Abstract
IMPORTANCE
Chronic kidney disease (CKD) is the 16th leading cause of years of life lost worldwide. Appropriate screening, diagnosis, and management by primary care clinicians are necessary to prevent adverse CKD-associated outcomes, including cardiovascular disease, end-stage kidney disease, and death.
OBSERVATIONS
Defined as a persistent abnormality in kidney structure or function (eg, glomerular filtration rate [GFR] <60 mL/min/1.73 m2 or albuminuria ≥30 mg per 24 hours) for more than 3 months, CKD affects 8% to 16% of the population worldwide. In developed countries, CKD is most commonly attributed to diabetes and hypertension. However, less than 5% of patients with early CKD report awareness of their disease. Among individuals diagnosed as having CKD, staging and new risk assessment tools that incorporate GFR and albuminuria can help guide treatment, monitoring, and referral strategies. Optimal management of CKD includes cardiovascular risk reduction (eg, statins and blood pressure management), treatment of albuminuria (eg, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers), avoidance of potential nephrotoxins (eg, nonsteroidal anti-inflammatory drugs), and adjustments to drug dosing (eg, many antibiotics and oral hypoglycemic agents). Patients also require monitoring for complications of CKD, such as hyperkalemia, metabolic acidosis, hyperphosphatemia, vitamin D deficiency, secondary hyperparathyroidism, and anemia. Those at high risk of CKD progression (eg, estimated GFR <30 mL/min/1.73 m2, albuminuria ≥300 mg per 24 hours, or rapid decline in estimated GFR) should be promptly referred to a nephrologist.
CONCLUSIONS AND RELEVANCE
Diagnosis, staging, and appropriate referral of CKD by primary care clinicians are important in reducing the burden of CKD worldwide.
Chronic kidney disease (CKD) affects between 8% and 16% of the population worldwide and is often underrecognized by patients and clinicians.1–4 Defined by a glomerular filtration rate (GFR) of less than 60 mL/min/1.73 m2, albuminuria of at least 30 mg per 24 hours, or markers of kidney damage (eg, hematuria or structural abnormalities such as polycystic or dysplastic kidneys) persisting for more than 3 months,5 CKD is more prevalent in low- and middle-income than in high-income countries.6 Globally, CKD is most commonly attributed to diabetes and/or hypertension, but other causes such as glomerulonephritis, infection, and environmental exposures (such as air pollution, herbal remedies, and pesticides) are common in Asia, sub-Saharan Africa, and many developing countries.4 Genetic risk factors may also contribute to CKD risk. For example, sickle cell trait and the presence of 2 APOL1 risk alleles, both common in people of African ancestry but not European ancestry, may double the risk of CKD.4,7–10
In the United States, the average rate of GFR decline is approximately 1 mL/min/1.73 m2 per year in the general population,11,12 and the lifetime risk of developing a GFR of less than 60 mL/min/1.73 m2 is more than 50%.13 Early detection and treatment by primary care clinicians is important because progressive CKD is associated with adverse clinical outcomes, including end-stage kidney disease (ESKD), cardiovascular disease, and increased mortality.14–17 Recent professional guidelines suggest a risk-based approach to the evaluation and management of CKD.5,18–20 This review includes discussion of new calculators for determining risk of CKD progression that may be useful in clinical practice (eg, https://kidneyfailurerisk.com/) and focuses on the diagnosis, evaluation, and management of CKD for primary care clinicians. Considerations for referral to a nephrologist and dialysis initiation are also covered.
Methods
A literature search to April 2019 was conducted using Medline and PubMed with search terms including CKD, chronic renal failure, chronic renal insufficiency, epidemiology, incidence, prevalence, occurrence, diagnosis, assessment, identification, screening, workup,etiology,causes,management,treatment,intervention,therapy, and prevention. Results were restricted to English-language, human studies, and academic journals and guidelines. The initial search resulted in 998 articles, including clinical trials, meta-analyses, practice guidelines, and systematic reviews, and was later expanded to include review articles and observational studies, including cross-sectional studies, and more recent publications contained in reference lists of identified articles. All clinical trials for treatment or prevention of CKD were included without regard to study size or age of patient population.
Clinical Presentation
Chronic kidney disease is typically identified through routine screening with serum chemistry profile and urine studies or as an incidental finding. Less commonly, patients may present with symptoms such as gross hematuria, “foamy urine” (a sign of albuminuria), nocturia, flank pain, or decreased urine output. If CKD is advanced, patients may report fatigue, poor appetite, nausea, vomiting, metallic taste, unintentional weight loss, pruritus, changes in mental status, dyspnea, or peripheral edema.21
In evaluating a patient with known or suspected CKD, clinicians should inquire about additional symptoms that might suggest a systemic cause (eg, hemoptysis, rash, lymphadenopathy, hearing loss, neuropathy) or urinary obstruction (eg, urinary hesitancy, urgency, or frequency or incomplete bladder emptying).21 Moreover, patients should be assessed for risk factors of kidney disease, including prior exposure to potential nephrotoxins (eg, nonsteroidal anti-inflammatory drugs [NSAIDs], phosphate-based bowel preparations, herbal remedies such as those containing aristolochic acid, antibiotic therapies such as gentamicin, and chemotherapies), history of nephrolithiasis or recurrent urinary tract infections, presence of comorbidities (eg, hypertension, diabetes, autoimmune disease, chronic infections), family history of kidney disease, and, if available, other known genetic risk factors such as sickle cell trait.9,18,21–24
A detailed physical examination may provide additional clues regarding the underlying cause of CKD and should include careful evaluation of a patient’s volume status. Signs of volume depletion may reflect poor oral intake, vomiting, diarrhea, or overdiuresis, whereas signs of volume overload may be due to decompensated heart failure, liver failure, or nephrotic syndrome. The presence of arterial-venous nicking or retinopathy on retinal examination suggests long-standing hypertension or diabetes. Patients with carotid or abdominal bruits may have renovascular disease. Flank pain or enlarged kidneys should prompt consideration of obstructive uropathy, nephrolithiasis, pyelonephritis, or polycystic kidney disease. Neuropathy may be due to diabetes or less commonly vasculitis, or amyloidosis. Skin findings may include rash (systemic lupus erythematosus, acute interstitial nephritis), palpable purpura (Henoch-Schonlein purpura, cryoglobulinemia, vasculitis), telangiectasias (scleroderma, Fabry disease), or extensive sclerosis (scleroderma). Patients with advanced CKD may exhibit pallor, skin excoriations, muscle wasting, asterixis, myoclonic jerks, altered mental status, and pericardial rub.21
CKD Definition and Staging
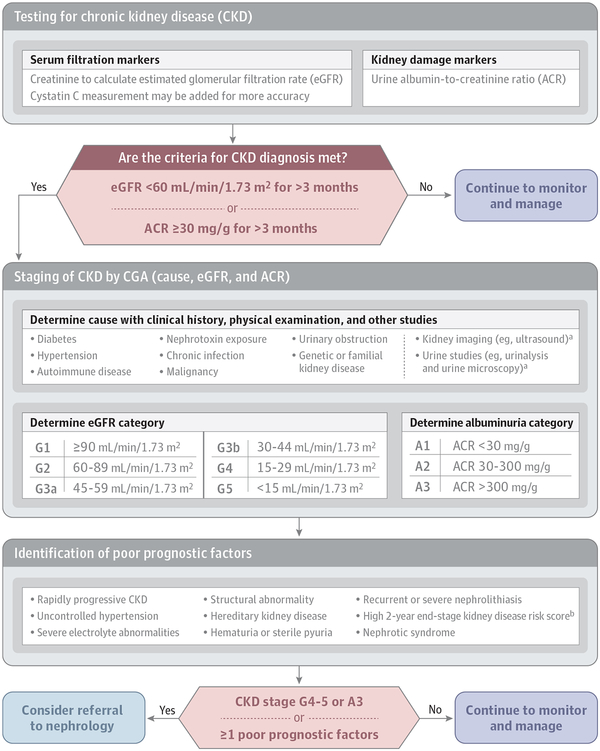
Chronic kidney disease is defined as the presence of an abnormality in kidney structure or function persisting for more than 3 months.5,25 This includes 1 or more of the following: (1) GFR less than 60 mL/min/1.73 m2; (2) albuminuria (ie, urine albumin ≥30 mg per 24 hours or urine albumin-to-creatinine ratio [ACR] ≥30 mg/g); (3) abnormalities in urine sediment, histology, or imaging suggestive of kidney damage; (4) renal tubular disorders; or (5) history of kidney transplantation.5 If the duration of kidney disease is unclear, repeat assessments should be performed to distinguish CKD from acute kidney injury (change in kidney function occurring within 2–7 days) and acute kidney disease (kidney damage or decreased kidney function present for ≤3 months).25 Evaluation for the etiology of CKD should be guided by a patient’s clinical history, physical examination, and urinary findings (Figure 1).5,18,21
Figure 1. Considerations for Diagnosis, Staging, and Referral of Patients With Chronic Kidney Disease.
