Abstract
OBJECTIVE
To report surgical and functional outcomes of buried penis surgery.
METHODS
Outcomes following buried penis surgery at the University of Washington were assessed from June 1, 2005 to June 1, 2016. Patient demographic and surgical data were abstracted from a retrospective chart review. All patients were attempted to be contacted by phone for long-term follow-up. Uni- and multivariate analysis was performed to evaluate for association with any complication.
RESULTS
A total of 42 men underwent buried penis repair surgery (mean short-term follow-up 8.1 months). There was an overall 33% 90-day complication rate (21 events). In univariate analysis, body mass index (BMI; P = .02) and no history of gastric bypass (P = .03) were significant predictors of any complication. In multivariate analysis, only BMI remained significant (odds ratio 1.1 for each increase in unit of BMI, 95% confidence interval 1.01–1.27). Twenty-seven patients were reached for long-term follow-up (mean 39 months). Patients reported improvements in every functional domain that was assessed. Of the patients, 85% reported they would undergo buried penis surgery again, 74% that surgery led to a positive change in their lives, and 85% that the surgery had remained a long-term success.
CONCLUSION
Surgical correction of buried penis with penile split-thickness skin graft and limited panniculectomy is well tolerated and results in functional, long-term improvements. BMI is associated with an increased likelihood of a complication following surgery.
Adult buried penis is an acquired disorder typically related to obesity and can result in the inability to direct one’s urine stream, maintain genital hygiene, and be sexually active related to a concealed penis. Men with buried penis often have had previous circumcision and this often leads to deficient penile shaft skin. This can result in secondary manifestations such as phimosis, lichen sclerosus (LS), balanitis, penile cancer, meatal stenosis, lower urinary tract symptoms, and sexual dysfunction.1,2 The excessive adiposity related to obesity can cause urine trapping and a moist environment that may lead to chronic infection or inflammation.2,3 These processes are thought to lead to phimosis and LS, which further potentiates the problem. Even after significant weight loss or bypass surgery, redundant lower abdominal skin can continue to pose a problem for patients despite their overall weight loss.4
Data from small series have shown that men with buried penis overall demonstrate a lower quality of life and have high rates of depression.5,6 Of note, some studies have identified postoperative improvements in these measures after surgical repair for buried penis. In 1 series of 9 patients, the authors noted that buried penis repair resulted in improvement in sexual pleasure and genital hygiene and less difficulty with urination.5 In a similar small series, Rybak et al reported that the majority of patients had improvement of voiding, erectile dysfunction scores, and quality of life measurements after repair compared to preoperative baselines.3
Despite these findings, the published data describing surgical and patient quality of life outcomes are confined to very small series of patients.2,3,6–8 Our objective was to report surgical and functional outcomes following buried penis repair.
METHODS
Men who underwent buried penis repair at our institution from June 1, 2005 to June 1, 2016 were retrospectively identified. Institutional Review Board (IRB) approval was obtained for the study. Surgical reconstruction consisted of limited suprapubic panniculectomy, radical excision of penile shaft skin with split-thickness skin graft (STSG), and scrotoplasty if needed. We excluded any patients who did not undergo both limited panniculectomy and STSG of the penile shaft to maintain homogeneity of the study population. Patient demographic data, surgical information, and 90-day complications were abstracted from a retrospective chart review. Complications assessed included readmission, deep venous thrombosis/pulmonary embolus, cardiac/pulmonary/vascular complications, panniculectomy complication (wound breakdown or infection), donor site infection or other complication, genital wound infection, graft complication (lymphedema, contracture, recurrent LS), or graft loss. Complications were categorized by the Clavien-Dindo classification system.9 Attempts were made to contact all patients for long-term follow-up by phone on at least 3 separate occasions to assess functional and quality of life outcomes. The long-term survey was administered via telephone and the questions can be found in the Supplementary Data. IRB approval was obtained for this study (University of Washington, Human Subjects Division—IRB 41440).
