Abstract
Background:
Provider-patient communication underpins many initiatives aimed at reducing the public health burden associated with prescription drug abuse in the United States. The purpose of this qualitative analysis was to examine the characteristics of provider-patient communication about prescription drug abuse from the perspective of prescribers.
Methods:
From 2014 to 2015, ten semi-structured interviews were conducted with a purposive sample of prescribers from multiple professions and medical fields in Central and South Central Appalachia. The interviews were conducted using a guide informed by Social Cognitive Theory and community theory research, audio-recorded, and transcribed verbatim. Thematic analysis, facilitated by NVivo 10 software, was used to generate themes.
Results:
Prescribers described three primary communication patterns with patients related to prescription drug abuse—informative, counteractive, and supportive. Prescribers also reported multiple factors—personal (e.g., education, experiences, and feelings of tension) and environmental (e.g., relationship with a patient, clinical resources, and policies on controlled prescription drugs)—that affect provider-patient communication and, by association, delivery of patient care related to prescription drug abuse.
Conclusions:
The findings suggest provider-patient communication about prescription drug abuse is multidimensional and dynamic, characterized by multiple communication patterns and contributory factors. They have implications for: 1) research aimed at advancing theoretical understanding of prescriber prescription drug abuse communication behaviors with patients and; 2) interventions aimed at strengthening prescriber prescription drug abuse communication behaviors with patients.
Keywords: communication, patients, prescription drug abuse, prescription drug misuse
INTRODUCTION
Prescription drug misuse and abuse are a pressing public health issue in the United States.1–4 In 2016, approximately 6.2 million persons 12 years or older misused prescription drugs in the past month, with approximately 3.3 million persons misusing prescription opioids in particular.5 Prescription opioid use disorder is among the most common types of substance use disorder related to illicit drug use.5, 6 In 2016, approximately 1.8 million persons 12 years or older had a prescription opioid use disorder in the past year.5 Prescription opioids helped fuel the drug overdose epidemic,7 contributing to more than 200,000 drug overdose deaths from 1999 to 2017 according to the Centers for Disease Control and Prevention (CDC).8
Multiple initiatives have been put forward in response to the public health burden associated with prescription drug misuse and abuse1, 3, 9–11—hereafter referred to as prescription drug abuse (PDA). They commonly target the clinical knowledge and practices of healthcare providers, a population optimally positioned to advance PDA prevention, identification, and treatment. Examples of provider-targeted initiatives include: 1) increased pain management and substance abuse education; 2) increased use of clinical practice tools (e.g., prescription drug monitoring program [PDMP]); and 3) increased substance abuse screening and treatment services. The emphasis on providers underscores their centrality to an effective public health response.
Interpersonal communication between providers and patients underpins many provider-targeted initiatives for PDA and associated harms.12 Provider-patient communication accordingly plays a fundamental role in clinical practice.13–15 When effective, provider-patient communication could contribute to positive outcomes for providers (e.g., reduced job-related stress) and patients (e.g., improved satisfaction).15–19 In clinical practice, however, communication problems can be common.17, 20 Ineffective provider-patient communication is concerning as it could contribute to negative outcomes for providers (e.g., malpractice claims) and patients (e.g., missed chances to enhance self-management).16, 18 Effective, situational communication about PDA between providers and patients could thus be critical to maximizing the public health impact of provider-targeted initiatives. PDA communication is especially salient to prescribers, referring herein to providers licensed to prescribe controlled prescription drugs (CPDs). Prescribers are among the gatekeepers of CPDs.21 Evidence suggests a sizable proportion of providers-physicians and pharmacists—consider physicians to hold the primary responsibility for preventing PDA and addiction.22 Similarly, provider-targeted initiatives frequently impact or necessitate action from physicians.23 Multiple provider-targeted initiatives, for example, aim to improve prescribing practices, often for opioids. The National Institute on Drug Abuse further indicated prescribers—specifically physicians—are in a “unique position” to recognize PDA and prevent progression to a substance use disorder.24 For example, they have the potential to facilitate recognition of a problem, access to treatment, and formation of recovery goals among patients.24 Communication between prescribers and patients is integral to all of these clinical practices.
Succinctly, provider-patient communication about PDA remains understudied relative to its underlying role in mitigating PDA and associated harms in the context of healthcare counters. Prior research suggests providers, including prescribers, agree PDA communication with patients is important and, if improved, could deter PDA.12, 25 A comprehensive report on CPD diversion and abuse, however, suggests many physicians do not inquire about PDA when taking the health history of patients and find it hard to discuss PDA with patients.22 A study of prescribers and pharmacists similarly found PDA communication to be “uncomfortable, variable, multifactorial, and often avoided.”12 While qualitative research methods could advance understanding of the characteristics of provider-patient communication about PDA, few studies have used them,12 and fewer, if any, have focused exclusively on prescribers. Hence, this qualitative analysis examined the characteristics of provider-patient communication about PDA using data collected through interviews with prescribers. The findings could inform prescriber-targeted interventions to strengthen provider-patient communication about PDA and, ultimately, prescriber capacity to mitigate PDA and associated harms.
METHODS
Study design and sample
This study employed a qualitative design involving semi-structured interviews with prescribers. Prescribers of CPDs practicing in a clinic affiliated with, or practicing within the service area of, the Appalachian Research Network (AppNET)—a rural, primary care practice-based research network in Central and South Central Appalachia—were eligible. The AppNET infrastructure supported efficient connection to and recruitment of prescribers. The scope of services delivered by AppNET-affiliated clinics, coupled with their rural locale, were presumed to be representative of many clinics in the region.
Purposive sampling was predominantly used to identify and recruit prescribers. Snowball sampling was incorporated after an enrolled prescriber recommended another prescriber for participation. Study staff selected prescribers for: 1) understanding of the PDA problem or clinic proximity to counties where PDA is prevalent; and 2) willingness to discuss the subject. Recruitment entailed an email invitation, followed by a telephone call to prescribers interested in participating. The sample (n=10) included three female and seven male prescribers from multiple professions (i.e., dentistry, medicine, and nursing) and medical fields (e.g., addiction and family medicine). Of relevance to the sample size, prescribers were sampled as part of a mixed methods study focused largely on the patient perspective. A primary goal was to collect data to inform the development of a theory-based, survey instrument to explain patient engagement in situational PDA communication with providers. Data saturation was reached on concepts related to the survey instrument.
