Abstract
Background
It is well known that the prevalence of obesity in Korea is increasing over time, however it is not known how the trends among occupational groups and sex differ in such increasing trends. This study was designed to provide recent trends of obesity among workers in Korea and to identify whether there were differences among occupational groups.
Methods
We used data from the Korean National Health and Nutrition Examination Survey, Phases I to VI (1998–2015), to analyze trends in the prevalence of obesity in adult Korean workers. Obesity was defined as a body mass index of 25 kg/m2 or higher. Occupations were classified into 3 groups: (a) nonmanual workers, (b) service/sales workers, and (c) manual workers.
Results
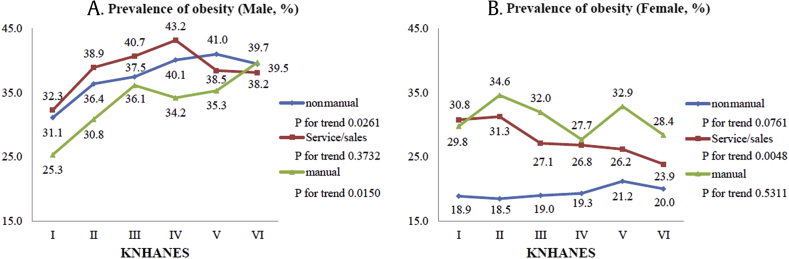
During the period of the Korean National Health and Nutrition Examination Survey Phases I to VI, the prevalence of obesity in male workers increased in all occupations (31.1% to 39.5% in manual workers, 32.3% to 38.2% in service/sales workers, and 25.3% to 39.7% in manual workers). However, female workers did not show any particular tendency toward obesity, except for a significant decrease in the prevalence rate in service/sales workers (30.8% to 23.9%, p for trend = 0.0048).
Conclusion
The trends of obesity prevalence by sex and occupation were different. For male manual workers, the prevalence rate increased steadily during the data period, while it decreased steadily in female sales/service workers.
Keywords: Obesity, Occupations, Prevalence, Trends
1. Introduction
Obesity is a well-known risk factor for many diseases, such as cardiovascular disease [1], cancer [2], and diabetes [3]. According to the World Health Organization, obesity increases the risk of non–insulin-dependent diabetes mellitus, dyslipidemia, coronary heart disease, hypertension, certain cancers (breast, endometrium, large bowel), polycystic ovary syndrome, and osteoarthritis by two to three times and triples the risk of sleep apnea [4]. This comorbidity can be explained through the following biochemical mechanisms. Excessive fat accumulation leads to accumulation of subcutaneous and visceral adipose tissue. The proinflammatory cytokines secreted from the adipose tissues increase the risk of diabetes by inducing insulin resistance, and the lipotoxicity of free fatty acids caused by decomposition of excess triglycerides leads to nonalcoholic fatty liver disease and liver cirrhosis. Overreaction of the chronic sympathetic nervous system, the renin–angiotensin–aldosterone system, causes systemic and pulmonary hypertension. In addition, mechanical stress due to excess weight causes gastroesophageal reflux disease and Barrett's esophagus by increasing intraabdominal pressure, obstructive sleep apnea by increasing pharyngeal soft tissue, and osteoarthritis by increasing mechanical load on joints [5].
The prevalence of obesity has significantly increased worldwide for the past three decades. Although this increase has recently stagnated in developed countries, it is steadily increasing in developing countries, which account for two-thirds of the entire obese population [6].
These harmful effects and high rates of obesity are a great burden on society. The social costs of obesity include not only direct costs, such as medical costs, but also indirect costs [7]. Moreover, most of these indirect costs arise in the workplace [8]. Obese workers are less productive [9], have more absenteeism [10], and are more likely to suffer from occupational injuries [11].
The social impact of obesity has been similarly reported in Korea. First, the rate of obesity in general adults in Korea is steadily increasing in men; on the contrary, it is slightly decreasing in women [12]. Nevertheless, the prevalence of obesity in the population as a whole is increasing, and the resulting socioeconomic costs are also increasing [13], [14]. Despite the growing social costs of obesity, there is a lack of research on obesity in the workplace to determine which groups should be the primary targets of prevention programs. Although prior studies have presented data on the socioeconomic factors of obesity in the general adult population [15], no studies have focused on obesity prevalence by occupation.
