Summary
Aims
Extra-articular fifth metacarpal fractures are treated operatively and non-operatively without consensus. We aim to establish whether there are differences in patient-reported outcome, objective clinical outcome and adverse events for skeletally mature patients with closed extra-articular fractures of the 5th metacarpal that are treated operatively versus non-operatively.
Patients
Skeletally mature patients with closed, extra-articular 5th metacarpal fractures.
Methods
A systematic review and meta-analysis of randomised controlled trials using methodology adapted from the Cochrane Handbook for Systematic Review of Interventions and compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. (PROSPERO CRD42018091633)
Results
Two trials of 5th metacarpal neck fractures met the inclusion criteria and were included in the final pooled analysis (n = 125). There were no significant differences in patient-reported, objective clinical or radiographic outcomes between the operative and non-operative groups at 12 months. Operatively managed patients reported greater time off work and were more likely to suffer an adverse event.
Conclusion
Existing trial data is limited and inconclusive in terms of patient-reported outcome measures. Given that there remains wide variation in the treatment of these common injuries around the world, there is a need for further high-quality evidence to guide clinical practice.
Keywords: Hand surgery, Trauma, Fracture, Systematic review
Introduction
Metacarpal fractures are among the most common upper extremity injuries in adults, representing 10% of all bony injuries.1 A study of a UK population found an annual incidence of 280 per 100,000 for hand fractures.2 The mean age for sustaining these injuries is 31.5 years old in European populations.2, 3 Fifth metacarpal fractures are the most commonly injured metacarpal, representing 20% of all hand fractures and occurring mostly in the young, working population.4 Some fifth metacarpal fracture patterns can cause functional detriment, including weakened 5th finger grip initiation and reduced active motion at the 5th MCPJ.4 This leads to diminished hand function and economic consequences through days off work.5, 6 Conversely, many 5th metacarpal fractures can be managed non-operatively with minimal intervention resulting in excellent long-term outcomes.6, 7
Open 5th metacarpal fractures almost always need operative management and are therefore not subject to discourse regarding non-operative intervention. Amongst closed injuries, operative treatment is generally indicated for intra-articular fractures. Fixation of intra-articular 5th metacarpal fractures is purported to restore congruency of the joint surfaces, restoring movement at the joint and preventing further joint destruction and osteoarthritis. For extra-articular 5th metacarpal fractures, the indications are more uncertain and generally include sufficient deformity, instability and/or shortening of the metacarpal to warrant surgical intervention. Operative techniques include closed reduction and percutaneous fixation with Kirschner wires (K-wires), or open reduction and internal fixation using K-wires, plates and screws. There is no consensus on the indications for surgery or best operative management for extra-articular 5th metacarpal fractures.7
There is a trend to non-operative management of extra-articular 5th metacarpal fractures. Good functional and objective clinical results are reported in the literature.6, 7, 8, 9, 10, 11, 12 A Cochrane systematic review of non-operative treatments found a lack of evidence to support one particular therapy over another.6 Operative intervention has progressed and closed reduction and stabilization with Kirschner wires (K-wires) with a variety of techniques is probably the most commonly adopted technique.7, 13, 14 This systematic review aims to provide a comprehensive assessment of the randomized trial evidence for operative versus non-operative treatment of closed extra-articular fractures of the 5th metacarpal.
Review question
Is there a difference in patient-reported outcome, objective clinical outcome and adverse events for skeletally mature patients with closed extra-articular fractures of the 5th metacarpal that are treated operatively versus non-operatively?
Aim
To establish the best treatment for adult patients with closed extra-articular 5th metacarpal fractures.
Objectives
-
1.
To evaluate the quality of the literature assessing the difference between operative and non-operative treatment of closed extra-articular 5th metacarpal fractures in skeletally mature patients.
-
2.
To determine any difference in outcomes as a result of operative versus non-operative management of closed extra-articular 5th metacarpal fractures.