The surgical team included both plastic surgery and urology. Our surgical technique has been previously described in detail with an accompanying video.4 This technique includes performing a limited suprapubic panniculectomy using a modified trapezoid incision. In doing so, we take care to stay below the waistline sulcus and fix the inferior border of the panniculectomy site to the pubic symphysis periosteum to prevent buried penis recurrence. One or more closed-suction drains are typically left in the panniculectomy bed. The diseased penile shaft skin is excised up to the coronal margin, with preservation of the dartos fascia if feasible. A 1:1 meshed or unmeshed 0.015-inch STSG from either the thigh or the excised pannus is then applied to the penis. We avoid placing the penis on excess tension when electing where to fix the native skin to the base of the penis to aid postsurgical wound healing. A bolster dressing is applied over the grafted skin, and the patient is maintained on bed rest for 5 days while being maintained on subcutaneous heparin for venous thromboembolism prophylaxis. A silver-impregnated or silicone (Mepilex; Mölnlycke Health Care; Norcross, GA) dressing is applied to the donor site and allowed to fall off on its own after discharge. After the bolster dressing is removed from the penile shaft, petroleum-impregnated gauze is applied daily for 5 days. Drains from the panniculectomy wound are removed when outputs are low (<25 cc/day).
Univariate analysis with Fisher exact test, t test, and logistic regression was performed to evaluate for association of demographic or surgical characteristics with any complication. Multivariate analysis including predictors found to be significant in univariate analysis was additionally performed. Univariate analysis of association between long-term quality of life outcomes with the occurrence of any complication, the presence of LS, and having undergone gastric bypass surgery before buried penis repair was also performed using Fisher exact test. A P value of <.05 was considered significant. STATA version 13 (College Station, TX) was utilized to perform statistical analysis.
RESULTS
A total of 42 men underwent buried penis repair, with a mean ± SD short-term postsurgical follow-up of 8.1 ± 8.1 months. Demographics and surgical characteristics by complication are shown in Table 1. All patients had a body mass index (BMI) greater than 35 kg/m2, with almost 60% having a BMI greater than 45 kg/m2. Nearly one-third had undergone previous gastric bypass; those who had previously undergone gastric bypass did have a lower mean BMI (43.1 ± 10.0) than those who had not (47.2 ± 9.0), although this difference was not statistically significant (P = .20). More than 80% had undergone previous circumcision, and 17% had required a previous dorsal slit. Medical comorbidities, such as hypertension (67%), diabetes (48%), and obstructive sleep apnea (74%), were common. In terms of etiology, the vast majority of patients were affected due to obesity, but one-third had LS identified as a sole or secondary etiology. Further, 10% of patients had phimosis identified as a sole or secondary etiology. Reconstruction was most commonly performed in one stage; however, a staged approach using a temporary allograft was done in 5 patients. Predominately, the STSG donor site was the leg, while skin from the excised pannus was used in the remainder (6/42). Of note, one of our surgeons has transitioned his practice over the past year to use the excised abdominal pannus, when allowable for STSG, as his preferred donor site. On pathologic examination of the penile skin, 3 additional patients were found to have LS that had not been identified preoperatively.
Table 1.
Characteristics of patients undergoing buried penis repair
| Demographics |
No Complication | Complication | P Value | |
|---|---|---|---|---|
| N = 42 (%) | n = 28 (%) | n = 14 (%) | ||
| Patient characteristics | ||||
| Age (y), mean ± SD | 53.3 ± 10.8 | 54.0 ± 10.2 | 51.7 ± 12.1 | .51 |
| BMI (mean ± SD) | 45.9 ± 9.4 | 43.3 ± 8.4 | 51.2 ± 9.3 | .02 |
| Hypertension | 28 (66.7) | 21 (75.0) | 7 (50.0) | .17 |
| Diabetes | 20 (47.6) | 15 (53.6) | 5 (35.7) | .34 |
| Obstructive sleep apnea | 31 (73.8) | 18 (64.3) | 13 (92.9) | .07 |
| Current tobacco use | 8 (19.1) | 5 (17.9) | 3 (21.4) | .78 |
| Previous circumcision | 34 (82.9) | 22 (81.5) | 12 (85.7) | .73 |
| Previous dorsal slit | 7 (16.7) | 5 (17.9) | 2 (14.3) | .77 |
| Previous gastric bypass | 13 (31.0) | 12 (42.9) | 1 (7.1) | .03 |
| Etiology of buried penis | ||||
| Obesity | 37 (88.1) | 24 (85.7) | 13 (92.9) | .65 |
| Lichen sclerosis | 14 (33.3) | 9 (32.1) | 5 (35.7) | .82 |
| Phimosis | 5 (11.9) | 4 (14.3) | 1 (7.1) | .65 |
| Penile cancer | 1 (2.4) | 1 (3.6) | 0 | .47 |
| Surgical characteristics | ||||
| STSG Donor site | ||||
| Thigh | 36 (85.7) | 25 (89.3) | 11 (78.6) | .38 |
| Pannus | 6 (14.3) | 3 (10.7) | 3 (21.4) | |
| STSG Graft size (cm2), mean ± SD | 101.4 ± 34.3 | 103.1 ± 38.9 | 97.8 ± 23.5 | .63 |
| Meshed | 27 (64.3) | 18 (64.3) | 9 (64.3) | 1.00 |
| Lichen sclerosis of penile skin on pathology | 17 (40.5) | 14 (50.0) | 3 (21.4) | .10 |
| Length of stay (d), mean ± SD | 5.9 ± 1.5 | 5.8 ± 1.3 | 6.1 ± 1.9 | .52 |
| Short-term follow-up (mo), mean ± SD | 8.1 ± 8.1 | 7.2 ± 8.2 | 10.1 ± 7.9 | .29 |
BMI, body mass index; SD, standard deviation; STSG, split-thickness skin graft.
