Abstract
Objective
To explore the causes and consequences of non-urgent visits to emergency departments in Iran and then suggest solutions from the healthcare providers’ viewpoint.
Design
Qualitative descriptive study with in-depth, open-ended, and semistructured interviews, which were inductively analysed using qualitative content analysis.
Setting
A territorial, educational and military hospital in Iran.
Participants
Eleven healthcare providers including eight nurses, two emergency medicine specialists and one emergency medicine resident.
Results
Three overarching themes of causes and consequences of non-urgent visits to the emergency department in addition to four suggested solutions were identified. The causes have encompassed the specialised services in emergency department, demand-side factors, and supply-side factors. The consequences have been categorised into three overarching themes including the negative consequences on patients, healthcare providers and emergency departments as well as the health system in general. The possible solutions for limiting and controlling non-urgent visits also involved regulatory plans, awareness-raising plans, reforms in payment mechanisms, and organisational arrangements.
Conclusion
We highlighted the need for special attention to the appropriate use of emergency departments in Iran as a middle-income country. According to the complex nature of emergency departments and in order to control and prevent non-urgent visits, it can be suggested that policy-makers should design and implement a combination of the possible solutions.
Keywords: accident & emergency medicine, qualitative research, health services administration & management
Strengths and limitations of this study.
This study is the first study which qualitatively explored the causes and consequences of non-urgent visits in Iran and other low-and-middle-income countries and suggested solutions to treat the arising problems.
The semistructured, in-depth and open-ended interviews with key informants allowed us to gather data from different perspectives.
This study did not include patients and then their perspectives were not considered in the proposed solutions.
Introduction
Emergency departments (EDs) are designed to provide rapid, high-quality, continuously accessible, and unscheduled care to emergency cases.1 2 It means that EDs are not ideal place for caring the non-urgent (NU) conditions.3 Patients with NU conditions are those patients who do not have life-threatening problems, nor require rapid care, their care can be safely delayed,4 and this delay would not increase the likely adverse outcomes.5 It is estimated that about one-third of patients who visit EDs have NU problems, which can potentially be addressed by the outpatient departments, primary care settings, and mobile centres.6 7 Some studies have reported even up to half of all visits to EDs are NU visits8, and the differences in these studies can be due to the various methodologies used in defining NU visits.9 Recently, the misuse of EDs by NU patients has been reported globally.6 10–13 This misuse has potentially negative consequences including overcrowding, increased costs, poor healthcare quality, lack of continuity of care, and timely urgent care for urgent and semiurgent (USU) patients in addition to the incidence of medical errors.14–16
Causes of NU visits are not clearly understood,17 especially in the low-and-middle-income countries. To the best of our knowledge, there is no comprehensive study to identify causes and consequences of that problem in Iran, as a middle-income country. Therefore, this study was conducted to determine the causes, consequences of NU visits to EDs from the healthcare providers’ viewpoint and then suggest solutions in the light of their perspectives.
Description of Iranian healthcare system
Iran has a unique model of medical education in which healthcare services and medical education have been integrated since 1985 under the supervision of Ministry of Health and Medical Education (MOHME). The healthcare network has been established and expanded by MOHME throughout the country aiming at reducing inequities, reaching universal coverage, and increasing access to healthcare services particularly in the deprived and rural areas. By achieving its goals, WHO has acknowledged this network as an incredible masterpiece and model of success.18 19 Although the normal flow of healthcare services is from the primary healthcare to secondary and tertiary hospitals, patients tend to bypass it and refer directly to the outpatient departments in the secondary and tertiary hospitals and healthcare centres, which in turn reflects the weak referral system in Iran.20 21
Methods
Design
Using a qualitative descriptive design,22 we held in-depth, open-ended, and semi-structured interviews to explore the experiences and perspectives of physicians and nurses working in the ED. Qualitative interviews give respondents the opportunity in order to discuss the topic of interest in a way that may not be anticipated by the study researchers.23 Face-to-face interview also ensures the effective discussion of information between the researchers and interviewees. Basically, the study protocol, methods and materials, and interview guide were reviewed and approved by the Research Committee of Baqiyatallah University of Medical Sciences. The Canadian Triage and Acuity Scale was used to sort the visits to the ED in which levels 4 and 5 had been considered as NU visits according to this scale.
Setting, recruitment, and sampling
The studied hospital, one of the largest in Tehran, is a territorial, military, and teaching hospital with 700 available beds. Its accreditation grade was one excellent, according to the most recent national accreditation undertaken by the MOHME. The ED provides 24-hours emergency care for all patients and successfully runs a residency programme for emergency medicine specialists (EMS). In each working shift in the ED, there are two EMSs, 10–15 nurses, and 4–5 nurse aides. The researchers used a combination of snowball and purposeful sampling methods to recruit key informants from among the healthcare providers working in the ED. Through which, nurses (n=8), EMSs (n=2) and emergency medicine resident (n=1) had been selected.
Data collection
The potential key informants were invited after the verbal informed consent was obtained from all participants and the confidentiality of their responses was assured. The researchers have asked the key informants about their viewpoints about the causes and consequences of NU visits to EDs and the possible solutions to be implemented. At the end of interviews, further questions were also asked about the discussion process and all related topics were checked whether they had been covered or not. One of the researchers (SMM) interviewed all key informants within the ED. The recruitment of new key informants continued until thematic/data saturation where no additional information nor new ideas could be developed.
Data analysis
All interviews were recorded by the written notes, transcribed verbatim, rechecked for more accuracy and entered into MAXQDA software in order to perform qualitative data management and analysis. By using inductive qualitative content analysis, we extracted and organised significant themes through internal discussion among the research team. Qualitative content analysis is a well-established method, which allows different levels of deep interpretation.24 Key steps of analysis include25 : preparing, organising and reporting. The data were discussed collaboratively in three virtual meetings among the research team through which discrepancies had been discussed till reaching consensus on thorough and consistent coding.
