Abstract
Introduction: The objective of this study was to determine if use of an automated irrigation pump (AIP) during ureteroscopy (URS) and percutaneous nephrolithotomy (PCNL) affects circulating nurse labor, irrigation-related issues, and surgeon and nurse satisfaction when compared to manual hand pump (HP) irrigation.
Methods: Eighty consecutive adult patients undergoing unilateral URS or PCNL were prospectively randomized to irrigation with the HP or AIP. Preoperative pump setup time, intraoperative pump maintenance time, total pump time (setup+maintenance), and the number of irrigation-related concerns verbalized by the surgeon intraoperatively were recorded; postoperatively, surgeons and nurses rated their satisfaction with the irrigation system (1 = highly dissatisfied to 10 = highly satisfied).
Results: Eighty patients were enrolled (39 AIP and 41 HP); 51 patients underwent URS and 29 patients underwent PCNL. On univariate analysis, the AIP resulted in a significantly reduced total pump time for URS (2.9 vs 5.9 minutes) and PCNL (4.6 vs 33.9 minutes; p < 0.001). The number of irrigation-related concerns was significantly lower in the AIP group during URS (1.2 vs 2.8, p < 0.001), but not during PCNL (1.9 vs 4.0, p = 0.07). The AIP was associated with significantly higher nurse satisfaction during URS (9.2/10 vs 6.5/10, p < 0.001) and PCNL (9.4/10 vs 4.4/10, p = 0.001). There was no significant association between pump type and surgeon satisfaction. On multivariate analysis of URS cases controlling for body mass index and number of stones, use of the AIP was a predictor of total pump time <5 minutes (odds ratio 25.8, 95% confidence interval [CI] 4.0–165.4; p < 0.001) and favorable (8–10/10) nurse satisfaction rating (odds ratio 25.4, 95% CI 4.1–164.0; p < 0.001). Operative time, stone-free rate, and liters of irrigant used with the HP and AIP were similar.
Conclusions: During URS and PCNL, the AIP was associated with a significant reduction in irrigation pump time and higher nurse satisfaction.
Keywords: irrigation, percutaneous nephrolithotomy, ureteroscopy, urolithiasis, endoscopy
Introduction
During endourological stone procedures, consistent irrigation flow is essential for optimizing the endoscopic view. The use of an automated irrigation pump (AIP) provides more consistent flow than irrigation devices that rely on pressure from external compression, such as pressure infusion sleeves that are inflated manually.1,2 Manual hand pump (HP) infuser irrigation systems do not maintain steady pressure and flow continuously, as compression from the pressurized sleeve decreases as irrigation fluid leaves the infusion bag. In addition to a suboptimal endoscopic field of view, this inconsistent pressure and resulting drop in flow may result in circulating nurses' expending excess time and physical effort in trying to maintain the irrigation flow.
Prior studies have characterized the performance of a variety of manual3–5 and automated2,6–8 endoscopic irrigation systems used in endourology, but have failed to examine the labor and operating room (OR) efficiency associated with these different irrigation systems. The potential for enhanced OR efficiency is notable, given that OR procedures account for an estimated 40% of hospital costs and generate over 60% of hospital revenue.9
The objective of this study was to determine if the use of an AIP during ureteroscopy (URS) and percutaneous nephrolithotomy (PCNL) favorably affects circulating nurse labor, intraoperative irrigation-related issues, and surgeon and nurse satisfaction compared to a manual HP irrigation system.
Methods
Study design and subject population
This was a prospective, randomized study approved by the institutional review board; all patients provided written informed consent. Adult patients undergoing unilateral URS or PCNL were randomized to HP or AIP irrigation. The study was performed using the Karl Storz Flex Xc (Karl Storz SE and Co. KG, Tuttlingen, Germany) and dual lumen COBRA Vision (Richard Wolf Medical Instruments Corporation, Vernon Hills, IL) ureteroscopes. Two separate irrigation systems were used during PCNL: one for the ureteroscope and one for the rigid and flexible nephroscopes; only data pertaining to the nephroscope irrigation were recorded.
