Abstract
Aging population presents a major challenge for many countries in the world and has made the development of efficient means for healthspan extension a priority task for researchers and clinicians worldwide. Anti-aging properties including antioxidant, anti-inflammatory, anti-tumor, and cardioprotective activities have been reported for various phytobioactive compounds (PBCs) including resveratrol, quercetin, curcumin, catechin, etc. However, the therapeutic potential of orally administered PBCs is limited by their poor stability, bioavailability, and solubility in the gastrointestinal tract. Recently, innovative nanotechnology-based approaches have been developed to improve the bioactivity of PBCs and enhance their potential in preventing and/or treating age-associated disorders, primarily those caused by aging-related chronic inflammation. PBC-loaded nanoparticles designed for oral administration provide many benefits over conventional formulations, including enhanced stability and solubility, prolonged half-life, improved epithelium permeability and bioavailability, enhanced tissue targeting, and minimized side effects. The present review summarizes recent advances in this rapidly developing research area.
Keywords: Aging, Age-associated disorder, Phytobioactive compound, Bioavailability, Nanoparticle, Antioxidant, Anti-inflammatory activity
Introduction
Over the past decades, the average life expectancy has been extended in all developed countries. According to the current demographic projections, the number of people over the age of 65 will rise worldwide from 524 million in 2010 to nearly 1.5 billion in 2050 (World Health Organization 2012). However, the trends observed in the rise in longevity are not commonly accompanied by the same trends toward the human healthspan extension (Hansen and Kennedy 2016). A rapid population aging presents an important challenge for most developed countries because aging is a major risk factor for almost all chronic pathological conditions. The incidence of age-associated disorders, including cardiovascular and neurodegenerative diseases, osteoporosis, type 2 diabetes, and different types of cancers, has been rising drastically over the past few decades, and this presents a serious problem for healthcare systems worldwide (Beard and Bloom 2015). Therefore, the development of efficient means for age-related disease prevention and healthspan extension becomes a priority task for policy makers and research organizations (Seals et al. 2016; Yabluchanskiy et al. 2018). Substantial progress in this field depends on our ability to fully decipher the process of aging and to understand and manipulate the basic processes contributing to aging (Crimmins 2015; Vaiserman and Marotta 2016; Vaiserman and Lushchak 2017).
Several compounds have been proposed to offer protection against or alleviate symptoms associated with chronic conditions. Of these, plant-derived natural compounds (phytochemicals) offer great hope for the development of novel drugs and supplements for treating age-related chronic conditions (Martel et al. 2019). Phytochemicals are secondary metabolites that protect plants from a wide range of environmental stresses such as environmental pollutants and microbial infections. Due to these properties, phytochemicals are regarded as promising candidates for the development of healthspan-promoting applications. Dietary supplementations with phytobioactive compounds (PBCs) such as resveratrol, quercetin, curcumin, epigallocatechin gallate, catechin, and sulforaphane have been repeatedly reported to have anti-aging potential (Corrêa et al. 2018; Santín-Márquez et al. 2019). In both animal and human studies, various antioxidant (Franco et al. 2019), anti-inflammatory (Zhu et al. 2018), anti-tumor (Chikara et al. 2018), cardioprotective (Shah et al. 2019), neuroprotective (Sarker and Franks 2018), and other anti-aging activities of these compounds have been repeatedly reported. Moreover, there is evidence that several flavonoids may affect the aging process at the cellular level by suppressing the senescence-associated secretory phenotype (SASP), a fundamental aging process that promotes aging-related systemic inflammation (Lim et al. 2015, 2017; Perrott et al. 2017).
The therapeutic potential of orally administered PBCs is, however, limited due to their low hydrophilicity, intrinsic dissolution rate, chemical instability, low absorption, scarce biodistribution, and poor penetration/accumulation in the body (Khadka et al. 2014). This ultimately governs the rate and extent of oral drug absorption from solid dosage forms and affects their bioavailability in the body. Recently, innovative nanotechnology-based approaches were developed in order to help maintain the bioactivity of PBCs following oral administration. PBC-loaded nanoparticles (NPs) designed for oral administration provide many benefits over conventional formulations, including increased stability, enhanced solubility, prolonged half-life, improved epithelium permeability and bioavailability, enhanced tissue targeting, and minimal side effects (Date et al. 2016; Lin et al. 2017). In recent years, these nanotechnological approaches have been increasingly applied for treating chronic age-related pathological conditions, including cardiovascular diseases (Martín Giménez et al. 2017; Li et al. 2018), neurodegenerative disorders such as Alzheimer’s and Parkinson’s diseases (Silva Adaya et al. 2017), obesity (Zhang et al. 2018), type 2 diabetes (Jeevanandam et al. 2015), and cancer (Iqbal et al. 2018; Qiao et al. 2019). The present review paper is specifically focused on the therapeutic potential of PBC-loaded nanodelivery systems in treating age-associated chronic diseases. For this review, we searched the PubMed database to identify relevant publications and used various combinations of search terms such as: “aging”, “age-related disease”, “anti-inflammatory activity”, “antioxidant”, “phytobioactive compound”, “phytochemical”, “bioavailability”, “nanoparticle”, “nanodelivery”. The search was limited to studies published in the English language from 2006 to the present.
Main types of nanodelivery systems
Nanosystems intended for delivery of therapeutic agents may be classified into two main types: liquid and solid (Borel and Sabliov 2014). Liquid nanosystems include nanoemulsions, nanoliposomes, and nanopolymersomes. Nanoemulsions are mixtures of immiscible liquids, such as water and oil (Jaiswal et al. 2015). The synthesis of nanoemulsions is generally carried out using either mechanical or chemical methods. Mechanical methods include high-energy processes in which larger emulsion droplets are broken down into smaller ones by certain mechanical operations, whereas chemical methods lead to spontaneous formation of emulsion droplets as a consequence of the hydrophobic effects of lipophilic molecules in the presence of emulsifiers. The basic difference between nanoemulsion and conventional emulsion lies in the size and shape of the particles dispersed in the suspension. Ordinarily, the nanoemulsion droplet size falls in the range of 20 to 200 nm.
Nanoliposomes are nanosized self-assembled vesicles composed of phospholipid bilayers entrapping one or more aqueous compartments (Chan and Král 2018). Methods for synthesizing liposomes include gentle hydration and layer-by-layer electrostatic deposition technique. These vesicles may be either unilamellar (~ 100 nm) or multilamellar (ranged from 500 to 5 μm). Importantly, nanoliposome-encapsulated biomaterials are considered to be protected from external conditions.
Nanopolymersomes are stable nanoscale vesicles composed of self-assembling block copolymers with tunable degradation properties (Tuguntaev et al. 2016). They are synthesized by methods similar to those used for producing polymeric NPs. Due to their properties, nanopolymersomes are able to encapsulate hydrophobic or hydrophilic molecules either in the membrane bilayer or in the aqueous core, respectively. Advantages of polymer nanocarriers, compared to lipid carriers, include controlled release and enhanced stability and versatility (Rastogi et al. 2009). Nanopolymersomes are considered to be attractive drug carriers due to their colloidal stability and low membrane fluidity.
Solid nanodelivery systems include nanocrystals, lipid NPs, and polymeric NPs. Nanocrystals are sub-micron (typically 10 to 800 nm) colloidal dispersion systems of pure (carrier-free) drug NPs, produced using mechanical or chemical methods. The main advantage of such NPs is reducing their particle size to nanoscale range, leading to an increase of the particle surface area in contact with the dissolution medium (Gigliobianco et al. 2018). Thereby, nanocrystal formulations have many benefits compared to conventional pharmaceutical formulations. These benefits include, among others, improved dissolution rate and saturation solubility, and also high drug loading (Zhou et al. 2017).
Solid-lipid NPs are similar to nanoemulsions, with the exception that they contain lipids in a solid phase. These NPs are sub-micron colloidal nanocarriers with diameters ranging from 50 to 1000 nm. They are composed of physiological lipids dispersed in water or in aqueous surfactant solutions (Naseri et al. 2015; Mishra et al. 2018; da Silva Santos et al. 2019). These NPs are most commonly produced by high-energy methods such as microfluidization and ultrasonication (Mehnert and Mäder 2001). The advantageous features of these NPs include small size, large surface area, high drug loading, and the interaction of phases at the interface. These types of nanocarriers were developed to overcome limitations of other colloidal nanocarriers (e.g., emulsions, polymeric NPs, and liposomes) since they demonstrate benefits such as targeted drug delivery with excellent physical stability and also a good release profile (Naseri et al. 2015). One more advantage of solid-lipid NPs is that they offer a means of entrapping lipophilic molecules in stable particles without using organic solvents. Due to unique size-dependent properties and capacity to incorporate drugs, solid-lipid NPs provide multiple therapeutic advantages, including feasibility for large-scale production, versatility of incorporation of hydrophilic and lipophilic drugs, high bioavailability of drugs, and low toxicity (Bayón-Cordero et al. 2019).
Polymeric NPs are solid colloidal NPs with a size of 10–1000 nm consisting of natural or synthetic polymers (Crucho and Barros 2017; Khan et al. 2017). Two main strategies for preparation of polymeric NPs are polymerization of monomers and dispersion of preformed polymers (Krishnamoorthy and Mahalingam 2015). They are commonly produced from biodegradable and biocompatible polymers or copolymers, in which drugs may be entrapped or encapsulated within the carriers, and are also physically adsorbed on or chemically linked to their surfaces. Polymeric NPs fall into two main subtypes, namely nanospheres where loaded drugs are uniformly dispersed and nanocapsules where drugs are confined to the inner oily or aqueous cavities surrounded by tiny polymeric membranes (Grottkau et al. 2013). Their attractive properties include stability during storage, water solubility, small size, nontoxicity, biodegradability, and long shelf life (Kamaly et al. 2016). Due to their physico-chemical properties, polymeric NPs have high stability in plasma and good encapsulation efficacy, and also enhanced solubility and stability of hydrophobic drugs. This allows a decrease in their toxicity, permitting a controlled release at target sites at relatively low doses (Kamaly et al. 2016).
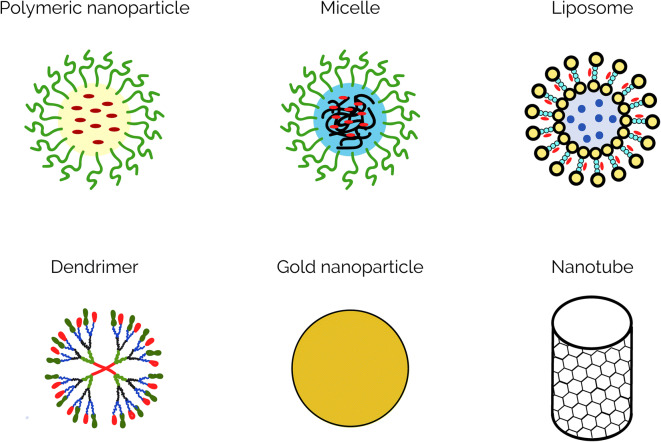
In addition, different types of metallic NPs such as gold, silver, copper, aluminum, magnesium, zinc, and titanium NPs are increasingly used for active or passive drug delivery in various biomedical applications. Metallic NPs with diameters ranging from 1 to 100 nm may be synthesized and modified with different chemical functional groups which allow them to be conjugated with various drugs of interest to specifically target particular cells (Mody et al. 2010). The relatively simple synthesis, biocompatibility, easy chemical modification, and tunable biophysical properties of metallic NPs make them highly advantageous in nanomedicine applications (Lushchak et al. 2018). Some of the most widely used nanodelivery systems are schematically presented in Fig. 1.
Fig. 1.
Graphical representation of the most common types of NPs
Nanocarrier-based drug delivery systems: achievements and perspectives
Oral delivery is regarded as the most accepted mode of drug administration due to the obvious advantages of this route compared to other delivery routes. The advantages include simplicity of administration, high patient compliance, painlessness, outpatient applicability, and easy self-administration (Anselmo and Mitragotri 2014). While advantageous, the efficiency of oral drug delivery may be substantially reduced due to chemical and enzymatic barriers in the gastrointestinal tract. Moreover, low bioavailability of many therapeutic biomolecules in the gastrointestinal tract is related to their poor gastrointestinal solubility. To overcome these limitations, novel and innovative drug delivery systems are currently being developed. The oral delivery of therapeutic compounds such as drugs or bioactive substances loaded onto nanocarrier systems has been a subject of rigorous study over the past few years and has proven to enhance the efficiency of compound delivery for therapeutic purposes (Lin et al. 2017; Kermanizadeh et al. 2018). The loading of drugs or bioactive agents occurs in two ways: they are either integrated in the core matrix of the NPs or attached on the surface (Lin et al. 2017). With respect to pharmacokinetic properties, drugs delivered by nanocarriers commonly exhibit increased half-life, prolonged circulation time, increased mean residence time, and reduced clearance from the body (Ravindran et al. 2018).
Currently, several nanodelivery systems for biotherapeutics are in clinical trials and are increasingly being introduced in clinical practice (Hajialyani et al. 2018). The most urgent challenge now is developing innovative multifunctional nanosized materials capable of specifically targeting particular cell types, tissues or organs, and which also contain functionalities that allow them to transfer therapeutics across biological barriers in the body. Successful drug carrier systems must be characterized by optimum properties for drug loading and release, long storage life, and high therapeutic efficiency with no or negligible side effects (Piazzini et al. 2018). A high therapeutic potential of naturally derived substances motivates nanotechnologists to design innovative nanomaterials that would improve their stability, solubility, specificity, efficiency of cellular uptake/internalization, tolerability, and therapeutic index (Bilia et al. 2017).
In present-day controlled drug delivery and release systems, various sorts of biocompatible drug nanocarriers are applied (for detailed review, see Borel and Sabliov 2014; Bilia et al. 2017; Ganesan et al. 2018a). Numerous materials and structures have been developed as nanocarriers for either passive or active therapeutic targeting. Following passive delivery, the loaded agent is released by the diffusion or erosion of the nanovector. The active delivery mode provides an opportunity for controlled release of the transported molecules at targeted sites by incorporating stimuli-responsive components that may be triggered by specific stimuli, including variations in pH, exposure to light, electric or magnetic field, ultrasound, heating, or contact with concentrated ionic solutions or enzymes (Gu et al. 2018). Metallic NPs such as iron oxide, silver, and gold NPs can be surface-modified to act as drug carriers (Kong et al. 2017). The use of organic materials, however, seems to be preferred in this context since their physicochemical properties may be finely tuned by modifying their size, shape, chemical composition, structural morphology, and surface characteristics (Conte et al. 2017). In NPs and nanocapsules, therapeutic agents may be conjugated to or encapsulated in polymer chains.
