Abstract
A significant problem among children with feeding disorders is packing (i.e., pocketing or holding accepted food in the mouth), which could hinder successful treatment. Previous research has identified effective treatments to reduce packing; however, an assessment model to guide treatment decisions is lacking. In the present study, we used a multielement design to identify conditions under which low levels of packing occurred for 4 children with feeding disorders. Results were used to empirically inform treatment selection to decrease packing for 3 children. Assessments indicated that packing was related to texture, food preference, or response effort and subsequently informed individualized treatments, which led to decreased levels of packing. Results suggest that this model may be useful in the design of treatment packages for children who engage in packing at clinically problematic levels.
Keywords: antecedent manipulation, assessment, packing, pediatric feeding disorder
Pediatric feeding disorders may be characterized by responses such as inadequate oral intake, food selectivity by type or texture of food, and expulsions or packing (Addison et al., 2012). Packing (i.e., pocketing or holding accepted food in the mouth; Patel, Piazza, Layer, Coleman, & Swartzwelder, 2005) can be extremely problematic among children with feeding disorders, as it prevents the child from consuming the food and may lead to nutritional deficiencies, such as failure to thrive, which can have detrimental effects on a child’s overall health (Patel et al., 2005). Packing may also contribute to interference with a previously successful feeding treatment, parental stress during mealtimes, and increased mealtime durations (Sevin, Gulotta, Sierp, Rosica, & Miller, 2002; Vaz et al., 2012).
Silbaugh, Swinnea, and Penrod (2017) identified studies in their review of packing literature, in which the clinical significance of packing among children was reported, but, to date, prior research has not identified an overall clinical prevalence of packing across a large sample of children. The authors also reported common treatments shown to reduce packing, some of which were food redistribution, chasers, texture manipulation, and simultaneous presentation. Redistribution involves using a bristled massaging toothbrush (i.e., a Nuk brush) to collect the packed bite of food (typically from the cheek or in the front of the mouth) and place the packed food back on the tongue to facilitate swallowing (e.g., Gulotta, Piazza, Patel, & Layer, 2005). Chasers are any liquid or solid reliably swallowed and are frequently presented immediately or 15 s after bite acceptance (e.g., Vaz et al., 2012). Decreasing texture (e.g., transitioning from regular texture to puree) has also been systematically evaluated and shown to be a viable treatment (e.g., Patel et al., 2005) for reducing packing. Patel et al. (2005) found that lower textures of nonpreferred foods were associated with increases in gram consumption and decreases in packing. Simultaneous presentation consists of presenting more than one food on a spoon at the same time (e.g., often a preferred food and a nonpreferred food) and has also been found to be effective in reducing packing (e.g., Buckley & Newchok, 2005). Comparative analyses suggest that packing may be related to different variables across children. For some, skill deficits may make it difficult to manipulate the bolus of food from the front to the back of the mouth, resulting in the bolus being packed and the child lacking the oral-motor skills to retrieve it (Gulotta et al., 2005). In other cases, packing may result in accessing reinforcement, as it will likely allow the child to avoid consuming the food (e.g., Piazza, Milnes, & Shalev, 2015). The treatments described may address these possible reasons for packing by potentially making swallowing less effortful (e.g., redistribution, chaser, texture manipulation) or less aversive due to pairing the food with readily consumed foods (e.g., chaser, simultaneous presentation; Piazza et al., 2002).
Applying a single intervention to every child could be ineffective and include unnecessary treatment components; therefore, each treatment package must be individualized and carefully selected. Practitioners could use a formal assessment model to select treatment packages targeting specific variables related to packing. Although such a model is not currently used in the selection of treatments for packing, an assessment model has been used to guide treatment selection in the context of mand training (Bourret, Vollmer, & Rapp, 2004). After identifying the conditions (i.e., prompt level) under which manding occurred, treatment packages were evaluated for each participant. Results showed that the assessment aided in including only necessary treatment components and in avoiding superfluous components. In parallel, an assessment to identify variables related to low levels of packing may be advantageous in the context of food refusal, by directing practitioners to perhaps the most likely effective intervention for packing.
Considering the serious risks associated with packing, there is a need for a formalized assessment-intervention model. Packing can be very difficult to treat, particularly when treatments in place may include unnecessary components that do not target specific variables that affect packing. For example, decreasing texture across all foods may restrict a child unnecessarily if he or she has the ability to chew some regular-texture foods in his or her repertoire. Practitioners often conduct functional analyses for food refusal (i.e., Piazza et al., 2003) to determine behavioral function and inform an individualized treatment. Food refusal typically assessed within a functional analysis includes common topographies of inappropriate mealtime behavior (IMB; e.g., head turning, covering the mouth, and pushing the food away). However, when a child’s most problematic topography of food refusal is packing, it is difficult to determine the stimuli responsible for differing levels of packing within the context of a typical functional analysis. Assessments aimed at identifying the conditions under which low levels of packing occur could help practitioners design effective treatments to reduce packing. Thus, we evaluated an assessment model to identify conditions under which low levels of packing were observed, and applied assessment results to guide treatment selection.
Method
Participants
Four children with a history of pediatric feeding disorders participated in the study. All four children had been admitted to an intensive pediatric feeding program due to food refusal or selectivity (i.e., the child did not consume sufficient foods or liquids orally or consumed only a small variety of foods or liquids). Children were included in the study if they packed more than 20% of bites on average for three consecutive sessions, or if they failed to consume 100% of their programmed meal volume (i.e., maximum session duration was met before all food was consumed) for at least 20% of meals, under their individualized mealtime protocol. Children were excluded from the study if they were at risk for aspiration, as indicated by a medical professional; had no prior history with eating orally; expelled bites at clinically high rates (i.e., 0.5 expels or greater per minute on average for three consecutive sessions); or did not permit bites to be deposited into the mouth.
Danny
Danny was a 4-year-old male with autism spectrum disorder (ASD), developmental delays, a speech and language delay, and a feeding disorder of infancy and childhood. He was admitted to the program due to food selectivity. That is, at the time of his admission, Danny only consumed preferred foods or liquids (i.e., McDonald’s French fries, crackers, chips, vanilla or strawberry PediaSure, water, and fruit juice). When presented with nonpreferred foods, Danny typically engaged in the following responses: crying, screaming, head turning, plate flipping, gagging, expelling, aggressing, and leaving the table. He could finger feed but had no history of utensil use, and his only reported allergies were to peaches, which were avoided as per a nutritionist. Following Danny’s treatment evaluation for IMB and acceptance, packing was identified as a problematic response, particularly when presented with the following foods: green beans, carrots, and chicken nuggets.
Jack
Jack was a 3-year-old male with ASD, attention deficit hyperactivity disorder (ADHD), mixed receptive-expressive language disorder, delayed developmental milestones, conduct disorder, torticollis, plagiocephaly, hypotonia, sensory-processing difficulty, and dysphagia. He was admitted to the program due to food selectivity. That is, at the time of his admission, Jack only consumed preferred foods or liquids (i.e., PediaSure, juice, saltine crackers, granola bars, French toast, hash browns, chips, and pizza) and refused fruits, vegetables, dairy products, and meats. When presented with nonpreferred foods, Jack typically engaged in the following responses: verbal refusal (e.g., saying, “No.”), crying, throwing food, expelling, aggressing (i.e., pinching, biting, hitting, punching), and elopement. He could feed himself liquids from a bottle or finger feed but did not use utensils. Jack had no reported allergies or diet restrictions. Following Jack’s treatment evaluation for IMB and acceptance, packing was identified as a problematic response, particularly when presented with the following foods: carrots, green beans, oranges, bananas, peaches, yogurt, fish sticks, and pizza.
Gus
Gus was a 2-year-old male with a feeding disorder of infancy and early childhood, oral aversion, and developmental delays. He was admitted to the program due to reliance on nasogastric-tube feeds and food refusal. That is, at the time of his admission, Gus only consumed preferred solids and liquids (i.e., PediaSure and French fries). When presented with nonpreferred foods, Gus typically engaged in the following responses: head turning, crying, mouth covering, packing, and expelling. His only reported allergies were to fava beans, which were avoided, and he did not feed himself. Following Gus’s treatment evaluation for IMB and acceptance, packing was identified as a problematic response, particularly when presented with the following foods: bananas, oranges, black beans, sausage, chicken nuggets, spinach, and pancakes.
