Abstract
Midazolam is a commonly used benzodiazepine in palliative care and is considered one of the four essential drugs needed for the promotion of quality care in dying patients. Acting on the benzodiazepine receptor, it promotes the action of gamma-aminobutyric acid. Gamma-aminobutyric acid action promotes sedative, anxiolytic, and anticonvulsant properties. Midazolam has a faster onset and shorter duration of action than other benzodiazepines such as diazepam and lorazepam lending itself to greater flexibility in dosing than other benzodiazepines. The kidneys excrete midazolam and its active metabolite. Metabolism occurs in the liver by the P450 system. This article examines the pharmacology, pharmacodynamics, and clinical uses of midazolam in palliative care.
Keywords: agitation, benzodiazepines, delirium, dyspnea, gamma-aminobutyric acid, imidazole ring, insomnia, midazolam, palliative sedation, seizures
Introduction
Since the accidental synthesis of the first benzodiazepine, chlordiazepoxide, in 1961, benzodiazepines have emerged as important agents for symptom control in palliative medicine.1 Benzodiazepines treat a variety of symptoms in palliative care, including anxiety, delirium associated with alcohol withdrawal, seizures, and when symptoms are refractory, they are used for palliative sedation therapy.2,3 Benzodiazepines combined with haloperidol is emerging as an effective treatment for delirium.4 Benzodiazepines if misused can lead to withdrawal symptoms and cognitive impairment.2 The ideal benzodiazepine for use in palliative care would be one where there is rapid onset of action, yet have a short duration to minimize adverse effects. Midazolam is one benzodiazepine fitting this description. This review examines the pharmacology, pharmacodynamics, and evidence for use in palliative medicine. Midazolam is considered one of the four essential drugs that should be available in all settings caring for dying patients.3
Structure of midazolam
Midazolam contains a benzene ring fused to a seven-membered diazepine ring (see Figure 1).5
Figure 1.
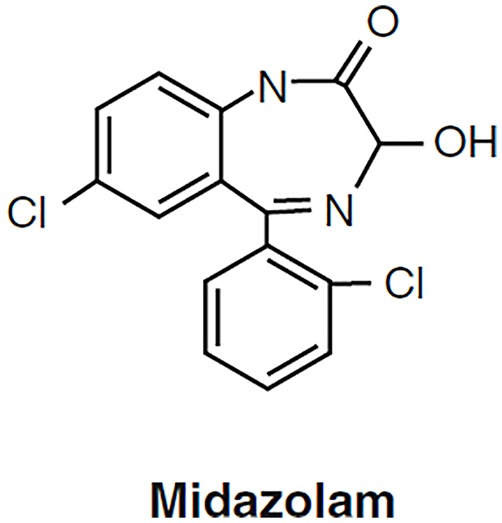
Structure Midazolam.
Pharmacodynamics
Midazolam binds with high affinity to the benzodiazepine receptor, which is at the interface of the α and γ subunits of the gamma-aminobutyric acid receptor (GABA).6 GABAA receptors mediate inhibitory functions in the human brain.7 They are protein complexes consisting of five subunits, arranged pseudo-symmetrically around an ion channel selective for chloride (Cl−).8 The major receptor, GABAA, consists of α1, β2, and γ2 subunits.9 Benzodiazepines bind to the α and γ interface leading to anxiolytic, sedative, muscle relaxant, and anticonvulsive actions. Benzodiazepines are considered exogenous modulators of the GABA receptor.10 When compared with other benzodiazepines, midazolam binds to the GABA benzodiazepine binding site as avidly as clonazepam (Ki 0.85 ± 0.02 nM) and lorazepam, but more avidly than diazepam (Ki 10 ± 1 nM).
Pharmacokinetics and metabolism
Midazolam exists in a pH equilibrium between closed and open ring structures.11 The benzodiazepine ring of midazolam opens at lower pH. At physiologic pH, the ring closes and the molecule becomes lipid soluble allowing rapid penetration across the blood–brain barrier.12–14 The pH characteristics of midazolam allow preparation of salts that are readily soluble in aqueous media.11 Midazolam onset of action is rapid regardless of the route. Both the intravenous (IV) and subcutaneous routes manifest onset of action within minutes.15 Following IV administration, midazolam has a distribution half-life of 6–15 min. Midazolam has an elimination half-life of 1.5–3 h. The duration of action is 60–120 min.16 The lipophilic nature of midazolam accounts for the relatively large volume of distribution at steady state, that is, 0.8–1.7 l/kg.17 Oxidation of the imidazole ring leads to greater clearance than other benzodiazepines such as diazepam.18 Intramuscular midazolam is rapidly absorbed with the onset of action within 2 min of administration.13 Peak serum concentrations occur between 23 and 40 min. Intramuscular midazolam has a bioavailability of 90%.13,19,20 Intranasal (IN) midazolam has a rapid onset of action with a Tmax of 10–14 min. Bioavailability ranges between 60% and 80%. Increases in Cmax and AUC are dose proportionate.21 Oral bioavailability is 40–50% due to extensive first-pass metabolism.22,23 When given orally, the onset of action is approximately 15 min reflecting its rapid absorption from the gastrointestinal (GI) tract.23 CYP3A4 and CYP3A5 hydroxylate midazolam.24 Patients with CYP3A4 mutations can experience increased sedation.25 Metabolism yields three metabolites, α-hydroxy midazolam, 4-hydroxy midazolam, and α,4-hydroxy midazolam, all excreted as glucuronides.14 α-hydroxy-midazolam is pharmacologically active with sedative properties like that of midazolam. It is a formation rate-limited metabolite and closely follows midazolam concentrations.26 When glucuronidated, the α-hydroxy metabolite loses its potency and is one-tenth as potent as midazolam.26 α-Hydroxy-midazolam accumulates to a greater extent after oral administration because of the first-pass metabolism. The α-hydroxy-midazolam metabolite has an elimination half-life of 1 h in humans. Excretion of midazolam is primarily by the kidneys.14 Table 1 compares the pharmacology of midazolam with other commonly used benzodiazepines.
Table 1.
