ABSTRACT
Background
The Dietary Guidelines for Americans (DGAs) provide dietary recommendations for the general population with the intent of preventing chronic disease such as cardiovascular disease. An evaluation of whether updated versions of the DGAs accomplish this goal is lacking.
Objective
The objective of this project was to determine whether updates to DGAs over time, reflected in subsequent versions of diet quality indices, strengthened the associations between diet quality and risk of cardiovascular disease outcomes.
Methods
Dietary data collected using an FFQ in the Framingham Heart Study Offspring cohort were used to assess adherence to sequential versions of the Healthy Eating Index (HEI) (1990, 2005, 2010, and 2015) and Alternative HEI (2000 and 2010) (n = 3267). We conducted prospective analyses using Cox regression to estimate the associations between diet indices and incident cardiovascular disease outcomes.
Results
Among the 3267 study participants, 54% were female, mean age was 55 y, and BMI was 27 kg/m2. There were a total of 544 events for the composite outcome of cardiovascular diseases (324 coronary artery disease events, 153 stroke events, and 187 heart failure events). Adherence to any dietary index was inversely associated with risk of cardiovascular disease, coronary artery disease, and heart failure, but not stroke. Compared with HEI-1990, scores for the more recent diet indices were more strongly associated with coronary artery disease risk, but not cardiovascular disease, heart failure, or stroke.
Conclusions
More recent iterations of diet indices, reflecting updates to the DGAs over time, are more strongly associated with risk of incident coronary artery disease than the original diet index (HEI-1990).
Keywords: diet, cardiovascular disease, coronary artery disease, heart failure, stroke
Introduction
All federally funded food programs (e.g., school lunch program, military food service, Supplemental Nutritional Assistance Program, Women and Infants Care) and nutrition education programs must adhere to the US Dietary Guidelines for Americans (DGAs). As such, they have the potential to influence population-wide food consumption. The USDA and US Department of Health and Human Services jointly oversee an update of these guidelines every 5 y to keep them consistent with the most recent evidence on dietary intake and health, with a major focus on chronic disease risk reduction, primarily cardiovascular diseases, the major cause of death in the United States (1, 2).
Subsequent to the publication of DGAs, diet quality indices are created that can be used to assess adherence to the dietary guidelines. These diet quality indices are updated concurrently with updating of the DGAs every 5 y. These adherence measures represent an attempt to quantify diet quality, because they are designed to reflect constituents of a healthy diet based on the available nutrition science at the time (3). The Dietary Patterns Methods Project found that higher diet quality, assessed using both the Healthy Eating Index (HEI)-2010 and the Alternative Healthy Eating Index (AHEI)-2010, was associated with a reduced risk of cardiovascular mortality and all-cause mortality in several cohorts (4). However, the Dietary Patterns Methods Project was limited to the 2010 versions of the HEI and AHEI and did not evaluate either prior or subsequent iterations of the diet quality indices.
The objective of this project was to determine whether updates to DGAs over time, reflected in subsequent versions of diet quality indices, strengthened the associations between diet quality and risk of cardiovascular disease outcomes.
Methods
Study population
The present study was conducted using data from the Framingham Heart Study (FHS) Offspring cohort (5). The FHS Offspring cohort was recruited starting in 1971 and consists of the children and spouses of children of the original FHS cohort participants. The primary objectives of the FHS Offspring cohort were to study cardiovascular disease incidence and prevalence and risk factors for cardiovascular disease and to examine patterns of risk factors within families (5). After enrollment, FHS Offspring cohort study participants underwent standardized examinations, provided medical histories every 4 to 8 y, and were followed for the occurrence of cardiovascular events and mortality. Written informed consent was obtained from study participants and procedures were approved by the Boston University Medical Center Institutional Review Board. The present analysis was approved by the Johns Hopkins Bloomberg School of Public Health and Tufts University Institutional Review Boards.
