Key Points
Question
What was the quality of diets among youth in the United States and how did it change between 1999 and 2016?
Findings
In this serial cross-sectional analysis of nationally representative data from 31 420 youth, diet quality modestly improved from 1999-2000 to 2015-2016 based on validated dietary quality scores. The estimated proportion of children with poor-quality diet significantly decreased (from 76.8% to 56.1%), the estimated proportion with intermediate quality diet significantly increased (from 23.2% to 43.7%), and the estimated proportion with an ideal quality significantly increased but remained low (from 0.07% to 0.25%).
Meaning
From 1999 to 2016, the estimated overall diet quality of US youth modestly improved, but more than half of children still had poor-quality diets.
Abstract
Importance
Prior studies of dietary trends among US youth have evaluated major macronutrients or only a few foods or have used older data.
Objective
To characterize trends in diet quality among US youth.
Design, Setting, and Participants
Serial cross-sectional investigation using 24-hour dietary recalls from youth aged 2 to 19 years from 9 National Health and Nutrition Examination Survey (NHANES) cycles (1999-2016).
Exposures
Calendar year and population sociodemographic characteristics.
Main Outcomes and Measures
The primary outcomes were the survey-weighted, energy-adjusted mean consumption of dietary components and proportion meeting targets of the American Heart Association (AHA) 2020 continuous diet score (range, 0-50; based on total fruits and vegetables, whole grains, fish and shellfish, sugar-sweetened beverages, and sodium). Additional outcomes were the AHA secondary score (range, 0-80; adding nuts, seeds, and legumes; processed meat; and saturated fat) and Healthy Eating Index (HEI) 2015 score (range, 0-100). Poor diet was defined as less than 40% adherence (scores, <20 for primary and <32 for secondary AHA scores); intermediate as 40% to 79.9% adherence (scores, 20-39.9 and 32-63.9, respectively); and ideal, as at least 80% adherence (scores, ≥40 and ≥64, respectively). Higher diet scores indicate better diet quality; a minimal clinically important difference has not been quantified.
Results
Of 31 420 youth aged 2 to 19 years included, the mean age was 10.6 years; 49.1% were female. From 1999 to 2016, the estimated AHA primary diet score significantly increased from 14.8 (95% CI, 14.1-15.4) to 18.8 (95% CI, 18.1-19.6) (27.0% improvement), the estimated AHA secondary diet score from 29.2 (95% CI, 28.1-30.4) to 33.0 (95% CI, 32.0-33.9) (13.0% improvement), and the estimated HEI-2015 score from 44.6 (95% CI, 43.5-45.8) to 49.6 (95% CI, 48.5-50.8) (11.2% improvement) (P < .001 for trend for each). Based on the AHA primary diet score, the estimated proportion of youth with poor diets significantly declined from 76.8% (95% CI, 72.9%-80.2%) to 56.1% (95% CI, 51.4%-60.7%) and with intermediate diets significantly increased from 23.2% (95% CI, 19.8%-26.9%) to 43.7% (95% CI, 39.1%-48.3%) (P < .001 for trend for each). The estimated proportion meeting ideal quality significantly increased but remained low, from 0.07% (95% CI, 0.01%-0.49%) to 0.25% (95% CI, 0.10%-0.62%) (P = .03 for trend). Persistent dietary variations were identified across multiple sociodemographic groups. The estimated proportion of youth with a poor diet in 2015-2016 was 39.8% (95% CI, 35.1%-44.5%) for ages 2 to 5 years (unweighted n = 666), 52.5% (95% CI, 46.4%-58.5%) for ages 6 to 11 years (unweighted n = 1040), and 66.6% (95% CI, 61.4%-71.4%) for ages 12 to 19 years (unweighted n = 1195), with persistent differences across levels of parental education, household income, and household food security status.
Conclusions and Relevance
Based on serial NHANES surveys from 1999 to 2016, the estimated overall diet quality of US youth showed modest improvement, but more than half of youth still had poor-quality diets.
This national survey study uses NHANES data to characterize trends in diet quality among US youth aged 2 to 19 years between 1999 and 2016.
Introduction
Poor diet is a major contributor to chronic diseases, including diabetes, heart disease, stroke, cancers, and obesity, accounting for substantial morbidity and premature mortality.1 Diets at early ages shape lifelong food preferences and health outcomes.2 Several national efforts since 2000 have aimed to improve the food available to and consumed by US children.3,4,5 At the same time, industry and market forces have increased the proportion of meals prepared outside of home, more than one-third of US calories consumed in 2011-20126; have aggressively marketed foods of low nutritional value to children7,8; and may have led to more products with whole grains and less added sugar.9,10
Prior studies have generally focused on a few components (eg, total energy, macronutrients) or a few foods (eg, sugary beverages, processed meat), or used older data and diet quality measures.11,12,13,14,15 Contemporary trends in diet quality of US youth across a broad range of dietary factors, including both dietary patterns and multiple individual foods and nutrients linked to major health outcomes, are not established. In addition, differences in trends across population subgroups in overall diet quality and major food groups and nutrients remain unclear. Understanding these trends is crucial to inform priorities and policies to help improve diets and long-term health among US youth.
To address these major knowledge gaps, data from the National Health and Nutrition Examination Survey (NHANES) from 1999-2000 to 2015-2016 were evaluated to examine trends in diet quality and individual foods and nutrients consumed by US youth, overall and by age, sex, race/ethnicity, parental education, household income, household food security status, and federal food assistance program participation.
Methods
Data Source, Study Population, and Dietary Assessment
NHANES is a series of cross-sectional surveys using a complex, multistage probability design to sample the civilian, noninstitutionalized population residing in the 50 states and District of Columbia. The NHANES protocol was approved by the Centers for Disease Control and Prevention/National Center for Health Statistics Ethics Review Board, and all participants provided written informed consent. Because the data are publicly available and deidentified, institutional review board approval was not required for this analysis. Details on the study design, protocol, and data collection methods have been documented.16 The overall response rate was 83.5%, with the cycle-specific rate ranging from 67.3% to 89.0%.
This investigation used data across 9 cycles of NHANES (1999-2000 through 2015-2016) including US youth aged 2 to 19 years who completed at least 1 valid 24-hour diet recall. All participants were eligible for dietary assessment, consisting of 1 (first 2 cycles) or up to 2 (later cycles) dietary recalls in which respondents reported all foods and beverages consumed during the previous 24 hours (midnight to midnight). Survey participants aged 12 years or older completed the dietary interview on their own. Proxy-assisted interviews were conducted for children aged 6 to 11 years, and proxy respondents reported diets for children who were aged 5 years or younger or for persons who could not self-report. The US Department of Agriculture (USDA) Automated Multiple-Pass Method was used for collecting 24-hour dietary recalls using “What We Eat In America,” the dietary interview component of NHANES.
The USDA Food Patterns Equivalents Database and MyPyramid Equivalents Database, which disaggregate mixed foods into their component parts, were used to assess changes in specific food groups. Nutrients were derived from cycle-specific versions of the USDA Food and Nutrient Database for Dietary Studies. Intakes of all dietary components were energy adjusted using the residual method to evaluate trends in dietary quality (composition) independent of the small changes in energy intake during this period, which could relate to nondietary factors such as changes in physical activity, and to minimize measurement error in dietary estimates.
Assessment of Dietary Quality
The primary outcomes were the mean consumption of dietary components and proportion meeting targets of the American Heart Association (AHA) 2020 continuous diet score (range, 0-50; based on total fruits and vegetables, whole grains, fish and shellfish, sugar-sweetened beverages, and sodium).17,18 We also evaluated the AHA secondary score (range, 0-80; adding nuts, seeds, and legumes; processed meat; and saturated fat), the Healthy Eating Index (HEI) 2015 score (range, 0-100), the individual components, and other food groups and nutrients linked to major health outcomes and of current policy or general public interest, including fish and shellfish, total fat, seafood omega-3 fat, protein, carbohydrate, cholesterol, fiber, potassium, and calcium. For calculating the AHA diet scores, intake of each dietary component was scored from 0 to 10 (beneficial components) and from 10 to 0 (harmful components) (eAppendix 1 and eTables 1 and 2 in the Supplement). Poor diet was defined as less than 40% adherence (scores, <20 for primary and <32 for secondary AHA scores); intermediate as 40% to 79.9% adherence (scores, 20-39.9 and 32-63.9, respectively); and ideal as at least 80% adherence (scores, ≥40 and ≥64, respectively). Higher diet scores indicate better diet quality; a minimal clinically important difference has not been quantified. The HEI-2015 score, a government measure of adherence to the Dietary Guidelines for Americans,19 was based on 9 adequacy food components (total fruits including 100% fruit juice, whole fruits, total vegetables including legumes, greens and beans, whole grains, total dairy, total protein foods, seafood and plant proteins, and the ratio of unsaturated to saturated fatty acids) and 4 moderation components (refined grains, sodium, added sugars, and saturated fats) (eTable 2 in the Supplement).
Assessment of Sociodemographic Characteristics
Trends in diet quality and intakes of major food groups and nutrients were evaluated by age (2-5, 6-11, and 12-19 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, and Mexican American), parental educational level (less than high school diploma, high school graduate or equivalent, some college, and college graduate), family income (ratio to the federal poverty level: <1.30, 1.30-1.84, 1.85-2.99, and ≥3.00), and household food security status. We evaluated information on race/ethnicity because of previously documented differences in diet quality and diet-related health outcomes depending on race/ethnicity.1,17 Information on race/ethnicity was collected by trained NHANES interviewers according to the fixed categories provided by the National Center for Health Statistics using the Computer-Assisted Personal Interview system, with classification identified by a household proxy for participants younger than 16 years and by the respondents directly for those aged 16 years and older. Information on household food security was collected by trained NHANES interviewers using the US Food Security Survey Module, including 18 items for households with children. The data derived from these responses were used by the National Center for Health Statistics to characterize the food security status of the entire household, used for this analysis. In addition, we evaluated population subgroups according to household participation in major federal nutrition assistance programs, including the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), the Supplemental Nutrition Assistance Program (SNAP), and the reduced-price/free National School Lunch Program/School Breakfast Program (eAppendix 2 in the Supplement).
