Summary
Transgender people are a diverse population affected by a variety of negative health indicators across high, middle, and low income settings. Studies consistently document high prevalence of adverse health outcomes in this population, including HIV and other sexually transmitted infections (STIs), mental health distress, and substance use and abuse. However, many other health areas remain understudied, population-based representative samples and longitudinal studies are lacking, and routine surveillance efforts for transgender population health are scarce. The absence of survey items with which to identify transgender respondents in general surveys often limits availability of data to estimate the magnitude of health inequities and characterize transgender population-level health globally. Despite limitations, there are sufficient data highlighting the unique biological, behavioral, social, and structural contextual factors surrounding health risks and resiliencies for transgender people. To mitigate these risks and foster resilience, a comprehensive approach is needed that includes gender affirmation as a public health framework, improved health systems and access to healthcare informed by high quality data, and effectively partnering with local transgender communities to ensure responsiveness of and cultural specificity in programming. Transgender health underscores the need to explicitly consider sex and gender pathways in epidemiologic research and public health surveillance more broadly.
Keywords: transgender, disease burden, sex and gender
Introduction
Transgender people have an assigned sex at birth different from their current gender identity or expression and represent a diverse population across regions and within countries worldwide (Sidebar 1).1,2 Although accurate data concerning the size of the transgender population globally are lacking, and population prevalence depends on transgender “case” definition, estimates suggest transgender identity prevalence of 0.3%−0.5% (see also White and colleagues Paper 1 of this issue).3 Despite small numbers, transgender people are a population burdened by substantial adverse health indicators across high, middle, and low income settings.4,5 Health inequities for transgender people are hypothesized to be multifactorial with risks including systematic social and economic marginalization, pathologization, stigma, discrimination, and violence, including healthcare systems and settings.6 The purpose of this data synthesis is to characterize the global health burden facing transgender populations, including the specific contexts and multiple determinants of health affecting them. Data from the peer-reviewed scientific literature were reviewed to characterize the burden and distribution of disease in transgender populations globally. This synthesis of information describes transgender population health and leverages data from different regions of the world to highlight the unique sex- and gender-related biological, behavioral, social, legal, and structural factors surrounding health risks and resiliencies for this underserved population. The review further seeks to inform future advocacy, funding, health surveillance, public health policy, monitoring, and reporting processes, and research initiatives to not only address and improve health, but also to promote health equity, social justice, and human rights, including the right of all people to self-determination.
Sidebar 1: Definitions: Transgender People.
Transgender people have a current gender identity or expression that is different from their sex assigned at birth. Gender minority was introduced in 2011 as part of the landmark Institute of Medicine report commissioned by the U.S. National Institutes of Health (NIH) entitled, The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding.1 Gender minority is meant to be an inclusive umbrella term which includes people who may identify as transgender or have other diverse genders. Transgender people have diverse sexual orientation identities, attractions, and behaviors.
Review and Synthesis
A review and synthesis of peer-reviewed recent literature (2008–2014) in transgender health was conducted. “Transgender” and associated terms (e.g., hijra, waria, travesti, trans masculine, MTF) were searched alongside health terms (e.g., HIV, disease, illness, mental health), related concepts (e.g., wellbeing), social factors (e.g., discrimination, stigma). Search databases included: Pubmed, Embase, OVID, PsychInfo, Web of Science, and ProQuest.
Inclusion criteria were: (1) any study design that included quantitative data on disease burden in transgender people of any age; (2) studies published between January 1, 2008-December 20, 2014 (inclusive) to limit information to the current context for this population; (3) studies in English, French, and Spanish. Primary exclusion criteria were: (1) studies published before 2008; (2) studies appearing online ahead of print; (3) qualitative studies; (4) studies focused on intersex individuals; (5) studies focused on neuroanatomy or neuropsychology; (6) clinical studies focused on gender reassignment outcomes including studies of sexual satisfaction and quality of life with surgical outcomes given recent reviews on these topics7,8; (7) studies where lesbian, gay, bisexual, transgender (LGBT) or men who have sex with men (MSM) participants were not disaggregated by gender identity (unless data were analyzed separately and meaningful inferences could be made about transgender people). Due to the overall objective of obtaining epidemiological trends among transgender people, sources were not excluded on the basis of quality provided that they met all the inclusion criteria and exclusion criteria as defined above (Sidebar 2).
Sidebar 2: Differentiating Transgender People from People Who are Intersex.
Intersex people/people with Disorders of Sex Development (DSD) [or in community terms Diverse Sexual Development (DSD)2] are those born with bodies that vary from both male and female bioanatomies, including chromosomes, gonads, genitals and/or other secondary sex characteristics. Some intersex/DSD people consider themselves to be transgender; however, most do not. This research synthesis does not include a review of intersex/DSD research. This is because many primary issues in intersex/DSD health are different from those of transgender people (i.e., infant genitoplasty and gonadectomy, ongoing care for intersex/DSD adults, iatrogenic effects of genital surgery and gonad removal, etc.).3−7 The heterogeneity and complexity of Intersex/DSD health warrants its own research synthesis which is beyond the scope of the current paper.
First and second reviewers (RM, CH) conducted parallel screening of titles found in the search. If either one or both reviewers selected the abstract for full article review, the article was pulled for full article review. If at the full article review there was a disagreement between the first two reviewers regarding data extraction, a third reviewer (SR) resolved the disagreement.
A codebook was created and refined to guide data abstraction using a collaborative consensus-based process among members of the author team. Health-related outcome categories were identified to synthesize and further organize the literature reviewed. The team incorporated principles from grounded theory,9 whereby codes were iteratively grouped into concepts and concepts into categories. Six health-related outcome categories emerged. Through this process in became apparent that stigma and discrimination were not only determinants of health (illness), but also critical outcomes in and of themselves for transgender populations globally.
An expert consultation with selected transgender health researchers was also conducted, and additional articles recommended that satisfied the inclusion criteria were included for data abstraction. The unique number of studies were captured, as well as the number of data points—for example, if an article reported on four health outcomes, it contributed four data points to the review. Similarly, if data were reported for specific subgroups (e.g., mental health prevalence estimates for trans feminine and trans masculine people separately), these were counted as unique data points and extracted accordingly (Sidebar 3).
Sidebar 3: Evolving Terminologies.
In public health research, transgender populations are categorized according to assigned sex at birth and gender identity. This is because some health indicators (e.g., prostate health), are only applicable for people assigned a male sex at birth. Trans feminine refers to transgender people assigned a male sex at birth who are on the transgender spectrum—identifying as women, female, male-to-female (MTF), transgender women, trans women, and many other diverse gender minority identities across the world (e.g., hijra, kathoey, travestis, waria). Trans masculine describes transgender people assigned a female sex at birth who are on the transgender spectrum—identifying as men, male, female-to-male (FTM), transgender men, trans men, and many other diverse gender minority identities (genderqueer, stud, aggressive, Sadhin). Greater attention to non-binary genders is needed in research, including transgender people who do not identify as feminine or masculine, or who integrate both. Transgender people exist all over the world. Definitions and terminology continue to dynamically evolve to describe the population across different local, national, and global contexts.
Overall Research Trends
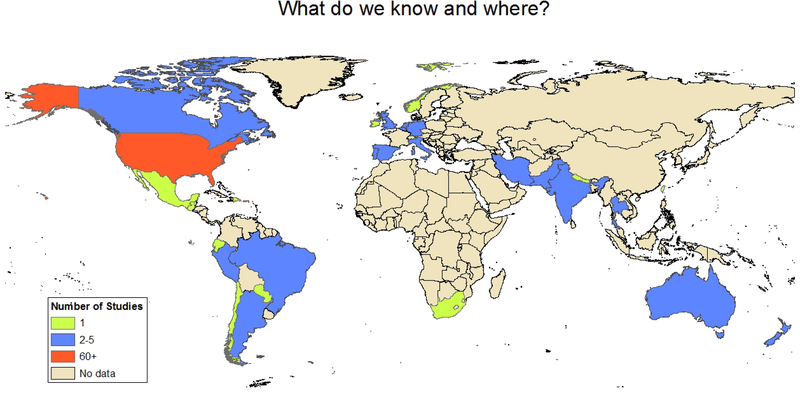
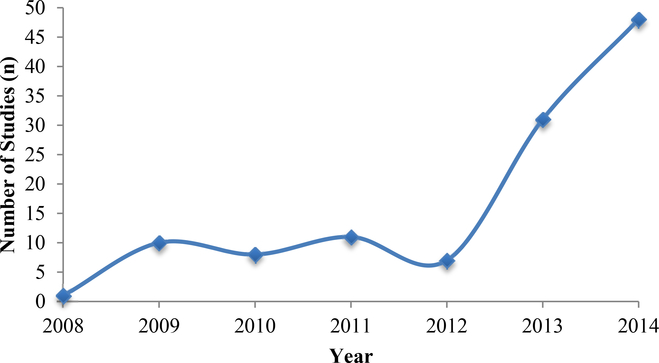
A total of 116 studies in 30 countries were identified. Table 1 presents the health outcome studies and key data extracted from each study (the table is organized by region, country, and then author). Table 2 presents health-related data on stigma, discrimination, violence/victimization, and sex work. A map of the geographic distribution of current studies in transgender health is shown in Figure 1. The vast majority of research is in the United States. Several countries have a single study (e.g., Mexico) or between two and five studies (e.g., Canada, Australia, Iran). No other country except for the United States has six or more studies reporting data in transgender health. Indeed, for the majority of countries no data are available at all and for many including the content of Sub-Saharan Africa, only a single study exists. This gap in research is important to consider in terms of the generalizability of current health research across regions and geographic settings. We note a growing interest in transgender health research over time, particularly in most recent years in 2013 and 2014 as shown in Figure 2. We also note a dearth of research on transgender children, adolescents and youth with only 15 studies.
| Table 1. Transgender and Other Gender Minority Population Health Research 2008–2014 by Region, Country, and then Author. | ||||||||
| Location | Sampling method | Sample | Assigned sex at birth | Sample size | Measure of prevalence/association | Significant associations | Health outcome measures | |
| North America | ||||||||
| Bauer, 20131 | Ontario, Canada | Respondent-driven sampling | Trans gay, bisexual, and/or have sex with men | Female | 173 | Prevalence | None | Depressive symptoms |
| Moody, 20132 | Canada | Internet-based | Transgender | Both | 133 | Beta | Perceived support from family, emotional stability, child-related concerns | Suicidal behavior |
| Alvarez-Wyssmann, 20133 | Mexico City, Mexico | Chart review | HIV infected transgender men on HAART | Female | 127 | Prevalence | None | Diabetes |
| Reisner, 20144 | Boston, USA | Chart review | Female to Male transgender with diagnosis of GID | Female | 23 | Prevalence | None | HIV seroprevalence, history of STIs, axis 1 diagnosis, axis 2 diagnosis, depression, anxiety, substance use disorder, PTSD, bipolar disorder, adjustment disorder, suicide attempt |
| Shipherd, 20125 | Boston, USA | Trans conference-based | Male to Female transsexual and cross dresser veterans | Male | 43 | Prevalence | None | High cholesterol, blood pressure, vision problems, hearing problems, chronic pain, arthritis, digestive problems, cancer, lung problems, kidney problems, diabetes, depression, PTSD, anxiety, other mental health |
| Dowshen, 20116 | Chicago, USA | Convenience sample | Young transgender women | Male | 92 | Prevalence | None | Drunk or buzzed in past 3 months |
| Garofalo, 20127 | Chicago, USA | Active recruitment at local transgender gathering spots and passive recruitment through flyer distribution | Young transgender women | Male | 51 | Prevalence | None | HIV self-report, new STI diagnosis past 3 months |
| Fletcher, 20148 | Los Angeles, USA | Venue-based recruitment | Community-based HIV prevention program attendees | Male | 517 | Prevalence | Marginally homeless, homeless | HIV self-report, cocaine use last 30 days, crack use last 30 days, methamphetamine use last 30 days, heroin use last 30 days, marijuana use last 30 days, hormone use last 30 days |
| Reback, 20149 | Los Angeles, USA | Outreach based | Male to female transgender | Male | 2136 | Adjusted odds ratio; prevalence | African-American, Methamphetimine, Crack, Injection drug, sex work, unprotected anal sex with sex work partner | HIV self-report; alcohol past 30 days, marijuana past 30 days, cocaine past 30 days, crack past 30 days, injection drug/hormone |
| Simons, 201210 | Los Angeles, USA | Clinic-based recruitment | Transgender adolescents | Both | 28 | Prevalence; pearson’s correlation coefficient | Less parental support | Significant depression; higher rates of depression |
| Simons, 201311 | Los Angeles, USA | Clinic-based recruitment | Transgender youth | Both | 66 | Beta | Parental support | Depressive symptoms |
| Rohde Bowers, 201112 | Los Angeles County, USA | Venue based | High risk HIV prevention program attendees | Male | 1033 (320 transgender) | Prevalence | None | HIV self-report, alcohol (5 or more drinks), marijuana, methamphetamine, injected methamphetamine, cocaine, crack, ecstasy, GHB, amyl nitrate, heroin, injected heroin, hormones (non-prescribed), injected hormones |
| Benotsch, 201313 | Mid-Atlantic, USA | Clinic-based recruitment | Transgender | Both | 155 | Prevalence | Individuals reporting non-medical use of prescription drugs | HIV-self report, BSI-depression, BSI-anxiety, BSI-somatic distress, BSI-Global Severity Index, alcohol use in past 3 months, cocaine use in past 3 months, methamphetamine use past 3 months, marijuana use past 3 months, poppers use past 3 months, ecstasy use past 3 months heroin use past 3 months, other recreational drug use past 3 months |
| McElory, 201214 | Missouri, USA | Pride festivals recruitment | Sexual and gender minority individuals | NS | 6537 | Prevalence | None | Smoking |
| Irwin, 201415 | Nebraska, USA | Community and internet-based | LGBT adults | Both | 770 (92 transgender) | Adjusted odds ratio | Transgender | Suicidal ideation |
| Reisner, 201016 | New England, USA | Venue-based | Transmen | Female | 16 | Prevalence | None | Herpes self-report, trichomonas self-report, bacterial vaginosis self-report, alcohol use during sex, marijuana use during sex, hallucinogen use during sex, ecstasy use during sex |
| Shipherd, 201117 | New England, USA | Trans conference | Transgender | Male | 97 | Prevalence | None | Post-traumatic stress disorder, depressive symptoms |
| Hwahng, 201418 | New York, USA | Organization based, venue referrals, and internet | HIV uninfected male to female transgender | Male | 572 | Prevalence | None | Major depression (early and late adolescence), suicidal ideation (early and late adolescence) |
| Koken, 200919 | New York, USA | Peer outreach and snowball | Transwomen | Male | 20 | Prevalence | None | HIV self-report |
| Leinung, 201320 | New York, USA | Clinic-based recruitment | Transsexual | Male | 192 | Prevalence | None | Drug and substance use, HIV |
| Female | 50 | Prevalence | None | Drug and substance abuse | ||||
| Nuttbrock, 200921 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 571 | Odds ratio | Commercial sex partners, androphilic, unemployment, sex identity disclosure, female attire in public, casual sex partners, substance use, psychoactive drug injection, Hispanic | HIV infected, syphilis, hepatitis B, hepatitis C |
| Nuttbrock, 201022 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 571 | Prevalence | None | Lifetime major depression, lifetime suicide plans, lifetime suicide attempt |
| Nuttbrock, 201323 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 230 | Adjusted odds ratio; odds ratio | Employment, sex work, transgender presentation, hormone therapy; psychological gender abuse, physical gender abuse | Major depression |
| Nuttbrock, 201324 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 230 | Prevalence; hazard ratio | Gender abuse, education, preoperative, non-white ethnicity, committed partners (unprotected) receptive anal intercourse, commercial partners (unprotected) receptive anal intercourse, depressive symptoms, legitimate income, hormone therapy, sexual reassignment surgery, younger age, sexually attracted to men only, casual partners (unprotected) receptive anal intercourse, CES-D score >=20 | HIV seroprevalence, depression; incident HIV/STI, depressive symptoms |
| Nuttbrock, 201425 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 230 | Adjusted odds ratio | Income, sex work, transgender presentation, hormone therapy, gender abuse, depressive symptoms | Alcohol use, cannabis use, cocaine use, any substance use |
| Pathela, 201426 | New York City, USA | HIV/STD surveillance registries | Transgender women living with HIV | Male | 345 | Incidence | Transgender, diagnosed with HIV at a younger age, living with HIV for less time | STD coinfection with HIV |