Therefore, in this study, we used data from “the Korean National Health and Nutrition Examination Survey (KNHANES)” to determine the prevalence of obesity by occupation over time and to identify the group most in need of a workplace obesity prevention program.
2. Materials and methods
2.1. Study population
In this study, we used KNHANES data from Phase I (1998) through Phase VI (2013–2015). The KNHANES is a cross-sectional, nationally representative survey conducted by the Korean Centers for Disease Control and Prevention and has been performed in 6 phases: Phase I (1998), Phase II (2001), Phase III (2005), Phase IV (2007–2009), Phase V (2010–2012), and Phase VI (2013–2015).
The KNHANES conducted stratification using data such as region, household characteristics, sex ratio, population ratio, the number of households, the number of apartment units, and average apartment size, to better reflect Koreans in the local population. Then, data were formed using stratified and a multistage clustered probability sampling method through a two-step extraction process of probability proportion extraction and system extraction. The total population surveyed during the target period was 184,436 people: Phase I, 39,060 people; Phase II, 37,878 people; Phase III, 34,145 people; Phase IV, 24,871 people; Phase V, 25,534 people; and Phase VI, 22,948 people. Among these groups, those younger than 19 years or older than 65 years were excluded. In Korea, the retirement age of a worker is 60 years. However, considering the high participation rate of the aged population in economic activities and the most common retirement age of manual workers being 65 years, the population aged up to 65 years was considered for inclusion in this study. We excluded cases in which physical measurements and occupations were missing.
2.2. Variable measurement
The KNHANES is composed of a health interview survey, a health behavior survey, a health examination survey, and a nutrition survey [16]. The KNHANES used the major categories of the Korean Standard Classification of Occupations for occupational classification. In this study, occupation was classified into 3 groups: (1) nonmanual workers including general managers, professionals, and office workers; (2) sales/service workers; and (3) manual workers including agriculture, fishery, and forestry workers; machine operating and assembling workers; and craft and related trade workers. Those who were unemployed at the time of survey were excluded.
Height and body weight were measured by physical examination and were presented in centimeters and kilograms, respectively. The body mass index (BMI) was calculated as the ratio of weight to height squared (kg/m2). Asians have different characteristics than Caucasian races in their risk of comorbidity (e.g., hypertension, dyslipidemia, and diabetes) according to the BMI. Thus, following the American Association of Clinical Endocrinologists/American College of Endocrinology comprehensive clinical practice guidelines, a BMI greater than 25 was defined as obese [17], [18]. Pregnant women were excluded from the analysis.
Age was classified into 4 groups: 20s, 30s, 40s, and 50 65 years.
The nutrition survey of the KNHANES consisted of dietary habits, 1-day 24-hour recall, and food frequency questionnaire. The daily calorie intake was calculated by the type, amount, and frequency of foods or drinks consumed during the previous day. To compare daily calorie intake for each occupation and phase, age standardization using the 2005 Korea Census population was conducted (Supplement 1).
2.3. Statistical analyses
KNHANES data are formed using stratified and a multi-stage clustered probability sampling method through a two-step extraction process of probability proportion extraction and system extraction. Therefore, it is recommended to use the ‘proc survey’ module for data analysis. We conducted SAS proc survey analysis considering sample weights and complex sample designs to represent the Korean population, if possible. All of the data are presented as an estimated percentage (standard error) or estimated mean (standard error). Analyses of variance (ANOVAs) were used for age comparisons and BMI mean values across occupations by sex, and the chi-square test was used to compare prevalence of obesity. The unadjusted and age-adjusted prevalence values of obesity by occupation were estimated. To avoid bias from changes in population structure across phases, age standardization by the direct method was conducted for prevalence using the 2005 Korea Census population. Because the 2005 Korea Census population, which was used as a standard population, is a general population structure including all age groups, we excluded minors and elderly who could not work to apply it to the main study which targeted current workers. The age structure of the standard population was divided into four age groups: 20s, 30s, 40s, and 50–65 years. Odds ratio and 95% confidence interval for obesity according to time trend in the phase were calculated using multiple logistic regression analyses after adjusting for age groups. All analyses were conducted using SAS statistical software, version 9.4, (SAS Institute Inc., Cary, NC, USA). A P value < 0.05 was considered statistically significant.