Statistical Analysis
All analyses accounted for the NHANES complex sampling design to derive nationally representative estimates. The estimated population means for total and component diet scores and intakes of major foods and nutrients were calculated for each NHANES cycle. The estimated proportions of youth adherent to the recommended AHA score targets (ie, poor, intermediate, or ideal quality) were also calculated. The statistical significance of trends was assessed by treating the survey year as a continuous variable in a survey-weighted linear regression model. Absolute and relative (percentage change) differences in estimated means with 95% CIs between 1999-2000 and 2015-2016 cycles were calculated using survey-weighted linear regression by treating each 2-year survey cycle as an indicator category, with the 1999-2000 cycle as the reference. To assess the statistical significance of population differences (interaction) in trends over time, a survey-weighted Wald F test was used to evaluate a multiplicative interaction term between the survey year as a continuous variable and each sociodemographic subgroup as an indicator category.
To calculate HEI-2015 scores, we used the simple scoring algorithm in the main analysis. The National Cancer Institute and USDA generally recommend the population ratio method, which adjusts for day-to-day within-person variation to derive a score that is closer to the usual population intake distribution in sensitivity analyses.20 We also used the more advanced and time-intensive Markov chain Monte Carlo method, which incorporates adjustment for measurement error, episodic consumption, skewness, and correlations between each and all of the included dietary factors and energy (eAppendix 1 and eTable 3 in the Supplement).19
To understand the extent to which observed trends over time might be associated with shifts in population demographic factors, sensitivity analyses were adjusted for age, sex, and race/ethnicity within each cycle, and statistically significant trend coefficients were evaluated before and after adjustment to quantify the percentage change in the coefficient. Participants with missing data on parental education, household income, or food security status were excluded from corresponding subgroup analyses. All analyses were performed using Stata version 14 (StataCorp) and SAS version 9.4 (SAS Institute Inc), with a 2-sided α = .05. No adjustments were made for multiple comparisons, and findings of secondary analyses should be interpreted as exploratory.
Results
Participant Characteristics
A total of 31 420 youth (mean age, 10.6 years; 49.1% female) who completed at least 1 valid 24-hour diet recall were included in this analysis, including 20 193 (64.3%) who also provided a second recall. From 1999 to 2016, the proportion of non-Hispanic white youth decreased from 59.6% to 50.6%, while the proportion of Mexican American youth increased from 11.0% to 16.3% (Table 1). The proportion of children with parents having a college degree or higher increased from 20.2% to 27.1%, while the proportion of youth participating in SNAP increased from 16.7% to 27.6% (corresponding to the period of the US economic recession after 2007).
Table 1. Sociodemographic Characteristics of US Youth Aged 2 to 19 Years by NHANES Survey Cycles From 1999 to 2016.
| Characteristics | No. of participants (survey-weighted %)a | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1999-2000 (n = 3833) | 2001-2002 (n = 4288) | 2003-2004 (n = 3825) | 2005-2006 (n = 4029) | 2007-2008 (n = 3109) | 2009-2010 (n = 3280) | 2011-2012 (n = 3134) | 2013-2014 (n = 3021) | 2015-2016 (n = 2901) | |
| Age group, y | |||||||||
| 2-5 | 665 (21.9) | 856 (21.4) | 763 (21.3) | 902 (21.6) | 832 (22.2) | 861 (22.2) | 836 (22.0) | 678 (20.4) | 666 (21.5) |
| 6-11 | 961 (34.3) | 1136 (33.8) | 900 (33.0) | 1012 (32.3) | 1121 (32.3) | 1154 (32.9) | 1146 (32.8) | 1047 (33.7) | 1040 (33.5) |
| 12-19 | 2207 (43.8) | 2296 (44.8) | 2162 (45.7) | 2115 (46.0) | 1156 (45.5) | 1265 (44.9) | 1152 (45.2) | 1296 (45.9) | 1195 (45.0) |
| Sex | |||||||||
| Female | 1893 (48.8) | 2158 (49.9) | 1923 (48.4) | 2046 (49.0) | 1497 (49.7) | 1568 (49.7) | 1548 (48.8) | 1501 (48.6) | 1438 (49.4) |
| Male | 1940 (51.2) | 2130 (50.0) | 1902 (51.6) | 1983 (51.0) | 1612 (50.3) | 1712 (50.3) | 1586 (51.2) | 1520 (51.4) | 1463 (50.6) |
| Race/ethnicity | |||||||||
| Non-Hispanic white | 839 (59.6) | 1325 (61.1) | 1067 (62.9) | 1075 (60.5) | 991 (59.6) | 1101 (57.3) | 690 (53.2) | 812 (52.7) | 831 (50.6) |
| Non-Hispanic black | 1052 (14.2) | 1312 (14.4) | 1322 (15.0) | 1251 (14.9) | 788 (14.8) | 654 (13.8) | 936 (15.2) | 753 (14.0) | 655 (14.6) |
| Mexican American | 1588 (11.0) | 1263 (12.1) | 1139 (12.5) | 1338 (13.3) | 778 (13.2) | 914 (14.3) | 601 (14.8) | 692 (16.0) | 630 (16.3) |
| Other Hispanic | 198 (7.5) | 203 (6.4) | 126 (3.8) | 134 (3.7) | 398 (6.9) | 374 (7.1) | 364 (8.0) | 305 (7.4) | 359 (8.6) |
| Other/mixed | 156 (7.7) | 185 (6.1) | 171 (5.8) | 231 (7.7) | 154 (5.5) | 237 (7.5) | 543 (8.8) | 459 (9.8) | 426 (9.9) |
| Parental education | |||||||||
| Total No. | 3637 | 4134 | 3673 | 3854 | 2997 | 3184 | 3023 | 2950 | 2786 |
| Less than high school diploma | 1555 (25.0) | 1498 (23.2) | 1224 (19.7) | 1212 (17.7) | 923 (19.5) | 966 (20.0) | 848 (23.4) | 704 (16.5) | 679 (18.3) |
| High school graduate or GED | 880 (25.2) | 982 (23.9) | 958 (25.7) | 917 (24.3) | 753 (24.4) | 738 (20.1) | 674 (19.2) | 701 (23.5) | 581 (18.5) |
| Some college | 758 (24.9) | 947 (22.9) | 1043 (33.3) | 1096 (32.9) | 834 (28.1) | 885 (29.7) | 824 (29.0) | 901 (30.5) | 907 (32.3) |
| College degree or higher | 444 (20.2) | 707 (26.5) | 448 (17.2) | 629 (21.3) | 487 (23.0) | 595 (27.2) | 677 (25.4) | 644 (26.8) | 619 (27.1) |
| Ratio of family income to poverty levelb | |||||||||
| Total No. | 3297 | 4037 | 3655 | 3851 | 2878 | 3000 | 2909 | 2826 | 2669 |
| <1.30 | 1566 (37.9) | 1697 (32.8) | 1678 (34.9) | 1580 (28.0) | 1296 (33.3) | 1422 (33.9) | 1383 (38.7) | 1372 (37.4) | 1074 (31.0) |
| 1.30 to <1.85 | 473 (12.4) | 543 (11.9) | 498 (10.9) | 484 (10.3) | 358 (10.8) | 406 (12.1) | 402 (12.0) | 336 (10.6) | 408 (12.9) |
| 1.85 to <3.00 | 537 (17.5) | 699 (18.9) | 633 (19.6) | 695 (21.9) | 524 (17.7) | 441 (16.5) | 415 (17.4) | 414 (17.4) | 529 (20.7) |
| ≥3.00 | 721 (32.1) | 1098 (36.4) | 846 (34.6) | 1092 (39.8) | 700 (38.1) | 731 (37.4) | 709 (31.8) | 704 (34.6) | 658 (35.4) |
| Food security statusc | |||||||||
| Total No. | 3758 | 4046 | 3659 | 3979 | 3091 | 3250 | 3124 | 2999 | NA |
| Very low food security | 255 (4.6) | 314 (6.2) | 341 (6.8) | 293 (5.2) | 254 (6.3) | 290 (6.9) | 254 (7.7) | 265 (6.6) | NA |
| Low food security | 614 (12.0) | 649 (11.0) | 598 (11.2) | 653 (10.1) | 525 (12.4) | 593 (12.6) | 596 (14.8) | 529 (14.8) | NA |
| Marginal food security | 393 (7.5) | 421 (7.8) | 393 (7.8) | 462 (8.8) | 396 (9.2) | 506 (11.3) | 526 (13.2) | 435 (11.9) | NA |
| Food secure | 2496 (74.0) | 2662 (69.1) | 2327 (70.0) | 2571 (75.0) | 1916 (71.5) | 1861 (67.6) | 1748 (63.8) | 1770 (65.7) | NA |
| Federal nutrition program participationd | |||||||||
| SNAP | 768 (16.7) | 805 (14.6) | 976 (17.7) | 932 (16.2) | 911 (21.8) | 1121 (23.8) | 1229 (31.0) | 1076 (27.6) | NA |
| WIC | 839 (16.2) | 793 (14.3) | 789 (13.6) | 818 (13.5) | 654 (13.6) | 825 (15.4) | 705 (17.7) | 636 (15.2) | NA |
| NSLP/SBP | 1591 (30.5) | 1536 (27.4) | 1442 (27.2) | 1445 (25.7) | 1312 (28.6) | 1428 (31.9) | 1352 (34.0) | 1359 (34.7) | 1404 (39.2) |
Abbreviations: GED, general equivalency diploma; NA, data not available; NHANES, National Health and Nutrition Examination Survey; NSLP/SPB, reduced-price/free National School Lunch Program/School Breakfast Program; SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Percentages are adjusted for NHANES survey weights.
Ratio of family income to poverty is adjusted for household size; higher numbers indicate higher income.
Data were collected in the food security module by a food security scale questionnaire at the household level during the past 12 months.
These programs are funded by the federal government and administered by states. For SNAP eligibility, a household must meet 3 criteria: (1) household gross monthly income (generally ≤130% of poverty level); (2) household net income after deductions; and (3) household asset limits (generally $2250, or $3500 if household includes ≥1 elderly or disabled member). Women are eligible for the WIC if pregnant or having a child up to age 5 years and having a household income ≤180% of poverty level. For the NSLP/SBP, children from households with incomes ≤130% of poverty level are eligible for free meals and children from households with incomes between 130% and 185% of poverty level are eligible for reduced-price meals.
