Abstract
Despite the widespread clinical use of cardioprotection by long-term direct antagonism of P2Y12 receptor, underlying mechanisms are unclear. Here, we identify how release of pro-survival exosomes from human cardiac-derived mesenchymal progenitor cells (hCPCs) is regulated by clinically relevant dose of ticagrelor (1 μM), an oral selective and reversible non-thienopyridine P2Y12 inhibitor. Ticagrelor-induced enhancement of exosome levels is related to increased mitotic activity of hCPCs. We show a drug-response threshold above which the effects on hCPCs are lost due to higher dose of ticagrelor and larger adenosine levels. While it is known that pan-Aurora kinase inhibitor halts cell proliferation through dephosphorylation of histone H3 residue Ser10, we demonstrate that it also prevents ticagrelor-induced effects on release of cardiac progenitor cell-derived exosomes delivering anti-apoptotic HSP70. Indeed, sustained pre-treatment of cardiomyocytes with exosomes released from explant-derived hCPCs exposed to low-dose ticagrelor attenuated hypoxia-induced apoptosis through acute phosphorylation of ERK42/44. Our data indicate that ticagrelor can be leveraged to modulate release of anti-hypoxic exosomes from resident hCPCs.
Subject terms: Cell biology, Molecular medicine
Introduction
Acute myocardial infarction (AMI) is an adverse cardiac event leading to high risk of morbidity and mortality worldwide1. Indeed, it has been demonstrated that a significant residual microvascular perfusion deficit remains after coronary revascularization2, which leads to cardiac cell death and progressive ventricular remodeling3. Post-ischemic left ventricular (LV) remodeling is a complex scenario mainly characterized by progressive loss of cardiomyocytes due to apoptosis and alteration of intercellular cross talk following prolonged exposure to hypoxic microenvironment3. In order to improve AMI care, adequate pharmacological approach to safely increase hypoxic tolerance of cardiomyocytes remains a critical need.
Numerous experimental4–8 and clinical9–12 studies have shown that long-term antagonism of P2Y12, a G protein-coupled (GPCR) purinergic receptor, protects the myocardium against ischemic LV remodeling. Chronic administration of ticagrelor, a selective and reversible P2Y12 receptor antagonist that does not require metabolic activation, is more cardioprotective than clopidogrel13,14, a prodrug that irreversibly inhibits P2Y12. The non-thienopyridine P2Y12 inhibitor such as ticagrelor enhances cardiomyocyte tolerance against ischemic microenvironment4,7,8,15 beyond its clinical efficacy in preventing intracoronary platelet aggregation. Although previous studies suggested that cardioprotective pleiotropic effects of ticagrelor are dependent on the enhanced levels of adenosine16, this mechanistic relationship was recently questioned by others17. In particular, recent study demonstrated that higher dose of ticagrelor (10 μM/L), which potentiates extracellular adenosine concentration compared to lower dose18, failed to protect ischemic reperfused rodent heart19. Although such a high dose of ticagrelor has not yet been tested in patients, we cannot exclude that chronic P2Y12 antagonism by lower dose of ticagrelor may lead to cardioprotective milieu in the myocardium through hitherto unexpected pleiotropic effects.
Cardiac-derived progenitor cells (CPCs), non-myocyte cells expressing mesenchymal/stromal cell surface markers even termed cardiac-derived mesenchymal progenitor cells, are involved in myocardial homeostasis after injury20. Indeed, these cells are able to release exosomes, smallest membrane-surrounded extracellular nanovesicles, which hamper cardiomyocyte apoptosis due to serum-nutrient starvation in a dose-dependent manner and attenuate LV remodeling in infarcted rodent heart21–23. Emerging evidences have also demonstrated that release of anti-apoptotic exosomes from explant-derived CPCs may be enhanced by microenvironment stimuli, such as hypoxia24. However, the study of the regulatory role of conventional cardiovascular drugs on release of human CPCs-derived exosomes is still at its infancy. Preliminary study demonstrated that P2Y12 antagonists decrease the release of pro-coagulant extracellular vesicles from activated platelets25, but the regulatory effects of ticagrelor on release of anti-apoptotic exosomes from adult cardiac-resident cells (i.e.: auricle-derived CPCs) has not yet been investigated. Since enrichment of plasma exosomes with those released from transplanted cardiac progenitor cells protected the ischemic myocardium26, we hypothesized that similar results might be obtained by pharmacological stimulation of cardiac-resident mesenchymal progenitor cells and without exosome transplantation. Since P2Y12 receptors are generally expressed in progenitor cells27, it is conceivable that long-term antagonism of P2Y12 receptor of human CPCs by ticagrelor may promote the release of exosomes protecting cardiomyocytes against hypoxia-induced apoptosis. For this purpose, we have used a well-characterized in vitro model of ischemic/hypoxic cardiomyocyte death based on murine HL1 cardiomyocytes chronically exposed to severe hypoxia28.
Results
Profile of adult explant-derived hCPCs
Cells were derived from human atrial appendage specimens cultured ex vivo as heart explants in accord with our previous studies21,23. Cells derived from auricle were a non-pure population. As shown in Supplemental Fig. 1, cells expressed mesenchymal/stromal markers (CD90, CD73, CD105), but not the common leukocyte antigen CD45. CD117 expression was almost absent. Since we have shown that atrial biopsy-derived cells express early cardiac markers (GATA4, MEF2c) and exhibit mesenchymal multilineage differentiation potential21,23, we term these cells human cardiac-derived mesenchymal progenitor cells, for which we used the acronym hCPCs for short.
Long-term treatment with lower dose of ticagrelor increases exosome levels
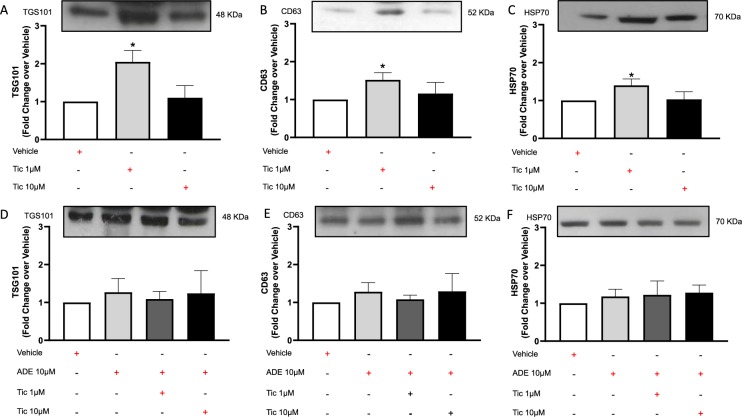
Adult hCPCs express P2Y12 receptors as for adult vascular smooth muscle cells (Supplemental Fig. 2). As shown in Fig. 1A–C, conditioned medium of proliferating hCPCs after treatment with lower dose of ticagrelor was enriched in vesicles expressing typical exosomal markers such as TSG101 + (A), CD63 + (B) and HSP70 + (C)29. Higher dose of ticagrelor did not increase exosome levels. Interestingly, effective dose of ticagrelor did not affect intracellular HSP70 levels (Supplemental Fig. 3). Exosome levels were not increased by long-term treatment of hCPCs with exogenous adenosine per se, which instead counteracted the effects of low-dose ticagrelor and did not enhance the effects of high-dose ticagrelor on extracellular exosome levels (Fig. 1D–F).
Figure 1.
Long-term treatment for 72 h of human cardiac progenitor cells (hCPCs) with low-dose (1 μM) of ticagrelor (Tic) enhances the release of TSG101+ (A; 48KDa MW), CD63 + (B; 52KDa MW) and heat shock protein (HSP)-70 + (C; 70KDa MW) exosomes, but not at higher dose (Tic 10 μM). As shown in panels D–F, adenosine (ADE, 10 μM) per se does not enhance exosome release and its addiction to culture medium counteracts the effects of Tic 1 µM. Adenosine is added in the presence of EHNA (10 μM). Representative images of cropped densitometric bands of proteins TSG101, CD63 and HSP70 are showed in each panel. The full-length blots/gels of panels A–C and D–F are presented in Supplementary Figure 5 panel A and B respectively. All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution).