| Flentje, 201427 | San Francisco, USA | Clinic based recruitment | Individuals entering substance abuse treatment | Male | 13649 (146 transgender) | Prevalence; adjusted odds ratio | Transgender status | Methamphetamine; alcohol, cocaine, heroin, marijuana, other drug use, |
| Female | 13649 (53 transgender) | Prevalence | None | Alcohol, cocaine, heroin, methamphetamine, other drug use | ||||
| Gamarel, 201428 | San Francisco, USA | Purposive sampling in community spaces | Transgender females and their primary non transgender male partner | Male | 382 (191 transwomen) | Adjusted odds ratio | Financial hardship, discrimination, relationship stigma | Depressive distress |
| Jefferson, 201329 | San Francisco, USA | NS | Transwomen | Male | 100 | Adjusted odds ratio; odds ratio | Coping self-efficacy; transgender identity, racism, transphobia, high combined discrimination | Depression |
| Operario, 201130 | San Francisco, USA | Venue-based | Transgender adults in relationship with non-trans men | Male | 174 | Prevalence | None | HIV self-report, STI diagnosis or symptoms past 12 months, any alcohol use past 3 months, any illicit drug use past 3 months, any injection drug use past 3 months, depression |
| Operario, 201431 | San Francisco, USA | Purposive community sampling | Self-identifying transgender women | Male | 191 | Prevalence | None | Self-reported HIV, depressive symptoms, alcohol intoxication past 30 days, illicit drug use past 30 days |
| Rapues, 201332 | San Francisco, USA | Respondent-driven sampling | Male to female transgender | Male | 314 | Prevalence (RDS weighted) | None | HIV seroprevalence, HIV self-report, hepatitis C |
| Reisner, 201433 | San Francisco, USA | Purposive sampling in community spaces | Transgender females and their primary non transgender male partner | Male | 382 (191 transwomen) | Prevalence; adjusted odds ratio | Age, financial hardship, discrimination | Depressive distress, HIV self-report; non-marijuana illicit drug use |
| Santos, 201434 | San Francisco, USA | Respondent-driven sampling | Transfemale | Male | 314 | Adjusted odds ratio; prevalence | Any methamphetamine | HIV seroprevalence; crack cocaine, powdered cocaine, club drugs, downers, painkiller, hallucinogens, heroin, marijuana, alcohol, binge drinking, any substance |
| Sevelius, 200935 | San Francisco, USA | Clinic and location based | Transgender | Male | 153 | Prevalence | None | HIV self-report, injecting drug use past year, alcohol use (five or more drinks per day) stimulant use |
| Wilson, 201436 | San Francisco, USA | Respondent-driven sampling | Transgender women | Male | 235 | Prevalence | None | HIV seroprevalence, injection drug use |
| Wilson, 201437 | San Francisco, USA | Respondent-driven sampling | Transgender women | Male | 233 | Prevalence | None | HIV seroprevalence, injected drugs |
| Nemoto, 201438 | San Francisco and Oakland, USA | Purposive community sampling | Transgender women with a history of sex work | Male | 573 | Prevalence | Race | Depressive symptoms, self-reported HIV, STI history in past 12 months |
| Brennan, 201239 | Chicago and Los Angeles, USA | Clinic-based, venue-based, and peer outreach and referral | Young transgender women | Male | 151 | Prevalence; point biserial correlations; adjusted odds ratio | Intimate partner violence, unprotected anal intercourse, polysubstance use; 3 or 4 syndemic index factors (low self-esteem, polysubstance use, victimization, and intimate partner violence) vs 0 | Polysubstance use; HIV self-report |
| Bradford, 201340 | Virginia, USA | Internet and peer referral | Transgender | Both | 350 | Prevalence | None | HIV seroprevalence |
| Blosnich, 201341 | USA | Clinic-based recruitment | Veterans Health Association users with diagnosis of GID | NS | 1326 in 2009 1162 in 2010 1326 in 2011 |
Period prevalence | None | Suicide-related event |
| Bockting, 201342 | USA | Internet-based | Transgender adults | Both | 1093 | Adjusted odds ratio | Transwomen compared to transmen, age, education, enacted stigma, felt stigma, peer support, family support, identity pride | Depression, anxiety, somatization, Global Severity Index |
| Budge, 201343 | USA | Internet-based | Transgender adults | Male | 226 | Beta | Transition status, social support | Depression, anxiety |
| Female | 125 | Beta | Transition status, social support | Depression, anxiety | ||||
| Effrig, 201144 | USA | College campus survey | College students | NS | 21686 (86 transgender or “other” gender | Prevalence | None | Attempted suicide, suicidal ideation |
| Feldman, 201445 | USA | Internet based | Transgender | Both | 1229 | Prevalence | None | HIV self-report |
| Fredriksen-Goldsen, 201446 | USA | Community-agency based | LGBT adults 50 and older | NS | 2201 (174 transgender) | Prevalence | None | Disability, Obesity |
| Horvath, 201447 | USA | Internet based | Rural and urban transgender | Male | 692 | Prevalence | None | HIV self-report, regular heavy alcohol use, binge alcohol use, marijuana use, non-marijuana drug use |
| Female | 523 | Prevalence | None | HIV self-report, regular heavy alcohol use, binge alcohol use, marijuana use, non-marijuana drug use | ||||
| Hotton, 201348 | USA | NS | Young transgender women | Male | 116 | Prevalence; odds ratio | Life stress | Substance use in past 3 months, alcohol use in the past 3 months |
| House, 201149 | USA | Internet-based | LGBT adults | Both | 1126 (164 transgender) | Adjusted odds ratio | Transgender compared with male | Non-suicidal self-harm, attempted suicide |
| Mustanski, 201350 | USA | Venue-based | LGBT youth | Both | 237 (21 transgender) | Prevalence | None | Lifetime suicidal attempt |
| Peitzmeier, 201451 | USA | Clinic-based | Clinic patients receiving Pap tests | Female | 3858 (233 transgender) | Prevalence | None | HIV seroprevalence |
| Rath, 201352 | USA | Probabilty-based | Young adults | NS | 4159 (12 transgender) | Prevalence | None | Major depressive disorder, current alcohol use, cigarette use |
| Reisner, 201353 | USA | Brief intercept | Transmasculine | Female | 73 | Prevalence | All health outcomes compared to depression only | Lifetime clinical depression, alcohol abuse, current or former smoking, asthma, obese; avoided/delayed health care, younger age, queer or non-binary sexual orientation |
| Reisner, 201454 | USA | Convenience sample | Transfeminine gender identity | Male | 3878 | Prevalence; risk ratio | Jail/prison time, mistreated/victimized in jail/prison, denied healthcare in jail/prison | HIV self-report, daily cigarette smoker, substance use to cope, suicide attempt |
| Reisner55 | USA | Clinic-based | Participants from the Community Health Center Core Data Project | Both | 2653 (31 transgender) | Prevalence | Transgender | Suicidal ideation, attempted suicide ever, substance abuse history, smoking, HIV self-report |
| Sánchez, 200956 | USA | Transgender event | Male to female transsexuals | Male | 53 | Beta | Transgender-related fears | Psychological distress |
| Sevelius, 200957 | USA | Snowball sampling, listservs, web sites | Trans MSM | Female | 45 | Prevalence | None | HIV self-report, STI diagnosis ever, HPV, gonorrhea, chlamydia, herpes, trichomoniasis, bacterial vaginosis, hepatitis C, pelvic inflammatory disease, pubic lice |
| South and Central America | ||||||||
| Toibaro, 200958 | Buenos Aires, Argentina | Clinic-based recruitment | Patients at a clinic | Both | 4118 (105 transgender) | Prevalence | None | HIV seroprevalence, syphilis, drug use, alcohol use |
| Carobene, 201459 | Argentina | Not specified | Trans sex workers | NS | 273 | Prevalence | None | HIV seroprevalence, HBV seroprevlance, HCV seroprevalence |
| Socias, 201460 | Argentina | Snowball sampling and quota sampling | Transgender | Male | 452 | Prevalence | None | HIV self-report |
| Rocha, 201361 | Brazil | Transvestite clinic case records | Transvestites | NS | 59 | Prevalence | None | Alcohol use, drug use |
| Johnston, 201362 | Dominican Republic | Respondent-driven sampling | Gay, transsexuals, and MSM | Male | 1388 (83 transsexuals) | Adjusted odds ratio | Transsexual compared to MSM | HIV seroprevalence |
| Aguayo, 201363 | Paraguay | NS | Transwomen | Male | 311 | Prevalence | None | HIV, syphilis |
| Lipsitz, 201364 | Lima, Peru | Clinic-based recruitment | Men and transwomen | Male | 2717 (332 transwomen) | Prevalence | None | HIV seroprevalence |
| Verre, 201465 | Peru | Peer outreach and snowball | MSM and transgender women | Male | 5148 (714 transgender) | Prevalence | None | HIV seroprevalence, syphilis seroprevalence |
| Europe | ||||||||
| Wierckx, 201366 | Ghent, Belgium | Clinic-based recruitment | Transgender persons diagnosed with GID and on cross-sex hormone therapy | Male | 214 | Cases/1000 persons | Transwomen compared to age matched women | Myocardial infarction, transient ischemic health attack, type 2 diabetes, |
| Female | 138 | Cases/1000 persons | Transmen compared to age matched men | Type 2 diabetes, cancer | ||||
| Auer, 201367 | Munich, Germany | Clinic based recruitment | Transsexuals with a diagnosis of GID, not in hormone therapy or undergone reassignment surgery | Female | 131 | Prevalence | None | Pubertal and menstrual irregularities, premature or delayed menarche, oligomenorrhea, polymenorrhea, amenorrhea, adrenal hyperplasia, polycystic ovary syndrome, hypogonadism, anorexia nervosa |
| Male | 192 | Prevalence | None | Pubertal irregularities, delayed oigarche, cryptorchidism, no pubertal voice change | ||||
| Judge, 201468 | Dublin, Ireland | Clinic-based recruitment | Patients with suspected or confirmed GID | Male | 159 | Prevalence | None | Hypertension, dyslipidemia, diabetes, depression, schizophrenia, bipolar affective disorder, self-harm/ suicide attempt, asthma, Asperger’s |
| Female | 59 | Prevalence | None | Hypertension, dyslipidemia, diabetes, depression, schizophrenia, bipolar affective disorder, self-harm/ suicide attempt, asthma, Asperger’s | ||||
| Manieri, 201469 | Torino, Italy | Clinic-based recruitment | Transgender subjects undergoing hormone therapy | Male | 56 | Prevalence | None | Obesity, hypercholesterolemia, hypertriglyceridemia, diabetes, metabolic syndrome, HIV seroprevalence, |
| Female | 27 | Prevalence | None | Obesity, metabolic syndrome | ||||
| Imbimbo, 200970 | Italy | Clinic-based recruitment | Male to female transsexuals who have undergone sexual reassignment surgery | Male | 139 | Prevalence | None | Contemplated suicide, attempted suicide |
| Asscheman, 200971 | Amsterdam, Netherlands | Clinic based recruitment | Transsexuals on cross-sex hormones | Male | 966 | Adjusted Hazard Ratio; Standardized Mortality Ratio | Male to Female transsexual compared to the age and sex adjusted general population | Cardiovascular mortality; All-cause mortality, mortality from malignant neoplasm, AIDS, external causes, illicit drug use, suicide |
| Female | 365 | Standardized Mortality Ratio | Female to male transsexual compared to the age and sex adjusted general population | Mortality from external causes, illicit drug use | ||||
| de Vries, 201072 | Amsterdam, Netherlands | Clinic-based recruitment | Children and adolescents referred to Gender Identity Clinic | Both | 205 | Incidence | None | Autism spectrum disorder |
| de Vries, 201173 | Amsterdam, Netherlands | Clinic-based recruitment | Adults and adolescents with a diagnosis of GID | Male Female |
207 adults, 43 adolescents | Prevalence | None | Depression, schizophrenia, hysteria, hypochondria, paranoia, psychopathic deviate, hypomania, other mental health outcomes |
| 86 adults, 40 adolescents | Prevalence | None | Depression, schizophrenia, hysteria, hypochondria, paranoia, psychopathic deviate, hypomania, other mental health outcomes | |||||
| Almeida, 201474 | Lisbon, Portugal | Clinic-based recruitment | Sex workers | NS | 151 (20 transgender) | Prevalence | None | HIV seroprevalence |
| Guzman-Parra, 201475 | Malaga, Spain | Clinic-based | Transsexuals | NS | 379 | Prevalence | None | Lifetime only cannabis use, lifetime only cocaine use, current cannabis use |
| Hill, 201176 | London, UK | Clinic-based recruitment | Transgender sex workers | Both | 24 | Prevalence | None | HIV seroprevalence, syphilis, genital herpes, chlamydia-negative urethritis or proctitis, gonorrhea, chlamydia, hepatitis B, any STI |
| Pasterski, 201477 | London, UK | Clinic-based recruitment | Adults with gender dysphoria or GID | Both | 91 | Prevalence | None | Autism spectrum disorder |
| Davey, 201478 | England | Clinic-based recruitment | Individuals diagnosed with gender dysphoria and age and gender-matched controls | Both | 206 (103 transgender) | PWI mean score; SCL-90-R mean score; SF-36 v.2 mean score | Gender dysphoric | PWI total score; global severity index, somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoneuroticism; mental health component summary, social functioning, role limitations due to emotional problems, mental health |
| Claes, 201479 | United Kingdom | Clinic-based recruitment | Transsexuals | Male | 103 | Prevalence | None | Non-suicidal self-injury |
| Female | 52 | Prevalence | None | Non-suicidal self-injury | ||||
| Turner, 201480 | United Kingdom | Clinic-based recruitment | Persons who sell sex | Male | 96 (13 transgender) | Prevalence | None | Chlamydia, gonorrhea, genital warts |
| Heylens, 201481 | Netherlands, Belgium, Germany Norway | Clinic-based recruitment | Adults seeking gender reassignment surgery | Both | 298 | Prevalence | None | One or more Axis 1 personality disorders, one or more Axis 2 personality disorders, affective disorders, anxiety disorders, substance-related disorders, eating disorders, psychotic disorders |
| Central and South Asia | ||||||||
| Kalra, 201382 | Mumbai, India | Clinic-based recruitment | Hijra (individuals who do not conform to the conventional notions of male or female gender) | Male | 50 (49 male, 1 female) | Prevalence | None | Depressive disorder, dysthymic disorder, alcohol abuse or dependence |
| Arora, 201383 | New Delhi, India | NS | MSM and transgender women | Male | 65 (24 transgender) | Prevalence | None | Anal dysplasia |
| Ramakrishnan, 201284 | Tamil Nadu, India | Probability-based | Transgender | Both | 807 | Prevalence | None | HIV seroprevalenece, lifetime syphilis |
| Brahmam, 200885 | India | Probability-based | MSM and Hijra | Male | 4600 (575 Hijra) | Prevalence | None | HIV seroprevalence, syphilis seroprevalence, HSV-2 seroprevalence |
| Aghabikloo, 201286 | Tehran, Iran | Clinic-based recruitment | Transsexuals with GID seeking sexual reassignment surgery | Female | 25 | Prevalence | None | Mood disorders, anxiety disorders, suicide attempts, substance-related disorder |
| Male | 44 | Prevalence | None | Mood disorders, anxiety disorders, suicide attempts, substance-related disorder | ||||
| Ahmadzad-Asl, 201387 | Tehran, Iran | Chart review | Transsexuals with a diagnosis of GID | Male | 138 | Prevalence | None | General medical condition co-morbidity; current smoker, psychiatric co-morbidity |
| Female | 143 | Prevalence | None | General medical condition co-morbidity; current smoker, psychiatric co-morbidity | ||||
| Javaheri, 201088 | Tehran, Iran | Clinic-based recruitment | Transsexuals | Both | 40 | Prevalence | None | Thought of committing suicide, suicide attempt |
| Bhatta, 201489 | Nepal | Snowball/cha in referral and venue-based | Male to female transgender persons | Male | 232 | Prevalence | None | Alcohol in last 6 months, smoking in last 6 months |
| Rehan, 201190 | Karachi and Lahore, Pakistan | Random sample of gurus | Hijras | Male | 400 | Prevalence | None | Extra-inguinal lymphadenopathy, urethral discharge, anal discharge, anal warts, anal tears, genital ulcers |
| Emmanuel, 201391 | Pakistan | Peer referral | Key populations | Male | 16642 (3714 Hijra sex workers) | Prevalence | None | HIV seroprevalence, injected drugs in the past 6 months |
| South East Asia | ||||||||
| Chemnasiri, 201092 | Bangkok, Chaing Mai, Phuket, Thailand | Venue-day-time | MSM and transgender women | Male | 827 (241 transgender) | Prevalence | None | HIV seroprevalence, history of STIs, used alcohol ever, used drugs ever |
| Gooren, 201593 | Thailand | Snowball sampling | Kathoeys (transgender women) | Male | 60 | Prevalence | None | Unprescribed hormone use |
| Toms (transgender men) | Female | 60 | Prevalence; t-test | Using cross-sex hormones | Unprescribed hormone use; bodily harm, mental health | |||
| Yadegarfard, 201394 | Thailand | Organization-based recruitment | Transgender | Male | 190 | MANOVA | Age, education, >10 sexual partners | PANSI-positive (Positive and Negative Suicide Ideation Inventory), PANSI-negative, depression, loneliness, HIV self-report |
| Lai, 201095 | Taiwan | Recruitment letter sent | First year college students | Male | 2585 (49 gender dysphoric) | Odds ratio | Gender dysphoria compared to non-gender dysphoric | Generalized anxiety disorder, panic disorder, hypochondriasis, major depressive disorder, body dysmorphic disorder, schizoid personality, suicidal ideation, anxiety disorder, depressive disorder, other mental health disorders |
| Female | 2615 (176 gender dysphoric) | Odds ratio | Gender dysphoria compared to non-gender dysphoric | Generalized anxiety disorder, hypochondriasis, major depressive disorder, body dysmorphic disorder, schizoid personality, suicidal ideation, anxiety disorder, depressive disorder, other mental health disorders | ||||
| Oceania | ||||||||
| Kelly, 201496 | Brisbane, Australia | Venue-based | LGBT youth | NS | 161 (24 transgender) | Prevalence | None | Alcohol, tobacco, any illicit drug use, poly-drug use, cannabis, stimulants, inhalants, prescription, medications, LSD, opiates, steroids |
| Pell, 201197 | Sydney, Australia | Clinic-based recruitment | Transgender | Male | 141 | Prevalence | None | Mental health diagnosis, HIV, past or present intravenous drug use |
| Female | 17 | Prevalence | None | Mental health diagnosis, past or present intravenous drug use | ||||
| Boza, 201498 | Australia | Internet-based | Transgender identity | Both | 243 | Prevalence | None | Depressive symptoms, suicide attempt |
