Abstract
This study examined prevalence of childhood overweight and obesity (ov/ob) and central obesity in five mega-cities across China (Beijing, Shanghai, Xian, Nanjing and Chengdu); described parental perceptions of children’s ideal body image (IBI); and prospectively examined associations between parental perception of child IBI and child weight changes over 3 years. In this NIH-funded, open cohort study, data were collected from students and their parents in 2015, 2016 and 2017 (n = 3298, in 3 waves). Cross-sectional analysis included all 3,298 children; longitudinal data analysis used mixed effects models and included 1691 children aged 6–17 years with ≥ two body mass index (BMI) measurements during 2015–2017. Ov/ob prevalence based on Chinese age-sex-specific BMI cut-points was 30.0%. Based on waist-to-height ratio (WHtR), the abdominal obesity rate was 19.8%. Parents reported different preferred IBI for boys vs girls, being about 3 times more likely to select ov/ob as ideal for boys than for girls (4.5% vs 1.5%, respectively, P < 0.001). In longitudinal analysis, children whose parents selected ov/ob as ideal had higher BMI Z-scores and WHtR increase over time than those whose parents selected an average body image (β [SE] = 0.042 [0.011], and β [SE] = 0.010 [0.004], respectively, all P < 0.05). Ov/ob rates were high among children in major cities in China. Chinese parents preferred a heavier ideal body image for their boys. Health promotion programs should help empower parents and their children to develop appropriate body images and maintain healthy body weight.
Keywords: obesity, overweight, ideal body image, child, adolescent, China
Introduction
Childhood obesity has become a serious public health problem that jeopardizes global public health.[1, 2] Over the past four decades, the prevalence of childhood obesity has increased in almost all countries worldwide.[3, 4] In the context of globalization, and with the rapid development of the social economy and tremendous changes in the lifestyle of residents, the prevalence of overweight and obesity (ov/ob) has increased rapidly in China.[5–7] Being in the forefront of China’s economic development, the mega-cities (like Beijing and Shanghai) with the fastest change in environment and consciousness have led the country’s development and reflected the country’s dynamics, including changes in childhood obesity.
Given that parents are the primary caregivers for children, understanding their perceptions of children’s actual and ideal body image (IBI) is an important step in developing intervention strategies for promoting healthy weight among children. Perception is a multifaceted expression that is highly influenced by different social and cultural environments, such as cultural ideas, social pressure, and social support networks of parents.[8] For instance, research has suggested that Mexican American mothers wanted their children to be smaller than they currently were, while mothers in Mexico wanted their children to be bigger than they were.[9] Influenced by traditional culture and attitudes, some Chinese parents view a bigger body size for boys as a symbol of physical health and thus beautiful. They have greater misperceptions of their children’s actual weight status compared with parents in some other countries.[10] It is reported that 56.0% of Chinese parents had an inaccurate assessment of their children’s weight status, with 14.0% of mothers over-perceiving their children’s actual weight status.[11, 12] However, little is known about how many Chinese parents may have an IBI for their children that is overweight, nor about the differences in IBI that parents have for boys vs girls.
Several previous studies, including ours, have examined the association between parental perception of children’s actual body image and children’s weight status, and the association between children’s self-perceived body image and their subsequent weight change. Our study using data from 6–17-year-old Chinese children found that children who perceived themselves as being obese had a higher body mass index (BMI) increase than those with an average-weight body image, increasing their BMI by 0.99 kg/m2 per year.[13] This may be related to children’s misperception of body shape, which may affect children’s eating habits.[14] In our study of African American children, children’s body image had a significant association with their subsequent weight change.[15] However, knowledge about parental perceptions of children’s IBI and how it might affect weight status among children remains limited.
Obesity risk is affected by economic development and cultural cognition. People with different economic and educational levels have large differences in obesity risks.[16] Although some studies in China have examined the prevalence of childhood obesity and the characteristics of children’s perception of body image and related social demographics, no previous research has studied parental perceptions of children’s IBI in Chinese mega-cities. There is also a paucity of research in the field on longitudinal associations between parental perceptions of children’s IBI and children’s weight change.
To fill these knowledge gaps, using longitudinal survey data collected from five mega-cities in China, this study examined: 1) the prevalence of ov/ob and central obesity in children; 2) parental perceptions of children’s IBI and any gender differences; and 3) the association between parental perceptions of children’s IBI and children’s weight changes, testing how the associations might differ by children’s gender, age, and weight status. These findings could provide useful insights for future efforts to fight the childhood obesity epidemic.
Methods and Materials
1. Study design and study sample
The Childhood Obesity Study in China Mega-cities (COCM) is part of a US NIH-funded study aimed at examining the etiology of childhood obesity and chronic diseases in China, especially in major cities, which have been experiencing rapid social and economic changes over the past three decades. COCM is an open cohort study. Initially, four major cities across China (Beijing [the capital of China, in North China], Shanghai [the largest city in China, in South China], Nanjing [the capital of China before 1949, in South China], and Xi’an [the ancient capital of China for over 1300 years, in the mid-west of China]) were included in 2015 at baseline. In 2016, Chengdu, the capital of Sichuan Province (with the largest population among provinces in China, in the west of China) was added.