Irrigation equipment
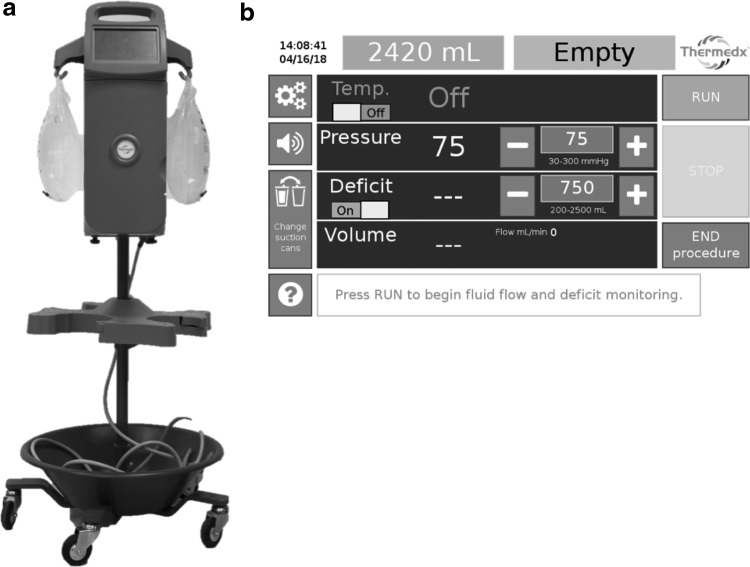
The Thermedx® FluidSmart® Fluid Management System (Richard Wolf Medical Instruments Corporation) (Fig. 1) is an AIP that automatically regulates irrigation pressure, flow, and temperature. The Thermedx pump exhibits accurate flow, pressure, and temperature data.7 Maximum infusion pressure with this AIP is 300 mm Hg.
FIG. 1.
(a) Thermedx® FluidSmart® Fluid Management System. (b) Thermedx touchscreen display.
The HP irrigation system (Infu-Surg® Pressure Infusion Bag; SunMed/Ethox) (Fig. 2) is a method for pressurizing the irrigant. It consists of a sleeve that fits around a 3000 mL bag of irrigation fluid. The user squeezes a handheld bulb pump to inflate the bladder within the sleeve, which exerts external pressure on the bag of irrigation fluid. The pressurized fluid then flows through a separate fluid-warming device (3M™ Ranger™ Irrigation Warming System, St. Paul, MN). The HP system can reach a maximum pressure of 300 mm Hg.
FIG. 2.
Hand pump infusion system (Infu-Surg® Pressure Infusion Bag; SunMed/Ethox).
Time and labor measurements
A dedicated independent observer equipped with a digital stopwatch served as the timekeeper. Operative time was recorded from the preoperative time-out to completion of closing. Preoperative pump setup time for the HP system included hanging of irrigation fluid bags on the irrigation tower, hand pumping the pressure infusion sleeves over the irrigation bags, connecting and priming the irrigation tubing, and preparing the fluid warming system. Pump setup time for the AIP included plugging the device into an electrical outlet, hanging the irrigation fluid bags, connecting and priming the irrigation tubing, and selecting the pressure setting.
Irrigation pump manipulation after the preoperative time-out and before completion of closing was recorded as intraoperative pump maintenance time (e.g., replacing irrigation fluid bags, additional hand pumping of pressure sleeves, or changing the pump pressure settings). Total pump time was calculated as the sum of the setup and maintenance times.
Surgeon and nurse satisfaction
The number of irrigation-related concerns verbalized by the surgeon during the case was recorded (e.g., complaints about flow or requests to increase irrigation pressure). After completion of the case, the primary operating surgeon and the primary circulating nurse assigned to irrigation pump maintenance recorded his/her satisfaction with the irrigation system (1 = highly dissatisfied to 10 = highly satisfied). Surveys were completed by 6 urologic surgeons and 28 nurses. During PCNL, irrigation-related concerns and satisfaction scores pertaining only to use of the nephroscope were recorded.
