Abstract
Indirubin is an active component of Dang Gui Long Hui Wan, which has been used in traditional Chinese medicine to treat inflammatory diseases as well as for the prevention and treatment of human cancer, such as chronic myeloid leukemia. The therapeutic effects of indirubin analogs have been underestimated due to its poor water solubility and low bioavailability. To improve the solubility and bioavailability of indirubin analogs, we prepared a mixed micellar formulation with Kolliphor® EL and Tween 80 as surfactants, and PEG 400 as a co-surfactant, followed by complexation with (2-hydroxyproply)-β-cyclodextrin at appropriate ratios. Overall, improving the solubility and skin penetration of indirubin analogs can increase clinical efficacy and provide maximum flux through the skin.
Keywords: mixed micellar formulation, transdermal drug delivery, solvent-free delivery system, lipophilic drugs
1. Introduction
The synthesis of novel compounds based on combinatorial chemistry is important for the improvement of therapeutic activity and industrialization [1]. However, approximately 40% of chemical compounds are limited in their pharmacological activities due to poor water solubility [2]. Although polar organic solvents such as dimethyl sulfoxide (DMSO) have been used for drug solubilization [3], they are limited in their usage in the pharmaceutical market due to biosafety concerns and harmful side effects on human health [4,5].
In recent years, numerous solvent-free delivery systems such as topical ointments, gels, and creams as well as nanocarriers such as nanoparticles, niosomes, liposomes, and mixed micellar formulations were developed to resolve the problem of poorly water-soluble drugs [6,7]. Mixed micelles are fabricated according to the physicochemical properties of the drugs and the compatibility between the micelle core and the drug molecules [7,8,9]. This fabricated micelle structure affords a high solubilization capacity of the bioactive compounds and exhibits a controlled release from the mixed micellar formulation [7]. The development of a mixed micellar formulation provides advantages to a transdermal drug delivery system [10,11]. First, the solubility of both lipophilic and hydrophilic drugs can be increased through microemulsification [10]. Second, microemulsion surfactants, performing as permeation enhancers, can weaken the structure of the stratum corneum (SC) and increase the flux of drugs through the skin [10,12]. Third, drug release from the microemulsion can be enhanced because the affinity of the drug to the internal phase can be easily modified [13]. The choice of an appropriative vehicle for transdermal delivery is critical to improve bioavailability with a minimum dosage of drugs [14]. The most important criteria for the selection of all the mixed micellar formulation components is that all excipients should be pharmaceutically acceptable for oral administration or topical application, depending upon the requirements, and fall under the generally-regarded-as-safe category by the Food and Drug Administration (FDA) [15,16]. Therefore, in this study, we formulated the poorly water-soluble drugs by screening the surfactants and co-surfactants in the safe category, followed by complexation with (2-hydroxyproply)-β-cyclodextrin (HP-β-CD) at 1:1 ratios. HP-β-CD is a family of cyclic oligosaccharides with a hydrophilic outer surface and a lipophilic center cavity [17]. Considering the structure of HP-β-CD, we postulated that the interior cavity of HP-β-CD would encapsulate most of the lipophilic functional groups in KY19382, while the hydrophilic hydroxyl groups at the external surface of the inclusion complex would remain exposed to the environment. HP-β-CD enhances the formulation and stabilization of poorly water-soluble drugs by binding to a drug to form a 1:1 inclusion complex [18]. The formulation was characterized by its ability to form a mixed micellar based on solubility, droplet size, polydispersity, thermodynamic stability, bioavailability, and its safety for topical application. Improving the solubility of indirubin analogs could increase clinical efficacy and could reduce the dosage required to achieve the same effect. Overall, through a series of in vitro and in vivo evaluations, we could successfully improve the solubility and efficiency of poorly water-soluble indirubin analogs by introducing a novel formulation.
2. Materials and Methods
2.1. Materials
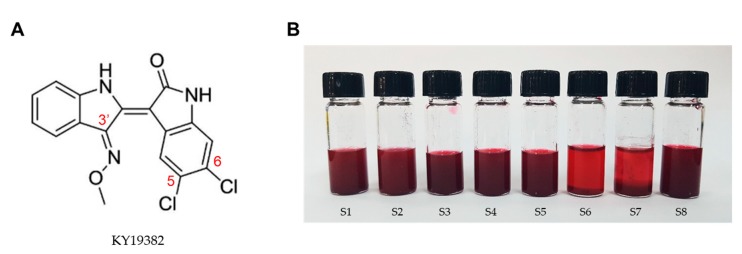
KY19382, 5, 6-dichloroindirubin-3′-methoxime (Figure 1a), was synthesized and supplied by Dr. G.H. Han (Yonsei University, Seoul, Korea) [19]. (2-hydroxyproply)-β-cyclodextrin (HP-β-CD), Kolliphor® EL (Polyoxyl castor oil, pH range 6.0–8.0), Tween 20, Tween 80, and polyethylene glycol (PEG) 400 were purchased from Sigma Aldrich (St. Louis, MO, USA). Propylene glycol was purchased from Junsei (Tokyo, Japan). Transcutol P (diethylene glycol monoethyl ether) was purchased from Merck Schuchardt (Hohenbrunn, Germany). All reagents used were analytical grade.