In each city, two primary schools and two middle schools were included. In each school, a class from each grade (grades 4–6 in primary schools, and grades 7–9 in middle schools) was included. Students in grades 6 and 9 in 2015 had graduated by the time of the second survey in 2016, so new students in grades 4 and 7 in the selected schools were recruited. This affected the attrition rate. At baseline in 2015, 1,648 children were enrolled, while 2,554 children were surveyed in 2016 (1,078 of the students having been surveyed in 2015). The attrition rate was 34.6% (= 570/1,648).
The study was approved by the Ethical Committee of the State University of New York at Buffalo and related collaborative institutes in China. Written informed consent was obtained from parents or children.
Children with missing data on age, gender, weight and height measurements were excluded from analysis (n = 70). Our cross-sectional data analysis used the children’s data from the first observation each year during 2015–2017 for all the students participating in the surveys (n = 3,298). For longitudinal data analysis, 1,691 children who had ≥ two BMI measurements during 2015–2017 were included to test associations between parental perceptions of children’s IBI and children’s BMI z-score and waist-to-height ratio (WHtR), respectively. (WHtR indicates central adiposity.)
2. Assessment and measures
1). BMI and WHtR.
Height was measured by a Seca 213 Portable Stadiometer Height-Rod with a precision of 0.1 centimeter; body weight was measured by a Seca 877 electronic flat scale with a precision of 0.1 kilogram. Waist circumference (WC) was measured by a tape with a precision of 0.1 centimeter. Children’s BMI (kg/m2) was calculated and transformed to a BMI Z-score according to the sex- and age-specific World Health Organization (WHO) reference growth charts.[17] General obesity was defined according to the age- and gender-specific BMI cutoffs points issued by the National Health Commission of the People’s Republic of China.[18] Abdominal obesity was defined as WHtR ≥ 0.48.[19]
2). Child IBI.
Line drawings used in previous studies showing 8 silhouette body sizes ranging from very thin to very heavy were adapted in our study. Students and parents were asked a question separately: a) “Which one do you wish that your body looked like?” and b) “Which one do you wish that your children’s body looked like?” For each question, students and parents were instructed to circle only one silhouette from the 8. The silhouettes were scored as A (thinnest) to H (heaviest) (see Figure 1). As previous studies did,[20, 21] we further grouped the 8 silhouettes into three levels: “underweight” (silhouettes A, B, and C), “normal” (silhouettes D and E), and “ov/ob” (silhouettes F, G, and H).
Figure 1.
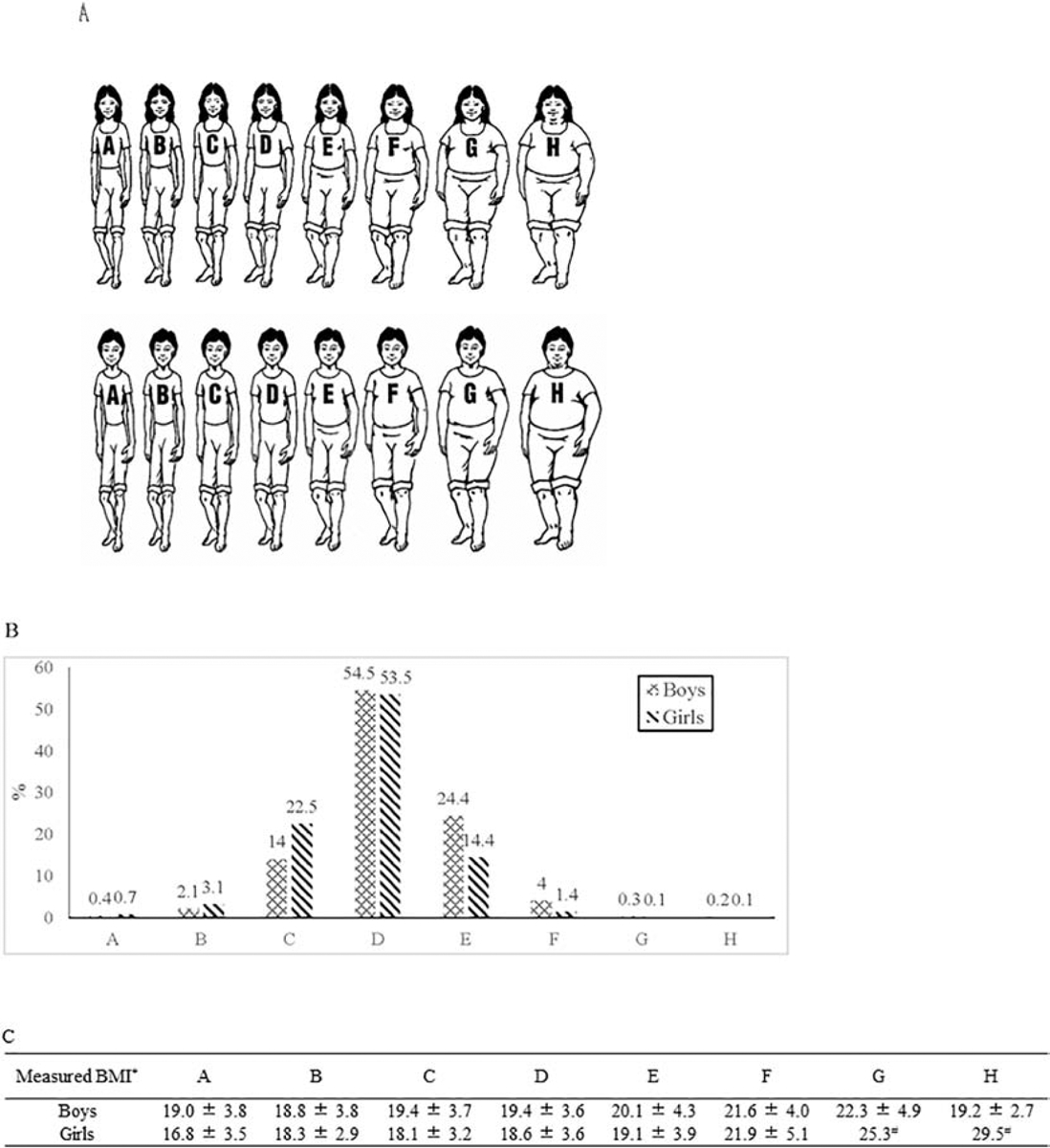
Distribution of parental perception of children’s ideal body image by gender
3). Lifestyle behaviors.