a Other imaging modalities or urine studies may also be considered.
b A variety of scores are available, eg, https://kidneyfailurerisk.com/.
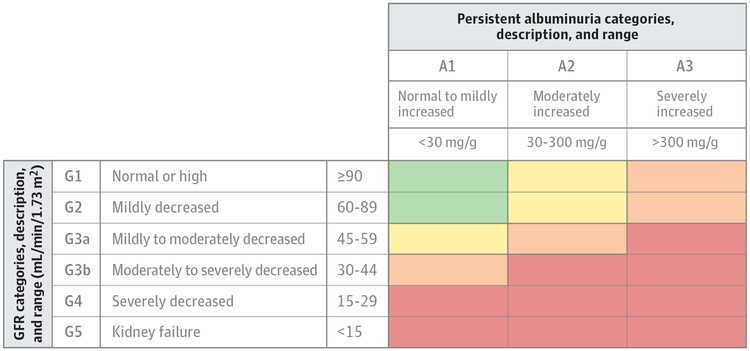
Once a diagnosis of CKD has been made, the next step is to determine staging, which is based on GFR, albuminuria, and cause of CKD (Figure 2).5 Staging of GFR is classified as G1 (GFR ≥90 mL/min/1.73 m2), G2 (GFR 60–89 mL/min/1.73 m2), G3a (45–59 mL/min/1.73 m2), G3b (30–44 mL/min/1.73 m2), G4 (15–29 mL/min/1.73 m2), and G5 (<15 mL/min/1.73 m2).5 Although GFR can be directly measured by clearance of agents such as iohexol or iothalamate,26–28 the development of estimating equations (eg, the Chronic Kidney Disease Epidemiology Collaboration [CKD-EPI] and Modification of Diet in Renal Disease Study [MDRD] equations) has largely replaced the need for direct measurement in clinical practice.29–31 Clinical laboratories now routinely report estimated GFR (eGFR) based on filtration markers. The most common filtration marker used is creatinine, a 113 dalton byproduct of creatine metabolism25 and one for which laboratory assays have been standardized since 2003.32 The preferred estimating equation in the United States and much of the world is the CKD-EPI 2009 creatinine equation, which is more accurate than the earlier MDRD equation, particularly for eGFR values greater than 60 mL/min/1.73 m2 (https://www.kidney.org/professionals/kdoqi/gfr_calculator).29,30 In situations requiring additional accuracy and precision, cystatin C can be used with creatinine in the CKD-EPI 2012 creatinine-cystatin C equation.31 Adding cystatin C may be particularly useful for individuals with altered creatinine production and/or metabolism (eg, extremely high or low body size or muscle mass, limb amputation, high-protein diet, use of creatinine supplements, or use of drugs affecting tubular secretion of creatinine).5,25
Figure 2. Definition and Prognosis of Chronic Kidney Disease by GFR and Albuminuria Categories, KDIGO 2012.
GFR indicates glomerular filtration rate; KDIGO, Kidney Disease Improving Global Outcomes. Categories are grouped by risk of progression, which includes chronic kidney disease progression, defined by a decline in GFR category (accompanied by a ≥25% decrease in estimated GFR from baseline) or sustained decline in estimated GFR greater than 5 mL/min/1.73 m2 per year. Green indicates low risk (if no other markers of kidney disease and no CKD); yellow, moderately increased risk; orange: high risk; and red, very high risk. Reproduced with permission from Kidney International Supplements.5
Albuminuria should ideally be quantified by a urine ACR. Albuminuria staging is classified as A1 (urine ACR <30 mg/g), A2 (30–300 mg/g), and A3 (>300 mg/g).5 Guidelines recommend the use of urine ACR to stage CKD rather than urine protein-to-creatinine ratio because assays for the former are more likely to be standardized and have better precision at lower values of albuminuria.5,33 The most precise measurements come from a first morning sample or 24-hour collection, as there is high biological variability in urine albumin excretion over the course of the day.5,34,35 Random samples, however, are also acceptable in initial screening.5 Compared with urine protein-to-creatinine ratio, urine ACR is believed to be a more sensitive and specific marker of glomerular pathology5 since some urine proteins such as uromodulin are present (and may even be protective) in normal physiology.36–38 If tubular or overflow proteinuria is suspected, then urine protein electrophoresis or testing for the specific protein can be pursued (eg, immunoglobulin heavy and light chains, α1-microglobulin, and β2-microglobulin).5 Imaging by kidney ultrasound to assess morphology and to rule out urinary obstruction should be considered in all patients diagnosed as having CKD.5
Cause of CKD can be difficult to discern but is generally classified by the presence or absence of systemic disease and the location of anatomic abnormality. Examples of systemic disease include diabetes, autoimmune disorders, chronic infection, malignancy, and genetic disorders in which the kidney is not the only organ affected. Anatomic locations are divided into glomerular, tubulointerstitial, vascular, and cystic/congenital diseases.5 Determining the cause of CKD may have important implications on prognosis and treatment. For example, polycystic kidney disease may progress to ESKD faster than other causes and often requires evaluation for extrarenal manifestations and consideration of specific therapies such as tolvaptan, a vasopressin V2 receptor antagonist that slows decline in GFR.39,40 Patients with unexplained causes of CKD should be referred to a nephrologist.
Screening for CKD
Given that most patients with CKD are asymptomatic, screening may be important to early detection of disease.18 The National Kidney Foundation has developed a kidney profile test that includes measuring both serum creatinine for estimating GFR and urine ACR.41 A risk-based approach to screening is suggested by many clinical practice guidelines, with screening recommended in those older than 60 years or with a history of diabetes or hypertension.18–20 Screening should also be considered in those with clinical risk factors, including autoimmune disease, obesity, kidney stones, recurrent urinary tract infections, reduced kidney mass, exposure to certain medications such as NSAIDs or lithium, and prior episodes of acute kidney injury, among others (Box).9,18,42–45 However, no randomized clinical trials have demonstrated that screening asymptomatic patients for CKD improves outcomes.
Box. Clinical, Sociodemographic, and Genetic Risk Factors for Chronic Kidney Disease.
