Abstract
Background: Specialist homeless primary health care services in the United Kingdom have arisen from the need for bespoke approaches to providing health care for people experiencing homelessness but descriptions of the design characteristics of homeless health services together with associated long-term condition (LTC) prevalence, health care utilization, and prescribing remain unexplored, thereby limiting our understanding of potential impact of service configuration on outcomes. Aim: Description of specialist homeless general practitioner services in Glasgow and Edinburgh, in terms of practice design (staff, skill mix, practice systems of registration, and follow-up); and exploration of the potential impact of differences on LTC prevalence, health care utilization, and prescribing. Method: Patient data were collected from computerized general practitioner records in Glasgow (2015, n = 133) and Edinburgh (2016, n = 150). Homeless health service configuration and anonymized patient data, including demographics, LTCs service utilization, and prescribing were summarized and compared. Results: Marked differences in infrastructure emerged between 2 practices, including the patient registration process, segmentation versus integration of services, recording systems, and the availability of staff expertise. Patient characteristics differed in terms of LTC diagnoses, health care utilization and prescribing. Higher rates of recorded mental health and addiction problems were found in Edinburgh, as well as higher rates of physical LTCs, for example, cardiovascular and respiratory conditions. There were significantly higher rates of consultations with nurses and other staff in Edinburgh, although more patients had consultations with pharmacists in Glasgow. Medication adherence was low in both cohorts, and attendance at referral appointments was particularly poor in Glasgow. Conclusion: Service design and professional skill mix influence recording of LTCs, service uptake, and identification and management of health conditions. Service configuration, professional skill mix, and resources may profoundly affect diagnoses, utilization of health care, and prescribing. Attention to homeless service design is important when providing care to this disadvantaged patient group.
Keywords: homeless health, primary care, service design, skill mix, long-term condition management
Introduction
People experiencing homelessness face extreme health inequities1 and Scottish data have shown that having ever been homeless significantly increases the risk of poor health and premature death for an individual, even when compared with never-homeless individuals from the most socioeconomically deprived areas.2 Large differences have been found in the prevalence of long-term conditions (LTCs) and health-related quality of life between homeless and housed individuals,3 with rates consistently raised across a range of LTCs, including infections, cardiovascular conditions, respiratory conditions, and mental health.1 Experiencing homelessness is an independent risk factor for mortality,4 with a median age of death of 51.6 years in a recent study, 20 years less than for patients living in the most socioeconomically deprived quintile of neighborhoods in England.5 There is evidence to suggest that lack of trust in health care providers and barriers to accessing health services persist,6,7 contributing to higher rates of health-harming behaviors, poorer disease control, and uncoordinated service utilization,8,9 including higher rates of unscheduled care use.10
Health services for this patient group have emerged either as specialist health centers, mainstream GP practices with homeless services or as mobile homeless health teams.11 These services generally include multidisciplinary health, social care, and addiction teams.11,12 In Scotland, specialist homeless primary care services exist in Edinburgh, Glasgow, and Aberdeen. There are more people experiencing homelessness in Glasgow and Edinburgh than in other Scottish cities. Glasgow dominates in terms of absolute numbers of people experiencing severe and multiple disadvantage, with double the number of cases of Edinburgh.13 In addition, Glasgow has recently experienced an unprecedented increase in the number of cases of HIV among people who are homeless and injecting drugs,14 and increases in drug-related deaths.15 Given the central importance of primary health care homelessness services to address the health needs of the population, we aimed to describe and compare the infrastructure (numbers and types of staff, approaches to registration and LTC management) of specialist homeless health services in Glasgow and Edinburgh, and explore the potential implications, for example, rates of detection and prescribing for LTCs, primary and secondary health care utilization.
Methods
The service configuration in specialist homelessness practices in Glasgow and Edinburgh was described based on professional key informant and routinely collected practice activity data, and compared.
The Edinburgh Access Practice is a specialist GP practice with services attached to it, whilst in Glasgow the specialist GP practice is one service within a number of different services, within the wider Homeless Health Service. Both are funded and run by their respective NHS health boards.
We then compared the characteristics of patients who were registered with the homeless GP practices in Glasgow and Edinburgh by analyzing patient level data from general practice records.
In both cities, data were extracted by transcribing anonymized information from practice computer systems onto a standardized Microsoft Excel data extraction template described previously16 on an encrypted NHS laptop. General practitioner (GP) practice systems in both cities comprised electronic records (EMIS17 in Glasgow and Vision18 in Edinburgh), which store demographic and clinical information about patient encounters, prescribing, referrals, and diagnoses. Both practices also used Docman,19 which stores correspondence from secondary care, social care and other services, for example, dietetics. Data extracted from EMIS/Vision included all relevant fields up to 1 year prior to the date of data collection. Data extracted from Docman included relevant fields over the previous 3 years. Collected data comprised demographics, acute and long-term conditions (LTCs), sexual health, addictions, prescribed medicines, service utilization, and social prescribing. Multimorbidity was recorded using the framework established by Barnett et al,20 with the increased burden from patients with more than 1 comorbidity of the same category, for example, 2 cardiovascular conditions, counted as multiple comorbidities. For prescribing, acute medicines were taken to be those coded under acute prescriptions on EMIS/Vision, and repeat medicines those coded under repeat prescriptions on EMIS/Vision. Medicine continuity was recorded using the number of times a medication prescription for LTCs (indicated for the patient’s LTC management and included in the Quality and Outcomes Framework [QOF] contract),21 was issued from EMIS/Vision in the respective 1-year periods of data collection (13-, 28-day periods), with 80% to 120% prescription issue rates taken as “adherent.”22-24 Data collection was conducted by trained researchers (JR and AQ in Glasgow, and JR in Edinburgh). Research ethics and data access permission approval was obtained from the University of Glasgow MVLS research ethics committee, NHS GG&C Caldicott Guardian and the NHS Lothian Caldicott Guardian.
Glasgow data were collected as part of a previous study,16 including all patients registered with Glasgow’s Homeless Health Service (GHHS) in October 2015 (n = 133). In Edinburgh, during October 2016, we randomly (RAND Excel command25) sampled the electronic case records of 150 (25%) patients registered with the Edinburgh Homeless Access Practice (EAP).