| Clark, 201499 | New Zealand | Randomly selected high school recruitment | Students | NS | 8166 (96 transgender) | Adjusted odds ratio | Transgender compared with non-transgender | Significant depressive symptoms, self-harmed in last 12 months, attempted suicide |
| Pitts, 2009100 | Australia and New Zealand | Internet based | Trans people | Both | 253 | Number and types of discrimination | Chi square; prevalence | Depression; thoughts of suicide or hurting self in past 2 weeks, thoughts of feeling down, depressed or hopeless, major depressive episode |
| Multi-country | ||||||||
| Becerra-Fernandez, 2014101 | Not specified-abstract | Not specified-abstract | Female to Male transsexuals prior to cross-sex hormone therapy | Female | 77 | Prevalence | None | Obesity, polycystic ovary syndrome, metabolic syndrome, hyperandrogenism |
| Reisner, 2014102 | Latin America/Caribbean, Portugal, Spain | Internet based | MSM | Male | 35483 (158 MtF transgender) | Prevalence | None | Suicide attempt ever, depressive distress past week, HIV self-report, any STI past 12 months, syphilis, gonorrhea, chlamydia, HPV, genital herpes |
| Female | 35483 (32 FtM transgender) | Prevalence | None | Suicide attempt ever, depressive distress past week, HIV self-report, any STI past 12 months, gonorrhea, HPV, genital herpes | ||||
| Buchbinder, 2014103 | Brazil, Ecuador, Peru, South Africa | NS | MSM and transgender women | Male | 2499 (162 transgender women) | Prevalence, incidence | None | HIV seroprevalence |
| Meier, 2013104 | 19 countries | Internet-based | Female to male transgender | Female | 503 | Contrast estimate | Attracted to both men and women | Anxiety |
| Table 2. Transgender and Other Gender Minority Population Health Research on Stigma, Discrimination, Violence/ Victimization, and Sex Work Among 2008–2014 by Region, Country, and then Author. | ||||||||
| Location | Sampling method | Sample | Assigned sex at birth | Sample size | Measure of prevalence/association | Significant associations | Health outcome measures | |
| North America | ||||||||
| Bauer, 2014105 | Ontario, Canada | Respondent-driven sampling | Trans emergency department patients | Male | 195 | RDS-weighted prevalence | None | Ever avoided emergency department because trans, negative emergency department experience, refused or ended care, hurtful or insulting language, refused to discuss trans concerns, told not really trans, discouraged from exploring gender, provider does not know enough to provide care, belittled or ridiculed, thought gender marker on ID was a mistake, refused to examine parts of body |
| Female | 214 | RDS-weighted prevalence | None | Ever avoided emergency department because trans, negative emergency department experience, refused or ended care, hurtful or insulting language, refused to discuss trans concerns, told not really trans, discouraged from exploring gender, provider does not know enough to provide care, belittled or ridiculed, thought gender marker on ID was a mistake, refused to examine parts of body | ||||
| McGuire, 2010106 | California, USA | Gay Straight Alliance organization-based recruitment | LGBT and allies students | NS | 2260 (68 transgender) | T-test | Transgender compared to non-transgender | Feeling unsafe at school |
| Harawa, 2010107 | Los Angeles, USA | Random sample from prison census | MSM and male to female transgender inmates | Male | 101 (19 transgender) | Prevalence | None | Receiving money, protection, food, or other goods in exchange for sex |
| Rohde Bowers, 201112 | Los Angeles County, USA | Venue based | High risk HIV prevention program attendees | Male | 1033 (320 transgender) | Prevalence | None | Exchange sex |
| Hwahng, 201418 | New York, USA | Organization based, venue referrals, and internet | HIV uninfected male to female transgender | Male | 572 | Prevalence | None | Verbal gender abuse early adolescence, physical gender abuse early adolescence, verbal or physical gender abuse early adolescence, verbal gender abuse late adolescence, physical gender abuse late adolescence, verbal or physical gender abuse late adolescence |
| Nuttbrock, 201022 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 571 | Prevalence | None | Lifetime gender-related psychological abuse, lifetime gender-related physical abuse |
| Nuttbrock, 201323 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 230 | Adjusted odds ratio | Employment, sex work, transgender presentation, hormone therapy | Psychological gender abuse, physical gender abuse |
| Nuttbrock, 201324 | New York, USA | Organization based, venue referrals, internet advertisements | HIV uninfected male to female transgender | Male | 230 | Prevalence | None | Psychological or physical gender abuse, psychological and physical gender abuse |
| Reisner, 201016 | New England, USA | Venue-based | Transmen | Female | 16 | Prevalence | None | Sex work ever, internalized homophobia |
| Rapues, 201332 | San Francisco, USA | Respondent-driven sampling | Male to female transgender | Male | 314 | Prevalence (RDS weighted) | None | Commercial sex work |
| Sevelius, 200935 | San Francisco, USA | Clinic and location based | Transgender | Male | 153 | Prevalence | None | Sex work |
| Wilson, 201437 | San Francisco, USA | Respondent-driven sampling | Transgender women | Male | 233 | Prevalence | None | Engagement in sex work |
| Nemoto, 201438 | San Francisco and Oakland, USA | Purposive community sampling | Transgender women with a history of sex work | Male | 573 | Prevalence | Race | Sex work in past 6 months |
| Brennan, 201239 | Chicago and Los Angeles, USA | Clinic-based, venue-based, and peer outreach and referral | Young transgender women | Male | 151 | Prevalence; point biserial correlations; beta | Intimate partner violence, unprotected anal intercourse, polysubstance use; syndemic index (low self-esteem, polysubstance use, victimization, intimate partner violence) | Victimization, intimate partner violence; history of sex work |
| Bradford, 201340 | Virginia, USA | Internet and peer referral | Transgender | Both | 350 | Prevalence; Adjusted odds ratio | Suburban vs urban setting, FTM spectrum, racial/ethnic minority, education, low-income, living full time, age at transawareness, hormones, hormone therapy needed but not obtained past 3 months, counseling or psychotherapy needed but not obtained past 3 months, forced or unwanted sex, physically attacked, tobacco problem ever, drinking problem, family not supportive, being connected to the transgender community, hostility or insensitivity in school | Health care discrimination, employment discrimination; discrimination |
| Benotsch, 201313 | Mid-Atlantic, USA | Clinic-based recruitment | Transgender | Both | 155 | Prevalence | Individuals reporting non-medical use of prescription drugs | Discrimination-gender identity |
| Bockting, 201342 | USA | Internet -based | Transgender adults | Both | 1093 | Prevalence, beta | Non-white race/ethnicity, income, investment in passing, outness, age, transgender women compared to transgender men | Enacted stigma, felt stigma |
| Cruz, 2014108 | USA | Internet based | Transgender participants from the National Discrimination Survey | Both | 4049 | Prevalence; odds ratio | Trans discrimination or both discrimination and affordability; male vs other identity, female vs male identity, female vs other identity, somewhat genderqueer identity, hormones, top surgery, bottom surgery main place seeking care,, no health insurance, income | Postponement of curative care due to discrimination |
| Dank, 2014109 | USA | School-based recruitment | Students | NS | 5647 (18 transgender) | Prevalence | Transgender status | Physical dating violence, psychological dating abuse, cyber dating abuse, sexual coercion |
| House, 201149 | USA | Internet-based | LGBT adults | Both | 1126 (164 transgender) | Prevalence | None | Interpersonal trauma, experiences of discrimination |
| Kosciw, 2009110 | USA | Internet-based | Secondary school students | NS | 5420 (245 transgender) | Beta | Transgender identity compared to male identity | Victimization related to sexual orientation, victimization related to gender expression |
| Mitchell, 2014111 | USA | Internet based | 13–18 year olds completing the Teen Health and Technology survey | Both | 5498 (189 transgender, 209 gender nonconforming or other gender) | Prevalence; adjusted conditional odds | Transgender vs cisgender male, gender nonconforming or other gender vs cisgender male | Sexual harassment (any mode, in-person, online, by text message, by phone call, some other way), made obscene or sexual comments, asked for sexual information, asked to do something sexual, touched grabbed or pinched, showed/sent obscene or sexual messages, intentionally brushed up against, spread sexual rumors, blocked/cornered; non-distressing sexual harassment; distressing sexual harassment |
| Reisner, 201353 | USA | Brief intercept | Transmasculine | Female | 73 | Prevalence | None | Perceived discrimination by health care provider |
| Reisner, 201454 | USA | Convenience sample | Transfeminine gender identity | Male | 3878 | Prevalence; risk ratio | Jail/prison time, mistreated/victimized in jail/prison, denied healthcare in jail/prison | Denied healthcare in jail, mistreated victimized in jail/prison; sex work, any physical assault, any sexual assault |
| Reisner, 201455 | USA | Clinic-based | Participants from the Community Health Center Core Data Project | Both | 2653 (31 transgender) | Prevalence | Transgender | Childhood abuse, experienced intimate partner violence, any victimization as adult, verbally attacked, physically attacked, sexually harmed, any discrimination, employment discrimination, healthcare discrimination |
| Ybarra, 2014112 | USA | Targeted online recruitment | LGBT youth | Both | 5542 (442 transgender) | Prevalence | None | Online peer victimization: bullying, in person peer victimization: bullying, online peer victimization: sexual harassment, in person peer victimization: harassment |
| South and Central America | ||||||||
| Marin, 2013113 | Argentina | Sexual Workers Union registration | Female sex workers and transvestites | NS | 950 (110 transgender) | Prevalence | None | Discrimination in health care |
| Socias, 201460 | Argentina | Snowball sampling and quota sampling | Transgender | Male | 452 | Prevalence; chi square; adjusted odds ratio | Any internalized stigma, history of sex work, experienced police violence, ever arrested, perceived discrimination by healthcare workers, perceived discrimination by patients, current residency in Buenos Aires; extended health insurance | Sex work, healthcare avoidance because of transgender identity |
| Delgado, 2014114 | Chile | Snowball | Gay men and transgender women | Male | 437 (121 transgender) | Prevalence | None | Not being hired or being fired, being denied access or permanence in a public place, poorly-assisted by public officials, not accepted or excluded from school, not accepted or excluded from a group of friends, molested or harassed by neighbors, not accepted or excluded from a social group, not accepted or excluded from family, not accepted or excluded from a religious environment, verbal or physical mistreatment or being denied help by the police |
| Miller, 2011115 | Guatemala city, Guatemala | Respondent-driven sampling | MSM and transgender women | Male | 505 (99 transgender) | Prevalence | None | Transactional sex |
| Europe | ||||||||
| Prunas, 2014116 | Milan, Italy | Census | Transgender victims of transphobic murder | Male | 20 | Prevalence | None | Sex work, primary indicator of LGBT hate crime, secondary indicator of LGBT hate crime |
| Central and South Asia | ||||||||
| Brahmam, 200885 | India | Probability-based | MSM and Hijra | Male | 4600 (575 Hija) | Prevalence | None | Selling sex |
| Javaheri, 201088 | Tehran, Iran | Clinic-based recruitment | Transsexuals | Both | 40 | Prevalence | None | Being discriminated against for being transsexual |
| Oceania | ||||||||
| Pell, 201197 | Sydney, Australia | Clinic-based recruitment | Transgender | Male | 141 | Prevalence | None | Past or present sex work |
| Multi-country | ||||||||
| Reisner, 2014102 | Latin America/Caribbean, Portugal, Spain | Internet based | MSM | Male | 35483 (158 MtF transgender) | Prevalence | None | Transactional sex past 12 months, childhood gender-related harassment, adulthood gender-related harassment |
| Female | 35483 (32 FtM transgender) | Prevalence | None | Transactional sex past 12 months, childhood gender-related harassment, adulthood gender-related harassment | ||||
GID=Gender identity disorder; NS=not specified; MSM=men who have sex with men.
Bauer GRR, Nik; Bradley Kaitlin; Scheim Ayden I. Sexual Health of Trans Men Who Are Gay, Bisexual, or Who Have Sex with Men: Results from Ontario, Canada. International Journal of Transgenderism 2013;14(2):66–74.
Moody CS, N. G. Suicide protective factors among trans adults. Archives of sexual behavior 2013;42(5):739–52.
Alvarez-Wyssmann VC-Z, M.; Casillas J.; Rodriguez- Nolasco E.; Nino-Vargas R.; Escobedo T.; Rodriguez A.; Magis-Rodriguez C. Diabetes prevalence and factors associated among patients at an outpatient HIV clinic in Mexico City. Journal of the International AIDS Society 2013;16:14.
Reisner SLW, Jaclyn M.; Mayer Kenneth H.; Mimiaga Matthew J. Sexual risk behaviors and psychosocial health concerns of female-to-male transgender men screening for STDs at an urban community health center. AIDS Care 2014;26(7):857–64.
Shipherd JCM, Lauren; Shira Maguen; Green Kelly E. Male-to-Female Transgender Veterans and VA Health Care Utilization. International Journal of Sexual Health 2012;24(1):78–87.
Dowshen NF, Christine M.; Johnson Amy K.; Kuhns Lisa M.; David Rubin; Robert Garofalo. Religiosity As a Protective Factor Against HIV Risk Among Young Transgender Women. Journal of Adolescent Health 2011;48(4):410–14.
Garofalo RJ, A. K.; Kuhns L. M.; Cotten C.; Joseph H.; Margolis A. Life Skills: Evaluation of a Theory-Driven Behavioral HIV Prevention Intervention for Young Transgender Women. Journal of Urban Health 2012;89(3):419–31.
Fletcher JBK, Kimberly A.; Reback Cathy J. Housing status and hiv risk behaviors among transgender women in los angeles. Archives of Sexual Behavior 2014.
Reback CF, Jesse. HIV Prevalence, Substance Use, and Sexual Risk Behaviors Among Transgender Women Recruited Through Outreach. AIDS & Behavior 2014;18(7):1359–67.
Simons LO, Johanna; Belzer Marvin; Clark Leslie; Schrager Sheree. 29. The Relationship Between Parental Support and Depression and Suicidality in Transgender Adolescents. Journal of Adolescent Health 2012;50(2):S29–S29.
Simons LS, Sheree M.; Clark Leslie F.; Belzer Marvin; Olson Johanna. Parental Support and Mental Health Among Transgender Adolescents. Journal of Adolescent Health 2013;53(6):791–93.
Rohde Bowers JB, C. M.; Fletcher J.; Reback C. J. Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Culture, Health & Sexuality 2011;13(6):629–42.
Benotsch EGZ, Rick; Laurie Cathers; Shawn McNulty; Juan Pierce; Ted Heck; Perrin Paul B.; Daniel Snipes. Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug & Alcohol Dependence 2013;132(1–2):391–94.
McElroy JE, K.; Ge B. Out, proud and healthy project: Characterizing smoking behaviors and beliefs for 6,537 sexual and gender minority individuals. Epidemiology 2012;23(5):S656.
Irwin JAC, J. D.; Fisher C. M.; Marasco V. M. Correlates of Suicide Ideation Among LGBT Nebraskans. Journal of Homosexuality 2014;61(8):1172–91.
Reisner SLP, B.; Mimiaga M. J. A Mixed Methods Study of the Sexual Health Needs of New England Transmen Who Have Sex with Nontransgender Men. AIDS Patient Care & STDs 2010;24(8):501–13.
Shipherd JCM, Shira; Skidmore W. Christopher; Abramovitz Sarah M. Potentially traumatic events in a transgender sample: Frequency and associated symptoms. Traumatology 2011;17(2):56–67.
Hwahng SJN, Larry. Adolescent gender-related abuse, androphilia, and HIV risk among transfeminine people of color in New York City. Journal of homosexuality 2014;61(5):691–713.
Koken JAB, D. S.; Parsons J. T. Experiences of Familial Acceptance-Rejection Among Transwomen of Color. Journal of Family Psychology 2009;23(6):853–60.
Leinung MCU, M. F.; Patel N.; Sood S. C. Endocrine treatment of transsexual persons: extensive personal experience. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists 2013;19(4):644–50.
Nuttbrock LH, S.; Bockting W.; Rosenblum A.; Mason M.; MacRi M.; Becker J. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. Journal of Acquired Immune Deficiency Syndromes 2009;52(3):417–21.
Nuttbrock LH, S.; Bockting W.; Rosenblum A.; Mason M.; Macri M.; Becker J. Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. Journal of sex research 2010;47(1):12–23.
Nuttbrock L, Bockting W, Rosenblum A, et al. Gender Abuse and Major Depression Among Transgender Women: A Prospective Study of Vulnerability and Resilience. American journal of public health 2013(0):e1–e8.
Nuttbrock LB, Walter; Rosenblum Andrew; Hwahng Sel; Mason Mona; Macri Monica; Becker Jeffrey. Gender Abuse, Depressive Symptoms, and HIV and Other Sexually Transmitted Infections Among Male-to-Female Transgender Persons: A Three-Year Prospective Study. American Journal of Public Health 2013;103(2):300–07.
Nuttbrock L, Bockting W, Rosenblum A, et al. Gender Abuse, Depressive Symptoms, and Substance Use Among Transgender Women: A 3-Year Prospective Study. American journal of public health 2014;104(11):2199–206.
Pathela PB, S.; Shepard C.; Schillinger J. Incidence of sexually transmitted diseases among transgender persons with HIV, New York City, 2000–2010. Sexually Transmitted Diseases 2014;41:S118.
Flentje AH, Nicholas C.; Sorensen James L. Characteristics of transgender individuals entering substance abuse treatment. Addictive Behaviors 2014;39(5):969–75.
Gamarel KER, Sari L.; Laurenceau Jean-Philippe; Nemoto Tooru; Don Operario. Gender minority stress, mental health, and relationship quality: A dyadic investigation of transgender women and their cisgender male partners. Journal of Family Psychology 2014;28(4):437–47.
