Abstract
Since 2009, the Neurosciences Intensive Care Nursery at Johns Hopkins Children’s Center has provided a multidisciplinary approach toward the care of newborns with neurological disorders. The program’s cornerstone is an interdisciplinary approach that involves the primary neonatology team plus experts from more than 10 specialties who convene at a weekly team conference at which newborns with neurological problems are discussed in detail. This interdisciplinary approach fosters in-depth discussion of clinical issues to optimize the management of neonates with neurological problems as well as the opportunity to generate research ideas and provide education about neonatal neuroscience at all levels (faculty, nurses, and trainees). The purpose of this article is to provide a 10-year reflection of our Neurosciences Intensive Care Nursery with a view toward expanding efforts in the 3 areas of our mission: clinical care, research, and education. We hope that our experience will enhance the spread of neonatal neuroscience education, care, and research as widely as possible.
Keywords: neonates, multidisciplinary care, neurosciences
There is a significant, currently unmet need for specialized neurological care of critically ill newborns in neonatal intensive care units. Several prior publications have described the evolution of neonatal neurocritical care services across the United States and Canada.1–3 The initial report, in 2011,4 addressed the benefits of expedited neonatology, neurology, and neurosurgery comanagement of newborns with acute neurological needs, including rapid access to brain monitoring, imaging, and consultations by experts trained in the management of a wide variety of neurological illnesses affecting newborns. As the list of neurological disorders that are encountered in the neonatal intensive care unit continues to expand (Table 1), so do increasing opportunities for novel management and therapeutics. This knowledge gap has necessitated the training of individuals from multiple specialties in neonatal-specific issues, and in response, several dedicated fellowship programs in neonatal neurology and neurocritical care have been established.5
Table 1.
Selected Diagnoses Among Infants Seen at the NICN at Johns Hopkins Hospital.
| Encephalopathy | Secondary to HIE or other causes |
| Seizures | Multiple etiologies, including HIE, stroke, infection, electrolyte disturbances, inborn metabolic errors, brain malformations |
| Brain malformations | Focal cortical dysplasia, schizencephaly, polymicrogyria, subcortial band heterotopias, periventricular nodular heterotopias |
| Metabolic | Inborn errors of metabolism, genetic epileptic encephalopathies |
| Neurosurgical | Hydrocephalus/ventriculomegaly, vascular anomalies, congenital brain malformations, intracranial tumors and cysts, traumatic injuries, myelomeningocele/spinal anomalies |
| Cerebrovascular | Intraventricular hemorrhage, stroke (fetal-remote, perinatal, venous ischemic), subdural/epidural/subpial hemorrhage, intraparenchymal hemorrhage, vascular malformations including vein of Galen malformation, cerebral sinovenous thrombosis |
| Musculoskeletal | Brachial plexus injuries during birth, neuromuscular junction disorders including spinal muscular atrophy, congenital and transient neonatal myasthenia gravis, myopathies, peripheral neuropathies |
| Infectious | Meningitis/encephalitis and other central nervous system infections including Zika virus |
| Toxic | Neurological sequelae from in utero drug exposures |
Abbreviations: HIE, hypoxic–ischemic encephalopathy; NICN, Neurosciences Intensive Care Nursery.
The rise in neonatal neurocritical care as a subspecialty has also provided benefits to populations at risk of long-term neurological comorbidity, including patients with hypoxic–ischemic encephalopathy,6 very preterm infants with neurological morbidity, patients with congenital central nervous system anomalies and prenatal exposures, and children with congenital heart disease, including those receiving extracorporeal membrane oxygenation who are at increased risk for white matter injury and stroke.7,8 The availability of dedicated pediatric neurologists and other neuroscience clinicians in the neonatal intensive care unit has enhanced neurologic care across institutions.3 Furthermore, the increased application of informative electroencephalogram (EEG) techniques in neonates, including continuous EEG monitoring,9 and the increased sophistication and utilization of neuroimaging techniques such as magnetic resonance imaging (MRI) and cranial ultrasonography10,11 have become instrumental components of a neonatal intensive care unit that provides state-of-the-art neurological care.
