Key Points
Carbohydrates coat the surfaces of all cells and most proteins. They contain molecular information used in recognition events with carbohydrate-binding proteins (such as the lectin families) that decode this information. These bioactive carbohydrates open up a new source of novel targets for drug development.
Although carbohydrates have prominent roles in a wide range of biological processes, the currently approved drugs are mainly glycosidase inhibitors and sulphated glycosaminoglycans (that is, heparin).
Current preclinical research on lectins that are found in humans and pathogens indicates that glycomimetics could provide an alternative strategy for the treatment of inflammatory diseases (by targeting selectins) and infectious diseases (by targeting dendritic cell-specific ICAM3-grabbing non-integrin 1 (DC-SIGN), FimH, PA-I galactophilic lectin (PA-IL) and fructose-binding PA-IIL lectins).
In general, carbohydrates lack drug-like properties such as high affinity or adequate bioavailability and therapeutically relevant plasma half-lives. In addition, their large-scale production is cumbersome and expensive. When developing this class of drugs, the goal is to mimic the biological information of a functional carbohydrate with a glycomimetic that overcomes these challenges and has appropriate pharmacodynamic and pharmacokinetic properties.
Cell surface carbohydrates and carbohydrate-binding proteins mediate many key recognition events. This article reviews current progress in the development of glycomimetics and the opportunities and challenges presented by this relatively untapped source of therapeutics.
Abstract
Carbohydrates are the most abundant natural products. Besides their role in metabolism and as structural building blocks, they are fundamental constituents of every cell surface, where they are involved in vital cellular recognition processes. Carbohydrates are a relatively untapped source of new drugs and therefore offer exciting new therapeutic opportunities. Advances in the functional understanding of carbohydrate–protein interactions have enabled the development of a new class of small-molecule drugs, known as glycomimetics. These compounds mimic the bioactive function of carbohydrates and address the drawbacks of carbohydrate leads, namely their low activity and insufficient drug-like properties. Here, we examine examples of approved carbohydrate-derived drugs, discuss the potential of carbohydrate-binding proteins as new drug targets (focusing on the lectin families) and consider ways to overcome the challenges of developing this unique class of novel therapeutics.
Main
All cells are coated with complex carbohydrates called glycans, which form a layer known as the glycocalyx, ranging from 10 to 100 nm in thickness1,2. Glycans are present in many different molecular forms, including glycoproteins, proteoglycans, glycolipids and glycophosphatidylinositol-linked proteins. Their broad diversity originates from their assembly from monosaccharide building blocks, which can be linked to each other at various positions on their pyranose or furanose rings. Each ring can establish several linkages, giving rise to branched structures. Finally, the structural complexity of glycans is further increased by the possibility of α- and β-isomers at the anomeric centre.
This dense structural information is decoded by carbohydrate-binding proteins, which are involved in important physiological and pathophysiological events. The need for an integrated approach to decipher the structure–activity relationships (SARs) between glycans and their protein receptors has led to the establishment of interdisciplinary collaborative efforts in the United States (Consortium for Functional Glycomics; see Further information), Europe (EuroCarb; see Further information) and Japan (Human Disease Glycomics/Proteome Initiative; see Further information).
Currently, over 80 carbohydrate-binding proteins have been identified. The binding specificities for many of them have been elucidated, and others are being screened on large glycoarrays to determine their glycan-binding epitopes. These discoveries have led to a renaissance in glycobiology. They also provide a continuous supply of carbohydrate-related targets for the structure-based design of new chemical entities that mimic bioactive carbohydrates, and form a novel class of therapeutics.
Carbohydrate and carbohydrate-derived drugs
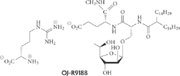
Although carbohydrates play an important part in a vast array of biological processes, carbohydrate and carbohydrate-derived drugs cover only a limited area of the world of therapeutics (Fig. 1). Many pathophysiologically important carbohydrate–protein interactions have yet to be exploited as a source of new drug targets. One reason might be the pharmacokinetic drawbacks that are inherently linked to carbohydrates. As a result of their high polarity, they are unable to cross passively through the enterocyte layer in the small intestine — a prerequisite for oral availability. In addition, once systemically available by parenteral administration, carbohydrates suffer from fast renal excretion.
Figure 1. Carbohydrate and carbohydrate-derived drugs.
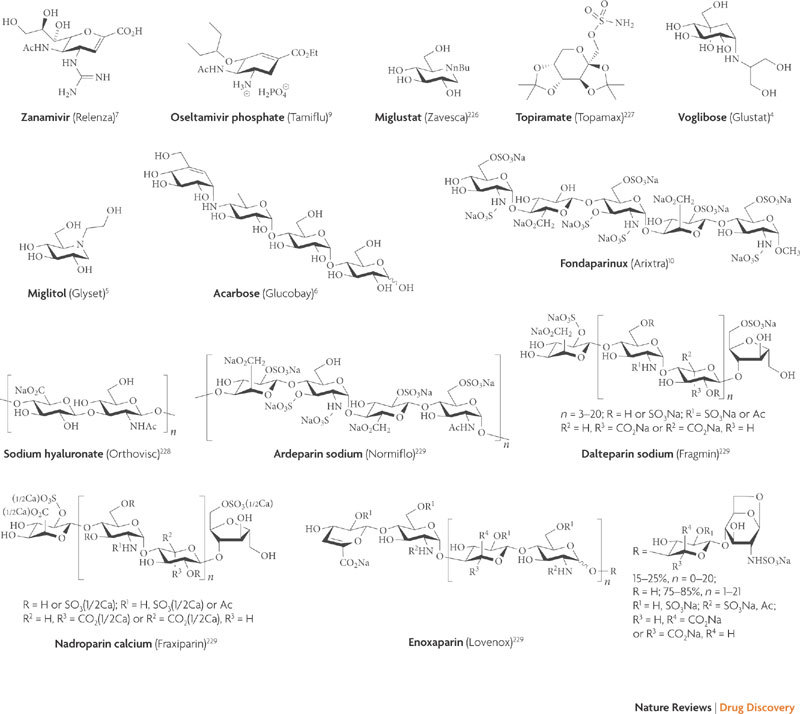
Structures of currently approved drugs (trade name in brackets). These include glycosidase inhibitors that prevent the digestion of carbohydrates for the treatment of diabetes (voglibose4, miglitol5 and acarbose6) and the prevention of influenza virus infections (zanamivir7 and oseltamivir9); and sulphated glycosaminoglycans, which function as anticoagulants by binding to antithrombin III for the treatment of thrombosis (fondaparinux3, dalteparin161, ardeparin161, nardoparin161 and enoxaparin161). In addition, carbohydrate-derived drugs are used to treat Gaucher's disease (miglustat162), epilepsy (topiramate163) and osteoarthritis (sodium hyaluronate164).
When interactions with blood plasma components are possible, the plasma half-life that is required for a successful therapeutic application can be achieved. Prominent examples are the low-molecular-weight heparins, derived from animal tissue, and fondaparinux3 (Arixtra; GlaxoSmithKline), which are used as anticoagulants. In other cases — such as the inhibition of α-glycosidases in the brush border of the small intestine for the treatment of diabetes (by voglibose4 (Basen/Glustat/Volix; Takeda), miglitol5 (Glyset; Pfizer) and acarbose6 (Glucobay/Prandase/Precose; Bayer)) or the inhibition of viral neuraminidases in the pharyngeal mucosa (by zanamivir7 (Relenza; GlaxoSmithKline)) — oral availability is not required.
The paradigm of a glycomimetic drug in the classical sense is oseltamivir (Tamiflu; Gilead/Roche). Starting from a carbohydrate lead, drug likeness was achieved by systematically eliminating polar groups and metabolic 'soft spots'8 that were not required for affinity. Finally, by designing a prodrug, oral availability became possible9.
Glycodrugs in preclinical and clinical evaluation
Carbohydrate-binding proteins are broadly classified into lectins10 and sulphated glycosaminoglycan (SGAG)-binding proteins11,12. There are two categories of lectins present in vertebrates: the families of intracellular lectins (for example, calnexin, L-type and P-type lectins), which bind core oligosaccharide structures and are involved in glycoprotein processing and quality control, and the families of extracellular lectins (for example, galectins, C-type, I-type and R-type lectins), which recognize terminal carbohydrate epitopes of other cells and pathogens. Extracellular lectins account for most of the molecular targets that are being investigated in current drug discovery programmes.
By contrast, SGAG-binding proteins are heterogeneous and difficult to classify11,12. Their ability to recognize SGAGs arises from clusters of cationic amino acids on unrelated proteins that confer the ability to recognize anionic structural motifs in extended SGAG chains. Typically, various SGAG-binding proteins interact with each SGAG with different affinities, and only a few SGAG sequences are exclusively recognized by a single SGAG-binding protein.