Nina
Nina was a 4-year-old female with ADHD, gastroesophageal reflux, constipation, chronic lung disease, grade 2 intraventricular hemorrhage, retinopathy of prematurity, developmental delay, speech delay, and a history of nasogastric-tube feeds. She was admitted to the program due to food and texture selectivity. At the time of her admission, Nina could feed herself and only consumed preferred solids and liquids (i.e., PediaSure®, cheddar cheese, crackers, and French fries). When presented with nonpreferred foods, Nina typically engaged in the following responses: verbal refusal (e.g., saying, “No.”), crying, head turning, mouth covering, and elopement. Nina’s parents reported a preference to avoid processed foods and asked Nina’s therapists to only present organic foods when possible. Following Nina’s treatment evaluation for IMB and acceptance, packing was identified as a problematic response, particularly when presented with the following foods: peaches, pears, carrots, green beans, macaroni and cheese, and baked beans.
Each child had varying communication and play skills, as per parent interview and review of medical records. Danny primarily used gesturing to communicate and often engaged in parallel play when placed in play settings with other children. Jack and Gus were vocal, and each played independently. Jack could maintain high-level conversations, and Gus communicated with one-word phrases. Although Nina’s play skills were typical for her age, and she could vocalize, she could only hold simple conversations, during which she often emitted echoics.
Materials and Setting
Sessions were conducted three times per day in a 3 m × 3 m treatment room equipped with a one-way observation window, a table, chairs, and a high chair or a wooden chair with a tray (i.e., a Rifton® chair). Appropriate utensils (e.g., large or small spoons), napkins, plates, and a timer were also present. If applicable, tangible items (i.e., highly preferred toys) were included.
Response Definitions and Measurement
The primary dependent variables were packing and mouth clean. We defined packing and mouth clean as a bite of food larger than the size of a pea in the mouth 30 s following bite acceptance, and no bites of food larger than the size of a pea in the mouth 30 s following bite acceptance, respectively. Trained bachelor’s- and master’s-level observers collected data using a data collection program (i.e., Instant Data) on laptop computers. We calculated levels of packing and mouth clean by dividing the number of packed bites by the number of total bites accepted and converting to a percentage, and dividing the number of bites with mouth clean by total bites accepted and converting to a percentage, respectively. We considered packing to be problematic if it was observed for more than 20% of bites, or if the therapist could not present the programmed volume of food because the participant held a bite of food in his or her mouth until the maximum session duration.
Interobserver Agreement
Trained data collectors assessed interobserver agreement (IOA) by having a second independent observer collect data on all measures during 33.3%, 34.3%, 42.7%, and 33.3% of assessment sessions for Danny, Jack, Gus, and Nina, respectively. A second observer was also present during 38.0%, 36.7%, and 23.1% of treatment evaluation sessions for Jack, Gus, and Nina, respectively. The second observer compared collected data to those collected by the primary observer. Evaluations of IOA were distributed randomly across observations. We calculated agreement (i.e., both observers recording the same response) using a block-by-block method, by dividing the session into 10-s intervals and dividing the smaller number of responses scored by each observer within each interval by the larger number of responses (i.e., Mudford, Martin, Hui, & Taylor, 2009), as well as averaging agreement across sessions and converting to a percentage. During assessments, mean IOA for packing was 100% for Danny, 97.9% (range 87.1%–100%) for Jack, 99.8% (range 93.6%–100%) for Gus, and 99.7% (range 93.6%–100%) for Nina. Mean IOA for mouth clean was 98.3% (range 83.3%–100%) for Danny, 99.4% (range 85.7%–100%) for Jack, 98.4% (range 90.0%–100%) for Gus, and 99.4% (range 87.5%–100%) for Nina. During treatment evaluations, mean IOA for packing was 99.2% (range 93.4%–100%) for Jack, 99.7% (range 96.7%–100%) for Gus, and 97.8% (range 96.7%–100%) for Nina. Mean IOA for mouth clean was 98.7% (range 94.4%–100%) for Jack, 98.1% (range 96.4%–100%) for Gus, and 99.5% (range 98.4%–100%) for Nina.
Treatment Integrity
We scored treatment integrity by recording the therapist’s adherence to programmed contingencies for 33% of sessions. Therapist responses included (a) prompting within 3 s of the bite presentation; (b) praising within 3 s of bite acceptance or mouth clean; (c) providing reinforcement for the appropriate duration of time, if applicable; and (d) presenting the finger prompt or Nuk® brush within the predetermined amount of time, per the child’s current mealtime protocol, if applicable. Treatment integrity was scored as a percentage of the aforementioned responses implemented correctly across sessions (i.e., the number of components completed correctly divided by the number of components completed correctly plus the number of components either not completed or completed incorrectly). We calculated treatment integrity across sessions by dividing the total instances of correct implementation by the total number of opportunities to implement the contingencies (i.e., correct implementation plus incorrect implementation) and converting to a percentage. Mean treatment integrity across assessments was 95% (range 82%–100%) for Danny, 96% (range 78%–100%) for Jack, 95% (range 77%–100%) for Gus, and 100% for Nina. Mean treatment integrity across treatment evaluations was 96% (range 96%–100%) for Jack, 98% (range 89%–100%) for Gus, and 100% for Nina.
Procedures and Experimental Design
We used a multielement design and reversal design to demonstrate experimental control during assessments and treatment evaluations, respectively. Staff predetermined the order of control and test sessions by random drawing. That is, team members randomly paired a number with each condition, which was unknown to the therapist, and the therapist randomly selected the given numbers to create an order of sessions. Experimental control was demonstrated when differentiation occurred between the control condition and at least one of the test conditions during assessments, or when packing decreased to less than 20% of bites during the intervention and increased to greater than 20% of bites when baseline conditions were reinstated.
Packing prevalence
Prior to the assessment and treatment of packing, we searched record reviews (i.e., treatment evaluations and initial intake documents) of former patients from the years 2014 to 2016 in order to obtain an estimated prevalence of packing in an intensive pediatric feeding disorders program. We recorded the total number of patients (N = 225), the percentage of patients that engaged in clinically high levels of packing (42%), the percentage of patients whose caregivers reported packing as a concern prior to admission (37%), the percentage of patients who developed packing during their admission (63%; most commonly following treatment for bite acceptance), and the percentage of children who did not completely meet their clinical goals (i.e., continued to engage in packing during greater than 20% of bite presentations across five consecutive sessions on average) to reduce packing.
Preexperimental assessment: Chewing assessment
The purpose of the pilot chewing assessment was to create a hierarchy of foods requiring high, medium, and low effort to chew to mastication, or wetground texture (i.e., oatmeal consistency). Nine staff members familiar with preparing food to a wet ground texture were asked to chew four foods, three times each, from each food group (i.e., fruits, vegetables, starches, and proteins) and record the number of chews required to fully masticate the foods. We determined a mean for each food across staff members, and compared those to determine differentiation between high-, moderate-, and low-effort foods. However, due to differentiation seen between the same foods across staff members, an overall ordinal ranking was created. That is, the foods that were most often ranked highest, in terms of the highest number of chews to masticate, were grouped into the high-effort group (i.e., difficult to chew; apples, chicken nuggets, fish sticks, pancakes). Subsequently, foods most often ranked in the middle were considered moderate effort (i.e., moderately difficult to chew; canned corn, cooked broccoli, hot dogs, French fries, canned green beans, canned sweet potatoes, baked beans, strawberries), and foods most often ranked last were considered low effort (i.e., easy to chew; macaroni and cheese, canned peaches, canned pears, canned carrots). We computed a Spearman’s correlation to compare this list with the rankings of three Board Certified Behavior Analysts (BCBAs; doctoral level and master’s level), each experienced in the assessment and treatment of pediatric feeding disorders. There was a positive correlation between the lists (r = 0.755).
Preexperimental assessment: preference assessment
The purpose of the pictorial without-access preference assessment was to determine high-, moderate-, and low-preferred foods (PWA; i.e., Groskreutz & Graff, 2009) for each participant. Two photos of foods were simultaneously placed 30 cm in front of the participant, and 30 cm away from each other. The order of these photos was predetermined, such that each photo appeared equally with every other photo in a pair. Due to previously observed packing, therapists did not provide access to the actual foods during these assessments. These results were used to identify an estimated preference between foods, as well as to inform the packing assessment for food preference.
