (2014) | Latent class growth analysis | Baseline, postintervention and 4-month follow up | Military | 3 | PCL-M | >50 | 62.32 | 54.93 | Improving moderate PTSD | 48.82 | Nonresponders | 89.81 |
| 72.59 | 69.11 | Stable high PTSD | 40.99 | Nonresponders | ||||||||
| 45.55 | 38.40 | Stable low PTSD | 10.19 | Subclinical | 10.19 | |||||||
| Elliott (2005) | Latent growth mixture modeling | Baseline, 6, 12, and 24 months postintervention | Military | 3 | PCL | >50 | 72.88 | ∼63.88 | Group 1 | 62.2 | Nonresponders | 96.1 |
| 60.73 | ∼56.73 | Group 2 | 33.9 | Nonresponders | ||||||||
| 44.14 | ∼47.14 | Group 3 | 3.9 | Subclinical | 3.9 | |||||||
| Fletcher (2017) | Latent class growth analysis | Baseline, 6 months, 12 months, and 18 months after baseline | Civilian; victims of CSA | 4 | HTQ | >40 | 42.58 | 36.3 | Moderate PTSD gradual response | 33.03 | Responders | 33.03 |
| 48.17 | 44.83 | High PTSD gradual response | 36.22 | Nonresponders | 51.25 | |||||||
| 53.09 | 52.51 | High PTSD treatment resistant | 15.03 | Nonresponders | ||||||||
| 36.37 | 26.94 | Moderate PTSD rapid response | 15.71 | Subclinical | 15.71 | |||||||
| Galovski (2016) | Latent class growth analysis | Baseline, at every therapy session, and 2 weeks postintervention | Civilian; victims of interpersonal violence | 3 | PDS | >17 | 25.28 | ]0, 10[ | Initial responders | 47.83 | Responders | 92.76 |
| 34.34 | ]10, 15[ | Consistent responders | 44.93 | Responders | ||||||||
| 42.56 | ]30, 40[ | Partial responders | 7.25 | Nonresponders | 7.25 | |||||||
| Phelps (2018) | Latent growth mixture modeling | Baseline, postintervention, 3- and 9-month follow-up | Military | 5 | PCL | >50 | 63.13 | 43.48 | High symptom extra-large change | 7.9 | Responders | 7.9 |
| 66.86 | 65.00 | Very high symptom small change | 32.5 | Nonresponders 1 | 85.4 | |||||||
| 67.28 | 62.62 | Very high symptom large change | 3.0 | Nonresponders 2 | ||||||||
| 59.93 | 53.24 | High symptom large change | 49.9 | Nonresponders 3 | ||||||||
| 43.91 | 37.84 | Low symptom large change | 6.7 | Subclinical | 6.7 | |||||||
| Rosenkranz (2011) | Latent class growth modeling | Baseline, postintervention, and 6-month follow up | Civilian; adult survivors of CSA | 3 | TSC-40 | −15 | 44.46 | 35.48 | Group 1 | 47.52 | Responders | 84.15 |
| 67.86 | 48.38 | Group 2 | 36.63 | Responders | ||||||||
| 70.88 | 70.81 | Group 3 | 15.84 | Nonresponders | 15.84 | |||||||
| Schumm (2013) | Growth mixture modeling | Baseline, each week during CPT treatment, within 2 weeks of postintervention | Military | 3 | PCL-S | >50 | 57.88 | 35.78 | Class 2 | 57.1 | Responders | 81.4 |
| 49.32 | 24.14 | Class 3 | 24.3 | Responders | ||||||||
| 70.64 | 51.38 | Class 1 | 18.6 | Nonresponders | 18.6 | |||||||
| Stein (2012) | Growth mixture modeling | Baseline, weekly, postintervention and follow up (3 or 6 months) | Civilian; female victims of interpersonal violence | 2 | PDS | >17 | 28.71 | ]0, 10[ | Responders | 87 | Responders | 87 |
| 35.19 | ns change | Nonresponders | 13 | Nonresponders | 13 | |||||||
| Taylor (2001) | Dynamic cluster analysis | Baseline, weekly, postintervention and 3-month follow-up | Civilian; victims of road accident | 2 | PSS | >17 | ]30, 35[ | ]20, 25[ | Responders | 60 | Nonresponders 1 | 100 |
| ]35, 40[ | ]35, 40[ | Partial responders | 40 | Nonresponders 2 | ||||||||
Note. For most studies, PTSD severity scores’ standard deviations were not available. CSA = childhood sexual abuse; CPT = Cognitive Processing Therapy; HTQ = Harvard Trauma Questionnaire; PDS = Posttraumatic Stress Diagnostic Scale; PCL= Posttraumatic Stress Disorder Checklist; PCL-M = PCL-Military Version; PCL-S = PCL-Specific Trauma Version; PTSD = post-traumatic stress disorder; PSS = PTSD Symptom Scale; TSC-40 = Trauma Symptom Checklist-40; CSA = childhood sexual abuse; ][= interval excluding extreme values; ∼ = about; − = not mentioned; ns = nonsignificative; av. = average.
