Abstract
South Africa (SA) has the largest HIV/AIDS burden globally. In SA, substance use is prevalent and interferes with HIV treatment adherence and viral suppression, yet is not routinely treated in HIV care. More research is needed to adapt scalable, evidence-based therapies for substance use for integration into HIV care in SA. Behavioral activation (BA), originally developed as an efficacious therapy for depression, has been feasibly delivered to treat depression in low- and middle-income countries (LMICs) and to treat substance use in high-income settings. Yet, to date, there is limited research on implementing BA for substance use in LMICs. Guided by the ADAPT-ITT framework, this study sought to adapt BA therapy for substance use in HIV care in SA. We conducted semi-structured individual interviews with patients (n=19), and HIV care providers and substance use treatment therapists (n=11) at two clinic sites in a peri-urban area of Cape Town. We enrolled patients with moderate/severe substance use (WHO-ASSIST≥4) and detectable viral load, and HIV providers and substance use treatment therapists across roles and disciplines. We assessed patient and provider/therapist views on the appropriateness of the BA therapy model and sought feedback on Xhosa-translated BA therapy components. Participants identified the central role of boredom in contributing to substance use and saw the BA therapy model as highly appropriate. Participants identified church and religious practices, sports, and yard and housework as relevant substance-free activities in this community. These findings will inform adaptations to BA therapy for substance use and HIV medication adherence in this setting.
Keywords: behavioral activation; HIV/AIDS; substance use, South Africa; global mental health
South Africa is home to the largest number of people living with HIV (PLWH) in the world (approximately 7.52 million) (STATSSA, 2018). Substance use is prevalent alongside the HIV/AIDS epidemic in South Africa, with over one-third of PLWH presenting to HIV care with unhealthy alcohol or other drug use (Kader, Seedat, Govender, Koch, & Parry, 2014; Magidson, Fatch, et al., 2019). Untreated substance use has been associated with poor adherence to antiretroviral therapy (ART) for the treatment of HIV/AIDS, which can lead to viral non-suppression and greater likelihood of HIV transmission in the context of detectable viremia (Cook et al., 2001; Kader et al., 2014; Kalichman, Simbayi, Kaufman, Cain, & Jooste, 2007; Morojele, Kekwaletswe, & Nkosi, 2014; Patterson, Semple, Zians, & Strathdee, 2005; Shisana et al., 2014). As a consequence of ART nonadherence, individuals may develop resistance to the limited ART regimens available in South Africa, requiring a switch from first- to second-line treatment, with only limited third-line regimens currently available. In turn, failing the existing ART regimens can lead to HIV disease progression, increased costs and burden on health care services, and greater likelihood of morbidity and mortality (Abaasa et al., 2008; Bangsberg et al., 2001; Marconi et al., 2008; Nachega et al., 2011).
Despite the high prevalence of substance use among PLWH in South Africa and the impact on HIV-associated morbidity and mortality, substance use treatment is not routinely integrated into HIV care in South Africa, and few psychotherapy approaches have been systematically adapted to ensure relevance to the local context. There has been research to evaluate problem solving therapy (PST) and motivational interviewing (MI) in this context to address problematic alcohol use among PLWH (Myers, Joska, et al., 2018; Myers, Lund, et al., 2018; Myers, Stein, Mtukushe, & Sorsdahl, 2012; Sorsdahl et al., 2015; Sorsdahl, Stein, Weich, Fourie, & Myers, 2012). However, prior research has identified therapist-level challenges with fidelity when delivering some existing therapy approaches (i.e., MI; Dewing et al., 2013). Further, MI and PST approaches for substance use generally do not provide targeted strategies to help individuals manage external triggers for substance use, including boredom, unstructured leisure time, and limited availability of alternative activities to substance use, which have been demonstrated to be risk factors for substance use and relapse in South Africa (Wegner, Flisher, Caldwell, Vergnani, & Smith, 2008; Wegner, Flisher, Muller, & Lombard, 2006). These therapy approaches have also been characterized by their brevity, ranging between one to four sessions, and some patients may require longer treatments to support change. As such, it is important to offer a range of therapy options that are feasible, acceptable and appropriate to address substance use in the context of HIV care in South Africa. A broad evidence base for adapted, empirically supported, and feasible therapy approaches will enable therapists and patients to select which components may be most appropriate based upon setting and specific patient needs.
A known barrier to integrating substance use treatment in HIV care in resource-constrained settings is the shortage of trained therapists to deliver mental health and substance use treatment, which must be a primary consideration when selecting a feasible therapy approach (Pasche, Kleintjes, Wilson, Stein, & Myers, 2015; Saxena, Thornicroft, Knapp, & Whiteford, 2007). To be sustainable and feasible in resource-constrained contexts, such as peri-urban communities in South Africa, a therapy may need to use a “task sharing” model. Task sharing models include training and closely supervising less specialized health care workers, such as peers, community health workers (CHWs), or lay counselors, as therapists. These individuals can be trained and supervised to deliver evidence-based therapy with fidelity to expand access to care in resource-constrained areas with therapist shortages (Magidson et al., 2017; Schaefer, 2015; WHO, 2008). Prior studies have demonstrated the acceptability and feasibility of training CHWs, nurses, and lay counselors to deliver psychotherapy (van der Water, Rossouw, Yadin, & Seedat, 2017) and other therapeutic content in sub-Saharan Africa (Chibanda et al., 2011; Mendenhall et al., 2014; Petersen, Bhana, Baillie, & Consortium, 2012); further, these studies have shown promising results for improving mental health outcomes (Singla, Kohrt, Murray, Anand, Chrpita, & Patel, 2017; Van Ginneken et al., 2013). Training for lay counselors in psychotherapy approaches as part of prior research trials typically includes a combination of teaching basic psychotherapy skills, didactic sessions on the therapy content, interactive role plays, and close supervision and monitoring (Magidson et al., 2017; Singla et al., 2017; Van Ginneken et al., 2013). Identifying appropriate approaches for delivering substance use treatment in HIV care should consider what types of therapy approaches will be appropriate, feasible, and acceptable in the local context.
