Abstract
Purpose
Bilateral acute iris depigmentation (BADI) and transillumination (BATI) syndromes have been linked with the use of antibiotics, especially fluoroquinolones. They are characterized by acute onset of pigment dispersion in the anterior chamber, depigmentation of the iris and pigment deposition in the angle and in the posterior surface of the cornea (BADI), with iris transillumination defects and atonic pupil with sphincter paralysis (BATI). The purpose of this paper is to report the development of clinical depigmentation and iris damage similar to BADI and BATI in patients who had undergone uneventful glaucoma surgery with intracameral moxifloxacin as prophylaxis for endophthalmitis.
Observations
Four patients who had undergone Ex-Press implantation (cases 1 and 2) or non-penetrating deep sclerotomy (cases 3 and 4) developed asymptomatic pigment dispersion in the anterior chamber, which cleared after treatment with topical corticosteroids and NSAIDS. However, pupillary damage ensued, with mid-midriasis and pigment deposition under the filtration bleb.
Conclusions and importance
This is, to the best of our knowledge, the first report of acute unilateral iris depigmentation and transillumination after intracameral use of moxifloxacin. Moxifloxacin's toxic effect may have been promoted by the subconjuntival mitomycin employed to prevent scarring at the filtration bleb. Surgeons should be aware of these potential side-effects of drugs used as widely as moxifloxacin and mitomycin.
Keywords: Intracameral moxifloxacin, Glaucoma surgery, Acute iris transillumination, Acute iris depigmentation, Mitomycin
Highlights
-
•
Moxifloxacin is widely used as prophylaxis for endophthalmitis after cataract surgery.
-
•
Bilateral acute iris depigmentation and transillumination syndromes have been reported after the use of antibiotics.
-
•
We report four cases of similar syndromes in patients undergoing glaucoma surgery after intracameral moxifloxacin.
1. Introduction
Bilateral acute iris depigmentation (BADI) and bilateral acute iris transillumination (BATI) syndromes have been linked with the use of systemic antibiotics, most frequently fluoroquinolones.1, 2, 3 BADI is characterized by acute onset of pigment dispersion in the anterior chamber, depigmentation of the iris and pigment deposition in the angle and in the posterior surface of the cornea.1,2 Patients with BADI usually complain of red eye, pain and photophobia. In BATI, in addition to these findings, there are clinically evident iris transillumination defects and atonic pupil with sphincter paralysis.
More recently, unilateral cases of pigment dispersion similar to BADI and BATI have been reported after topical treatment with moxifloxacin.4 However, no cases have been reported up-to-date after intracameral use of moxifloxacin. The purpose of this paper is to report the development of clinical depigmentation and iris damage in patients who had undergone uneventful glaucoma surgery with intracameral moxifloxacin as prophylaxis for endophthalmitis. Institutional review board approval was obtained and informed consent for patient information and images to be published was provided by the patients.
2. Findings
2.1. Case 1
A 52 year old man was diagnosed in 2010 with bilateral open-angle glaucoma. In September 2012 he underwent Ex-press shunt, P50 model (Alcon Laboratories, Fort Worth, TX, USA), implantation due to visual field progression in his left eye. A fornix-based conjunctival flap was made in the superior quadrant, then a 4 × 4 mm square-shaped scleral flap (of approximately one-third of the scleral thickness) was dissected 1.0 mm into the clear cornea. A surgical sponge soaked in 0.2 mg/ml mitomycin C was applied under the conjunctiva, over the scleral flap, for 90 s, followed by thorough irrigation with a balanced salt solution. A 1 mm clear-cornea temporal paracentesis was used to inject sodium hyaluronate 10 mg/mL into the anterior chamber. An incision into the anterior chamber parallel to the iris along the gray line was made with a 25-G needle under the scleral flap and the shunt was inserted using its applicator. The scleral flap was then closed with four 10–0 nylon sutures and the conjunctiva with 8–0 vicryl. At the end of the procedure, 0.1ml of 5mg/ml moxifloxacin was injected through the temporal paracentesis into the anterior chamber. Postoperative treatment prescribed was: moxifloxacin 5mg/ml 1 drop 4 times daily for ten days, diclofenac sodium 1mg/ml 1 drop three times daily for two weeks and prednisolone acetate 10mg/ml starting 6 times daily and tapered 1 drop per week.