Clinical
Diabetes
Hypertension
Autoimmune diseases
Systemic infections (eg, HIV, hepatitis B virus, hepatitis C virus)
Nephrotoxic medications (eg, nonsteroidal anti-inflammatory drugs, herbal remedies, lithium)
Recurrent urinary tract infections
Kidney stones
Urinary tract obstruction
Malignancy
Obesity
Reduced kidney mass (eg, nephrectomy, low birth weight)
History of acute kidney injury
Smoking
Intravenous drug use (eg, heroin, cocaine)
Family history of kidney disease
Sociodemographic
Age >60 years
Nonwhite race
Low income
Low education
Genetic
APOL1 risk alleles
Sickle cell trait and disease
Polycystic kidney disease
Alport syndrome
Congenital anomalies of the kidney and urinary tract
Other familial causes
Other Risk Factors for CKD
There are several sociodemographic factors that contribute to increased risk of CKD, including nonwhite race, low education, low income, and food insecurity.18,43,46 Compared with whites, African Americans and Pacific Islanders have a substantially greater risk of ESKD.47 This is in part due to an increased prevalence of hypertension, diabetes, and obesity.11 However, genetic factors likely also contribute. More specifically, risk alleles in the gene encoding apolipoprotein L1 (APOL1) may increase risk of kidney disease in a recessive genetic manner7,8: individuals with 2 APOL1 risk alleles (present in approximately 13% of African Americans) have a 2-fold risk of CKD progression and up to a 29-fold risk of specific CKD etiologies (eg, focal-segmental glomerulosclerosis and HIV-associated nephropathy) compared with those with 0 or 1 risk allele.11,44,45,48,49 Sickle cell trait (present in approximately 8% of African Americans) has also been associated with an increased risk of kidney disease. Compared with noncarriers, individuals with sickle cell trait have a 1.8-fold odds of incident CKD, 1.3-fold odds of eGFR decline greater than 3 mL/min/1.73 m2, and 1.9-fold odds of albuminuria.9
Management of Patients With CKD
Reducing Risk of Cardiovascular Disease
The prevalence of cardiovascular disease is markedly higher among individuals with CKD compared with those without CKD. For example, in a Medicare 5% sample, 65% of the 175 840 adults aged 66 years or older with CKD had cardiovascular disease compared with 32% of the 1 086 232 without CKD.47 Moreover, presence of CKD is associated with worse cardiovascular outcomes. For example, in the same population, the presence of CKD was associated with lower 2-year survival in people with coronary artery disease (77% vs 87%), acute myocardial infarction (69% vs 82%), heart failure (65% vs 76%), atrial fibrillation (70% vs 83%), and cerebrovascular accident/transient ischemic attack (73% vs 83%).47
Therefore, a major component of CKD management is reduction of cardiovascular risk. It is recommended that patients aged 50 years or older with CKD be treated with a low- to moderate-dose statin regardless of low-density lipoprotein cholesterol level.50–52 Smoking cessation should also be encouraged.5,53 Both the Eighth Joint National Committee (JNC 8) and Kidney Disease: Improving Global Outcomes (KDIGO) guidelines have recommended goal systolic and diastolic blood pressures of less than 140 mm Hg and less than 90 mm Hg, respectively, among adults with CKD based on expert opinion.5,54 The KDIGO guidelines further recommend that adults with urine ACR of at least 30 mg per 24 hours (or equivalent) have systolic and diastolic blood pressures maintained below 130 mm Hg and 80 mm Hg, respectively.5 More recently, the Systolic Blood Pressure Intervention Trial (SPRINT) demonstrated that among individuals with increased risk of cardiovascular disease but without diabetes, more intensive blood pressure control (goal systolic blood pressure <120 mm Hg) was associated with a 25% lower (1.65% vs 2.19% per year) risk of a major cardiovascular event and a 27% lower risk of all-cause mortality compared with standard blood pressure control (goal systolic blood pressure <140 mm Hg).55 The intensive treatment group had a greater risk of at least a 30% decline in eGFR to a level below 60 mL/min/1.73 m2; however, this may have been due to hemodynamic changes rather than true kidney function loss.55,56 Importantly, the benefits of intensive blood pressure control on cardiovascular events were similar in participants with and without baseline CKD.57
Management of Hypertension
Many guidelines provide algorithms detailing which agents should be used to treat hypertension in people with CKD.54,58 Presence and severity of albuminuria should be evaluated. Blockade of the renin-angiotensin-aldosterone system with either an angiotensin-converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB) is recommended for adults with diabetes and a urine ACR of at least 30 mg per 24 hours or any adult with a urine ACR of at least 300 mg per 24 hours.5,18,58 Dual therapy with an ACE-I and an ARB is generally avoided, given associated risks of hyperkalemia and acute kidney injury.5,18,59 Aldosterone receptor antagonists may also be considered in patients with albuminuria, resistant hypertension, or heart failure with reduced ejection fraction.58,60–64
Management of Diabetes Mellitus
Optimal management of diabetes is also important. First, glycemic control may delay progression of CKD, with most guidelines recommending a goal hemoglobin A1c of ~ 7.0%.5,18,19,65–67 Second, dose adjustments in oral hypoglycemic agents may be necessary. In general, drugs that are largely cleared by the kidneys (eg, glyburide) should be avoided, whereas drugs metabolized by the liver and/or partially excreted by the kidneys (eg, metformin and some dipeptidyl peptidase 4 [DPP-4] and sodium-glucose cotransporter-2 [SGLT-2] inhibitors) may require dose reduction or discontinuation, particularly when eGFR falls below 30 mL/min/1.73 m2.18,19 Third, use of specific medication classes such as SGLT-2 inhibitors in those with severely increased albuminuria should be considered. The Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial demonstrated that, among 4401 patients with type 2 diabetes and CKD stage G2-G3/A3 (baseline eGFR 30 to <90 mL/min/1.73 m2 and urine ACR>300 to 5000 mg/24 hours) taking ACE-I or ARB therapy, those randomized to canagliflozin had a 30% lower risk (43.2 vs 61.2 events per 1000 patient-years) of developing the primary composite renal outcome (doubling of serum creatinine, ESKD, or death from a renal or cardiovascular cause) compared with those randomized to placebo.68 Prior trials have also suggested cardiovascular benefit with this class of medications, which may extend to patients with CKD who have lower levels of albuminuria.69,70
Nephrotoxins
All patients with CKD should be counseled to avoid nephrotoxins. Although a complete list is beyond the scope of this review, a few warrant mentioning. Routine administration of NSAIDs in CKD is not recommended, especially among individuals who are taking ACE-I or ARB therapy.5,18 Herbal remedies are not regulated by the US Food and Drug Administration, and some (such as those containing aristolochic acid or anthraquinones) have been reported to cause a myriad of kidney abnormalities, including acute tubular necrosis, acute or chronic interstitial nephritis, nephrolithiasis, rhabdomyolysis, hypokalemia, and Fanconi syndrome.22 Phosphate-based bowel preparations (both oral and enema formulations) are readily available over the counter and can lead to acute phosphate nephropathy.23,24 Proton pump inhibitors are widely used and have been associated with acute interstitial nephritis in case reports and incident CKD in population-based studies.71–73 In the population-based Atherosclerosis Risk in Communities cohort, the incidence of CKD was 14.2 events in those taking proton pump inhibitors and 10.7 per 1000 events in people who did not take them.71 Uniform discontinuation of proton pump inhibitors in CKD is not necessary. However, indications for use should be addressed at each primary care visit.
