Abstract
Background & Objectives
A growing body of work supports linear associations between sleep and socioemotional adjustment in adolescence. However, associations between sleep and adjustment are not necessarily linear and investigations of nonlinear effects are scarce. This study examined linear and nonlinear relations between several sleep-wake parameters and externalizing behavior and internalizing symptoms in adolescence, and assessed the role of adolescent sex as a moderator of effects.
Participants
Participants were high school students (N = 180; M age = 17.49, SD = .62; 59% female; 68% White/European American, 32% Black/African American) from a wide range of socio-economic backgrounds living in semirural communities and small towns in Alabama.
Methods
Sleep-wake parameters were indexed by actigraphy-derived sleep minutes and adolescents’ reports on morningness-eveningness (circadian preference), sleep-wake problems (sleep quality), and sleepiness. Adolescents completed questionnaires on externalizing behaviors and internalizing symptoms.
Results
Controlling for sleep duration, a higher preference for eveningness and poor sleep quality were associated in a linear fashion with increased externalizing and internalizing symptoms. Nonlinear relations between sleepiness and internalizing symptoms emerged with pronounced sex-related effects, including somewhat delayed accelerating relations for males and rapidly accelerating associations that tended to plateau for females.
Conclusions
Results illustrate the importance of examining multiple sleep-wake and adjustment variables as well as linear and nonlinear associations.
Keywords: adolescence, morningness-eveningness, sleep-wake problems, sleepiness, adjustment
Sleep plays an important role in healthy development during adolescence, yet insufficient sleep is common (Carskadon, 2011). High schoolers stay up particularly late, showing a remarkable delay in bedtime compared to younger adolescents in middle school (National Sleep Foundation, 2006). Prior work has demonstrated age-related changes during adolescence, including an increase in eveningness preferences (Roenneberg et al., 2004), a delay in sleep onset time (Sadeh, Dahl, Shahar, & Rosenblat-Stein, 2009), and a later phase of dim light melatonin onset (Crowley, Tarokh, & Carskadon, 2014). Due to changes in the circadian phase along with increasing social and academic demands, adolescents often struggle to fall asleep early at night and wake early in the morning to attend school (Carskadon, 2011; Carskadon, Acebo, & Jenni, 2004; Owens, 2014; Owens, Belon, & Moss, 2010), resulting in daytime sleepiness (Owens, 2014). Adolescent daytime sleepiness also has a biological component that may be independent of their sleep duration (Campbell, Higgins, Trinidad, Richardson, & Feinberg, 2007; Feinberg, 2013). Building on this literature, the present study sought to explicate associations between developmentally significant sleep-wake parameters and adjustment in youth.
Prior findings indicate that shorter sleep and poor sleep quality are related to aggression (Umlauf, Bolland, & Lian, 2011), externalizing behaviors (Pieters et al., 2015), and internalizing symptoms including depression (Kelly & El-Sheikh, 2014) and anxiety (McMakin & Alfano, 2015) in adolescents. Likewise, daytime sleepiness has been associated with adjustment problems in youth (Hershner & Chervin, 2014; Liu et al., 2019). In comparison to assessments of sleep duration and quality, fewer studies have examined associations between circadian phase preference (i.e., chronotype) and adjustment in adolescence, and existing evidence generally reveals relations between a higher preference for eveningness and higher levels of externalizing behavior (Lange & Randler, 2011; Merikanto et al., 2017), depression (Kaur & Tung, 2017), and anxiety (Díaz-Morales, 2016).
Almost all studies with youth have examined linear associations between sleep and adjustment. Examination of linear associations rests on the assumption that the rate of change in outcomes (adjustment in this study) is the same across all levels of sleep (Cohen, Cohen, West, & Aiken, 2003). However, associations between sleep and adjustment may be nonlinear (Matricciani, Blunden, Rigney, Williams, & Olds, 2013). For example, the positive effects of better sleep quality on adolescents’ adjustment may not appear until, or may plateau beyond, certain levels of sleep quality. In a small number of studies with youth, nonlinear associations between sleep duration and adjustment problems have been observed. For example, both short and long sleep duration are related to greater internalizing and externalizing behavior problems (Fuligni, Arruda, Krull, & Gonzales, 2018; James & Hale, 2017). Although multiple sleep-wake parameters are associated with adolescents’ adjustment (Feinberg, 2013; Liu et al., 2019; Merikanto et al., 2017), we are aware of a very few investigations of nonlinear associations with a sleep-wake variable other than duration with youth. In a study with children (9–10 years), the association between subjective sleep-wake problems and teacher-reported internalizing symptoms was nonlinear, rapidly increasing from low to average levels of sleep problems and then (El-Sheikh, Philbrook, Kelly, Hinnant, & Buckhalt, 2019). Other investigations that examined nonlinear associations between sleep parameters and physical health reported such relations involving BMI in young adults (Kalak, Brand, Beck, Holsboer-Trachsler, & Wollmer, 2015) and inflammatory markers in children and adolescents (Mählmann et al., 2017).
The present study builds on the literature by examining linear and nonlinear associations between multiple key sleep-wake parameters and externalizing behavior and internalizing symptoms with a large sample in late adolescence. Sleep duration, circadian preference, sleep-wake problems (also referred to as sleep quality) and daytime sleepiness were assessed. Based on previous work (Kelly & El-Sheikh, 2014; Randler, 2011), we expected that shorter sleep, later circadian preference, poorer sleep quality, and greater sleepiness would be associated in a linear fashion with both externalizing behaviors and internalizing symptoms. The call for examining nonlinear associations between sleep and developmental outcomes has been growing (Feinberg, 2013; Matricciani et al., 2013), and recent studies have demonstrated nonlinear associations between sleep duration and mental health in adults (Zhai, Zhang, & Zhang, 2015), adolescents (Fuligni et al., 2018), and school-aged children (James & Hale, 2017). Responsive to recommendations in the literature, and consistent with growing empirical evidence, we expected nonlinear associations to emerge between various sleep parameters and adolescents’ adjustment. However, we proposed no directional hypotheses about the shape of nonlinear relations (e.g., U-shaped, accelerating, rapidly accelerating or decelerating).
The second research question was whether linear and nonlinear relations between sleep and adjustment are moderated by adolescent sex. Examination of moderation effects can identify youth who may be at particular risk for adjustment problems in the context of sleep disruptions. In late adolescence, sex differences in multiple sleep variables have been reported, including sleep duration (Short, Gradisar, Lack, Wright, & Carskadon, 2012), circadian preference (Roenneberg et al., 2004), sleep quality (Chung & Cheung, 2008), and sleepiness (Vilela, Bittencourt, Tufik, & Moreira, 2016), yet findings have been inconsistent. Importantly, most of the relevant studies examined mean differences in sleep between males and females, and less is known about the role of sex as a moderator of linear or nonlinear associations between sleep and developmental outcomes in youth. Examination of gender as a moderator of linear and nonlinear relations was considered exploratory in the present study.
Methods
Participants
The study is part of the Family Stress and Youth Development Study, a longitudinal investigation of a school-recruited sample of youth in Alabama that began in 2005. Inclusion criteria at the time of recruitment required participants have no diagnosis of developmental delay, attention-deficit/hyperactivity disorder, and chronic illnesses, and also that they reside in two-parent homes due to a focus of the larger study on the effects of marital conflict on children. The present paper is based on data from the 6th wave of collection in 2014–2015 with an analytic sample of 180 adolescents (M age = 17.49 years, SD = 7.38 months), all of whom were attending high school.