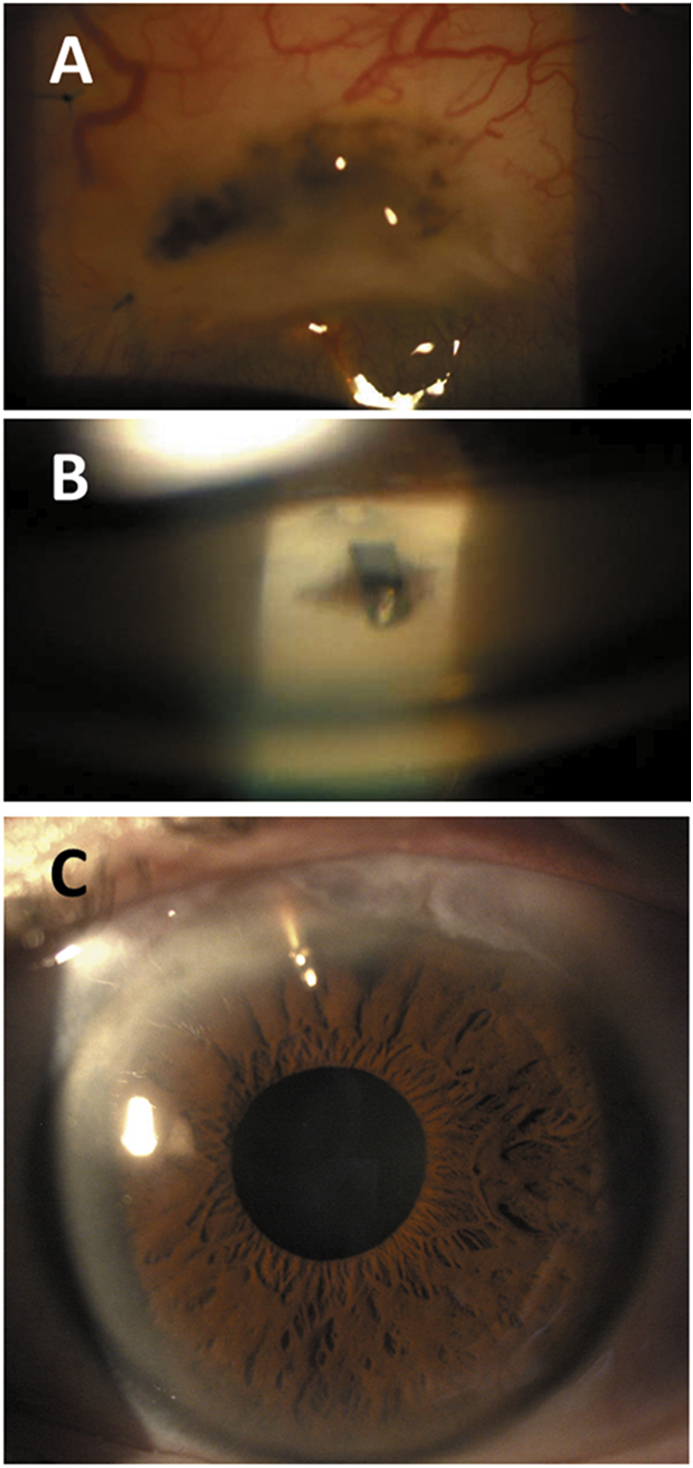
One month after surgery, in a scheduled follow-up visit, pigment was detected in the anterior chamber. The patient was instructed to continue treatment with prednisolone three times daily and to reinitiate diclofenac three times daily. Two weeks later, there was no pigment in the anterior chamber, but there was in the filtration bleb and in the angle surrounding the Ex-press shunt (Fig. 1a and b). Intraocular pressure was 9 mmHg and the patient remained asymptomatic. During follow-up, there have been no further episodes of pigment dispersion. In April 2019, corrected visual acuity was 20/20 and intraocular pressure was 10 mmHg with no treatment. The left pupil was slightly dilated and the iris responded sluggishly to light (Fig. 1c).