Drug Dosing
Adjustments in drug dosing are frequently required in patients with CKD. Of note, the traditional Cockcroft-Gault equation often poorly reflects measured GFR, whereas estimation of GFR using the CKD-EPI equation likely correlates better with drug clearance by the kidneys.74,75 Common medications that require dose reductions include most antibiotics, direct oral anticoagulants, gabapentin and pregabalin, oral hypoglycemic agents, insulin, chemotherapeutic agents, and opiates, among others.5,18 In general, use of medications with low likelihood of benefit should be minimized because patients with CKD are at high risk of adverse drug events.76–79 Gadolinium-based contrast agents are contraindicated in individuals with acute kidney injury, eGFR less than 30 mL/min/1.73 m2, or ESKD given the risk of nephrogenic systemic fibrosis, a painful and debilitating disorder characterized by marked fibrosis of the skin and occasionally other organs.5,18,80,81 Newer macrocyclic chelate formulations (eg, gadoteridol, gadobutrol, or gadoterate) are much less likely to cause nephrogenic systemic fibrosis, but the best prevention may still be to avoid gadolinium altogether. If administration of gadolinium is deemed essential, the patient must be counseled on the potential risk of nephrogenic systemic fibrosis and a nephrologist may be consulted for consideration of postexposure hemodialysis.5,18,80–82
Dietary Management
Dietary management to prevent CKD progression is controversial since large trials have had equivocal results.83–85 For example, the MDRD study evaluated 2 levels of protein restriction in 840 patients, finding that a low-protein diet compared with usual protein intake resulted in slower GFR decline only after the initial 4 months, and that a very low-protein diet compared with a low-protein diet was not significantly associated with slower GFR decline. Both levels of protein restriction appeared to have benefit in the subgroup with proteinuria greater than 3 g per day, although this group was small.83 Other, smaller trials have suggested a benefit of protein restriction in the prevention of CKD progression or ESKD.86–88 The KDIGO guidelines recommend that protein intake be reduced to less than 0.8 g/kg per day (with proper education) in adults with CKD stages G4-G5 and to less than 1.3 g/kg per day in other adult patients with CKD at risk of progression.5 The possible benefits of dietary protein restriction must be balanced with the concern of precipitating malnutrition and/or protein wasting syndrome.5,83,84,89 Lower dietary acid loads (eg, more fruits and vegetables and less meats, eggs, and cheeses) may also help protect against kidney injury.90,91 Low-sodium diets (generally <2 g per day) are recommended for patients with hypertension, proteinuria, or fluid overload.5
Monitoring of Established CKD and Treatment of Complications
Once CKD is established, the KDIGO guidelines recommend monitoring eGFR and albuminuria at least once annually. For patients at high risk, these measures should be monitored at least twice per year; patients at very high risk should be monitored at least 3 times per year (Figure 2).5 Patients with moderate to severe CKD are at increased risk of developing electrolyte abnormalities, mineral and bone disorders, and anemia.92 Screening and frequency of assessment for laboratory abnormalities is dictated by stage of CKD and includes measurement of complete blood count, basic metabolic panel, serum albumin, phosphate, parathyroid hormone, 25-hydroxyvitamin D, and lipid panel (Table).5,50,93,94
Table.
Screening, Monitoring, and Management of the Complications of Chronic Kidney Disease (CKD)
| Complication | Relevant Tests | Frequency of Repeat Testing | Management |
|---|---|---|---|
| Anemia | Hemoglobin | No anemia: CKD stages G1-G2: when clinically indicated CKD stage G3: at least once per year CKD stages G4-G5: at least twice per year With anemia: CKD stages 3–5: at least every 3 months |
Rule out other causes of anemia: iron deficiency, vitamin B12 deficiency, folate deficiency, occult bleeding Consider iron supplementation and referral to a nephrologist for erythropoietin-stimulating agent therapy when hemoglobin <10 g/dL |
| Mineral and bone disorder | Serum calcium, phosphate, parathyroid hormone, 25-hydroxyvitamin D | Calcium/phosphate: CKD stage G3: every 6–12 months CKD stage G4: every 3–6 months CKD stage G5: every 1–3 months Parathyroid hormone: CKD stage G3: at baseline, then as needed CKD stage G4: every 6–12 months CKD stage G5: every 3–6 months Vitamin D: CKD stages 3–5: at baseline, then as needed |
Consider phosphate-lowering therapy (eg, calcium acetate, sevelamer, iron-based binders) and vitamin D supplementation |
| Hyperkalemia | Serum potassium | At baseline and as needed | Low-potassium diet, correction of hyperglycemia and acidemia, consider potassium binders |
| Metabolic acidosis | Serum bicarbonate | At baseline and as needed | Oral bicarbonate supplementation (eg, sodium bicarbonate, baking soda, or sodium citrate/citric acid) for values persistently <22 mmol/L |
| Cardiovascular disease | Lipid panel | At baseline and as needed | Low- to moderate-dose statin therapy for patients aged ≥50 years with CKD Statin therapy for patients aged 18–49 years with CKD and coronary artery disease, diabetes, prior ischemic stroke, or high risk of myocardial infarction or cardiovascular death |
Anemia and the Role of Erythropoietin in CKD
Anemia is among the most common complications of CKD. In a study that included 19 CKD cohorts from across the world, 41% of the 209 311 individuals had low levels of hemoglobin (defined as <13 g/dL in men and <12 g/dL in women).92 The initial workup of anemia should include assessment of iron stores: those who are iron deficient may benefit from oral or intravenous iron repletion. Patients with hemoglobin levels persistently below 10 g/dL despite addressing reversible causes can be referred to a nephrologist for consideration of additional medical therapy, including erythropoietin-stimulating agents; however, erythropoietin-stimulating agents have been associated with increased risk of death, stroke, and venous thromboembolism, and these risks must be weighed against any potential benefits.93
Electrolyte, Mineral, and Bone Abnormalities in CKD
Electrolyte abnormalities are present in 3% to 11% of patients with CKD.92 Initial treatment strategies usually involve dietary restrictions and prescription of supplements. For example, primary care clinicians should recommend low-potassium diets for patients with hyperkalemia and low-phosphorus diets for patients with hyperphosphatemia.5,18,94,95 For patients with a serum bicarbonate level persistently below 22 mmol/L, oral bicarbonate supplementation should be considered, as studies have suggested that chronic metabolic acidosis is associated with faster CKD progression.5,18,96–99
Mineral and bone disorders are also common. In a study that included 42 985 patients with CKD, 58% had intact parathyroid hormone levels greater than 65 pg/mL.92 Although the optimal intact parathyroid hormone level for CKD remains unclear, most nephrologists agree that concomitant hyperphosphatemia, hypocalcemia, and vitamin D deficiency should be addressed, such as with a low-phosphate diet, phosphate binders, adequate elemental calcium intake, and vitamin D supplementation (Table).94,95
Prognosis of CKD
The incidence of ESKD varies by the presence of risk factors and geographical location. For example, in North America, the incidence among individuals with eGFR less than 60 mL/min/1.73 m2 ranged from 4.9 to 168.3 ESKD events per 1000 patient-years in 16 cohorts; in 15 non–North American cohorts, the incidence ranged from 1.2 to 131.3 ESKD events per 1000 patient-years.100 Most patients with CKD do not require kidney replacement therapy during their lifetime.101 Simple online tools are available to help with risk stratification. For example, the Kidney Failure Risk Equation (KFRE; https://kidneyfailurerisk.com/) predicts the 2-year and 5-year probabilities of requiring dialysis or transplant among individuals with eGFR less than 60 mL/min/1.73 m2.100,102 The KFRE, which has been validated in more than 700 000 individuals from more than 30 countries, uses readily available clinical and laboratory variables. The 4-variable equation includes age, sex, eGFR, and urine ACR, whereas the 8-variable equation further incorporates serum albumin, phosphate, calcium, and bicarbonate levels.100,102 Some health systems have tested the implementation of KFRE in clinical practice: nephrology referrals based on a 5-year KFRE greater than 3% led to shorter wait times,103 and a 2-year KFRE greater than 10% was used to guide referrals to multidisciplinary CKD clinics.104 An ongoing trial is evaluating whether a KFRE risk-based approach improves CKD management.105 For patients with eGFR less than 30mL/min/1.73m2, the CKD G4+ risk calculator (https://www.kdigo.org/equation/) may provide additional information on the risks of cardiovascular disease and death.106,107 Importantly, risk prognostication may be helpful in not only identifying individuals at high risk of disease progression but also providing reassurance to those with mild CKD such as stage G3a A1.
