Summary
Background
Antilaminin‐332 mucous membrane pemphigoid is a chronic severe pemphigoid disease characterized by autoantibodies to laminin‐332. At present no commercial assay is available to demonstrate antilaminin‐332 antibodies, and diagnosis relies on in‐house techniques with limited sensitivities.
Objectives
In order to move, keratinocytes cultured in vitro secrete laminin‐332 to attach to the culture dish. In that way, they leave behind a unique footprint trail of laminin‐332. We aimed to develop a sensitive and specific laboratory assay to determine antilaminin‐332 autoantibodies in patient serum based on binding of patient IgG to these unique footprints.
Methods
Normal human keratinocytes were grown on glass coverslips and incubated with patient or control serum for 1 h. The binding of IgG was then investigated by immunofluorescence. After validating the test for its ability to identify antilaminin‐332 autoantibodies it was converted into a daily available test based on binding of IgG to dried coverslips that can be stored frozen. The staining patterns of sera from patients with antilaminin‐332 pemphigoid were then compared with those of sera from patients with other autoimmune bullous diseases and normal human sera.
Results
IgG of all antilaminin‐332 pemphigoid sera (n = 16) bound to laminin‐332 footprints, while all normal human controls (n = 55) were negative. From the sera of patients with other diseases (n = 72) four sera tested positive. The footprint assay was also positive for sera that were negative by salt‐split skin analysis, demonstrating that it is a very sensitive technique.
Conclusions
The keratinocyte footprint assay is a fast and specific assay to confirm or rule out the presence of antilaminin‐332 autoantibodies.
What's already known about this topic?
Antilaminin‐332 mucous membrane pemphigoid is a severe form of pemphigoid, and patients may have an increased risk of malignancies.
The diagnosis of antilaminin‐332 mucous membrane pemphigoid is complicated by the lack of specific commercial tests for antilaminin‐332 antibodies and can be confirmed only in specialized laboratories.
Keratinocytes in culture need laminin‐332 for adhesion and migration and therefore deposit it on the bottom of the culture dish.
What does this study add?
The keratinocyte footprint assay detects antilaminin‐332 autoantibodies in patient serum using the native laminin‐332 produced by cultured keratinocytes.
What is the translational message?
The keratinocyte footprint assay is a fast and specific assay to confirm or rule out the presence of antilaminin‐332 autoantibodies.
Short abstract
Linked Comment: https://doi.org/10.1111/bjd.18372.
https://doi.org/10.1111/bjd.18761 available online
Mucous membrane pemphigoid (MMP) is a subepidermal autoimmune blistering disease affecting single or multiple mucous membranes of the mouth, eyes, nasopharynx, oropharynx, larynx and anogenital region, with associated skin involvement in about 30% of cases.1 Formerly termed cicatricial pemphigoid because of the often observed scarring evolution of the lesions, it is associated with autoantibodies directed against different antigens located at the basement membrane zone (BMZ) level.2 These are the intracellular hemidesmosomal protein BP230, the transmembrane hemidesmosomal proteins BP180 and integrin α6β4, and laminin‐332 (Ln‐332). Recent reviews found that 6·4–23·3% of patients with MMP have autoantibodies against Ln‐332, the pathogenicity of which has been proved by passive transfer in mice and human skin graft models.1, 3, 4, 5, 6, 7, 8
Ln‐332, formerly known as kalinin, epiligrin, nicein and laminin‐5, is a heterotrimer that consists of the laminin chains α3, β3 and γ2. In a systematic review of 57 studies, Amber et al. found that for 59 patients the IgG was mostly directed to the α3 subunit (86%), followed by the γ2 subunit (46%) and the β3 subunit (29%).9 Most Ln‐332 is found in the lamina densa and lower lamina lucida underneath hemidesmosomes, and is an essential component of the anchoring filaments that connect the hemidesmosomes via the adhesion receptors integrin α6β4 and BP180 to the underlying anchoring fibrils. Similarly, it binds to integrin α3β1 to bridge focal adhesions and anchoring fibrils.10, 11 Genetic absence of the protein leads to severe generalized junctional epidermolysis bullosa, formerly named type Herlitz, a devastating blistering disease fatal in early childhood.12
Apart from its adhesion function Ln‐332 also has roles in cell migration, tissue maturation and wound repair.13, 14 Since 1997, 36 anti‐Ln‐332 cases have been reported in association with an underlying malignancy.15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 Early studies reported that 20–30% of patients had a solid cancer.30, 32, 33, 34 However, later studies found no statistically significant differences for the occurrence of cancer between Ln‐332 and non‐Ln‐332 MMP, and according to Bernard et al. the prevalence rate of cancer in patients with MMP did not differ from that of the general population in the same age range in France.3, 4, 5
Laboratory diagnosis of anti‐Ln‐332 is complicated. Immunofluorescence analysis of a skin biopsy and serum can give clues but not a definitive diagnosis. The IgG deposition at the BMZ of a skin biopsy is n‐serrated as in pemphigoid diseases, with antibodies to BP180 or p200. Indirect immunofluorescence (IIF) on salt‐split skin (SSS) substrate serum shows binding of IgG to the floor of the blister, as do antibodies to type VII collagen and p200. The combination of n‐serrated deposition and floor binding thus leaves a diagnosis of either anti‐p200 or anti‐Ln‐332 pemphigoid. The final diagnosis therefore relies on the identification of anti‐Ln‐332 antibodies, and as commercial tests for this are not available, this is mainly achieved in specialized laboratories that have in‐house techniques such as immunoprecipitation, immunoblot, enzyme‐linked immunosorbent assay (ELISA) or knockout analysis.3, 35, 36
As elegantly shown by Frank and Carter, keratinocytes in culture need Ln‐332 to attach to the surface of the culture dish.14 When migrating, the cells polarize and deposit precursor Ln‐332 at the rear of the moving cell. This Ln‐332 is left behind and forms a unique footprint trail. We made use of this phenomenon to develop a fast and simple serum assay that discriminates anti‐Ln‐332 MMP from all other forms of pemphigoid diseases.