In this study, two criteria had to be met in order to prove trustworthiness: credibility and transferability.26 Credibility refers to the believability of the data and whether the findings are faithfully linked to the real descriptions provided by the participants.26 To enhance the credibility of findings, we used a wide range of key informants to capture deep information about the research questions. Regarding the transferability, it should be noted that the local context may influence the findings27; therefore, we clearly described the study setting and context, selection process, and characteristics of key informants in addition to the methods of data collection and analysis. Moreover, we appropriately presented the findings and selected quotations based on consensus in order to enhance transferability.24
The quotes, which had corresponded the different themes and subthemes, were selected, translated from Persian to English, then read, checked and evaluated by the team to ensure accuracy and fluency. Generally translation was literal meanwhile the specific Persian idioms, which were not easy to translate, were altered by native English speakers in the research team for more fair content, and bilingual team members have checked for confirming the accuracy. Any potential misinterpretations were clarified and agreed on. Original quotes are available on reasonable request.
In the light of study aim and objectives, verbal informed consents were obtained from all participants before conducting the interviews.
Patients and public involvement
Patients and public were not involved in the research design, recruitment or conducting this study.
Results
We identified three overarching themes for causes and consequences of NU visits to EDs in addition to four solutions for NU visits to EDs.
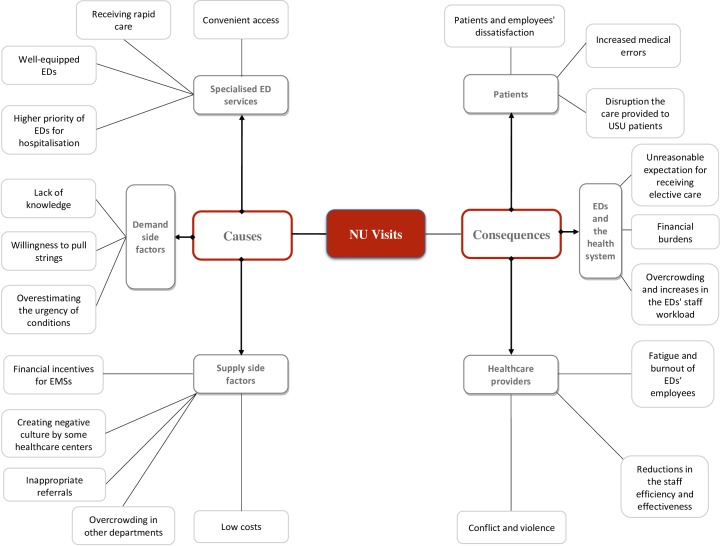
The causes included the specialised services provided in ED, demand-side factors, and supply-side factors. It is worth noting that the specialised ED services involve convenient access, receiving rapid care, well-equipped EDs, and higher priority EDs for hospitalisation. Demand-side factors are the factors, which are related to service users (ie, patients referred to EDs). In other words, they are the factors, which encourage patients to refer to EDs, including lack of knowledge, willingness to pull strings, and overestimating the urgency of their conditions. Pulling strings is a term means making use of one’s influence and contacts to gain an advantage unofficially or unfairly. Supply-side factors were also those factors related to service providers and directly affect the NU visits embracing the financial incentives for EMSs, creating negative culture by some healthcare center, inappropriate referrals, overcrowding in other departments, and low costs (figure 1).
Figure 1.
Themes of causes and consequences of NU visits. ED, emergency department; EMSs, emergency medicine specialists; NU, non-urgent; USU, urgent and semiurgent.
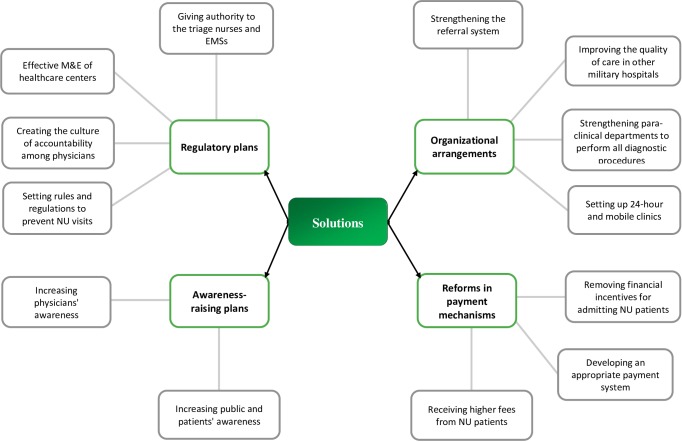
The consequences of NU visits were categorised into three overarching themes including the negative consequences on patients, healthcare providers, and EDs as well as the health system in general. The possible solutions for limiting and controlling NU visits also encompassed regulatory plans, awareness-raising plans, reforms in payment mechanism, and organisational arrangements (figure 2). The detailed descriptions of each theme are as follows:
Figure 2.
Possible solutions for limiting and controlling NU visits to EDs. ED, emergency department; EMSs, emergency medicine specialists; M&E, monitoring and evaluation; NU, non-urgent.
Causes
Specialised ED services
Convenient access
Because the ED provides healthcare services 24-hours all the week, patients access is relatively higher, better, and easier than outpatient departments and other healthcare centres.
The idea implanted in people minds is that access to EDs is easier than other healthcare centers and it can make their admission easier [P1, a triage nurse].
EDs are open all the time while the access to other health centers is limited to specific hours [P8, a nurse].
Receiving rapid care
Due to the nature of EDs, prompt diagnostic and therapeutic services should be provided. This was not neglected by the participants and they acknowledged the quick care as a reason for NU visits.