Statistical Analysis
Descriptive analysis of the previously described dataset16 was repeated to ensure findings were consistent with previous summaries.
For both data sets, continuous data were summarized using mean and SD or median (min-max). Summary statistics were compared using a 2-sample t test, or Mann-Whitney U test. For categorical data, percentages were calculated and the 2 samples compared using chi-square test (or Fisher’s exact test where applicable). A P value less than .05 was taken to mean statistical significance. All analyses were carried out using MINITAB version 17.26
Results
Service Characteristics
Both homeless services provide collocated physical health, mental health, and addictions support; however, differences exist in approaches to registration, skill mix, and staffing levels (Table 1). Glasgow’s GP service has distinct teams, administrative and clinical record systems and a formal process of referral between the GP service and collocated services, for example, mental health or addictions services. Edinburgh had 4.5 times more registered patients than Glasgow but only half of the patient turnover. However, Edinburgh homeless practice either had greater numbers of staff, or dedicated, core practice staff or both, for example, a practice manager, GPs, practice nurses, and a psychologist. In Edinburgh, in addition to providing comprehensive physical and mental health care, the GP service directly provide addictions care, for example, prescribing of opiate replacement therapy, and all patient data (physical health, mental health, and addictions) are recorded on a shared clinical record system, visible to staff in mental health and addictions services. Glasgow’s service offers permanent registration to patients with complex health needs and patients who seek registration. Otherwise uptake is variable and Glasgow patients often stay registered with their mainstream GP and see the Homeless Health Services GP for an undefined period of time. In Edinburgh, patients are permanently registered if they attend more than once. On registering with both practices, patients are asked questions as part of a health check. The content of the health check is locally developed and differs in Glasgow and Edinburgh. The Edinburgh practice holds monthly meetings involving all staff of all disciplines whereas the multidisciplinary staff meetings in Glasgow have staff group representation and are focused on patient complex case discussion.
Table 1.
Characteristics of Edinburgh and Glasgow Homeless Services.
| Edinburgh Access Practicea | Glasgow Homeless Health Serviceb |
|---|---|
| Patient population | |
| 599 patients permanently registered; patient turnover around 1600/year. | 133 permanently registered patients, 570 temporarily registered; patient turnover 3000-4000/year. |
| Patient records | |
| All staff use single set of shared electronic records: health, addictions, and social care. | Separate patient records created and accessed by different staff groups: health (GP); addictions; psychiatry; nursing. |
| Staff | |
| ▪ Practice manager.c
▪ 2 whole-time-equivalent GPs, 0.5 academic fellow.c ▪ 2 full-time practice nurses, 1 part-time.c ▪ Full-time health care assistant.c ▪ Practice mental health team: 6 whole-time-equivalent community psychiatric nurses (CPNs), 1 part-time psychologist.c ▪ Psychiatrist (1-2/month).d ▪ Pharmacist (1/week).d ▪ Welfare rights worker.d ▪ Podiatrist (1/week).d ▪ Community midwife (1/week).d ▪ Optician (1/week).d ▪ Community health worker (1/week).d ▪ Clinics: weekly hepatitis C treatment clinic,c women’s only clinic.c |
▪ Generic administration manager.e
▪ 1.5 whole-time-equivalent GPs, 0.5 academic fellow.c ▪ 5 full-time joint addiction/general nurses.e ▪ Full-time health care assistant.e ▪ Mental health team includes part-time psychiatrist.e ▪ Addiction team including full-time addiction psychiatrist.e ▪ Pharmacist (2/week, practice based and street outreach).e ▪ Welfare rights worker (2/week).d ▪ Podiatrist (2/week).d ▪ Community midwife.d ▪ Dietetics.d ▪ Families’ health care team.e ▪ Sexual health team.e ▪ Occupational therapy (OT) team.e ▪ Clinics: blood-borne viruses (BBV),d vision clinic.d |
| Team meetings | |
| Multidisciplinary clinical meetings every 2 weeks, Monthly whole team meetings. | Monthly GP meetings. |
2016.
2015.
Core team.
Visiting.
Attached.
Patient Demographics
The majority of patients were male in both samples, with a mean age of 39.4 ± 10.9 years in Edinburgh; Glasgow’s patients were older by 3 years on average (42.8 ± 11 years). Patients in Glasgow reported being homeless for a year longer than those in Edinburgh; and fewer had a record of having children. In Glasgow, less than one-third of patients had recorded phone numbers, whereas 81% of the Edinburgh sample had a recorded phone number (Table 2).
Table 2.
Patient Demographics.
| Demographicsa | Edinburgh (n = 150) | Glasgow (n = 133) | P |
|---|---|---|---|
| Age (years) | 39.4 ± 10.9 | 42.8 ± 11 | <.05 |
| Gender (male) | 117 (78.0) | 114 (85.7) | .09 |
| Time since first homeless presentation (years)b | 2 (0-23) | 3 (0-12) | <.05 |
| Contact number available | 122 (81.3) | 38 (28.6) | <.05 |
| Place of originc | |||
| Africa | 5 (3.3) | 7 (5.3) | |
| Asia | 1 (0.7) | 4 (3) | |
| Europe | 13 (8.7) | 3 (2.3) | |
| UK | 131 (87.3) | 112 (84.2) | <.05 |
| Citizenshipd | |||
| British | 130 (86.7) | 120 (90.9) | |
| European | 15 (10) | 1 (0.8) | |
| Refugee/asylum | 0 (0) | 7 (5.3) | |
| African | 5 (3.3) | 0 (0) | <.05 |
| Main spoken language | |||
| English | 134 (89.3) | 123 (92.5) | .36 |
| Polish | 7 (4.7) | 0 (0) | |
| Arabic | 2 (1.3) | 0 (0) | |
| Romanian | 2 (1.3) | 0 (0) | |
| Other | 5 (3.3) | 10 (7.5) | |
| Interpreter required | 11 (7.3) | 2 (1.5) | <.05 |
| Marital statuse | |||
| Divorced | 6 (4) | 4 (3) | |
| In a relationship | 0 (0) | 9 (6.8) | |
| Married | 3 (2) | 2 (1.5) | |
| Separated | 2 (1.3) | 0 (0) | |
| Single | 118 (78.7) | 89 (66.9) | <.05 |
| Widowed | 2 (1.3) | 0 (0) | |
| Children | 85 (56.7) | 50 (37.6) | <.05 |
| In prison in the past year | 53 (35.3) | 26 (27.1) | .14 |
| No. times in prison in the past yearf | 0 (0-2) | 0 (0-3) | .26 |
n (%) or median (min-max) or mean ± SD unless stated otherwise.