Trends in Dietary Quality
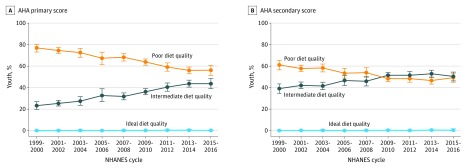
From 1999 to 2016, estimated overall dietary quality improved, whether based on the AHA primary score, AHA secondary score, or HEI-2015 score (Table 2). The estimated mean primary AHA score significantly increased from 14.8 (95% CI, 14.1-15.4) to 18.8 (95% CI, 18.1-19.6) out of 50 (an improvement of 27.0%), the estimated mean secondary AHA score significantly increased from 29.2 (95% CI, 28.1-30.4) to 33.0 (95% CI, 32.0-33.9) out of 80 (an improvement of 13%), and the estimated mean HEI-2015 score significantly increased from 44.6 (95% CI, 43.5-45.8) to 49.6 (95% CI, 48.5-50.8) out of 100 (an improvement of 11.2%) (P < .001 for trend for each). Based on the AHA primary score, the estimated proportion of US youth with poor dietary quality significantly decreased from 76.8% (95% CI, 72.9%-80.2%) to 56.1% (95% CI, 51.4%-60.7%), while the estimated proportion with intermediate quality significantly increased from 23.2% (95% CI, 19.8%-26.9%) to 43.7% (95% CI, 39.1%-48.3%) (P < .001 for trend for each). The estimated proportion with an ideal diet significantly improved but remained low (from 0.07% to 0.25%; P = .03) (Figure 1 and eTable 4 in the Supplement). In sensitivity analyses using alternative methods of population ratio and the Markov chain Monte Carlo method for calculating HEI-2015 scores, results were not materially altered (eTables 5 and 6 in the Supplement).
Table 2. Trends in Estimated Scores for Dietary Components of the AHA 2020 Strategic Impact Goals and HEI-2015 Among US Youth Aged 2 to 19 Years by NHANES Survey Cycles From 1999 to 2016.
| AHA and HEI-2015 scores | Score point range | Scoring extremes | Survey-weighted mean score (95% CI)a | P value for trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maximum | Minimum | 1999-2000 (n = 3833) | 2001-2002 (n = 4288) | 2003-2004 (n = 3825) | 2005-2006 (n = 4029) | 2007-2008 (n = 3109) | 2009-2010 (n = 3280) | 2011-2012 (n = 3132) | 2013-2014 (n = 3019) | 2015-2016 (n = 2901) | |||
| AHA scoresb | |||||||||||||
| Primary score | 0-50 | 50 | 0 | 14.8 (14.1-15.4) | 15.5 (15.0-16) | 15.8 (15.0-16.5) | 16.7 (15.7-17.6) | 16.6 (15.9-17.3) | 17.6 (17.1-18.2) | 18.3 (17.8-18.9) | 18.6 (17.8-19.3) | 18.8 (18.1-19.6) | <.001 |
| Fruits and vegetablesc | 0-10 | ≥4.5 c equivalents/d | 0 | 3.54 (3.38-3.71) | 3.56 (3.36-3.77) | 4.03 (3.84-4.23) | 4.03 (3.89-4.17) | 4.02 (3.79-4.25) | 4.19 (3.96-4.43) | 4.22 (4.01-4.43) | 4.08 (3.93-4.24) | 3.96 (3.75-4.17) | <.001 |
| Whole grains | 0-10 | ≥3 oz equivalents/d | 0 | 1.45 (1.26-1.64) | 1.68 (1.56-1.80) | 1.58 (1.43-1.73) | 1.78 (1.53-2.04) | 1.88 (1.68-2.08) | 2.18 (2.08-2.28) | 2.64 (2.46-2.81) | 2.81 (2.58-3.04) | 3.02 (2.79-3.24) | <.001 |
| Fish and shellfish | 0-10 | ≥2 oz equivalents/d | 0 | 0.73 (0.55-0.91) | 0.85 (0.70-0.99) | 1.26 (1.07-1.45) | 1.36 (1.03-1.69) | 1.08 (0.89-1.27) | 1.10 (0.84-1.35) | 1.17 (0.95-1.40) | 1.18 (0.93-1.43) | 0.90 (0.74-1.06) | .11 |
| Sugar-sweetened beverages | 10-0 | ≤5.14 fl oz/d | >16 fl oz/d | 4.33 (3.89-4.77) | 4.70 (4.38-5.03) | 4.40 (4.03-4.78) | 5.22 (4.83-5.6) | 5.43 (5.14-5.71) | 6.01 (5.80-6.22) | 5.97 (5.72-6.23) | 6.47 (6.11-6.84) | 6.89 (6.58-7.21) | <.001 |
| Sodium | 10-0 | ≤1500 mg/d | >4500 mg/d | 4.70 (4.52-4.89) | 4.69 (4.59-4.8) | 4.49 (4.38-4.61) | 4.26 (4.12-4.41) | 4.17 (4.04-4.29) | 4.15 (3.99-4.30) | 4.34 (4.15-4.52) | 4.01 (3.86-4.15) | 4.06 (3.93-4.18) | <.001 |
| Secondary score | 0-80 | 80 | 0 | 29.2 (28.1-30.4) | 30.0 (29.3-30.8) | 30.1 (29.2-31.1) | 31.3 (29.9-32.6) | 31.1 (30.0-32.1) | 32.8 (32.1-33.5) | 33.4 (32.6-34.3) | 33.2 (32.3-34.0) | 33.0 (32.0-33.9) | <.001 |
| Nuts, seeds, and legumes | 0-10 | ≥4 servings/wk | 0 | 2.62 (2.36-2.89) | 2.48 (2.27-2.69) | 3.19 (2.92-3.46) | 3.46 (3.11-3.81) | 3.20 (2.98-3.41) | 3.52 (3.20-3.83) | 3.65 (3.38-3.92) | 3.20 (2.91-3.49) | 3.42 (3.09-3.75) | <.001 |
| Processed meat | 10-0 | ≤0.5 oz/d | >1.764 oz/d | 7.21 (6.83-7.58) | 7.23 (7.01-7.45) | 6.79 (6.6-6.98) | 6.94 (6.64-7.24) | 6.90 (6.64-7.15) | 6.89 (6.63-7.15) | 6.71 (6.46-6.96) | 6.87 (6.58-7.16) | 6.78 (6.51-7.05) | .01 |
| Saturated fat | 10-0 | ≤7% of energy | >15% of energy | 4.64 (4.36-4.92) | 4.84 (4.64-5.04) | 4.39 (4.16-4.61) | 4.22 (4.1-4.33) | 4.38 (4.18-4.59) | 4.76 (4.55-4.97) | 4.71 (4.49-4.94) | 4.54 (4.33-4.75) | 3.92 (3.66-4.18) | .01 |
| HEI-2015 total scored | 0-100 | 100 | 0 | 44.6 (43.5-45.8) | 46.0 (44.9-47.1) | 48.5 (47.4-49.6) | 47.8 (46.8-48.7) | 48.2 (47.1-49.3) | 49.6 (48.6-50.5) | 51.3 (50.5-52) | 49.9 (49.0-50.9) | 49.6 (48.5-50.8) | <.001 |
| Adequacy components | |||||||||||||
| Total fruitse | 0-5 | ≥0.8 c equivalents/1000 kcal | No fruit | 2.30 (2.18-2.41) | 2.30 (2.16-2.44) | 2.61 (2.42-2.81) | 2.75 (2.61-2.89) | 2.74 (2.56-2.93) | 2.83 (2.67-2.99) | 2.90 (2.73-3.06) | 2.75 (2.58-2.92) | 2.74 (2.58-2.9) | <.001 |
| Whole fruitsf | 0-5 | ≥0.4 c equivalents/1000 kcal | No whole fruit | 2.80 (2.67-2.92) | 2.85 (2.70-3.00) | 3.40 (3.19-3.61) | 2.48 (2.34-2.62) | 2.56 (2.38-2.74) | 2.69 (2.51-2.87) | 2.77 (2.59-2.94) | 2.72 (2.53-2.90) | 2.69 (2.49-2.88) | .005 |
| Total vegetablesg | 0-5 | ≥1.1 cup equiv. per 1000 kcal | No vegetables | 2.28 (2.14-2.42) | 2.24 (2.15-2.33) | 2.47 (2.39-2.56) | 2.31 (2.23-2.40) | 2.26 (2.18-2.34) | 2.29 (2.21-2.37) | 2.28 (2.21-2.36) | 2.30 (2.23-2.37) | 2.34 (2.24-2.44) | .90 |
| Greens and beansg | 0-5 | ≥0.2 c equivalents/1000 kcal | No dark-green vegetables or legumes | 0.75 (0.64-0.86) | 0.71 (0.60-0.82) | 0.93 (0.79-1.06) | 1.01 (0.88-1.14) | 0.98 (0.83-1.13) | 1.14 (1.00-1.27) | 1.24 (1.10-1.38) | 1.26 (1.19-1.33) | 1.24 (1.12-1.36) | <.001 |
| Whole grains | 0-10 | ≥1.5 oz equivalents/1000 kcal | No whole grains | 1.52 (1.32-1.72) | 1.72 (1.60-1.84) | 1.59 (1.45-1.73) | 1.85 (1.60-2.10) | 2.0 (1.8-2.19) | 2.32 (2.21-2.43) | 2.75 (2.57-2.93) | 2.97 (2.74-3.21) | 3.20 (2.96-3.44) | <.001 |
| Dairyh | 0-10 | ≥1.3 c equivalents/1000 kcal | No dairy | 6.36 (6.08-6.64) | 6.73 (6.5-6.96) | 7.12 (6.83-7.40) | 7.26 (7.09-7.42) | 7.16 (6.98-7.35) | 7.56 (7.36-7.76) | 7.54 (7.32-7.76) | 7.33 (7.15-7.50) | 6.98 (6.61-7.35) | <.001 |
| Total protein foodsg | 0-5 | ≥2.5 oz equivalents/1000 kcal | No protein foods | 3.41 (3.29-3.54) | 3.36 (3.28-3.43) | 3.77 (3.67-3.87) | 3.81 (3.72-3.9) | 3.91 (3.85-3.97) | 3.88 (3.8-3.97) | 3.91 (3.82-4) | 3.88 (3.76-4) | 3.85 (3.77-3.94) | <.001 |
| Seafood and plant proteinsg,i | 0-5 | ≥0.8 oz equivalents/1000 kcal | No seafood or plant proteins | 1.44 (1.29-1.59) | 1.47 (1.33-1.60) | 1.88 (1.73-2.03) | 1.91 (1.67-2.14) | 1.77 (1.65-1.88) | 1.93 (1.81-2.06) | 2.18 (2.06-2.29) | 1.91 (1.79-2.03) | 1.98 (1.85-2.11) | <.001 |
| Fatty acidsj | 0-10 | (PUFAs + MUFAs)/SFAs ≥2.5 | (PUFAs + MUFAs)/SFAs ≤1.2 | 3.79 (3.56-4.02) | 3.81 (3.65-3.97) | 3.58 (3.43-3.73) | 3.35 (3.17-3.53) | 3.54 (3.39-3.69) | 3.74 (3.54-3.95) | 4.01 (3.78-4.25) | 3.62 (3.38-3.85) | 3.64 (3.43-3.84) | .91 |
| Moderation components | |||||||||||||
| Refined grains | 10-0 | ≤1.8 oz equivalents/1000 kcal | ≥4.3 oz equivalents/1000 kcal | 4.98 (4.72-5.24) | 4.91 (4.67-5.15) | 5.15 (4.9-5.39) | 5.19 (4.96-5.43) | 5.36 (5.16-5.55) | 4.98 (4.80-5.15) | 5.15 (4.95-5.34) | 5.01 (4.86-5.17) | 5.01 (4.80-5.23) | .82 |
| Sodium | 10-0 | ≤1.1 g/1000 kcal | ≥2.0 g/1000 kcal | 5.28 (5.06-5.49) | 5.60 (5.46-5.74) | 5.41 (5.24-5.59) | 5.15 (4.95-5.35) | 5.0 (4.80-5.20) | 4.51 (4.27-4.76) | 4.79 (4.57-5.01) | 4.39 (4.20-4.58) | 4.41 (4.23-4.58) | <.001 |
| Added sugars | 10-0 | ≤6.5% of energy | ≥26% of energy | 4.18 (3.83-4.52) | 4.53 (4.34-4.73) | 5.10 (4.81-5.39) | 5.40 (5.14-5.65) | 5.45 (5.26-5.65) | 5.90 (5.69-6.11) | 5.97 (5.8-6.15) | 6.26 (6.04-6.48) | 6.64 (6.44-6.85) | <.001 |
| Saturated fats | 10-0 | ≤8% of energy | ≥16% of energy | 5.56 (5.26-5.86) | 5.77 (5.57-5.97) | 5.47 (5.23-5.71) | 5.29 (5.16-5.42) | 5.45 (5.23-5.66) | 5.79 (5.59-5.99) | 5.79 (5.57-6.01) | 5.54 (5.33-5.76) | 4.93 (4.65-5.21) | .05 |
Abbreviations: AHA, American Heart Association; HEI, Healthy Eating Index; MUFA, monounsaturated fatty acid; NHANES, National Health and Nutrition Examination Survey; PUFA, polyunsaturated fatty acid; SFA, saturated fatty acid.