Here, we present the most promising drug candidates from the lectin families: selectins and dendritic cell-specific ICAM3-grabbing non-integrin 1 (DC-SIGN; also known as CD209) from the C-type lectin family, myelin-associated glycoprotein (MAG; also known as sialic acid-binding immunoglobulin-like lectin 4A (Siglec 4A)) as an example of an I-type lectin, and PA-I galactophilic lectin (PA-IL), fucose-binding lectin PA-IIL and minor component of type 1 fimbriae (FimH) as representatives of bacterial lectins.
C-type lectins
The hallmark of C-type lectins is the involvement of Ca2+ in the binding of glycans to their carbohydrate recognition domain (CRD). They have a wide range of biological functions, such as intercellular adhesion, serum glycoprotein removal and pathogen recognition.
Selectins. These are perhaps the most intensely studied mammalian carbohydrate-binding proteins. First discovered in 1989 (Refs 13–15), their functions as adhesion molecules are well understood16. The family consists of three members: E-selectin (also known as CD62E), P-selectin (also known as CD62P) and L-selectin (also known as CD62L). They are composed of a Ca2+-dependent CRD, an epidermal growth factor (EGF) domain, various short complement-like consensus repeats, a single transmembrane domain and an intracellular tail. Although carbohydrates bind to a receptor site within the CRD, the neighbouring EGF domain influences binding affinity and specificity17.
The three selectins have overlapping and distinct expression patterns, both temporally and spatially. E-selectin is expressed on endothelial cells by de novo protein synthesis 2–4 hours after stimulation by inflammatory mediators, such as interleukin 1β and tumour necrosis factor-α. P-selectin is expressed on activated platelets and is also stored in Weibel–Palade bodies in endothelial cells, which fuse to the cell surface on activation, leading to the expression of P-selectin within minutes. L-selectin is constitutively expressed by most leukocytes and plays a major part in homing and trafficking of lymphocytes through the blood and lymphatic systems.
All three selectins bind a common carbohydrate domain shared by sialyl Lea/x (sialyl Lewisa (sLea) and sialyl Lewisx (sLex))18 Interestingly, both of these carbohydrate sequences were originally discovered as cancer-associated antigens19,20,21 and are prognostic indicators of metastatic disease22. Tumour cells coated with these carbohydrate chains are recognized as migrating leukocytes, allowing them to escape the bloodstream and metastasize to other organs and tissues, such as the lymph nodes and bone marrow23,24.
To functionally bind sialyl Lea/x in vivo, both P- and L-selectins require additional interactions with negatively charged sulphate groups, either on the carbohydrate chain itself or on an adjacent peptide sequence. E-selectin has no such requirement and can functionally bind sialyl Lea/x in glycolipids25 and glycoproteins26.
The involvement of negatively charged groups, such as sulphates and carboxylates, in the binding of L- and P-selectin has led to one of the major pitfalls in designing small-molecule inhibitors for the selectins. A wide range of structurally diverse, negatively charged molecules has been reported to bind P- and L-selectins. These include sulphatides27, heparins28, fucoidan29, sulphated dextran30, chondroitin sulphate31, dermatan sulphate32, tyrosine sulphates33, sulphated hyaluronic acid34 and sulphogalabiose35. Such a range of molecules suggests that their inhibitory activity is due to nonspecific negative-charge interactions. In fact, a cautionary publication36 described potent P-selectin activity found in trace contaminants of polyanions from ion exchange media used in the preparation samples. Thus, the specificity of small-molecule, highly charged selectin antagonists that inhibit P- and L- but not E-selectin must be carefully evaluated.
In diseases in which cell adhesion, extravasation of cells from the bloodstream or the migration of specific lymphocytes has been implicated in the pathology, selectins present an attractive therapeutic target. For example, E- and P-selectins have been shown to mediate the acute adhesion and aggregation of leukocytes and erythrocytes during a vaso-occlusive crisis in a mouse model of sickle cell disease37,38. Furthermore, aberrant extravasation of cells from the bloodstream is the hallmark of many inflammatory diseases (such as asthma, colitis, arthritis and psoriasis) and cancer. Tumour cells that extravasate out of the bloodstream use the selectin pathway to metastasize. Many solid tumours and adenocarcinomas, such as gastrointestinal39, pancreatic40, breast41, lung42 and prostate43 cancers, express high levels of sLex and sLea. Expression of these selectin ligands on the tumour cells of patients with gastric and colon cancers44 is significantly correlated with poor survival22. Cimetidine (Tagamet; GlaxoSmithKline), a histamine receptor antagonist that also suppresses vascular expression of E-selectin, markedly and specifically improved survival of high-risk patients identified by tumour expression of sLea and sLex (Ref. 45), further supporting the usefulness of selectins as therapeutic targets for cancer.
Selectins and their ligands have also been reported to play key parts in the dissemination of haematological cancers46 and the homing of leukaemic stem cells to microdomains within the bone marrow47. E-selectin is constitutively expressed in the bone marrow48 and binds carbohydrate ligands that are found on leukaemic stem cells. Once adherent to these microdomains in the bone marrow, leukaemic cells become quiescent and less susceptible to killing by anti-proliferative chemotherapy drugs such as cytosine arabinoside49. Potent selectin antagonists present new therapeutic opportunities for treating these diseases. By preventing sequestration of leukaemic cells in the bone marrow and keeping them in circulation, combination therapy with selectin antagonists is likely to make the cells more susceptible to chemotherapy. Some examples of glycomimetic, small-molecule antagonists of the selectins are presented in Table 1.
Table 1.
Small-molecule selectin antagonists in preclinical and clinical trials
| Name and structure | Specificity | Disease | Institution | Status | Refs |
|---|---|---|---|---|---|
|
E-, P- and L-selectin | Cardio-vascular injury | Cytel | Stopped | 179 |
|
E-, P- and L-selectin | Asthma and psoriasis | Revotar | Phase IIa | 180 |
|
E-, P- and L-selectin | Allergic dermatitis | Nippon Organon | Preclinical | 181 |
|
E-, P- and L-selectin | Sickle cell crisis | Glyco-Mimetics | Phase I | 182 |
|
P-selectin | Athero-thrombotic and venous thrombotic diseases | Wyeth | Phase I | 183 |
|
E-, P- and L-selectin | Metastatic cancer | Kanebo | Unknown | 184 |
|
E- and P-selectin | Psoriasis | Bayer | Preclinical | 185 |
DC-SIGN. Mucosal surfaces present barriers to the environment that are potentially susceptible to infection. Migrating dendritic cells guard mucosal surfaces, capturing microorganisms and presenting processed antigens to activated T cells, thereby inducing an immune response against the invading pathogens. By screening a library of dendritic cell-specific monoclonal antibodies that inhibit binding to intercellular adhesion molecule 3 (ICAM3; an adhesion molecule that activates T cells), a single cell surface protein was discovered: DC-SIGN50.
The amino-acid sequence of DC-SIGN is identical to a previously described HIV glycoprotein 120 (gp120)-binding C-type lectin51,52. DC-SIGN that is expressed on patrolling dendritic cells in the mucosa binds to carbohydrate structures on the gp120 protein coat of HIV, which is the initial entry port of HIV to the host. HIV particles bound to DC-SIGN on the surface of dendritic cells are protected from destruction in the blood and migrate to the lymph nodes where they trans-infect T cells through the CD4–CCR5 (CC-chemokine receptor 5) complex on the T cell surface51. The binding specificity of DC-SIGN is for fucose and mannose residues, with higher affinity and specificity for the fucose linkage in Lea/x-type oligosaccharide structures. Formation of the active structure and binding of DC-SIGN occurs in a Ca2+-dependent manner52,53.
In addition to HIV, various other pathogens — such as the hepatitis C virus54, Dengue virus55, Ebola virus56, Marburg virus57, coronavirus (which causes severe acute respiratory syndrome)58 and cytomegalovirus59, as well as bacteria such as Mycobacterium tuberculosi s60 and Helicobacter pylor i52 and yeast (Candida albicans) — exploit DC-SIGN to infect their host. More recently, even parasites such as Leishmani a spp.61 and Schistosoma manson i62 have also been shown to bind DC-SIGN.
The fact that different pathogens have capitalized on this infection strategy makes DC-SIGN an interesting target for therapeutic intervention. In a study on the binding and transfer of HIV in human rectal mucosa cells, more than 90% of bound virus was bound to cells expressing DC-SIGN, although these cells represented only 1–5% of the total mucosal mononuclear cells. Furthermore, DC-SIGN-specific antibodies blocked more than 90% of HIV binding63. Other studies have shown that multivalent glycoconjugates of Lewisx or D-mannose prevented the attachment of Ebola or herpes virus to dendritic cells through DC-SIGN and thus prevented the subsequent infection of immune cells64,65,66.
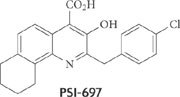
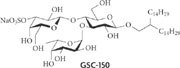
Glycomimetic compounds that inhibit DC-SIGN are based on two lead structures. The first are high-mannose oligosaccharides and the second is L-fucose as part of a Lewis epitope67. These determinants are synthesized by pathogens to camouflage their appearance as host tissue. To improve the affinity and pharmacokinetic properties of these naturally occuring antagonists, glycomimetics of both types of ligands have been synthesized.