Missing data: n = 1 Glasgow, n = 4 Edinburgh.
Missing data: n = 7 Glasgow.
Missing data: n = 4 Glasgow.
Missing data: n = 29 Glasgow, n = 19 Edinburgh.
Missing data: n = 3 Glasgow, n = 1 Edibnurgh.
Most patients were of UK origin. The Glasgow sample included more patients from Asia, but fewer originating from Europe and more patients describing themselves as a refugee or asylum seeker. In Edinburgh, the greater proportions describing themselves as Polish, Arab, or Romanian are likely to have contributed to the greater observed requirement for an interpreter during consultations. Around one-third of both cohorts had been in prison within the past year.
Multimorbidity
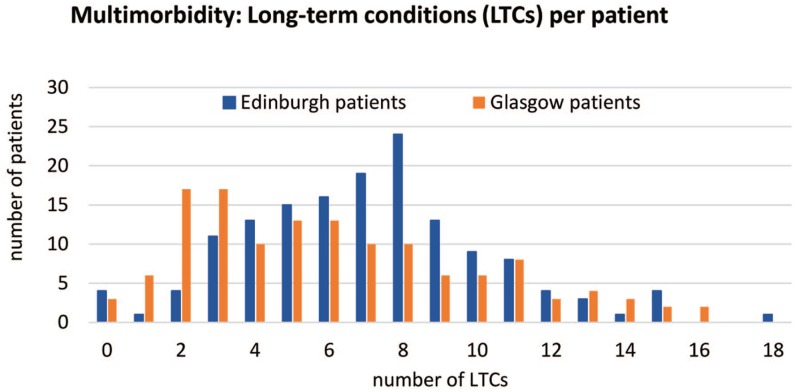
The majority of patients in both cohorts were multimorbid; only 3% of patients in Glasgow and 7% in Edinburgh had no recorded LTCs. The median number of all LTCs was 7 (±3.3) per patient in Edinburgh and 6 (±3.88) in Glasgow (P < .05). Figure 1 shows the distribution of the number of recorded LTCs per patient: the multimorbidity peak in Glasgow is at 2 and 3 LTCs per patient, compared with 8 LTCs per patient in Edinburgh. Most patients had a record of comorbid physical health, mental health, and addiction problems—71% of patients in Edinburgh and 49% in Glasgow had a diagnosis from all 3 of these categories.
Figure 1.
Multimorbidity—recorded long-term conditions per patient.
Long-Term Physical Conditions
More than 80% of patients in both cohorts had a recorded physical LTC. The median number of physical LTCs per patient was 3 for both groups, with up to 12 to 13 conditions per patient (Table 3).
Table 3.
Physical Long-Term Conditions.
| Physical Long-Term Conditions (pLTCs)a | Edinburgh (n = 150) | Glasgow (n = 133) | P |
|---|---|---|---|
| Patients with pLTC | 130 (86.7) | 110 (82.7) | .35 |
| pLTCs per patient | 3 (0-13) | 3 (0-12) | .29 |
| Chronic painful condition | 42 (28) | 24 (18.1) | <.05 |
| Chronic painful conditions per patient | 0 (0-3) | 0 (0-3) | .06 |
| Hepatitis A | NC | 0 (0) | |
| Hepatitis B | 3 (2) | 6 (4.5) | .23 |
| Hepatitis C | NC | 33 (24.8) | |
| Any hepatitis (including A,B,C) | 45 (30) | 35 (26.3) | .49 |
| Chronic liver disease | 7 (4.7) | 2 (1.5) | .13 |
| Any liver condition | 48 (32) | 37 (27.8) | .44 |
| HIV | 0 (0) | 5 (3.8) | <.05 |
| Cardiovascular | 29 (19.3) | 14 (10.5) | <.05 |
| Cardiovascular diagnoses per patient | 0 (0-3) | 0 (0-5) | .12 |
| Respiratory | 52 (34.7) | 21 (15.8) | <.05 |
| Respiratory diagnoses per patient | 0 (0-2) | 0 (0-3) | <.05 |
| Gastrointestinal | 22 (14.7) | 32 (24) | <.05 |
| Gastrointestinal diagnoses per patient | 0 (0-3) | 0 (0-4) | .20 |
| Vascular | 22 (14.8) | 19 (14.3) | .93 |
| Vascular diagnoses per patient | 0 (0-2) | 0 (0-3) | .84 |
| Diabetes/endocrine | 11 (7.3) | 6 (4.5) | .32 |
| Head injury | 34 (22.7) | 39 (29.3) | .20 |
| Physical trauma | 32 (21.3) | 36 (27.1) | .26 |
| Epilepsy | 9 (6) | 4 (3) | .23 |
| Alcohol related | |||
| Brain injury | 5 (3.33) | Data not collected | |
| Seizures | 11 (7.3) | Data not collected | |
| Total head/brain condition | 60 (40) | 41 (30.8) | .11 |
| Neurological | 11 (7.3) | 21 (15.8) | <.05 |
| Chronic kidney disease | 0 (0) | 0 (0) | |
| Fractures | 17 (11.3) | 49 (36.8) | <.05 |
| Rheumatic condition | 13 (8.7) | 4 (3) | .65 |
| Anemia | 3 (2) | 5 (3.8) | .37 |
| Prostate disorders | 5 (4.2) | 0 (0) | <.05 |
| Genitourinary/pelvic disease | 7 (4.7) | 12 (9) | .14 |
| Skin condition | 28 (18.7) | 13 (9.8) | <.05 |
| Other conditions | 17 (11.3) | 37 (27.8) | <.05 |
n (%) or median (min-max) unless stated otherwise.