Physicochemical characteristics of NPs such as their absorption, distribution, metabolism, and excretion depend on their size, charge, hydrophobicity, and targeted biomolecules. The size of NP is an important parameter that determines its entry into cells, pharmacokinetics, and its interaction with the immune system (Hoshyar et al. 2016). Surface properties of NPs such as their hydrophobicity or hydrophilicity determine many of the biological responses induced by these structures, including interactions with plasma proteins, cellular uptake, phagocytosis, immune responses, and particle removal (Ajdary et al. 2018). Moreover, the cellular uptake and cytotoxicity of medical NPs are largely dependent on their surface charge (Fröhlich 2012). An important feature of orally administered nanomedicines is their ability to overcome the physical and chemical barriers in the intestine, such as the acidic pH of the stomach, the mucosal lining of the intestine, and the selectively permeable enterocyte membranes, all of which govern drug absorption (Moss et al. 2018). Due to these properties, NPs can protect encapsulated bioactive compounds from degradation following gastrointestinal digestion and cellular metabolism. NP-entrapped bioactive compounds are ultimately released in the intestines, in the circulatory system or in the cells of various tissues. The subsequent biological fate of these bioactive compounds depends on their chemical and physical properties and the site of their release. An important point is that the location of bioactive release may be tailored using nanomaterials with specific surface chemistry, thereby enabling the release of these therapeutics in specific tissues (Martínez-Ballesta et al. 2018). In nanomedicine, targeting strategies play a pivotal role in overcoming side effects and minimizing systemic drug administration. These strategies include passive and active targeting (Kydd et al. 2017). Passive targeting is achieved by modifying physiochemical characteristics, hydrophobicity and pH of NPs, and utilizing the enhanced permeability and retention (EPR) effect of inflamed blood vessels. In active targeting, biomarkers such as RNAs, proteins, carbohydrates, lipids, and small metabolite molecules are used to reach particular target sites (Conte et al. 2017). The efficacy of entrapment of PBCs is also dependent on the molecular weights of the compounds loaded onto the NPs. Increasing the molecular weight leads to a decrease in entrapment efficacy of these PBCs, resulting in lower bioavailability (Ganesan et al. 2018b). Each type of nanodelivery system provides distinct health benefits depending on the compatibility of their properties, the properties of the loaded bioactive agents and the desired therapeutic applications (Gupta and Xie 2018; Rizvi and Saleh 2018).
PBC-loaded nanodelivery systems
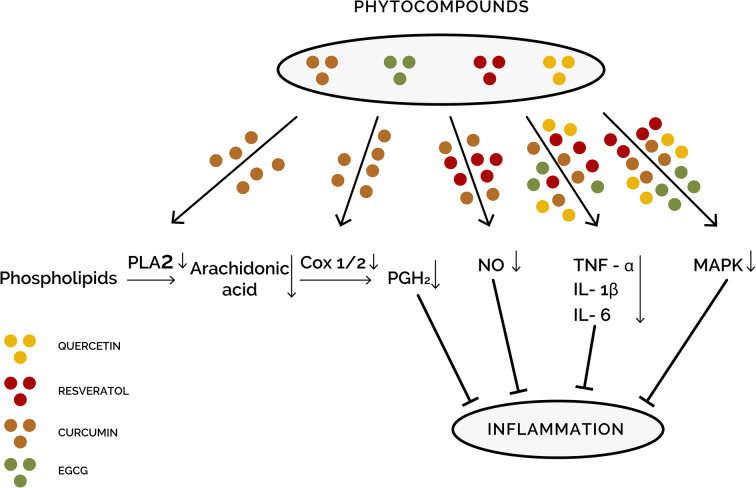
PBCs undoubtedly have great therapeutic potential in treating complex diseases (Chikara et al. 2018; Sarker and Franks 2018; Shah et al. 2019). Many PBC-loaded nanodelivery systems have been repeatedly shown to be efficient in modulating unfavorable processes such as chronic oxidative stress and inflammation that are well-known mediators of most age-associated pathological conditions. A schematic diagram outlining the impact of NP-delivered PBCs on the main cellular pathways involved in inflammation is presented in Fig. 2.
Fig. 2.
Schematic representation of inflammation-related molecular pathways potentially affected by PBC-loaded NPs. The anti-inflammatory effects of such NPs might be mediated through inhibiting the production of nitric oxide (NO) by nitric oxide synthase (iNOS), lowering the levels of prostaglandins and arachidonic acid metabolites through inhibiting phospholipase A2 (PLA2) and cyclooxygenase (COX) pathways, or down-regulating the mitogen-activated protein kinase (MAPK) and nuclear factor kappa B (NF-κB) pathways
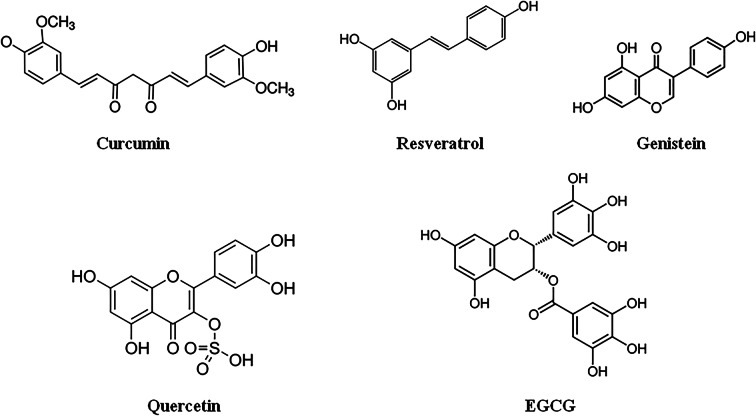
PBC-loaded nanostructures which are the most well studied to date are described in the subsections below. Chemical structures of these PBCs are given in Fig. 3 below.
Fig. 3.
Chemical structures of the most widely used PBCs
Curcumin
Curcumin (diferuloylmethane) is a polyphenol extracted from the rhizome of the Curcuma longa herb, which has been widely used in Asia for centuries as a spice and herbal medicine. It is known for its biological activities that include anti-inflammatory, anti-oxidative, anti-neurodegenerative, and anti-cancer properties that are attributed to its unique molecular structure (Sarker and Franks 2018). The therapeutic potentials of curcumin in treating age-related pathological conditions, such as chronic inflammation, atherosclerosis, hypertension, type 2 diabetes, cardiovascular and neurodegenerative diseases, rheumatoid arthritis, osteoporosis, chronic kidney disorders, ocular diseases, and cancer, have been well documented in the literature (for review, see Sundar et al. 2018). In recent years, the health-promoting and disease-preventing capabilities of this compound have been increasingly examined in clinical trials (Salehi et al. 2019). However, the therapeutic potential of curcumin is currently limited due to its poor bioavailability (Kumar et al. 2010). To overcome these obstacles, the development of nanodelivery systems that improve the therapeutic efficiency of curcumin has been emerging as a promising innovative delivery approach (Flora et al. 2013; Ahmad et al. 2014). Better anti-aging properties of nanocurcumin formulations compared to those of native curcumin have been shown in both in vitro and in vivo studies. By encapsulating curcumin in lipid NPs, nanogels, dendrimers or polymeric NPs, or by conjugating it to metal oxide NPs, the water solubility and bioavailability of this agent have been substantially improved resulting in an increase in its pharmacological efficiency (Shome et al. 2016). For example, the oral bioavailability of poly lactic-co-glycolic acid (PLGA) nano-formulation of curcumin was found to be 22-fold higher than that of conventional curcumin (Tsai et al. 2011). In a cerebral ischemia rat model, the use of curcumin-loaded solid lipid NPs led to a 16 times greater bioavailability of curcumin in the brain as compared with the use of native curcumin (Kakkar et al. 2013). Significantly improved oral bioavailability and brain distribution of curcumin in comparison with free curcumin was also observed in N-trimethyl chitosan surface-modified solid lipid NPs (Ramalingam and Ko 2015). In both in vitro and in vivo models, convincing evidence was also obtained that curcumin-loaded NPs may exert significant antioxidant (Fan et al. 2018) and anti-inflammatory (Wang et al. 2015a; Ameruoso et al. 2017; Dewangan et al. 2017; Li et al. 2017b; El-Naggar et al. 2019) activities.
Quercetin
Quercetin is an important flavonoid present in various fruits, vegetables, grains, and leaves. This compound is well known for its antioxidant, anti-inflammatory, anti-atherosclerotic, anti-obesity, anti-diabetic, anti-hypertensive, and anti-hypercholesterolemic properties (Anand David et al. 2016). However, the health benefits of quercetin are limited due to its relatively low bioavailability (Kawabata et al. 2015; Ganesan et al. 2017). Indeed, initial studies of quercetin pharmacokinetics in humans showed that oral bioavailability of this compound is very low (less than 2% after a single oral dose). The estimated absorption of quercetin glucoside, which is the naturally occurring form of this compound, ranges only from 3 to 17% in healthy individuals per 100 mg of quercetin ingested (Li et al. 2016). Some innovative approaches have been developed in recent years to improve the bioavailability of quercetin. Among them, the nanodelivery approach seems one of the most promising. Recently, quercetin-loaded solid lipid NPs were developed that showed a significantly enhanced bioavailability in comparison with a pure quercetin powder (Vijayakumar et al. 2016). Quercetin-loaded NPs have also been shown to improve antioxidant defense mechanisms in animal models (Chitkara et al. 2012; Alam et al. 2016). Moreover, they were found to exert antioxidant effects and ameliorate inflammatory conditions in different cell lines (Lee et al. 2016).
Resveratrol
Resveratrol is a well-known polyphenolic compound with many pleiotropic activities including anti-aging actions in various model organisms and in humans. The anti-aging effects of resveratrol are attributed to its ability to activate the mammalian silent information regulator 1 (SIRT1), and modulate the activity of numerous proteins, such as peroxisome proliferator-activated receptor coactivator-1α (PGC-1α), Akt/protein kinase B, NF-κβ, and the FOXO family, all of which are known to play important roles in aging processes (Camins et al. 2009). Many of these activities exhibit similar patterns to those seen in calorie restriction (CR) treatments, thereby implicating the potential of resveratrol as a CR mimetic (Li et al. 2017c). To date, the efficiency and safety of resveratrol have been well documented in 244 clinical trials, with an additional 27 clinical trials presently ongoing (Singh et al. 2019). These studies provide evidence for the therapeutic potential of resveratrol in treating various aging-associated conditions including hypertension, obesity, type 2 diabetes, metabolic syndrome, cardiovascular disorders, stroke, breast and colorectal cancers, chronic kidney and inflammatory diseases, and also Alzheimer’s disease (Berman et al. 2017; Singh et al. 2019). Although the clinical usefulness of resveratrol has been well documented, the therapeutic use of this compound is substantially limited due to its rapid metabolism and poor bioavailability (Smoliga and Blanchard 2014; Csiszár et al. 2015). Moreover, resveratrol has very low solubility in water, which results in its poor absorption by oral administration (Chauhan 2015). Many preclinical studies and clinical trials are currently in progress to determine the appropriate dosage of resveratrol for oral administration given its rapid metabolism and to create structurally modified resveratrol derivatives that can have higher bioavailability upon ingestion (Popat et al. 2013). For example, SRT501, a micronized liquid formulation of trans-resveratrol, was shown to possess roughly 5 times higher bioavailability than non-micronized compound (Elliot and Jirousek 2008). However, this formulation was not well tolerated in several clinical trials due to side effects including vomiting and diarrhea in patients, which led to dehydration and renal failure (Popat et al. 2013). As such, there was a strong drive to investigate other formulations that act in a similar manner to SRT501, but with fewer or no side effects (Smoliga et al. 2012). Recently, several nanosized resveratrol-loaded formulations were developed and studied for their potential clinical application. For example, in male Wistar rats, the bioavailability of trans-resveratrol through oral delivery with trans-resveratrol-loaded lipid-core nanocapsules was shown to be 2 times higher in the brain, kidney, and liver when compared to free trans-resveratrol (Frozza et al. 2010). Gastrointestinal safety was also improved compared to free trans-resveratrol in the same animal model. The bioavailability of intravenous administered folate-conjugated human serum albumin-encapsulated resveratrol NPs has been also found to be 6-fold higher than that of free resveratrol (Lian et al. 2019). In several in vitro studies, antioxidant (Chen et al. 2015) and anti-inflammatory (Siu et al. 2018) abilities of resveratrol-loaded NPs have been also reported.
Genistein
Genistein is a soy isoflavonoid with promising therapeutic potential in combating many aging-related pathological conditions, including oxidative stress, inflammation, obesity, type 2 diabetes, cancer, osteoporosis, and neurodegenerative disorders (for review, see Saha et al. 2014). However, a reduced bioavailability of genistein was observed in different animal models. Moreover, higher doses of this estrogen-like substance can lead to toxicity and have endocrine-disrupting effects (Patisaul 2017). Over the past few years, several innovative nanoscale materials have been developed and validated to improve the oral delivery of genistein and to overcome its potential toxic effects (Rassu et al. 2018). Genistein-loaded polymeric micelles showed a higher bioavailability through oral delivery than genistein powder, most likely due to their higher solubility and release in the gastrointestinal tract (Kwon et al. 2007). The oral bioavailability of genistein loaded in solid lipid NPs was also significantly enhanced in rats in comparison with that of bulk powders or suspensions of genistein (Kim et al. 2017). Moreover, a high cytotoxicity of genistein-conjugated gold NPs against cancerous cells was demonstrated in a cell line test (Stolarczyk et al. 2017).
Epigallocatechin-3-gallate
Epigallocatechin-3-gallate (EGCG) is a type of catechin and the most abundantly found type of polyphenol in green tea. It is known to exhibit a variety of healthspan-promoting and anti-aging activities due to its antioxidant, anti-inflammatory, anti-atherogenic, and anti-tumor properties (Singh et al. 2011; Shi et al. 2018). However, the findings obtained in epidemiological studies of this compound are ambiguous and often conflicting with data from in vitro studies. This contradiction may be at least partially due to the compound’s poor stability and low bioavailability (Mereles and Hunstein 2011; Krupkova et al. 2016; Chu et al. 2017). In order to enhance the bioavailability of this PBC and improve its delivery, many nanocarrier-based delivery systems such as solid lipid NPs have been developed (Granja et al. 2017). For example, a study by Frias et al. (2016) showed that EGCG can be successfully loaded onto solid lipid NPs with a particle size of about 300–400 nm. This formulation was shown to have a greater stability and a higher potential for oral delivery than non-processed EGCG. The pH-sensitive EGCG-loaded polymeric NPs were also shown to significantly modify the pharmacokinetic profile of this compound and enhance EGCG bioavailability by more than 2.4-fold compared to EGCG powder alone (Zhang and Zhang 2018). Moreover, an effect of NPs loaded with EGCG on inhibiting breast cancer cells was observed (Zeng et al. 2017). EGCG-loaded NPs were also shown to exert antioxidant (Avadhani et al. 2017) and anti-inflammatory (Wu et al. 2017) effects with in vitro models.
Potential of PBC-loaded nanodelivery systems in prevention and treatment of age-related diseases
Over the last few years, accumulating evidence has shown that PBC-loaded nanodelivery systems may be efficient in preventing and treating a range of age-related pathological conditions. The main findings from these studies are summarized and discussed in subsequent sections.
