Abstract
Background:
Imaging tests are one of the most sophisticated types of diagnostic tools used in health care, yet there are concerns that imaging is overused. Currently, tests are typically evaluated and implemented based on their accuracy, and there is limited knowledge about the range of patient-centered outcomes (PCOs) that imaging tests may lead to. This study explores patients’ experiences and subsequent outcomes of imaging tests most notable to patients.
Methods:
Adult patients from four primary care clinics who had an x-ray, CT, MRI, or ultrasound in the 12 months before recruitment participated in a single semistructured interview to recount their imaging experience. Interview transcripts were analyzed thematically.
Results:
Four themes related to PCOs were identified from 45 interviews. Participants’ mean age was 53 years (25-83 years), 30 had undergone a diagnostic imaging test, and 15 underwent imaging for screening or monitoring. Themes included knowledge gained from the imaging test, its contribution to their overall health care journey, physical experiences during the test procedure, and impacts of the testing process on emotions.
Conclusions:
Patients identified various imaging test outcomes that were important to them. Measurement and reporting these outcomes should be considered more often in diagnostic research. Tools for providers and patients to discuss and utilize these outcomes may help promote shared decision making around the use and impact of imaging tests.
Keywords: Radiology, imaging, patient-centered outcomes, patient-reported experience
INTRODUCTION
Imaging tests fulfill multiple roles in primary care, including screening, diagnosis, and monitoring of disease. A recent survey found that imaging tests were ordered or conducted in approximately 14% of office visits in the United States [1]. The United States ranks as one of the highest users of advanced imaging tests among high-income countries [2]. Frequent use of imaging tests reflects not only their clinical value but also concerns of medical malpractice and patient pressure for greater diagnostic certainty. However, there are growing concerns that some imaging tests are overused [3]. In a national survey, three quarters of US physicians indicated that unnecessary medical tests, including imaging tests, constituted a “very or somewhat serious problem” [4]. Organizations such as the American Board of Internal Medicine’s Choosing Wisely campaign have highlighted imaging tests that are frequently overused and should be used judiciously [5,6].
To facilitate appropriate utilization of imaging tests, clinicians and patients need information and effective tools to weigh their risks and benefits. Currently, the utility of imaging tests is predominantly guided by diagnostic accuracy and the consequences of false-positives and false-negatives [7] rather than a comprehensive evaluation of all positive and negative outcomes, including nonclinical outcomes [8]. An evidence-based summary of the effects of imaging on patient-centered outcomes seems essential for facilitating value-based health care decisions.
To promote judicious use of imaging tests, initiatives to better understand patients’ experiences of these tests are vital. This could facilitate the design and development of tools that enable physicians and patients to navigate the complexities of decision making together, taking into account patient-centered outcomes (PCOs) [9]. PCOs include experiences important to patients, such as biomedical, cognitive, emotional, social, financial, physical, and behavioral effects of imaging tests [10–14]. Researchers have proposed that studies of imaging tests should evaluate the direct impact on patients and establish the potential “net benefit” to the patient [8,15]. The aim of this study was therefore to explore patients’ experiences and subsequent outcomes of imaging tests, identified from family medicine clinics in the United States. This study is part of a larger project called the Patient-Centered Research for Standards of Outcomes in Diagnostic Tests (PROD), which aims to provide guidance for patients, clinicians, and researchers on more comprehensive ways of evaluating the risks and benefits of imaging tests.
METHODS
Study Design
We qualitatively explored imaging test experiences that patients noticed and reported through semi-structured interviews [10]. These experiences were explored for thematic trends to identify PCOs related to their testing experience(s).