Materials and methods
Human sera
Sixteen sera from patients with anti‐Ln‐332 MMP were included in the study. One (patient 16) had IgG to both Ln‐332 and type VII collagen, and one (patient 12) had Orf‐induced anti‐Ln‐332 pemphigoid.37, 38 IIF on SSS was positive for dermal IgG binding in 15 cases, and one was judged as dubious. The final diagnosis was achieved by either immunoblot analysis, immunoprecipitation, ELISA or IIF knockout analysis on type VII collagen‐deficient skin and Ln‐332‐deficient skin (Table 1). We further included 25 sera that also stained the floor of SSS, 12 sera from patients with epidermolysis bullosa acquisita (EBA) and 13 sera from patients with anti‐p200 pemphigoid. All patients with EBA had u‐serrated IgG deposition on the BMZ on direct immunofluorescence and dermal staining on SSS IIF. The anti‐p200 pemphigoid had been characterized by immunoblot and IIF on type VII collagen and Ln‐332‐deficient skin.39
Table 1.
Diagnostic findings in 16 patients with antilaminin‐332 mucous membrane pemphigoid
| Sample | Sex | Age (years) | DIF (BMZ) | SSS dermal binding | IB Ln‐332 | IP Ln‐332 | ELISA | IIF (KO skin) | Cancer | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ln‐332 | Col7 | Col7 | Ln‐332 | ||||||||
| 1 | M | 54 | IgG 4+, C3c 3+, IgA 2+, IgM 2+ | IgG 3+, IgA+ | Neg | np | np | − | + | − | Yes |
| 2 | F | 59 | Neg | IgG 2+ | α3, β3 | np | np | − | + | − | No |
| 3 | M | 65 | IgG 3+, C3c 2+, IgA 1+ | IgG 1+ | α3 | np | np | np | np | np | No |
| 4 | F | 86 | IgG 3+, C3c 3+, IgA 2+, IgM ± | IgG 1+ | γ2 | np | np | − | + | − | No |
| 5a | M | 27 | IgG 2+, C3c 3+ | IgG 2+ | α3 | np | + | − | np | np | No |
| 6a | M | 25 | IgG 3+,C3c 3+ | IgG 2+ | α3 | np | + | − | np | np | No |
| 7a | F | 65 | IgG 3+, C3c +/2+ | IgG 2+ | α3 | np | + | np | np | np | No |
| 8a | F | 42 | IgG 3+, C3c 2+ | IgG 2+ | α3 | np | + | − | np | np | No |
| 9a | M | 70 | IgG 2+ | IgG 1+ | α3 | + | np | np | np | np | Yes |
| 10 | M | 82 | IgG 3+, C3c 3+ | IgG 3+ | α3, β3, γ2 | np | np | − | np | np | No |
| 11 | M | 77 | np | IgG 2+ | α3, β3 | np | np | − | + | − | na |
| 12b | F | 52 | IgG 3+, C3c 3+, IgA 1+ | IgG 2+ | Neg | np | np | − | + | − | No |
| 13 | M | 81 | np | IgG 3+ | α3 | np | np | np | np | np | na |
| 14a | M | 56 | IgG 2+, IgA 2+ | IgG dubious | α3 | np | + | np | np | np | Yes |
| 15 | M | 63 | IgG 3+, C3c 2+ | IgG 1+ | α3 | np | np | np | np | np | na |
| 16a , c | F | 64 | IgG 3+/4+, C3c +/2+ | IgG 3+ | α3 | − | + | np | np | np | No |
BMZ, basement membrane zone; Col7, type VII collagen; DIF, direct immunofluorescence; ELISA, enzyme‐linked immunosorbent assay; F, female; IB, immunoblot; IIF, indirect immunofluorescence; IP, immunoprecipitation; KFA, keratinocyte footprint assay; Ln‐332, laminin‐332; M, male; na, not available; Neg, negative; np, not performed; SSS, salt‐split skin. IP was performed with radiolabelled human keratinocyte extract.34 IB was performed for all sera on extract of cultured keratinocytes, and for sera of patients 7, 9 and 16 also on human keratinocyte matrix proteins. ELISA for anti‐Col7 was performed with a kit from MBL (Nagoya, Japan) and ELISA for anti‐Ln‐332 was performed on affinity‐purified Ln‐332 as described previously.34 a–cDescribed previously by aTerra et al.;34 bvan den Bos et al.38 and cJonkman et al.37
We also included 55 sera from patients who also had mucosal lesions but who had not been diagnosed with anti‐Ln‐332 MMP. These were 30 MMP sera from which 15 labelled the roof of SSS and 15 were negative on SSS, 10 sera from patients with erosive lichen planes, 11 sera from patients with paraneoplastic pemphigus, two sera from patients with erythema exsudativum multiforme, and two sera that stained both the roof and floor of SSS. Also included were seven sera from patients with bullous pemphigoid (BP) that stained the epidermal side of SSS and recognized BP180 and/or BP230 by immunoblot and/or ELISA. As controls we used 55 normal human sera.