Metabolic disorders
The prevalence of obesity and other metabolic syndromes including high cholesterol levels, high blood pressure, and insulin resistance is well known to increase significantly with age. The co-occurrence of aging and obesity was shown to substantially increase low-grade inflammation (“inflammaging”), which was found to be an important link between obesity, insulin resistance, and age-related chronic disorders (Frasca et al. 2017). An obesity-related disease such as type 2 diabetes (adult-onset or non-insulin-dependent diabetes) is currently one of the most common age-related chronic disorders around the globe. The pathophysiology of this disease is characterized by impaired glucose metabolism, declining beta-cell function and peripheral insulin resistance (Skyler et al. 2017).
Various PBCs have been used for centuries in treating metabolic disorders, especially in Asian traditional medicine (Governa et al. 2018). Since most PBCs have strong anti-oxidative and anti-inflammatory potentials, recent studies have focused on the anti-obesogenic and anti-diabetic effects of these compounds. For example, long-term green tea intake significantly improved lipid metabolism and reduced waist circumference and body mass index, whereas cocoa decreased blood glucose levels and blood pressure (Amiot et al. 2016). In addition, soy isoflavones such as quercetin, hesperidin, and citrus products improved lipid metabolism and cinnamon reduced blood glucose levels (Amiot et al. 2016). Moreover, the anti-obesity and anti-diabetic effects of PBCs such as curcumin (Wojcik et al. 2018), resveratrol (Hou et al. 2019), genistein (Behloul and Wu 2013), quercetin (Chen et al. 2016), and EGCG (Eng et al. 2018) have been reported in numerous studies. Secondary metabolites derived from seaweeds have also demonstrated substantial anti-obesity and anti-hypertensive properties and could provide additional compounds for dealing with these conditions (Muradian et al. 2015; Seca and Pinto 2018).
The intake of conventional anti-diabetic medications is often associated with long-term side effects. Therefore, the use of PBC-loaded NPs is receiving considerable attention as a promising alternative to synthetic anti-diabetic medications (Anand et al. 2017; Ganesan et al. 2017). In several animal models, orally administered PBC-loaded NPs demonstrated an enhanced anti-diabetic potential compared to native PBCs. For example, NPs loaded with the isoquinoline alkaloid berberine have anti-diabetic properties (Lee 2006) and demonstrated both improved bioavailability and higher anti-diabetic effects in a diabetic mouse model (Xue et al. 2013). More specifically, a substantial suppression of body weight gains and improved glucose tolerance and insulin sensitivity were observed in db/db mice when berberine-loaded NPs were administered. In addition, oral administration of such NPs led to a higher concentration of berberine, which correlated with the suppression of several lipogenic genes such as fatty acid synthase, stearoyl-CoA desaturase, and sterol regulatory element-binding protein 1c, and the induction of the lipolytic carnitine palmitoyltransferase-1 gene in liver of db/db mice (Xue et al. 2015). More recently, significant hypoglycemic effects were revealed in both normal and diabetic rats orally administered with selenium-layered NPs loaded with plant extracts known to exhibit hypoglycemic properties, such as extracts of mulberry leaf and Pueraria lobata (Deng et al. 2019). The same study showed that these NPs can also promote glucose utilization by adipocytes, attenuate the oxidative damage, and enhance pancreatic function. Thus, it is a potential remedy for dealing with diabetes.
Cardiovascular diseases
Many natural polyphenols are also known to have protective effects against atherosclerotic, arteriopathy, and cardiovascular diseases due to their antioxidant, anti-inflammatory, and vascular-protective properties (Alfaras et al. 2016; Campesi et al. 2018). Recently, PBC-loaded nanodelivery systems were developed to improve oral bioavailability and amplify cardioprotective effects of these compounds. For example, solid lipid NPs loaded with puerarin (the major bioactive constituent in kudzu roots widely used in China for the treatment of cardiovascular diseases) showed 3 times higher bioavailability following oral administration in heart and brain compared to free puerarin (Luo et al. 2011). In an in vitro study, attenuation of palmitate-induced cardiomyocyte apoptosis was achieved by inhibiting NADPH-mediated oxidative stress and increasing the Bcl-2/Bax ratio following curcumin-loaded NP treatment in H9C2 embryonic rat heart-derived cells (Li et al. 2017d). Moreover, using colloidal curcumin NPs dissolved in gum ghatti solution led to the restoration of the left ventricular fractional shortening, a deterioration that is associated with heart failure following myocardial infarction in male rats (Sunagawa et al. 2012). Better therapeutic effects against myocardial ischemia-reperfusion injury compared to that of the non-modified extract were observed in rats treated with solid lipid NPs loaded with the total flavonoid extract from Dracocephalum moldavica L. (Tan et al. 2017).
Most aging-associated cardiometabolic disorders are well known to be accompanied by microvascular endothelial dysfunction (Ungvari et al. 2018a, b). Accumulating evidence suggests that this dysfunction may be largely preventable by plant bioactives (Heiss et al. 2018). The supposed mechanisms by which PBCs provide endothelial protection include attenuated level of oxidative stress, enhanced eNOS/NO bioavailability, inhibited NF-κB activity, and also decreased expression of cell adhesion molecules (Monsalve et al. 2017). Therefore, an important question is whether nanodelivery of PBCs could have the potential for prevention and treatment of this dysfunctional condition. However, this potential is still poorly understood and needs further investigation.
Neurodegenerative disorders
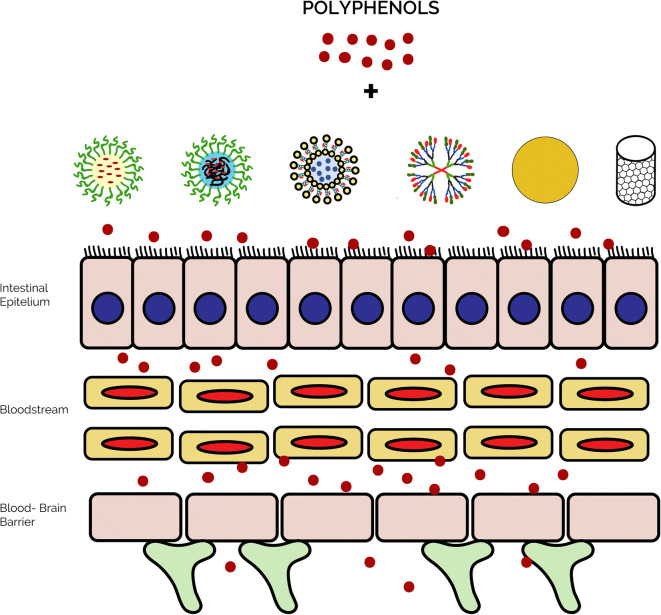
The incidence of age-related neurodegenerative disorders, such as Alzheimer’s and Parkinson’s diseases, has increased dramatically over the last decades and is presenting an important socio-economic problem across most developed countries. The development of effective strategies for the treatment of age-associated neurodegeneration is, therefore, regarded as a public health priority. However, the treatment of these diseases is very difficult due to the existence of the blood-brain barrier. This selective permeability system that acts as a local gateway against circulating foreign substances represents an important challenge in delivering therapeutic agents to the brain. The development of nanotechnology-based systems for brain delivery, such as polymeric and metallic NPs, liposomes, micelles, dendrimers, and carbon nanotubes, is currently being investigated by many researchers and drug designers as a promising solution for addressing this challenge (Teleanu et al. 2018; Saeedi et al. 2019); see Fig. 4 for schematic representation.
Fig. 4.
Schematic representation of nanotechnology-based systems used for brain delivery of PBCs
Alzheimer’s disease
The nanotechnology-based approach might be a promising treatment strategy for patients with Alzheimer’s disease (de la Torre and Ceña 2018; Wong et al. 2019). This disease is characterized by abnormal accumulation of extracellular amyloid-beta plaques and intraneuronal neurofibrillary tangles in the brain. It commonly manifests as a type of dementia in aging individuals, leading to cognitive abnormalities and memory loss that substantially interferes with their quality of life (Magalingam et al. 2018). Alzheimer’s dementia is one of the most common neurodegenerative disorders affecting about 5.7 million Americans, with the number of affected individuals projected to rapidly increase because of an aging population (Rabinovici 2019). Although a vast amount of information has been accumulated over the past few decades regarding the causality of this disease, effective drug treatments for Alzheimer”s disease have yet to be identified. As such, numerous researchers and drug developers are urgently looking for alternative treatment strategies to prevent this disease from occurring or alleviate symptoms in those already affected (Magalingam et al. 2018).
Over the last few years, PBC-loaded nanodelivery systems were developed and tested in animal models and have demonstrated a great potential in treating this neurodegenerative disease (Karthivashan et al. 2018; Kermanizadeh et al. 2018; Del Prado-Audelo et al. 2019). In several studies, NPs administered by intranasal or intravenous routes provided enhanced bioavailability in the brain when compared to free drug administration, thus preventing neuroinflammation and further progression of the disease (Masserini 2013; Gao 2016). For example, in a rat model of Alzheimer’s disease, rats that were intravenously administered with quercetin-loaded solid lipid NPs exhibited substantially better memory-retention vis-à-vis test compared to those treated with pure quercetin (Dhawan et al. 2011). Moreover, these NPs demonstrated a higher delivery of quercetin to the brain with enhanced antioxidant effect in brain cells. Similarly, NPs loaded with the alkaloid piperine (an active compound found in black pepper) demonstrated increased bioavailability in brain cells following intraperitoneal administration (Yusuf et al. 2012). In an experimentally induced model of Alzheimer’s disease, the piperine-loaded NPs exhibited therapeutic effects on disease progression by reducing oxidative stress and cholinergic degradation.
In several recent studies, the anti-Alzheimer’s potential of NPs loaded with curcumin, known to modulate the activity of several transcription factors and their pro-inflammatory signaling pathways, was examined. Since curcumin shows low bioavailability in vivo, nanotechnology-based curcumin formulations were developed to achieve therapeutically relevant concentrations of this compound in the brain (Ullah et al. 2017). In a study by Barbara et al. (2017), the anti-amyloidogenic potential of curcumin-loaded NPs was examined in an in vitro model. In this research, a significant decrease of amyloid-beta aggregates was observed in primary hippocampal cell cultures treated with curcumin-loaded polylactide-co-glycolic-acid (PLGA) NPs. In an aluminum-induced mouse model of Alzheimer’s disease, oral administration of curcumin-loaded solid lipid NPs led to 32–155 times enhanced bioavailability of curcumin compared to the control group, and resulted in complete abolition of aluminum-induced adverse behavioral changes, and improved biochemical and histopathological alterations in the brain (Kakkar and Kaur 2011). Improved treatment efficiency of poly (lactic-co-glycolic acid) curcumin NPs was also observed in Tg2576 mouse model of this disease (Cheng et al. 2013).
Resveratrol is also regarded as a promising candidate for the treatment of Alzheimer’s disease, owing to its neuroprotective properties. Since resveratrol was found to be rapidly metabolized in liver and intestinal epithelial cells (within less than 2 h after intravenous injection), solid lipid NPs functionalized with monoclonal antibodies against the transferrin receptor, were developed (Loureiro et al. 2017). These NP-antibody conjugates showed enhanced cellular uptake and proposed a promising function as possible carriers to transport resveratrol extracts to the brain in an effort to treat Alzheimer’s disease.
Quercetin-loaded NPs also showed a more stable release of this compound over time with quercetin NPs showing a 5% release of this compound in the first hour post-administration and reaching 25% release after 8 h (Han et al. 2018). By contrast, powder quercetin only showed a 2% release in the first hour after administration before reaching a release saturation profile of just 4% after 2 h. Additionally, quercetin-loaded NPs showed a 6-fold greater release of quercetin compared to the powder form. These characteristics made quercetin NPs an attractive therapeutic potential for various conditions. Indeed, the same study demonstrated that quercetin NPs have promising therapeutic potentials in preventing and or treating Alzheimer’s disease due to their activity as amyloid β inhibitors and free radical scavengers (Han et al. 2018).
In a rat model of Alzheimer’s disease, EGCG-loaded NPs were found to be effective in attenuating aluminum chloride-induced adverse neurobehavioral impairments by reducing the formation of neuritic plaque and neurofibrillary tangles (Singh et al. 2018). Furthermore, a recent study demonstrated that oral administration of NPs loaded with EGCG and ascorbic acid enhanced the accumulation of EGCG in the brain, resulting in an increase in the number of synapses and reduced neuroinflammation and amyloid-beta plaque/peptide accumulation in a mouse model of familial Alzheimer’s disease (Cano et al. 2019).
Parkinson’s disease
Parkinson’s disease is the second most common neurodegenerative pathological condition after Alzheimer’s disease, affecting about 10 million individuals worldwide (Rousseaux et al. 2017). This disease occurs most commonly in the elderly and is characterized by the progressive loss of dopaminergic neurons and activation of microglial cells. While various efficient symptomatic treatments are presently available, there are no curative or disease-modifying therapies available for this disorder. Since neuroinflammation associated with the loss of dopamine-producing neurons in the brain is a pathologic hallmark of Parkinson’s disease (Vivekanantham et al. 2015), PBCs that demonstrate strong anti-neuroinflammatory responses are increasingly being investigated as potential therapeutics to treat Parkinson's disease (da Costa et al. 2017). These compounds, however, have limitations for therapeutic oral delivery because of their extensive first-pass metabolism and difficulties in crossing the blood-brain barrier (Ganesan et al. 2018b).
To overcome these issues and to maximize efficacy in treating Parkinson’s disease, PBC-loaded nanomedicines with a controlled size of 1–100 nm were engineered and examined in animal models during recent years (Ganesan et al. 2015). Nanosizing of PBCs such as curcumin, quercetin, resveratrol, catechin, and ginsenosides was shown to enhance their permeability into the brain with maximized stability and therapeutic effectiveness. In particular, several studies have demonstrated the enhanced oral bioavailability of curcumin loaded solid lipid NPs in the brain (Ramalingam and Ko 2015, 2016). Similarly, the bioavailability of resveratrol loaded in N-trimethyl chitosan-g-palmitic acid surface-modified solid lipid NPs was shown to be 3.8-fold higher than that from resveratrol suspension (Ramalingam et al. 2016). In the study by da Rocha Lindner et al. (2015), polysorbate 80-coated poly(lactide) NPs loaded with resveratrol exerted significant neuroprotective effects against behavioral and neurochemical changes induced by the neurotoxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, which is known to damage dopaminergic neurons and induce Parkinson-like symptoms.
Rheumatoid arthritis
Rheumatoid arthritis is a systemic autoimmune disease caused by chronic inflammation due to age-associated decline of the immune system (immunosenescence) (van Onna and Boonen 2016). The incidence of this disease increases with age and peaks around the age of 70 to 79 years (Cleutjens et al. 2019). The chronic immune system stimulation occurring in rheumatoid arthritis is suggested to promote premature aging and cause comorbidities, such as cardiovascular disorders, osteoporosis, and cancers.
