Prolonged intensive care unit (ICU) hospitalizations are costly, increasing in prevalence, and strain ICU resources.[1–4] One year mortality is high and the recovery for survivors of prolonged ICU hospitalizations is typically long and marked by new morbidities.[3, 4] Thus, with advances in critical care technology, patients with prolonged ICU hospitalizations, their families, and physicians are challenged to make complex, high-stakes decisions without clear guidance about long-term prognosis.
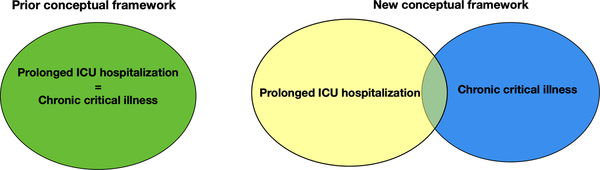
Recent work has focused on who these patients are and why they remain in the ICU for prolonged periods of time.[5–8] Commonly measured patient characteristics on admission such as age and co-morbidities have not consistently been associated with the need for prolonged ICU hospitalizations. (Of note, other premorbid patient characteristics such as frailty have not been studied as a risk factor for persistent critical illness.)These findings have challenged pre-conceived beliefs that prolonged ICU hospitalizations only occur for older patients or those with multiple comorbidities.[5, 8] Instead, observational data suggest the development of new organ dysfunctions not present on admission contribute to the development of prolonged ICU hospitalizations.[6, 7] This finding moves our understanding of prolonged ICU hospitalizations beyond the prototype of chronic critical illness—a patient with unresolving respiratory failure—and towards a more complete picture of how prolonged ICU hospitalizations emerge over time in the ICU.[3] (Figure)
Figure.
New framework of prolonged ICU hospitalizations.
In this issue of Thorax, Hermans et al describe the long-term mortality and morbidity of patients with prolonged ICU hospitalizations who are matched to short-stayers (patients who remained in the ICU for < 8 days).[9] The authors created 3 different matched cohorts to evaluate long-term mortality (total and post-28 day 5-year mortality) and morbidity. The authors performed a re-analysis of prospectively collected data of the EPaNIC-trial, which was a randomized control trial conducted in 7 ICUs at the University of Hospitals of Leuven and Jessa and evaluated early versus late parental supplementation of enteral nutrition.[10]
Given the lack of consensus about the definition of a “prolonged ICU hospitalization”, the authors operationally defined this construct as ≥ 8 days and utilized propensity matching with short-stayers. The cut-off of 8 days, while noted to be arbitrary by the authors, resonates with empirically derived population-level definitions of persistent critical illness.[11] In sensitivity analysis, Hermans et al noted that between ICU day 6 to 8, mortality was no longer associated to the severity of illness and diagnosis on admission. This affirms prior studies which demonstrate that, over time, ICU admission characteristics become increasingly less associated with a patient’s inpatient mortality.[11, 12] Hermans et al also found the patients with prolonged ICU stays developed more organ dysfunctions compared to patients with short-stays: mechanical ventilation >2 days, new dialysis, utilization of vasopressors/inotropes > 2 days, and elevated bilirubin. While it is not reported when in the ICU course these organ dysfunctions developed, it is plausible that at least some of these organ dysfunctions newly developed after admission.
The primary outcomes of their analyses were total and post-28 day 5-year mortality which were both higher for patients with prolonged ICU hospitalizations as compared to propensity matched short-stayers with an absolute total and post-28-day 5-year mortality difference of 12% and 11.1% respectively. These findings are intriguing—the post-28 day 5-year mortality, to be clear, looks at only those who survive the initial 28-days after ICU admission, and therefore separates initial mortality from later mortality. The importance of this method allows for patient characteristics which are associated with short-term mortality (e.g. severity of illness) to be disentangled from long term mortality by using the survivors.[13] In Cox regression, patients with prolonged ICU hospitalization compared to short-stayers were at increased risk of dying (total mortality HR: 1.447 95% CI: 1.286–1.697 and post-28 day-5-year mortality HR: 1.556 95% CI: 1.019–1.774).
