Abstract
Background:
Evidence suggests that behavioral, social, and environmental factors may modify the effects of life stress on health and performance of new nurses as they transition to hospitals.
Objectives:
To describe the methods of a study designed to investigate the role of social, behavioral, and environmental factors in modifying the adverse effects of stress on new nurses and discuss demographic, health, and life stress characteristics of the cohort at baseline.
Methods:
A prospective cohort design was used to conduct a comprehensive assessment of health endpoints, life stress, behaviors, personal traits, social factors, indicators of engagement and performance, and environmental exposures in nursing students. Adjusted odds ratios and analyses of covariance were used to examine associations between these factors at baseline.
Results:
Health indicators in the cohort were comparable or better than in the broader U.S. population and lifetime stress exposure was lower than among students from other majors. Exposure to more lifetime stressors was associated with greater risk for various health conditions, including hypertension, diabetes, and depression. Conversely, better social, environmental, behavioral, and personal profiles were associated with protective effects for the same health conditions.
Discussion:
These data comprehensively summarize the lives of predominately Hispanic nursing students and highlight risk and resilience factors associated with their health and wellbeing. The findings are timely, as the nursing field diversifies in preparation to care for a diverse and aging population. Comprehensively assessing stress-health relationships among student nurses ought to inform the policies, practices, and curricula of nursing schools to better prepare nurses to thrive in the often-strenuous healthcare environment.
Keywords: childhood adversity, mental health, inflammation, health disparities, environmental exposure
As the largest group of healthcare professionals in the world, nurses play a far-reaching role in health care systems. In hospitals, direct patient contact places nurses in a position to directly affect the outcomes, safety, and satisfaction of patients. However, chronic psychosocial stress can negatively affect the capacity of nurses to provide quality care by increasing risk for medical error (Elfering, Semmer, & Grebner, 2006) and reducing job satisfaction (Roberts & Grubb, 2014). Nurses experience stress as a result of demanding work responsibilities, long shifts, frequently changing roles (Moustaka & Constantinidis, 2010), and—in some instances—incivility between co-workers (Oyeleye, Hanson, O’Connor, & Dunn, 2013). This type of frequent and prolonged stress exposure can cause biological deterioration (i.e., allostatic load) that increases individuals’ susceptibility to numerous health problems and cognitive decline (McEwen, 1998).
Among nurses, work-related stress has been associated with health problems such as obesity, cardiovascular disease, and type 2 diabetes (McNeely, 2005), as well as with greater risk for depression, burnout, and suicidality (Karasek & Theorell, 1990). Chronic stress can also affect cognitive function, including attention and memory, which among nurses could increase their risk of committing medication errors, failing to recognize life-threatening signs and symptoms, or missing other critical patient safety issues (Karimi, Adel-Mehraban, & Moeini, 2018; McEwen, 1998). Stress also increases turnover (i.e., quitting current job) and attrition (i.e., quitting nursing) (Hayes et al., 2012; Shader, Broome, Broome, West, & Nash, 2001), particularly among new nurses (Blythe et al., 2008; Rudman, Omne-Ponten, Wallin, & Gustavsson, 2010), which in turn reduces the effectiveness and productivity of understaffed nursing teams (Newman, Maylor, & Chansarkar, 2001; Squillace, Bercovitz, Rosenoff, & Remsburg, 2008).
New nurses appear to be particularly vulnerable to stress during their transition from nursing school to the work environment (Fink, Krugman, Casey, & Goode, 2008). During the first two years after graduation, 34% of nurses change jobs, with stress being among the more frequent reasons for leaving (Kovner, Brewer, Fatehi, & Jun, 2014; Kovner & Djukic, 2009). Studies have also reported that professions that require continuous human contact, such as nursing, are susceptible to stress and burnout even before employment (Moreira & Furegato, 2013; Rudman & Gustavsson, 2012). Nursing students, for example, encounter stressors unique to the nursing curriculum, such as clinical training (Pulido-Martos, Augusto-Landa, & Lopez-Zafra, 2012), and experience more stress from experiences common to other college students, such as test anxiety (Turner & McCarthy, 2017). The need to balance financial, family, and other life issues along with academic demands can also lead to severe stress among students. At this time, little is known about how stress experienced in nursing school is associated with susceptibility to stress in the work environment. Understanding of how students experience stress could improve the performance and wellbeing of new nurses and, ultimately, the health of their patients.
The effect that stress has on the health and performance of nursing students can be mediated by other life stressors, as well as personal, behavioral, social, and environmental factors that are experienced during school or earlier in life. For instance, the type, number, and severity of stressors experienced during childhood appears to increase the sensitivity and inflammatory response to stress experienced later in life (Nusslock & Miller, 2016), which can in turn elevate risk for depression, cardiovascular disease, and hypersensitivity to chemicals and air pollutants (Bell, Baldwin, Russek, Schwartz, & Hardin, 1998; Black, Okiishi, Gabel, & Schlosser, 1999; Olvera Alvarez, Kubzansky, Campen, & Slavich, 2018). Personality might also modify the stress experience of nursing students (Aldwin, Spiro, Levenson, & Cupertino, 2001; Judge & Ilies, 2002). Behaviors such as sleep, diet, and physical activity lessen or amplify the effect of stress on health as a result of inflammation in the body (Cecil, McHale, Hart, & Laidlaw, 2014; Gleeson et al., 2011; Minihane et al., 2015). The amount and type of social support (Thoits, 2011) and attachment (Mattanah, Lopez, & Govern, 2011) have also been associated with protective health outcomes. Although research on stress among nurses and nursing students is abundant, no studies have examined how behavioral, social, and environmental factors interact in nursing students. This has occurred despite the fact that comprehensive assessments of how these multi-level and multi-dimensional factors interact could help us prepare the next generation of nurses to thrive and deliver high-quality care in often-challenging work environments.
The Nurse Engagement and Wellness Study (NEWS) addresses these important issues by examining how behavioral, social, and environmental factors interact to modify the effects of stress on the health and performance of nursing students. NEWS also seeks to investigate how the stress experience in nursing school transcends into the work environment. In this first paper on NEWS, we provide an overview of the study design and describe key associations between stress and health-related characteristics in the cohort at baseline.
METHODS
Study Design
The NEWS is a prospective cohort study of nursing students and early career nurses directed by a team of nursing, social, and environmental health researchers. Data and biological samples are stored at the Biobehavioral Research Laboratory at the University of Texas at El Paso. The study was approved by institutional review boards at the University of Texas at El Paso (857149–1) and Harvard University (16–0080).
Sampling
Female and male individuals between 18 and 55 years old, enrolled in the Bachelor of Science in Nursing (BSN) program at the University of Texas at El Paso, were eligible to participate. Participants were recruited via emails, posters, flyers, media outlets (e.g., magazine, newsletter) and in-class information sessions. No member of the research team was an instructor in the BSN program during the study. Interested students were asked to visit the laboratory where they provided written informed consent. Participants who dropped out of the BSN program, transferred to another university, or failed to graduate from the program were removed from the sample.