Pharmacology of Midazolam with Other Commonly Used Benzodiazepines.
| Drug | Bioavailability (oral) | Half-life (h) | Tmax (h) |
|---|---|---|---|
| Midazolam | 40–50% | 1–4 | 0.5–1.0 |
| Lorazepam | 90% | 10–20 | 2.5 |
| Diazepam | 90% | 25–50 | 0.5–1.5 |
| Clonazepam | >80% | 20–40 | 1–4 |
Adapted from Howard and colleagues.27
Dosing in special populations
Liver disease
Advanced cirrhosis reduces the plasma clearance and prolongs the half-life of midazolam. MacGilchrist and coworkers showed that cirrhotic patients had a significantly (p < 0.05) prolonged elimination half-life of midazolam (3.9 versus 1.6 h) compared with a control group.28 The cirrhotic group experienced more profound sedation for up to 6 h when compared with controls. Critically ill patients with liver failure need careful dosing of midazolam.
Renal disease
Midazolam accumulates and can cause prolonged sedation in patients with renal dysfunction.29 Patients can experience prolonged sedation in the setting of severe renal failure.30 The active metabolite α-hydroxymethyl midazolam accumulates and contributes to sedation. Because patients with chronic renal failure and hypoalbuminemia have a higher fraction of unbound drug at greater risk for adverse effects, careful dosing of continuous infusions is necessary.31
Advanced illness
Terminally ill patients experience significant physiologic changes affecting drug disposition. Loss of body weight and cachexia can lead to a decrease in Vd (volume of distribution). Decreasing Vd leads to increases in drug concentration and effect for lipophilic drugs like midazolam.32 Low albumin levels, commonly seen in advanced illness, decrease the clearance of midazolam.33
Elderly
Midazolam clearance decreases in the elderly. Prolonged elimination of half-life occurs in the elderly.34 Liver blood flow decreases with age, and midazolam is a drug with a low hepatic extraction (0.3), so elimination prolongs in low hepatic blood flow states.32,35
Pediatric
In healthy neonates, the half-life (t1/2) and the clearance (Cl) are 3.3-fold longer and 3.7-fold shorter, respectively, than in adults owing to low levels of CYP3A4 and CYP3A5. These enzymes do not surge until the fourth week of life. Disease affects the pharmacokinetics of midazolam in neonates; multiple organ failure reduces the clearance of midazolam, and mechanical ventilation prolongs the t1/2 of this drug. Extracorporeal membrane oxygenation (ECMO) therapy increases t1/2, Cl, and Vd of midazolam several times.36 Large inter-individual variations in midazolam clearance values exist in critically ill neonates, infants, children, and adolescents.37 Midazolam appears to be a safe drug to use in neonates with incidences of hypotension and respiratory depression in low percentages.36
Drug interactions
CYP3A4 metabolizes midazolam almost exclusively to its hydroxyl metabolites.38 Inducers and inhibitors of CYP3A4 potentially affect midazolam levels. Drugs such as glucocorticoids, antifungals, antibiotics, retrovirals, antidepressants, calcium channel blockers, and H2 blockers interact to influence the disposition of midazolam.38,39 Table 2 summarizes the effects of midazolam drug interactions.
Table 2.
Drug Interactions.
| Drug | Effect | Mechanism of action | Clinical importance |
|---|---|---|---|
| Glucocorticoids | Decreased AUC (64%) and increased clearance of midazolam (127%)40 | Induction of CYP3A | Prednisone does not affect pharmacokinetics of midazolam41 |
| Phenytoin | Phenytoin lowers midazolam levels. Bioavailability may be reduced as much as 90% according to some studies42 | Induction of CYP3A4 | Unknown |
| Herbal medicine St John’s wort |
Increased midazolam clearance43–45 | Induction of CYP3A4 | Unknown |
| Non-nucleoside reverse transcriptase inhibitor (efavirenz) | Oral clearance increased by 70%, and midazolam systemic clearance after intravenous administration was significantly increased by 27%46 | Induction of CYP3A4 | Unknown |
| Fluconazole Itraconazole47 Ketoconazole47 Posaconazole47 |
Increase AUC and half-life of midazolam48,49 | Inhibition of CYP3A | Unknown |
| Chemotherapy agents Nilotinib Idelalisib Crizotinib Pazopanib Paclitaxel Ceritinib |
Nilotinib inhibits CYP3A450
Idelalisib increases the AUC of midazolam fivefold51 Crizotinib inhibits CYP3A452 Pazopanib only weakly inhibits CYP3A53 Midazolam may interfere with paclitaxel metabolism54 and AUC of midazolam47 |
Inhibition of CYP3A4 | Unknown |
| Grapefruit juice | Delays absorption and reduces first-pass effect on midazolam resulting in increased blood plasma levels of midazolam of 56% and increased midazolam bioavailability of 35%55 | Inhibition of CYP3A4 | Unknown |
| Protease inhibitors (ritonavir, atazanavir, darunavir, fosamprenavir) | Inhibit CYP3A4 leading to increased midazolam levels56,57 | Inhibition of CYP3A4 | May prolong sedation and increase sedation risk58 |
| Simeprevir (treatment of hepatitis C infection) | Increased AUC of midazolam (oral) by 1.3–1.459 | Inhibition of CYP3A4 | Unknown |
| Calcium channel blockers | Increase the AUC for midazolam60,61 | Inhibition of CYP3A4 | Unknown |
| Antidepressants Fluvoxamine Paroxetine Citalopram |
Nefazodone (now discontinued) inhibits CYP3A4 and increases the AUC by 400%62 | Inhibition of CYP3A4 | No reported interaction with mirtazapine |
| Aprepitant | Increases the AUC63–66 | Inhibition of CYP3A4 | Especially at doses of 125 mg aprepitant63
Oral midazolam |
| Netupitant/palonosetron combination | Increases Cmax by 40% and AUC increased by 144%67 | Inhibition of CYP3A4 | Unknown |
AUC, Area under the curve.
Specific drug interactions are noted below. In general, the combination of benzodiazepines with drugs like opioids and antihistamines increases the risk of sedation and respiratory depression.