Mounting evidence supports a multidisciplinary approach to the management of neurological disorders in the neonatal intensive care unit for optimizing care, and standardization of some management practices, leading to improved patient outcomes. Our Neurosciences Intensive Care Nursery specialists work together to establish protocols to promote neuroprotection and brain recovery from injury such as hypoxic–ischemic encephalopathy, stroke, intracranial hemorrhage, seizures, and central nervous system infections while also initiating measures that might prevent further injury, that is, optimizing brain perfusion, cerebral autoregulation, and oxygenation.12–20 Standardization of video EEG monitoring during therapeutic hypothermia has resulted in improved rapid seizure detection, optimization of EEG recording techniques, and reduced use of unnecessary antiseizure medications in this vulnerable population.21 Additional collaborative research has identified key imaging and clinical signs associated with long-term outcomes among preterm children with post-hemorrhagic hydrocephalus.22–24 Recent projects have led to improved understanding of the immediate and long-term consequences of neonatal cerebellar injury.25 Ongoing research efforts can pave the way toward the widespread use of molecular biomarkers for the evaluation of newborns with brain injury.26
Beginnings of the Johns Hopkins Hospital Neurosciences Intensive Care Nursery
In 2009, several faculty at Johns Hopkins Hospital with an interest in neonatal neurological care established our Neurosciences Intensive Care Nursery, based on successes at other institutions such as the Children’s National Medical Center in Washington, District of Columbia, and the University of California, San Francisco,4 and in an effort to address a growing gap in specialized neonatal neurocritical care. Our program arose from the vision of several clinical leaders, including Dr Frances J. Northington (neonatologist), Dr Thierry A.G.M. Huisman (pediatric neuroradiologist), and Dr Adam Hartman (pediatric neurologist) with the goal to provide optimal neonatal neurocritical care by means of a multidisciplinary approach. The support of Dr Edward Lawson, the division chief of neonatology at Hopkins at the time, was instrumental in fostering the Neurosciences Intensive Care Nursery program in its early stages. Early discussions with Drs Michael Johnston, Ali Fatemi, and Marilee Allen of the Kennedy Krieger Institute ensured that our Neurosciences Intensive Care Nursery program included a strong neurodevelopmental focus, including early assessment in the neonatal intensive care unit. Integrated infant follow-up clinics (now called the Infant Neurodevelopment Center) were established at the Hopkins-affiliated Kennedy Krieger Institute, located adjacent to the John Hopkins Children’s Center and at the nearby Mount Washington Pediatric Hospital (which focuses on rehabilitation and long-term care), ensuring ongoing collaborative care for Neurosciences Intensive Care Nursery graduates and their families. Funding for our Neurosciences Intensive Care Nursery was initially provided by a generous grant from the Dana and Albert R. Broccoli Charitable Foundation, and subsequently we have received funding from the Pakula Family to support research of junior faculty.
During the acute stage following birth, Neurosciences Intensive Care Nursery patients are physically housed in the Johns Hopkins neonatal intensive care unit, staffed by the neonatology teams who request consultations from various subspecialists as appropriate. The centerpiece of our Neurosciences Intensive Care Nursery program is a weekly multidisciplinary team conference at which the clinical care, neuroimaging findings, electrophysiological studies, and other patient data are discussed in detail by all services involved, with the aim of improving the clinical management of neurologically ill newborns. Numerous faculties from allied fields (associated with the neonatal neurosciences) contribute to the care of each Neurosciences Intensive Care Nursery patient. Our multidisciplinary approach is unique and, per our understanding, unparalleled across all institutions that provide neonatal neurocritical care.
A typical case presentation during the Neurosciences Intensive Care Nursery weekly meeting begins with a summary of the infant’s neonatal intensive care unit course by the neonatology team, followed by an update on the current neurological status and examination by the consulting neurology team. Fetal and postnatal neuroimaging is reviewed by the pediatric neuroradiologists to assist with prospective planning and management. The EEG findings are presented by our epileptologist or neonatal neurology fellow. A neurosurgeon is available to comment on any neurosurgical needs that the baby might have. Neurodevelopmental specialists comment on expected short- and long-term outcomes for each infant, offering an important and highly appreciated perspective that can be communicated to families. Finally, neuroscientists in attendance are able to provide insight into any ongoing research that can impact the team’s understanding of the patient’s pathophysiology. Any questions pertaining to management are thoroughly discussed among the various experts, which often results in a rich and far-reaching discussion. Perhaps most importantly, a timely update is provided to the family of each newborn discussed, by the primary neonatology team, promptly after the Neurosciences Intensive Care Nursery conference, representing the aggregate consensus of the multiple specialists. If appropriate, specialists also participate in this family discussion. Families greatly appreciate this timely multidisciplinary feedback.
The weekly Neurosciences Intensive Care Nursery conference continues to be regarded and attended enthusiastically by attendees. Over the decade since its inception, the initial enthusiasm about our Neurosciences Intensive Care Nursery has continued and increased, generating a current program that is vigorous and comprehensive. Although the cadre of specialists has changed over the years, the original core principles and vision continue to form the basis of our current Neurosciences Intensive Care Nursery (Figure 1). Our expanded Neurosciences Intensive Care Nursery now includes specialists in maternal–fetal medicine, neurological surgery, basic neuroscience, palliative care, and several other fields.27 A typical weekly Neurosciences Intensive Care Nursery conference attracts more than 30 attendees from more than 10 subspecialties, covering the wide spectrum of trainees, faculty, and multidisciplinary expertise and perspectives mentioned earlier. The collaborative spirit promoted by these weekly meetings has led to the development of new protocols for various aspects of clinical care, as discussed earlier, and has initiated research projects related to neonatal neurological care.
Figure 1.
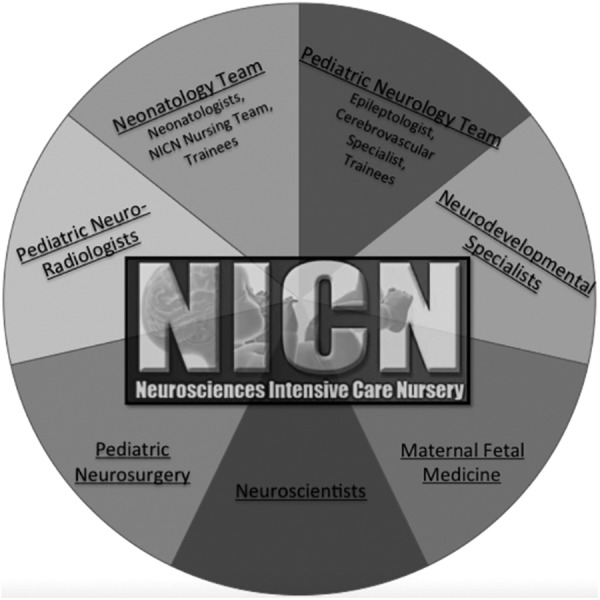
The Johns Hopkins Neurosciences Intensive Care Nursery includes specialists in neonatology, pediatric neurology, neurodevelopmental neuroscience, maternal–fetal medicine, neurological surgery, neuroradiology, and basic neuroscience.