Data Collection
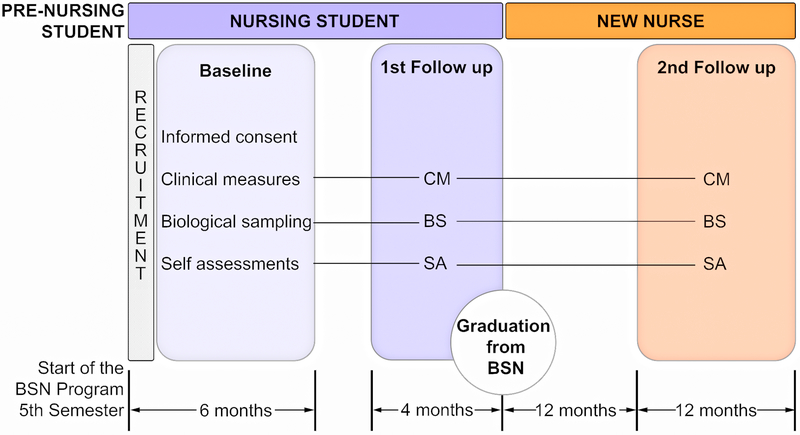
Data were collected at three timepoints. Baseline measurements were conducted within six months of students entering the BSN program. The first follow-up was within four months prior to graduation from the BSN program. Finally, the second follow-up was within 12 to 24 months after graduation (Figure 1).
Figure 1.
Schematic of the Nurse Engagement and Wellness Study (NEWS) study design. Baseline assessments were conducted during their first six month in the Bachelor of Science in Nursing (BSN) program, the first follow-up was conducted four months prior to graduation, and the second follow up was conducted one year after graduation. CM = clinical measures; BS = biological sampling; SA = self-assessments.
Study assessments included health endpoints, biomarkers, life stress exposure, behaviors and personal traits, social factors, indicators of engagement and performance, and environmental exposures, which were conducted via clinical measures, biological samples, and self-reports as described in Supplemental Digital Content Table 1 (SDC 1). Clinical measures and biological samples were collected during laboratory visits. Serum and plasma were separated from blood samples by centrifugation within an hour of collection. Saliva was collected using the passive drool technique (Salimetrics, 2015). Stool samples were collected by participants using two Para-Pak vials: one containing 5 mL of RNAlater preservative, and another containing 10 mL of glycerol solution and 2 mL of acid-washed glass beads. Participants placed a small, teaspoon-sized sample in each tube, stored the samples in their freezer in a designated package, and delivered the sample to the laboratory within 24 hrs. Then, serum, plasma, saliva and stool samples were stored at −80° C until analysis.
During each timepoint, participants also completed the list of self-assessments described in SDC 1. Participants had twelve weeks, starting at the beginning of the academic semester, to complete these instruments. They were required to complete each assessment once enrolled in the cohort. The date and time of completion of each assessment were recorded.
Study Assessments
Health endpoints and biomarkers:
Indicators of metabolic health included: systolic blood pressure (SBP), diastolic blood pressure (DBP), body mass index (BMI), and fasting levels of triglycerides, cholesterol (total, LDL, HDL), glucose and glycohemoglobin (A1c). Cardiovascular endpoints included carotid intima-media thickness (CIMT) measured via ultrasound (Stein et al., 2008), heart rate variability measured via electrocardiogram (ECG), and retinal blood vessel caliber measured via fundus imaging (De Boever, Louwies, Provost, Int Panis, & Nawrot, 2014). Retinal arterial narrowing has been shown to predict hypertension, and venular widening has been linked with systemic inflammation, endothelial dysfunction, and atherosclerosis (Adar et al., 2010; Louwies, Panis, Kicinski, De Boever, & Nawrot, 2013). Depressive severity was measured with the patient health questionnaire for depression (PHQ-9). Symptoms of chemical sensitivity such as skin and eye irritation, dizziness, pain, fatigue, stomachache, asthma and allergies diagnosis, headache, and balance problems were assessed using a modified survey version of an existing environmental sensitivities survey (Andersson, Andersson, Bende, Millqvist, & Nordin, 2009; Nordin, Palmquist, & Claeson, 2013).
The health state of participants was assessed using the following definitions. Hypertension stage 1 was defined as SBP between 130–139 mmHg or DBP between 80–89 mmHg (Whelton et al., 2018). Hypertension stage 2 was defined as SBP ≥ 140 mmHg or DBP ≥ 90 mmHg (Whelton et al., 2018). Overweight was defined as BMI between 25 and 29 and obese as BMI ≥ 30 (Centers for Disease Control and Prevention, 2016). LDL ≥ 130 mg/dL was considered high and HDL ≤ 40 mg/dL was considered low (Zwald, Akinbami, Fakhouri, & Fryar, 2017). Triglycerides ≥ 150 mg/dL were considered elevated (Carroll, Kit, & Lacher, 2015). Prediabetes was defined as fasting glucose between 100 mg/dL and 125 mg/dL or A1c between 5.7% and 6.4% (Centers for Disease Control and Prevention, 2017). Diabetes was defined as fasting glucose > 125 mg/dL or A1c > 6.4% (Centers for Disease Control and Prevention, 2017). Moderate or worse depression severity was defined as a PHQ-9 score ≥ 10 (Brody, Pratt, & Hughes, 2018).
Systemic inflammation was assessed via serum levels of C-reactive protein (CRP) and the inflammatory cytokines interleukin (IL)-1β, IL-6, IL-8, and tumor necrosis factor-alpha (TNFα). Serum levels of Fetuin A (FA) and Amyloid P (SAP) were also assessed as markers of cardiovascular disease risk. Serum samples were analyzed in duplicate wells using the Milliplex™ MultiAnalyte Profiling (MAP) Human CVD Panel 3 pre-mixed kit (EMD Millipore Corp, Billerica, MA) for CRP, FA and SAP, and the Human High Sensitivity T Cell pre-mixed kit (EMD Millipore Corp, Billerica, MA) for IL-1β, IL-6, IL-8, and TNFα. The plates were read on a Luminex 200 analyzer (Luminex Corporation, Austin, TX) running Milliplex Analyst Version 5.1 software (Vigene Tech Inc. Carlisle, MA). Concentrations for each biomarker were calculated in reference to a five-point best-fitting standard curve. Salivary cortisol levels were assessed using an enzyme immunoassay (Salimetrics, State College, PA, USA).
Lifetime stress exposure.
Cumulative count and severity of the acute and chronic stressors that participants experienced across the lifespan were measured with the Stress and Adversity Inventory for Adults (Adult STRAIN) (Slavich & Shields, 2018). The STRAIN is an online system for assessing stressors occurring across the life course that may exert a cumulative effect on biological processes that promote disease. The STRAIN adheres to commonly agreed-upon best practices by assessing the specific timing of stress exposure, distinguishing between different forms and types of stress, and accounting for both “objective” exposure (i.e., counts) as well as “subjective” experiences (i.e., perceived stress severity) (Slavich & Shields, 2018). Because the STRAIN produces a set of indices for multiple types of stressors (e.g., work, education, financial), it is ideally suited for the investigation of interactions between education-related stress and non-education related stress among nursing students (see http://www.strainsetup.com).
Behaviors and personal traits.
The frequency of consumption by food type (i.e., vegetables, fruit, sugary drinks), type and duration of physical activity (e.g., walking, swimming, running), smoking frequency, frequency of drug and alcohol consumption, sleep duration, and sleep quality was obtained via self-reports. Personality type, stress coping style, forgiveness, empathy, and self-efficacy were measured with the psychometric instruments listed in SDC 1. Emotional intelligence was assessed using the Mayer-Salovey-Caruso Emotional Intelligence Test™ and cognitive ability was assessed using the overclaiming technique (Paulhus & Harms, 2004).