High-density arrays of unbranched Manα(1-2)Man-terminated oligosaccharides bind to DC-SIGN almost as effectively as the entire Man9 oligosaccharide (Ref. 68). Therefore, the non-reducing end Manα(1-2)Man fragment of Man9 was suggested to play a crucial part in DC-SIGN recognition. To mimic 1,2-mannobiose, one hexose moiety was replaced by a cyclohexanediol derivative, leading to the pseudo-1,2-mannobioside compound 1 (Fig. 2), which had a threefold greater affinity for DC-SIGN than did 1,2-mannobiose (half-maximal inhibitory concentration (IC50) = 0.62 mM and 1.91 mM, respectively)69. Furthermore, in infection studies using an in vivo model of Ebola infection, the glycomimetic compound 1 inhibited infection of DC-SIGN-expressing Jurkat cells more efficiently than the corresponding natural disaccharide. Although the inhibitory concentration in these experiments was in the millimolar range, compound 1 might be useful in the preparation of high-affinity multivalent antagonists. Such an approach is encouraged by the strong inhibitory effects of multivalent antagonists on DC-SIGN binding, as observed for dendritic mannose conjugates70 or oligolysine-based oligosaccharide clusters71.
Figure 2. Ligands of dendritic cell-specific ICAM3-grabbing non-integrin 1 (DC-SIGN).
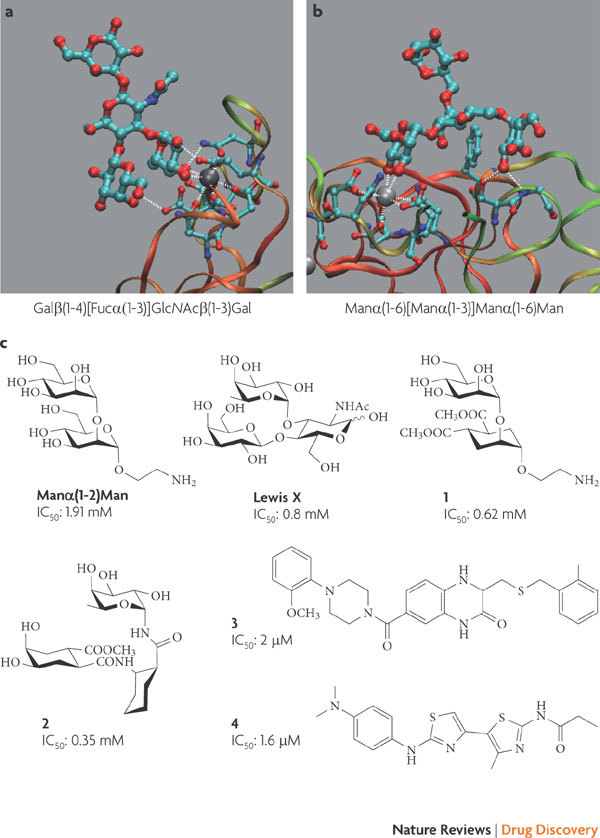
DC-SIGN co-crystallized with the natural epitopes Galβ(1-4)[Fucα(1-3)]GlcNAcβ(1-3)Gal (Protein Data Bank code 1SL5) (a) and Manα(1-6)[Manα(1-3)]Manα(1-6)Man (PDB code 1SL4) (b). The protein backbone is depicted in ribbon style, carbohydrates are shown in ball and stick style and the grey sphere is Ca2+. Part c shows the structures of DC-SIGN antagonists. The glycomimetics compound 1 (Ref. 69) and compound 2 (Ref. 72) have only a slightly improved affinity compared with the natural ligands Manα(1-2)Man68 and Lewisx (Ref. 72), whereas the non-carbohydrate antagonists compound 3 and compound 4 have half-maximal inhibitory concentration (IC50) values in the low micromolar range73.
Similarly, α-fucosylamine linked to 2-aminocyclohexanecarboxylic acid (compound 2) mimics Lewisx trisaccharide and inhibits DC-SIGN with a twofold greater potency (IC50 = 0.35 mM and 0.8 mM, respectively)72. These binding affinities are too weak for these compounds to have any therapeutic promise; however, when the oligosaccharides are displayed on large multivalent dendrimers, activity is greatly improved and biological activity can be shown in vitro71. Although such large multivalent presentations of carbohydrates or mimics thereof are a relatively simple means to increase activity, they pose a pharmaceutical challenge in terms of routes of administration and possible side effects, such as unwanted immune responses.
A classical approach to discovering DC-SIGN antagonists was successfully demonstrated by screening large libraries of small molecules in an automated assay format. By screening over 35,000 compounds, 7 hits with IC50 values in the low micromolar range were identified, such as compound 3 and compound 4 (Ref. 73). Interestingly, the structures of these hits bear no resemblance to the native carbohydrate ligands of oligomannose or the Lewis epitopes and do not contain functional groups to interact with Ca2+ in the CRD. Their inhibitory activity could be caused by binding to other domains on DC-SIGN, leading to an allosteric effect.
I-type lectins
I-type lectins are a family of carbohydrate-binding proteins in the immunoglobulin superfamily, and include Siglecs74. The Siglecs function as cell signalling co-receptors and are primarily expressed on leukocytes that mediate acquired and innate immune functions. The cytoplasmic domains of most Siglecs contain immunoreceptor tyrosine-based inhibitory motifs, which are characteristic of accessory proteins that regulate transmembrane signalling and endocytosis of cell surface receptor proteins. The diverse specificity for their sialoside ligands and variable cytoplasmic regulatory elements enable Siglecs to carry out unique roles at the cell surface. Siglecs can be broadly divided into an evolutionarily conserved group (Siglec 1 (also known as sialoadhesin), Siglec 2 (also known as CD22) and Siglec 4 (also known as MAG)) and a Siglec 3-related group (Siglec 3 and Siglecs 5–13). The evolutionarily conserved group shows selective binding properties: Siglec 1 and MAG preferentially bind α(2-3)-linked N-acetylneuraminic acid (Neu5Ac) and Siglec 2 is highly specific for α(2-6)-linked Neu5Ac. By contrast, members of the Siglec 3-related group are more promiscuous in their binding, often recognizing more than one presentation of Neu5Ac.
The most comprehensively characterized Siglecs are Siglec 2, a regulatory protein that prevents the overactivation of the immune system and the development of autoimmune diseases, and MAG, a protein that blocks regeneration of the central nervous system (CNS) after injury75.
MAG. Unlike the peripheral nervous system (PNS), the injured adult CNS inherently lacks the capacity for axon regeneration. Although neurite outgrowth is possible in principal, it is blocked by inhibitor proteins expressed on residual myelin and on astrocytes that are recruited to the site of injury. To date, three major inhibitor proteins have been identified: reticulon 4 (RTN4; also known as nogo A)76, myelin oligodendrocyte glycoprotein (MOG)77 and MAG78. These three proteins bind to and activate the RTN4 receptor, which is located on the surface of the neuron. This leads to the formation of a complex with the nerve growth factor receptor (NGFR; also known as p75NTR) and the activation of the RhoA–ROCK (Rho-associated, coiled coil-containing protein kinase) cascade, which results in growth cone collapse79.
The RhoA–ROCK inhibitory cascade can also be triggered by a complex formed by MAG, brain gangliosides (especially GM1b, GD1a, GT1b, GT1β and GQ1bα)80 and NGFR81. Although the exact biological role of the MAG–ganglioside interaction has yet to be resolved, in some systems inhibition of axon regeneration by MAG could be completely reversed by sialidase treatment, suggesting that sialidated glycans are the main axonal ligands of MAG82. SAR studies83,84,85 have revealed that the terminal tetrasaccharide epitope Neu5Acα(2→3)-Galβ(1→3)-[Neu5Acα(2→6)]-GalNAc of GQ1bα shows superior binding to MAG compared with the terminal trisaccharide epitope, which is present in GD1a and GT1b, for example86. Further refinements of the SAR profile have led to the identification of MAG antagonists that have improved affinities and, at least in some cases, remarkably simple structures (Fig. 3). However, owing to the use of different assay formats, it has been difficult to compare the reported affinities of these compounds for various ligands.
Figure 3. Myelin-associated glycoprotein (MAG) antagonists.