Ticagrelor-induced Exosome release is related to higher hCPCs proliferation
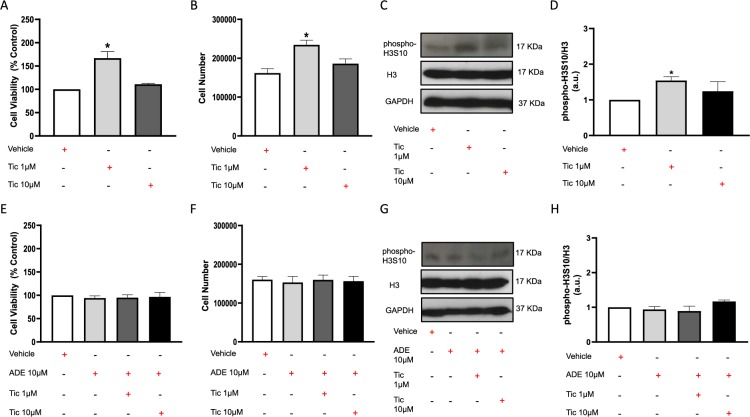
As shown in Fig. 2A,B, 72 h treatment with low-dose ticagrelor (1 μM) significantly increased viability and number of cultured hCPCs, but not at higher dose (10 μM). The elevated levels of phospho-H3S10/H3 in hCPCs treated with lower dose of drug defined threshold for proliferative effects of ticagrelor (Fig. 2C,D). Of note, ticagrelor did not alter H3 expression. This effect was not induced by long-term treatment of cells with exogenous adenosine per se, which instead counteracted the effects of low-dose ticagrelor and did not enhance the effects of high-dose ticagrelor on cell viability and proliferation (Fig. 2E–H).
Figure 2.
Long-term treatment for 72 h of human cardiac progenitor cells (hCPCs) with low-dose (1 μM) of ticagrelor (Tic) increases the cell viability (A), the cell number of viable cells (B) and the human phosphorylated Histone H3 on Serine 10 (phospho-H3S10; 17KDa MW)/total histone H3 (H3; 17KDa MW) ratio (C,D), but not at higher dose (Tic 10 μM). As shown in panels E-H, adenosine (ADE, 10 μM) per se does not enhance cell viability and proliferation and its addiction to culture medium counteracts the effects of Tic 1 μM. Adenosine is added in the presence of EHNA (10 μM). Levels of phospho-H3S10 and H3 are normalized on glyceraldehyde 3-phosphate dehydrogenase (GAPDH) levels and values of ratio are expressed as arbitrary units (a.u.). Representative images of cropped densitometric bands of proteins phospho-H3S10, H3 and GAPDH are showed in each panel. In Supplemental Fig. 6: the full-length blots/gels of panel C are presented as V, T1-1, T10-1 (A); the full-length blots/gels of panel G are presented as V2, A2, AT1-2, AT10-2 (B). All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution).
Reduced histone H3 phosphorylation inhibits ticagrelor-driven effects on hCPCs
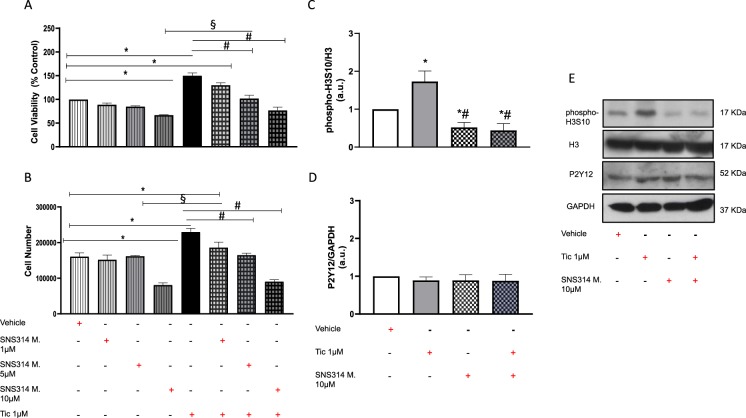
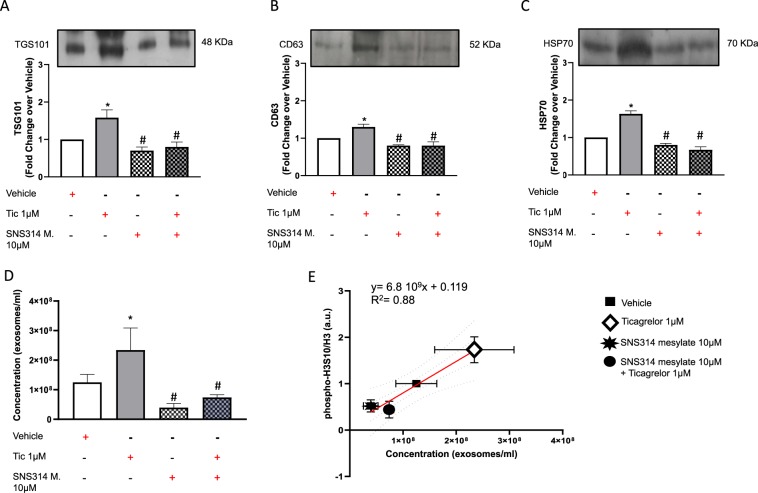
As shown in Fig. 3, co-treatment of hCPCs with higher doses of SNS314 mesylate, an inhibitor of histone H3 phosphorylation, reverted the effects of ticagrelor to control level (vehicle) in terms of both cell viability (A) and number of cells (B) in a dose-dependent manner. In light of these results, selected dose of SNS314 mesylate (10 μM) prevented the ticagrelor-induced increase of phospho-H3S10/H3 ratio (C, E) without altering P2Y12 levels (D, E). As shown in Fig. 4, co-treatment with SNS314 mesylate prevented ticagrelor-induced medium enrichment in exosomes as assessed by the expression of TSG101 (A), CD63 (B) and HSP70 + (C). The relationship between extent of histone H3 phosphorylation and exosome levels was confirmed by NanoSight technology (Fig. 4D and Supplemental Fig. 4). Of importance, we found a positive relationship among phospho-H3S10/H3 values and exosome levels (Fig. 4E).
Figure 3.
SNS314 mesylate (SNS314 M), an inhibitor phosphorylation of histone H3 at serine 10 (phospho-H3S10), reduces cell viability (A) and proliferation (B) in a dose dependent manner in hCPCs untreated and treated with ticagrelor (Tic 1 μM). Higher dose of SNS314 M (10 μM) counteracts ticagrelor (Tic 1 μM) effects (A,B). SNS314 M 10 μM counteract effects of Tic 1 μM on levels of phospho-H3S10/H3 ratio (C) without altering expression of P2Y12 (D; 52KDa MW) of hCPCs. Levels of phospho-H3S10, H3 and P2Y12 are normalized on glyceraldehyde 3-phosphate dehydrogenase (GAPDH) levels and expressed as arbitrary units (a.u.). Representative images of cropped densitometric bands of proteins phospho-H3S10, H3, P2Y12 and GAPDH are showed in panel E. The full-length blots/gels are presented in Supplemental Fig. 7 panel A. All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution); #p < 0.05 vs. Tic 1 μM; §p < 0.05 vs. SNS314 M (10 μM).
Figure 4.
SNS314 mesylate (SNS314 M), an inhibitor phosphorylation of histone H3 at serine 10 (phospho-H3S10), counteracts the effects of ticagrelor (Tic) 1uM on levels of TSG101 + (A; 48KDa MW), CD63 + (B; 52KDa MW) and heat shock protein 70 (HSP70) + (C; 70KDa MW) exosomes. Representative images of cropped densitometric bands of proteins TSG101, CD63 and HSP70 are showed in each panel. The full-length blots/gels are presented in Supplemental Fig. 7 panel B. As confirmed in panel D, SNS314 M prevents rising of exosome concentration in culture medium induced by Tic 1 μM assessed by NanoSight technology. As shown in panel E, there is a positive correlation between changes in phospho-H3S10/H3 values and exosome concentration in each experimental condition. All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution); #p < 0.05 vs. Tic 1 μM.
Ticagrelor enhances anti-apoptotic effects of hCPCs-exosomes
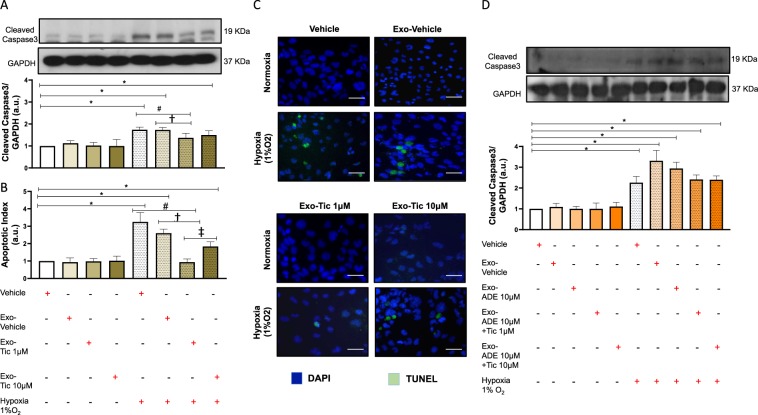
As shown in Fig. 5A, 48 h pre-treatment of HL1 cardiomyocytes with exosomes (100 μg) released by hCPCs primed with low-dose ticagrelor significantly prevented rising levels of cleaved caspase 3 due to chronic severe hypoxia. Anti-apoptotic effects of ticagrelor-induced exosomes were confirmed by TUNEL assay (Fig. 5B,C). Prevention of hypoxia-driven cardiomyocytes apoptosis was not observed after treatment with similar dose of exosomes released by hCPCs treated with vehicle or 10 μM ticagrelor (Fig. 5A,B) even in presence of adenosine (Fig. 5D). Interestingly, similar dose of exosomes released from hCPCs co-treated with 1 μM ticagrelor and adenosine were unable to prevent cardiomyocyte apoptosis due to sustained severe hypoxia (Fig. 5D).