Adverse effects
Besides somnolence, most adverse effects are of low frequency.68 Clinical trials show that midazolam is safe to give with opioids for the treatment of dyspnea in advanced illness.69,70 Hiccups occur with an incidence of approximately 3.6%.71 Benzodiazepines cause disinhibition reactions to occur in both adult and pediatric patients, and midazolam is no exception.72 However, benzodiazepines in combination with antipsychotics help control delirium.73 Vorsanger and Roberts reported two cases of athetoid movements after receiving midazolam as a premedication.74 Physostigmine reversed the movement. Midazolam can cause prolonged anterograde amnesia.75–77
Clinical applications of midazolam in palliative care
Palliative sedation therapy
Terminally ill cancer patients near the end of life can experience refractory symptoms, which require palliative sedation. Midazolam is the most common benzodiazepine used for palliative sedation therapy.78,79 It is also considered the first-line drug because of its ability to be easily reversed, lending itself to use in respite sedation and short-term palliative sedation.80 One report in adult palliative sedation found mean midazolam doses of 29 mg/day (median: 30 mg, range: 15–60 mg/day).81 A recent study in an Israeli hospice found average doses of midazolam up to 79 mg/day.82 Mercadante and coworkers found mean doses were 23–58 mg/day.83 Midazolam is useful for palliative sedation in the home setting for pediatric patients.84 Initial doses were in the range of 0.02–0.08 mg/kg/h.84 Mean dose was 0.02–1.0 mg/kg/h.84 In treating terminal restlessness and agitation, Bottomley and Hanks15 used continuous infusion of subcutaneous midazolam in 23 advanced cancer patients in hospice. The investigators achieved symptom control in 22 of 23 patients using initial doses of 0.4–0.8 mg/h. The mean maximum dose was 2.9 mg/h. Dosing varied between patients highlighting the need to individualize dosing. Midazolam along with droperidol or olanzapine remains a treatment option for agitated patients in the emergency room.85
Dyspnea
Opioids are useful for the treatment of terminal dyspnea and anxiolytics help manage the anxiety associated with dyspnea. One trial (single-blinded) studied subcutaneous midazolam as an adjunct therapy to morphine in treating severe dyspnea in terminally ill cancer patients (N = 101).69 Patients received one of three treatments. The morphine group consisted of subcutaneous scheduled morphine (2.5 mg every 4 h for opioid-naïve patients or a 25% increment over the daily dose for those receiving baseline opioids) with midazolam rescue doses (5 mg) for breakthrough dyspnea. The midazolam group received scheduled midazolam (5 mg every 4 h) with morphine rescues (2.5 mg) for breakthrough dyspnea. The morphine–midazolam group received scheduled morphine (2.5 mg every 4 h for opioid-naïve patients or a 25% increment over the daily dose for those receiving baseline opioids) and midazolam (5 mg every 4 h) with morphine rescue doses (2.5 mg) for breakthrough dyspnea; 35 patients entered in the morphine group, 33 in the midazolam group, and 33 in the morphine–midazolam group. At 24 h, the frequency of dyspnea relief was 69%, 46%, and 92% in the morphine, midazolam, and combined groups, respectively (p = 0.0004 and p = 0.03 for combined versus midazolam and combined versus morphine, respectively). At 48 h, the percentage of no relief was lowest on the morphine–midazolam group (those receiving scheduled morphine and midazolam; 4%). The data show that adding midazolam to morphine enhances dyspnea control.
Another study by the same author70 compared morphine with midazolam for symptom relief during evaluations for dyspnea in patients with advanced cancer; 63 ambulatory patients with advanced cancer and dyspnea were clinically characterized and then randomized to receive either oral morphine or oral midazolam. Titration occurred in the clinic, and starting doses were 2 mg for midazolam and 3 mg for morphine, with incremental steps of 25% of the preceding dosing every 30 min. Reduction of dyspnea by 50% was the goal. Patients continued outpatient status during diagnostic studies; 31 patients with dyspnea entered the morphine arm, and 32 patients entered the midazolam arm. During the initial in-clinic phase, alleviation of dyspnea by 50% occurred in all patients, whether they received morphine or midazolam. At 3–5 days follow-up, the dyspnea intensity was less in the midazolam arm [numeric rating scale (NRS): 0–10; p = .0001–.0002], and these significant differences extended to breakthrough dyspnea over the same time frame in the midazolam arm. Patients tolerated both treatments well with mild somnolence being the most common adverse event. Neither morphine nor midazolam use led to needing additional diagnostic and therapeutic interventions. The study showed that midazolam was better than morphine for the immediate and long-term relief of dyspnea.70 IN midazolam showed no clinical benefit for the management of dyspnea in one randomized, double-blind controlled trial.86 Dyspnea scores did not differ between IN midazolam and placebo. Baseline anxiety levels were low. There were concerns about drug delivery in that it was difficult for participants to use spray bottles.86
Seizures
Midazolam, as well as diazepam and lorazepam, are drugs most widely used as initial management for status epilepticus which is defined as seizures lasting more than 5 min or more than one seizure without recovery in between.87,88 Midazolam is one of the best studied drugs in the out-of-hospital setting. The RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial) study identified intramuscular midazolam as being non-inferior to IV lorazepam in both adults and children for seizures persisting more than 5 min.89,90 Midazolam is versatile in that it controls status epilepticus by a variety of routes, including IV and subcutaneous routes. It is effective when given buccally, intranasally, or rectally.91 Potential drawbacks when using the IN route include seizing patients spitting or blowing out medication during administration.90 In the hospice setting, lorazepam or midazolam can be considered for status. Lorazepam may be favored due to its longer half-life, but as seen with the RAMPART study, both drugs are efficacious.91
Analgesic effect
Ho and Ismail analyzed 13 randomized controlled trials (RCTs) looking at the analgesic effect of intrathecal midazolam. Studies suggest a delay in need of rescue analgesia in the postoperative setting. Intrathecal midazolam did not affect motor blockade.92
Insomnia and terminal illness
Matsuo and Morita evaluated IV midazolam for insomnia in palliative care patients and found it to be as effective as flunitrazepam, but more costly.93 Incidences of a hangover effect, delirium, treatment withdrawal, or death did not differ. Respiratory depression, defined as apnea, respiratory arrest, and decreased respiratory rate, occurred significantly more often in those receiving flunitrazepam than midazolam. Midazolam given subcutaneously works well also for insomnia in palliative care.94
Delirium and agitation
Goncalves and coworkers95 found the combination of intramuscular haloperidol and midazolam to control agitation in advanced cancer in 91% of cases. Agar and coworkers used midazolam as a rescue medication for refractory delirium. In that study, there were better outcomes in the placebo–midazolam rescue arm than the other arms which used antipsychotics and rescue midazolam.73
Ketamine emergence phenomena
Midazolam has been used to treat or prophylactically treat emergence phenomenon associated with ketamine use.96
Hiccups
Midazolam may be useful in the management of hiccups in terminal illness.97
Pruritis and biliary obstruction
Prieto found the use of continuous infusion of midazolam to be effective in refractory pruritis associated with biliary obstruction. The original intent was to use midazolam for sedation given the refractory nature of the pruritis. Surprisingly, the pruritis improved and there was minimal sedation. Midazolam was started subcutaneously at 1 mg per hour after a 2 mg bolus. The dose was increased 1 mg every 15 min as needed for itching. During the next 4 weeks, the patient was slowly titrated to 84 mg/h of midazolam, with total control of his itching.98
Muscle spasm
Parenteral benzodiazepines, such as midazolam, can be used to relieve muscle spasm and spasticity in the last days of life (Table 3).27
Table 3.