Data were weighted to be nationally representative. Higher scores indicate greater adherence to the AHA 2020 dietary Strategic Impact Goals or the 2015 Dietary Guidelines for Americans.
Dietary components associated with AHA scores were adjusted for energy to 2000 kcal/d using the residual method prior to analysis. Each AHA consumption target was evaluated based on a continuous scoring system. Intake of each dietary component was scored from 0 to 10 (higher scores indicating higher consumption of beneficial components) and from 10 to 0 (higher scores indicating lower consumption of harmful components). For beneficial dietary components, individuals with zero intake received a score of 0. Intermediate dietary intake was scored linearly between 0 and 10. The primary total diet score is the sum of the scores for the 5 dietary components included in the primary score. The secondary total diet score is the sum of the score for all 8 components included in the primary and secondary scores.
According to the AHA 2020 Strategic Impact Goals, up to 3 c/wk (0.42 c/d) of starchy vegetables (eg, potatoes, peas, corn) could be included; this maximum was incorporated into the analysis, with higher intake not contributing toward the score. Consumption of 100% fruit juice could also be included; however, its contribution was not capped in the original AHA 2020 Strategic Impact Goals and not in our score. Some organizations recommend no more than 1 serving/d of 100% fruit juice.
The HEI-2015 total diet score is the sum of the scores for the 9 dietary components included in adequacy components and 4 dietary components included in moderation components. Intakes between the minimum and maximum standards were scored proportionately.
Includes 100% fruit juice.
Includes all forms except juice.
Includes legumes (beans and peas).
Includes all milk products, such as fluid milk, yogurt, and cheese, and fortified soy beverages.
Includes seafood, nuts, seeds, soy products (other than beverages), and legumes (beans and peas).
Ratio of PUFAs and MUFAs to SFAs.
Figure 1. Trends in Estimated Proportions of US Youth Aged 2 to 19 Years With Poor, Intermediate, or Ideal Diet Quality.
Trends are according to the American Heart Association (AHA) 2020 Strategic Impact Goals, based on a continuous scoring system by National Health and Nutrition Examination Survey (NHANES) cycles from 1999-2000 to 2015-2016. The primary score is based on total fruits and vegetables, whole grains, fish and shellfish, sugar-sweetened beverages, and sodium, and the secondary score further adds nuts, seeds, and legumes, processed meat, and saturated fat. Data were weighted to be nationally representative. Data points indicate estimated percentages; error bars, 95% CIs. For dietary quality based on the AHA primary score, P < .001 for trend for poor (decrease) and intermediate (increase) quality and P = .03 for ideal quality (increase). For dietary quality based on the AHA secondary score, P< .001 for trend for poor (decrease) and intermediate (increase) quality and P = .03 for ideal quality (increase).
Trends in Specific Foods and Nutrients
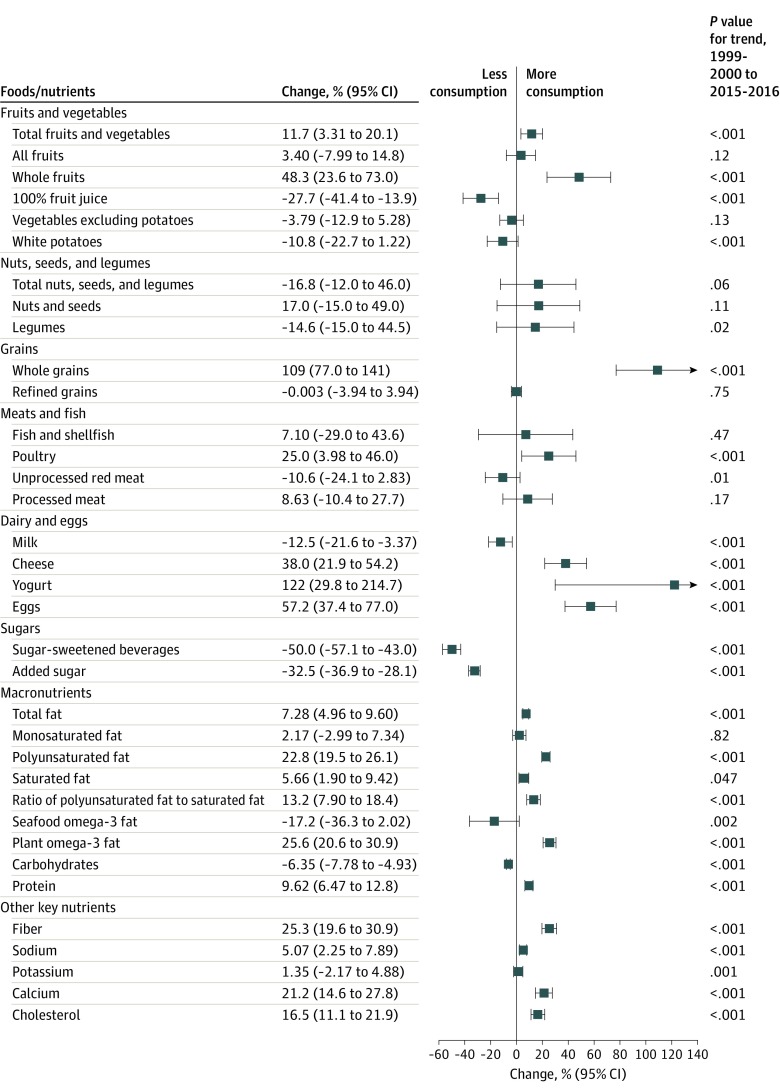
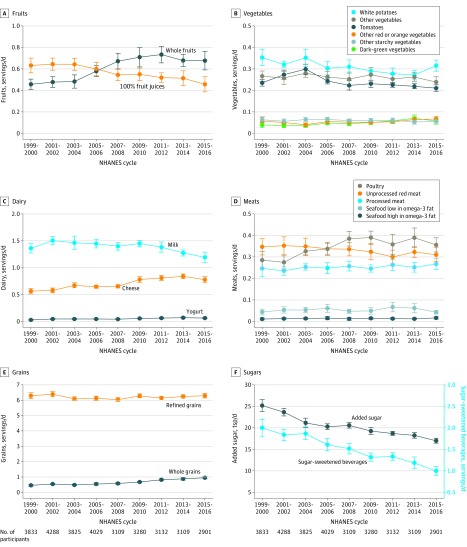
Statistically significant changes were found among individual components of the diet scores (Figure 2, Figure 3, Table 3, and eFigure 1 in the Supplement). From 1999 to 2016, the estimated mean consumption of sugar-sweetened beverages significantly decreased from 2.0 to 1.0 servings/d (difference, −1.0 [95% CI, −1.2 to −0.78] servings/d; P < .001 for trend) and added sugar from 106 g/d to 71.4 g/d (difference, −34.4 [95% CI, −40.8 to −28.1] g/d; P < .001 for trend). The estimated mean consumption of whole grains significantly increased from 0.46 to 0.95 servings/d (difference, +0.50 [95% CI, 0.40-0.59] servings/d), total fruits and vegetables from 1.62 to 1.81 servings/d (difference, +0.19 [95% CI, 0.06-0.32] servings/d), poultry from 0.28 to 0.36 servings/d (difference, +0.07 [95% CI, 0.02-0.12] servings/d), and eggs from 0.25 to 0.39 servings/d (difference, +0.14 [95% CI, 0.10-0.19] servings/d) (P < .001 for trend for all). The estimated mean consumption of sodium significantly increased from 3166 mg/d to 3326 mg/d (difference, +160 [95% CI, 74-247] mg/d; P < .001 for trend). Intakes of processed meat, refined grains, nuts and seeds, and fish and shellfish did not significantly change.
Figure 2. Changes in Estimated Mean Consumption of Dietary Components Among US Youth Aged 2 to 19 Years.
Based on National Health and Nutrition Examination Survey (NHANES) data from 1999-2000 to 2015-2016. Data represent estimated mean change in population dietary intake from 1999-2000 to 2015-2016. The analyses were based on energy-adjusted values to 2000 kcal/d using the residual method. P values for trend were estimated across all NHANES cycles from 1999 to 2016.