Referral to a Nephrologist and Timing of Kidney Replacement Therapy
The KDIGO guidelines recommend that patients with CKD be referred to a nephrologist when eGFR falls below 30 mL/min/1.73 m2 (stage G4) and/or urine ACR increases above 300 mg per 24 hours (stage A3).5 The presence of albuminuria greater than 2200 mg per 24 hours should prompt expedited evaluation by a nephrologist and consideration of nephrotic syndrome. Additional indications for referral include the following: presence of greater than 20 red blood cells per high-power field of unclear etiology, red blood cell casts on urine microscopy or other indication of glomerulonephritis, CKD with uncontrolled hypertension despite 4 or more antihypertensive medications, persistent hypokalemia or hyperkalemia, anemia requiring erythropoietin replacement, recurrent or extensive kidney stones, hereditary kidney disease, acute kidney injury, and rapid CKD progression (a decrease in eGFR ≥25% from baseline or a sustained decline in eGFR >5 mL/min/1.73 m2).5 In persons without CKD, even small changes in serum creatinine (eg, from 0.7 mg/dL to 1.2 mg/dL) reflect large declines in eGFR, and primary care clinicians should attempt to identify reversible causes. Indications for kidney biopsy may include but are not limited to unexplained persistent or increasing albuminuria, presence of cellular casts or dysmorphic red blood cells on urine sediment, and unexplained or rapid decline in GFR.5 Specific thresholds vary depending on patient characteristics and by institution. Patients with polycystic kidney disease, certain types of glomerulonephritis, and nephrotic-range albuminuria are at particularly high risk of progressing to ESKD.5,39,102
Referral to nephrology is important for planning kidney replacement therapy and transplant evaluation. The decision to begin kidney replacement therapy is based on the presence of symptoms and not solely on level of GFR.108 Urgent indications include encephalopathy, pericarditis, and pleuritis due to severe uremia.109 Otherwise, initiation of dialysis should be individualized and considered when patients have uremic signs or symptoms (eg, nausea, vomiting, poor appetite, metallic taste, pericardial rub or effusion, asterixis, or altered mental status), electrolyte abnormalities (eg, hyperkalemia or metabolic acidosis), or volume overload (eg, pulmonary or lower extremity edema) refractory to medical management.5,18,109 A shared decision-making approach is best. Patients should be educated about treatment options and actively contribute to decision-making. Early education should include information on the potential complications of CKD as well as the different modalities of kidney replacement therapy. Kidney transplantation is considered the optimal therapy for ESKD, with living donor kidney transplantations performed before or shortly after dialysis initiation having the best outcomes.110,111 As such, early referral (eg, eGFR <30 mL/min/1.73 m2 and an elevated 2-year risk of ESKD) for transplant evaluation is important.112,113 Alternative therapies for ESKD may include in-center hemodialysis, home hemodialysis, peritoneal dialysis, or conservative care without dialysis.107 Patient preference should be taken into consideration when selecting dialysis modality; however, patients with multiple abdominal surgeries with resultant peritoneal scarring or unstable housing are likely poor candidates for peritoneal dialysis.107,109 Patients planning for hemodialysis who exhibit rapid decline in eGFR should be referred to an experienced vascular surgeon for arteriovenous fistula placement. The KDOQI guidelines recommend that access creation should occur when eGFR is between 15 and 20 mL/min/1.73 m2.114 Of note, dialysis initiation has been associated with accelerated functional decline and high short-term mortality among older patients with poor functional status.115,116 Patient preferences for conservative approaches to medical management should be discussed and honored.
Conclusions
Chronic kidney disease affects 8% to 16% of the population worldwide and is a leading cause of death. Optimal management of CKD includes cardiovascular risk reduction, treatment of albuminuria, avoidance of potential nephrotoxins, and adjustments to drug dosing. Patients also require monitoring for complications of CKD, such as hyperkalemia, metabolic acidosis, anemia, and other metabolic abnormalities. Diagnosis, staging, and appropriate referral of CKD by primary care clinicians are important in reducing the burden of CKD worldwide.
Funding/Support:
Dr Chen was supported by a Clinician Scientist Career Development Award from Johns Hopkins University and is supported by a George M. O’Brien Center for Kidney Research Pilot and Feasibility Grant from Yale University and award K08DK117068 from the National Institutes of Health/NIDDK. Dr Grams is supported by NIDDK grants DK1008803, DK100446, and DK115534.
Role of the Funder/Sponsor: The supporting institutions had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Dr Chen reported receipt of grants from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and Yale University. Dr Grams reported receipt of grants from the NIDDK and the National Kidney Foundation and travel support from Dialysis Clinics Inc for an invited speakership at a directors’ meeting in May 2019. No other disclosures were reported.
Submissions: We encourage authors to submit papers for consideration as a Review. Please contact Edward Livingston, MD, at Edward. livingston@jamanetwork.org or Mary McGrae McDermott, MD, at mdm608@northwestern.edu.
REFERENCES
- 1.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–2047. doi: 10.1001/jama.298.17.2038 [DOI] [PubMed] [Google Scholar]
- 2.Hsu CY, Vittinghoff E, Lin F, Shlipak MG. The incidence of end-stage renal disease is increasing faster than the prevalence of chronic renal insufficiency. Ann Intern Med. 2004;141(2):95–101. doi: 10.7326/0003-4819-141-2-200407200-00007 [DOI] [PubMed] [Google Scholar]
- 3.Plantinga LC, Boulware LE, Coresh J, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med. 2008;168(20): 2268–2275. doi: 10.1001/archinte.168.20.2268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–272. doi: 10.1016/S0140-6736(13)60687-X [DOI] [PubMed] [Google Scholar]
- 5.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150. [Google Scholar]
- 6.Mills KT, Xu Y, Zhang W, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88(5):950–957. doi: 10.1038/ki.2015.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science. 2010; 329(5993):841–845. doi: 10.1126/science.1193032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tzur S, Rosset S, Shemer R, et al. Missense mutations in the APOL1 gene are highly associated with end stage kidney disease risk previously attributed to the MYH9 gene. Hum Genet. 2010;128 (3):345–350. doi: 10.1007/s00439-010-0861-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naik RP, Derebail VK, Grams ME, et al. Association of sickle cell trait with chronic kidney disease and albuminuria in African Americans. JAMA. 2014;312(20):2115–2125. doi: 10.1001/jama.2014.15063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Seaghdha CM, Parekh RS, Hwang SJ, et al. The MYH9/APOL1 region and chronic kidney disease in European-Americans. Hum Mol Genet. 2011;20 (12):2450–2456. doi: 10.1093/hmg/ddr118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grams ME, Rebholz CM, Chen Y, et al. Race, APOL1 risk, and eGFR decline in the general population. J Am Soc Nephrol. 2016;27(9):2842–2850. doi: 10.1681/ASN.2015070763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peralta CA, Vittinghoff E, Bansal N, et al. Trajectories of kidney function decline in young black and white adults with preserved GFR: results from the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Kidney Dis. 2013;62(2):261–266. doi: 10.1053/j.ajkd.2013.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grams ME, Chow EK, Segev DL, Coresh J. Lifetime incidence of CKD stages 3–5 in the United States. Am J Kidney Dis. 2013;62(2):245–252. doi: 10.1053/j.ajkd.2013.