Schedule of Administration.
| Indication | Dosing | Comment |
|---|---|---|
| Palliative sedation | 1–5 mg IV bolus every 5 min until comfortable or maximum of 20 mg.99,100 Continuous infusion is started generally 0.5–1 mg/h101
Usual effective dose range is 1–20 mg/h subcutaneously or intravenously100 |
If the continuous infusion rate reaches 20 mg/h, then some have recommended switching to another sedating agent.102 Can also be given subcutaneously103 |
| Terminal agitation | Wide dosing range. Usual starting dose 0.4–0.8 mg/h15
Doses may go up to 3 mg/h. Patients may become tolerant to midazolam necessitating dose increase. As needed dosing can match the hourly dose and can be given as frequently as q 15 min |
If necessary, increase both the as-needed dose and the infusion until the patient is calm. Some experts recommend considering adding an antipsychotic if the dose reaches >30 mg/24 h by continuous infusion27
Haloperidol is suggested as an antipsychotic |
| Dyspnea | Midazolam dosing for dyspnea is up to 5 mg subcutaneously or intravenously every 4 h.69 Oral midazolam at 2 mg orally as often as every 4 h has been shown to be beneficial.70 Rescue doses at 50–100% of the scheduled dose are given as frequent as every 15 min | |
| Seizures | Midazolam boluses of 0.1–0.3 mg/kg are used for status epilepticus.104 Continuous infusions of 0.05–0.4 mg/kg/h can also be used.105 Other dosing recommendations for seizures include 10 mg intranasally, intramuscularly, or buccally for patients with a body weight of >40 kg or 5 mg for a patient with a body weight of 13–40 kg89 | It may take up to 10 min to abort the seizure; doses can be repeated if the seizure persists after 5 min |
| Catastrophic bleeding | 5–10 mg IV every 5 min to a maximum dose of 20 mg106 | |
| Insomnia | Midazolam 2.0 mg subcutaneously/IV to maximum dose of 18 mg qhs93,94 |
IV, intravenous.
Pediatric dosing
Dosing in children is weight based.37 There is a fourfold variation in dosage administration (30–120 µg/kg/h) for children between the ages of 6 months and 12 years. In critically ill children, there is greater than fourfold variation in midazolam clearance. The greater variation in midazolam clearance values than the dosage schedule suggests that many children may receive too high or too low a dose of midazolam to obtain satisfactory sedation. This may explain the poor sedation achieved in clinical trials with midazolam in critically ill children. As a group, pediatric patients generally require higher dosages of midazolam hydrochloride (mg/kg) than do adults. Younger (less than 6 years) pediatric patients may require higher dosages (mg/kg) than older pediatric patients and may require close monitoring. Midazolam should not be administered by rapid injection in the neonatal population. Severe hypotension and seizures have been reported following rapid IV administration, particularly with concomitant use of fentanyl.107 Doses given to children must be calculated on a mg/kg basis. For children 6 months to 5 years of age, a dose of 0.05–0.1 mg/kg is recommended. Dosages up to 0.6 mg/kg titrated slowly may be necessary to achieve the desired endpoint. For children 6–12 years of age, the recommended dose is 0.025–0.05 mg/kg with doses up to 0.4 mg/kg to achieve the desired endpoint.14
Route conversions and conversions from other benzodiazepines
Converting midazolam from the oral to IV/subcutaneous route uses a 2:1 ratio.22,108 Midazolam’s potency in comparison with other benzodiazepines is shown in Table 4.27 This may be useful when switching from one benzodiazepine to another when greater clinical efficacy is required.
Table 4.
Benzodiazepine Equivalents.27
| Drug | Dose (mg) |
|---|---|
| Diazepam | 5 |
| Lorazepam | 0.5 |
| Midazolam | 5 |
| Alprazolam | 0.5 |
Pharmacoeconomics
The cost of giving midazolam given by IV injection/subcutaneous injection ranges from 1.75 to 8 US dollars/dose depending on concentration. This is comparable with the cost of IV Ativan.109
Conclusion
Midazolam is a benzodiazepine with sedative, anxiolytic, muscle relaxant, and anticonvulsant properties. Its lipid soluble properties allow rapid action. Advantages also include the ability to be given by multiple routes and its short half-life. The short half-life allows for reversibility of drug effect if desired. Clinicians should consider this drug when there is a need for a short-acting, rapid-onset benzodiazepine. As a versatile drug, it is used for the management of palliative sedation, terminal restlessness, seizures, and dyspnea. It can be used to manage anxiety and symptoms of dyspnea in the setting of withdrawal of care and catastrophic bleeding. Disadvantages of the drug include propensity to be rapidly metabolized with continued use.