Participants and Setting
Study sites were enrolled through the WWAMI region Practice and Research Network, a practice-based research network in the 5-state Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI) area. Participants were recruited from four family medicine clinics across Washington and Idaho: a large urban medical center, an urban clinic, a small urban federally qualified health center servicing rural areas, and a rural-serving nonprofit community health center. Participants were identified through electronic medical record queries from the following criteria: aged 18 years or older, ability to communicate in English, received at least one imaging test (including mammogram, joint, limb, or body x-ray, pelvic or abdominal ultrasound, abdominal or lung CT, back or head and neck MRI), for any reason, within 12 months before recruitment. Patients were excluded if they had a terminal illness or cognitive impairment. Participants were recruited through purposive sampling by imaging modality, gender, age, and insurance coverage to ensure diversity in participants and experiences. The University of Washington Human Subjects Division approved this study. All participants interviewed provided informed verbal consent and received a $50 gift card for participation.
Data Collection
A number of frameworks that outline PCO domains of diagnostic tests directed the development of the semistructured interview guide [12–14,16]. We designed the guide with guidance from these frameworks to elicit the patient experiences of emotional, cognitive, behavioral, physical, financial, and other outcomes that could occur before, during, and after an imaging test. Patient demographic, health insurance, and imaging history information were also collected during the interview. Interview guides were reviewed and revised by the PROD study patient stakeholder advisory group as well as research champions or coordinators at each study site before use. The interview guide was revised twice after data collection began, once to refine clarity of wording and once to prompt details of outcomes mentioned in previous interviews.
Interviews were conducted by phone between September 2016 and March 2017 by one of three trained interviewers (M.L.Z.S., E.W., and A.R.T.). Participants were recruited and interviewed until thematic saturation was met, meaning no more new themes emerged from the data [17]. Interviews, varying between 15 and 45 min, were recorded and transcribed. Transcripts were reviewed with the audio for accuracy and contextual details by the interviewer and a second researcher.
Analysis
Development of a coding framework commenced midway through data collection. After data immersion, two researchers (M.L.Z.S., E.W.) initially coded five transcripts using open coding, assigning descriptive terms to portions of text [18,19]. Initial codes were organized into potential categories and subcategories, which were presented to the broader PROD study team and patient stakeholder advisory group. Revisions to this initial framework were implemented based on feedback from these groups. Steered by the transcript text, codes were developed, refined, and organized into categories and subcategories through an iterative process.
Thematic analysis informed our exploration of patient experiences [20,21]. Two coders (M.L.Z.S. and E.W.) completed coding by applying the final coding framework to the entire interview text. A third coder (A.R.T.) reconciled discrepancies in data interpretation. Through an iterative process of coding, reconciling, and discussion, coders came to a consensus about coding application. Dedoose qualitative analysis software (Dedoose Version 7.0.23, Los Angeles, California: SocioCultural Research Consultants, LLC, www.dedoose.com) was used to facilitate data analysis. Excerpts from the coded transcripts were reviewed. Pertinent codes were organized into potential themes and subthemes representing PCOs [20]. Final themes were defined and quotes selected to represent those themes.
RESULTS
Over the data collection period, 141 eligible patients were approached for participation, of whom 63 agreed to participate. Eighteen could not be reached for interview, and 45 successfully completed an interview. Recruitment concluded after saturation had been met (ie, no new topics emerged). Participants’ mean age was 53 years (range: 25-83) (Table 1). Of those interviewed, 30 experienced an imaging test for diagnostic reasons and 15 for screening or monitoring. Thirty-two participants reported their provider as the main reason for having the test. The majority of patients, 31 reported no financial concerns related to their imaging test. Eleven patients had concerns about financial costs of the test or broader costs, such as days lost from work. Thematic analysis produced four themes identified as influential to the patient experience (Fig. 1).
Table 1.