Figure 5.
Long-term pre-treatment for 48 h of normoxic HL1 cardiomyocytes with exosomes (100 μg) derived from hCPCs treated with low-dose ticagrelor (Tic 1 μM) prevents rising of cleaved caspase 3 levels (A) and apoptosis index (B) during severe hypoxia (1% O2), but not exosomes derived from hCPCs treated with high-dose ticagrelor (Tic 10 μM). Representative images of TUNEL staining of HL1 cells in each experimental condition are showed in panel C. As shown in panels D, exosomes released from hCPCs treated in the presence of adenosine (ADE, 10 μM) and EHNA (10 μM) do not prevents rising of cleaved caspase 3 levels in hypoxic cardiomyocytes. Representative images of full-length blots/gels of proteins cleaved caspase 3 and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) are showed in panel A and D. Levels of cleaved caspase 3 are normalized on GAPDH levels and expressed as arbitrary units (a.u.) of cleaved caspase 3 (19 kDa, MW)/GAPDH (37 kDa, MW) ratio. All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution); #p < 0.05 vs. hypoxia; †p < 0.05 vs. Exo-Vehicle; ‡p < 0.05 vs. Exo-Tic 1 μM.
Ticagrelor-induced hCPCs exosomes activate ERK42/44 in cardiomyocytes
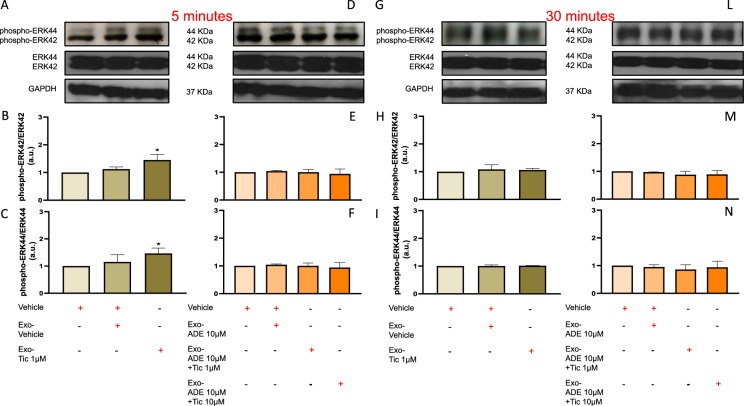
As shown in Fig. 6, long-term exposure of HL1 cardiomyocytes with defined amount of exosomes (100 μg) released from hCPCs treated with 1 μM ticagrelor increased phosphorylation of ERK42 and 44 at 5 min (A-C), which decreased after 30 min (Figure H-I). The rapid phosphorylation of ERK42 and 44 was not induced by similar dose of exosomes released by hCPCs in other experimental conditions (Fig. 6A–C). Of note, similar dose of exosomes released from hCPCs treated with adenosine per se or co-treated with increasing doses of ticagrelor and adenosine did not increase phosphorylation of ERK42 and 44 at 5 (Fig. 6D–F) and 30 min (Fig. 6L–N).
Figure 6.
Long-term pre-treatment for 48 h of normoxic HL1 cardiomyocytes with exosomes (100 μg) derived from hCPCs treated with low-dose ticagrelor (Tic 1 μM) increase levels of phosphorylated ERK42/total ERK42 (B; 42KDa MW) and phosphorylated ERK44/ total ERK44 (C; 44KDa MW) ratios after 5 min. Representative images of cropped densitometric bands of phosphorylated and total ERK 42/44, and glyceraldehyde 3-phosphate dehydrogenase (GAPDH; 37KDa MW) are showed in panel A and D. All full-length blots/gels are presented in Supplemental Fig. 8 panel A. As shown in panels E,F, exosomes released from hCPCs treated in the presence of adenosine (ADE, 10 μM) and EHNA (10 μM) do not induce rising of intracellular phosphorylated ERK42/44 levels. Representative images of cropped densitometric bands of phosphorylated and total ERK 42/44, and GAPDH are showed in panel D. Intracellular levels of phosphorylation of ERK42/44 are normal in HL1 cells after 30 min of treatment with ticagrelor-induced exosomes in the absence (H,I) or presence (L,M) of adenosine (ADE 10 μM) + EHNA (10 μM). Representative images of cropped densitometric bands of phosphorylated and total ERK 42/44, and GAPDH are showed in panel G and L. All full-length blots/gels are presented in Supplemental Fig. 8 panel B. Levels of ERK42/44 are normalized on GAPDH levels and ratios are expressed as arbitrary units (a.u.). All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution).
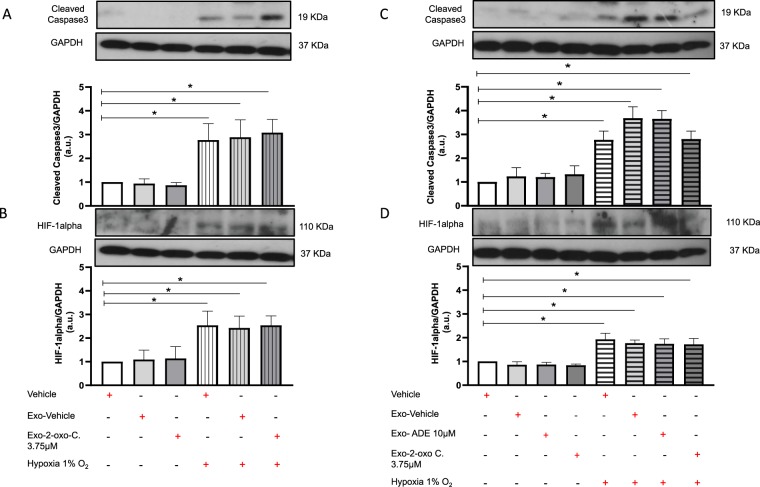
Ticagrelor-induced hCPCs exosomes attenuate the rise HIF1α levels in hypoxic cardiomyocytes
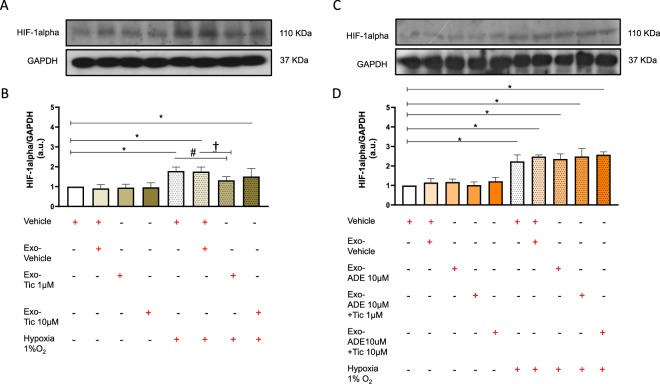
As shown in Fig. 7, long-term exposure of HL1 cardiomyocytes with defined amount of exosomes (100 μg) released from hCPCs treated with low-dose ticagrelor attenuated the rise of intracellular HIF1α levels during severe hypoxia (A-B). Conversely, similar dose of exosomes released from hCPCs co-treated with 1 μM ticagrelor and adenosine were unable to attenuate HIF1α levels in hypoxic cardiomyocytes (Fig. 7C,D).
Figure 7.
Long-term pre-treatment for 48 h of normoxic HL1 cardiomyocytes with exosomes (100 μg) derived from hCPCs treated with low-dose ticagrelor (Tic 1 μM) prevents rising of hypoxia inducible factor 1-alpha (HIF1-alpha; 110KDa MW) during severe hypoxia (1% O2), but not exosomes derived from hCPCs treated with high-dose ticagrelor (Tic 10 μM) (B). Representative images of full-length blots/gels of HIF1-alpha and glyceraldehyde 3-phosphate dehydrogenase (GAPDH; 37KDa MW) are showed in panel A. As shown in panels (D), exosomes released from hCPCs treated in the presence of adenosine (ADE, 10 μM) and EHNA (10 μM) do not reduce intracellular HIF1-alpha levels in hypoxic HL1. Representative images of full-length blots/gels of HIF1-alpha and GAPDH are showed in panel (C). Levels of HIF1-alpha are normalized on GAPDH levels and ratios are expressed as arbitrary units (a.u.). All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution); #p < 0.05 vs. hypoxia; †p < 0.05 vs. Exo-Vehicle.