Statistical analysis
Primary outcome variables included irrigation pump setup and maintenance time, total pump time, number of irrigation-related concerns verbalized by the surgeon intraoperatively, and surgeon and nurse satisfaction scores. Secondary outcome variables included operative time, liters of irrigation fluid used, and stone-free rate on postoperative computed tomography. PCNL and URS were analyzed separately. Continuous data were reported as mean ± standard deviation and were analyzed using the Welch's t-test and the Wilcoxon rank sum test when normally and non-normally distributed, respectively. Categorical data were compared using Fisher's exact test.
For URS, multivariate regression controlling for body mass index (BMI) and proportion of patients with >1 stone was also used. Odds ratios were reported with a 95% confidence interval (CI). Bonferroni correction was applied for outcome variables, resulting in a significance level of alpha <0.01. For all other variables, alpha <0.05 was considered statistically significant. For PCNL, no multivariate analysis was performed, as all baseline characteristics were statistically similar between the HP and AIP groups on univariate analysis. All tests were two sided. Statistical analyses were completed using RStudio version 1.1.456 (RStudio, Boston, MA).
Results
Fifty-one patients undergoing URS (26 HP, 25 AIP) and 29 patients undergoing PCNL (15 HP, 14 AIP) were included. For all URS cases, one circulating nurse was assigned to the OR. After the first two PCNL cases that were randomized to AIP irrigation, one circulating nurse was assigned for PCNL cases randomized to the AIP, although two nurses (one of whom was solely responsible for maintaining the irrigation) were assigned for those randomized to the HP. OR staffing was not a metric included in the study protocol, but rather was established independently by the nursing team based on perceived need. There were no intraoperative complications or any case of postoperative sepsis. A cost comparison of the HP and AIP systems is summarized in Supplementary Table S1.
Ureteroscopy
Baseline characteristics for patients undergoing URS were similar between the HP and AIP groups, except for mean BMI (27.7 ± 4.5 vs 25.3 ± 3.8 kg/m2, respectively; p = 0.04) and number of patients with >1 stone (9 [34.6%] vs 2 [8.0%], respectively; p = 0.04) (Table 1). The mean preoperative pump setup time was 3.7 ± 1.1 and 2.3 ± 1.2 minutes for the HP and AIP, respectively, mean intraoperative pump maintenance time was 2.3 ± 2.3 and 0.6 ± 0.5 minutes, respectively, and mean total pump time was 5.9 ± 2.6 and 2.9 ± 1.6 minutes, respectively (all p < 0.001) (Table 2). During URS with HP irrigation, surgeons verbalized an average of 2.8 ± 2.1 irrigation-related concerns compared with 1.2 ± 1.8 when the AIP was used (p < 0.001). Postoperatively, both surgeons and nurses rated their irrigation-related satisfaction higher when the AIP was used compared to the HP; this association was significant for nurses (9.2 ± 1.3 vs 6.5 ± 2.9, p < 0.001). Operative time, stone-free rate, and liters of irrigation fluid used during the HP and AIP cases did not differ significantly.
Table 1.
Baseline Characteristics
| Variable | Ureteroscopy |
Percutaneous nephrolithotomy |