Patients come to the ED to receive rapid care and consultations. For example, if we ourselves (the personnel) want to make an appointment with a rheumatologist, it will take us month but for the ED’s patients, it will be faster [P4, a nurse].
The delay in the clinics’ workflow is a cause of NU visits to the ED. Meanwhile, providing care such as lung consultation occurs promptly [P10, a nurse].
Well-equipped EDs
Having all diagnostic facilities as well as skilled personnel in EDs were one of the reasons that had been stated by the participants.
In addition to EMSs, other specialists are available in the ED [P6, a nurse].
Focus on patients is prioritised in the ED in which all diagnostic procedures and facilities are available. But if a patient goes to a physician's office and then has been asked to do a CT-Scan, the patient will go to the CT-Scan center and then if the same patient has been recommended to perform MRI, the patient should go through another process. In general, the patient is assured that physicians, nurses and other staff are well-trained as well as all necessary equipment are available in the ED [P8, a nurse].
Higher priority of EDs for hospitalisation
One of the main ED’s roles is admitting patients and referring them to inpatient departments more than other departments such as inpatient admission unit and clinics. Thus, patients tend to go to EDs to be admitted to inpatient departments directly or to remain in the ED until having a space in case of overcrowded inpatient departments.
Some NU patients occupy ED beds until having a space in inpatient departments [P4, a nurse].
In addition to prompt care, the ED has a priority over other departments with regards to admission and patients have higher priority to be admitted and referred to other departments as well [P8, a nurse].
Demand-side factors
Lack of knowledge
Lack of patients' knowledge and awareness towards the definition of urgent conditions negatively affects NU visits to EDs. This is due to lack of influential role of mass media in addition to the formation of negative culture.
The main factor is the knowledge of our people. They do not have sufficient knowledge. The mass media don’t provide enough information for the community about this issue [P2, an EMS].
However, another interviewee believed that:
A small percentage of patients do not know that they are urgent or not [P5, an EMS resident].
Also, lack of awareness about the main duties of clinics in providing care to the NU patients can be another cause.
People are not aware of the duties of some departments such as clinics [P11, a triage nurse].
Willingness to pull strings
Willingness to pull strings was one of the causes that participants mentioned during the interviews.
We had a patient came to the ED and said he is a close friend to Mr. X who told him to come to the ED and said don’t worry, the personnel will deal with your illness sooner [P9, a triage nurse].
There was another type of pulling the strings:
Having kinship relationships is important. For example, patients bring a letter from the hospital's technical officer or other managers in order to facilitate their admission to the ED. The monitoring and evaluation (M&E) office at this hospital also may inform the ED staff to allow patients admission till specific time, for example, evening, and then to refer them to other departments [P10, a nurse].
Overestimating the urgency of conditions
Some patients seek refuge to several ways for being admitted to EDs. One of these unwise ways is to exaggerate the severity and urgency of suffered conditions.
Some of patients exaggerate illnesses and severity of their conditions as an attempt to convince the staff about providing them the necessary care in the ED [P5, an EMS resident].
Supply-side factors
Financial incentives for EMSs
Participants declared that EMSs’ fee-for-service (FFS) payment is an important factor which is associated with the admission of NU patients thereby depending on the number of admitted patients. In other words, there is a direct financial relationship between patient's admission to EDs and the increases in EMSs’ income in Iran.
There is a financial relationship between the number of patients admitted to the ED and specialist's FFS payment. Some of the EMSs in the screening room have been previous medical students of senior physicians. One a day, one of these EMSs showed me a text message in which a senior physician in the ED in that day asking him to let patients enter the ED [P10, a nurse].
Creating negative culture by some healthcare centres
Previous referrals of patients to some healthcare centres, especially private centres, have a significant effect on their current NU visits to EDs. That is because patients have received unnecessary services in these private centres in order to accomplish unfair profit from those patients.
Private hospitals encourage this behavior in which unnecessary services are provided which in turn created this patients’ mentality that leads to NU visits to EDs in order to get some services according to their desire. As a result, negative attitude of patients has been formed especially when they seek care at public hospitals in which they expect to receive similar services as happened at the private ones [P2, an EMS].
Inappropriate referrals
Referring the NU patients to EDs, either verbally or by written form, common. Some physicians who do not have beds at their hospital departments often do not feel accountability and easily refer patients to the ED. It should be noted that this is rooted in some physicians as a sort of profiteering or at least to keep their patients. Physicians are not willing to lose their patients and then urge them to come to their own private offices or to the private hospital where they are working at through which referring those patients to the ED.
We have a lot of patients to whom their physicians gave two letters: one for the hospital admission officer and the other one for the ED. The physicians also tell the patients to go first to the admission officer and if he/she doesn't respond, they can go to the ED with the second letter [P10, a nurse].
Not only physicians refer patients inappropriately but also some other hospitals do the same using ambulance without any coordination. Moreover, some other employees such as secretaries and security guards within the health sector, hospitals in particular, may also advise patients to receive care in the ED.
Patients are referred in a bad manner. Employees such as secretaries and security guards encourage patients to refer to the ED. We have patients from other towns who visit the clinics and they are recommended by some other employees to refer to the ED because of the limited number of patients on clinics’ lists and in order to avoid their disturbances [P9, a triage nurse].
Overcrowding in other departments
Overcrowding in other departments such as outpatient clinics and admission department is an important cause of NU visits to EDs. Overcrowding in the clinics wanders patients and they inevitably go to the ED. Importantly, patients from other provinces also used to come to this hospital as it is famous for its high-quality services.
Departments and clinics are overcrowded, so patients choose the ED to receive care especially when they travel for a long time and can’t wait patiently [P5, an EMS resident].