Various PBCs including resveratrol, curcumin, hesperidin, thymoquinone, celastrol, and gambogic acid have demonstrated high efficiency in treating rheumatoid arthritis (Rahman et al. 2017). Such activity of PBCs may be likely attributed to their ability to decrease levels of inflammatory mediators such as cytokines, chemokines, nitric oxides, activity of NF-kβ signaling, adhesion molecules, lipoxygenase, and arachidonic acid molecules. Since the bioavailability of PBCs is poor due to their low aqueous solubility and high first-pass metabolism after oral administration, application of nanomedicines in treating rheumatoid arthritis has gained significant attention recently. In a rat model of the Complete Freund’s adjuvant (CFA)-induced arthritis, oral and topical administration of piperine-loaded solid lipid NPs resulted in a significant reduction in TNFα protein levels, suggesting that treatment with this NP has an anti-rheumatic therapeutic potential (Bhalekar et al. 2017). In the same rat model, the protective potential of curcumin-loaded solid lipid NPs in ameliorating CFA-induced arthritis via attenuating the anti-oxidative and anti-inflammatory responses in treated rats was demonstrated (Arora et al. 2015).
Osteoporosis
Osteoporosis is an age-associated disease characterized by deterioration in bone mass and micro-architecture, resulting in an increased risk of fragility fractures in older individuals (Alejandro and Constantinescu 2018). Osteoporotic bone loss is accompanied by elevated expression of proinflammatory cytokines. The FDA-approved anti-osteoporosis drugs are expensive and have numerous side effects. Therefore, searching for novel, efficient, and safe drugs for treating this disease is warranted. PBCs known to possess anti-inflammatory properties such as curcumin, genistein, resveratrol, quercetin, etc. are increasingly being regarded as potential medications that prevent age-related bone loss (Pandey et al. 2018). The results from recent in vitro and in vivo studies are indicative of effects of PBC-loaded NPs on biochemical markers and biomechanical parameters during osteoporosis, suggesting the potential of nanotechnological applications in preventing and or treating osteoporosis (Barry et al. 2016). In in vivo studies, the curcumin-loaded poly(lactic-co-glycolicacid) NPs were shown to potentiate the protective effect of curcumin against bone loss in ovariectomized rats (Ahn et al. 2017). The administration of curcumin-loaded β-cyclodextrin conjugated gold NPs resulted in improved bone density and prevented bone loss in ovariectomized C57Bl/6 mice (Heo et al. 2014). In an ovariectomized rat model, a formulation of quercetin-based solid lipid NPs was shown to be more effective than free quercetin in restoring bone mineral density in osteopenic animals (Ahmad et al. 2016).
Cancer
Cancer is among the leading causes of mortality worldwide. Treatment of cancer patients with chemotherapeutic agents is known to be associated with unfavorable pharmacokinetics, poor bioavailability, and severe systemic toxicity. Problems with conventional anti-cancer drugs have prompted the development of innovative nanobiotechnological approaches that allow drug delivery to specific tumor sites and minimize toxicity in healthy tissues in close proximity to the tumor (Zamboni et al. 2012; Ahmad et al. 2018). NPs are currently being extensively studied for their application in oral delivery of PBCs in anti-cancer therapies. In in vitro studies, enhanced anti-tumor activity was obtained for nanoengineered PBCs such as curcumin (Hazzah et al. 2016; Meena et al. 2017; Dhivya et al. 2018; Montalban et al. 2018; Wang et al. 2018a, b; van der Vlies et al. 2019; Somu and Paul 2019; Ni et al. 2019), resveratrol (Rodenak-Kladniew et al. 2017; Wang et al. 2017), berberine (Wang et al. 2014a; Zheng et al. 2018), aloe-emodin (Wang et al. 2012; Chen et al. 2014), oridonin (Wang et al. 2014b), and EGCG (Chavva et al. 2019) compared to respective unmodified PBCs. Using in vivo models of induced cancer, substantial inhibition of tumor proliferation and angiogenesis and increased apoptosis of tumor cells were repeatedly reported in mice given either intravenous or oral administered with NPs co-loaded with curcumin and specific anti-cancer drugs (Yang et al. 2015; Wang et al. 2015b; Kumari et al. 2017; Cui et al. 2017; Wang et al. 2016; Yan et al. 2016; Li et al. 2017a), as compared to free drugs. Similarly, strong anti-tumor properties were observed during in vivo studies with NPs loaded with resveratrol (Xu et al. 2016; Zhang et al. 2019), quercetin (Gao et al. 2012; Zhu et al. 2017), EGCG (Siddiqui et al. 2014; Tang et al. 2018), or berberine (Wang et al. 2018a, b).
Conclusions
The recent increase in life expectancy has led to a growing burden of aging-associated diseases among many human populations. Thus, population aging is becoming an increasingly important economic and social challenge across developed countries. This is because aging per se is a major determining factor for all age-associated conditions (Seals and Melov 2014; Seals et al. 2016; Yabluchanskiy et al. 2018). Therefore, development of interventions that target the aging process is one of the most important current goals in biomedical research (Vaiserman and Marotta 2016; Vaiserman and Lushchak 2017; Myers and Lithgow 2019). Progress in this field is undoubtedly largely dependent on elucidating the mechanistic pathways underlying aging (Crimmins 2015; Zierer et al. 2015; Campisi et al. 2019). It is becoming increasingly apparent that age-related chronic oxidative stress and associated systemic inflammation are among the most important processes contributing to the development of aging phenotypes. Therefore, pharmacological modulation of pro-oxidative and pro-inflammatory pathways is considered to be a promising strategy to combat aging and associated pathological conditions (Tan et al. 2018). However, the use of pharmacological agents such as synthetic antioxidants has, to date, produced rather disappointing outcomes. Indeed, long-term supplementation with synthetic antioxidants failed to improve health status and prevent age-related pathological conditions in many clinical trials and epidemiological studies (Myung et al. 2013; Bjelakovic et al. 2014; Gruber and Halliwell 2017). One possible explanation for these disappointing results comes from the fact that chronic oxidative stress and inflammation coexist in most aging-associated phenotypes. Therefore, the failure of clinical trials with synthetic antioxidant supplementations might be explained, at least in part, by an inability to simultaneously target both oxidative stress and inflammation by these pharmacological substances. Indeed, such agents can block particular pro-oxidative and/or proinflammatory pathways but reinforce others (Biswas 2016). Based on these considerations, the use of natural compounds exhibiting both antioxidant and anti-inflammatory properties, such as polyphenols, seems preferable in comparison with synthetic ones because they are capable of simultaneously reducing both oxidative stress and inflammation levels (Ganesan et al. 2017). Phytochemicals have been shown repeatedly to have a substantial potential for preventing and/or treating many disorders caused by age-associated chronic oxidative stress and systemic inflammation. However, poor stability, bioavailability and solubility in the gastrointestinal tract have limited their clinical applications until recently. The use of nanocarriers to delivery PBCs was found to enhance their solubility and stability, increase absorption in the gastrointestinal tract, protect from premature enzymatic degradation and metabolism, and also prolong their circulation time, thereby limiting the negative side effects of these compounds (Conte et al. 2017; Martínez-Ballesta et al. 2018). Currently, phytonanotherapy represents a promising innovative approach that can overcome some of the drawbacks present in conventional therapeutic strategies. Using PBC-loaded nanoformulations may provide synergistic benefits since this therapeutic option may be clinically equivalent to standard treatment with synthetic drugs, but with much lower side effects (Anand et al. 2017). Therefore, such an approach would provide an alternative method to conventional therapeutic modalities for management of age-related disorders and provide an opportunity to overcome disadvantages related to using these synthetic drugs. One more advantageous feature of nanodelivery systems is that they may help deliver PBCs to various vital organs, particularly the brain, through oral delivery. Indeed, the available research evidence suggests that the bioavailability of particular PBCs loaded in NPs may be 5 to 10 times higher than that of their native forms, where surface modification of these NPs allows sustained release of PBCs via oral delivery (Ganesan et al. 2018b).
Despite obvious advantages of NPs for drug delivery, some important challenges remain to be resolved for better future application. For some PBC-loaded nanoformulations, a burst drug release can lead to cellular toxicity concerns, whereas oppositely, a very slow drug release may cause insufficient therapeutic activity to treat the disease. Therefore, the development of different nanoformulation designs with optimized release profiles specific to the physicochemical properties of the NP-loaded PBCs presents an important research challenge (Lin et al. 2017). Moreover, nanomaterials that are being used to encapsulate PBCs need to be further thoroughly investigated to determine if these carriers themselves have any harmful effects, especially if they will be used over a long period of time by patients. More specifically, these outstanding issues include: whether these nanomaterials can bioaccumulate in the human body? Would they be metabolized into potentially harmful products? Would they be completely degraded and excreted after delivering their drug load? Are they going to become a biohazard when excreted (in urine or feces) and accumulated in the environment? In light of these outstanding issues, we can conclude that, although significant steps have already been taken to bringing nanotherapeutic approaches closer to clinical applications, additional research is needed to improve the efficacy, long-term safety and cost-effectiveness of nanosized delivery systems.
Funding
The work was partially supported by the Science and Technology Center in Ukraine (#6274) to OL and by Natural Sciences and Engineering Research Council of Canada (#6793) to KBS.
Compliance with ethical standard
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statements
This is a review article. It has not involved any human subjects and animal experiments.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Oleh Lushchak, Email: olehl@pu.if.ua.
Alexander Vaiserman, Email: vaiserman23@gmail.com.
References
- Ahmad MZ, Akhter S, Mohsin N, Abdel-Wahab BA, Ahmad J, Warsi MH, Rahman M, Mallick N, Ahmad FJ. Transformation of curcumin from food additive to multifunctional medicine: Nanotechnology bridging the gap. Curr Drug Discov Technol. 2014;11:197–213. doi: 10.2174/1570163811666140616153436. [DOI] [PubMed] [Google Scholar]
- Ahmad N, Banala VT, Kushwaha P, Karvand A, Sharma S, Tripathi AK, Verma A, Trivedi R, Mishra PR. Quercetin-loaded solid lipid nanoparticles improve osteoprotective activity in an ovariectomized rat model: a preventive strategy for post-menopausal osteoporosis. RSC Adv. 2016;6:97613–97628. doi: 10.1039/C6RA17141A. [DOI] [Google Scholar]
- Ahmad K, Rabbani G, Baig MH, Lim JH, Khan ME, Lee EJ, Ashraf GM, Choi I. Nanoparticle-based drugs: A potential armamentarium of effective anti-cancer therapies. Curr Drug Metab. 2018;19:839–846. doi: 10.2174/1389200218666170823115647. [DOI] [PubMed] [Google Scholar]
- Ahn J, Jeong J, Lee H, Sung MJ, Jung CH, Lee H, Hur J, Park JH, Jang YJ, Ha TY. Poly(lactic-co-glycolic acid) nanoparticles potentiate the protective effect of curcumin against bone loss in ovariectomized rats. J Biomed Nanotech. 2017;13:688–698. doi: 10.1166/jbn.2017.2372. [DOI] [Google Scholar]
- Ajdary M, Moosavi MA, Rahmati M, Falahati M, Mahboubi M, Mandegary A, Jangjoo S, Mohammadinejad R, Varma RS. Health concerns of various nanoparticles: A review of their in vitro and in vivo toxicity. Nanomaterials (Basel) 2018;8:E634. doi: 10.3390/nano8090634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam MM, Abdullah KM, Singh BR, Naqvi AH, Naseem I. Ameliorative effect of quercetin nanorods on diabetic mice: mechanistic and therapeutic strategies. RSC Adv. 2016;6:55092–55103. doi: 10.1039/C6RA04821H. [DOI] [Google Scholar]
- Alejandro P, Constantinescu F. A review of osteoporosis in the older adult: An update. Rheum Dis Clin North Am. 2018;44:437–451. doi: 10.1016/j.rdc.2018.03.004. [DOI] [PubMed] [Google Scholar]
- Alfaras I, Di Germanio C, Bernier M, Csiszar A, Ungvari Z, Lakatta EG, de Cabo R. Pharmacological strategies to retard cardiovascular aging. Circ Res. 2016;118:1626–1642. doi: 10.1161/CIRCRESAHA.116.307475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameruoso A, Palomba R, Palange AL, Cervadoro A, Lee A, Mascolo DD, Decuzzi P. Ameliorating amyloid-β fibrils triggered inflammation via curcumin-loaded polymeric nanoconstructs. Front Immunol. 2017;8:1411. doi: 10.3389/fimmu.2017.01411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amiot MJ, Riva C, Vinet A. Effects of dietary polyphenols on metabolic syndrome features in humans: a systematic review. Obes Rev. 2016;17:573–586. doi: 10.1111/obr.12409. [DOI] [PubMed] [Google Scholar]