Footnotes
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Eric Prommer  https://orcid.org/0000-0002-2985-016X
https://orcid.org/0000-0002-2985-016X
References
- 1. Pandeya SN, Rajput N. Synthesis and anticonvulsant activity of various Mannich and Schiff bases of 1,5-benzodiazepines. Int J Med Chem 2012; 2012: 237965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Riss J, Cloyd J, Gates J, et al. Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta Neurol Scand 2008; 118: 69–86. [DOI] [PubMed] [Google Scholar]
- 3. Lindqvist O, Lundquist G, Dickman A, et al. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med 2013; 16: 38–43. [DOI] [PubMed] [Google Scholar]
- 4. Hui D, Frisbee-Hume S, Wilson A, et al. Effect of lorazepam with haloperidol vs haloperidol alone on agitated delirium in patients with advanced cancer receiving palliative care: a randomized clinical trial. JAMA 2017; 318: 1047–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lopez-Romero B, Evrard G, Durant F, et al. Molecular structure and stereoelectronic properties of sarmazenil: a weak inverse agonist at the omega modulatory sites (benzodiazepine receptors): comparison with bretazenil and flumazenil. Bioorg Med Chem 1998; 6: 1745–1757. [DOI] [PubMed] [Google Scholar]
- 6. Sigel E, Steinmann ME. Structure, function, and modulation of GABA(A) receptors. J Biol Chem 2012; 287: 40224–40231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stephenson FA. The GABAA receptors. Biochem J 1995; 310(Pt. 1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baumann SW, Baur R, Sigel E. Forced subunit assembly in alpha1beta2gamma2 GABAA receptors. J Biol Chem 2002; 277: 46020–46025. [DOI] [PubMed] [Google Scholar]
- 9. Chang Y, Wang R, Barot S, et al. Stoichiometry of a recombinant GABAA receptor. J Neurosci 1996; 16: 5415–5424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mozrzymas JW, Wojtowicz T, Piast M, et al. GABA transient sets the susceptibility of mIPSCs to modulation by benzodiazepine receptor agonists in rat hippocampal neurons. J Physiol 2007; 585: 29–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gerecke M. Chemical structure and properties of midazolam compared with other benzodiazepines. Br J Clin Pharmacol 1983; 16(Suppl. 1): 11S–16S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yuan R, Flockhart DA, Balian JD. Pharmacokinetic and pharmacodynamic consequences of metabolism-based drug interactions with alprazolam, midazolam, and triazolam. J Clin Pharmacol 1999; 39: 1109–1125. [PubMed] [Google Scholar]
- 13. Towne AR, DeLorenzo RJ. Use of intramuscular midazolam for status epilepticus. J Emerg Med 1999; 17: 323–328. [DOI] [PubMed] [Google Scholar]
- 14. Blumer JL. Clinical pharmacology of midazolam in infants and children. Clin Pharmacokinet 1998; 35: 37–47. [DOI] [PubMed] [Google Scholar]
- 15. Bottomley DM, Hanks GW. Subcutaneous midazolam infusion in palliative care. J Pain Symptom Manage 1990; 5: 259–261. [DOI] [PubMed] [Google Scholar]
- 16. Olkkola KT, Ahonen J. Midazolam and other benzodiazepines. Handb Exp Pharmacol 2008: 335–360. [DOI] [PubMed] [Google Scholar]
- 17. Heizmann P, Eckert M, Ziegler WH. Pharmacokinetics and bioavailability of midazolam in man. Br J Clin Pharmacol 1983; 16(Suppl. 1): 43S–49S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dundee JW, Halliday NJ, Harper KW, et al. Midazolam. A review of its pharmacological properties and therapeutic use. Drugs 1984; 28: 519–543. [DOI] [PubMed] [Google Scholar]
- 19. Avram MJ, Fragen RJ, Caldwell NJ. Dose-finding and pharmacokinetic study of intramuscular midazolam. J Clin Pharmacol 1987; 27: 314–317. [DOI] [PubMed] [Google Scholar]
- 20. Bell DM, Richards G, Dhillon S, et al. A comparative pharmacokinetic study of intravenous and intramuscular midazolam in patients with epilepsy. Epilepsy Res 1991; 10: 183–190. [DOI] [PubMed] [Google Scholar]
- 21. Knoester PD, Jonker DM, Van Der Hoeven RT, et al. Pharmacokinetics and pharmacodynamics of midazolam administered as a concentrated intranasal spray. A study in healthy volunteers. Br J Clin Pharmacol 2002; 53: 501–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kanto JH. Midazolam: the first water-soluble benzodiazepine. Pharmacology, pharmacokinetics and efficacy in insomnia and anesthesia. Pharmacotherapy 1985; 5: 138–155. [DOI] [PubMed] [Google Scholar]
- 23. Nordt SP, Clark RF. Midazolam: a review of therapeutic uses and toxicity. J Emerg Med 1997; 15: 357–365. [DOI] [PubMed] [Google Scholar]
- 24. Wandel C, Bocker R, Bohrer H, et al. Midazolam is metabolized by at least three different cytochrome P450 enzymes. Br J Anaesth 1994; 73: 658–661. [DOI] [PubMed] [Google Scholar]
- 25. MacKenzie M, Hall R. Pharmacogenomics and pharmacogenetics for the intensive care unit: a narrative review. Can J Anaesth 2017; 64: 45–64. [DOI] [PubMed] [Google Scholar]
- 26. Franken LG, de Winter BCM, Masman AD, et al. Population pharmacodynamic modelling of midazolam induced sedation in terminally ill adult patients. Br J Clin Pharmacol 2018; 84: 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Howard P, Twycross R, Shuster J, et al. Benzodiazepines. J Pain Symptom Manage 2014; 47: 955–964. [DOI] [PubMed] [Google Scholar]