Figure 1.
Characterization and solubilization of KY19382. (A) Chemical structure of KY19382. (B) Solubilization of KY19382 in various vehicles at 25 °C.
2.2. Solubility Test
An excess amount of KY19382 containing HP-β-CD at a 1:1 ratio was tested for its solubility by adding 2 mL of vehicle, independently, in 5 mL-capacity glass vials, followed by mixing for 3 h with a vortex mixer. The mixture samples were centrifuged at 1000× g for 10 min to separate the undissolved chemicals. The supernatants were filtered with a 0.45 µm filter membrane, and the concentration of KY19382 was quantified using liquid chromatography–electrospray tandem mass spectrometry (LC-MS) methods. The KY19382 in samples was determined with a LC-MS system (Ultimate 3000 RS-LTQ Orbitrap XL; ThermoFisher Scientific, Waltham, MA, USA) using a C18 column (150 × 4.6 mm, 5 µm; ThermoFisher Scientific). The mobile phase contained 60% acetonitrile and 40% distilled water in 0.05% formic acid with a flow rate of 0.7 mL/min at 30 °C. Detection was conducted at a wavelength of 254 nm. The injection volume was 3 µL.
2.3. Construction of Phase Diagrams
Surfactant (Tween 80) and co-surfactant (PEG 400) were mixed in different weight ratios (1:2, 1:1, 2:1). For each phase diagram, Kolliphor® EL and specific surfactant/co-surfactant (Smix) ratios were mixed thoroughly in different volume ratios from 1:9 to 9:1 in each glass vial. Pseudoternary phase diagrams were developed using the aqueous titration method. The amount of water added varied in the range of 5% to 95% of the total volume. After each 5% addition of water to the Kolliphor® EL: Smix mixture, transparency and easily flowable condition ratios were recorded. For each water: Kolliphor® EL: Smix ratio, a pseudoternary phase diagram was constructed using CHEMIX School 3.51 software.
2.4. Droplet Size and Polydispersity
An aliquot of chosen formulations was diluted with 150 mL water with stirring. The droplet size and zeta potential of the diluted formulations were determined with a zetasizer (ELS-2000ZS; Otsuka Electronics, Osaka, Japan) equipped with a 4.0 mW He-Ne red laser (633 nm) at 25 °C. Experiments were repeated three times. The zetasizer measured the potential, which ranged from −0.12 to 0.12 mV.
2.5. Viscosity
The viscosity of the formulations was determined using a Brookfield R/S plus rheometer (Brookfield Engineering, Middleborough, MA, USA) with a C50-1 spindle in triplicate at 25 °C.
2.6. Drug Release and Skin Permeation Tests
Drug release and skin permeation tests were performed using Franz Cell diffusion (Logan Instrument Corp., Somerset, NJ, USA). Formulated-indirubin analogs were applied onto human artificial skin (Strat-M™ Membrane Transdermal Diffusion Test Model, Millipore, Billerica, MA, USA) composed of polyethersulfone and polyolefin, then placed into the donor compartment of the Franz cell. The receptor compartment consisted of PBS with 20% methanol. A total of 1 mL of each sample was dropped onto human artificial skin until the formulation covered a diffusion area of 2 × 2 cm2. Samples were analyzed at intervals of 0, 1, 2, 3, 4, 5, 6, 8, 10, and 12 h, then quantified using the LC-MS system.
2.7. Transmission Electron Microscopy (TEM)
The morphology of micelles was photographed using a transmission electron microscope (Hitachi 7600, Tokyo, Japan) at an accelerating voltage of 100 kV. Briefly, one drop of nanoparticle dispersion was deposited onto a carbon-coated copper grid to form a thin liquid film. The grid was negatively stained immediately by adding a drop of 1% w/w phosphotungstic acid, followed by air-drying at room temperature for five minutes.
2.8. Thermodynamic Stability Study
The sealed formulations were stored at 25 and 4 °C for three months. Then, samples were collected once a month to examine the physical stability of the indirubin analog and emulsifying properties by LC-MS.
2.9. Statistical Analysis
Data are presented as the mean ± standard deviation (SD). Statistical analysis was performed using an unpaired two-tailed Student’s t test. Asterisks denote statistically significant differences (*, p < 0.05; **, p < 0.005; ***, p < 0.0005).
3. Results
3.1. Screening of the Mixed Micellar Formulation Components
KY19382, one of the indirubin analogs, had a backbone of 5,6-dichloroindirubin-3′-oxime, which was formed by a π-conjugated system (Figure 1A). To obtain the maximum drug-loading capacity, an excess amount of KY19382 containing HP-β-CD at 1:1 ratio tested the solubility in various oil, surfactant, and co-surfactants (Figure 1B and Figure S1).