For some conditions, the number of patients with a record of a diagnosis were similar when comparing Edinburgh and Glasgow; this included liver disease (hepatitis, chronic liver disease), vascular conditions, endocrine conditions including diabetes, accidents such as head injury or trauma, epilepsy and other head/brain conditions, rheumatic conditions, and anemia.
Glasgow had a statistically significantly higher number of recorded HIV diagnoses (3.8%), while no cases were recorded in the Edinburgh sample. Recorded fractures were more than 3 times higher in Glasgow and recorded prevalence of gastrointestinal conditions was also higher. Amongst others, Edinburgh had more recorded diagnoses of cardiovascular and especially respiratory conditions, the latter affecting 35% compared with only 16% in Glasgow.
Long-Term Mental Health/Addiction Problems and Adverse Experiences
Statistically significantly more patients in Edinburgh had a record of a mental health issue—87% compared with 65% in Glasgow (Table 4). The average number of mental health issues per patient was 3 in Edinburgh compared with 1 in Glasgow.
Table 4.
Mental health, addictions and adverse experiences.
| Addiction/Mental Health/Adverse Experiencesa | Edinburgh (n = 150) | Glasgow (n = 133) | P |
|---|---|---|---|
| Heroin | 80 (53.3) | 62 (46.6) | .26 |
| Other opiates | 45 (30) | 20 (15.04) | <.05 |
| Cannabis | 41 (27.3) | 19 (14.3) | <.05 |
| Benzodiazepines | 51 (34) | 30 (22.6) | <.05 |
| Other | 50 (33) | 30 (22.6) | <.05 |
| Cocaine | 4 (2.7) | 19 (14.3) | |
| New psychoactive substances | 29 (19.3) | 7 (5.3) | |
| Ecstasy | 5 (3.3) | 1 (0.8) | |
| Unprescribed methadone | 5 (3.3) | 1 (0.8) | |
| Others | 14 (9.3) | 10 (7.5) | |
| Solvents, steroids, gambling, gabapentin, crystal meth, SPICE, steroids, street yellow, butane gas | LSD, speed, butane gas, solvents, DHC (dihydrocodeine), zopiclone | ||
| Problem drug use | 110 (73.3) | 82 (61.7) | <.05 |
| Problem alcohol | 55 (36.7) | 72 (54.1) | <.05 |
| Depression | 83 (55.3) | 44 (33.1) | <.05 |
| Anxiety | 97 (64.7) | 20 (15) | <.05 |
| Personality disorder | 22 (14.7) | 9 (6.8) | <.05 |
| Self-harm (including suicide) | 54 (36) | 35 (26.3) | .08 |
| Accidental overdose | 19 (12.8) | Data not collected | |
| Intentional overdose | 34 (22.7) | Data not collected | |
| Mania/hypomania | 4 (2.7) | 0 (0) | .06 |
| Posttraumatic stress disorder (PTSD) | 20 (13.3) | 5 (3.8) | <.05 |
| Complex trauma | 46 (30.7) | 2 (1.5) | <.05 |
| On at-risk register | 8 (5.3) | Data not collected | |
| Any mental health issue | 131 (87.3) | 86 (64.7) | <.05 |
| Median no. per patient | 3 (0-7) | 1 (0-4) | <.05 |
| Cognitive impairment | 6 (4) | 13 (9.8) | .05 |
| Multiagency public protecion arrangements | 1 (0.7) | 1 (0.8) | .16 |
| Documented risk of violence to staff | 30 (20) | 27 (20.3) | .95 |
| Victim of violence | 51 (34) | 66 (49.6) | <.05 |
| Victim domestic violence | 25 (16.7) | 11 (8.3) | <.05 |
| Childhood abuse/neglect | 49 (32.7) | 21 (15.8) | <.05 |
| Previously in care | 24 (16) | 9 (6.8) | <.05 |
n (%) or median (min-max) unless stated otherwise.
In Edinburgh statistically significantly more patients had a recorded diagnosis of depression, 55% compared with 33% in Glasgow. Anxiety was recorded for 15% of patients in Glasgow, whereas 65% had this diagnosis in Edinburgh. While 1.5% of patients were recorded as diagnosed with complex trauma in Glasgow, the prevalence was statistically significantly higher in Edinburgh at 31%. Self-harm, including attempted suicide, was high among both groups—26.3% in Glasgow and 36% in Edinburgh, two-thirds of whom in Edinburgh were recorded as having a history of taking an intentional overdose.
Problem alcohol use was commonly recorded, with Glasgow having a statistically significantly higher prevalence at 54% compared with 37% in Edinburgh. Problem drug use was even more common and was much higher in Edinburgh than in Glasgow at 73% and 62%, respectively. Patterns in drug use varied: heroin was the most common drug of misuse among both cohorts with no statistically significant difference. Edinburgh had higher recorded rates of benzodiazepines, other opiates, and cannabis use, the latter 2 with rates twice as high as in Glasgow. While patients in Glasgow were recorded as using more cocaine—14% of patients compared with 3%—the recorded use of new psychoactive substances was higher in Edinburgh.
Statistically significantly more patients in Edinburgh had a record of experiencing domestic violence, previous institutional care, and childhood abuse/neglect, with the latter affecting 33% in Edinburgh and 16% in Glasgow. Glasgow had a higher rate of patients recorded as victims of violence: 50% compared with 34% in Edinburgh.
Medication
Continuity of prescribing medication for the LTCs assessed (those included in QOF contract) was low in both cohorts. Overall, patients in the study received 5 prescriptions on average (repeat + acute) over the respective 1-year periods of data collection, with significantly more acute prescriptions issued than repeats (P < .05). Differences in prescribing patterns were observed: Glasgow patients were on a median of 1 repeat (max 14) and 4 acute (max 25) prescriptions, while in Edinburgh the median per patient was at 0 repeats (max 5) and 4.5 acutes (max 17) (P < .05).