The sample was diverse in terms of adolescent sex (59% female) and race (68% White/European American, 32% Black/African-American). Participants also were from a wide range of socio-economic backgrounds, as measured by income-to-needs, a ratio dividing family income by the poverty threshold for a given household size (U.S. Department of Commerce, 2014). One-third (31%) of participants’ families were living at or near the federal poverty line (ratio < 2), 28% were middle class (ratio 2–2.99), and 41% were upper middle class (ratio ≥ 3).1
Procedure
The university’s Institutional Review Board approved study procedures. Parents consented and youth assented to participation. Adolescents wore actigraphs for one week at night to derive an objective measure of sleep duration. An average of 0.36 days later (SD = 5.49), families visited a laboratory on campus where youth reported on their sleep and adjustment.
Measures
Sleep
To obtain an objective measurement of sleep duration, adolescents wore Octagonal Basic Motionlogger actigraphs (Ambulatory Monitoring, Ardsley, NY, USA) on their non-dominant wrists at home while sleeping for up to seven nights. Data were scored in Action-W2 using the Sadeh algorithm and zero crossing mode (Sadeh, Sharkey, & Carskadon, 1994) to derive the number of 1-minute epochs scored as sleep. Per common practice, sleep minutes were calculated from sleep onset to wake time excluding periods of wakefulness. This variable was stable across the week (α = .75), and an average across nights was used in analyses, excluding any nights on which participants took medication for acute illnesses or allergies. Individuals’ sleep minutes were used in analyses if they had at least five nights of actigraphic data (after exclusion of nights with medication), following recommendations in the field (Meltzer, Montgomery-Downs, Insana, & Walsh, 2012); otherwise, actigraph data were treated as missing (though subjects with missing data were not excluded from analyses).
Youth completed the School Sleep Habits Survey (SSHS; Wolfson & Carskadon, 1998), which has excellent reliability and validity (Lewandowski, Toliver-Sokol, & Palermo, 2011; Wolfson et al., 2003). The measure has been used in many studies to examine children’s and adolescents’ sleep parameters (El-Sheikh et al., 2013; Vernon, Modecki, & Barber, 2018). Three scales of the Survey were used: morningness-eveningness, sleep-wake problems (SWP), and sleepiness. There are advantages and disadvantages to the various methodologies used to examine sleep (Sadeh, 2015); subjective reports of several sleep-wake parameters examined in this study (e.g., circadian preference, quality, sleepiness) are effective for representing individual variability in sleep needs (Blunden & Galland, 2014; Matricciani et al., 2013).
The morningness-eveningness scale (10 items; α = .71) surveyed the times of day that individuals prefer to wake and sleep given no other constraints, ease with which they wake in the morning, and alertness throughout the day. Responses could range from 1 to either 4 or 5 on various items, with higher scores indicating more morningness. Summed scores were used in analyses, with a full possible range of 10 (more eveningness) to 43 (more morningness).
The SWP scale (10 items; α = .80) assessed frequency of difficulties that adolescents experienced in initiating and maintaining sleep at night and waking in the morning. Responses on each item could range from 1 (never) to 5 (everyday/night) and were summed, giving the scale a possible range of 10 (no SWP) to 50 (daily or nightly SWP).
The sleepiness scale (9 items; α = .78) measured whether participants struggled to stay awake or fell asleep during the day while participating in activities such as talking to others, completing homework, or taking a test. Given the age of the sample and that not all youth had driver permits or licenses, one item regarding sleepiness while driving was not administered. Responses on each item could range from 1 (did not struggle to stay awake or fell asleep) to 4 (both struggled to stay awake and fell sleep), providing a full possible range of 9 (no incidents of sleepiness) to 36 (high sleepiness).
Externalizing Behaviors and Internalizing Symptoms
Adolescents reported on their externalizing behaviors and internalizing symptoms using the Youth Self-Report (YSR), a well-validated instrument used frequently in both research and clinical settings (Achenbach & Rescorla, 2001). The externalizing scale is composed of 32 items (α = .85) examining rule-breaking and aggressive behaviors such as using alcohol or destroying property. The internalizing scale is comprised of 31 items (α = .92) assessing depression, anxiety, and somatic complaints such as feeling worthless, withdrawing from others, or having excessive stomachaches. For each item, adolescents indicated whether statements were not true (0), somewhat or sometimes true (1), or very true or often true (2) over the previous six months. T scores, which are normed for age and sex, were used in analyses; these have a full possible range of 0 to 100. For both scales, 17% of youth met criteria for borderline or clinical-level problems (T score ≥ 60; Achenbach & Rescorla, 2001).
For a thorough examination of internalizing symptoms, adolescents also completed the Child Depression Inventory (CDI; Kovacs, 1992) and the Revised Children’s Manifest Anxiety Scale (RCMAS-2; Reynolds & Richmond, 2008). Both measures are widely used and well-established instruments for surveying youths’ mental health. The CDI includes 27 items indicating the degree to which individuals experienced symptoms of depression over the previous two weeks across statements such as “Things will work out for me O.K.” (0), “I am not sure if things will work out for me” (1), and “Nothing will ever work out for me” (2). Two questions pertaining to sleep disturbances were excluded from analyses. Without those items, the CDI had high reliability in our sample (α = .89), and scores could range from 0 to 50. Six percent of participants met a clinical cutoff for depression screening (scores ≥ 20; Kovacs, 1992).
The Total Anxiety scale of the RCMAS was used in analyses, and includes 45 items surveying three dimensions of anxiety in adolescence: physiology, worry, and social anxiety. Adolescents indicated whether they agreed (1) or disagreed (0) with statements such as, “I worry about what is going to happen,” and “I fear other kids will laugh at me in class.” Five items surveying sleep problems were excluded, producing a modified scale with high reliability in our sample (α = .93), and scores could range from 0 to 40. Six percent of participants had anxiety symptoms in the clinical range (≥ 2 SD from the mean; Reynolds & Richmond, 2008).
Henceforth, externalizing behaviors and internalizing symptoms reported on the YSR are referred to as externalizing and internalizing symptoms, depression symptoms derived with the CDI are referred to as depression, and symptoms of anxiety reported through the RCMAS-2 are referred to as anxiety.
Covariates
Parents reported on adolescents’ race and sex, family income, and the number of people living in the household. The last two variables were used to determine the family’s socioeconomic status (SES) indexed by income-to-needs ratio (U.S. Department of Commerce, 2014). Body mass index (zBMI) was obtained during the laboratory session through a measurement of weight using a Tanita digital weight scale (Model BC-418) and wall-mounted stadiometer (Arlington Heights, IL).
Statistical Analyses
Four multiple regression models were conducted to examine whether each of the sleep parameters (sleep minutes, circadian preference [morningness-eveningness], sleep-wake problems, and sleepiness) was linearly and nonlinearly related to adjustment in youths, and whether adolescent sex moderated these associations. A linear and a nonlinear term of a sleep parameter, a Linear x Sex interaction, and a Nonlinear x Sex interaction were simultaneously included in the model along with covariates (adolescent race, SES, and zBMI). To ascertain the unique effects of circadian preference, sleep quality problems, and sleepiness on adolescents’ adjustment independent of sleep duration, the latter was included in the models as a covariate and thus its association with adjustment was statistically controlled.