Social factors.
Socio-economic status was assessed by maternal educational attainment, household income, poverty level, and median income of the census block group in which the participant resides. Childhood adversity was measured with the Adverse Childhood Experiences (ACE) questionnaire (Felitti et al., 1998). Social support (Mitchell et al., 2003) and attachment to parent and peers (Mattanah et al., 2011) were also assessed.
Engagement and performance endpoints.
Burnout was measured using the Maslach Burnout Inventory (MBI) (Maslach & Jackson, 1981; Yavuz & Dogan, 2014). The student version of the general survey [MBI-GS (S)] was used at baseline and at first follow-up, and the human services survey at second follow-up. Academic performance was assessed via course grades, grade point average (GPA), and nursing licensure examination (NCLEX) results. Voluntary attrition from nursing program was used as a measure of engagement. After graduation, clinical performance was tracked with the Six Dimension Scale of Nursing Performance (SDNS) (Schwirian, 1978).
Environmental exposures.
Frequency and quantity of use of hazardous chemicals commonly encountered by nurses, including drugs (e.g., aerosolized antibiotics, antineoplastic drugs), sterilizers and disinfectants, anesthetic gases, and surgical smoke was assessed with a modified version of the Health and Safety Practices Survey of Healthcare Workers (Steege, Boiano, & Sweeney, 2014). The type and frequency of personal care products used in daily life was assessed with a questionnaire modified from Wu et al. (2010). Exposure to green spaces was assessed via satellite imagery (Browning & Lee, 2017) and Google® Streetview™ images based on geocoded addresses (Li, Deal, Zhou, Slavenas, & Sullivan, 2018). Serum levels of cadmium, aluminum, iron, copper, and arsenic were measured via inductively coupled plasma mass spectrometry (ICPMS) (Centers for Disease Control and Prevention, 2012; Funk, Pleil, Sauter, McDade & Holl, 2015; Harkema et al., 2009).
Data Analysis
Descriptive statistics [e.g., means, standard deviations (SD), and percentages] were used to describe the prevalence of common health conditions in the cohort, which in turn were compared against the national prevalence for adults between 20 and 39 years of age using the most recent data from the National Health and Nutrition Survey (NHANES; Centers for Disease Control and Prevention, 2018), unless otherwise specified. Biomarker (e.g., IL-1β, IL-6, IL-8, TNFα, FA, and SAP) and metal levels were transformed with a logarithmic function (base 10) and subsequently standardized. Odds ratios (ORs) were used as measures of associations between the life stress variables and unhealthy states (e.g., hypertension, obesity, depression). For life stress variables tertiles were calculated and ORs were calculated for top versus bottom tertiles via binomial logistic regression. ORs were adjusted for age and gender based on evidence showing that these variables can affect associations between stress and health (Appelman, van Rijn, Ten Haaf, Boersma, & Peters, 2015; Mazure & Swendsen, 2016; Slavich & Irwin, 2014; Tamres, Janicki, & Helgeson, 2002). Analysis of covariance (ANCOVA) were used to characterize the variance of biomarkers (e.g., cytokines, A1c) across stress, behavioral, and environmental variables while controlling for age and gender.
RESULTS
Demographic and Behavioral Characteristics
At baseline, the cohort included 436 participants, 20% of whom were males, with an average age of 25.2 years old (SD = 2.3). Most participants self-identified as white (93%) and Hispanic (90%), and 20% were born outside the United States. Also, most participants (98%) were full-time students, just a few (4%) had a fulltime job, 29% had a part-time job, 20% were living below the poverty line, and 20% were married. A small percentage of participants were current smokers (5%) or drank alcohol more than once a week (7%). Most participants ate fruits (79%) and vegetables (83%) at least twice a week. Although 86% of participants slept at least seven hours on a typical night, 61% did not rate their sleep quality as good. Twenty-one percent of participants had an ACE score equal or greater than four, which is seven percentage points higher than in the general U.S. population (Centers for Disease Control and Prevention, 2015). Descriptive statistics are provided in SDC 2.
Lifetime Stress Exposure
Participants were exposed to an average of 14.8 stressors across the lifespan (SD = 10.7; range, 1–60; possible range, 0–166) as assessed by the Adult STRAIN, with an average overall severity score of 35.3 (SD = 26.0; range, 0–115; possible range, 0–265). When compared to students form the same university but enrolled in other majors (n = 1,186), nursing students experienced fewer total stressors over the life course, F(1, 1807) = 102.4, p < 0.001, with relatively lower cumulative lifetime severity, F(1, 1807) = 82.5, p < 0.001 (Figure 2). Students from other majors reported an average lifetime stressor count of 20.0 (SD = 12.3; range, 1–111) and an average overall cumulative lifetime stressor severity of 49.9 (SD = 30.3; range, 0–245). The variation of stressor count and severity scores across the primary life domains and core social-psychological characteristics assessed by the Adult STRAIN was similar and consistent with prior results (Slavich & Shields, 2018); therefore, we focused the main results on stressor counts.
Figure 2.
Comparison of lifetime stressor exposure by stressor category for nursing and non-nursing male and female students. (A) Nursing students experienced a lower average total exposure to stressors across the lifetime than non-nursing students, F(1,1511) = 49.63, p < .001. With respect to the life domains, female nursing students experienced more marital/partner stressors, F(1,326) = 4.21, p = .041, and reproduction stressors, F(1,326) = 8.35, p = .004, than male nursing students. (B) With respect to stress exposure across core social- psychological characteristics there were no significant differences between female and male nursing students. Color image is available only in online version.
Females experienced an average of 15.3 stressors across the lifespan (SD = 10.2) as compared to 13.2 experienced by males (SD = 12.1) (p = .15). The life stressors most commonly endorsed were from “Other Relationships” (23% by females, 25% by males) and “Marital/Partner” sources (21% by females, 18% by males) (Figure 2A). With respect to the core social-psychological characteristics, the stressors most commonly experienced were “Interpersonal Loss” (27% by females, 30% by males) and “Role Change/Disruption” (23% by females, 21% by males) (Figure 2B).
Across the lifespan, Hispanic participants experienced an average of 14.5 stressors (SD = 10.2) as compared to 17.3 (SD = 13.4) by non-Hispanics (p = .13). Participants with a full-time job experienced an average of 19.2 stressors across the lifespan (SD = 11.1) as compared to 15.5 (SD = 10.1) for those with a part-time job (p = .22) and 14.2 (SD = 10.9) for those without a job (p = .11). Participants younger than 25 years old experienced an average of 12.1 stressors across the lifespan (SD= 8.8), whereas those 25 years of age or older experienced an average of 19.6 stressors (SD = 12.0), with the difference between these groups being significant, F(1, 326) = 42.53, p < 0.001. Participants with an ACE score of zero reported a significantly lower lifetime stress exposure (mean = 8.78; SD = 5.55) than participants with an ACE score ≥ 4 (M = 25.1; SD = 12.4), F(1, 158) = 128.1, p < 0.001. A significant difference persisted when comparing the average lifetime stressor count of participants with ACE scores ≥ 4 and those with ACE score < 4 (M = 12.3; SD = 8.54), F(1, 325) = 94.72, p < 0.001.