The solubility of KY19382 was found to be highest in surfactants compared to oils. The solubility of KY19382 in Kolliphor® EL, Tween 80, and PEG 400 was relatively higher than other excipients (Table 1). Thus, Kolliphor® EL and Tween 80 as surfactants, and PEG 400 as a co-surfactant were selected for the development of the mixed micellar formulation.
Table 1.
Solubility of KY19382 in selected excipients.
| Function in Formulation | Vehicles | Solubility (mg/mL) | p-Value | |
|---|---|---|---|---|
| Oils | S1 | Olive oil | 0.83 ± 0.02 | 0.0312 |
| S2 | Sunflower oil | 1.35 ± 0.98 | 0.0182 | |
| Surfactants | S3 | Kolliphor® EL | 5.4 ± 0.95 | 0.0031 |
| S4 | Tween 20 | 4.58 ± 0.13 | 0.0269 | |
| S5 | Tween 80 | 4.92 ± 0.23 | 0.0005 | |
| Co-surfactants | S6 | Transcutol P | 1.15 ± 0.87 | 0.0443 |
| S7 | Propylene glycol | 0.25 ± 0.03 | 0.0052 | |
| S8 | PEG 400 | 3.1 ± 0.46 | 0.0003 |
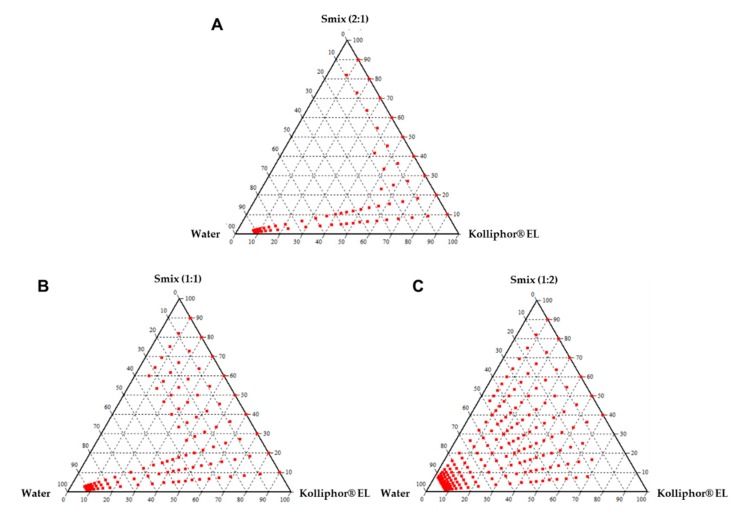
3.2. Construction of Pseudoternary Phase Diagrams
A phase diagram was constructed to identify the soluble regions and to optimize the concentration of the surfactant and co-surfactant in the mixed micellar formulation. A series of formulations at Tween 80/PEG 400 (Smix) ratios were prepared at 2:1, 1:1, 1:2 (v/v). Phase diagrams were constructed of different Kolliphor® EL and Smix ratios from 1:9 to 9:1 (Figure 2A–C). A narrow microemulsion area was observed at the Smix 2:1 (Figure 2A). When the co-surfactant was added with the surfactant in equal amounts, the transparent region increased in area as compared to the region in Smix 2:1 (Figure 2B). On further increasing the co-surfactant ratio, at Smix 1:2, the maximum transparent region was observed (Figure 2C). Hence, the optimal ratio of surfactant to co-surfactant was established to be 1:2 for a three-component mixed micellar formulation.
Figure 2.
Pseudoternary phase diagrams containing Kolliphor® EL, Tween 80:PEG 400 (Smix), and water. (A) Smix ratio 2:1, (B) Smix ratio 1:1, (C) Smix ratio 2:1.
3.3. The Characterization and Evaluation of Mixed Micellar Formulations
We constructed mixed micellar formulations containing increasing concentrations of Kolliphor® EL at a fixed Smix 1:2 ratio (Table 2). Incorporation of the indirubin analog in selective formulations including Kolliphor® EL, Tween 80, and PEG 400 from 50:16:34 (F5), 60:13:27 (F6), 70:10:20 (F7), 80:6:14 (F8), and 90:3:7 (F9) ratios significantly contributed to an increase in the solubility of KY19382 compared to its solubility in Kolliphor® EL only (Table 2). The droplet size decreased with increasing concentrations of Kolliphor® EL in the formulations, whereas viscosity tended to increase with increasing concentrations of Kolliphor® EL (Table 2). We measured the droplet size of the mixed micellar formulation as 41.5 nm (F8) and 29.3 nm (F9), and the zeta potential as −20.38 mV (F8) and −20.99 mV (F9) (Table 2).
Table 2.