In each regression model, predictors and covariates were allowed to correlate with one another. Sleep variables were standardized to aid convergence of our models with a relatively small sample size (N = 180). Covariates were mean-centered so that the intercept had a meaningful value (Whisman & McClelland, 2005). When both the linear and nonlinear terms were significant, only the parameter estimate for the nonlinear term was interpreted because the lower-order term (linear) is subsumed under the higher-order term (nonlinear). When a Linear x Sex interaction was significant, a simple slope analysis was conducted to examine differences in slope parameters between females and males. We probed significant Nonlinear x Sex interactions in two ways. The first approach examined sex differences in slope parameters (simple slope analysis), and a peak or trough of the association between sleep and an outcome was computed (–Blinear / 2*Bnonlinear) (Singer & Willett, 2003). The second approach compared male and female adolescents’ adjustment at low, average and high levels of the sleep parameter. We re-scaled each of the sleep parameters by centering the intercept at –1.5 SD and +1.5 SD, and examined the sex difference in an adjustment outcome at a low, an average, and a high level of sleep. An online tool was utilized to plot significant interactions (http://www.jeremydawson.co.uk/slopes.htm).
All analyses were conducted in Mplus Version 8 (Muthén & Muthén, 2017), which uses full information maximum likelihood (FIML) estimation to handle missing data. FIML has been shown to have the least biased estimates and the lowest Type I error rates compared to other methods such as listwise or pairwise deletion (Enders & Bandalos, 2001; Raykov, 2005). Data that exceeded 4 SD were winsorized for nonlinear terms of sleep-wake problems (8 cases) and sleepiness (9 cases) and recorded as the score corresponding to 4 SD (Cousineau & Chartier, 2010). Skewness values were less than 2.0 for all variables, suggesting that the variables used in the present study were relatively normally distributed. Missingness for study variables ranged 0–29%, which is within the acceptable range for our sample size (McNeish, 2017).
Results
Table 1 presents correlations, means, and standard deviations for sleep parameters (predictors), externalizing behaviors and internalizing symptoms (outcomes), and covariates. Raw scores of the sleep variables (morningness-eveningness, sleep-wake problems, and sleepiness) were utilized for this preliminary analysis. As seen in Table 1, moderate associations among circadian preference, sleep-wake problems, and sleepiness emerged. In addition, a higher level of evening preference, poorer sleep quality, and sleepiness were each associated with the four adjustment outcomes. Sleep minutes was not associated with any of the externalizing or internalizing variables. Further, T-tests showed that in comparison to males, females had greater sleep minutes (t = 4.05, p < .001), sleepiness (t = 2.83, p < .01), and anxiety (t = 2.89, p < .01) than males.
Table 1.
Bivariate Correlations, Means, and Standard Deviations for Main Study Variables and Covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | – | |||||||||||
| 2. Race/ethnicity | −.07 | – | ||||||||||
| 3. SES | .03 | −.23** | – | |||||||||
| 4. zBMI | −.03 | .29*** | .15 | – | ||||||||
| 5. Sleep minutes | −.34*** | −.18* | .11 | −.11 | – | |||||||
| 6. M-E | .02 | .07 | −.02 | .08 | .13 | – | ||||||
| 7. Sleep-wake problems | −.03 | .00 | .01 | −.06 | −.17 | −.42*** | – | |||||
| 8. Sleepiness | −.21* | .16* | −.12 | .03 | −.06 | −.29*** | .44** | – | ||||
| 9. Externalizing | −.02 | −.08 | −.01 | −.01 | −.06 | −.39*** | .46*** | .30*** | – | |||
| 10. Internalizing | −.13 | .07 | −.05 | .03 | −.15 | −.25*** | .38*** | .43*** | .58*** | – | ||
| 11. Depression | −.08 | .00 | −.14 | −.01 | −.10 | −.33*** | .53*** | .28*** | .61*** | .76*** | – | |
| 12. Anxiety | −.22** | .00 | −.10 | .04 | −.14 | −.21** | .35*** | .37*** | .51*** | .83*** | .70*** | – |
| M | – | – | 2.99 | 0.77 | 397.30 | 27.53 | 19.76 | 13.40 | 49.45 | 49.36 | 7.40 | 8.90 |
| SD | – | – | 1.82 | 1.06 | 56.90 | 4.51 | 7.06 | 4.19 | 9.79 | 12.27 | 8.06 | 8.06 |
| Range (Minimum) | – | – | 0.00 | –2.65 | 228.50 | 15.00 | 10.00 | 9.00 | 29.00 | 27.00 | 0.00 | 0.00 |
| (Maximum) | 8.91 | 2.88 | 506.83 | 41.00 | 50.00 | 36.00 | 76.00 | 95.00 | 36.00 | 33.00 |
Note. Sex was coded as 0 = female, 1 = male; race/ethnicity was coded as 0 = White, 1 = Black. SES = socioeconomic status (income-to-needs ratio); zBMI = standardized body mass index. Sleep minutes: 397.30 minutes = 6 hours, 37 minutes. M-E = Morningness-eveningness; higher score = more morningness. For morningness-eveningness, sleep-wake problems, and sleepiness, raw scores were used for correlations. Externalizing problems and internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
p < .05.
p < .01.
p < .001.
Sleep Minutes
The first regression model examined whether a linear and a nonlinear term of sleep minutes, or the interaction terms between sleep minutes and adolescent sex (Linear x Sex interaction and Nonlinear x Sex interaction), were related to adjustment. No significant associations emerged (Table 2).2
Table 2.
Estimates for Regression Models Showing Linear and Nonlinear Effects for Adolescent Sleep Minutes on Adjustment Variables
| Externalizing | Internalizing | Depression | Anxiety | |
|---|---|---|---|---|
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Intercept | 49.52*** (1.37) | 50.85*** (1.64) | 8.23*** (0.87) | 11.32*** (1.00) |
| Sex | 1.01 (2.23) | −4.12 (2.60) | −1.83 (1.38) | −4.86** (1.59) |
| Race/ethnicity | −1.59 (1.88) | 0.36 (2.33) | −0.30 (1.25) | −1.51 (1.46) |
| SES | 0.01 (0.54) | −0.25 (0.67) | −0.45 (0.37) | −0.46 (0.41) |
| zBMI | −0.02 (0.81) | −0.18 (0.99) | −0.17 (0.60) | 0.05 (0.66) |
| Sleep minutes | 0.33 (1.51) | −2.55 (1.70) | 0.05 (0.93) | −1.48 (1.06) |
| Sleep minutes2 | 1.41 (1.24) | 0.81 (1.41) | −0.45 (0.76) | 0.46 (0.87) |
| Sleep minutes x Sex | −2.82 (2.54) | 0.60 (2.90) | −2.45 (1.56) | −0.37 (1.79) |
| Sleep minutes2 x Sex | −2.49 (1.80) | −0.68 (2.05) | −0.14 (1.10) | −0.02 (1.25) |
| R2 | .04 (0.04) | .05 (0.04) | .06 (0.04) | .11* (0.05) |
Note. Unstandardized parameter estimates and standard errors are reported. Sex was coded as 0 = female, 1 = male; race/ethnicity was coded as 0 = White, 1 = Black. SES = socioeconomic status (income-to-needs ratio); zBMI = standardized body mass index; Externalizing problems and internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
p < .05.
p ≤ .01.
p < .001.