Health Conditions at Baseline
The prevalence of stage 2 hypertension in the NEWS cohort (9%) was similar to the national prevalence (8%). Overweight (24%) and obesity (20%) in the cohort was lower than the corresponding national prevalence (30% and 38%). The prevalence of high LDL levels (12%) and low HDL levels in the cohort (20%) were close to their respective national prevalence (12% and 21%). The prevalence of elevated triglycerides (34%) in the cohort was higher than the national prevalence (20%) among individuals between 20 – 39 years but was closer to the same prevalence among Hispanic women (28%) older than 20 years. Prediabetes prevalence (13%) was less than the national average (24%) among individuals between 18 and 44 years of age (Centers for Disease Control and Prevention, 2017). The prevalence of moderate or worse depression severity (23%) was higher than the national prevalence (8%).
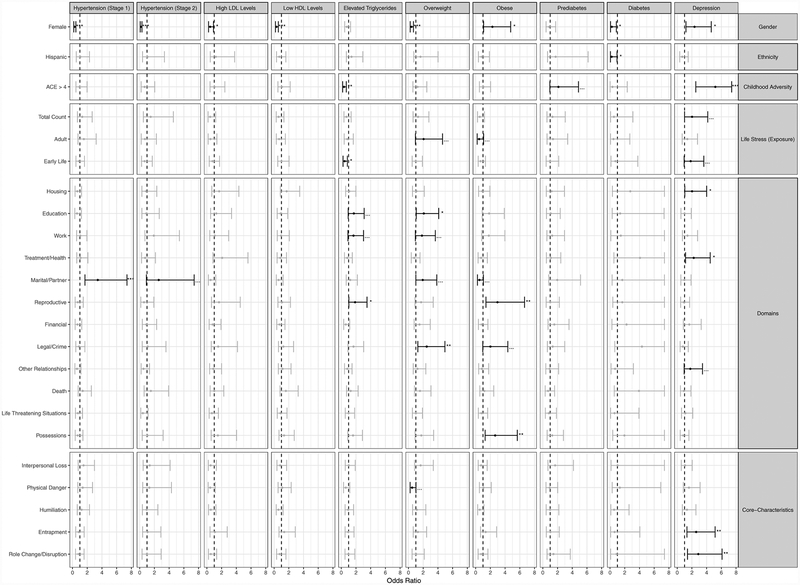
Compared to males, females in the NEWS cohort had lower odds of having hypertension (stage 1 or 2), high LDL, low HDL, being overweight, or having diabetes (for ORs see Figure 3; for summary statistics see SDC 3). Conversely, females had higher odds of being obese or having moderate or worst depression severity than males. Hispanics had lower odds of being diabetic and of suicidal ideation than non-Hispanics.
Figure 3.
Odd ratios and 95% confidence intervals for selected health conditions by life stressor type and selected factors, adjusting for age and gender. Hypertension: Stage 1, systolic blood pressure (SBP) 130–139 mmHg or diastolic blood pressure (DBP) 80–89 mmHg; Stage 2, SBP ≥ 140 mmHg or DBP ≥ 90 mmHg. High low-density lipoproteins (LDL) levels ≥ 130 mg/dL, low high-density lipoproteins (HDL) levels ≤ 40 mg/dL, elevated triglycerides ≥ 150 mg/dL. Overweight, body mass index (BMI) 25–29; Obesity, BMI ≥ 30. Prediabetes, fasting glucose 100 mg/dL - 125 mg/dL or glycated hemoglobin (A1c) 5.7% - 6.4%; diabetes fasting glucose ≥ 125 mg/dL or A1c ≥ 6.4%. Depression, PHQ-9 score ≥ 10, which represents moderate or worse severity. TT = Top tertile, BT = Bottom tertile. † p < 0.10; * p < 0.05; ** p < 0.01; *** p < 0.001; = unadjusted
Several patterns of associations between participants’ life stress exposure and health conditions were observed (for ORs see Figure 3; for summary statistics see SDC 3). Participants with high early life stress exposure (stressor counts in the top tertile) or with ACE scores ≥ 4 had lower odds of having elevated triglycerides as compared to participants with low early life stress exposure (stressor counts in the bottom tertile) or to participants with an ACE score equal to zero, respectively. Compared to low lifetime exposure to marital/partner stressors, high lifetime exposure to marital/partner stressors was associated with greater odds of both stage 1 and stage 2 hypertension (see Figure 3). Similarly, elevated triglycerides were positively associated with lifetime exposure to education, work, and reproductive stressors. Being overweight was positively associated with stress exposure during adulthood, as well as with lifetime exposure to education, work, marital/partner, and legal/crime stressors. Being obese was positively associated with lifetime exposure to reproductive, legal/crime, and possessions stressors (see Figure 3). Moderate or worst depression was positively associated with total lifetime stress exposure, early life stress exposure and ACE scores ≥ 4, and with lifetime stressors involving housing, treatment/health, other relationships, entrapment, and role change/disruption.
Biomarker Levels
The ANCOVA also revealed several significant associations between participants’ lifetime stress exposure and biomarker levels (for detailed results, see SDC 4 and SDC 5). For instance, IL-8 was positively associated with stress exposure across the lifespan F(1,208) = 4.37, p = 0.038, as well as with lifetime exposure to financial F(1,208) = 5.16, p = 0.024 and life-threatening situations stressors F(1,209) = 4.09, p = 0.045. IL-6 was negatively associated with lifetime exposure to housing F(1,209) = 3.57, p = 0.060, education F(1,207) = 3.37, p = 0.068, and reproductive stressors F(1,206) = 3.06, p = 0.082. TNFα was negatively associated with lifetime exposure to housing F(1,209) = 3.61, p = 0.059, education F(1,207) = 4.66, p = 0.032, work F(1,208) = 3.11, p = 0.079, and possessions stressors F(1,206) = 3.69, p = 0.056. Lifetime exposure to possession stressors was also negatively associated with IL-8 F(1,206) = 2.74, p = 0.099.
CIMT was positively associated with lifetime exposure to stressors from multiple sources, including housing F(1,202) = 9.97, p = 0.002, education F(1,198) = 9.53, p = 0.002, work F(1,207) = 10.43, p = 0.001, reproductive F(1,198) = 18.42, p < 0.001, financial F(1,206) = 7.83, p = 0.006, legal F(1,198) = 13.83, p < 0.001, and possessions F(1,197) = 11.76, p < 0.001. RBC was negatively associated with lifetime stress exposure F(1,34) = 3.53, p = 0.069, stress exposure occurring during both early life F(1,31) = 4.36, p = 0.045 and adulthood F(1,34) = 5.02, p = 0.032, as well as with lifetime exposure to housing F(1,34) = 5.94, p = 0.023, marital/partner F(1,34) = 7.87, p = 0.008, and financial stressors F(1,34) = 8.23, p = 0.012. Lifetime exposure to stressors involving treatment/health was positively associated with lymphocyte F(1,22) = 5.57, p = 0.028 and basophil counts F(1,22) = 7.08, p = 0.014. Finally, ACE score was negatively associated with WBC F(1,33) = 4.98, p = 0.033 and RBC F(1,33) = 4.06, p = 0.052, as well as with neutrophil F(1,33) = 4.05, p = 0.052 and monocyte counts F(1,33) = 6.51, p = 0.016.