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsushita K, Coresh J, Sang Y, et al. ; CKD Prognosis Consortium. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 2015;3(7):514–525. doi: 10.1016/S2213-8587(15)00040-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Astor BC, Matsushita K, Gansevoort RT, et al. ; Chronic Kidney Disease Prognosis Consortium. Lower estimated glomerular filtration rate and higher albuminuria are associated with mortality and end-stage renal disease: a collaborative meta-analysis of kidney disease population cohorts. Kidney Int. 2011;79(12):1331–1340. doi: 10.1038/ki.2010.550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gansevoort RT, Matsushita K, van der Velde M, et al. ; Chronic Kidney Disease Prognosis Consortium. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes: a collaborative meta-analysis of general and high-risk population cohorts. Kidney Int. 2011; 80(1):93–104. doi: 10.1038/ki.2010.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Velde M, Matsushita K, Coresh J, et al. ; Chronic Kidney Disease Prognosis Consortium. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality: a collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011;79(12):1341–1352. doi: 10.1038/ki.2010.536 [DOI] [PubMed] [Google Scholar]
- 18.Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713–735. doi: 10.1053/j.ajkd.2014.01.416 [DOI] [PubMed] [Google Scholar]
- 19.Bilo H, Coentrão L, Couchoud C, et al. ; Guideline Development Group. Clinical practice guideline on management of patients with diabetes and chronic kidney disease stage 3b or higher (eGFR <45 mL/min). Nephrol Dial Transplant. 2015;30(suppl 2):ii1–ii142. doi: 10.1093/ndt/gfv100 [DOI] [PubMed] [Google Scholar]
- 20.Farrington K, Covic A, Aucella F, et al. ; ERBP Guideline Development Group. Clinical practice guideline on management of older patients with chronic kidney disease stage 3b or higher (eGFR <45 mL/min/1.73 m2). Nephrol Dial Transplant. 2016;31(suppl 2):ii1–ii66. doi: 10.1093/ndt/gfw356 [DOI] [PubMed] [Google Scholar]
- 21.Skorecki K, Chertow GM, Marsden PA, Taal MW, Yu ASL. Brenner & Rector’s the Kidney. 10th ed Philadelphia, PA: Elsevier; 2016. [Google Scholar]
- 22.Yang B, Xie Y, Guo M, Rosner MH, Yang H, Ronco C. Nephrotoxicity and Chinese herbal medicine. Clin J Am Soc Nephrol. 2018;13(10):1605–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocuts AK, Waikar SS, Alexander MP, Rennke HG, Singh AK. Acute phosphate nephropathy. Kidney Int. 2009;75(9):987–991. doi: 10.1038/ki.2008.293 [DOI] [PubMed] [Google Scholar]
- 24.Markowitz GS, Perazella MA. Acute phosphate nephropathy. Kidney Int. 2009;76(10):1027–1034. doi: 10.1038/ki.2009.308 [DOI] [PubMed] [Google Scholar]
- 25.Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313(8):837–846. doi: 10.1001/jama.2015.0602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown SC, O’Reilly PH. Iohexol clearance for the determination of glomerular filtration rate in clinical practice: evidence for a new gold standard. J Urol. 1991;146(3):675–679. doi: 10.1016/S0022-5347(17)37891-6 [DOI] [PubMed] [Google Scholar]
- 27.Elwood CM, Sigman EM, Treger C. The measurement of glomerular filtration rate with 125I-sodium iothalamate (Conray). Br J Radiol. 1967; 40(476):581–583. doi: 10.1259/0007-1285-40-476-581 [DOI] [PubMed] [Google Scholar]
- 28.Sigman EM, Elwood CM, Knox F. The measurement of glomerular filtration rate in man with sodium iothalamate 131-I (Conray). J Nucl Med. 1966;7(1):60–68. [PubMed] [Google Scholar]
- 29.Levey AS, Stevens LA, Schmid CH, et al. ; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D; Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999; 130(6):461–470. doi: 10.7326/0003-4819-130-6-199903160-00002 [DOI] [PubMed] [Google Scholar]
- 31.Inker LA, Schmid CH, Tighiouart H, et al. ; CKD-EPI Investigators. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–29. doi: 10.1056/NEJMoa1114248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Myers GL, Miller WG, Coresh J, et al. ; National Kidney Disease Education Program Laboratory Working Group. Recommendations for improving serum creatinine measurement: a report from the Laboratory Working Group of the National Kidney Disease Education Program. Clin Chem. 2006;52(1): 5–18. doi: 10.1373/clinchem.2005.0525144 [DOI] [PubMed] [Google Scholar]
- 33.Lieske JC, Bondar O, Miller WG, et al. ; National Kidney Disease Education Program–IFCC Working Group on Standardization of Albumin in Urine. A reference system for urinary albumin: current status. Clin Chem Lab Med. 2013;51(5):981–989. doi: 10.1515/cclm-2012-0768 [DOI] [PubMed] [Google Scholar]
- 34.Miller WG, Bruns DE. Laboratory issues in measuring and reporting urine albumin. Nephrol Dial Transplant. 2009;24(3):717–718. doi: 10.1093/ndt/gfp022 [DOI] [PubMed] [Google Scholar]
- 35.Witte EC, Lambers Heerspink HJ, de Zeeuw D, Bakker SJ, de Jong PE, Gansevoort R. First morning voids are more reliable than spot urine samples to assess microalbuminuria. J Am Soc Nephrol. 2009; 20(2):436–443. doi: 10.1681/ASN.2008030292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rampoldi L, Scolari F, Amoroso A, Ghiggeri G, Devuyst O. The rediscovery of uromodulin (Tamm-Horsfall protein): from tubulointerstitial nephropathy to chronic kidney disease. Kidney Int. 2011;80(4):338–347. doi: 10.1038/ki.2011.134 [DOI] [PubMed] [Google Scholar]
- 37.El-Achkar TM, Wu XR. Uromodulin in kidney injury: an instigator, bystander, or protector? Am J Kidney Dis. 2012;59(3):452–461. doi: 10.1053/j.ajkd.2011.10.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garimella PS, Biggs ML, Katz R, et al. Urinary uromodulin, kidney function, and cardiovascular disease in elderly adults. Kidney Int. 2015;88(5): 1126–1134. doi: 10.1038/ki.2015.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergmann C, Guay-Woodford LM, Harris PC, Horie S, Peters DJM, Torres VE. Polycystic kidney disease. Nat Rev Dis Primers. 2018;4(1):50. doi: 10.1038/s41572-018-0047-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Torres VE, Chapman AB, Devuyst O, et al. ; REPRISE Trial Investigators. Tolvaptan in later-stage autosomal dominant polycystic kidney disease. N Engl J Med. 2017;377(20):1930–1942. doi: 10.1056/NEJMoa1710030 [DOI] [PubMed] [Google Scholar]
- 41.National Kidney Foundation. National Kidney Foundation, American Society for Clinical Pathology, leading laboratories and clinical laboratory societies unite to diagnose chronic kidney disease. https://www.kidney.org/news/national-kidney-foundation-american-society-clinical-pathology-leading-laboratories-and Published February 21, 2018 Accessed August 13, 2019. [Google Scholar]
- 42.Chang AR, Grams ME, Ballew SH, et al. ; CKD Prognosis Consortium. Adiposity and risk of decline in glomerular filtration rate: meta-analysis of individual participant data in a global consortium. BMJ. 2019;364:k5301. doi: 10.1136/bmj.k5301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kazancioğlu R Risk factors for chronic kidney disease: an update. Kidney Int Suppl (2011). 2013;3 (4):368–371. doi: 10.1038/kisup.2013.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peralta CA, Bibbins-Domingo K, Vittinghoff E, et al. APOL1 genotype and race differences in incident albuminuria and renal function decline. J Am Soc Nephrol. 2016;27(3):887–893. doi: 10.1681/ASN.2015020124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Foster MC, Coresh J, Fornage M, et al. APOL1 variants associate with increased risk of CKD among African Americans. J Am Soc Nephrol. 2013;24(9): 1484–1491. doi: 10.1681/ASN.2013010113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Banerjee T, Crews DC, Wesson DE, et al. ; CDC CKD Surveillance Team. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70(1):38–47. doi: 10.1053/j.ajkd.2016.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.US Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 2018. [Google Scholar]