Circadian Preference (Morningness-Eveningness)
The second regression model examined whether a linear and a nonlinear term of morningness-eveningness, or the interaction terms between morningness-eveningness and adolescent sex (Linear x Sex interaction and Nonlinear x Sex interaction), were associated with adolescents’ externalizing and internalizing symptoms. Four linear terms were significant (Table 3). Significant negative linear effects were found for all the adjustment outcomes: greater morningness preference was related to lower levels of externalizing problems, internalizing symptoms, depression, and anxiety. (Table 3). No sex-related effects emerged and thus these associations did not vary significantly between boys and girls.
Table 3.
Estimates for Regression Models Showing Linear and Nonlinear Effects for Adolescent Morningness-Eveningness on Adjustment Variables
| Externalizing | Internalizing | Depression | Anxiety | |
|---|---|---|---|---|
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Intercept | 50.03*** (1.27) | 50.74*** (1.62) | 7.87*** (0.82) | 11.17*** (1.00) |
| Sex | 0.28 (2.01) | −3.97 (2.54) | −0.95 (1.32) | −4.69** (1.61) |
| Race/ethnicity | −1.59 (1.68) | 0.99 (2.18) | −0.36 (1.14) | −1.23 (1.38) |
| SES | −0.55 (0.53) | −0.47 (0.68) | −0.64† (0.36) | −0.50 (0.42) |
| zBMI | 0.32 (0.73) | 0.09 (0.94) | −0.15 (0.55) | 0.11 (0.64) |
| Sleep minutes | 0.01 (0.02) | −0.03 (0.02) | −0.01 (0.01) | −0.03* (0.01) |
| M-E | −4.87*** (1.03) | −3.36** (1.34) | −2.70*** (0.67) | −1.90* (0.81) |
| M-E2 | 0.37 (0.71) | 0.64 (0.92) | 0.38 (0.47) | 0.15 (0.57) |
| M-E x Sex | 2.20 (1.68) | 1.10 (2.19) | 1.30 (1.07) | 1.13 (1.13) |
| M-E2 x Sex | −0.67 (1.17) | −0.56 (1.52) | −0.42 (0.74) | 0.02 (0.90) |
| R2 | .18** (0.06) | .12* (0.05) | .15** (0.05) | .14** (0.05) |
Note. Unstandardized parameter estimates and standard errors are reported. Sex was coded as 0 = female, 1 = male; race/ethnicity was coded as 0 = White, 1 = Black. SES = socioeconomic status (income-to-needs ratio); zBMI = standardized body mass index; M-E = morningness-eveningness. Morningness-eveningness was standardized in analyses; higher score = more morningness. Externalizing problems and internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
p < .10.
p < .05.
p ≤ .01.
p < .001.
Sleep-Wake Problems
The third regression model pertained to sleep-wake problems. Four linear terms were significant (Table 4). Significant positive linear effects were found for all the adjustment outcomes: greater sleep-wake problems were associated with higher levels of externalizing problems, internalizing symptoms, depression, and anxiety. These associations were not moderated by adolescents’ sex.
Table 4.
Estimates for Regression Models Showing Linear and Nonlinear Effects for Adolescent Sleep-Wake Problems on Adjustment Variables
| Externalizing | Internalizing | Depression | Anxiety | |
|---|---|---|---|---|
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Intercept | 49.86*** (1.25) | 51.31*** (1.59) | 8.33*** (0.78) | 11.83*** (0.99) |
| Sex | 1.09 (2.05) | −4.62† (2.59) | −1.70 (1.29) | −5.96*** (1.63) |
| Race/ethnicity | −2.26 (1.61) | 0.05 (2.06) | −0.79 (1.03) | −1.76 (1.31) |
| SES | −0.29 (0.47) | −0.67 (0.60) | −0.62* (0.30) | −0.63† (0.38) |
| zBMI | 0.31 (0.69) | 0.11 (0.89) | −0.05 (0.49) | 0.17 (0.60) |
| Sleep minutes | 0.01 (0.02) | −0.02 (0.02) | 0.00 (0.01) | −0.02† (0.01) |
| Sleep-wake problems | 5.77*** (1.21) | 6.78*** (1.56) | 3.69*** (0.76) | 3.23*** (0.96) |
| Sleep-wake problems2 | 0.31 (1.33) | −2.24 (1.73) | −0.58 (0.86) | −1.86† (1.08) |
| Sleep-wake problems x Sex | −1.77 (1.65) | −3.14 (2.13) | −0.34 (1.03) | −0.80 (1.29) |
| Sleep-wake problems2 x Sex | −1.55 (1.95) | 1.08 (2.51) | 0.97 (1.23) | 2.38 (1.56) |
| R2 | .25*** (0.06) | .21*** (0.06) | .31*** (0.06) | .22*** (0.06) |
Note. Unstandardized parameter estimates and standard errors are reported. Sex was coded as 0 = female, 1 = male; race/ethnicity was coded as 0 = White, 1 = Black. SES = socioeconomic status (income-to-needs ratio); zBMI = standardized body mass index. Sleep-wake problems were standardized in analyses. Externalizing problems and internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
p ≤ .10.
p ≤ .05.
p < .01.
p < .001.
Sleepiness
The final regression model examined sleepiness as the predictor of adolescents’ adjustment. One linear term and three Nonlinear x Sex interactions were significant (Table 5). Sleepiness was linearly associated with externalizing behaviors, such that greater sleepiness was related to higher levels of externalizing behaviors.
Table 5.
Estimates for Regression Models Showing Linear and Nonlinear Effects for Adolescent Sleepiness on Adjustment Variables
| Externalizing | Internalizing | Depression | Anxiety | |
|---|---|---|---|---|
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Intercept | 50.85*** (1.38) | 14.22*** (1.22) | 9.53*** (0.87) | 12.12*** (0.10) |
| Sex | −1.24 (2.26) | −7.58*** (1.99) | −3.82** (1.44) | −5.87*** (1.66) |
| Race/ethnicity | −2.59 (1.77) | −1.88 (1.57) | −1.86 (1.16) | −2.65* (1.32) |
| SES | 0.12 (0.52) | −0.20 (0.49) | −0.67† (0.35) | −0.40 (0.39) |
| zBMI | 0.12 (0.75) | 0.35 (0.66) | −0.06 (0.56) | 0.33 (0.61) |
| Sleep minutes | 0.00 (0.02) | −0.03* (0.14) | −0.01 (0.01) | −0.02* (0.01) |
| Sleepiness | 3.57** (1.18) | 5.06*** (1.05) | 3.28*** (0.78) | 3.11*** (0.88) |
| Sleepiness2 | −0.41 (1.41) | −2.83* (1.26) | −2.70** (0.91) | −1.74† (1.03) |
| Sleepiness x Sex | −1.52 (2.04) | 0.62 (1.82) | −1.01 (1.33) | 1.52 (1.52) |
| Sleepiness2 x Sex | 3.01 (2.45) | 5.45* (2.18) | 4.63** (1.60) | 4.56* (1.82) |
| R2 | .11* (0.05) | .29*** (0.06) | .17** (0.06) | .24*** (0.06) |
Note. Unstandardized parameter estimates and standard errors are reported. Sex was coded as 0 = female, 1 = male; race/ethnicity was coded as 0 = White, 1 = Black. SES = socioeconomic status (income-to-needs ratio); zBMI = standardized body mass index. Sleepiness was standardized in analyses. Externalizing problems and internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
p ≤ .10.
p ≤ .05.
p < .01.
p ≤ .001.