Neonatologists
The primary neonatology team admits infants to the neonatal neurocritical care service and provides brain monitoring and resuscitation as needed.27,28 The neonatology team coordinates neuroimaging for infants with suspected neurological involvement, which is critical for clarifying the suspected primary diagnosis. The primary team coordinates consultations from appropriate specialists such as neurology, neurosurgery, and genetics as well as our neurodevelopmental consult service. A recent enhancement in our weekly Neurosciences Intensive Care Nursery conference is inclusion, by teleconference, of our cognate neonatal intensive care unit at the Johns Hopkins Bayview Medical Center, a Level IIIb neonatal intensive care unit 3 miles from our main campus, and other affiliated regional neonatal intensive care units. We also have the ability to teleconference with other tertiary care neonatal facilities on an as needed basis. These technological developments facilitate communication among local and regional specialists and enhance care of sick neonates in a wide geographic area.
Specialized Neurosciences Intensive Care Nursery Nursing Team
Our neonatal intensive care unit is championed by a dedicated nurse coordinator as well as neonatal nurses who are specially trained in the assessment and management of the neurologically ill neonate.29 The nurse coordinator organizes the weekly Neurosciences Intensive Care Nursery conference, in conjunction with the primary neonatology team, and provides education to new fellows and nurses about Neurosciences Intensive Care Nursery protocols, practices, and culture. Our nurse coordinator also maintains databases of neonatal intensive care unit newborns with neurological diagnoses and facilitates research study enrollment for eligible patients during their neonatal intensive care unit stay.
In the Johns Hopkins Neurosciences Intensive Care Nursery, the specialized nursing team receives advanced training in neurological examination skills and the recognition of seizures and other signs of acute neurologic deterioration. These specialized nurses are well versed in the use of amplitude-integrated EEG (aEEG) and receive training in near-infrared spectroscopy for the monitoring of cerebral oxygenation. The specialized Neurosciences Intensive Care Nursery nursing team is experienced in the therapeutic hypothermia protocol for treatment of hypoxic–ischemic encephalopathy in term and near-term babies and is responsible for a neuroprotection protocol for premature patients, which aims to decrease the rate of intraventricular hemorrhages by optimizing head position, fluid and respiratory status, as well as by limiting noxious stimuli, to minimize pain and stress. Further information is available at https://hpo.johnshopkins.edu/hopkins/policies/158/31304/neuro_protective_bundle.pdf.
Pediatric Neurologists
Pediatric neurologists are consulted to provide expert neurological assessment of the critically ill infant. They provide recommendations on the diagnostic evaluation and management of a wide range of neurological problems. As seizures constitute a common presenting symptom among patients with hypoxic–ischemic encephalopathy, neonatal stroke, metabolic, epileptic encephalopathy, and other acute disorders, these patients are monitored closely with continuous EEG from the first concern of an acute neurologic problem28; management recommendations are discussed promptly based on real-time EEG interpretation. The EEG readers provide frequent updates to guide ongoing clinical management. At our institution, continuous video monitoring is interpreted by an epileptologist with experience in neonatal EEG. A committed pediatric epileptologist with expertise in neonatal EEG attends the weekly Neurosciences Intensive Care Nursery conference and reviews EEGs collected over the previous week, providing teaching with each case.
A neurologist with fellowship training in pediatric cerebrovascular disorders provides consultation and attends the weekly Neurosciences Intensive Care Nursery conference. This stroke expert provides guidance on the management and associated outcomes of patients with cerebrovascular complications and contributes to the differential diagnosis of disorders that can mimic neurovascular disease.30
Neuroradiologists
The success of our Neurosciences Intensive Care Nursery program has relied on the expertise of our dedicated pediatric neuroradiology team. Neuroradiologists with subspecialty interest in neonatal neuroimaging offer interpretation of diverse neuroimaging studies that are essential for neonatal neurologic care. Common imaging modalities utilized in the Neurosciences Intensive Care Nursery include cranial ultrasound10,24,31 and brain MRI.32 Our use of head computed tomography is highly limited except when there is concern for calvarial fractures. Understanding the subtleties of neuroimaging findings in healthy and sick neonates is challenging and the techniques in this field are evolving rapidly, with advanced neuroimaging techniques helping to promote a better understanding of the injury associated with preterm birth, hypoxic–ischemic encephalopathy, and neonatal stroke. This information aids in the long-term prediction of outcomes and family counseling.11,15,33–38 Well-established interdepartmental protocols and direct communication between neonatal intensive care unit nursing and pediatric radiology technologists greatly influence successful acquisition of diagnostic examinations.
Neurodevelopmental Specialists
Neurodevelopmental specialists (pediatricians, neurologists, and neuropsychologists) with specific interest and training in assessment and prognostication of early neonatal neurological insults are proving essential for optimal acute and chronic care of neurologically impaired infants. Neurodevelopmental specialists provide detailed assessments in the neonatal period to allow for the behavioral, cognitive, and motor prognostication following premature birth as well as in the diagnosis of hydrocephalus, hypoxic–ischemic encephalopathy, congenital anomalies, seizures, prenatal opioid exposure, and perinatal stroke. Assessment in the neonatal intensive care unit is critical, given the increasing understanding of the significance of very subtle early findings; tests include the Amiel-Tison neurologic assessment, the Neonatal Intensive Care Unit Network Neurobehavioral Scale, and the Prechtl General Movement Assessment. This in-depth neurodevelopmental examination during the neonatal intensive care unit stay provides insight into future neurologic function, which is one of the most frequent questions asked by parents. This approach has been instrumental in advancing our research objectives to develop a combined use of imaging and neurodevelopmental examination for prognostication.