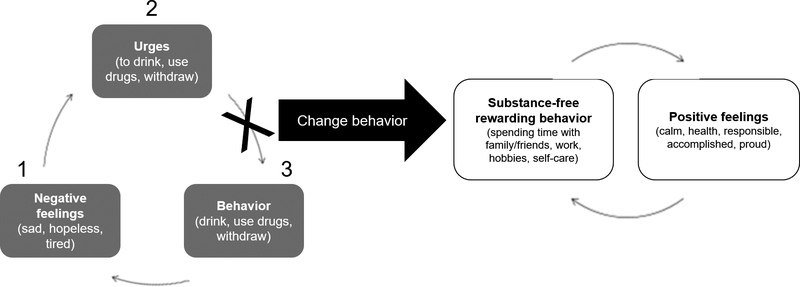
Behavioral theories of psychotherapy are built upon the foundation of reinforcement principles, such that increasing enjoyable, rewarding behaviors, and decreasing maladaptive, unwanted behaviors by shifting how an individual interacts with one’s environment can improve mood and mental health symptoms (Gros & Haren, 2011; Jacobson, Martell, & Dimidjian, 2006). The goal of behavioral activation (BA) therapy is to increase behaviors that bring mastery and pleasure; in turn, this allows for continued positive reinforcement in one’s environment (Kanter, Manos, Busch, & Rusch, 2008). Although BA was initially developed as a therapy for depression based upon reinforcement theory (Lejuez, Hopko, & Hopko, 2001), it has since accumulated empirical support as an effective, feasible, and acceptable therapy to treat substance use (Daughters et al., 2017; Magidson et al., 2011; Martinez-Vispo, Martinez, Lopez-Duran, Fernandez del Rio, & Becona, 2018; Mimiaga et al., 2012). BA promotes scheduling of substance-free, alternative reinforcing activities (Daughters, Magidson, Lejuez, & Chen, 2016). The framework for BA as a psychotherapy for substance use focuses on fostering the development of an environment that builds reinforcement for healthy, substance-free activities seen as incompatible with substance use (see also Figure 1 below). BA has been evaluated in residential substance use treatment and outpatient HIV primary care in the US for a range of substance types, including alcohol, tobacco, methamphetamine, and polysubstance use (MacPherson et al., 2010; Mimiaga et al., 2012; Reynolds, MacPherson, Tull, Baruch, & Lejuez, 2011). Given the role of boredom as a risk factor for relapse in impoverished communities in Cape Town (Myers, Carney, & Wechsberg, 2016; Reed, Emanuel, Myers, Johnson, & Wechsberg, 2013; Wegner, 2011; Wegner et al., 2006), BA may be particularly appropriate for addressing substance use in this context by providing specific skills to increase activation in one’s environment and counter boredom. BA has been found to be a feasible and acceptable therapy for people living with HIV specifically (Daughters, Magidson, Schuster, & Safren, 2010; Magidson, Seitz-Brown, Safren, & Daughters, 2014; Tull, Berghoff, Bardeen, Schoenleber, & Konkle-Parker, 2018). Further, lay counselors have been feasibly trained as BA therapists in the treatment of depression (Ekers, Richards, McMillan, Bland, & Gilbody, 2011; Magidson et al., 2015; Patel et al., 2014; Patel et al., 2017; Richards et al., 2016).
Figure 1.
Behavioral Activation model applied to substance use, as presented in therapy.
Despite the evidence to support the feasibility and acceptability of implementing BA to treat depression in low- and middle-income countries (LMICs) (Magidson et al., 2015; Patel et al., 2014; Patel et al., 2017) and the accumulating empirical support for BA as a therapy for substance use in high-income settings (Daughters et al., 2017; Magidson et al., 2011; Martinez-Vispo et al., 2018), limited work has evaluated implementing BA therapy for substance use in LMICs (Patel et al., 2014). The overall aim of this study was to adapt BA to address substance use in a resource-limited HIV care setting in South Africa. Specific aims of this study were to explore (1) patient, HIV care provider, and substance use treatment therapist perspectives on BA therapy components to assess perceived appropriateness and acceptability of the therapy approach; and (2) barriers and facilitators to implementation of BA therapy in this context.
Methods
This study was designed to evaluate the appropriateness and acceptability of BA for treating substance use in HIV care and to guide adaptation for the South African HIV care context. ADAPT-ITT was used as the framework to guide the BA therapy adaptation (Wingood & DiClemente, 2008).
ADAPT-ITT
ADAPT-ITT is an empirically supported framework for adapting psychotherapies (Wingood & DiClemente, 2008) that has been previously used in the context of HIV research in sub-Saharan Africa (Myers, Carney, Browne, & Wechsberg, 2018). ADAPT-ITT guides the researcher through a series of sequential steps to adapt a therapy. This study focused on the first three steps of the ADAPT-ITT framework (Assessment, Decision, and Administration). “Assessment” involves conducting formative qualitative research with the target population and key stakeholders to determine therapy needs, preferences for therapy delivery, and barriers and facilitators to implementation. “Decision” involves deciding which therapy components to include based upon findings from the assessment phase and relevance to the local setting (Wingood & DiClemente, 2008). The third step, “Administration”, involves a pretesting method called “theater testing,” or a demonstration of possible therapy components. In response, participants provide feedback regarding their reaction to the therapy. We utilized individual interviews and feedback due to the sensitive nature of the topics (HIV and substance use). This methodology is used to provide guidance on how the materials, language, and content of the proposed therapy should be adapted to ensure relevance for the target population and setting.
Recruitment
Patients, HIV care providers, and substance use treatment therapists were purposively sampled from HIV and substance use services. For patient recruitment, patients were referred from either a risk of treatment failure program (ROTF), available at both HIV clinic sites, or from the Matrix substance use treatment center, co-located at one of the primary care clinics. A field worker then screened these patients using an abbreviated WHO-ASSIST measure (WHO-ASSIST, 2002) to indicate severity of lifetime and past-three-month problematic substance use. The ASSIST screens for alcohol, cannabis, cocaine, opiates, amphetamines, hallucinogens, and other drugs and has been used extensively in South Africa (Gouse et al., 2016). Patients were eligible to participate if they: 1) reported at least moderate substance use and related problems on the WHO-ASSIST (score 4–26) (WHO-ASSIST, 2002); 2) were HIV positive; 3) were on antiretroviral therapy (ART); 4) had either a detectable viral load, had been re-initiated on first-line treatment due to poor adherence, or switched to second line treatment; 5) spoke English or isiXhosa; and 6) were between 18 and 65 years of age. Patients were recruited until we reached theoretical saturation.
For HIV care provider and substance use treatment therapist recruitment, the medical officer at each site identified individuals involved in HIV or substance use care at one of the medical clinic sites, including the co-located Matrix center. Identified providers and therapists were purposively sampled across disciplines and roles. Roles included but were not limited to physicians, nurses, treatment directors, adherence counselors, community health workers, and substance use treatment counselors. We recruited all available providers and therapists at the two clinics who were involved in HIV or substance use care within those disciplines.
Procedures
After describing the study to eligible participants, research staff asked participants if they would be willing to be interviewed. Staff emphasized the voluntary and confidential nature of participation. Participants provided informed consent to have their interviews digitally audio-recorded. All interviews were conducted between October 2016 and February 2017, took place in private rooms at the clinics, and lasted approximately one hour. Participants were compensated with a ZAR 150 grocery voucher (approximately 11 US dollars at the time of the interview). Recruitment sites were approved by the City of Cape Town and study procedures were reviewed and approved by the University of Maryland, College Park Institutional Review Board, the Partners Human Research Committee and the Human Research Ethics Committee at the University of Cape Town.