Associated predictors
In this review, a total of 22 factors that were investigated in at least two studies were examined as predictors of treatment response trajectories. The factors examined by each study are presented in Table 1. The trajectories reclassified as responder, nonresponder, and subclinical were compared as a function of demographic, clinical, and PTSD-related variables to identify what describes individuals assigned to the three response patterns.
Demographic predictors
Age was the only demographic variable that was repeatedly found to be a significant predictor. Most studies indicated that younger age predicted being in the responder subgroup. As for ethnicity, sex, marital status, and education, most studies did not find a difference among responders, nonresponders, and subclinical participants on these variables.
PTSD-related predictors
Baseline hyperarousal symptoms and combat exposure severity were the most consistently supported predictors. In fact, multiple studies found that they significantly predicted assignment to the nonresponse trajectories. In addition, baseline avoidance and reexperiencing symptoms and anger were also supported in some studies while not in others. Such as, some found that nonresponders had higher anger, avoidance, and reexperiencing symptoms at the beginning of treatment.
Clinical predictors
Of the clinical predictors investigated, baseline depression symptoms and diagnosis, alcohol use and abuse, and anxiety symptoms were strongly supported. In fact, nearly all studies that investigated these predictors found that they significantly predicted assignment to the nonresponse trajectories. Finally, one study found that higher baseline social support predicted being in the subclinical participants subgroup and lower baseline social support predicted being in the nonresponder category.
Discussion
The studies revealed between two and five heterogeneous PTSD symptom severity trajectories, while most supported a three-trajectory model: responders, nonresponders, and subclinical participants. The summed proportion of samples reclassified into each trajectory varied across studies. However, on average, responders accounted for 35.5% (SD = 37.84) of samples, nonresponders for 58.5% (SD = 36.58), and 3.3% (SD = 5.38) of samples were subclinical. Although the mean prevalence of nonresponders is higher than the rates usually found in therapies for PTSD,11 many elements could explain this discrepancy. First, since trajectory analysis procedures typically do not exclude dropouts, the prevalence of nonresponders has greater ecological validity since it also includes participants who abandoned treatment. Second, many authors have suggested that one of the drawbacks of exposure-based treatments for PTSD is that they may be less well tolerated by patients,46 resulting in higher dropout rates.11,47 In this review, five studies reported using at least one exposure strategy.28,38–40,43 They all reported high proportions of nonresponders, suggesting that exposure may have increased the number of dropouts, and this might be reflected in a greater rate of nonresponders: 82.3%, 41.3%, 96.1%, 85.4%, and 100.0% of their samples were nonresponders. However, four of these studies used veteran samples that are known to not respond as well to psychotherapy for PTSD as civilians,10 and this should also be taken into account. Third, given that the psychotherapies used across studies were varied in type, duration, and setting, it was not possible to determine whether some were less efficient than others, thereby contributing to an increased proportion of nonresponders. Taken together, these results highlight the necessity for studies examining trajectories and predictors of treatment response to different types of psychotherapies using randomized controlled trials. Given that some subgroups may respond differently to therapy parameters, treatment-related predictors (e.g., number of sessions, therapist training, patient–therapist relationship) should also be investigated.