One unique aspect of our program is “NEST” (Nurturing Environmental Support Team) rounds, whereby a multidisciplinary neurodevelopmental team consisting of a neurodevelopmental neurologist, neuropsychologist, child life specialist, and physical, occupational, and respiratory therapists together round weekly on neurologically ill neonates in the neonatal intensive care unit. This team engages with the infants and their parents directly and allows establishment of an individualized developmental care plan for each patient. Care plans include parental teaching and counseling, with particular attention to the environmental factors in the neonatal intensive care unit setting that could affect a baby’s cognitive and motor function. The NEST team also provides advanced planning of the type and frequency of therapies that are initiated while the baby is still in the neonatal intensive care unit, with an effort to promote better long-term neurodevelopmental outcomes. Improved adherence to outpatient follow-up in the high-risk neonatal intensive care unit follow-up clinic (Infant Neurodevelopment Center) has been observed among families participating in NEST rounds.
After discharge, patients with brain injury, exposures, or malformations deemed at high risk for motor and cognitive deficits are followed up at the Infant Neurodevelopment Center, our neonatal intensive care unit follow-up clinic. Importantly, Neurosciences Intensive Care Nursery faculty from multiple subspecialties coordinate care across subspecialties and across the life span, providing a unique, integrated care model that enhances patient outcomes and research progress. Children benefit from such close monitoring, which can pave the way toward early diagnosis of wide myriad of disorders (including cerebral palsy and hemiplegia)39,40 as well as the establishment of appropriate early interventions and therapies. Patients needing additional management of seizures with antiseizure medications or other therapies are typically followed up in our Pediatric Neurology Clinic and at integrated clinics at the Kennedy Krieger Institute and Mount Washington Pediatric Hospital.
Neurosurgeons
The pediatric neurosurgical team provides essential management in cases of intracranial hemorrhage, tumor and infection, ventriculomegaly, vascular and other congenital anomalies, myelomeningocele, and other spine and brain disorders. The ability of neonatologists at the Johns Hopkins Bayview Medical Center campus and affiliated hospitals to interact and discuss their patients with a pediatric neurosurgeon during the weekly Neurosciences Intensive Care Nursery conference by teleconference has led to more appropriate decisions regarding timing for transfer of infants, improved utilization of resources, and reduced family stress. Fetoscopic repair of myelomeningocele offered at Johns Hopkins Children’s Center represents an exciting option for highly selected maternal–fetal candidates, exemplifying the complex teamwork by the integrated Neurosurgical–Fetal Medicine team (described in next section).41 Collaboration with the Neurosciences Intensive Care Nursery has also facilitated participation in national multicenter clinical trials for neonatal hydrocephalus and other congenital disorders.42,43
Maternal–Fetal Medicine and Fetal Therapy Specialists
An active Maternal–Fetal medicine and Fetal Therapy program at Johns Hopkins integrates and elevates the work of the Neurosciences Intensive Care Nursery. The Maternal–Fetal medicine group at Johns Hopkins often seeks consultation from neurology and neurosurgical specialists after identifying fetuses with potential brain developmental anomalies by ultrasound or fetal MRI. Pediatric neurologists, neurosurgeons, and other relevant staff from the Johns Hopkins neonatal intensive care unit routinely meet with families ahead of any planned deliveries of infants with suspected neurological involvement or brain anomalies. At the Neurosciences Intensive Care Nursery conference, Maternal–Fetal medicine specialists report on radiological and clinical aspects of fetuses being followed closely and treated for neurologic abnormalities, some of whom warrant prenatal medical or surgical interventions. Clinical aspects of these cases are discussed and followed during their course, with bidirectional discussions enhancing care, both prenatally and postnatally.
Developmental Neuroscientists
At Johns Hopkins University, we are fortunate to have a community of pediatric neuroscientists of international repute, whose work focuses on disorders of the developing brain and nervous system. Several neuroscientists as well as clinical faculty with translational neuroscience research interests are directly involved in our Neurosciences Intensive Care Nursery, attend the weekly conference, and provide wide-ranging perspectives on the scientific basis of brain development and protection. Input from such neuroscientists has provided valuable insights into potential contributions of laboratory efforts as well as a useful perspective on clinical questions. The monthly Pediatric Neurosciences Collaborative seminar series showcases recent advances by Neurosciences Intensive Care Nursery members and their collaborators. State-of-the-art scientific advances are ongoing in several laboratories at our institution, resulting in numerous collaborative publications and ongoing projects. Recent publications span the spectrum from basic research to clinical trials.44–49 Productive, cutting-edge collaborations are ongoing between clinicians and neuroscientists. The direct, frequent interactions during the weekly Neurosciences Intensive Care Nursery and monthly Pediatric Neurosciences Collaborative fosters interaction across the spectrum from basic, translational, and clinical investigation, with propagation and acceleration of research in every realm.
