Abstract
Background:
As future practitioners, undergraduate medical students have a key role in the antimicrobial stewardship program (ASP). However, at present, there are not much data about their knowledge and perception of antibiotic resistance and ASP.
Methods:
This was a cross-sectional questionnaire-based survey administered to the prefinal- and final-year undergraduate medical students of a tertiary care institution.
Results:
One hundred and ninety-seven students participated in our study constituting 70% response rate. The mean difference in knowledge score between prefinal- and final-year students was 0.77 (95% confidence interval: 0.30–1.24, P = 0.0016). Thirty-seven (39.7%) prefinal- and 57 (54.8%) final-year students knew the correct definition of antimicrobial stewardship. Majority of the participants, i.e., 66 (70.9%) prefinal-year and 80 (76.9%) final-year students perceived antibiotic resistance as a public health problem. Principal component analysis revealed the greater role of attitude-related questions.
Conclusion:
Good knowledge and positive attitude are paramount for the effective implementation of the antibiotic stewardship program. Our study revealed that the knowledge gap exists among the undergraduate students about the rational use of the antibiotic stewardship program. It was also revealed that the role of attitude plays a more significant role than knowledge for the proper understanding of the program. A sustained effort is required to make them aware of the rational use of antibiotics by incorporating the knowledge and practice of the ASP into their study curriculum.
Keywords: Antibiotic resistance, antimicrobial stewardship, rational antibiotic use, undergraduate medical students
INTRODUCTION
Antibiotic resistance is a serious public health problem and is rising alarmingly in all parts of the world.[1,2,3] As the innovation and development of new antibiotic has waned up, resistance to the majority of currently used lifesaving antibiotics has caused concern among the health professionals, policy experts, and health agencies including the World Health Organization (WHO).[4,5,6] It would not be an exaggeration if we said that the world is staring into a possible situation akin to preantibiotic era.[7] There are a plethora of reasons which have led to this precarious position, and inappropriate and indiscriminate use of antibiotics in human and veterinary medicine is prominent among those.[8] The WHO along with other stakeholders is working in tandem to combat the growing menace of antibiotic resistance. A multipronged strategy is the need of the hour to overcome the enormous challenges posed by it. Adoption of various measures such as better surveillance of resistant strains, stringent infection control practice, and antimicrobial stewardship (AMS) is required to reduce the rise of antibiotic resistance.[9] Antimicrobial stewardship program (ASP) refers to the coordinated intervention designed to improve the appropriate use of antimicrobial agents by promoting the selection of the optimal antimicrobial drug regimen, dose, duration of therapy, and routes of administration.[10,11]
One of the key facets of ASP is to disseminate knowledge about the adverse outcomes of antibiotic resistance among health-care professionals and patients.[12] Currently, most of the AMS education and training programs involve practicing physicians.[13] Many studies have been undertaken to evaluate the knowledge, perception, and practice of AMS among medical practitioners.[14,15]
Postgraduate and undergraduate training period in medical science is an important time to foster correct practice about the prudent uses of antibiotic. Education of medical students on AMS is important for the promotion of rational use of antibiotics.[16,17] Although few countries have included education and training program about the appropriate use of antibiotics in the undergraduate curricula, the comprehensive evaluation of awareness and perception of AMS among undergraduate medical students is largely lacking.[18]
Hence, this study was carried out with the objectives to assess the knowledge and attitude of undergraduate medical students toward antimicrobial resistance (AMR) and stewardship.
MATERIALS AND METHODS
Study design and population
This study was a cross-sectional study designed to evaluate the knowledge and attitude of undergraduate medical students regarding antibiotic resistance and ASP. The final- and prefinal-year undergraduate medical students who had completed pharmacology training were included in this study (n = 270).
Study site
This study was conducted in a tertiary care teaching institute of South Indian city, Pondicherry.