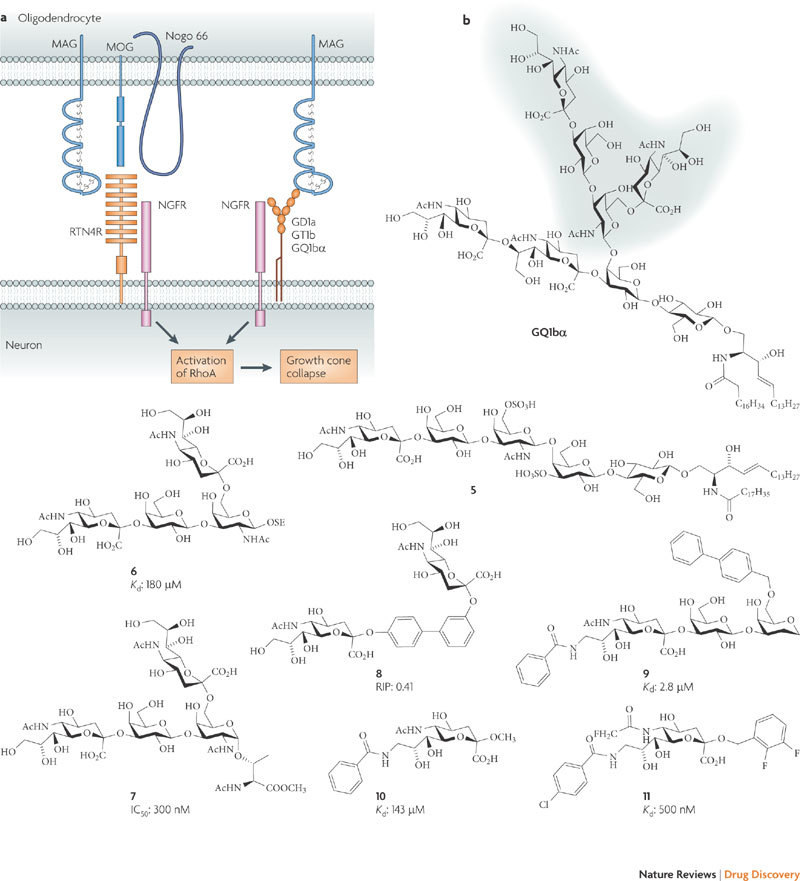
a | MAG, nogo 66 and myelin oligodendrocyte glycoprotein (MOG) bind to the reticulon 4 receptor (RTN4R; also known as the nogo receptor). The inhibitory signal is transduced into the cytosol of the neuron through the co-receptor NGFR (nerve growth factor receptor; also known as p75NTR). MAG bound to the brain gangliosides GD1a, GT1b and GQ1bα also transduces the inhibitory signal, with the help of NGFR as a co-receptor, into the cytosol79. b | GQ1bα is the brain ganglioside with the highest affinity for MAG80; replacement of its inner sialic acids by sulphates (to produce compound 5) led to a fourfold increase in affinity165. The tetrasaccharide compound 6 (Ref. 87) is the minimal carbohydrate epitope of GQ1bα for MAG binding and has served as a lead structure for the development of antagonists; with compound 7, an excellent correlation between the degree of neurite outgrowth and the binding affinities was established88. Further modifications involved the replacement of the Galβ(1-3)GalNAc core (to produce compound 8 (Ref. 166)) or the α(2-6)-linked Neu5Ac (to produce compound 9 (Ref. 135)). Following studies on compound 10 (Ref. 167), numerous Neu5Ac derivatives168,169, for example, compound 11, with up to nanomolar affinities have been synthesized. Affinity data of the different compounds should be compared with caution as they were obtained from different assays. IC50, half-maximal inhibitory concentration; Kd, dissociation constant; RIP, relative inhibitory potency.
Overall, starting from the low-affinity tetrasaccharide lead structure compound 6 (Ref. 87), low-molecular-mass MAG antagonists with nanomolar affinity and excellent stability in the spinal cord fluid have been identified (S. Mesch, D. Moser, A. Vedani, B. Cutting, M. Wittwer, H. Gäthje, S. Shelke, D. Strasser, O. Schwardt, S. Kelm and B. Ernst, unpublished observations). The high correlation between the degree of neurite outgrowth and the binding affinities of these antagonists further validates MAG as a therapeutic target and suggests that potent glycan inhibitors of MAG have the potential to enhance axon regeneration88.
Bacterial and viral lectins
For colonization and subsequent development of an infectious disease, enteric, oral and respiratory bacteria require adhesion to the host's tissue. This grants them a substantially greater resistance to clearance and killing by immune factors, bacteriolytic enzymes and antibiotics. In addition, such bacteria are better able to acquire nutrients, further enhancing their ability to survive and infect the host. Therefore, anti-adhesive drugs that prevent the adhesion of pathogens to host tissues may offer a novel strategy to fight infectious diseases89. The alarming increase in drug-resistant bacterial pathogens makes a search for new approaches to fight bacterial infections essential90. Because anti-adhesive agents are not bactericidal, they are less likely to promote the propagation of resistant strains than bactericidal agents, such as antibiotics.
The carbohydrate epitopes on the surface of host cells that are used by bacteria and viruses for colonization and infection (Table 2) are the starting point of the search for glycomimetic entry inhibitors.
Table 2.
Carbohydrate epitopes used by bacteria and viruses for recognition and entry
| Pathogen | Binding epitope | Refs |
|---|---|---|
| Bacteria | ||
| Escherichia coli type 1 pili | Manα(1-3)Manα(1-6)Man | 109 |
| Helicobacter pylori | Neu5Acα(2-3)Galβ(1-4)Glc | 109 |
| Pseudomonas aeruginosa (PA-IL and PA-IIL) | α-Galactoside and Lewisx | 109 |
| Neisseria gonorrhoea | Galβ(1-4)GlcNAc | 109 |
| E. coli K99 | Neu5Gcα(2-3)Galβ(1-4)Glc | 109 |
| E. coli CFA1 | Neu5Acα(2-8)Neu5Ac | 109 |
| Klebsiella pneumonite | Man | 109 |
| Campylobacter jejuni | Fucα(1-2)Galβ(1-4)GlcNAc | 109 |
| E. coli K1 | GlcNAcβ(1-4)GlcNAc | 109 |
| E. coli P | Galα(1-4)Gal | 109 |
| E. coli S | Neu5Acα(2-3)Galβ(1-4)GalNAc | 109 |
| Haemophylus influenzae | Neu5Acα(2-3)Galβ(1-4)GlcNAc | 109 |
| Neisseria meningitidis | Neu5Acα(2-3)Galβ(1-4)GlcNAc | 109 |
| Salmonella typhimurium | Man | 109 |
| Streptococcus pneumoniae | Neu5Acα(2-3)Gal | 109 |
| Streptococcus suis | Galα(1-4)Galα(1-4)Glc | 109 |
| Viruses | ||
| Influenza A | α(2-3)- or α(2-6)-linked sialic acid | 186 |
| Human parainfluenza virus type 1 | α(2-3)SLN and sialyl Lewisx | 187 |
| Norwalk virus | H and Leb blood types | 188 |
| Rotavirus | Sialylated glycans | 189 |
| Herpes simplex virus type 1 | 3-O-sulphated heparin sulphate | 190 |
| Calcivirus | Blood group antigens | 191 |
| Corona virus | Sialylated glycans | 192 |
| Murid herpes virus | Glycosaminoglycans | 193 |
| Coxsackivirus A24 | Sialylated glycans | 194 |
| Papilloma virus L1 | Heparan sulphate | 195 |
| Polyomaviruses (JCV and BKV) | α(2-3)- or α(2-6)-linked sialic acid | 196 |
| Simian virus SV40 | GM1 ganglioside | 197 |
| Newcastle disease virus | Sialylated glycans | 198 |
| BKV, B. K. virus; JCV, John Cunningham virus; Leb, Lewisb antigen; PA-IIL, fucose-binding lectin PA-IIL; PA-IL, PA-I galactophilic lectin; SLN, sialyl lactoseamine. | ||
A challenge of anti-adhesion therapy is that most pathogens possess genes encoding several types of adhesins, so that, during the infection process, they may express more than one of these adhesins. Glycomimetic antagonists that are designed to inhibit multiple adhesins are feasible to develop, and examples are described below for Pseudomonas aeruginosa.
P. aeruginosa virulence factors (PA-IL and PA-IIL). P. aeruginosa can be part of the normal flora in healthy adults but becomes a deadly pathogen in individuals who are immunocompromised, patients with cystic fibrosis and hospitalized, critically ill patients. An increasing percentage of P. aeruginosa infections are antibiotic resistant.
For its adhesion to host cells, the pathogen expresses lectins such as PA-IL and PA-IIL91. These lectins are virulence factors under quorum sensing control and are, by themselves, cytotoxic to primary epithelial cells in culture92. At low concentrations, they inhibit ciliary beating of epithelial cells in explants of nasal polyps93. Inhibition can be completely reversed by treatment with the carbohydrate ligand of the lectin. Thus, 24 hours after addition of fucose, ciliary beating returns to normal frequency94.
PA-IL and PA-IIL are tetrameric lectins that require Ca2+ for carbohydrate binding. The crystal structures of both lectins complexed with their carbohydrate ligands have been resolved (Fig. 4). PA-IL preferentially binds to terminal α-linked D-galactose in the presence of one Ca2+ ion, whereas PA-IIL binds with an unusually strong micromolar affinity to L-fucose and requires two Ca2+ ions95,96. PA-IL and PA-IIL are soluble intracellular lectins. However, once released from the cells, these lectins cause bacteria to adhere to host tissue — a process that can be reversed by incubation with D-galactose and D-mannose, respectively97.