Progress to Date
Patient Care
More than 1200 patients have been evaluated and discussed as part of weekly Neurosciences Intensive Care Nursery conferences over the past 10 years, including more than 300 patients with hypoxic–ischemic encephalopathy. Approximately 100 continuous EEGs are performed each year in our neonatal intensive care unit, and over 60 neurosurgical consults are obtained. Parents of babies with primary neurological issues often express gratitude that their baby’s care is discussed by numerous specialists at the multidisciplinary Neurosciences Intensive Care Nursery meeting; parents are provided prompt feedback after the Neurosciences Intensive Care Nursery discussion.
Education
Multiple educational initiatives have been offered over the past decade. The Neurosciences Intensive Care Nursery “Foundations Course” (held in 2009, 2011, 2014, and 2016) has been an extremely popular series of lectures and discussions provided by Neurosciences Intensive Care Nursery faculty as an 8-hour educational program aimed at Neurosciences Intensive Care Nursery nurses, pediatrics residents, and neonatology fellows. Typical course content is listed in Table 2.
Table 2.
Sampling of “Foundations Course” Educational Lectures.
| How Cooling Prevents Cerebral Palsy |
| Erythropoietin Studies in HIE |
| Neonatal Seizures |
| Hands-on aEEG |
| Neurodevelopmental Assessment in the NICU |
| Neurodevelopmental Outcomes After Perinatal Brain Injury |
| Neuro-Imaging in the Newborn |
| Perinatal Stroke: Causes and Consequences |
| Evidence for Improving Family Outcomes After HIE |
| Fetal Hydrocephalus: A Diagnostic Challenge |
Abbreviations: aEEG, amplitude-integrated electroencephalogram; HIE, hypoxic–ischemic encephalopathy; NICN, Neurosciences Intensive Care Nursery.
Additional training of residents and fellows within Johns Hopkins Hospital is available. All pediatric neurology and neurodevelopmental neurology residents at Johns Hopkins and Kennedy Krieger Institute complete an intensive 2- to 4-week rotation in the Neurosciences Intensive Care Nursery during their postgraduate 4 or 5 years. The rotation includes lectures on various neonatal neuroscience topics; training in neonatal aEEG, continuous video-EEG, and HUS/MRI; opportunities to round with the neurodevelopmental team and to engage in the Nurturing Environmental Support Team rounds; and the opportunity to spend time at the Kennedy Krieger Institute Infant Neurodevelopment Center, our neonatal intensive care unit follow-up clinic. Each resident presents a talk on a neonatal neuroscience topic during one of our weekly Pediatric Neurology Grand Rounds. Opportunities also exist for interested residents in pediatrics and other disciplines or medical students to get an intensive Neurosciences Intensive Care Nursery exposure.
We have established a fellowship program in Neonatal Neuroscience for individuals who have completed a pediatric neurology residency, neonatal fellowship, or related training program and seek advanced training in the neonatal neurosciences. The program has recently enrolled its second fellow. This fellowship provides specialty training in neonatal neurocritical care (including the evaluation of newborns with the conditions listed in Table 1), intensive training in neonatal EEG, neuroradiological and neurobehavioral assessment, and exposure to other technologies used in neonatal assessment. Fellows attend the Infant Neurodevelopment Center follow-up clinic, perform fetal and neonatal consultations (inpatient and outpatient), and assist with the education of nurses, residents, and other learners. They also play an important educational role in the residents’ Neurosciences Intensive Care Nursery rotation. Neonatal Neuroscience fellows have ample time to develop and pursue research interests under the guidance of faculty.
Beyond Johns Hopkins Hospital, our core faculty has provided regional, national, and international continuing medical education courses focusing on recent practice guidelines in neonatal neurology, neuroradiology, neurodevelopment, and neurosurgery, aimed at physicians, neonatal nurse practitioners, and other nurses who care for neonates. Johns Hopkins Hospital neonatal intensive care unit faculty members have assisted other institutions in developing their own Neurosciences Intensive Care Nursery programs, including those at the University of Virginia, the University of Alabama at Birmingham, and Duke University. The Duke and Virginia programs were developed by and are directed by graduates of the Johns Hopkins Neurosciences Intensive Care Nursery training program.
Current Research Endeavors
More than 100 joint publications have emerged from our group, promoting advances in the understanding of many areas of the neonatal neurosciences, including neuroprotection following brain injury, neural recovery therapy, neuroimaging, fetal therapy, and diagnostics. Selected ongoing research studies are listed in Table 3.
Table 3.
Selected Ongoing Studies in the Neonatal Neurosciences at Johns Hopkins.
| HIE |
|
| Prematurity |
|
| Hydrocephalus |
|
| Neurodevelopment |
|
| Neuroimaging |
|
| Autoregulation |
|
| Seizures |
|
Abbreviations: HIE, hypoxic–ischemic encephalopathy; NICN, Neurosciences Intensive Care Nursery; HI, hypoxic–ischemic; MRI, magnetic resonance imaging; DTI, diffusion tensor imaging.
To summarize, the Johns Hopkins Neurosciences Intensive Care Nursery is thriving and continues to make advancements across several areas (including patient care, education, and research) that contribute to improved patient outcomes. The number of consults to the neurology and neurosurgical teams (as well as the utilization of cEEG in the neonatal intensive care unit and the number of neurosurgical interventions received by our patients) have also continued to increase over the years. Inclusion of the Neurodevelopmental NEST program within our Neurosciences Intensive Care Nursery program has increased outpatient follow-up rates for infants seen by NEST specialists to >95%, well above our usual follow-up rates of ∼70%. We also track adherence to our program’s protocols, especially, the execution of therapeutic hypothermia, and use our regular meetings to incorporate needed changes or emphasize the value of consistency. We have constructed databases to allow questions of either quality improvement or other type of research questions to be asked, so it is a rich resource that has to date primarily been mined for non-quality improvement questions. In the meantime, our educational and research initiatives continue to grow. Finally, the multidisciplinary expertise brought in by Neurosciences Intensive Care Nursery continues to benefit the neonatal intensive care unit newborns and has translated into greater patient satisfaction (among parents) over the years.