- 28. MacGilchrist AJ, Birnie GG, Cook A, et al. Pharmacokinetics and pharmacodynamics of intravenous midazolam in patients with severe alcoholic cirrhosis. Gut 1986; 27: 190–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bastien O, Bolon M, Flamens C, et al. [Use of midazolam in postoperative sedation of patients with multiple organ failure treated with hemodiafiltration. Clinical study and pharmacokinetics]. Ann Fr Anesth Reanim 2002; 21: 692–697. [DOI] [PubMed] [Google Scholar]
- 30. Bauer TM, Ritz R, Haberthur C, et al. Prolonged sedation due to accumulation of conjugated metabolites of midazolam. Lancet 1995; 346: 145–147. [DOI] [PubMed] [Google Scholar]
- 31. Hatsiopoulou O, Cohen RI, Lang EV. Postprocedure pain management of interventional radiology patients. J Vasc Interv Radiol 2003; 14: 1373–1385. [DOI] [PubMed] [Google Scholar]
- 32. Franken LG, de Winter BC, van Esch HJ, et al. Pharmacokinetic considerations and recommendations in palliative care, with focus on morphine, midazolam and haloperidol. Expert Opin Drug Metab Toxicol 2016; 12: 669–680. [DOI] [PubMed] [Google Scholar]
- 33. Franken LG, Masman AD, de Winter BCM, et al. Hypoalbuminaemia and decreased midazolam clearance in terminally ill adult patients, an inflammatory effect. Br J Clin Pharmacol 2017; 83: 1701–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Holazo AA, Winkler MB, Patel IH. Effects of age, gender and oral contraceptives on intramuscular midazolam pharmacokinetics. J Clin Pharmacol 1988; 28: 1040–1045. [DOI] [PubMed] [Google Scholar]
- 35. Amrein R, Hetzel W. Pharmacology of Dormicum (midazolam) and Anexate (flumazenil). Acta Anaesthesiol Scand Suppl 1990; 92: 6–15. [PubMed] [Google Scholar]
- 36. Pacifici GM. Clinical pharmacology of midazolam in neonates and children: effect of disease – a review. Int J Pediatr 2014; 2014: 309342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Altamimi MI, Sammons H, Choonara I. Inter-individual variation in midazolam clearance in children. Arch Dis Child 2015; 100: 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Frechen S, Gaertner J. Author’s reply to Kotlinska-Lemieszek: ‘should midazolam drug-drug interactions be of concern to palliative care physicians?’ Drug Saf 2013; 36: 791–792. [DOI] [PubMed] [Google Scholar]
- 39. Kotlinska-Lemieszek A. Should midazolam drug–drug interactions be of concern to palliative care physicians? Drug Safety 2013; 36: 789–790. [DOI] [PubMed] [Google Scholar]
- 40. Nakajima M, Suzuki T, Sasaki T, et al. Effects of chronic administration of glucocorticoid on midazolam pharmacokinetics in humans. Ther Drug Monit 1999; 21: 507–513. [DOI] [PubMed] [Google Scholar]
- 41. Marcantonio EE, Ballard J, Gibson CR, et al. Prednisone has no effect on the pharmacokinetics of CYP3A4 metabolized drugs: midazolam and odanacatib. J Clin Pharmacol 2014; 54: 1280–1289. [DOI] [PubMed] [Google Scholar]
- 42. Backman JT, Olkkola KT, Ojala M, et al. Concentrations and effects of oral midazolam are greatly reduced in patients treated with carbamazepine or phenytoin. Epilepsia 1996; 37: 253–257. [DOI] [PubMed] [Google Scholar]
- 43. Gurley BJ, Swain A, Hubbard MA, et al. Supplementation with goldenseal (Hydrastis canadensis), but not kava kava (Piper methysticum), inhibits human CYP3A activity in vivo. Clin Pharmacol Ther 2008; 83: 61–69. [DOI] [PubMed] [Google Scholar]
- 44. Zhou S, Chan E, Pan SQ, et al. Pharmacokinetic interactions of drugs with St John’s wort. J Psychopharmacol 2004; 18: 262–276. [DOI] [PubMed] [Google Scholar]
- 45. Izzo AA. Interactions between herbs and conventional drugs: overview of the clinical data. Med Princ Pract 2012; 21: 404–428. [DOI] [PubMed] [Google Scholar]
- 46. Mikus G, Heinrich T, Bodigheimer J, et al. Semisimultaneous midazolam administration to evaluate the time course of CYP3A activation by a single oral dose of efavirenz. J Clin Pharmacol 2017; 57: 899–905. [DOI] [PubMed] [Google Scholar]
- 47. Micromedex® (electronic version). IBM Watson Health, Greenwood Village, Colorado, USA: Available at: https://www.micromedexsolutions.com/ [Google Scholar]
- 48. Ahonen J, Olkkola KT, Takala A, et al. Interaction between fluconazole and midazolam in intensive care patients. Acta Anaesthesiol Scand 1999; 43: 509–514. [DOI] [PubMed] [Google Scholar]
- 49. Olkkola KT, Ahonen J, Neuvonen PJ. The effects of the systemic antimycotics, itraconazole and fluconazole, on the pharmacokinetics and pharmacodynamics of intravenous and oral midazolam. Anesth Analg 1996; 82: 511–516. [DOI] [PubMed] [Google Scholar]
- 50. Zhang H, Sheng J, Ko JH, et al. Inhibitory effect of single and repeated doses of nilotinib on the pharmacokinetics of CYP3A substrate midazolam. J Clin Pharmacol 2015; 55: 401–408. [DOI] [PubMed] [Google Scholar]
- 51. Ramanathan S, Jin F, Sharma S, et al. Clinical pharmacokinetic and pharmacodynamic profile of idelalisib. Clin Pharmacokinet 2016; 55: 33–45. [DOI] [PubMed] [Google Scholar]
- 52. Filppula AM, Neuvonen PJ, Backman JT. In vitro assessment of time-dependent inhibitory effects on CYP2C8 and CYP3A activity by fourteen protein kinase inhibitors. Drug Metab Dispos 2014; 42: 1202–1209. [DOI] [PubMed] [Google Scholar]
- 53. Goh BC, Reddy NJ, Dandamudi UB, et al. An evaluation of the drug interaction potential of pazopanib, an oral vascular endothelial growth factor receptor tyrosine kinase inhibitor, using a modified Cooperstown 5+1 cocktail in patients with advanced solid tumors. Clin Pharmacol Ther 2010; 88: 652–659. [DOI] [PubMed] [Google Scholar]