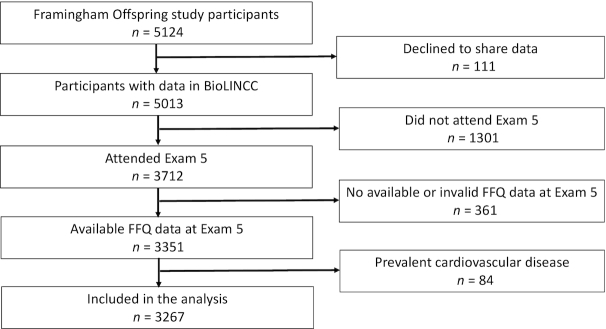
The entire FHS Offspring cohort was eligible for inclusion in the analysis (n = 5124) (Figure 1). We excluded those individuals who declined storage of their data in the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository Information Coordinating Center (n = 111), those who did not attend Exam 5 (n = 1301), those with missing dietary data (n = 361), and those with prevalent cardiovascular disease at Exam 5 (n = 84). The final sample size for the present analysis was 3267.
FIGURE 1.
Flowchart of study participant selection. BioLINCC, Biologic Specimen and Data Repository Information Coordinating Center.
Exposures
The Harvard semiquantitative FFQ, which has been validated against diet records and biomarkers in other study populations, was used to estimate dietary intake (6, 7). The FFQ was administered at Exam 5 (conducted in 1991 to 1995), which was considered baseline for the prospective analysis. We used data on reported frequency of food and beverage intake and derived nutrient data. These dietary data were then used to assess adherence to the DGAs using established criteria for different versions of the HEI, HEI-1990, HEI-2005, HEI-2010, and HEI-2015, and AHEI, AHEI-2000 and AHEI-2010, as previously described (8–12). The participants were not advised to adhere to a particular dietary pattern, but rather the term adherence is used to represent the consistency of participant diets with the DGAs according to the established criteria of the diet quality indices.
Covariates
Covariates were measured at Exam 5 (1991–1995). Multivariable regression models were adjusted for the following confounding factors: age, sex, cigarette smoking, BMI, diabetes status, hypertension status, HDL cholesterol, non-HDL cholesterol, total energy intake, antihypertensive medication, and lipid-lowering medication.
Outcomes
The primary outcome was incident cardiovascular disease, defined as a composite of coronary artery disease, stroke, and heart failure, which were ascertained from Exam 5 (1991–1995) through December 31, 2010. The secondary outcomes were incident coronary artery disease, incident stroke, and incident heart failure as separate outcomes.
Statistical analysis
The components and construction of the dietary guideline adherence indices were compared, identifying factors that have remained stable through the years and those that have been eliminated or added over time. The scoring system for each index was applied according to the methods used by the investigators who developed these established indices (8–12). Descriptive statistics were used to describe dietary adherence (mean and range for each index) and characteristics of study participants according to tertiles of HEI-2015.
Adherence scores were related to incident cardiovascular disease using survival analysis to incorporate time to event. Cox proportional hazards regression models were adjusted for demographics (age, sex), health behaviors (cigarette smoking), anthropometry (BMI), additional established cardiovascular disease risk factors (diabetes status, hypertension status, HDL cholesterol, and non-HDL cholesterol), and medication use (antihypertensive and lipid-lowering). In addition, models were adjusted for total energy intake to account for extraneous variation introduced through the use of an FFQ to assess dietary intake (13). Seemingly unrelated regression (SUR) was used to compare coefficients from different Poisson regression models in order to determine whether the strength of association between diet indices and cardiovascular outcomes were stronger from more recent diet indices relative to the original HEI (1990) (14). We compared Poisson regression models which incorporated follow-up time since it is not possible to apply to seemingly unrelated regression analyses to Cox regression models. Stata statistical software version 14.2 was used for all analyses (StataCorp LLC).
Results
All 6 diet indices included similar components for total fruits and total vegetables (Table 1). Sodium was a component in all of the diet indices except for AHEI-2000. Older versions of diet indices assessed intake of total grains, whereas more recent versions separately assessed whole grains (or fiber) and refined grains. The original HEI (1990) assessed intake of protein as dairy and meat, but more recent versions used more nuanced categories for sources of protein to reflect intake of seafood, nuts, and plant protein (beans, soy protein, legumes) in addition to dairy as a separate category. HEI-1990 included components for total fat and cholesterol, whereas later versions of diet indices assessed subcatagories of fatty acids, including trans fat, saturated fat, polyunsaturated fat, and omega-3 fatty acids. Sugar consumption was assessed for all indices except for HEI-1990 but used different categories, i.e., added sugars, empty calories, discretionary calories, and sugar-sweetened beverages and fruit juice, reflecting the terminology of the DGA version at the time. Alcohol was a component of AHEI-2000 and AHEI-2010, but not for any version of HEI. The mean ± SD of the diet indices was 64.5 ± 9.6 for HEI-1990, 38.5 ± 10.3 for AHEI-2000, 65.5 ± 7.6 for HEI-2005, 50.3 ± 10.6 for AHEI-2010, 70.2 ± 8.6 for HEI-2010, and 68.3 ± 9.1 for HEI-2015.