Solubility, droplet size, viscosity, and zetapotential for the mixed micellar formulations.
| Code | Formulation Composition (Kolliphor® EL:Tween 80:PEG400) | Solubility (mg/mL) | Droplet size (nm) | Viscosity (mPas) | Zetapotential (mV) |
|---|---|---|---|---|---|
| F1 | 10:30:60 | 2.99 ± 0.20 | 1525.7 ± 10.6 | 23.33 ± 0.85 | −5.14 ± 0.14 |
| F2 | 20:26:54 | 3.58 ± 0.13 | 921.3 ± 2.6 | 44.46 ± 1.35 | −6.87 ± 0.15 |
| F3 | 30:23:47 | 3.81 ± 0.04 | 624.9 ± 9.2 | 59.12 ± 1.66 | −7.23 ± 0.17 |
| F4 | 40:20:40 | 4.11 ± 0.20 | 479.4 ± 3.8 | 65.07 ± 1.35 | −6.94 ± 0.16 |
| F5 | 50:16:34 | 5.67 ± 0.23 | 332.3 ± 3.8 | 72.72 ± 1.17 | −7.99 ± 0.18 |
| F6 | 60:13:27 | 6.86 ± 0.12 | 264.9 ± 4.2 | 88.85 ± 0.98 | −9.72 ± 0.20 |
| F7 | 70:10:20 | 7.59 ± 0.23 | 183.8 ± 2.2 | 91.39 ± 0.56 | −10.83 ± 0.22 |
| F8 | 80:6:14 | 7.69 ± 0.17 | 41.5 ± 1.7 | 98.3 ± 0.91 | −20.38 ± 0.32 |
| F9 | 90:3:7 | 6.88 ± 0.07 | 29.3 ± 1.0 | 99.52 ± 1.27 | −20.99 ± 0.33 |
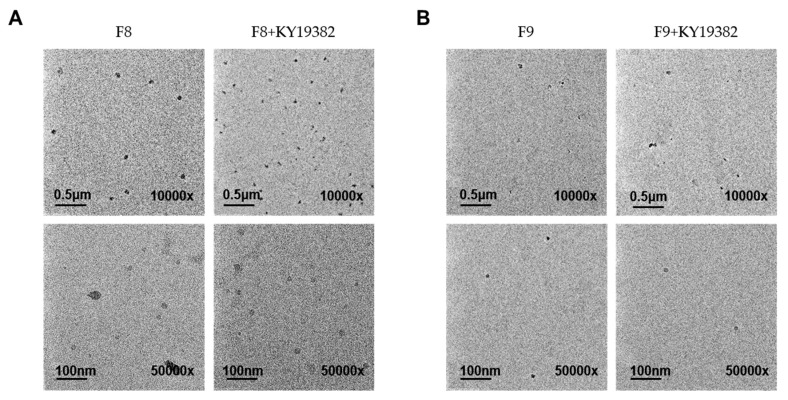
TEM images of blank F8, F9, and KY19382-loaded F8, F9 formulations displayed the formation of discrete and monodispersed micelles (Figure 3A,B). The images obtained from F8 and F9 formulations were similar to those prepared with KY19382 (Figure 3A,B). Furthermore, drug loading did not influence the size of the nanoparticles, and showed no apparent signs of aggregation (Figure 3A,B).
Figure 3.
Transmission electronic microscopy (TEM) images of the mixed micellar formation from the (A) F8 and (B) F9 formulation with or without KY19382. Formulation details are presented in Table 2. The scale bars are 0.5 μm (10,000×) and 100 nm (50,000×), respectively.
Therefore, the selected F8 and F9 formulations were appropriated to the mixed micellar formulation with a particle size of <100 nm in the stability of the mixed micellar formulation. Based on the above results, the mixed micellar formulations of F8 and F9 possessed the optimal emulsifying properties among all examined formulations. In addition, the mixed micellar formulations F8 and F9 may increase skin permeability due to the small droplet size, and may be more convenient for administration onto the skin due to their high viscosity.
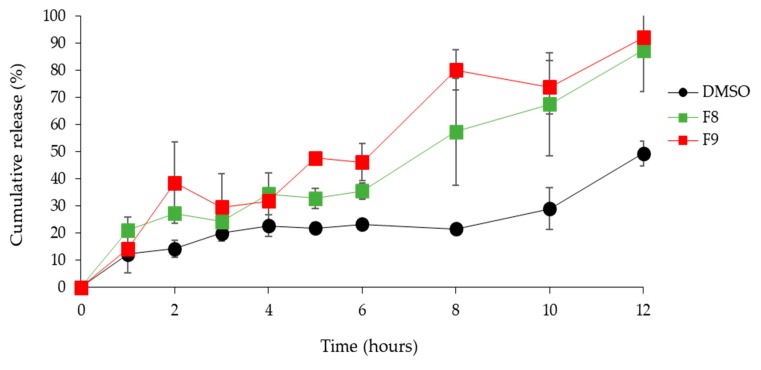
3.4. Skin Permeation Study
Skin permeation studies showed a significant increase in the KY19382 permeation in the F8 and F9 formulations compared with that of the permeation in DMSO (Figure 4), indicating that the transdermal delivery of KY19382 from the mixed micellar formulation played a key role in the enhancement of both the penetration and release rate.