We used a validated questionnaire that includes a series of questions to ask about the type and frequency of the child’s diet. Children were asked to report weekly consumption frequencies of the following foods (livestock meat or red meat, poultry, vegetables, fruits, pure milk, dairy products, soybeans and soy products.) over the last 3 months. Then, based on their reported dietary intake frequencies, the students were classified as low- (< 3 days/week) vs. high-consumers (3–7 days/week) for data analysis. This was done for each of the food items [22].
The validated Chinese Children Physical Activity Questionnaire was used to measure the physical activity patterns of the children[23]. Physical activity was assessed by asking the students to report how often and how long they had engaged in the following activities outside of school time in the previous seven days: cycling, roller-skating, running, swimming, dancing, team sports, tennis, sit-ups, push-ups, etc. The intensity of their physical activity was classified based on the total days per week in which they reported spent at least 30 minutes/day participating in extracurricular, off-campus physical activities. The subjects were divided into 2 categories of having high or moderate (3–7 days/week) vs low (< 3 days/week) physical activity.[24]
4). Parental and household characteristics.
To consider the influence of family and household characteristics on the associations between IBI and children’s weight status, we used parents’ BMI, highest parental education (up to middle school or below, high or vocational schools, and college or above), family homeownership (rent or share residency with relatives, own apartment, own house) in our analysis.
3. Statistical analysis
First, we described children’s characteristics such as socio-demographics, distributions of actual weight statuses, and children’s or their parents’ perceptions of IBI using cross-sectional analysis of data collected from different children during 2015–2017 (n = 3,298). The chi-square tests were used to compare the gender differences for categorical variables and the t-test was used for continuous variables. Weighted kappa tested the child-parent agreement. The weight was given by (1-|i-j|)/(k-1), where i and j index the rows of columns of the ratings by the two raters and k is the maximum number of possible ratings. (Where “1” is the weight for the cells in the diagonal, and 0 and 0.5 are the values for the cells moving sequentially away from the diagonal.)
In longitudinal data analysis, mixed effects model were used to assess the associations between parental perceptions of their children’s IBI and their children’s actual BMI z-score and WHtR, adjusted for children’s perceptions of their IBI, age, gender, father’s BMI, mother’s BMI, parental highest education level, family homeownership, consumption of red meat, poultry, vegetables, fruits, pure milk, dairy products, and soybeans and soy products, and amount of off-campus physical activity. Further subgroup analyses were conducted by gender, age groups, and baseline weight status.
Analyses were conducted using Stata software version 14 (StataCorp, College Station, Texas, USA). The effect size was presented as beta coefficients with standard error (SE). Statistical significance was set at P < 0.05.
Results
1. Participants’ characteristics and prevalence of overweight and obesity in cross-sectional data analysis of 3,298 students
Table 1 shows the sample characteristics. Boys had higher BMI and WC than girls (all P < 0.05), and girls’ mothers were slightly heavier and their parents more likely to have more education. Based on BMI, 15.3% of children were obese (19.2% of boys and 11.2% of girls), while based on WHtR, the abdominal obesity rate was 19.8% (28.1% for boys and 11.3% for girls).
Table 1.
Sample characteristics of Chinese school children based on cross-sectional analysis of data from the Childhood Obesity Study in China Mega-cities (n = 3,298 different children)
| All (n = 3298) |
Boys (n =1675) |
Girls (n = 1623) |
P | |
|---|---|---|---|---|
| Age | 11.0 ± 2.0 | 11.0 ± 2.0 | 11.0 ± 2.1 | 0.734 |
| BMI (kg/m2) | 19.1 ± 3.8 | 19.7 ± 3.9 | 18.6 ± 3.6 | < 0.001 |
| Waist (cm) | 65.3 ± 10.3 | 68.0 ± 11.2 | 63.3 ± 8.8 | < 0.001 |
| Demographics & family socioeconomic status | ||||
| Father’s BMI (kg/m2) | 24.2 ± 3.6 | 24.3 ± 3.6 | 24.2 ± 3.6 | 0.538 |
| Mather’s BMI (kg/m2) | 22.2 ± 3.7 | 22.1 ± 3.5 | 22.4 ± 3.8 | 0.019 |
| Parental highest education level (%) | 0.008 | |||
| Middle school or below | 15.6 | 17.4 | 13.9 | |
| High or vocational schools | 25.7 | 25.5 | 25.9 | |
| College or above | 53.4 | 51 | 55.9 | |
| Family homeownership (%) | 0.249 | |||
| Rent or share residency with relatives | 27.1 | 28 | 26.1 | |
| Own apartment | 56.4 | 54.6 | 58.3 | |
| Own house | 10.9 | 10.9 | 10.8 | |
| General obesity (%) | < 0.001 | |||
| Underweight | 4.6 | 4.7 | 4.6 | |
| Normal | 62.4 | 54.8 | 70.2 | |
| Overweight | 17.7 | 21.4 | 13.9 | |
| Obesity | 15.3 | 19.2 | 11.2 | |
| Abdominal obesity (%) | < 0.001 | |||
| Non-obesity | 80.2 | 71.9 | 88.7 | |
| Obesity | 19.8 | 28.1 | 11.3 | |
Values are means ± SDs unless otherwise indicated; P values were calculated using t-test or chi-square test. General obesity was defined according to age- and gender-specific BMI cutoff points issued by the National Health Commission of the People’s Republic of China [17]. Abdominal obesity was defined as WHtR ≥ 0.48 [18]. BMI, body mass index. WHtR, waist-to-height ratio.