Jefferson KN, Torsten B.; Jae Sevelius. Transgender women of color: discrimination and depression symptoms. Ethnicity & Inequalities in Health & Social Care 2013;6(4):121–36.
Operario DN, Tooru; Iwamoto Mariko; Toni Moore. Unprotected Sexual Behavior and HIV Risk in the Context of Primary Partnerships for Transgender Women. AIDS & Behavior 2011;15(3):674–82.
Operario DY, M. F.; Reisner S. L.; Iwamoto M.; Nemoto T. Stigma and the syndemic of HIV-related health risk behaviors in a diverse sample of transgender women. Journal of Community Psychology 2014;42(5):544–57.
Rapues JW, Erin C.; Packer Tracey; Colfax Grant N.; Raymond Fisher. Correlates of HIV Infection Among Transfemales, San Francisco, 2010: Results From a Respondent-Driven Sampling Study. American Journal of Public Health 2013;103(8):1485–92.
Reisner SLG, Kristi E.; Nemoto Tooru; Don Operario. Dyadic effects of gender minority stressors in substance use behaviors among transgender women and their non-transgender male partners. Psychology of Sexual Orientation and Gender Diversity 2014;1(1):63–71.
Santos G-MR, Jenna; Wilson Erin C.; Macias Oscar; Packer Tracey; Colfax Grant; Henry Fisher Raymond. Alcohol and substance use among transgender women in San Francisco: Prevalence and association with human immunodeficiency virus infection. Drug & Alcohol Review 2014;33(3):287–95.
Sevelius JMR, O. G.; Hart S. L.; Schwarcz S. Informing interventions: the importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Education & Prevention 2009;21(2):113–27.
Wilson ECS, Glen-Milo; Raymond H. Fisher. Sexual mixing and the risk environment of sexually active transgender women: data from a respondent-driven sampling study of HIV risk among transwomen in San Francisco, 2010. BMC Infectious Diseases 2014;14:430–30.
Wilson ER, J.; Jin H.; Raymond H. F. The use and correlates of illicit silicone or “fillers” in a population-based sample of transwomen, San Francisco, 2013. Journal of Sexual Medicine 2014;11(7):1717–24.
Nemoto TB, Birte; Iwamoto Mariko; Sakata Maria. Practices of receptive and insertive anal sex among transgender women in relation to partner types, sociocultural factors, and background variables. AIDS Care 2014;26(4):434–40.
Brennan JK, Lisa M.; Johnson Amv K.; Belzer Marvin; Wilson Erin C.; Garofalo Robert. Syndemic Theory and HIV-Related Risk Among Young Transgender Women: The Role of Multiple, Co-Occurring Health Problems and Social Marginalization. American Journal of Public Health 2012;102(9):1751–57.
Bradford JR, Sari L.; Honnold Julie A.; Jessica Xavier. Experiences of Transgender-Related Discrimination and Implications for Health: Results From the Virginia Transgender Health Initiative Study. American Journal of Public Health 2013;103(10):1820–29.
Blosnich JRB, George R.; Shipherd Jillian C.; Kauth Michael; Piegari Rebecca I.; Bossarte Robert M. Prevalence of Gender Identity Disorder and Suicide Risk Among Transgender Veterans Utilizing Veterans Health Administration Care. American Journal of Public Health 2013;103(10):e27–32.
Bockting WOM, M. H.; Swinburne Romine R. E.; Hamilton A.; Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. American journal of public health 2013;103(5):943–51.
Budge SLA, Jill L.; Howard Kimberly A. S. Anxiety and depression in transgender individuals: The roles of transition status, loss, social support, and coping. Journal of Consulting and Clinical Psychology 2013;81(3):545–57.
Effrig JCB, Kathleen J.; Locke Benjamin D. Examining victimization and psychological distress in transgender college students. Journal of College Counseling 2011;14(2):143–57.
Feldman JR, R. S.; Bockting W. O. HIV Risk Behaviors in the U.S. Transgender Population: Prevalence and Predictors in a Large Internet Sample. Journal of homosexuality 2014;61(11):1558–88.
Fredriksen-Goldsen KIC-D, Loree; Kim Hyun-Jun; Erosheva Elena A.; Emlet Charles A.; Hoy-Ellis Charles P.; Goldsen Jayn; Muraco Anna. Physical and Mental Health of Transgender Older Adults: An At-Risk and Underserved Population. Gerontologist 2014;54(3):488–500.
Horvath KJI, A.; Swinburne-Romine R.; Bockting W. A comparison of mental health, substance use, and sexual risk behaviors between rural and non-rural transgender persons. Journal of homosexuality 2014;61(8):1117–30.
Hotton ALG, Robert; Kuhns Lisa M.; Johnson Amy K. Substance Use as a Mediator of the Relationship Between Life Stress and Sexual Risk Among Young Transgender Women. AIDS Education & Prevention 2013;25(1):62–71.
House ASVH, Elizabeth; Coppeans Christopher; Stepleman Lara M. Interpersonal trauma and discriminatory events as predictors of suicidal and nonsuicidal self-injury in gay, lesbian, bisexual, and transgender persons. Traumatology 2011;17(2):75–85.
Mustanski BL, R. T. A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Archives of sexual behavior 2013;42(3):437–48.
Peitzmeier SMR, Sari L.; Harigopal Padmini; Potter Jennifer. Female-to-Male Patients Have High Prevalence of Unsatisfactory Paps Compared to Non-Transgender Females: Implications for Cervical Cancer Screening. JGIM: Journal of General Internal Medicine 2014;29(5):778–84.
Rath JMV, A. C.; Rubenstein R. A.; Vallone D. M. Tobacco use by sexual identity among young adults in the united states. Nicotine and Tobacco Research 2013;15(11):1822–31.
Reisner SLG, Kristi E.; Dunham Emilia; Hopwood Ruben; Hwahng Sel. Female-to-Male Transmasculine Adult Health: A Mixed-Methods Community-Based Needs Assessment. Journal of the American Psychiatric Nurses Association 2013;19(5):293–303.
Reisner SL, Bailey Z, Sevelius J. Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the US. Women & health 2014(just-accepted).
Reisner SL, White JM, Bradford JB, et al. Transgender Health Disparities: Comparing Full Cohort and Nested Matched-Pair Study Designs in a Community Health Center. LGBT Health.
Sanchez FJV, E. Collective Self-Esteem as a Coping Resource for Male-to-Female Transsexuals. J Couns Psychol 2009;56(1):202–09.
Sevelius J. “There’s no pamphlet for the kind of sex I have”: HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. JANAC: Journal of the Association of Nurses in AIDS Care 2009;20(5):398–410.
Toibaro JJE, J. F.; Parlante A.; Burgoa P.; Freyre A.; Romero M.; Losso M. H. Sexually transmitted infections among transgender individuals and other sexual identities. Medicina 2009;69(3):327–30.
Carobene MB, F.; Farias M. S. D. R.; Quarleri J.; Avila M. M. HIV, HBV, and HCV molecular epidemiology among trans (transvestites, transsexuals, and transgender) sex workers in Argentina. Journal of Medical Virology 2014;86(1):64–70.
Socías ME, Marshall BD, Arístegui I, et al. Factors associated with healthcare avoidance among transgender women in Argentina. International journal for equity in health 2014;13(1):81.
Rocha RMGP, D. L.; Dias T. M. The context of drug use among transvestite sex workers. Saude Soc 2013;22(2):554–65.
Johnston LGV, T. C.; Dolores Y.; Vales H. M. HIV, hepatitis B/C and syphilis prevalence and risk behaviors among gay, transsexuals and men who have sex with men, Dominican Republic. International Journal of STD & AIDS 2013;24(4):313–21.
Aguayo NM, S. R.; Aguilar G. HIV and SYPHILIS prevalence and behaviour, practises and attitudes of the TRANS population in paraguay, 2011. Sexually Transmitted Infections 2013;89.
Lipsitz MCS, E. R.; Anton C.; Castro J.; Clark J. L.; Lake J. E.; Cabello R. Bringing HIV testing to the people - Benefits of mobile unit testing in Lima, Peru, 2007–2009. Sexually Transmitted Infections 2013;89.
Verre MCP, Jesus Segura, Eddy R.; Clark Jesse; Gonzales Pedro; Benites Carlos; Cabello Robinson; Sanchez Jorge; Lama Javier R. Socialization patterns and their associations with unprotected anal intercourse, hiv, and syphilis among high-risk men who have sex with men and transgender women in peru. AIDS and Behavior 2014.
Wierckx KE, E.; Declercq E.; Heylens G.; De Cuypere G.; Taes Y.; Kaufman J. M.; T’Sjoen G. Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: A case-control study. European Journal of Endocrinology 2013;169(4):471–78.
Auer MKF, J.; Stalla G. K.; Athanasoulia A. P. Twenty years of endocrinologic treatment in transsexualism: Analyzing the role of chromosomal analysis and hormonal profiling in the diagnostic work-up. Fertility and Sterility 2013;100(4):1103–10.
Judge COD, C.; Callaghan G.; Gaoatswe G.; O’Shea D. Gender dysphoria - prevalence and co-morbidities in an Irish adult population. Frontiers in Endocrinology 2014;5(June).
Manieri CC, Elena; Crespi Chiara; Di Bisceglie Cataldo; Dell’Aquila Carlotta; Gualerzi Anna; Molo Mariateresa. Medical Treatment of Subjects with Gender Identity Disorder: The Experience in an Italian Public Health Center. International Journal of Transgenderism 2014;15(2):53–65.
Imbimbo CV, P.; Palmieri A.; Longo N.; Fusco F.; Arcaniolo D.; Mirone V. A report from a single institute’s 14-year experience in treatment of male-to-female transsexuals. Journal of Sexual Medicine 2009;6(10):2736–45.
Asscheman HG, L. Long term mortality in hormone-treated transsexuals. Journal of Sexual Medicine 2009;6:420.
de Vries ALN, I. L.; Cohen-Kettenis P. T.; van Berckelaer-Onnes I. A.; Doreleijers T. A. Autism spectrum disorders in gender dysphoric children and adolescents. Journal of autism and developmental disorders 2010;40(8):930–6.
de Vries ALCD, T. A. H.; Steensma T. D.; Cohen-Kettenis P. T. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry 2011;52(11):1195–202.
Almeida AB, A.; Costa J.; Eusebio M.; Fernandes R. Prevalence of and factors mediating HIV infection among sex workers in Lisbon, Portugal: the 5-year experience of a community organisation. Sexually Transmitted Infections 2014;90(6).
Guzman-Parra JP-M, Pedro; de Diego-Otero Yolanda; Perez-Costillas Lucia; Villena-Jimena Amelia; Garcia-Encinas Maria A.; Bergero-Miguel Trinidad. Substance Use and Social Anxiety in Transsexual Individuals. Journal of Dual Diagnosis 2014;10(3):162–67.
Hill SCD, J.; Benzie A.; Ayres J.; King G.; Smith A. Sexual health of transgender sex workers attending an inner-city genitourinary medicine clinic. International Journal of STD & AIDS 2011;22(11):686–87.
Pasterski VG, Liam; Richard Curtis. Traits of autism spectrum disorders in adults with gender dysphoria. Archives of Sexual Behavior 2014;43(2):387–93.
Davey AB, W. P.; Arcelus J.; Meyer C. Social Support and Psychological Well-Being in Gender Dysphoria: A Comparison of Patients With Matched Controls. Journal of Sexual Medicine 2014.
Claes LB, W. P.; Witcomb G.; Thurston M.; Fernandez-Aranda F.; Arcelus J. Non-Suicidal Self-Injury in Trans People: Associations with Psychological Symptoms, Victimization, Interpersonal Functioning, and Perceived Social Support. The journal of sexual medicine 2014.
Turner RH, M.; Campbell M.; Day S.; Sullivan A. High rates of STIs in SWISH clinic-a dedicated service for sex workers. HIV Medicine 2014;15:38.
Heylens GE, E.; Kreukels B. P. C.; Paap M. C. S.; Cerwenka S.; Richter-Appelt H.; Cohen-Kettenis P. T.; Haraldsen I. R.; De Cuypere G. Psychiatric characteristics in transsexual individuals: Multicentre study in four European countries. British Journal of Psychiatry 2014;204(2):151–56.
Kalra GS, Nilesh. The Cultural, Psychiatric, and Sexuality Aspects of Hijras in India. International Journal of Transgenderism 2013;14(4):171–81.
Arora RP, D.; Mishra K.; Bhattacharya S. N.; Yhome V. A. Screening for anal dysplasia in HIV positive and HIV negative men who have sex with men using anal cytology and P16/Ink4 immunostaining; a crossectional study. Sexually Transmitted Infections 2013;89.
Ramakrishnan LG, P.; Subramaniam T.; Mathew S.; Ramanathan S.; George B.; Adhikary R.; Mainkar M. K.; Paranjape R. S. Transgender in Tamil Nadu are still highly vulnerable to HIV and STIs: Findings from bio-behavioral surveys. Journal of the International AIDS Society 2012;15:154–55.
Brahmam GNK, V.; Rajkumar H.; Rachakulla H. K.; Kallam S.; Myakala S. P.; Paranjape R. S.; Gupte M. D.; Ramakrishnan L.; Kohli A.; Ramesh B. M. Sexual practices, HIV and sexually transmitted infections among self-identified men who have sex with men in four high HIV prevalence states of India. Aids 2008;22 Suppl 5:S45–57.
Aghabikloo AB, M.; Saberi S. M.; Emamhadi M. A. Gender identity disorders in Iran; request for sex reassignment surgery. International Journal of Medical Toxicology and Forensic Medicine 2012;2(4):128–34.
Ahmadzad-Asl MJ, A. H.; Alavi K.; Naserbakht M.; Taban M.; Mohseninia-Omrani K.; Eftekhar M. The epidemiology of transsexualism in Iran. European Psychiatry 2013;28.
Javaheri F. A Study of Transsexuality in Iran. Iranian Studies 2010;43(3):365–77.
Bhatta DN. HIV-related sexual risk behaviors among male-to-female transgender people in Nepal. International Journal of Infectious Diseases 2014;22:e11–e15.
Rehan N. Genital examination of hijras. Journal of the Pakistan Medical Association 2011;61(7):695–96.
Emmanuel FM, Salim; Naeem Akhtar; Salwa Arshad; Reza T. E. Second-generation surveillance for HIV/AIDS in Pakistan: results from the 4th round of Integrated Behavior and Biological Survey 2011–2012. (Special Issue: HIV/STI research in MENA.). Sexually Transmitted Infections 2013;89(Suppl. 3).
Chemnasiri TN, T.; Visarutratana S.; Varangrat A.; Li A.; Phanuphak P.; Jommaroeng R.; Akarasewi P.; van Griensven F. Inconsistent condom use among young men who have sex with men, male sex workers, and transgenders in Thailand. AIDS Education & Prevention 2010;22(2):100–09.
Gooren LJ, Sungkaew T, Giltay EJ, et al. Cross-sex hormone use, functional health and mental well-being among transgender men (Toms) and Transgender Women (Kathoeys) in Thailand. Culture, health & sexuality 2015;17(1):92–103.
Yadegarfard MH, Robert; Bahramabadian Fatemeh. Influences on loneliness, depression, sexual-risk behaviour and suicidal ideation among Thai transgender youth. Culture, Health & Sexuality 2013;15(6):726–37.
Lai MCC, Y. N.; Gadow K. D.; Gau S. S.; Hwu H. G. Correlates of gender dysphoria in taiwanese university students. Archives of Sexual Behavior 2010;39(6):1415–28.
Kelly JD, Cassandra; Schlesinger Carla. Substance use by same sex attracted young people: Prevalence, perceptions and homophobia. Drug and Alcohol Review 2014.
Pell CP, I.; Vlahakis E. Comparison of male to female (MTF) and female to male (FTM) transgender patients attending taylor square private clinic (TSPC) Sydney, Australia; clinical audit results. Journal of Sexual Medicine 2011;8:179.
Boza CNP, Kathryn. Gender-Related Victimization, Perceived Social Support, and Predictors of Depression Among Transgender Australians. International Journal of Transgenderism 2014;15(1):35–52.
Clark TCL, Mathijs F. G.; Bullen Pat; Denny Simon J.; Fleming Theresa M.; Robinson Elizabeth M.; Rossen Fiona V. The Health and Well-Being of Transgender High School Students: Results From the New Zealand Adolescent Health Survey (Youth’12). Journal of Adolescent Health 2014;55(1):93–99.
Pitts MKC, M.; Mulcare H.; Crow S.; Mitchell A. Transgender people in Australia and New Zealand: health, well-being and access to health services. Feminism & Psychology 2009;19(4):475–95.
Becerra-Fernandez AP-L, G.; Roman M. M.; Martin-Lazaro J. F.; Lucio Perez M. J.; Asenjo Araque N.; Rodriguez-Molina J. M.; Berrocal Sertucha M. C.; Aguilar Vilas M. V. Prevalence of hyperandrogenism and polycystic ovary syndrome in female to male transsexuals. Endocrinologia y Nutricion 2014;61(7):351–58.
Reisner SLB, Katie; Rosenberger Joshua G.; Austin S. Bryn; Haneuse Sebastien; Perez-Brumer Amaya; Novak David S.; Mimiaga Matthew J. Using a two-step method to measure transgender identity in latin america/the caribbean, portugal, and spain. Archives of Sexual Behavior 2014.
Buchbinder SPG, David V.; Liu Albert Y.; McMahan Vanessa; Guanira Juan V.; Mayer Kenneth H.; Goicochea Pedro; Grant Robert M. HIV pre-exposure prophylaxis in men who have sex with men and transgender women: a secondary analysis of a phase 3 randomised controlled efficacy trial. Lancet Infectious Diseases 2014;14(6):468–75.
Meier SCP, S. T.; Labuski C.; Babcock J. Measures of clinical health among female-to-male transgender persons as a function of sexual orientation. Archives of sexual behavior 2013;42(3):463–74.