Patient interviews
Eligible patient participants who provided informed consent participated in a semi-structured individual interview. The interview guide was translated into isiXhosa and back-translated into English to ensure consistent translation of key concepts. Two bilingual (English and isiXhosa) research assistants, trained and experienced in conducting qualitative interviews in community treatment settings, conducted the interviews. All participants chose to be interviewed in isiXhosa. Interview recordings were translated and transcribed into English by an independent, trained bilingual translator with experience in qualitative interview transcription. Research assistants also collected demographic and other basic information from participants (prior substance use treatment history).
HIV care provider and substance use treatment therapist interviews
Interview guides varied based on whether the provider/therapist worked in substance use treatment or HIV care, which was balanced across participants interviewed. One of the trained bilingual research assistants conducted an interview with a CHW who chose to be interviewed in isiXhosa. A trained clinical psychology doctoral student conducted the remaining provider/therapist interviews in English. The interviewers collected demographic and job-related information from all participants, including role type, years of experience in the role, and years of experience overall.
Semi-structured interview guides
Interviews followed pre-set, semi-structured guides developed based on theoretically-driven domains from ADAPT-ITT (Wingood & DiClemente, 2008) and adapted from key stakeholder feedback. Questions included suggested probes to further explore participant responses. Patient and provider/therapist interviews used separate interview guides that consisted of the same primary domains. Patient and provider/therapist interview guides each had two sections. First, we assessed the appropriateness of the proposed BA therapy model. Appropriateness, defined as the perceived fit, relevance or compatibility of an approach (Proctor et al., 2011) was assessed by gauging the relevance of the BA therapy model to primary environmental and behavioral factors contributing to substance use (following step one of ADAPT-ITT) (Wingood & DiClemente, 2008), assessing whether participants thought the BA therapy components met their personal needs, taking into account the high levels of unemployment and poverty in this community, and identifying other barriers and facilitators to participation. Providers/therapists responded about their patients’ reported reasons for using, how BA therapy components might map onto those reasons, and perceived barriers and facilitators to participation.
In the second part of the interview, following the second and third steps of ADAPT-ITT, we sought initial feedback on the acceptability of BA therapy components (translated into isiXhosa for patients) to guide future adaptation. Acceptability, defined as the perceived satisfaction with various aspects of the therapy such as content and delivery (Proctor et al., 2011), was assessed as participants’ interest in participating in the approach (or perceptions of their patients’ interest) and querying for additional substance-free activities to include in BA therapy adaptation to increase acceptability, particularly in this resource-limited setting.
In line with the “Administration” step of ADAPT-ITT (Wingood & DiClemente, 2008), the participants were introduced to the BA therapy model applied to substance use (see Figure 1). We explained that the rationale for this therapy is to promote scheduling of substance-free alternative reinforcing activities, or activities that are incompatible and not associated with substance use.
After a brief introduction to the BA therapy model as applied to substance use, participants were asked to identify substance-free rewarding activities in their environment and share how engaging in those activities was (or was not) associated with substance use. Specifically, participants were first asked to identify at least three activities that brought pleasure and/or mastery that they did not associate with substance use (either for themselves or providers/therapists reported based on their clinical experience). All participants were then introduced to an adapted Pleasant Events Schedule (PES) (MacPhillamy & Lewinsohn, 1982; see Appendix A). The PES is a behavioral self-report inventory of potentially reinforcing events that is widely used in behavioral depression interventions and dialectical behavior therapy (DBT; Linehan, 2015). The PES had been translated into isiXhosa and adapted for the Khayelitsha HIV care setting for a previous depression treatment study (Andersen et al., 2018). In the prior adaptation, 32 items were removed to eliminate culturally inappropriate items (e.g., snowshoeing) and to increase feasibility of administration. Eight culture-specific items were incorporated (e.g., having your hair braided, going to church/mosque, playing soccer/cricket, going to Mzoli’s and Mapindi’s—local “braai” or barbeque places nearby this community). Participants were asked to identify which activities in the PES were feasible to do, incompatible with substance use, and acceptable. This feedback was gathered to inform the use of the PES in the BA therapy applied to substance use in this community.
Data Analysis
Interviews were translated and transcribed immediately to facilitate iterative data analysis to determine theoretical saturation. Transcripts were analyzed using thematic analysis and the dataset was managed in NVivo Version 11. Two trained, independent coders open-coded the first five interviews to develop a codebook, which included higher order codes, sub-codes, and definitions arrived at through consensus. If new concepts emerged which did not fit into the coding scheme, the codebook was modified and all prior interviews were re-coded using the modified codebook. Coders met weekly and resolved discrepancies by discussion. A third person arbiter was not needed. The coders obtained a Kappa score >0.80 after the final inter-coder reliability checks.
Participants
Patient participants (n=19) were 58% female, had a median age of 41 years (IQR=33–46), and all identified as Black African. Fifteen patients were recruited from HIV care (79%), and four (21%) from the co-located Matrix program. Alcohol (n=18) and cannabis (n=8) were the most commonly reported substances. None of the participants recruited from HIV care had received prior substance use treatment.
HIV care providers and substance use treatment therapists (n=11) were 82% female, had a median age of 44 years (IQR=36–52). Seventy-three percent identified as Black African and 27% identified as white. HIV care providers held a variety of treatment roles in HIV care, including HIV adherence counsellor (n=1), HIV and TB nurse (n=3), physician/clinical medical officer (n=2), and CHW (n=2). Therapists from the co-located substance use treatment facility included a treatment director (n=1) and substance use treatment counselors (n=2). Providers/therapists reported a median of four years of experience in their current role, and a median of 11 years of career experience overall.
Results
Appropriateness of BA Therapy for Substance Use among PLWH in this Context
Boredom.
Boredom was found to play an important role in contributing to substance use according to both patient and provider/therapist perspectives. Without activities to occupy their time, patients reported turning to using substances. One patient commented: “One thinks to himself, I am just sitting here, I have nothing to do to keep busy—no exercising, jogging, or playing soccer. I may as well drink. Another tells himself, ‘I should just smoke all the time.’ Most people I live with are in that situation” [HIV Clinic Patient (P1)].
Other patients also reflected boredom as contributing to substance use. An HIV Clinic Patient (P2) commented, “You know, when a person is not working, you find that they are bored because they are not busy, there’s nothing that they are busy with. Then that person will end up using substances.” Another patient echoed this sentiment, elaborating on the interplay of boredom with the environmental context: “Everyone gets bored when he’s sitting without anything to do—he’s always around the township. So, he just takes any opportunity that comes his way” [HIV Clinic Patient (P3)].
In addition to patients, providers/therapists also perceived boredom as a main contributing factor to substance use in their patients and as a risk factor for future relapse. This perception was consistent across HIV care providers and substance use treatment therapists at various levels. For instance, one substance use treatment therapist described that:
“One of the biggest challenges for a lot of people is that there isn’t any activities for them to get into…too much boredom isn’t a good thing because it dissolves in their heads” [Matrix Therapist (H1)].