||||
|---|---|---|---|---|---|---|
| HP (n = 26) | AIP (n = 25) | p | HP (n = 15) | AIP (n = 14) | p | |
| Age (years) | 56.8 ± 12.2 | 57.8 ± 13.2 | 0.70 | 60.1 ± 18.0 | 62.4 ± 7.2 | 0.70 |
| BMI (kg/m2) | 27.7 ± 4.5 | 25.3 ± 3.8 | 0.04a | 32.1 ± 7.2 | 28.7 ± 10.2 | 0.30 |
| Gender | ||||||
| Female | 10 (38.5%) | 12 (48.0%) | 0.60 | 9 (60.0%) | 9 (64.3%) | 1.0 |
| Male | 16 (61.5%) | 13 (52.0%) | 6 (40.0%) | 5 (35.7%) | ||
| ASA score | ||||||
| 1 | 0 (0.0%) | 2 (8.0%) | 0.50 | 0 (0.0%) | 0 (0.0%) | 0.50 |
| 2 | 17 (65.4%) | 15 (60.0%) | 5 (33.3%) | 7 (50.0%) | ||
| 3 | 9 (34.6%) | 8 (32.0%) | 10 (66.7%) | 7 (50.0%) | ||
| Preoperative nephrostomy tube | ||||||
| Yes | 1 (3.8%) | 1 (4.0%) | 1.0 | 1 (6.7%) | 1 (7.1%) | 1.0 |
| No | 25 (96.2%) | 24 (96.0%) | 14 (93.3%) | 13 (92.9%) | ||
| Preoperative ureteral stent | ||||||
| Yes | 7 (26.9%) | 6 (24.0%) | 1.0 | 4 (26.7%) | 3 (21.4%) | 1.0 |
| No | 19 (73.1%) | 19 (24.0%) | 11 (73.3%) | 11 (78.6%) | ||
| Stone density (HU) | 791.8 ± 318.7 | 837.2 ± 307.7 | 0.40 | 830.9 ± 274.0 | 937.0 ± 333.9 | 0.40 |
| Stone volumeb (cm3) | 0.4 ± 0.4 | 1.2 ± 1.8 | 0.20 | 6.7 ± 8.9 | 9.3 ± 10.9 | 0.30 |
| No. of stones | ||||||
| 1 | 17 (65.4%) | 23 (93.0%) | 0.04a | 8 (53.3%) | 10 (71.4%) | 0.40 |
| >1 | 9 (34.6%) | 2 (8.0%) | 7 (46.7%) | 4 (28.6%) | ||
| Ureteroscopec | ||||||
| Single lumen (3.6F) | 12 (46.2%) | 9 (36.0%) | 0.50 | N/A | N/A | N/A |
| Dual lumen (3.6F) | 10 (38.5%) | 10 (40.0%) | ||||
| Semirigid (7.0F) | 3 (11.5%) | 6 (24.0%) | ||||
| Noned | 1 (3.8%) | 0 0.0%) | ||||
Alpha <0.05 considered statistically significant.
Stone volume = l × w × d × π × 0.52.
Irrigation channel diameter.
Only used cystoscope (distal ureteral stone).
AIP = automated irrigation pump; ASA = American Society of Anesthesiologists™; BMI = body mass index; HP = hand pump; HU = Hounsfield units.
Table 2.
Primary Outcomes for Patients Undergoing Ureteroscopy and Percutaneous Nephrolithotomy: Univariate Analysis
| Outcome | Ureteroscopy |
Percutaneous nephrolithotomy |
||||
|---|---|---|---|---|---|---|
| HP (n = 26) | AIP (n = 25) | p | HP (n = 15) | AIP (n = 14) | p | |
| Pump setup time (minutes) | 3.7 ± 1.1 | 2.3 ± 1.2 | <0.001a | 9.8 ± 4.0 | 2.2 ± 1.0 | <0.001a |
| Pump maintenance time (minutes) | 2.3 ± 2.3 | 0.6 ± 0.5 | <0.001a | 24.0 ± 29.9 | 2.5 ± 1.6 | <0.001a |
| Total pump time (setup+maintenance; minutes) | 5.9 ± 2.6 | 2.9 ± 1.6 | <0.001a | 33.9 ± 29.6 | 4.6 ± 1.3 | <0.001a |
| Intraoperative irrigation-related concerns | 2.8 ± 2.1 | 1.2 ± 1.8 | <0.001a | 4.0 ± 3.3 | 1.9 ± 1.2 | 0.07 |
| Surgeon satisfaction (1–10)b | 7.9 ± 2.3 | 8.8 ± 2.0 | 0.07 | 7.3 ± 2.7 | 8.9 ± 2.4 | 0.05 |
| Nurse satisfaction (1–10)b | 6.5 ± 2.9 | 9.2 ± 1.3 | <0.001a | 4.4 ± 3.5 | 9.4 ± 1.0 | 0.001a |
| Operative time (minutes) | 69.0 ± 35.1 | 76.2 ± 42.0 | 0.50 | 140.8 ± 81.1 | 131.3 ± 56.9 | 0.90 |
| Irrigation fluid used (L) | 1.8 ± 1.4 | 2.5 ± 1.7 | 0.10 | 22.5 ± 36.7 | 20.5 ± 16.6 | 0.40 |
| Stone-free ratec | ||||||
| No fragments | 8 (29.6%) | 3 (37.5%) | 0.39 | 6 (42.9%) | 6 (42.9%) | 1.0 |
| Fragments ≤4 mm | 8 (29.6%) | 5 (62.5%) | 1.0 | 7 (50.0%) | 11 (78.6%) | 0.24 |
Alpha <0.01 considered statistically significant after adjustment with Bonferroni correction, given comparison of five outcome variables.