Figure 4.
KY19382 transdermal permeation profiles obtained after application of different mixed micellar formations or KY19382 in DMSO to artificial skin. Formulation details are presented in Table 2. Data are presented as the mean ± standard deviation (SD).
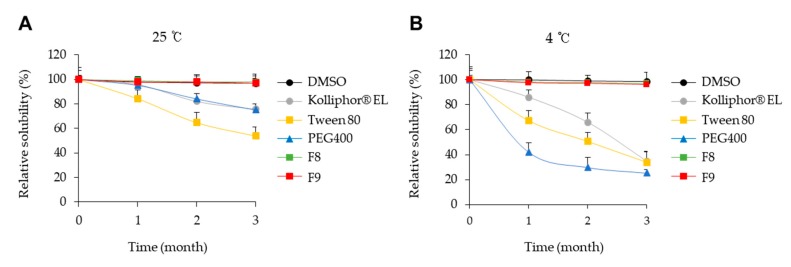
3.5. Thermodynamic Stability of the Mixed Micellar Formulations
To confer a long shelf-life to the mixed micellar formulation, as compared to ordinary emulsion, aliquots of KY19382 in DMSO, Kolliphor® EL, Tween 80, PEG 400, and mixed micellar formulation (F8, F9) were stored at 25 °C and 4 °C for three months. KY19382 was thermodynamically stable in the optimized mixed micellar formulation; therefore, it maintained physical stability without precipitation for up to three months of storage at 4 °C and 25 °C (Figure 5A,B). However, the stability of KY19382 was significantly reduced in Kolliphor® EL, Tween 80, and PEG 400 after storage at 4 °C (Figure 5B). KY19382 formulated with individual excipients such as Kolliphor® EL, Tween 80 and PEG 400 was unstable, and the drug solution had a tendency to return to its equilibrium state via precipitation (Figure 5A,B). To test whether these results were due to chemical interactions between KY19382 and excipients, we assessed the chemical stability of the formulations. The degradation products were not monitored in a validated HPLC assay (Figure S2). Altogether, these findings indicated that the mixed micellar formulations, including Kolliphor® EL, Tween 80 and PEG 400, had thermodynamic stability in comparison with formulations made with the individual excipients.
Figure 5.
Time evolution of the concentration of KY19382 in F8 and F9 formulations. Concentrations of KY19382 at 25 °C (A) and 4 °C (B).
4. Discussion
Here, we formulated a mixed micellar based delivery system to improve the solubility of the poorly water-soluble indirubin analog. Indirubin analogs have one hexameric ring formed by intramolecular hydrogen bonds [20,21]. Therefore, the KY19382 molecule was stable and poorly water-soluble.
There are various systems, including solid dispersion, liposomes, polymer micelles, nanoemulsions, and cyclodextrin that are developed for the enhancement of drug solubility [22,23]. Considering the molecular characteristics of KY19382, we selected HP-β-CD as a solubility enhancer from a list of FDA-approved substances. However, HP-β-CD is limited in its penetration into lipophilic membranes [24]. To overcome this bioavailability problem, we optimized a mixed micellar formulation composed of HP-β-CD with various oils, surfactants, and co-surfactants. The PEG 400 molecule opens two parallel helical bonds [25] so that the indirubin molecule complex and HP-β-CD are incorporated into the coiling chain and form a molecular dispersion. Meanwhile, the intramolecular hydrogen bond was activated upon dissolving the indirubin analog in a mixed micellar formulation, so exchange of a hydrogen bond with PEG 400 may occur [26]. Tween 80, which is derived from oleic acid, contributes to the fluidity increments of the SC lipids, enhancing the permeability of the skin for drugs [27,28]. In addition, the presence of monooleate, such as Kolliphor® EL, in the formulation further improves bioavailability by affecting the drug absorption in the skin [29].
A mixed micellar formulation is a function of system composition [30,31]. The optimal ratio of the surfactant and co-surfactant is a major determining factor that influences the phase properties, droplet size, and position of the microemulsion region [30,31]. When Tween 80 was added with PEG 400 in the 1:2 ratio, a higher transparent region was observed as compared to the 1:1 and 2:1 ratios, perhaps due to the further reduction in the interfacial tension and increased fluidity of the interface at Smix 1:2. It was also observed that increasing the Kolliphor® EL ratio led to an increased region of mixed micellar formulation. The concentration of Kolliphor® EL is a major factor influencing the phase properties, droplet size, and position of the liquid crystalline region [32]. The high loading capacity of the formulation components can be attributed to the unique structural organization of the microemulsion system [33,34]. We confirmed that the droplet size of mixed micellar formulation was 41.5 nm (F8) and 29.3 nm (F9), and the zeta potential as −20.38 mV (F8) and −20.99 mV (F9). In general, the zeta potential value of ±30 mV is sufficient for the stability of a microemulsion [35].