DISCUSSION
These results represent one of the most comprehensive summaries of the lives and health of nursing students to date. Prevalence of most health conditions measured at baseline in the NEWS cohort was comparable—and sometimes better—than the U.S. population. The prevalence of moderate-to-severe depression in the cohort was comparable to the prevalence (26%) among North American nursing students estimated via meta-analysis (Tung, Lo, Ho, & Tam, 2018) and might be partially explained by the fact that our cohort is predominately young, Hispanic, and female. Evidence shows that females (WHO, 2012), Hispanics (Shattell, Smith, Quinlan-Colwell, & Villalba, 2008), and college students (Buchanan, 2012) are particularly susceptible to depression. NEWS participants also reported fewer lifetime stressors than students from all other majors at the same university and approximately half as many lifetime stressors—with approximately half the total severity—as was recently reported in a nationwide assessment of adults who completed the STRAIN (Slavich & Shields, 2018).
Although NEWS participants generally exhibited relatively good health, there was substantial variability in health risk factors, thus supporting the need to assess factors that might predict disease risk on an individual basis. For example, elevated exposure to lifetime stressors was associated with greater risk of hypertension, diabetes, and depression. More education-related stressors, in turn, were associated with elevated triglycerides, BMI, and CIMT, but also with lower inflammation (e.g., TNFα).
The relevance of investigating the effects of life stress and other factors on health trends in young adults—especially among high-stress exposure groups such as nursing students—is supported by studies showing that health during early life and young adulthood affects lifespan risk for health problems. For example, a case-control study found that depressive disorders often emerge in childhood and continue through the adult life (Harrington, Fudge, Rutter, Pickles, & Hill, 1990). Likewise, a longitudinal study revealed that cardiovascular risk factors such as blood pressure and cholesterol levels in early adulthood predicted subsequent risk of cardiovascular disease in older adulthood (Pletcher, Vittinghoff, Thanataveerat, Bibbins-Domingo, & Moran, 2016).
Among nursing students specifically, it is unclear how health conditions that are present during nursing school affect, or are affected by, the transition into the work environment, and what role stress plays in structuring these effects. It is important to determine the extent to which health risks, susceptibilities, and psychosocial assets persist into the early stages of the nursing profession. Moreover, if these factors persist into the work environment, it will be important to understand how these factors interact and how they moderate or mediate the effects of lifetime stress exposure on health.
Strengths and Limitations
Several strengths and limitations of the present study are noteworthy. For example, although we only report baseline data in the present paper, the NEWS cohort provides a prospective cohort study design, which permits the examination of how early life stressors—as well as behavioral, social, and environmental factors—affect young nurses’ susceptibility and resilience to stress in the workforce. Also, because most students at the University of Texas at El Paso progress through the BSN program as a cohort and hence experience the same coursework and similar clinical experiences, the NEWS supports the assessment of students’ sensitivity to education-related stress and modifying factors as they progress through the program. In contrast, an important limitation to the NEWS is the temporal discordance of some assessments. We plan to account for measures that are not perfectly aligned in time by relying on assessment dates, course, and clinical training schedules, and by asking participants to report on historic data in questionnaires (e.g., “in the last two weeks…”). Still, we might not be able to overcome the fact that some measures are collected at different times in some important analyses. In these cases, the interpretation of results will account for this discordance. Another limitation of the NEWS is that some analyses might fail to properly reject the null hypothesis of no sex effect, given the limited number of males in the cohort.
Importantly, the observations from this study were drawn from a cohort that is predominately Hispanic (90%), with a substantial proportion being foreign-born (20%). Baseline measures and observed associations may thus not apply to the general population of nursing students across the U.S., which in 2014 included 28% racial-ethnic minorities, 8% Hispanics, and 4% foreign-born (NLN, 2014). For instance, minority populations (American Psychological Association, 2017) as well as foreign-born nursing students (Vardaman & Mastel-Smith, 2016) experience higher levels of stress as compared to whites and U.S. born students, respectively. Evidence also shows that Hispanics are at higher risk than non-Hispanics of developing health problems (e.g., diabetes) that are typically associated with stress exposure (Centers for Disease Control and Prevention, 2004).
Despite these shortcomings, the results of this study are valuable as they represent one of the most comprehensive studies on Hispanics and foreign-born nursing students to date. Studying the stress-health relationship in this group of future nurses is timely and relevant, as both the U.S. population—and the healthcare force in the U.S.—is rapidly becoming more diverse (Patel, Ly, Hicks, & Jena, 2018).
CONCLUSION
In conclusion, as the U.S. population ages and the incidence of chronic illness continues to rise, ensuring the availability of a competent nursing force to deal with these challenges will be a central challenge for healthcare systems. Meeting this demand will be difficult if the present shortage of nurses persists. Indeed, workforce problems could get worse if work-related stressors increase and affect the prevalence of major health problems in new nurses. Likewise, it is urgent that the we enhance the learning and working environments of registered nurses in ways that increase their capacity to attain and conserve physical and psychological wellbeing. These efforts will help improve the long-term health and wellbeing of nurses, as well as reduce turnover and attrition in hospitals.
Given the unique demographic composition of its cohort, we believe that the NEWS will result in important contributions to these efforts by identifying factors that could be targeted by schools of nursing and healthcare institutions to minimize the effect of stress on young Hispanic male and female nurses. Indeed, understanding how young Hispanic nurses respond to, and are affected by, life stress is timely and relevant. Institutions like the Health Resources and Services Administration’s Division of Nursing and the National Institute of Nursing Research are striving to diversify the nursing profession to respond to health care needs and disparity-associated challenges of a diversifying U.S. population, and additional research is warranted to help ensure the sustained good physical health, psychological wellness, and productivity of this workforce.
Supplementary Material
Acknowledgement:
This work was supported by a JPB Environmental Health Fellowship award granted to Hector A. Olvera Alvarez by The JPB Foundation and managed by the Harvard T.H. Chan School of Public Health; by Grant 5G12MD007592 from the National Institutes on Minority Health and Health Disparities (NIMHD), a component of the National Institutes of Health (NIH) to Hector Olvera Alvarez; by the Orville Edward Egbert, M.D. Chair endowment to Leslie Robbins; and by the Hoffman Program on Chemicals and Health at the Harvard T.H. Chan School of Public Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to thank the nursing students that participated in this study for their support. They also thank the nursing faculty and the staff of the Biobehavioral Research Laboratory at the School of Nursing at the University of Texas at El Paso for supporting the recruitment and data collection efforts of this study.
Footnotes
The authors have no conflicts of interest to report.
Ethical Conduct of Research: The institutional review boards at UTEP (857149–1) and Harvard University (16–0080) approved this study.
Clinical Trial Registration: None applicable
Contributor Information
Hector A. Olvera Alvarez, School of Nursing, University of Texas at El Paso, El Paso, TX.
Elias Provencio-Vasquez, College of Nursing, University of Colorado, Aurora, CO.
George M. Slavich, Cousins Center for Psychoneuroimmunology and Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, CA.
Jose Guillermo Cedeño Laurent, T.H. Chan School of Public Health, Harvard University, Boston, MA.
Matthew Browning, Department of Recreation, Sport and Tourism, University of Illinois Urbana-Champaign, IL.