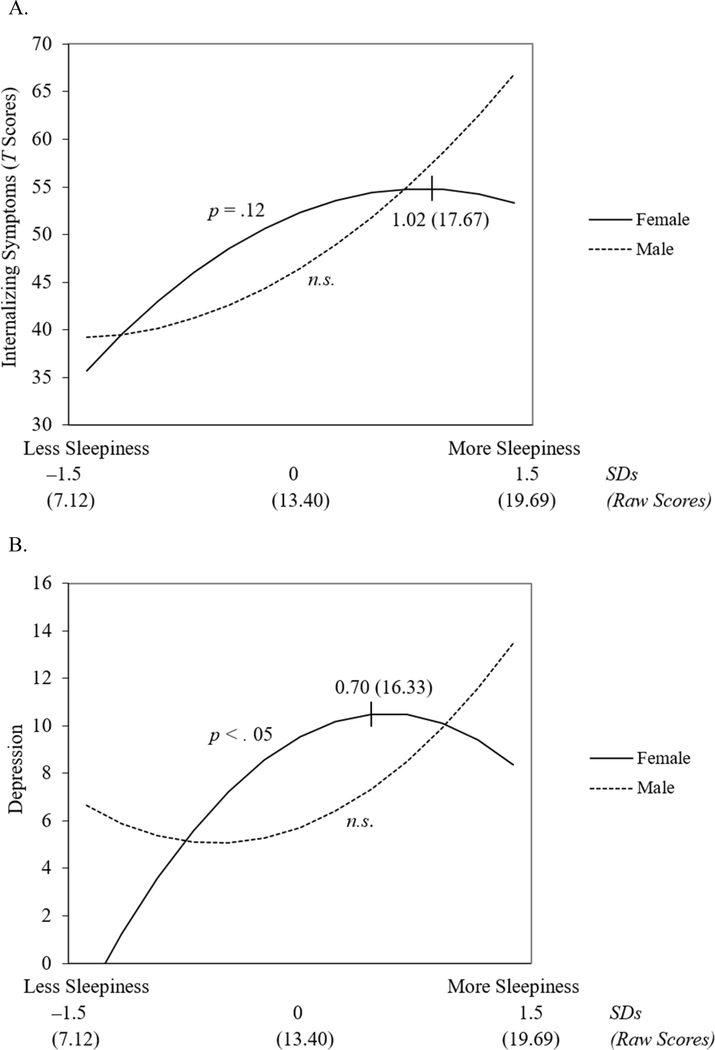
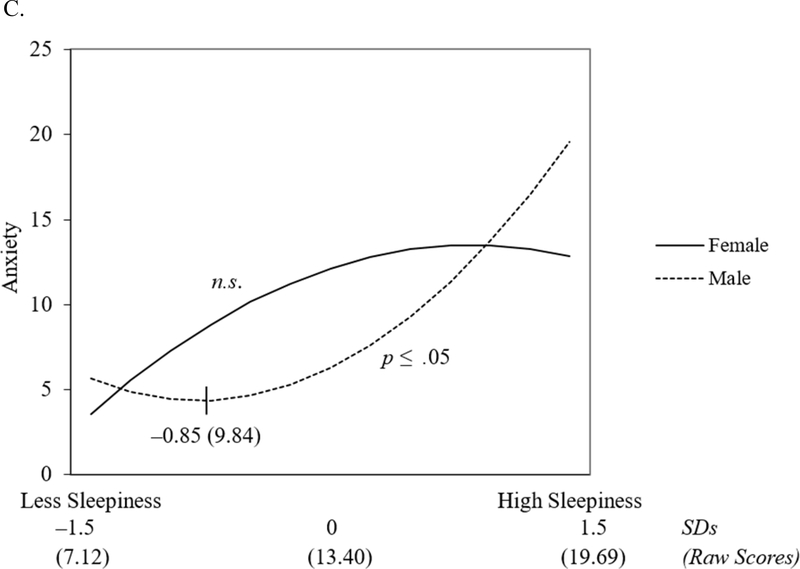
Significant Nonlinear x Sex interactions were found for internalizing symptoms, depression, and anxiety (Table 5). Per the aforementioned description of our analysis plan, we assessed the sex-related effects in nonlinear associations between sleepiness and adjustment in two ways: differences in the shape of the slope (simple slope analyses) between boys and girls, and differences between boys and girls in adjustment at low, average, and high levels of sleepiness. Results of the simple slope analyses indicated that females showed a rapid acceleration in internalizing symptoms (p = .12) (Figure 1A) and depression (Figure 1B) that plateaued or slightly decreased between average and high levels of sleepiness. The highest levels of internalizing symptoms and depression were found at l .02 SD (raw score = 17.67) and 0.70 SD (raw score = 16.33) above the mean of the sleepiness score, respectively. For males, the slopes representing the associations between sleepiness and both overall internalizing symptoms and depression were not significant. Furthermore, the slope representing the association between sleepiness and anxiety symptoms was significant only for males and illustrated a delayed acceleration in anxiety (Figure 1C), with a steep increase occurring at 0.85 SD (raw score = 9.84) below the average sleepiness score. The highest level of anxiety was detected at 1.5 SD above the average sleepiness score (raw score = 19.69).
Figure 1.
Nonlinear effect for standardized sleepiness2 and sex predicting (A) internalizing symptoms, (B) depression, and (C) anxiety. Points were plotted at ± 1.5 SDs for standardized sleepiness. Peaks and troughs of nonlinear curves are represented in SDs with raw scores in parentheses. Internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
As a second way of probing interaction effects, we examined sex differences in adjustment outcomes at various levels of sleepiness. We re-scaled sleepiness by centering the intercept at –1.5 SD and +1.5 SD. A parameter estimate for sex (Bsex) in each of the original (Table 5 for an average level) and the re-scaled models represented the sex difference in an adjustment score (male mean score minus female mean score). The results indicated that, at an average sleepiness level, females had greater internalizing symptoms, Bsex = –7.58 (Figure 1A), depression, Bsex = –3.82 (Figure 1B), and anxiety, Bsex = –5.87 (Figure 1C) than males, ps < .01. At a lower level of sleepiness (–1.5 SD), males had greater depression, Bsex = 6.64, p < .05 (Figure 1B) than females. At a higher level of sleepiness (+1.5 SD), males showed greater internalizing symptoms, Bsex = 13.49, p < .05 (Figure 1A), and anxiety, Bsex = 6.70, p < .05 (Figure 1C) than females, which were the highest levels of these outcomes observed across sex and sleepiness levels. No sex differences emerged in internalizing symptoms and anxiety at a low level of sleepiness, or in depression at a high level of sleepiness.
Summary of Findings
We summarized the results of all the models reported above (Table 6).3 Only the significant effects (linear, nonlinear, Linear x Sex interaction, or Nonlinear x Sex interaction) were presented. Morningness-eveningness, sleep-wake problems, and sleepiness were associated with all adjustment outcomes (externalizing behaviors, internalizing symptoms, depression, and anxiety), but sleep minutes was not. There were twelve linear effects, two nonlinear effects, and three Nonlinear x Sex interactions. The largest number of significant effects was found for internalizing symptoms and depression.