Preassessment intervention (all participants)
All participants were exposed to interventions to target acceptance prior to the packing assessment. Each intervention was informed by functional analysis results, which all indicated that escape from demands and contingent attention or tangibles reinforced IMB. In all sessions, 10 bites of three to four commonly packed foods were presented per meal block (i.e., set of sessions) using individualized treatment protocols. For all participants, bites were initially presented using an upright spoon. Regular-texture bites were presented at a dime size (Danny, Jack, Gus) or half-dime size (Nina); naturally lower texture bites were presented using a level spoon (Danny, Jack, Gus, Nina). Occupational and speech-language therapists were consulted to ensure appropriateness of bite size for each participant. For Danny, therapists implemented escape extinction (i.e., nonremoval of the spoon and re-presentation of expels), and differential reinforcement of alternative behavior (DRA; attention and preferred tangible item following acceptance) to increase bite acceptance. A finger prompt procedure, in which the therapist inserted his or her index finger along the participant’s upper gum line after 5 s of nonacceptance (i.e., Borrero, Schlereth, Rubio, & Taylor, 2013), and side deposit procedure, in which the therapist used a finger or Nuk® brush to insert the food into the participant’s cheek after 10 s of nonacceptance (i.e., Rubio, Borrero, & Taylor, 2015) were included to further increase bite acceptance. After acceptance increased, high levels of packing were observed, so the DRA procedure was modified to provide reinforcement contingent on mouth cleans.
For Jack, therapists implemented escape extinction and DRA (contingent on acceptance) along with finger prompt and side deposit procedures to increase bite acceptance. After acceptance increased and high levels of packing were observed, DRA contingencies were modified to provide reinforcement for mouth cleans. For Gus, treatment in the form of escape extinction and DRA for acceptance was in place. Increases in acceptance were observed with high levels of packing, so the team modified DRA contingencies to provide reinforcement for mouth cleans. For Nina, treatment in the form of escape extinction and DRA with attention contingent on bite acceptance was in place prior to packing assessments. All participants engaged in packing at clinically problematic levels in the three sessions prior to the packing assessment (100% of bites for Danny and Jack, 93% of bites for Gus, and 40% with an increasing trend for Nina).
Control condition
The purpose of the control condition was for researchers to compare levels of packing during the participants’ current mealtime protocols (i.e., the control) and the test conditions in the current evaluation. For all participants, packing was observed at problematic levels under their current mealtime protocol. Control conditions were identical to the preassessment intervention condition for each participant with the exception of the number of bites presented. To promote efficiency and avoid health risks (i.e., choking), no more than three bites were presented during these sessions. Sessions were terminated when the child consumed all three bites or the when 5-min time cap was met.
Test conditions
We compared levels of packing during test conditions and the control condition (i.e., participants’ current mealtime protocol) to identify conditions under which low levels of packing were observed. Separate comparisons were conducted to evaluate the role of a number of variables, including demands, food preferences, textures, effort, bite or bolus size, and the use of a modified chaser procedure. Variables were targeted on an individual basis and were selected depending on the conditions under which packing was observed. That is, the therapists and a doctoral-level BCBA, with a minimum of 5 years of experience working in feeding, used clinical observations to target the most likely variables to assess, based on clinical relevance and safety. Assessments were discontinued when one to two variables were associated with low levels of packing, as that information indicated a potential starting point for further treatment.
All commonly packed foods were presented across all sessions for Jack, Gus, and Nina (three to four foods per meal block). Due to a small number of commonly packed foods for Danny (i.e., only vegetables and proteins), each of Danny’s foods was evaluated separately. Each packing assessment continued until differentiation was observed between at least one of the test conditions and the control condition. No more than three bites per session were presented during all but two conditions, and sessions were terminated when the child consumed all three bites or when the 5-min session duration was reached. Each assessment was conducted across 2 days on average. All sessions were identical to the control session except for the specific variations described next (i.e., demand, bite or bolus size, texture, effort, food preference, and the use of a modified chaser). Each variable was evaluated in a separate condition within each assessment and was based on empirically evaluated treatments or clinical judgment. That is, research has shown that texture manipulation or simultaneous presentation can lead to reduced levels of packing, for example.
Demand assessment (all participants)
Three-bite, five-bite, and ten-bite (control) presentations were compared to determine if the number of demands (i.e., bite presentations) affected levels of packing. From the child’s perspective, each bite of food could be considered to be one demand (i.e., the child must take the bite off of the spoon, hold the bite in the mouth, contact the taste and texture of the food, chew and manipulate the food, and swallow the bolus). Potentially, decreasing the number of demands (i.e., bites) could affect packing if decreasing the number of times those actions were required made the steps “less aversive” to the child. That is, if fatigue (or an unpleasant taste) came into play, 3 bites may be easier for a child to eat than 10 bites. Regular-texture bites were presented at a dime size (Danny, Jack, Gus) or half-dime size (Nina) during this assessment. Low levels of packing during the test conditions of the demand assessment indicated that decreasing the number of bites presented during sessions may lead to reduced levels of packing.
Bite- or bolus-size assessment (all participants)
If therapists observed the child packing regular-texture foods in the preassessment intervention, then bite sizes (i.e., dime size, half-dime size, and fork-pressed half-dime size) were compared to determine if bite size affected levels of packing. The bite size the child was presented with during the preassessment intervention was presented in the control condition for Danny, Jack, Gus (dime size), and Nina (half-dime size). If the child consumed and packed lower textures, then bolus sizes (level spoon [control], half-level spoon, and quarter-level spoon) were compared. Only Nina participated in the bolus-size assessment, due to variable levels of packing and gagging with wetground texture and a level bolus. Low levels of packing during the test conditions of the bite or bolus assessment indicated that decreasing the bite or bolus size could be a viable intervention for packing.
Texture assessment (Danny, Jack, and Nina)
Regular-texture foods (i.e., the texture the child was presented with during preassessment intervention) were presented in the control condition at a dime size (Danny and Jack) or half-dime size (Nina). Regular-texture foods were compared to all other textures (i.e., puree, junior, wetground), with a level spoon, to determine if the texture of foods affected levels of packing. Puree texture refers to smooth food with no lumps, and ju nior texture refers to food blended with small lumps, similar to applesauce. Gus did not participate in the texture assessment because, in addition to regular-texture foods, he also packed naturally lower texture foods (e.g., applesauce). Low levels of packing during the test conditions of the texture assessment indicated that decreasing texture may lead to reduced levels of packing.
Effort assessment (Gus and Nina)
For participants presented with regular-texture foods, high-effort (control; Gus), moderate-effort (Gus and Nina), low-effort (Gus), or soft dissolvable (Nina) foods were compared to determine if response effort (i.e., frequency of chews) affected levels of packing. Bites were presented at a dime size (Gus) or half-dime size (Nina). Therapists grouped foods into each category, as indicated by results from the preexperimental chew assessment. Danny and Jack did not participate in the effort assessment due to identification of one to two variables associated with packing prior to the effort assessment. Low levels of packing during the test conditions of the effort assessment indicated that presenting lower effort foods may lead to reduced levels of packing.
Preference assessment (Jack)
High-preferred, moderately preferred, and low-preferred (control) foods were compared to determine if food preference affected levels of packing. Foods were grouped into each category, as indicated by results from the PWA. Danny, Gus, and Nina did not participate in the preference assessment due to identification of one to two variables associated with packing prior to the preference assessment. Additionally, a preference hierarchy was not identified for Danny. Low levels of packing during the test conditions of the preference assessment indicated that presenting more highly preferred foods could result in reduced levels of packing.
Modified chaser assessment (Jack)
We evaluated the use of a modified chaser following discussions with oral-motor therapists due to concerns about choking from swallowing foods whole and potential risks associated with strengthening swallowing whole. That is, instead of providing liquid while the food remained in the mouth (e.g., Vaz et al., 2012), we presented water contingent on mouth clean. This will be referred to as a modified chaser (i.e., a contingent drink). Conditions in which no modified chaser was present (control) were compared to conditions in which a modified chaser (i.e., water) was presented following mouth cleans to determine if the presentation of water affected levels of packing. Danny, Gus, and Nina did not participate in the modified chaser assessment due to identification of one to two variables associated with packing prior to the modified chaser assessment. Low levels of packing during the test condition of the modified chaser assessment indicated that presenting water following a swallow could lead to reduced levels of packing.
Postassessment baseline
Baseline sessions were conducted for Jack, Gus, and Nina and were identical to the preassessment intervention conditions. For all participants, packing occurred at problematic levels in the preassessment intervention condition, suggesting a packing assessment was needed. During the postassessment baseline conditions, the previous treatment was reintroduced for Jack, Gus, and Nina to determine if packing was still problematic after the assessment. Danny did not participate because, during the bite-size assessment, he began to swallow the majority of foods that he previously packed, and the team decided to target other responses deemed more clinically significant than evaluating the packing of proteins (i.e., spoon acceptance and parent training). His mother also expressed interest in discontinuing the assessments.