The transdermal drug release rate is correlated with the flux values; therefore, a smaller droplet dimension and lower interfacial tension of the mixed micellar formulation is assumed to improved drug permeation [36,37]. Higher surfactant concentration causes an increase in the fluidity of the membrane, and eventually an increase in the permeability of the drug [38]. Therefore, it has been suggested that a dose-dependent increase in the permeability of the SC is responsible for the surfactant-induced permeability of drugs.
Mixed micellar formulations also present an advantage in storage stability [7]. KY19382 formulated with individual excipients such as Kolliphor® EL, Tween 80, and PEG 400 was unstable, and the drug solution had a tendency to return to its equilibrium state via precipitation after 3 months of storage at 4 °C and 25 °C. Due to this instability, additional stabilization was required by mixed micellar formulation. After KY19382 was formulated, it showed thermodynamic stability and precipitation was not observed in the optimized formulation after 3 months of storage at 4 and 25 °C.
In conclusion, based on a series of in vitro and in vivo evaluations, we demonstrated a mixed micellar formulation which is an effective approach for the dissolution of poorly water-soluble drugs. A mixed micellar formulation promotes bioavailability and permeability across cellular lipid membranes with smaller droplets. Although further detailed examinations are required, the findings of this study suggest that developing a mixed micellar formulation is a promising method to enhance transdermal drug delivery while reducing the potential risk of side effects.
5. Conclusions
A mixed micellar formulation is a promising approach for the enhancement of transdermal drug delivery. In the present study, we developed a mixed micellar formulation that included Kolliphor® EL, Tween 80, and PEG 400 for efficient administration of poorly water-soluble compounds by an enhancement of their solubility and bioavailability. The mixed micellar formulation could provide the excipients with high flexibility at the optimum viscosity, as the formulations retained their efficacies after phase transition. In addition, the mixed micellar formulation enhanced transdermal delivery with a nano-sized droplet. All the excipients for the mixed micellar formulation were pharmaceutically acceptable for topical application based on the safety guidelines of the FDA. Therefore, the mixed micellar formulation developed in this study could be a promising approach for human dermal delivery of poorly water-soluble drugs.
Supplementary Materials
The following are available online at https://www.mdpi.com/1999-4923/12/2/175/s1, Figure S1: Schematic representation of the mechanism of a mixed micellar formulations, Figure S2: HPLC chromatograms of KY19382 in DMSO, Kolliphor® EL, Tween 80, and PEG400.
Author Contributions
Conceptualization, S.H.S. and K.T.O.; Data curation, S.H.S.; Formal analysis S.H.S., Y.J. and J.L.; Investigation, S.H.S.; Project administration, S.H.S.; Supervision, S.-J.H. and K.-Y.C.; Writing original draft, S.H.S. and K.-Y.C.; Writing review and editing, E.K. and S.-J.H.; Funding acquisition, K.-Y.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant from the National Research Foundation (NRF), the Ministry of Information and Science and ICT of Korea; A Mid-Career Researcher Program National Research Lab (2019R1A2C3002751).
Conflicts of Interest
K.-Y.C. is an inventor on a patent application for liquid crystalline nanoparticles for indirubin derivatives including KY19382, which have been licensed to CK Biotechnology Inc., a company headquartered in Seoul, Korea.
References
- 1.Schreiber S.L. Target-oriented and diversity-oriented organic synthesis in drug discovery. Science. 2000;287:1964–1969. doi: 10.1126/science.287.5460.1964. [DOI] [PubMed] [Google Scholar]
- 2.Savjani K.T., Gajjar A.K., Savjani J.K. Drug solubility: Importance and enhancement techniques. ISRN Pharm. 2012;2012:195727. doi: 10.5402/2012/195727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tetko I.V., Novotarskyi S., Sushko I., Ivanov V., Petrenko A.E., Dieden R., Lebon F., Mathieu B. Development of dimethyl sulfoxide solubility models using 163,000 molecules: Using a domain applicability metric to select more reliable predictions. J. Chem. Inf. Model. 2013;53:1990–2000. doi: 10.1021/ci400213d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galvao J., Davis B., Tilley M., Normando E., Duchen M.R., Cordeiro M.F. Unexpected low-dose toxicity of the universal solvent DMSO. FASEB J. 2014;28:1317–1330. doi: 10.1096/fj.13-235440. [DOI] [PubMed] [Google Scholar]