TABLE 1.
Scores for food and nutrient components of dietary guideline adherence indices in the FHS Offspring cohort1
| Version of the dietary guideline adherence indices | ||||||
|---|---|---|---|---|---|---|
| Component | HEI-1990 | AHEI-2000 | HEI-2005 | AHEI-2010 | HEI-2010 | HEI-2015 |
| Total fruits | 6.8 ± 3.1 | 3.1 ± 2.4 | 4.2 ± 1.3 | 3.1 ± 2.4 | 4.2 ± 1.3 | 4.2 ± 1.3 |
| Whole fruits | 4.1 ± 1.5 | 4.1 ± 1.5 | 4.1 ± 1.5 | |||
| Total vegetables | 6.8 ± 2.8 | 5.2 ± 2.7 | 4.2 ± 1.2 | 5.2 ± 2.7 | 4.2 ± 1.2 | 4.4 ± 1.0 |
| Greens and beans | 3.7 ± 1.7 | 4.6 ± 0.9 | ||||
| Dark green and orange vegetables and legumes | 4.0 ± 1.4 | |||||
| Total grains | 5.6 ± 2.4 | 3.6 ± 1.1 | ||||
| Whole grains | 1.4 ± 1.4 | 1.5 ± 1.9 | 2.8 ± 2.8 | 2.8 ± 2.8 | ||
| Refined grains | 8.4 ± 2.7 | 8.4 ± 2.7 | ||||
| Fiber | 9.1 ± 1.6 | |||||
| Total protein foods | 2.2 ± 0.8 | 2.2 ± 0.8 | ||||
| Dairy/milk | 6.5 ± 3.2 | 6.0 ± 3.1 | 6.0 ± 3.1 | 6.0 ± 3.1 | ||
| Meat2 | 5.0 ± 2.3 | 3.7 ± 3.1 | 5.3 ± 3.0 | |||
| Meats and beans | 3.2 ± 1.3 | |||||
| Seafood and plant proteins | 2.5 ± 1.3 | 2.5 ± 1.3 | ||||
| Nuts and soy protein/legumes | 0.9 ± 1.7 | 5.5 ± 3.1 | ||||
| Oils3 | 2.1 ± 2.3 | |||||
| Total fat | 8.2 ± 2.5 | |||||
| Fatty acids4 | 5.4 ± 2.1 | 3.7 ± 2.5 | 3.7 ± 2.5 | |||
| Saturated fats | 7.5 ± 3.3 | 5.6 ± 3.0 | 6.6 ± 2.9 | |||
| Polyunsaturated fat | 4.8 ± 1.9 | |||||
| Trans fat | 7.2 ± 2.0 | 7.2 ± 2.0 | ||||
| Omega-3 fats | 7.0 ± 3.0 | |||||
| Cholesterol | 9.1 ± 2.3 | |||||
| Sodium | 9.1 ± 1.8 | 7.2 ± 1.8 | 4.5 ± 2.9 | 8.6 ± 1.8 | 8.6 ± 1.8 | |
| Added sugars | 10.0 ± 0.3 | |||||
| Empty/discretionary calories | 19.7 ± 1.5 | 19.7 ± 1.5 | ||||
| SSBs and fruit juice | 0.7 ± 2.5 | |||||
| Alcohol | 3.9 ± 3.9 | 5.4 ± 3.4 | ||||
| Total score | 64.5 ± 9.6 | 38.5 ± 10.3 | 65.5 ± 7.6 | 50.3 ± 10.6 | 70.2 ± 8.6 | 68.3 ± 9.1 |
Data presented are mean ± SD scores for each component and the total score. AHEI, Alternative Healthy Eating Index; FHS, Framingham Heart Study; HEI, Healthy Eating Index; SSB, sugar-sweetened beverage.
For AHEI-2000, meat was quantified as the ratio of white meat (poultry, fish) to red meat (beef, pork, lamb, processed meat). For AHEI-2010, only red and processed meat were scored.