Treatment evaluation (Jack, Gus, and Nina)
We designed each participant’s treatment evaluation based on his or her assessment results. Danny did not participate in the treatment evaluation due to parental request. Conditions in which low levels of packing occurred were incorporated into the individualized treatment conditions. If more than one condition was associated with low levels of packing, a combined intervention was designed to increase the likelihood of effectiveness; however, a component analysis was not conducted. Because packing was related to multiple variables for Jack and Gus, the selected interventions were designed to target multiple variables related to packing. Figure 1 includes a flowchart depicting the order of events during each packing assessment, indicating whether to select a treatment based on the results or to move on to the next assessment. Table 1 includes a table depicting which assessments were conducted for each participant, which assessments yielded differentiated results, and the identified treatments.
Fig. 1.
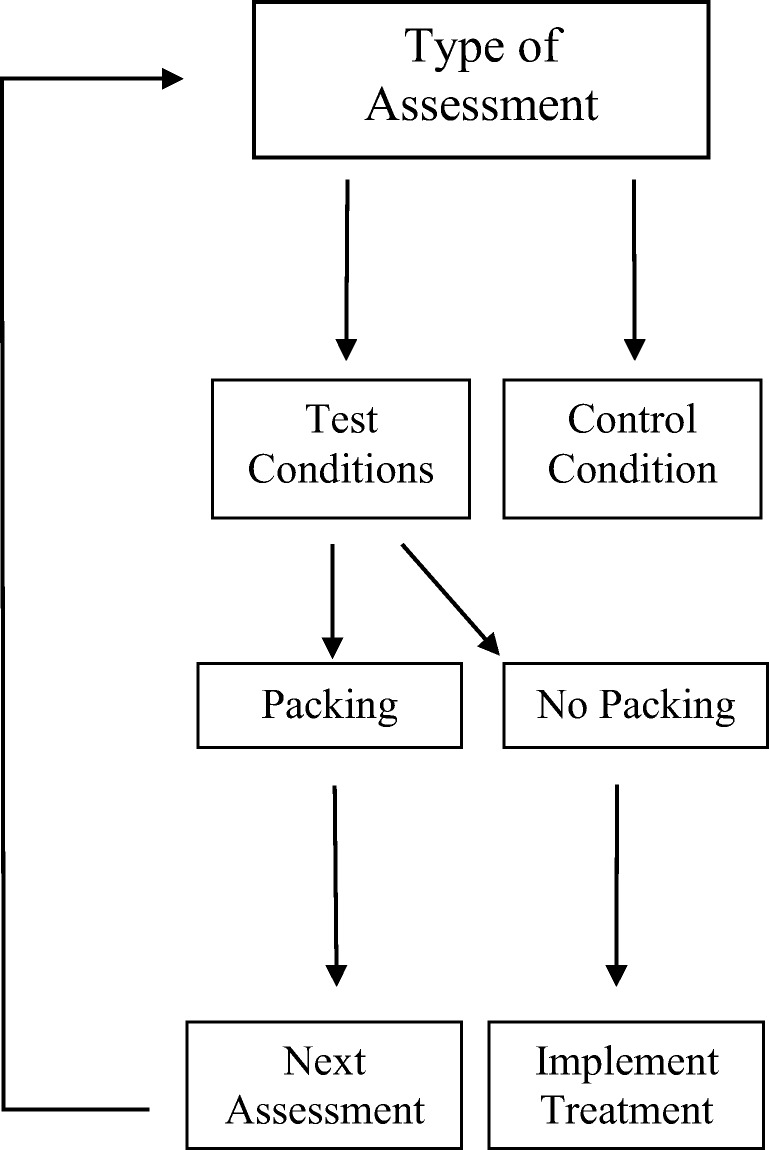
Flowchart depicting the order of events during each packing assessment, indicating whether to select a treatment based on the results or to move on to the next assessment. Assessments continued until low levels of packing were identified in one to two assessments
Table 1.
Table Depicting Which Assessments Were Conducted for Each Participant, Which Assessments Informed Treatment as Indicated by “Yes” or “No,” and Identified Treatments
| Assessment | Identified Treatment | ||||||
|---|---|---|---|---|---|---|---|
| Demand | Bite/Bolus Size | Texture | Effort | Preference | Modified Chaser | ||
| Test Conditions Conducted | |||||||
| Danny |
Conducted No |
Conducted Yes |
Conducted Yes |
||||
| Jack |
Conducted No |
Conducted No |
Conducted Yes |
Conducted Yes |
Conducted No |
Decreased texture (low-preferred foods) | |
| Gus |
Conducted No |
Conducted Yes |
Conducted Yes |
Decreased bite size (moderate-effort foods) | |||
| Nina |
Conducted No |
Conducted No |
Conducted Yes |
Conducted No |
Decreased texture (all foods) | ||
Note. Blank cells indicate data are not applicable.
Results
Assessment Results
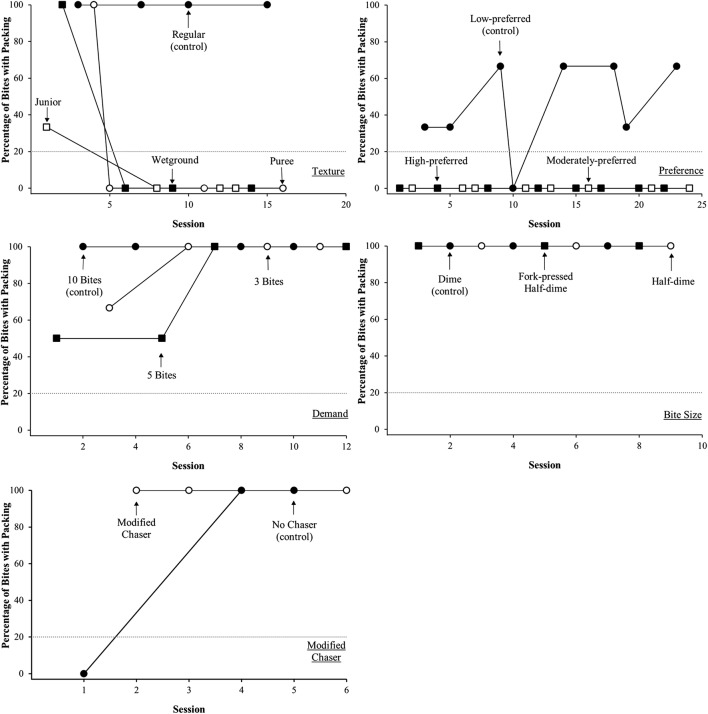
Danny
Figure 2 shows the percentage of packing per session for the demand (top panel), texture (middle panel), and bite-size (bottom panel) assessments. The evaluation of the demand assessment shows the percentage of bites with packing during the 10-bite, 5-bite, and 3-bite conditions. Levels of packing remained high across all conditions (M = 100%) and showed no differentiation across conditions for demands (10-bite, 5-bite, 3-bite). The evaluation of texture yielded differentiated results; packing was high (M = 100%) with regular texture, but low (M = 0%) with the wetground, junior, and puree texture conditions of the assessment. The evaluation of bite size shows the percentage of bites with packing with the dime, half-dime, and fork-pressed half-dime conditions. Protein and vegetable probes were also conducted with novel proteins and vegetables because these foods were commonly packed. Levels of packing were initially high during the dime and half-dime fork-pressed conditions, suggesting differentiation, but decreased across sessions (M = 20%; range 0%–100%) and were low during the half-dime condition (M = 0%). Levels of packing were high during the protein probes (M = 100%) and low during the vegetable probes (M = 0%). For Danny, the results of the assessments suggested that presentation of lower texture foods and smaller bite sizes for proteins would be a potentially effective intervention for packing. That is, because lower levels of packing occurred during the test conditions of the texture and bite-size assessments, variables related to texture and bite size were selected for intervention.
Fig. 2.