2. Gender difference of parental perceptions of children’s IBI in cross-sectional data analysis of 3,298 students
Figure 1 shows the distribution of parental perception of children’s IBI by gender. The most common selection among boys and girls was figure D (boys 54.5% and girls 53.5%), corresponding with the BMI classification for normal weight. In general, the objectively assessed BMI clearly increased with higher ideal body size.
As shown in Figure 2, 3.0% of parents thought that the IBI for children should be ov/ob, and it differed for boys and girls (4.5% vs 1.5%, respectively, P < 0.001). As for the IBI as perceived by children, boys were also different from girls (3.7% vs 0.8%, respectively, P < 0.001). Boys and boys’ parents were more inclined to see ov/ob as ideal.
Figure 2.
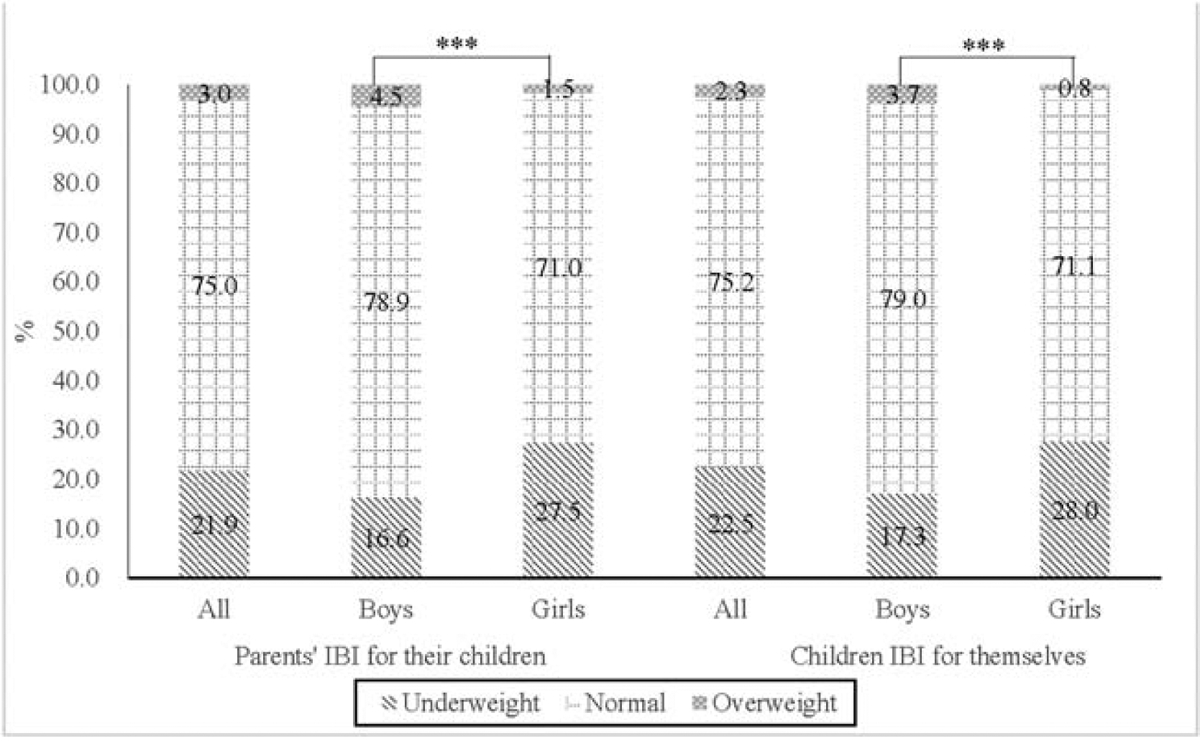
Distribution children’s ideal body image (%) evaluated by himself/herself or his/her parents
Table 2 presents the weighted kappa between parental perception of children’s IBI, children’s perception of their own IBI, and children’s BMI-based weight status. As the parents evaluated their children’s IBI from underweight to ov/ob, the ratio of childhood weight status showed an increasing trend: nearly 2% of the children whose IBI was evaluated by their parents as ov/ob actually measured as ov/ob. The resemblance between parental perception of their children’s ideal body and the children’s perception of their IBI, however, was weak, as shown by weighted kappa (0.168), just as the resemblance between parental perception of children’s IBI and children’s BMI-based weight status (0.033).