Methods
We performed a systematic review using methodology adapted from the Cochrane Handbook for Systematic Review of Interventions and with regard to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.15, 16
Search strategy
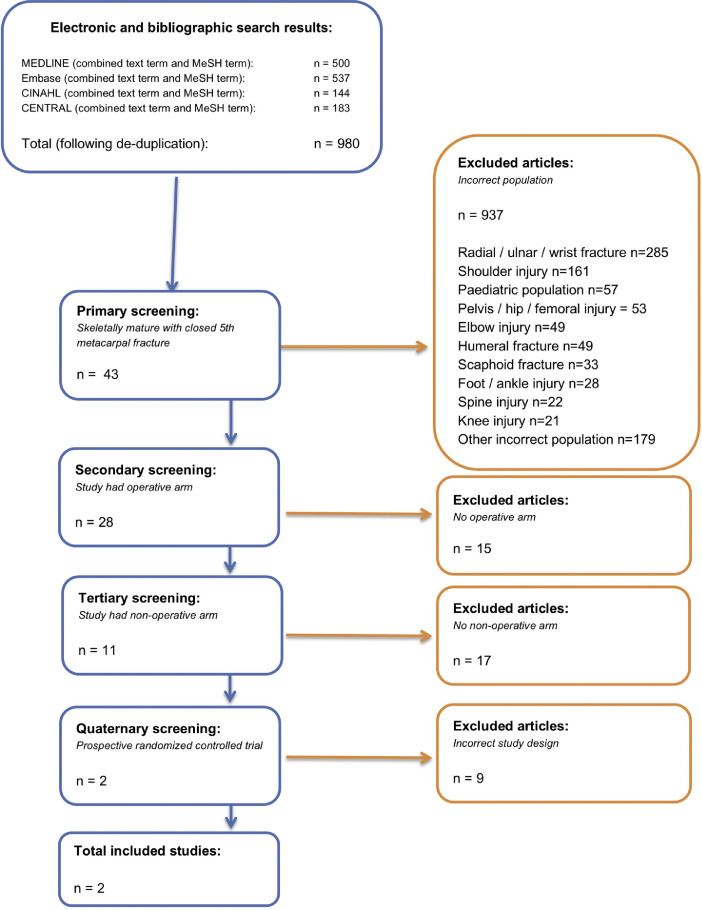
Search terms were used to build two search strategies for each database: a text-term strategy and a database specific MeSH term strategy. These search strategies were uploaded prospectively onto the PROPERO record (CRD42018091633). No date or language limits were applied. We applied the search strategy to the following bibliographic databases using the NHS Evidence Search engine: MEDLINE and EMBASE provided by Ovid, The Cochrane Central Register of Controlled Trials (CENTRAL) and CINAHL provided by the NICE Healthcare Databases Advanced Search (HDAS) interface. Searches were run on 20th March 2018 and included all records from database inception to that date: MEDLINE (1946- March 2018), EMBASE (1974- March 2018), CINAHL (1981- March 2018). The reference list of included articles were hand searched for further relevant publications. EndNote version X8 (Thomas Reuters, New York City, NY, USA) was used to combine and organise the text term and MeSH term searches from each database and then to filter duplicate articles. Grey literature was searched at the time of the primary search via Google Scholar. A study attrition chart was built to display the results of the search strategy and subsequent screening process in accordance with the PRISMA statement (Figure 1).
Figure 1.
PRISMA flow chart of study attrition.
Study eligibility
The inclusion and exclusion criteria were set out during protocol development. Studies were included if they evaluated skeletally mature patients with an extra-articular fracture of the 5th metacarpal receiving operative intervention of any kind directly compared with non-operative intervention of any kind. Studies were excluded if they included patients with more than one hand fracture, open fractures or pathological fractures and did not directly compare operative versus non-operative management.
Outcome data were extracted at the following time points: baseline, 1 week, 6 weeks, 3 months and 12 months post-injury where available. The primary outcome for this review was a patient-reported outcome measure (PROM). Secondary outcomes for this review were: 1. objective functional assessment such as Total active mobilisation (TAM) and other measures of stiffness, grip strength and range of motion at 5th metacarpo-phalangeal joint; 2. Radiological outcomes, such as change in fracture angulation; 3. Adverse events, including infection, mal-union, non-union and osteomyelitis. Only prospective randomized or quasi-randomised controlled clinical trials (RCTs) were included.
Data extraction
From the title, abstract or descriptor, two authors (JCRW, HC) independently screened abstracts to identify potential studies for review, using a pre-specified checklist of the criteria for inclusion. The Rayyan QCRI Tool was used to perform parallel, blinded screening of abstracts.17 Disagreements were resolved by discussion and by referral to a third review author where required (DF). If data were not immediately available for extraction then the authors of the study were contacted by email with a request for unpublished data.