Low costs
All inpatient services are free of charge for some patients, hence they will endeavour to be hospitalised in any way in order to considerably reduce their costs.
To pay less … their services will be free of charge if they are hospitalized but this is not the case for outpatient services [P6, a nurse].
Patients usually come to the ED … as soon as the patient's record is set, they will not pay for rendered services [P8, a nurse].
Consequences
Negative consequences on patients
Patients and employees’ dissatisfaction
NU visits to EDs result in dissatisfaction of both patients and healthcare providers. In addition, decelerating the workflow of procedures in EDs will lead to dissatisfaction in both NU and USU patients. In USU patients, dissatisfaction can be due to the lack of timely delivery of care.
With NU visits, the satisfaction decreases [P5, an EMS resident].
In addition, problems caused by crowding and the arising complaints from patients also lead to dissatisfaction and may be burnout of ED’s staff as well as.
NU patients themselves became pessimistic about the system because they think that they are trying for nothing. If they are not admitted to the ED, they say that they have been disrespected, and they will complain to hospital managers [P9, a triage nurse].
Increased medical errors
Since the given time for providing care in EDs is too short for diagnosis and assessment the cases, the quality of care would decrease and this may raise the probability of medical errors. These are some of the consequences of increasing NU visits.
When the ED is crowded by NU visits, the physicians spend less time with the single patient. Therefore, quality, monitoring and also follow-up of patients will decrease [P8, a nurse].
Disruption the care provided to USU patients
NU visits to EDs would hinder the provision of care to truly USU patients. This is often happens as a result of lacking the knowledge and awareness of the seriousness of USU circumstances which may be aggravated because of the increase in NU visits. In other words, the lesser NU visits, the lesser the crowding, the more available time and effort for USU cases.
Whenever the department isn't crowded, the whole work is getting faster and the patients will receive care faster. In this ED, there was a patient suffering cardiovascular problems, the time he came the department wasn't crowded so we did an electrocardiogram test once for him without observing any problem. When we repeated the test again, a serious problem has been discovered and immediately managed. Sometimes, crowding and the available time is a matter of life or death [P4, a nurse].
If we want to admit the NU patients, we will oppress the urgent patients [P9, a triage nurse].
One participant had an awful experience:
The real urgent patients are not dealt with. We had a patient suffering myocardial infarction, he was taken for doing angiography two hours after his arrival to the ED meanwhile his golden time was only 30 min [P10, a nurse].
Negative consequences on EDs and the health system
Unreasonable expectation for receiving elective care
When they are admitted to ED, NU patients expect receiving elective care according to their desire as they think that their situation is also urgent. Therefore, they start to ask for several treatment procedures.
NU visits lead to unreasonable expectation of elective services. When these patients are admitted to the ED, they ask for different procedures. For example, we had a patient with low back pain and constantly was asking: when will I do my Magnetic Resonance Image (MRI)? [P3, a nurse].
Financial burdens
Every patient admitted to EDs needs more specialised staff, equipment, medicines, fluids, laboratory tests, imaging. However, receiving necessary care in outpatient departments will be at lower costs. Therefore, NU visits impose additional financial burdens on the healthcare centre and the health system in general as well.
NU visits might yield in squandering hospital resources as a result of overuse. For instance, blood testing is a routine procedure in the ED for the vast majority of admitted patients. However, some of those patients will be discharged on the behalf of the specialist before getting the laboratory results. This means misuse and wastage of the scarce materials [P10, a nurse].
NU visits can result in imposing extra costs on the ED and health insurance organisations through which any patient admitted to the ED needs at least a secretary, nurse, nurse assistant and equipment, while this patient could be treated simply in the outpatient clinic [P3, a nurse].
Overcrowding and increases in the EDs' staff workload
It is inevitable that EDs would be overcrowded due to the excess in NU visits which potentially raise the workload of EDs’ staff:
This has a negative effect on the load of the ED’s staff, and it can slow down work and disorganize duties [P6, a nurse].
NU visits might lead to unreasonable crowding and disrupt the accurate triage [P8, a nurse].
Negative consequences on healthcare providers
Fatigue and burnout of EDs’ employees
The huge number of NU visits to EDs is critical especially when we shed light on the supply side, that is, healthcare providers, for whom NU visits will be accountable for their fatigue and burnout.
NU visits raise the tension among personnel, because of overload and the attention which should be paid to all patients, NU and USU [P1, a triage nurse].
They cause burnout [P5, an EMS resident].
Reductions in the staff efficiency and effectiveness
NU visits reduce the efficiency and effectiveness of ED’s staff.
As an obstacle, NU visits hinder the quality assurance of the work and this could reflected negatively on the performance of the staff [P1, a triage nurse].
They can diminish nurses’ performance and proficiency [P8, a nurse].
Conflict and violence
One of the crucial risks of NU visits is the creation of tension and conflict between patients and providers or between the staff members themselves. At the time in which patients’ expectations magnify, employees cannot properly meet these expectations because of work overload, and this creates stress and conflict.
NU visits can lead to physical violence. Providers can’t provide appropriate services while patients expect to receive perfect care [P5, an EMS resident].
Solutions
In our study, the participants proposed different solutions for limiting and controlling NU visits. These solutions can be categorised into four groups; regulatory plans, awareness-raising plans, reforms in payment mechanisms, and organisational arrangements.
Regulatory plans include: giving authority to the triage nurses and EMSs, creating the culture of accountability among physicians, effective M&E of healthcare centres, and setting rules and regulations to prevent NU visits. Awareness-raising plans encompass: increasing the awareness of public, patients and physicians as well. Reforms in payment mechanisms include: removal of financial incentives for admitting NU patients, developing an appropriate payment system, and hiking the fees for NU cases. Organisational arrangements embrace: setting up 24-hours and mobile clinics, improving the quality of care in other military hospitals, strengthening paraclinical departments to perform all diagnostic procedures, and strengthening the referral system.