Table 2.
Agreement between parental perception of children’s ideal body image (IBI), children’s perception of own IBI, and children’s BMI-based weight status in cross-sectional data analysis in the Childhood Obesity Study in China Mega-cities (n = 3,298 different children).
| Parental IBI for their children | ||||
|---|---|---|---|---|
| Underweight | Normal weight | Overweight/obesity | ||
| Children’s IBI for themselves | Underweight | 8 | 14.2 | 0.3 |
| Normal weight | 13.8 | 57.7 | 2.4 | |
| Overweight/obesity | 0.3 | 1.8 | 0.4 | |
| Weighted agreement | 83.4 | |||
| Weight kappa | 0.168 | |||
| P | < 0.001 | |||
| Children’s weight status based on BMI | Underweight | 1.1 | 4 | 0 |
| Normal weight | 16.4 | 47 | 1.1 | |
| Overweight/obesity | 5.3 | 24 | 1.9 | |
| Weighted agreement | 72.5 | |||
| Weight kappa | 0.033 | |||
| P | < 0.001 | |||
P values calculated by using weighted kappa. Weight given by (1-|i-j|)/(k-1), where i and j index the rows of columns of the ratings by the two raters and k is the maximum number of possible ratings.
3. Association between parental perception of children’s IBI and BMI Z-score and WHtR in longitudinal data analysis of 1,691 students
Table 3 shows that children whose IBI was considered by their parents as ov/ob were more likely to have a higher BMI Z-score and WHtR increase during follow-up (β [SE] = 0.042 [0.011], and β [SE] = 0.010 [0.004], respectively; all P < 0.05). Significant gender differences were found for the associations between parental perceptions of children’s IBI and children’s weight status. Boys whose parents selected large body sizes (i.e., “ov/ob”) as the IBI were more likely to increase their BMI Z-score and WHtR (β [SE] = 0.041 [0.011], and β [SE] = 0.012 [0.005], respectively; all P < 0.05), but no significant associations were found among girls.
Table 3.
Longitudinal data analysis of associations between parental perception of children’s ideal body image (IBI) and child BMI Z-score and WHtR in the Childhood Obesity Study in China Mega-cities (n = 1,691)
| Parental IBI for their children (reference = average) |
||
|---|---|---|
| Overweight/obesity (β [SE]) |
Underweight (β [SE]) |
|
| BMI Z-score | ||
| All | 0.042 (0.011)*** | −0.003 (0.004) |
| Analysis stratified by: | ||
| 1. Gender | ||
| Boys | 0.041 (0.011)*** | 0.005 (0.006) |
| Girls | 0.029 (0.027) | −0.009 (0.006) |
| 2. Age at baseline | ||
| 6–11 | 0.003 (0.017) | −0.006 (0.006) |
| 12–17 | 0.046 (0.012)*** | −0.001 (0.005) |
| 3. Weight at baseline | ||
| Not overweight/obese | −0.006 (0.011) | −0.001 (0.003) |
| Overweight/obese | 0.046 (0.019)* | −0.001 (0.011) |
| WHtR | ||
| All | 0.010 (0.004)* | 0.001 (0.002) |
| Analysis stratified by: | ||
| 1. Gender | ||
| Boys | 0.012 (0.005)* | 0.005 (0.003) |
| Girls | 0.005 (0.007) | −0.003 (0.002) |
| 2. Age at baseline | ||
| 6–11 | 0.014 (0.006)* | −0.001 (0.002) |
| 12–17 | 0.006 (0.006) | 0.002 (0.003) |
| 3. Weight at baseline | ||
| Not overweight/obese | −0.002 (0.005) | −0.001 (0.001) |
| Overweight/obese | 0.004 (0.006) | 0.008 (0.003)* |
Participants had ≥ two BMI measurements during follow-up, thus, sample size became smaller. Parental perception of children’s ideal body image as “average” (silhouettes 4–5) used as reference in models. Mixed effect model after adjustment for IBI by children, age, gender, father’s BMI, mother’s BMI, parental highest education level, family homeownership, consumption frequency of red meat, poultry, vegetables, fruits, pure milk, dairy products, and soybeans and soy products, and engagement in off-campus physical activity, as well as cohort and considering COCM sampling methods and hierarchical data structure. Subgroup analysis applied same mixed model except for stratified variable.
P < 0.05.
P < 0.01.
P < 0.001. BMI, body mass index. WHtR, waist-to-height ratio.
Adolescents (12–17 years old) whose IBI was considered by their parents as ov/ob were more likely to have increased their BMI Z-score during follow-up than those who were assessed as normal (β [SE] = 0.046 [0.012], P < 0.001), while young children (7–11 years old) whose IBI was evaluated by their parents as ov/ob were more likely to have increased their WHtR than those who were assessed as normal (β [SE] = 0.014 [0.006], P < 0.05).
In addition, among children who were ov/ob at baseline, children whose IBI was considered by their parents as ov/ob were more likely to have a higher BMI Z-score (β [SE] = 0.046 [0.019], P < 0.05), while girls who were ov/ob at baseline and whose IBI was considered by their parents as thin had a higher WHtR (β [SE] = 0.008 [0.003], P < 0.05).