This review has investigated many of the factors that could explain the differences across our subgroups. Many studies included demographic variables as potential predictors of therapy response. When testing ethnicity, sex, marital status, and education of individuals, little significant differences were found. Only some studies found that more responders were married,43 Caucasian,42 and female.29 Age, on the other hand, was the only demographic predictor that was sufficiently supported. Specifically, Currier,41 Galovski,44 and Schumm42 all found a tendency for responders to be younger than nonresponders. Although research suggests that younger populations have higher dropout rates,19 this demographic seems to benefit more from therapy. In fact, meta-analysis also shows that older adults benefit less from therapy than their younger counterparts.48,49 Given that, with age, cognitive flexibility seems to decreases,50 younger patients may be better equipped to challenge existing beliefs and change maladaptive patterns of thinking than are older patients.51
Two studies considered if baseline social support differed among trajectories. Allan and colleagues43 found no difference between groups. However, Fletcher29 found that the nonresponse subgroups had significantly lower social support at baseline than all other trajectories. This is consistent with a recent meta-analysis that found that lower perceived social and marital support were related to higher PTSD symptoms after cognitive-behavioral therapy.52 Interestingly, Fletcher29 also found that the subclinical group reported more social support than did responders. As social support is one of the strongest predictors of PTSD severity,53,54 this could explain why subclinical groups report the highest levels of support and therefore had slightly subclinical PTSD at baseline. Finally, lack of social support may also explain findings from one study where significantly fewer nonresponders were married.43 However, more studies are needed to clarify the underlying mechanisms of social support and the protective role that different types of support play in the association between PTSD and treatment response.
Characteristics of traumatic event were sparsely investigated. Only combat exposure severity produced consistently strong results. Currier,41 Elliott,28 and Schumm42 all found that nonresponders had been more severely exposed to combat than other subgroups, thus suggesting that current therapies may be disregarding some consequences specific to combat exposure, such as the impact of killing.55–57 Future studies should therefore investigate trauma severity as a predictor of treatment response given that it is an important risk factor for PTSD development.3 It would also be important to examine characteristics of traumatic events, such as additional exposure to nonfear-based traumatic events in veteran populations or contact with sexual abuser in survivors of childhood sexual abuse, as these characteristics may impact response to treatment. Two studies found that higher baseline levels of PTSD symptoms predicted classification into nonresponder trajectories over other trajectories. Yet, four studies did not find such a difference, indicating that preintervention severity was similar between subgroups. It seems possible that clinical presentation of PTSD and of comorbid disorders rather than PTSD severity may be interfering with treatment response.