- 5.Dangol M., Yang H., Li C.G., Lahiji S.F., Kim S., Ma Y., Jung H. Innovative polymeric system (IPS) for solvent-free lipophilic drug transdermal delivery via dissolving microneedles. J. Control. Release. 2016;223:118–125. doi: 10.1016/j.jconrel.2015.12.038. [DOI] [PubMed] [Google Scholar]
- 6.Goke K., Lorenz T., Repanas A., Schneider F., Steiner D., Baumann K., Bunjes H., Dietzel A., Finke J.H., Glasmacher B., et al. Novel strategies for the formulation and processing of poorly water-soluble drugs. Eur. J. Pharm. Biopharm. 2017;126:40–56. doi: 10.1016/j.ejpb.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Li X., Zhang Y., Fan Y., Zhou Y., Wang X., Fan C., Liu Y., Zhang Q. Preparation and evaluation of novel mixed micelles as nanocarriers for intravenous delivery of propofol. Nanoscale Res. Lett. 2011;6:275. doi: 10.1186/1556-276X-6-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y., Li X., Zhou Y., Wang X., Fan Y., Huang Y., Liu Y. Preparation and evaluation of poly(ethylene glycol)-poly(lactide) micelles as nanocarriers for oral delivery of cyclosporine a. Nanoscale Res. Lett. 2010;5:917–925. doi: 10.1007/s11671-010-9583-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Funari S.S., Nuscher B., Rapp G., Beyer K. Detergent-phospholipid mixed micelles with a crystalline phospholipid core. Proc. Natl. Acad. Sci. USA. 2001;98:8938–8943. doi: 10.1073/pnas.161160998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karande P., Mitragotri S. Enhancement of transdermal drug delivery via synergistic action of chemicals. Biochim. Biophys. Acta. 2009;1788:2362–2373. doi: 10.1016/j.bbamem.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Akula S., Gurram A.K., Devireddy S.R. Self-Microemulsifying Drug Delivery Systems: An Attractive Strategy for Enhanced Therapeutic Profile. Int. Sch. Res. Notices. 2014;2014:964051. doi: 10.1155/2014/964051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alkilani A.Z., McCrudden M.T., Donnelly R.F. Transdermal Drug Delivery: Innovative Pharmaceutical Developments Based on Disruption of the Barrier Properties of the stratum corneum. Pharmaceutics. 2015;7:438–470. doi: 10.3390/pharmaceutics7040438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel P.V., Patel H.K., Panchal S.S., Mehta T.A. Self micro-emulsifying drug delivery system of tacrolimus: Formulation, in vitro evaluation and stability studies. Int. J. Pharm. Investig. 2013;3:95–104. doi: 10.4103/2230-973X.114899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Georgetti S.R., Casagrande R., Verri W.A., Lopez R.F., Fonseca M.J. Evaluation of in vivo efficacy of topical formulations containing soybean extract. Int. J. Pharm. 2008;352:189–196. doi: 10.1016/j.ijpharm.2007.10.037. [DOI] [PubMed] [Google Scholar]
- 15.Kalepu S., Nekkanti V. Insoluble drug delivery strategies: Review of recent advances and business prospects. Acta Pharm. Sin. B. 2015;5:442–453. doi: 10.1016/j.apsb.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rahman M.A., Hussain A., Hussain M.S., Mirza M.A., Iqbal Z. Role of excipients in successful development of self-emulsifying/microemulsifying drug delivery system (SEDDS/SMEDDS) Drug Dev. Ind. Pharm. 2013;39:1–19. doi: 10.3109/03639045.2012.660949. [DOI] [PubMed] [Google Scholar]
- 17.Tiwari G., Tiwari R., Rai A.K. Cyclodextrins in delivery systems: Applications. J. Pharm. Bioallied. Sci. 2010;2:72–79. doi: 10.4103/0975-7406.67003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stella V.J., He Q. Cyclodextrins. Toxicol. Pathol. 2008;36:30–42. doi: 10.1177/0192623307310945. [DOI] [PubMed] [Google Scholar]
- 19.Choi S., Kim H.Y., Cha P.H., Seo S.H., Lee C., Choi Y., Shin W., Heo Y., Han G., Lee W., et al. CXXC5 mediates growth plate senescence and is a target for enhancement of longitudinal bone growth. Life Sci. Alliance. 2019;10:2. doi: 10.26508/lsa.201800254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Efstathiou A., Gaboriaud-Kolar N., Smirlis D., Myrianthopoulos V., Vougogiannopoulou K., Alexandratos A., Kritsanida M., Mikros E., Soteriadou K., Skaltsounis A.L. An inhibitor-driven study for enhancing the selectivity of indirubin derivatives towards leishmanial Glycogen Synthase Kinase-3 over leishmanial cdc2-related protein kinase 3. Parasit. Vectors. 2014;7:234. doi: 10.1186/1756-3305-7-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leclerc S., Garnier M., Hoessel R., Marko D., Bibb J.A., Snyder G.L., Greengard P., Biernat J., Wu Y.Z., Mandelkow E.M., et al. Indirubins inhibit glycogen synthase kinase-3 beta and CDK5/p25, two protein kinases involved in abnormal tau phosphorylation in Alzheimer’s disease. A property common to most cyclin-dependent kinase inhibitors? J. Biol. Chem. 2001;276:251–260. doi: 10.1074/jbc.M002466200. [DOI] [PubMed] [Google Scholar]