Table 6.
Summary of Significant Linear and Nonlinear Effects
| Externalizing | Internalizing | Depression | Anxiety | |
|---|---|---|---|---|
| Sleep Minutes | ||||
| Morningness-Eveningness | Linear | Linear | Linear | Linear |
| Sleep-Wake Problems | Linear | Linear | Linear | Linear |
| Sleepiness | Linear | Linear | Linear | Linear |
| Nonlinear | Nonlinear | |||
| Nonlinear x Sex | Nonlinear x Sex | Nonlinear x Sex |
Note. Externalizing problems and internalizing symptoms were derived with YSR (T scores); depression symptoms were derived with CDI; anxiety symptoms were derived with RCMAS-2.
Discussion
Despite a growing body of work examining linear associations between sleep and socioemotional adjustment in adolescence, studies examining nonlinear associations are scarce. Moreover, the few existing studies that examined such nonlinear associations in youth tended to assess sleep duration. Utilizing multiple sleep-wake parameters (sleep minutes, morningness-eveningness, sleep quality, sleepiness), we investigated linear and nonlinear associations between sleep and socioemotional adjustment in a community sample of high school students, and examined adolescent sex as a moderator of effects. We controlled sleep minutes in the models involving sleep-wake parameters to ascertain their unique effects on outcomes independent of sleep minutes. Both eveningness and sleep quality problems were associated in a linear fashion with externalizing behavior and internalizing symptoms. In addition, nonlinear relations between sleepiness and internalizing symptoms were found and were moderated by adolescents’ sex.
Notable changes in sleep occur in late adolescence (Crowley, Wolfson, Tarokh, & Carskadon, 2018), and the linear relations between eveningness preference and adjustment problems in the present investigation are consistent with prior work utilizing various sleep and outcome measures in samples of youth ranging in age between 11 and 18 (Díaz-Morales, 2016; Kaur & Tung, 2017; Lange & Randler, 2011). Highlighting the importance of adolescents’ chronotype for their adjustment, results held even with covarying sleep duration in our models.
Positive linear relations also emerged between sleep-wake problems and negative adjustment outcomes independent of sleep minutes. Results from the present investigation corroborate others that reported linear associations between sleep quality problems and adolescents’ poorer adjustment (Alfano, Zakem, Costa, Taylor, & Weems, 2009; El-Sheikh, Kelly, Buckhalt, & Hinnant, 2010; Meijer, Reitz, Dekovic, van den Wittenboer, & Stoel, 2010). One study investigated non-linear relations between sleep quality and mental health in 9-year-olds (El-Sheikh et al., 2019) and demonstrated that the association between sleep-wake problems and teacher-reported internalizing symptoms was nonlinear, rapidly increasing from low to average levels of sleep problems and then plateauing. Developmental changes in sleep occur throughout adolescence (Crowley et al., 2018). Thus, the discrepancy in the shapes of the associations between sleep-wake problems and adjustment may be due in part to age differences or other sample characteristics. Obviously, no firm conclusions can be made until more studies investigate both linear and nonlinear associations between sleep and developmental outcomes.
Associations between daytime sleepiness and adolescents’ internalizing symptoms were nonlinear in nature. Specifically, nonlinear associations emerged between daytime sleepiness and overall internalizing, depression, and anxiety; the latter approached a conventional level of statistical significance. These findings contribute to the literature in two ways. First, consistent with the Feinberg’s (2013) propositions, our results suggest that daytime sleepiness is related to adolescents’ functioning independent of sleep minutes. This highlights the importance of examining variables other than sleep duration, including sleepiness, which taps into sleep need and vulnerability to sleep loss (Dewald, Meijer, Oort, Kerkhof, & Bögels, 2010). Excessive daytime sleepiness compromises alertness and neurobehavioral functioning (Dewald et al., 2010; Gregory & Sadeh, 2012; Millman, 2005), thereby increasing risk for emotional, behavioral and cognitive problems (Fallone, Owens, & Deane, 2002).
Second, the nonlinear associations involving daytime sleepiness also demonstrate the importance of examining adolescents’ sex as a moderator of relations between sleep-wake processes and socioemotional adjustment. Females showed a rapid acceleration in internalizing symptoms and depression that plateaued between average and high levels of sleepiness, whereas males showed a delayed acceleration in anxiety that steeply increased between average and high levels of sleepiness. It appears that females’ vulnerability to internalizing symptoms, particularly depression, is maximized at an average level of sleepiness, but males’ vulnerability to anxiety is pronounced at a higher level of sleepiness. Females’ vulnerability to internalizing symptoms at average levels of sleepiness and males’ vulnerability to anxiety at higher levels of sleepiness were corroborated by analyses that examined sex differences in adjustment at various levels of sleepiness.
Girls experience higher levels of anxiety and depressive symptoms across the adolescent years compared to boys (Hankin et al., 1998; Letcher, Sanson, Smart, & Toumbourou, 2012), suggesting that girls may be more susceptible to at least some risk factors for internalizing symptoms than boys (e.g., Alloy, Hamilton, Hamlat, & Abramson, 2016; Hamilton, Stange, Abramson, & Alloy, 2015; Shih, Eberhart, Hammen, & Brennan, 2006). Results of the present study suggest that even moderate levels of sleepiness may be sufficient to increase risk for depressive and internalizing symptoms among girls, with more extreme levels of sleepiness maintaining but not increasing the risk. In contrast, if boys are less susceptible to some risk factors for internalizing symptoms, only more extreme levels of sleepiness may increase risk for anxiety among boys. Although this interpretation is plausible, it is unclear why similar results were not found for other combinations of sleep and internalizing variables. Tests of sex differences in non-linear associations between sleep and socioemotional adjustment were novel and exploratory, and the explanation for results is post-hoc and requires further research before conclusions can be drawn.
Sleep duration was not associated with externalizing problems or internalizing symptoms, neither linearly nor nonlinearly. These findings are not consistent with other studies that have examined linear associations between sleep duration assessed through actigraphy and externalizing and internalizing symptoms in youth (Aronen, Paavonen, Fjallberg, Soininen, & Torronen, 2000; Kelly & El-Sheikh, 2014). Our results also stand in contrast to recent findings in the literature of nonlinear associations between sleep duration and adjustment. For example, a study with Mexican-American adolescents demonstrated a U-shape pattern of shorter and longer sleep durations relating to externalizing problems and internalizing symptoms (Fuligni et al., 2018). A similar trend was found in a study of younger children (James & Hale, 2017). Both studies utilized subjective reports of sleep, the former using daily diaries and the latter using parent reports, and also varied along other methodological features and sample characteristics.
Results of the present study should be interpreted with several limitations in mind. Although our sample is socioeconomically and ethnically diverse, it is composed of older adolescents living in semi-rural areas and relatively small towns in south eastern USA, which may limit generalizability to youth of other ages and locales. Additionally, youth in our sample were attending high school during the day. In other parts of the world where vocational training programs are more common, such as South America and Europe (Gerber et al., 2015), daytime work schedules for teens have been associated with shorter nocturnal sleep, later onset and earlier wake times, and higher daytime sleepiness than nonworking students (Teixeira, Fischer, de Andrade, Louzada, & Nagai, 2004). Thus, the generalizability of our findings may further be limited. Finally, the cross-sectional study design precludes inferences regarding causality. Notwithstanding these limitations, our findings shed additional light on the importance of examining multiple sleep-wake parameters, nonlinear associations between sleep and adjustment, and the moderating effects of sex on these relations.