Keratinocyte footprint assay on living keratinocyte substrate
Primary normal human keratinocytes (NHKs) were isolated from redundant healthy skin obtained from breast reduction surgery upon written informed consent. NHKs were grown on 12‐mm‐diameter glass coverslips (Thermo Fisher Scientific Inc., Waltham, MA, U.S.A.) in 24‐well plates using CnT‐Prime medium (CELLnTEC, Bern, Switzerland) at 37 °C and 5% CO2. Keratinocytes were seeded at a density of 1 × 104 cells in 500 μL medium in a 1·9‐cm2 well, and after 3 days of culture the coverslips were incubated with 200 μL 2·5% serum in medium for 1 h at 37 °C. The cells were then rinsed three times with phosphate‐buffered saline (PBS), fixed in 2% formaldehyde for 10 min and stored frozen at −80 °C until staining. Fixed keratinocytes were stained using 1 : 400 DyLight488‐labelled goat antihuman IgG (Thermo Fisher Scientific Inc.) in PBS containing 1% ovalbumin (PBS/OVA).
Keratinocyte footprint assay on air‐dried frozen keratinocyte substrate
NHKs were cultured as described above and after 3 days they were rinsed three times with PBS and air dried. Cells were stored frozen at −80 °C until further use. After thawing, the coverslips were incubated with 1 : 10 serum in PBS/OVA for 1 h at 37 °C. After three washes in PBS, they were stained with 1 : 400 DyLight488‐labelled goat antihuman IgG in PBS/OVA. Of five sera where the corresponding biopsy had additional linear IgA BMZ deposition, incubated coverslips were also stained with 1 : 400 DyLight488‐labelled goat antihuman IgA (Bethyl Laboratories, Montgomery, TX, U.S.A.) in PBS/OVA.
Immunofluorescence microscopy
To visualize Ln‐332 we used monoclonal antibodies for all of the separate chains: clone 546215 for the α3 subunit, K140 for the β3 subunit and D4B5 for the γ2 subunit. Type VII collagen was stained with monoclonal LH7·2 and BP180/LAD‐1 with monoclonal 233. As a secondary step we used Alexa 488‐conjugated goat antimouse IgG, and in case of double staining Alexa 568‐conjugated goat antimouse IgG (Thermo Fisher Scientific Inc.). All coverslips were examined with a Leica DMRA fluorescence microscope and images were acquired with a Leica DFC350 FX digital camera (Leica, Wetzlar, Germany).
Results
Keratinocytes in culture deposit laminin‐332 but not type VII collagen or BP180
When we stained coverslips with monoclonal antibodies to Ln‐332, binding was observed outside cells in a pattern described before as migration trails. The same pattern was obtained for the α3, β3 and γ2 chains, showing that each subunit is available on the coverslip. In contrast, monoclonal antibodies to the ectodomain of BP180, which is shed in culture, and type VII collagen did not bind outside cells (Fig. 1). Therefore, cultured keratinocytes could potentially be used in a diagnostic assay for anti‐Ln‐332 MMP.
Figure 1.
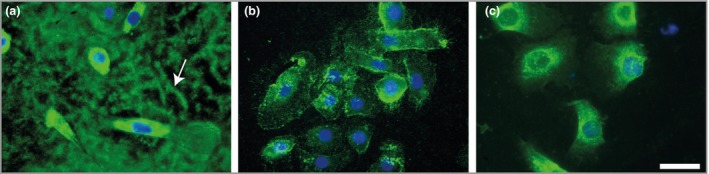
Keratinocytes deposit laminin‐332 but not type VII collagen or the ectodomain of BP180 on the bottom of the culture dish. Air‐dried coverslips were stained for (a) the laminin‐332 β3 subunit, (b) the BP180 ectodomain and (c) type VII collagen. Only laminin‐332 is present as footprints. The white bar represents 20 μm.
Keratinocyte footprint assay on a living keratinocyte substrate
The anti‐Ln‐332 patient IgG that bound to the coverslips in the footprint pattern colocalized with the binding of monoclonal antibodies to all three laminin chains (Fig. 2 shows overlap with the γ2 subunit). Such footprints were observed for all anti‐Ln‐332 pemphigoid sera, including those that were negative in SSS IIF (Fig. 33a–c). All of the EBA, anti‐p200, bullous pemphigoid and normal control group sera did not show any binding to the Ln‐332 footprints, except one (Fig. 33d–l). The exception was a patient with anti‐p200 pemphigoid who was positive for anti‐p200 IgG by immunoblot and whose serum also bound to Ln‐332‐deficient skin (not shown). Sera from six of the seven patients with bullous pemphigoid bound to the membrane of the cells, in line with the accessibility of the BP180 ectodomain.
Figure 2.