Ethics
The study was commenced after obtaining the approval from the Institutional Ethics Committee. The participation by the students in this study was voluntary, and at no point, they were coerced or induced in any manner. The written informed consent was sought from all the participants before including them in the study.
Survey instrument
A 20-item survey tool was designed to collect information about AMR and ASP from the participants. The structured survey instrument was designed collaboratively by faculties from the department of pharmacology, microbiology, and general medicine. It contains 20 questions, 10 each to assess the knowledge and attitude. The content validity of the questionnaire was carried out by an expert panel to assess the relevance, clarity, and simplicity of questions. Then, the survey tools were pretested in 30 numbers of students to assess the appropriateness, relevance, and comprehensibility of questions. Test–retest method was used to measure the reliability of the questionnaire (Cronbach's coefficient alpha – 0.75).
Survey administration
The modified survey instrument was distributed to the participants by investigators after explaining the purpose of the study. Twenty-minute time was given to the participants to fill up the questionnaire. The completely filled questionnaires returned by the participants were included in the final analysis. Knowledge was assessed by a scoring system. A score of 1 was allocated to each correct answer; there was no negative score for the wrong answer. Mean knowledge score of <50%, 50%–70%, and >70% was considered poor, average, and good performance, respectively. The attitude was assessed using three-point Likert scales (0 – agree, 1 – disagree, and 2 – do not know).
Statistical analysis
The data were managed by Microsoft Excel 2016 and analyzed using the R programming language (version 3.4, R-core team, Vienna, Austria). Continuous data were expressed as mean ± standard deviation and categorical data were represented in proportions. The normality of the data was assessed by the Shapiro–Wilk test. The difference between the groups was assessed using the t-test for continuous data and Fisher's exact test for categorical data.
A sample of 79 in each group was required to detect the difference of 0.9 in the mean knowledge score between the prefinal- and final-year groups. The standard deviation assumed was 2. This sample was powered at 80% to detect the difference allowing an alpha error rate of 5%.
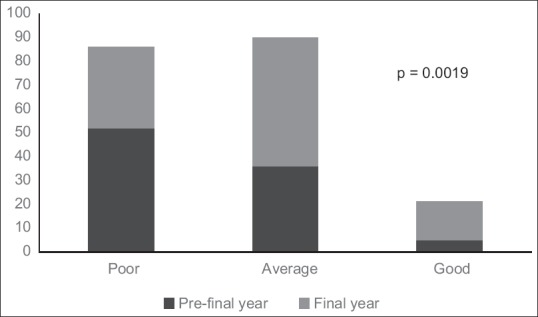
We performed principal component analysis (PCA), a dimensionality reduction method to find the important variables determining the pattern or trend of overall data obtained from the study. This method detected the indispensable questions from the tool which was used in evaluating the knowledge and attitude regarding the AMS. This would guide in determining the relevant questions to assess the knowledge about the ASP among the undergraduate medical students.
RESULTS
Out of the 270 respondents (130 prefinal-year and 140 final-year students), 197 (93 prefinal-year and 104 final-year students) returned the completely filled questionnaire. Hence, the response rate of our study was approximately 70% (74% and 71% for final- and prefinal-year students, respectively).
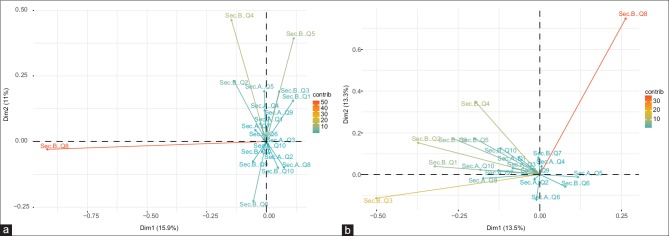
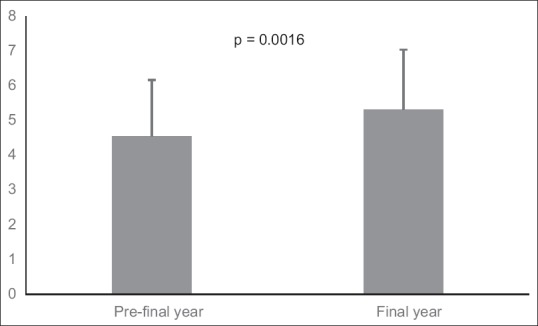
In this survey, the mean knowledge score of the prefinal- and final-year students was 4.56 ± 1.62 and 5.33 ± 1.72, respectively. The difference in the score was significant (0.778 [0.30–1.24], P = 0.0016) [Figure 1]. In the prefinal group, 52, 36, and 5 secured poor, average, and good scores, respectively, which were significantly different (P = 0.0019) from the final-year group where 34, 54, and 16 secured poor, average, and good scores, respectively [Figure 2].