Acknowledgements
This study was supported by funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01-HD046795) awarded to M. El-Sheikh. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We wish to thank our participants and the lab staff, most notably Bridget Wingo and Lori Elmore-Staton, for data collection and preparation.
Footnotes
Declaration of Interest Statement
None of the authors has a financial conflict.
The present study is distinct from El-Sheikh et al.’s (2019) with younger children and the two studies are based on two entirely independent samples.
We also examined whether a linear and a nonlinear term of actigraph-measured sleep efficiency, or the interactions between sleep efficiency and adolescent sex (linear x sex interaction and nonlinear x sex interaction), were related to externalizing and internalizing symptoms, but no significant associations emerged.
We also fit the models excluding sleep minutes and compared them to those that covaried sleep minutes. The statistical significance of the two sets of models did not vary and there were only slight variations in coefficient values.
References
- Achenbach TM, & Rescorla L (2001). ASEBA school-age forms & profiles. Burlington, VT: ASEBA. [Google Scholar]
- Alfano CA, Zakem AH, Costa NM, Taylor LK, & Weems CF (2009). Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depression and Anxiety, 26(6), 503–512. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Hamilton JL, Hamlat EJ, & Abramson LY (2016). Pubertal development, emotion regulatory styles, and the emergence of sex differences in internalizing disorders and symptoms in adolescence. Clinical Psychological Science, 4(5), 867–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronen ET, Paavonen EJ, Fjallberg M, Soininen M, & Torronen J (2000). Sleep and psychiatric symptoms in school-aged children. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 502–508. 10.1097/00004583-200004000-00020 [DOI] [PubMed] [Google Scholar]
- Blunden S, & Galland B (2014). The complexities of defining optimal sleep: Empirical and theoretical considerations with a special emphasis on children. Sleep Medicine Reviews, 18(5), 371–378. doi: 10.1016/j.smrv.2014.01.002 [DOI] [PubMed] [Google Scholar]
- Campbell IG, Higgins LM, Trinidad JM, Richardson P, & Feinberg I (2007). The increase in longitudinally measured sleepiness across adolescence is related to the maturational decline in low-frequency EEG power. Sleep, 30(12), 1677–1687. doi: 10.1093/sleep/30.12.1677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA (2011). Sleep in adolescents: The perfect storm. Pediatric Clinics of North America, 58(3), 637–647. doi: 10.1016/j.pcl.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Acebo C, & Jenni OG (2004). Regulation of adolescent sleep: Implications for behavior. Annals of the New York Academy of Sciences, 1021(1), 276–291. doi: 10.1196/annals.1308.032 [DOI] [PubMed] [Google Scholar]
- Chung K-F, & Cheung M-M (2008). Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep, 31(2), 185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, & Aiken LS (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Cousineau D, & Chartier S (2010). Outliers detection and treatment: A review. International Journal of Psychological Research, 3(1), 58–67. [Google Scholar]
- Crowley SJ, Tarokh L, & Carskadon MA (2014). Sleep during adolescence In Sheldon SH, Kryger MH, Ferber R, & Gozal D (Eds.), Principles and practice of pediatric sleep medicine (2nd ed., pp. 45–52). London, UK: Elsevier Saunders. [Google Scholar]
- Crowley SJ, Wolfson AR, Tarokh L, & Carskadon MA (2018). An update on adolescent sleep: New evidence informing the perfect storm model. Journal of Adolescence, 67, 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, & Bögels SM (2010). The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews, 14(3), 179–189. doi: 10.1016/j.smrv.2009.10.004 [DOI] [PubMed] [Google Scholar]
- Díaz-Morales JF (2016). Anxiety during adolescence: Considering morningness-eveningness as a risk factor. Sleep and Biological Rhythms, 14(2), 141–147. [Google Scholar]
- El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, & Buckhalt JA (2013). Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychology, 32(8), 849–859. doi: 10.1037/a0030413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RJ, Buckhalt JA, & Hinnant JB (2010). Children’s sleep and adjustment over time: The role of socioeconomic context. Child Development, 81(3), 870–883. doi: 10.1111/j.1467-8624.2010.01439.x [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Philbrook LE, Kelly RJ, Hinnant JB, & Buckhalt JA (2019). What does a good night’s sleep mean? Nonlinear relations between sleep and children’s cognitive functioning and mental health. Sleep, 42(6), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457. doi: 10.1207/s15328007sem0803_5 [DOI] [Google Scholar]
- Fallone G, Owens JA, & Deane J (2002). Sleepiness in children and adolescents: Clinical implications. Sleep Medicine Reviews, 6(4), 287–306. [DOI] [PubMed] [Google Scholar]
- Feinberg I (2013). Recommended sleep durations for children and adolescents: The dearth of empirical evidence. Sleep, 36(4), 461–462. doi: 10.5665/sleep.2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, Arruda EH, Krull JL, & Gonzales NA (2018). Adolescent sleep duration, variability, and peak levels of achievement and mental health. Child Development, 89(2), e18–e28. doi: 10.1111/cdev.12729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber M, Lang C, Feldmeth AK, Elliot C, Brand S, Holsboer‐Trachsler E, & Pühse U (2015). Burnout and mental health in Swiss vocational students: The moderating role of physical activity. Journal of Research on Adolescence, 25(1), 63–74. [Google Scholar]
- Gregory AM, & Sadeh A (2012). Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews, 16(2), 129–136. doi: 10.1016/j.smrv.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Hamilton JL, Stange JP, Abramson LY, & Alloy LB (2015). Stress and the development of cognitive vulnerabilities to depression explain sex differences in depressive symptoms during adolescence. Clinical Psychological Science, 3(5), 702–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, & Angell KE (1998). Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology, 107(1), 128–140. [DOI] [PubMed] [Google Scholar]
- Hershner SD, & Chervin RD (2014). Causes and consequences of sleepiness among college students. Nature and Science of Sleep, 6, 73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S, & Hale L (2017). Sleep duration and child well-being: A nonlinear association. Journal of Clinical Child & Adolescent Psychology, 46(2), 258–268. doi: 10.1080/15374416.2016.1204920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalak N, Brand S, Beck J, Holsboer-Trachsler E, & Wollmer MA (2015). Association between subjective actual sleep duration, subjective sleep need, age, body mass index, and gender in a large sample of young adults. Neuropsychiatric Disease and Treatment, 11, 107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur P, & Tung S (2017). Risk taking behaviours among early adolescents in relation with morningness-eveningness and depressive symptoms. Indian Journal of Health and Wellbeing, 8(5), 388–390. [Google Scholar]