Figure 4. PA-IL and PA-IIL inhibitors.
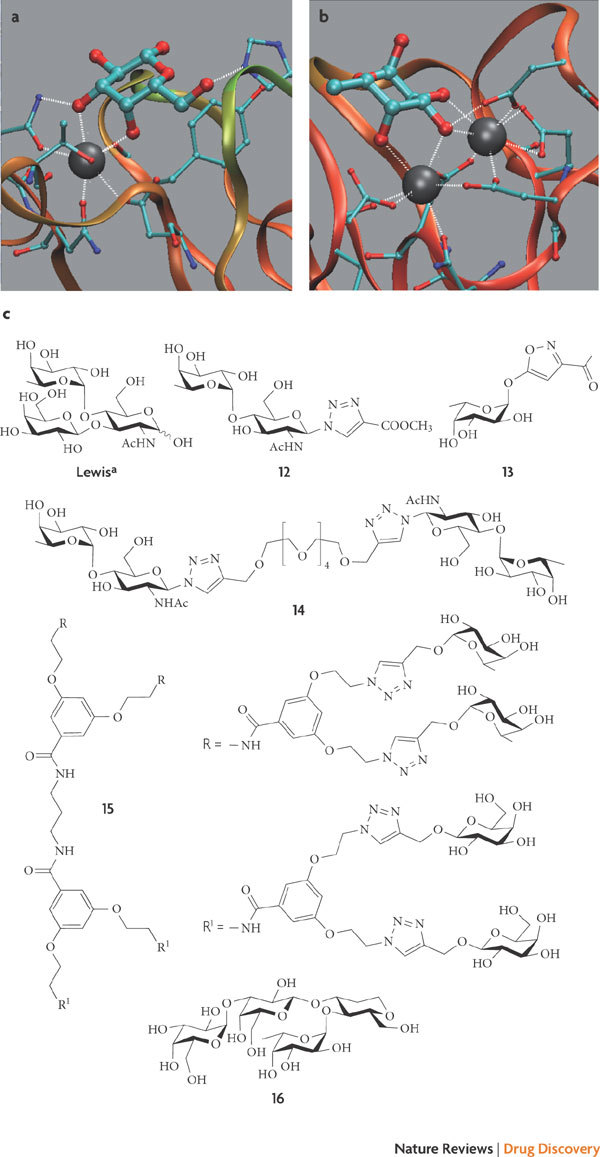
a | Binding sites of PA-I galactophilic lectin (PA-IL) complexed with D-galactose (Protein Data Bank code: 1OKO (Ref. 170)). b | Binding sites of fucose-binding lectin PA-IIL complexed with L-fucose (PDB code: 1GZT143). In parts a and b, the protein backbones are depicted in ribbon style, carbohydrates are shown in ball and stick style and the grey spheres are Ca2+. c | The monovalent ligands compound 12 (Ref. 101) and compound 13 (Ref. 99) exhibit affinity for PA-IL and PA-IIL that is similar to that of Lewisa (Ref. 100); the most potent oligovalent ligand is compound 14 (Ref. 102), but it has only a modest effect on a per saccharide basis; the heterobifunctional glycodendrimer compound 15 (Ref. 104) and the low-molecular-mass glycomimetic compound 16 (Ref. 105) bind to both PA-IL and PA-IIL from Pseudomonas aeruginosa.
The native carbohydrate inhibitors of PA-IL and PA-IIL, D-galactose and L-fucose, were successfully used to treat a tobramycin-resistant P. aeruginosa infection in a case report98. Combination therapy of tobramycin with D-galactose and L-fucose to inhibit the virulence factors PA-IL and PA-IIL cured an 18-month-old infant with systemic and pulmonary infections, as determined by microbiological testing.
Screening with the glycan arrays of the Consortium for Functional Glycomics revealed that the Lewisa trisaccharide, Galβ(1-3)[Fucα(1-4)]GlcNAc, is a high-affinity ligand for PA-IIL99, with a dissocation constant of 210 nM100. To reduce the complexity of the trisaccharide antagonists, glycomimetics based on the Fucα(1-4)GlcNAc disaccharide — for example, the antagonist compound 12 — were synthesized. By titration calorimetry experiments, increased entropy costs upon binding were detected as a result of the higher flexibility of Fucα(1-4)GlcNAc compared with Lewisa. However, additional enthalpic interactions that originate from a network of hydrogen bonds compensate for this entropic penalty101. A further simplification of the PA-IIL antagonists was achieved when α-L-fucosides bearing heterocyclic substituents as aglycons were synthesized. Surprisingly, some candidates — for example, compound 13 —have a similar potency to Lewisa (Ref. 99).
Oligovalent forms of the Fucα(1-4)GlcNAc epitope, such as compound 14 (Ref. 102), exhibit increased activity compared with monovalent forms; however, in most cases, this effect was only modest on a per saccharide basis. To date, multivalency has only been explored with dendrimers that present L-fucose, which show an increase in affinity of up to a factor of 20 on a per saccharide basis103. Finally, to prevent adhesion of P. aeruginosa mediated simultaneously by the PA-IL and PA-IIL lectins, heterobifunctional ligands that present both D-galactose and L-fucose in an oligovalent array (as in compound 15 (Ref. 104)) or as a small-molecule glycomimetic (as in compound 16 (Ref. 105)) have been constructed. In a study to determine the efficacy of compound 16 in mice surgically stressed by 30% hepatectomy, 60% of the control group died 48 hours after acute infection with P. aeruginosa, whereas 100% of mice treated with compound 16 survived105.
FimH. Urinary tract infections (UTIs) are among the most prevalent inflammatory diseases that are caused by pathogens106,107. The predominant pathogen in UTIs is uropathogenic Escherichia coli (UPEC), which causes more than 80% of all infections in otherwise healthy people (uncomplicated UTI). In healthy individuals, most uropathogens originate from the rectal microbiota and enter the normally sterile urinary bladder through the urethra, where they trigger the infection (cystitis). Once in the urinary tract, bacteria attach to the urinary tract epithelium through fimbrial adhesion molecules to avoid the host's defence mechanisms. Once bound, the bacteria are presumably internalized in an active process that is similar to phagocytosis108.
Uncomplicated UTI can be effectively treated with oral antibiotics such as fluoroquinolones, cotrimoxazol or amoxicillin and clavanulate, depending on the susceptibility of the pathogen involved. However, recurrent infections and subsequent antibiotic exposure can result in the emergence of antimicrobial resistance, which often leads to treatment failure and reduces the range of therapeutic options. So, there is an urgent need for efficient, cost-effective and safe non-antibiotic therapy to prevent and treat UTIs without facilitating antimicrobial resistance. Inhibition of type 1 fimbriae-mediated bacterial attachment to the bladder epithelium is a promising approach to achieve this goal109. Studies showed that α-mannosides are the primary bladder cell ligands for UPEC and that the attachment event requires the highly conserved FimH lectins, which are located at the tip of the bacterial fimbriae. A structure–function analysis showed that the residues of the FimH mannose binding pocket are invariant across 200 UPEC strains110.
More than two decades ago, various oligomannosides111 and aromatic α-mannosides112 that antagonize type 1 fimbriae-mediated bacterial adhesion were identified. Two approaches have been taken to improve their affinity: the rational design of ligands guided by information obtained from the crystal structure of FimH, and the multivalent presentation of the α-mannoside epitope.
The crystal structure of the FimH receptor-binding domain was solved in 1999 (Ref. 113) and the corresponding complex with oligomannoside-3 (Ref. 114) has recently become available. Despite this detailed knowledge of the binding event, few attempts to translate this information into low-molecular-mass antagonists have been reported112,115,116,117. A selection of monovalent FimH antagonists is depicted in Fig. 5. The reference compound, methyl α-D-mannoside (compound 17) binds in the millimolar range118, but the most potent monovalent antagonist reported so far, compound 22, binds with nanomolar affinity117.
Figure 5. FimH antagonists.