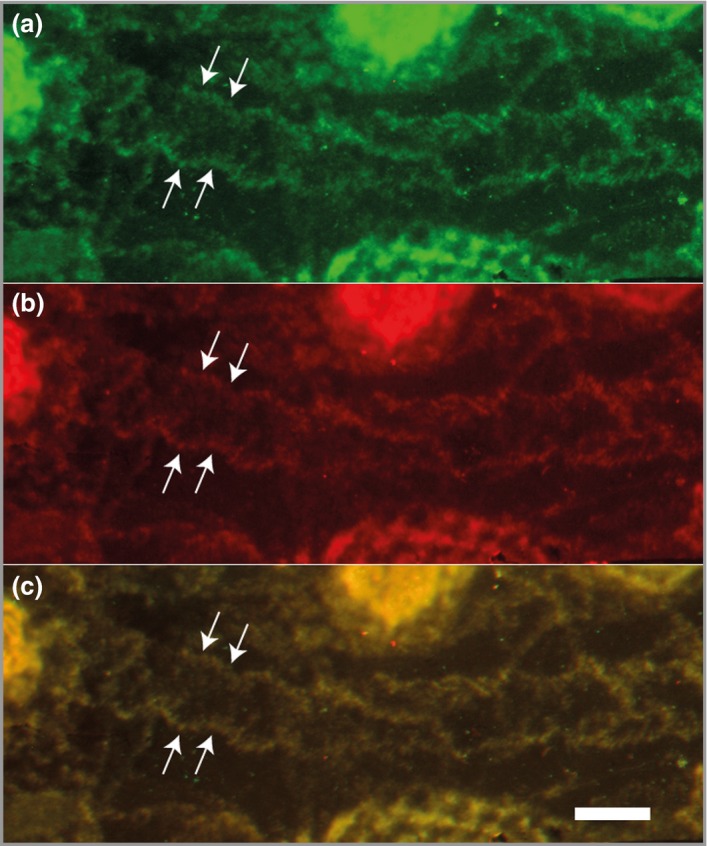
Patient IgG binds to deposited laminin‐332. Double staining of living cells incubated with antilaminin‐332 patient IgG for (a) human IgG and (b) the laminin‐332 γ2 subunit shows complete colocalization in the merged panel (c). The white bar represents 50 μm.
Figure 3.
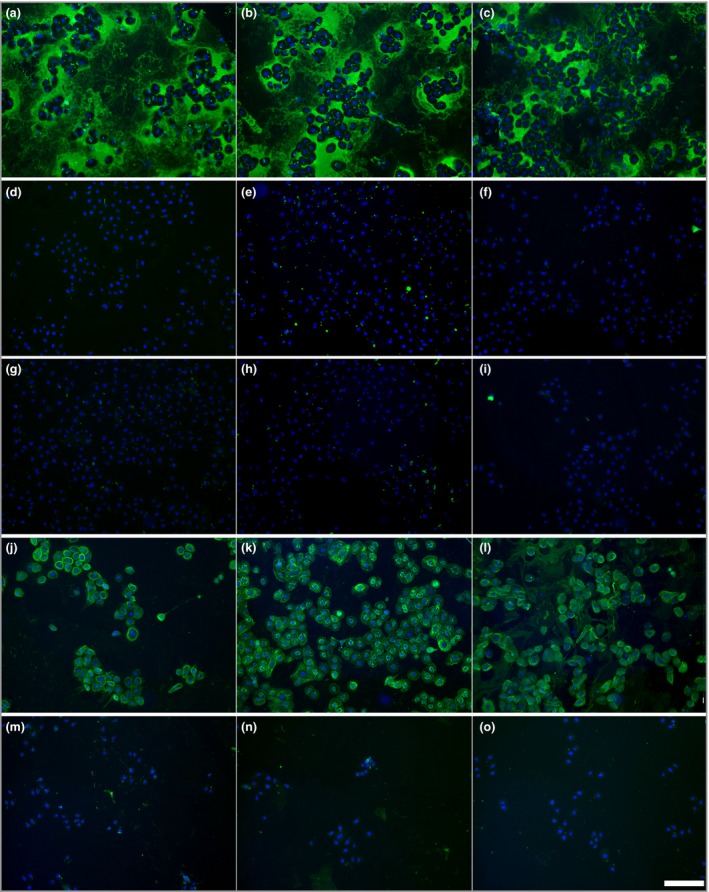
IgG binding patterns after incubation of different types of pemphigoid sera with living keratinocytes. Binding patterns after 1‐h incubation with sera of patients with (a–c) antilaminin‐332 mucous membrane pemphigoid, (d–f) epidermolysis bullosa acquisita, (g–i) anti‐p200 pemphigoid and (j–l) bullous pemphigoid and (m–o) normal human control sera. The white bar represents 150 μm.
Keratinocyte footprint assay on air‐dried frozen keratinocyte substrate
As living cell incubation is labour intensive we tested whether patient IgG would also bind to footprints on coverslips that after 3 days had been air dried and frozen. The results were identical to the living cell incubation in terms of binding to laminin (Fig. 4). Tests performed on coverslips stored for 18 months at −30 °C gave the same results as freshly frozen coverslips (not shown). The only difference from living cell assays was that all sera also bound to the cells, as the cytoplasm of dried cells is accessible to IgG and this contains newly synthesized but not yet secreted antigens. We also tested the sera of five patients who had, besides IgG, deposition of IgA along the BMZ, although only one serum sample bound with IgA to the floor of SSS. Of these five sera the IgA of two bound to the laminin footprints. Furthermore, we screened the 55 sera of patients with mucosal lesions that had not been diagnosed as anti‐Ln‐332 MMP. We found that in four cases IgG was present that bound to the Ln‐332 on the coverslip.
Figure 4.