Figure 3. Trends in Estimated Mean Consumption of Key Food Groups and Nutrients Among US Youth Aged 2 to 19 Years by NHANES Cycles From 1999-2000 to 2015-2016.
Data are weighted to be nationally representative. Data points indicate estimated means; error bars, 95% CIs. Added sugar: 1 tsp = 4.2 g. Analyses were based on energy-adjusted values to 2000 kcal/d using the residual method. P < .001 for trend for whole fruits (increase), 100% fruit juices (decrease), white potatoes (decrease), tomatoes (decrease), dark-green vegetables (increase), milk (decrease), cheese (increase), yogurt (increase), poultry (increase), whole grains (increase), sugar-sweetened beverages (decrease), and added sugar (decrease). Other significant trends were observed for other red or orange vegetables (increase; P = .03 for trend) and unprocessed red meat (decrease; P = .01 for trend). Trends for the remaining dietary components remained stable.
Table 3. Trends in Estimated Mean Consumption of Key Dietary Components Among US Youth Aged 2 to 19 Years by NHANES Survey Cycles From 1999 to 2016.
| Dietary factors | Survey-weighted mean (95% CI)a | P value for trend | Difference, 2015-2016 vs 1999-2000 (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999-2000 (n = 3833) | 2001-2002 (n = 4288) | 2003-2004 (n = 3825) | 2005-2006 (n = 4029) | 2007-2008 (n = 3109) | 2009-2010 (n = 3280) | 2011-2012 (n = 3132) | 2013-2014 (n = 3019) | 2015-2016 (n = 2901) | |||
| AHA primary component goals | |||||||||||
| Fruits and vegetables, servings/d | 1.62 (1.54-1.69) | 1.65 (1.56-1.75) | 1.83 (1.74-1.92) | 1.83 (1.76-1.9) | 1.84 (1.73-1.95) | 1.93 (1.80-2.05) | 1.93 (1.83-2.03) | 1.86 (1.79-1.94) | 1.81 (1.70-1.91) | <.001 | 0.19 (0.06 to 0.32) |
| Whole grains, servings/d | 0.46 (0.39-0.52) | 0.54 (0.49-0.58) | 0.48 (0.43-0.53) | 0.55 (0.47-0.63) | 0.58 (0.51-0.65) | 0.67 (0.64-0.71) | 0.82 (0.76-0.88) | 0.87 (0.79-0.95) | 0.95 (0.88-1.03) | <.001 | 0.50 (0.40 to 0.59) |
| Fish and shellfish, servings/d | 0.06 (0.04-0.07) | 0.07 (0.05-0.08) | 0.07 (0.05-0.08) | 0.08 (0.05-0.10) | 0.06 (0.05-0.07) | 0.06 (0.05-0.08) | 0.08 (0.06-0.10) | 0.07 (0.05-0.10) | 0.06 (0.05-0.07) | .47 | 0.004 (−0.02 to 0.02) |
| Sugar-sweetened beverages, servings/d | 2.00 (1.80-2.20) | 1.83 (1.70-1.97) | 1.87 (1.72-2.03) | 1.61 (1.46-1.76) | 1.52 (1.39-1.64) | 1.32 (1.22-1.42) | 1.33 (1.24-1.43) | 1.19 (1.05-1.32) | 1.00 (0.90-1.10) | <.001 | −1.0 (−1.22 to −0.78) |
| Sodium, mg/d | 3166 (3089-3242) | 3148 (3111-3184) | 3193 (3154-3232) | 3263 (3205-3322) | 3302 (3261-3343) | 3307 (3252-3362) | 3241 (3180-3303) | 3387 (3287-3486) | 3326 (3285-3367) | <.001 | 160 (73.8 to 247) |
| AHA secondary component goals | |||||||||||
| Nuts, seeds, and legumes, servings/d | 0.37 (0.30-0.45) | 0.34 (0.28-0.39) | 0.38 (0.32-0.44) | 0.39 (0.34-0.44) | 0.39 (0.34-0.43) | 0.41 (0.35-0.47) | 0.43 (0.36-0.49) | 0.37 (0.33-0.42) | 0.44 (0.38-0.50) | .06 | 0.06 (−0.04 to 0.16) |
| Processed meat, servings/d | 0.25 (0.21-0.28) | 0.24 (0.21-0.26) | 0.25 (0.24-0.27) | 0.25 (0.22-0.27) | 0.26 (0.23-0.28) | 0.25 (0.23-0.26) | 0.26 (0.24-0.29) | 0.25 (0.23-0.27) | 0.27 (0.24-0.29) | .17 | 0.02 (−0.02 to 0.07) |
| Saturated fat, % of energy | 11.5 (11.2-11.8) | 11.3 (11.1-11.5) | 11.6 (11.4-11.8) | 11.8 (11.7-11.9) | 11.6 (11.4-11.8) | 11.3 (11.1-11.5) | 11.3 (11.1-11.5) | 11.5 (11.3-11.7) | 12.1 (11.9-12.4) | .05 | 0.65 (0.23 to 1.07) |
| HEI-2015 componentsb | |||||||||||
| Total fruits, servings/d | 1.01 (0.93-1.09) | 1.05 (0.96-1.14) | 1.07 (0.97-1.17) | 1.09 (1.03-1.16) | 1.11 (1.01-1.21) | 1.16 (1.05-1.26) | 1.19 (1.10-1.28) | 1.08 (1.00-1.17) | 1.04 (0.96-1.13) | .12 | 0.03 (−0.08 to 0.15) |
| Intact/whole fruit, servings/d | 0.46 (0.41-0.51) | 0.48 (0.43-0.53) | 0.48 (0.42-0.55) | 0.58 (0.53-0.63) | 0.67 (0.60-0.75) | 0.71 (0.62-0.80) | 0.73 (0.66-0.81) | 0.68 (0.62-0.74) | 0.68 (0.59-0.76) | <.001 | 0.22 (0.12 to 0.32) |
| Total vegetables, servings/d | 1.02 (0.95-1.09) | 1.00 (0.96-1.04) | 1.08 (1.03-1.13) | 0.99 (0.95-1.03) | 0.97 (0.91-1.02) | 0.98 (0.93-1.03) | 0.95 (0.91-0.99) | 0.98 (0.93-1.02) | 0.98 (0.94-1.02) | .02 | −0.04 (−0.12 to 0.04) |
| Dark-green vegetables, servings/d | 0.04 (0.03-0.05) | 0.04 (0.03-0.05) | 0.04 (0.03-0.04) | 0.05 (0.04-0.05) | 0.05 (0.04-0.06) | 0.05 (0.04-0.06) | 0.06 (0.05-0.07) | 0.07 (0.06-0.09) | 0.06 (0.04-0.07) | <.001 | 0.02 (0 to 0.04) |
| Legumes, servings/d | 0.07 (0.05-0.08) | 0.06 (0.05-0.07) | 0.06 (0.05-0.08) | 0.06 (0.04-0.07) | 0.06 (0.04-0.07) | 0.07 (0.06-0.08) | 0.07 (0.06-0.09) | 0.07 (0.06-0.08) | 0.08 (0.06-0.09) | .02 | 0.01 (−0.009 to 0.03) |
| Refined grains, servings/d | 6.29 (6.09-6.49) | 6.39 (6.22-6.57) | 6.09 (5.96-6.22) | 6.12 (5.97-6.27) | 6.04 (5.92-6.17) | 6.28 (6.16-6.41) | 6.13 (6.01-6.26) | 6.24 (6.14-6.35) | 6.29 (6.14-6.44) | .75 | 0 (−0.25 to 0.25) |
| Total dairy, servings/d | 1.99 (1.88-2.10) | 2.18 (2.08-2.27) | 2.22 (2.09-2.36) | 2.20 (2.13-2.28) | 2.19 (2.11-2.27) | 2.38 (2.30-2.46) | 2.35 (2.23-2.46) | 2.29 (2.19-2.39) | 2.13 (1.98-2.28) | .005 | 0.14 (−0.04 to 0.33) |
| Unprocessed red meat, servings/d | 0.35 (0.31-0.39) | 0.35 (0.31-0.39) | 0.35 (0.31-0.39) | 0.34 (0.31-0.36) | 0.34 (0.30-0.37) | 0.32 (0.29-0.36) | 0.30 (0.27-0.33) | 0.32 (0.30-0.35) | 0.31 (0.28-0.34) | .01 | −0.04 (−0.09 to 0.01) |
| Poultry, servings/d | 0.28 (0.24-0.33) | 0.27 (0.24-0.31) | 0.33 (0.31-0.35) | 0.34 (0.31-0.37) | 0.38 (0.35-0.42) | 0.39 (0.36-0.42) | 0.36 (0.31-0.41) | 0.39 (0.34-0.44) | 0.36 (0.32-0.39) | <.001 | 0.07 (0.02 to 0.12) |
| Eggs, servings/d | 0.25 (0.23-0.27) | 0.29 (0.25-0.32) | 0.30 (0.26-0.33) | 0.35 (0.33-0.38) | 0.37 (0.34-0.41) | 0.36 (0.32-0.4) | 0.36 (0.32-0.39) | 0.36 (0.34-0.38) | 0.39 (0.36-0.43) | <.001 | 0.14 (0.10 to 0.19) |
| Nuts and seeds, servings/d | 0.34 (0.26-0.42) | 0.31 (0.25-0.36) | 0.35 (0.29-0.41) | 0.36 (0.31-0.41) | 0.36 (0.31-0.40) | 0.37 (0.31-0.43) | 0.39 (0.32-0.46) | 0.34 (0.29-0.39) | 0.40 (0.34-0.46) | .11 | 0.06 (−0.04 to 0.16) |
| Soy, servings/d | 0.01 (0.008-0.02) | 0.03 (0.02-0.04) | 0.04 (0.03-0.05) | 0.02 (0.02-0.03) | 0.03 (0.02-0.04) | 0.04 (0.03-0.04) | 0.06 (0.05-0.07) | 0.05 (0.03-0.06) | 0.05 (0.04-0.07) | <.001 | 0.04 (0.03 to 0.05) |
| Seafood high in omega-3, servings/d | 0.01 (0.007-0.02) | 0.01 (0.009-0.02) | 0.01 (0.009-0.02) | 0.02 (0.008-0.02) | 0.01 (0.005-0.02) | 0.01 (0.01-0.02) | 0.01 (0.009-0.02) | 0.01 (0.008-0.02) | 0.02 (0.01-0.02) | .45 | 0.005 (−0.002 to 0.01) |
| Seafood low in omega-3, servings/d | 0.04 (0.03-0.06) | 0.05 (0.04-0.07) | 0.05 (0.04-0.07) | 0.06 (0.04-0.08) | 0.05 (0.04-0.06) | 0.05 (0.03-0.06) | 0.07 (0.04-0.09) | 0.06 (0.04-0.08) | 0.04 (0.03-0.05) | .54 | −0.001 (−0.02 to 0.02) |
| Polyunsaturated fat, % of energy | 6.17 (6.03-6.32) | 5.94 (5.80-6.09) | 6.46 (6.35-6.56) | 6.41 (6.23-6.59) | 6.53 (6.43-6.64) | 6.84 (6.72-6.97) | 7.41 (7.28-7.55) | 7.29 (7.10-7.47) | 7.58 (7.47-7.69) | <.001 | 1.41 (1.23 to 1.58) |
| Monounsaturated fat, % of energy | 14.8 (14.2-15.3) | 14.5 (13.9-15.0) | 13.4 (12.8-14.0) | 14.0 (13.5-14.4) | 15.0 (14.6-15.4) | 13.7 (13.3-14.1) | 13.4 (13.1-13.8) | 13.9 (13.5-14.4) | 15.1 (14.6-15.6) | .82 | 0.32 (−0.44 to 10.1) |
| Added sugar, g/d | 106 (99.9-112) | 99.4 (95.7-103) | 88.9 (84.2-93.6) | 85.2 (82.4-88.0) | 86.6 (83.7-89.4) | 80.9 (77.5-84.3) | 78.5 (76.5-80.5) | 76.7 (73.9-79.6) | 71.4 (69.0-73.9) | <.001 | −8.18 (−9.70 to −6.66) |
Abbreviation: AHA, American Heart Association; HEI, Healthy Eating Index; NHANES, National Health and Nutrition Examination Survey.