Figure 1.
Bar diagram showing the mean (standard deviation) knowledge score of the respondents
Figure 2.
Graph showing the number of students in various categories of scoring in the knowledge component in both the groups
The maximum number of participants in both the groups (69 prefinal-year and 81 final-year students) knew that antibiotic is not useful in viral diseases (P = 0.54). Twenty-eight (30.1%) prefinal-year and 14 (13.4%) final-year students correctly replied to the most effective method for prevention of methicillin-resistant Staphylococcus aureus (MRSA) infection. The difference between the two groups of respondents was found to be statistically significant (P = 0.004). More number of final-year students (57, 54.8%) correctly defined ASP than final-year (37, 39.7%) students (P = 0.04). Table 1 depicts the response of participants to the knowledge-based questions.
Table 1.
Summary of medical students' knowledge about antibiotic resistance and antibiotic stewardship
| Knowledge-based questions | Correct response |
P | |
|---|---|---|---|
| Grade I (prefinal year) (n=93), n (%) | Grade II (final year) (n=104), n (%) | ||
| In which of the following disease antibiotic is not useful? | 69 (74.1) | 81 (77.8) | 0.54 |
| Which of the following is a bactericidal agent? | 51 (54) | 76 (73) | 0.001 |
| Which of the following antibiotic has the narrow spectrum of activity? | 50 (53) | 74 (71) | 0.001 |
| What is antimicrobial stewardship? | 37 (39.7) | 57 (54.8) | 0.04 |
| Which of the following does not contribute to the development of antibiotic resistance? | 51 (54.8) | 72 (69.2) | 0.001 |
| R factors are ___ that contains a code for ___ | 62 (66.6) | 60 (57.6) | 0.2 |
| Which of the following WHO statements are true regarding AMR? | 37 (39.7) | 53 (50.9) | 0.12 |
| Currently, two-third of the health-care-associated infection is caused by just six multidrug resistant organisms with acronym ESKAPE. Which of the following organism is not among them? | 30 (32.2) | 28 (26.9) | 0.33 |
| Which of the following drug is useful for MRSA infection? | 35 (37.6) | 26 (25) | 0.06 |
| Which of the following is the most effective method for prevention of MRSA infection? | 28 (30.1) | 14 (13.4) | 0.004 |
AMR=Antimicrobial resistance, ESKAPE=Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species, MRSA=Methicillin-resistant Staphylococcus aureus, WHO=World Health Organization
In this study, attitude of the respondents to Antibiotic Resistance (AR), Antibiotic Stewardship Programme (ASP) was measured by applying three-point Likert scales. It was observed that a large number of students (75 prefinal and 91 final year students respectively; P = 0.42) agreed that the indiscriminate use of antibiotics is harmful. The respondents (89.2% and 85.5% for final- and prefinal-year students, respectively; P = 0.60) also agreed that health-care professionals are obliged to create awareness about antibiotic resistance among common public. Students (66% and 80% for final- and prefinal-year students, respectively; P = 0.62) participated in this study disagreed that antibiotic resistance is not a public health problem. They also disagreed with the question that there is no harm in selling antibiotics as over-the-counter drugs. Table 2 summarizes the response of students to attitude-based questions.