Fig. 1.
Case 1. Six weeks after Ex-press filtration surgery and two weeks after detection of pigment dispersion, there was no pigment in the anterior chamber, but there was in the filtration bleb (A) and in the angle surrounding the shunt (B). Six years after surgery, the left pupil is slightly dilated and responds sluggishly to light, with no transillumination defects and a functioning filtration bleb (C).
2.2. Case 2
A 65 year-old man with chronic angle closure glaucoma in his left eye was scheduled for glaucoma surgery because he did not tolerate topical treatment. He underwent isolated Ex-press shunt implantation in February 2016 (since he had previously undergone cataract surgery in 2015). Surgery was performed as described above, with the same postoperative treatment regime.
There were no initial postoperative complications. One week after surgery, the anterior chamber was quiet and intraocular pressure was 6 mmHg. However, two weeks later there was ample pigment in the anterior chamber, with no other inflammatory signs. The patient was by then using only prednisolone 3 times daily; he was told to extend treatment for a further twenty days and to add cyclopentolate 10mg/ml one drop daily for one week. Five weeks after surgery, there was almost no free pigment in the anterior chamber, but there was pigment under the filtering bleb and the pupil was fixed in mid-dilation. Intraocular pressure was 10 mmHg. The patient has been followed-up regularly, with no new episodes of pigment dispersion or inflammation. In March 2019, he remained asymptomatic, corrected visual acuity was 20/25, intraocular pressure remained low with no treatment (14 mmHg), there remained slight pigmentation of the filtering bleb and pupil mid-dilation.
2.3. Case 3
A 76 year-old woman, who had been diagnosed with glaucoma in 2008, pseudophakic, with Fuchs corneal dystrophy, developed an allergic reaction to timolol and brimonidine and was unable to use brinzolamide due to a very low endothelial count. In November 2016 she underwent uneventful non-penetrating deep sclerotomy (NPDS) in her left eye. A corneal traction suture was placed before dissecting a superior fornix-based conjunctival flap. A 5 × 5 mm square superficial scleral flap was dissected at the superior quadrant and extended anteriorly 1 mm into clear cornea. Then mitomycin C was applied under the conjunctiva for 40 s. A second triangular scleral flap was cut, and dissection continued anteriorly, beyond Schlemm's canal to expose the trabeculo-Descemet membrane. A temporal 1-mm paracentesis was performed to decrease intraocular pressure. The inner wall of Schlemm's canal was peeled with a forceps and the deep scleral flap removed. A supra-ciliary hema implant (Esnoper V-2000, AJL Ophthalmic, Álava, Spain) was sutured in the scleral bed with a 10–0 nylon suture. The superficial scleral flap was closed with two Nylon sutures. At the end of the procedure, 0.1ml of 5mg/ml moxifloxacin was injected through the temporal paracentesis. Postoperative treatment was the same as for Ex-press implantation.