Description of study participants
| Characteristics | n | % |
|---|---|---|
| Gender | ||
| Male | 14 | 31 |
| Female | 31 | 69 |
| Race and ethnicity | ||
| American Indian or Alaska Native | 1 | 2 |
| Black or African American | 4 | 9 |
| White | 35 | 78 |
| Hispanic or Latino (of any race) | 4 | 9 |
| Other | 1 | 2 |
| Age range | ||
| 18-39 | 10 | 22 |
| 40-59 | 21 | 47 |
| 60 and above | 14 | 31 |
| General health | ||
| Excellent | 4 | 9 |
| Very good | 10 | 22 |
| Good | 16 | 36 |
| Fair | 12 | 27 |
| Poor | 2 | 4 |
| Insurance type | ||
| Private | 11 | 24.4 |
| Medicaid | 20 | 44.4 |
| Medicare | 14 | 31.1 |
| Education level | ||
| Some primary or secondary school, no diploma | 9 | 20 |
| High school graduate or equivalent | 12 | 27 |
| Some college, no degree | 5 | 11 |
| Undergraduate and graduate education | 19 | 42 |
| Current employment status | ||
| Employed | 14 | 31 |
| Not working (retired, unemployed, student) | 31 | 69 |
| Type of test | ||
| MRI | 11 | 24.4 |
| Ultrasound | 12 | 26.7 |
| CT | 5 | 11.1 |
| X-ray | 13 | 28.9 |
| Mammogram | 4 | 8.9 |
| Time between imaging test and interview (months) | ||
| 0-3 | 37 | 82.2 |
| 3-6 | 6 | 13.3 |
| 6-9 | 0 | 0 |
| 9-12 | 2 | 4.4 |
Fig 1.
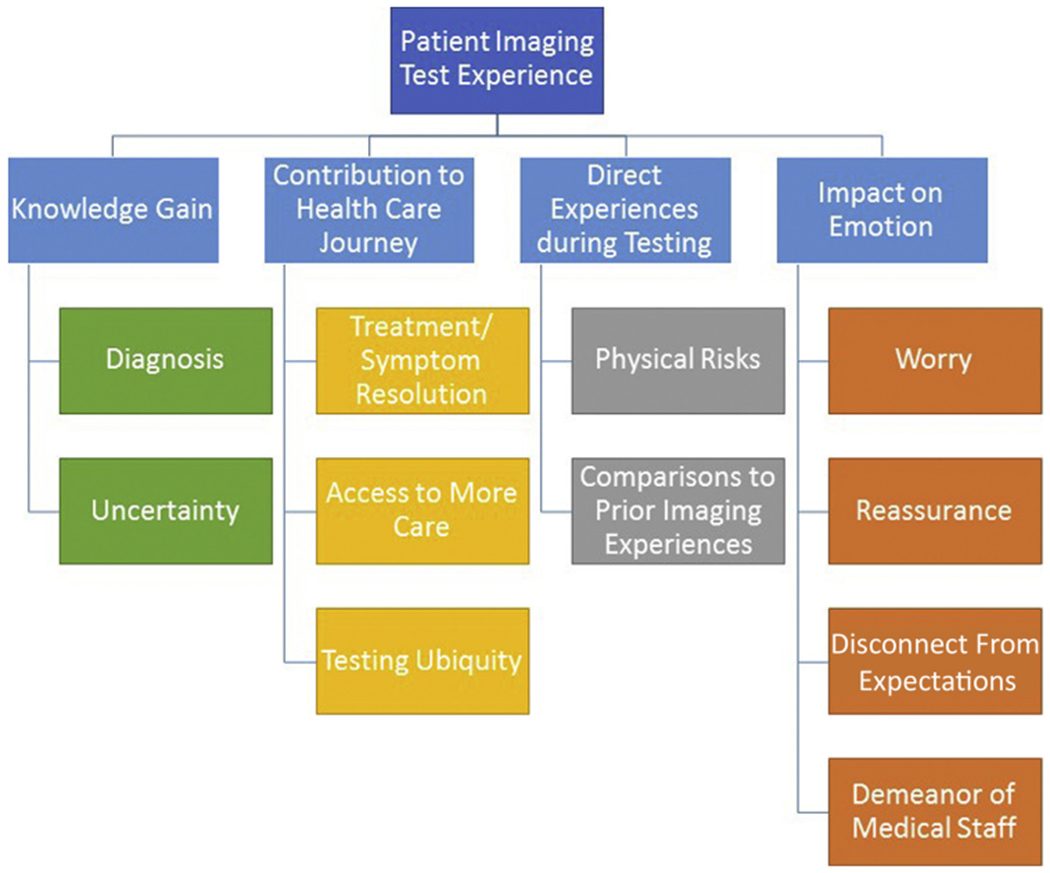
The four qualitative themes and their PCO subthemes comprising the patient imaging test experience.