Data collection
From May 2014 to April 2015, ten semi-structured interviews were conducted using a guide. The guide was grounded in Social Cognitive Theory26 and communication theory research,27 internally reviewed and refined, and pilot tested with several prescribers prior to use. Prescriber perceptions, behaviors, and experiences regarding PDA communication with patients, along with general perceptions of PDA, were explored. Specific to the development of the patient-targeted survey instrument, prescriber perceptions of four survey instruments—three validated28–30 and one-researcher developed—were explored. One male researcher with interviewing experience and PDA expertise conducted the interviews in a private setting selected by the prescriber, often the clinic where he/she practiced. Another researcher or research assistant took field notes. The interviews were audio-recorded and transcribed verbatim. The transcripts were de-identified and imported into QSR International’s NVivo 10 software.31
Data analysis
Inductive thematic analysis was used to generate themes.32, 33 The researchers, most of whom had experience in qualitative research, engaged in an iterative process of independent transcript review and open dialogue to generate preliminary codes. One researcher refined and finalized the codes, to include defining and organizing the codes into a coding frame. An initial subset of transcripts (n=2) was randomly selected and independently coded by two researchers to evaluate coding consistency and coding frame reliability.34 Consensus-based discussion was used to resolve coding inconsistencies and modify the coding frame for improved reliability. The remaining transcripts were coded by the two researchers thereafter. One researcher compared and combined codes to generate themes, to include a repetitive process whereby the themes were assessed in relation to the coded data and complete dataset.32, 33 The same researcher defined and named the themes and selected representative quotes.32, 33
Ethical considerations
The Institutional Review Board at East Tennessee State University reviewed and approved this study. One researcher explained the study and attained written informed consent before interviews. Prescribers received modest compensation ($50).
RESULTS
Two themes and nine subthemes were identified (Figure 1). Specifically, theme one—factors affecting prescriber communication with and care of patients—included six subthemes, and theme two—prescriber communication patterns with patients—included three subthemes.
Figure 1.
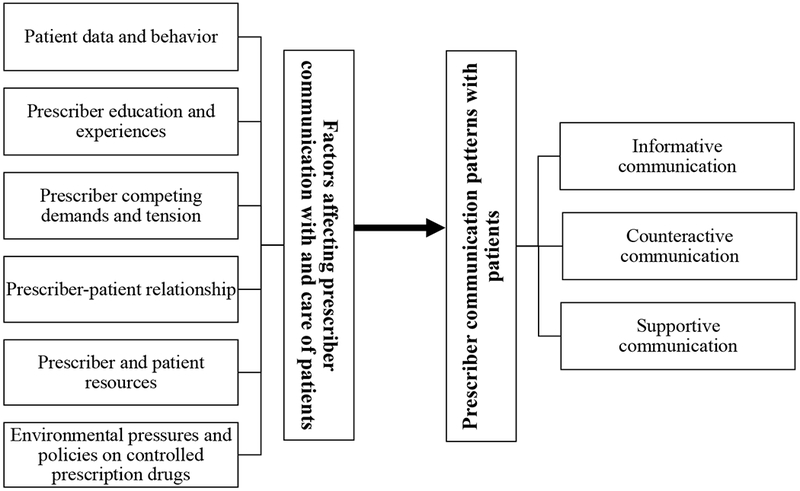
Thematic map of the themes and subthemes identified in provider-patient communication about prescription drug abuse from the prescriber perspective.
Theme one: factors affecting prescriber communication with and care of patients
Prescribers described multiple factors that affect patient communication and care. They focused on not only PDA and addiction, but also the intersection of PDA with pain evaluation and treatment, particularly prescribing CPDs. Six subthemes were generated, with representative quotes presented in Table 1.
Table 1.
Representative Quotes for Theme 1: Factors Affecting Prescriber Communication with and Care of Patients
| Subtheme(s) | Representative Quote(s) |
|---|---|
| Patient data and behavior | … I’ll also look at the medical history for recent or uh, surgeries and, and when I look I’ll say … ‘[Y]ou’re taking Percocet® couple times a day, okay you’re on benzos to sleep right now, okay. Or you’re taking Xanax® and you take two a day right now.’ I’m looking for the benzos, I’m looking for the opiates. I’m looking to see their medical history … then I’m a bit skeptical if the next thing out of their mouth is now uhh, ‘When you do this crown prep here you gonna give me a prescription for drugs?’ |
| … [W]e track those patients [on chronic pain management], we’ve got a log, we track them, it’s part of our QI process. We keep a close eye on them and we bring them in for randomized pill counts, randomized drug screens … we’ve got a very straight protocol that we follow… . | |
| … [P]ain is a subjective data point. And you know our best efforts for the pain scales and everything else I mean it’s not uncommon at all that I’ll work in the ER and be talkin’ to someone who says they have 10 out of 10 pain, texting on their cell phone not paying attention to me with a perfectly flat face while I’m doing it. Like you know so even when we try to apply the objective points to it, it’s not well received and you know and there’s no, no way to measure it quantitatively and so patients will tell us what they want to tell us you know. | |
| … [P]ain medication or other drugs that are more stigmatized than tobacco people tend to be more defensive, they don’t want to talk about it. Tobacco anybody will answer what they do, other drugs most people try to not answer exactly—and will get more defensive. | |
| … [We’ve] all been burned by someone that was either using or diverting and um so you uh there’s always you know a voice in the back of your head when you’re prescribing you know okay this looks legit but I’ve been you know burned before. Um. It’s just there’s a level of uh, of um uneasiness in a relationship I think at times. | |
| Prescriber education and experiences | … [W]e were never really taught how to treat pain…. it has been kind of on the fly. |
| Conducting a risk assessment or drug abuse screen. Yeah, I mean, that is the thing where I feel I’m not as qualified … as I should be … I don’t feel that I’ve had enough education in that regard… . ideally you would do that um but the reality is … I don’t feel very confident in exactly how to do that. | |
| … I self-reported … had the struggles that most addicts have with this, trying to gain, you lose control … that’s when I went to rehab in [city] and that’s … when I first got any kind of information on the pathophysiology and biology of addiction. Wasn’t taught that in medical school, and I was fascinated … I said, you know, there are not accidents and there are no coincidences, there is a purpose in this and that helped fueled me wanting to do addiction medicine. | |
| Prescriber competing demands and tension | I tell [patients] it’s often because then the entire focus of all their issues is about your pain medicine you know. You’ve got diabetes, hypertension, high cholesterol, and COPD and all you wanna talk about is your Lortab® … I’ve got other things I need to focus on you know. And not, not that I’m trying to be negative toward your pain but of all these things, this will kill you, this won’t. You know I’ve got to focus on these first and all you wanna talk about is your pain medicine and so we’ve got to get away from that and I’ve got to talk about your other issues first… . It’s difficult. |