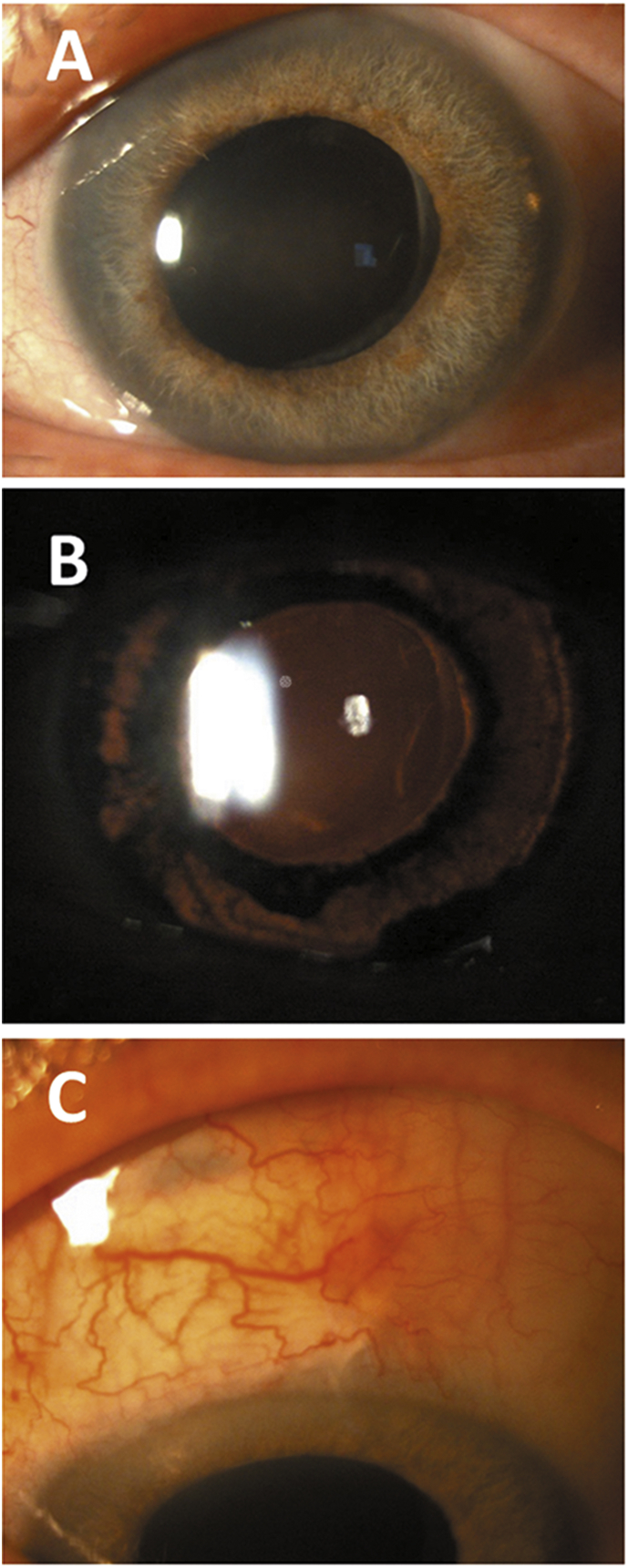
There was initial corneal edema which resolved after one week. At the one-month follow-up visit, there was pigment in the anterior chamber, significant pigment deposition on the endothelial surface in the visual axis, the iris was dilated and responded poorly to light (Fig. 2a). The patient was using prednisolone thrice daily and diclofenac thrice daily; she was instructed to increase prednisolone to one drop four times daily and to taper it slowly. Two weeks later there was no pigment in the anterior chamber. The iris remained unresponsive. Intraocular pressure was 14 mmHg without treatment and corrected visual acuity was 20/25. In February 2017, the patient was seen with an intraocular pressure of 42 mmHg due to the obstruction of the trabeculo-descemet membrane by pigment deposition. After laser goniopuncture, intraocular pressure dropped to 17 mmHg. The patient was last seen in November 2017. Corrected visual acuity was 20/32, intraocular pressure was 16 mmHg with latanoprost and timolol in a fixed combination and she was being treated with fluormetalone once daily and sodium chloride 5% thrice daily for her corneal decompensation due to Fuchs dystrophy. There was diffuse iris transillumination with a mid-dilated pupil and pigment deposition at the edge of the scleral window (Fig. 2b and c).
Fig. 2.