There was an overall 33% complication rate (21 events in 14 individuals), with the majority of these complications relating to the pannus or genital wound (wound breakdown or infection) or the graft (Table 2). Of these, 11 were grade I complications, 3 were grade II complications, 6 were grade III complications, and 1 was a grade IV complication. In univariate analysis of predictors of any complication, higher BMI (P = .02) and those without a previous history of gastric bypass (P = .03) were more likely to develop a complication. In multivariate analysis of these predictors, only BMI remained significant (odds ratio 1.1, 95% confidence interval 1.01–1.27 for each increase in unit of BMI).
Table 2.
90-Day complications following buried penis repair
| Individuals With Any Complication | 14 (33.3%) |
| Complication events | n = 21 |
| PE | 1 |
| Pannus wound breakdown | 4 |
| Pannus wound infection | 2 |
| Genital wound breakdown | 1 |
| Genital wound infection | 1 |
| UTI | 1 |
| Lymphedema | 3 |
| Graft contracture | 1 |
| Graft loss | 6 |
| % Graft loss (median ± IQR) | 10 ± 15 |
IQR, interquartile range; PE, pulmonary embolus; UTI, urinary tract infection.
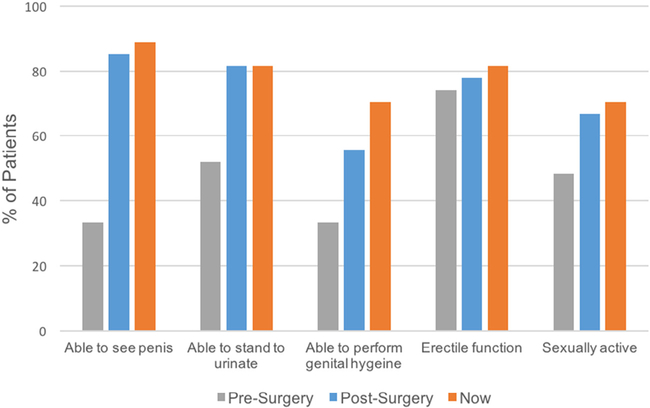
Of the 42 patients who underwent repair, 3 had died of unrelated causes, and 27 of the remaining 39 (69%) patients were able to be reached for long-term follow-up (mean 39.4 ± 34.5 months). Preoperatively, only 52% were able to stand to urinate, 67% had at least some difficulty with genital hygiene, 33% were able to see their penis, 74% were able to get erections, and 48% were sexually active. Patients’ reported long-term improvements in every functional domain that was assessed, and these postsurgical improvements either persisted or continued to improve in the long-term (Fig. 1).
Figure 1.
Functional outcomes following buried penis repair. (Color version available online.)
If given the chance to go back in time, 85% of patients reported that they would undergo buried penis surgery again, with a mean satisfaction score of 3.6 ± 1.2 on a 5-point Likert scale (1 = not at all satisfied, 3 = moderately satisfied, 5 = extremely satisfied). In stratifying patients by the presence of LS and gastric bypass before buried penis repair, 92% of patients with LS would undergo surgery again compared with 80% of patients without LS (P = .61), and 100% of patients with prior gastric bypass would undergo surgery again compared with 80% of patients without prior bypass (P = .55). Similar differences were also evident in mean satisfaction scores, with mean satisfaction among LS vs non-LS patients of 3.8 ± 1.2 compared with 3.4 ± 1.3 (P = .47) and among those with a prior gastric bypass was 4.2 ± 0.6 compared with 3.3 ± 1.3 for those without prior bypass (P = .10).