Gloria McKee-Lopez, School of Nursing, University of Texas at El Paso, El Paso, TX.
Leslie Robbins, School of Nursing, University of Texas at El Paso, El Paso, TX.
John D. Spengler, T.H. Chan School of Public Health, Harvard University, Boston, MA.
References
- Adar SD, Klein R, Klein BE, Szpiro AA, Cotch MF, Wong TY, … & Kaufman JD (2010). Air pollution and the microvasculature: A cross-sectional assessment of in vivo retinal images in the population-based multi-ethnic study of atherosclerosis (MESA). PLoS Medicine, 7(11), e1000372. doi: 10.1371/journal.pmed.1000372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldwin CM, Spiro III A, Levenson MR, & Cupertino AP (2001). Longitudinal findings from the Normative Aging Study: III. Personality, individual health trajectories, and mortality. Psychology and Aging, 16, 450–465. doi: 10.1037/0882-7974.16.3.450 [DOI] [PubMed] [Google Scholar]
- American Psychological Association. (2017). Stress and health disparities: Contexts, mechanisms, and interventions among racial/ethnic minority and low-socioeconomic status populations. Washington, DC. [Google Scholar]
- Andersson MJ, Andersson L, Bende M, Millqvist E, & Nordin S (2009). The idiopathic environmental intolerance symptom inventory: Development, evaluation, and application. Journal of Occupational and Environmental Medicine, 51, 838–847. doi: 10.1097/JOM.0b013e3181a7f021 [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, & Silver D (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5, 237–249. [Google Scholar]
- Appelman Y, van Rijn BB, Ten Haaf ME, Boersma E, & Peters SA (2015). Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis, 241, 211–218. doi: 10.1016/j.atherosclerosis.2015.01.027 [DOI] [PubMed] [Google Scholar]
- Bell IR, Baldwin CM, Russek LG, Schwartz GE, & Hardin EE (1998). Early life stress, negative paternal relationships, and chemical intolerance in middle-aged women: Support for a neural sensitization model. Journal of Women’s Health, 7, 1135–1147. 10.1089/jwh.1998.7.1135 [DOI] [PubMed] [Google Scholar]
- Black DW, Okiishi C, Gabel J, & Schlosser S (1999). Psychiatric illness in the first-degree relatives of persons reporting multiple chemical sensitivities. Toxicology and Industrial Health, 15(3–4), 410–414. doi: 10.1177/074823379901500315 [DOI] [PubMed] [Google Scholar]
- Blythe J, Baumann A, Zeytinoglu IU, Denton M, Akhtar-Danesh N, Davies S, & Kolotylo C (2008). Nursing generations in the contemporary workplace. Public Personnel Management, 37, 137–159. doi: 10.1177/009102600803700201 [DOI] [Google Scholar]
- Brody DJ, Pratt LA, & Hughes JP (2018). Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief, (303), 1–8. [PubMed] [Google Scholar]
- Browning M, & Lee K (2017). Within what distance does “greenness” best predict physical health? A systematic review of articles with GIS buffer analyses across the lifespan. International Journal of Environmental Resesearch and Public Health, 14(7). doi: 10.3390/ijerph14070675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan JL (2012). Prevention of depression in the college student population: A review of the literature. Archives of Psychiatric Nursing, 26, 21–42. doi: 10.1016/j.apnu.2011.03.003 [DOI] [PubMed] [Google Scholar]
- Camm AJ, Malik M, Bigger JT, Breithardt G, Cerutti S, Cohen RJ, … & Singer D(1996). Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation, 93, 1043–1065. doi: 10.1161/01.CIR.93.5.1043 [DOI] [PubMed] [Google Scholar]
- Carroll M, Kit B, & Lacher D (2015). Trends in elevated triglyceride in adults: United States, 2001–2012. NCHS Data Brief, (198), 198. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2004). Prevalence of diabetes among Hispanics -- selected areas, 1998–2002. MMWR Morbidity and Mortality Weekly Report, 53, 941–944. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2011). Vital signs: Prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol -- United States, 1999–2002 and 2005–200. MMWR Morbidity and Mortality Weekly Report , 60(4), 109–114. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2012). Laboratory Procedure Manual: Cadmium, Lead, Manganese, Mercury, and Selenium. Retrieved from: https://www.cdc.gov/Nchs/Data/Nhanes/Nhanes_13_14/PbCd_H_MET.pdf
- Centers for Disease Control and Prevention (CDC). (2015). Adverse Childhood Experiences (ACEs). Retrieved from: https://www.cdc.gov/violenceprevention/acestudy/index.html
- Centers for Disease Control and Prevention (CDC). (2016). Defining Adult Overweight and Obesity. Retrieved from: https://www.cdc.gov/obesity/adult/defining.html
- Centers for Disease Control and Prevention (CDC). (2017). National Diabetes Statistics Report. Retrieved from: https://www.cdc.gov/diabetes/data/statistics/statistics-report.html
- Centers for Disease Control and Prevention (CDC). (2018). NHANES Qeustionanires, Datasets, and Related Documentation. Retrieved from: https://wwwn.cdc.gov/nchs/nhanes/default.aspx
- Cecil J, McHale C, Hart J, & Laidlaw A (2014). Behaviour and burnout in medical students. Medical Education Online, 19(1), 25209. doi: 10.3402/meo.v19.25209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Boever P, Louwies T, Provost E, Int Panis L, & Nawrot TS (2014). Fundus photography as a convenient tool to study microvascular responses to cardiovascular disease risk factors in epidemiological studies. Journal of Visualized Experiments, (92). doi: 10.3791/51904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- duPont NC, Wang KH, Wadhwa PD, Culhane JF, & Nelson EL (2005). Validation and comparison of luminex multiplex cytokine analysis kits with ELISA: Determinations of a panel of nine cytokines in clinical sample culture supernatants. Journal of Reproductive Immunology, 66, 175–191. doi: 10.1016/j.jri.2005.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfering A, Semmer NK, & Grebner S (2006). Work stress and patient safety: Observer-rated work stressors as predictors of characteristics of safety-related events reported by young nurses. Ergonomics, 49(5–6), 457–469. doi: 10.1080/00140130600568451 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Fink R, Krugman M, Casey K, & Goode C (2008). The graduate nurse experience: qualitative residency program outcomes. Journal of Nursing Administration, 38(7–8), 341–348. doi: 10.1097/01.NNA.0000323943.82016.48 [DOI] [PubMed] [Google Scholar]
- Funk WE, Pleil JD, Sauter DJ, McDade T, & Holl JL (2015). Use of dried blood spots for estimating children’s exposures to heavy metals in epidemiological research. Journal of Environmental & Analytical Toxicology, S7(2). 10.4172/2161-0525.S7-002 [DOI] [Google Scholar]
- Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, & Nimmo MA (2011). The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nature Reviews Immunology, 11, 607–615. doi: 10.1038/nri3041 [DOI] [PubMed] [Google Scholar]
- Gosling SD, Rentfrow PJ, & Swann WB (2003). A very brief measure of the Big-Five personality domains. Journal of Research in Personality, 37, 504–528. doi: 10.1016/s0092-6566(03)00046-1 [DOI] [Google Scholar]