Similarly, when a CHW was asked about factors in the home environment that she observed as contributing to substance use, the CHW responded “One lacks activities at home, do you understand?” [H2] and described that she had observed how boredom contributes to substance use during home visits to patients.
Appropriateness of BA therapy model.
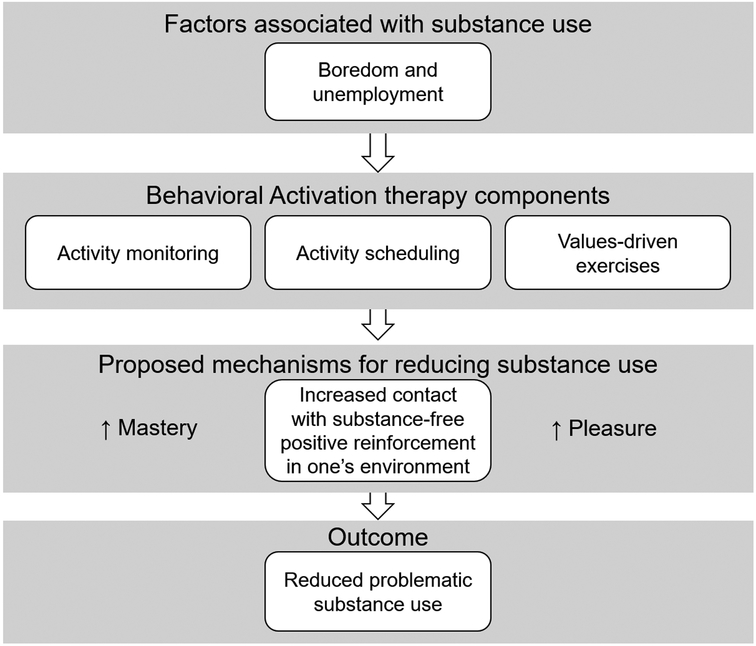
Figure 2 illustrates how we conceptualize the components of BA addressing boredom, which was a primary contributing factor to substance use in this population. Specifically, the core BA therapy components of activity monitoring, and values-driven activity scheduling map onto boredom as a key risk factor for substance use. The primary aim of these BA therapy components are to increase contact with positive reinforcement in one’s environment. BA is intended to increase feelings of pleasure and mastery that are not associated with substance use. By increasing these alternative forms of substance-free positive reinforcement in one’s environment, BA may be associated with reductions in substance use.
Figure 2.
Conceptual model of proposed BA therapy components applied to factors associated with substance use in this population.
Both patients and providers/therapists described the appropriateness of reducing boredom as a way to reduce risk of relapse or ongoing use. Specifically, participants explained that activities can clear the mind of triggering thoughts and give individuals something other than substance use to fill their time. One patient remarked,
“Because the busier you are, you don’t think of anything because of course, you are busy. Your mind’s schedule…is full.” [Matrix Patient (P6)]
Similarly, providers/therapists shared that staying mentally and physically active would keep their patients from negative thought patterns and behaviors. H1 explained,
“So one of the coping techniques for a lot of guys…is to keep busy, keep their minds occupied, because if there is nothing to do, then that becomes a very difficult thing.”
In response to the BA therapy components, BA was seen by patients and providers/therapists as acceptable and fitting with the local culture. Specifically, providers/therapists reflected that the therapy approach would be an acceptable way of helping patients re-engage in rewarding activities and reduce or stop using substances, and participants demonstrated interest in participating in BA. For instance, one patient in HIV care (P1) shared,
“I can do it even if you say let us start it tomorrow.”
Identifying Substance-Free Rewarding Activities
Participants identified a range of substance-free rewarding activities to guide future adaptation of BA for this setting. Patients most commonly shared activities relating to church and other religious practices (reported by n=13), sports (n=11), and yard or housework (n=11). Specific types of activities within these broad categories are elaborated upon below.
Religious behaviors seen as incompatible with substance use.
Involvement in religious practices emerged as a predominant activity that was seen to be rewarding and incompatible with substance use. Discussing church attendance, participants explained the differentiation between religious activity and substance use. Matrix Patient, P8 said, “Ok. It’s going to church. Because when I’m in church I don’t think of smoking—nor think of smoking before going to church.” HIV Clinic Patient, P9 reflected this sentiment: “If I go to church, I forget about alcohol.”
Providers/therapists similarly noted a preference among patients to go to church and read the Bible. Therapist 8 (from Matrix) explained, “Reading the Bible…I mean, some of our clients they do that like on their schedule as a way of dealing with boredom.”
Sports.
Participants also mentioned sports and exercise as substance-free, rewarding activities. HIV clinic patient P5 mentioned enjoying going to the gym and playing soccer. He later elaborated, “they can help me, especially if I am going to play myself.” While this individual did not believe that watching others play sports could help keep the mind from substance use, they believed that playing sports themselves could help.
Providers/therapists also observed that individuals recovering from substance use could turn to sports that they enjoyed as kids to keep away from alcohol and drugs. Matrix Therapist, H3 made this point: “For instance, there are guys who were into sports before they were addicted, and then now that they are recovered, they have started going back to sports, doing sports, so I think that could help.”
Yard or housework.
Other patients described how other housework-related activities, such as cooking, bathing children, or gardening could reduce boredom, occupy the mind, and reduce urges to use substances. HIV Clinic Patient, P10 commented,
“I really like gardening. Because even at home, it’s something that I do with the hands …. The whole day, if I’m busy with something, I don’t pay attention to that thing of leaving and going over there—I get rid of the boredom there.”
Responses largely reflected how participation in activities keeps individuals from boredom, and subsequently, reduces one’s risk for use or relapse.
Barriers and Facilitators to BA
Regarding BA, some patients noted that physical and health limitations preventing them from participating in some substance-free rewarding activities (i.e., sports). Providers/therapists also discussed barriers limiting participation in activities on the PES, including the logistics and costs associated with engaging patients in activities in the community. Without adequate resources, certain activities from the PES, for instance going to the movies, may not be feasible. Some participants provided potential adaptations or suggestions to address the barriers mentioned. HIV Provider H4, for example, recommended incorporating a ‘community hero’ into the therapy to encourage cultural adaptation, while Matrix Therapist H3 suggested an incentive system, for instance including contingency management type approaches alongside BA. While participants generally felt BA was appropriate and applicable to the local context, they noted general barriers to participation in psychological therapies, including transportation costs, ambivalence around substance use-related behavior change, and the role of both HIV and substance use stigma in reducing motivation to seek care. Participants also described the need to tailor the intervention adaptation for patients with low literacy levels and providers with limited experience delivering psychological therapies.