Irrigation satisfaction scoring: 1 = highly dissatisfied to 10 = highly satisfied.
Stone-free status based on postoperative computed tomography.
On multivariate analysis, use of the AIP was a significant predictor of decreased setup time (β = −1.67 minutes, 95% CI −2.4 to −1.0; p < 0.001), maintenance time of <1 minute (odds ratio 15.8, 95% CI 3.3–73.7; p < 0.001), total pump time of <5 minutes (odds ratio 25.8, 95% CI 4.0–165.4; p < 0.001), and favorable (8–10/10) nurse satisfaction rating (odds ratio 25.4, 95% CI 4.1–164.0; p < 0.001) (Table 3). The AIP was not associated with a more favorable (8–10/10) surgeon satisfaction rating (odds ratio 1.6, 95% CI 0.4–6.7; p = 0.60). Although fewer surgeon-generated intraoperative concerns occurred with the AIP, this association did not reach statistical significance (odds ratio 6.9, 95% CI 1.2–40.4; p = 0.03).
Table 3.
Primary Outcomes for Patients Undergoing Ureteroscopy: Multivariate Analysis
| Outcomea | Ureteroscopy |
Estimated difference (β) (95% CI) | p | ||
|---|---|---|---|---|---|
| HP (n = 26) | AIP (n = 25) | ||||
| Pump setup time | 3.7 ± 1.1 | 2.3 ± 1.2 | −1.67 (−2.4 to −1.0) | <0.001b | |
| Outcomec | HP (n = 26)d | AIP (n = 25) | Estimated odds ratio (95% CI) | p |
|---|---|---|---|---|
| Pump maintenance time | ||||
| <1 minute | 7 (26.9%) | 20 (80.0%) | 15.8 (3.3 to 73.7) | <0.001b |
| ≥1 minutes | 19 (73.1%) | 5 (20.0%) | ||
| Total pump time | ||||
| <5 minutes | 9 (36%) | 22 (88%) | 25.8 (4.0 to 165.4) | <0.001b |
| ≥5 minutes | 16 (64%) | 3 (12%) | ||
| Intraoperative irrigation-related concerns | ||||
| None | 2 (7.6%) | 11 (44.0%) | 6.9 (1.2 to 40.4) | 0.03 |
| One or more | 24 (92.4%) | 14 (56.0%) | ||
| Surgeon satisfactione | ||||
| Favorable (8–10/10) | 19 (73.1%) | 20 (80.0%) | 1.6 (0.4 to 6.7) | 0.60 |
| Unfavorable (0–7/10) | 7 (26.9%) | 5 (20.0%) | ||
| Nurse satisfactione | ||||
| Favorable (8–10/10) | 11 (42.3%) | 23 (92.0%) | 25.4 (4.1 to 164.0) | <0.001b |
| Unfavorable (0–7/10) | 15 (57.7%) | 2 (8.0%) | ||
Linear regression used for analysis (normally distributed data).
Alpha <0.01 considered statistically significant after adjustment with Bonferroni correction, given comparison of five outcome variables.
Logistic regression used for analysis (data not normally distributed).
Twenty-five patients included for pump maintenance time and total pump time.
Irrigation satisfaction scoring: 1 = highly dissatisfied to 10 = highly satisfied.
CI = confidence interval.