Regulatory plans
Giving authority to the triage nurses and EMSs
The triage nurses and EMSs should be delegated with a real authority, which could give them the ability to guide and refer NU patients properly.
EMSs and nurses should be given power to refuse admission of NU patients [P6, a nurse].
A triage nurse should be supported and allowed to refer NU visits to the outpatient clinics [P8, a nurse].
Creating the culture of accountability among physicians
Creating and developing the culture which implant the feeling of accountability among physicians for referring and admitting patients to EDs is considered an important approach. This can contribute in raising physicians’ sensitivity towards referrals as well as admission of NU patients to EDs:
The accountability perspective among physicians should be enhanced [P1, a triage nurse].
Effective M&E of healthcare centres
In order to avoid healthcare centres profiteering which in turn forces the people to search for another way to get the service and this may be carried out inappropriately such as NU visits. An interviewee stated that:
M&E of healthcare centers in the private sector should be increased to prevent profiteering against patients … this is helpful in reducing NU visits to the ED [P2, an EMS].
Setting rules and regulations to prevent NU visits
Implementation of strong and inflexible rules and regulations is also a suitable way in preventing or at least reducing NU visits.
Rules and regulations should be set properly to prevent such these visits [P2, an EMS].
Another solution is to enforce immutable rules for those who want to be admitted to the ED through personal relationships [P2, an EMS].
Awareness-raising plans
Increasing public and patients’ awareness
The community should be aware of USU and NU conditions through promoting their awareness in the schools, social networks, mass media, and in EDs as well:
Information should be provided to patients through the mass media but this is not used properly. For example, some TV series show that everything in the EDs is ideal which inspires people to go for receiving the desired care. Unfortunately, this isn’t realistic [P1, a triage nurse].
Also people should be informed about the difference between early and late visits to the EDs and the consequences of both of each.
We need to teach people the consequences of early and late visits for receiving services through the mass media [P2, an EMS].
People have to understand that EDs are not a place for NU patients [P8, a nurse].
Creating a culture about that should be all the time. We tell our colleagues that admitting a patient to the ED for once means admitting all forever [P11, a triage nurse].
Increasing physicians’ awareness
The EMSs should be advised to refrain from admitting NU patients to EDs under any circumstances:
EMSs see the ED empty in some hours and just for that reason they say let NU patients be admitted [P3, a nurse].
The awareness of physicians who don't work in EDs should be raised because some of them try to get rid of patients and refer them to the ED [P1, a triage nurse].
Reforms in payment mechanisms
Removing financial incentives for admitting NU patients
As mentioned in the causes section, financial incentives for physicians have negative effects on admitting NU patients to EDs. Admission of patients to the EDs should be irrelevant to physicians’ income and this could be inverted effectively on improving quality of care provided by the physicians. Nonetheless, policy-makers have to look carefully at the role of incentives in motivating the physicians towards rendering the essential services to patients perfectly:
There should be no relationship between the physicians' income and the hospital admission rate in the ED [P1, a triage nurse].
Developing an appropriate payment system
The reform of payment system was a solution that the interviewees mentioned. Since physicians often have a motivation for admitting patients who have NU problems because this has no significant effect on their income, compared with those with acute conditions, and therefore, they prefer to admit patients with more stable conditions, which has a great effect on the NU visits.
The policies of a health care system should be tailored … the patient who needs more care should pay more money [P2, an EMS].
Receiving higher fees from NU patients
When the patients come to the ED with the idea that receiving urgent services in EDs for NU cases costs more fees than that in other healthcare centres such as clinics, para-clinics, they will not prefer EDs for receiving care and this has it’s consequent effect on reducing the number of NU visits to the ED in both short-term as well as long-term period.
NU patients who come to the ED should pay fees from 30% to 40% of total costs [P9, a triage nurse].
In order to prevent NU visits, more fees should be paid by NU patients who visit the ED [P6, a nurse].
Organisational arrangements
Setting up 24-hour and mobile clinics
Setting up a 24-hour and mobile clinics was also one of the solutions to which some interviewees referred.
The 24-hours health centers should be set up. Clinics are just open for up to 23:00 … Any patient has any problem, for example, sore throat, will come to the ED directly [P1, a triage nurse].
Some of interviewees were not agreed on the establishment of 24-hours clinics. One of them stated that:
Establishing like these clinics are not reasonable because they are not cost-effective [P3, a nurse].
Also, we should consider high burden of visits in some days of the year.
The clinics should be developed and expanded in order to fit for more patients. During some annual occasions and events, the number of people increases in some places within the country which requires more facilities for providing health services, that is, 24-hours and mobile clinics. We could visit the patients in the morning or even in the evening [P9, a triage nurse].
Nevertheless, studies are recommended for determining the volume of visits, referrals and the need for setting up specialised clinics are essential in order to support evidence-based decisions.
Taking turns in the clinics should be strengthened. There is a need to study in this regard, for example, how many neurosurgery patients have referred to the clinic. Night shifts in the clinic should be managed by the new graduates and I think they will also welcome that [P10, a nurse].
Improving the quality of care in other military hospitals
Improving quality of care rendered by other military healthcare centres and hospitals can reduce NU visits in the long run.
Strengthening paraclinical departments to perform all diagnostic procedures
The clinic should be strengthened to perform all diagnostic procedures in order to diminish the referred patients to EDs.
The para-clinical system should be strengthened and all diagnostic procedures, such as sonography, should be performed. Para-clinical system shouldn't refer patients to the hospital itself, so it should be strengthened in terms of time, number of visits and personnel. This will lead to patient’s confidence [P8, a nurse].