Bauer GRS, Ayden I.; Deutsch Madeline B.; Massarella Carys. Reported emergency department avoidance, use, and experiences of transgender persons in ontario, Canada: results from a respondent-driven sampling survey. Annals of Emergency Medicine 2014;63(6):713–20.e1.
McGuire JKA, C. R.; Toomey R. B.; Russell S. T. School climate for transgender youth: a mixed method investigation of student experiences and school responses. Journal of Youth & Adolescence 2010;39(10):1175–88.
Harawa NTS, J.; George S.; Sylla M. Sex and condom use in a large jail unit for men who have sex with men (MSM) and male-to-female transgenders. Journal of Health Care for the Poor & Underserved 2010;21(3):1071–87.
Cruz TM. Assessing access to care for transgender and gender nonconforming people: A consideration of diversity in combating discrimination. Social Science & Medicine 2014;110:65–73.
Dank ML, Pamela; Zweig Janine M.; Yahner Jennifer. Dating violence experiences of lesbian, gay, bisexual, and transgender youth. Journal of Youth and Adolescence 2014;43(5):846–57.
Kosciw JGG, E. A.; Diaz E. M. Who, what, where, when, and why: Demographic and ecological factors contributing to hostile school climate for lesbian, gay, bisexual, and transgender youth. Journal of Youth and Adolescence 2009;38(7):976–88.
Mitchell KJY, M. L.; Korchmaros J. D. Sexual harassment among adolescents of different sexual orientations and gender identities. Child Abuse and Neglect 2014;38(2):280–95.
Ybarra MLM, K. J.; Palmer N. A.; Reisner S. L. Online social support as a buffer against online and offline peer and sexual victimization among U.S. LGBT and non-LGBT youth. Child Abuse and Neglect 2014.
Marin GS, M.; Martinez S.; Sanguinetti C. Healthcare program for sex workers: a public health priority. The International journal of health planning and management 2013.
Delgado JBC, M. C. Construction and Validation of a Subjective Scale of Stigma and Discrimination (SISD) for the Gay Men and Transgender Women Population in Chile. Sex Res Soc Policy 2014;11(3):187–98.
Miller WA, B.; Boyce S.; Alvarado A.; Barrington C.; Paz-Bailey G. Transgender persons in guatemala - Overexposed and under-protected - The findings of an RDS behavioural survey. Sexually Transmitted Infections 2011;87:A132.
Prunas A, Clerici CA, Gentile G, et al. Transphobic Murders in Italy An Overview of Homicides in Milan (Italy) in the Past Two Decades (1993–2012). Journal of interpersonal violence 2014:0886260514554293.
Figure 1.
Map of the Distribution of Studies in Transgender Health (n=116).
Figure 2.
Number of Studies Containing Transgender Health and Disease Burden Per Year (n=116).
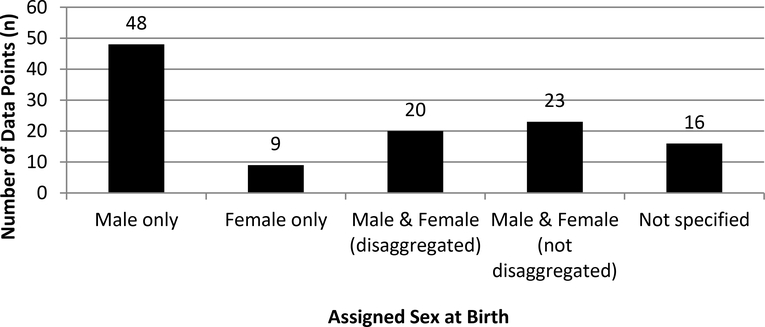
Distribution of Studies by Sex and Gender
The distribution of studies by natal sex (e.g., sex assigned at birth) are depicted graphically in Figure 3. The majority of studies focus on natal males. Operationalization of “transgender” is inconsistent making generalization of scientific findings difficult by gender identity. Specifically, we found 95 distinct operationalizations of “transgender” across the 116 studies. These can be summarized into two approaches to measuring transgender populations: identity-based measures (i.e., identify as transgender, FTM, MTF, trans masculine, trans feminine, transsexual, genderqueer; n=75/95, 78.9%) or psychiatric clinical diagnostic criteria such as gender identity disorder (GID) or gender dysphoria (GD) (n=20/95, 21.1%). The predominance of identity-based research is consistent with the trend toward de-pathologization of gender diversity in transgender health research.10
Figure 3.
Distribution of Studies By Assigned Sex at Birth in Transgender Health Research (n=116 studies)
Summary of Methodological Limitations in Current Research
The most common study design is cross-sectional (90/116, 77.6% of studies). We note the dearth of longitudinal data (7/16, 6.0% of studies), and identified only a single randomized-controlled efficacy trial of an intervention to improve the health of transgender people globally; two studies utilized a pre-/post-intervention design. Only three studies were identified that used probability-based sampling methods (3/116, 2.6%). Many studies use convenience sampling methods and deploy multiple sampling strategies simultaneously (e.g., online, venue-based, peer referral, snowball sampling). Some sampling schemes are more focused, for example clinic samples (29/116, 25.0%), exclusively Internet-based samples (17/116, 14.7%), or respondent-driven samples (8/116, 6.9%). Most studies (95/116, 81.9%) are descriptive, only presenting prevalence data (predominately unadjusted prevalences) and do not present any measures of association to examine the relationship of risk factors(s) and/or social determinant(s) with health outcomes. Few studies compare transgender and non-transgender people (e.g., offer comparative data); most are within-group focused not allowing for documentation of health inequities.
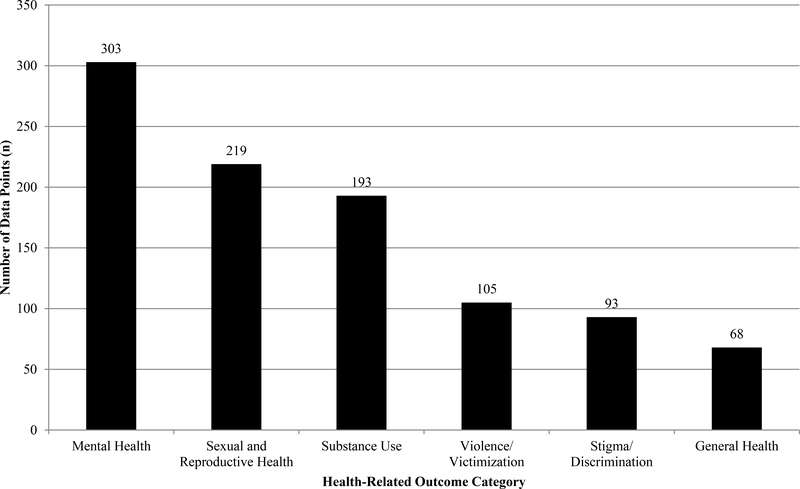
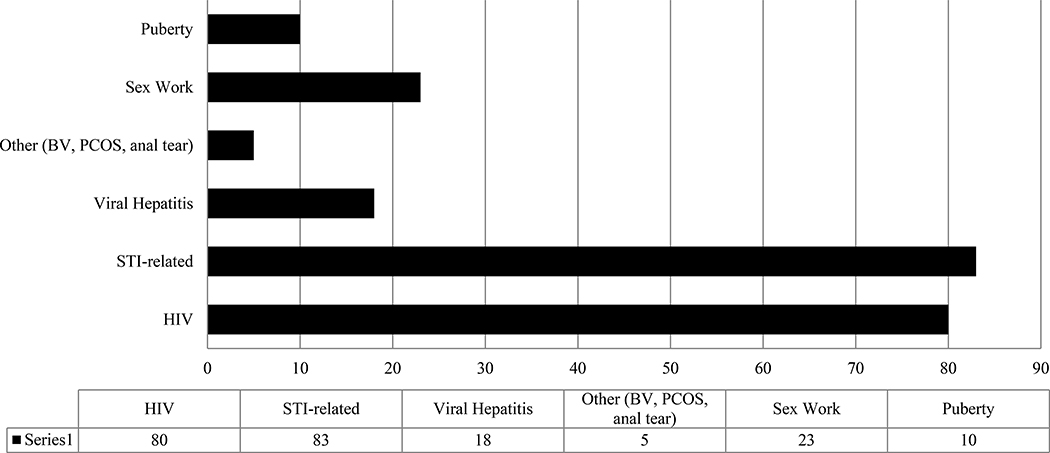
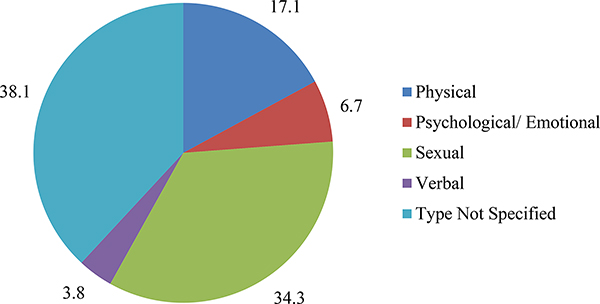
Data Points Categorized By Health Outcome Domain
Overall 981 unique health-related data points were identified from the 116 studies. Figure 4 presents these data points grouped into six health-related outcome categories by frequency: (1) mental health (e.g., depression, anxiety), (2) sexual and reproductive health (e.g., HIV, STIs), (3) substance use (e.g., alcohol, drugs), (4) violence/victimization (e.g., sexual, physical abuse), (5) stigma/ discrimination (e.g., internalized stigma, fired from employment), and (6) general health (e.g., diabetes, cancer). High burden of adverse health and disease outcomes face transgender populations globally where data are available. We briefly summarize data on each of the health areas below.
Figure 4.
Distribution of Data Points Grouped Into Six Health-Related Outcome Categories in Global Transgender Health Research (n=981).
(1). Mental Health
Mental health is the most commonly studied area of transgender health (n=303 data points; 30.9%). The majority of data points focus on mood disorders (n=96, 31.6%), suicidal and non-suicidal self-injury (n=50, 16.5%), and anxiety disorders (n=44, 14.5%). Mental health outcomes are inconsistently operationalized across studies. For example, within mood disorders (n=96), there are 80 data points focused on depression. Many studies of depression use diverse clinical screening cut-points for clinical syndromes (e.g., past week depressive distress assessed via Center for Epidemiologic Studies Depression Scale (CESD) with differing cut-points), differing timeframes of assessment (e.g., lifetime depression, past week depressive distress, clinical diagnosis of current major depressive episode), and heterogeneous subpopulations of transgender people (e.g., MTF, hijra, FTM). Despite these limitations, data consistently show that transgender adults are burdened by mental health concerns. For example, depression prevalence estimates are as high as 64.2% (CESD 16+) in a sample of 573 transgender women11 and 63.0% (operationalized as CESD 20+) in a sample of 230 MTF.12 Studies using clinical diagnosis of depression rather than screeners show lower prevalences. For example, 31.4% in 207 MTF (% in clinical range of MMPI) in Amsterdam13 and 36.2% experiencing a current major depressive episode in 253 transgender people (both MTF and FTM) in Australia.14
Understanding risk factors for mental health problems is critical to decreasing global mental health morbidity, yet remarkably few studies have done so in transgender people. The majority of mental health research (n=161/981 data points, 53.2%) report prevalence data only. Measures of association between risk factors and mental health conditions are an important area for future research efforts. Additional gaps in mental health research include few studies examining PTSD or traumatic stress (n=3 data points), surprising given many transgender people experience violence and/or victimization (see below for summary); and little data on eating disorders (n=3 data points), despite body image concerns15 and the hypothesized relation between body image and sexual risk.16
(2). Sexual and Reproductive Health
Sexual and reproductive health is the second most frequently studied area of transgender health (n=219/981 data points; 22.3%). The number of STI data points compared to other sexual and reproductive health data points is inflated because many studies of STIs tested for multiple specific organisms (e.g., gonorrhea and chlamydia), thereby creating multiple data points for that study. Transgender women are disproportionately impacted by HIV and other STIs, therefore it may not be surprising that 75% (163/219) of the sexual and reproductive health outcomes in the published literature include HIV or STI prevalence. However, when examined by assigned sex at birth, it becomes clear that this focus on HIV/STIs reflects a focus on transgender people assigned a male sex at birth. This also demonstrates that other sexual and reproductive health concerns receive little attention in research among transgender populations. For example, only 15 data points addressed non-infectious reproductive health concerns, and none addressed fertility or pregnancy.
(3). Substance Use
Substance use is the third most frequently studied health indicator (n=193/981 data points). Data more commonly focus on alcohol (n=35 data points, 18.2%), marijuana (n=25 data points, 13.0%), any illicit drug use (type not specified, n=16 data points, 8.3%), and tobacco use (n=14 data points, 7.3%). A noteworthy finding is that research on substance abuse, dependence, or disorder only comprises 5.2% of substance use data (n=10 data points). Substance use outcomes are heterogeneous and inconsistently operationalized across data points, including time of recall (e.g., last 30 days, last 3 months, past 6 months, last year, lifetime) making comparison across studies difficult. Substance use has been conceptualized as a coping mechanism to manage minority stress;17 however, scarce are data examining this association among transgender people.
(4). Violence/Victimization
Research on violence and/or victimization experiences among transgender people faces methodological challenges, most commonly use of unstandardized and often non-validated measures of violence and victimization. Despite these limitations, research demonstrates a high burden of violence and/or victimization experiences in transgender people globally. Overall, 105 data points were identified examining violence and/or victimization in transgender people, 80 data points (76.2%) presenting prevalence data only. The median prevalence estimate for violence and/or victimization experienced is 44.0%. Violence and/or victimization data points were sexual (34.3%), physical (17.1%), psychological/ emotional (6.7%), verbal (3.8%), or type not specified (38.1%). Verbal and psychological/ emotional violence and victimization appear under-researched highlighting the need for studies to include multiple dimensions of abuse.
(5). Stigma/ Discrimination
Only 14 articles (93 data points) in the published literature included stigma/discrimination as health outcomes. Of these 14 studies, the majority (n=10) were conducted in North America. Chile, Argentina, and Iran are the only other countries that published data on stigma/discrimination against transgender people as health outcomes, leaving notable gaps in data from regions outside of North and South America. A little over half (54%) of outcomes specifically address stigma and discrimination in healthcare, including denial of care and postponement of care due to stigma. However, there remains a dearth of literature on the outcomes of interventions designed to reduce anti-transgender stigma and discrimination. Clearly, more research is needed to better understand how to address stigma and discrimination in order to improve healthcare access and utilization for transgender populations (Sidebar 4).
Sidebar 4: Gender Affirmation: A Key Determinant of Transgender Health.
A key social determinant of health for transgender populations worldwide is gender affirmation. Gender affirmation has been defined as an interpersonal and shared process through which a person’s gender identity is socially recognized.8−10 However, gender affirmation is not only social—social recognition of gender also involves other institutions such as healthcare and law. Gender affirmation can thus be conceptualized as having four core facets: social (e.g., name, pronoun), psychological (e.g., internal, felt self), medical (e.g., cross-sex hormones, surgical intervention, other body modification), and legal (e.g., legal gender markers, name change). Gender affirmation depends on a variety of factors—including context and setting (i.e., country and region) and issues relating to accessibility of cross-sex hormones (in terms of availability of medications, accessibility to culturally competent healthcare providers), socioeconomics and poverty, criminalization of sexual and gender minorities, legal barriers to changing gender markers and identity recognition, etc. There is not a single path to gender affirmation—no “one size fits all” approach describes how transgender people affirm and embody their gender.11 Some people may socially, but not medically, affirm their gender; others may socially and medically but not legally do so. Gender affirmation sometimes, but not always conforms to binary categories of being female or male. Non-binary refers to having a transgender identity that does not utilize female or male dichotomies as reference points.
(6). General Health
The general health of transgender people is the least researched aspect of the transgender global burden of disease. The general health category (e.g., mortality, diabetes, hormone use, metabolic syndrome, cancer) has the fewest data points (n=68/981 data points) with 40 distinct health indicators (28 health indicators have only a single data point). The majority of research (76.5%, n=52) reports unadjusted prevalence estimates only.
Current Gaps and Opportunities
For transgender people, health inequities are hypothesized to arise from systematic exposure to multiple, intersecting social stressors, including legal and other structural factors that are a result of being part of a socially marginalized group.18 Social and economic exclusion are therefore conceptualized as causal pathways to adverse health—however, we found very few studies actually linking these social stressors to health indicators. Further, study designs are largely cross-sectional, limiting causal inference. Also scarce are intervention studies examining changes in health status alongside implementation of heath behavior or other social and structural change interventions to improve the lives of transgender people. Studies of legal issues and their impact on transgender health are needed, including research on structural factors relating to human rights like criminalization (related to gender identity and expression as well as sex work) and legal recognition.
The Way Forward: Recommendations
Below we offer recommendations based on our research synthesis to guide future health research focused on transgender populations.
“Count” Transgender Populations
Social determinants (e.g., age, sex, gender, race, socioeconomic status) shape health status of people across the world. The World Health Organization (WHO) defines social determinants of health as “the conditions in which people are born, grow, live, work and age” and states explicitly that “these circumstances are shaped by the distribution of money, power and resources at global, national and local levels.”19 Social inequalities resulting from social determinants are conceptualized as driving health inequities.20 Health inequities refer to avoidable, remediable, unfair health inequalities between populations.20 A social determinants perspective explicitly links reductions in health inequality to achievement of health equity.21
Health inequality monitoring refers to the systematic tracking of health inequalities over time, including the magnitude of disparities in the face of interventions such as policies, programs, and practices.22 Equity stratifiers refer to dimensions of social inequalities being monitored (i.e., place or residence, race or ethnicity, etc.).22 Few population-level data exist to monitor the health of transgender people worldwide. This is because routine national and international health surveillance efforts in the vast majority of countries do not assess gender identity as an equity stratifier. This is a major gap in furthering understanding of the health inequities burdening transgender people (Sidebar 5). It is also a missed opportunity to understand intersecting social statuses (e.g., disability status, caste) and health. There is a need for surveillance definitions of transgender people for global use. Studies restricting samples to people with diagnosed gender identity disorder or gender dysphoria do not capture the range of transgender people who comprise the overall population (e.g., non-binary transgender identities).