Percutaneous nephrolithotomy
Patients undergoing PCNL with use of the HP and AIP systems were similar in regard to baseline characteristics (Table 1). Mean pump setup time was 9.8 ± 4.0 and 2.2 ± 1.0 minutes for the HP and AIP, respectively, mean intraoperative pump maintenance time was 24.0 ± 29.9 and 2.5 ± 1.6 minutes, respectively, and mean total pump time was 33.9 ± 29.6 and 4.6 ± 1.3 minutes, respectively (all p < 0.001) (Table 2). More irrigation-related concerns (4.0 ± 3.3 vs 1.9 ± 1.2; p = 0.07) and lower surgeon satisfaction (7.3 ± 2.7 vs 8.9 ± 2.4 points out of 10; p = 0.05) were observed in the HP group compared to the AIP group, although these associations did not reach statistically significant levels. Circulating nurses rated their satisfaction significantly lower with the HP compared to the AIP (4.4 ± 3.5 vs 9.4 ± 1.0 points out of 10, respectively; p = 0.001). Operative time, stone-free rate, and liters of irrigation fluid used during HP and AIP cases did not differ significantly.
Discussion
In this report, compared to HP irrigation, the use of the AIP was associated with a significant decrease in the total time dedicated to preparing and maintaining the irrigation system during both URS and PCNL. For patients undergoing URS, use of the AIP was an independent predictor of an overall pump time of <5 minutes, a decreased pump setup time, and a pump maintenance time of <1 minute. Notably, the clinical significance of the 3-minute decrease in total pump time during URS was marginal. In contrast, for PCNL cases, the AIP provided a statistically and clinically significant drop in total pump time of 29 minutes.
These findings are of interest, given that OR turnover time is generally >20 minutes.10,11 Based on this study, OR turnover time and excess staffing costs, which are established metrics of OR inefficiency,10,12,13 are mitigated by the use of the AIP, with greater benefit seen during PCNL. Indeed, after the first two PCNL cases that were randomized to AIP irrigation, OR administrative personnel at our institution reduced OR staffing by one nurse for PCNL cases randomized to AIP; this decision was made exclusive from the study protocol and was based on administrators' perception of workload. The average hourly salary of a circulating nurse at our institution is $57.00/hour. Thus, based on the average operative time of a PCNL in which HP irrigation was used (2.3 hours), an additional $131.10 per case was allotted for the auxiliary circulating nurse whose sole responsibility was to maintain the irrigation intraoperatively.
For both URS and PCNL, the AIP was associated with a significantly higher nurse satisfaction rating, but was not associated with higher surgeon satisfaction or with decreased irrigation-related surgeon concerns. Taken together, these findings indicate that use of the AIP had a higher beneficial impact on the nursing team rather than for the surgeon, especially during PCNL. Indeed, a prior report of manual irrigation systems highlighted user fatigue as a primary concern with HP irrigation compared to the AIP.14 Furthermore, HP irrigation systems have been shown to exhibit a marked reduction in flow rate after the first 5 minutes of irrigation flow compared to the more consistent flow provided by an AIP.2 With HP irrigation, as fluid is used, the pressure exerted by the inflated pressure sleeve diminishes, and the irrigation flow weakens. In addition, manual systems such as handheld syringes and foot pumps provide flow in spikes, resulting in high maximal retro-pulsing forces and peak pressures that vary based on the strength of the user.3–5,14 Although increasing the height of the irrigation bag can increase the flow rate, this effect plateaus at a height of ∼80 cm above the level of the patient.1 In contrast, automated irrigation systems maintain steady flow without pressure peaks.8 Our findings indicate that automated control of irrigation pressure and flow reduces the burden of pump maintenance for nurses. In addition, when irrigation fluid levels fall below 600 mL, the Thermedx sounds an alarm notifying circulating nurses that the fluid will soon require replacement, ensuring uninterrupted flow during procedures.
Of note, we used a ureteral access sheath (UAS) in the majority of URS (76%) and PCNL (97%) cases; UAS utilization and UAS size were similar between the HP and AIP groups. This offers one possible explanation for the similarity in surgeon satisfaction and intraoperative irrigation-related concerns, as the UAS enhances irrigation fluid outflow from the ureter and the renal collecting system, which improves the endoscopic view.15,16 In addition, there were no cases of postoperative sepsis as defined by the Sequential Organ Failure Assessment (SOFA) scoring system17; this was likely attributable to the high rate of UAS utilization and our departmental mandate for a documented sterile urine culture before URS or PCNL. Pressurized irrigation increases intrarenal pressure, which is a risk factor for postoperative infectious complications after PCNL18 and URS,19 especially if the intrarenal pressure exceeds 30 to 45 mm Hg20,21; however, placement of a UAS significantly decreases intrarenal pressure.15,16,22,23 We utilized pump pressure settings ranging from 70 to 250 mm Hg and 100 to 250 during URS and PCNL, respectively, dependent upon the presence of an instrument in the working channel.