Knowledge Gain
The desire “to know” or “find answers” was raised by patients as the main motivation for the test (Table 2). The knowledge obtained from imaging tests was seen as a valuable outcome. Patients’ emotions about the test shifted as knowledge developed depending on what point during imaging they discussed: before—knowledge void or fear; during—wonder or anticipation; or after a test—conclusions drawn from the test. On the positive side, patients were relieved by learning their symptoms were not caused by something serious or if results led to an answer. Uncertainty that remained even after testing led to negative impressions of the test. Although patients rarely mentioned downstream outcomes as a potential risk before having a test, those who received indeterminate, incidental, or inconclusive test results reported negative emotional outcomes, such as worry and frustration, about why the test had been ordered. Also, patients’ prior knowledge or understanding about the test’s purpose or capability seemed to leave them unprepared for these scenarios.
Table 2.
Thematic outcomes of reported patient experiences during imaging testing–knowledge gain
| Subtheme | Illustrative Quotes |
|---|---|
| Diagnosis | “I was hoping that they would see something, and then be like, ‘Hey, look, I know how to help!’ And then we’d figure out how to help. [Laughs] So the x-ray would actually shed some light on the problem.” (patient 22) “Well, I was actually fine with it being cancer or not being cancer. That probably sounds strange, but I really would have been fine either way. I just wanted to know.” (patient 26) |
| Uncertainty | A patient who did not receive a diagnosis after a foot x-ray and needed to go in for more testing: “Well, it makes me worry actually, because I’m not sure what’s going on with my foot. I have a bit of history of health problems. It kind of makes you worry not knowing what’s going on.” (patient 09) “I’m just frustrated. I guess you can say it. I’ve been like that. They’ve been doing all this stuff because it didn’t solve the problem.” (patient 07) When asked, “How have the test results impacted you?” one patient after an x-ray confirmed pain was not from a broken bone stated: “I don’t know. I’m kind of curious what’s going on with it right now, because it’s starting to hurt. If it didn’t break, what is going on?” (patient 20) |
Contribution to Their Health Care “Journey”
Patients typically considered symptom resolution as a main benefit to testing and reported satisfaction with an imaging test if this was achieved, testing furthered their “journey” through the health care system (Table 3). In situations where the test did not lead to symptom resolution or a treatment strategy, patients accepted this as long as they felt that a serious illness had been ruled out. If not, patients were frustrated with having to go through steps with inconclusive results.
Table 3.
Thematic outcomes of reported patient experiences during imaging testing–contribution to the health care journey
| Subtheme | Illustrative Quotes |
|---|---|
| Treatment plan or symptom resolution | “My understanding is that the benefit would be that the MRI would provide a three-dimensional image of my knee that would show any damage to the meniscus and perhaps any other ligaments in my knee so that we could make a decision about how to proceed with my care.” (patient 31) “They’ve showed us the way forward; there was some treatment to begin with. The route that we’re going right now, it has eased up the pain and where I can start functioning in life again. I can walk around the house or the yard and do things without being in constant pain. So, as far as an impact, I think it’s had a huge impact, as far as my quality of life and everything going forward so far.” (patient 39) |
| Access to more care | “I’ve been having a lot of problems with my hands going numb and a lot of pain and migraines. I’ve been telling my doctor about it for close to a year now. He finally got me into MRI so I can get into a specialist.” (patient 12) |
| Testing ubiquity | A patient who had a CT scan for rib pain summed up the testing experience: “I’ve had so many before this that it was no different than going in and giving a sample of blood or an x-ray.” When asked about the impacts from the test, the patient replied: “No. I don’t think there’s going to be anything urgent or anything to worry about. I have had so many surgeries and I have [condition] and I’m constantly going in for tests so it’s just a part of my life.” (patient 30) |
Another outcome for some patients undergoing imaging testing was whether it led to referral to a “higher level” of care. Access to someone with more knowledge of the affected area or a higher level of imaging, such as MRI, seemed important to patients. Moreover, 43 patients mentioned undergoing at least one prior imaging test. Thus, imaging tests were generally viewed by patients as being quite common and familiar and not particularly remarkable.