Oils includes nonhydrogenated vegetable oils and oils in fish, nuts, and seeds.
For HEI-2010 and HEI-2015, fatty acids were quantified as the ratio of polyunsaturated fatty acids and monounsaturated fatty acids to saturated fatty acids. For AHEI-2000, fatty acids were quantified as the ratio of polyunsaturated fatty acids to saturated fatty acids.
In the overall study population (n = 3267), about half of the study participants were female (54.3%), the mean age was 54.5 y, and the mean BMI was 27.4 kg/m2 (Table 2). At higher tertiles of HEI-2015, participants were more likely to be female, older, and have a lower BMI, and were less likely to be current smokers. Participants at higher levels of adherence to HEI-2015 were more likely to have hypertension and to be using antihypertensive and lipid-lowering medication. The higher mean HDL cholesterol concentration in participants in the higher tertiles of HEI-2015 was observed among women but not among men.
TABLE 2.
Baseline characteristics according to tertile of HEI-20151
| Tertile of HEI-2015 | |||
|---|---|---|---|
| Characteristic | Tertile 1: 30.7–64.8 (n = 1059) | Tertile 2: 64.9–72.8 (n = 1059) | Tertile 3: 72.9–94.3 (n = 1059) |
| Female | 44.8% (474) | 54.6% (578) | 63.6% (673) |
| Age, y | 53.2 ± 9.8 | 54.1 ± 9.8 | 56.3 ± 9.4 |
| BMI, kg/m2 | 27.7 ± 4.9 | 27.5 ± 5.1 | 26.9 ± 4.8 |
| Current smoker | 28.9% (306) | 17.4% (184) | 10.3% (109) |
| Hypertension | 19.5% (205) | 20.9% (220) | 22.8% (240) |
| SBP, mmHg | 126 ± 18 | 125 ± 19 | 127 ± 19 |
| Antihypertensive medication use | 16.3% (172) | 18.4% (194) | 20.2% (213) |
| Hemoglobin A1c, % | 5.5 ± 1.1 | 5.4 ± 0.9 | 5.4 ± 1.0 |
| Diabetes | 6.2% (65) | 5.8% (61) | 7.9% (83) |
| Diabetes treatment | 2.9% (31) | 2.6% (27) | 3.7% (39) |
| Fasting glucose, mg/dL | 101 ± 27 | 100 ± 26 | 100 ± 27 |
| Lipid-lowering medication use | 4.3% (46) | 5.8% (61) | 8.5% (90) |
| Total cholesterol, mg/dL | 205 ± 36 | 204 ± 35 | 206 ± 38 |
| Non-HDL cholesterol, mg/dL | 156 ± 37 | 154 ± 37 | 154 ± 40 |
| Triglycerides, mg/dL | 150 ± 115 | 151 ± 118 | 141 ± 90 |
| HDL cholesterol,2 mg/dL | 48 ± 14 | 50 ± 15 | 52 ± 15 |
Data presented are % (n) or means ± SDs. HEI, Healthy Eating Index; SBP, systolic blood pressure.
Means ± SDs of HDL cholesterol concentrations for women were 55 ± 15, 56 ± 15, and 57 ± 15 mg/dL for tertiles 1, 2, and 3, respectively, and for men were 43 ± 11, 43 ± 12, and 43 ± 11 mg/dL for tertiles 1, 2, and 3, respectively.
Over a median follow-up of 17 y, there were 544 events for the composite outcome of cardiovascular diseases; 324 coronary artery disease events, 153 stroke events, and 187 heart failure events. For nearly all diet indices, there was a statistically significant inverse association with risk of the composite outcome of cardiovascular diseases, coronary artery disease, and heart failure after adjusting for age, sex, smoking, BMI, diabetes, hypertension, HDL cholesterol, non-HDL cholesterol, total energy intake, antihypertensive medication, and lipid-lowering medication (Table 3). For example, those in the highest tertile of adherence to HEI-2015 had a 32% lower risk of coronary artery disease than those in the lowest tertile (HR: 0.68; 95% CI: 0.51, 0.89; P value for trend across tertiles = 0.004). A 10-unit higher HEI-2015 score was associated with 17% lower risk of coronary artery disease (HR: 0.83; 95% CI: 0.74, 0.94). Results were similar for heart failure, e.g., a 10-unit higher score in more recent diet indices (AHEI-2010, HEI-2010, HEI-2015) was associated with 17–18% lower risk of heart failure. Results were also similar for the composite outcome of cardiovascular diseases in that a 10-unit higher score for all of the diet indices was significantly associated with a 10–13% lower risk of cardiovascular disease in the continuous analyses. In contrast, there were no significant associations between the diet indices and incident stroke.