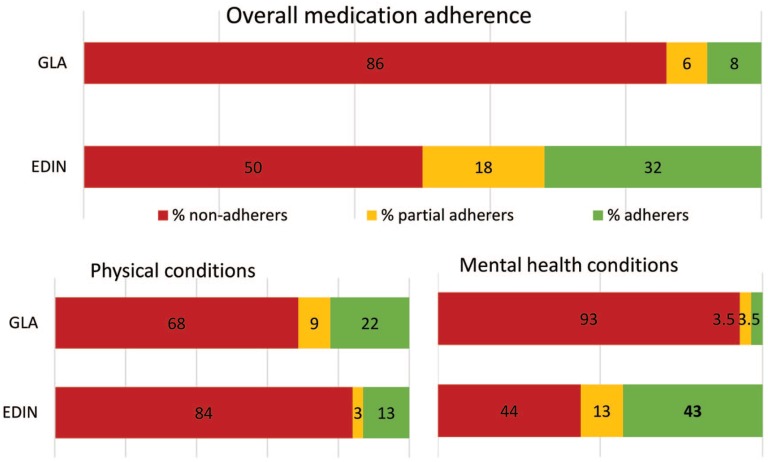
Patients in Glasgow had statistically significantly lower rates of prescription reordering for LTCs in the QOF framework (P < .05): overall only 8% were issued all of their prescriptions between 80% and 120% of times within the year (“adherers”), compared with 32% in Edinburgh. Eighty-six percent of patients in Glasgow were “nonadherers”; this includes both underordering (<80%) and overordering (>120%) of medication; compared with 50% in Edinburgh. Differences in trends of prescription reordering by patient group and prescription indication (physical vs mental health/addiction) are summarized in Figure 2; for mental health/addiction prescriptions, a higher proportion of Edinburgh patients were “adherers.”
Figure 2.
Continuity of prescribing medication, n (%): 80% to 120% requested prescriptions per medication = adherent (adherent to none of their medications = nonadherers; adherent to some medications = partial adherers; adherent to all medications = adherers).
Service Utilization
Registered patients in Glasgow had a median number of 7 consultations with any health care professional within the GP service in the previous year, statistically significantly less than Edinburgh’s average of 15 consultations (Table 5).
Table 5.
Service Utilization in a 1-Year Period.
| Service utilisationa | Edinburgh (n = 150) | Glasgow (n = 133) | P |
|---|---|---|---|
| Consultations in service per patient | 15 (0-127) | 7 (0-47) | <.05 |
| Patients with general practitioner (GP) consultation | 140 (93.3) | 124 (93.2) | .97 |
| Patients with GP consultation in Homeless accommodation | 0 (0) | 28 (21.1) | <.05 |
| GP consultations per patientb | 6 (0-31) | 6 (0-32) | .89 |
| Patients with nurse consultation | 127 (84.7) | 35 (26.3) | <.05 |
| Nurse consultation per patientc | 2 (4-49) | 0 (0-6) | <.05 |
| Patients with pharmacist consultations | 4 (2.7) | 34 (25.6) | <.05 |
| Bloodborne virus (BBV) clinic attendances | 46 (30.7) | 8 (6) | <.05 |
| Third sector referrals | 46 (30.7) | 25 (18.8) | <.05 |
| Vaccinations | |||
| Influenza | 50 (33.3) | 15 (11.3) | <.05 |
| Pneumococcal | 14 (9.3) | 3 (2.3) | <.05 |
| Hepatitis A | 35 (23.3) | 12 (9) | <.05 |
| Hepatitis B | 67 (44.7) | 14 (10.5) | <.05 |
n (%) or median (min-max) unless specified.
Missing data: n = 1 Edinburgh
Missing data: n = 15 Glasgow, n = 2 Edinburgh.
Within the service, 93% of patients in both cities had at least 1 GP consultation within the previous year, with an average of 6 for both groups. In Glasgow 21% of patients had a GP consultation in their homeless accommodation, compared with none in Edinburgh. Statistically significantly more patients in Edinburgh had a nurse consultation in the practice: 85% compared with 26% in Glasgow. One-quarter of Glasgow’s homeless population who were registered with the GHHS had seen a pharmacist in the practice in the preceding year compared with 3% in Edinburgh. In Edinburgh, 30% of patients had a record of referral to a third sector organization, Glasgow’s referral rate was lower at 20%.
Recorded vaccination coverage was higher in Edinburgh than in Glasgow for influenza, pneumococcal, hepatitis A, and hepatitis B.
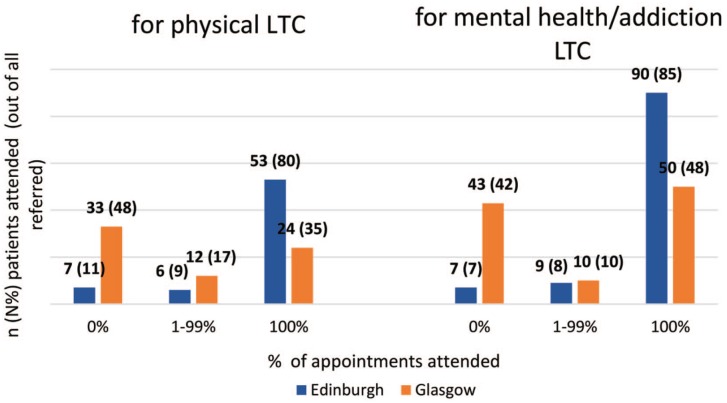
Figure 3 describes patient attendance at appointments following GP referral to other primary care services or secondary care specialists. Fewer patients in Glasgow attended referral appointments than in Edinburgh, with never-attenders more than three times higher in Glasgow.
Figure 3.
Attendance of patients at their referral appointments, n (%): 0% never attended any appointments; 1% to 99% attended some, 100% attended all).
Interpretation of Findings
Practice infrastructure differs between the 2 services, and statistical analysis of patient-level data also showed differences in health and health care utilization. While it is not possible to say whether differences in some patient demographics (eg, age, duration of homelessness) had an influence on health, diagnoses, and health care utilization, we identified aspects of service design and delivery that could play a role in this.
The context in which patients were registered was identified as a potential contributing factor to some of the differences found in LTC prevalence and health service utilization. EAP and GHHS have differing approaches to registration, which means the Glasgow sample were potentially also a different subgroup of the population experiencing homelessness. This sample were characterized by patients who opt to register and patients the GP team assessed as requiring registration to enable coordinated “sticky” GP team input, compared with the EAP sample who were all registered at second presentation. The process of offering registration or not in GHHS is therefore subjective and may be prone to variation between clinicians. It is possible, given this difference, that patients in GHHS may also move between the GHHS and their own GP for a period of time until they either become permanently registered with the GHHS or leave the practice and register with another mainstream practice. This may tend to reduce the opportunities to conduct baseline and follow-up assessments, which are prerequisites in LTC diagnoses and management.