Quality assessment
The review authors JCRW and HC independently assessed risk of bias for each study using the Cochrane Risk of Bias Tool, described in the Cochrane Handbook for Systematic Reviews of Interventions.18 Disagreements were resolved by discussion with a third review author (DF). Domains assessed included: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other sources of bias, e.g. bias arising because of bilateral cases. Each study was graded as high, low or unclear with a justification for the judgement in the 'Risk of Bias' table (Table 2).
Table 2.
Operative outcome data.
| PROM |
Objective at 12 months |
Radiological at 12 months |
Pain (VAS)* |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | n | Satisfaction score | QuickDASH* | Mean MCPJ flexion, degrees (SD) | MCPJ extension, degrees (SD) | Mean grip strength, kg (SD) | TAM, degrees (SD) | Mean post-intervention palmar angulation, degrees (SD) | Mean post-intervention palmar angulation, degrees (SD) | Mean pre-intervention shortening, mm (SD) | Mean post-intervention shortening, mm (SD) | 3 months | 1 year | |
| Strub 2010 | Operative | 20 | 95% very satisfied or satisfied | – | 92 (5) | 6 (5) | 51 (11) | – | 44 (10) | 9 (11) | 2.7 (1.1) | 1.1 (1.3) | 0.53 (0–4) | 0.03 (0–1) |
| Non-operative | 20 | 90% very satisfied or satisfied | – | 93 (4) | 3 (5) | 46 (9) | – | 39 (9) | 34 (11) | 2.6 (1.5) | 2.0 (1.2) | 0.57 (0–3) | 0.1 (0–2) | |
| Sletten 2015 | Operative | 42 | VAS 100 (25-100)* 99% satisfied |
4.10 (6.67) | 75 (11) | 22 (13) | 48 (10) | 259 (20) | – | – | – | – | – | – |
| Non-operative | 43 | VAS 97 (19–100)* 83% satisfied |
3.82 (8.06) | 74 (15) | 22 (9) | 48 (9) | 257(18) | – | – | – | – | – | – | |
All values are mean(SD) unless stated otherwise.
Median (range).
Two review authors independently used the GRADE approach to assess the quality of the evidence for each outcome to determine confidence in the estimate of the observed effects, independently rating the outcomes as high, moderate, low, or very low quality/certainty evidence.19 Consensus on rating was achieved by involvement of a third review author (DF) when required.
Strategy for data synthesis
We performed simple descriptive statistics for patient demographics, using a narrative synthesis to summarise the identified outcomes, and variations in outcome definitions. The study report for Strub et al. contained published data suitable for immediate extraction and potential meta-analysis. This was not the case for Sletten et al., 2015. However, following request, the author provided unpublished data which allowed us to perform data synthesis.20 We performed direct comparison meta-analysis with RevMan5 to generate mean differences for continuous outcomes and odds ratios for dichotomous outcomes with 95% confidence intervals using the Cochrane-Mantel-Haenszel method.21, 22 We used a random effects model due to anticipated differences between study effect sizes.15, 23 No subgroup analysis was planned or undertaken. No indirect comparison meta-analysis was planned or indicated as all included studies contained direct comparisons.21 Statistical heterogeneity was quantified for all direct comparisons using the I2 statistic and ranged from 0-43%, with overall low to moderate heterogeneity.24 Significance was set at the 5% level. Meta-analysis results are displayed in forest plots. If more than two studies were included then they were displayed in a funnel plot for assessment of publication bias.
Results
A total of 980 articles were identified through the searching process. Of these, 937 were excluded (see Figure 1). This resulted in 43 studies of skeletally mature patients (all over 18 years old) with 5th metacarpal fractures of which 28 studies included assessment of an operative intervention. Of these studies, 17 did not compare an operative intervention to a non-operative intervention and so were excluded, resulting in 11 studies that compared operative vs. non-operative management of 5th metacarpal fractures. Two of these studies utilised a prospective randomised controlled trial design and so were included in the final analysis (Figure 1).20, 25
The first RCT by Strub et al. randomised 40 patients with 5th metacarpal neck fractures to either operative fracture fixation with intramedullary bouquet K-wires (n = 20) or non-operative management (n = 20) (Table 1). The non-operative arm (n = 20) received closed reduction, immobilization in a palmar two-finger splint for 5 days, followed by functional mobilisation in a metacarpal brace for 5 weeks. This study used a quasi-randomisation method to allocate patients to operative or non-operative management and was conducted over a 15 month period, following-up patients at 2 weeks, 6 weeks, 3 months, 6 months and 12 months. The quasi-randomisation method consisted of allocating participants to the operative arm if the injury occurred on an even numbered date and the non-operative arm if it occurred on an odd numbered date. Demographics were comparable between the two groups. Outcomes included patient satisfaction scores, pain, objective measures of hand function, radiographic measures and adverse events (Table 2). There was an a priori sample size calculation performed by Strub et al., indicating a sample of 20 per arm, based on ability to detect differences between the groups for range of motion.