| … [W]hen I get somebody … what they expect is a narcotic. They, they expect that and you know I’m in a business and if I don’t give it to ‘em, I know I’m gonna lose ‘em as … a client… . that is a point for a lot of people, uh so a lot of people just write you know they think uh you know tramadol’s not that bad or 5 milligrams hydrocodone just to appease the patient because they know that’s what they want. | |
| … [I]n our location it’s a challenge [with prescription drug monitoring programs] because we’ve got three other states… . and you know we can do Virginia on the same website you know which is helpful as the Tennessee but you have to have a separate log in for North Carolina and I just not even bother with it anymore. It’s just you, you have less and less time to do more and more administrative work … and less patient care. | |
| … [T]hose are always the difficult decisions um because you know my compassion doesn’t allow me to just say well ‘I can’t ever give [pain medication] to you.’ But then on the other hand it’s very um, very, very difficult to do that in a way that doesn’t put them right back into uh an addiction. | |
| Prescriber-patient relationship | … [Y]ou can have a totally different approach and level of giving, uh, with certain patients versus other patients. Like you might just cut yourself off ‘okay, I’ve given you two tries, I’m moving on to the third, forget it, I’m out of here.’ Whereas, a patient that’s very important to you, you have a great relationship, you know, I’m going to try number four, to number five and then pushes to number six. ‘I know, you have to be hearing me. I know you are.’ You know, sometimes you just really go that far with a patient that you have such a relationship with. |
| … I’ve seen providers feel like they’re powerless over the patient… . And they feel like that the patient is more in charge than they are. And that they have no control [in a situation involving drug seeking behavior] … And it’s like well no, you do have control… . And you don’t have to [prescribe]. You can say to the patient, ‘No, I’m not comfortable with this.’ | |
| As far as prescription pain meds … when I first moved here especially, the most frequent visit I would get would be back pain. People who wanted umm treatment for back pain, which has slowed down now a little bit. I think just because I have been here a little bit longer. I think at first people try new providers to see if they get pain medications from them. | |
| Prescriber-patient relationship | … I’ve got patients that have been to those pain clinics … and the pain clinics want to put ‘em, escalate their [pain medication] and the patients don’t want to escalate it and then they get fired from the pain clinic and then they come back to me sayin’ you know ‘I’m perfectly fine takin’ 5 milligrams 3 times a day but I didn’t want to get put on morphine or whatever and they fired me.’ You know then it puts the burden back on me. |
| Prescriber and patient resources | We have care managers here, people who are experienced, know who to look for, know the resources in the community, have context of those, I think those people are helpful to connect people who are here and want help [for prescription drug abuse] to help, um yeah. |
| … [W]hat I have envisioned would be great is if we had um, a psychologist on board with us who could help us, um, first of all make sure um that we pick the right people for chronic narcotics uh, you know have a profile, know whether this person is um, has an addictive personality, or um, and then also help with pain management um just uh you know techniques. | |
| … [Our] patients that are ummm uninsured, limited access… . specialists won’t see them because they are uninsured. And they won’t, they won’t see our patients like this. The, even the pain clinics will tell them they want two hundred and fifty dollars, up front, and they don’t have that kind of resources and that kind of money. | |
| I say, ‘I know you got a toothache right here and I know it’s hurting right now and I’m gonna take it out.’ And I’ve even taken them out for free because generally most addicts are usually, they’re like lower income, they don’t have any money and I said, ‘I’m going to take it out at no charge to you.’ | |
| Environmental pressures and policies on controlled prescription drugs | Oh, I think Joint Commission, the sixth uh vital sign … all of that just pushed [to treat pain] … I can’t tell you how many people we had, once that notice was up front from Joint Commission that you had to post saying … ‘We’ll treat your pain.’ You know, just out of the wood work. Come in say, ‘Oh yeah, doc I come because I have so much pain.’ And it’s like, okay. I’ve been doing this and for how long and I don’t remember that every patient, or every other patient I see, is ‘Oh doc, I’m here because I’m having pain.’ … And all of a sudden you were having this. |
| Prescriber: Well a lot of [patients] come to us, especially nowadays saying ‘My doctor won’t write pain meds for me anymore.’ Pretty much every patient is saying that nowadays. Researcher: So why won’t their doctor write them pain medicine anymore? Prescriber: Because they know about the pain medicine abuse epidemic in this region. And they think that the feds are gonna be knockin’ on their doors any moment. And they are just in quote getting out of the pain medicine business. | |
| So we don’t refill narcotics now without a visit you know as a policy… . If you need a narcotic you have to come in. There may be individual doctors that on certain occasions will write one and leave it up front or something else, but you know as a policy we say we don’t. |
Patient data and behavior
Most prescribers identified patient data as a significant factor, including data from direct and self-reported measures. They indicated data may not only influence and, at times, initiate patient communication and care related to PDA and addiction, but also influence CPD prescribing. Many prescribers described “red flags” considered indicative of PDA, addiction, or related problems. Among these were: “failed” urine drug screens and pill counts; PDMP query results; patient inquiries into and requests for CPD prescriptions; and patient self-reported drug abuse, addiction, and unintentional diversion (e.g., “medications being stolen”). In addition to the influence of data, multiple prescribers reported the collection of data through patient monitoring, especially patients on CPDs. Terms such as “monitor” and “police” were used.