Secondary outcomes focused on morbidity as measured by the 6-minute walking distance, handgrip strength, and the physical function component of the SF-36. Activities of daily living were measured by the Barthel index and quality of life was measured by the SF-36. Patients with prolonged ICU hospitalizations performed worse as compared to propensity matched short-stayers and notably rated their overall health as inferior compared to short-stayers.
Hermans et al then ask: what potentially modifiable in-ICU events are more common during prolonged ICU stays. Such an analysis must be interpreted with care, subject as it is to varying exposure times, inability to differentiate markers from causes, and censoring of the extreme phenotype (e.g. really bad care on ICU day 4 might lead to death and so may be more common in short ICU stays) With those caveats, an exploratory regression analysis of events occurring during the ICU stay found hypoglycemia, use of any corticosteroids, use of any neuromuscular agents, use of any benzodiazepines for more than 1 day, the need for mechanical ventilation for > 2 days, initiation of new dialysis, and the occurrence of new infection were associated with increased total and post-28 day 5-year mortality.
These findings begin to shed light on the long-term outcomes of patients with prolonged ICU hospitalizations with a focus not just on mortality but also, importantly, on morbidity and its drivers. In this study, propensity matching after randomization to the EPaNIC-trial facilitated comparison between similar patients, and demonstrated that: (1) patients with prolonged ICUs can be matched to similar patients with shorts stays on admission, and (2) implies that patient characteristics on admission (e.g. age, gender, comorbidities, type and severity of illness) do not fully explain the increased long-term mortality. Consequently, providers should take caution on utilizing patient characteristics on admission for prognostication in patients with prolonged ICU stays.
It is worth noting that the patients with prolonged ICU hospitalizations differ in important ways from patients previously labeled as “chronic critical illness”—defined by unresolving respiratory failure. In this cohort, the patients with prolonged ICU hospitalizations had a 5-year survival of 51.8% which is significantly higher than the previously reported 1 year mortality for the chronically critically ill of 40–60%.[3] The functional limitations were also not as bleak for the patients with prolonged ICU stays as compared to the patients with chronic critical illness with one oft-quoted study reporting only 12% of chronic critically ill patients being functional in the 1st year after the hospitalization.[3]
Hermans et al also highlight potentially modifiable events (eg. hypoglycemia, utilization of benzodiazepines, and steroids) in the ICU which are associated with long term mortality and morbidity. If validated in other cohorts, these findings provide a starting point for a deeper dive into why prolonged ICU hospitalizations are happening and whether poor patient outcomes in this population are modifiable or preventable. This line of investigation may lead to the development of interventions that ultimately change the trajectory for patients with prolonged ICU hospitalizations.
Prior to intervention development, though, one needs to consider the limitations of the work of Hermans et al.[9] This study was based on a cohort of patients from two centers in Europe, and the findings may not be generalizable to other ICUs. The adjustment for confounders was limited due to available data and may cause residual confounding, thereby over-estimating the risk of mortality and morbidity. Furthermore, the baseline, pre-hospitalization functional status of the patients was unknown. Therefore, it is possible that the differences in functional outcomes seen in this study were not a result of the prolonged ICU exposure, but, instead, related to poorer baseline function. Lastly, the authors operationally defined 8 or more days as a prolonged ICU stay, which is not directly comparable to other studies of prolonged ICU hospitalizations that do not use this timeframe. Using terms consistently in research is paramount to moving our collective understanding of how to best care and prognosticate for these patients and their families and points to a need for consensus in research definitions.
For too long have we assumed that all prolonged ICU hospitalizations are synonymous with prolonged mechanical ventilation, overlooking the events which are occurring in the ICU driving these stays. The findings of Hermans et al help to illuminate the events which are occurring in the ICU, driving prolonged ICU hospitalizations and reinforcing the limited role patient characteristics at the time of ICU admission have on prognostication for long term outcomes. Moving forward, this study raises difficult questions and challenges about how to improve care for patients with prolonged ICU stays: how do we prognosticate for these patients and families when commonly used admission characteristics such as age, comorbidities and severity of illness are not useful; how do we guide patients and their families through complex, high-stakes decisions; and can we truly intervene sooner to prevent prolonged ICU hospitalizations or improve long-term outcomes?