2.4. Ethics statement
The original study was approved by the Institutional Review Board (IRB) of the Korean Centers for Disease Control and Prevention (IRB: 2007-02-CON-04-P; 2008-04EXP-01-C; 2009-01CON-03-2C; 2010-02CON-21-C; 2011-02CON-06-C; 2012- 01EXP-01-2C; 2013-07CON-03-4C; 2013-12EXP-03-5C). Since 2015, the KNHANES has been conducted in accordance with the Article 2, Clause 1 of the Bioethics and Safety Act and Article 2, Clause 2, Paragraph 1 of the Enforcement Rule of the act without consideration of the IRB for research conducted by the State for public welfare (http://knhanes.cdc.go.kr).
3. Results
The analysis was conducted on 15,748 men (I: 2,607; II: 2,068; III: 1,615; IV: 4,672; V: 4,786; and VI: 3,966) and 16,504 women (I: 1,911; II: 1,473; III: 1,338; IV: 3,897; V: 4,144; and VI: 3,741).
In men, age significantly increased in manual and nonmanual workers during the target period (Table 1). Manual workers were older than those in other occupations, and this difference was statistically significant (p value <.0001). The mean BMI value significantly increased in nonmanual workers (p for trend = 0.0004) and manual workers (p for trend <.0001). The prevalence of obesity without age adjustment significantly increased in nonmanual and manual workers. Although the trend of obesity prevalence in the service/sales workers decreased from IV to VI, the mean prevalence of obesity of all male participants increased significantly.
Table 1.
Trends in the prevalence of obesity according to sex and occupation of workers younger than 65 yrs
| Male |
I (1998) |
II (2001) |
III (2005) |
IV (2007-2009) |
V (2010-2012) |
VI (2013-2015) |
P for trend | ||||||
|
n = 2,607 |
p |
n = 2,068 |
p |
n = 1,615 |
p |
n = 4,672 |
p |
n = 4,786 |
p |
n = 3,966 |
p |
||
| Age (yr) | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | |||||||
| Nonmanual | 37.5 (0.43) | 39.1 (0.50) | 38.2 (0.56) | 39.4 (0.32) | 39.6 (0.30) | 40.5 (0.30) | 0.0004 | ||||||
| Service/sales | 39.8 (0.54) | 41.8 (0.67) | 39.6 (0.69) | 38.9 (0.42) | 39.2 (0.54) | 38.6 (0.55) | 0.0007 | ||||||
| Manual | 42.6 (0.36) | 44.2 (0.46) | 42.2 (0.60) | 43.2 (0.35) | 44.7 (0.33) | 45.6 (0.34) | <.0001 | ||||||
| Overall | 40.4 (0.26) | 42.1 (0.30) | 40.3 (0.38) | 41.0 (0.22) | 41.8 (0.23) | 42.3 (0.22) | 0.0059 | ||||||
| BMI (kg/m2) | 0.0020 | 0.0110 | 0.5520 | <.0001 | <.0001 | 0.1444 | |||||||
| Nonmanual | 23.6 (0.12) | 24.1 (0.14) | 24.3 (0.14) | 24.4 (0.08) | 24.6 (0.10) | 24.6 (0.09) | 0.0004 | ||||||
| Service/sales | 23.7 (0.13) | 24.1 (0.17) | 24.3 (0.21) | 24.5 (0.12) | 24.3 (0.17) | 24.3 (0.15) | 0.7496 | ||||||
| Manual | 23.2 (0.10) | 23.7 (0.10) | 24.1 (0.16) | 24.0 (0.08) | 24.0 (0.08) | 24.5 (0.09) | <.0001 | ||||||
| Overall | 23.5 (0.08) | 23.9 (0.08) | 24.2 (0.10) | 24.2 (0.05) | 24.3 (0.06) | 24.5 (0.06) | <.0001 | ||||||
| Obesity (%) | 0.0065 | 0.0204 | 0.4849 | 0.0004 | 0.0022 | 0.4805 | |||||||
| Nonmanual | 29.3 (1.86) | 37.3 (2.28) | 38.6 (2.28) | 40.8 (1.28) | 42.4 (1.46) | 40.4 (1.35) | <.0001 | ||||||
| Service/sales | 33.0 (2.11) | 38.6 (2.80) | 41.0 (3.13) | 43.1 (1.96) | 37.7 (2.25) | 37.5 (2.05) | 0.0033 | ||||||