Data are weighted to be nationally representative. The majority of means were adjusted for energy to 2000 kcal/d using the residual method. The means for saturated fat, monounsaturated fat, and polyunsaturated fat were adjusted as a percentage of total energy.
The HEI-2015 components are disaggregated into separate parts. For example, greens and beans are presented separately as dark-green vegetables and legumes. Total protein foods are presented as poultry, processed meat, unprocessed red meat, seafood, soy, and nuts and seeds. Components such as processed meat, saturated fat, and sodium that are covered by the AHA are not presented again under the HEI components (eTables 3 and 4 in the Supplement).
Among subcomponents of these food groups (Figure 2, Figure 3, and eFigure 1 and eTable 7 in the Supplement), intakes of intact/whole fruit significantly increased from 0.46 to 0.68 servings/d (difference, +0.22 [95% CI, 0.12-0.32] servings/d; P < .001 for trend), while 100% fruit juice significantly decreased from 0.63 to 0.46 servings/d (difference, −0.17 [95% CI, −0.27 to −0.07] servings/d; P < .001 for trend). Milk significantly decreased from 1.36 to 1.19 servings/d (difference, −0.17 [95% CI, −0.30 to −0.04] servings/d), cheese significantly increased from 0.56 to 0.78 servings/d (difference, +0.21 [95% CI, 0.14-0.29] servings/d), and yogurt significantly increased from 0.03 to 0.06 servings/d (difference, +0.03 [95% CI, 0.02-0.05] servings/d) (P < .001 for trend for all).
Among other foods and nutrients, consumption of unprocessed red meat significantly decreased from 0.35 to 0.31 servings/d (difference, −0.04 [95% CI, −0.09 to 0.01] servings/d; P = .01 for trend), while processed meat consumption remained stable (P = .17 for trend) (Figure 2, Table 3, and eTable 7 in the Supplement). Significant increases were also observed for total fat, with estimated means increasing from 33.2% to 34.5% of energy (difference, +2.34% [95% CI, 1.62%-3.06%] of energy), polyunsaturated fat from 6.17% to 7.58% of energy (difference, +1.41% [95% CI, 1.23%-1.58%] of energy), and protein from 13.4% to 14.8% of energy (difference, +1.29% [95% CI, 0.90%-1.69%] of energy) (P < .001 for trend for all). The estimated mean consumption of total carbohydrate significantly decreased from 55.4% to 51.9% of energy (difference, −3.52% [95% CI, −4.34% to −2.69%] of energy; P < .001 for trend). The estimated mean consumption of plant omega-3 fat significantly increased from 116 mg/d to 146 mg/d (difference, +29.7 [95% CI, 24.9-34.6] mg/d; P < .001 for trend), whereas the estimated mean consumption of seafood omega-3 fat significantly decreased from 51 mg/d to 42.3 mg/d (difference, −8.74 [95% CI, −19.8 to 2.33] mg/d; P = .002 for trend). Other significant increases were identified for dietary cholesterol from 218 mg/d to 254 mg/d (difference, +36.0 [95% CI, 24.8-47.2] mg/d), fiber from 12.4 mg/d to 15.6 mg/d (difference, +3.14 [95% CI, 2.53-3.76] mg/d), and calcium from 875 mg/d to 1061 mg/d (difference, +186 [95% CI, 132-240] mg/d) (P < .001 for trend for all).
In sensitivity analyses, the findings for most dietary components were not materially altered by adjustment for sociodemographic shifts in age, sex, and race/ethnicity over time (eTable 8 in the Supplement). Exceptions included legumes, in which observed increases were partially attenuated (by 53.2%) by these adjustments, total dairy (increased further by 14.7%), and unprocessed red meat (increased further by 13.7%).
Trends in Population Subgroups
From 1999 to 2016, significant improvements in diet quality were observed among all subgroups, but with mostly persistent or increasing differences based on mean dietary scores (eTables 9 and 10 in the Supplement) or proportions having poor, intermediate, or ideal diet quality (eTables 11 and 12 in the Supplement). For example, while diet quality significantly improved in all age groups, the estimated proportion of youth having poor diet quality in 2015-2016 was 39.8% (95% CI, 35.1%-44.5%) for ages 2 to 5 years, 52.5% (95% CI, 46.4%-58.5%) for ages 6 to 11 years, and 66.6% (95% CI, 61.4%-71.4%) for ages 12 to 19 years (P < .001 for differences by age in 2015-2016). Similarly, while diet quality improved over time among youth with higher or lower parental education, household income, or household food security status, the estimated proportion with poor diet quality in 2015-2016 was 64.5% (95% CI, 59.5%-69.1%) among youth with household income less than 1.30 times the poverty level and 47.2% (95% CI, 39.4%-55.3%) among youth with household income of at least 3.00 times the poverty level (P = .02 for differences by income in 2015-2016), with similar differences across levels of parental education or household food security status. In contrast, the estimated proportions of youth having poor diet quality in 2015-2016 were statistically nonsignificant among youth participating or not participating in SNAP (yes: 59.8% [95% CI, 54.7%-64.7%]; no: 54.4% [95% CI, 50.4%-58.4%]) or WIC (yes: 54.4% [95% CI, 46.9%-61.8%]; no: 56.2% [95% CI, 52.6%-59.7%]).
Trends in individual food groups and nutrients according to population subgroups are shown in eFigures 2 through 7 and eTables 13 through 21 in the Supplement. Dietary factors with notable population subgroup differences in trends over time included refined grains, sugar-sweetened beverages, white potatoes, processed meat, fruit juice, whole fruit, nuts and seeds, and sodium. For example, the estimated mean consumption of refined grains significantly increased from 6.22 servings/d (95% CI, 6.10-6.34 servings/d) to 6.60 servings/d (95% CI, 6.45-6.75 servings/d) among Mexican American youth (P < .001 for trend) but remained stable among non-Hispanic white and non-Hispanic black youth (P < .001 for interaction). Intakes of sugar-sweetened beverages significantly decreased across all subgroups but with larger decreases among youth aged 12 to 19 years, males, and youth not participating in federal food assistance programs (P ≤ .01 for interaction for all). Increases in whole fruit were larger among youth not participating in reduced-price/free school nutrition programs (P = .005 for interaction), while fruit juice intake decreased more among females than males and among those with higher vs lower parental education level (P < .05 for interaction for each). Nuts and seeds increased more among youth aged 12 to 19 years; those with higher parental education, household income, or food security; and those not participating in federal food assistance programs (P < .05 for interaction for each).
Discussion
From 1999 to 2016, overall dietary quality improved among US youth, associated with increased consumption of fruits and vegetables (especially whole fruits) and whole grains, with additional increases in total dairy, total protein foods, seafood, and plant proteins and decreased consumption of sugar-sweetened beverages and added sugar. Based on the different validated dietary scores, mean dietary quality improved by 11.2% to 27.0%. The proportion of US youth with poor diets decreased substantially (from 71.8% to 54.4%), with these youth shifting to diets that were intermediate but not ideal in quality. Yet overall diet quality remained low, with more than half of US youth still having a poor diet. Significant trends were not identified for consumption of total vegetables, fish and shellfish, processed meats, or refined grains, and statistically significant but small changes were observed for other food components.
Dietary sodium increased and greatly exceeded the 2019 National Academies of Sciences, Engineering, and Medicine dietary reference intake of 2300 mg/d,21 which may relate to steadily increasing consumption of processed foods and food prepared away from home.22,23 These findings support the need for reactivating the currently suspended long-term US Food and Drug Administration voluntary sodium targets and timelines for reducing sodium in packaged foods and restaurant foods.24
Persistent differences in overall diet quality were identified by major population sociodemographic factors, with little evidence for declining differences during this 18-year period and some increasing differences for certain foods. For example, compared with younger children, older youth had persistently worse diet quality (with an estimated 66.6% of adolescents having poor diet quality in 2015-2016), consistent with increased marketing, availability, and/or selection of less healthy foods at older ages. Similar persistent differences were identified by parental education, household income, and household food security status. Differences in diet quality were much smaller by participation in SNAP or WIC. These results support the need for continued efforts from federal and local governments, nonprofit organizations, and industry to improve diet quality among all sectors of US youth.25,26
Prior analyses of diets among US youth generally assessed a limited number of factors,12,14,22,27 with few reporting on overall diet quality.15,28,29 A study assessing trends in HEI-2010 among US youth through 201212 identified modest improvements overall and in component scores for whole fruits, whole grains, dairy, total protein foods, sugar-sweetened beverages, and added sugar. These findings build on and extend previous reports by assessing dietary trends through 2016, evaluating several diet quality scores and diverse individual foods and nutrients, and assessing differences in trends according to multiple sociodemographic factors. Compared with recent analyses among US adults,17,30 some similarities and differences are evident. Similar to the present findings for youth, overall diet quality among US adults slowly improved, mainly because of increased whole grains and decreased sugar-sweetened beverages and added sugar; yet large proportions continued to have poor diet quality, with persistent or increasing differences among key sociodemographic subgroups.17 Adults, but not children, exhibited increased consumption of nuts and seeds and fish and shellfish and decreased consumption of refined grains.17 These results highlight the need for future research to illuminate the reasons for both similarities and differences in dietary trends in US children vs adults.