- 54. Product information TAXOL IV injection, paclitaxel injection. Princeton, NJ: Bristol-Myers Squibb Company, 2010. [Google Scholar]
- 55. Goho C. Oral midazolam-grapefruit juice drug interaction. Pediatr Dent 2001; 23: 365–366. [PubMed] [Google Scholar]
- 56. Mangum EM, Graham KK. Lopinavir-Ritonavir: a new protease inhibitor. Pharmacotherapy 2001; 21: 1352–1363. [DOI] [PubMed] [Google Scholar]
- 57. Hughes CA, Tseng A, Cooper R. Managing drug interactions in HIV-infected adults with comorbid illness. CMAJ 2015; 187: 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Stolbach A, Paziana K, Heverling H, et al. A review of the toxicity of HIV medications II: interactions with drugs and complementary and alternative medicine products. J Med Toxicol 2015; 11: 326–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ouwerkerk-Mahadevan S, Snoeys J, Peeters M, et al. Drug-drug interactions with the NS3/4A protease inhibitor simeprevir. Clin Pharmacokinet 2016; 55: 197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zhang X, Quinney SK, Gorski JC, et al. Semiphysiologically based pharmacokinetic models for the inhibition of midazolam clearance by diltiazem and its major metabolite. Drug Metab Dispos 2009; 37: 1587–1597. [DOI] [PubMed] [Google Scholar]
- 61. Sager JE, Lutz JD, Foti RS, et al. Fluoxetine- and norfluoxetine-mediated complex drug-drug interactions: in vitro to in vivo correlation of effects on CYP2D6, CYP2C19, and CYP3A4. Clin Pharmacol Ther 2014; 95: 653–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lam YW, Alfaro CL, Ereshefsky L, et al. Pharmacokinetic and pharmacodynamic interactions of oral midazolam with ketoconazole, fluoxetine, fluvoxamine, and nefazodone. J Clin Pharmacol 2003; 43: 1274–1282. [DOI] [PubMed] [Google Scholar]
- 63. Patel P, Leeder JS, Piquette-Miller M, et al. Aprepitant and fosaprepitant drug interactions: a systematic review. Br J Clin Pharmacol 2017; 83: 2148–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Majumdar AK, Yan KX, Selverian DV, et al. Effect of aprepitant on the pharmacokinetics of intravenous midazolam. J Clin Pharmacol 2007; 47: 744–750. [DOI] [PubMed] [Google Scholar]
- 65. Stoch SA, Gargano C, Valentine J, et al. Double-blind crossover study to assess potential differences in cytochrome P450 3A4 activity in healthy subjects receiving ondansetron plus dexamethasone, with and without aprepitant. Cancer Chemother Pharmacol 2011; 67: 1313–1321. [DOI] [PubMed] [Google Scholar]
- 66. Aapro MS, Walko CM. Aprepitant: drug-drug interactions in perspective. Ann Oncol 2010; 21: 2316–2323. [DOI] [PubMed] [Google Scholar]
- 67. Natale JJ, Spinelli T, Calcagnile S, et al. Drug-drug interaction profile of components of a fixed combination of netupitant and palonosetron: review of clinical data. J Oncol Pharm Pract 2016; 22: 485–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shorr RI, Robin DW. Rational use of benzodiazepines in the elderly. Drugs Aging 1994; 4: 9–20. [DOI] [PubMed] [Google Scholar]
- 69. Navigante AH, Cerchietti LC, Castro MA, et al. Midazolam as adjunct therapy to morphine in the alleviation of severe dyspnea perception in patients with advanced cancer. J Pain Symptom Manage 2006; 31: 38–47. [DOI] [PubMed] [Google Scholar]
- 70. Navigante AH, Castro MA, Cerchietti LC. Morphine versus midazolam as upfront therapy to control dyspnea perception in cancer patients while its underlying cause is sought or treated. J Pain Symptom Manage 2010; 39: 820–830. [DOI] [PubMed] [Google Scholar]
- 71. de Mendonca MJ. Midazolam-induced hiccoughs. Br Dent J 1984; 157: 49. [DOI] [PubMed] [Google Scholar]
- 72. Mancuso CE, Tanzi MG, Gabay M. Paradoxical reactions to benzodiazepines: literature review and treatment options. Pharmacotherapy 2004; 24: 1177–1185. [DOI] [PubMed] [Google Scholar]
- 73. Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med 2017; 177: 34–42. [DOI] [PubMed] [Google Scholar]
- 74. Vorsanger GJ, Roberts JT. Midazolam-induced athetoid movements of the lower extremities during epidural anesthesia reversed by physostigmine. J Clin Anesth 1993; 5: 494–496. [DOI] [PubMed] [Google Scholar]
- 75. Malamed SF, Nikchevich D, Jr, Block J. Anterograde amnesia as a possible postoperative complication of midazolam as an agent for intravenous conscious sedation. Anesth Prog 1988; 35: 160–162. [PMC free article] [PubMed] [Google Scholar]
- 76. McKay AC, McKinney MS, Clarke RS. Effect of flumazenil on midazolam-induced amnesia. Br J Anaesth 1990; 65: 190–196. [DOI] [PubMed] [Google Scholar]
- 77. Liang P, Manelis A, Liu X, et al. Using arterial spin labeling perfusion MRI to explore how midazolam produces anterograde amnesia. Neurosci Lett 2012; 522: 113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lo B, Rubenfeld G. Palliative sedation in dying patients: ‘we turn to it when everything else hasn’t worked’. JAMA 2005; 294: 1810–1816. [DOI] [PubMed] [Google Scholar]
- 79. Calvo-Espinos C, Ruiz de Gaona E, Gonzalez C, et al. Palliative sedation for cancer patients included in a home care program: a retrospective study. Palliat Support Care 2015; 13: 619–624. [DOI] [PubMed] [Google Scholar]
- 80. Lux MR, Protus BM, Kimbrel J, et al. A survey of hospice and palliative care physicians regarding palliative sedation practices. Am J Hosp Palliat Care 2017; 34: 217–222. [DOI] [PubMed] [Google Scholar]