Table 2.
Summary of medical students' attitude towards antibiotic resistance and antibiotic stewardship
| Attitude-based questions | Response | Grade I (Pre final year) (n=93) | Grade II (Final year) (n=104) | P |
|---|---|---|---|---|
| Indiscriminate use of antibiotic is harmful | 0 | 75 (80.6) | 91 (87.5) | 0.42 |
| 1 | 8 (8.6) | 6 (5.7) | ||
| 2 | 10 (10.75) | 7 (6.7) | ||
| Lack of knowledge of infectious disease and antibiotics may hamper the quality of prescription | 0 | 59 (63.4) | 82 (78.9) | 0.06 |
| 1 | 16 (8.6) | 10 (9.6) | ||
| 2 | 18 (19.35) | 12 (11.5) | ||
| Over prescription of broad spectrum antibiotic increases antibiotic resistance | 0 | 58 (62.3) | 76 (73) | 0.23 |
| 1 | 20 (21.5) | 14 (13.4) | ||
| 2 | 15 (16.12) | 14 (13.4) | ||
| Poor infection control practices by health-care professionals cause the spread of antibiotic resistance | 0 | 63 (67.7) | 66 (63.4) | 0.66 |
| 1 | 16 (17.2) | 23 (22.1) | ||
| 2 | 14 (15) | 14 (13.4) | ||
| It is the obligation of health-care professionals to create awareness about the rational use of antibiotics among the general public | 0 | 83 (89.2) | 89 (85.5) | 0.60 |
| 1 | 6 (6.4) | 7 (6.7) | ||
| 2 | 4 (4) | 8 (7.6) | ||
| Education on the appropriate use of antibiotics is an unnecessary burden for an undergraduate medical student | 0 | 13 (13.9) | 21 (20.1) | 0.49 |
| 1 | 71 (76.3) | 73 (70.1) | ||
| 2 | 9 (9.6) | 9 (8.6) | ||
| Antibiotic resistance is not a public health problem | 0 | 16 (17.2) | 15 (14.4) | 0.62 |
| 1 | 66 (70.9) | 80 (76.9) | ||
| 2 | 11 (11.8) | 9 (8.6) | ||
| Antibiotic resistance is a significant problem at my institution | 0 | 33 (35.4) | 49 (47.1) | 0.02 |
| 1 | 25 (26.8) | 12 (11.8) | ||
| 2 | 35 (37.6) | 43 (41.3) | ||
| Proper laboratory investigation should be made mandatory before starting antibiotic therapy | 0 | 74 (79.5) | 88 (84.6) | 0.97 |
| 1 | 7 (7.5) | 7 (6.7) | ||
| 2 | 12 (13) | 9 (8.6) | ||
| There is no harm in selling antibiotics as an over the counter drugs | 0 | 16 (17.2) | 16 (15.3) | 0.95 |
| 1 | 63 (67.7) | 71 (68.2) | ||
| 2 | 14 (15) | 15 (14.4) |
0=Agree, 1=Disagree, 2=Don't know
The PCA revealed that the questions in Section B [Table 2] which determine the attitude of the students toward the ASP contributed more to the pattern observed in the data. The question numbers 2, 3, 4, 5, and 8 had more influence in determining the pattern as shown in the graphs [Figure 3a, b and Table 3]. The other questions gained prominence only when the above-mentioned questions were removed from the PCA analysis.
Figure 3.
Principal component analysis showing the relative contribution of all the questions toward the trend of response in our study in prefinal-year (a) and final-year (b) students. (a) Shows that questions 2, 3, 4, and 8 of Section B contribute more toward the data trend. Similarly, (b) shows that the questions 4, 5, and 8 contribute more toward the trend generated
Table 3.