In fact, clinical presentation of PTSD can vary substantially depending on severity of each symptom cluster and on the presence of comorbid conditions. Interestingly, some studies tested whether the severity of PTSD symptom clusters (i.e., numbing, reexperiencing, hyperarousal, avoidance, dissociation, anger, guilt) could distinguish responders from nonresponders. Results were mixed for most symptom clusters. However, nonresponders tended to have higher hyperarousal symptoms29,45 and more severe anger28 than did other groups. This result is consistent with Stapleton et al.,58 who suggested that although PTSD treatments (i.e., exposure therapy, relaxation training, Eye Movement Desensitization and Reprocessing [EMDR]) reduced anger, this is not sufficient, and significant residual anger remained. Some authors have even suggested that anger, guilt, and shame, which, contrary to anxiety, are not amendable to a habituation effect, may even be exacerbated through exposure.59,60 Taken together, these results suggest that some symptoms and clinical features common in PTSD may not be adequately targeted in current therapies. It may thus be necessary to include treatment strategies that specifically focus on anger (i.e., cognitive restructuring). Effective therapy may need to move from a “one size fits all” approach, where treatment solely focuses on treatment of PTSD, to one that is more tailored to clinical presentation of PTSD and that considers comorbid conditions of patients. This is especially true when treating PTSD since the presence of comorbid disorders represents a rule rather than an exception.6
In this review, eight studies examined baseline symptoms of depression as a predictor of treatment response and most studies found a strong association. Elliott,28 Fletcher,29 and Schumm42 consistently found that nonresponders had notably higher levels of depression. Likewise, a baseline diagnosis of MDD significantly predicted assignment to a nonresponder pattern.45 However, because the lowest levels of depressive symptoms were not steadily present among responders, more research is needed to understand under which circumstances depression hinders treatment response. Riso and colleagues61 found that individuals suffering from chronic depression have deep-rooted maladaptive beliefs and incapacitating symptoms. Therefore, responders and nonresponders could have different clinical and cognitive presentations of depression,61 rendering them differentially reactive to PTSD treatment. Sleep disturbances, found in both PTSD and depression,4 are associated to symptom exacerbation,62 chronic fatigue,63 and poorer clinical outcomes.64 If not addressed in treatment, these disturbances could affect treatment response. Symptoms of anxiety28,43 and alcohol use or abuse28,41 were also consistently predictors of nonresponse. In sum, results strongly support the presence of comorbid disorders (e.g., anxiety symptoms, diagnosis of MDD, alcohol use, depression symptoms) as significant predictors of nonresponse to therapy for PTSD.
Overall, these findings emphasize the need for further research given that the presence of comorbid disorders could provide a rationale for the subtyping of individuals with PTSD and more accurate triaging of patients based on individual-level factors. Further, these results support the importance of developing interventions that target comorbid mental health difficulties either before engaging in trauma-focused psychotherapy or by integrating treatment strategies that specifically focus on theses comorbid symptoms over the course of therapy, as this may be more adapted to the complex presentation of the nonresponder group. Finally, some of the other predictors of poorer response to treatment, such as having more anger or less social support, are ones that could be addressed during treatment, again warranting a more flexible approach to treatment. For instance, including significant others in treatment or, as mentioned, cognitive restructuring aimed at anger could be beneficial for the nonresponder subgroup.
Limitations
Despite the strengths of this review, a few caveats should be noted. First, in terms of the generalizability of these conclusions, all included studies were from high-income countries, despite the absence of publication date or language search restrictions. However, samples were mostly representative in terms of age, sex, education level, and ethnic background while they excluded severely distressed individuals (e.g., suicidal or psychotic). This allows for the generalization of results to adults from high-income countries receiving psychotherapy for PTSD and who are not severely distressed. Second, the quality assessment of studies using the DBI should be interpreted with caution as this tool does not consider relative importance of different validity indicators. In fact, criticism has been raised toward the available quality assessment tools as some suggest that they are problematic and unreliable.65,66 Nonetheless, until new methods of assessment are made available, the DBI is useful in ensuring that the literature in this review is not impacted by major biases. Third, some of the predictors yielded inconsistent findings, which may be due to utilization of different measures for treatment outcomes of interest. Fourth, response to specific treatments could be predicted by different factors. Because psychotherapies in this review were so diverse, the predictors for specific treatments could not be examined. This may, in part, explain the inconsistent results for the predictors. More studies are needed to investigate if predictors of response vary according to specific treatment modalities. Fifth, while impossible in the current study, a reclassification method using a reliable change criterion, rather than a probable PTSD criterion, would have been more accurate. However, this was impossible in the current study given that reliable change criterions have yet to be identified for many of the tools used for PTSD symptomatology assessment. Nevertheless, trajectories were generally well accounted for. Future studies should use PTSD severity measures that suggest such a clinical change criterion, as it would allow for more precise analysis of trajectories and identification of predictors. Finally, given the important variability in measurement time points and trajectory characteristics across study, the comparison of trajectory subgroups required a pre–post comparison of each latent subgroup’s PTSD severity scores. Although this method provides greater insight on psychotherapy response than traditional pre–post comparison of entire samples, it does not capture the essence of trajectory modeling. Nonetheless, given that this review includes all available studies on trajectories of response to psychotherapy for PTSD, it allows for a comprehensive and exhaustive understanding of this topic. However, since only 11 studies on this topic were identified, this limits the scope of the results. Therefore, the current review highlights the importance of using a similar method of compilation and comparison of predictors of response trajectories to investigate other noteworthy research questions, such as confirming that predictors of response are consistent across treatments. Despite these limitations, this review identified predictors essential for furthering our understanding of who benefits from psychotherapy for PTSD, which is its main implication.