P2Y12 antagonism by 2-oxo-clopidogrel does not recapitulate the ticagrelor-driven effects on release of anti-hypoxic exosomes from hCPCs
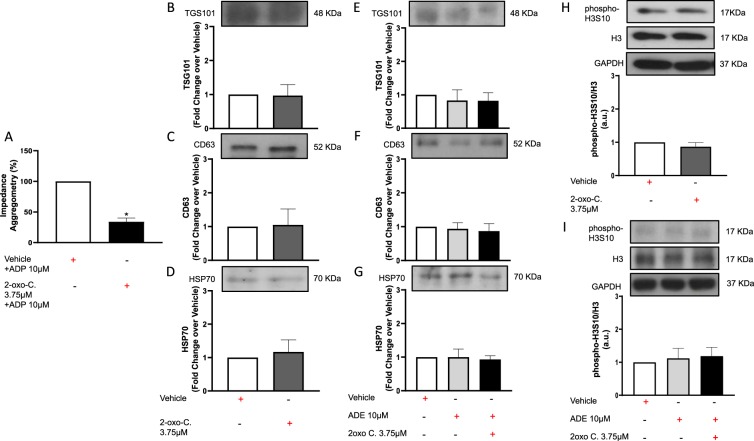
As shown in Fig. 8, anti-aggregant dose of 2-oxo-clopidogrel, established in additional experiments (A), did not increase exosome levels as assessed by expression of TSG101 (B), CD63(C) and HSP70 (D). Moreover, additional exogenous adenosine did not enhance 2-oxo-clopidogrel effects on exosome release (Fig. 8E–G). Similarly, 2-oxo-clopidogrel with or without adenosine failed to increase phospho-H3S10/H3 ratio values (Fig. 8H–I). Finally, chronic pre-treatment of HL1 cardiomyocytes with exosomes released by CPCs treated with 2-oxo-clopidogrel did not prevent hypoxia-driven rising of cleaved caspase 3 (Fig. 9A,C) nor change HIF1α levels compared to untreated cells (Fig. 9B,D).
Figure 8.
Long-term treatment for 72 h of human cardiac progenitor cells (hCPCs) with anti-aggregant dose (3.75 μM) of 2-oxo-clopidogrel (2-oxo-C) (A; in the presence of ADP 10 μM) does not recapitulate the ticagrelor-driven effects on release of TSG101 + (48KDa MW), CD63 + (52KDa MW) and heat shock protein (HSP)-70 + (70KDa MW) exosomes from hCPCs in the absence (B–D) or presence (E–G) of adenosine (ADE 10 μM) + EHNA (10 μM). Representative images of cropped densitometric bands of proteins TSG101, CD63, HSP70 are showed in each corresponding panel. The full-length blots/gels are presented in Supplemental Fig. 9 panel A. In addition, 2-oxo-C does not increase intracellular levels of phosphorylated histone H3 on Serine 10 (phospho-H3S10; 17KDa MW)/total histone H3 (H3; 17KDa MW) ratio in the absence (H) or presence (I) of adenosine (ADE 10 μM) + EHNA (10 μM). Representative images of cropped densitometric bands of proteins phospho-H3S10, H3 and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) are showed in each corresponding panel. The full-length blots/gels are presented in Supplemental Fig. 9 panel B. Levels of each analyzed protein are normalized on GAPDH (37KDa MW) levels and ratios are expressed as arbitrary units (a.u.). All measurements are mean ± SD. *p < 0.05 vs. control condition.
Figure 9.
Long-term pre-treatment for 48 h of normoxic HL1 cardiomyocytes with exosomes (100 μg) derived from hCPCs treated with anti-aggregant dose (3.75 μM) of 2-oxo-clopidogrel (2-oxo-C) does not prevent rising of cleaved caspase 3 (19KDa MW) and hypoxia inducible factor 1-alpha (HIF1-alpha; 110KDa MW) during severe hypoxia (1% O2) in the absence (A,B) or presence (C,D) of adenosine (ADE 10 μM) + EHNA (10 μM). Representative images of cropped densitometric bands of proteins cleaved caspase 3, HIF1-alpha and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) are showed in each corresponding panel. The full-length blots/gels of abovementioned proteins in absence or presence of adenosine (ADE 10 μM) + EHNA (10 μM) are presented in panel A and B of Supplemental Fig. 10 respectively. Levels of each analyzed protein are normalized on GAPDH (37KDa MW) levels and ratios are expressed as arbitrary units (a.u.). All measurements are mean ± SD. *p < 0.05 vs. untreated condition (Vehicle: sterile phosphate buffer solution).
Discussion
In the present study, we have demonstrated that long-term treatment of viable human cardiac-derived mesenchymal progenitor cells with 1 μmol ticagrelor increases the release of TGS101 + and CD63 + exosomes delivering anti-apoptotic HSP70 as consequence of increased number of viable hCPCs. Since the mean maximal total plasma concentrations after 4 weeks of ticagrelor treatment (60–90 mg bid) is 1–1.5 μmol/l30, our in vitro cell culture findings could support the development of novel clinically relevant pharmacological interventions for exosome-based cardioprotection, even suggesting a dose-dependent causal relationship with treatment.
Our data reveal an hitherto unexpected role of direct-acting P2Y12 receptor antagonist in regulating function of hCPCs, which are cells resident in human heart and potentially involved in protection of adult myocardium against ischemic injury through release of exosomes limiting cardiomyocytes apoptosis31. Although previous studies have demonstrated that chemical compounds may augment exosome release despite their toxicity32, the development of safe pharmacological approach to managing the local release of hCPCs-derived exosomes conferring pro-survival signals to hypoxic cardiomyocytes remains a desirable goal. Indeed, targeted therapies by means of compound that acts on a specific target receptor still represent an attractive perspective in cardioprotection. Since P2Y12 belongs to the family of G-protein coupled receptors, which signaling may trigger exosome release from adult mature cells33, we tested, for the first time, the regulatory role of ticagrelor, a cardioprotective inverse agonist of the P2Y12 receptor34, on exosome-mediated paracrine effects of explant-derived hCPCs. Like human hematopoietic stem/progenitor cells27 and vascular smooth muscle cells, we have demonstrated that P2Y12 receptors are also expressed in hCPCs.
Significantly, long-term treatment of hCPCs with clinically relevant dose of ticagrelor increases levels of TGS101 + , CD63 + and HSP70 + exosomes in culture medium. Of importance, this effect is not observed during treatment with higher dose of ticagrelor. Since exosome levels in culture medium depend on cell viability and densities35, we assessed dose-dependent effects of ticagrelor on viability and proliferation of cultured normoxic hCPCs. Interestingly, long-term treatment for 72 h with only 1μmol ticagrelor increases the number of viable hCPCs and the magnitude of phospho-H3S10/H3 ratio, an established hallmark of progenitor cells proliferation36. Like exosome levels, ten-fold higher dose of ticagrelor does not affect cell viability and proliferation. Our data exclude dose-dependent toxicity of the drug and reveal a positive relationship between extracellular exosome levels and magnitude of mitotic activity of human explant-derived cardiac stromal cells during ticagrelor treatment in vitro. These findings are well supported by previous clinical study showing an increased number of circulating endothelial progenitor cells in patients with acute coronary syndrome treated with ticagrelor37. In order to assess underlying mechanisms, we first investigated the role played by adenosine, an established mediator of ticagrelor effects.
Although it is known that some exosomes may increase proliferation of non-tumoral cells through autocrine vicious cycle38, it is conceivable that rising of exosome levels related to higher cell proliferation rate might be mediated by ticagrelor-induced adenosine. Although cultured normoxic cells at resting conditions release adenosine in the nanomolar range39, P2Y12 antagonism by ticagrelor may increase extracellular adenosine levels due to both dose-dependent ATP release40 and inhibition of the equilibrative nucleoside transporter 1 (ENT1)41, an adenosine transporter even expressed in different types of progenitor cells42,43. Therefore, extracellular adenosine amount following treatment with clinically relevant dose of ticagrelor might be enough to induce hCPCs proliferation through activation of high-affinity adenosine receptors, such as A1 and A2A. Indeed, activation of A1 and A2A adenosine receptor promotes neural progenitor cells proliferation44. Conversely, exposure of cells to ten-fold higher dose of ticagrelor further increases extracellular adenosine levels19 and activates A2B45, a low-affinity adenosine receptor even expressed by cardiac mesenchymal stem-like cells46 that arrest cell cycle46. In order to highlight the dose-dependent role of adenosine as mediator of ticagrelor effects, we have also performed further experiments by adding exogenous adenosine. Indeed, the effects of low-dose ticagrelor on exosome release and cell proliferation are counteracted by co-treatment with higher dose of exogenous adenosine and EHNA, a potent inhibitor of extracellular adenosine deaminase47 that prevents adenosine degradation. Of note, the evidence that high concentration of adenosine per se does not prompt rising of exosome levels in the culture medium and cell proliferation further support the regulatory role played by ticagrelor-induced adenosine at lower rather than higher dose.