Danny’s percentage of packing per session during the demand assessment (top panel), the texture assessment (middle panel), and the bolus assessment (bottom panel). Protein and vegetable probes are also shown in the bolus assessment, conducted under the control condition (i.e., dime-sized bites were presented)
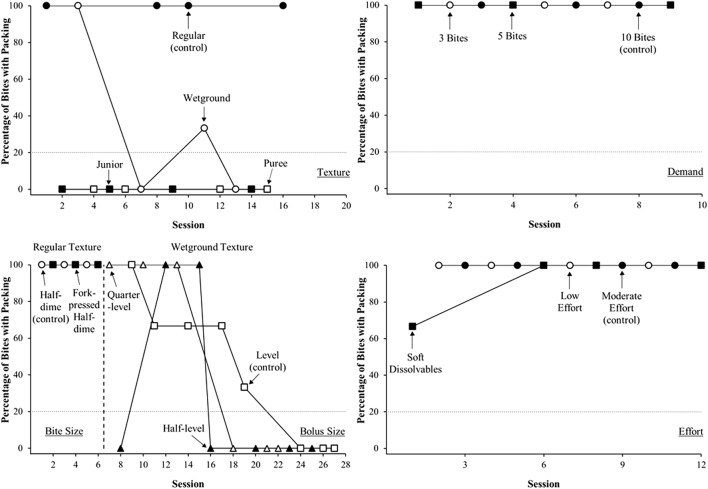
Jack
Figure 3 shows the percentage of packing per session for the texture (top-left panel), preference (top-right panel), demand (middle-left panel), bite-size (middle-right panel), and modified chaser (bottom-left panel) assessments. The evaluation of texture yielded differentiated results. Packing was initially high across all conditions, remained high (M = 100%) with regular texture and decreased across conditions with wetground, junior, and puree textures (M = 19%; range 0%–100%). The evaluation of preference also yielded differentiated results. Packing was relatively high and variable (M = 45%; range 0%–66%) during the low-preferred condition as compared to all other conditions (M = 0%; high preferred and moderately preferred). The evaluation of demands showed no differentiation and high levels of packing across the 10-bite (M = 100%), 5-bite (M = 91; range 50%–100%), and 3-bite (M = 75; range 66%–100%) conditions. The evaluation of bite size yielded no differentiation (M = 100%) across conditions (dime, half-dime, and fork-pressed half-dime). The evaluation of the modified chaser yielded no differentiation across the modified chaser (M = 100%) and no chaser (M = 66%; range 0%–100%) conditions. For Jack, the results of the assessments suggested that presentation of lower texture, low-preferred foods would be a potentially effective treatment for packing. That is, because low levels of packing occurred during the test conditions of the texture and preference assessments, manipulation of texture based on food preference was selected to reduce packing.
Fig. 3.
Jack’s percentage of packing per session during the texture assessment (top-left panel), the preference assessment (top-right panel), the demand assessment (middle-left panel), the bite-size assessment (middle-right panel), and the modified chaser assessment (bottom-left panel)
Gus
Figure 4 shows the percentage of packing per session for the demand (top panel), bite-size (middle panel), and effort (bottom panel) assessments. The evaluation of demands yielded no differentiation with the number of demands (10-bite, 5-bite, 3-bite), as packing was relatively variable across the 10-bite (M = 27%; range 0%–80%), 5-bite (M = 28%; range 0%–100%), and 3-bite (M = 31%; range 0%–100%) conditions. The evaluation of the bite-size assessment shows the percentage of bites with packing for the dime, half-dime, and fork-pressed half-dime conditions. Levels of packing were consistently highest during the dime condition (M = 36%; range 0%–100%) and lower with the half-dime (M = 13%; range 0%–66%) and fork-pressed half-dime (M = 8%; range 0%–33%) conditions, although packing decreased in all conditions over time. The evaluation of the effort assessment yielded differentiated results between the moderate-effort (M = 52; range 33%–100%), high-effort (M = 19; range 0%–33%), and low-effort (M = 0%) conditions. For Gus, the results of the assessments suggested that providing smaller (i.e., no larger than half-dime size) bite sizes for moderate-effort foods might be an effective intervention. That is, because low levels of packing occurred during the test conditions of the bite-size and effort assessments, an intervention altering bite size and effort was selected to decrease packing.
Fig. 4.
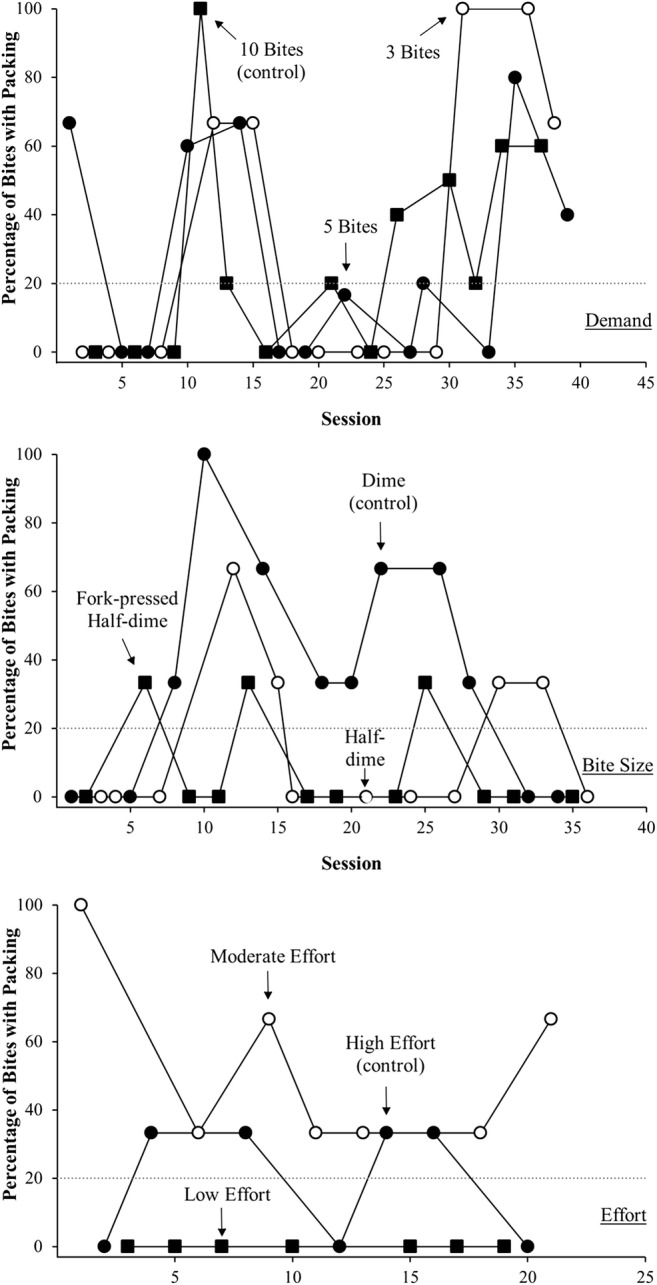
Gus’s percentage of packing per session during the demand assessment (top panel), the bite-size assessment (middle panel), and the effort assessment (bottom panel)
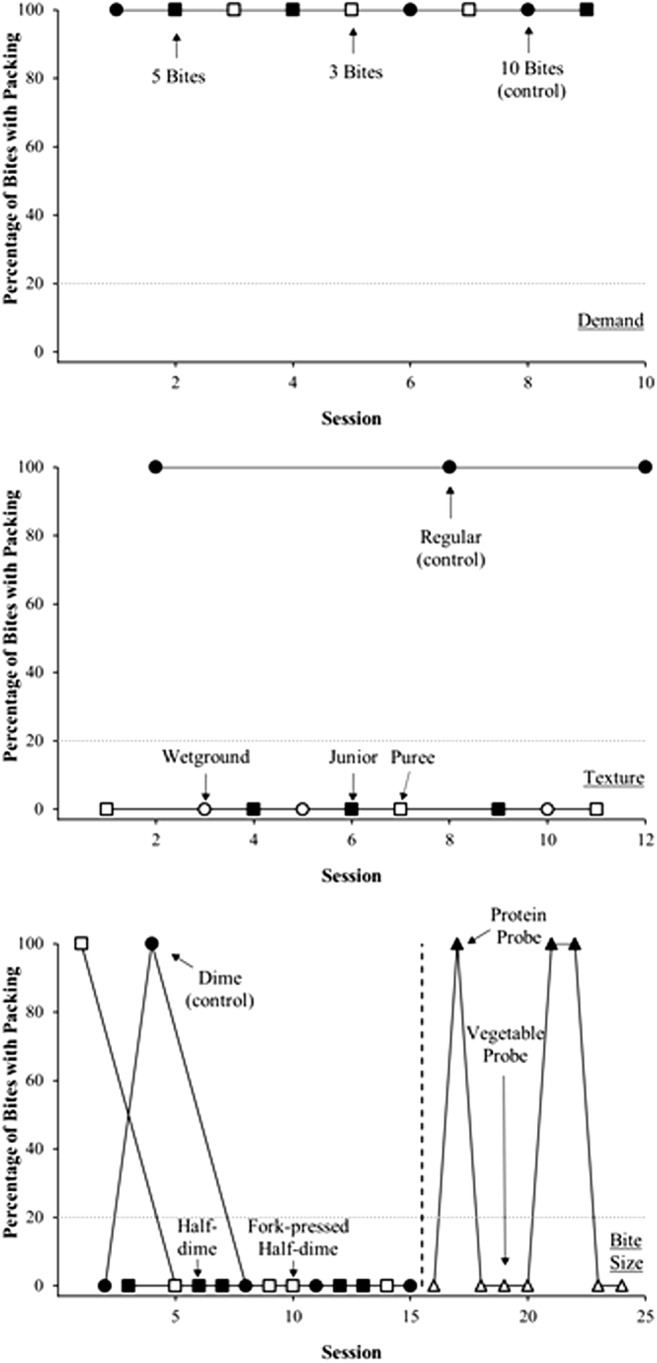
Nina
Figure 5 shows the percentage of packing per session during the texture (top-left panel), demand (top-right panel), bite- and bolus-size (bottom-left panel), and effort (bottom-right panel) assessments. The texture assessment shows the percentage of bites with packing during the regular, wetground, junior, and puree conditions. Levels of packing were differentiated, and the most packing was observed with regular texture (M = 100%), as compared to wetground (M = 33%; range 0%–100%), junior (M = 0%), and puree (M = 0%). The demand assessment yielded no differentiation across conditions (M = 100% for all conditions). The bite-size assessment yielded no differentiation for regular-texture presentations (half-dime and fork-pressed half-dime; M = 100%), although levels of packing were lower during the bolus-size assessment for wetground-texture presentations. Initially, packing was lowest when a level spoon was presented (M = 42%; range 0%–100%) but decreased to zero with the level, half-level (M = 29%; range 0%–100%), and quarter-level (M = 50%; range 0%–100%) conditions. The effort assessment shows the percentage of packs per session with moderate-effort, low-effort, and soft dissolvable conditions of the effort assessment. Levels of packs were high and undifferentiated across all conditions (M = 97%; range 66%–100% across all conditions). For Nina, because the results of the assessments suggested low levels of packing occurred during the test conditions of the texture assessment, presentation of lower texture foods was selected as an intervention to decrease levels of packing.