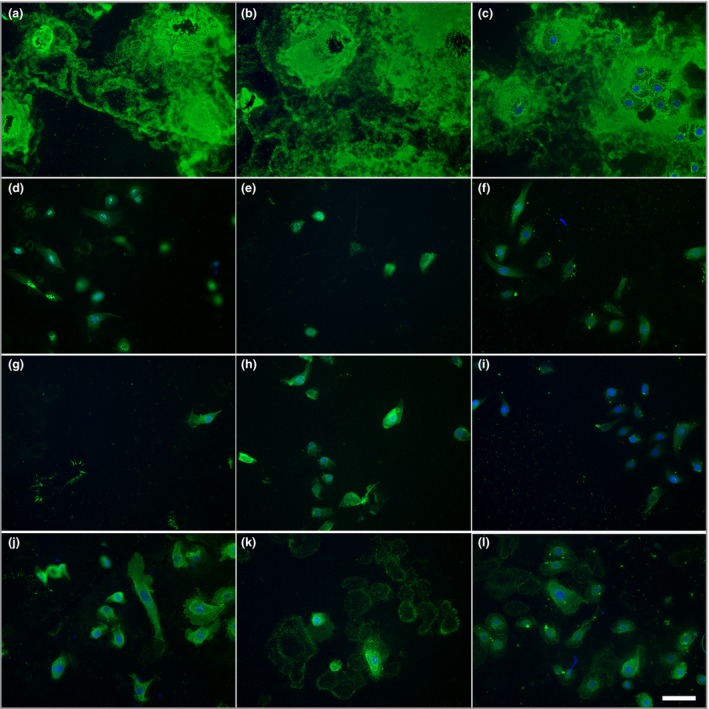
IgG binding patterns after incubation of different types of pemphigoid sera with air‐dried coverslips. Binding patterns of sera of patients with (a–c) antilaminin‐332 mucous membrane pemphigoid, (d–f) epidermolysis bullosa acquisita, (g–i) anti‐p200 pemphigoid and (j–l) bullous pemphigoid. The white bar represents 60 μm.
Discussion
Specific commercial tests to detect anti‐Ln‐332 autoantibodies are lacking, which results in missed or delayed diagnoses of anti‐Ln‐332 MMP. Of tests that have been developed in house, immunoprecipitation using radiolabelled keratinocyte extracts is the most sensitive and specific, but it is restricted to specialized laboratories. It is labour intensive and its high costs and risks do not make it a practical test. Immunoblot analysis has a lower and also variable sensitivity due to the amount of Ln‐332 in the substrate and the absence of conformational epitopes.35, 40, 41 A commercial ELISA for anti‐Ln‐332 IgG is not available, but a few in‐house ELISAs have been developed by independent laboratories with varying success. The first reported ELISA for anti‐Ln‐332 used a recombinant form of Ln‐332. Its sensitivity was 91% but specificity was low as it was also positive for 40% of tested bullous pemphigoid sera.42
Extraction of the extracellular matrix that keratinocytes deposit on the bottom of the culture dish results in a substrate that is extremely rich in Ln‐332.43 When this substrate was used in ELISA a high number of false‐positives were again found in the bullous pemphigoid group when polyclonal secondary antibodies were used, but when a monoclonal antibody to IgG4 was used as a secondary antibody the sensitivity became 91% with a specificity of 98%, although here also 13% of the bullous pemphigoid patient sera tested positive. More recently an ELISA based on purified Ln‐332 from SCC25 cells found only 2% positives in BP and 9% in hospitalized patients without autoimmune bullous disease; however, the sensitivity and specificity were not provided.5
The keratinocyte footprint assay we developed is based on the exclusive binding of anti‐Ln‐332 IgG to the deposited extracellular matrix Ln‐332. No deposition of type VII collagen or the shed ectodomain of BP180 was found on the plate, although it is known that both proteins are secreted in the medium.44, 45 Also, the laminin γ1 chain is not deposited on the culture dish, as reported before.46 In our series, all sera from patients diagnosed with anti‐Ln‐332 MMP tested positive for footprint binding, while all 55 normal human control sera tested negative. IgG of 24 EBA and anti‐p200 pemphigoid sera, which, as with anti‐Ln‐322, also bind the floor of SSS, did not bind to the footprints. For one case that had proven anti‐p200 IgG antibodies we found that the serum also contained antibodies to Ln‐332 as it bound to the footprints, making this case mixed anti‐p200 and anti‐Ln‐332 pemphigoid. IgG of six bullous pemphigoid sera bound to living cells in line with the accessibility of the BP180 ectodomain. One case that by immunoblot and ELISA only demonstrated IgG to BP230 did not bind to the cells in accordance with the cytoplasmic location of BP230 (not shown).
Together these results demonstrate that the specificity of the assay is probably close to 100%. When we analysed patients with non‐Ln‐332 MMP we found no binding for sera from patients with oral erosive lichen planus or erythema exsudativum multiforme. One of the 11 cases of paraneoplastic pemphigus also demonstrated anti‐Ln‐332 IgG. A similar case of paraneoplastic pemphigus with additional anti‐Ln‐332 IgG has been described before.47
One of the two sera that stained both the roof and floor of SSS was also positive for anti‐Ln‐332. Such cases have been described before by Hayakawa et al.3 Two of the other 30 MMP sera also contained anti‐Ln‐332 IgG antibodies. One serum sample was from a patient who had oral, nasal, pharyngeal and laryngeal mucous membranes affected without skin involvement. A skin biopsy demonstrated BMZ deposition of IgG and IgA; however, all serology was negative. Based on the positive keratinocyte footprint assay a final diagnosis of anti‐Ln‐332 MMP was made. The other serum sample bound the roof of SSS and was anti‐NC16A ELISA positive; immunoblotting demonstrated both anti‐BP180 IgG and IgA antibodies.
The concomitant presence of antibodies to Ln‐332 and BP180 has been described already several times.24, 48, 49 These last two patients show that a small percentage of patients with MMP who are not initially diagnosed with anti‐Ln‐332 MMP may have antibodies to Ln‐332. Although the titres are below the detection level of SSS IIF the antibodies might still contribute to the clinical phenotype. However, this has to await a larger series of patients to compare the clinical details of those with and without additional anti‐Ln‐332 antibodies.