TABLE 3.
Risk of cardiovascular disease outcomes according to tertile and continuous dietary guideline adherence indices1
| Tertile of dietary guideline adherence indices | ||||||
|---|---|---|---|---|---|---|
| Index | Tertile 1 | Tertile 2 | Tertile 3 | P-trend2 | Continuous (per 10 points) | P-difference3 |
| Cardiovascular disease4 | ||||||
| HEI-1990 | 1 [Ref] | 0.83 (0.68, 1.03) | 0.76 (0.61, 0.94) | 0.01 | 0.90 (0.82, 0.99) | — |
| AHEI-2000 | 1 [Ref] | 0.87 (0.71, 1.07) | 0.71 (0.57, 0.89) | 0.003 | 0.88 (0.80, 0.96) | 0.73 |
| HEI-2005 | 1 [Ref] | 0.94 (0.76, 1.17) | 0.75 (0.59, 0.94) | 0.01 | 0.87 (0.77, 0.99) | 0.32 |
| AHEI-2010 | 1 [Ref] | 0.81 (0.66, 0.99) | 0.77 (0.63, 0.96) | 0.02 | 0.90 (0.82, 0.98) | 0.87 |
| HEI-2010 | 1 [Ref] | 0.85 (0.69, 1.04) | 0.81 (0.65, 1.01) | 0.06 | 0.89 (0.81, 0.99) | 0.91 |
| HEI-2015 | 1 [Ref] | 0.76 (0.62, 0.94) | 0.73 (0.59, 0.91) | 0.004 | 0.87 (0.79, 0.96) | 0.40 |
| Coronary artery disease | ||||||
| HEI-1990 | 1 [Ref] | 1.07 (0.82, 1.40) | 0.96 (0.72, 1.27) | 0.76 | 0.97 (0.86, 1.09) | — |
| AHEI-2000 | 1 [Ref] | 0.99 (0.76, 1.27) | 0.61 (0.45, 0.82) | 0.002 | 0.84 (0.75, 0.95) | 0.03 |
| HEI-2005 | 1 [Ref] | 0.83 (0.63, 1.09) | 0.75 (0.56, 1.00) | 0.05 | 0.90 (0.77, 1.05) | 0.21 |
| AHEI-2010 | 1 [Ref] | 0.81 (0.62, 1.05) | 0.67 (0.50, 0.88) | 0.005 | 0.86 (0.77, 0.95) | 0.08 |
| HEI-2010 | 1 [Ref] | 0.71 (0.54, 0.93) | 0.67 (0.51, 0.89) | 0.004 | 0.84 (0.74, 0.95) | 0.04 |
| HEI-2015 | 1 [Ref] | 0.68 (0.52, 0.90) | 0.68 (0.51, 0.89) | 0.004 | 0.83 (0.74, 0.94) | 0.01 |
| Stroke | ||||||
| HEI-1990 | 1 [Ref] | 0.723 (0.49, 1.10) | 0.83 (0.56, 1.23) | 0.37 | 0.97 (0.81, 1.16) | — |
| AHEI-2000 | 1 [Ref] | 0.81 (0.54, 1.23) | 1.13 (0.75, 1.68) | 0.55 | 1.00 (0.84, 1.19) | 0.70 |
| HEI-2005 | 1 [Ref] | 1.15 (0.77, 1.71) | 0.79 (0.51, 1.22) | 0.27 | 0.88 (0.70, 1.10) | 0.26 |
| AHEI-2010 | 1 [Ref] | 0.82 (0.54, 1.23) | 1.06 (0.72, 1.57) | 0.74 | 1.00 (0.85, 1.17) | 0.67 |
| HEI-2010 | 1 [Ref] | 0.75 (0.50, 1.12) | 0.78 (0.52, 1.15) | 0.21 | 0.88 (0.73, 1.06) | 0.39 |
| HEI-2015 | 1 [Ref] | 0.84 (0.57, 1.24) | 0.70 (0.47, 1.05) | 0.09 | 0.88 (0.74, 1.05) | 0.28 |
| Heart failure | ||||||
| HEI-1990 | 1 [Ref] | 0.77 (0.53, 1.12) | 0.77 (0.54, 1.12) | 0.19 | 0.88 (0.75, 1.04) | — |
| AHEI-2000 | 1 [Ref] | 0.87 (0.61, 1.24) | 0.79 (0.54, 1.15) | 0.22 | 0.85 (0.73, 1.00) | 0.85 |
| HEI-2005 | 1 [Ref] | 0.79 (0.55, 1.13) | 0.69 (0.47, 1.00) | 0.05 | 0.81 (0.66, 1.00) | 0.53 |
| AHEI-2010 | 1 [Ref] | 0.71 (0.50, 1.01) | 0.66 (0.46, 0.94) | 0.02 | 0.83 (0.72, 0.96) | 0.62 |
| HEI-2010 | 1 [Ref] | 0.62 (0.43, 0.89) | 0.63 (0.44, 0.90) | 0.01 | 0.83 (0.70, 0.98) | 0.72 |
| HEI-2015 | 1 [Ref] | 0.48 (0.33, 0.70) | 0.65 (0.46, 0.91) | 0.01 | 0.82 (0.70, 0.96) | 0.46 |
Data presented as HRs (95% CIs) were calculated from multivariable adjusted Cox proportional hazard regression models adjusted for demographics (age, sex), health behaviors (cigarette smoking), anthropometrics (BMI), health status (diabetes status, hypertension status, HDL cholesterol, and non-HDL cholesterol), total energy intake, antihypertensive medication, and lipid-lowering medication. AHEI, Alternative Healthy Eating Index; HEI, Healthy Eating Index.