Table 1.
Patient demographics.
| Operative |
Non-operative |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | N | Age | Gender (M:F) | Active smokers (%) | Injured dominant hand (%) | Manual employment (%) | N | Age | Sex (M:F) | Active Smokers (%) | Injured dominant hand (%) | Manual employment (%) |
| Strub 2010 | 20 | 28* | 19:1 | – | 17 (85) | 13 (65) | 20 | 32* | 19:1 | – | 19 (95) | 11 (55) |
| Sletten 2015 | 42 | 25⁎⁎ | 14:1 | 15 (36) | 31 (74) | 16 (43) | 43 | 29⁎⁎ | 11:1 | 17 (40) | 31 (72) | 7 (16) |
Median.
Mean.
The second RCT by Sletten et al. was performed in 2015 and randomised 85 participants with 5th metacarpal neck fractures to either intramedullary bouquet K-wires (n = 42) or non-operative management (n = 43), consisting of immobilization in Plaster-of-Paris and buddy taping. Participants were recruited over 29 months and follow-up was at 1 week, 6 weeks, 3 months, 6 months and 12 months. The baseline demographics were similar to the previous RCT. There were minimal differences between the two arms of the trial, other than a higher proportion of manual workers in the operative group (18 vs 7) (Table 2). Sletten et al. performed an a priori sample size calculation indicating 34 participants per arm to detect a change of 8 points in the QuickDASH score at 1 year.
There were no significant differences in patient-reported outcome measure between the operative and non-operative groups in both studies at 12 months (Level 1 Evidence, n = 125). Sletten et al. reported QuickDASH scores at 12 months as a primary outcome. The mean QuickDASH score for the operative group was 4.10, SD 6.67 (95% CI 1.96–6.24) and the mean score for the non-operative group was 3.82, SD 8.06 (95% CI 1.15–6.52). Strub et al. reported a satisfaction score using a visual analogue scale (VAS) as a secondary outcome, with 95% very satisfied or satisfied in the operative group and 90% very satisfied or satisfied in the non-operative group (Table 2).
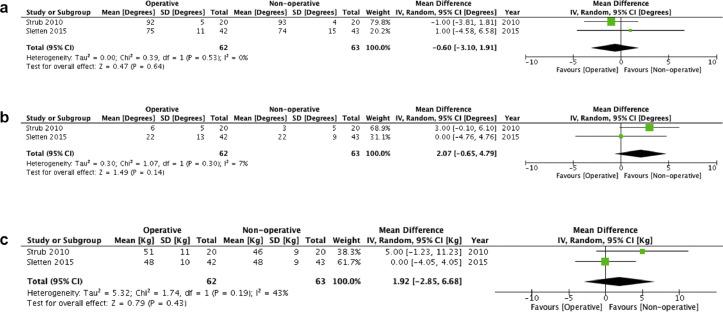
There were no significant differences between objective clinical and radiological outcome measures at 12 months. Both studies reported range of movement (ROM) at the MCPJ and mean grip strength. Sletten et al. additionally reported total active movement (TAM). Strub et al. reported the radiological outcome measures of metacarpal shortening and angulation, which also did not show significant differences at 12 months. Direct comparison meta-analysis of MCPJ flexion (MD –0.60, 95% CI [–3.10–1.91], Figure 2a), MCPJ extension (MD 2.07 95%CI [–0.065–4.79], Figure 2b) and grip strength (MD 1.92 95% CI [–2.85–6.68], Figure 2c) showed no statistical differences between the operatively and non-operatively managed groups, which is consistent with the findings of the individual studies.
Figure 2.
a. Meta-analysis of mean MCPJ flexion (degrees) b. Meta-analysis of mean MCPJ extension (degrees) c. Meta-analysis of mean grip strength (kg).