Fig. 5.
Nina’s percentage of packing per session during the texture assessment (top-left panel), the demand assessment (top-right panel), the bite or bolus assessment (bottom-left panel), and the effort assessment (bottom-right panel)
Treatment Results
Jack
Figure 6 (top panel) shows the percentage of bites with packing per session during the postassessment baseline and treatment conditions. Levels of packing were high during the postassessment baseline condition (M = 60%) but decreased immediately during the treatment condition (M = 0%). Levels of packing remained low during the reversal to baseline (M = 0%) and during vegetable probes (M = 0%), when all foods were presented at regular texture. This indicated that additional components for treating packing were no longer required.
Fig. 6.
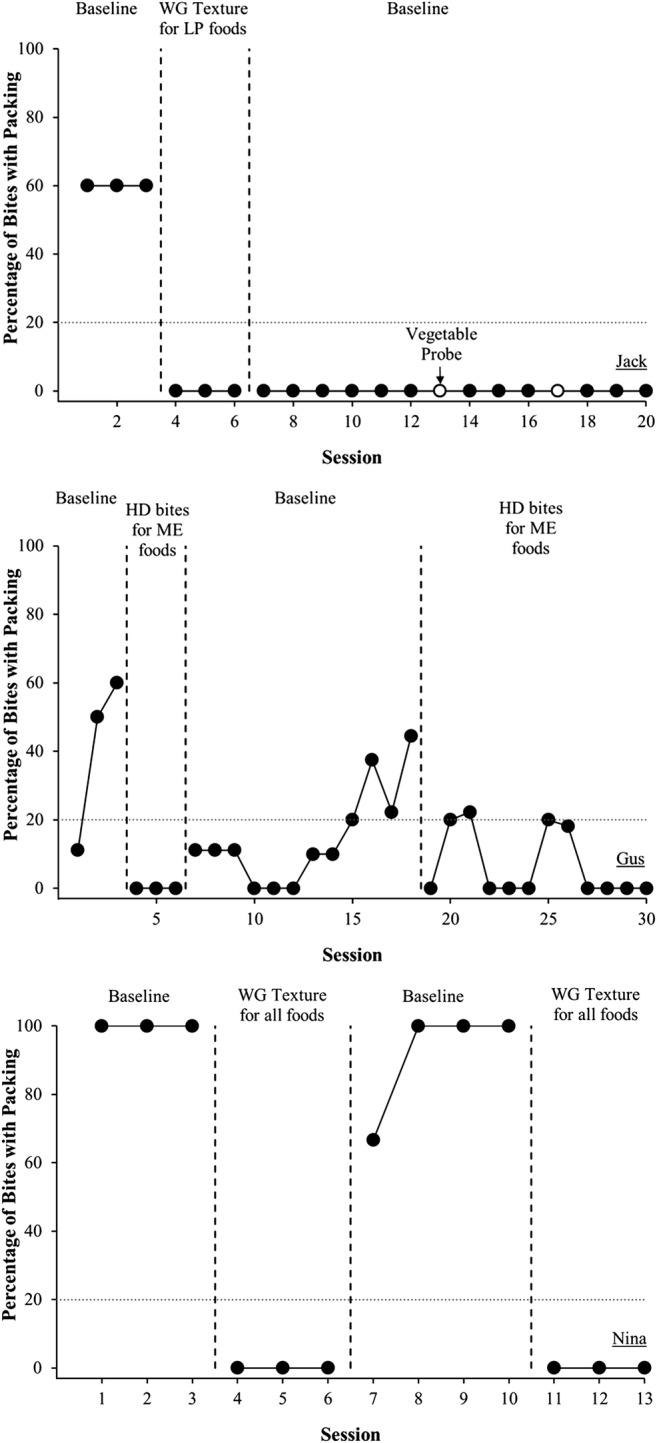
Percentage of packing in postassessment evaluations for Jack (top panel), Gus (middle panel), and Nina (bottom panel). Jack’s treatment included reducing texture of low-preferred (LP) foods to wetground (WG). Gus’s treatment included reducing bite size of moderate-effort (ME) foods to half-dime (HD) size. Nina’s treatment included reducing texture of all foods to WG
Gus
Figure 6 (middle panel) shows the percentage of packing per session during the postassessment baseline and treatment conditions. Levels of packing were on an increasing trend during the postassessment baseline condition (M = 40; range 11%–60%) and low during the treatment condition (M = 0%). During the reversal to baseline, packing increased again to problematic levels (M = 14; range 0%–44%) and decreased when treatment was reintroduced (M = 6; range 0%–22%).
Nina
Figure 6 (bottom panel) shows the percentage of packing per session during the postassessment baseline and treatment conditions. Levels of packing were high during the postassessment baseline condition (M = 100%) and low during the treatment condition (M = 0%). Results were replicated during the reversal to baseline (M = 91%; range 66%–100%) and return to treatment (M = 0%).
Discussion
Through the use of this pretreatment assessment model and prior empirically evaluated treatments to decrease packing, we were able to more closely evaluate several variables that may affect levels of packing. Results suggest that this pretreatment assessment model was successful at identifying conditions in which low levels of packing occurred for all four participants. For all participants, high levels of packing were associated with texture, food preference, or response effort. The assessment results suggested unique, individualized treatment packages for three participants, which were demonstrated to effectively reduce packing. Unfortunately, we did not collect follow-up data to demonstrate the results maintained after discharge, but results did maintain through the remainder of each child’s admission. We selected bite number (conceptualized as demands) to determine if the number of times the participants were asked to eat certain foods was related to packing. That is, if the taste of the food or fatigue was related to packing, requiring a child to take fewer bites could have resulted in less packing. The level of demands (i.e., number of bites) did not appear to differentially affect packing for these participants, suggesting it may not be a viable treatment for packing, although further research should be conducted to determine this.
Similar to the synthesized results from Silbaugh et al. (2017), the majority of children (i.e., 63%) in the record reviews who engaged in clinically high levels of packing developed the response following treatment of acceptance (i.e., during their intensive admission, rather than prior to receiving services). Additionally, three of our participants (Danny, Jack, and Nina) did not engage in clinically high levels of packing until treatment for IMB was initiated. As Silbaugh et al. note, this suggests that packing was not a preexisting problem for most children. Because packing may develop following treatment of acceptance, this may not become an issue until later in the child’s treatment. This may be particularly relevant for practitioners working in home or school settings, as packing may be an unexpected novel response that must then be addressed.