Conclusion
This review is the first to systematically compile data on the heterogeneous response trajectories to psychotherapy for PTSD and to inform on demographic, clinical, and PTSD-related predictors of these trajectories. The converging evidence from multiple studies, presented in this review, provides more robust evidence on the role of some predictors while highlighting the need to further research others. In fact, the studies reviewed reported relatively similar types of PTSD symptom trajectories. The subgroup of responders tended to be younger, female, Caucasian, married, and, most importantly, they reported less comorbid disorders and symptoms. The subclinical group was the least prevalent and tended to report lower PTSD severity and anger, and the highest levels of social support. The nonresponder subgroup was the most prevalent: They tended to be older, less were married, more were male, they had been more severely exposed to combat, they reported more anger, hyperarousal, depression (symptoms and diagnosis), anxiety and alcohol abuse, and they reported less social support. All studies reported a nonresponse subgroup, suggesting that current psychotherapies are not sufficiently efficient in treating this subpopulation with treatment refractory symptoms and comorbid symptoms. Furthermore, comorbidity rates found in this subgroup highlights the urgent necessity to treat not only the primary disorder but to also to address comorbid conditions that are associated with nonresponse to treatment using a more tailored approach. Analysis of predictors also underline a need to further test how treatment-related variables (e.g., therapist training, treatment strategies), as well as psychological (e.g., comorbid conditions, sleep disturbances,), social (e.g. social support characteristic, partner support, disability benefits), and trauma-related factors (e.g., trauma characteristics), may explain why some benefit from treatment while others do not. Finally, this review supports latent trajectories as a method to better capture distinct treatment responses and effectiveness while identifying the factors related to poor treatment response.
Research Data
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access page (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Research Data abstract for Identifying Trajectories and Predictors of Response to Psychotherapy for Post-Traumatic Stress Disorder in Adults: A Systematic Review of Literature by Michelle Dewar, Alison Paradis and Christophe A. Fortin in The Canadian Journal of Psychiatry
Supplemental Material, 875602_supplemental_data_file for Identifying Trajectories and Predictors of Response to Psychotherapy for Post-Traumatic Stress Disorder in Adults: A Systematic Review of Literature by Michelle Dewar, Alison Paradis and Christophe A. Fortin in The Canadian Journal of Psychiatry
Footnotes
Authors’ Note: The data file is provided as a supplementary file. It should be noted that some of the data were obtained through correspondence with authors of the included articles. All data were double-entered, the data presented in the data file are the result of this double entry.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Fonds de recherche du Québec en santé (FRQS) master’s training grant awarded to Michelle Dewar. The FRQS was not involved in conducting any part of this review.