Concerning patient behavior, many prescribers described the role of possible deception among patients. They indicated patients can not only be “deceiving” and “pretending and hiding” drug abuse, but will also “manipulate” and “try to trick” prescribers for CPD prescriptions. Some prescribers suggested connections between deceptive patient behaviors and challenges in pain evaluation and treatment, including an inability to “measure [pain] quantitatively” and having to “trust” patients are in pain. Moreover, several prescribers described deceptive patient behaviors as possible barriers to communication. For example, one prescriber expressed doubt “people are really willin’ to be honest” about drug abuse histories. Several prescribers further indicated incidents in clinical practice involving deceptive patient behaviors that could have residual effects, such as apprehension about the legitimacy of patient problems and “lower confidence” in patient communication.
Prescriber education and experiences
Most prescribers identified education and training as a factor in patient communication and care related to PDA and addiction. Multiple prescribers reported limited or inadequate education and training on addiction or pain, including in medical school and residency. A few prescribers similarly described the impact of education and training, including not “enough education,” on specific clinical practices (e.g., screening). Moreover, some prescribers described the impact of time since education or training completion. Challenges associated with “first start[ing]” and the “different mindset” of an “older practitioner” and a “newer practitioner,” for example, were noted.
Similarly, several prescribers described the influence of personal and familial experiences on patient care related to addiction and pain. A prescriber reporting personal experience with addiction, for example, suggested it prompted the attainment of addiction information and specialization in addiction medicine. Likewise, a prescriber reporting familial experience with addiction suggested it limited the strength and dosage of CPDs prescribed for pain.
Prescriber competing demands and tension
Many prescribers described competing demands—multiple “demand[s]” on their “time”—as a factor. They generally posited competing demands can limit patient communication and care related to PDA and addiction. Multiple prescribers specifically described the role of competing demands in face-to-face patient interactions, including “a ton of other things to talk about” and contrasting priority health issues or treatment goals/preferences between prescribers and patients. Treatment goals/preferences were conveyed as particularly impactful. Multiple prescribers indicated patients “expect” and “want pain medications” and may resist “taking them away.” They suggested not fulfilling or aligning with patient treatment preferences/goals (e.g., refusing to prescribe CPDs, prescribing CPDs at dosages that do not satisfy perceived needs, or discussing drug abuse histories) could contribute to the realization of negative or unwanted outcome expectations (e.g., monetary repercussions). Although less common, several prescribers reported competing demands outside of patient interactions, including administrative and other “time consuming” tasks.
Relatedly, many prescribers reported experiencing tension related to CPD prescribing, primarily “narcotics.” They described difficulties and “internal battle[s]” inherent in deciding to prescribe CPDs and feelings of discomfort and concern for patients on CPDs, especially “higher doses.” Further, some prescribers mentioned tension related to the realization of negative outcome expectations by prescribing CPDs, including patient addiction and overdose.
Prescriber-patient relationship
Many prescribers described characteristics of the prescriber-patient relationship as a factor. First, some prescribers indicated the influence of the relationship quality and “dynamic” on patient communication and care related to PDA and addiction. Multiple relationship elements were mentioned, including knowledge, trust, and the balance of power between prescribers and patients. Second, some prescribers mentioned the relationship length, especially its influence on patient communication and care related to CPDs. For example, the “initial visit” and receipt of patients formerly “under the care of other providers” were noted as conditions that may increase the likelihood of prescribing. Lastly, some prescribers described, at times with frustration, the influence of cyclic relationships with chronic pain patients, particularly on CPD prescribing. They reported referring patients to specialty care for pain management, or “pain clinics,” only for patients to “come back,” often because they were “stable,” “discharged,” or “fired.”
Prescriber and patient resources
Many prescribers identified “resources” as a factor, including prescriber and patient resources. Specific to prescriber resources, they described both available clinical resources and clinical resources that if available could facilitate patient communication and care related to PDA and pain. Risk assessment and communication tools, “ancillary staff,” and mental health professionals (e.g., “psychologist”) were among those noted. Similarly, some prescribers reported the influence of deficits in patient resources, including “money,” health insurance, and social support. They often described such deficits as barriers to patient communication and care (e.g., referring patients to specialty care). Concurrently, several prescribers reported actions taken to compensate for patient deficits and facilitate patient care (e.g., “free” services).
Environmental pressures and policies on controlled prescription drugs
Multiple prescribers described the influence of “external pressures” or “voices” as a factor. Several prescribers mentioned pressures to “treat pain,” including those from healthcare accreditation organizations and accrediting patient experience surveys. They suggested such pressures influenced CPD prescribing and amplified patient treatment seeking and expectations for pain relief. Moreover, some prescribers reported pressures informing and regulating CPD prescribing, such as clinical guidelines, state laws, and state/federal actions. Several prescribers indicated such pressures have contributed to prescribing reductions, while others indicated they could “make it harder and more stressful” and contribute to prescribers “getting out of the pain medicine business.”
Consistent with pressures, some prescribers highlighted the role of clinic policies. As one explained, “I think there’s external pressures on doctors … We in turn are applying that pressure to all of our patient populations as well.” Prescribers mentioned multiple policies, many standardizing CPD prescribing. They suggested policies influenced CPD prescribing and, at times, informed patient communication related to PDA and pain. Policies establishing processes for new prescriptions (e.g., requiring a “contract”) and prescription refills (e.g., no “early refill”) and prohibiting CPD prescribing (e.g., “strict no narcotic policy”) were among those noted.
Theme two: prescriber communication patterns with patients
Prescribers described multiple communication patterns with patients related to PDA, generating three subthemes.