We did not observe a significant difference in liters of irrigation fluid used, operative time, or stone-free rate between the HP and AIP cases during URS or PCNL. In a single-surgeon experience comparing an automated irrigation-suction pump to HP irrigation during flexible URS, Lechevallier and colleagues also reported a similar amount of irrigation fluid used, although they did observe a statistically significant 53% reduction in URS time, which was measured from the time of placement of the ureteroscope at the ureteral orifice to the end of the case.6 In contrast, we measured operative time from the end of the preoperative time-out to completion of closing for both URS and PCNL, which allowed for the clear distinction between pump setup time and pump maintenance time.
There are several limitations to this study. First, surgeon and nurse irrigation-related satisfaction were assessed with a subjective survey. However, post hoc analysis showed that a similar cohort of surgeons and nurses responded to the survey for HP and AIP cases (Supplementary Table S2). Second, given that an additional nurse was assigned to PCNL cases in which HP irrigation was used, the true time allotted to irrigation-related matters may have been biased in favor of the HP irrigation system. Finally, this is a single-center experience; the outcomes reported in this study are subject to factors, including institutional resources and protocols. For example, institutions that do not allocate two nurses for standard PCNL cases may not experience the cost savings that we experienced. Nevertheless, the ability to allocate an additional circulating nurse at our institution served to demonstrate the extent to which the pump type affected OR efficiency.
Conclusions
During URS and PCNL, use of the AIP resulted in a significant decrease in total irrigation pump management time. In addition, the AIP was associated with significantly improved nurse satisfaction during both URS and PCNL.
Supplementary Material
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH). We would also like to acknowledge Ramy F. Youssef, MD and Peter Ghamarian, MD, both of whom contributed patients for this study.
Abbreviations Used
- AIP
automated irrigation pump
- BMI
body mass index
- CI
confidence interval
- HP
manual hand pump infuser
- NIH
National Institutes of Health
- OR
operating room
- PCNL
percutaneous nephrolithotomy
- UAS
ureteral access sheath
- URS
ureteroscopy
Authors' Contributions
F.A.J.: study design, data collection, data analysis, and article writing. J.M.S.: study design, data collection, data analysis, and article writing. L.L.: data analysis and article review. S.L.: data collection and article review. C.M.C.: data collection and article review. S.T.: data collection and article review. R.M.P.: study design and data collection. R.V.C.: study design, data collection, and article review. J.L.: study design, data analysis, data collection, and article review.
Author Disclosure Statement
J.L.: paid speaker for Richard Wolf Medical Instruments Corporation. All other authors have no competing financial interests exist.
Funding Information
This work was partially supported by grant UL1 TR001414 from the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through the Biostatistics, Epidemiology and Research Design Unit.