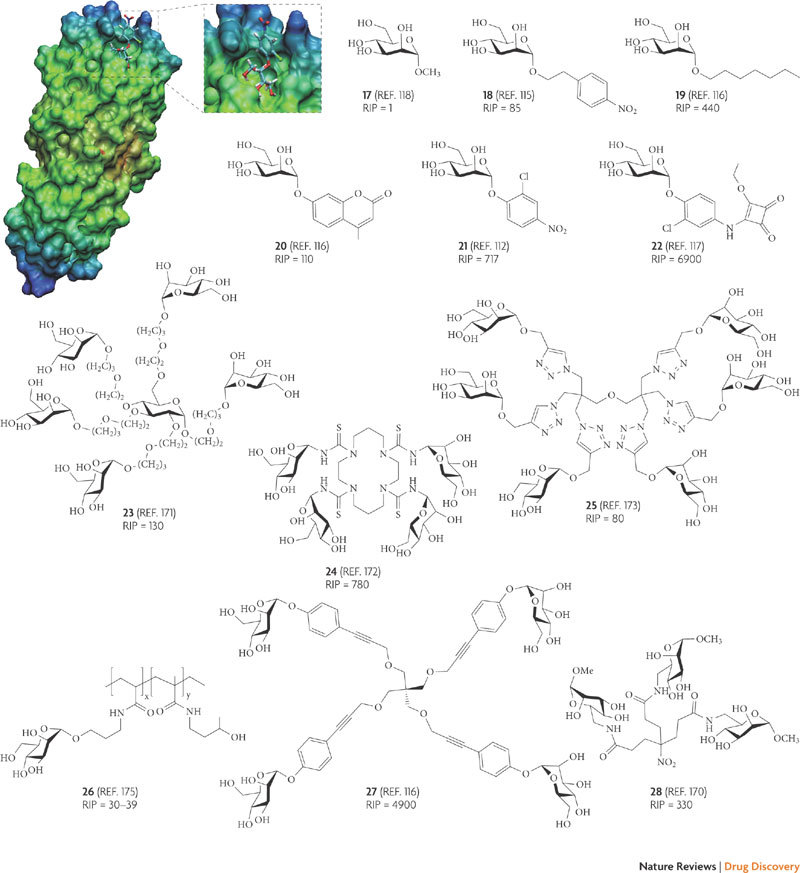
The crystal structure representation shows the mannose derivative compound 21 docked to the mannose-binding pocket of FimH (Protein Data Bank code: 1KFL). The relative inhibitory potencies (RIPs) of the FimH antagonists compounds 18 to 28are based on methyl α-D-mannoside (compound 17; RIP = 1). As the RIPs were obtained from different assays (yeast agglutination, adherence to cell lines derived from human urinary bladder epithelium or guinea pig epithelial cells as well as surface plasmon resonance experiments with immobilized FimH), they should be compared with caution.
The reported affinities can be explained on the basis of the structure of the CRD that is located on the tip of the FimH protein (Fig. 5). First, the hydroxyl groups at the 2, 3, 4 and 6 positions of mannose form an extended hydrogen bond network114,118. Second, the entrance to the binding site formed by two tyrosines and one isoleucine — the so-called 'tyrosine gate' — supports hydrophobic contacts118. The aromatic aglycons of antagonists — as occur in compounds 20 and 21, for example — can establish energetically favourable π–π interactions with this tyrosine gate, leading to substantially improved affinities. A further enhancement of affinity was achieved using oligovalent and multivalent FimH antagonists (for example, compounds 23 to 28).
Soluble FimH antagonists that are applied to prevent bacterial adhesion to the host tissue are faced with the challenge of mechanical forces resulting from fluid flow. It is commonly presumed that the duration of receptor–ligand interactions is shortened by shear stress. However, it was recently discovered that the ability of E. coli to avoid detachment is dramatically increased by shear stress119. As a consequence of shear stress-enhanced adhesion, E. coli evades detachment from body surfaces by soluble glycoproteins or peptides that are ubiquitous in body fluids. An example is the glycoprotein uromodulin (also known as the Tamm–Horsfall urinary glycoprotein), which binds to FimH and is thought to function as a body defence against E. coli infections120. On the basis of simulations121, it is thought that force-induced separation of FimH from its mannose ligand causes a conformational change of the binding pocket from a low-affinity to a high-affinity conformation. Instead of the application of competitive antagonists, allosteric antagonists that are capable of stabilizing the low-affinity conformation might lead to a successful therapy.
Although monovalent and oligovalent antagonists with nanomolar affinity have been reported, there are no data available regarding their pharmacokinetic properties. However, for the treatment of UTI, oral bioavailability and fast renal excretion to reach the targets in the urinary tract are prerequisites for therapeutic success.
Rational design: challenges and lessons learned
As in other fields that have spawned successful new therapeutics (for example, monoclonal antibodies), years of effort have been required to understand the unique challenges that are inherently linked to carbohydrate-derived drugs and to develop the basic skills and the specific knowledge to move from the excitement of scientific discovery to the development of a new class of therapeutics.
Although animal lectins usually show a high degree of specificity for glycan structures, their single-site binding affinities are typically low. In biological systems, functional affinity is often attained by the oligovalent presentation of CRDs, either in an oligomeric protein (for example, cholera toxin122) or through clustering at cell surfaces (for example, asialoglycoprotein receptor123). Additionally, the pharmacokinetic properties of carbohydrate hits, such as bioavailability or plasma half-life, are typically unsatisfactory for therapeutic applications. Finally, although tremendously improved novel glycosylation protocols124 and solid-phase approaches125 have become available, oligosaccharides are still only manufactured by cumbersome multi-step syntheses.
Therefore, the challenge is to mimic the structural information of a functional carbohydrate with a compound that has drug-like characteristics. The first step in this process is to understand the SAR of a carbohydrate lead, specifically the contribution made by each functional group to binding as well as the three-dimensional presentation of the pharmacophores. Based on this information, it is possible to identify glycomimetics that are pre-organized in their bioactive conformation — that is, which will adopt their bound conformation in solution. In addition, the mimics should show improved pharmacokinetic properties — in particular, improved bioavailability and serum half-life — while minimizing toxicity and cost of synthesis. In the past, the development of carbohydrate-derived drugs was often not entirely focused on simultaneously solving all of the above requirements and some high-profile failures resulted, notably in the field of selectin antagonists. Nevertheless, rationally designed glycomimetics have the potential to reap the rewards of a relatively untapped source of novel therapeutics for wide-ranging and important biological and medical applications.
Understanding native interactions. The starting point for the rational design of glycomimetics is the analysis of the binding characteristics of the carbohydrate–CRD binary complex. The three-dimensional structure of the lectin or the carbohydrate–lectin complex has been solved for a number of therapeutically interesting targets. Thus, E-, P- and L-selectin co-crystallized with sLex or PSGL1 (P-selectin glycoprotein ligand 1)126, sialoadhesin co-crystallized with 3′-sialyl lactose127, or DC-SIGN co-crystallized with the pentasaccharide GlcNAc2Man3 (Ref. 128) hold valuable information for the rational design of glycomimetics. In cases in which the structure has not yet been solved, homology models can be generated — as is the case for MAG, for example129.
Detailed insight into the binding event can be gained by nuclear magnetic resonance (NMR) experiments. For example, the bound conformation of a functional carbohydrate ligand in the CRD of the target lectin can be determined using transferred nuclear Overhauser effect (NOE)130. In addition, the binding epitope can be identified by saturation transfer difference NMR spectroscopy (STD NMR spectroscopy)131. This technique has been used to study interactions of carbohydrate ligands with the rotavirus receptor, VP8 (Ref. 132), the anti-carbohydrate tumour-associated antibody GSLA1 (Ref. 133), E-selectin134 and MAG87,135. Overall, transfer NOE NMR and STD NMR experiments allow a rapid insight into the binding characteristics of carbohydrate–lectin interactions and can replace, at least partially, X-ray investigations and the time-consuming mapping of binding epitopes by chemical means136.
Enhancing binding affinity. The generally low affinity of carbohydrate–lectin interactions is a consequence of shallow binding sites of lectins, leading to a high solvent accessibility of the complex forming hydrogen bonds and salt bridges. Owing to large off-rates (koff), the binary complexes are characterized by short dissociative half-lives (t1/2), typically in the range of seconds — as shown for selectins and their physiological ligands137,138,139, the carbohydrate-recognizing antibody GSLA1, sLea (Ref. 133) and MAG antagonists135. Given that, for a therapeutic application, the t1/2 of a drug–target binary complex is expected to be in the range of minutes to a few hours, improving the koff of glycomimetic compounds is mandatory for therapeutic applications140.
Often, mammalian lectins undergo numerous directed, but weak, interactions with their ligands. A specific example, the interaction of sLex with E-selectin, is outlined in Fig. 6a. It consists of six solvent-exposed hydrogen bridges and a salt bridge (to produce complex 29). One possible approach to improve affinity is to pre-organize the antagonist in its bioactive conformation to compensate for the low enthalpic contributions by reducing the entropy costs on binding. For E-selectin, this strategy was successful (see complex 30 in Fig. 6a). As elucidated by X-ray126 or STD NMR134 studies, the GlcNAc moiety does not interact with the binding site and serves solely as a linker that positions the galactose and the fucose moiety in the correct spatial orientation. It was successfully replaced by non-carbohydrate linkers141,142. In addition, steric repulsion deriving from properly placed substituents on the linker moiety can further improve the pre-organization of the core and, as a result, the affinity of the corresponding antagonist130. Furthermore, the pre-organization of the carboxylate was optimized as well, revealing (S)-cyclohexyl lactic acid as the best mimic of Neu5Ac141.
Figure 6. Enhancing the affinity of carbohydrate-derived drugs.