Acknowledgments
Funding: This work was supported by NIH K12HL138039-02 (EMV, TJI) and K23 HL146890 (JMK).
Footnotes
Disclosure: This article represents the authors views and not those of the US Government or the Department of Veterans Affairs.
References:
- 1.Kahn JM, Le T, Angus DC, et al. The epidemiology of chronic critical illness in the United States*. Crit Care Med 2015;43(2):282–7. doi: 10.1097/CCM.0000000000000710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iwashyna TJ, Hodgson CL, Pilcher D, et al. Persistent critical illness characterised by Australian and New Zealand ICU clinicians. Crit Care Resusc 2015;17(3):153–8. [PubMed] [Google Scholar]
- 3.Nelson JE, Cox CE, Hope AA, et al. Chronic critical illness. Am J Respir Crit Care Med 2010;182(4):446–54. doi: 10.1164/rccm.201002-0210CI [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson JE, Meier DE, Litke A, et al. The symptom burden of chronic critical illness. Crit Care Med 2004;32(7):1527–34. [DOI] [PubMed] [Google Scholar]
- 5.Viglianti EM, Zajic P, Iwashyna TJ, et al. Neither vitamin D levels nor supplementation are associated with the development of persistent critical illness: a retrospective cohort analysis. Crit Care Resusc 2019;21(1):39–44. [published Online First: 2019/03/13] [PMC free article] [PubMed] [Google Scholar]
- 6.Iwashyna TJ, Viglianti EM. Patient and Population-Level Approaches to Persistent Critical Illness and Prolonged Intensive Care Unit Stays. Crit Care Clin 2018;34(4):493–500. doi: 10.1016/j.ccc.2018.06.001 [published Online First: 2018/09/19] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darvall JN, Boonstra T, Norman J, et al. Persistent critical illness: baseline characteristics, intensive care course, and cause of death. Crit Care Resusc 2019;21(2):110–18. [published Online First: 2019/05/31] [PubMed] [Google Scholar]
- 8.Viglianti EM, Kramer R, Admon AJ, et al. Late organ failures in patients with prolonged intensive care unit stays. J Crit Care 2018;46:55–57. doi: 10.1016/j.jcrc.2018.03.029 [published Online First: 2018/04/24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hermans G, Van Aerde N, Meersseman P, et al. Five-year mortality and morbidity impact of prolonged versus brief ICU stay: a propensity score matched cohort study. Thorax 2019. (epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 10.Casaer MP, Mesotten D, Hermans G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med 2011;365(6):506–17. doi: 10.1056/NEJMoa1102662 [published Online First: 2011/07/01] [DOI] [PubMed] [Google Scholar]
- 11.Iwashyna TJ, Hodgson CL, Pilcher D, et al. Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. Lancet Respir Med 2016;4(7):566–73. doi: 10.1016/S2213-2600(16)30098-4 [DOI] [PubMed] [Google Scholar]
- 12.Bagshaw SM, Stelfox HT, Iwashyna TJ, et al. Timing of onset of persistent critical illness: a multi-centre retrospective cohort study. Intensive Care Med 2018;44(12):2134–2144. doi: 10.1007/s00134-018-5440-1 [published Online First: 2018/11/14] [DOI] [PubMed] [Google Scholar]
- 13.Shankar-Hari M, Harrison DA, Ferrando-Vivas P, et al. Risk Factors at Index Hospitalization Associated With Longer-term Mortality in Adult Sepsis Survivors. JAMA Netw Open 2019;2(5):e194900. doi: 10.1001/jamanetworkopen.2019.4900 [published Online First: 2019/06/01] [DOI] [PMC free article] [PubMed] [Google Scholar]