One difficulty specific to packing is that to reduce packing, and eliminate the potential escape a child may access by packing a bite of food, the child is required to swallow a bite of food. Swallowing is a response that the child must engage in independently. Otherwise, escape from eating will occur and likely strengthen packing. Although we did not conduct a functional analysis of packing, a natural consequence of packing is escape from swallowing the bite, which may function to reinforce packing. For this reason, and because a relatively high number of children (37%) in our record reviews did not meet their goal to decrease packing in 8 weeks, a timely identification of an effective packing treatment may help limit this outcome. Children who did not meet goals for packing may require additional outpatient services, have longer than ideal mealtimes (e.g., >30 min), or require additional modifications to maintain clinical gains (e.g., avoid packed foods during meals). These results provide additional support for the use of a packing assessment model, which could decrease the time to effective treatment. This assessment and subsequent treatment evaluation had an average range of 6 days (range 4–9 days), and packing goals were met for all individuals.
This evaluation is a novel assessment model for packing, such that prior literature has not demonstrated a way to effectively assess packing. In practice, we typically select a packing intervention by means of our clinical judgment, rather than using empirical support. For practitioners, this can be time-consuming, especially considering packing may not develop until later in a child’s evaluation. We were able to assess and intervene on packing over the course of 6 days on average, targeting multiple variables affecting packing, a notable advantage of this assessment model. For Jack and Gus, we identified multiple variables related to packing. Jack did not pack when he was presented with highly preferred foods and lower texture foods. Had we presented him with only highly preferred foods or with only lower texture foods, it is likely he would not have packed any bites. Doing so, however, would have interfered with his goals to eat a wide variety of foods and provided him with foods well below his skill level for chewing. Considering Jack had the ability to consume regular-texture foods, presenting only lower texture foods in meals would not have been age-appropriate or in line with his eating skills. Similarly, for Gus, selecting one variable to treat would have resulted in him being presented with all foods at a smaller bite size than necessary and avoiding foods that were moderately difficult to chew, unnecessarily restricting his eating. Avoiding moderate-effort foods would also not have been a complete intervention. Future research could continue to evaluate interventions targeting multiple variables to treat packing using this model, as they could be beneficial for practitioners in reducing the latency to identify an effective treatment. As previously noted, considering the percentage of children for whom packing was problematic in the intensive feeding program, complex and nuanced interventions are needed, and these could be derived from more sensitive assessments.
The texture, bite or bolus, preference, and effort assessments all yielded valuable data in terms of treatment identification. That is, in each of those assessments, we were able to identify low levels of packing in at least one of the test conditions. The results of the texture assessment replicate the findings of previous research (e.g., Patel et al., 2005), such that lower levels of packing were observed when the child was presented with manipulated textures; thus, this validates the practicality of the texture assessment. Additionally, the results were validated during Jack and Nina’s treatment evaluations. The results of the bite- or bolus-size assessment, although inconsistent, generated important information for Danny, Gus, and Nina. Although Danny began to swallow under the control condition, our continued investigation of the data led us to speculate that effort or food preference may have played a role in his packing. Although Gus’s results were variable, the slight differentiation between the control and test conditions suggested that bite size played a role in his packing, and this was validated in his treatment evaluation. Notably, Gus was often sick or had trouble staying awake during late afternoon sessions, which could have contributed to the variability in his levels of packing. Finally, for Nina, no differentiation was observed during the bite-size assessment when presented with regular-texture bites. However, although packing eventually decreased across all bolus sizes, this still provided us with important information in terms of determining an appropriate bolus size for lower textures.
The results of the preference assessment indicated that food preference played a role in Jack’s packing, and this was validated during his treatment evaluation. Additionally, this replicates the findings of prior research (e.g., Buckley & Newchok, 2005). The results of the effort assessment indicated that response effort played a role in Gus’s packing, and this was validated during his treatment evaluation. Although packing only moderate-effort foods was surprising, there are two possible explanations. First, the chewing assessment was a novel way to create an effort hierarchy. Future research could consider other ways to define effort and better refine the effort assessment, such as asking oral-motor therapists to assist with a hierarchy. Second, Gus was not exposed to the preference assessment; therefore, it is possible that the moderate-effort foods he packed were also low-preferred foods.
Going forward, we need more data to validate the use of the demand and modified chaser assessments in practice. The participants exposed to the demand and modified chaser assessments did not demonstrate differentiated responding. By decreasing the demand, we wanted to determine if presenting fewer bites would make eating less aversive; however, at least for these participants, that did not appear to be the case. In addition, we used a modified chaser procedure, which may not be an effective treatment for packing. Typically, chasers are presented while the bolus is still in the mouth, rather than after the bite is swallowed. One potential concern with the chaser procedure is that, if effective, it is possible that the child will only swallow with the aid of a liquid. To avoid that possible outcome, we used a modified chaser that could clear any residue or taste from the mouth without occurring simultaneously with swallowing the bolus. Perhaps, future research could consider a more typical application of a chaser (i.e., following bite acceptance, rather than a swallow) or evaluate other ways to lower demand.
To assess preference, a pictorial preference assessment was used. This is potentially problematic in that it is unclear if selection of preference based on a picture corresponds to preference based on consuming the food. For the participants in this study, this was unknown. In the initial paired-stimulus preference assessment, we observed a hierarchy for only two participants: Jack and Nina. Thus, the pictorial preference assessment was conducted, although we cannot be sure of its accuracy. A pictorial assessment was used to limit potential difficulties with presenting a bite of the food selected in a paired-choice arrangement. Should the participant not accept the food, a decision must be made to permit escape or implement escape extinction, and if the participant packed the food, escape (i.e., removing the food from the mouth) would be necessary to complete the preference assessment, which would have introduced a novel contingency for packing. This difficulty may be unique when conducting preference assessments for children who refuse to eat or are selective, and future research could thoroughly evaluate the contributions of a pictorial preference assessment.
Danny and Jack’s continued low levels of packing during the bite-size assessment and treatment evaluation, respectively, should be noted. It is possible that, due to repeated exposure to commonly packed foods, mouth cleans generalized across foods. Due to sudden decreases in packing, generalization was tested by probing new, similar foods during the evaluations. For Danny, new vegetables and proteins were probed, and for Jack, new vegetables were probed, because each of their commonly packed foods primarily belonged to those food groups. Both Danny and Jack continued to swallow new vegetables, but Danny continued to pack the proteins. Due to parental request, packing assessments were discontinued so the clinical team could proceed with targeting other clinically problematic responses. As a result, it is unclear if bite size was the only variable related to packing proteins. Future research could consider if repeated exposure led to reduced levels of packing. That is, will packing cease due to repeated exposure, and if so, how long must exposure occur before packing decreases? For Jack and Danny, the preassessment conditions were in place for three sessions, and packing occurred at problematic levels for 100% of bites for both participants. It is not clear if further exposure would have eventually been effective, although the concern of delaying an effective treatment is still valid.
It may have been beneficial to conduct the effort or preference assessment to more clearly identify whether the difficulty to chew proteins or preference for vegetables affected levels of packing.
These results notwithstanding, a limitation of the current investigation is the lack of maintenance, generalization data, and social validity data obtained. It is unknown whether low levels of packing continued following each participant’s admission or whether the participants’ caregivers found the assessments and selected treatments to be socially acceptable. During Danny’s bite-size assessment, his mother expressed interest in discontinuing the packing assessments before we could run additional assessments or select an intervention. This could be due to evaluating each food in separate sessions, which could have further delayed treatment identification. With all other participants, all commonly packed foods were evaluated together, which might have been more efficient. It would have been beneficial to collect social validity data to identify the nonpreferred aspects of the assessment that led to this decision, although satisfaction questionnaires provided to all caregivers at the end of their child’s admission generated scores of an average of 4.7 out of 5, which indicated that they were mostly satisfied with their overall admission process. Future research could consider obtaining caregiver scores of overall satisfaction with assessments and treatment conditions, the delay to effective treatment, and the assessment and treatment process.
Due to the lack of discriminative stimuli correlated with the conditions in each assessment, it is possible that the participants had difficulties discriminating between conditions. That is, when differentiation was not observed in a particular assessment, it was not considered for intervention. Pairwise comparisons could have been used to limit this possibility. However, for two participants, experimental control was demonstrated for the intervention, suggesting that the assessment was valid. For Jack, mouth cleans generalized following exposure to the intervention based on the assessment results, following a stable baseline, suggesting that the intervention may have been on the right track.