Correlation coefficient of variables against the dimensions obtained through principal component analysis
| Variables | Correlation coefficient with various dimensions |
|||
|---|---|---|---|---|
| Prefinal year |
Final year |
|||
| Dimension 1 | Dimension 2 | Dimension 1 | Dimension 2 | |
| Section A - Q5 | 0.017 | 0 | 0 | 0.059 |
| Section B - Q1 | 0.123 | 0.002 | 0.001 | 0.004 |
| Section B - Q2 | 0.165 | 0.028 | 0.020 | 0.084 |
| Section B - Q3 | 0.297 | 0.016 | 0.003 | 0.058 |
| Section B - Q4 | 0.046 | 0.147 | 0.002 | 0.336 |
| Section B - Q5 | 0.048 | 0.036 | 0.014 | 0.243 |
| Section B - Q8 | 0.081 | 0.669 | 0.905 | 0.001 |
| Section B - Q9 | 0.085 | 0.036 | 0.004 | 0.010 |
DISCUSSION
AMR is a global health problem and cause of grave concern for the humankind. Many studies have demonstrated that effective implementation of ASP has improved the AMR.[19,20,21] Given the importance of undergraduate teaching in fostering positive behavior in budding medical professionals, extensive training in antibiotic stewardship should be incorporated in the curricula.
There are few studies which have assessed the knowledge and perception of undergraduate medical students about antibiotic prescribing AMR and AMS.[17,22,23,24,25] However, to the best of our knowledge, this is the first study to perform PCA to find the important variable determining the trend of response along with assessing the knowledge and attitude of respondents.
The present study revealed that respondents possess inadequate knowledge about AMR and AMS. A previous study conducted among undergraduate medical and dental students in a tertiary care institution of North India also reported a similar result.[24]
In our study, majority of the students knew that antibiotic is not useful in viral diseases, but most of them did not know the appropriate antibiotic and preventive method for MRSA infections. Many of the respondents could not expand the acronym ESKAPE pathogens (Enterococcus faecium, S. aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). However, they identified the indiscriminate use of broad-spectrum antibiotic cause of antibiotic resistance which is in accordance with multiple studies conducted across the globe.
In our study, majority of the students acknowledged that AMR is a public health problem and has the detrimental effect on health and financial well-being of patients. The students in our study disagreed that education on appropriate use of antibiotic is unnecessary. This suggests that they recognize the importance of correct use of antibiotics and the importance of education and training on antibiotic uses. It also reflects their positive behavior and responsiveness to imbibe the skill of rational antibiotic prescribing practice. Some other studies also found the similar observations about the perception of students toward the importance of training for the prudent antibiotic prescription.[17,26,27,28]
Most of the respondents in this study opined that antibiotics should not be sold as over-the-counter drugs; similar observation was made in a study done among the junior doctors where they perceived that restricted prescription of some antibiotics is helpful in reducing the emergence of resistance.[29] In this study, the results from PCA had shown that the attitude section of the questionnaire, especially the questions 2, 3, 4, 5, and 8, determines the pattern of answering. This puts an emphasis on the attitude for a successful understanding of the ASP.
AMS is a team effort and needs a multidisciplinary approach. The success of ASP depends on the critical involvement of everyone associated with the patients care. The WHO has recognized the importance of molding the prescribing behavior of physicians and other paramedical workers and recommended that training and education health workers and medical students at both graduate and postgraduate levels are an integral part of antibiotic resistance containment activities.[30,31] It is clear from our study that undergraduate medical students are aware of the burgeoning problem of antibiotic resistance and its potential consequences. They also know the importance of judicious use of antibiotics. They have a very positive attitude toward ASP. However, their knowledge about antibiotic and AMS is not adequate. We believe that there is a scope to bridge this knowledge gap by incorporating innovative training modules about the appropriate use of antimicrobial agents and ASP in the undergraduate curricula.
The strength of our study was that PCA was performed to analyze the trend of response. The weakness of our study was that it was conducted in only one institute with a small population which may not be the correct representation of all undergraduate medical students in India. The interns were not included in our study so we could not evaluate the change in the behavior of the students when they were exposed to direct patient care.