Case 3. (A) One month after uneventful non-penetrating deep-sclerotomy there was pigment in the anterior chamber, significant pigment deposition on the endothelial surface in the visual axis, the iris was dilated and responded poorly to light. One year after surgery, there was diffuse iris transillumination with a mid-dilated pupil (B) and pigment deposition at the edge of the scleral window (C).
2.4. Case 4
A 64 year-old woman, diagnosed with bilateral primary open-angle glaucoma in 2012, was scheduled for glaucoma surgery in her right eye due to visual field progression while treated with maximum topical treatment. In April 2019, NPDS was performed as described above.
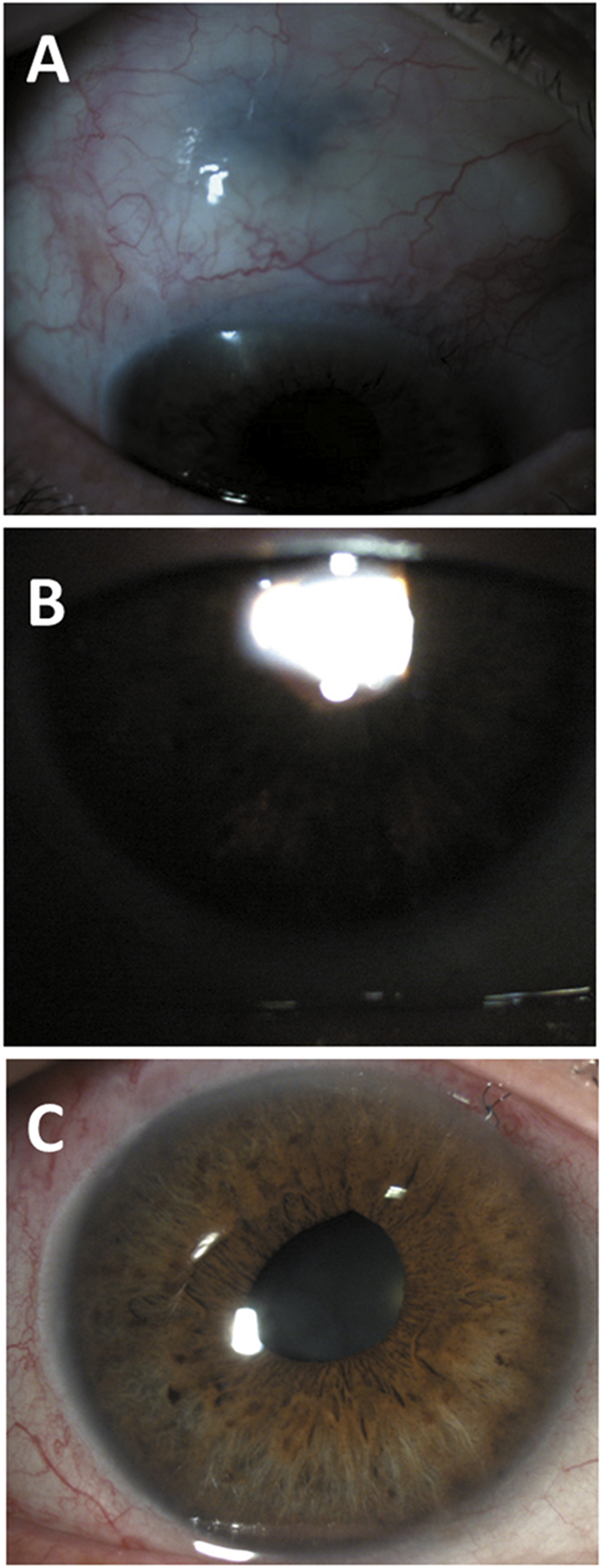
The early postoperative visits were unremarkable, but three weeks after surgery pigment was noted in the anterior chamber and under the filtration bleb. The patient was using prednisolone thrice daily. Diclofenac thrice daily was added. Six weeks after surgery, there was no pigment in the anterior chamber but plenty under the filtration bleb. Corrected visual acuity was 20/20 and intraocular pressure was 12 mmHg. Ten weeks after surgery, the anterior chamber remained quiet, with pigment under the filtration bleb (Fig. 3a), inferior transillumination defects (Fig. 3b), an irregular pupil (Fig. 3c) and controlled intraocular pressure with no topical hypotensive or anti-inflammatory treatment.