Several of the changes in mean daily servings were modest, yet such small changes in daily intake may sum to more meaningful changes in weekly, monthly, or yearly consumption. In addition, small mean changes across an entire population can influence the overall exposure distribution and corresponding risk in that population.31 Consistent with this, the modest changes in mean intake of individual foods led to meaningful changes in the estimated proportions of US youth consuming poor vs intermediate diets. While diets later in life are linked to many major health outcomes, determining these relationships in youth is more challenging, given their low absolute risk of disease. The strongest evidence is generally for childhood overweight and obesity linked to intakes of sugar-sweetened beverages and ultraprocessed foods.32 The findings of modest overall dietary improvements but persistent poor diets among the majority of children and adolescents are consistent with the slowing or potential plateauing, but not reversing, of obesity rates among US youth.33 Because dietary habits in earlier life influence habits in adulthood,2,34 these findings suggest potential long-term benefits of the modest observed improvements in diet quality as well as major continuing concerns for the large numbers of youth with poor diets and the enduring differences by sociodemographic factors.
During the period of this study, 3 iterations of the Dietary Guidelines for Americans progressively focused on healthy foods and diet patterns rather than isolated nutrient targets35; the White House Let’s Move program focused on healthier eating and physical activity in children36; the Child Nutrition Act improved and strengthened child nutrition programs3; and the Healthy, Hunger-Free Kids Act set more rigorous nutrition standards for school meals and competitive foods.4 Advocacy organizations like the American Academy of Pediatrics and the AHA promoted fruits, vegetables, and whole grains and avoidance of sugar-sweetened beverages and added sugar.18,37 Industry also reduced added sugar in beverages, stimulated by both market demand and voluntary targets. Other national actions, which may be too recent to have significantly influenced the observed trends through 2015-2016, include passage of the SNAP FINI (now GusNIP) program in 20149 and implementation of sugar-sweetened beverage taxes and proposed warning labels in several US localities.38 The findings support the need for rigorous evaluation of national and community strategies to improve diet quality to identify the most influential actions.
Limitations
This study has several limitations. First, self-reported dietary information is subject to random and systematic error. Yet interview-administered 24-hour recalls using computer-assisted personal interview system were used; results were further adjusted for total energy, each of which reduce measurement error; and random error does not bias population or stratum-specific mean intakes. Second, no single metric of diet quality is established. However, the results were generally consistent among 2 AHA diet scores and the HEI-2015 score. Third, methodologic changes over time in NHANES data collection and food and nutrition databases might influence the estimated trends. Such effects were minimized by pairing each NHANES cycle with the corresponding “What We Eat in America” database. Fourth, the cross-sectional nature of each NHANES cycle does not allow direct evaluation of changes in diet among individuals, only of national dietary trends. Fifth, although these dietary scores have been validated against clinical outcomes in diverse adult populations,39 their potential clinical relevance among youth may not be generalizable and requires validation against clinical outcomes relevant to youth. Sixth, even though these may be the most recent data available, it is uncertain whether the findings observed are applicable to diet quality among youth in 2020.
Conclusions
Based on serial NHANES surveys from 1999 to 2016, the estimated overall diet quality of US youth showed modest improvement, but more than half of youth still had poor-quality diets.
eAppendix 1. Methods of Estimating American Heart Association (AHA) Dietary Scores and Healthy Eating Index (HEI)-2015 Scores
eAppendix 2. Identification for Participation in Federal Nutrition Assistance Program and Harmonization Across NHANES Cycles
eTable 1. Dietary Components of the American Heart Association (AHA) 2020 Strategic Impact Goals Scoring Standards
eTable 2. Dietary Components of Healthy Eating Index (HEI)-2015 and Scoring Standards
eTable 3. The Disaggregated Dietary Components Modeled in Markov Chain Monte Carlo (MCMC) Method
eTable 4. Trends in Estimated Percentage of US Children Aged 2-19 Years Old With Poor or Intermediate Diet Based on Primary and Secondary American Heart Association (AHA) Continuous Diet Score by NHANES Survey Cycles, 1999-2016
eTable 5. Sensitivity Analysis of the Healthy Eating Index (HEI)-2015 Total and Component Scores Estimated Using the Population Ratio Methods Among US Children Aged 2-19 Years Old by NHANES Survey Cycles, 1999-2016
eTable 6. Sensitivity Analysis of the Healthy Eating Index (HEI)-2015 Total and Component Scores Estimated Using the Markov Chain Monte Carlo (MCMC) Method Among US Children Aged 2-19 Years Old by NHANES Survey Cycles, 2003-2016
eTable 7. Trends in Estimated Mean Consumption of Key Food Groups and Nutrients Among US Children Aged 2-19 Years Old by NHANES Survey Cycles, 1999-2016
eTable 8. Impact of Adjusting for Demographic Changes in Age, Sex, and Race/Ethnicity on Observed Trends for Selected Dietary Factors Among US Children Aged 2-19 Years Old From 1999 to 2016
eTable 9. Trends in Estimated Primary and Secondary American Heart Association (AHA) Diet Scores by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 10. Trends in Estimated Healthy Eating Index (HEI)-2015 by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 11. Trends in Estimated Percentage of US Children With Poor or Intermediate Diet Based on Primary American Heart Association (AHA) Continuous Diet Score by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 12. Trends in Estimated Percentage of US Children With Poor or Intermediate Diet Based on Secondary American Heart Association (AHA) Continuous Diet Score by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 13. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Age Group Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 14. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Sex Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 15. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Race/Ethnicity Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 16. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Parental Education Levels Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 17. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Family Income to Poverty Ratio (PIR) Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 18. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Household Food Security Status Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2014
eTable 19. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Participation of Supplemental Nutrition Assistance Program (SNAP) Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2014
eTable 20. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Participation of Women, Infants, & Children (WIC) Nutrition Program Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2014
eTable 21. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Participation of National School Lunch Program (NSLP)/School Breakfast Program (SBP) Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eFigure 1. Trends in Estimated Mean Consumption of Nuts/Seeds and Legumes (Panel A), Sodium and Potassium (Panel B), and Dietary Fat (Panel C) Among US Children Based on NHANES Data From 1999-2016
eFigure 2. Trends in Estimated Mean Consumption of Sugar-Sweetened Beverages (Panel A), Refined Grain (Panel B), White Potato (Panel C), Processed Meat (Panel D), Sodium (Panel E), and Fruit Juice (Panel F) by Age, Sex, and Race/Ethnicity Among US Children Based on NHANES Data From 1999-2016
eFigure 3. Trends in Estimated Mean Consumption of Whole Grains (Panel A), Nuts/Seeds (Panel B), Fruits (Panel C), and Seafoods (Panel D) by Age, Sex, and Race/Ethnicity Among US Children Based on NHANES Data From 1999-2016
eFigure 4. Trends in Estimated Mean Consumption of Sugar-Sweetened Beverages (Panel A), Refined Grain (Panel B), White Potato (Panel C), Processed Meat (Panel D), Sodium (Panel E), and Fruit Juice (Panel F) by Parental Education Level, Household Income Level, and Household Food Security Level Among US Children Based on NHANES Data From 1999-2016
eFigure 5. Trends in Estimated Mean Consumption of Whole Grains (Panel A), Nuts/Seeds (Panel B), Fruits (Panel C), and Seafoods (Panel D) by Parental Education Level, Household Income Level, and Household Food Security Level Among US Children Based on NHANES Data From 1999-2016
eFigure 6. Trends in Estimated Mean Consumption of Sugar-Sweetened Beverages (Panel A), Refined Grain (Panel B), White Potato (Panel C), Processed Meat (Panel D), Sodium (Panel E), and Fruit Juice (Panel F) by Participation of Women, Infants, and Children (WIC), Supplemental Nutrition Assistance Program (SNAP), and National School Lunch/Breakfast Program Among US Children Based on NHANES Data From 1999-2016
eFigure 7. Trends in Estimated Mean Consumption of Whole Grains (Panel A), Nuts/Seeds (Panel B), Fruits (Panel C), and Seafoods (Panel D) by Participation of Women, Infants, and Children (WIC), Supplemental Nutrition Assistance Program (SNAP), and National School Lunch/Breakfast Program Among US Children Based on NHANES Data From 1999-2016
eReferences
References
- 1.Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912-924. doi: 10.1001/jama.2017.0947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scaglioni S, De Cosmi V, Ciappolino V, Parazzini F, Brambilla P, Agostoni C. Factors influencing children’s eating behaviours. Nutrients. 2018;10(6):706. doi: 10.3390/nu10060706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Healthy, Hunger-Free Kids Act, Pub L No. 111-296 (2010).