Direct Experiences During Testing
Patients identified a number of direct physical experiences related to the performance of the test that influenced their perceptions (Table 4). General discomfort during the test included pain from holding certain positions, noise, or claustrophobia. In patients’ reflections on their perceived risks of the test, patients almost exclusively focused on the physical risks; broader risks, such as cost or additional testing, were not widely reported. This finding corresponds to the 32 patients reporting that there were either no anticipated risks or had not been told of any risks to the imaging test. In contrast, other patients noted that some tests (eg, plain radiographs, ultrasound) were more comfortable, took less time, or were simpler compared with more sophisticated imaging. Patients with prior experience with the imaging test modality recounted fewer physical or emotional responses during the testing process.
Table 4.
Thematic outcomes of reported patient experiences during imaging testing–direct experiences during testing
| Subtheme | Illustrative Quotes |
|---|---|
| Physical risks | “With my neck issues I have stiffness in my back so laying flat on my back was very uncomfortable with my head level–that wasn’t … I’m not criticizing them because I think that was necessary. I assume that was necessary because of the pictures they wanted but that was not very comfortable to lay there for 20 minutes flat on my back. That was an effort on my part to comply with that.” (patient 17) |
| Comparisons with prior imaging experiences | “I had had a test a few years ago that made me drink dye and get dye injected. That had not been totally pleasant, but I knew an ultrasound didn’t require any preparation so I wasn’t worried at all.” (patient 26) “I got x-rays before, so I’m quite ready. I know what to expect from them.” (patient 8) |
Impacts on Emotion
A pervasive theme that emerged was the effect of testing on patients’ emotional experience (Table 5). Prominent emotional outcomes resulting from imaging tests included dichotomous experiences of peace of mind or reassurance and worry. Patient expectations, originating from personal experience or prior knowledge, served as a cause of emotional response to their imaging test. Patients recounted knowledge from previous health care encounters, Internet searches, or anecdotes from family or friends’ testing experiences. This prior knowledge influenced expectations and thoughts about the test, including perceived test capabilities and risks. Patients reacted emotionally to the test when they encountered unexpected testing procedures; for example, being surprised by the number of images required or unexpectedly receiving injected contrast medium. Medical staff played a significant role in managing patient emotions around testing. Depending on their actions toward patients, medical staff members either exacerbated emotions of frustration or worry or provided comfort or relief.
Table 5.
Thematic outcomes of reported patient experiences during the imaging testing–impact on emotion
| Subtheme | Illustrative Quotes |
|---|---|
| Reassurance | A patient described the most important aspect of a mammogram: “I think it would be the freedom of mind. Just knowing that everything is fine and that that element of my life is taken care of. I’ve done what I can do. Even if I were to develop a tumor, or something, in my breast today, I would have thought, ‘Well, I did everything that I could,’ and we just deal with what we have in front of us and move forward. I think that it is the peace of mind, that’s what I mean, the peace of mind that I’ve done what I can do, and we just go forward from here.” (patient 42) |
| Worry | “Well, I was looking forward to it, so I was kind of anxious to get in and get it done, I guess I was anxious all morning until–I think I went in at one and had the ultrasound done.” (patient 40) “Just worried about if something was there. If they were to see something I wouldn’t know until they send it to the clinic.” (patient 07) |
| Disconnect from expectations | “I guess it wasn’t really clear to me what all that they were looking for, that nobody had explained it to me, either my physical therapist, my primary care doctor, anyone beforehand, just that … They had mentioned some degeneration, but I hadn’t really understood all what that meant, and I hadn’t questioned them about that. Being a retired nurse usually I’m very much the information seeker, but I’ve been really overwhelmed already this summer, and I didn’t probe like I normally do, and I, so I’m feeling kind of blindsided and overwhelmed now.” (patient 03) |
| Demeanor of medical staff | “I was a little nervous because I didn’t know what they were going to find. But they eased my mind. The ladies that did it, they were really good. They told me what they were doing and talked me through it. They let me see what they were seeing. I couldn’t understand it but they let me see what they were doing.” (patient 16) “It was kind of weird when we were talking just fine and then the more she had to click the buttons and the longer she had to measure things I did get a little more nervous because I figured she must’ve found something else.” (patient 13) |
DISCUSSION
Main Findings
We set out to explore the outcomes that patients experience when undergoing imaging tests in primary care to inform more patient-centered approaches to decision making around use of imaging tests. The four PCOs that emerged from patients’ experiences with various imaging modalities included knowledge gained from the test, contribution to their overall health care journey, direct experiences during the test procedure, and impacts of the testing process on emotions.