Additional limitations of the current study pertain to the IOA and treatment integrity evaluations. During Nina’s treatment evaluation sessions, a second observer was present during only 23.1% of sessions. Due to staffing, it was not feasible to obtain IOA on the majority of sessions conducted. Additionally, although we did calculate treatment integrity for the preassessment treatment components, we did not assess integrity of the actual packing treatment components (e.g., ensuring the proper textures, bite sizes, or correct preferred or nonpreferred foods were presented). However, all therapists were highly trained on food preparation (e.g., texture manipulation); were familiar with appropriate textures, bite sizes, and so on; and were required to pass evaluation of these skills by the supervising BCBA.
Another potential limitation is the lack of exposure to all assessments for participants. It may have been the case that additional variables related to packing would have been identified had each participant been exposed to all assessments. Generally, this was approached from a clinical perspective with the goal of intervening on packing in a timely manner and considering the relevance and safety of each assessment working within an interdisciplinary team. For example, from an ethical standpoint, it would be a potential safety risk to assess bite size of regular-texture foods for a child with limited chewing skills. Thus, it is possible that additional variables related to packing were missed, and it is unknown if those variables would have led to an effective intervention.
The assessments conducted for all participants (i.e., demand and bite- or bolus-size manipulation) were deemed clinically relevant. That is, asking the child to eat fewer bites or smaller amounts would continue to expose the child to the foods without drastically changing the food’s appearance. The texture assessment was conducted for all but one participant, as this is a known intervention for packing (Patel et al., 2005), and one participant did not demonstrate differential responding to texture in the preassessment intervention. The effort, preference, and chaser assessments were not conducted for participants if one or more assessments yielded results that could inform treatment. This may be more similar to decision-making in home- or school-based practice, as the work will likely be done in a less controlled environment and assessments must be conducted in a thorough yet timely manner. Conducting only those assessments most relevant for an individual client, or not conducting additional assessments (if packing can be reduced with more simple interventions), is likely to happen in practice. Future research evaluating these procedures in a home or school setting could be useful to practitioners.
From a clinical perspective, taking a step back in treatment (e.g., reducing texture or bite size) may be viewed as disadvantageous. Jack and Nina had the ability to chew and swallow regular-texture foods; however, some or all of their foods were decreased to wetground texture. Due to these reductions in effort, each participant was eventually exposed to additional treatment procedures to increase either texture or bite size. Future research could consider including additional treatment procedures (e.g., Shore, Babbitt, Williams, Coe, & Snyder, 1998; Vollmer, Iwata, Zarcone, Smith, & Mazaleski, 1993) to further progress in treatment and maximize eating skills in a mealtime setting.
Although these pretreatment assessments are a first step at assessing packing and identifying more individualized interventions, there is more work to be done in this line of research. Applying this model to other forms of food refusal, such as expelling, coughing, gagging, or emesis, could expand upon this research. Similar antecedent manipulations could aid in identifying conditions under which appropriate mealtime behaviors occur (i.e., swallowing quickly without excessive gagging or coughing). The utility of this method as a standardized assessment approach to quickly evaluate and intervene on varying topographies of food refusal may be clinically advantageous.
These results add to the growing literature on the treatment of packing in pediatric feeding disorders. This model could be used to identify variables related to packing and inform treatment design, resulting in a more individualized treatment package. Currently, although interventions for packing have been identified, it is sometimes difficult to determine which should be selected, and multiple options may have to be evaluated. This model could aid in targeting multiple variables related to packing. More importantly, reductions in packing in turn will increase food consumption, as well as decrease mealtime duration. Considering these results, practitioners could consider this model as an aid in treatment selection to reduce packing.
Compliance with Ethical Standards
Conflict of Interest
The first author received financial support from the aforementioned pediatric feeding disorders program to attend a national conference to present these data. Additionally, both authors are employed by this program.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Addison LR, Piazza CC, Patel MR, Bachmeyer MH, Rivas KM, Milnes SM, Oddo J. A comparison of sensory integrative and behavioral therapies as treatment for pediatric feeding disorders. Journal of Applied Behavior Analysis. 2012;45:455–471. doi: 10.1901/jaba.2012.45-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero CSW, Schlereth GJ, Rubio EK, Taylor T. A comparison of two physical guidance procedures in the treatment of pediatric food refusal. Behavioral Interventions. 2013;28:261–280. doi: 10.1002/bin.1373. [DOI] [Google Scholar]
- Bourret J, Vollmer TR, Rapp JT. Evaluation of a vocal mand assessment and vocal mand training procedures. Journal of Applied Behavior Analysis. 2004;37:129–144. doi: 10.1901/jaba.2004.37-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley SD, Newchok DK. An evaluation of simultaneous presentation and differential reinforcement with response cost to reduce packing. Journal of Applied Behavior Analysis. 2005;38:405–409. doi: 10.1901/jaba.2005.71-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groskreutz MP, Graff RB. Evaluating pictorial preference assessment: The effect of differential outcomes on preference assessment results. Research in Autism Spectrum Disorders. 2009;3:113–128. doi: 10.1016/j.rasd.2008.04.007. [DOI] [Google Scholar]
- Gulotta CS, Piazza CC, Patel MR, Layer SA. Using food redistribution to reduce packing in children with severe food refusal. Journal of Applied Behavior Analysis. 2005;38:39–50. doi: 10.1901/jaba.2005.168-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudford OC, Martin NT, Hui JKY, Taylor SA. Assessing observer accuracy in continuous recording of rate and duration: Three algorithms compared. Journal of Applied Behavior Analysis. 2009;42:527–539. doi: 10.1901/jaba.2009.42-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MR, Piazza CC, Layer SA, Coleman R, Swartzwelder DM. A systematic evaluation of food textures to decrease packing and increase oral intake in children with pediatric feeding disorders. Journal of Applied Behavior Analysis. 2005;38:89–100. doi: 10.1901/jaba.2005.161-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza CC, Fisher WW, Brown KA, Shore BA, Patel MR, Katz RM, et al. Functional analysis of inappropriate mealtime behaviors. Journal of Applied Behavior Analysis. 2003;36:187–204. doi: 10.1901/jaba.2003.36-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza CC, Milnes SM, Shalev RA. A behavior-analytic approach to the assessment and treatment of pediatric feeding disorders. In: Roane HS, Ringdahl JL, Falcomata TS, editors. Clinical and organizational applications of applied behavior analysis. London: Elsevier; 2015. pp. 69–94. [Google Scholar]
- Piazza CC, Patel MR, Santana CM, Goh HL, Delia MD, Lancaster BM. An evaluation of simultaneous and sequential presentation of preferred and nonpreferred food to treat food selectivity. Journal of Applied Behavior Analysis. 2002;35:259–270. doi: 10.1901/jaba.2002.35-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio EK, Borrero CSW, Taylor T. Use of a side deposit to increase consumption in children with food refusal. Behavioral Interventions. 2015;30:231–246. doi: 10.1002/bin.1404. [DOI] [Google Scholar]
- Sevin BM, Gulotta CS, Sierp BJ, Rosica LA, Miller LJ. Analysis of response covariation among multiple topographies of food refusal. Journal of Applied Behavior Analysis. 2002;35:65–68. doi: 10.1901/jaba.2002.35-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore BA, Babbitt RL, Williams KE, Coe DA, Snyder A. Use of texture fading in the treatment of food selectivity. Journal of Applied Behavior Analysis. 1998;31:621–633. doi: 10.1901/jaba.1998.31-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silbaugh, B. C., Swinnea, S., & Penrod, B. (2017). Synthesis of applied behavior analytic interventions for packing in pediatric feeding disorders. Behavior Modification. Advance online publication. 10.1177/0145445517724541. [DOI] [PubMed]
- Vaz PCM, Piazza CC, Stewart V, Volkert VM, Groff RA, Patel MR. Using a chaser to decrease packing in children with feeding disorders. Journal of Applied Behavior Analysis. 2012;45:97–105. doi: 10.1901/jaba.2012.45-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer TR, Iwata BA, Zarcone JR, Smith RG, Mazaleski JL. The role of attention in the treatment of attention-maintained self-injurious behavior: Noncontingent reinforcement and differential reinforcement of other behavior. Journal of Applied Behavior Analysis. 1993;26:9–21. doi: 10.1901/jaba.1993.26-9. [DOI] [PMC free article] [PubMed] [Google Scholar]