CONCLUSION
Good knowledge and attitude are essential for the proper understanding and implementation of the ASP. However, our study suggests the existence of knowledge gap among the students. As the torchbearer of the medical profession, undergraduate medical students can play a potentially key role in the successful implementation of the ASP. Hence, it should be ensured that they get proper teaching and training about the principles of rational antibiotic prescribing practice and ASP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lawrence R, Jeyakumar E. Antimicrobial resistance: A cause for global concern. BMC Proc. 2013;7:S1. doi: 10.1186/1753-6561-7-S3-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antibiotic resistance. [Last accessed on 2018 Apr 18]. Available from: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance .
- 3.Ventola CL. The antibiotic resistance crisis: Part 1: Causes and threats. P T. 2015;40:277–83. [PMC free article] [PubMed] [Google Scholar]
- 4.Spellberg B, Bartlett JG, Gilbert DN. The future of antibiotics and resistance. N Engl J Med. 2013;368:299–302. doi: 10.1056/NEJMp1215093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright GD. Something old, something new: Revisiting natural products in antibiotic drug discovery. Can J Microbiol. 2014;60:147–54. doi: 10.1139/cjm-2014-0063. [DOI] [PubMed] [Google Scholar]
- 6.Shlaes DM, Sahm D, Opiela C, Spellberg B. The FDA reboot of antibiotic development. Antimicrob Agents Chemother. 2013;57:4605–7. doi: 10.1128/AAC.01277-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Pre-Antibiotic Era Looming Large – The World is Almost Out of Time. SEARO. 2017 [Google Scholar]
- 8.Chereau F, Opatowski L, Tourdjman M, Vong S. Risk assessment for antibiotic resistance in South East Asia. BMJ. 2017;358:j3393. doi: 10.1136/bmj.j3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toner E, Adalja A, Gronvall GK, Cicero A, Inglesby TV. Antimicrobial resistance is a global health emergency. Health Secur. 2015;13:153–5. doi: 10.1089/hs.2014.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerding DN. The search for good antimicrobial stewardship. Jt Comm J Qual Improv. 2001;27:403–4. doi: 10.1016/s1070-3241(01)27034-5. [DOI] [PubMed] [Google Scholar]
- 11.Doron S, Davidson LE. Antimicrobial stewardship. Mayo Clin Proc. 2011;86:1113–23. doi: 10.4065/mcp.2011.0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kufel WD, Jeffres MN, MacDougall C, Cho JC, Marx AH, Williams DM, et al. Antimicrobial stewardship education in US colleges and schools of pharmacy. J Antimicrob Chemother. 2018;73:2252–8. doi: 10.1093/jac/dky166. [DOI] [PubMed] [Google Scholar]
- 13.Rawson TM, Butters TP, Moore LS, Castro-Sánchez E, Cooke FJ, Holmes AH, et al. Exploring the coverage of antimicrobial stewardship across UK clinical postgraduate training curricula. J Antimicrob Chemother. 2016;71:3284–92. doi: 10.1093/jac/dkw280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salsgiver E, Bernstein D, Simon MS, Eiras DP, Greendyke W, Kubin CJ, et al. Knowledge, attitudes, and practices regarding antimicrobial use and stewardship among prescribers at acute-care hospitals. Infect Control Hosp Epidemiol. 2018;39:316–22. doi: 10.1017/ice.2017.317. [DOI] [PubMed] [Google Scholar]
- 15.García C, Llamocca LP, García K, Jiménez A, Samalvides F, Gotuzzo E, et al. Knowledge, attitudes and practice survey about antimicrobial resistance and prescribing among physicians in a hospital setting in Lima, Peru. BMC Clin Pharmacol. 2011;11:18. doi: 10.1186/1472-6904-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vickers H. International antibiotic resistance crisis, Better training needed to maintain therapeutic arsenal. [Last accessed on 2018 April 20]. Available from: http://student.bmj.com/student/view-article.html?id=sbmj.d3207 .