Informative communication
Most prescribers reported informative communication, a pattern that provided PDA-related information, instructions, or explanations to patients. They commonly conveyed it as one-way communication in the context of prescribing CPDs for the treatment of pain and, to a lesser extent, addiction. Some prescribers reported informing patients of the abuse potential of CPDs or instructing patients on the “proper way to take” CPDs. One stated, “… I discuss the side effects and possibility of … addiction.” Another said, “… ‘[D]on’t take any other medicines or alcohol or drive or operate any machinery’ that’s what I say….” Likewise, some prescribers mentioned informing patients of treatment plan components, including stipulations for CPD prescriptions. Several specifically reported providing a “contract,” while another recalling a previous patient situation explained:
… I went through everything on that [researcher-developed instrument] practically about why we shouldn’t be going here [prescribing CPDs] … I finally just said, ‘Fine, this is what you’re getting.’ … Signed the prescription, but you know I made my goals clear, cut off clear, and that was the end of that.
Conversely, many prescribers described informative communication in the context of refusing to prescribe CPDs, especially “narcotics.” Prescribers reported multiple explanations used to justify a refusal, including patient history of addiction, clinic policies, and state laws. One said, “… I really use … the state laws now because I tell people that I’m not gonna be a pain clinic so I’m not going to be writing prescriptions.” Likewise, several prescribers mentioned clinic signs informing patients of “no narcotic” policies, with one stating, “[T]hey have signs saying they don’t prescribe.”
Counteractive communication
Many prescribers described counteractive communication, a pattern that involved “address[ing]” PDA-related “problems” with patients. Problems included PDA, addiction, and other behaviors (e.g., diversion). Prescribers frequently framed it as reactive communication in the context of problems that were suspected or verified, whether by observation or “data.” One stated:
Again it’s typically initiated by … some trigger that has led me to think that they have an issue with [PDA]. Whether that’s requesting prescriptions early a pharmacy calling me to tell me that you know they’re getting from multiple pharmacies the controlled substance database … when I do feel like there’s an issue then I certainly will address it.
Another said, “Um discussing the results of PDMP query yeah I have when I actually found something.” When addressing problems, some prescribers described two-way communication that entailed seeking information from patients. Referring to telephone calls by persons alleging a patient of PDA, one explained, “… [I] confront the patient and say, ‘Hey, you know I’m getting some phone calls. Here’s what they’re telling me. Tell me why I shouldn’t believe this.” Several prescribers, however, reported a more austere approach—dismissal. One stated, “[W]hen they do fail their drug screen and you know that they’ve brought in urine. We’re done with them.”
While more commonly described as a response, some prescribers reported counteractive communication that may preempt problems. One said, “And in fact we tell them if you go to the ER, then you’ll be kicked outta here.” Apart from clinical repercussions, several prescribers noted warning patients through oral or written communication of legal repercussions, especially for diversion. One explained, “I had to a get letter from the Sherriff and post it in every exam room saying that … you will be prosecuted if you are found selling or distributing.”
Supportive communication
Some prescribers reported supportive communication, a pattern that supplied various types of social support (e.g., informational and instrumental) to patients. It was commonly described in the context of concerns and treatment needs related to PDA, addiction, and pain, including those expressed by patients. One prescriber said:
And I get patients that say, ‘I’m addicted.’ And I will say, ‘Why do you say you’re addicted?’ And they will say, ‘Well ‘cause I missed a dose and god I felt terrible. … I took a dose and then I was okay.’ And I have to explain to them that’s dependence. … And they feel better about themselves.
Another stated:
… [W]hat I tell a patient, ‘if you’ve been doing great and … your brother-in-law … had this Roxicet®, and you took it … for me personally, that’s not a relapse … that’s a bad damn decision’… if I immediately go, ‘you’ve relapsed.’ It’s going to be like … ‘what’s the use, I’m back to square one.’ I go look, ‘you’re not under a bridge with a needle in your arm.’ … That was a bad decision… . So, let’s learn from those.’ …
Several prescribers reported supportive communication specific to facilitating treatment seeking or receipt, including specialty care for chronic pain and addiction. One explained:
… I’ll say, ‘look, man … you might have … some drug issues … But if I can help you, I’m on your team and I want to help you. So what I’m going to do is I’m going to tell you where to go to a Suboxone® clinic where they have counselors.’ … and I give them one of these pamphlets … where the AA and the NA meetings are in [city].
DISCUSSION
This qualitative analysis examined provider-patient communication about PDA from the prescriber perspective. Prescribers reported different communication patterns with patients and multi-level factors that affect communication with and care of patients. By advancing knowledge of these patterns and factors, the findings can inform prescriber-targeted interventions to improve provider-patient communication about PDA.
Three communication patterns with patients were identified. First, prescribers reported informative communication, characterized by giving PDA-related information, instructions, or explanations to patients. Though most reported at least one form of informative communication, prescribers generally did not report communication behaviors to verify patient understanding. Patient understanding could be associated with patient recall.35, 36 Given such an association, the findings align with prior research that suggests patient recall of verbal counseling from providers when receiving a new prescription for an opioid-acetaminophen drug, including topics pertinent to averting harm, is often limited.37 Information verifying behaviors, however, could be “critical to many aspects of clinical care.”38 Patient understanding could likewise be a prerequisite for patients to take steps and make decisions concerning their health.39 Taken together, the findings point to a potentially significant, yet modifiable gap in provider-patient communication about PDA. Prescriber use of effective methods (e.g., teach-back40–42) to verify patient understanding in the context of PDA-related communication, for example, could be beneficial.
Second, prescribers reported counteractive communication, characterized by addressing PDA and related problems with patients. Although a common purpose, they described different approaches. One dimension on which the approaches differed was the extent to which they were patient-centered. According to the Institute of Medicine, patient-centered care is characterized by “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.”43 It involves patients in care and individualizes care to patients.44, 45 Communication is important in patient-centered care43, 44, 46; patient-centered communication is likewise recognized as a “central component of high-quality health care.”47 Prescribers described some approaches that aligned more closely with patient-centered communication and care (e.g., seeking information from patients), while others aligned far less (e.g., patient dismissal). By extension, the approaches underscore opportunities—often missed—for PDA identification and treatment. Given the current unmet need for substance use treatment5, 48 and drug overdose epidemic in the nation,7 the potential for even one missed opportunity to address PDA, and substance abuse in general, is concerning.