ORCID iD: Michelle Dewar, PhD  https://orcid.org/0000-0001-8492-1365
https://orcid.org/0000-0001-8492-1365
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;48(3):216–222. [DOI] [PubMed] [Google Scholar]
- 2. Van Ameringen M, Mancini C, Patterson B, Boyle MH. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. 2008;14(3):171–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132(6):959. [DOI] [PubMed] [Google Scholar]
- 4. American Psychiatry Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed). Washington: Author; 2013. [Google Scholar]
- 5. Davidson JR. Recognition and treatment of posttraumatic stress disorder. JAMA. 2001;286(5):584–588. [DOI] [PubMed] [Google Scholar]
- 6. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. [DOI] [PubMed] [Google Scholar]
- 7. Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events?. Am Psychol. 2004;59(1):20–28. [DOI] [PubMed] [Google Scholar]
- 8. Santiago PN, Ursano RJ, Gray C, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PLoS One. 2013;8(4):e59236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morina N, Wicherts JM, Lobbrecht J, Priebe S. Remission from post-traumatic stress disorder in adults: a systematic review and meta-analysis of long term outcome studies. Clin Psychol Rev. 2014;34(3):249–255. [DOI] [PubMed] [Google Scholar]
- 10. Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162(2):214–227. [DOI] [PubMed] [Google Scholar]
- 12. Kelly KA, Rizvi SL, Monson CM, Resick PA. The impact of sudden gains in cognitive behavioral therapy for posttraumatic stress disorder. J Trauma Stress. 2009;22(4):287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134–168. [DOI] [PubMed] [Google Scholar]
- 14. Forbes D, Creamer M, Hawthorne G, Allen N, McHugh T. Comorbidity as a predictor of symptom change after treatment in combat-related posttraumatic stress disorder. J Nerv Ment Dis. 2003;191(2):93–99. [DOI] [PubMed] [Google Scholar]
- 15. Ehlers A, Clark DM, Dunmore E, Jaycox L, Meadows E, Foa EB. Predicting response to exposure treatment in PTSD: the role of mental defeat and alienation. J Trauma Stress.1998;11(3):457–471. [DOI] [PubMed] [Google Scholar]
- 16. Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: a controlled study. Arch Gen Psychiatry. 1998;55(4):317–325. [DOI] [PubMed] [Google Scholar]
- 17. Jaycox LH, Foa EB, Morral AR. Influence of emotional engagement and habituation on exposure therapy for PTSD. J Consult Clin Psychol. 1998;66(1):185. [DOI] [PubMed] [Google Scholar]
- 18. Tarrier N, Sommerfield C, Pilgrim H, Faragher B. Factors associated with outcome of cognitive-behavioural treatment of chronic post-traumatic stress disorder. Behav Res Ther. 2000;38(2):191–202. [DOI] [PubMed] [Google Scholar]
- 19. Cloitre M, Chase Stovall-McClough K, Miranda R, Chemtob CM. Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse-related posttraumatic stress disorder. J Consult Clin Psychol. 2004;72(3):411. [DOI] [PubMed] [Google Scholar]
- 20. Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol. 2005;73(5):953. [DOI] [PubMed] [Google Scholar]
- 21. Rizvi SL, Vogt DS, Resick PA. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behav Res Ther. 2009;47(9):737–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kluft RP, Bloom SL, Kinzie JD. Treating traumatized patients and victims of violence. New Dir Ment Health Serv. 2000. Summer;(86):79–102. [DOI] [PubMed] [Google Scholar]
- 23. Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 1999;4(2):139–157. [DOI] [PubMed] [Google Scholar]
- 24. Muthén B. Second-generation structural equation modeling with a combination of categorical and continuous latent variables: New opportunities for latent class–latent growth modeling In: Sayers A, Collins L, editors. New methods for the analysis of change. Washington (DC): American Psychiatry Association; 2001. [Google Scholar]
- 25. McCutcheon AL. Latent class analysis. Thousand Oaks (CA): Sage; 1987. p. 64. [Google Scholar]