Overall, 74% of patients reported that surgery led to a positive change in their lives, and 85% of patients reported that the surgery had remained a success in the long-term. Notably, in the cohort having previously undergone gastric bypass, 100% of patients reported that surgery both led to a positive change in their lives and had remained a long-term success, although these results were not statistically significant (P = .14 and .55, respectively). Occurrence of a complication was not significantly associated with patients’ long-term quality of life in any of the metrics we assessed (wish to undergo surgery again (P = .61), surgery leading to a positive change in their lives (P = .39), surgery remaining a long-term success (P = .99)).
DISCUSSION
This study offers the largest series to date of surgical and functional outcomes following buried penis repair using a homogenous surgical technique. Overall, we found that surgical correction of buried penis with penile STSG and limited panniculectomy is well-tolerated and results in functional, long-term improvements.
Our analysis did reveal that higher BMI is associated with a 10% increased risk of any complication for every unit increase in BMI, with the majority of those complications related to the wounds or graft. Studies of urologic procedures evaluating the association between BMI and surgical complications have shown that BMI is associated with a higher risk of overall complications in pediatric patients undergoing surgery (with a greater than 2-fold increased odds of wound complications) and that a BMI of ≥40 kg/m2 predicted surgical site infections in patients undergoing surgery for renal masses.10,11 In other surgical populations, obesity has similarly been found to be linked to increased risk of complications. Obesity has been linked to wound complications and prolonged hospital stay in ovarian cancer patients, an increased risk of overall surgical morbidity in endometrial cancer patients, an increased risk of developing a hospital-acquired condition in adult spinal deformity patients, and an increased risk of wound and respiratory complications in intestinal surgery patients.12–15 Furthermore, a BMI >40 kg/m2 has been linked to an increased risk of morbidity due to wound infections, thromboembolism, and renal complications in vascular surgery patients and increased early major adverse clinical outcomes in cardiac surgery patients.16,17
Associations between obesity and ensuing surgical complications raise the question of whether physicians should be counseling patients about weight loss before surgery. In fact, in our own univariate analysis, those who had undergone previous gastric bypass surgery had a statistically significant lower likelihood of complications, yet this significance disappeared in multivariate analysis, pointing again to the patient’s BMI as the most important predictor of complications. As such, there may be patients who are morbidly obese (BMI ≥40 and <50 kg/m2) or super obese (BMI ≤50 kg/m2) who may gain significant benefit from undergoing weight-loss surgery before buried penis repair. In addition, our data suggested that long-term quality of life outcomes were better for those who had undergone gastric bypass surgery before buried penis repair, which may speak to a higher likelihood of long-term functional and quality of life success in these patients, although more numbers of patients are required to know if this represents a true difference.
Our results also showed that functional outcomes improved after surgery, and this effect persisted in all domains and even improved in most domains in the long-term. These data support and expand upon previous findings from small series that surgical repair of buried penis has resulted in improved genital hygiene, voiding, and erectile dysfunction.3,5 In addition, we found in long-term follow-up that the vast majority of patients felt the surgery was a success and would repeat the surgery again if faced with the same choice. These results validate previous findings of improved quality of life measurements of these patients after surgery.3
Regarding surgical technique, there are a vast array of reported methods for surgical correction of buried penis, including Z-plasty, pubic Y-V advancement flaps, scrotal flaps, and various methods of applying STSG for coverage of the penile shaft, as well as lipectomy vs liposuction for managing the suprapubic escutcheon. It has been our observation that a limited panniculectomy combined with fixation of the inferior border of the panniculectomy site to the pubic symphysis is a key step in the correction of buried penis. Fixation of the inferior border of the pannus skin is crucial to keeping the penis exposed following surgery.4 Additionally, we found a very high rate of LS on pathology of the excised penile skin, suggesting an aggressive approach in terms of excising any skin that does not appear healthy.
Similar to other buried penis series, this study is limited in that it is a single-institution series of a surgery that is performed relatively uncommonly. However, the study procedures were similar and included outcomes from 2 urologists who work separately with the same plastic surgeon. As such, it was not based on one surgical team. We acknowledge that recall bias could impact the quality and reliability of data obtained by phone calls and have now augmented the data obtained during clinical visits to maintain objectivity. Unfortunately, 30% of patients (12/39) were unable to be contacted for questionnaire administration after surgery. This is an important limitation, and we acknowledge that there may have been important content from these missing patients. Finally, the survey is not validated but was designed specifically for this patient population, given that there is no patient-reported outcome measure assessment that exists in this area. Despite these limitations, we believe that our results enhance the existing literature in terms of reporting both surgical and functional outcomes after buried penis repair.