- Kelly RJ, & El-Sheikh M (2014). Reciprocal relations between children’s sleep and their adjustment over time. Developmental Psychology, 50(4), 1137–1147. doi: 10.1037/a0034501 [DOI] [PubMed] [Google Scholar]
- Kovacs M (1992). Children’s Depression Inventory. North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Lange L, & Randler C (2011). Morningness-eveningness and behavioural problems in adolescents. Sleep and Biological Rhythms, 9(1), 12–18. [Google Scholar]
- Letcher P, Sanson A, Smart D, & Toumbourou JW (2012). Precursors and correlates of anxiety trajectories from late childhood to late adolescence. Journal of Clinical Child & Adolescent Psychology, 41(4), 417–432. [DOI] [PubMed] [Google Scholar]
- Lewandowski AS, Toliver-Sokol M, & Palermo TM (2011). Evidence-based review of subjective pediatric sleep measures. Journal of Pediatric Psychology, 36(7), 780–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Zhang J, Li SX, Chan NY, Yu MWM, Lam SP, . . . Wing YK (2019). Excessive daytime sleepiness among children and adolescents: Prevalence, correlates, and pubertal effects. Sleep Medicine, 53, 1–8. doi: 10.1016/j.sleep.2018.08.028 [DOI] [PubMed] [Google Scholar]
- Mählmann L, Gerber M, Furlano RI, Legeret C, Kalak N, Holsboer-Trachsler E, & Brand S (2017). Impaired objective and subjective sleep in children and adolescents with inflammatory bowel disease compared to healthy controls. Sleep Medicine, 39, 25–31. [DOI] [PubMed] [Google Scholar]
- Matricciani L, Blunden S, Rigney G, Williams MT, & Olds TS (2013). Children’s sleep needs: Is there sufficient evidence to recommend optimal sleep for children? Sleep, 36(4), 527–534. doi: 10.5665/sleep.2538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin DL, & Alfano CA (2015). Sleep and anxiety in late childhood and early adolescence. Current Opinion in Psychiatry, 28(6), 483–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish D (2017). Missing data methods for arbitrary missingness with small samples. Journal of Applied Statistics, 44(1), 24–39. [Google Scholar]
- Meijer AM, Reitz E, Dekovic M, van den Wittenboer GL, & Stoel RD (2010). Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. Journal of Child Psychology and Psychiatry, 51(11), 1278–1286. doi: 10.1111/j.1469-7610.2010.02261.x [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Montgomery-Downs HE, Insana SP, & Walsh CM (2012). Use of actigraphy for assessment in pediatric sleep research. Sleep Medicine Reviews, 16(5), 463–475. doi: 10.1016/j.smrv.2011.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikanto I, Pesonen A-K, Kuula L, Lahti J, Heinonen K, Kajantie E, & Räikkönen K (2017). Eveningness as a risk for behavioral problems in late adolescence. Chronobiology International, 34(2), 225–234. doi: 10.1080/07420528.2016.1267739 [DOI] [PubMed] [Google Scholar]
- Millman RP (2005). Excessive sleepiness in adolescents and young adults: Causes, consequences, and treatment srategies. Pediatrics, 115(6), 1774–1786. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Author. [Google Scholar]
- National Sleep Foundation. (2006). Sleep in America Poll. Retrieved from https://sleepfoundation.org/sites/default/files/2006_summary_of_findings.pdf
- Owens JA (2014). Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics, 134(3), e921–e932. doi: 10.1542/peds.2014-1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JA, Belon K, & Moss P (2010). Impact of delaying school start time on adolescent sleep, mood, and behavior. Archives of Pediatrics & Adolescent Medicine, 164(7), 608–614. [DOI] [PubMed] [Google Scholar]
- Pieters S, Burk WJ, Van der Vorst H, Dahl RE, Wiers RW, & Engels RC (2015). Prospective relationships between sleep problems and substance use, internalizing and externalizing problems. Journal of Youth and Adolescence, 44(2), 379–388. doi: 10.1007/s10964-014-0213-9 [DOI] [PubMed] [Google Scholar]
- Randler C (2011). Association between morningness–eveningness and mental and physical health in adolescents. Psychology, Health & Medicine, 16(1), 29–38. [DOI] [PubMed] [Google Scholar]
- Raykov T (2005). Analysis of longitudinal studies with missing data using covariance structure modeling with full-information maximum likelihood. Structural Equation Modeling, 12(3), 493–505. doi: 10.1207/s15328007sem1203_8 [DOI] [Google Scholar]
- Reynolds CR, & Richmond BO (2008). Revised Children’s Manifest Anxiety Scale (RCMAS-2) (2nd ed.). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, & Merrow M (2004). A marker for the end of adolescence. Current Biology, 14(24), R1038–R1039. [DOI] [PubMed] [Google Scholar]
- Sadeh A (2015). III. Sleep assessment methods. In El-Sheikh M & Sadeh A (Eds.), Sleep and development: Advancing theory and research (Vol. 80, pp. 33–48). [DOI] [PubMed] [Google Scholar]
- Sadeh A, Dahl RE, Shahar G, & Rosenblat-Stein S (2009). Sleep and the transition to adolescence: A longitudinal study. Sleep, 32(12), 1602–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A, Sharkey KM, & Carskadon MA (1994). Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep, 17(3), 201–207. doi: 10.1093/sleep/17.3.201 [DOI] [PubMed] [Google Scholar]
- Shih JH, Eberhart NK, Hammen CL, & Brennan PA (2006). Differential exposure and reactivity to interpersonal stress predict sex differences in adolescent depression. Journal of Clinical Child and Adolescent Psychology, 35(1), 103–115. [DOI] [PubMed] [Google Scholar]
- Short MA, Gradisar M, Lack LC, Wright H, & Carskadon MA (2012). The discrepancy between actigraphic and sleep diary measures of sleep in adolescents. Sleep Medicine, 13(4), 378–384. [DOI] [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press. [Google Scholar]
- Teixeira LR, Fischer FM, de Andrade MMM, Louzada FM, & Nagai R (2004). Sleep patterns of day-working, evening high-schooled adolescents of São Paulo, Brazil. Chronobiology International, 21(2), 239–252. [DOI] [PubMed] [Google Scholar]
- Umlauf MG, Bolland JM, & Lian BE (2011). Sleep disturbance and risk behaviors among inner-city African-American adolescents. Journal of Urban Health, 88(6), 1130–1142. doi: 10.1007/s11524-011-9591-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon L, Modecki KL, & Barber BL (2018). Mobile phones in the bedroom: Trajectories of sleep habits and subsequent adolescent psychosocial development. Child Development, 89(1), 66–77. [DOI] [PubMed] [Google Scholar]
- Vilela T. d. S., Bittencourt LRA, Tufik S, & Moreira GA (2016). Factors influencing excessive daytime sleepiness in adolescents. Jornal de Pediatria, 92(2), 149–155. [DOI] [PubMed] [Google Scholar]
- Whisman MA, & McClelland GH (2005). Designing, testing, and interpreting interactions and moderator effects in family research. Journal of Family Psychology, 19(1), 111–120. doi: 10.1037/0893-3200.19.1.111 [DOI] [PubMed] [Google Scholar]
- Wolfson AR, & Carskadon MA (1998). Sleep schedules and daytime functioning in adolescents. Child Development, 69(4), 875–887. doi: 10.1111/j.1467-8624.1998.tb06149.x [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, & Martin JL (2003). Evidence for the validity of a sleep habits survey of adolescents. Sleep, 26(2), 213–216. [DOI] [PubMed] [Google Scholar]
- Zhai L, Zhang H, & Zhang D (2015). Sleep duration and depression among adults: A meta-analysis of prospective studies. Depression and Anxiety, 32(9), 664–670. doi: 10.1002/da.22386 [DOI] [PubMed] [Google Scholar]