The possibility to perform the keratinocyte footprint assay on freezer‐stored coverslips makes it a practical assay that within a few hours will confirm or rule out anti‐Ln‐332 MMP. If a biopsy is available, it is possible to discriminate most cases with IIF SSS floor‐binding sera between EBA, anti‐Ln‐332 pemphigoid and anti‐p200 pemphigoid. In EBA the IgG BMZ deposition in the biopsy will be u‐serrated; if the deposition in the biopsy is n‐serrated then sera with a positive keratinocyte footprint assay are from patients with anti‐Ln‐332 pemphigoid and sera that are negative are from patients with anti‐p200 (Fig. 5).
Figure 5.
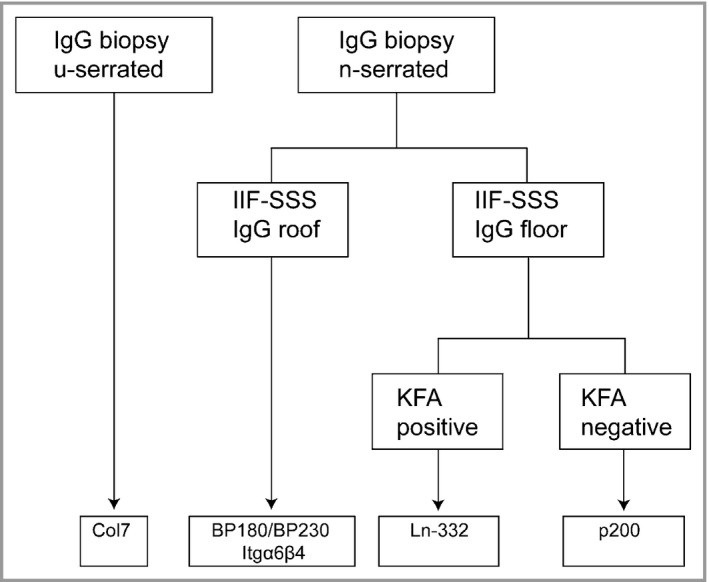
Flowchart for the diagnosis of different subtypes of pemphigoid diseases. By combining (i) the serration pattern of basement membrane zone deposition in the skin, (ii) indirect immunofluorescence (IIF) of serum on salt‐split skin (SSS) and (iii) the keratinocyte footprint assay (KFA), rapid identification of the antigens recognized can be achieved. Col7, type VII collagen; Itgα6β4, integrin α6β4; Ln‐332, laminin‐332.
The keratinocyte footprint assay that we report here represents a simple and reliable assay for routine diagnostics that rapidly identifies the presence of anti‐Ln‐332 antibodies. The keratinocyte footprint assay could be of help for prospective case–control studies to demonstrate or not the reality of the association of Ln‐332 MMP with cancer.
Supporting information
Powerpoint S1 Journal Club Slide Set.
Funding sources None.
Conflicts of interest None to declare.
https://doi.org/10.1111/bjd.18761 available online
References
- 1. Chan LS, Ahmed AR, Anhalt GJ et al The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol 2002; 138:370–9. [DOI] [PubMed] [Google Scholar]
- 2. Amber KT, Murrell DF, Schmidt E et al Autoimmune subepidermal bullous diseases of the skin and mucosae: clinical features, diagnosis, and management. Clin Rev Allergy Immunol 2018; 54:26–51. [DOI] [PubMed] [Google Scholar]
- 3. Hayakawa T, Furumura M, Fukano H et al Diagnosis of oral mucous membrane pemphigoid by means of combined serologic testing. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 117:483–96. [DOI] [PubMed] [Google Scholar]
- 4. Cozzani E, Di Zenzo G, Calabresi V et al Autoantibody profile of a cohort of 78 Italian patients with mucous membrane pemphigoid: correlation between reactivity profile and clinical involvement. Acta Derm Venereol 2016; 96:768–73. [DOI] [PubMed] [Google Scholar]
- 5. Bernard P, Antonicelli F, Bedane C et al Prevalence and clinical significance of anti‐laminin 332 autoantibodies detected by a novel enzyme‐linked immunosorbent assay in mucous membrane pemphigoid. JAMA Dermatol 2013; 149:533–40. [DOI] [PubMed] [Google Scholar]
- 6. Chan LS, Majmudar AA, Tran HH et al Laminin‐6 and laminin‐5 are recognized by autoantibodies in a subset of cicatricial pemphigoid. J Invest Dermatol 1997; 108:848–53. [DOI] [PubMed] [Google Scholar]
- 7. Lazarova Z, Yee C, Darling T et al Passive transfer of anti‐laminin 5 antibodies induces subepidermal blisters in neonatal mice. J Clin Invest 1996; 98:1509–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lazarova Z, Hsu R, Yee C, Yancey KB. Human anti‐laminin 5 autoantibodies induce subepidermal blisters in an experimental human skin graft model. J Invest Dermatol 2000; 114:178–84. [DOI] [PubMed] [Google Scholar]
- 9. Amber KT, Bloom R, Hertl M. A systematic review with pooled analysis of clinical presentation and immunodiagnostic testing in mucous membrane pemphigoid: association of anti‐laminin‐332 IgG with oropharyngeal involvement and the usefulness of ELISA. J Eur Acad Dermatol Venereol 2016; 30:72–7. [DOI] [PubMed] [Google Scholar]
- 10. Aumailley M, El Khal A, Knoss N, Tunggal L. Laminin 5 processing and its integration into the ECM. Matrix Biol 2003; 22:49–54. [DOI] [PubMed] [Google Scholar]
- 11. Rousselle P, Beck K. Laminin 332 processing impacts cellular behavior. Cell Adh Migr 2013; 7:122–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yuen WY, Lemmink HH, van Dijk‐Bos KK et al Herlitz junctional epidermolysis bullosa: diagnostic features, mutational profile, incidence and population carrier frequency in the Netherlands. Br J Dermatol 2011; 165:1314–22. [DOI] [PubMed] [Google Scholar]