Lower extracellular adenosine levels, through its A2A receptor, can activate tyrosine kinases and influence several signaling pathways involved in cell proliferation including the PI3-kinase/Akt pathway and the ERK/MAPK pathways48, whose activation induces histone H3 phosphorylation at serine 1049. However, similar activation of the MAPK signaling pathway can also increase the number of exosomes released per cell50. To investigate the downstream pathways involved in ENT1-dependent activation of A2A receptor, we have pre-treated explant-derived hCPCs with nontoxic dose of SNS314 mesylate, an inhibitor of histone H3 phosphorylation at serine 10 through inhibition of Aurora kinases that are downstream MAPK51. Interestingly, the subsequent treatment of these cells with clinically relevant dose of ticagrelor fails to increase proliferation rate and exosome concentration is similar to control cells. Therefore, we suggest that A2A-dependent effects of ticagrelor on exosome release are mainly due to regulation of histone H3 phosphorylation at serine 10.
Given that lack of ENT1 is cardioprotective52, it may play a key role in modulating A2A-dependent effects of ticagrelor on mitotic activity of hCPCs and exosome release. For this purpose, we have performed additional experiments by treating hCPCs with anti-aggregant nontoxic dose of 2-oxo-clopidogrel, an irreversible P2Y12 antagonist that does not activate ENT141. Interestingly, 2-oxo-clopidogrel does not increase levels of extracellular exosome levels and histone H3 phosphorylation at serine 10, even in the presence of exogenous adenosine and EHNA. Thus, our data suggest that inhibition of ENT1 is required to mediate ticagrelor effects.
It is well established that hCPCs-derived exosomes exert anti-apoptotic effects in vitro on cardiomyocytes undergoing starvation21 or treated with pro-apoptotic staurosporine23, as well in rodent model of myocardial infarction21–23,52. However, their anti-hypoxic effects have never been addressed. In fact, the intensity and severity of hypoxic stress promote cell injury through different regulatory mechanisms compared to those induced by glucose or serum deprivation53. Given the emerging interest in testing the effect of conventional cardiovascular drugs on the cardioprotective potential of exosomes derived from stem/progenitor cells54, we have assessed the role of ticagrelor-induced hCPCs-derived exosomes in increasing resistance of cardiomyocytes to severe hypoxia. We found, for the first time, that exosomes released from auricle-derived hCPCs treated with low-dose ticagrelor attenuates hypoxia-induced caspase-3 activation in HL1 cardiomyocytes. Since anti-apoptotic effects of hCPCs-derived exosomes are dose-dependent21, similar dose of hCPCs-derived exosomes released in other experimental conditions is not effective in preventing hypoxia-induced apoptosis at least in our in vitro setting.
The present results highlight the new role of ticagrelor in enhancing anti-hypoxic properties of hCPCs-derived exosomes. Greater anti-hypoxic effects of exosomes induced by low-dose ticagrelor might be related to HSP70, a well-known inducible protein that protects against hypoxia-induced apoptosis55. Although ticagrelor does not increase HSP70 expression of hCPCs, it is plausible that ticagrelor may expose cardiomyocytes to extracellular milieu rich of exosomal HSP70 released from resident hCPCs.
Exosomal HSP70 is essential to protect adult cardiomyocytes through rapid ERK42/44 phosphorylation56 and its activity depends on the microenvironment surrounding cell source. Indeed, rodent and human exosomes released under hyperglycemic conditions show either lower HSP70 levels or HSP70 inactivated by non-enzymatic glycosylation that are unable to prevent apoptosis of cardiomyocytes after hypoxia and re-oxygenation57. In our in vitro model, ERK42/44 phosphorylation is rapidly increased after 5 min of exposure of HL1 to exosomes derived from hCPCs treated with clinically relevant dose of ticagrelor. Conversely, there was no significant increase in ERK42/44 phosphorylation after treatment with similar dose of exosomes released in other experimental conditions. In order to further support the exosome-based anti-hypoxic effect, we measured cardiomyocyte HIF1α levels, a transcription factor activated by low oxygen concentrations, which expression is downregulated when hypoxia-induced oxidative stress and cardiomyocyte apoptosis are attenuated by other agents58. In our experimental setting, HIF1α levels were significantly lower in viable HL1 cardiomyocytes pre-treated with exosomes, released after treatment of hCPCs with low-dose ticagrelor, and then exposed to severe hypoxia. Our results are in line with previous study showing that intracellular enrichment of HSP70 inhibits the expression of HIF1α by protecting hypoxic cells59. Indeed, hCPCs-derived exosomes are effectively internalized by cardiomyocytes21–23,26.
Limitations of the study
In our study we did not performed analytical approach for analyzing the cargo of single hCPC-derived exosome in each experimental condition in order to evaluate the effects of clinically relevant dose of ticagrelor on exosomal content. Although pro-survival effects of HSP70 are supported by the present results and by others56, we cannot exclude that other proteins may synergize the anti-hypoxic effects of ticagrelor-induced exosomes. Despite our limited understanding of cardiac-derived mesenchymal progenitor cells function in vivo in terms of cardiac regeneration, these cells reside in human heart23,26 and may be a potential target of ticagrelor in mediating exosome-based cardiomyocyte protection. However, further experiments should be performed in an in vivo setting in order to confirm our in vitro results supporting wide evidence of ticagrelor-induced cardioprotection.
Conclusions
To the best of our knowledge, this is the first evidence demonstrating that clinically relevant dose of ticagrelor acts on human cardiac-derived mesenchymal progenitor cells safely increasing the release of anti-hypoxic exosomes. This effect is achieved through the simultaneous rising of proliferation rate of viable hCPCs, which requires ENT1 activation and is counteracted by higher dose of adenosine. Ticagrelor-induced exosomes early activate pro-survival protein kinase signaling pathways including ERK42/44 by protecting hypoxic cardiomyocytes. Our results assume clinical significance in the development of new noninvasive pharmacological approach to enhance endogenous exosome-based anti-hypoxic response and protect heart at risk for developing myocardial ischemic injury.
Methods
Chemicals
Ticagrelor (Tic) was kindly provided by AstraZeneca (Mölndal, Sweden). Adenosine (ADE), a purine nucleoside mainly derived from the metabolism of ADP or adenosine triphosphate after myocardial damage60, and erythro-9- (2-hydroxy-3-nonyl) adenine (EHNA) hydrochloride, a potent adenosine deaminase inhibitor47, were purchased from Sigma-Aldrich Chemical Co (Missouri, USA). 2-oxo-clopidogrel, a key intermediate metabolite from which the active metabolite of clopidogrel is rapidly formed via oxidation61, was purchased from Santa Cruz Biotechnology (CA, USA). SNS314 mesylate, an ATP-competitive and selective pan-Aurora kinase inhibitor leading to inhibition phosphorylation of histone H3 at serine 1051, was purchased from Cayman Chemical (Michigan, USA).
Cell Lines
hCPCs were isolated from the right atrial appendage of adult non-diabetic patients (n = 5; M/F = 3/2; mean age, 71.2 ± 7.82 years) with normal LV ejection fraction (56.6 ± 9.5%) undergoing open-heart surgery for coronary artery bypass grafting alone (n = 3) or combined to heart valve surgery (n = 2) as previously described by us21,23. Protocols used in this study to isolate hCPCs were approved by Ethical Committee for Clinical Research of Ticino Canton, Switzerland (Rif. CE 2923) and performed according to the Declaration of Helsinki. All patients gave written informed consent to the collection of atrial specimen. hCPCs were growth in Iscove’s Modified Dulbecco’s Medium (IMDM, Sigma-Aldrich Chemical Co, Missouri, USA) supplemented with 20% exosome-depleted fetal bovine serum (FBS), L-glutamine (Sigma-Aldrich Chemical Co, Missouri, USA) and antibiotics.
Murine HL-1 cardiomyocytes (a kind gift of Professor W. Claycomb, Department of Biochemistry and Molecular Biology, LSUHSC, New Orleans, LA, USA), a cell line used to study cardiomyocytes structure and function62 and exosomes effects21,23, were cultured in Claycomb Medium (Sigma-Aldrich Chemical Co, MO, USA) supplemented with 10% exosomes-depleted FBS, antibiotics, L-glutamine, and 100 μM norepinephrine (Sigma-Aldrich Chemical Co, MO, USA). All assays were conducted using low cell passage cells (2–5 passages).
Flow cytometry
Surface markers expressed on explant-derived hCPCs were analyzed by flow cytometry. Phycoerythrin (PE)-conjugated antibodies against surface markers expressed on cardiac mesenchymal stromal cells (CD90, CD105, CD73, CD45, CD117; all from Beckman Coulter) were used. Beads incubated with an antibody in the absence of cells served as a control. Analyses were performed on a MACS-Quant flow cytometer (Miltenyi Biotec).