- Anand David AV, Arulmoli R, Parasuraman S. Overviews of biological importance of quercetin: a bioactive flavonoid. Pharmacog Rev. 2016;10:84–89. doi: 10.4103/0973-7847.194044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand K, Tiloke C, Naidoo P, Chuturgoon AA. Phytonanotherapy for management of diabetes using green synthesis nanoparticles. J Photochem Photobiol B. 2017;173:626–639. doi: 10.1016/j.jphotobiol.2017.06.028. [DOI] [PubMed] [Google Scholar]
- Anselmo AC, Mitragotri S. An overview of clinical and commercial impact of drug delivery systems. JJ Control Release. 2014;190:15–28. doi: 10.1016/j.jconrel.2014.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora R, Kuhad A, Kaur IP, Chopra K. Curcumin loaded solid lipid nanoparticles ameliorate adjuvant-induced arthritis in rats. Eur J Pain. 2015;19:40–952. doi: 10.1002/ejp.620. [DOI] [PubMed] [Google Scholar]
- Avadhani KS, Manikkath J, Tiwari M, Chandrasekhar M, Godavarthi A, Vidya SM, Hariharapura RC, Kalthur G, Udupa N, Mutalik S. Skin delivery of epigallocatechin-3-gallate (EGCG) and hyaluronic acid loaded nano-transfersomes for antioxidant and anti-aging effects in UV radiation induced skin damage. Drug Deliv. 2017;24:61–74. doi: 10.1080/10717544.2016.1228718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbara R, Belletti D, Pederzoli F, Masoni M, Keller J, Ballestrazzi A, Vandelli MA, Tosi G, Grabrucker AM. Novel curcumin loaded nanoparticles engineered for blood-brain barrier crossing and able to disrupt Abeta aggregates. Int J Pharm. 2017;526:413–424. doi: 10.1016/j.ijpharm.2017.05.015. [DOI] [PubMed] [Google Scholar]
- Barry M, Pearce H, Cross L, Tatullo M, Gaharwar AK. Advances in nanotechnology for the treatment of osteoporosis. Curr Osteoporos Rep. 2016;14:87–94. doi: 10.1007/s11914-016-0306-3. [DOI] [PubMed] [Google Scholar]
- Bayón-Cordero L, Alkorta I, Arana L. Application of solid lipid nanoparticles to improve the efficiency of anticancer drugs. Nanomaterials (Basel) 2019;9:E474. doi: 10.3390/nano9030474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard JR, Bloom DE. Towards a comprehensive public health response to population ageing. Lancet. 2015;385:658–661. doi: 10.1016/S0140-6736(14)61461-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behloul N, Wu G. Genistein: a promising therapeutic agent for obesity and diabetes treatment. Eur J Pharmacol. 2013;698:31–38. doi: 10.1016/j.ejphar.2012.11.013. [DOI] [PubMed] [Google Scholar]
- Berman AY, Motechin RA, Wiesenfeld MY, Holz MK. The therapeutic potential of resveratrol: a review of clinical trials. NPJ Precis Oncol. 2017;1:35. doi: 10.1038/s41698-017-0038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhalekar MR, Madgulkar AR, Desale PS, Marium G. Formulation of piperine solid lipid nanoparticles (SLN) for treatment of rheumatoid arthritis. Drug Dev Ind Pharm. 2017;43:1003–1010. doi: 10.1080/03639045.2017.1291666. [DOI] [PubMed] [Google Scholar]
- Bilia AR, Piazzini V, Guccione C, Risaliti L, Asprea M, Capecchi G, Bergonzi MC. Improving on nature: The role of nanomedicine in the development of clinical natural drugs. Planta Med. 2017;83:66–381. doi: 10.1055/s-0043-102949. [DOI] [PubMed] [Google Scholar]
- Biswas SK. Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid Med Cell Longev. 2016;2016:5698931. doi: 10.1155/2016/5698931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelakovic G, Nikolova D, Gluud C. Antioxidant supplements and mortality. Curr Opin Clin Nutr Metab Care. 2014;17:40–44. doi: 10.1097/MCO.0000000000000009. [DOI] [PubMed] [Google Scholar]
- Borel T, Sabliov CM. Nanodelivery of bioactive components for food applications: types of delivery systems, properties, and their effect on ADME profiles and toxicity of nanoparticles. Annu Rev Food Sci Technol. 2014;5:197–213. doi: 10.1146/annurev-food-030713-092354. [DOI] [PubMed] [Google Scholar]
- Camins A, Junyent F, Verdaguer E, Beas-Zarate C, Rojas-Mayorquín AE, Ortuño-Sahagún D, Pallàs M. Resveratrol: An antiaging drug with potential therapeutic applications in treating diseases. Pharmaceuticals (Basel) 2009;2:194–205. doi: 10.3390/ph2030194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campesi I, Marino M, Cipolletti M, Romani A, Franconi F. Put "gender glasses" on the effects of phenolic compounds on cardiovascular function and diseases. Eur J Nutr. 2018;57:2677–2691. doi: 10.1007/s00394-018-1695-0. [DOI] [PubMed] [Google Scholar]
- Campisi J, Kapahi P, Lithgow GJ, Melov S, Newman JC, Verdin E. From discoveries in ageing research to therapeutics for healthy ageing. Nature. 2019;571:183–192. doi: 10.1038/s41586-019-1365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano A, Ettcheto M, Chang JH, Barroso E, Espina M, Kühne BA, Barenys M, Auladell C, Folch J, Souto EB, Camins A, Turowski P, García ML. Dual-drug loaded nanoparticles of Epigallocatechin-3-gallate (EGCG)/Ascorbic acid enhance therapeutic efficacy of EGCG in a APPswe/PS1dE9 Alzheimer's disease mice model. J Control Release. 2019;301:62–75. doi: 10.1016/j.jconrel.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan H, Král P. Nanoparticles self–assembly within lipid bilayers. ACS Omega. 2018;3:10631–10637. doi: 10.1021/acsomega.8b01445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan AS. Dendrimer nanotechnology for enhanced formulation and controlled delivery of resveratrol. Ann N Y Acad Sci. 2015;1348:134–140. doi: 10.1111/nyas.12816. [DOI] [PubMed] [Google Scholar]
- Chavva SR, Deshmukh SK, Kanchanapally R, Tyagi N, Coym JW, Singh AP, Singh S. Epigallocatechin gallate-gold nanoparticles exhibit superior antitumor activity compared to conventional gold nanoparticles: potential synergistic interactions. Nanomaterials (Basel) 2019;9:E396. doi: 10.3390/nano9030396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Wang S, Zhang J, Chen M, Wang Y. Aloe-emodin loaded solid lipid nanoparticles: formulation design and in vitro anti-cancer study. Drug Deliv. 2014;22:666–674. doi: 10.3109/10717544.2014.882446. [DOI] [PubMed] [Google Scholar]
- Chen Y, Zhang H, Yang J, Sun H. Improved antioxidant capacity of optimization of a self-microemulsifying drug delivery system for resveratrol. Molecules. 2015;20:21167–21177. doi: 10.3390/molecules201219750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Jiang H, Wu X, Fang J (2016, 2016) Therapeutic effects of quercetin on inflammation, obesity, and type 2 diabetes. Mediators Inflamm:9340637. 10.1155/2016/9340637 [DOI] [PMC free article] [PubMed]
- Cheng KK, Yeung CF, Ho SW, Chow SF, Chow AH, Baum L. Highly stabilized curcumin nanoparticles tested in an in vitro blood–brain barrier model and in Alzheimer’s disease Tg2576 mice. AAPS J. 2013;15:324–336. doi: 10.1208/s12248-012-9444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chikara S, Nagaprashantha LD, Singhal J, Horne D, Awasthi S, Singhal SS. Oxidative stress and dietary phytochemicals: Role in cancer chemoprevention and treatment. Cancer Lett. 2018;413:122–134. doi: 10.1016/j.canlet.2017.11.002. [DOI] [PubMed] [Google Scholar]
- Chitkara D, Nikalaje SK, Mittal A, Chand M, Kumar N. Development of quercetin nanoformulation and in vivo evaluation using streptozotocin induced diabetic rat model. Drug Deliv Transl Res. 2012;2:112–123. doi: 10.1007/s13346-012-0063-5. [DOI] [PubMed] [Google Scholar]
- Chu C, Deng J, Man Y, Qu Y. Green tea extracts epigallocatechin-3-gallate for different treatments. Biomed Res Int. 2017;2017:5615647. doi: 10.1155/2017/5615647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleutjens FAHM, Boonen AERCH, van Onna MGB. Geriatric syndromes in patients with rheumatoid arthritis: a literature overview. Clin Exp Rheumatol. 2019;37:496–501. [PubMed] [Google Scholar]
- Conte R, Marturano V, Peluso G, Calarco A, Cerruti P. Recent advances in nanoparticle-mediated delivery of anti-inflammatory phytocompounds. Int J Mol Sci. 2017;18:E709. doi: 10.3390/ijms18040709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrêa RCG, Peralta RM, Haminiuk CWI, Maciel GM, Bracht A, Ferreira ICFR. New phytochemicals as potential human anti-aging compounds: Reality, promise, and challenges. Crit Rev Food Sci Nutr. 2018;58:942–957. doi: 10.1080/10408398.2016.1233860. [DOI] [PubMed] [Google Scholar]
- Crimmins EM. Lifespan and healthspan: Past, present, and promise. Gerontologist. 2015;55:901–911. doi: 10.1093/geront/gnv130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crucho CIC, Barros MT. Polymeric nanoparticles: A study on the preparation variables and characterization methods. Mater Sci Eng C Mater Biol Appl. 2017;80:771–784. doi: 10.1016/j.msec.2017.06.004. [DOI] [PubMed] [Google Scholar]
- Csiszár A, Csiszar A, Pinto JT, Gautam T, Kleusch C, Hoffmann B, Tucsek Z, Toth P, Sonntag WE, Ungvari Z. Resveratrol encapsulated in novel fusogenic liposomes activates Nrf2 and attenuates oxidative stress in cerebromicrovascular endothelial cells from aged rats. J Gerontol A Biol Sci Med Sci. 2015;70:303–313. doi: 10.1093/gerona/glu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui T, Zhang S, Sun H. Co-delivery of doxorubicin and pH-sensitive curcumin prodrug by transferrin-targeted nanoparticles for breast cancer treatment. Oncol Rep. 2017;37:1253–1260. doi: 10.3892/or.2017.5345. [DOI] [PubMed] [Google Scholar]
- da Costa IM, Cavalcanti JRLP, de Queiroz DB, do Rêgo ACM, Araújo Filho I, Parente P, Botelho MA, Guzen FP. Supplementation with herbal extracts to promote behavioral and neuroprotective effects in experimental models of Parkinson’s disease: a systematic review. Phytother Res. 2017;31:959–970. doi: 10.1002/ptr.5813. [DOI] [PubMed] [Google Scholar]
- da Rocha Lindner G, Bonfanti Santos D, Colle D, Gasnhar Moreira EL, Daniel Prediger R, Farina M, Khalil NM, Mara Mainardes R. Improved neuroprotective effects of resveratrol-loaded polysorbate 80-coated poly(lactide) nanoparticles in MPTP-induced Parkinsonism. Nanomedicine (Lond) 2015;10:1127–1138. doi: 10.2217/nnm.14.165. [DOI] [PubMed] [Google Scholar]
- da Silva Santos V, Badan Ribeiro AP, Andrade Santana MH. Solid lipid nanoparticles as carriers for lipophilic compounds for applications in foods. Food Res Int. 2019;122:610–626. doi: 10.1016/j.foodres.2019.01.032. [DOI] [PubMed] [Google Scholar]
- Date AA, Hanes J, Ensign LM. Nanoparticles for oral delivery: Design, evaluation and state-of-the-art. J Control Releas. 2016;240:504–526. doi: 10.1016/j.jconrel.2016.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Torre C, Ceña V. The delivery challenge in neurodegenerative disorders: the nanoparticles role in Alzheimer's disease therapeutics and diagnostics. Pharmaceutics. 2018;10:E190. doi: 10.3390/pharmaceutics10040190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Prado-Audelo ML, Caballero-Florán IH, Meza-Toledo JA, Mendoza-Muñoz N, González-Torres M, Florán B, Cortés H, Leyva-Gómez G. Formulations of curcumin nanoparticles for brain diseases. Biomolecules. 2019;9:E56. doi: 10.3390/biom9020056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng W, Wang H, Wu B, Zhang X. Selenium-layered nanoparticles serving for oral delivery of phytomedicines with hypoglycemic activity to synergistically potentiate the antidiabetic effect. Acta Pharm Sin B. 2019;9:74–86. doi: 10.1016/j.apsb.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewangan AK, Perumal Y, Pavurala N, Chopra K, Mazumder S. Preparation, characterization and anti-inflammatory effects of curcumin loaded carboxymethyl cellulose acetate butyrate nanoparticles on adjuvant induced arthritis in rats. J Drug Deliv Sci Technol. 2017;41:269–279. doi: 10.1016/j.jddst.2017.07.022. [DOI] [Google Scholar]
- Dhawan S, Kapil R, Singh B. Formulation development and systematic optimization of solid lipid nanoparticles of quercetin for improved brain delivery. J Pharm Pharmacol. 2011;63:342–351. doi: 10.1111/j.2042-7158.2010.01225.x. [DOI] [PubMed] [Google Scholar]
- Dhivya R, Ranjani J, Rajendhran J, Mayandi J, Annaraj J. Enhancing the anti-gastric cancer activity of curcumin with biocompatible and pH sensitive PMMA-AA/ZnO nanoparticles. Mater Sci Eng C Mater Biol Appl. 2018;82:182–189. doi: 10.1016/j.msec.2017.08.058. [DOI] [PubMed] [Google Scholar]
- Elliot PJ, Jirousek M. Sirtuins: novel targets for metabolic disease. Curr Opin Investig Drugs. 2008;9:371–378. doi: 10.1016/j.bbrc.2008.06.048. [DOI] [PubMed] [Google Scholar]
- El-Naggar ME, Al-Joufi F, Anwar M, Attia MF, El-Bana MA. Curcumin-loaded PLA-PEG copolymer nanoparticles for treatment of liver inflammation in streptozotocin-induced diabetic rats. Colloids Surf B Biointerfaces. 2019;177:389–398. doi: 10.1016/j.colsurfb.2019.02.024. [DOI] [PubMed] [Google Scholar]
- Eng QY, Thanikachalam PV, Ramamurthy S. Molecular understanding of Epigallocatechin gallate (EGCG) in cardiovascular and metabolic diseases. J Ethnopharmacol. 2018;210:296–310. doi: 10.1016/j.jep.2017.08.035. [DOI] [PubMed] [Google Scholar]
- Fan Y, Yi J, Zhang Y, Yokoyama W. Fabrication of curcumin-loaded bovine serum albumin (BSA)-dextran nanoparticles and the cellular antioxidant activity. Food Chem. 2018;239:1210–1218. doi: 10.1016/j.foodchem.2017.07.075. [DOI] [PubMed] [Google Scholar]
- Flora G, Gupta D, Tiwari A. Nanocurcumin: A promising therapeutic advancement over native curcumin. Crit Rev Ther Drug Carrier Sys. 2013;30:331–368. doi: 10.1615/CritRevTherDrugCarrierSyst.2013007236. [DOI] [PubMed] [Google Scholar]
- Franco R, Navarro G, Martínez-Pinilla E. Hormetic and mitochondria–related mechanisms of antioxidant action of phytochemicals. Antioxidants (Basel) 2019;8:E373. doi: 10.3390/antiox8090373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasca D, Blomberg BB, Paganelli R. Aging, obesity, and inflammatory age-related diseases. Front Immunol. 2017;8:1745. doi: 10.3389/fimmu.2017.01745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frias I, Neves AR, Pinheiro M, Reis S. Design, development, and characterization of lipid nanocarriers-based epigallocatechin gallate delivery system for preventive and therapeutic supplementation. Drug Des Devel Ther. 2016;10:3519–3528. doi: 10.2147/DDDT.S109589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fröhlich E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int J Nanomedicine. 2012;7:5577–5591. doi: 10.2147/IJN.S36111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frozza RL, Bernardi A, Paese K, Hoppe JB, da Silva T, Battastini AM, Pohlmann AR, Guterres SS, Salbego C. Characterization of trans-resveratrol-loaded lipid-core nanocapsules and tissue distribution studies in rats. J Biomed Nanotechnol. 2010;6:694–703. doi: 10.1166/jbn.2010.1161. [DOI] [PubMed] [Google Scholar]