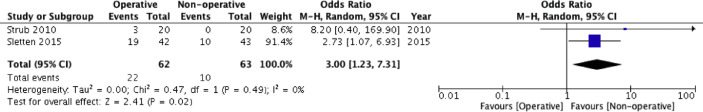
Participants who underwent operative treatment were three times more likely to suffer an adverse event (OR 3.0, 95% CI 1.23–7.31, Figure 3). The direction of effects was consistent between both studies. In the operative groups, adverse events included neurological symptoms (chronic pain, paraesthesia and cold intolerance, n = 12), extrusion of the k-wire (n = 4), infection (n = 2), loosening (n = 1), delayed wound healing (n = 1) and complex regional pain syndrome (n = 2).
Figure 3.
Direct comparison meta-analysis of total rate of adverse events.
In terms of socioeconomic outcomes, Strub et al. reported a greater average time off work for operative participants (6.0 weeks vs 4.8 weeks) than for the non-operative groups, with all patients returning to their previous jobs. Sletten et al. showed a significantly longer time off work for the operative group (42 days vs. 8 days (p =<0.001).
The risk of bias in the two included papers is summarised in Table 3. Strub et al. assigned patients to operative or non-operative treatment using the pseudo-randomisation strategy described above. This attracts a high risk of selection bias as the person randomising patients knows what the next treatment allocation will be on a given day. Blinding of the intervention was not relevant to either of the trial designs. However, outcome assessment at follow-up could have been blinded but was not in this study. No patients were lost to follow up and there was no evidence of selective reporting. Overall the Strub et al. study was judged to be at high risk of bias due to the randomisation method and lack of blinding at outcome assessment.
Table 3.
Risk of Bias.
| Strub 2010 | High risk | High risk | High risk | High risk | Low risk | Unclear risk | Unclear risk | High risk |
|---|---|---|---|---|---|---|---|---|
| Sletten 2015 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Unclear risk | Low risk |
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias | Overall risk of bias |
Sletten et al. randomly assigned patients to operative or non-operative treatment using sealed envelopes. These were shuffled, placed in order, and numbered to give the allocation sequence. This represents an established and generally accepted randomisation technique but is imperfect. This could be improved in future trials with computerized randomisation techniques. Allocation was sufficiently concealed as envelopes were not opened until participants had consented to join the study. As above, clinician and participant blinding would not be possible in this trial. Again, outcome assessors were not blinded which may have introduced detection bias. However, those outcomes that were patient reported would be unaffected (QuickDASH, pain, satisfaction, and quality of life) and those which were measured are unlikely to have been affected (finger range of motion, grip strength). At one year, loss to follow up was 3 of 43 participants in the conservative arm, and 5 of 42 participants were operative arm. This represents <10% loss to follow, and therefore there is low risk of attrition bias. There is no evidence of selective reporting. Overall this paper was judged to be at low risk of bias.
Discussion
We have performed a systematic review and direct comparison meta-analysis of operative versus non-operative management of closed extra-articular 5th metacarpal fractures. A considerable amount of primary research evaluating the treatment of 5th metacarpal fractures has been performed, reflecting its importance in day-to-day hand surgery practice. At the time of writing, there has been a Cochrane review of non-operative interventions for 5th metacarpal fractures, but no research synthesis for alternative operative interventions or non-operative vs. operative interventions.6 We have provided a systematic evaluation of the literature addressing this question and have performed a meta-analysis of published and unpublished trial data (Level 1 Evidence).26
Two randomised controlled trials of operative versus non-operative management of 5th meta-carpal fractures met our inclusion criteria. Despite evidence of sample size calculations, no significant differences were found in the outcomes assessed when operative and non-operative interventions were directly compared in terms of the primary outcomes measured. This is in keeping with two non-randomised comparative studies of 5th metacarpal fractures.12, 27 Westbrook et al. retrospectively compared operative vs non-operative treatment for 5th metacarpal neck and shaft fractures and found no difference in DASH scores or other clinical outcomes for neck fractures, with better outcomes in the non-operatively managed shaft fractures.27 Consistent with our analysis, there was also a significantly higher rate of adverse events in the operative group. McKerrel et al. performed the only other comparative study of operative vs. non-operative management of 5th metacarpal fractures, employing a retrospective observational design and once again finding no compelling differences, other than worse cosmesis in the non-operative group.12