Supplementary Material
References
- 1. Chang D, Manecksha RP, Syrrakos K, et al. . An investigation of the basic physics of irrigation in urology and the role of automated pump irrigation in cystoscopy. ScientificWorldJournal 2012;2012:476759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lama DJ, Owyong M, Parkhomenko E, et al. . Fluid dynamic analysis of hand-pump infuser and Uromat endoscopic automatic system for irrigation through a flexible ureteroscope. J Endourol 2018;32:431–436 [DOI] [PubMed] [Google Scholar]
- 3. Blew BD, Dagnone AJ, Pace KT, et al. . Comparison of Peditrol irrigation device and common methods of irrigation. J Endourol 2005;19:562–565 [DOI] [PubMed] [Google Scholar]
- 4. Hendlin K, Weiland D, Monga M. Impact of irrigation systems on stone migration. J Endourol 2008;22:453–458 [DOI] [PubMed] [Google Scholar]
- 5. Proietti S, Dragos L, Somani BK, et al. . In vitro comparison of maximum pressure developed by irrigation systems in a kidney model. J Endourol 2017;31:522–527 [DOI] [PubMed] [Google Scholar]
- 6. Lechevallier E, Luciani M, Nahon O, et al. . Transurethral ureterorenolithotripsy using new automated irrigation/suction system controlling pressure and flow compared with standard irrigation: A randomized pilot study. J Endourol 2003;17:97–101 [DOI] [PubMed] [Google Scholar]
- 7. De S, Torricelli FC, Sarkissian C, et al. . Evaluating the automated Thermedx Fluid Management System in a ureteroscopy model. J Endourol 2014;28:549–553 [DOI] [PubMed] [Google Scholar]
- 8. Nagele U, Walcher U, Bader M, et al. . Flow matters 2: How to improve irrigation flow in small-calibre percutaneous procedures-the purging effect. World J Urol 2015;33:1607–1611 [DOI] [PubMed] [Google Scholar]
- 9. Healey T, El-Othmani MM, Healey J, et al. . Improving operating room efficiency, part 1: General managerial and preoperative strategies. JBJS Rev 2015;3:e3. [DOI] [PubMed] [Google Scholar]
- 10. Saha P, Pinjani A, Al-Shabibi N, et al. . Why we are wasting time in the operating theatre? Int J Health Plann Manage 2009;24:225–232 [DOI] [PubMed] [Google Scholar]
- 11. Girotto JA, Koltz PF, Drugas G. Optimizing your operating room: Or, why large, traditional hospitals don't work. Int J Surg 2010;8:359–367 [DOI] [PubMed] [Google Scholar]
- 12. Fixler T, Wright JG. Identification and use of operating room efficiency indicators: The problem of definition. Can J Surg 2013;56:224–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pimentel MT, Flanagan H, Philip BK, et al. . Qualitative analysis of barriers to efficient operating room turnovers in a tertiary care academic medical center. J Med Pract Manage 2015;30(6 Spec No.):30–35 [PubMed] [Google Scholar]
- 14. Tarplin S, Byrne M, Farrell N, et al. . Endoscopic valves and irrigation devices for flexible ureteroscopy: Is there a difference? J Endourol 2015;29:983–992 [DOI] [PubMed] [Google Scholar]
- 15. Landman J, Venkatesh R, Ragab M, et al. . Comparison of intrarenal pressure and irrigant flow during percutaneous nephroscopy with an indwelling ureteral catheter, ureteral occlusion balloon, and ureteral access sheath. Urology 2002;60:584–587 [DOI] [PubMed] [Google Scholar]
- 16. Rehman J, Monga M, Landman J, et al. . Characterization of intrapelvic pressure during ureteropyeloscopy with ureteral access sheaths. Urology 2003;61:713–718 [DOI] [PubMed] [Google Scholar]
- 17. Singer M, Deutschman CS, Seymour CW, et al. . The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016;315:801–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhong W, Zeng G, Wu K, et al. . Does a smaller tract in percutaneous nephrolithotomy contribute to high renal pelvic pressure and postoperative fever? J Endourol 2008;22:2147–2151 [DOI] [PubMed] [Google Scholar]
- 19. Zhong W, Leto G, Wang L, et al. . Systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy: A study of risk factors. J Endourol 2015;29:25–28 [DOI] [PubMed] [Google Scholar]
- 20. Thomsen HS. Pyelorenal backflow. Clinical and experimental investigations. Radiologic, nuclear, medical and pathoanatomic studies. Dan Med Bull 1984;31:438–457 [PubMed] [Google Scholar]
- 21. Boccafoschi C, Lugnani F. Intra-renal reflux. Urol Res 1985;13:253–258 [DOI] [PubMed] [Google Scholar]
- 22. Auge BK, Pietrow PK, Lallas CD, et al. . Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol 2004;18:33–36 [DOI] [PubMed] [Google Scholar]
- 23. Patel RM, Owyong M, Ayad M, et al. . Pd08-03 characterization of intracalyceal pressure during ureteroscopy. J Urol 2019;201(Suppl 4):e148–e149 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.