- 48.Kopp JB, Nelson GW, Sampath K, et al. APOL1 genetic variants in focal segmental glomerulosclerosis and HIV-associated nephropathy. J Am Soc Nephrol. 2011;22(11):2129–2137. doi: 10.1681/ASN.2011040388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parsa A, Kao WH, Xie D, et al. ; AASK Study Investigators; CRIC Study Investigators. APOL1 risk variants, race, and progression of chronic kidney disease. N Engl J Med. 2013;369(23):2183–2196. doi: 10.1056/NEJMoa1310345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kidney Disease: Improving Global Outcomes (KDIGO) Lipid Work Group. KDIGO clinical practice guideline for lipid management in chronic kidney disease. Kidney Int Suppl. 2013;3(3):259–305. [Google Scholar]
- 51.Tonelli M, Wanner C; Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. Lipid management in chronic kidney disease: synopsis of the Kidney Disease: Improving Global Outcomes 2013 clinical practice guideline. Ann Intern Med. 2014;160(3):182. doi: 10.7326/M13-2453 [DOI] [PubMed] [Google Scholar]
- 52.Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society Guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32(11):1263–1282. doi: 10.1016/j.cjca.2016.07.510 [DOI] [PubMed] [Google Scholar]
- 53.Ricardo AC, Anderson CA, Yang W, et al. ; CRIC Study Investigators. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis. 2015;65(3):412–424. doi: 10.1053/j.ajkd.2014.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 55.Wright JT Jr, Williamson JD, Whelton PK, et al. ; SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang WR, Craven TE, Malhotra R, et al. ; SPRINT Research Group. Kidney damage biomarkers and incident chronic kidney disease during blood pressure reduction: a case-control study. Ann Intern Med. 2018;169(9):610–618. doi: 10.7326/M18-1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cheung AK, Rahman M, Reboussin DM, et al. ; SPRINT Research Group. Effects of intensive BP control in CKD. J Am Soc Nephrol. 2017;28(9):2812–2823. doi: 10.1681/ASN.2017020148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 59.Fried LF, Emanuele N, Zhang JH, et al. ; VA NEPHRON-D Investigators. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369(20):1892–1903. doi: 10.1056/NEJMoa1303154 [DOI] [PubMed] [Google Scholar]
- 60.Williams B, MacDonald TM, Morant S, et al. ; British Hypertension Society’s PATHWAY Studies Group. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–2068. doi: 10.1016/S0140-6736(15)00257-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pitt B, Zannad F, Remme WJ, et al. ; Randomized Aldactone Evaluation Study Investigators. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341(10):709–717. doi: 10.1056/NEJM199909023411001 [DOI] [PubMed] [Google Scholar]
- 62.Zannad F, McMurray JJ, Krum H, et al. ; EMPHASIS-HF Study Group. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364(1):11–21. doi: 10.1056/NEJMoa1009492 [DOI] [PubMed] [Google Scholar]
- 63.Ando K, Ohtsu H, Uchida S, Kaname S, Arakawa Y, Fujita T; EVALUATE Study Group. Anti-albuminuric effect of the aldosterone blocker eplerenone in non-diabetic hypertensive patients with albuminuria: a double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2014;2(12):944–953. doi: 10.1016/S2213-8587(14)70194-9 [DOI] [PubMed] [Google Scholar]
- 64.Bakris GL, Agarwal R, Chan JC, et al. ; Mineralocorticoid Receptor Antagonist Tolerability Study–Diabetic Nephropathy Study Group. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015;314(9):884–894. doi: 10.1001/jama.2015.10081 [DOI] [PubMed] [Google Scholar]
- 65.Shurraw S, Hemmelgarn B, Lin M, et al. ; Alberta Kidney Disease Network. Association between glycemic control and adverse outcomes in people with diabetes mellitus and chronic kidney disease: a population-based cohort study. Arch Intern Med. 2011;171(21):1920–1927. doi: 10.1001/archinternmed.2011.537 [DOI] [PubMed] [Google Scholar]
- 66.Nathan DM, Zinman B, Cleary PA, et al. ; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications and Pittsburgh Epidemiology of Diabetes Complications experience (1983–2005). Arch Intern Med. 2009;169(14):1307–1316. doi: 10.1001/archinternmed.2009.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853. doi: 10.1016/S0140-6736(98)07019-6 [DOI] [PubMed] [Google Scholar]
- 68.Perkovic V, Jardine MJ, Neal B, et al. ; CREDENCE Trial Investigators. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–2306. doi: 10.1056/NEJMoa1811744 [DOI] [PubMed] [Google Scholar]
- 69.Neal B, Perkovic V, Mahaffey KW, et al. ; CANVAS Program Collaborative Group. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–657. doi: 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 70.Zinman B, Wanner C, Lachin JM, et al. ; EMPA-REG OUTCOME Investigators. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. doi: 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 71.Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016;176(2):238–246. doi: 10.1001/jamainternmed.2015.7193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Muriithi AK, Leung N, Valeri AM, et al. Biopsy-proven acute interstitial nephritis, 1993–2011: a case series. Am J Kidney Dis. 2014;64 (4):558–566. doi: 10.1053/j.ajkd.2014.04.027 [DOI] [PubMed] [Google Scholar]
- 73.Blank ML, Parkin L, Paul C, Herbison P. A nationwide nested case-control study indicates an increased risk of acute interstitial nephritis with proton pump inhibitor use. Kidney Int. 2014;86(4): 837–844. doi: 10.1038/ki.2014.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Palacio-Lacambra ME, Comas-Reixach I, Blanco-Grau A, Suñé-Negre JM, Segarra-Medrano A, Montoro-Ronsano JB. Comparison of the Cockcroft-Gault, MDRD and CKD-EPI equations for estimating ganciclovir clearance. Br J Clin Pharmacol. 2018;84(9):2120–2128. doi: 10.1111/bcp.13647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Okparavero AA, Tighiouart H, Krishnasami Z, et al. Use of glomerular filtration rate estimating equations for drug dosing in HIV-positive patients. Antivir Ther. 2013;18(6):793–802. doi: 10.3851/IMP2676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chan KE, Giugliano RP, Patel MR, et al. Nonvitamin K anticoagulant agents in patients with advanced chronic kidney disease or on dialysis with AF. J Am Coll Cardiol. 2016;67(24):2888–2899. doi: 10.1016/j.jacc.2016.02.082 [DOI] [PubMed] [Google Scholar]
- 77.Chapin E, Zhan M, Hsu VD, Seliger SL, Walker LD, Fink JC. Adverse safety events in chronic kidney disease: the frequency of “multiple hits”. Clin J Am Soc Nephrol. 2010;5(1):95–101. doi: 10.2215/CJN.06210909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dreisbach AW, Lertora JJ. The effect of chronic renal failure on drug metabolism and transport. Expert Opin Drug Metab Toxicol. 2008;4(8):1065–1074. doi: 10.1517/17425255.4.8.1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fink JC, Brown J, Hsu VD, Seliger SL, Walker L, Zhan M. CKD as an underrecognized threat to patient safety. Am J Kidney Dis. 2009;53(4):681–688. doi: 10.1053/j.ajkd.2008.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bahrainwala JZ, Leonberg-Yoo AK, Rudnick MR. Use of radiocontrast agents in CKD and ESRD. Semin Dial. 2017;30(4):290–304. doi: 10.1111/sdi.12593 [DOI] [PubMed] [Google Scholar]
- 81.Abu-Alfa AK. Nephrogenic systemic fibrosis and gadolinium-based contrast agents. Adv Chronic Kidney Dis. 2011;18(3):188–198. doi: 10.1053/j.ackd.2011.03.001 [DOI] [PubMed] [Google Scholar]
- 82.Perazella MA. Advanced kidney disease, gadolinium and nephrogenic systemic fibrosis: the perfect storm. Curr Opin Nephrol Hypertens. 2009; 18(6):519–525. doi: 10.1097/MNH.0b013e3283309660 [DOI] [PubMed] [Google Scholar]
- 83.Klahr S, Levey AS, Beck GJ, et al. ; Modification of Diet in Renal Disease Study Group. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. N Engl J Med. 1994;330(13):877–884. doi: 10.1056/NEJM199403313301301 [DOI] [PubMed] [Google Scholar]