a | The affinity of carbohydrate-derived drugs can be improved by pre-organization in the bioactive conformation. In solution, the core conformation (shown in red) of sialyl Lewisx is in the range of +10° to −60° and the acid orientation (shown in blue) is in the range of +80° to +150°. In the bioactive conformation (complex 29), the core conformation is approximately −40° and an acid orientation is approximately 110° (Refs 175–178). The degree of pre-organization of a mimetic in the bioactive conformation, as shown in complex 30, can be correlated with its affinity130,141. b | Affinity can be improved by establishing new enthalpic interactions; comparisons of the binding mode of Neu5Ac2en (compound 31), zanamivir (Relenza)7 and oseltamivir (Tamiflu)9 to neuraminidase are depicted. bb, backbone; sc, side chains.
If the target lectin offers a well-structured binding pocket, the free energy of binding can be improved by incorporating additional enthalpic contributions. Successful examples are the neuraminidase inhibitors zanamivir7 and oseltamivir9. For the influenza viral coat protein neuraminidase, the natural substrate Neu5Ac and the corresponding glycal Neu5Ac2en (compound 31), which mimics the transition state of the hydrolytic reaction, have only millimolar to micromolar affinities. The improved affinities of the transition state analogues zanamivir and oseltamivir result from a guanidinium substitution in the 4 position, enabling the formation of a new salt bridge7, or from the replacement of the glycerol side chain in the 6 position, leading to a new, favourable lipophilic interaction by induced fit9 (Fig. 6b).
Finally, multivalency frequently occurs in nature and leads to tight binding in situations in which univalent protein–ligand binding is weak143,144,145. Recognition of carbohydrate ligands by bacterial and mammalian lectins are examples of this phenomenon. For the specific inhibition of these recognition events, oligovalent ligands have been proposed (see, for example, Figs 4,5). However, the design of tight-binding oligovalent ligands is, for the most part, an empirical endeavour. Tailored oligovalency, whereby the spacing of a limited number of tethered branches is matched to that between adjacent sugar binding sites of a protein or a protein cluster, potentially offers substantial increases in avidity for the target143,146,147.
Pharmacokinetics. Unfortunately, only limited pharmacokinetic data are reported for any carbohydrate or glycomimetic. For oral absorption by passive permeation through the membrane barrier of the small intestine148, there are limitations regarding molecular mass, polarity and the number of hydrogen bridge donors and acceptors149. The hydrophilic nature of oligosaccharides caused by the large number of hydroxyl groups and charges (sulphates and carboxylates) makes their oral availability virtually impossible. Therefore, when glycomimetics are designed, the pharmacokinetic as well as the pharmacodynamic profile should be adjusted. Possible strategies to improve passive absorption are the bioisoteric replacement of crucial groups150 or a prodrug approach151. A successful example of the prodrug approach is oseltamivir, which is an ester prodrug. Once absorbed, the ester is metabolized to the corresponding carboxylate, the active metabolite RO64-0802 (Ref. 152). Its absolute bioavailablity from the orally administered prodrug is 80%. It is detectable in plasma within 30 minutes and reaches maximal concentrations after 3–4 hours153.
In addition, the feasibility of using an active-transport system that is abundant in the intestine, liver, kidney or brain should also be considered154. Many drugs that are rationally designed or derived from natural products that cannot be absorbed by passive transport (such as β-lactam antibiotics, heart glycosides or fungicides) take advantage of active transport. In addition, active transport can be enforced by rational design — for example, by incorporating an amino acid into the structure and thereby creating a substrate for active transport by peptide transporter 1 (PEPT1; also known as SLC15A1) and PEPT2 (also known as SLC15A2). A successful example is valacyclovir (Valtrex/Zelitrex; GlaxoSmithKline), an antiviral drug used in the management of herpes simplex, in which valine was attached to the parent drug acyclovir (Zovirax; GlaxoSmithKline/Biovail), leading to a fivefold increase of the oral availability155. Extensive analysis of the structural requirements of the PEPT1 transporter identified numerous analogues with higher affinity than valine; this information will be valuable for improving the oral availability of glycomimetics156.
The usually short serum half-life and rapid excretion of carbohydrates presents an additional challenge for the design of glycomimetic drugs. Degradation in the presence of serum or liver microsomes are routine assays of metabolic stability that must be incorporated early in the design process of glycomimetics157.
Organic anion and cation transport systems located in the liver and kidney are responsible for active excretion from the circulation158. The organic anion transporter family (OAT1 to OAT5) recognizes anions (specifically, carboxyl groups) connected to hydrophobic ring structures. RO64-0802, the active metabolite that is formed from oseltamivir, is an example of a glycomimetic drug with a serum half-life that is diminished by recognition and removal by the OAT system159. When probenecid, a competitive inhibitor of OAT1, is administered in combination with oseltamivir, the serum half-life of the active metabolite is extended160. This strategy has been suggested to extend the supply of the US government's stockpile of oseltamivir in case of a national emergency in response to a pandemic outbreak of influenza. Both interactions with probenecid and specific transporter assays should be examined early in the development of a glycomimetic containing charged groups to identify structural elements that may adversely affect serum half-life.
Conclusions
Recent efforts to elucidate the complexity and functions of the human glycome by pooling resources and technologies among academic centres has led to a rapid influx of discoveries and the acknowledgement of a new source of structural information that is not apparent from the human genome. The efforts in drug discovery reviewed here show the challenges in medicinal chemistry that need to be met for the development of drug-like glycomimetics.
Past efforts in this field have highlighted the drawbacks of using native oligosaccharides as drugs. Typically, both their pharmacodynamic and pharmacokinetic properties are insufficient for a therapeutic application. In addition to the lack of affinity, they suffer from low tissue permeability, short serum half-life and poor stability. Glycomimetics are designed to correct these shortcomings. The detailed insight into carbohydrate–lectin interactions that is required is predominantly provided by recent progress in NMR spectroscopy and X-ray crystallography. Thus, the identification of the bound conformation of a functional carbohydrate by transferred NOE NMR allows the design of mimetics with pharmacophores that are pre-organized in their bioactive conformation, leading to reduced entropy costs upon binding. By incorporating additional binding sites, which frequently leads to hydrophobic contacts, a further enhancement of affinity can often be achieved. Finally, the knowledge of the binding epitope as obtained by STD NMR allows the identification of negligible and replaceable functional groups. As a consequence, the design of glycomimetics that have improved absorption, distribution, metabolism and excretion can be accomplished.
Currently, these principles for the rational design of glycomimetics are being implemented in both academic institutions and industrial laboratories. As successful examples of glycomimetic drugs emerge, the strategies developed for their design will pave the way to realize the potential of this relatively untapped source of therapeutics.
Glossary
- Glycocalyx
Literally meaning sugar coat, it is the outer component of a cell surface and contains a network of polysaccharides and complex carbohydrates.
- Anomeric centre
The centre of chirality of a glycan that is generated by hemiacetal ring closure.
- Lectin
A carbohydrate-binding protein which is highly specific for sugar moieties and typically plays a part in biological recognition phenomena.
- Sulphated glycosaminoglycan
A long polysaccharide chain consisting of repeating sulphated dissacharide units.
- Carbohydrate recognition domain
The three-dimensional domain in a lectin that binds carbohydrate.
- Lea/x
A common three-dimensional structural domain shared by the carbohydrate structures Lewisa (Galβ(1–3)[Fuc(α1–4)]GlcNAc) and Lewisx (Galβ(1–4)[Fuc(α1–3)]GlcNAc).
- Glycomimetic
A molecular mimic of a functional carbohydrate that has improved affinity for its target and drug-like pharmacokinetic properties.
- Dendrimer
A large, synthetically produced polymer in which the atoms are arranged in many branches and subbranches radiating out from a central core.
- Allosteric effect
An effect that is exerted on a protein by the binding of an effector molecule at a site other than the protein's active site or binding site.
- Growth cone
A dynamic extension at the tips of axons that is supported by actin and grows towards synaptic targets.
- Adhesin
A protein produced by many bacteria to effectively adhere to host surfaces.
- Quorum sensing
A type of decision-making process used by bacteria to coordinate gene expression and behaviour according to the local density of their population.
- Entropy
A quantitative measurement of the disorder in a system. The change in heat divided by the absolute temperature is the entropy change or cost of the thermodynamic process.
- Aglycon
The non-sugar component that remains after hydrolysis of a glycoside.
- π–π interaction
A non-covalent interaction between organic compounds that contain aromatic moieties.
- Nuclear Overhauser effect
The cross-relaxation between two nuclei, which is observable through the longitudinal magnetization of a given nucleus after a second nucleus is perturbed from equilibrium.
- STD NMR spectroscopy
(Saturation transfer difference nuclear magnetic resonance spectroscopy). An experiment in which spin-diffusion of the nuclear Overhauser effect spreads magnetization throughout the hydrogen nuclei of a receptor, which is partially transferred to the hydrogen nuclei of a binding ligand.