An unanticipated finding was the importance patients placed on the knowledge that their test provided, even if this did not always directly influence their health care. Furthermore, patients seemed to view imaging tests as routine and as an overtly accepted component of their health care experience. This may be a reflection of the frequent use (or overuse) of imaging, with its increasing availability within physicians’ offices and the rise in frequency of complex imaging (CT, MRI) [22]. It may also reflect greater patient demand for tests and patients’ desire for greater diagnostic certainty [23].
The GRADE approach to developing clinical guidance for diagnostic tests incorporates testing accuracy as a surrogate to patient-important outcomes, such as a test’s clinical impact on downstream testing and actionable diagnoses, but does not include the additional attributes or PCOs that our study suggests may be important to patients [24–27]. Research on cancer screening has found that although the consequences of inaccurate tests were potentially concerning at the time, they did not change patients’ positive feelings about screening tests [28,29].
Comparison With Existing Literature
Little research exists on which outcomes patients identify or prioritize related to imaging tests. Although sparse, our findings mirror existing evidence where PCOs related to screening tests have been reported. The cancer-screening literature provides evidence that false-positive mammograms and other screening tests can lead to emotional distress as well as reassurance and can be associated with physical discomfort [14,30–32]. In two reports, screening was viewed positively overall, with the knowledge gained far outweighing any negative implications from screening [31,32].
Patients undergoing other forms of imaging also described outcomes, such as pain, fear, anxiety, as well as the value of information gained about their diagnoses, that gave them a sense of control over their health care [33–35]. Knowledge about a diagnosis has also been observed to relieve anxiety in multiple studies [36–38]. Our study strengthens these findings that knowledge (or lack thereof) from test results is related to the emotional impact. Leveraging the link between knowledge and emotion could improve outcomes for patients.
Strengths and Limitations
This is one of the first studies addressing PCOs across a wide range of imaging modalities and clinical conditions in primary care. Recruiting patients with diverse imaging modalities and clinical experiences, drawn from family medicine settings in four different locations, strengthens our generalizability. We acknowledge several limitations to our study. First, our broad scope limited our ability to explore PCOs in depth for every combination of modality, clinical condition, and patient demographic. Our preference for breadth may overlook important PCOs for certain patients and scenarios. Second, our study was conducted in English only, limiting the populations whose experiences could be included in this research. Third, given our inclusion criteria, we could not capture perspectives of patients who had a test ordered but decided not to proceed with it, nor patients from other clinical specialties; these should be explored in future research. Finally, recall bias is a potential concern, although 82% of respondents had their test within the previous 3 months. We did not explore concerns or anxieties around pending test findings because all patients had received test results.
Implications of Findings for Clinicians, Researchers, Policymakers, Other Stakeholders
Our findings suggest several outcomes of imaging tests that are important to patients. The primary outcome was the knowledge gained from imaging tests. Patients reflected on physical experiences of tests and valued tests that produced information that direct care decisions and ease emotions. Also, previous imaging test experiences and encounters with medical staff influenced patients’ perceptions of the quality of care.
There seems to be a disconnect between current studies evaluating imaging tests and what patients care about, given that at least some of these outcomes are not routinely measured or included in clinical decision-making guidelines about tests. To fully capture the potential benefits and risks of imaging studies, researchers need to derive consistent ways to identify and measure a broader set of outcomes alongside accuracy measures.