| Manual | 25.5 (1.54) | 31.2 (1.75) | 36.5 (2.22) | 35.3 (1.21) | 35.5 (1.20) | 40.2 (1.29) | <.0001 | ||||||
| Overall |
28.4 (1.16) |
34.9 (1.40) |
38.1 (1.37) |
38.8 (0.79) |
38.5 (0.87) |
39.8 (0.84) |
<.0001 |
||||||
|
Female |
n = 1,911 |
p |
n = 1,473 |
p |
n = 1,338 |
p |
n = 3,897 |
p |
n = 4,144 |
p |
n = 3,741 |
p |
|
| Age (yr) | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | |||||||
| Nonmanual | 29.7 (0.46) | 31.5 (0.57) | 31.4 (0.50) | 33.8 (0.31) | 34.5 (0.30) | 36.2 (0.30) | <.0001 | ||||||
| Service/sales | 39.5 (0.53) | 40.9 (0.46) | 42.5 (0.65) | 41.4 (0.41) | 43.1 (0.43) | 43.5 (0.45) | <.0001 | ||||||
| Manual | 46.8 (0.50) | 46.2 (0.58) | 46.4 (0.56) | 48.4 (0.31) | 48.4 (0.38) | 48.6 (0.50) | <.0001 | ||||||
| Overall | 39.6 (0.37) | 40.2 (0.37) | 39.8 (0.44) | 40.6 (0.24) | 41.3 (0.25) | 41.4 (0.26) | <.0001 | ||||||
| BMI (kg/m2) | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | |||||||
| Nonmanual | 21.6 (0.15) | 21.6 (0.15) | 21.7 (0.20) | 22.0 (0.10) | 22.1 (0.12) | 22.2 (0.09) | 0.0002 | ||||||
| Service/sales | 23.6 (0.16) | 23.8 (0.17) | 23.6 (0.17) | 23.3 (0.12) | 23.5 (0.13) | 23.2 (0.13) | 0.0099 | ||||||
| Manual | 23.7 (0.15) | 24.3 (0.18) | 24.2 (0.23) | 23.9 (0.10) | 24.1 (0.13) | 24.0 (0.12) | 0.0619 | ||||||
| Overall | 23.1 (0.10) | 23.4 (0.11) | 23.1 (0.13) | 23.0 (0.07) | 23.1 (0.08) | 22.9 (0.07) | 0.0028 | ||||||
| Obesity (%) | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | |||||||
| Nonmanual | 13.5 (1.78) | 10.2 (1.73) | 13.5 (2.01) | 14.5 (1.10) | 17.7 (1.20) | 17.5 (1.06) | <.0001 | ||||||
| Service/sales | 30.4 (1.95) | 32.8 (2.27) | 30.2 (2.56) | 28.7 (1.60) | 28.9 (1.51) | 25.9 (1.53) | 0.0302 | ||||||
| Manual | 33.3 (1.96) | 39.7 (2.73) | 35.2 (2.70) | 33.2 (1.45) | 35.5 (1.68) | 33.5 (1.67) | 0.9504 | ||||||
| Overall | 27.0 (1.24) | 29.1 (1.31) | 25.9 (1.51) | 24.7 (0.79) | 26.3 (0.83) | 24.0 (0.80) | 0.0026 | ||||||
BMI, body mass index; SE, standard error.
All values are presented as mean (SE). Significant values (P < .05) are in italics.
For women, regardless of age, the tendency was slightly different from that of men. First, as in men, the age of workers in all occupations increased significantly during the study period (all p for trend <.0001). In addition, manual workers were found to be older than workers in other occupations. In female service/sales workers, the mean BMI decreased significantly (p for trend = 0.0099), while that in nonmanual workers increased significantly (p for trend = 0.0002). Unlike the trend of the prevalence of obesity among men, which only showed significant increases in manual workers, the trend of the prevalence of obesity among women showed significant decreases in service/sales workers and significant increases in manual workers. In nonmanual workers, the prevalence rate of obesity increased with time (p for trend <.0001), while that in service/sales workers decreased with time (p for trend = 0.0302). The prevalence of manual workers did not show significant trend (p for trend = 0.9504).