Discussion
Using the data collected during 2015–2017 from five mega-cities across China, we studied childhood obesity and overweight rates, Chinese parents’ weight perception of IBI for children, and the effect of parental perceptions of children’s IBI on the subsequent changes in child BMI Z-scores and WHtR. To our knowledge, this is the first study examining the association between parental perceptions of children’s IBI and children’s weight changes using longitudinal data in China. Studying the world’s second-largest economy and the nation with the largest number of ov/ob people had several important findings. First, one-third of children in big cities in China were ov/ob, and more boys than girls were ov/ob (40.6% vs 25.1%, respectively). Second, parents reported very different IBIs for boys vs girls. They were about 3 times more likely to select “ov/ob” as an IBI for boys than for girls (4.5% vs 1.5%, respectively). Third, parents who perceived their children as ov/ob were more likely to increase their children’s BMI and WHtR. Stratified analysis found that boys, older children (≥ 12 years old), and ov/ob children had higher BMI gains than girls, young children, and non-ov/ob children.
Actual and ideal body image are two important aspects of the evaluation of body (dis)satisfaction. There are several studies examining the association between children’s actual body image and childhood obesity, with some reporting that body weight misperception is associated with unhealthy eating.[14, 25–28] One of those studies has tested the association between children’s IBI and childhood obesity in other countries [21]. Body image concern among children may be strong enough to exert a positive influence, along with social support, in motivating health behaviors.[29] Another source of children’s ideas about ideal body image and their motivations to act upon those ideas may come from their parents. The relationship between parental perceptions of children’s IBI and childhood obesity has remained to be examined in China.”. In our study, the degree of parent-child resemblance in children’s IBI was weak, just as the resemblance in parental perception of children’s IBI and children’s weight status (weighted kappa: 0.168 and 0.033, respectively). We did not find a similar study, but our result was generally consistent with some research that has examined parent-child resemblance in body weight status. For example, one of our previous US studies (among 4,846 boys, 4,725 girls, and their parents) reported weighted kappa coefficients between BMI quintiles of parent and child ranging from −0.02 to 0.25.[30] Previous research regarding weak parent-child resemblance in energy balance-related behaviors may help explain the relatively weak resemblance in actual weight status,[31] and the weak parent-children resemblance in children’s IBI might be due to increased independence in children.[32]
In this study, the prevalence of ov/ob children in mega-cities in China reached 33%, and the prevalence of ov/ob was higher than the national level of about 19.4% in 2014.[33] This is consistent with the association between socioeconomic status and ov/ob in developing countries, that is, the higher the socioeconomic status, the higher the ov/ob rates.[34] However, Monteiro et al. concluded that with the economic growth and nutritional transformation of developing countries, the relationship between obesity and socioeconomic status would gradually change, and there would be a negative correlation between obesity and socioeconomic status.[35] According to the idea of “nutritional transition,” with the development of a nation’s economy, the change of the overall nutritional status of a country will go through three stages: hunger reduction, a higher incidence of chronic diseases, and behavior change.[36] Our research indicated that even in China’s economically developed regions, “nutritional transition” was still in the second stage.
Some research indicates Chinese parents and grandparents have a stereotypical image of children—chubby boys and slim girls.[37] Our study found that 3.0% of parents chose large body sizes (ov/ob) as children’s IBI, with 4.0% of parents thinking that boys’ IBI was ov/ob and 3.7% of boys reporting their IBI as ov/ob, while 1.5% of parents thought that girls’ IBI was ov/ob, yet only 0.8% of girls’ self-reported IBI was ov/ob. That highlights unique gender-specific cultural views about body image: the preference for thinness in girls and bigger body size in boys was prevalent.[38] Our figure was higher than those in a study of 374 Mexican mothers. In that study, 4.0% of mothers chose underweight or overweight as children’s IBI,[9] but 23.9% of parents chose underweight or overweight as their children’s IBI in our study.
Another important finding was the positive association between parental perception of children’s IBI and children’s BMI and WHtR. This association might be due to the acceptance of a large IBI among parents putting less pressure on children to try to control their own weight. We also found a significant association between children’s self-assessed IBI and children’s BMI and WHtR (Supplemental Table 1); boys who self-evaluated their IBI as ov/ob had a higher BMI Z-score and WHtR increase over time than those who assessed themselves as normal.
Our gender-stratified analysis showed that boys whose parents selected ov/ob as an IBI were more likely to increase their BMI and WHtR than boys whose parents selected normal weight as an IBI. This might partly explain the difference in the prevalence of obesity between boys and girls in China. In Mexican mothers’ perceptions of their children’s body weight, they appropriately perceived overweight children; however, these mothers were not concerned by this situation because for them, it was something temporary that would disappear as the child grew. But mothers typically perceived overweight and obesity in girls with greater precision, which motivated them to change their children’s habits and behaviors.[39] Our age-stratified analysis in China found that parental perceptions of children’s IBI was associated with adolescents’ (12–17 years old) BMI, and children’s self-assessed IBI was associated with adolescents’ (12–17 years old) BMI and WHtR (Supplemental Table 1). This might be due to parents paying more attention to their children’s growth and development when the children enter puberty,[40] thus adolescents were more likely to have a weight status consistent with their IBI and to maintain their body image over time than were younger children. In addition, we found that ov/ob children at baseline whose parents selected “ov/ob” as an IBI were more likely to increase their BMI than those whose parents selected “normal weight” as the ideal. Other longitudinal studies have revealed that children who are obese or have a negative self-perceived body image have a higher weight gain (e.g., β in BMI = 0.38 [SE = 0.13], P < 0.01 and 0.25 [95% CI: 0.10–0.39], respectively) and an increased risk of obesity (e.g., odds ratio of having obesity = 1.6 [95% CI: 1.20–2.30]) compared to the children who are their counterparts.[41, 42]
Key strengths of this study include that it examined the little-studied issue of parental attitudes toward IBI; it targeted the emergence of these attitudes in a rapidly developing economy like China’s; and it was a prospective study, utilizing data collected from 5 mega-cities across China. The findings will be useful to policy makers addressing the obesity problem. The study also has some limitations. It only investigated the prevalence of overweight and obesity in large cities, but not nationwide. In addition, the follow-up period of 3 years is not long.