- 26. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22(3):276. [PMC free article] [PubMed] [Google Scholar]
- 28. Elliott P, Biddle D, Hawthorne G, Forbes D, Creamer M. Patterns of treatment response in chronic posttraumatic stress disorder: an application of latent growth mixture modeling. J Trauma Stress. 2005;18(4):303–311. [DOI] [PubMed] [Google Scholar]
- 29. Fletcher S, Elklit A, Shevlin M, Armour C. Predictors of PTSD treatment response trajectories in a sample of childhood sexual abuse survivors: the roles of social support, coping, and PTSD symptom clusters. J Interpers Violence. 2017. doi: 10.1177/0886260517741212. [DOI] [PubMed] [Google Scholar]
- 30. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34(8):669–673. [DOI] [PubMed] [Google Scholar]
- 31. McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD checklist: a critical review. Clin Psychol Rev. 2010;30(8):976–987. [DOI] [PubMed] [Google Scholar]
- 32. Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the PDS. Psychol Assess. 1997;9:445–451. [Google Scholar]
- 33. Griffin MG, Uhlmansiek MH, Resick PA, Mechanic MB. Comparison of the posttraumatic stress disorder scale versus the clinician-administered posttraumatic stress disorder scale in domestic violence survivors. J Trauma Stress. 2004;17(6):497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Foa EB. PDS: Posttraumatic Stress Diagnostic Scale: Manual. London: Pearson; 1995. [Google Scholar]
- 35. Zimmerman C, Hossain M, Yun K, et al. The health of trafficked women: a survey of women entering posttrafficking services in Europe. Am J Public Health. 2008;98(1):55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rosenkranz SE, Muller RT. Outcome following inpatient trauma treatment: differential response based on pre-treatment symptom severity. Psychol Trauma. 2011;3(4):453–461. [Google Scholar]
- 37. Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59(1):12. [DOI] [PubMed] [Google Scholar]
- 38. Phelps AJ, Steel Z, Metcalf O, et al. Key patterns and predictors of response to treatment for military veterans with post-traumatic stress disorder: a growth mixture modelling approach. Psychol Med. 2018;48(1):95–103. [DOI] [PubMed] [Google Scholar]
- 39. Taylor S, Fedoroff IC, Koch WJ, Thordarson DS, Fecteau G, Nicki RM. Posttraumatic stress disorder arising after road traffic collisions: patterns of response to cognitive-behavior therapy. J Consult Clin Psychol. 2001;69(3):541. [PubMed] [Google Scholar]
- 40. Clapp JD, Kemp JJ, Cox KS, Tuerk PW. Patterns of change in response to prolonged exposure: implications for treatment outcome. Depress Anxiety. 2016;33(9):807–815. [DOI] [PubMed] [Google Scholar]
- 41. Currier JM, Holland JM, Drescher KD. Residential treatment for combat-related posttraumatic stress disorder: identifying trajectories of change and predictors of treatment response. PLoS One. 2014;9(7):e101741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schumm JA, Walter KH, Chard KM. Latent class differences explain variability in PTSD symptom changes during cognitive processing therapy for veterans. Psychol Trauma. 2013;5(6):536–544. [Google Scholar]
- 43. Allan NP, Gros DF, Myers US, Korte KJ, Acierno R. Predictors and outcomes of growth mixture modeled trajectories across an exposure-based PTSD intervention with veterans. J Clin Psychol. 2017;73(9):1048–1063. [DOI] [PubMed] [Google Scholar]
- 44. Galovski TE, Harik JM, Blain LM, Farmer C, Turner D, Houle T. Identifying patterns and predictors of PTSD and depressive symptom change during cognitive processing therapy. Cognit Ther Res. 2016;40(5):617–626. [Google Scholar]
- 45. Stein NR, Dickstein BD, Schuster J, Litz BT, Resick PA. Trajectories of response to treatment for posttraumatic stress disorder. Behav Ther. 2012;43(4):790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Foa EB, Zoellner LA, Feeny NC, et al. Does imaginal exposure exacerbate PTSD symptoms?. J Consult Clin Psychol. 2002;70(4):1022. [DOI] [PubMed] [Google Scholar]