CONCLUSION
Surgical correction of buried penis with a penile STSG and limited panniculectomy is well-tolerated and results in long-term functional improvements. BMI is associated with an increased likelihood of a complication following surgery. As a result, consideration should be given to weight loss via diet/exercise or gastric bypass surgery for those who have a very high BMI preoperatively.
Supplementary Material
Footnotes
Financial Disclosure: The authors declare that they have no relevant financial interests.
APPENDIX
Supplementary Data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.urology.2017.07.021.
References
- 1.Tausch TJ, Tachibana I, Siegel JA, Hoxworth R, Scott JM, Morey AF. Classification system for individualized treatment of adult buried penis syndrome. Plast Reconstr Surg. 2016;138:703–711. doi: 10.1097/PRS.0000000000002519. [DOI] [PubMed] [Google Scholar]
- 2.Donatucci CF, Ritter EF. Management of the buried penis in adults. J Urol. 1998;159:420–424. [DOI] [PubMed] [Google Scholar]
- 3.Rybak J, Larsen S, Yu M, Levine LA. Single center outcomes after reconstructive surgical correction of adult acquired buried penis: measurements of erectile function, depression, and quality of life. J Sex Med. 2014;11:1086–1091. doi: 10.1111/jsm.12417. [DOI] [PubMed] [Google Scholar]
- 4.Figler BD, Chery L, Friedrich JB, Wessells H, Voelzke BB. Limited panniculectomy for adult buried penis repair. Plast Reconstr Surg. 2015;136:1090–1092. doi: 10.1097/PRS.0000000000001722. [DOI] [PubMed] [Google Scholar]
- 5.Hughes DB, Perez E, Garcia RM, Aragón OR, Erdmann D. Sexual and overall quality of life improvements after surgical correction of “buried penis.” Ann Plast Surg. 2016;76:532–535. doi: 10.1097/SAP.0000000000000378. [DOI] [PubMed] [Google Scholar]
- 6.Tang S-H, Kamat D, Santucci RA. Modern management of adultacquired buried penis. Urology. 2008;72:124–127. doi: 10.1016/j.urology.2008.01.059. [DOI] [PubMed] [Google Scholar]
- 7.Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. J Urol. 1999;161:455–459. [PubMed] [Google Scholar]
- 8.Alwaal A, McAninch JW, Harris CR, Breyer BN. Utilities of split-thickness skin grafting for male genital reconstruction. Urology. 2015;86:835–839. doi: 10.1016/j.urology.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grimes MD, Blute ML, Wittmann TA, et al. A critical analysis of perioperative outcomes in morbidly obese patients following renal mass surgery. Urology. 2016;doi: 10.1016/j.urology.2016.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurtz MP, McNamara ER, Schaeffer AJ, Logvinenko T, Nelson CP. Association of BMI and pediatric urologic postoperative events: results from pediatric NSQIP. J Pediatr Urol. 2015;11:224, e1–.e6. doi: 10.1016/j.jpurol.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smits A, Lopes A, Das N, et al. Surgical morbidity and clinical outcomes in ovarian cancer—the role of obesity. BJOG. 2016;123:300–308. doi: 10.1111/1471-0528.13585. [DOI] [PubMed] [Google Scholar]
- 13.Bouwman F, Smits A, Lopes A, et al. The impact of BMI on surgical complications and outcomes in endometrial cancer surgery—an institutional study and systematic review of the literature. Gynecol Oncol. 2015;139:369–376. doi: 10.1016/j.ygyno.2015.09.020. [DOI] [PubMed] [Google Scholar]
- 14.Di Capua J, Somani S, Kim JS, et al. Hospital acquired conditions (HACs) in adult spinal deformity surgery: predictors for HACs and other 30-day postoperative outcomes. Spine. 2016;doi: 10.1097/BRS.0000000000001840. [DOI] [PubMed] [Google Scholar]
- 15.Wakefield H, Vaughan-Sarrazin M, Cullen JJ. Influence of obesity on complications and costs after intestinal surgery. Am J Surg. 2012;204:434–440. doi: 10.1016/j.amjsurg.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Davenport DL, Xenos ES, Hosokawa P, Radford J, Henderson WG, Endean ED. The influence of body mass index obesity status on vascular surgery 30-day morbidity and mortality. J Vasc Surg. 2009;49:140–7, 147.e1; discussion147. doi: 10.1016/j.jvs.2008.08.052. [DOI] [PubMed] [Google Scholar]
- 17.Gao M, Sun J, Young N, et al. Impact of body mass index on outcomes in cardiac surgery. J Cardiothorac Vasc Anesth. 2016;doi: 10.1053/j.jvca.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.