Experimental protocol
hCPCs, seeded at density of 5 × 105, were treated for 72 h with sterile phosphate buffer solution (PBS), non-cytotoxic increasing doses of ticagrelor (1 or 10 μM) or 2-oxo-clopidogrel (3.75 μM) when they reached about 80% confluence. Each chemical compound was added to IMDM medium supplemented with exosome-depleted FBS, L-glutamine and antibiotics at 37 °C in humidified air with 5% CO2. All experiments were performed with or without exogenous adenosine (10 μM) + EHNA (10 μM) or SNS314 mesylate (10 μM). At the end of each experimental treatment, culture medium was collected and exosomes were isolated as previously described by us21,23. Exosome pellets were suspended in PBS, aliquoted and stored at −80 °C until further use. Exosome concentrations were assessed using Western blot assay to measure TGS101, CD63 and HSP70 protein levels, well-established exosomes markers63, and by NanoSight technology (NanoSight LM10, Malvern Instrument, Amesbury, UK) as previously described by us21,23.
MTT cell viability assay
After each pharmacological treatment, the cell viability was assessed using the 3-(4,5-dimethylthiazolyl-2)-2,5-diphenyltetrazolium bromide (MTT) reduction assay (Sigma-Aldrich Chemical Co, MO, USA) according to the manufacturer’s instructions. All measurements were performed in triplicate.
Trypan blue assay and hemocytometer cell count
Trypan blue dye exclusion test by staining cells with 0.2% Trypan blue solution (Sigma-Aldrich Chemical Co, MO, USA) was performed to reveal necrotic cells after each experimental condition according to the manufacturer’s instructions. Moreover, unstained viable cells were manually counted using a hemocytometer. Counts were performed by triplicate under a 10X objective according to standard methodology64. All measurements were performed in triplicate.
Apoptosis assay of HL-1 cardiomyocytes
HL-1 cardiomyocytes were seeded at a density of 6 × 104/well in six-well culture dishes and allowed to reach ~80% confluence. Cells were pre-treated for 48 h with hCPC-exosomes (100 μg) isolated from culture medium as previously reported by us21. HL-1 cells treated with different hCPC-exosomes were randomly exposed for 24 h to severe hypoxia (1–2% O2) using a hypoxia incubator chamber (STEMCELL Technologies Inc., Canada), a well-established model of cardiomyocytes damage following myocardial infarction27, or to normoxia (21%O2) as control condition. Detection of TUNEL staining by fluorescence microscopy (in situ cell death detection kit, Roche Diagnostic Corporation, Indianapolis, IN, USA)65 and measurement of cleaved caspase-3 levels by Western blot assay66 were performed to evaluate the magnitude of hypoxia-induced apoptosis of HL-1 cardiomyocytes. All measurements were performed in triplicate.
Western blot assay
hCPCs-exosomes, CPCs and HL-1 pellets were homogenized at 4 °C in RIPA buffer containing protease and phosphatase inhibitors (Pierce, Rockford, USA). Homogenates were centrifuged at 12,000 g for 15 minutes at 4 °C to remove nuclei and cell debris. Protein concentration in supernatant was determined using BCA protein assay kit (Pierce, Rockford, USA). Equal amounts of protein were fractionated by 8–15% SDS polyacrylamide gel and transferred to nitrocellulose membrane (Bio-Rad Laboratories Inc., CA, USA). Equal loading was controlled by Ponceau staining. Membranes were blocked with 5% nonfat dried milk in TBS/Tween20 (0,01%) at room temperature for 1 hour, and then probed with primary antibodies at a predetermined concentration at 4 °C overnight. Primary antibodies were used to detect: (1) human CD63 (polyclonal antibody, 1:1000; #SAB4301607, Sigma-Aldrich Chemical Co, MO, USA) and human TGS101 (polyclonal antibody, 1:1000; #T5701, Sigma-Aldrich Chemical Co, MO, USA) which are established exosomal markers63; (2) human heat shock protein 70 (HSP70) (polyclonal antibody, 1:1000; #ADI-SPA-812F, Enzo Life Sciences, NYC, USA), an antiapoptotic protein even used as exosomal marker56; (3) human P2Y12 on surface of CPCs (polyclonal antibody, 1:1000; #SC27152, Santa Cruz Biotechnology Inc., USA); (4) human phosphorylated Histone H3 on Serine 10 (phospho-H3S10) (polyclonal antibody, 1:1000; #9701 S, Cell Signaling, Danvers, MA) and human histone H3 (H3) (monoclonal antibody, 1:1000; #4499 S, Cell Signaling, Danvers, MA), which ratio is an established hallmark of cell proliferation36; (5) murine cleaved caspase-3 (polyclonal antibody, 1:1000; #SC7148, Santa Cruz Biotechnology Inc., USA), a marker of cell apoptosis66; (6) murine phospho-ERK42/44 (polyclonal antibody, 1:1000; #SC23759, Santa Cruz Biotechnology Inc., USA) and murine ERK42/44 (polyclonal antibody, 1:2000; #SC94, Santa Cruz Biotechnology Inc., USA) in HL-1 cells, which ratio is an established hallmark of exosome-mediated pro-survival pathway23,56; (7) murine hypoxia inducible factor 1-alpha (HIF1α; monoclonal antibody, 1:1000; #ab179483, Abcam, UK), a transcription factor activated by low oxygen concentrations67; (8) glyceraldehyde 3-phosphate dehydrogenase (GAPDH; monoclonal antibody, 1:3000; #G8795, Sigma-Aldrich Chemical Co, MO, USA) as loading control for protein normalization. After incubation with the above-mentioned primary antibodies, and rinsing with TBS/Tween20 (0.01%) 3 times for 10 min, membranes were incubated with appropriate horseradish peroxidase-conjugated (HRP-conjugated) anti-rabbit (#A0545), anti-goat (#A5420) or anti-mouse (#A9044) secondary antibodies (Sigma-Aldrich Chemical Co, MO, USA) for 1 hour at room temperature. After incubation with the specific secondary antibodies, membranes were washed 3 times for 10 minutes with TBS/Tween20 (0.01%). Specific protein bands were detected using ECL Plus Western Blotting Detection System (Pierce, Rockford, USA). Densitometry analysis of protein bands was performed using ImageJ software (National Institute of Health, USA). All measurements were performed in triplicate.
Platelet aggregometry assay
Impedance aggregometry was performed with an optical aggregation system (CHRONO-LOG series 590, Havertown, PA), equipped with an infrared light beam and the AGGRO/LINK software68. Human whole blood sample (500 μl) was diluted 50:50 in 0.9% saline solution and heated for 5 min at 37 °C while stirring. After baseline measurement, platelet aggregation was evaluated after adding ADP (10 μM) in presence or absence of 2-oxo-clopidogrel (3.75 μM). The increase of impedance was recorded for 10 min. All measurements were performed in triplicate.
Statistical analysis
All results are presented as mean ± standard deviation (SD). Statistical comparisons were made by analysis of variance (ANOVA) and Bonferroni test was used as the post-hoc test. Value p < 0.05 was considered statistically significant using GraphPad PRISM software (GraphPad Software Inc., San Diego, California).
Supplementary information
Acknowledgements
We thank Drs. Angelo Ferraro and Sven Nylander of AstraZeneca, and Dr. Tiziano Torre of Cardiocentro Ticino Foundation for their helpful technical support.
Author contributions
E.P. and V.L. contributed to the study concept and design. R.F.-D. contributed to drug substance manufacturing. V.C., A.P. and L.B. contributed to data acquisition. M.M. performed the statistical analyses. All authors critically revised the manuscript and approved the submitted version.
Competing interests
This study was funded by AstraZeneca and in part by institutional funds of Scuola Superiore Sant’Anna (V.L.). R.F.-D. is employee of AstraZeneca and may own stock or stock options.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-020-59225-7.