- 22.Yang M., Gong W., Wang Y., Shan L., Li Y., Gao C. Bioavailability Improvement Strategies for Poorly Water-Soluble Drugs Based on the Supersaturation Mechanism: An Update. J. Pharm. Pharm. Sci. 2016;19:208–225. doi: 10.18433/J3W904. [DOI] [PubMed] [Google Scholar]
- 23.Wu L., Qiao Y., Wang L., Guo J., Wang G., He W., Yin L., Zhao J. A Self-microemulsifying Drug Delivery System (SMEDDS) for a Novel Medicative Compound Against Depression: A Preparation and Bioavailability Study in Rats. AAPS Pharm. Sci. Tech. 2015;16:1051–1058. doi: 10.1208/s12249-014-0280-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tinwalla A.Y., Hoesterey B.L., Xiang T.X., Lim K., Anderson B.D. Solubilization of thiazolobenzimidazole using a combination of pH adjustment and complexation with 2-hydroxypropyl-beta-cyclodextrin. Pharm. Res. 1993;10:1136–1143. doi: 10.1023/A:1018908032686. [DOI] [PubMed] [Google Scholar]
- 25.Franco R.W.A., Brasil C.A., Mantovani G.L., Azevedo E.R., Bonagamba T.J. Molecular Dynamics of Poly(Ethylene Glycol) Intercalated in Clay, Studied Using (13)C Solid-State NMR. Materials. 2012;6:47–64. doi: 10.3390/ma6010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen Z.Q., Liu Y., Zhao J.H., Wang L., Feng N.P. Improved oral bioavailability of poorly water-soluble indirubin by a supersaturatable self-microemulsifying drug delivery system. Int. J. Nanomedicine. 2012;7:1115–1125. doi: 10.2147/IJN.S28761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mittal A., Sara U.V., Ali A., Aqil M. The effect of penetration enhancers on permeation kinetics of nitrendipine in two different skin models. Biol. Pharm. Bull. 2008;31:1766–1772. doi: 10.1248/bpb.31.1766. [DOI] [PubMed] [Google Scholar]
- 28.Som I., Bhatia K., Yasir M. Status of surfactants as penetration enhancers in transdermal drug delivery. J. Pharm. Bioallied Sci. 2012;4:2–9. doi: 10.4103/0975-7406.92724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Erdal M.S., Özhan G., Mat M.C., Özsoy Y., Güngör S. Colloidal nanocarriers for the enhanced cutaneous delivery of naftifine: Characterization studies and in vitro and in vivo evaluations. Int. J. Nanomedicine. 2016;11:1027–1037. doi: 10.2147/IJN.S96243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Azeem A., Rizwan M., Ahmad F.J., Iqbal Z., Khar R.K., Aqil M., Talegaonkar S. Nanoemulsion components screening and selection: A technical note. AAPS Pharm. Sci. Tech. 2009;10:69–76. doi: 10.1208/s12249-008-9178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prajapati S.T., Joshi H.A., Patel C.N. Preparation and Characterization of Self-Microemulsifying Drug Delivery System of Olmesartan Medoxomil for Bioavailability Improvement. J. Pharm. 2013;2013:728425. doi: 10.1155/2013/728425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yuan Y., Li S.M., Mo F.K., Zhong D.F. Investigation of microemulsion system for transdermal delivery of meloxicam. Int. J. Pharm. 2006;321:117–123. doi: 10.1016/j.ijpharm.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 33.Nazar M.F., Khan A.M., Shah S.S. Microemulsion system with improved loading of piroxicam: A study of microstructure. AAPS Pharm. Sci. Tech. 2009;10:1286–1294. doi: 10.1208/s12249-009-9328-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karasulu H.Y. Microemulsions as novel drug carriers: The formation, stability, applications and toxicity. Expert Opin. Drug Deliv. 2008;5:119–135. doi: 10.1517/17425247.5.1.119. [DOI] [PubMed] [Google Scholar]
- 35.Le Roy Boehm A.L., Fessi H. Pharmaceutical applications of the zeta potential--use in characterization of colloidal drug carriers. J. Pharm. Belg. 2000;55:40–48. [PubMed] [Google Scholar]
- 36.Lou H., Qiu N., Crill C., Helms R., Almoazen H. Development of w/o microemulsion for transdermal delivery of iodide ions. AAPS Pharm. Sci. Tech. 2013;14:168–176. doi: 10.1208/s12249-012-9901-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shang L., Zhang S., Du H., Venkatraman S.S. A novel approach for the control of drug release rate through hydrogel membrane: I. Effect of drug immobilization on drug release rate by copolymerization method. Eur. J. Pharm. Biopharm. 2008;68:715–723. doi: 10.1016/j.ejpb.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 38.Madheswaran T., Baskaran R., Yong C.S., Yoo B.K. Enhanced topical delivery of finasteride using glyceryl monooleate-based liquid crystalline nanoparticles stabilized by cremophor surfactants. AAPS Pharm. Sci.Tech. 2014;15:44–51. doi: 10.1208/s12249-013-0034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.