- 17.Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz-Cochran R, Srinivasan A, et al. Medical students' perceptions and knowledge about antimicrobial stewardship: How are we educating our future prescribers? Clin Infect Dis. 2013;57:631–8. doi: 10.1093/cid/cit370. [DOI] [PubMed] [Google Scholar]
- 18.Silverberg SL, Zannella VE, Countryman D, Ayala AP, Lenton E, Friesen F, et al. A review of antimicrobial stewardship training in medical education. Int J Med Educ. 2017;8:353–74. doi: 10.5116/ijme.59ba.2d47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcell HG, Arias AV, Sandoval CP, Valle Gamboa ME, Sado AB, Alfonso Serrano RN, et al. Impact of a focused antimicrobial stewardship program in adherence to antibiotic prophylaxis and antimicrobial consumption in appendectomies. J Infect Public Health. 2017;10:415–20. doi: 10.1016/j.jiph.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 20.DiDiodato G, McArthur L. Evaluating the effectiveness of an antimicrobial stewardship program on reducing the incidence rate of healthcare-associated clostridium difficile infection: A non-randomized, stepped wedge, single-site, observational study. PLoS One. 2016;11:e0157671. doi: 10.1371/journal.pone.0157671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaki R, Elligsen M, Walker S, Simor A, Palmay L, Daneman N, et al. Impact of antimicrobial stewardship in critical care: A systematic review. J Antimicrob Chemother. 2011;66:1223–30. doi: 10.1093/jac/dkr137. [DOI] [PubMed] [Google Scholar]
- 22.Ferdoush J, Parveen K, Ata M, Reza F, Rahman MS. Knowledge, perception and preparedness of future prescribers about antimicrobial stewardship. Bangladesh Journal of Pharmacology. 2016;11:928–34. [Google Scholar]
- 23.Yang K, Wu D, Tan F, Shi S, Guo X, Min Q, et al. Attitudes and perceptions regarding antimicrobial use and resistance among medical students in central China. Springerplus. 2016;5:1779. doi: 10.1186/s40064-016-3454-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharma K, Jain P, Sharma A. Knowledge, attitude and perception of medical and dental undergraduates about antimicrobial stewardship. Indian J Pharmacol. 2015;47:676–9. doi: 10.4103/0253-7613.169572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chuenchom N, Chaiwarith R, Deoisares R, Thamlikitkul V, Rattanaumpawan P. Perception, Attitude and Knowledge of Antimicrobial Resistance, Appropriate Antimicrobial Use, and Infection Control Among the Sixth Year Medical Students in Three Medical Schools, Open Forum Infectious Diseases. 2015;2:424. [Google Scholar]
- 26.Heaton A, Webb DJ, Maxwell SR. Undergraduate preparation for prescribing: The views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008;66:128–34. doi: 10.1111/j.1365-2125.2008.03197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minen MT, Duquaine D, Marx MA, Weiss D. A survey of knowledge, attitudes, and beliefs of medical students concerning antimicrobial use and resistance. Microb Drug Resist. 2010;16:285–9. doi: 10.1089/mdr.2010.0009. [DOI] [PubMed] [Google Scholar]
- 28.Ross S, Loke YK. Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol. 2009;67:662–70. doi: 10.1111/j.1365-2125.2009.03395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pulcini C, Williams F, Molinari N, Davey P, Nathwani D. Junior doctors' knowledge and perceptions of antibiotic resistance and prescribing: A survey in france and Scotland. Clin Microbiol Infect. 2011;17:80–7. doi: 10.1111/j.1469-0691.2010.03179.x. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Everyone Has a Role to Play | Antibiotic Stewardship Report | Get Smart | Centers for Disease Control and Prevention. 2017 [Google Scholar]
- 31.World Health Organization. The Evolving Threat of Antimicrobial Resistance: Options for Action. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]