References
- 1.Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017;389:197–210. doi: 10.1016/S0140-6736(16)30677-8. [DOI] [PubMed] [Google Scholar]
- 2.Araszkiewicz A, et al. Effect of impaired myocardial reperfusion on left ventricular remodeling in patients with anterior wall acute myocardial infarction treated with primary coronary intervention. Am. J. Cardiol. 2006;98:725–728. doi: 10.1016/j.amjcard.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Lionetti V, Bianchi G, Recchia FA, Ventura C. Control of autocrine and paracrine myocardial signals: an emerging therapeutic strategy in heart failure. Heart Fail. Rev. 2010;15:531–542. doi: 10.1007/s10741-010-9165-7. [DOI] [PubMed] [Google Scholar]
- 4.Vilahur G, et al. Protective Effects of Ticagrelor on Myocardial Injury After Infarction. Circulation. 2016;134:1708–1719. doi: 10.1161/CIRCULATIONAHA.116.024014. [DOI] [PubMed] [Google Scholar]
- 5.Vilahur G, et al. P2Y12 antagonists and cardiac repair post-myocardial infarction: global and regional heart function analysis and molecular assessments in pigs. Cardiovasc. Res. 2018;114:1860–1870. doi: 10.1093/cvr/cvy201. [DOI] [PubMed] [Google Scholar]
- 6.Audia JP, et al. Caspase-1 inhibition by VX-765 administered at reperfusion in P2Y12 receptor antagonist-treated rats provides long-term reduction in myocardial infarct size and preservation of ventricular function. Basic Res. Cardiol. 2018;113:32. doi: 10.1007/s00395-018-0692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ye Y, et al. Ticagrelor protects the heart against reperfusion injury and improves remodeling after myocardial infarction. Arterioscler. Thromb. Vasc. Biol. 2015;35:1805–1814. doi: 10.1161/ATVBAHA.115.305655. [DOI] [PubMed] [Google Scholar]
- 8.Nanhwan MK, et al. Chronic treatment with ticagrelor limits myocardial infarct size: an adenosine and cyclooxygenase-2-dependent effect. Arterioscler. Thromb. Vasc. Biol. 2014;34:2078–2085. doi: 10.1161/ATVBAHA.114.304002. [DOI] [PubMed] [Google Scholar]
- 9.Bansilal S, et al. Ticagrelor for Secondary Prevention of Atherothrombotic Events in Patients With Multivessel Coronary Disease. J. Am. Coll. Cardiol. 2018;71:489–496. doi: 10.1016/j.jacc.2017.11.050. [DOI] [PubMed] [Google Scholar]
- 10.Khan, J.N. et al. Infarct Size Following Treatment With Second- Versus Third-Generation P2Y12 Antagonists in Patients With Multivessel Coronary Disease at ST-Segment Elevation Myocardial Infarction in the CvLPRIT Study. J. Am. Heart Assoc. 5, 10.1161/JAHA.116.003403 (2016). [DOI] [PMC free article] [PubMed]
- 11.Bonaca MP, et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N. Engl. J. Med. 2015;372:1791–800. doi: 10.1056/NEJMoa1500857. [DOI] [PubMed] [Google Scholar]
- 12.Roubille F, et al. Cardioprotection by clopidogrel in acute ST-elevated myocardial infarction patients: a retrospective analysis. Basic Res. Cardiol. 2012;107:275. doi: 10.1007/s00395-012-0275-3. [DOI] [PubMed] [Google Scholar]
- 13.Wallentin L, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 14.Cannon CP, et al. Comparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomised double-blind study. Lancet. 2010;375:283–293. doi: 10.1016/S0140-6736(09)62191-7. [DOI] [PubMed] [Google Scholar]
- 15.Findik O, et al. Ticagrelor Attenuates Apoptosis of Lung and Myocardial Cells Induced by Abdominal Aorta Ischemia/Reperfusion. In Vivo. 2016;30:243–249. [PubMed] [Google Scholar]
- 16.Cattaneo M, Schulz R, Nylander S. Adenosine-mediated effects of ticagrelor: evidence and potential clinical relevance. J. Am. Coll. Cardiol. 2014;63:2503–2509. doi: 10.1016/j.jacc.2014.03.031. [DOI] [PubMed] [Google Scholar]
- 17.van den Berg TN, et al. Ticagrelor Does Not Inhibit Adenosine Transport at Relevant Concentrations: A Randomized Cross-Over Study in Healthy Subjects In Vivo. PLoS One. 2015;10:e0137560. doi: 10.1371/journal.pone.0137560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Löfgren L, Pehrsson S, Hägglund G, Tjellström H, Nylander S. Accurate measurement of endogenous adenosine in human blood. PLoS One. 2018;13:e0205707. doi: 10.1371/journal.pone.0205707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang XM, et al. Ticagrelor Does Not Protect Isolated Rat Hearts, Thus Clouding Its Proposed Cardioprotective Role Through ENT 1 in Heart Tissue. J. Cardiovasc. Pharmacol. Ther. 2019;24:371–376. doi: 10.1177/1074248419829169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mauretti A, Spaans S, Bax NAM, Sahlgren C, Bouten CVC. Cardiac Progenitor Cells and the Interplay with Their Microenvironment. Stem Cells Int. 2017;2017:7471582. doi: 10.1155/2017/7471582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barile L, et al. Extracellular vesicles from human cardiac progenitor cells inhibit cardiomyocyte apoptosis and improve cardiac function after myocardial infarction. Cardiovasc. Res. 2014;103:530–541. doi: 10.1093/cvr/cvu167. [DOI] [PubMed] [Google Scholar]
- 22.Ibrahim AG, Cheng K, Marbán E. Exosomes as critical agents of cardiac regeneration triggered by cell therapy. Stem Cell Reports. 2014;2:606–619. doi: 10.1016/j.stemcr.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barile L, et al. Cardioprotection by cardiac progenitor cell-secreted exosomes: role of pregnancy-associated plasma protein-A. Cardiovasc. Res. 2018;114:992–1005. doi: 10.1093/cvr/cvy055. [DOI] [PubMed] [Google Scholar]
- 24.Gray WD, et al. Identification of therapeutic covariant microRNA clusters in hypoxia-treated cardiac progenitor cell exosomes using systems biology. Circ. Res. 2015;116:255–263. doi: 10.1161/CIRCRESAHA.116.304360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gasecka, A. et al. P2Y12 antagonist ticagrelor inhibits the release of procoagulant extracellular vesicles from activated platelets: Preliminary results. Cardiol. J. (In press) 19 Apr 2018. [DOI] [PMC free article] [PubMed]
- 26.Saha Progyaparamita, Sharma Sudhish, Korutla Laxminarayana, Datla Srinivasa Raju, Shoja-Taheri Farnaz, Mishra Rachana, Bigham Grace E., Sarkar Malini, Morales David, Bittle Gregory, Gunasekaran Muthukumar, Ambastha Chetan, Arfat Mir Yasir, Li Deqiang, Habertheuer Andreas, Hu Robert, Platt Manu O., Yang Peixin, Davis Michael E., Vallabhajosyula Prashanth, Kaushal Sunjay. Circulating exosomes derived from transplanted progenitor cells aid the functional recovery of ischemic myocardium. Science Translational Medicine. 2019;11(493):eaau1168. doi: 10.1126/scitranslmed.aau1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang L, Jacobsen SE, Bengtsson A, Erlinge D. P2 receptor mRNA expression profiles in human lymphocytes, monocytes and CD34+ stem and progenitor cells. BMC Immunol. 2004;5:16. doi: 10.1186/1471-2172-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiong H, et al. Up-regulation of miR-138 inhibits hypoxia-induced cardiomyocyte apoptosis via down-regulating lipocalin-2 expression. Exp. Biol. Med. (Maywood) 2016;241:25–30. doi: 10.1177/1535370215591831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Théry C, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nylander S, et al. Ticagrelor inhibits human platelet aggregation via adenosine in addition to P2Y12 antagonism. J. Thromb. Haemost. 2013;11:1867–1876. doi: 10.1111/jth.12360. [DOI] [PubMed] [Google Scholar]
- 31.Barile L, Moccetti T, Marbán E, Vassalli G. Roles of exosomes in cardioprotection. Eur. Heart J. 2017;38:1372–1379. doi: 10.1093/eurheartj/ehw304. [DOI] [PubMed] [Google Scholar]
- 32.Savina A, Furlán M, Vidal M, Colombo MI. Exosome release is regulated by a calcium-dependent mechanism in K562 cells. J. Biol. Chem. 2003;278:20083–20090. doi: 10.1074/jbc.M301642200. [DOI] [PubMed] [Google Scholar]
- 33.Verweij FJ, et al. Quantifying exosome secretion from single cells reveals a modulatory role for GPCR signaling. J. Cell. Biol. 2018;217:1129–1142. doi: 10.1083/jcb.201703206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aungraheeta R, et al. Inverse agonism at the P2Y12 receptor and ENT1 transporter blockade contribute to platelet inhibition by ticagrelor. Blood. 2016;128:2717–2728. doi: 10.1182/blood-2016-03-707844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel DB, et al. Impact of cell culture parameters on production and vascularization bioactivity of mesenchymal stem cell-derived extracellular vesicles. Bioeng. Transl. Med. 2017;2:170–179. doi: 10.1002/btm2.10065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oh H, et al. Cardiac progenitor cells from adult myocardium: homing, differentiation, and fusion after infarction. Proc. Natl. Acad. Sci. USA. 2003;100:12313–12318. doi: 10.1073/pnas.2132126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bonello L, et al. Ticagrelor increases endothelial progenitor cell level compared to clopidogrel in acute coronary syndromes: A prospective randomized study. Int. J. Cardiol. 2015;187:502–507. doi: 10.1016/j.ijcard.2015.03.414. [DOI] [PubMed] [Google Scholar]