Sidebar 5: The Right to Inclusion in Health Surveillance.
A first-line argument made for non-inclusion of measures to identify transgender people in routine health surveillance efforts has been the small population size. How large is the transgender population globally? It depends how the population is measured. Over the past 15 or so years there has been a paradigm shift in transgender health from a disease-based model (transgender as disorder or mental health “diagnosis”) to an identity-based model (transgender as identity).11,12 (Please see Paper 1 for history and details). Conceptualizing transgender people as having diverse, non-pathological genders rather than as “disordered” re-defines how a “case” is operationalized and measured in health research.13 Such re-definition of a “case” also necessarily affects prevalence estimates as to the number of transgender people in the world and, potentially, estimation of the distribution, burden, and magnitude of disease inequity in the population. Still, most conservative estimates suggest 0.1%−0.5% of the world population may be transgender.14,15 Assuming the world population is approximately 7 billion people,16 this is an estimated 7 to 35 million transgender people globally. That said, does the number of transgender people matter in a population so grossly underserved worldwide?
As White and colleagues described in Paper 1 of this issue, a recommended approach to capturing health-related data by transgender status is to use a two-step method.3,23–25 This method uses assigned sex at birth and current gender identity to cross-classify respondents as transgender (discordant sex/gender responses) or non-transgender (concordant sex/gender responses). It also allows for diverse gender identities to be captured. Researchers have operationalized the two-step method using a variety of questions and response options (Sidebar 6). There have also been differences in the order of question asking (sex followed by gender identity, or vice versa) and whether gender identity is assessed using “check one” or “check all” instructions. The strength of a two-step method is that it explicitly captures dimensions of both natal sex (sex at birth) and gender (current gender identity). It also permits categorization of subpopulations of transgender people by natal sex and gender identity. A two-step method has not been used widely across the world. Studies are needed in different contexts and settings that implement this approach using consistent definitions of transgender. We recommend that special care be taken in designing instructions and lead-in text for the two-step method, including adaptations for the specific geographic context in terms of language and cultural understandings of sex and gender. Training of interviewer staff and research teams are also recommended, as well as a process to confirm transgender responses in order to minimize misclassification bias.
Sidebar 6: Example of Two-Step Method in Data Collection.
Standardization of data collection to routinely monitor health and disease distribution among transgender people represents a critical step. A two-step method is recommended,17−20 including by the World Professional Association for Transgender Health (WPATH).21 Appropriate adaptations to the two-step method are needed in different geographic regions, cultures, and languages.
Reisner and colleagues (2014) implemented the two-step method in the Growing Up Today Study (GUTS), a U.S. prospective cohort of >16,000 youth enrolled in 1996.22 Step 1 asked: “What sex were you assigned at birth, on your original birth certificate? (check one)” with response options “female” and “male.” Step 2 asked: “How do you describe yourself? (check one)” with response options “female”, “male”, “transgender”, “do not identify as female, male, or transgender.” Cross-tabulating these questions gives a two by four (2×4) contingency table with eight cells demonstrating different sex and gender combinations. Overall, 0.33% of the cohort self-identified as transgender or another gender minority in 2010.
Table.
Example of Using a Two-Step Method to Capture Data on Transgender People from the U.S. Growing Up Today Study (GUTS).
| Assigned Sex at Birth | ||
|---|---|---|
| Current Gender Identity | Male | Female |
| Male | Cisgender | Trans Masculine* |
| Female | Trans Feminine* | Cisgender |
| Transgender | Trans Feminine* | Trans Masculine* |
| Do Not Identify As Male, Female, or Transgender | Trans Feminine* | Trans Masculine* |
Cisgender = Non-Transgender
Adding these cells results in overall prevalence of Transgender.
The two-step approach can help to not only understand population size and health inequities facing transgender people, but can also aide in explicit consideration of sex and gender differences more broadly—and health inequities that may be due to assigned sex, current gender, both, or neither. The two-step method thus facilitates a gender analysis in population health.23−25
Put the “Gender” Back into Transgender Health
Sex and gender are determinants of health across a wide variety of geographic contexts.19,26–31 Causal mechanisms for poor health are both sex- and gender-related; however, sex and gender are commonly conflated in research.26 For example, terms referring to assigned sex at birth (“male” and “female”) and gender identity (“men” and “women”, respectively) are commonly used interchangeably in the scientific literature, including in transgender research. This leads to a lack of attention as to whether health differences are due to sex, gender, both, or neither,26 which affects understanding of health inequities. Synthesizing research on the health of transgender people reveals gaps in the specificity and operationalization of sex and gender differences in population research more broadly.
Developing new conceptual models and integrating and testing existing frameworks is needed to guide research in transgender population health. Several conceptual models have been applied to transgender health, including social determinants and social ecological models,19,32 gender affirmation,33 gender minority stress,17,34,35 syndemic production,36 and health and human rights.2,37 These models overlap in their shared recognition that multiple and intersecting levels of risk and resiliency shape the health of transgender people and that, therefore, multilevel contextually-relevant interventions are necessary. However, these models do not apply a gender analysis,26 a social epidemiologic approach that explicitly considers socially derived gender exposures and outcomes, sex-linked physiological or biological differences, and the interplay of both gender and sex.26,38–40 Transgender people share many of the same risks and social and structural determinants of disease, health, and wellbeing as non-transgender people (e.g., socioeconomic status). However, transgender people also experience unique biological, behavioral, social, and structural contextual factors surrounding health risks and resiliencies—including those related to challenging the congruence or conflation of sex and gender such as legal recognition of gender identity. We therefore recommend that future research in transgender population health use a gendered situated vulnerabilities framework to investigate whether and how sex-gender mechanisms26 shape health-related risks and resiliencies for population health outcomes.
Gendered situated vulnerabilities refer to the ways in which health is shaped by the distribution of power along lines of gender.41,42 The vulnerabilities transgender people face vis a vis health are related to challenging gendered relations of power and policing of gender by social structures. We refer to these as situated because the health risks and resiliencies facing transgender populations cannot be understood devoid of the multilevel sexed and gendered contexts which shape them. We use the term vulnerabilities to describe the ways that these contexts put transgender people “at risk for risk.”43,44 We do not conceptualize transgender people as an inherently vulnerable population; but rather, view this community as a population facing sex- and gender-related situated vulnerabilities for different health conditions. As shown in the synthesis of current research, some of the health conditions differentially distributed by transgender status include mental health, infectious diseases, and substance use and abuse.
Integrate Health and Human Rights and Multi-Sectorial Approaches
Transgender people have the right to legal recognition of their gender identity, access to gender affirmation, and a right to self-determination and autonomy.45–48 Although the Office of the High Commissioner for Human Rights denounces widespread discrimination against transgender people,6 systematic social and economic marginalization, stigma, pathologization, discrimination, violence, and other human rights violations, including in healthcare, continue to drive and/or exacerbate health inequities. Improving the health and access to healthcare of transgender people globally requires a wide array of stakeholders and mobilizing diverse multi-sector partnerships. Many barriers to healthcare and adverse health risks are addressable through law and policy, which some countries have begun to address through gender identity laws, legislation regarding gender affirmative care, anti-discrimination and protective measures. For example, in 2012 the Argentinian Senate passed the first gender identity law in the world authorizing transgender people to change their legal gender markers with the only requirement being a simple administrative process, with improved access to hormonal treatments and/or surgical procedures that only requires informed consent (as per standards of care endorsed by the World Professional Association for Transgender Health; WPATH),49,50 and under governmental coverage.51 Evaluation of the effect of these legal changes and improvements on the health of transgender people is needed. Implementation science, an emerging domain of methods aiming to harness generalizable information that can inform the effectiveness of programs and policies,52 is well-suited for such evaluations.
Transgender health research is not without challenges. Public health researchers must work together with policymakers, healthcare providers, and communities and their political organizations to address systematic institutionalized marginalization. In general, social, ethnical, and psychological aspects of research are not considered “high” on the hierarchy of evidence-for-practice.53,54 This is compounded by challenges of researching a discriminated population where there is institutionalized censure, and in some cases criminalization, of not only transgender communities themselves, but the researchers and clinicians who engage with them. In most countries, transgender is not included in formal training curricula for medicine, epidemiology, public health, education, legal, and social service systems, shaping a poor foundation for research and core competency in transgender health. Integrating public health practice, research, education, advocacy, and funding is critical to address the health needs of transgender people and their allies seeking to understand and ameliorate transgender health disparities.
Engage Transgender People: A Participatory Population Perspective
Within transgender communities, immediate survival needs may supersede perceived health risks and undermine traditional research approaches—i.e., research may seem to have little meaning and relevance to people’s lives. Poverty, food insecurity, mobility, and security issues may affect research participation and attrition rates, as may intersectional issues of sex work, refugee status, and homelessness. Inclusion of transgender people in public health efforts and working with the local community and its political organizations in each geographic area to advance transgender health and human rights agendas is essential. The use of a “participatory population perspective”55 and community-based participatory research principles56 represent an important future step to ensure health-related research and interventions are responsive to the real-life issues transgender people face. This means conducting research “with” and not “on” transgender populations,57 as well as being transparent in methodological sections of research articles about whether and how transgender communities were engaged in the research process. Meaningful engagement of transgender people will ensure research is culturally specific to local community needs, research questions and surveys are gender-affirming, and the science (e.g., study design, sampling) is appropriately aligned with and feasible for the study population.
Limitations of the Review
Given the lack of definitional consistency within research among transgender populations, conducting a synthesis of transgender population health requires a complex set of diverse search terms and key words to accurately identify the current health research (See Web Appendix for protocol). Notably, the term “transgender” was only recently added to PubMED as a MeSH term in 2013. From 2001–2012, “transsexualism” was the index term. In the U.S., the phrase gender minority has been used to describe transgender people to be inclusive of a broad array of diverse gender identities, not just people who self-identify as transgender.1 “Gender minority” is currently not indexed. We recommend that it be added as a MeSH term.
Some data characterizing transgender populations did not satisfy the objectives of the review. Data describing sexual satisfaction or quality of life were not included because these measures are often reported in clinical studies of gender reassignment surgical outcomes. While the focus here was on public health studies, we refer readers to recent review papers of gender reassignment outcomes.7,8 Studies examining neuroanatomical or neuropsychological differences between transgender populations were excluded. These data are critical, especially as new surgical procedures are developed, but they are also outside of the scope of the current review on the global burden of disease in transgender people from a public health perspective.
A noteworthy limitation of this synthesis pertains to reporting data at the level of data points in some instances, rather than reporting at the study level. This could inflate some estimates reported (i.e., studies with more data points contribute more data). Thus, the count of data points presented in this review is not to be interpreted as a measure of the quality of data. We also excluded qualitative studies which are a rich source of inquiry.
This review was limited to peer-reviewed literature. Many non-peer reviewed sources from the World Health Organization, Pan American Health Organization, Public Health Agency of Canada, UNAIDS, Centers for Disease Control, and additional health agencies and organizations including grassroots community-based needs assessments provide invaluable data. Partnerships between community members and researchers to collect data represent an important step in improving future transgender health research worldwide.
Conclusions
The global disease and health burden of transgender people remain understudied, particularly in relation to the impact of stigma, discrimination, social, and structural factors that affect the health of this underserved population.48 Lack of standardized survey items to identify transgender respondents limits existing health surveillance efforts. Lack of consistent operationalization of transgender status across studies limits generalizability of findings. Using a two-step approach to standardize data collection in health—modified for the specific geographic context, language, and locale—will allow researchers, policymakers, and transgender people themselves to add to monitor and evaluate efforts to achieve health equity. Measuring sex and gender dimensions in health research will contribute to understanding and ameliorating health inequities for all.
Despite substantial gaps in empirical research, there are sufficient actionable data highlighting unique biological, behavioral, social, and structural contextual factors surrounding health risks and resiliencies for transgender people that need interventions.48 Studies are needed that conceptually integrate and examine transgender-specific social determinants of health, including incorporating a framework of gendered situated vulnerabilities. A comprehensive public health approach including access to gender affirmation (social, medical, legal), improved health systems informed by high quality data, and effectively partnering with local transgender communities to ensure responsiveness of and cultural specificity of programming represents an important next step. Dedicated funding to ensure consistency of definitions for health surveillance and research initiatives involving transgender people are essential to inform evidence-based decisions regarding the scale and content of programs. Multisector partnerships that integrate health and human rights represent a critical next step to advance social justice and ultimately the health of transgender people worldwide.
Supplementary Material
Key Messages.
A comprehensive public health approach to address the health of transgender people requires ensuring access to gender affirmation, evidence-based healthcare delivery systems, and effective partnerships with local transgender communities.
The health-related vulnerabilities among transgender people underscore the need to explicitly consider sex and gender pathways and mechanisms in epidemiologic research and public health surveillance more broadly.
Multi-sector partnerships linking health with advocacy, social justice, and human rights are critical to address the public health needs of transgender people across the world.
Lack of standardized survey items on population-based surveys to identify transgender respondents limits existing public health surveillance efforts and availability of representative samples.
The global disease and health burden of transgender people remains understudied, particularly the impact of stigma, discrimination, violence, and other social and structural factors that affect the health of this underserved population, as well as interventions to mitigate stigma.
Despite substantial gaps in empirical research, there are sufficient actionable data highlighting unique biological, behavioral, social, and structural contextual factors surrounding health risks and resiliencies for transgender people that need interventions.
Consistency of definitions for health surveillance and research initiatives that include transgender people are essential, including dedicated funding to support these efforts.
APPENDIX
Table I.
Non-Standardized Operationalizations of “Transgender” (n=95 Definitions) Across 116 Studies.
| # | Definition of Transgender (and subpopulation focus if within-group data) |
|---|---|
| 1 | assigned male at birth but subsequently did not regard themselves as “completely male” in all situations or roles |
| 2 | Transgender adults |
| 3 | Participants reporting “often” or “very often” to the item “I wish I was the opposite sex” |
| 4 | responded “transgender” or “other (specify)” to the survey question “What is your gender?” |
| 5 | DSM-IV-TR criteria for GID |
| 6 | transgender women |
| 7 | answered “transgender” to the survey |
| 8 | any person who believed her male biological sex assigned at birth was in conflict with her gender identity as a transwoman |
| 9 | Identifying as transgender |
| 10 | Transgender |
| 11 | self-identified as a transgender woman |
| 12 | Two-step method of measuring natal sex/gender status |
| 13 | self-identified transgender or transsexual woman |
| 14 | self identified as transgender (defined as transsexual, crossdresser/transvestite, drag queen/king, or other transgender) |
| 15 | self-identified MtF transsexual (21), MtF cross-dresser (22) |
| 16 | patients from 1992–2012 with a diagnosis of GID, not yet in hormone treatment or undergone reassignment surgery |
| 17 | self-identified as male-to-female or transfemale |
| 18 | self-identified male-to-female, male-to-other, female-to-male, and female-to-other |
| 19 | all self-identified transgender women, regardless of stage of gender transition |
| 20 | assigned male sex at birth, but assume a feminine gender expression or identity |
| 21 | suspected or diagnosed GID |
| 22 | diagnosis of gender dysphoria by ICD-10 criteria |
| 23 | Trans GB-MSM, who are defined as trans men who had indicated they had a sexual minority identity and were not exclusively attracted to cis women |
| 24 | gender identity disorder |
| 25 | self-identified as male-to-female or female-to-male for gender identity |
| 26 | self-identified transwoman |
| 27 | Transgender men |
| 28 | “gender diverse” (self-identified as either transgender or gender queer) |
| 29 | (1) were born or assigned female at birth; (2) self-identified as male or along the transmasculine spectrum |
| 30 | Hijra |
| 31 | Male to female transsexuals on cross-sex hormones |
| 32 | GID diagnosis |
| 33 | self identified as transgender |
| 34 | self-identified as a transgender woman or not identifying with assigned male birth gender |
| 35 | criteria for early- or late-onset gender identity disorder |
| 36 | Identified as transwomen |
| 37 | Individuals with GID seeking sexual reassignment surgery |
| 38 | Transgender persons |
| 39 | All persons diagnosed with GID at the Center for Sexology and Gender Problems at the Ghent University Hospital (Ghent, Belgium) between 1986 and June 2012 and who underwent at least 3 months of cross-sex hormone therapy |
| 40 | assigned male gender at birth but identifying as a woman |
| 41 | Diagnosis of gender identity disorder according to DSM-IV |
| 42 | Male to female transgender youth |
| 43 | Transwomen |
| 44 | Discrepancy between a person’s psychological gender and the morphological, biological, and social sex, which is often perceived as “non-self” and belonging to the opposite sex |
| 45 | Participants were assigned a male gender at birth but identify as female and currently or previously identify as transgender |
| 46 | Hijras are the transgender individuals found in the Indian subcontinent, popularly known as the “third gender,” probably because these individuals do not conform to the conventional notions of male or female gender, but move between the two, challenging accepted gender definitions. |
| 47 | identifying as a transgender woman (categorized as male sex at birth but identify as a woman) |
| 48 | self-identified as transgender |
| 49 | self-identified as transgender/gender-queer |
| 50 | TGs were enrolled based on their outward characteristics from sex-work venues and cabaret show theaters |
| 51 | Trans people |
| 52 | Transgender individuals are persons whose gender identity differs from their biological sex |
| 53 | Transgender, gender nonconforming, and other gender youth |
| 54 | Wide variety of trans identities |
| 55 | self identify on questionnaire: “Do you think you are transgender?” |
| 56 | Transgender females |
| 57 | transgender person |
| 58 | transgendered subject enters into a relationship with medical, psychotherapeutic, and juridical institutions in order to gain access to certain hormonal and surgical technologies for enacting and embodying itself |
| 59 | Transvestite |
| 60 | transvestites, transsexuals, and transgender |
| 61 | VHA users from FY2009 with at least one diagnosis of GID |
| 62 | All self identified transgender types (e.g. transsexuals, cross-dressers, and so on) |
| 63 | biologically male at birth, self-identified as a woman, 16 or older |
| 64 | children and adolescents referred to the Gender Identity Clinic and diagnosed with gender identity disorder |
| 65 | diagnosis of transsexualism |
| 66 | Female to male transsexuals on cross-sex hormones |
| 67 | Hijra sex workers |
| 68 | identify within the umbrella of transgender |
| 69 | Male sex at birth that self-identify as females |
| 70 | Male to female transsexuals who have undergone sexual reassignment surgery |
| 71 | self identified as transgender or “other” in response to gender |
| 72 | self identify on questionnaire: “Are you transgender?” |
| 73 | self-identified as transgender, transsexual, and/or female with a biological or birth sex of male |
| 74 | Self-report HIV negative transgender women with anal or oral intercourse with a male or transgender woman partner in the previous 12 months |
| 75 | assigned a female sex at birth who identify as male, man, or genderqueer |
| 76 | Biological males who idenitifed as female or transgender for at least the previous three months, and reported sexual activity (oral and/or anal sex) with men in the same time period |
| 77 | Diagnosis of gender identity disorder by a mental health professional |
| 78 | formal diagnosis of GD/GID |
| 79 | HIV infected transgender men on HAART |
| 80 | Male to female transgender |
| 81 | male to female transgenders who have not had sexual reassignment surgery |
| 82 | Participants who self-identified as transgender, queer, or questioning on a survey item about their gender identity |
| 83 | Self identification of an internal gender identity different from the one assigned at birth |
| 84 | self identified as transgender on survey |
| 85 | self identify on questionnaire: “Do you identify as transgender/gender-nonconforming?” |
| 86 | Self-identified FTM transgender persons |
| 87 | self-identified MTF transsexual |
| 88 | self-identify as transsexual |
| 89 | self-identifying as a transwoman or feminine-identified/male-born person |
| 90 | Transgender MSM |
| 91 | Female to male transsexuals prior to cross-sex hormone therapy |
| 92 | Transgender individuals |
| 93 | Transgender women: born male, express female identity |
| 94 | Female to male transmasculine adults |
| 95 | Transsexuals |
Table II.