The prevalence of age-standardized obesity was calculated based on the population of the Korea National Statistical Office in 2005 to take into account changes in population structure across phases (Fig. 1). The differences in the prevalence of obesity by sex and occupation were clarified. For example, male service/sales workers showed a decrease after a high prevalence rate of 43.2% in Phase IV (p for trend = 0.3782), although the trend of the mean prevalence of obesity in all male workers increased, as shown in Table 1. Besides, the prevalence rate of manual workers, which was the lowest among the three occupations during the target period, became the highest in Phase VI (p for trend = 0.0150).
Fig. 1.
Trends in age-standardized prevalence of obesity according to sex and occupation in workers younger than 65 years. Age-standardized prevalence was calculated using the age- and sex-specific structures of the estimated population based on the 2005 Korea Census. KNHANES, Korean National Health and Nutrition Examination Survey.
There were more occupational differences in the prevalence of obesity in women than in men. While the prevalence of obesity in nonmanual workers increased slightly (p for trend = 0.0761), it decreased significantly in service/sales workers (p for trend = 0.0048), but there was no specific tendency in manual workers (p for trend = 0.5311).
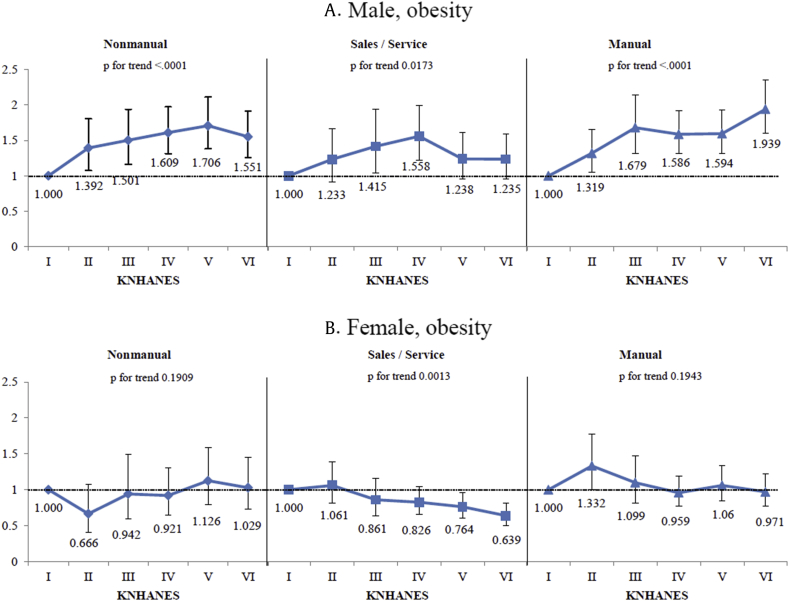
Compared with Phase I, the odds ratios for each sex were estimated by adjusting age groups for prevalence of obesity, according to phase (Fig. 2). The odds ratio of obesity in men increased significantly in nonmanual workers, sales/service workers, and manual workers, compared with the odds ratios in women (p for trend <.0001, p = 0.0173, p < .0001, respectively). There was a significant decrease in the odds ratio of obesity in sales/service workers in women, but no significant changes were observed in manual or nonmanual workers.
Fig. 2.
Age group–adjusted odds ratio of obesity prevalence by sex and occupation, according to the KNHANES. KNHANES, Korean National Health and Nutrition Examination Survey.
4. Discussion
In this study, we found differences in the trend of obesity prevalence by sex and occupation. While the prevalence rate of obesity in male workers showed an overall increased trend, the prevalence of female workers did not show a particular trend, except a steady decrease in sales/service workers.