Sletten et al. employed a PROM as the primary outcome for their study: the QuickDASH. The mean score for the operative group was 4.10, SD 6.67 (95% CI 1.96–6.24) and the mean score for the non-operative group was 3.82, SD 8.06 (95% CI 1.15–6.52). The minimum clinically important difference (MCID) for the QuickDASH, which is a scale of 0–100, is defined in the literature as around 15.9–19 points.28, 29 This equates to a non-inferiority limit of 8 points, which was used by Sletten et al. to calculate a sample size of 34 patients per arm. However, the MCID of 16 reported in the literature is much higher than is normally quoted in relation to similar scales for use in fractures of the hand and wrist.29, 30, 31, 32 An MCID of 6–10 is much more commonly employed. Empirically, a smaller MCID would be expected given the sort of effect size normally expected in clinical trials. Using a MCID of 8, the non-inferiority margin in a trial would be 4. As the 95% CIs reported in the trial by Sletten et al. include a non-inferiority margin of 4, it is likely to be underpowered to detect this as difference in terms of non-inferiority. We expect that a much larger trial would be required to detect a true difference in QuickDASH scores, i.e. over 100 participants in each arm. A power calculation with an SD of 10 and a non-inferiority margin of 4 equates to a total of 216 participants (90% power, 5% significance level).33 Strub et al. did not employ a validated measure of hand function as an outcome, focusing on clinical and radiographic outcomes.
We have interrogated the risk of bias of the two included randomised studies using the Cochrane Risk of Bias tool and have found one to be at high risk and one to be low risk. This reduces the reliability of the results and means that recommendations to guide treatment choice cannot currently be made, according to the GRADE approach.
Based on the results of this systematic review and meta-analysis of the two included RCTs, we are unable to reliably advocate operative management of 5th extra-articular metacarpal fractures over non-operative management, especially considering the higher rate of adverse events.12, 20, 25, 27 We have added a meta-analysis of trial data to the growing body of literature on the management of these common injuries, as well as a formal assessment of bias of the two included trials. The data shows there is no discernible difference in outcomes, but the data are not reliable enough to make definitive recommendations and are underpowered to show a difference in PROM. The existing randomised trial evidence is inconclusive. Given that there remains wide variation in the treatment of these common injuries around the world, there is a need for further high-quality evidence to guide clinical practice’.
Our systematic review and meta-analysis was limited by a small number of studies that met the inclusion criteria. Both studies included only 5th metacarpal neck fractures, so we are unable to draw any conclusions about outcomes for other fracture patterns. Similarly, both studies employed a K-wire ‘bouquet’ technique as the operative intervention and so we are unable to ascertain outcomes of other surgical fixation techniques. Widening the scope to include observational studies would have increased the data available for analysis but would have muddied the meta-analysis, reducing the validity of our results. There was one difference between the full review and the protocol: the meta-analysis, which was performed following provision of unanticipated data and was performed using standard methods as described above.
Conclusion
Our systematic review and meta-analysis of two RCTs has shown no discernible difference between patient-reported and clinician-captured outcomes between operative and non-operative management of 5th metacarpal fractures, with a higher rate of adverse events for operative candidates. The included RCTs have some shortcomings in terms of including small sample sizes and methodological faults. At present the best management of one of the most common fractures in the UK is unclear and so a definitive, large scale, multi-centre, pragmatic design, RCT with precise outcome measurement is indicated to guide future practice.
Funding statement
Justin Wormald is funded by the NIHR. The research was supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). The views expressed are those of the authors and not necessarily those of the NIHR, NHS or Department of Health and Social Care.