Discussion
Using ADAPT-ITT as a methodological framework, this study obtained feedback to inform adaptation of BA to address substance use in HIV care in South Africa and explored participants’ perspectives about the appropriateness and acceptability of BA as a therapy to treat substance use in this context. Findings highlighted the important role of boredom in contributing to the initiation of substance use or return to substance use after a period of abstinence, the perceived appropriateness of the BA therapy model, and specific recommendations for tailoring a BA approach for this context. Although resource-limited settings, such as Khayelitsha, the peri-urban community where this study was conducted, may have limited opportunities for employment or activity selection compared to high income settings where the majority of work developing and evaluating BA approaches has been conducted, findings suggested the acceptability of BA in this context.
The conceptual model for BA mapped onto boredom, a primary reason that people reported substance use in this community. The theoretical model underlying BA was seen as appropriate in this context, specifically the emphasis on increasing value-driven activity scheduling as a means to increase response-contingent positive reinforcement in one’s environment. According to the BA therapy approach, as an individual creates more daily structure and routine in their lives, they increase the likelihood that they will come into contact with positive reinforcement in their environment. In turn, alternative, substance-free, sources of positive reinforcement may alleviate boredom, which was seen as a main contributing factor to substance use in this population and is consistent with other work in South Africa (Myers et al., 2016; Wegner, 2011; Wegner et al., 2008; Wegner et al., 2006).
Although boredom is a subjective and personal experience, there are also structural and contextual factors that influence people’s experience of boredom. Many South African townships, such as the one where our data were collected, are characterized by high levels of unemployment, poor quality of education, and limited and under-resourced amenities such as sports venues and entertainment opportunities, including cinemas and theatres. Opportunities to occupy free time usually involve visiting shebeens, which are illegal drinking establishments (Charman, Petersen, Piper, Liedeman, & Legg, 2017; Rogerson, 2017), watching television if accessible, and church-going. Residing in such resource-constrained environments may result in a lack of personal agency for many township dwellers. The experience of boredom therefore may be a function of economic deprivation in townships which in turn has its roots in apartheid spatial planning and social engineering. Further, there are pervasive social influences in this community that, in addition to boredom, also contribute to substance use. These social influences include social norms that perpetuate heavy alcohol use and a high prevalence of substance use in most of our participants’ social networks. Although this study aimed to adapt BA as an individual therapy, our team is also exploring in future work how to tailor couples and family therapy for this context to address these social influences on substance use.
Results from this formative research will guide the adaptation of the BA therapy for implementation in this context. When adapting behavioral therapies, it is important to consider these circumstantial, contextual, and structural factors that may be barriers to implementing BA in this context, as well as other resource-limited settings. An ongoing challenge in this work is addressing the lack of purpose felt in these communities, while also aiming to identify activities that are engaging and meaningful yet feasible. BA has been found to be a feasible and acceptable therapy for treating depression in other resource-limited contexts (Magidson et al., 2011; Patel et al., 2014; Patel et al., 2017), and among people living with HIV specifically (Magidson et al., 2014). Similar to its implementation in other resource-limited settings, there are low cost activities that individuals can engage in that are seen as protective for reducing substance use risk. Participants were able to identify activities that they viewed as accessible, important and/or enjoyable, and incompatible with substance use. Specifically, we will use participant feedback on specific value-driven, substance-free rewarding activities to tailor the BA therapy for this patient population. Consistent with other research in South Africa demonstrating the role of religious activity as a protective factor for substance use (Francis et al., 2019), the most commonly reported activities included religious activities (e.g., church attendance and bible study), as well as sports (e.g., soccer), and yard and housework. Patients reported engaging in several of these activities prior to using substances more heavily or prior to receiving their HIV diagnosis. Our future research will evaluate the implementation and effectiveness of BA therapy in this setting and will tailor the focus of the BA activity scheduling based on this feedback.
Further, our approach of generating meaningful activities accompanied by an adapted PES, and using the ADAPT-ITT framework as a guide, may be a helpful model for other psychotherapy researchers to adapt BA therapy for other resource-limited settings globally where the burden of HIV and mental health is high. In addition to using the PES, it may be useful to supplement this list to include additional free activities which would allow individuals to get involved in their community and surrounding neighborhoods. Particularly for individuals who struggle to identify rewarding activities or may need additional support to attend these activities, it may be useful, when shaping future psychotherapy efforts using BA, to develop resources to inform individuals about low cost activities available in their community and how to access these.
Our preliminary work in this program of research has also demonstrated that participants have a preference for working with a lay counselor as their therapist, specifically someone from their community with similar lived experiences (Magidson, Joska, et al., 2019). Participants have described stigmatizing experiences with their HIV physicians and nurses; some felt “scolded” for using substances or missing HIV medication, and thus described a preference for someone they could relate to as their psychotherapist—specifically someone who had lived experience with HIV and/or substance use, and who would be nonjudgmental towards their behaviors (Magidson, Joska, et al., 2019). In response to this feedback, one primary adaptation incorporated into future implementation efforts from this work was selecting who would be the therapist for implementation. In response to this formative feedback, we prioritized identifying a therapist with lived experience with HIV and substance use and who displayed non-judgmental attitudes towards substance use and HIV. Identifying a therapist with lived experience can also help foster empathy, which is identified as a partial mediator of therapeutic alliance (Leonard, Campbell, & Gonzalez, 2018). Furthermore, in therapy focused on problematic substance use, empathy is a significant predictor of treatment outcome, with an absence of empathy associated with poor outcomes including higher drop out, higher rates of relapse, weaker therapeutic alliance, and worse patient progress (Miller & Moyers, 2015; Moyers & Miller, 2013).
Finally, another adaptation made for implementation of BA following this formative feedback to tailor the intervention adaptation for patients with low literacy levels and providers with limited experience delivering psychological therapies was the use of a flipchart in session. In this flipchart, the therapist sees the main therapy content on one side—with prompts, scripts, and reminders to guide fidelity—and participants see largely visual depictions of the therapy content. Further, the format of the flipchart is also intended to enhance therapeutic alliance, as it allows for the therapist to maintain eye contact while also following the structured guide for content delivery. This adaptation was made based on formative feedback for two reasons: 1) to promote fidelity to the psychotherapy for therapists with limited background in psychotherapy delivery, as it was seen to be an easy to use therapy manual in session; and 2) to support patent preference for visual depictions of therapy material as opposed to written given the low literacy rates in this population. As such, this format allows for greater ease of psychotherapy delivery for less experienced therapists and accessible therapy content for low literacy populations.