We had a successful experience, that is, setting up the wounds clinic in which patients with bedsores, diabetics, etc. have visited. With establishing this clinic, NU visits to the ED have significantly been decreased [P10, a nurse].
Strengthening the referral system
Justifying and rationalising the referrals from clinics to EDs is another solution, to which the interviewees referred:
Referrals from clinics to EDs should be rational, and this depends on the patient's culture [P8, a nurse].
Furthermore, it is important to boost the referral system and implement the family physician programme across the country, through which it is expected that NU cases are easily handled by the family physicians.
Discussion
The aim of our study was to explore the causes and consequences of NU visits to EDs in Iran and then suggest solutions from the healthcare providers’ perspectives. The results showed that NU visits to EDs had several causes with negative consequences. We identified three overarching themes of causes and consequences NU visits to EDs and four subsequent solutions.
In this study, the causes of NU visits were categorised into three themes including specialised ED services, demand-side factors, and supply-side factors. Consequences were also categorised into three themes: negative consequences on patients, healthcare providers, EDs and the health system. In addition, potential solutions for limiting and controlling NU visits were classified into four themes encompassing regulatory plans, awareness-raising plans, reforms in payment mechanisms, and organisational arrangements. In this section, the results of our study has been discussed and compared with previous studies.
The good accessibility, the well-equipped EDs, the high-quality care provided there were among the reasons for increased NU visits, which have been addressed in other studies.28 29 In some studies, lack of access to family physicians has been reported as a reason for NU visits to EDs.30 31 Although the family physician programme in Iran has been implemented since more than 10 years, it did not become nationwide.
Our study showed that patients prefer to approach to well-equipped centres in order to receive the required care, and this was consistent by another study.32 Developing paraclinical departments to perform all diagnostic procedures can reduce the number of NU visits in addition to conducting need assessment studies and determining the importance of setting up 24-hours and mobile clinics. Improving the referral system and the quality of care provided by other centres can also help in control and reduction of NU visits in the long run.
Tendency to use the beds of EDs temporarily for admitting to the hospital inpatient departments is one of the causes of NU visits. To the best of our knowledge and based on the literature review, we did not find studies that focused on addressing such these problems. This misuse of EDs’ beds till finding a space for the admitted patients can lead to negative consequences on USU patients and result in financial burdens on the health system as well as health insurance organisations. Like this wastage of resources requires decisive actions from healthcare managers and policy-makers.
With regard to our results, low costs which paid by patients might be another reason and this was in line with the results of preceding studies.33 34 It is recommended to hike the fees of services which are provided to NU patients who visit EDs. Crowding in other healthcare centres, for example, clinics and physicians’ offices, encourages patients to visit EDs for receiving faster care and this also corresponds other studies conducted in several countries such as in Iran,33 Turkey,35 Jordan,36 France37 and the USA.38
Financial incentives given to EMSs was an important cause. In 1991, the FFS payment policy was proposed by the Minister of Health and Medical Education and was approved by the Cabinet.39 The evidence showed that this policy had negative consequences such as providing unnecessary services and admitting more patients and, consequently, imposing additional financial burdens on the health system. The adverse effects of this plan on EDs are also evident, one of which can be the admission of NU patients. Special attention should be paid by healthcare managers and policy-makers to reforming the payment mechanisms without linking the physicians’ income to patients’ admission. The FFS plan has more negative effects on the behaviour of physicians and on the behaviour of private centres. So, patients in the private centres could undertake a lot of tests, images and take several medicines and this in turn yield in creating an inconvenient culture through expecting receiving similar healthcare services in public hospitals. Therefore, monitoring physicians’ behaviour in addition to that of private centres should be performed in order to avoid their profiteering.
Lack of patients’ knowledge and awareness of the urgent conditions for referral to EDs has also been revealed by other studies.40–44 The design and implementation of awareness-raising plans in EDs as well as in the mass media, schools and universities, social networks, clinics and healthcare centres can help in promoting the knowledge and awareness of patients and community in general.
NU referrals recommended by clinics’ physicians, secretaries and security guards have also its adverse effects, which had been discovered by studies in the literature.43 45 46 To overcome such referrals, a combination of awareness-raising plans for physicians and other healthcare professionals, empowering triage nurses and EMSs, creating culture of accountability among physicians, and setting rules and regulations to deny NU visits should be considered. Taking punitive measures can be effective against those who try to use kinship relationships and pull strings to admit patients to EDs. This study showed that patients’ exaggeration of the severity of their illness in order to be admitted is one of the reasons of NU visits to EDs, and this was consistent with other studies.47 48 This matter can be resolved by educating physicians, triage nurses, patients and caregivers, and increasing public awareness. In the awareness-raising plans, the negative effects of NU visits should be well addressed, so that patients become aware of the adverse effects of such visits. This can act as a factor in reducing NU visits.
Designing and implementing of clinical guidelines in EDs is one of the issues that unfortunately have not been considered in Iran. Most physicians are reluctant to use available guidelines. Interestingly, it also seems that senior policy-makers are less willing to design and implement guidelines in EDs.
It is suggested to do some researches in order to appraise the influence of incentives and punitive rules, improve payment mechanisms, develop patients and providers’ awareness-raising plans, and identify factors which affect overcrowding in healthcare centres and EDs. Further quantitative studies should be conducted to determine the consequences of NU visits on crowding and overcrowding in EDs.
Strengths and limitation
This study has been conducted as the first qualitative study in Iran for determining causes and consequences of NU visits, as well as for suggesting possible solutions for preventing such visits, which are the strengths of this study. In the present study, expert EMSs and nurses who had in the ED had been also interviewed.