Twitter handles
Wormald JCR - @JCRWormald
Claireaux H - @harryclax
Gardiner MD - @mattgardiner
Furniss D - @DominicFurniss
Review team and contributions
Mr. Justin C R Wormald MBBS MRes MRCS
NIHR Academic Clinical Fellow and Specialist Registrar in Plastic, Reconstructive and Hand Surgery, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford, Oxford, UK
Review lead, manuscript preparation, screening, data extraction, review methodology, statistics
Dr. Harry Claireaux BSc MBChB
Academic Foundation Doctor, Thames Valley Foundation School
Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford and Trauma Research Department, Kadoorie Centre for Critical Care Research and Education, John Radcliffe Hospital, Oxford
Junior review member, manuscript preparation, screening, data extraction
Mr. Matthew Gardiner MA PhD FRCS(Plast)
Honorary Clinical Lecturer and Specialist Registrar in Plastic, Reconstructive and Hand Surgery, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford, Oxford, UK
Manuscript review, methodology, clinical and trial expertise
Prof. Abhilash Jain MBBS MRCS MSc PhD FRCS (Plast)
Associate Professor and Consultant in Plastic, Reconstructive and Hand Surgery, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford, Oxford, UK
Senior manuscript review, methodology, clinical and trial expertise
Prof. Dominic Furniss DM MA MBBCh FRCS(Plast)
Associate Professor and Honorary Consultant Plastic, Reconstructive and Hand Surgery, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford, Oxford, UK
Senior manuscript review, manuscript preparation, methodology, statistics, clinical and research expertise
Prof. Matthew Costa PhD FRCS(Tr&Orth)
Professor of Orthopaedic Trauma Surgery and Honorary Consultant Trauma Surgeon
Oxford Trauma, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University, Oxford, UK.
Senior review lead, manuscript preparation, methodology, statistics, trial expertise
Acknowledgments
Acknowledgments
We are grateful to Dr. Ida Sletten for her support in conducting this review and for the provision of additional data.
Conflict of Interest
None.
Footnotes
Parts of this article has been presented at the following meetings/conferences: 1. RSTN Trials Day – Viper's Nest Session, Edinburgh, United Kingdom on 22nd June 2018. 2. Hand Fracture Research Workshop – Centre of Evidence Based Hand Surgery, Nottingham, United Kingdom on 23rd November 2018. 3. BAPRAS Winter Meeting – RSTN Session, London, United Kingdom on 29th November 2018.
References
- 1.Bucholz R.W. 7th Ed. Vol. 1. Lippincott Williams & Wilkins; 2009. The epidemiology of fractures. (Rockwood and Green's Fractures in Adults). Chapter 3. [Google Scholar]
- 2.Anakwe R.E., Aitken S.A., Cowie J.G., Middleton S.D., Court-Brown C.M. The epidemiology of fractures of the hand and the influence of social deprivation. J Hand Surg Eur. 2011;36:62–65. doi: 10.1177/1753193410381823. [DOI] [PubMed] [Google Scholar]
- 3.Greeven A., Bezstarosti S., Krijnen P., Schipper I. Open reduction and internal fixation versus percutaneous transverse Kirschner wire fixation for single, closed second to fifth metacarpal shaft fractures: A systematic review. Eur J Trauma Emerg Surg. 2016;42:169–175. doi: 10.1007/s00068-015-0507-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ali A., Hamman J., Mass D.P. The biomechanical effects of angulated boxer's fractures. J Hand Surg Eur. 1999;24:835–844. doi: 10.1053/jhsu.1999.0835. [DOI] [PubMed] [Google Scholar]
- 5.Hunter J.M., Cowen N.J. Fifth metacarpal fractures in a compensation clinic population: A report on one hundred and thirty-three cases. J Bone Joint Surg. 1970;52:1159–1165. [PubMed] [Google Scholar]
- 6.Poolman R.W., Goslings J.C., Lee J.B., Statius Muller M., Steller E.P., Struijs P.A. Conservative treatment for closed fifth (small finger) metacarpal neck fractures. Cochrane Database Syst Rev. 2005;20(3) doi: 10.1002/14651858.CD003210.pub3. CD003210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giddins G.E. The non-operative management of hand fractures. J Hand Surg Eur. 2015;40:33–41. doi: 10.1177/1753193414548170. [DOI] [PubMed] [Google Scholar]
- 8.Al-Qattan M.M. Outcome of conservative management of spiral/long oblique fractures of the metacarpal shaft of the fingers using a palmar wrist splint and immediate mobilisation of the fingers. J Hand Surg Eur. 2008;33:723–727. doi: 10.1177/1753193408093559. [DOI] [PubMed] [Google Scholar]
- 9.Ali H., Rafique A., Bhatti M., Ghani S., Sadiq M., Beg S.A. Management of fractures of metacarpals and phalanges and associated risk factors for delayed healing. J Pak Med Assoc. 2007;57:64–67. [PubMed] [Google Scholar]