In conclusion, our results highlight the high rates of childhood obesity/overweight (based on BMI) and central obesity, and much higher rates in boys than in girls, in mega-cities in China. Chinese parents preferred large body sizes for boys and thinness for girls. Children of parents who perceived a childhood IBI as heavier had a faster BMI increase with age than those with parents who had an average-size body image for children, especially among boys, older children, and those who were overweight/obese at baseline. Health promotion programs in China should communicate about and help parents recognize healthy ideal body image in children. Parents and children should be empowered to develop an appropriate body image and maintain healthy body weight.
Supplementary Material
Highlights.
High rates of childhood ov/ob and central obesity in mega-cities in China
Chinese parents preferred large body sizes for boys and thinness for girls
Children of parents who perceived a childhood IBI as heavier had a rapid BMI growth
Health programs should help parents recognize healthy IBI in children
Acknowledgements
The study was funded in part by the US National Institutes of Health (NIH, U54 HD070725), National Basic Research Program of China (973 Program) (2017YFC0907200), and the Xi’an Jiaotong University. The U54 project (U54 HD070725) is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Office of the Director, National Institutes of Health (OD). Prof. Youfa Wang is the principal investigator of the study. The content of the paper is solely the responsibility of the authors and does not necessarily represent the official views of the funders. We thank study participants and school personnel who participated in the data collection and thank our collaborators from multiple institutions in China and the United States. We also thank Dr. Brenda Denzler for her professional language editing of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015; 385(9986): 2510–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 2014; 384(9945): 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017; 390(10113): 2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. IJPO 2006; 1(1): 11–25. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Wang L, Qu W. New national data show alarming increase in obesity and noncommunicable chronic diseases in China. Eur J Clin Nutr 2017; 71(1): 149–150. [DOI] [PubMed] [Google Scholar]
- 6.Jia P, Xue H, Zhang J, Wang Y. Time Trend and Demographic and Geographic Disparities in Childhood Obesity Prevalence in China-Evidence from Twenty Years of Longitudinal Data. Int J Environ Res Public Health 2017; 14(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Mi J, Shan XY, Wang QJ, Ge KY. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. IJO 2007; 31(1): 177–188. [DOI] [PubMed] [Google Scholar]
- 8.Lindsay AC, Sussner KM, Greaney ML, Peterson KE. Latina mothers’ beliefs and practices related to weight status, feeding, and the development of child overweight. Public health nurs 2011; 28(2): 107–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosas LG, Harley KG, Guendelman S, Fernald LC, Mejia F, Eskenazi B. Maternal perception of child weight among Mexicans in California and Mexico. Matern Child Health J 2010; 14(6): 886–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: a meta-analysis. Pediatrics 2014; 133(3): e689–703. [DOI] [PubMed] [Google Scholar]
- 11.Wen X, Hui SS. Chinese parents’ perceptions of their children’s weights and their relationship to parenting behaviours. Child Care Health Dev 2011; 37(3): 343–351. [DOI] [PubMed] [Google Scholar]
- 12.Min J, Wang VH, Xue H, Mi J, Wang Y. Maternal perception of child overweight status and its association with weight-related parenting practices, their children’s health behaviours and weight change in China. Public Health Nutr 2017; 20(12): 2096–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Min J, Fang Yan A, Wang Y. Mismatch in Children’s Weight Assessment, Ideal Body Image, and Rapidly Increased Obesity Prevalence in China: A 10-Year, Nationwide, Longitudinal Study. Obesity (Silver Spring) 2018; 26(11): 1777–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yan H, Wu Y, Oniffrey T, Brinkley J, Zhang R, Zhang X, et al. Body Weight Misperception and Its Association with Unhealthy Eating Behaviors among Adolescents in China. Int J Environ Res Public Health 2018; 15(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Liang H, Chen X. Measured body mass index, body weight perception, dissatisfaction and control practices in urban, low-income African American adolescents. BMC Public Health 2009; 9: 183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fruhstorfer BH, Mousoulis C, Uthman OA, Robertson W. Socio-economic status and overweight or obesity among school-age children in sub-Saharan Africa - a systematic review. Clinical obesity 2016; 6(1): 19–32. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. 2007:http://www.who.int/growthref/en/.