- 47. Tarrier N, Pilgrim H, Sommerfield C, et al. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. J Consult Clin Psychol. 1999;67(1):13. [DOI] [PubMed] [Google Scholar]
- 48. Hendriks GJ, Oude Voshaar RC, Keijsers GPJ, Hoogduin CA, van Balkom AJ. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatr Scand. 2008;117(6):403–411. [DOI] [PubMed] [Google Scholar]
- 49. Thorp SR, Ayers CR, Nuevo R, Stoddard JA, Sorrell JT, Wetherell JL. Meta-analysis comparing different behavioral treatments for late-life anxiety. Am J Geriatr Psychiatry. 2009;17(2):105–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Daigneault S, Braun CM, Whitaker HA. Early effects of normal aging on perseverative and non-perseverative prefrontal measures. Dev Neuropsychol. 1992;8(1):99–114. [Google Scholar]
- 51. Johnco C, Wuthrich VM, Rapee RM. The role of cognitive flexibility in cognitive restructuring skill acquisition among older adults. J Anxiety Disor. 2013;27(6):576–584. [DOI] [PubMed] [Google Scholar]
- 52. Fredette C, El-Baalbaki G, Palardy V, Rizkallah E. Social support and cognitive–behavioral therapy for posttraumatic stress disorder: a systematic review. Traumatology. 2016;22(2):131–144. [Google Scholar]
- 53. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748. [DOI] [PubMed] [Google Scholar]
- 54. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52. [DOI] [PubMed] [Google Scholar]
- 55. Ford JD. Disorders of extreme stress following war-zone military trauma: associated features of posttraumatic stress disorder or comorbid but distinct syndromes?. J Consult Clin Psychol. 1999;67(1):3. [DOI] [PubMed] [Google Scholar]
- 56. Gray RM, Liotta RF. PTSD: extinction, reconsolidation, and the visual-kinesthetic dissociation protocol. Traumatology. 2012;18(2):3–16. [Google Scholar]
- 57. Shay J. Moral injury. Intertexts. 2012;16(1):57–66. [Google Scholar]
- 58. Stapleton JA, Taylor S, Asmundson GJ. Effects of three PTSD treatments on anger and guilt: exposure therapy, eye movement desensitization and reprocessing, and relaxation training. J Trauma Stress. 2006;19(1):19–28. [DOI] [PubMed] [Google Scholar]
- 59. Kubany ES, Manke FP. Cognitive therapy for trauma-related guilt: conceptual bases and treatment outlines. Cogn Behav Pract. 1995;2(1):27–61. [Google Scholar]
- 60. Pitman RK, Altman B, Greenwald E, et al. Psychiatric complications during flooding therapy for posttraumatic stress disorder. J Clin Psychiatry. 1991;52(1):17–20. [PubMed] [Google Scholar]
- 61. Riso LP, Du Toit PL, Blandino JA, et al. Cognitive aspects of chronic depression. J Abnorm Psychol. 2003;112(1):72–80. [PubMed] [Google Scholar]
- 62. Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: a 1-year prospective study of injured survivors of motor vehicle accidents. Am J Psychiatry. 2002;159(5):855–857. [DOI] [PubMed] [Google Scholar]
- 63. Pillar G, Malhotra A, Lavie P. Post-traumatic stress disorder and sleep—what a nightmare!. Sleep Med Rev. 2000;4(2):183–200. [DOI] [PubMed] [Google Scholar]
- 64. Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress. 2004;17(1):69–73. [DOI] [PubMed] [Google Scholar]
- 65. Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019;70:747–770. [DOI] [PubMed] [Google Scholar]
- 66. Jüni P, Witschi A, Bloch R, et al. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282(11):1054–1060. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access page (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Research Data abstract for Identifying Trajectories and Predictors of Response to Psychotherapy for Post-Traumatic Stress Disorder in Adults: A Systematic Review of Literature by Michelle Dewar, Alison Paradis and Christophe A. Fortin in The Canadian Journal of Psychiatry
Supplemental Material, 875602_supplemental_data_file for Identifying Trajectories and Predictors of Response to Psychotherapy for Post-Traumatic Stress Disorder in Adults: A Systematic Review of Literature by Michelle Dewar, Alison Paradis and Christophe A. Fortin in The Canadian Journal of Psychiatry