In clinical practice, discussing with patients why a test is being ordered, what the other options are (including other tests, or not testing at all), and how the information gained will inform care can facilitate improvements in the decision-making process and set clearer expectations of imaging [5]. Additional research into improving patient understanding about diagnostic imaging tests should be a priority. Overall, our results suggest that the full range of risks and benefits that patients perceive from imaging testing is more complex than “test accuracy” alone.
TAKE-HOME POINTS.
Knowledge gained from imaging tests, contributions to the health care journey, direct experiences during testing, and impacts on emotions are all PCOs that should be considered when evaluating and reporting imaging tests.
Above and beyond accuracy measures, researchers need to derive consistent ways to identify and measure a broader set of PCOs.
Additional research into improving patient understanding about diagnostic imaging tests should be a priority.
ACKNOWLEDGMENTS
The authors acknowledge the support and contributions of the PROD Study Team, a body of stakeholders, study site champions and coordinators, and researchers. We also acknowledge Jessica Cruz, Sabrina Billon, Jordan Tuia, Shen Yan for their assistance with data cleaning, as well as our participants whose time and stories made this work possible.
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Program Award (ME-1503-29245). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the PCORI, its Board of Governors, or Methodology Committee.
This study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1 TR002319. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors state that they have no conflict of interest related to the material discussed in this article.
REFERENCES
- 1.Rui P, Hing E, Okeyode T. National ambulatory medical care survey: 2014 state and national summary tables. 2014. Available at: https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf Accesssed March 15, 2018.
- 2.Squires D, Anderson C. U.S. health care from a global perspective: spending, use of services, prices, and health in 13 countries. Commonwealth Fund; Published October 8, 2015. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2015/oct/us-health-care-from-a-global-perspective Accesssed March 22, 2018. [PubMed] [Google Scholar]
- 3.The Good Stewardship Working Group. The “top 5” lists in primary care. Arch Intern Med 2011;171:1385–9. [DOI] [PubMed] [Google Scholar]
- 4.ABIM Foundation. Unnecessary tests and procedures in the health care system: what physicians say about the problem, the causes, and the solutions. Available at:. http://www.choosingwisely.org/wp-content/uploads/2015/04/Final-Choosing-Wisely-Survey-Report.pdf Accesssed March 20, 2018.
- 5.Wolfson D, Santa J, Slass L. Engaging physicians and consumers in conversations about treatment overuse and waste: a short history of the Choosing Wisely Campaign. Acad Med 2014;89:990–5. [DOI] [PubMed] [Google Scholar]
- 6.Project of the ABIM Foundation, ACP–ASIM Foundation, and European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med 2002;136: 243–6. [DOI] [PubMed] [Google Scholar]
- 7.The ACR Task Force on Appropriateness Criteria. ACR Appropriateness Criteria Overview. 2015;1–3. Available at: https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria/Overview Accessed May 22, 2018.