Interviews were only from healthcare providers’ perspective while patients were not included. Another prospective study to explore the causes of NU visits from the patients’ perspectives is recommended through conducting a qualitative study. Another limitation was the inability of digital recording of interviews due to the refusal of ED’s head. However, it was overcome by taking notes during the interviews.
Conclusion
NU visits to EDs have undesirable consequences on patients, providers and on the health system as well. It is suggested that national policy-makers should design and implement a combination of solutions categorised into four groups of regulatory plans, awareness-raising plans, reforms in payment mechanisms, and organisational arrangements. As a long-term strategy, improving the referral system and expanding the family physician programme across the country should be considered as a national priority. For the first time in Iran, it is the first study which has proposed solutions for NU visits to EDs. This could be beneficial for evidence-informed policy as well as decision making.
Supplementary Material
Acknowledgments
We are grateful to Iyad Shaqura (PhD candidate, Department of Health Management and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran) for his assistance in editing the language of this article.
Footnotes
Contributors: SMM was responsible for the conception, design, implementation, analysis, drafting the manuscript and supervision of the whole process of the study. MB is the principal researcher, who was involved in the conception, development, implementation, data collection, data analysis and writing the manuscript. ET and RR were responsible for the intellectual development of the manuscript. All authors have read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The approval for this study was obtained from the Ethics Research Committee at Baqiyatallah University of Medical Sciences (Ref: IR.BMSU.REC.1394.271).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. Gonçalves-Bradley D, Khangura JK, Flodgren G, et al. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev 2018;311 10.1002/14651858.CD002097.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ieraci S, Cunningham P, Talbot-Stern J, et al. Emergency medicine and "acute" general practice: comparing apples with oranges. Aust Health Rev 2000;23:152–61. 10.1071/AH000152 [DOI] [PubMed] [Google Scholar]
- 3. Weisz D, Gusmano MK, Wong G, et al. Emergency department use: a reflection of poor primary care access? Am J Manag Care 2015;21:e152–60. [PubMed] [Google Scholar]
- 4. Ng C-J, Liao P-J, Chang Y-C, et al. Predictive factors for hospitalization of nonurgent patients in the emergency department.. Medicine 2016;95:e4053 10.1097/MD.0000000000004053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Durand A-C, Gentile S, Devictor B, et al. Ed patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med 2011;29:333–45. 10.1016/j.ajem.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 6. O’Keeffe C, Mason S, Jacques R, et al. Characterising non-urgent users of the emergency department (ED): a retrospective analysis of routine ED data. PLoS One 2018;13:e0192855 10.1371/journal.pone.0192855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 8. Bahadori M, Mousavi SM, Teymourzadeh E, et al. Emergency department visits for non-urgent conditions in Iran: a cross-sectional study. BMJ Open 2019;9:e030927 10.1136/bmjopen-2019-030927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McCormack LA, Jones SG, Coulter SL. Demographic factors influencing nonurgent emergency department utilization among a Medicaid population. Health Care Manag Sci 2017;20:395–402. 10.1007/s10729-016-9360-8 [DOI] [PubMed] [Google Scholar]
- 10. Gulacti U, Lok U, Celik M, et al. The ED use and non-urgent visits of elderly patients. Turk J Emerg Med 2016;16:141–5. 10.1016/j.tjem.2016.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yang HJ, Jeon W, Yang HJ, et al. The clinical differences between urgent visits and non-urgent visits in emergency department during the neonatal period. J Korean Med Sci 2017;32:1870–5. 10.3346/jkms.2017.32.11.1870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Williams RM. The costs of visits to emergency departments. N Engl J Med 1996;334:642–6. 10.1056/NEJM199603073341007 [DOI] [PubMed] [Google Scholar]
- 13. Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009;16:1–10. 10.1111/j.1553-2712.2008.00295.x [DOI] [PubMed] [Google Scholar]
- 14. Ohns MJ, Oliver-McNeil S, Nantais-Smith LM, et al. Nonurgent Use of the Emergency Department by Pediatric Patients: A Theory-Guided Approach for Primary and Acute Care Pediatric Nurse Practitioners. J Pediatr Health Care 2016;30:339–46. 10.1016/j.pedhc.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 15. Parry YK, Ullah S, Raftos J, et al. Deprivation and its impact on non-urgent paediatric emergency department use: are nurse practitioners the answer? J Adv Nurs 2016;72:99–106. 10.1111/jan.12810 [DOI] [PubMed] [Google Scholar]
- 16. Valent F, Busolin A. Distance to the pediatric emergency department and Nonurgent visits in Friuli Venezia Giulia, Italy. Pediatr Emerg Care 2018;34:193–7. 10.1097/PEC.0000000000000852 [DOI] [PubMed] [Google Scholar]
- 17. Atenstaedt R, Gregory J, Price-Jones C, et al. Why do patients with nonurgent conditions present to the emergency department despite the availability of alternative services? Eur J Emerg Med 2015;22:370–3. 10.1097/MEJ.0000000000000224 [DOI] [PubMed] [Google Scholar]
- 18. Tavassoli M. Iranian health houses open the door to primary care. Bull World Health Organ 2008;86:585–6. 10.2471/BLT.08.030808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mousavi SM, Sadeghifar J. Universal health coverage in Iran. Lancet Glob Health 2016;4:e305–6. 10.1016/S2214-109X(16)00068-1 [DOI] [PubMed] [Google Scholar]
- 20. Mehrdad R. Health system in Iran. JMAJ 2009;52:69–73. [Google Scholar]