Findings must be interpreted in the context of the study limitations. First, this study aimed to elicit initial feedback on the appropriateness of the BA therapy model and input on specific activities in this community to guide future adaptation. This study did not pilot the adapted intervention, thus we cannot yet discuss the feasibility of lay counselor delivery, describe the training or supervision, or evaluate the effectiveness of this approach; the next phase of this research will explore the implementation and effectiveness to address these important questions, including whether lay counselor therapists can feasibly deliver the adapted BA therapy. Lay counselor therapists may not have prior therapy experience and are not licensed professionals, which may bring challenges, particularly without appropriate training, monitoring, and/or supervision. However, previous research has shown that lay counselors can feasibly and acceptably serve as therapists with appropriate training, fidelity monitoring, and clinical supervision (Chibanda et al., 2011; Mendenhall et al., 2014; Petersen et al., 2012; van der Water et al., 2017), and that their role may even act as a strength due to their close ties with the community. Second, we followed the ADAPT-ITT model for treatment adaptation (Wingood & DiClemente, 2008), which has been used extensively in prior HIV research, and includes theater testing to gauge reactions to and input on therapy components. However, there is a possibility that this method may prime patients with the model and therapy components before asking about appropriateness and thus limit perspectives on whether BA was an appropriate therapy approach. Additionally, we recruited participants from two clinics with only a few providers/therapists in each role, and as such, findings may not be generalizable to other clinic settings or types of professionals. Patient recruitment was clinic-based in both HIV care and substance use treatment; thus, responses may not reflect views of patients not currently engaged in HIV care, or substance use treatment, such as those of people with more severe active substance use and/or lower motivation to engage in care compared to the participants in this study.
Future Directions
This formative work will guide a subsequent hybrid Type 1 effectiveness-implementation trial (Curran, Bauer, Mittman, Pyne, & Stetler, 2012) to evaluate the effectiveness and implementation of an adapted, task-shared BA therapy to treat substance use in HIV care. In this subsequent trial, BA is being integrated with other therapy approaches that have been previously adapted and piloted in this setting, and found to be acceptable and feasible for lay counselor delivery, including problem solving and motivational interviewing (Myers et al., 2019). If it proves feasible to deliver and effective for reducing substance use in subsequent research, BA may also be an important approach for addressing substance use in this context.
As this study is only a starting point in a specific community in South Africa, we hope this work contributes to other psychotherapy research to expand the adaptation and dissemination of BA for substance use and HIV in other resource-limited contexts where HIV and substance use are prevalent, and where there is a need to identify scalable, appropriate therapy approaches for underserved communities with shortages of trained therapists to meet behavioral health needs. For instance, our team is actively working to evaluate the application of this therapy model to address the unmet behavioral health needs in the opioid crisis, with ongoing work in Baltimore to train peers with lived substance use experience in BA (Magidson, Jack, Regenauer, & Myers, In press). We hope this work guides other psychotherapists and psychotherapy researchers to extend the research of low-cost, accessible therapies to improve the lives of underserved individuals with substance use and HIV globally.
Clinical Impact Statement.
Question:
This study aimed to assess the appropriateness and acceptability of the behavioral activation (BA) therapy model applied to substance use in HIV care in South Africa to guide future adaptation of this therapy model.
Findings:
The BA therapy model was seen as highly appropriate given the role of boredom in contributing to substance use in this community, and substance-free, accessible activities were identified, including church and religious practices, sports, yard and housework.
Meaning:
The BA therapy model was seen as appropriate and acceptable, and the findings will guide adapting this therapy model in future work.
Next Steps:
This work can contribute to psychotherapy research to adapt BA therapy for substance use and HIV for other underserved communities with shortages of trained therapists to meet behavioral health needs.
Appendix A: Adapted Pleasant Events Schedule*
Going on Facebook and chatting to friends
Joining a sewing club
Going to church/mosque
Watching a soccer match live
Visiting family
Playing soccer/cricket with friends
Going to the movies
Having your hair braided
Joining a support group
Speaking to a friend on the phone
Relaxing in a park or backyard
Singing
Going for a walk with a friend or partner
Playing a game with a child or friend
Getting involved in your community
Getting a pet
Telling jokes and funny stories
Bird watching
Going to the beach
Going to a gospel/music show
Having a cup of tea
Going on a date
Going to a club
Going to Mzoli’s
Joining a stokvel
Relaxing
Jogging, walking, running
Listening to gospel
Recalling happy memories
Reading magazines
Laughing
Playing an instrument
Meeting new people
Eating healthy foods
Fixing things around the house
Going to a friend’s house
Taking care of my plants
Starting a small garden
Swimming
Drawing or painting
Exercising
Praying
Going to a party
Having family get-togethers
Having safe sex
Joining a choir
Doing something spontaneous
Doing embroidery, crocheting, or knitting
Inviting friends over for a braai
Flirting/kissing
Making a gift for someone
Having your nails done
Writing
Being with/playing with children
Writing in a journal
Writing and sending letters
Getting a new haircut
Going on a picnic
Sky diving
Reading a book for pleasure
Seeing and/or showing photos
Dressing up and looking nice
Joining a burial society
Going to museums
Reading the bible
Saying “I love you” to someone
Thinking about my good qualities
Dancing
Going to a cultural event
Footnotes
Andersen et al., 2018; English version presented here; list translated into isiXhosa for the study
References
- Abaasa AM, Todd J, Ekoru K, Kalyango JN, Levin J, Odeke E, & Karamagi CA (2008). Good adherence to HAART and improved survival in a community HIV/AIDS treatment and care programme: The experience of The AIDS Support Organization (TASO), Kampala, Uganda. BMC Health Services Research, 8(1), 241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen L, Magidson JF, O’Cleirigh C, Remmert JE, Kagee A, Leaver M, … Joska JA (2018). A pilot study of a nurse-delivered cognitive behavioral therapy intervention (Ziphamandla) for adherence and depression in HIV in South Africa. Journal of Health Psychology, 23(6), 776–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangsberg DR, Perry S, Charlebois ED, Clark RA, Robertson M, Zolopa AR, & Moss A (2001). Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS, 15(9), 1181–1183. [DOI] [PubMed] [Google Scholar]
- Charman AJ, Petersen LM, Piper LE, Liedeman R, & Legg T (2017). Small area census approach to measure the township informal economy in South Africa. Journal of Mixed Methods Research, 11(1), 36–58. [Google Scholar]
- Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, & Abas MA (2011). Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health, 11(1). doi: 10.1186/1471-2458-11-828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook R, Sereika S, Hunt S, Woodward W, Erlen J, & Conigliaro J (2001). Problem drinking and medication adherence among persons with HIV infection. Journal of General Internal Medicine, 16(2), 83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, & Stetler C (2012). Effectiveness-implementation Hybrid Designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50(3), 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Anand D, Seitz-Brown CJ, Chen Y, & Baker S (2017). The effect of a behavioral activation treatment for substance use on post-treatment abstinence: a randomized controlled trial. Addiction, 113(3), 535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Lejuez CW, & Chen Y (2016). LETS ACT: a behavioral activation treatment for substance use and depression. Advances in Dual Diagnosis, 9(2), 74–84. [Google Scholar]
- Daughters SB, Magidson JF, Schuster RM, & Safren SA (2010). ACT HEALTHY: A combined cognitive-behavioral depression and medication adherence treatment for HIV-infected substance users. Cognitive and Behavioral Practice. doi: 10.1016/j.cbpra.2009.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewing S, Matthews C, Cloete A, Schaay N, Shah M, Simbayi L, & Louw J (2013). From research to practice: lay adherence counsellors’ fidelity to an evidence-based intervention for promoting adherence to antiretroviral treatment in the Western cape, South Africa. AIDS and Behavior, 17(9), 2935–2945. [DOI] [PubMed] [Google Scholar]
- Ekers D, Richards D, McMillan D, Bland JM, & Gilbody S (2011). Behavioural activation delivered by the non-specialist: phase II randomised controlled trial. British Journal of Psychiatry, 198(1), 66–72. [DOI] [PubMed] [Google Scholar]
- Francis JM, Myers B, Nkosi S, Petersen Williams P, Carney T, Lombard C, … Morojele N (2019). The prevalence of religiosity and association between religiosity and alcohol use, other drug use, and risky sexual behaviours among grade 8–10 learners in Western Cape, South Africa. PLoS One, 14(2), e0211322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouse H, Magidson JF, Burnhams W, Remmert JE, Myers B, Joska JA, & Carrico AW (2016). Implementation of cognitive-behavioral substance abuse treatment in sub-Saharan Africa: Treatment engagement and abstinence at treatment exit. PLoS One, 11(1), e0147900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros DF, & Haren WB (2011). Open trial of brief behavioral activation psychotherapy for depression in an integrated veterans affairs primary care setting. The Primary Care Companion for CNS Disorders, 13(4). doi: 10.4088/PCC.11m01136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR, & Dimidjian S (2006). Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice, 8(3), 255–270. doi: 10.1093/clipsy.8.3.255 [DOI] [Google Scholar]
- Kader R, Seedat S, Govender R, Koch J, & Parry C (2014). Hazardous and harmful use of alcohol and/or other drugs and health status among South African patients attending HIV clinics. AIDS Behavior, 18(3), 525–534. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, & Jooste S (2007). Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: Systematic review of empirical findings. Prevention Science, 8(2), 141–151. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Manos RC, Busch AM, & Rusch LC (2008). Making behavioral activation more behavioral. Behavior Modification, 32(6), 780–803. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, & Hopko SD (2001). A Brief Behavioral Activation Treatment for Depression. Behavior Modification, 25(2), 255–286. [DOI] [PubMed] [Google Scholar]
- Leonard HD, Campbell K, & Gonzalez VM (2018). The relationships among clinician self-report of empathy, mindfulness, and therapeutic alliance. Mindfulness, 9(6), 1837–1844. [Google Scholar]
- Linehan MM (2015). DBT Skills Training Manual (2 ed.). New York, NY: The Guildford Press. [Google Scholar]
- MacPherson L, Tull MT, Matusiewicz AK, Rodman S, Strong DR, Kahler CW, … Lejuez CW (2010). Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology, 78(1), 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPhillamy DJ, & Lewinsohn PM (1982). The pleasant events schedule: Studies on reliability, validity, and scale intercorrelation. Journal of Consulting and Clinical Psychology, 50(3), 363. [Google Scholar]
- Magidson JF, Fatch R, Orrell C, Amanyire G, Haberer JE, & Hahn JA (2019). Biomarker-measured unhealthy alcohol use in relation to CD4 count among individuals starting ART in sub-Saharan Africa. AIDS and Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Gorka SM, MacPherson L, Hopko DR, Blanco C, Lejuez CW, & Daughters SB (2011). Examining the effect of the Life Enhancement Treatment for Substance use (LETS ACT) on residential substance abuse treatment retention. Addictive Behaviors, 36, 615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Gouse H, Psaros C, Remmert JE, O’Cleirigh C, & Safren SA (2017). Task shifting and delivery of behavioral medicine interventions in resource-poor global settings: HIV/AIDS treatment in sub-Saharan Africa In Vranceanu AM, Greer JA, & Safren SA (Eds.), The Massachusetts General Hospital Handbook of Behavioral Medicine: A clinician’s guide to evidence-based psychosocial interventions for individuals with medical illness (pp. 297–320). New York, NY: Human Press. [Google Scholar]
- Magidson JF, Jack HE, Regenauer KS, & Myers B (In press). Applying lessons from task sharing in global mental health to the opioid crisis: A response to “Integrating addiction medicine into rural primary care: Strategies and initial outcomes”. Journal of Consulting and Clinical Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Joska JA, Regenauer KS, Satinsky E, Andersen L, Seitz-Brown CJ, … Myers B (2019). “Someone who is in this thing that I am suffering from”: The role of peers and other facilitators for task sharing substance use treatment in South African HIV care. International Journal of Drug Policy, 70, 61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Lejuez CW, Kamal T, Blevins EJ, Murray LK, Bass JK, … Pagoto S (2015). Adaptation of community health worker-delivered behavioral activation for torture survivors in Kurdistan, Iraq. Global Mental Health, 2(e24). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Seitz-Brown CJ, Safren SA, & Daughters SB (2014). Implementing behavioral activation and life-steps for depression and HIV medication adherence in a community health center. Cognitive and Behavioral Practice, 21, 386–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marconi VC, Sunpath H, Lu Z, Gordon M, Koranteng-Apeagyei K, Hampton J, … Team SARCS (2008). Prevalence of HIV-1 drug resistance after failure of a first highly active antiretroviral therapy regimen in KwaZulu Natal, South Africa. Clinical Infectious Diseases, 46(10), 1589–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Vispo C, Martinez U, Lopez-Duran A, Fernandez del Rio E, & Becona E (2018). Effects of behavioural activation on substance use and depression: A systematic review. Substance Abuse Treatment, Prevention, and Policy, 13(36). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E, De Silva M, Hanlon C, Petersen I, Shidhaye R, Jordans M, … Lund C (2014). Acceptability and feasibility of using non-specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Social Science & Medicine, 118, 33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Moyers TB (2015). The forest and the trees: Relational and specific factors in addiction treatment. Addiction, 110(3), 401–413. doi: 10.1111/add.12693 [DOI] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Pantalone DW, O’Cleirigh C, Mayer KH, & Safren SA (2012). A pilot trial of integrated behavioral activation and sexual risk reduction counseling for HIV-uninfected men who have sex with men abusing crystal methamphetamine. AIDS Patient Care and STDs, 26(11), 681–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morojele NK, Kekwaletswe CT, & Nkosi S (2014). Associations between alcohol use, other psycosocial factors, structural factors and antiretroviral therapy (ART) adherence among South African ART recipients. AIDS and Behavior, 18(3), 519–524. [DOI] [PubMed] [Google Scholar]