- Ganesan P, Ko HM, Kim IS, Choi DK. Recent trends in the development of nanophytobioactive compounds and delivery systems for their possible role in reducing oxidative stress in Parkinson’s disease models. Int J Nanomedicine. 2015;10:6757–6772. doi: 10.2147/IJN.S93918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan P, Arulselvan P, Choi DK. Phytobioactive compound-based nanodelivery systems for the treatment of type 2 diabetes mellitus - current status. IInt J Nanomedicine. 2017;12:1097–1111. doi: 10.2147/IJN.S124601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan P, Karthivashan G, Park SY, Kim J, Choi DK (2018a) Microfluidization trends in the development of nanodelivery systems and applications in chronic disease treatments Int J Nanomedicine 13:6109-6121. 10.2147 /IJN.S178077. [DOI] [PMC free article] [PubMed]
- Ganesan P, Ramalingam P, Karthivashan G, Ko YT, Choi DK. Recent developments in solid lipid nanoparticle and surface-modified solid lipid nanoparticle delivery systems for oral delivery of phyto-bioactive compounds in various chronic diseases. Int J Nanomedicine. 2018;13:1569–1583. doi: 10.2147/IJN.S155593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao H. Progress and perspectives on targeting nanoparticles for brain drug delivery. Acta Pharm Sin B. 2016;6:268–286. doi: 10.1016/j.apsb.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao X, Wang B, Wei X, Men K, Zheng F, Zhou Y, Zheng Y, Gou M, Huang M, Guo G, Huang N, Qian Z, Wei Y. Anticancer effect and mechanism of polymer micelle-encapsulated quercetin on ovarian cancer. Nanoscale. 2012;4:7021–7030. doi: 10.1039/c2nr32181e. [DOI] [PubMed] [Google Scholar]
- Gigliobianco MR, Casadidio C, Censi R, Di Martino P. Nanocrystals of Poorly Soluble Drugs: Drug Bioavailability and Physicochemical Stability. Pharmaceutics. 2018;10:E134. doi: 10.3390/pharmaceutics10030134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Governa P, Baini G, Borgonetti V, Cettolin G, Giachetti D, Magnano AR, Miraldi E, Biagi M. Phytotherapy in the management of diabetes: a review. Molecules. 2018;23:E105. doi: 10.3390/molecules23010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granja A, Frias I, Rute Neves A, Pinheiro M, Reis S. Therapeutic potential of epigallocatechin gallate nanodelivery systems. Biomed Res Int. 2017;2017:5813793. doi: 10.1155/2017/5813793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grottkau BE, Cai X, Wang J, Yang X, Lin Y. Polymeric nanoparticles for a drug delivery system. Curr Drug Metab. 2013;14:840–846. doi: 10.1007/978-1-60761-609-2_11. [DOI] [PubMed] [Google Scholar]
- Gruber J, Halliwell B. Approaches for extending human healthspan: from antioxidants to healthspan pharmacology. Essays Biochem. 2017;61:389–399. doi: 10.1042/EBC20160091. [DOI] [PubMed] [Google Scholar]
- Gu M, Wang X, Toh TB, Chow EK. Applications of stimuli-responsive nanoscale drug delivery systems in translational research. Drug Discov Today. 2018;23:1043–1052. doi: 10.1016/j.drudis.2017.11.009. [DOI] [PubMed] [Google Scholar]
- Gupta R, Xie H. Nanoparticles in daily life: Applications, toxicity and regulations. J Environ Pathol Toxicol Oncol. 2018;37:209–230. doi: 10.1615/JEnvironPatholToxicolOncol.2018026009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajialyani M, Tewari D, Sobarzo-Sánchez E, Nabavi SM, Farzaei MH, Abdollahi M. Natural product-based nanomedicines for wound healing purposes: therapeutic targets and drug delivery systems. Int J Nanomedicine. 2018;13:5023–5043. doi: 10.2147/IJN.S174072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Q, Wang H, Cai S, Liu X, Zhang Y, Yang L, Wang C, Yang R. Quercetin nanoparticles with enhanced bioavailability as multifunctional agents toward amyloid induced neurotoxicity. J Mater Chem B. 2018;6:1387–1393. doi: 10.1039/C7TB03053C. [DOI] [PubMed] [Google Scholar]
- Hansen M, Kennedy BK. Does longer lifespan mean longer healthspan? Trends Cell Biol. 2016;26:565–568. doi: 10.1016/j.tcb.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazzah HA, Farid RM, Nasra MM, Zakaria M, Gawish Y, El-Massik MA, Abdallah OY. A new approach for treatment of precancerous lesions with curcumin solid-lipid nanoparticle-loaded gels: in vitro and clinical evaluation. Drug Deliv. 2016;23:1409–1419. doi: 10.3109/10717544.2015.1065524. [DOI] [PubMed] [Google Scholar]
- Heiss C, Spyridopoulos I, Haendeler J. Interventions to slow cardiovascular aging: Dietary restriction, drugs and novel molecules. Exp Gerontol. 2018;109:108–118. doi: 10.1016/j.exger.2017.06.015. [DOI] [PubMed] [Google Scholar]
- Heo DN, Ko WK, Moon HJ, Kim HJ, Lee SJ, Lee JB, Bae MS, Yi JK, Hwang YS, Bang JB, Kim EC, Do SH, Kwon IK. Inhibition of osteoclast differentiation by gold nanoparticles functionalized with cyclodextrin curcumin complexes. ACS Nano. 2014;8:12049–12062. doi: 10.1021/nn504329u. [DOI] [PubMed] [Google Scholar]
- Hoshyar N, Gray S, Han H, Bao G. The effect of nanoparticle size on in vivo pharmacokinetics and cellular interaction. Nanomedicine (Lond) 2016;11:673–692. doi: 10.2217/nnm.16.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou CY, Tain YL, Yu HR, Huang LT. The effects of resveratrol in the treatment of metabolic syndrome. Int J Mol Sci. 2019;20:E535. doi: 10.3390/ijms20030535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal J, Abbasi BA, Ahmad R, Mahmood T, Ali B, Khalil AT, Kanwal S, Shah SA, Alam MM, Badshah H, Munir A. Nanomedicines for developing cancer nanotherapeutics: from benchtop to bedside and beyond. Appl Microbiol Biotechnol. 2018;102:9449–9470. doi: 10.1007/s00253-018-9352-3. [DOI] [PubMed] [Google Scholar]
- Jaiswal M, Dudhe R, Sharma PK (2015) Nanoemulsion: an advanced mode of drug delivery system. 3 Biotech 5:123–127. 10.1007/s13205-014-0214-0 [DOI] [PMC free article] [PubMed]
- Jeevanandam J, Danquah MK, Debnath S, Meka VS, Chan YS. Opportunities for nano-formulations in type 2 diabetes mellitus treatments. Curr Pharm Biotechno. 2015;16:853–870. doi: 10.2174/1389201016666150727120618. [DOI] [PubMed] [Google Scholar]
- Kakkar V, Kaur IP. Evaluating potential of curcumin loaded solid lipid nanoparticles in aluminium induced behavioural, biochemical and histopathological alterations in mice brain. Food Chem Toxicol. 2011;49:2906–2913. doi: 10.1016/j.fct.2011.08.006. [DOI] [PubMed] [Google Scholar]
- Kakkar V, Muppu SK, Chopra K, Kaur IP. Curcumin loaded solid lipid nanoparticles: an efficient formulation approach for cerebral ischemic reperfusion injury in rats. Eur J Pharm Biopharm. 2013;85:339–345. doi: 10.1016/j.ejpb.2013.02.005. [DOI] [PubMed] [Google Scholar]
- Kamaly N, Yameen B, Wu J, Farokhzad OC. Degradable controlled–release polymers and polymeric nanoparticles: mechanisms of controlling drug release. Chem Rev. 2016;116:2602–2663. doi: 10.1021/acs.chemrev.5b00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karthivashan G, Ganesan P, Park SY, Kim JS, Choi DK. Therapeutic strategies and nano-drug delivery applications in management of ageing Alzheimer's disease. Drug Deliv. 2018;25:307–320. doi: 10.1080/10717544.2018.1428243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawabata K, Mukai R, Ishisaka A. Quercetin and related polyphenols: new insights and implications for their bioactivity and bioavailability. Food Funct. 2015;6:1399–1417. doi: 10.1039/c4fo01178c. [DOI] [PubMed] [Google Scholar]
- Kermanizadeh A, Powell LG, Stone V, Møller P. Nanodelivery systems and stabilized solid-drug nanoparticles for orally administered medicine: current landscape. Int J Nanomedicine. 2018;13:7575–7605. doi: 10.2147/IJN.S177418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadka P, Ro J, Kim H, Kim I, Kim JT, Kim H, Cho JM, Yun G, Lee J. Pharmaceutical particle technologies: An approach to improve drug solubility, dissolution and bioavailability. J Pharm Sci. 2014;9:304–316. doi: 10.1016/j.ajps.2014.05.005. [DOI] [Google Scholar]
- Khan I, Kumar H, Mishra G, Gothwal A, Kesharwani P, Gupta U. Polymeric Nanocarriers: A New Horizon for the Effective Management of Breast Cancer. Curr Pharm Des. 2017;23:5315–5326. doi: 10.2174/1381612823666170829164828. [DOI] [PubMed] [Google Scholar]
- Kim JT, Barua S, Kim H, Hong SC, Yoo SY, Jeon H, Cho Y, Gil S, Oh K, Lee J. Absorption study of genistein using solid lipid microparticles and nanoparticles: Control of oral bioavailability by particle sizes. Biomol Ther (Seoul) 2017;25:452–459. doi: 10.4062/biomolther.2017.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong FY, Zhang JW, Li RF, Wang ZX, Wang WJ, Wang W. Unique roles of gold nanoparticles in drug delivery, targeting and imaging applications. Molecules. 2017;22:E1445. doi: 10.3390/molecules22091445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy K, Mahalingam M. Selection of a suitable method for the preparation of polymeric nanoparticles: multi–criteria decision making approach. Adv Pharm Bull. 2015;5:57–67. doi: 10.5681/apb.2015.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupkova O, Ferguson SJ, Wuertz-Kozak K. Stability of (-)-epigallocatechin gallate and its activity in liquid formulations and delivery systems. J Nutr Biochem. 2016;37:1–12. doi: 10.1016/j.jnutbio.2016.01.002. [DOI] [PubMed] [Google Scholar]
- Kumar A, Ahuja A, Ali J, Baboota S. Conundrum and therapeutic potential of curcumin in drug delivery. Crit Rev Ther Drug Carrier Syst. 2010;27:279–312. doi: 10.1615/CritRevTherDrugCarrierSyst.v27.i4. [DOI] [PubMed] [Google Scholar]
- Kumari P, Muddineti O S, Rompicharla SV, Ghanta P, B B N AK, Ghosh B, Biswas S (2017) Cholesterol-conjugated poly (D, L-lactide)-based micelles as a nanocarrier system for effective delivery of curcumin in cancer therapy. Drug Deliv 24:209–223. 10.1080/10717544.2016.1245365. [DOI] [PMC free article] [PubMed]
- Kwon SH, Kim SY, Ha KW, Kang MJ, Huh JS, Im TJ, Kim YM, Park YM, Kang KH, Lee S, Chang JY, Lee J, Choi YW. Pharmaceutical evaluation of genistein-loaded pluronic micelles for oral delivery. Arch Pharm Res. 2007;30:1138–1143. doi: 10.1007/BF02980249. [DOI] [PubMed] [Google Scholar]
- Kydd J, Jadia R, Velpurisiva P, Gad A, Paliwal S, Rai P. Targeting strategies for the combination treatment of cancer using drug delivery systems. Pharmaceutics. 2017;9:E46. doi: 10.3390/pharmaceutics9040046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KZ. Clinical trials of berberine chloride as pharmaceutical agent of type II diabetes. HBTCM. 2006;28:38–41. doi: 10.2337/db06-0006. [DOI] [Google Scholar]
- Lee GH, Lee SJ, Jeong SW, Kim HC, Park GY, Lee SG, Choi JH. Antioxidative and antiinflammatory activities of quercetin-loaded silica nanoparticles. Colloids Surf B Biointerfaces. 2016;143:511–517. doi: 10.1016/j.colsurfb.2016.03.060. [DOI] [PubMed] [Google Scholar]
- Li Y, Yao J, Han C, Yang J, Chaudhry MT, Wang S, Liu H, Yin Y. Quercetin, inflammation and immunity. Nutrients. 2016;8:167. doi: 10.3390/nu8030167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Ge X, Wang L. Construction and comparison of different nanocarriers for co-delivery of cisplatin and curcumin: A synergistic combination nanotherapy for cervical cancer. Biomed Pharmacother. 2017;86:628–636. doi: 10.1016/j.biopha.2016.12.042. [DOI] [PubMed] [Google Scholar]
- Li M, Xin M, Guo C, Lin G, Wu X. New nanomicelle curcumin formulation for ocular delivery: Improved stability, solubility, and ocular anti-inflammatory treatment. Drug Dev Ind Pharm. 2017;43:1846–1857. doi: 10.1080/03639045.2017.1349787. [DOI] [PubMed] [Google Scholar]
- Li J, Zhang CX, Liu YM, Chen KL, Chen G. A comparative study of anti-aging properties and mechanism: resveratrol and caloric restriction. Oncotarget. 2017;8:65717–65729. doi: 10.18632/oncotarget.20084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Zhou Y, Zhang W, Bao C, Xie Z. Relief of oxidative stress and cardiomyocyte apoptosis by using curcumin nanoparticles. Colloids Surf B Biointerfaces. 2017;153:174–182. doi: 10.1016/j.colsurfb.2017.02.023. [DOI] [PubMed] [Google Scholar]
- Li T, Liang W, Xiao X, Qian Y. Nanotechnology, an alternative with promising prospects and advantages for the treatment of cardiovascular diseases. Int J Nanomedicine. 2018;13:7349–7362. doi: 10.2147/IJN.S179678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian B, Wu M, Feng Z, Deng Y, Zhong C, Zhao X. Folate-conjugated human serum albumin-encapsulated resveratrol nanoparticles: preparation, characterization, bioavailability and targeting of liver tumors. Artif Cells Nanomed Biotechnol. 2019;47:154–165. doi: 10.1080/21691401.2018.1548468. [DOI] [PubMed] [Google Scholar]
- Lim H, Park H, Kim HP. Effects of flavonoids on senescence–associated secretory phenotype formation from bleomycin–induced senescence in BJ fibroblasts. Biochem Pharmacol. 2015;96:337–348. doi: 10.1016/j.bcp.2015.06.013. [DOI] [PubMed] [Google Scholar]
- Lim H, Park BK, Shin SY, Kwon YS, Kim HP. Methyl caffeate and some plant constituents inhibit age–related inflammation: effects on senescence–associated secretory phenotype (SASP) formation. Arch Pharm Res. 2017;40:524–535. doi: 10.1007/s12272-017-0909-y. [DOI] [PubMed] [Google Scholar]