- 18.National Health Commission of the People’s Republic of China. Screening for overweight and obesity among school-age children and adolescents. In. http://www.moh.gov.cn/xxgk/pages/wsbzsearch.jsp; 2018. [Google Scholar]
- 19.Meng L, Mi J, Cheng H, Hou D, Zhao X, Ding X. Using waist circumference and waist-to-height ratio to access central obesity in children and adolescents. Chin J Evid Based Pediatr 2007; 2(4):;245–252. [Google Scholar]
- 20.Min J, Yan AF, Wang VHC, Wang Y. Obesity, body image, and its impact on children’s eating and exercise behaviors in China: A nationwide longitudinal study. Prev Med 2018; 106: 101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen X, Wang Y. Is ideal body image related to obesity and lifestyle behaviours in African American adolescents? Child Care Health Dev 2012; 38(2): 219–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xi B, Zhang M, Shen Y, Zhao X, Wang X, Mi J. Impact on the risk of obesity due to interactions between fat mass- and obesity-associated gene rs9939609 variants and behavioral factors, in the Chinese school-aged children. Chin J Epidemiol 2010; 31(7): 737–741. [PubMed] [Google Scholar]
- 23.Chu W, Wang Z, Zhou H, Xu F. The reliability and validity of a physical activity questionnaire in Chinese children. Chin J Dis Control Prev 2014; 18(11): 1079–1082. [Google Scholar]
- 24.Xi B, Wang C, Wu L, Zhang M, Shen Y, Zhao X, et al. Influence of physical inactivity on associations between single nucleotide polymorphisms and genetic predisposition to childhood obesity. Am J Epidemiol 2011; 173(11): 1256–1262. [DOI] [PubMed] [Google Scholar]
- 25.Ling J, Stommel M. Parental and Self-Weight Perceptions in U.S. Children and Adolescents, NHANES 2005–2014. West J Nurs Res 2019; 41(1): 42–57. [DOI] [PubMed] [Google Scholar]
- 26.Hossain MS, Siddiqee MH, Ferdous S, Faruki M, Jahan R, Shahik SM, et al. Is Childhood Overweight/Obesity Perceived as a Health Problem by Mothers of Preschool Aged Children in Bangladesh? A Community Level Cross-Sectional Study. Int J Environ Res Public Health 2019; 16(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Queally M, Doherty E, Matvienko-Sikar K, Toomey E, Cullinan J, Harrington JM, et al. Do mothers accurately identify their child’s overweight/obesity status during early childhood? Evidence from a nationally representative cohort study. Int J Behav Nutr Phys Act 2018; 15(1): 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutin AR, Terracciano A. Body weight misperception in adolescence and incident obesity in young adulthood. Psychol Sci 2015; 26: 507–511 [DOI] [PubMed] [Google Scholar]
- 29.Yayan EH, Celebioglu A. Effect of an obesogenic environment and health behaviour-related social support on body mass index and body image of adolescents. Glob Health Promot 2018; 25(3): 33–42. [DOI] [PubMed] [Google Scholar]
- 30.Liu Y, Chen HJ, Liang L, Wang Y. Parent-child resemblance in weight status and its correlates in the United States. PloS one 2013; 8(6): e65361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beydoun MA, Wang Y. Parent-child dietary intake resemblance in the United States: evidence from a large representative survey. Soc Sci Med 2009; 68(12): 2137–2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hesketh KR, Brage S, Cooper C, Godfrey KM, Harvey NC, Inskip HM, et al. The association between maternal-child physical activity levels at the transition to formal schooling: cross-sectional and prospective data from the Southampton Women’s Survey. Int J Behav Nutr Phys Act 2019; 16(1): 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang S, Dong Y, Wang Z, Zou Z, Ma J. Trends in overweight and obesity among Chinese children of 7– 18 years old during 1985– 2014. Chin J Prev Med 2017; 51(4): 300–305. [DOI] [PubMed] [Google Scholar]
- 34.McLaren L Socioeconomic status and obesity. Epidemiologic reviews 2007; 29: 29–48. [DOI] [PubMed] [Google Scholar]
- 35.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord 2004; 28(9): 1181–1186. [DOI] [PubMed] [Google Scholar]
- 36.Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord 2004; 28 Suppl 3: S2–9. [DOI] [PubMed] [Google Scholar]
- 37.Jiang J, Rosenqvist U, Wang H, Greiner T, Lian G, Sarkadi A. Influence of grandparents on eating behaviors of young children in Chinese three-generation families. Appetite 2007; 48(3): 377–383. [DOI] [PubMed] [Google Scholar]
- 38.Chen H, Jackson T. Predictors of changes in body image concerns of Chinese adolescents. J Adolesc 2009; 32(4): 977–994. [DOI] [PubMed] [Google Scholar]
- 39.Avila-Ortiz MN, Castro-Sanchez AE, Zambrano-Moreno A. Mexican mothers’ perceptions of their child’s body weight. Health Soc Care Community 2017; 25(2): 569–577. [DOI] [PubMed] [Google Scholar]
- 40.Paikoff RL, Brooks-Gunn J. Do parent-child relationships change during puberty? Psychol Bull 1991; 110(1): 47–66. [DOI] [PubMed] [Google Scholar]
- 41.Robinson E, Sutin AR. Parental Perception of Weight Status and Weight Gain Across Childhood. Pediatrics 2016; 137(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hunger JM, Tomiyama AJ. Weight labeling and obesity: a longitudinal study of girls aged 10 to 19 years. JAMA pediatrics 2014; 168(6): 579–580. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