Challenges
We are proud of the successes of our nascent Neurosciences Intensive Care Nursery program, which include overcoming considerable logistical hurdles to initiate the program, sustain funding for the nurse coordinator who is vital to the program’s function, maintain a vibrant weekly Neurosciences Intensive Care Nursery conference with consistently high attendance and passionate participation, and facilitate outreach efforts to other institutions. All of these successes are a result of coordinated efforts of many individuals who maintain an optimistic vision of what a Neurosciences Intensive Care Nursery program is and what it can be. Yet, the challenges should not be underestimated. Similar to most subspecialty pediatric programs, our Neurosciences Intensive Care Nursery program constantly struggles to maintain financial viability. Equipment purchases, maintenance, and updates are dependent on hospital-based requests. All faculty participation is voluntary with no tangible compensation for their efforts. Some individuals have grant funding as a result of Neurosciences Intensive Care Nursery collaborations and the infrastructure made possible by the Neurosciences Intensive Care Nursery program, a circumstance that we hope will grow and expand. Convincing departmental and hospital leadership of the importance of a Neurosciences Intensive Care Nursery program for children, families, and the wider research and medical community is an ongoing effort. Leadership changes and personnel transitions have been challenging but represent an opportunity for new directions and growth.
Plans for Expansion
Many aspects of the Neurosciences Intensive Care Nursery program are ripe for expansion. In particular, new clinical and research protocols being developed by us and other Neurosciences Intensive Care Nursery programs are shared at professional meetings such as the Neonatal Neurocritical Care Special Interest Group held at the Pediatric Academic Societies annual meeting and the “ONE Conference” for Neuro-Critical Care Nurses whose motto is “one baby, one nurse, one brain, one moment, one connection makes the difference.” Of great excitement to clinicians and researchers is the imminent establishment of a new professional society devoted to newborn neurological disorders and research, which will be called the Newborn Brain Society (organizer: Dr Mohamed El-Dib, Brigham & Women’s Hospital, Boston, MA; personal communication, August 08, 2019). Our Maternal–Fetal and Fetal Therapy programs and palliative care efforts are bringing additional patients for review and improving our overall patient discussions. An additional challenge is obtaining financial and institutional support to sustain the fellowship in neonatal neurosciences and thereby provide the next generation of specialists for Johns Hopkins Children’s Center and other institutions. One of our constant goals is to encourage well-trained neonatologists, pediatric neurologists, and other specialists who desire to develop a Neurosciences Intensive Care Nursery at their own institution. Our program’s 10-year anniversary celebration, held in May 2019, was the inspiration for this article and provided an opportunity for self-reflection and planning future growth of our place in this exciting field, ultimately maximizing the potential for every child with a neurologic concern in the perinatal period.
Acknowledgments
The authors would like to extend gratitude to the many individuals who have been a pivotal part of the Johns Hopkins Neurosciences Intensive Care Nursery since its inception. The authors also thank colleagues from other departments who assisted with this article: Eva Ritzl, MD, and Nirma Carballido Martinez, MSc Eng, REEGT.
Authors’ Note: The Johns Hopkins Neurosciences Intensive Care Nursery: Marilee Allen, MD, Renee Boss, MD, Vera Joanna Burton, MD, PhD, Raul Chavez-Valdez, MD, May Chen, MD, Allen Everett, MD, Ryan Felling, MD, PhD, Gwendolyn J. Gerner, Psy D, Maureen Gilmore, MD, Christopher Golden, MD, Ernest Graham, MD, Lauren Jantzie, PhD, Jennifer Lee, MD, and Shenandoah Robinson, MD, USA.
Author Contributions: MC, CES, AT, CP, FJN, and the Johns Hopkins Neurosciences Intensive Care Nursery personnel and staff made substantial contributions toward the conception of the manuscript. MC drafted the original manuscript and CES revised it extensively, multiple times, for style and content. AT, CP, and FJN subsequently revised drafts. Finally, the manuscript was circulated to all listed Neurosciences Intensive Care Nursery personnel for final approval.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: All information and data described in this topical review are aligned with the Johns Hopkins University ethics. There was no required written IRB consent for this topical review in our institution.