Lastly, prescribers reported supportive communication, characterized by supplying social support to patients. Despite its potential positive implications, supportive communication was less commonly reported than informative and counteractive communication. The distribution suggests prescriber communication behaviors related to PDA could have a stronger tendency to be characterized by a more prescriber-directed, biomedical style relative to a more patient-centered, psychosocial style. Although this finding aligns with prior research on communication patterns in the primary care setting,49 it remains noteworthy. Patient-centered care, for example, has become of interest to multiple stakeholders (e.g., healthcare organizations).45–47 Evidence suggests it could contribute to positive patient outcomes44, 45, 50 and that patients frequently prefer a patient-centered communication style.51, 52 Patient preferences in communication, though, have been posited as a potential intermediary between physician style and patient outcomes.51 Future research could therefore explore the degree of concordance between provider styles and patient preferences specific to PDA communication.
Similar to communication patterns, previous qualitative research identified approaches for PDA communication with patients among prescribers and pharmacists.12 Along with approaches describing behavioral engagement in PDA communication, an approach describing non-engagement was identified—“communication avoidance.”12 Though not distinct patterns, findings within informative and counteractive communication are consistent with avoidance of and withdrawal from communication.27 Posting clinic signs and providing patient contracts, for example, could indicate avoidance of communication. Written communication could thus be a means of avoiding oral communication related to PDA with patients. Alternatively, patient dismissal and refusal to prescribe patients CPDs, for example, could reflect partial withdrawal from communication.27 In other words, prescribers could be only communicating as much as needed to minimize further interactions with patients.27 Avoidance of and withdrawal from communication denote a decrease in willingness to communicate; communication apprehension and self-perceived communication competence are antecedents of willingness to communicate.27 Such relationships suggest the findings are consistent with previous qualitative research12 and the communication theory research27 that partially guided interviews.
Prescribers identified an array of factors that affect provider-patient communication and, by association, delivery of patient care related to PDA. Multiple factors paralleled, at least in part, the “influencers” of PDA communication and prescribing/dispensing behaviors found in prior qualitative research.12 For example, the factor patient data is similar to the influencer “subjective vs. objective patient information,” prescriber education to “level of [healthcare professional] training and experience,” and prescriber-patient relationship to “patient relationships.”12 The parallels underscore provider-patient communication about PDA is a dynamic process and provide a solid basis from which future research can draw to better quantify its contributing factors. When considered as a whole, a commonality across the factors was the intersection of PDA with pain evaluation and treatment. Though notable, this is not surprising. Opioid prescribing and sales, particularly for chronic non-cancer pain, increased substantially in recent decades, concomitant with opioid-related harms.53–56 Prescribers could be a direct, or indirect, source of prescription opioids for misuse.57, 58 Individuals often report physical pain relief as a reason for misuse,59 and a notable proportion of patients prescribed opioids for chronic pain have been estimated to misuse them.60, 61 The connection between aspects of pain care (e.g., lack of an objective measure) and prescriber difficulty, discomfort, and even frustration at times in PDA-related patient interactions emphasized the intersection of the two conditions. The CDC Guideline for Prescribing Opioids for Chronic Pain likewise describes chronic pain prevention, assessment, and treatment as “challenges.”62 Moreover, “improv[ing] communication between clinicians and patients about the risks and benefits of opioid therapy for chronic pain” is among the intended purposes of the guideline.62 In short, the findings substantiate both the need for the guideline and its potential utility in PDA-related patient interactions.
Interestingly, the factors identified by prescribers represent personal and environmental factors, illustrating the perceived role of factors at different levels of influence. Education, experiences, and tension, for example, represent personal factors. Conversely, prescriber-patient relationship, prescriber and patient resources, and pressures and policies on CPDs, for example, represent social and physical environmental factors. Multi-level influence is consistent with Social Cognitive Theory (SCT),26 a theory that partially guided interviews. Specifically, it is consistent with reciprocal triadic causation, describing the interplay between behavior, personal factors, and environmental factors.63, 64 Additional findings within the factors identified align with SCT constructs. For example, low self-efficacy, or “confidence,” in patient communication was connected to insufficient education and experiences with patient deception, whereas negative or unwanted outcome expectations were connected to competing demands and tension. While these findings may not substantiate SCT in totality (i.e., all constructs), they provide support for its utility in understanding prescriber PDA communication behaviors and a theory-based direction for future research.
Evidence suggests interventions could improve physician communication behaviors during patient interactions.38 The findings of this qualitative analysis could inform prescriber-targeted interventions specific to PDA communication. Patient-centered communication can be conceptualized as a trait (i.e., “overall style of practice”) and a state (i.e., “behaviors during a particular interaction”).47 Hence, interventions aimed at increasing state-like patient-centered communication behaviors during PDA-related patient interactions could be beneficial. A focus on patient-centered communication behaviors is supported by both the growing interest in patient-centered care and its relevance to PDA and the findings. For example, patient-centered communication aims to “build trust and understanding between physicians and patients,”46 a relevant characteristic considering the prescriber-patient relationship was found to be an influential factor. Patients could also be more inclined to discuss sensitive information, such as PDA, with providers they trust,65 potentially facilitating PDA identification and treatment. Similarly, patient-centered communication could enhance chronic disease self-management,46 a relevant characteristic considering addiction is a chronic disease.66 Although further research is needed, the examples illustrate the possible benefits of state-like patient-centered communication behaviors in PDA-related patient interactions.
Limitations
Prescribers were recruited from one region and represented multiple professions and medical fields. The findings may not represent the diversity of prescriber perspectives in general, or prescriber perspectives in a specific profession or field. Given the biases associated with self-reported data and that providers could overestimate competence in patient communication,15 some prescribers could have described communication with patients as more frequent or positive than that which transpires. Despite the potential role of nonverbal communication in provider-patient communication, only verbal communication was examined. Future research can address these limitations and use the findings to inform quantitative, theory-based research on provider-patient communication about PDA.