Prevalence of several LTCs differed significantly between Glasgow and Edinburgh, with the pattern being increased detection and recording in Edinburgh. The differences included physical health problems, for example, cardiovascular disease, respiratory problems, skin conditions, and mental health problems, for example, anxiety, personality disorder, and complex trauma. Together these suggest increased focus on assessment and detection, that may have resulted from a practice configuration, including staff/skill mix, for example, nursing staff, conducive to recording these conditions through serial encounters and opportunistic attempts at engagement by different practice staff sharing the same electronic record system.
Differences in permeability/proximity of staff/services may have influenced the recorded rates between the 2 services. One aspect of this is the role of recording systems. In Glasgow, recording systems between the GP service and the homeless addiction teams (including blood-borne viruses clinic) or mental health teams are separate. Not having a shared record system means clinicians have less information about their patient at the time of consultations. While patients may well have diagnosed mental health/addiction issues, the separate records for the services potentially mean GPs in GHHS are not aware of these diagnoses. As we only accessed GP records, this might explain the comparatively lower recorded disease rates in the Glasgow cohort. The shared IT information system in the EAP means that GPs have a comprehensive overview over their patient’s health problems.
Linked in with this are differences in the segmentation of services—in the EAP, drug/alcohol and mental health treatment is integrated within routine care provided in-house by the GP service, while in the GHHS these services are colocated, that is, they are under the same roof, but the services are separate and so are their records.
The practice mental health team integrated into the Edinburgh service consists of CPNs and a clinical psychologist. This means there is potentially more scope to diagnose and manage mental health conditions in patients and this will therefore contribute to the significantly higher rates of recorded mental health diagnoses in Edinburgh. It may also explain the higher rates of adherence to mental health/addiction prescription medication in Edinburgh.
The EAP offers in-house opioid-substitution therapy as part of their routine primary care, which may contribute to higher rates of recorded problem drug use amongst Edinburgh’s service users—on one hand due to more opportunities to diagnose and record this but also potentially by attracting other patients with substance misuse problems into the service. Provision of ORT may also play a part in higher number of adherers to mental health/addiction prescriptions in Edinburgh. For patients of the GHHS, addiction service policy is that, when patients become homeless, they remain linked in with their existing community addiction team—the advantage of this being continuity of care. For some patients this may have the effect of making engagement in homelessness services and continued addiction care more difficult. Of note is that the blood-borne viruses clinic nurses are embedded into this separate addiction team too.
Another contributing factor to some of the observed differences is the availability of staff expertise, particularly through the effect this has on important aspects of patient care such as LTC management and disease coding.
The EAP has dedicated practice nurses while the GHHS is covered by joint addiction/general nurses; this is reflected in the considerably higher rates of nurse consultations recorded in Edinburgh. Amongst others, the role of practice nurses entails preventative care through health checks and LTC management, exemplified by the higher recorded rates of vaccinations in Edinburgh. This may explain the higher recorded rates of physical LTCs such as respiratory and cardiovascular disease in Edinburgh too. Glasgow in turn had higher records of GI conditions and fractures—these arguably can be considered more emergency/ patient-driven presentations, that is, as opposed to a patient with hypertension and no symptoms, a patient with acute abdominal pain will be more inclined to present to see the GP.
The EAP also has a practice manager, while the GHHS has a generic administration manager. Dedicated practice managers have a direct role in practice improvement activities such as disease coding, call and recall for LTC consultations and performance evaluation. Only coded data were extracted from records and it was thought that gaps in coding in Glasgow, and conversely more thorough coding in Edinburgh, rather than actual differences in underlying disease prevalence, are likely to account for some of the significantly differing incidence rates between the 2 patient populations. Diagnoses recorded in free text might also be missed by healthcare staff at subsequent appointments, potentially leading to less continuous care for these diagnosed conditions, which is especially important in LTC management. A higher proportion having contact numbers and greater utilization of interpreters in Edinburgh despite comparable rates of spoken languages, may be due to having a practice manager supporting reception and administration staff to collect contact numbers and arrange interpreters.
There might also be external drivers for diagnostic focus in the 2 services responsible for some differences. One example of this is the higher recorded rates of HIV diagnoses in the Glasgow cohort. The driver for this is the ongoing outbreak of HIV infections amongst injecting drug users in Glasgow, with most affected people being coinfected with hepatitis C virus.14,27 Since the beginning of the epidemic in 2015, targeted multidisciplinary interventions and services have been resourced and implemented to test and treat hepatitis C virus and HIV. These include a multidisciplinary team street outreach service, close links between blood-borne viruses clinic and drug treatment services, community pharmacy prescribing of antiretroviral therapy and a sustained focus on testing those at risk.14,27
Discussion
Summary
Patient level data of specialist homeless GP services in Scotland with differing practice infrastructure was analyzed, looking at service utilization, recording of LTCs, as well as prescribing and adherence to explore the impact of service design and delivery on patient’s outcomes.
Differences existed in the reported characteristics of patients who were homeless in Glasgow and Edinburgh. Patterns of service utilization were noted, as well as differences in recorded disease rates of physical health, mental health, and addiction LTCs.
It is likely that some of these statistically significantly differing results have been influenced by differences in health service configuration and professional skill mix; for example, differing policies on who is registered potentially resulted in the sample populations covering different patient subgroups. Other factors identified in the Edinburgh and Glasgow services as potential contributors include differences in permeability and segmentation of services, in recording systems, availability of staff expertise—and associated with this LTC management (practice nurses) and practice improvement activities (practice managers)—, and finally external drivers for diagnostic focus like the Glasgow HIV outbreak.
Strengths and Limitations
The strengths of this study are that the method of data collection was the same for both cohorts, and the same variables were collected. The size of the study cohort is comparable to other studies of this type.28,29 Data were extracted from routine records in primary care with some secondary care information, eliminating potential bias arising from using self-reported information. The direct comparison of two specialist services allows for more informed evaluation of the impact of practice infrastructure on health and healthcare utilization of patients.