- Harkema JR, Wagner JG, Kaminski NE, Morishita M, Keeler GJ, McDonald JD, Barrett EG, & HEI Health Review Committee. (2009). Effects of concentrated ambient particles and diesel engine exhaust on allergic airway disease in Brown Norway rats. Research Report (Health Effects Institute), (145), 5–55. [PubMed] [Google Scholar]
- Harrington R, Fudge H, Rutter M, Pickles A, & Hill J (1990). Adult outcomes of childhood and adolescent depression. I. Psychiatric status. Archives of General Psychiatry, 47, 465–473. doi: 10.1001/archpsyc.1990.01810170065010 [DOI] [PubMed] [Google Scholar]
- Hayes LJ, O’Brien-Pallas L, Duffield C, Shamian J, Buchan J, Hughes F, … & North N (2012). Nurse turnover: A literature review: An update. International Journal of Nursing Studies, 49, 887–905. 10.1016/j.ijnurstu.2011.10.001 [DOI] [PubMed] [Google Scholar]
- Judge TA, & Ilies R (2002). Relationship of personality to performance motivation: A meta-analytic review. Journal of Applied Psychology, 87, 797–807. doi: 10.1037/0021-9010.87.4.797 [DOI] [PubMed] [Google Scholar]
- Karasek R, & Theorell T (1990). Healthy work: Stress, productivity, and the reconstruction of working life. New York: Basic Books. [Google Scholar]
- Karimi A, Adel-Mehraban M, & Moeini M (2018). Occupational stressors in nurses and nursing adverse events. Iranian Journal of Nursing and Midwifery Research, 23, 230–234. doi: 10.4103/ijnmr.IJNMR_253_15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, & Hellhammer DH (1993). The Trier Social Stress Test: A tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology, 28(1–2), 76–81. doi: 10.1159/000119004 [DOI] [PubMed] [Google Scholar]
- Kovner CT, Brewer CS, Fatehi F, & Jun J (2014). What does nurse turnover rate mean and what is the rate? Policy, Politics, & Nursing Practice, 15(3–4), 64–71. doi: 10.1177/1527154414547953 [DOI] [PubMed] [Google Scholar]
- Kovner CT, & Djukic M (2009). The nursing career process from application through the first 2 years of employment. Journal of Professional Nursing, 25, 197–203. doi: 10.1016/j.profnurs.2009.05.002 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D, Deal B, Zhou X, Slavenas M, & Sullivan WC (2018). Moving beyond the neighborhood: Daily exposure to nature and adolescents’ mood. Landscape and Urban Planning, 173, 33–43. doi: 10.1016/j.landurbplan.2018.01.009 [DOI] [Google Scholar]
- Louwies T, Panis LI, Kicinski M, De Boever P, & Nawrot TS (2013). Retinal microvascular responses to short-term changes in particulate air pollution in healthy adults. Environmental Health Perspectives, 121, 1011–1016. doi: 10.1289/ehp.1205721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach C, & Jackson SE (1981). The measurement of experienced burnout. Journal of Occupational Behaviour, 2, 9–113. 10.1002/job.4030020205 [DOI] [Google Scholar]
- Mattanah JF, Lopez FG, & Govern JM (2011). The contributions of parental attachment bonds to college student development and adjustment: A meta-analytic review. Journal of Counseling Psychology, 58, 565–596. doi: 10.1037/a0024635 [DOI] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44. 10.1111/j.1749-6632.1998.tb09546.x [DOI] [PubMed] [Google Scholar]
- McNeely E (2005). The consequences of job stress for nurses’ health: Time for a check-up. Nursing Outlook, 53, 291–299. doi: 10.1016/j.outlook.2005.10.001 [DOI] [PubMed] [Google Scholar]
- Mayer JD, Salovey P, Caruso DR, & Sitarenios G (2003). Measuring emotional intelligence with the MSCEIT V2.0. Emotion, 3, 97–105. doi: 10.1037/1528-3542.3.1.97 [DOI] [PubMed] [Google Scholar]
- Mazure CM, & Swendsen J (2016). Sex differences in Alzheimer’s disease and other dementias. The Lancet Neurology, 15, 451–452. doi: 10.1016/S1474-4422(16)00067-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller CS, & Prihoda TJ (1999). The Environmental Exposure and Sensitivity Inventory (EESI): a standardized approach for measuring chemical intolerances for research and clinical applications. Toxicology and Industrial Health, 15(3–4), 370–385. 10.1177/074823379901500311 [DOI] [PubMed] [Google Scholar]
- Miller GE, Rohleder N, Stetler C, & Kirschbaum C (2005). Clinical depression and regulation of the inflammatory response during acute stress. Psychosomatic Medicine, 67, 679–687. doi: 10.1097/01.psy.0000174172.82428.ce [DOI] [PubMed] [Google Scholar]
- Minihane AM, Vinoy S, Russell WR, Baka A, Roche HM, Tuohy KM, … Calder PC (2015). Low-grade inflammation, diet composition and health: Current research evidence and its translation. British Journal of Nutrition, 114, 999–1012. doi: 10.1017/S0007114515002093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, Froelicher ES, … & Berkman LF (2003). A short social support measure for patients recovering from myocardial infarction: The ENRICHD Social Support Inventory. Journal of Cardiopulmonary Rehabilitation and Prevention, 23, 398–403. doi: 10.1097/00008483-200311000-00001 [DOI] [PubMed] [Google Scholar]
- Moreira DP, & Furegato AR (2013). Stress and depression among students of the last semester in two nursing courses. Revista Latino-Americana de Enfermagem, 21, 155–162. doi: 10.1590/S0104-11692013000700020 [DOI] [PubMed] [Google Scholar]
- Moustaka E, & Constantinidis TC (2010). Sources and effects of work-related stress in nursing. Health Science Journal, 4(4), 210–216. [Google Scholar]
- National League for Nursing (NLN) (2014). Annual Survey of Schools of Nursing, Academic Year 2013–2014. Retrieved from: http://www.nln.org/newsroom/nursing-education-statistics/annual-survey-of-schools-of-nursing-academic-year-2013-2014
- Newman K, Maylor U, & Chansarkar B (2001). The nurse retention, quality of care and patient satisfaction chain. International Journal of Health Care Quality Assurance, 14(2–3), 57–68. doi: 10.1108/09526860110386500 [DOI] [PubMed] [Google Scholar]
- Nordin S, Palmquist E, & Claeson AS (2013). The Environmental Symptom-Attribution Scale: Metric properties and normative data. Journal of Environmental Psychology, 36, 9–17. doi: 10.1016/j.jenvp.2013.06.006 [DOI] [Google Scholar]
- Nusslock R, & Miller GE (2016). Early-life adversity and physical and emotional health across the lifespan: A neuroimmune network hypothesis. Biological Psychiatry, 80, 23–32. doi: 10.1016/j.biopsych.2015.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogedegbe G, & Pickering T (2010). Principles and techniques of blood pressure measurement. Cardiology Clinics, 28, 571–586. doi: 10.1016/j.ccl.2010.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olvera Alvarez HA, Kubzansky LD, Campen MJ, & Slavich GM (2018). Early life stress, air pollution, inflammation, and disease: An integrative review and immunologic model of social-environmental adversity and lifespan health. Neuroscience and Biobehavioral Reviews, 92, 226–242. doi: 10.1016/j.neubiorev.2018.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyeleye O, Hanson P, O’Connor N, & Dunn D (2013). Relationship of workplace incivility, stress, and burnout on nurses’ turnover intentions and psychological empowerment. Journal of Nursing Administration, 43, 536–542. doi: 10.1097/NNA.0b013e3182a3e8c9 [DOI] [PubMed] [Google Scholar]