- 21. Shahabi S, Fazlalizadeh H, Stedman J, et al. The impact of international economic sanctions on Iranian cancer healthcare. Health Policy 2015;119:1309–18. 10.1016/j.healthpol.2015.08.012 [DOI] [PubMed] [Google Scholar]
- 22. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 23. Ritchie J, Lewis J, Nicholls CM. Qualitative research practice: a guide for social science students and researchers. Sage, 2013. [Google Scholar]
- 24. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24:105–12. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 25. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 26. Lincoln YS, Guba EG, Pilotta JJ. Naturalistic inquiry. Sage, 1985: 438–9. 10.1016/0147-1767(85)90062-8 [DOI] [Google Scholar]
- 27. Sandberg M, Jakobsson U, Midlöv P, et al. Case management for frail older people – a qualitative study of receivers’ and providers’ experiences of a complex intervention. BMC Health Serv Res 2014;14:14 10.1186/1472-6963-14-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Boushy D, Dubinsky I. Primary care physician and patient factors that result in patients seeking emergency care in a hospital setting: the patient’s perspective. J Emerg Med 1999;17:405–12. 10.1016/S0736-4679(99)00015-3 [DOI] [PubMed] [Google Scholar]
- 29. Coleman P, Irons R, Nicholl J. Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency? Emerg Med J 2001;18:482–7. 10.1136/emj.18.6.482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Steele S, Anstett D, Milne WK. Rural emergency department use by CTAS IV and V patients. CJEM 2008;10:209–14. 10.1017/S1481803500010125 [DOI] [PubMed] [Google Scholar]
- 31. Unwin M, Kinsman L, Rigby S. Why are we waiting? Patients’ perspectives for accessing emergency department services with non-urgent complaints. Int Emerg Nurs 2016;29:3–8. 10.1016/j.ienj.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 32. Schmiedhofer M, Möckel M, Slagman A, et al. Patient motives behind low-acuity visits to the emergency department in Germany: a qualitative study comparing urban and rural sites. BMJ Open 2016;6:e013323 10.1136/bmjopen-2016-013323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jalili M, Shirani F, Hosseininejad M, et al. Emergency department Nonurgent visits in Iran: prevalence and associated factors. Am J Manag Care 2013;19:E1–8. [PubMed] [Google Scholar]
- 34. Northington WE, Brice JH, Zou B. Use of an emergency department by nonurgent patients. Am J Emerg Med 2005;23:131–7. 10.1016/j.ajem.2004.05.006 [DOI] [PubMed] [Google Scholar]
- 35. Idil H, Kilic TY, Toker İbrahim, et al. Non-Urgent adult patients in the emergency department: causes and patient characteristics. Turk J Emerg Med 2018;18:71–4. 10.1016/j.tjem.2017.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Al-Mherat A, Essalim A, Sahwehne B. Non-urgent visits among patients seen at the emergency department of King Hussein medical center. Journal of The Royal Medical Services 2014;21:38–44. 10.12816/0002577 [DOI] [Google Scholar]
- 37. Durand A-C, Palazzolo S, Tanti-Hardouin N, et al. Nonurgent patients in emergency departments: rational or irresponsible consumers? perceptions of professionals and patients. BMC Res Notes 2012;5:525 10.1186/1756-0500-5-525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Glover CM, Purim-Shem-Tov YA. Emergency department utilization: a qualitative analysis of Illinois medical home network patients. Journal of Health Disparities Research and Practice 2016;9:10. [Google Scholar]
- 39. Doshmangir L, Rashidian A, Jafari M, et al. Opening the black box: the experiences and lessons from the public hospitals autonomy policy in Iran. Arch Iran Med 2015;18:416–24. doi:0151807/AIM.005 [PubMed] [Google Scholar]
- 40. Baker DW, Stevens CD, Brook RH. Determinants of emergency department use by ambulatory patients at an urban public hospital. Ann Emerg Med 1995;25:311–6. 10.1016/S0196-0644(95)70285-7 [DOI] [PubMed] [Google Scholar]
- 41. Gentile S, Vignally P, Durand A-C, et al. Nonurgent patients in the emergency department? A French formula to prevent misuse. BMC Health Serv Res 2010;10 10.1186/1472-6963-10-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Masso M, Bezzina AJ, Siminski P, et al. Why patients attend emergency departments for conditions potentially appropriate for primary care: reasons given by patients and clinicians differ. Emergency Medicine Australasia 2007;19:333–40. 10.1111/j.1742-6723.2007.00968.x [DOI] [PubMed] [Google Scholar]
- 43. Redstone P, Vancura JL, Barry D, et al. Nonurgent use of the emergency department. J Ambul Care Manage 2008;31:370–6. 10.1097/01.JAC.0000336555.54460.fe [DOI] [PubMed] [Google Scholar]
- 44. Tsai JC-H, Liang Y-W, Pearson WS. Utilization of emergency department in patients with non-urgent medical problems: patient preference and emergency department convenience. J Formos Med Assoc 2010;109:533–42. 10.1016/S0929-6646(10)60088-5 [DOI] [PubMed] [Google Scholar]
- 45. Scherer M, Lühmann D, Kazek A, et al. Patients attending emergency departments: a cross-sectional study of Subjectively perceived treatment urgency and motivation for attending. Deutsches Ärzteblatt International 2017;114:645–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shesser R, Kirsch T, Smith J, et al. An analysis of emergency department use by patients with minor illness. Ann Emerg Med 1991;20:743–8. 10.1016/S0196-0644(05)80835-2 [DOI] [PubMed] [Google Scholar]
- 47. Kubicek K, Liu D, Beaudin C, et al. A profile of Nonurgent emergency department use in an urban pediatric hospital. Pediatr Emerg Care 2012;28:977–84. 10.1097/PEC.0b013e31826c9aab [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ruud SE, Hjortdahl P, Natvig B. Is it a matter of urgency? A survey of assessments by walk-in patients and doctors of the urgency level of their encounters at a general emergency outpatient clinic in Oslo, Norway. BMC Emerg Med 2016;16:22 10.1186/s12873-016-0086-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.