Methodological Overview of Transgender Health Study Designs as Reported by Study Authors (n=116 studies).
| Column A | Column B | Column C | |||
|---|---|---|---|---|---|
| Study Design | # Studies | Sampling Method | # Studies | Measures of Association | # Studies |
| Cross-sectional | 90 | Clinic-based recruitment (gender dysphoric participants) and internet-based recruitment (controls) | 29 | Prevalence | 95 |
| Prospective cohort | 7 | Internet-based or online recruitment | 17 | Age-standardized prevalence | 1 |
| Repeated cross sectional survey | 2 | Approached through trans organizations, referrals from venues, and internet advertisements | 6 | RDS-weighted prevalence | 3 |
| Pre post intervention design | 2 | Probability-based sampling | 3 | Standardized Mortality Ratio (SMR) | 1 |
| Randomized controlled efficacy trial | 1 | Respondent-driven sampling | 8 | Period prevalence (per 100,000 patients) | 3 |
| Retrospective chart review, case review, case series, case records | 11 | Recruitment from transgender events and conferences, or LGBT events including Pride Festivals | 7 | Incidence rate | 4 |
| Retrospective cohort | 2 | Not Specified | 4 | Cases/1000 persons | 1 |
| Case-control | 1 | Purposive community sampling | 4 | Risk ratio | 1 |
| Recruited from HIV-prevention program or outreach | 3 | Odds ratio | 7 | ||
| Convenience sample | 2 | Adjusted Odds Ratio | 16 | ||
| Peer outreach and snowball sampling | 2 | Unadjusted conditional odds | 1 | ||
| Venue-based sampling | 2 | Adjusted conditional odds | 1 | ||
| Snowball sampling | 2 | Hazard ratio | 2 | ||
| Snowball sampling and quota sampling | 1 | Beta (regression coefficient) | 7 | ||
| Snowball sampling, listservs, and websites | 1 | Point-biserial correlations | 1 | ||
| Brief-intercept sampling | 1 | Contrast estimate | 1 | ||
| Recruitment letter to students | 1 | Median | 1 | ||
| Organization-based recruitment | 1 | Mean score | 4 | ||
| Clinic-based, venue-based, peer outreach and referral | 1 | Chi square | 2 | ||
| Random sample from prison census | 1 | t-test | 2 | ||
| Random sample of selected gurus with all associated hijiras | 1 | MANOVA | 1 | ||
| Clinic service case records | 2 | Pearson’s correlation | 1 | ||
| HIV/STD Surveillance Registries | 1 | ||||
| Clinic and location-based recruitment | 1 | ||||
| School-based | 1 | ||||
| Randomly selected high-schools | 1 | ||||
| Venue-day-time sampling | 1 | ||||
| Census | 1 | ||||
| Clinic-based recruitment and peer referral | 1 | ||||
| Community agency-based recruitment | 1 | ||||
| Peer referral | 2 | ||||
| Snowball/chain referral and venue based | 1 | ||||
| Argentine Union of Sexual Workers registration | 1 | ||||
| Community and internet-based | 1 | ||||
| GSA organization-based recruitment | 1 | ||||
| Venue-based sampling and incentivized snowball sampling | 1 | ||||
| Consecutive clinic referral | 1 | ||||
| Internet and peer referral | 1 | ||||
Table III.
Mental Health Outcomes in Transgender Health Research (n=303 Mental Health Data Points).
| Classification: | # Data Points | % |
|---|---|---|
| Mood Disorders (depression, dysthymia, bipolar) | 96 | 31.6 |
| Suicidal and Non-Suicidal Self-Injury (suicide ideation, suicide attempt, self-harm without lethal intent) | 50 | 16.5 |
| Anxiety Disorders (generalized anxiety, PTSD, phobias, OCD) | 44 | 14.5 |
| General Distress and Wellbeing (Psychological Distress, Personal Wellbeing Index) | 25 | 8.3 |
| Somatoform Disorders (Body Dysmorphic Disorders, Somatization) | 17 | 5.6 |
| Schizophrenia and Other Psychotic Disorders | 11 | 3.7 |
| Other Mental Health Issues (grief and loss, loneliness, relationship problems) | 10 | 3.3 |
| Personality Disorders (schizoid, borderline, antisocial) | 10 | 3.3 |
| Impulse Control Disorders Not Elsewhere Classified (Intermittent Explosive Disorder, pathological gambling) | 8 | 2.7 |
| Other Mental Health Diagnosis Not Specified (Other Axis 1 Diagnosis) | 8 | 2.7 |
| Dissociative Disorders | 7 | 2.4 |
| Sleep Disorders | 7 | 2.4 |
| Pervasive Developmental Disorders (Autism, Asperger’s) | 4 | 1.4 |
| Eating Disorders (Anorexia Nervosa) | 3 | 1.0 |
| Attention-Deficit and Disruptive Behavior Disorders (Conduct Disorder) | 3 | 1.0 |
Percent exceeds 100% due to rounding.
Figure I.
Sexual and Reproductive Health Outcomes in Transgender Health Research (n=219 Data Points).+
+Author Note: Studies that reported HIV and STI data were coded in the “HIV” category. “STI-related” indicates studies reporting only on STIs.
Table IV.
Substance Use Outcomes in Transgender Health Research (n=193 Data Points).
| Substance Use Outcome | # Data Points | % |
|---|---|---|
| Alcohol Use | 35 | 18.2 |
| Marijuana | 25 | 13.0 |
| Any Illicit Drug Use (Type Not Specified) | 16 | 8.3 |
| Tobacco Use | 14 | 7.3 |
| Cocaine | 14 | 7.3 |
| Methamphetamine | 11 | 5.7 |
| Injection Drug Use (IDU) | 11 | 5.7 |
| Any Substance Use | 10 | 5.2 |
| Heroin | 9 | 4.7 |
| Substance Abuse, Dependence, Disorder | 10 | 5.2 |
| Crack | 7 | 3.7 |
| Substance Use to Cope | 5 | 2.6 |
| Inhalents (Amyl Nitrate, poppers) | 3 | 1.6 |
| Downers | 3 | 1.6 |
| Ecstasy | 3 | 1.6 |
| Hallucinogens | 3 | 1.6 |
| Morality Due to Illicit Drug Use | 2 | 1.1 |
| Stimulant use (Type Not Specified) | 2 | 1.1 |
| Painkiller | 2 | 1.1 |
| Polysubstance Use | 2 | 1.1 |
| Club Drugs | 1 | 0.6 |
| GHB | 1 | 0.6 |
| Steroids | 1 | 0.6 |
| “Other” Recreational Drug Use | 1 | 0.6 |
| Prescription Medication Use | 1 | 0.6 |
| Poly-Drug Use | 1 | 0.6 |
Percent exceeds 100% due to rounding.
Figure II.
Violence/Victimization in Transgender Health Research (n=105 Data Points).
Table V.
General Health Outcomes in Transgender Research (n=68 Data Points).
| General Health Indicator (40 total unique general health indicators) | # Data Points |
|---|---|
| Diabetes | 8 |
| Hormone Use (4 on previous 30 days, 3 on non-prescribed, 1 on injected hormones) | 8 |
| Obesity | 5 |
| Metabolic syndrome (ATP-III) | 3 |
| Asthma | 2 |
| Cancer | 2 |
| Dyslipidemia | 2 |
| Familial hypercolesterolemia | 2 |
| General medical condition co-morbidity | 2 |
| Hypertension | 2 |
| Mortality External causes | 2 |
| Venous thrombosis and/or pulmonary embolism | 2 |
| All cause mortality | 1 |
| Arthritis | 1 |
| Blood pressure | 1 |
| Cardiovascular mortality | 1 |
| Chronic pain | 1 |
| Cryptorchidism | 1 |
| Digestive problems | 1 |
| Disability | 1 |
| Hearing | 1 |
| High cholesterol | 1 |
| Hyperandrogenism | 1 |
| Hypercolesterolemia | 1 |
| Hyperprolactinemia | 1 |
| Idiopathic hyperadrogenemia | 1 |
| Kidney problems | 1 |
| Lung problems | 1 |
| Metabolic syndrome (IDF) | 1 |
| Mortality Ischemic heart disease | 1 |
| Mortality Malignant neoplasm: Digestive tract | 1 |
| Mortality Malignant neoplasm: Hematological | 1 |
| Mortality Malignant neoplasm: Lung | 1 |
| Mortality Unknown cause | 1 |
| Myocardial infarction | 1 |
| Nonclassic adrenal hyperplasia | 1 |
| Primary hypogonadism | 1 |
| Secondary hypogonadism | 1 |
| Transient ischemic attack; cerebrovascular disease | 1 |
| Vision problems | 1 |
Sidebar: Gender Affirmation is Multi-Level.
Gender affirmation is not just individual-level—it is a concept that can be applied to healthcare systems and structural, macro-level factors through a social ecological model.26 For example, gender affirming healthcare refers to care that is sensitive, responsive, and affirming to people’s genders. Healthcare systems and models of care need to consider social, psychological, medical, and legal dimensions of people’s lives in delivery of care.
Sidebar: Gender Affirmation and Health and Human Rights.
Gender affirmation is a human right.27,28 According to Sevelius (2013), outcomes from lacking gender affirmation can take the form of violence (including sexual violence), experiences of discrimination, and harassment.8 The International Covenant on Civil and Political Rights adopted in 1966 by the United Nations General Assembly, with170 state parties, has been a foundation of global human rights law,29 with the main objective that “all peoples have the right of self-determination,” the right to human dignity, and equality under the law. Two decades prior, in 1948 United Nations adopted the Universal Declaration of Human Rights (UDHR), widely recognized as one of the most influential statements on human rights.30 The 2011 Annual report of the United Nations High Commissioner for Human Rights and reports of the Office of the High Commissioner and the Secretary-General acknowledges that transgender people experience high rates of violence, discrimination and denial of rights as a result of their gender identity or expression.31 The UN report further describes instances of discriminatory laws including state-sponsored violence against transgender people across the globe.
Despite clear inclusion of transgender people in the UN, nations outside the UN, the Vatican, the Organization of Islamic Cooperation, and the United States have routinely opposed global measures to protect sexual orientation and gender identity.32 In the United States, only eighteen states plus the District of Columbia have non-discrimination policies, and eight states have interpreted these protections to prohibit discrimination of transition-related healthcare in private and/or state-sponsored health insurance.33 In contrast, as early as 1972, Sweden became the first in the world to allow transgender people to legally change their gender, and access accessible hormone therapy. In a more sweeping decision, in 2006, the European Union recast its definition of sex equality to include transgender people,34 whereby it was formerly only implicitly covered via legal precedent. With denial of human rights leading to discrimination, stress, sexual risk-taking, codified gender affirmation may result in reduced discrimination, and better health outcomes for transgender and other gender minority people.32 Integrating health and human rights is essential for transgender public health.35,36
Sidebar: A Call for Health Equity.
Health differences are not necessarily inequities.37–39 In a social determinants of health framework, health inequities involve a health difference produced by injustice or social oppression—by a power differential between groups with less disadvantage compared to groups with advantage. Documenting and understanding population-level health inequities by transgender status necessitates having comparative data. Without comparative data, it is inaccurate to state that “transgender people are disproportionately burdened by or experience an inequity in depression.” A study consisting of a sample of exclusively transgender people allows examination of within-group health indicators. Thus, findings can indicate that “transgender people bear a high burden of depression” or that “depression is highly prevalent among transgender people sampled.” Without a comparison group, such within-group data are not sufficient evidence of a health inequity per say (particularly when prevalence estimates are not age-adjusted). Monitoring health inequities requires comparative data to understand the distribution of disease in transgender people relative to non-transgender people, as well as the opportunity to unpack the mechanisms and pathways (i.e., mediators and potential intervention points) that cause poor health differentially by gender identity.
Sidebar: Sex and Gender as Social Determinants of Population Health.
Understanding sex and gender pathways to health means attending to the biological, psychological, social, structural, and behavioral dimensions that shape embodied sex and gender differences—assigned sex at birth, gender identity, gender expression, embodiment, gender roles, and other relevant dimensions that may influence individual health and wellbeing and contribute to population-level health inequities. Gender is multidimensional.40 Gender pathways to health are multilevel, socio-historically and culturally-dependent, and dynamically change over time. Dimensions of gender affect people’s health and wellbeing at multiple levels of influence.41 Understanding gender as a population determinant of health for ALL people, means not only conceptualizing and measuring different dimensions of gender—including the gendering of the actual material body itself—but also considering the dynamic nature of gender, including that: 1) sex and gender are not the same, a distinction particularly important in examining transgender people’s health;42 2) gender is relational (i.e., “a person’s gender is not simply an aspect of what one is, but, more fundamentally, it is something that one does, and does recurrently, in interaction with others” (p. 140);43 and 3) gender is fundamental to the social structuring of power and privilege.44,45 A social ecological model integrating gender analysis examines how sex and gender influence individual, interpersonal, organizational, community and public policy levels can shed light on sex- and gender-related embodiment pathways producing population-level health inequities.
Sidebar: Gender Minority Stress.
Building on social stress theories,46−49 a gender minority stress framework has been used to conceptualize adverse health outcomes that burden transgender people.50−52 This framework posits that experiences of social stress disproportionately affect transgender people relative to non-transgender people due to a disadvantaged social status and are largely responsible for health inequities. Such a framework integrates vulnerabilities at multiple levels of influence through which social processes become embedded in, and fundamentally shape, biological health outcomes. The distribution of power and capital along lines of gender as well as the social, economic, and psychological consequences of making visible the false conflation of sex and gender situate transgender people in stigmatized minority group. Stressors such as experiences of discrimination, stigma, violence and victimization, social and economic exclusion are all too common among transgender people.
Sidebar: Resilience: A Public Health Opportunity.
Health-promoting, salutogenic, and resilience-related factors that may be protective for health risks in transgender populations are grossly under-studied.53 Deficits-based models permeate existing public health research. Positive growth-fostering coping processes may mitigate health inequities by transgender status. Health promotion will benefit from integrating salutogenic and resilience-focused (i.e., strengths-based frameworks) into public health approaches for transgender people. Multi-level strategies that integrate evidence-based biomedical, behavioral, and structural interventions, and that attend to the gender minority stressors that lead to health risk and vulnerability, as well as resiliencies, are required to successfully address the health needs of transgender people.
References
- 1.IOM (Institute of Medicine). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Liao L-M, Simmonds M. A values-driven and evidence-based health care psychology for Diverse Sex Development. Psychology & Sexuality. 2014;5(1):83–101. [Google Scholar]
- 3.Council of Europe: Commissioner for Human Rights. Human Rights and Intersex People. Strasbourg: 2015. [Google Scholar]
- 4.European Union Agency for Fundamental Rights (FRA). The fundamental rights situation of intersex people 2015.