- Lin CH, Chen CH, Lin ZC, Fang JY. Recent advances in oral delivery of drugs and bioactive natural products using solid lipid nanoparticles as the carriers. JJ Food Drug Anal. 2017;25:219–234. doi: 10.1016/j.jfda.2017.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loureiro JA, Andrade S, Duarte A, Neves AR, Queiroz JF, Nunes C, Sevin E, Fenart L, Gosselet F, Coelho MA, Pereira MC. Resveratrol and grape extract-loaded solid lipid nanoparticles for the treatment of Alzheimer's disease. Molecules. 2017;22:E277. doi: 10.3390/molecules22020277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo CF, Yuan M, Chen MS, Liu SM, Zhu L, Huang BY, Liu XW, Xiong W. Pharmacokinetics, tissue distribution and relative bioavailability of puerarin solid lipid nanoparticles following oral administration. Int J Pharm. 2011;410:138–144. doi: 10.1016/j.ijpharm.2011.02.064. [DOI] [PubMed] [Google Scholar]
- Lushchak O, Zayachkivska A, Vaiserman A. Metallic Nanoantioxidants as Potential Therapeutics for Type 2 Diabetes: A Hypothetical Background and Translational Perspectives. Oxid Med Cell Longev. 2018;2018:3407375. doi: 10.1155/2018/3407375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magalingam KB, Radhakrishnan A, Ping NS, Haleagrahara N. Current concepts of neurodegenerative mechanisms in Alzheimer's disease. Biomed Res Int. 2018;2018:3740461. doi: 10.1155/2018/3740461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel J, Ojcius DM, Ko YF, Chang CJ, Young JD (2019) Antiaging effects of bioactive molecules isolated from plants and fungi. Med Res Rev. 10.1002/med.21559 [DOI] [PubMed]
- Martín Giménez VM, Kassuha DE, Manucha W. Nanomedicine applied to cardiovascular diseases: latest developments. Ther Adv Cardiovasc Dis. 2017;11:133–142. doi: 10.1177/1753944717692293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Ballesta M, Gil-Izquierdo Á, García-Viguera C, Domínguez-Perles R. Nanoparticles and controlled delivery for bioactive compounds: Outlining challenges for new "smart-foods" for health. Foods. 2018;7:E72. doi: 10.3390/foods7050072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masserini M. Nanoparticles for brain drug delivery. ISRN Biochemistry. 2013;2013:238428. doi: 10.1155/2013/238428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meena R, Kumar S, Kumar R, Gaharwar US, Rajamani P. PLGA-CTAB curcumin nanoparticles: Fabrication, characterization and molecular basis of anticancer activity in triple negative breast cancer cell lines (MDA-MB-231 cells) Biomed Pharmacother. 2017;94:944–954. doi: 10.1016/j.biopha.2017.07.151. [DOI] [PubMed] [Google Scholar]
- Mehnert W, Mäder K. Solid lipid nanoparticles: production, characterization and applications. Adv Drug Deliv Rev. 2001;47:165–196. doi: 10.1016/S0169-409X(01)00105-3. [DOI] [PubMed] [Google Scholar]
- Mereles D, Hunstein W. Epigallocatechin-3-gallate (EGCG) for clinical trials: more pitfalls than promises? Int J Mol Sci. 2011;12:5592–5603. doi: 10.3390/ijms12095592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra V, Bansal KK, Verma A, Yadav N, Thakur S, Sudhakar K, Rosenholm JM. Solid lipid nanoparticles: emerging colloidal nano drug delivery systems. Pharmaceutics. 2018;10:E191. doi: 10.3390/pharmaceutics10040191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mody VV, Siwale R, Singh A, Mody HR. Introduction to metallic nanoparticles. J Pharm Bioallied Sci. 2010;2:282–289. doi: 10.4103/0975-7406.72127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monsalve B, Concha-Meyer A, Palomo I, Fuentes E. Mechanisms of endothelial protection by natural bioactive compounds from fruit and vegetables. An Acad Bras Cienc. 2017;89:615–633. doi: 10.1590/0001-3765201720160509.. [DOI] [PubMed] [Google Scholar]
- Montalban MG, Coburn JM, Lozano-Perez AA, Cenis JL, Villora G, Kaplan DL. Production of curcumin-loaded silk fibroin nanoparticles for cancer therapy. Nanomaterials (Basel) 2018;8:E126. doi: 10.3390/nano8020126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss DM, Curley P, Kinvig H, Hoskins C, Owen A. The biological challenges and pharmacological opportunities of orally administered nanomedicine delivery. Expert Rev Gastroenterol Hepatol. 2018;12:223–236. doi: 10.1080/17474124.2018.1399794. [DOI] [PubMed] [Google Scholar]
- Muradian K, Vaiserman A, Min KJ, Fraifeld VE. Fucoxanthin and lipid metabolism: A minireview. Nutr Metab Cardiovasc Dis. 2015;25:891–897. doi: 10.1016/j.numecd.2015.05.010. [DOI] [PubMed] [Google Scholar]
- Myers A, Lithgow GJ. Drugs that target aging: how do we discover them? Expert Opin Drug Discov. 2019;14:541–548. doi: 10.1080/17460441.2019.1597049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myung SK, Ju W, Cho B, Oh SW, Park SM, Koo BK, Park BJ (2013) Korean meta–analysis study group. efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta–analysis of randomised controlled trials. BMJ 346:f10. 10.1136/bmj.f10 [DOI] [PMC free article] [PubMed]
- Naseri N, Valizadeh H, Zakeri-Milani P. Solid lipid nanoparticles and nanostructured lipid carriers: structure, preparation and application. Adv Pharm Bull. 2015;5:305–313. doi: 10.15171/apb.2015.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni W, Li Z, Liu Z, Ji Y, Wu L, Sun S, Jian X, Gao X. Dual-targeting nanoparticles: codelivery of curcumin and 5-fluorouracil for synergistic treatment of hepatocarcinoma. J Pharm Sci. 2019;108:1284–1295. doi: 10.1016/j.xphs.2018.10.042. [DOI] [PubMed] [Google Scholar]
- Pandey MK, Gupta SC, Karelia D, Gilhooley PJ, Shakibaei M, Aggarwal BB. Dietary nutraceuticals as backbone for bone health. Biotechnol Adv. 2018;36:1633–1648. doi: 10.1016/j.biotechadv.2018.03.014. [DOI] [PubMed] [Google Scholar]
- Patisaul HB. Endocrine disruption by dietary phyto-oestrogens: impact on dimorphic sexual systems and behaviours. Proc Nutr Soc. 2017;76:130–144. doi: 10.1017/S0029665116000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrott KM, Wiley CD, Desprez PY, Campisi J. Apigenin suppresses the senescence–associated secretory phenotype and paracrine effects on breast cancer cells. Geroscience. 2017;39:161–173. doi: 10.1007/s11357-017-9970-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazzini V, Lemmi B, D’Ambrosio M, Cinci L, Luceri C, Bilia AR, Bergonzi MC. Nanostructured lipid carriers as promising delivery systems for plant extracts: The case of silymarin. Appl Sci. 2018;8:1163. doi: 10.3390/app8071163. [DOI] [Google Scholar]
- Popat R, Plesner T, Davies F, Cook G, Cook M, Elliott P, Jacobson E, Gumbleton T, Oakervee H, Cavenagh J. A phase 2 study of SRT501 (resveratrol) with bortezomib for patients with relapsed and or refractory multiple myeloma. Br J Haematol. 2013;160:714–717. doi: 10.1111/bjh.12154. [DOI] [PubMed] [Google Scholar]
- Qiao Y, Wan J, Zhou L, Ma W, Yang Y, Luo W, Yu Z, Wang H. Stimuli-responsive nanotherapeutics for precision drug delivery and cancer therapy. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2019;11:e1527. doi: 10.1002/wnan.1527. [DOI] [PubMed] [Google Scholar]
- Rabinovici GD. Late-onset Alzheimer disease. Continuum (Minneap Minn) 2019;25:14–33. doi: 10.1212/CON.0000000000000700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M, Beg S, Verma A, Al Abbasi FA, Anwar F, Saini S, Akhter S, Kumar V. Phytoconstituents as pharmacotherapeutics in rheumatoid arthritis: challenges and scope of nano/submicromedicine in its effective delivery. J Pharm Pharmacol. 2017;69:1–14. doi: 10.1111/jphp.12661. [DOI] [PubMed] [Google Scholar]
- Ramalingam P, Ko YT. Enhanced oral delivery of curcumin from N-trimethyl chitosan surface-modified solid lipid nanoparticles: pharmacokinetic and brain distribution evaluations. Pharm Res. 2015;32:89–402. doi: 10.1007/s11095-014-1469-1. [DOI] [PubMed] [Google Scholar]
- Ramalingam P, Ko YT. Improved oral delivery of resveratrol from N-trimethyl chitosan-g-palmitic acid surface-modified solid lipid nanoparticles. Colloids Surf B Biointerfaces. 2016;139:52–61. doi: 10.1016/j.colsurfb.2015.11.050. [DOI] [PubMed] [Google Scholar]
- Ramalingam P, Yoo SW, Ko YT. Nanodelivery systems based on mucoadhesive polymer coated solid lipid nanoparticles to improve the oral intake of food curcumin. Food Res Int. 2016;84:113–119. doi: 10.1016/j.foodres.2016.03.031. [DOI] [Google Scholar]
- Rassu G, Porcu EP, Fancello S, Obinu A, Senes N, Galleri G, Migheli R, Gavini E, Giunchedi P. Intranasal delivery of genistein-loaded nanoparticles as a potential preventive system against neurodegenerative disorders. Pharmaceutics. 2018;11:E8. doi: 10.3390/pharmaceutics11010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastogi R, Anand S, Koul V. Flexible polymerosomes––an alternative vehicle for topical delivery. Colloids Surf B Biointerfaces. 2009;72:161–166. doi: 10.1016/j.colsurfb.2009.03.022. [DOI] [PubMed] [Google Scholar]
- Ravindran S, Suthar JK, Rokade R, Deshpande P, Singh P, Pratinidhi A, Khambadkhar R, Utekar S. Pharmacokinetics, metabolism, distribution and permeability of nanomedicine. Curr Drug Metab. 2018;19:327–334. doi: 10.2174/1389200219666180305154119. [DOI] [PubMed] [Google Scholar]
- Rizvi SAA, Saleh AM. Applications of nanoparticle systems in drug delivery technology. Saudi Pharm J. 2018;26:64–70. doi: 10.1016/j.jsps.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodenak-Kladniew B, Islan GA, de Bravo MG, Durán N, Castro GR. Design, characterization and in vitro evaluation of linalool-loaded solid lipid nanoparticles as potent tool in cancer therapy. Colloids Surf B Biointerfaces. 2017;154:123–132. doi: 10.1016/j.colsurfb.2017.03.021. [DOI] [PubMed] [Google Scholar]
- Rousseaux MWC, Shulman JM, Jankovic J. Progress toward an integrated understanding of Parkinson's disease. F1000Res. 2017;6:1121. doi: 10.12688/f1000research.11820.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeedi M, Eslamifar M, Khezri K, Dizaj SM. Applications of nanotechnology in drug delivery to the central nervous system. Biomed Pharmacother. 2019;111:666–675. doi: 10.1016/j.biopha.2018.12.133. [DOI] [PubMed] [Google Scholar]
- Saha S, Sadhukhan P, Sil PC. Genistein: a phytoestrogen with multifaceted therapeutic properties. Mini Rev Med Chem. 2014;14:920–940. doi: 10.2174/1389557514666141029233442. [DOI] [PubMed] [Google Scholar]
- Salehi B, Stojanović-Radić Z, Matejić J, Sharifi-Rad M, Anil Kumar NV, Martins N, Sharifi-Rad J. The therapeutic potential of curcumin: A review of clinical trials. Eur J Med Chem. 2019;163:527–545. doi: 10.1016/j.ejmech.2018.12.016. [DOI] [PubMed] [Google Scholar]
- Santín-Márquez R, Alarcón-Aguilar A, López-Diazguerrero NE, Chondrogianni N, Königsberg M (2019) Sulforaphane – role in aging and neurodegeneration. Geroscience (In press). [DOI] [PMC free article] [PubMed]
- Sarker MR, Franks SF. Efficacy of curcumin for age–associated cognitive decline: a narrative review of preclinical and clinical studies. Geroscience. 2018;40:73–95. doi: 10.1007/s11357-018-0017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seals DR, Melov S. Translational geroscience: emphasizing function to achieve optimal longevity. Aging (Albany NY) 2014;6:718–730. doi: 10.18632/aging.100694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seals DR, Justice JN, LaRocca TJ. Physiological geroscience: targeting function to increase healthspan and achieve optimal longevity. J Physiol. 2016;594:2001–2024. doi: 10.1113/jphysiol.2014.282665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seca AML, Pinto DCGA. Overview on the antihypertensive and anti-obesity effects of secondary metabolites from seaweeds. Mar Drugs. 2018;16:E237. doi: 10.3390/md16070237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah SMA, Akram M, Riaz M, Munir N, Rasool G. Cardioprotective potential of plant–derived molecules: a scientific and medicinal approach. Dose Response. 2019;17:1559325819852243. doi: 10.1177/1559325819852243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi M, Shi YL, Li XM, Yang R, Cai ZY, Li QS, Ma SC, Ye JH, Lu JL, Liang YR, Zheng XQ. Food-grade encapsulation systems for (−)-epigallocatechin gallate. Molecules. 2018;23:445. doi: 10.3390/molecules23020445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shome S, Talukdar AD, Choudhury MD, Bhattacharya MK, Upadhyaya H. Curcumin as potential therapeutic natural product: a nanobiotechnological perspective. J Pharm Pharmacol. 2016;68:1481–1500. doi: 10.1111/jphp.12611. [DOI] [PubMed] [Google Scholar]
- Siddiqui IA, Bharali DJ, Nihal M, Adhami VM, Khan N, Chamcheu JC, Khan MI, Shabana S, Mousa SA, Mukhtar H. Excellent anti-proliferative and pro-apoptotic effects of (-)-epigallocatechin-3-gallate encapsulated in chitosan nanoparticles on human melanoma cell growth both in vitro and in vivo. Nanomedicine. 2014;10:1619–1626. doi: 10.1016/j.nano.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Silva Adaya D, Aguirre-Cruz L, Guevara J, Ortiz-Islas E. Nanobiomaterials' applications in neurodegenerative diseases. J Biomater Appl. 2017;31:953–984. doi: 10.1177/0885328216659032. [DOI] [PubMed] [Google Scholar]
- Singh BN, Shankar S, Srivastava RK. Green tea catechin, epigallocatechin-3-gallate (EGCG): mechanisms, perspectives and clinical applications. Biochem Pharmacol. 2011;82:1807–1821. doi: 10.1016/j.bcp.2011.07.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh NA, Bhardwaj V, Ravi C, Ramesh N, Mandal AKA, Khan ZA. EGCG nanoparticles attenuate aluminum chloride induced neurobehavioral deficits, beta amyloid and tau pathology in a rat model of Alzheimer's disease. Front Aging Neurosci. 2018;10:244. doi: 10.3389/fnagi.2018.00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AP, Singh R, Verma SS, Rai V, Kaschula CH, Maiti P, Gupta SC (2019) Health benefits of resveratrol: Evidence from clinical studies. Med Res Rev. 10.1002/med.21565 [DOI] [PubMed]