- 13. Nguyen BP, Gil SG, Carter WG. Deposition of laminin 5 by keratinocytes regulates integrin adhesion and signaling. J Biol Chem 2000; 275:31896–907. [DOI] [PubMed] [Google Scholar]
- 14. Frank DE, Carter WG. Laminin 5 deposition regulates keratinocyte polarization and persistent migration. J Cell Sci 2004; 117:1351–63. [DOI] [PubMed] [Google Scholar]
- 15. Sadler E, Lazarova Z, Sarasombath P, Yancey KB. A widening perspective regarding the relationship between anti‐epiligrin cicatricial pemphigoid and cancer. J Dermatol Sci 2007; 47:1–7. [DOI] [PubMed] [Google Scholar]
- 16. Gibson GE, Daoud MS, Pittelkow MR. Anti‐epiligrin (laminin 5) cicatricial pemphigoid and lung carcinoma: coincidence or association? Br J Dermatol 1997; 137:780–2. [PubMed] [Google Scholar]
- 17. Lenz P, Hsu R, Yee C et al Cicatricial pemphigoid with autoantibodies to laminin 5 (epiligrin) in a patient with metastatic endometrial carcinoma. Hautarzt 1998; 49:31–5. [DOI] [PubMed] [Google Scholar]
- 18. Setterfield J, Shirlaw PJ, Lazarova Z et al Paraneoplastic cicatricial pemphigoid. Br J Dermatol 1999; 141:127–31. [DOI] [PubMed] [Google Scholar]
- 19. Uchiyama K, Yamamoto Y, Taniuchi K et al Remission of antiepiligrin (laminin‐5) cicatricial pemphigoid after excision of gastric carcinoma. Cornea 2000; 19:564–6. [DOI] [PubMed] [Google Scholar]
- 20. Fukushima S, Egawa K, Nishi H et al Two cases of anti‐epiligrin cicatricial pemphigoid with and without associated malignancy. Acta Derm Venereol 2008; 88:484–7. [DOI] [PubMed] [Google Scholar]
- 21. Shibuya T, Komatsu S, Takahashi I et al Mucous membrane pemphigoid accompanied by ovarian cancer: a case with autoantibodies solely against γ2‐subunit of laminin‐332. J Dermatol 2012; 39:882–4. [DOI] [PubMed] [Google Scholar]
- 22. Mitsuya J, Hara H, Ito K et al Metastatic ovarian carcinoma‐associated subepidermal blistering disease with autoantibodies to both the p200 dermal antigen and the γ2 subunit of laminin 5 showing unusual clinical features. Br J Dermatol 2008; 158:1354–7. [DOI] [PubMed] [Google Scholar]
- 23. Takahara M, Tsuji G, Ishii N et al Mucous membrane pemphigoid with antibodies to the β3 subunit of laminin 332 in a patient with acute myeloblastic leukemia and graft‐versus‐host disease. Dermatology 2009; 219:361–4. [DOI] [PubMed] [Google Scholar]
- 24. Demitsu T, Yoneda K, Iida E et al A case of mucous membrane pemphigoid with IgG antibodies against all the α3, β3 and γ2 subunits of laminin‐332 and BP180 C‐terminal domain, associated with pancreatic cancer. Clin Exp Dermatol 2009; 34:e992–4. [DOI] [PubMed] [Google Scholar]
- 25. Dainichi T, Hirakawa Y, Ishii N et al Mucous membrane pemphigoid with autoantibodies to all the laminin 332 subunits and fatal outcome resulting from liver cirrhosis and hepatocellular carcinoma. J Am Acad Dermatol 2011; 64:1199–200. [DOI] [PubMed] [Google Scholar]
- 26. Ding DC, Chu TY, Hsu YH. Remission of anti‐epiligrin cicatricial pemphigoid after excision of cervical adenocarcinoma. J Cutan Pathol 2014; 41:692–3. [DOI] [PubMed] [Google Scholar]
- 27. Young AL, Bailey EE, Colaco SM et al Anti‐laminin‐332 mucous membrane pemphigoid associated with recurrent metastatic prostate carcinoma: hypothesis for a paraneoplastic phenomenon. Eur J Dermatol 2011; 21:401–4. [DOI] [PubMed] [Google Scholar]
- 28. Fukuchi O, Suko A, Matsuzaki H et al Anti‐laminin‐332 mucous membrane pemphigoid with autoantibodies to α3, β3 and γ2 subunits of laminin‐332 as well as to BP230 and periplakin associated with adenocarcinoma from an unknown primary site. J Dermatol 2013; 40:61–2. [DOI] [PubMed] [Google Scholar]
- 29. Lambiel S, Dulguerov P, Laffitte E, Leuchter I. Paraneoplastic mucous membrane pemphigoid with ocular and laryngeal involvement. BMJ Case Rep 2017; 2017:220887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matsushima S, Horiguchi Y, Honda T et al A case of anti‐epiligrin cicatricial pemphigoid associated with lung carcinoma and severe laryngeal stenosis: review of Japanese cases and evaluation of risk for internal malignancy. J Dermatol 2004; 31:10–15. [DOI] [PubMed] [Google Scholar]