Fig. 3.
Case 4. Three weeks after uneventful non-penetrating deep sclerotomy, pigment was noted in the anterior chamber and under the filtration bleb. Ten weeks after surgery, the anterior chamber remained quiet, with pigment under the filtration bleb (A), inferior transillumination defects (B), an irregular pupil (C).
3. Discussion
BADI and BATI are clinical entities which have been reported after systemic use of antibiotics, especially fluorquinolones, which share the characteristic of intense pigment release into the anterior chamber. They differ in the main tissue affected: the iris stroma in BADI and the iris pigment epithelium in BATI. Recently, several cases of BADI have been reported after topical treatment with fluorquinolones (with no documented oral intake) with unilateral presentation.4
In this paper we report four cases of pigment dispersion similar to BADI (cases 1 and 2) and BATI (cases 3 and 4), which developed after uneventful glaucoma surgery with mitomycin C application and intracameral moxifloxacin. Topical moxifloxacin was also used as prophylaxis for endophthalmitis. Patients were asymptomatic, with pigment detected in the anterior chamber during scheduled follow-up visits. Pigment release ceased after 2–3 weeks of treatment with topical steroids and non-steroidal anti-inflammatory drugs, with pigment deposition in the filtration bleb. There were iris transillumination defects in two patients and pupillary damage in all cases, with different degrees of sphincter paralysis. In three cases pupillary mid-dilation did not affect visual acuity and the success of filtration surgery was not compromised. In case 3, the patient had advanced Fuchs dystrophy, which might have increased the clinical repercussion of pigment showering. Pigment deposition in the scleral window led to an intraocular pressure spike, which resolved after goniopuncture. However, in addition of pigment deposition, corneal damage progressed, leading to visual acuity worsening.
In contrast to previous reports on BADI and BATI, the patients in our series were initially asymptomatic and there were no intraocular pressure rises (except as commented in case 3). This was probably due to the fact that the patients were receiving treatment with topical steroids, which would have limited the inflammatory response to pigment dispersion.
The mechanism by which moxifloxacin might lead to pigment dispersion is unclear. Several reports have suggested that moxifloxacin might be toxic to iris melanocytes. Mahanty et al. evaluated the toxicity of topical moxifloxacin by measuring both the activity and the presence of the melanogenic enzyme tyrosinase (TYR) in aqueous humor specimens taken just before cataract surgery. Although there was no increase in TYR activity after treatment with moxifloxacin, immunoblotting analysis showed the presence of soluble TYR enzyme.5 The authors speculated that this might be due to the inhibitory effect moxifloxacin has on TYR activity. None of the patients in their series developed any clinically appreciable ocular side effects characteristic of BATI or BADI. Interestingly, the aqueous TYR activity within the group was quite variable possibly due to variability in the effective concentration of antibiotics on iris melanocyte toxicity among the patients.5
Perin et al. reported that moxifloxacin had a significant toxic effect on cultivated human iris pigment epithelium (hIPE) cells: at 100μg/mL, cell viability decreased to 84.12% relative to the control group.6 This toxicity effect increased with greater concentrations, and at 500μg/mL cell viability decreased to 59.09%. Moxifloxacin concentrations might come up to 150μg/mL with intracameral administration.6 However, there must clearly be some other factor influencing moxifloxacin toxicity, since no reports of BATI, BADI, or moxifloxacin-associated uveitis have been reported up-to-date following intracameral administration, in spite of the widespread use of moxifloxacin for endophthalmitis prevention after cataract surgery.7,8 We speculate that in our series, moxifloxacin toxicity may have been promoted by mitomycin C application.