- 81. Fainsinger RL, Landman W, Hoskings M, et al. Sedation for uncontrolled symptoms in a South African hospice. J Pain Symptom Manage 1998; 16: 145–152. [DOI] [PubMed] [Google Scholar]
- 82. Azoulay D, Shahal-Gassner R, Yehezkel M, et al. Palliative sedation at the end of life: patterns of use in an Israeli hospice. Am J Hosp Palliat Care 2016; 33: 369–373. [DOI] [PubMed] [Google Scholar]
- 83. Mercadante S, Porzio G, Valle A, et al. Palliative sedation in patients with advanced cancer followed at home: a prospective study. J Pain Symptom Manage 2014; 47: 860–866. [DOI] [PubMed] [Google Scholar]
- 84. Korzeniewska-Eksterowicz A, Przyslo L, Fendler W, et al. Palliative sedation at home for terminally ill children with cancer. J Pain Symptom Manage 2014; 48: 968–974. [DOI] [PubMed] [Google Scholar]
- 85. Taylor DM, Yap CYL, Knott JC, et al. Midazolam-droperidol, droperidol, or olanzapine for acute agitation: a randomized clinical trial. Ann Emerg Med 2017; 69: 318–26.e1. [DOI] [PubMed] [Google Scholar]
- 86. Hardy J, Randall C, Pinkerton E, et al. A randomised, double-blind controlled trial of intranasal midazolam for the palliation of dyspnoea in patients with life-limiting disease. Support Care Cancer 2016; 24: 3069–3076. [DOI] [PubMed] [Google Scholar]
- 87. Pellock JM. Treatment considerations: traditional antiepileptic drugs. Epilepsy Behav 2002; 3: 18–23. [DOI] [PubMed] [Google Scholar]
- 88. Fernandez A, Claassen J. Refractory status epilepticus. Curr Opin Crit Care 2012; 18: 127–131. [DOI] [PubMed] [Google Scholar]
- 89. Silbergleit R, Durkalski V, Lowenstein D, et al. Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med 2012; 366: 591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Silbergleit R, Lowenstein D, Durkalski V, et al. Lessons from the RAMPART study – and which is the best route of administration of benzodiazepines in status epilepticus. Epilepsia 2013; 54(Suppl. 6): 74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Gronheit W, Popkirov S, Wehner T, et al. Practical management of epileptic seizures and status epilepticus in adult palliative care patients. Front Neurol 2018; 9: 595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ho K, Ismail H. Use of intrathecal midazolam to improve perioperative analgesia: a meta-analysis. Anaesth Intensive Care 2008; 36: 365–373. [DOI] [PubMed] [Google Scholar]
- 93. Matsuo N, Morita T. Efficacy, safety, and cost effectiveness of intravenous midazolam and flunitrazepam for primary insomnia in terminally ill patients with cancer: a retrospective multicenter audit study. J Palliat Med 2007; 10: 1054–1062. [DOI] [PubMed] [Google Scholar]
- 94. Kaneishi K, Kawabata M, Morita T. Single-dose subcutaneous benzodiazepines for insomnia in patients with advanced cancer. J Pain Symptom Manage 2015; 49: e1–2. [DOI] [PubMed] [Google Scholar]
- 95. Goncalves F, Almeida A, Pereira S. A protocol for the control of agitation in palliative care. Am J Hosp Palliat Care 2016; 33: 948–951. [DOI] [PubMed] [Google Scholar]
- 96. Prommer EE. Ketamine for pain: an update of uses in palliative care. J Palliat Med 2012; 15: 474–483. [DOI] [PubMed] [Google Scholar]
- 97. Jeon YS, Kearney AM, Baker PG. Management of hiccups in palliative care patients. BMJ Support Palliat Care 2018; 8: 1–6. [DOI] [PubMed] [Google Scholar]
- 98. Prieto LN. The use of midazolam to treat itching in a terminally ill patient with biliary obstruction. J Pain Symptom Manage 2004; 28: 531–532. [DOI] [PubMed] [Google Scholar]
- 99. Rousseau P. Palliative sedation in the management of refractory symptoms. J Support Oncol 2004; 2: 181–186. [PubMed] [Google Scholar]
- 100. Cherny NI, Radbruch L. European Association for Palliative Care (EAPC) recommended framework for the use of sedation in palliative care. Palliat Med 2009; 23: 581–593. [DOI] [PubMed] [Google Scholar]
- 101. Bodnar J. A review of agents for palliative sedation/continuous deep sedation: pharmacology and practical applications. J Pain Palliat Care Pharmacother 2017; 31: 16–37. [DOI] [PubMed] [Google Scholar]
- 102. Vissers KC, Hasselaar J, Verhagen SA. Sedation in palliative care. Curr Opin Anaesthesiol 2007; 20: 137–142. [DOI] [PubMed] [Google Scholar]
- 103. Pecking M, Montestruc F, Marquet P, et al. Absolute bioavailability of midazolam after subcutaneous administration to healthy volunteers. Br J Clin Pharmacol 2002; 54: 357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Trinka E, Brigo F, Shorvon S. Recent advances in status epilepticus. Curr Opin Neurol 2016; 29: 189–198. [DOI] [PubMed] [Google Scholar]
- 105. Shorvon S. The treatment of status epilepticus. Curr Opin Neurol 2011; 24: 165–170. [DOI] [PubMed] [Google Scholar]
- 106. Prommer E. Management of bleeding in the terminally ill patient. Hematology 2005; 10(3): 167–175. [DOI] [PubMed] [Google Scholar]
- 107. Burtin P, Daoud P, Jacqz-Aigrain E, Mussat P, Moriette G. Hypotension with midazolam and fentanyl in the newborn. The Lancet, 1991; 337(8756): 1545–1546. [DOI] [PubMed] [Google Scholar]
- 108. Whitwam JG, Al-Khudhairi D, McCloy RF. Comparison of midazolam and diazepam in doses of comparable potency during gastroscopy. Br J Anaesth 1983; 55: 773–777. [DOI] [PubMed] [Google Scholar]
- 109. Wolfe TR, Macfarlane TC. Intranasal midazolam therapy for pediatric status epilepticus. Am J Emerg Med 2006; 24: 343–346. [DOI] [PubMed] [Google Scholar]