- 31. Yamada H, Nobeyama Y, Matsuo K et al A case of paraneoplastic pemphigus associated with triple malignancies in combination with antilaminin‐332 mucous membrane pemphigoid. Br J Dermatol 2012; 166:230–1. [DOI] [PubMed] [Google Scholar]
- 32. Egan CA, Lazarova Z, Darling TN et al Anti‐epiligrin cicatricial pemphigoid and relative risk for cancer. Lancet 2001; 357:1850–1. [DOI] [PubMed] [Google Scholar]
- 33. Egan CA, Lazarova Z, Darling TN et al Anti‐epiligrin cicatricial pemphigoid: clinical findings, immunopathogenesis, and significant associations. Medicine (Baltimore) 2003; 82:177–86. [DOI] [PubMed] [Google Scholar]
- 34. Terra JB, Pas HH, Hertl M et al Immunofluorescence serration pattern analysis as a diagnostic criterion in antilaminin‐332 mucous membrane pemphigoid: immunopathological findings and clinical experience in 10 Dutch patients. Br J Dermatol 2011; 165:815–22. [DOI] [PubMed] [Google Scholar]
- 35. Lazarova Z, Sitaru C, Zillikens D, Yancey KB. Comparative analysis of methods for detection of anti‐laminin 5 autoantibodies in patients with anti‐epiligrin cicatricial pemphigoid. J Am Acad Dermatol 2004; 51:886–92. [DOI] [PubMed] [Google Scholar]
- 36. Vodegel RM, Kiss M, Cjm De Jong M et al The use of skin substrates deficient in basement membrane molecules for the diagnosis of subepidermal autoimmune bullous disease. Eur J Dermatol 1998; 8:83–5. [PubMed] [Google Scholar]
- 37. Jonkman MF, Schuur J, Dijk F et al Inflammatory variant of epidermolysis bullosa acquisita with IgG autoantibodies against type VII collagen and laminin α3. Arch Dermatol 2000; 136:227–31. [DOI] [PubMed] [Google Scholar]
- 38. van den Bos RR, Middelburg T, van Biezen P et al Orf‐induced pemphigoid with antilaminin‐332 antibodies. Br J Dermatol 2012; 167:956–8. [DOI] [PubMed] [Google Scholar]
- 39. Meijer JM, Diercks GF, Schmidt E et al Laboratory diagnosis and clinical profile of anti‐p200 pemphigoid. JAMA Dermatol 2016; 152:897–904. [DOI] [PubMed] [Google Scholar]
- 40. Hisamatsu Y, Nishiyama T, Amano S et al Usefulness of immunoblotting using purified laminin 5 in the diagnosis of anti‐laminin 5 cicatricial pemphigoid. J Dermatol Sci 2003; 33:113–19. [DOI] [PubMed] [Google Scholar]
- 41. Lazarova Z, Hsu R, Yee C, Yancey KB. Antiepiligrin cicatricial pemphigoid represents an autoimmune response to subunits present in laminin 5 (α3β3γ2). Br J Dermatol 1998; 139:791–7. [DOI] [PubMed] [Google Scholar]
- 42. Bekou V, Thoma‐Uszynski S, Wendler O et al Detection of laminin 5‐specific auto‐antibodies in mucous membrane and bullous pemphigoid sera by ELISA. J Invest Dermatol 2005; 124:732–40. [DOI] [PubMed] [Google Scholar]
- 43. Lazarova Z, Salato VK, Lanschuetzer CM et al IgG anti‐laminin‐332 autoantibodies are present in a subset of patients with mucous membrane, but not bullous, pemphigoid. J Am Acad Dermatol 2008; 58:951–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Marinkovich MP, Taylor TB, Keene DR et al LAD‐1, the linear IgA bullous dermatosis autoantigen, is a novel 120‐kDa anchoring filament protein synthesized by epidermal cells. J Invest Dermatol 1996; 106:734–8. [DOI] [PubMed] [Google Scholar]
- 45. Bremer J, Bornert O, Nystrom A et al Antisense oligonucleotide‐mediated exon skipping as a systemic therapeutic approach for recessive dystrophic epidermolysis bullosa. Mol Ther Nucleic Acids 2016; 5:e379. [DOI] [PubMed] [Google Scholar]
- 46. Kariya Y, Sato H, Katou N et al Polymerized laminin‐332 matrix supports rapid and tight adhesion of keratinocytes, suppressing cell migration. PLOS ONE 2012; 7:e35546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sugiura K, Koga H, Ishikawa R et al Paraneoplastic pemphigus with anti‐laminin‐332 autoantibodies in a patient with follicular dendritic cell sarcoma. JAMA Dermatol 2013; 149:111–13. [DOI] [PubMed] [Google Scholar]
- 48. Mulyowa GK, Jaeger G, Sitaru C et al Scarring autoimmune bullous disease in a Ugandan patient with autoantibodies to BP180, BP230, and laminin 5. J Am Acad Dermatol 2006; 54:43. [DOI] [PubMed] [Google Scholar]
- 49. Yasumizu M, Imanishi H, Morita S et al A case of mucous membrane pemphigoid with IgG antibodies against the β3 and γ2 subunits of laminin‐332, and the C‐terminal domain of BP180. Int J Dermatol 2018; 57:86–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Powerpoint S1 Journal Club Slide Set.