- Patel YM, Ly DP, Hicks T, & Jena AB (2018). Proportion of non-US-born and noncitizen health care professionals in the United States in 2016. JAMA, 320, 2265–2267. doi: 10.1001/jama.2018.14270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulhus DL, & Harms PD (2004). Measuring cognitive ability with the overclaiming technique. Intelligence, 32, 297–314. doi: 10.1016/j.intell.2004.02.001 [DOI] [Google Scholar]
- Pletcher MJ, Vittinghoff E, Thanataveerat A, Bibbins-Domingo K, & Moran AE (2016). Young adult exposure to cardiovascular risk factors and risk of events later in life: The Framingham Offspring Study. PLoS One, 11(5), e0154288. doi: 10.1371/journal.pone.0154288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulido-Martos M, Augusto-Landa JM, & Lopez-Zafra E (2012). Sources of stress in nursing students: A systematic review of quantitative studies. International Nursing Review, 59, 15–25. doi: 10.1111/j.1466-7657.2011.00939.x [DOI] [Google Scholar]
- Roberts RK, & Grubb PL (2014). The consequences of nursing stress and need for integrated solutions. Rehabilitation Nursing, 39, 62–69. doi: 10.1002/rnj.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EJ, Misner L, Ockene IS, & Nicolosi RJ (1993). Evaluation of 7 Cholestech LDX Analyzers for total cholesterol determinations. Clinical Chemistry, 39(5), 860–864. [PubMed] [Google Scholar]
- Rudman A, & Gustavsson JP (2012). Burnout during nursing education predicts lower occupational preparedness and future clinical performance: A longitudinal study. International Journal of Nursing Studies, 49, 988–1001. doi: 10.1016/j.ijnurstu.2012.03.010 [DOI] [PubMed] [Google Scholar]
- Rudman A, Omne-Ponten M, Wallin L, & Gustavsson PJ (2010). Monitoring the newly qualified nurses in Sweden: The Longitudinal Analysis of Nursing Education (LANE) study. Human Resources for Health, 8(1), 10. doi: 10.1186/1478-4491-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salimetrics. (2015). Saliva Collection Handbook. Retrieved from: https://www.salimetrics.com/saliva-collection-handbook/
- Schwirian PM (1978). Evaluating the performance of nurses: A multidimensional approach. Nursing Research, 27, 347–351. doi: 10.1097/00006199-197811000-00004 [DOI] [PubMed] [Google Scholar]
- Shader K, Broome ME, Broome CD, West ME, & Nash M (2001). Factors influencing satisfaction and anticipated turnover for nurses in an academic medical center. Journal of Nursing Administration, 31, 210–216. [DOI] [PubMed] [Google Scholar]
- Shattell MM, Smith KM, Quinlan-Colwell A, & Villalba JA (2008). Factors contributing to depression in latinas of mexican origin residing in the United States: Implications for nurses. Journal of the American Psychiatric Nurses Association, 14, 193–204. doi: 10.1177/1078390308319034 [DOI] [PubMed] [Google Scholar]
- Simon GE, Coleman KJ, Rossom RC, Beck A, Oliver M, Johnson E, … & Rutter C (2016). Risk of suicide attempt and suicide death following completion of the Patient Health Questionnaire depression module in community practice. The Journal of Clinical Psychiatry, 77, 221–227. doi: 10.4088/JCP.15m09776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, & Irwin MR (2014). From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychological Bulletin, 140, 774–815. doi: 10.1037/a0035302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, & Shields GS (2018). Assessing lifetime stress exposure using the Stress and Adversity Inventory for Adults (Adult STRAIN): An overview and initial validation. Psychosomatic Medicine, 80, 17–27. doi: 10.1097/PSY.0000000000000534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squillace MR, Bercovitz A, Rosenoff E, & Remsburg R (2008). An Exploratory Study of Certified Nursing Assistants’ Intent to Leave. Retrieved from: https://aspe.hhs.gov/system/files/pdf/75566/intent.pdf
- Steege AL, Boiano JM, & Sweeney MH (2014). NIOSH health and safety practices survey of healthcare workers: Training and awareness of employer safety procedures. American Journal of Industrial Medicine, 57, 640–652. doi: 10.1002/ajim.22305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, … & Post WS (2008). Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: A consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force endorsed by the Society for Vascular Medicine. Journal of the American Society of Echocardiography, 21(2), 93–111. doi: 10.1016/j.echo.2007.11.011 [DOI] [PubMed] [Google Scholar]
- Stump GS, Husman J, & Brem SK (2012). The Nursing Student Self-Efficacy Scale Development using item response theory. Nursing Research, 61, 149–158. doi: 10.1097/NNR.0b013e318253a750 [DOI] [PubMed] [Google Scholar]
- Tamres LK, Janicki D, & Helgeson VS (2002). Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Personality and Social Psychology Review, 6(1), 2–30. doi:Doi 10.1207/S15327957pspr0601_1 [DOI] [Google Scholar]
- Thoits PA (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52, 145–161. doi: 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Tobin DL, Holroyd KA, Reynolds RV, & Wigal JK (1989). The hierarchical factor structure of the coping strategies inventory. Cognitive Therapy and Research, 13, 343–361. doi: 10.1007/bf01173478 [DOI] [Google Scholar]
- Tung YJ, Lo KKH, Ho RCM, & Tam WSW (2018). Prevalence of depression among nursing students: A systematic review and meta-analysis. Nurse Education Today, 63, 119–129. doi: 10.1016/j.nedt.2018.01.009 [DOI] [PubMed] [Google Scholar]
- Turner K, & McCarthy VL (2017). Stress and anxiety among nursing students: A review of intervention strategies in literature between 2009 and 2015. Nurse Education in Practice, 22, 21–29. doi: 10.1016/j.nepr.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Vardaman SA, & Mastel-Smith B (2016). The transitions of international nursing students. Teaching and Learning in Nursing, 11(2), 34–43. doi: 10.1016/j.teln.2015.12.008 [DOI] [Google Scholar]
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, … & Wright JT Jr. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Journal of the American College of Cardiology, 71, 2199–2269. doi: 10.1016/j.jacc.2017.11.005 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2012). Depression. Retrieved from: http://www.who.int/mediacentre/factsheets/fs369/en/
- Wu XM, Bennett DH, Ritz B, Cassady DL, Lee K, & Hertz-Picciotto I (2010). Usage pattern of personal care products in California households. Food and Chemical Toxicology, 48, 3109–3119. doi: 10.1016/j.fct.2010.08.004 [DOI] [PubMed] [Google Scholar]
- Yavuz G, & Dogan N (2014). Maslach Burnout Inventory-Student Survey (MBI-SS): A validity study. Procedia - Social and Behavioral Sciences, 116, 2453–2457. doi: 10.1016/j.sbspro.2014.01.590 [DOI] [Google Scholar]
- Zwald ML, Akinbami LJ, Fakhouri TH, & Fryar CD (2017). Prevalence of low high-density lipoprotein cholesterol among adults, by physical activity: United States, 2011–2014. NCHS Data Brief (276), 1–8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.