- Siu FY, Ye S, Lin H, Li S. Galactosylated PLGA nanoparticles for the oral delivery of resveratrol: enhanced bioavailability and in vitro anti-inflammatory activity. Int J Nanomedicine. 2018;13:4133–4144. doi: 10.2147/IJN.S164235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, Groop PH, Handelsman Y, Insel RA, Mathieu C, McElvaine AT, Palmer JP, Pugliese A, Schatz DA, Sosenko JM, Wilding JP, Ratner RE. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. 2017;66:241–255. doi: 10.2337/db16-0806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoliga JM, Blanchard O. Enhancing the delivery of resveratrol in humans: if low bioavailability is the problem, what is the solution? Molecules. 2014;19:17154–17172. doi: 10.3390/molecules191117154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoliga JM, Vang O, Baur JA. Challenges of translating basic research into therapeutics: resveratrol as an example. J Gerontol A Biol Sci Med Sc. 2012;67:158–167. doi: 10.1093/gerona/glr062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somu P, Paul S. Supramolecular nanoassembly of lysozyme and α-lactalbumin (apo α-LA) exhibits selective cytotoxicity and enhanced bioavailability of curcumin to cancer cells. Colloids Surf B Biointerfaces. 2019;178:297–306. doi: 10.1016/j.colsurfb.2019.03.016. [DOI] [PubMed] [Google Scholar]
- Stolarczyk EU, Stolarczyk K, Łaszcz M, Kubiszewski M, Maruszak W, Olejarz W, Bryk D. Synthesis and characterization of genistein conjugated with gold nanoparticles and the study of their cytotoxic properties. Eur J Pharm Sci. 2017;96:176–185. doi: 10.1016/j.ejps.2016.09.019. [DOI] [PubMed] [Google Scholar]
- Sunagawa Y, Wada H, Suzuki H, Sasaki H, Imaizumi A, Fukuda H, Hashimoto T, Katanasaka Y, Shimatsu A, Kimura T, Kakeya H, Fujita M, Hasegawa K, Morimoto T. A novel drug delivery system of oral curcumin markedly improves efficacy of treatment for heart failure after myocardial infarction in rats. Biol Pharm Bull. 2012;35:139–144. doi: 10.1248/bpb.35.139. [DOI] [PubMed] [Google Scholar]
- Sundar DKS, Houreld NN, Abrahamse H. Therapeutic potential and recent advances of curcumin in the treatment of aging-associated diseases. Molecules. 2018;23:E835. doi: 10.3390/molecules23040835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan ME, He CH, Jiang W, Zeng C, Yu N, Huang W, Gao ZG, Xing JG. Development of solid lipid nanoparticles containing total flavonoid extract from Dracocephalum moldavica L. and their therapeutic effect against myocardial ischemia-reperfusion injury in rats. Int J Nanomedicine. 2017;12:253–3265. doi: 10.2147/IJN.S131893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan BL, Norhaizan ME, Liew WP, Sulaiman Rahman H. Antioxidant and oxidative stress: a mutual interplay in age–related diseases. Front Pharmacol. 2018;9:1162. doi: 10.3389/fphar.2018.01162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang P, Sun Q, Yang H, Tang B, Pu H, Li H. Honokiol nanoparticles based on epigallocatechin gallate functionalized chitin to enhance therapeutic effects against liver cancer. Int J Pharm. 2018;545:74–83. doi: 10.1016/j.ijpharm.2018.04.060. [DOI] [PubMed] [Google Scholar]
- Teleanu DM, Chircov C, Grumezescu AM, Volceanov A, Teleanu RI. Blood-brain delivery methods using nanotechnology. Pharmaceutics. 2018;10:269. doi: 10.3390/pharmaceutics10040269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai YM, Jan WC, Chien CF, Lee WC, Lin LC, Tsai TH. Optimised nano-formulation on the bioavailability of hydrophobic polyphenol, curcumin, in freely-moving rats. Food Chem. 2011;127:918–925. doi: 10.1016/j.foodchem.2011.01.059. [DOI] [PubMed] [Google Scholar]
- Tuguntaev RG, Okeke CI, Xu J, Li C, Wang PC, Liang XJ. Nanoscale polymersomes as anti–cancer drug carriers applied for pharmaceutical delivery. Curr Pharm Des. 2016;22:2857–2865. doi: 10.2174/1381612822666160217142319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah F, Liang A, Rangel A, Gyengesi E, Niedermayer G, Münch G. High bioavailability curcumin: an anti-inflammatory and neurosupportive bioactive nutrient for neurodegenerative diseases characterized by chronic neuroinflammation. Arch Toxicol. 2017;91:1623–1634. doi: 10.1007/s00204-017-1939-4. [DOI] [PubMed] [Google Scholar]
- Ungvari Z, Tarantini S, Kiss T, Wren JD, Giles CB, Griffin CT, Murfee WL, Pacher P, Csiszar A. Endothelial dysfunction and angiogenesis impairment in the ageing vasculature. Nat Rev Cardiol. 2018;15:555–565. doi: 10.1038/s41569-018-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungvari Z, Tarantini S, Donato AJ, Galvan V, Csiszar A. Mechanisms of vascular aging. Circ Res. 2018;123:849–867. doi: 10.1161/CIRCRESAHA.118.311378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaiserman A, Lushchak O. Implementation of longevity-promoting supplements and medications in public health practice: achievements, challenges and future perspectives. J Transl Med. 2017;15:160. doi: 10.1186/s12967-017-1259-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaiserman AM, Marotta F. Longevity-promoting pharmaceuticals: is it a time for implementation? Trends Pharmacol Sci. 2016;37:331–333. doi: 10.1016/j.tips.2016.02.003. [DOI] [PubMed] [Google Scholar]
- van der Vlies AJ, Morisaki M, Neng HI, Hansen EM, Hasegawa U. Framboidal nanoparticles containing a curcumin-phenylboronic acid complex with antiangiogenic and anticancer activities. Bioconjug Chem. 2019;30:861–870. doi: 10.1021/acs.bioconjchem.9b00006. [DOI] [PubMed] [Google Scholar]
- van Onna M, Boonen A. The challenging interplay between rheumatoid arthritis, ageing and comorbidities. BMC Musculoskelet Disord. 2016;17:184. doi: 10.1186/s12891-016-1038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar A, Baskaran R, Jang YS, Oh SH, Yoo BK. Quercetin-loaded solid lipid nanoparticle dispersion with improved physicochemical properties and cellular uptake. AAPS PharmSciTech. 2016;18:875–883. doi: 10.1208/s12249-016-0573-4. [DOI] [PubMed] [Google Scholar]
- Vivekanantham S, Shah S, Dewji R, Dewji A, Khatri C, Ologunde R. Neuroinflammation in Parkinson's disease: role in neurodegeneration and tissue repair. Int J Neurosci. 2015;125:717–725. doi: 10.3109/00207454.2014.982795. [DOI] [PubMed] [Google Scholar]
- Wang S, Chen T, Chen R, Hu Y, Chen M, Wang Y. Emodin loaded solid lipid nanoparticles: preparation, characterization and antitumor activity studies. Int J Pharm. 2012;430:238–246. doi: 10.1016/j.ijpharm.2012.03.027. [DOI] [PubMed] [Google Scholar]
- Wang L, Li H, Wang S, Liu R, Wu Z, Wang C, Wang Y, Chen M. Enhancing the antitumor activity of berberine hydrochloride by solid lipid nanoparticle encapsulation. AAPS PharmSciTech. 2014;15:834–844. doi: 10.1208/s12249-014-0112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Wang S, Chen R, Wang Y, Li H, Wang Y, Chen M. Oridonin loaded solid lipid nanoparticles enhanced antitumor activity in MCF-7 cells. J Nanomater. 2014;2014:903646. doi: 10.1155/2014/903646. [DOI] [Google Scholar]
- Wang J, Wang H, Zhu R, Liu Q, Fei J, Wang S. Anti-inflammatory activity of curcumin-loaded solid lipid nanoparticles in IL-1b transgenic mice subjected to the lipopolysaccharide-induced sepsis. Biomaterials. 2015;53:475–483. doi: 10.1016/j.biomaterials.2015.02.116. [DOI] [PubMed] [Google Scholar]
- Wang J, Ma W, Tu P. Synergistically improved anti-tumor efficacy by co-delivery doxorubicin and curcumin polymeric micelles. Macromol Biosci. 2015;15:1252–1261. doi: 10.1002/mabi.201500043. [DOI] [PubMed] [Google Scholar]
- Wang L, Wang W, Rui Z, Zhou D. The effective combination therapy against human osteosarcoma: doxorubicin plus curcumin co-encapsulated lipid-coated polymeric nanoparticulate drug delivery system. Drug Deliv. 2016;23:3200–3208. doi: 10.3109/10717544.2016.1162875. [DOI] [PubMed] [Google Scholar]
- Wang W, Zhang L, Chen T, Guo W, Bao X, Wang D, Ren B, Wang H, Li Y, Wang Y, Chen S, Tang B, Yang Q, Chen C. Anticancer effects of resveratrol-loaded solid lipid nanoparticles on human breast cancer cells. Molecules. 2017;22:E1814. doi: 10.3390/molecules22111814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Chen T, Xu H, Ren B, Cheng X, Qi R, Liu H, Wang Y, Yan L, Chen S, Yang Q, Chen C. Curcumin-loaded solid lipid nanoparticles enhanced anticancer efficiency in breast cancer. Molecules. 2018;23:E1578. doi: 10.3390/molecules23071578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Wen B, Yu H, Ding D, Zhang J, Zhang Y, Zhao L, Zhang W. Berberine hydrochloride-loaded chitosan nanoparticles effectively targets and suppresses human nasopharyngeal carcinoma. J Biomed Nanotechnol. 2018;14:1486–1495. doi: 10.1166/jbn.2018.2596. [DOI] [PubMed] [Google Scholar]
- Wojcik M, Krawczyk M, Wojcik P, Cypryk K, Wozniak LA. Molecular mechanisms underlying curcumin-mediated therapeutic effects in type 2 diabetes and cancer. Oxid Med Cell Longev. 2018;2018:9698258. doi: 10.1155/2018/9698258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong KH, Riaz MK, Xie Y, Zhang X, Liu Q, Chen H, Bian Z, Chen X, Lu A, Yang Z. Review of current strategies for delivering Alzheimer's disease drugs across the blood-brain barrier. Int J Mol Sci. 2019;20:E381. doi: 10.3390/ijms20020381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (2012) World health statistics. http://www.who.int/gho/publications/world_health_statistics/2012/en/.
- Wu YR, Choi HJ, Kang YG, Kim JK, Shin JW. In vitro study on anti-inflammatory effects of epigallocatechin-3-gallate-loaded nano- and microscale particles. Int J Nanomedicine. 2017;12:7007–7013. doi: 10.2147/IJN.S146296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H, Jia F, Singh PK, Ruan S, Zhang H, Li X. Synergistic anti-glioma effect of a coloaded nano-drug delivery system. Int J Nanomedicine. 2016;12:29–40. doi: 10.2147/IJN.S116367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue M, Yang MX, Zhang W, Li XM, Gao DH, Ou ZM, Li ZP, Liu SH, Li XJ, Yang SY. Characterization, pharmacokinetics, and hypoglycemic effect of berberine loaded solid lipid nanoparticles. Int J Nanomedicine. 2013;8:4677–4687. doi: 10.2147/IJN.S51262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue M, Zhang L, Yang MX, Zhang W, Li XM, Ou ZM, Li ZP, Liu SH, Li XJ, Yang SY. Berberine-loaded solid lipid nanoparticles are concentrated in the liver and ameliorate hepatosteatosis in db/db mice. Int J Nanomedicine. 2015;10:5049–5057. doi: 10.2147/IJN.S84565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabluchanskiy A, Ungvari Z, Csiszar A, Tarantini S. Advances and challenges in geroscience research: An update. Physiol Int. 2018;105:298–308. doi: 10.1556/2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan J, Wang Y, Zhang X, Liu S, Tian C, Wang H. Targeted nanomedicine for prostate cancer therapy: docetaxel and curcumin co-encapsulated lipid-polymer hybrid nanoparticles for the enhanced anti-tumor activity in vitro and in vivo. Drug Deliv. 2016;23:1757–1762. doi: 10.3109/10717544.2015.1069423. [DOI] [PubMed] [Google Scholar]
- Yang X, Li Z, Wang N, Li L, Song L, He T, Sun L, Wang Z, Wu Q, Luo N, Yi C, Gong C. Curcumin-encapsulated polymeric micelles suppress the development of colon cancer in vitro and in vivo. Sci Rep. 2015;5:10322. doi: 10.1038/srep10322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf M, Khan M, Khan RA, Ahmed B. Preparation, characterization, in vivo and biochemical evaluation of brain targeted Piperine solid lipid nanoparticles in an experimentally induced Alzheimer’s disease model. J Drug Target. 2012;21:300–311. doi: 10.3109/1061186X.2012.747529. [DOI] [PubMed] [Google Scholar]
- Zamboni WC, Torchilin V, Patri AK, Hrkach J, Stern S, Lee R, Nel A, Panaro NJ, Grodzinski P. Best practices in cancer nanotechnology: perspective from NCI nanotechnology alliance. Clin Cancer Res. 2012;18:3229–3241. doi: 10.1158/1078-0432.CCR-11-2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng L, Yan J, Luo L, Ma M, Zhu H. Preparation and characterization of (-)-Epigallocatechin-3-gallate (EGCG)-loaded nanoparticles and their inhibitory effects on Human breast cancer MCF-7 cells. Sci Rep. 2017;7:45521. doi: 10.1038/srep45521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang G, Zhang J. Enhanced oral bioavailability of EGCG using pH-sensitive polymeric nanoparticles: characterization and in vivo investigation on nephrotic syndrome rats. Drug Des Devel Ther. 2018;12:2509–2518. doi: 10.2147/DDDT.S172919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Yu J, Qiang L, Gu Z. Nanomedicine for obesity treatment. Sci China Life Sci. 2018;61:373–379. doi: 10.1007/s11427-017-9257-1. [DOI] [PubMed] [Google Scholar]
- Zhang D, Zhang J, Zeng J, Li Z, Zuo H, Huang C, Zhao X. Nano-gold loaded with resveratrol enhance the anti-hepatoma effect of resveratrol in vitro and in vivo. J Biomed Nanotechnol. 2019;15:288–300. doi: 10.1166/jbn.2019.2682. [DOI] [PubMed] [Google Scholar]
- Zheng X, Zhang F, Shao D, Zhang Z, Cui L, Zhang J, Dawulieti J, Meng Z, Zhang M, Chen L. Gram-scale production of carrier-free fluorescent berberine microrods for selective liver cancer therapy. Biofactors. 2018;44:496–502. doi: 10.1002/biof.1450. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Du J, Wang L, Wang Y. Nanocrystals technology for improving bioavailability of poorly soluble drugs: a mini–review. J Nanosci Nanotechnol. 2017;17:18–28. doi: 10.1166/jnn.2017.13108. [DOI] [PubMed] [Google Scholar]
- Zhu B, Yu L, Yue Q. Co-delivery of vincristine and quercetin by nanocarriers for lymphoma combination chemotherapy. Biomed Pharmacother. 2017;91:287–294. doi: 10.1016/j.biopha.2017.02.112. [DOI] [PubMed] [Google Scholar]
- Zhu F, Du B, Xu B. Anti–inflammatory effects of phytochemicals from fruits, vegetables, and food legumes: A review. Crit Rev Food Sci Nutr. 2018;58:1260–1270. doi: 10.1080/10408398.2016.1251390. [DOI] [PubMed] [Google Scholar]
- Zierer J, Menni C, Kastenmüller G, Spector TD. Integration of 'omics' data in aging research: from biomarkers to systems biology. Aging Cell. 2015;14:933–944. doi: 10.1111/acel.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]