P value from test of trend across tertiles.
P value for seemingly unrelated regression for the dietary guideline adherence index compared with HEI-1990.
Cardiovascular disease is a composite outcome consisting of coronary artery disease, stroke, and heart failure.
In terms of the strength of the association, the more recent diet indices were similarly associated with cardiovascular disease, stroke, and heart failure relative to HEI-1990 (SUR P values for difference >0.05) (Table 3). AHEI-2000 (SUR P value for difference = 0.03), HEI-2010 (SUR P value for difference = 0.04), and HEI-2015 (SUR P value for difference = 0.01) were more strongly associated with coronary artery disease than HEI-1990, whereas HEI-2005 (SUR P value for difference = 0.21) and AHEI-2010 (SUR P value for difference = 0.08) were similar to HEI-1990 with respect to the strength of the association with coronary artery disease.
Discussion
In this prospective study of 3267 adult men and women in the FHS Offspring cohort, we found that more recent versions of the diet indices designed to evaluate diet quality on the basis of adherence to the DGAs (HEI-2010, HEI-2015, and AHEI-2000) were more strongly associated with incident coronary artery disease than the original HEI (HEI-1990). The more recent versions of the diet indices were not significantly different in the strength of their association with the other outcomes, including the composite outcome of cardiovascular diseases, stroke, and heart failure.
Our findings are consistent with a recent analysis in the Atherosclerosis Risk in Communities study demonstrating a 16% lower risk of cardiovascular disease for those in the highest compared with the lowest quintile, and similar results were reported for AHEI-2010, the alternative Mediterranean diet score, and the Dietary Approaches to Stop Hypertension (DASH) diet score (15). Aside from this 1 publication that included HEI-2015, to our knowledge prior work on this topic has been limited to comparing the 2010 versions of the HEI and AHEI scores, DASH diet score, and alternative Mediterranean diet score in multiple cohorts, including the NIH-American Association of Retired Persons (AARP) Diet and Health Study, the Multiethnic Cohort, and the Women's Health Initiative-Observational Study (4). The results of these studies were qualitatively similar for the diet indices and mortality across cohorts, with higher diet quality associated with lower risk of cardiovascular mortality and all-cause mortality. Our findings, using scores updated over time to reflect modifications in the DGAs, were similar to those of these previous studies in that higher adherence to the diet scores were associated with lower risk of incident cardiovascular disease, coronary artery disease, and heart failure events, particularly for the newer versions of the diet indices.