This trend was consistent with that in the general population at some points. Shin and Kang [12] reported the prevalence of obesity in the Korean general adult population by sex, using KNHANES data for the period from 1998 to 2014. In their study, the prevalence of obesity in the male general population increased significantly from 25.7% (Phase I) to 37.9% (Phase VI), while that in the female general population decreased from 27.2% (Phase I) to 25.9% (Phase VI). Similar to the prevalence of obesity in the general male population, the prevalence of obesity in male workers has increased steadily, except for a decrease after Phase IV in male sales/service workers. In female workers, the trend was similar to that in the general population, except for slight increase in nonmanual workers and a greater decreasing trend in service/sales workers.
The change in obesity rates can be explained by calorie intake and calorie consumption. First, calorie intake by occupation was obtained using KNHANES data (Supplement 1). Calorie intake during Phase I through Phase VI was different by sex and occupation. In men, the overall trend of calorie intake increased, as we might have guessed by the increasing prevalence of obesity. In addition, this increase was particularly prominent in manual workers, whose absolute calorie intake per phase was also highest among all workers. This partially explains the rapid increase in obesity in male manual workers. In contrast, female workers did not show a specific increase in calorie intake. The calorie intake of nonmanual workers was the lowest among workers at the onset (Phase I), but it increased over time, resulting in the highest calorie intake in Phases V and VI. However, these increases in calorie intake did not result in an increase in obesity rate in nonmanual workers. In nonmanual workers, as well as in other groups, it is difficult to explain the change in obesity rate with changes in calorie intake.
The reason why the trend of obesity rate cannot be explained by calorie intake is because calorie consumption was not considered. Unfortunately, the KNHANES data used in this study did not quantify calorie consumption. However, through other studies, calorie consumption in the workplace can be deduced indirectly. Much of the hardest physical work has been decreased over time because of automation, mechanization, and computerization, which result in worker obesity [19]. In addition, the reduction of hard manual labor was more pronounced for men [20], especially in manual workers. Thus, the overall increase in obesity rate of male manual workers may be partially explained by a decrease in physical activity.
In addition, as the phases progressed, the obesity rate converged to about 40% in men, which made it more difficult to discern obesity rates among various occupations. A follow-up of the prevalence rates after Phase VI is required to confirm whether this trend will continue.
The most distinctive result of this study was that obesity rate is decreasing in female sales/service workers. This decreased trend was also found in male sales/service workers. There could be many reasons for the decreases in body weight and obesity rates, but the reason for the decline only in certain occupations might be considered as having a social cause. For sales/service workers who personally interact with customers, there may be more social pressure to be in ‘good shape’ than in other occupations. This same pressure may likely have lowered the obesity rate by pushing out obese sales/service workers from the labor market. According to actual reports, obesity produces social prejudice, which can affect employment, health, and education [21]. People with obesity are more likely to be excluded from the job search process and are more likely to be dismissed because of prejudice. This discrimination due to obesity is more easily found in women. And this discrimination in the labor market may depend on economic circumstances [22]. According to Han et al [23], in Korea, the instability of work after the recession in 1997 forced workers to lose weight, as workers with obesity were driven from the labor market. In addition, this trend occurs not only in women but also in men. The social pressure on men also can explain the decrease in male sales/service worker obesity rates after Phase IV. A decrease in the rate of obesity is welcome in the public health sense, but we have to consider whether this decrease was due to the success of obesity prevention policy or consideration of “survival of fittest workers” in the labor market.
Several potential problems were inherent to the design of this study. First, the BMI has limitations in measuring obesity. According to a strict definition, obesity is an accumulation of excess fat, while the BMI reflects only simple weight and height. The BMI cannot distinguish whether the increase in body weight is from muscle or fat. Therefore, the obesity rate can be overestimated by classifying people who weigh more because they are muscular as opposed to being obese and can be underestimated by classifying people with normal weight but with high fat ratio as “normal.” Second, we did not reveal the mechanism of change in obesity rate. The KNHANES data can be used to derive calorie intake, which could explain some of the changes in obesity rates. However, because the KNHANES data did not have a quantitative index of physical activity, calorie consumption, which is the other axis of obesity, could not be determined. Third, we excluded those who had missing values, which may have included cases where people with obesity refuse measurement because of negative social prejudices. This could have resulted in underestimation of the actual obesity rates.