- Moyers TB, & Miller WR (2013). Is low therapist empathy toxic? Psychology of Addictive Behaviors, 27(3), 878–884. doi: 10.1037/a0030274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Carney T, Browne F, & Wechsberg WM (2018). Development of a substance use and sexual risk reduction intervention for young South African women. Patient Preference and Adherence, 12, 1997–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Carney T, & Wechsberg WM (2016). “Not on the agenda”: A qualitative study of influences on health services use among poor young women who use drugs in Cape Town, South Africa. International Journal of Drug Policy, 30, 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Joska JA, Lund C, Levitt NS, Butler CC, Naledi T, … Sorsdahl K (2018). Patient preferences for the integration of mental health counseling and chronic disease care in South Africa. Patient Preference and Adherence, 12, 1797–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Lund C, Lombard C, Joska JA, Levitt NS, Butler CC, … Sorsdahl K (2018). Comparing dedicated and designated models of integrating mental health into chronic disease care: study protocol for a cluster randomized controlled trial. Trials, 19(1), 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Petersen Williams P, van der Westhuizen C, Lund C, Lombard C, Joska JA, & Stein DJ (2019). Community health worker-delivered counselling for common mental disorders among chronic disease patients in South Africa: A feasibility study. BMJ Open, 9(1), e024277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Stein DJ, Mtukushe B, & Sorsdahl K (2012). Feasibility and acceptability of screening and brief interventions to address alcohol and other drug use among patients presenting for emergency services in Cape Town, South Africa. Advances in Preventive Medicine, 2012. doi: 10.1155/2012/569153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nachega JB, Marconi VC, van Zyl G, Gardner EM, Preiser W, Hong SY, … Gross R (2011). HIV treatment adherence, drug resistance, virologic failure: Evolving concepts. Infectious Disorders - Drug Targets, 11(2), 167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasche S, Kleintjes S, Wilson D, Stein DJ, & Myers B (2015). Improving addiction care in South Africa: Development and challenges to implementing training in addictions care at the University of Cape Town. International Journal of Mental Health and Addiction, 13(3), 322–332. [Google Scholar]
- Patel V, Weobong B, Nadkarni A, Weiss HA, Anand A, Naik S, … Kirkwood BR (2014). The effectiveness and cost-effectiveness of lay counsellor-delivered psychological treatments for harmful and dependent drinking and moderate to severe depression in primary care in India: PREMIUM study protocol for randomized controlled trials. Trials, 15(101). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Weobong B, Weiss HA, Anand A, Bhat B, Katti B, … Fairburn CG (2017). The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet, 389, 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson T, Semple S, Zians J, & Strathdee S (2005). Methamphetamine-using HIV-positive men who have sex with men: Correlatesof polydrug use. Journal of Urban Health, 82(1 Suppl 1), i120–i126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen I, Bhana A, Baillie K, & Consortium MRP (2012). The feasibility of adapted group-based interpersonal therapy (IPT) for the treatment of depression by community health workers within the context of task shifting in South Africa. Community Mental Health Journal, 48(3), 336–341. [DOI] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, … Hensley M (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38(2), 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed E, Emanuel AN, Myers B, Johnson K, & Wechsberg WM (2013). The relevance of social contexts and social action in reducing substance use and victimization among women participating in an HIV prevention intervention in Cape Town, South Africa. Substance Abuse and Rehabilitation, 4, 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds EK, MacPherson L, Tull MT, Baruch DE, & Lejuez CW (2011). Integration of the brief behavioral activation treatment for depression (BATD) into a college orientation program: Depression and alcohol outcomes. Journal of Counseling Psychology, 58(4), 555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, … Finning K (2016). Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): A randomised, controlled, non-inferiority trial. The Lancet, 388(10047), 871–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogerson C (2017). Consumerism, the state, and the informal sector: Shebeens in South Africa’s Black townships In Economic growth and urbanization in developing areas (pp. 287–303): Routledge. [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, & Whiteford H (2007). Resources for mental health: scarcity, inequity, and inefficiency. Lancet, 370(9590), 878–889. doi: 10.1016/S0140-6736(07)61239-2 [DOI] [PubMed] [Google Scholar]
- Schaefer L (2015). Task sharing implant insertion by community health workers: Not just can it work, but how it might work practically with impact in the real world. Global Health: Science and Practice, 3(3), 327–329. doi: 10.9745/GHSP-D-15-00230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, … Onoya D (2014). South African National HIV Prevalence, Incidence and Behaviour Survey. [DOI] [PubMed]
- Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, & Patel V (2017). Psychological treatments for the world: lessons from low-and middle-income countries. Annual Review of Clinical Psychology, 13, 149–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorsdahl K, Myers B, Ward CL, Matzopoulos R, Mtukushe B, Nicol A, … Stein DJ (2015). Adapting a blended motivational interviewing and problem-solving intervention to address risky substance use amongst South Africans. Psychotherapy Research, 25(4), 435–444. [DOI] [PubMed] [Google Scholar]
- Sorsdahl K, Stein DJ, Weich L, Fourie D, & Myers B (2012). The effectiveness of a hospital-based intervention for patients with substance-use problems in the Western Cape. South African Medical Journal, 10(7), 634–635. [DOI] [PubMed] [Google Scholar]
- STATSSA. (2018). Mid-year population estimates. Statistical Release P0302. [Google Scholar]
- Tull MT, Berghoff CR, Bardeen JR, Schoenleber M, & Konkle-Parker DJ (2018). An initial open trial of a brief behavioral activation treatment for depression and medication adherence in HIV-infected patients. Behavior Modification, 42(2), 196–209. [DOI] [PubMed] [Google Scholar]
- van der Water T, Rossouw J, Yadin E, & Seedat S (2017). Impediments and catalysts to task-shifting psychotherapeutic interventions for adolescents with PTSD: perspectives of multi-stakeholders. Child and Adolescent Psychiatry and Mental Health, 11(48). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera SM, Pian J, … & Patel V (2013). Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database of Systematic Reviews, (11). [DOI] [PubMed] [Google Scholar]
- Wegner L (2011). Through the lens of a peer: Understanding leisure boredom and risk behaviour in adolescence. South Africa Journal of Occupational Therapy, 41(1), 18–24. [Google Scholar]
- Wegner L, Flisher AJ, Caldwell LL, Vergnani T, & Smith EA (2008). Healthwise South Africa: Cultural adaptation of a school-based risk prevention programme. Health Education Research, 23(6), 1085–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegner L, Flisher AJ, Muller M, & Lombard C (2006). Leisure boredom and substance use amongst high school students in Cape Town. Journal of Leisure Research, 38(2), 249–266. [Google Scholar]
- WHO-ASSIST. (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction, 97(9), 1183–1194. [DOI] [PubMed] [Google Scholar]
- WHO. (2008). Task shifting: Rational redistribution of tasks among health workforce teams: Global recommendations and guidelines. Retrieved from Geneva, Switzerland: [Google Scholar]
- Wingood GM, & DiClemente RJ (2008). The ADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. Journal of Acquired Immune Deficiency Syndrome, 47, S40–S46. [DOI] [PubMed] [Google Scholar]