ORCID iD: Melisa Carrasco  https://orcid.org/0000-0001-7468-7691
https://orcid.org/0000-0001-7468-7691
References
- 1. Van Meurs KP, Yan ES, Randall KS, et al. Development of a NeuroNICU with a broader focus on all newborns at risk of brain injury: the first 2 years. Am J Perinatol. 2018;35(12):1197–1205. [DOI] [PubMed] [Google Scholar]
- 2. Glass HC, Ferriero DM, Rowitch DH, Shimotake TK. The neurointensive nursery: concept, development, and insights gained. Curr Opin Pediatr. 2019;31(2):202–209. [DOI] [PubMed] [Google Scholar]
- 3. Roychoudhury S, Esser MJ, Buchhalter J, et al. Implementation of neonatal neurocritical care program improved short-term outcomes in neonates with moderate-to-severe hypoxic ischemic encephalopathy. Pediatr Neurol. 2019;101:64–70. [DOI] [PubMed] [Google Scholar]
- 4. Glass HC, Bonifacio SL, Shimotake T, Ferriero DM. Neurocritical care for neonates. Curr Treat Options Neurol. 2011;13(6):574–589. [DOI] [PubMed] [Google Scholar]
- 5. Smyser CD, Tam EWY, Chang T, Soul JS, Miller SP, Glass HC. Fellowship training in the emerging fields of fetal-neonatal neurology and neonatal neurocritical care. Pediatr Neurol. 2016;63:39–44.e3. [DOI] [PubMed] [Google Scholar]
- 6. Glass HC, Rowitch DH. The role of the neurointensive care nursery for neonatal encephalopathy. Clin Perinatol. 2016;43(3):547–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peyvandi S, Chau V, Guo T, et al. Neonatal brain injury and timing of neurodevelopmental assessment in patients with congenital heart disease. J Am Coll Cardiol. 2018;71(18):1986–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Verrall CE, Walker K, Loughran-Fowlds A, et al. Contemporary incidence of stroke (focal infarct and/or haemorrhage) determined by neuroimaging and neurodevelopmental disability at 12 months of age in neonates undergoing cardiac surgery utilizing cardiopulmonary bypass. Interact Cardiovasc Thorac Surg. 2018;26(4):644–650. [DOI] [PubMed] [Google Scholar]
- 9. Mulkey SB, Swearingen CJ. Advancing neurologic care in the neonatal intensive care unit with a neonatal neurologist. J Child Neurol. 2014;29(1):31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Salas J, Tekes A, Hwang M, Northington FJ, Huisman TAGM. Head ultrasound in neonatal hypoxic-ischemic injury and its mimickers for clinicians: a review of the patterns of injury and the evolution of findings over time. Neonatology. 2018;114(3):185–197. [DOI] [PubMed] [Google Scholar]
- 11. Gerner GJ, Burton VJ, Poretti A, et al. Transfontanellar duplex brain ultrasonography resistive indices as a prognostic tool in neonatal hypoxic-ischemic encephalopathy before and after treatment with therapeutic hypothermia. J Perinatol. 2016;36(3):202–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qi Y, Liu P, Lin Z, Lu H, Wang X. Hemodynamic and metabolic assessment of neonates with punctate white matter lesions using phase-contrast MRI and T2-relaxation-under-spin-tagging (TRUST) MRI. Front Physiol. 2018;9:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu P, Huang H, Rollins N, et al. Quantitative assessment of global cerebral metabolic rate of oxygen (CMRO2) in neonates using MRI. NMR Biomed. 2014;27(3):332–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee JK, Perin J, Parkinson C, et al. Relationships between cerebral autoregulation and markers of kidney and liver injury in neonatal encephalopathy and therapeutic hypothermia. J Perinatol. 2017;37(8):938–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Carrasco M, Perin J, Jennings JM, et al. Cerebral autoregulation and conventional and diffusion tensor imaging magnetic resonance imaging in neonatal hypoxic-ischemic encephalopathy. Pediatr Neurol. 2018;82:36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chavez-Valdez R, O’Connor M, Perin J, et al. Sex-specific associations between cerebrovascular blood pressure autoregulation and cardiopulmonary injury in neonatal encephalopathy and therapeutic hypothermia. Pediatr Res. 2017;81(5):759–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burton VJ, Gerner G, Cristofalo E, et al. A pilot cohort study of cerebral autoregulation and 2-year neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy who received therapeutic hypothermia. BMC Neurol. 2015;15:209 DOI:10.1186/s12883-015-0464-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Howlett JA, Northington FJ, Gilmore MM, et al. Cerebrovascular autoregulation and neurologic injury in neonatal hypoxic-ischemic encephalopathy. Pediatr Res. 2013;74(5):525–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tekes A, Poretti A, Scheurkogel MM, et al. Apparent diffusion coefficient scalars correlate with near-infrared spectroscopy markers of cerebrovascular autoregulation in neonates cooled for perinatal hypoxic-ischemic injury. AJNR Am J Neuroradiol. 2015;36(1):188–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jiang D, Lu H, Parkinson C, et al. Vessel-specific quantification of neonatal cerebral venous oxygenation. Magn Reson Med. 2019;82(3):1129–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jan S, Northington FJ, Parkinson CM, Stafstrom CE. EEG monitoring technique influences the management of hypoxic-ischemic seizures in neonates undergoing therapeutic hypothermia. Dev Neurosci. 2017;39(1-4):82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dorner RA, Soares BP, Robinson S, Allen MC, Perin J, Burton VJ. The relationship between clinical imaging and neurobehavioral assessment in posthemorrhagic ventricular dilation of prematurity. Front Physiol. 2019;10:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dorner RA, Burton VJ, Allen MC, Robinson S, Soares BP. Preterm neuroimaging and neurodevelopmental outcome: a focus on intraventricular hemorrhage, post-hemorrhagic hydrocephalus, and associated brain injury. J Perinatol. 2018;38(11):1431–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hwang M, Riggs BJ, Katz J, et al. Advanced pediatric neurosonography techniques: Contrast-enhanced ultrasonography, elastography, and beyond. J Neuroimaging. 2018;28(2):150–157. [DOI] [PubMed] [Google Scholar]