In the present study, we focused on several cardiovascular disease outcomes, given the clinical significance of these endpoints and the high quality of data collection for these outcomes, as a primary focus of the FHS. However, it is important to note that the DGAs were created to optimize health and reduce disease risk from not only cardiovascular disease but also other outcomes of concern. These health priorities have changed over time, with a more recent focus on achieving energy balance and a healthy eating pattern, and preventing chronic disease events in response to changes in diet-related health concerns in the United States (2, 16).
An interesting finding in the present analysis was that more recent indices—specifically, AHEI-2000, HEI-2010, and HEI-2015—were more strongly associated with coronary artery disease than the original index that assessed adherence to the DGAs (HEI-1990). This observation may be due to the fact that more recent indices preferentially represent dietary components that are related to coronary artery disease risk. Coronary artery disease is highly prevalent and the primary cause of cardiovascular death in the United States, and coronary artery disease may be the predominant outcome in the body of scientific literature on diet and cardiovascular disease on which the DGAs were designed (17). The stronger associations with coronary artery disease with later indices compared with HEI-1990 may have also been in part due to the structural changes in the indices, which are described below.
By applying all available diet indices of the DGAs to a single dataset, we were able to compare composition and scoring of the diet indices over time. Total fruits and total vegetables have consistently been a component in all indices, and sodium was a component of nearly all diet indices. In contrast, the manner by which grains, types of protein, types of fat, and so-called “empty calories” were classified changed over the time period assessed. The diet indices have also differed in how they incorporate total energy intake, by using different thresholds for number of servings in the case of HEI-1990, by using nutrient density estimates of each component (e.g., grams of nutrient per 1000 kcal; percentage of total energy contributed by that nutrient) in the case of HEI-2005, HEI-2010, and HEI-2015, or by not incorporating total energy intake in the case of AHEI-2000 and AHEI-2010. Another important difference is that the weights assigned to each variable (components of the diet indices) were different. The diet indices may be more strongly associated with cardiovascular disease risk and other outcomes by weighting the components of the scores based on the strength of their association with chronic disease outcomes, similar to how current cardiovascular disease risk calculators are created (18).
More recent versions of the DGAs, and the 2015–2020 edition in particular, have emphasized eating patterns more so than individual food groups and nutrients (19). However, the HEI and AHEI quantify intake of foods and nutrients. Similarly, other diet scores, such as the DASH diet, Mediterranean diet, and plant-based diet, might also be appropriate indices for assessing adherence to the more recent guidelines (20–27).
The main strength of the present study was that we quantified all 6 available versions of the HEI and AHEI to assess adherence to the DGAs within a single population. This approach allowed for a direct comparison of these indices in terms of their scoring strategies and their association with multiple cardiovascular outcomes. Extensive long-term follow-up information was available on the study participants, which allowed for the ascertainment of a substantial number of events for multiple cardiovascular disease outcomes. However, there were fewer stroke events than heart failure and coronary artery disease events. While the magnitudes of the associations between some diet indices and stroke were similar to those for coronary artery disease, the CIs were wider for stroke. Future research in studies with more stroke events may be useful to determine whether our observed associations between diet indices and other cardiovascular disease outcomes can be extended to stroke. We were able to account for multiple potential confounding factors using rigorously collected data on baseline characteristics of the study participants. However, diet quality is correlated with other health behaviors, and we may not have been able to adequately measure and account for these related confounding factors. As is the case for any observational study, we cannot rule out the possibility of residual confounding explaining at least part of the observed associations. Since the present study was conducted in a single cohort of participants from a single study site, the external validity of the findings is limited to primarily Caucasian US men and women with similar characteristics.
In conclusion, more recent iterations of diet indices, reflecting updates to the DGAs over time, were more strongly associated with incident coronary artery disease than the original diet index (HEI-1990). The indices developed to assess adherence to the DGAs may not sufficiently reflect modifications to the DGAs over time, which have primarily consisted of more nuanced classifications of protein sources, degree of grain refinement, types of fats, and inclusion of empty calories. Development and adjudication of alternate approaches to assess adherence to the DGAs by modifying the weights of individual food components or restructuring to assess overall dietary patterns might improve their usefulness.
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—CMR, JM, PFJ, DL, AHL: designed the research; CMR, HK: performed the statistical analysis; CMR: wrote the paper; AHL: supervised the study; HK, JM, PFJ, DL, AHL: critically revised the paper; CMR, AHL: had primary responsibility for final content; and all authors: read and approved the final manuscript.