- 10.Bloom J.M., Hammert W.C. Evidence-based medicine: Metacarpal fractures. Plast Reconstr Surg. 2014;133:1252–1260. doi: 10.1097/PRS.0000000000000095. [DOI] [PubMed] [Google Scholar]
- 11.Diaz-Garcia R., Waljee J.F. Current management of metacarpal fractures. Hand Clin. 2013;29:507–518. doi: 10.1016/j.hcl.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 12.McKerrell J., Bowen V., Johnston G., Zondervan J. Boxer's fractures–conservative or operative management? J Trauma. 1987;27:486–490. [PubMed] [Google Scholar]
- 13.Adams J.E., Miller T., Rizzo M. The biomechanics of fixation techniques for hand fractures. Hand Clin. 2013;29:493–500. doi: 10.1016/j.hcl.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Foucher G. Bouquet osteosynthesis in metacarpal neck fractures: A series of 66 patients. J Hand Surg Am. 1995;20:86. doi: 10.1016/s0363-5023(95)80176-6. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JPT. Green S. (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
- 16.Moher D., Liberati A., Tetzlaff J., Altman D.G. The PRISMA group (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:2535. [PMC free article] [PubMed] [Google Scholar]
- 17.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins J., Altman D.G. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Book Series; 2008. Assessing risk of bias in included studies; pp. 187–241. [Google Scholar]
- 19.Guyatt G.H., Oxman A.D., Vist G.E. Grade: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sletten I.N., Hellund J.C., Olsen B., Clementsen S., Kvernmo H.D., Nordsletten L. Conservative treatment has comparable outcome with bouquet pinning of little finger metacarpal neck fractures: A multicentre randomized controlled study of 85 patients. J Hand Surg Eur. 2015;40:76–83. doi: 10.1177/1753193414560119. [DOI] [PubMed] [Google Scholar]
- 21.Song F., Loke Y.K., Walsh T., Glenny A.-M., Eastwood A.J., Altman D.G. Methodological problems in the use of indirect comparisons for evaluating healthcare interventions: Survey of published systematic reviews. BMJ. 2009;338:1147. doi: 10.1136/bmj.b1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- 23.Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 24.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strub B., Schindele S., Sonderegger J., Sproedt J., von Campe A., Gruenert J.G. Intramedullary splinting or conservative treatment for displaced fractures of the little finger metacarpal neck? A prospective study. J Hand Surg Eur. 2010;35:725–729. doi: 10.1177/1753193410377845. [DOI] [PubMed] [Google Scholar]
- 26.OCEBM Levels of Evidence Working Group. “The Oxford Levels of Evidence 2”, Oxford Centre for Evidence-Based Medicine. https://www.cebm.net/index.aspx?o=5653. [Accessed Fri Sep 28 2018].
- 27.Westbrook A.P., Davis T.R.C., Armstrong D., Burke F.D. The clinical significance of malunion of fractures of the neck and shaft of the little finger metacarpal. J Hand Surg Eur. 2008;33:732–739. doi: 10.1177/1753193408092497. [DOI] [PubMed] [Google Scholar]
- 28.Franchignoni F., Vercelli S., Giordano A., Sartorio F., Bravini E., Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH) J Orthop Sports Phys Ther. 2014;44:30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 29.Polson K., Reid D., McNair P.J., Larmer P. Responsiveness, minimal importance difference and minimal detectable change scores of the shortened disability arm shoulder hand (QuickDASH) questionnaire. Man Ther. 2010;15:404–407. doi: 10.1016/j.math.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 30.Adams A., Ketchersid J., Tan W.H., Calfee R.P., Howard D. Minimal clinically important differences on the DASH, Quick-DASH and PRWE: Level 2 evidence. J Hand Surg Eur. 2012;37:17. [Google Scholar]
- 31.Costa M.L., Achten J., Parsons N.R. Percutaneous fixation with Kirschner wires versus volar locking plate fixation in adults with dorsally displaced fracture of distal radius: Randomised controlled trial. BMJ. 2014;349:4807. doi: 10.1136/bmj.g4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dias J., Brealey S., Choudhary S. Scaphoid waist internal fixation for fractures trial (swifft) protocol: A pragmatic multi-centre randomised controlled trial of cast treatment versus surgical fixation for the treatment of bi-cortical, minimally displaced fractures of the scaphoid waist in adults. BMC Musculoskelet Disord. 2016;17:248. doi: 10.1186/s12891-016-1107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sealed Envelope Ltd. 2012. Power calculator for continuous outcome non-inferiority trial. [Online] Available from: https://www.sealedenvelope.com/power/continuous-noninferior/ [Accessed Fri Sep 28 2018].