There are no population data available to suggest that the characteristics of people experiencing homelessness in Glasgow and Edinburgh are different. However, limitations included that data collection was performed in 2015 for Glasgow and one year later, in 2016, for Edinburgh, meaning external factors that could influence the characteristics and outcomes analyzed were not controlled for. Furthermore, Edinburgh’s data was derived from a random 25% sample and Glasgow’s sample was all registered patients in the practice at that time. The absolute numbers for adherence and attendance were lower than for other collected variables.
While the comparison of 2 services allowed us to explore the impact that service design and delivery have on recorded disease rates, other variables might also have had an impact on some of the statistically significant differences in our results. It would be interesting to explore these further, for example, thinking about other explanatory factors for the differences in types of drugs used by the 2 patient cohorts. While we did not set out to test any hypothesis that differences in practice design impact on outcomes such as LTC recording, health service utilization, and prescribing, it is possible that the strength of any associations could have been explored using quantitative statistical techniques, for example, regression. By design, our work was exploratory, but subsequent work may benefit from inclusion of additional homeless health services and hypothesis-driven, robust statistical analyses.
Comparison With Existing Literature
No previous study to our knowledge has sought to compare 2 specialist services and our findings highlight the impact that differences in service configuration and skill mix have on uptake of care, recorded health conditions, and medicines adherence. It illustrates very clearly how results from retrospective cohort studies can be skewed by the health service setting the data are extracted from, possibly especially in the complex high turnover clinical setting that homelessness health services tend to operate in. Differences in practice configuration and management seem to have a direct impact on recorded rates of disease prevalence and health care utilization.
Overall, our findings match those of other studies investigating the health of people experiencing homelessness: compared with the general population, patients registered with a specialist homeless GP had more multimorbidity, including long-term physical health conditions, long-term mental health problems, and addictions.9,29,30 Recent work on morbidity and mortality among people who are currently homeless3,5 suggests that to address deep social exclusion, in addition to the current focus on mental health and substance misuse, physical health, and LTC management for common conditions like cardiovascular disease should be incorporated into the tailored care for this patient group. It points out the lack of research on effective interventions to tackle LTCs for people experiencing homelessness,8 including support for medication adherence.6 The need for monitoring of health outcomes and collection of routine surveillance data to help implement this is stressed.3,5
A recent national study in mainstream general practice found that patients with a higher number of LTCs were found to be at increased risk of missing GP appointments, especially patients with diagnosed mental health conditions. Low appointment attendance was found to be a significant risk marker for all-cause mortality and premature death.31 This becomes particularly relevant to consider when configuring health care delivery for a marginalized patient group who struggle to engage in preventative health measured, may mistrust health care providers and experience barriers to accessing services.6,12
Implications for Research/Practice
The analysis of 2 specialist homeless services allows for the appreciation of differences in service configuration and professional skill mix and the possible impacts that this may have beyond our reporting in this study.
Research suggests that registration increases the likelihood of good continuity of care for patients,32 partly as it enables clinicians to access patient’s notes and health data, including past medical history and correspondence with secondary care, although admittedly the transient nature of experiencing homelessness can make continuity more difficult. Segmentation versus integration of services and the referral process between colocated/integrated services, as well as the location of services all play a role in service permeability; our findings suggest that services need to be integrated not just colocated to optimize diagnoses, management, and monitoring of patients. Linked in with this is the recording system: our results were shaped by the information available to a GP during a patient consultation and illustrate that shared information systems across primary care professional groups can facilitate a holistic approach to patient treatment.
Recent evidence suggests that close to one-third of homeless deaths occur due to causes amenable to timely health care,5 and early health care interventions through better surveillance management of LTCs is likely to improve health outcomes for this patient cohort. Patients experiencing homelessness often only present to health services when they are acutely unwell or in need of medication for distress or pain.33 Practice management techniques and clinical systems can be used to monitor LTCs and screening, which is vital especially with the high turnover in homelessness services. Coding plays a vital role in LTC management and consistent coding of chronic disease diagnoses has been found to be associated with better quality of care for patients,34 for example, by enabling automated recalls, point of care reminders, practice population quality improvement activities and computerized decision support.35 While GPs commonly treat acute presentations and manage complex health issues, pharmacists and practice nurses may be responsible for more routine tasks and anticipatory care like general health checks and the management of LTCs. It is likely that with evidence-based resources and skill mix, clinicians will have more scope to address unmet needs and more accurate coding is more likely to follow.
Our findings suggest that health service design and delivery drive recording of patient information and therefore have an impact on what we can measure and evaluate in patient populations, which will in turn directly affect patient care and health outcomes. In a complex high turnover setting with patients known to experience inequity and increased barriers to accessing care, evidence-based attention to service configuration, professional skill mix and resources are important to enable patients to have their health needs identified and then met.
Acknowledgments
We would like to extend our gratitude to Janice Richardson for her invaluable contribution and support to this project.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Martina Zeitler  https://orcid.org/0000-0002-2042-2505
https://orcid.org/0000-0002-2042-2505
References
- 1. Aldridge RW, Story A, Hwang SW, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391:241-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Waugh A, Clarke A, Knowles J, Rowley D. Health and Homelessness in Scotland: Research. https://www.gov.scot/publications/health-homelessness-scotland/. Published June 19, 2018. Accessed February 17, 2020.
- 3. Lewer D, Aldridge RW, Menezes D, et al. Health-related quality of life and prevalence of six chronic diseases in homeless and housed people: a cross-sectional study in London and Birmingham, England. BMJ Open. 2019;9:e025192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Morrison D. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol. 2009;38:877-883. [DOI] [PubMed] [Google Scholar]
- 5. Aldridge R, Menezes D, Lewer D, et al. Causes of death among homeless people: a population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome Open Res. 2019;4:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paudyal V, MacLure K, Buchanan C, Wilson L, Macleod J, Stewart D. “When you are homeless, you are not thinking about your medication, but your food, shelter or heat for the night”’: behavioural determinants of homeless patients’ adherence to prescribed medicines. Public Health. 2017;148:1-8. [DOI] [PubMed] [Google Scholar]
- 7. Homeless Link, St Mungo’s. Improving hospital admission and discharge for people who are homeless. https://www.homeless.org.uk/sites/default/files/site-attachments/HOSPITAL_ADMISSION_AND_DISCHARGE._REPORTdoc.pdf. Published 2012. Accessed February 17, 2020.