Despite these limitations, the strength of this study was that sampling weights were applied to account for the complex sampling and to represent the Korean workers aged 20 through 65 years without biased estimates. Another asset of our study is that we presented the prevalence trends in obesity according to occupation, so more detailed information for preventive intervention was gathered.
The results of our study showed that the trends in the prevalence of obesity differed according to occupation and sex. There were sharp increases among male manual workers and steady decreases among female service/sales workers. This study helped to establish priority target groups, such as male manual workers, for obesity prevention programs.
Conflicts of interest
All authors have no conflicts of interest to declare.
Funding
The authors received no specific funding for this work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.shaw.2019.08.003.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Murphy N.F., MacIntyre K., Stewart S., Hart C.L., Hole D., McMurray J.J. Long-term cardiovascular consequences of obesity: 20-year follow-up of more than 15 000 middle-aged men and women (the Renfrew-Paisley study) Eur Heart J. 2006;27:96–106. doi: 10.1093/eurheartj/ehi506. [DOI] [PubMed] [Google Scholar]
- 2.Calle E.E., Rodriguez C., Walker-Thurmond K., Thun M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 3.Cloostermans L., Wendel-Vos W., Doornbos G., Howard B., Craig C.L., Kivimäki M., Tabak A.G., Jefferis B.J., Ronkainen K., Brown W.J., Picavet S.H., Ben-Shlomo Y., Laukkanen J.A., Kauhanen J., Bemelmans W.J. Independent and combined effects of physical activity and body mass index on the development of Type 2 Diabetes - a meta-analysis of 9 prospective cohort studies. Int J Behav Nutr Phys Act. 2015;12:147. doi: 10.1186/s12966-015-0304-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva: 2000. Obesity : preventing and managing the global epidemic [Internet] [cited 2019 Jan 21]. Available from: http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [PubMed] [Google Scholar]
- 5.Heymsfield S.B., Wadden T.A. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:1492. doi: 10.1056/NEJMc1701944. [DOI] [PubMed] [Google Scholar]
- 6.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C., Abera S.F., Abraham J.P., Abu-Rmeileh N.M., Achoki T., AlBuhairan F.S., Alemu Z.A., Alfonso R., Ali M.K., Ali R., Guzman N.A., Ammar W., Anwari P., Banerjee A., Barquera S., Basu S., Bennett D.A., Bhutta Z., Blore J., Cabral N., Nonato I.C., Chang J.C., Chowdhury R., Courville K.J., Criqui M.H., Cundiff D.K., Dabhadkar K.C., Dandona L., Davis A., Dayama A., Dharmaratne S.D., Ding E.L., Durrani A.M., Esteghamati A., Farzadfar F., Fay D.F., Feigin V.L., Flaxman A., Forouzanfar M.H., Goto A., Green M.A., Gupta R., Hafezi-Nejad N., Hankey G.J., Harewood H.C., Havmoeller R., Hay S., Hernandez L., Husseini A., Idrisov B.T., Ikeda N., Islami F., Jahangir E., Jassal S.K., Jee S.H., Jeffreys M., Jonas J.B., Kabagambe E.K., Khalifa S.E., Kengne A.P., Khader Y.S., Khang Y.H., Kim D., Kimokoti R.W., Kinge J.M., Kokubo Y., Kosen S., Kwan G., Lai T., Leinsalu M., Li Y., Liang X., Liu S., Logroscino G., Lotufo P.A., Lu Y., Ma J., Mainoo N.K., Mensah G.A., Merriman T.R., Mokdad A.H., Moschandreas J., Naghavi M., Naheed A., Nand D., Narayan K.M., Nelson E.L., Neuhouser M.L., Nisar M.I., Ohkubo T., Oti S.O., Pedroza A., Prabhakaran D., Roy N., Sampson U., Seo H., Sepanlou S.G., Shibuya K., Shiri R., Shiue I., Singh G.M., Singh J.A., Skirbekk V., Stapelberg N.J., Sturua L., Sykes B.L., Tobias M., Tran B.X., Trasande L., Toyoshima H., van de Vijver S., Vasankari T.J., Veerman J.L., Velasquez-Melendez G., Vlassov V.V., Vollset S.E., Vos T., Wang C., Wang X., Weiderpass E., Werdecker A., Wright J.L., Yang Y.C., Yatsuya H., Yoon J., Yoon S.J., Zhao Y., Zhou M., Zhu S., Lopez A.D., Murray C.J., Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tremmel M., Gerdtham U.G., Nilsson P.M., Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14:435. doi: 10.3390/ijerph14040435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trogdon J.G., Finkelstein E.A., Hylands T., Dellea P.S., Kamal-Bahl S.J. Indirect costs of obesity: a review of the current literature. Obes Rev. 2008;9:489–500. doi: 10.1111/j.1467-789X.2008.00472.x. [DOI] [PubMed] [Google Scholar]