- 38.Zhang M, et al. Exosomal 15-LO2 mediates hypoxia-induced pulmonary artery hypertension in vivo and in vitro. Cell Death Dis. 2018;9:1022. doi: 10.1038/s41419-018-1073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Helenius M, Jalkanen S, Yegutkin G. Enzyme-coupled assays for simultaneous detection of nanomolar ATP, ADP, AMP, adenosine, inosine and pyrophosphate concentrations in extracellular fluids. Biochim. Biophys. Acta. 2012;1823:1967–1975. doi: 10.1016/j.bbamcr.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 40.Ohman J, Kudira R, Albinsson S, Olde B, Erlinge D. Ticagrelor induces adenosine triphosphate release from human red blood cells. Biochem. Biophys. Res. Commun. 2012;418:754–758. doi: 10.1016/j.bbrc.2012.01.093. [DOI] [PubMed] [Google Scholar]
- 41.Armstrong D, et al. Characterization of the adenosine pharmacology of ticagrelor reveals therapeutically relevant inhibition of equilibrative nucleoside transporter 1. J. Cardiovasc. Pharmacol. Ther. 2014;19:209–219. doi: 10.1177/1074248413511693. [DOI] [PubMed] [Google Scholar]
- 42.Ezura Y, Lin X, Hatta A, Izu Y, Noda M. Interleukin-1β Suppresses the Transporter Genes Ank and Ent1 Expression in Stromal Progenitor Cells Retaining Mineralization. Calcif. Tissue Int. 2016;99:199–208. doi: 10.1007/s00223-016-0139-1. [DOI] [PubMed] [Google Scholar]
- 43.Guzmán-Gutiérrez E, et al. Differential expression of functional nucleoside transporters in non-differentiated and differentiated human endothelial progenitor cells. Placenta. 2010;31:928–936. doi: 10.1016/j.placenta.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 44.Lv J, Shao Y, Gao Y. Activation of A1 and A2a adenosine receptors promotes neural progenitor cell proliferation. Brain Res. 2018;1686:65–71. doi: 10.1016/j.brainres.2018.02.028. [DOI] [PubMed] [Google Scholar]
- 45.Carroll SH, et al. A2B adenosine receptor promotes mesenchymal stem cell differentiation to osteoblasts and bone formation in vivo. J. Biol. Chem. 2012;287:15718–15727. doi: 10.1074/jbc.M112.344994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryzhov S, et al. Role of adenosine A2B receptor signaling in contribution of cardiac mesenchymal stem-like cells to myocardial scar formation. Purinergic Signal. 2014;10:477–486. doi: 10.1007/s11302-014-9410-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pragnacharyulu PV, Varkhedkar V, Curtis MA, Chang IF, Abushanab E. Adenosine deaminase inhibitors: synthesis and biological evaluation of unsaturated, aromatic, and oxo derivatives of (+)-erythro-9-(2′S-hydroxy-3′R-nonyl)adenine [(+)-EHNA] J. Med. Chem. 2000;43:4694–4700. doi: 10.1021/jm0002533. [DOI] [PubMed] [Google Scholar]
- 48.Ahmad A, Schaack JB, White CW, Ahmad S. Adenosine A2A receptor-dependent proliferation of pulmonary endothelial cells is mediated through calcium mobilization, PI3-kinase and ERK1/2 pathways. Biochem. Biophys. Res. Commun. 2013;434:566–571. doi: 10.1016/j.bbrc.2013.03.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Drobic B, Pérez-Cadahía B, Yu J, Kung SK, Davie JR. Promoter chromatin remodeling of immediate-early genes is mediated through H3 phosphorylation at either serine 28 or 10 by the MSK1 multi-protein complex. Nucleic Acids Res. 2010;38:3196–3208. doi: 10.1093/nar/gkq030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Agarwal K, et al. Analysis of exosome release as a cellular response to MAPK pathway inhibition. Langmuir. 2015;31:5440–5448. doi: 10.1021/acs.langmuir.5b00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arbitrario JP, et al. SNS-314, a pan-Aurora kinase inhibitor, shows potent anti-tumor activity and dosing flexibility in vivo. Cancer Chemother. Pharmacol. 2010;65:707–717. doi: 10.1007/s00280-009-1076-8. [DOI] [PubMed] [Google Scholar]
- 52.Rose JB, et al. Equilibrative nucleoside transporter 1 plays an essential role in cardioprotection. Am. J. Physiol. Heart Circ. Physiol. 2010;298:H771–777. doi: 10.1152/ajpheart.00711.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kacimi R, Chentoufi J, Honbo N, Long CS, Karliner JS. Hypoxia differentially regulates stress proteins in cultured cardiomyocytes: role of the p38 stress-activated kinase signaling cascade, and relation to cytoprotection. Cardiovasc. Res. 2000;46:139–150. doi: 10.1016/S0008-6363(00)00007-9. [DOI] [PubMed] [Google Scholar]
- 54.Huang, P. et al. Atorvastatin Enhances the Therapeutic Efficacy of Mesenchymal Stem Cells Derived Exosomes in Acute Myocardial Infarction via Up-regulating Long Non-coding RNA H19. Cardiovasc. Res. 2019 May 22. pii: cvz139 (In Press). [DOI] [PMC free article] [PubMed]
- 55.Chang W, et al. Mesenchymal stem cells pretreated with delivered Hph-1-Hsp70 protein are protected from hypoxia-mediated cell death and rescue heart functions from myocardial injury. Stem Cells. 2009;27:2283–2292. doi: 10.1002/stem.153. [DOI] [PubMed] [Google Scholar]
- 56.Vicencio JM, et al. Plasma exosomes protect the myocardium from ischemia-reperfusion injury. J. Am. Coll. Cardiol. 2015;65:1525–1536. doi: 10.1016/j.jacc.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 57.Davidson SM, et al. Cardioprotection mediated by exosomes is impaired in the setting of type II diabetes but can be rescued by the use of non-diabetic exosomes in vitro. J. Cell. Mol. Med. 2018;22:141–151. doi: 10.1111/jcmm.13302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yu B, Meng F, Yang Y, Liu D, Shi K. NOX2 Antisense Attenuates Hypoxia-Induced Oxidative Stress and Apoptosis in Cardiomyocyte. Int. J. Med. Sci. 2016;13:646–652. doi: 10.7150/ijms.15177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Luo W, et al. Hsp70 and CHIP selectively mediate ubiquitination and degradation of hypoxia-inducible factor (HIF)-1alpha but Not HIF-2alpha. J. Biol. Chem. 2010;285:3651–3663. doi: 10.1074/jbc.M109.068577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Headrick JP, Lasley RD. Adenosine receptors and reperfusion injury of the heart. Handb. Exp. Pharmacol. 2009;193:189–214. doi: 10.1007/978-3-540-89615-9_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Floyd JS, et al. A screening study of drug-drug interactions in cerivastatin users: an adverse effect of clopidogrel. Clin. Pharmacol. Ther. 2012;91:896–904. doi: 10.1038/clpt.2011.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.White SM, Constantin PE, Claycomb WC. Cardiac physiology at the cellular level: use of cultured HL-1 cardiomyocytes for studies of cardiac muscle cell structure and function. Am. J. Physiol. Heart Circ. Physiol. 2004;286:H823–829. doi: 10.1152/ajpheart.00986.2003. [DOI] [PubMed] [Google Scholar]
- 63.Terrasini N, Lionetti V. Exosomes in Critical Illness. Crit. Care Med. 2017;45:1054–1060. doi: 10.1097/CCM.0000000000002328. [DOI] [PubMed] [Google Scholar]
- 64.Louis, K. S., Siegel, A. C. & Levy, G. A. Comparison of manual versus automated trypan blue dye exclusion method for cell counting. In: Stoddart, M.J., editor. Mammalian Cell Viability: Methods and Protocols. Series Methods in Molecular Biology. Springer Protocols; New York: 7–12 (2011).
- 65.Agostini S, et al. A new dual-promoter system for cardiomyocyte-specific conditional induction of apoptosis. Biomed Res. Int. 2013;2013:845816. doi: 10.1155/2013/845816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jamnicki-Abegg M, et al. Isoflurane inhibits cardiac myocyte apoptosis during oxidative and inflammatory stress by activating Akt and enhancing Bcl-2 expression. Anesthesiology. 2005;103:1006–1014. doi: 10.1097/00000542-200511000-00015. [DOI] [PubMed] [Google Scholar]
- 67.Salceda S, Caro J. Hypoxia-inducible factor 1alpha (HIF-1alpha) protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J. Biol. Chem. 1997;272:22642–22647. doi: 10.1074/jbc.272.36.22642. [DOI] [PubMed] [Google Scholar]
- 68.Ivandic BT, et al. Determination of clopidogrel resistance by whole blood platelet aggregometry and inhibitors of the P2Y12 receptor. Clin. Chem. 2006;52:383–388. doi: 10.1373/clinchem.2005.059535. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.