- 25. Lemmon ME, Wagner MW, Bosemani T, et al. Diffusion tensor imaging detects occult cerebellar injury in severe neonatal hypoxic-ischemic encephalopathy. Dev Neurosci. 2017;39(1-4):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Graham EM, Everett AD, Delpech JC, Northington FJ. Blood biomarkers for evaluation of perinatal encephalopathy: state of the art. Curr Opin Pediatr. 2018;30(2):199–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Glass HC, Rogers EE, Peloquin S, Bonifacio SL. Interdisciplinary approach to neurocritical care in the intensive care nursery. Semin Pediatr Neurol. 2014;21(4):241–247. [DOI] [PubMed] [Google Scholar]
- 28. Boylan GB, Stevenson NJ, Vanhatalo S. Monitoring neonatal seizures. Semin Fetal Neonatal Med. 2013;18(4):202–208. [DOI] [PubMed] [Google Scholar]
- 29. Peloquin S, Carley A, Bonifacio SL, Glass HC. The neurointensive care nursery and evolving roles for nursing. Neonatal Netw. 2016;35(2):87–94. [DOI] [PubMed] [Google Scholar]
- 30. Adami RR, Grundy ME, Poretti A, Felling RJ, Lemmon M, Graham EM. Distinguishing arterial ischemic stroke from hypoxic-ischemic encephalopathy in the neonate at birth. Obstet Gynecol. 2016;128(4):704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Orman G, Benson JE, Kweldam CF, et al. Neonatal head ultrasonography today: A powerful imaging tool! J Neuroimaging. 2015;25(1):31–55. [DOI] [PubMed] [Google Scholar]
- 32. Lee S, Mirsky DM, Beslow LA, et al. Pathways for neuroimaging of neonatal stroke. Pediatr Neurol. 2017;69:37–48. [DOI] [PubMed] [Google Scholar]
- 33. Lockwood Estrin G, Wu Z, Deprez M, et al. White and grey matter development in utero assessed using motion-corrected diffusion tensor imaging and its comparison to ex utero measures. MAGMA. 2019;32(4):473–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Intrapiromkul J, Northington F, Huisman TA, Izbudak I, Meoded A, Tekes A. Accuracy of head ultrasound for the detection of intracranial hemorrhage in preterm neonates: comparison with brain MRI and susceptibility-weighted imaging. J Neuroradiol. 2013;40(2):81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kitamura G, Kido D, Wycliffe N, Jacobson JP, Oyoyo U, Ashwal S. Hypoxic-ischemic injury: utility of susceptibility-weighted imaging. Pediatr Neurol. 2011;45(4):220–224. [DOI] [PubMed] [Google Scholar]
- 36. Watson CG, Dehaes M, Gagoski BA, Grant PE, Rivkin MJ. Arterial spin labeling perfusion magnetic resonance imaging performed in acute perinatal stroke reveals hyperperfusion associated with ischemic injury. Stroke. 2016;47(6):1514–1519. [DOI] [PubMed] [Google Scholar]
- 37. Gerner GJ, Newman EI, Burton VJ, et al. Correlation between white matter injury identified by neonatal diffusion tensor imaging and neurodevelopmental outcomes following term neonatal asphyxia and therapeutic hypothermia: an exploratory pilot study. J Child Neurol. 2019;34(10): 556–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chin EM, Jayakumar S, Ramos E, et al. Preschool language outcomes following perinatal hypoxic-ischemic encephalopathy in the age of therapeutic hypothermia. Dev Neurosci. 2018;40:627–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Maitre NL, Chorna O, Romeo DM, Guzzetta A. Implementation of the Hammersmith Infant Neurological Examination in a high-risk infant follow-up program. Pediatr Neurol. 2016;65:31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Novak I, Morgan C, Adde L, et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017;171(9):897–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Miller JL, Groves ML, Baschat AA. Fetoscopic spina bifida repair. Minerva Ginecol. 2019;71(2):163–170. [DOI] [PubMed] [Google Scholar]
- 42. Furey CG, Choi J, Jin SC, et al. De novo mutation in genes regulating neural stem cell fate in human congenital hydrocephalus. Neuron. 2018;99(2):302–314.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Duran D, Zeng X, Jin SC, et al. Mutations in chromatin modifier and ephrin signaling genes in vein of Galen malformation. Neuron. 2019;101(3):429–443.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lee JK, Poretti A, Perin J, et al. Optimizing cerebral autoregulation may decrease neonatal regional hypoxic-ischemic brain injury. Dev Neurosci. 2017;39(1-4):248–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yellowhair TR, Noor S, Mares B, et al. Chorioamnionitis in rats precipitates extended postnatal inflammatory lymphocyte hyperreactivity. Dev Neurosci. 2018;40:523–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Robinson S, Conteh FS, Oppong AY, et al. Extended combined neonatal treatment with erythropoietin plus melatonin prevents posthemorrhagic hydrocephalus of prematurity in rats. Front Cell Neurosci. 2018;12:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fang J, Chavez-Valdez R, Flock DL, et al. An inhibitor of the mitochondrial permeability transition pore lacks therapeutic efficacy following neonatal hypoxia ischemia in mice. Neuroscience. 2019;406:202–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McNally MA, Chavez-Valdez R, Felling RJ, Flock DL, Northington FJ, Stafstrom CE. Seizure susceptibility correlates with brain injury in male mice treated with hypothermia after neonatal hypoxia-ischemia. Dev Neurosci 2018;40:576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wu D, Martin LJ, Northington FJ, Zhang J. Oscillating-gradient diffusion magnetic resonance imaging detects acute subcellular structural changes in the mouse forebrain after neonatal hypoxia-ischemia. J Cereb Blood Flow Metab. 2019;39(7):1336–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]