- 5.Swiss National Advisory Commission on Biomedical Ethics. On the management of differences of sex development: Ethical issues relating to “intersexuality”. Bern: 2012. [Google Scholar]
- 6.World Health Organization (WHO). Eliminating forced, coercive and otherwise involuntary sterilization: An interagency statement. Geneva, Switzerland: OHCHR, UN Women, UNAIDS, UNDP, UNFPA, UNICEF and WHO;2014. [Google Scholar]
- 7.World Health Organization (WHO). Sexual health, human rights and the law. Geneva, Switzerland: World Health Organization;2015. [Google Scholar]
- 8.Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex roles. 2013;68(11–12):675–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melendez RM, Pinto R. ‘It’s really a hard life’: Love, gender and HIV risk among male‐to‐female transgender persons. Culture, Health & Sexuality. 2007/05/01 2007;9(3):233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nuttbrock LA, Bockting WO, Hwahng S, et al. Gender identity affirmation among male-to-female transgender persons: a life course analysis across types of relationships and cultural/lifestyle factors. Sexual and Relationship Therapy. 2009/05/01 2009;24(2):108–125. [Google Scholar]
- 11.Bockting WO. Psychotherapy and the real-life experience: From gender dichotomy to gender diversity. Sexologies. 2008;17:211–224. [Google Scholar]
- 12.Bockting WO. Transforming the paradigm of transgender health: A field in transition. Sexual and Relationship Therapy. 2009;24(2):103–107. [Google Scholar]
- 13.Reisner SL, Conron KJ, Scout N, Mimiaga MJ, Haneuse S, Austin SB. Comparing In-Person and Online Survey Respondents in the U.S. National Transgender Discrimination Survey: Implications for Transgender Health Research LGBT Health. 2014;1(2):98–106. [DOI] [PubMed] [Google Scholar]
- 14.Gates GJ. How many people are lesbian, gay, bisexual and transgender?: The Williams Institute; April 2011. [Google Scholar]
- 15.Van Kesteren PJ, Gooren LJ, Megens JA. An epidemiological and demographic study of transsexuals in the Netherlands. Archives of sexual behavior. 1996;25(6):589–600. [DOI] [PubMed] [Google Scholar]
- 16.United States Census Bureau. U.S. World and Population Clock. 2014; http://www.census.gov/popclock/. Accessed October 10, 2014.
- 17.Sausa LA, Sevelius J, Keatley J, Iñiguez JR, Reyes M. Policy Recommendations for Inclusive Data Collection of Trans People in HIV Prevention, Care & Services. 2009; http://www.transhealth.ucsf.edu/trans?page=lib-data-collection.
- 18.Cahill S, Singal R, Grasson C, et al. Do ask, do tell: High levels of acceptability by patients of routine data collection of sexual orientation and gender identity data in hour diverse American community health centers PLos One. 2014;9(9):e107104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The GenIUSS Group. Best Practices for Asking Questions to Identify Transgender and Other Gender Minority Respondents on Population-Based Surveys. In: Herman JL, ed. Los Angeles, CA: The Williams Institute; 2014: http://williamsinstitute.law.ucla.edu/wp-content/uploads/geniuss-report-sep-2014.pdf. [Google Scholar]
- 20.Reisner SL, Biello K, Rosenberger JG, et al. Using a two-step method to measure transgender identity in Latin America/the Caribbean, Portugal, and Spain. Arch Sex Behav. November 2014;43(8):1503–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc. Jul-Aug 2013;20(4):700–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB. Monitoring the health of transgender and other gender minority populations: Validity of natal sex and gender identity survey items in a U.S. national cohort of young adults. BMC Public Health. 2014;14:1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pan American Health Organization (PAHO). Guidelines for gender-based analysis of health data for decision making 2008.
- 24.World Health Organization (WHO). Gender analysis in health: A review of selected tools. Geenva, Switzerland: Department of Gender and Women’s Health, World Health Organization (WHO);2002. [Google Scholar]
- 25.Clougherty JE. A growing role for gender analysis in air pollution epidemiology. Environmental health perspectives. February 2010;118(2):167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.International Commission of Jurists and International Service for Human Rights. The Yogyakarta Principles: Principles on the Application of International Human Rights Law in Relation to Sexual Orientation and Gender Identity 2007.
- 28.Baral SD, Beyrer C, Poteat T Human Rights, the Law, and HIV among Transgender People. Working Paper prepared for the Third Meeting of the Technical Advisory Group of the Global Commission on HIV and the Law2011. [Google Scholar]
- 29.Hoag RW. International Covenant on Civil and Political Rights Encyclopedia of Global Justice: Springer; 2011:544–545. [Google Scholar]
- 30.Universal Declaration of Human Rights, (1948).
- 31.Human Rights Council. Discriminatory laws and practices and acts of violence against individuals based on their sexual orientation and gender identity: United Nations General Assembly; November 17 2011. [Google Scholar]
- 32.Marks SM. Global Recognition of Human Rights for Lesbian, Gay, Bisexual, and Transgender People. Health and Human Rights. 2006;9(1):33–42. [PMC free article] [PubMed] [Google Scholar]
- 33.Reisner SL, White JM, Dunham EE, Heflin K, Begenyi J, Cahill S. Discrimination and Health in Massachusetts: A Statewide Survey of Transgender and Gender NonConforming Adults. Boston MA: The Fenway Instiute;2014. [Google Scholar]
- 34.Directive 2006/54/EC of the European Parliament and of the Council of 5 July 2006 on the implementation of the principle of equal opportunities and equal treatment of men and women in matters of employment and occupation (recast). Official Journal of the European Union. L 204 ed. European Union 2006:23–36. [Google Scholar]
- 35.United Nationas Development Programme (UNDP). Discussion Paper: Transgender Health and Human Rights New York: HIV, Health and Development Group, Bureau of Development Policy, United Nations Development Programme (UNDP),;2013. [Google Scholar]
- 36.Open Society Foundations (OSF). Transforming Health: International Rights-Based Advocacy for Trans Health. New York, NY: Public Health Program, Open Society Foundations (OSF);2013. [Google Scholar]
- 37.Braveman P What are health disparities and health equity? We need to be clear. Public Health Rep. Jan-Feb 2014;129 Suppl 2:5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Braveman P Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194. [DOI] [PubMed] [Google Scholar]
- 39.Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. American journal of public health. December 2011;101 Suppl 1:S149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Conron KJ, Landers SJ, Reisner SL, Sell RL. Sex and gender in the US health surveillance system: a call to action. American journal of public health. June 2014;104(6):970–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrant G The Multidimensional Gender Inequalities Index (MGII): A Descriptive Analysis of Gender Inequalities Using MCA. Social Indicators Research. 2014;115(2):653–690. [Google Scholar]
- 42.Genders Krieger N., sexes, and health: what are the connections--and why does it matter? Int J Epidemiol. August 2003;32(4):652–657. [DOI] [PubMed] [Google Scholar]
- 43.West C, Zimmerman DH. Doing Gender Gender & Society. 1987;1(2):125–151. [Google Scholar]
- 44.Courtenay WH. Constructions of masculinity and their influence on men’s well-being: a theory of gender and health. Soc Sci Med. May 2000;50(10):1385–1401. [DOI] [PubMed] [Google Scholar]
- 45.Connell RW. Gender and power: Society, the person and sexual politics. Stanford, CA: Stanford University Press; 1987. [Google Scholar]
- 46.Meyer IH. Minority stress and mental health in gay men. Journal of health and social behavior. March 1995;36(1):38–56. [PubMed] [Google Scholar]
- 47.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin. September 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. Journal of health and social behavior. June 2005;46(2):205–219. [DOI] [PubMed] [Google Scholar]
- 49.Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. May 2013;103(5):943–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice. 2012;43(5):460–467. [Google Scholar]
- 51.Reisner S, Greytak E, Parsons J, Ybarra M. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. The Journal of Sex Research. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reisner SL, Gamarel KE, Nemoto T, Operarior D. Dyadic effects of gender minority stressors in substance use behaviors among transgender women and their non-transgender male sex partners. Psychology of Sexual Orientation and Gender Diversity. 2014;1(1):63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Poteat T, Reisner SL, Radix A. HIV epidemics among transgender women. Curr Opin HIV AIDS. March 2014;9(2):168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 1.IOM (Institute of Medicine). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Open Society Foundations (OSF). Transforming Health: International Rights-Based Advocacy for Trans Health. New York, NY: Public Health Program, Open Society Foundations (OSF);2013. [Google Scholar]
- 3.Gender Identity in U.S. Surveillance (GenIUSS) Group. Best Practices for Asking Questions to Identify Transgender and Other Gender Minority Respondents on Population-Based Surveys. Los Angeles: The Williams Institute at the UCLA School of Law;2014. [Google Scholar]
- 4.Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. The Lancet. Infectious diseases. March 2013;13(3):214–222. [DOI] [PubMed] [Google Scholar]
- 5.Reisner SL, Bailey Z, Sevelius J. Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the U.S. Women & health. 2014;54(8):750–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations. Report of the United Nations High Commissioner for Human Rights, Discriminatory laws and practices and acts of violence against individuals based on their sexual orientation and gender identity, A/HRC/22/53 United Nations;2011. [Google Scholar]
- 7.Callens N, De Cuypere G, Van Hoecke E, et al. Sexual quality of life after hormonal and surgical treatment, including phalloplasty, in men with micropenis: a review. The journal of sexual medicine. December 2013;10(12):2890–2903. [DOI] [PubMed] [Google Scholar]
- 8.Horbach SE, Bouman MB, Smit JM, Ozer M, Buncamper ME, Mullender MG. Outcome of Vaginoplasty in Male-to-Female Transgenders: A Systematic Review of Surgical Techniques. The journal of sexual medicine. June 2015;12(6):1499–1512. [DOI] [PubMed] [Google Scholar]
- 9.Charmaz K Constructing grounded theory: A practical guide through qualitative analysis. London, UK: Sage Publications Ltd; 2006. [Google Scholar]
- 10.Bockting WO. Transforming the paradigm of transgender health: A field in transition. Sexual and Relationship Therapy. 2009;24(2):103–107. [Google Scholar]
- 11.Nemoto T, Bodeker B, Iwamoto M, Sakata M. Practices of receptive and insertive anal sex among transgender women in relation to partner types, sociocultural factors, and background variables. AIDS Care. April 2014;26(4):434–440. [DOI] [PubMed] [Google Scholar]
- 12.Nuttbrock L, Bockting W, Rosenblum A, et al. Gender abuse, depressive symptoms, and HIV and other sexually transmitted infections among male-to-female transgender persons: a three-year prospective study. Am J Public Health. February 2013;103(2):300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Vries AL, Doreleijers TA, Steensma TD, Cohen-Kettenis PT. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry. November 2011;52(11):1195–1202. [DOI] [PubMed] [Google Scholar]
- 14.Pitts MK, Couch M, Mulcare H, Crow S, Mitchell A. Transgender people in Australia and New Zealand: health, well-being and access to health services. Feminism & Psychology. 2009;19(4):475–495. [Google Scholar]
- 15.Pfeffer CA. Bodies in relation--bodies in transition: Lesbian partners of t rans men and body image. Journal of Lesbian Studies. 2008;12(4):325–345. [DOI] [PubMed] [Google Scholar]
- 16.Robinson BE, Bockting WO, Rosser BRS, Miner M, Coleman E The Sexual Health Model: Application fo a sexological approach to HIV prevention. Health Educ Res. 2002;17(1):43–57. [DOI] [PubMed] [Google Scholar]
- 17.Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice. 2012;43(5):460–467. [Google Scholar]
- 18.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51(1s):s28–s40. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization (WHO). Closing the gap in a generation: Health equity through action on the social determinants of health, Final Report of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization (WHO); 2008: http://www.who.int/social_determinants/thecommission/finalreport/en/. Accessed February 22, 2014. [Google Scholar]
- 20.Braveman P Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194. [DOI] [PubMed] [Google Scholar]
- 21.Braveman P, Gruskin S. Defining equity in health. Journal of epidemiology and community health. April 2003;57(4):254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO). Handbook of health inequality monitoring with a special focus on low- and middle-income countries. Geneva, Switzerland: World Health Organization;2013. [Google Scholar]
- 23.Reisner SL, Biello K, Rosenberger JG, et al. Using a Two-Step Method to Measure Transgender Identity in Latin America/the Caribbean, Portugal, and Spain. Arch Sex Behav. July 17 2014;43(8):1503–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sausa LA, Sevelius J, Keatley J, Iñiguez JR, Reyes M. Policy Recommendations for Inclusive Data Collection of Trans People in HIV Prevention, Care & Services. San Francisco, CA: Center of Excellence for Transgender HIV Prevention, University of California, San Francisco;2009. [Google Scholar]
- 25.Tate CC, Ledbetter JN, Youssef CP. A two-question method for assessing gender categories in the social and medical sciences. J Sex Res. 2013;50(8):767–776. [DOI] [PubMed] [Google Scholar]
- 26.Genders Krieger N., sexes, and health: what are the connections--and why does it matter? Int J Epidemiol. August 2003;32(4):652–657. [DOI] [PubMed] [Google Scholar]
- 27.Vlassoff C Gender differences in determinants and consequences of health and illness. J Health Popul Nutr. March 2007;25(1):47–61. [PMC free article] [PubMed] [Google Scholar]
- 28.Nieuwenhoven L, Klinge I. Scientific excellence in applying sex- and gender-sensitive methods in biomedical and health research. J Womens Health (Larchmt). February 2010;19(2):313–321. [DOI] [PubMed] [Google Scholar]
- 29.Nowatzki N, Grant KR. Sex is not enough: the need for gender-based analysis in health research. Health Care Women Int. April 2011;32(4):263–277. [DOI] [PubMed] [Google Scholar]
- 30.Sex Doyal L. and gender: the challenges for epidemiologists. Int J Health Serv. 2003;33(3):569–579. [DOI] [PubMed] [Google Scholar]
- 31.Sex Doyal L., gender, and health: the need for a new approach. BMJ. November 3 2001;323(7320):1061–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex Roles. June 1 2013;68(11–12):675–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reisner S, Greytak E, Parsons J, Ybarra M. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. The Journal of Sex Research. 2015;52(3):243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. May 2013;103(5):943–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Operario D, Nemoto T. HIV in transgender communities: Syndemic dynamics and a need for multicomponent interventions. J Acquir Immune Defic Syndr. 2010;55(s2):s91–s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gruskin S, Bogecho D, Ferguson L. ‘Rights-based approaches’ to health policies and programs: Articulations, ambiguities, and assessment. J Public Health Policy. 2010;31(2):129–145. [DOI] [PubMed] [Google Scholar]
- 38.Clougherty JE. A growing role for gender analysis in air pollution epidemiology. Environmental health perspectives. February 2010;118(2):167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan American Health Organization (PAHO). Guidelines for gender-based analysis of health data for decision making 2008.
- 40.World Health Organization (WHO). Gender analysis in health: A review of selected tools. Geenva, Switzerland: Department of Gender and Women’s Health, World Health Organization (WHO);2002. [Google Scholar]
- 41.Connell RW. Gender and power: Society, the person and sexual politics. Stanford, CA: Stanford University Press; 1987. [Google Scholar]
- 42.Connell RW. Gender: In World Perspective. Cambridge, UK: Polity; 2009. [Google Scholar]
- 43.Link BG, Phelan JC. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- 44.Link BG, Phelan JC. Understanding sociodemographic differences in health--The role of fundamental social causes American Journal of Public Health. 1996;86(4):471–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baral SD, Beyrer C, Poteat T Human Rights, the Law, and HIV among Transgender People. Working Paper prepared for the Third Meeting of the Technical Advisory Group of the Global Commission on HIV and the Law 2011.
- 46.International Commission of Jurists and International Service for Human Rights. The Yogyakarta Principles: Principles on the Application of International Human Rights Law in Relation to Sexual Orientation and Gender Identity 2007. [Google Scholar]
- 47.O’Flaherty M, Fisher J. Sexual Orientation, Gender Identity and International Human Rights Law: Contextualising the Yogyakarta Principles. Human Rights Law Review 2008;8(2):207–248. [Google Scholar]
- 48.World Health Organization (WHO). Transgender People and HIV: Policy Brief. Geneva, Switzerland: World Health Organization;2015. [Google Scholar]
- 49.World Professional Association for Transgender Health (WPATH). Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. 2012; http://www.wpath.org/site_page.cfm?pk_association_webpage_menu=1351.
- 50.Coleman E, Bockting W, Botzer M, et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. International Journal of Transgenderism. 2011;13:165–232. [Google Scholar]
- 51.Global Action for Trans* Equality (GATE). English Translation of Argentina’s Gender Identity Law as approved by teh Senate of Argentina on may 8, 2012. 2012; http://globaltransaction.files.wordpress.com/2012/05/argentina-gender-identity-law.pdf. Accessed January 20, 2015.
- 52.Madon T, Hofman KJ, Kupfer L, Glass RI. Public health. Implementation science. Science. December 14 2007;318(5857):1728–1729. [DOI] [PubMed] [Google Scholar]
- 53.Daly J, Willis K, Small R, et al. A hierarchy of evidence for assessing qualitative health research. Journal of clinical epidemiology. January 2007;60(1):43–49. [DOI] [PubMed] [Google Scholar]
- 54.Leys M Health care policy: qualitative evidence and health technology assessment. Health policy. September 2003;65(3):217–226. [DOI] [PubMed] [Google Scholar]
- 55.Smedley BD, Syme SL. Promoting health: intervention strategies from social and behavioral research. Am J Health Promot. Jan-Feb 2001;15(3):149–166. [DOI] [PubMed] [Google Scholar]
- 56.Wallerstein NB, Yen IH, Syme SL. Integration of social epidemiology and community-engaged interventions to improve health equity. Am J Public Health. May 2011;101(5):822–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leung MW, Yen IH, Minkler M. Community based participatory research: a promising approach for increasing epidemiology’s relevance in the 21st century. Int J Epidemiol. June 2004;33(3):499–506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.