- 8. Hanlon P, Yeoman L, Gibson L, et al. A systematic review of interventions by healthcare professionals to improve management of non-communicable diseases and communicable diseases requiring long-term care in adults who are homeless. BMJ Open. 2018;8:e020161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fazel S, Geddes J, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384:1529-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bramley G, Fitzpatrick S, Edwards J, et al. Hard Edges—Mapping Severe and Multiple Disadvantage. London, England: LankellyChase Foundation; 2015. [Google Scholar]
- 11. Crane M, Cetrano G, Joly L, et al. Mapping of Specialist Primary Health Care Services in England for People Who are Homeless. London, England: King’s College London; 2018. [Google Scholar]
- 12. Lowrie R, Williamson A, Spencer R, Hair A, Gallacher I, Hewett N. Collaborative engagement for long term conditions by clinical pharmacists for people who are homeless in Glasgow, Scotland. https://www.feantsa.org/download/march-2017-health-and-homelessness-newsletter2959399951318964653.pdf. Accessed February 17, 2020.
- 13. Bramley G, Fitzpatrick S, Wood J, et al. Hard Edges Scotland: New Conversations About Severe and Multiple Disadvantage. London, England: LankellyChase Foundation; 2019. [Google Scholar]
- 14. Public Health Protection Unit, NHS Greater Glasgow and Clyde. HIV infections in people who inject drugs—update 2019. https://www.nhsggc.org.uk/your-health/public-health/public-health-protection-unit-phpu/bloodborne-virus/hiv/hiv-infections-in-people-who-inject-drugs-update-2019/#. Accessed February 17, 2020.
- 15. National Records of Scotland. Drug-related deaths in Scotland in 2018. nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/drug-related-deaths-in-scotland. Published 2019. Accessed February 17, 2020.
- 16. Queen AB, Lowrie R, Richardson J, Williamson AE. Multimorbidity, disadvantage, and patient engagement within a specialist homeless health service in the UK: an in-depth study of general practice data. BJGP Open. 2017;1:bjgpopen17X100941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. EMIS Health. EMIS web for primary care. https://www.emishealth.com/products/emis-web/emis-web-for-primary-care/. Published 2019. Accessed October 2019.
- 18. Vision. https://www.visionhealth.co.uk/. Published 2019. Accessed November 2019.
- 19. Docman. What we do? https://www.docman.com/what-we-do/primary-care/docman-gp/. Published 2019. Accessed October 2019.
- 20. Barnett K, Mercer S, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;280:37-43. [DOI] [PubMed] [Google Scholar]
- 21. NHS Employers. 2016/17 General Medical Services (GMS) contract Quality and Outcomes Framework (QOF). https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomes-framework-qof-2016-17. Published October 26, 2017. Accessed February 17, 2020.
- 22. Covvey JR, Mullen AB, Ryan M, et al. A comparison of medication adherence/persistence for asthma and chronic obstructive pulmonary disease in the United Kingdom. Int J Clin Pract. 2014;68:1200-1208. [DOI] [PubMed] [Google Scholar]
- 23. Andersson K, Melander A, Svensson C, Lind O, Lars J, Nilsson G. Repeat prescriptions: refill adherence in relation to patient and prescriber characteristics, reimbursement level and type of medication. Eur J Public Health. 2005;15:621-626. [DOI] [PubMed] [Google Scholar]
- 24. Lam W, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cheusheva S. How to select random sample in Excel. https://www.ablebits.com/office-addins-blog/2018/01/31/excel-random-selection-random-sample/. Published 2019. Accessed October 2019.
- 26. Minitab. Minitab 17. https://www.minitab.com/uploadedFiles/Documents/getting-started/Minitab17_GettingStarted-en.pdf. Published 2014. Accessed October 2019.
- 27. National AIDS Trust. Policy briefing: HIV outbreak in Glasgow—more needs to be done. Published July 2018. Accessed February 17, 2020. [Google Scholar]
- 28. Keogh C, O’Brien K, Hoban A, O’Carroll A, Fahey T. Health and use of health services of people who are homeless and at risk of homelessness who receive free primary health care in Dublin. BMC Health Serv Res. 2015;15. doi: 10.1186/s12913-015-0716-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wagner J, Diehl K, Mutsch L, Loeffler W, Burkert N, Freidl W. Health status and utilisation of the healthcare system by homeless and non-homeless people in Vienna. Health Soc Care Community. 2014;22:300-307. [DOI] [PubMed] [Google Scholar]
- 30. Homeless Link. The unhealthy state of homelessness. Health audit results 2014. https://www.homeless.org.uk/sites/default/files/site-attachments/The%20unhealthy%20state%20of%20homelessness%20FINAL.pdf. Published 2014. Accessed February 17, 2020.
- 31. McQueenie R, Ellis D, McConnachie A, Wilson P, Williamson A. Morbidity, mortality and missed appointments in healthcare: a national retrospective data linkage study. BMC Med. 2019;17:2. doi: 10.1186/s12916-018-1234-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. NHS Primary Care & Community Services. Inclusion health: improving primary care for socially excluded people. https://www.bl.uk/collection-items/inclusion-health-improving-primary-care-for-socially-excluded-people. Published March 22, 2010. Accessed February 17, 2020.
- 33. Hanlon P, Yeoman L, Esiovwa R, et al. Interventions by healthcare professionals to improve management of physical long-term conditions in adults who are homeless: a systematic review protocol. BMJ Open. 2017;7:e016756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Holt T, Gunnarsson C, Cload P, Ross S. Identification of undiagnosed diabetes and quality of diabetes care in the United States: cross-sectional study of 11.5 million primary care electronic records. CMAJ Open. 2014;2:E248-E255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Greiver M, Wintemute K, Aliarzadeh B, et al. Implementation of data management and effect on chronic disease coding in a primary care organisation: a parallel cohort observational study. J Innov Health Inform. 2016;23:843. [DOI] [PubMed] [Google Scholar]