- 4.US Department of Agriculture Food and Nutrition Service Healthy Hunger-Free Kids Act. Accessed September 26, 2019. https://www.fns.usda.gov/school-meals/healthy-hunger-free-kids-act
- 5.US Department of Agriculture Gus Schumacher Nutrition Incentive Program (formerly FINI). Accessed September 28, 2019. https://nifa.usda.gov/program/gus-schumacher-nutrition-incentive-grant-program
- 6.Saksena MJ, Okrent AM, Anekwe TD, et al. . America’s Eating Habits: Food Away From Home. US Dept of Agriculture Economic Research Service; 2018. [Google Scholar]
- 7.Kraak VI, Gootman JA, McGinnis JM. Food Marketing to Children and Youth: Threat or Opportunity? National Academies Press; 2006. [Google Scholar]
- 8.Powell LM, Wada R, Kumanyika SK. Racial/ethnic and income disparities in child and adolescent exposure to food and beverage television ads across the U.S. media markets. Health Place. 2014;29:124-131. doi: 10.1016/j.healthplace.2014.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whole Grains Council Success and awareness of the Whole Grain Stamp. Accessed September 26, 2019. https://wholegrainscouncil.org/newsroom/whole-grain-statistics
- 10.Fortune PepsiCo sets a global target to reduce sugar in its soft drinks. Accessed September 26, 2019. https://fortune.com/2016/10/17/pepsico-sugar-soft-drinks/
- 11.Dunford EK, Popkin BM. 37 year snacking trends for US children 1977-2014. Pediatr Obes. 2018;13(4):247-255. doi: 10.1111/ijpo.12220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gu X, Tucker KL. Dietary quality of the US child and adolescent population: trends from 1999 to 2012 and associations with the use of federal nutrition assistance programs. Am J Clin Nutr. 2017;105(1):194-202. doi: 10.3945/ajcn.116.135095 [DOI] [PubMed] [Google Scholar]
- 13.Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage consumption among children and adults, 2003-2014. Obesity (Silver Spring). 2018;26(2):432-441. doi: 10.1002/oby.22056 [DOI] [PubMed] [Google Scholar]
- 14.Rehm CD, Drewnowski A. Trends in consumption of solid fats, added sugars, sodium, sugar-sweetened beverages, and fruit from fast food restaurants and by fast food restaurant type among US children, 2003-2010. Nutrients. 2016;8(12):804. doi: 10.3390/nu8120804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomson JL, Tussing-Humphreys LM, Goodman MH, Landry AS. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am J Clin Nutr. 2019;109(1):127-138. doi: 10.1093/ajcn/nqy284 [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention NHANES survey methods and analytic guidelines. Accessed June 8, 2019. https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx
- 17.Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among us adults, 1999-2012. JAMA. 2016;315(23):2542-2553. doi: 10.1001/jama.2016.7491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lloyd-Jones DM, Hong Y, Labarthe D, et al. ; American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586-613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 19.Krebs-Smith SM, Pannucci TE, Subar AF, et al. . Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591-1602. doi: 10.1016/j.jand.2018.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Cancer Institute The Healthy Eating Index. Accessed June 12, 2019. https://epi.grants.cancer.gov/hei/
- 21.National Academies of Sciences, Engineering, and Medicine Dietary Reference Intakes for Sodium and Potassium. National Academies Press; 2019. doi: 10.17226/25353 [DOI] [PubMed] [Google Scholar]
- 22.Bleich SN, Wolfson JA. Trends in SSBs and snack consumption among children by age, body weight, and race/ethnicity. Obesity (Silver Spring). 2015;23(5):1039-1046. doi: 10.1002/oby.21050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saksena M, Okrent AM, Hamrick KS, et al. , eds. America’s Eating Habits: Food Away From Home. US Department of Agriculture Economic Research Service; September 2018. [Google Scholar]
- 24.Roman L; Salt Institute Re: docket No. FDA-2014-D-0055; voluntary sodium reduction goals: target mean and upper bound concentrations for sodium in commercially processed, packaged, and prepared foods. Accessed July 16, 2019. https://www.agri-pulse.com/ext/resources/pdfs/s/a/l/t/s/salt-institute-comments.pdf
- 25.Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133(2):187-225. doi: 10.1161/CIRCULATIONAHA.115.018585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mozaffarian D, Angell SY, Lang T, Rivera JA. Role of government policy in nutrition-barriers to and opportunities for healthier eating. BMJ. 2018;361:k2426. doi: 10.1136/bmj.k2426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slining MM, Popkin BM. Trends in intakes and sources of solid fats and added sugars among U.S. children and adolescents: 1994-2010. Pediatr Obes. 2013;8(4):307-324. doi: 10.1111/j.2047-6310.2013.00156.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297-306. doi: 10.1016/j.jand.2012.08.011 [DOI] [PubMed] [Google Scholar]
- 29.Hiza H, Guenther P, Rihane C. Diet Quality of Children Age 2-17 Years as Measured by the Healthy Eating Index-2010. Nutrition Insight; 2013. [Google Scholar]
- 30.Shan Z, Rehm CD, Rogers G, et al. . Trends in dietary carbohydrate, protein, and fat intake and diet quality among US adults, 1999-2016. JAMA. 2019;322(12):1178-1187. doi: 10.1001/jama.2019.13771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32-38. doi: 10.1093/ije/14.1.32 [DOI] [PubMed] [Google Scholar]
- 32.Costa CS, Del-Ponte B, Assunção MCF, Santos IS. Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review. Public Health Nutr. 2018;21(1):148-159. doi: 10.1017/S1368980017001331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723-1725. doi: 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. 2007;35(1):22-34. doi: 10.1111/j.1748-720X.2007.00111.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dietary Guidelines for Americans US Department of Health and Human Services. Accessed February 25, 2020. https://www.hhs.gov/fitness/eat-healthy/dietary-guidelines-for-americans/index.html
- 36.Let’s Move: America’s Move to Raise a Healthier Generation of Kids. White House Task Force on Childhood Obesity report to the President. The White House. Accessed September 22, 2019. https://letsmove.obamawhitehouse.archives.gov/white-house-task-force-childhood-obesity-report-president
- 37.Gidding SS, Dennison BA, Birch LL, et al. ; American Heart Association; American Academy of Pediatrics . Dietary recommendations for children and adolescents: a guide for practitioners: consensus statement from the American Heart Association. Circulation. 2005;112(13):2061-2075. doi: 10.1161/CIRCULATIONAHA.105.169251 [DOI] [PubMed] [Google Scholar]
- 38.Paarlberg R, Mozaffarian D, Micha R, Chelius C.. Keeping soda in SNAP: understanding the other iron triangle. Society. 2018;55(4):308-317. doi: 10.1007/s12115-018-0260-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwingshackl L, Bogensberger B, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2018;118(1):74-100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Methods of Estimating American Heart Association (AHA) Dietary Scores and Healthy Eating Index (HEI)-2015 Scores
eAppendix 2. Identification for Participation in Federal Nutrition Assistance Program and Harmonization Across NHANES Cycles
eTable 1. Dietary Components of the American Heart Association (AHA) 2020 Strategic Impact Goals Scoring Standards
eTable 2. Dietary Components of Healthy Eating Index (HEI)-2015 and Scoring Standards
eTable 3. The Disaggregated Dietary Components Modeled in Markov Chain Monte Carlo (MCMC) Method
eTable 4. Trends in Estimated Percentage of US Children Aged 2-19 Years Old With Poor or Intermediate Diet Based on Primary and Secondary American Heart Association (AHA) Continuous Diet Score by NHANES Survey Cycles, 1999-2016
eTable 5. Sensitivity Analysis of the Healthy Eating Index (HEI)-2015 Total and Component Scores Estimated Using the Population Ratio Methods Among US Children Aged 2-19 Years Old by NHANES Survey Cycles, 1999-2016
eTable 6. Sensitivity Analysis of the Healthy Eating Index (HEI)-2015 Total and Component Scores Estimated Using the Markov Chain Monte Carlo (MCMC) Method Among US Children Aged 2-19 Years Old by NHANES Survey Cycles, 2003-2016
eTable 7. Trends in Estimated Mean Consumption of Key Food Groups and Nutrients Among US Children Aged 2-19 Years Old by NHANES Survey Cycles, 1999-2016
eTable 8. Impact of Adjusting for Demographic Changes in Age, Sex, and Race/Ethnicity on Observed Trends for Selected Dietary Factors Among US Children Aged 2-19 Years Old From 1999 to 2016
eTable 9. Trends in Estimated Primary and Secondary American Heart Association (AHA) Diet Scores by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 10. Trends in Estimated Healthy Eating Index (HEI)-2015 by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 11. Trends in Estimated Percentage of US Children With Poor or Intermediate Diet Based on Primary American Heart Association (AHA) Continuous Diet Score by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 12. Trends in Estimated Percentage of US Children With Poor or Intermediate Diet Based on Secondary American Heart Association (AHA) Continuous Diet Score by Age Group, Sex, Race/Ethnicity, Parental Education, Household Income, Food Security Status, and Participation of Food Assistance Programs by NHANES Survey Cycles, 1999-2016
eTable 13. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Age Group Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 14. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Sex Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 15. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Race/Ethnicity Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 16. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Parental Education Levels Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 17. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Family Income to Poverty Ratio (PIR) Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eTable 18. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Household Food Security Status Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2014
eTable 19. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Participation of Supplemental Nutrition Assistance Program (SNAP) Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2014
eTable 20. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Participation of Women, Infants, & Children (WIC) Nutrition Program Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2014
eTable 21. Trends in Estimated Mean Consumption of Food Groups and Nutrients of Interest by Participation of National School Lunch Program (NSLP)/School Breakfast Program (SBP) Among US Children by NHANES Survey Cycles, 1999-2004, 2005-2010 and 2011-2016
eFigure 1. Trends in Estimated Mean Consumption of Nuts/Seeds and Legumes (Panel A), Sodium and Potassium (Panel B), and Dietary Fat (Panel C) Among US Children Based on NHANES Data From 1999-2016
eFigure 2. Trends in Estimated Mean Consumption of Sugar-Sweetened Beverages (Panel A), Refined Grain (Panel B), White Potato (Panel C), Processed Meat (Panel D), Sodium (Panel E), and Fruit Juice (Panel F) by Age, Sex, and Race/Ethnicity Among US Children Based on NHANES Data From 1999-2016
eFigure 3. Trends in Estimated Mean Consumption of Whole Grains (Panel A), Nuts/Seeds (Panel B), Fruits (Panel C), and Seafoods (Panel D) by Age, Sex, and Race/Ethnicity Among US Children Based on NHANES Data From 1999-2016
eFigure 4. Trends in Estimated Mean Consumption of Sugar-Sweetened Beverages (Panel A), Refined Grain (Panel B), White Potato (Panel C), Processed Meat (Panel D), Sodium (Panel E), and Fruit Juice (Panel F) by Parental Education Level, Household Income Level, and Household Food Security Level Among US Children Based on NHANES Data From 1999-2016
eFigure 5. Trends in Estimated Mean Consumption of Whole Grains (Panel A), Nuts/Seeds (Panel B), Fruits (Panel C), and Seafoods (Panel D) by Parental Education Level, Household Income Level, and Household Food Security Level Among US Children Based on NHANES Data From 1999-2016
eFigure 6. Trends in Estimated Mean Consumption of Sugar-Sweetened Beverages (Panel A), Refined Grain (Panel B), White Potato (Panel C), Processed Meat (Panel D), Sodium (Panel E), and Fruit Juice (Panel F) by Participation of Women, Infants, and Children (WIC), Supplemental Nutrition Assistance Program (SNAP), and National School Lunch/Breakfast Program Among US Children Based on NHANES Data From 1999-2016
eFigure 7. Trends in Estimated Mean Consumption of Whole Grains (Panel A), Nuts/Seeds (Panel B), Fruits (Panel C), and Seafoods (Panel D) by Participation of Women, Infants, and Children (WIC), Supplemental Nutrition Assistance Program (SNAP), and National School Lunch/Breakfast Program Among US Children Based on NHANES Data From 1999-2016
eReferences