- 9.Gates D.M., Succop P., Brehm B.J., Gillespie G.L., Sommers B.D. Obesity and presenteeism: the impact of body mass index on workplace productivity. J Occup Environ Med. 2008;50:39–45. doi: 10.1097/JOM.0b013e31815d8db2. [DOI] [PubMed] [Google Scholar]
- 10.Howard J.T., Potter L.B. An assessment of the relationships between overweight, obesity, related chronic health conditions and worker absenteeism. Obes Res Clin Pract. 2014;8:e1–e15. doi: 10.1016/j.orcp.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Schmier J.K., Jones M.L., Halpern M.T. Cost of obesity in the workplace. Scand J Work Environ Health. 2006;32:5–11. doi: 10.5271/sjweh.970. [DOI] [PubMed] [Google Scholar]
- 12.Shin H.Y., Kang H.T. Recent trends in the prevalence of underweight, overweight, and obesity in Korean adults: the Korean National Health and Nutrition Examination Survey from 1998 to 2014. J Epidemiol. 2017;27:413–419. doi: 10.1016/j.je.2016.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee J.W., Choi Y.E., Kim D.W., Lee S., Cho K.H. Trends in socioeconomic costs of morbid obesity among Korean adults, 2009-2013: data from National Health Insurance Service. Obes Res Clin Pract. 2018;12:389–393. doi: 10.1016/j.orcp.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Kang J.H., Jeong B.G., Cho Y.G., Song H.R., Kim K.A. Socioeconomic costs of overweight and obesity in Korean adults. J Korean Med Sci. 2011;26:1533–1540. doi: 10.3346/jkms.2011.26.12.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoo S., Cho H.J., Khang Y.H. General and abdominal obesity in South Korea, 1998-2007: gender and socioeconomic differences. Prev Med. 2010;51:460–465. doi: 10.1016/j.ypmed.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Kweon S., Kim Y., Jang M.J., Kim Y., Kim K., Choi S., Chun C., Khang Y.H., Oh K. Data resource profile: the Korea national health and nutrition examination survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garvey W.T., Mechanick J.I., Brett E.M., Garber A.J., Hurley D.L., Jastreboff A.M., Nadolsky K., Pessah-Pollack R., Plodkowski R. American association of clinical endocrinologists and american college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(Suppl. 3):1–203. doi: 10.4158/EP161365.GL. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . 2000. The Asia-Pacific perspective : redefining obesity and its treatment. sydney.https://iris.wpro.who.int/handle/10665.1/5379 [Google Scholar]
- 19.Choi B., Schnall P.L., Yang H., Dobson M., Landsbergis P., Israel L., Karasek R., Baker D. Sedentary work, low physical job demand, and obesity in US workers. Am J Ind Med. 2010;53:1088–1101. doi: 10.1002/ajim.20886. [DOI] [PubMed] [Google Scholar]
- 20.Lakdawalla D., Philipson T. Labor supply and weight. J Hum Res. 2007;42:85–116. [Google Scholar]
- 21.Puhl R.M., Heuer C.A. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 22.O'Brien K.S., Latner J.D., Ebneter D., Hunter J.A. Obesity discrimination: the role of physical appearance, personal ideology, and anti-fat prejudice. Int J Obes (Lond) 2013;37:455–460. doi: 10.1038/ijo.2012.52. [DOI] [PubMed] [Google Scholar]
- 23.Han S.Y., Brewis A.A., SturtzSreetharan C. Employment and weight status: the extreme case of body concern in South Korea. Econ Hum Biol. 2018;29:115–121. doi: 10.1016/j.ehb.2018.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.