- 8.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991;11:88–94. [DOI] [PubMed] [Google Scholar]
- 9.Lijmer JG, Leeflang M, Bossuyt PMM. Proposals for a phased evaluation of medical tests. Med Decis Making 2009;29:E13–21. [DOI] [PubMed] [Google Scholar]
- 10.Carlos RC, Buist DSM, Wernli KJ, Swan JS. Patient-centered outcomes in imaging: quantifying value. J Am Coll Radiol 2012;9:725–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fleurence R, Whicher D, Dunham K, Gerson J, Newhouse R, Luce B. The patient-centered outcomes research institute’s role in advancing methods for patient-centered outcomes research. Med Care 2015;53:2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agapova M, Bresnahan BB, Higashi M, Kessler L, Garrison LP, Devine B. A proposed approach for quantitative benefit-risk assessment in diagnostic radiology guideline development: the American College of Radiology Appropriateness Criteria Example. J Eval Clin Pract 2017;23:128–38. [DOI] [PubMed] [Google Scholar]
- 13.Bossuyt PMM, McCaffery K. Additional patient outcomes and pathways in evaluations of testing. Med Decis Making 2009;29:E30–8. [DOI] [PubMed] [Google Scholar]
- 14.Harris RP, Sheridan SL, Lewis CL, Barclay C, Vu MB, Kistler CE, et al. The harms of screening. JAMA Intern Med 2014;174:281. [DOI] [PubMed] [Google Scholar]
- 15.Ferrante di Ruffano L, Hyde CJ, McCaffery KJ, Bossuyt PMM, Deeks JJ. Assessing the value of diagnostic tests: a framework for designing and evaluating trials. BMJ 2012;344:e686. [DOI] [PubMed] [Google Scholar]
- 16.Sabbatini AK, Merck LH, Froemming AT, et al. Optimizing patient-centered communication and multidisciplinary care coordination in emergency diagnostic imaging: a research agenda. Acad Emerg Med 2015;22:1427–34. [DOI] [PubMed] [Google Scholar]
- 17.O’Reilly M, Parker N. “Unsatisfactory saturation”: a critical exploration of the notion of saturated sample sizes in qualitative research. Qual Res 2013;13:190–7. [Google Scholar]
- 18.Saldana J The Coding Manual for Qualitative Researchers. London: SAGE Publications; 2009. [Google Scholar]
- 19.Macqueen K, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cultural Anthropology Methods 1998;10:31–6. [Google Scholar]
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 21.Attride-Stirling J Thematic networks: an analytic tool for qualitative research. Qual Res 2001;1:385–405. [Google Scholar]
- 22.Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health systems. JAMA 2012;307:2400–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ollivier L, Leclère J, Dolbeault S, Neuenschwander S. Doctor-patient relationship in oncologic radiology. Cancer Imaging 2005;5:83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elena R, Evaluation T. GRADE: grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008;336:1106–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ. GRADE: what is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y. GRADE: going from evidence to recommendations. BMJ 2008;336:1049–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwartz LM. Enthusiasm for cancer screening in the United States. JAMA 2004;291:71–8. [DOI] [PubMed] [Google Scholar]
- 29.Schwartz LM, Woloshin S, Sox HC, Fischhoff B, Welch HG. US women’s attitudes to false-positive mammography results and detection of ductal carcinoma in situ: cross-sectional survey. BMJ 2000;320: 1635–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brewer NT, Salz T, Lillie SE. Systematic review: the long-term effects of false-positive mammograms. Ann Intern Med 2007;146:502–10. [DOI] [PubMed] [Google Scholar]
- 31.Thornton RH, Dauer LT, Shuk E, et al. Patient perspectives and preferences for communication of medical imaging risks in a cancer care setting. Radiology 2015;275:545–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Evans R, Taylor S, Janes S, et al. Patient experience and perceived acceptability of whole-body magnetic resonance imaging for staging colorectal and lung cancer compared with current staging scans: a qualitative study. BMJ Open 2017;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Swan JS, Furtado VF, Keller LA, et al. Pilot study of a patient-centered radiology process model. J Am Coll Radiol 2017;14:274–81. [DOI] [PubMed] [Google Scholar]
- 34.Schleifer D, Rothman DJ. “The ultimate decision is yours”: exploring patients’ attitudes about the overuse of medical interventions. PloS One 2012;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Makanjee CR, Bergh AM, Hoffmann WA. Healthcare provider and patient perspectives on diagnostic imaging investigations. Afr J Prim Health Care Fam Med 2015;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Undeland M, Malterud K. Diagnostic work in general practice: more than naming a disease. Scand J Prim Health Care 2002;20:145–50. [DOI] [PubMed] [Google Scholar]
- 37.Van Ravesteijn H, Van Dijk I, Darmon D, et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns 2012;86:3–8. [DOI] [PubMed] [Google Scholar]
- 38.Carlin LE, Smith HE, Henwood F. To see or not to see: a qualitative interview study of patients’ views on their own diagnostic images. BMJ Open 2014;4:e004999. [DOI] [PMC free article] [PubMed] [Google Scholar]