Notes
Supported by the NIH National Heart, Lung, and Blood Institute (NHLBI) Framingham Heart Study NHLBI contract number HHSN268201500001I with additional support from other sources. This current work was also supported in part by the US Department of Agriculture–Agricultural Research Service (ARS) agreement number 58-1950-4-003.
Author disclosures: CMR was supported by a Mentored Research Scientist Development Award from the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK107782) and a grant from the National Heart, Lung, and Blood Institute (R21 HL143089). All other authors report no conflicts of interest.
Abbreviations used: AHEI, Alternative Healthy Eating Index; DASH, Dietary Approaches to Stop Hypertension; DGAs, Dietary Guidelines for Americans; FHS, Framingham Heart Study; HEI, Healthy Eating Index; SUR, seemingly unrelated regression.
References
- 1. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, et al.. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–492. [DOI] [PubMed] [Google Scholar]
- 2. Jahns L, Davis-Shaw W, Lichtenstein AH, Murphy SP, Conrad Z, Nielsen F. The history and future of dietary guidance in America. Adv Nutr. 2018;9:136–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Krebs-Smith SM, Subar AF, Reedy J. Examining dietary patterns in relation to chronic disease: matching measures and methods to questions of interest. Circulation. 2015;132:790–3. [DOI] [PubMed] [Google Scholar]
- 4. Liese AD, Krebs-Smith SM, Subar AF, George SM, Harmon BE, Neuhouser ML, Boushey CJ, Schap TE, Reedy J. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145:393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281–90. [DOI] [PubMed] [Google Scholar]
- 6. Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135:1114–26.; discussion 27–36. [DOI] [PubMed] [Google Scholar]
- 7. Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69:243–9. [DOI] [PubMed] [Google Scholar]
- 8. Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95:1103–8. [DOI] [PubMed] [Google Scholar]
- 9. Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, Kahle LL, Krebs-Smith SM. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113:569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108:1896–901. [DOI] [PubMed] [Google Scholar]
- 11. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Krebs-Smith SM, Pannucci TE, Subar AF, Kirkpatrick SI, Lerman JL, Tooze JA, Wilson MM, Reedy J. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118:1591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–8S.; discussion 9S–31S. [DOI] [PubMed] [Google Scholar]
- 14. Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stat Assoc. 1962;57:348–68. [Google Scholar]
- 15. Hu EA, Steffen LM, Coresh J, Appel LJ, Rebholz CM. Adherence to the Healthy Eating Index-2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr. 2019. [E-published ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmaco-economics. 2015;33:673–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al.. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 18. Goff DC Jr., Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, et al.. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–73. [DOI] [PubMed] [Google Scholar]
- 19. US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2015–2020. Washington, DC: US Government Printing Office; 2015. [Google Scholar]
- 20. Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–20. [DOI] [PubMed] [Google Scholar]
- 21. Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, Rexrode KM, Rimm EB, Hu FB. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. 2017;70:411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–608. [DOI] [PubMed] [Google Scholar]
- 23. Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N, Willett WC, Hu FB. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82:163–73. [DOI] [PubMed] [Google Scholar]
- 24. Miller PE, Cross AJ, Subar AF, Krebs-Smith SM, Park Y, Powell-Wiley T, Hollenbeck A, Reedy J. Comparison of 4 established DASH diet indexes: examining associations of index scores and colorectal cancer. Am J Clin Nutr. 2013;98:794–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Salas-Salvado J, Guasch-Ferre M, Lee CH, Estruch R, Clish CB, Ros E. Protective effects of the Mediterranean diet on type 2 diabetes and metabolic syndrome. J Nutr. 2016; 146:920S–7S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Grams ME, Coresh J, Rebholz CM. Plant-based diets and incident CKD and kidney function. Clin J Am Soc Nephrol. 2019;14:682–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Martinez-Gonzalez MA, Sanchez-Tainta A, Corella D, Salas-Salvado J, Ros E, Aros F, Gomez-Gracia E, Fiol M, Lamuela-Raventos RM, Schroder H, et al.. A provegetarian food pattern and reduction in total mortality in the Prevencion con Dieta Mediterranea (PREDIMED) study. Am J Clin Nutr. 2014;100:Suppl 1:320S–8S. [DOI] [PubMed] [Google Scholar]