Mitomycin C is used in glaucoma surgery to reduce fibroblast activity and postoperative scarring at the site of the scleral flap and the subconjunctival space. It reduces the relative risk of failure of trabeculectomy and leads to a lower intraocular pressure twelve months after filtration surgery compared to surgery performed with no antimetabolite application.9 Although mitomycin C use seems to lead to an increased risk of bleb leak, hypotony and endophthalmitis, no significant increase in permanent sight-threatening complications was detected in a 2015 Cochrane review.9 In a survey completed in 2016 by glaucoma surgeons, 97% reported using mitomycin C when performing trabeculectomy.10 In our center, patients undergoing isolated glaucoma surgery with mitomycin C also receive intracameral moxifloxacin to decrease the risk of endophthalmitis.
4. Conclusion
We report four cases of unilateral pigment dispersion, with iris transillumination defects in two of them, and pupillary mid-dilation after uneventful glaucoma surgery with intracameral moxifloxacin. It appears to be a rare side effect which develops in certain patients and of which glaucoma surgeons should be aware.
Patient consent
Informed consent for patient information and images to be published was provided by the patients.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments and Disclosures section
No funding or grant support. The Authors declare that there is no conflict of interest. All authors attest that they meet the current ICMJE criteria for Authorship.
References
- 1.Tugal-Tutkun I., Urgancioglu M. Bilateral acute depigmentation of the iris. Graefes Arch Clin Exp Ophthalmol. 2006;244(6):742–746. doi: 10.1007/s00417-005-0137-x. [DOI] [PubMed] [Google Scholar]
- 2.Tugal-Tutkun I., Araz B., Taskapili M. Bilateral acute depigmentation of the iris: report of 26 new cases and four-year follow-up of two patients. Ophthalmology. 2009;116(8):1552–1557. doi: 10.1016/j.ophtha.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 3.Tugal-Tutkun I., Onal S., Garip A. Bilateral acute iris transillumination. Arch Ophthalmol. 2011;129(10):1312–1319. doi: 10.1001/archophthalmol.2011.310. [DOI] [PubMed] [Google Scholar]
- 4.Kawali A., Mahendradas P., Shetty R. Acute depigmentation of the iris: a retrospective analysis of 22 cases. Can J Ophthalmol. 2019;54(1):33–39. doi: 10.1016/j.jcjo.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 5.Mahanty S., Kawali A.A., Dakappa S.S. Aqueous humor tyrosinase activity is indicative of iris melanocyte toxicity. Exp Eye Res. 2017;162:79–85. doi: 10.1016/j.exer.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perin A., Lyzogubov V., Bora N. In vitro assessment of moxifloxacin toxicity to human iris pigment epithelium. Invest Ophthalmol Vis Sci. 2015;56:5729. [Google Scholar]
- 7.Melega M.V., Alves M., Cavalcanti Lira R.P. Safety and efficacy of intracameral moxifloxacin for prevention of post-cataract endophthalmitis: randomized controlled clinical trial. J Cataract Refract Surg. 2019;45(3):343–350. doi: 10.1016/j.jcrs.2018.10.044. [DOI] [PubMed] [Google Scholar]
- 8.Bowen R.C., Zhou A.X., Bondalapati S. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: a meta-analysis. Br J Ophthalmol. 2018;102(9):1268–1276. doi: 10.1136/bjophthalmol-2017-311051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilkins M., Indar A., Wormald R. Intra-operative mitomycin C for glaucoma surgery. Cochrane Database Syst Rev. 2005;4 doi: 10.1002/14651858.CD002897.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vinod K., Gedde S.J., Feuer W.J. Practice preferences for glaucoma surgery: a survey of the American glaucoma society. J Glaucoma. 2017;26(8):687–693. doi: 10.1097/IJG.0000000000000720. [DOI] [PMC free article] [PubMed] [Google Scholar]