- 84.Menon V, Kopple JD, Wang X, et al. Effect of a very low-protein diet on outcomes: long-term follow-up of the Modification of Diet in Renal Disease (MDRD) study. Am J Kidney Dis. 2009;53 (2):208–217. doi: 10.1053/j.ajkd.2008.08.009 [DOI] [PubMed] [Google Scholar]
- 85.Robertson L, Waugh N, Robertson A. Protein restriction for diabetic renal disease. Cochrane Database Syst Rev. 2007;(4):CD002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rosman JB, ter Wee PM, Meijer S, Piers-Becht TP, Sluiter WJ, Donker AJ. Prospective randomised trial of early dietary protein restriction in chronic renal failure. Lancet. 1984;2(8415):1291–1296. doi: 10.1016/S0140-6736(84)90818-3 [DOI] [PubMed] [Google Scholar]
- 87.Hansen HP, Christensen PK, Tauber-Lassen E, Klausen A, Jensen BR, Parving HH. Low-protein diet and kidney function in insulin-dependent diabetic patients with diabetic nephropathy. Kidney Int. 1999;55(2):621–628. doi: 10.1046/j.1523-1755.1999.00274.x [DOI] [PubMed] [Google Scholar]
- 88.Hansen HP, Tauber-Lassen E, Jensen BR, Parving HH. Effect of dietary protein restriction on prognosis in patients with diabetic nephropathy. Kidney Int. 2002;62(1):220–228. doi: 10.1046/j.1523-1755.2002.00421.x [DOI] [PubMed] [Google Scholar]
- 89.Knight EL, Stampfer MJ, Hankinson SE, Spiegelman D, Curhan GC. The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann Intern Med. 2003;138(6):460–467. doi: 10.7326/0003-4819-138-6-200303180-00009 [DOI] [PubMed] [Google Scholar]
- 90.Goraya N, Simoni J, Jo C, Wesson DE. Dietary acid reduction with fruits and vegetables or bicarbonate attenuates kidney injury in patients with a moderately reduced glomerular filtration rate due to hypertensive nephropathy. Kidney Int. 2012;81(1):86–93. doi: 10.1038/ki.2011.313 [DOI] [PubMed] [Google Scholar]
- 91.Banerjee T, Crews DC, Wesson DE, et al. ; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team. High dietary acid load predicts ESRD among adults with CKD. J Am Soc Nephrol. 2015;26(7):1693–1700. doi: 10.1681/ASN.2014040332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Inker LA, Grams ME, Levey AS, et al. ; CKD Prognosis Consortium. Relationship of estimated GFR and albuminuria to concurrent laboratory abnormalities: an individual participant data meta-analysis in a global consortium. Am J Kidney Dis. 2019;73(2):206–217. doi: 10.1053/j.ajkd.2018.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kidney Disease: Improving Global Outcomes (KDIGO) Anemia Work Group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl. 2012;2(4):279–335. [Google Scholar]
- 94.Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD). Kidney Int Suppl (2011). 2017;7(1):1–59. doi: 10.1016/j.kisu.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Isakova T, Nickolas TL, Denburg M, et al. KDOQI US commentary on the 2017 KDIGO clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD). Am J Kidney Dis. 2017;70(6):737–751. doi: 10.1053/j.ajkd.2017.07.019 [DOI] [PubMed] [Google Scholar]
- 96.de Brito-Ashurst I, Varagunam M, Raftery MJ, Yaqoob MM. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J Am Soc Nephrol. 2009;20(9):2075–2084. doi: 10.1681/ASN.2008111205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dobre M, Yang W, Chen J, et al. ; CRIC Investigators. Association of serum bicarbonate with risk of renal and cardiovascular outcomes in CKD: a report from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis. 2013;62(4): 670–678. doi: 10.1053/j.ajkd.2013.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Driver TH, Shlipak MG, Katz R, et al. Low serum bicarbonate and kidney function decline: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Kidney Dis. 2014;64(4):534–541. doi: 10.1053/j.ajkd.2014.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mahajan A, Simoni J, Sheather SJ, Broglio KR, Rajab MH, Wesson DE. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 2010;78(3):303–309. doi: 10.1038/ki.2010.129 [DOI] [PubMed] [Google Scholar]
- 100.Tangri N, Grams ME, Levey AS, et al. ; CKD Prognosis Consortium. Multinational assessment of accuracy of equations for predicting risk of kidney failure: a meta-analysis. JAMA. 2016; 315(2):164–174. doi: 10.1001/jama.2015.18202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med. 2004;164(6):659–663. doi: 10.1001/archinte.164.6.659 [DOI] [PubMed] [Google Scholar]
- 102.Tangri N, Stevens LA, Griffith J, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA. 2011;305 (15):1553–1559. doi: 10.1001/jama.2011.451 [DOI] [PubMed] [Google Scholar]
- 103.Hingwala J, Wojciechowski P, Hiebert B, et al. Risk-based triage for nephrology referrals using the kidney failure risk equation. Can J Kidney Health Dis. 2017;4:2054358117722782. doi: 10.1177/2054358117722782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Smekal MD, Tam-Tham H, Finlay J, et al. Patient and provider experience and perspectives of a risk-based approach to multidisciplinary chronic kidney disease care: a mixed methods study. BMC Nephrol. 2019;20(1):110. doi: 10.1186/s12882-019-1269-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Harasemiw O, Drummond N, Singer A, et al. Integrating risk-based care for patients with chronic kidney disease in the community: study protocol for a cluster randomized trial. Can J Kidney Health Dis. 2019;6:2054358119841611. doi: 10.1177/2054358119841611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Grams ME, Sang Y, Ballew SH, et al. Predicting timing of clinical outcomes in patients with chronic kidney disease and severely decreased glomerular filtration rate. Kidney Int. 2018;93(6):1442–1451. doi: 10.1016/j.kint.2018.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Eckardt KU, Bansal N, Coresh J, et al. ; Conference Participants. Improving the prognosis of patients with severely decreased glomerular filtration rate (CKD G4+): conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2018;93(6): 1281–1292. doi: 10.1016/j.kint.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cooper BA, Branley P, Bulfone L, et al. ; IDEAL Study. A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med. 2010;363 (7):609–619. doi: 10.1056/NEJMoa1000552 [DOI] [PubMed] [Google Scholar]
- 109.Daugirdas JT, Blake BG, Ing TS, eds. Handbook of Dialysis. 4th ed Philadelphia, PA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 110.Mange KC, Joffe MM, Feldman HI. Effect of the use or nonuse of long-term dialysis on the subsequent survival of renal transplants from living donors. N Engl J Med. 2001;344(10):726–731. doi: 10.1056/NEJM200103083441004 [DOI] [PubMed] [Google Scholar]
- 111.Terasaki PI, Cecka JM, Gjertson DW, Takemoto S. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995;333(6):333–336. doi: 10.1056/NEJM199508103330601 [DOI] [PubMed] [Google Scholar]
- 112.United Network for Organ Sharing. Frequently asked questions about kidney transplant evaluation and listing. https://unos.org/wp-content/uploads/unos/Kidney_Eval_Brochure.pdf. Published 2018. Accessed August 6, 2019. [Google Scholar]
- 113.Organ Procurement and Transplantation Network. Educational guidance on patient referral to kidney transplantation. https://optn.transplant.hrsa.gov/resources/guidance/educational-guidance-on-patient-referral-to-kidney-transplantation/. Published September 2015. Accessed August 6, 2019.
- 114.National Kidney Foundation. KDOQI Clinical Practice Guideline For Vascular Access: 2018. https://www.kidney.org/sites/default/files/kdoqi_vasc-access-review2019_v2.pdf. Published April 2019. Accessed August 13, 2019. [DOI] [PubMed] [Google Scholar]
- 115.Couchoud CG, Beuscart JB, Aldigier JC, Brunet PJ, Moranne OP; REIN Registry. Development of a risk stratification algorithm to improve patient-centered care and decision making for incident elderly patients with end-stage renal disease. Kidney Int. 2015;88(5):1178–1186. doi: 10.1038/ki.2015.245 [DOI] [PubMed] [Google Scholar]
- 116.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361(16):1539–1547. doi: 10.1056/NEJMoa0904655 [DOI] [PMC free article] [PubMed] [Google Scholar]