Conclusions
Provider-patient communication about PDA underpins many initiatives aimed at curbing the PDA-related public health burden. A comprehensive understanding of this interactive process is important for optimizing these initiatives. The findings of this qualitative analysis suggest it is multidimensional and dynamic, characterized by multiple communication patterns and factors at different levels of influence. They support the application of SCT as a theoretical foundation for understanding prescriber PDA communication behaviors. Further, they suggest enhancing prescriber state-like patient-centered communication behaviors during PDA-related patient interactions could be beneficial.
Acknowledgements:
The authors extend appreciation to the prescribers for their participation in the study. The authors also thank the study staff, graduate students, and other key collaborators for their support and assistance with the study.
Funding: This study was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number R24DA036409. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding agency had no role in the design of the study; the collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
REFERENCES
- 1.Office of National Drug Control Policy. Epidemic: Responding to America’s Prescription Drug Abuse Crisis. Washington, DC: Executive Office of the President of the United States; 2011. [Google Scholar]
- 2.McHugh RK, Nielsen S and Weiss RD. Prescription drug abuse: from epidemiology to public policy. J Subst Abuse Treat. 2015;48(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brady KT, McCauley JL and Back SE. Prescription opioid misuse, abuse, and treatment in the United States: an update. Am J Psychiatry. 2016;173(1):18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration. Prescription drug misuse and abuse [Webpage]. Available at: http://www.samhsa.gov/prescription-drug-misuse-abuse Accessed May 12, 2017.
- 5.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health HHS Publication No. SMA 17-5044, NSDUH Series H-52. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. [Google Scholar]
- 6.Lipari R and Van Horn S. Trends in substance use disorders among adults aged 18 or older The CBHSQ Report. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. [PubMed] [Google Scholar]
- 7.Seth P, Scholl L, Rudd RA and Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants - United States, 2015-2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Prescription opioid data [Webpage]. Available at: https://www.cdc.gov/drugoverdose/data/prescribing.html Accessed March 25, 2019.
- 9.U.S. Department of Health and Human Services. Addressing Prescription Drug Abuse in the United States: Current Activities and Future Opportunities. Washington, DC: Behavioral Health Coordinating Committee, Prescription Drug Abuse Subcommittee, U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 10.Association of State and Territorial Health Officials. ASTHO 2014 Policy Inventory: State Action to Prevent and Treat Prescription Drug Abuse. Arlington, VA: Association of State and Territorial Health Officials; 2015. [Google Scholar]
- 11.Alexander C, Frattaroli S and Gielen A. The Prescription Opioid Epidemic: An Evidence-Based Approach. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 2015. [Google Scholar]
- 12.Hagemeier NE, Tudiver F, Brewster S, Hagy EJ, Hagaman A and Pack RP. Prescription drug abuse communication: a qualitative analysis of prescriber and pharmacist perceptions and behaviors. Res Social Adm Pharm. 2016;12(6):937–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Travaline JM, Ruchinskas R and D’Alonzo GE Jr. Patient-physician communication: why and how. J Am Osteopath Assoc. 2005;105(1):13–18. [PubMed] [Google Scholar]
- 14.Ong LM, de Haes JC, Hoos AM and Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995;40(7):903–918. [DOI] [PubMed] [Google Scholar]
- 15.Ha JF and Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38–43. [PMC free article] [PubMed] [Google Scholar]
- 16.King A and Hoppe RB. “Best practice” for patient-centered communication: a narrative review. J Grad Med Educ. 2013;5(3):385–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stewart M Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart M, Brown JB, Boon H, Galajda J, Meredith L and Sangster M. Evidence on patient-doctor communication. Cancer Prev Control. 1999;3(1):25–30. [PubMed] [Google Scholar]
- 19.Beck RS, Daughtridge R and Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15(1):25–38. [PubMed] [Google Scholar]
- 20.Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303(6814):1385–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright RE, Reed N, Carnes N and Kooreman HE. Concern about the expanding prescription drug epidemic: a survey of licensed prescribers and dispensers. Pain Physician. 2016;19(1):E197–208. [PubMed] [Google Scholar]
- 22.The National Center on Addiction and Substance Abuse at Columbia University. Under the Counter: The Diversion and Abuse of Controlled Prescription Drugs in the U.S New York, NY: The National Center on Addiction and Substance Abuse at Columbia University; 2005. [Google Scholar]
- 23.Kennedy-Hendricks A, Busch SH, McGinty EE, et al. Primary care physicians’ perspectives on the prescription opioid epidemic. Drug Alcohol Depend. 2016;165:61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Institute on Drug Abuse. Misuse of prescription drugs: how can prescription drug misuse be prevented? [Webpage]. Available at: https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/how-can-prescription-drug-misuse-be-prevented Accessed March 25, 2019.
- 25.Hagemeier NE, Gray JA and Pack RP. Prescription drug abuse: a comparison of prescriber and pharmacist perspectives. Subst Use Misuse. 2013;48(9):761–768. [DOI] [PubMed] [Google Scholar]
- 26.Bandura A Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 27.McCroskey JC. Willingness to communicate, communication apprehension, and self-perceived communication competence: conceptualizations and perspectives In: Daly JA, McCroskey JC, Ayres J, Hopf T and Ayres DM eds. Avoiding Communication: Shyness, Reticence, and Communication Apprehension. 2nd ed. Cresskill, NJ: Hampton Press, Inc; 1997:75–108. [Google Scholar]
- 28.McCroskey JC. Validity of the PRCA as an index of oral communication apprehension. Commun Monogr. 1978;45:192–203. [Google Scholar]
- 29.McCroskey JC and McCroskey LL. Self-report as an approach to measuring communication competence. Comm Res Rep. 1988;5(2):108–113. [Google Scholar]
- 30.McCroskey JC. Reliability and validity of the willingness to communicate scale. Commun Q. 1992;40(1):16–25. [Google Scholar]
- 31.NVivo Qualitative Data Analysis Software [computer program]. Version 10. QSR International Pty Ltd; 2014. [Google Scholar]
- 32.Braun V and Clarke V. Using thematic analysis in pyschology. Qual Res in Psychol. 2006;3(2):77–101. [Google Scholar]
- 33.Braun V and Clarke V. Thematic analysis In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D and Sher KJ eds. APA Handbook of Research Methods in Psychology. Vol 2: Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological Washington, DC: American Psychological Association; 2012:57–71. [Google Scholar]
- 34.Joffe H Thematic analysis In: Harper D and Thompson AR eds. Qualitative Research Methods in Mental Health and Psychotherapy: A Guide for Students and Practicioners. 1st ed. Chichester: John Wiley & Sons, Ltd; 2012:209–223. [Google Scholar]
- 35.Kessels RPC. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ley P Improving patients’ understanding, recall, satisfaction and compliance In: Broome A ed. Health Psychology: Processes and Applications. Boston, MA: Springer; 1989:74–102. [Google Scholar]
- 37.McCarthy DM, Cameron KA, King JP, et al. Patient recall of health care provider counseling for opioid-acetaminophen prescriptions. Pain Med. 2014;15(10):1750–1756. [DOI] [PubMed] [Google Scholar]
- 38.Rao JK, Anderson LA, Inui TS and Frankel RM. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care. 2007;45(4):340–349. [DOI] [PubMed] [Google Scholar]
- 39.Graham S and Brookey J. Do patients understand? The Permanente journal. 2008;12(3):67–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klingbeil C and Gibson C. The teach back project: a system-wide evidence based practice implementation. J Pediatr Nurs. 2018;42:81–85. [DOI] [PubMed] [Google Scholar]
- 41.National Quality Forum. Chapter 3: improving patient safety through informed consent, life-sustaining treatment, disclosure, and care of the caregiver Safe Practices for Better Healthcare-2010 Update: A Consensus Report. Washington, DC: National Quality Forum; 2010:117–150. [Google Scholar]
- 42.Brega AG, Barnard J, Mabachi NM, et al. Tool 5: use the teach-back method AHRQ Health Literacy Universal Precautions Toolkit. 2nd ed. (Prepared by Colorado Health Outcomes Program, University of Colorado Anschutz Medical Campus under Contract No. HHSA290200710008, TO#10.) AHRQ Publication No. 15-0023-EF Rockville, MD: Agency for Healthcare Research and Quality; 2015:18–20. [Google Scholar]
- 43.Institute of Medicine. Improving the 21st-century health care system Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001:39–60. [PubMed] [Google Scholar]
- 44.Reynolds A Patient-centered care. Radiol Technol. 2009;81(2):133–147. [PubMed] [Google Scholar]
- 45.Robinson JH, Callister LC, Berry JA and Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600–607. [DOI] [PubMed] [Google Scholar]
- 46.Levinson W, Lesser CS and Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood). 2010;29(7):1310–1318. [DOI] [PubMed] [Google Scholar]
- 47.Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005;61(7):1516–1528. [DOI] [PubMed] [Google Scholar]
- 48.Lipari RN, Park-Lee E and Van Horn S. America’s Need for and Receipt of Substance Use Treatment in 2015. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2016. [PubMed] [Google Scholar]
- 49.Roter DL, Stewart M, Putnam SM, Lipkin M Jr., Stiles W and Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277(4):350–356. [PubMed] [Google Scholar]
- 50.Rathert C, Wyrwich MD and Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2012;70(4):351–379. [DOI] [PubMed] [Google Scholar]
- 51.Swenson SL, Buell S, Zettler P, White M, Ruston DC and Lo B. Patient-centered communication: do patients really prefer it? J Gen Intern Med. 2004;19(11):1069–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Swenson SL, Zettler P and Lo B. ‘She gave it her best shot right away’: patient experiences of biomedical and patient-centered communication. Patient Educ Couns. 2006;61(2):200–211. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers--United States, 1999--2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 54.Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–574. [DOI] [PubMed] [Google Scholar]
- 55.Manchikanti L, Helm S, Fellows B, et al. Opioid epidemic in the United States. Pain Physician. 2012;15(3 Suppl):Es9–38. [PubMed] [Google Scholar]
- 56.Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017;20(2s):S93–s109. [PubMed] [Google Scholar]
- 57.Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017. [Google Scholar]
- 58.Lipari RN and Hughes A. How People Obtain the Prescription Pain Relievers They Misuse The CBHSQ Report. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. [PubMed] [Google Scholar]
- 59.Lipari RN, Williams M and Van Horn SL. Why Do Adults Misuse Prescription Drugs? Rockville, MD: The CBHSQ Report. Substance Abuse and Mental Health Services Administration; 2013. [PubMed] [Google Scholar]
- 60.Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP and van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4). [DOI] [PubMed] [Google Scholar]
- 61.National Institute on Drug Abuse. Opioid overdose crisis [Webpage]. Available at: https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis Accessed March 26, 2019.
- 62.Dowell D, Haegerich TM and Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. [DOI] [PubMed] [Google Scholar]
- 63.McAlister AL, Perry CL and Parcel GS. How individuals, environments, and health behaviors interact: social cognitive theory In: Glanz K, Rimer BK and Viswanath K eds. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008:169–188. [Google Scholar]
- 64.Crosby RA, Salazar LF and DiClemente RJ. Social cognitive theory applied to health behavior In: DiClemente RJ, Salazar LF and Crosby RA eds. Health Behavior Theory for Public Health: Principles, Foundations, and Applications. Burlington, MA: Jones & Bartlett Learning; 2013:163–185. [Google Scholar]
- 65.Thom DH, Hall MA and Pawlson LG. Measuring patients’ trust in physicians when assessing quality of care. Health Aff (Millwood). 2004;23(4):124–132. [DOI] [PubMed] [Google Scholar]
- 66.National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction. NIH Pub No. 14-5605 Rockville, MD: National Institute on Drug Abuse, National Institutes of Health, U.S. Department of Health and Human Services; 2014. [Google Scholar]