Biographies
Beat Ernst received his Ph.D. in synthetic chemistry from the Swiss Federal Institute of Technology Zürich, Switzerland, under the supervision of Professor Oskar Jeger. From 1979 to 1981, he was a postdoctoral fellow working in the laboratory of Professor Robert E. Ireland at Caltech, Pasadena, California, USA. He then joined the Central Research Laboratory of Ciba–Geigy in Basel, Switzerland, where he became Group Leader in 1984 and Section Head in 1992. In 1998 he moved to the University of Basel where he currently holds the position of a full professor in molecular pharmacy.
John Magnani received his Ph.D. from Princeton University, New Jersey, USA, and then joined the Laboratory of Biological Pharmacology under Dr Victor Ginsburg at the National Institutes of Health (NIH). After obtaining a tenured Research Chemist position, Magnani left the NIH in 1988. He helped co-found BioCarb and became its Vice President of Research. In 1992, he founded and managed GlycoTech Corporation as its President and Chief Executive Officer. In 2003, he co-founded GlycoMimetics and currently serves as the company's Chief Science Officer and Vice President.
Related links
FURTHER INFORMATION
Competing interests
J.L.M. is an employee and shareholder of GlycoMimetics Inc.
Footnotes
GlycoMimetics, Inc., 101 Orchard Ridge Drive, Gaithersburg, Maryland 20878, USA.
References
- 1.Van Teeffelen JW, Brands J, Stroes ES, Vink H. Endothelial glycocalyx: sweet shield of blood vessels. Trends Cardiovasc. Med. 2007;17:101–105. doi: 10.1016/j.tcm.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Nieuwdorp M, et al. Measuring endothelial glycocalyx dimensions in humans: a potential novel tool to monitor vascular vulnerability. J. Appl. Physiol. 2008;104:845–852. doi: 10.1152/japplphysiol.00440.2007. [DOI] [PubMed] [Google Scholar]
- 3.Petitou M, et al. The synthetic pentasaccharide fondaparinux: first in the class of antithrombotic agents that selectively inhibit coagulation factor Xa. Semin. Thromb. Hemost. 2002;28:393–402. doi: 10.1055/s-2002-34309. [DOI] [PubMed] [Google Scholar]
- 4.Chen X, Zheng Y, Shen Y. Vogliobose (Basen, AO-128), one of the most important α-glucosidase inhibitors. Curr. Med. Chem. 2006;13:109–116. doi: 10.2174/092986706789803035. [DOI] [PubMed] [Google Scholar]
- 5.Campbell LK, Baker DE, Campbell RK. Miglitol: assessment of its role in the treatment of patients with diabetes mellitus. Ann. Pharmacother. 2000;34:1291–1301. doi: 10.1345/aph.19269. [DOI] [PubMed] [Google Scholar]
- 6.Truscheit E, et al. Chemistry and biochemistry of microbial α-glucosidase inhibitors. Angew. Chem. Int. Ed. Engl. 1981;20:744–761. [Google Scholar]
- 7.von Itzstein M, et al. Rational design of potent sialidase-based inhibitors of influenza virus replication. Nature. 1993;363:418–423. doi: 10.1038/363418a0. [DOI] [PubMed] [Google Scholar]
- 8.Trunzer M, Faller B, Zimmerlin A. Metabolic soft spot identification and compound optimization in early discovery phases using Metasite and LC-MS/MS validation. J. Med. Chem. 2009;52:329–335. doi: 10.1021/jm8008663. [DOI] [PubMed] [Google Scholar]
- 9.Kim CU, et al. Influenza neuraminidase inhibitors possessing a novel hydrophobic interaction in the enzyme active site: design, synthesis, and structural analysis of carbocyclic sialic acid analogues with potent anti-influenza activity. J. Am. Chem. Soc. 1997;119:681–690. doi: 10.1021/ja963036t. [DOI] [PubMed] [Google Scholar]
- 10.Drickhamer K, Taylor ME. Identification of lectins from genomic sequence data. Methods Enzymol. 2003;362:560–567. doi: 10.1016/S0076-6879(03)01037-1. [DOI] [PubMed] [Google Scholar]
- 11.Mulloy B, Linhardt RJ. Order out of complexity — protein structures that interact with heparin. Curr. Opin. Struct. Biol. 2001;11:623–628. doi: 10.1016/s0959-440x(00)00257-8. [DOI] [PubMed] [Google Scholar]
- 12.Esko JD, Selleck SB. Order out of chaos: assembly of ligand binding sites in heparan sulfate. Annu. Rev. Biochem. 2002;71:435–471. doi: 10.1146/annurev.biochem.71.110601.135458. [DOI] [PubMed] [Google Scholar]
- 13.Bevilacqua MP, Stengelin S, Gimbrone MA, Seed B. Endothelial leukocyte adhesion molecule 1: an inducible receptor for neutrophils related to complement regulatory proteins and lectins. Science. 1989;243:1160–1165. doi: 10.1126/science.2466335. [DOI] [PubMed] [Google Scholar]
- 14.Tedder TF, et al. Isolation and chromosomal localization of cDNAs encoding a novel human lymphocyte cell surface molecule, LAM-1. Homology with the mouse lymphocyte homing receptor and other human adhesion proteins. J. Exp. Med. 1989;170:123–133. doi: 10.1084/jem.170.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston GI, Cook RG, McEver RP. Cloning of GMP-140, a granule membrane protein of platelets and endothelium: sequence similarity to proteins involved in cell adhesion and inflammation. Cell. 1989;56:1033–1044. doi: 10.1016/0092-8674(89)90636-3. [DOI] [PubMed] [Google Scholar]
- 16.Barthel SR, Gavino JD, Descheny L, Dimitroff CJ. Targeting selectins and selectin ligands in inflammation and cancer. Expert Opin. Ther. Targets. 2007;11:1473–1491. doi: 10.1517/14728222.11.11.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kansas GS, et al. A role for the epidermal growth factor-like domain of P-selectin in ligand recognition and cell adhesion. J. Cell Biol. 1994;124:609–618. doi: 10.1083/jcb.124.4.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berg EL, Robinson MK, Mansson O, Butcher EC, Magnani JL. A carbohydrate domain common to both sialyl Lea and sialyl Lex is recognized by the endothelial cell leukocyte adhesion molecule ELAM-1. J. Biol. Chem. 1991;266:14869–14872. [PubMed] [Google Scholar]
- 19.Magnani JL, et al. A monosialoganglioside is a monoclonal antibody-defined antigen of colon carcinoma. Science. 1981;212:55–56. doi: 10.1126/science.7209516. [DOI] [PubMed] [Google Scholar]
- 20.Magnani JL. The tumor markers, sialyl Lea and sialyl Lex bind ELAM-1. Glycobiology. 1991;1:318–320. doi: 10.1093/glycob/1.4.318. [DOI] [PubMed] [Google Scholar]
- 21.Fukushima K, et al. Characterization of sialosylated Lewisx as a new tumor-associated antigen. Cancer Res. 1984;44:5279–5285. [PubMed] [Google Scholar]
- 22.Ziske C, et al. Prognostic value of CA-19-9 levels in patients with inoperable adenocarcinoma of the pancreas treated with gemcitabine. Br. J. Cancer. 2003;89:1413–1417. doi: 10.1038/sj.bjc.6601263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakamori S, et al. Expression of carbohydrate antigen sialyl Lea: a new functional prognostic factor in gastric cancer. J. Clin. Oncol. 1997;15:816–825. doi: 10.1200/JCO.1997.15.2.816. [DOI] [PubMed] [Google Scholar]
- 24.Jorgensen T, et al. Up-regulation of the oligosaccharide sialyl Lewisx: a new prognostic parameter in metastatic prostate cancer. Cancer Res. 1995;55:1817–1819. [PubMed] [Google Scholar]
- 25.Nimrichter L, et al. E-selectin receptors on human leukocytes. Blood. 2008;112:3744–3752. doi: 10.1182/blood-2008-04-149641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hidalgo A, Peired AJ, Wild MK, Vestweber D, Frenette PS. Complete identification of E-selectin ligands on neutrophils reveals distinct functions of PSGL-1, ESL-1 and CD-44. Immunity. 2007;26:477–489. doi: 10.1016/j.immuni.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mulligan MS, et al. In vitro and in vivo selectin-blocking activities of sulfated lipids and sulfated sialyl compounds. Int. Immunol. 1998;10:569–575. doi: 10.1093/intimm/10.5.569. [DOI] [PubMed] [Google Scholar]
- 28.Skinner MP, et al. Characterization of human platelet GMP-140 as a heparin-binding protein. Biochem. Biophys. Res. Commun. 1989;164:1373–1379. doi: 10.1016/0006-291x(89)91821-4. [DOI] [PubMed] [Google Scholar]
- 29.Malhotra R, Priest R, Foster MR, Bird MI. P-selectin binds to bacterial lipopolysaccharide. Eur. J. Immunol. 1998;28:983–988. doi: 10.1002/(SICI)1521-4141(199803)28:03<983::AID-IMMU983>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 30.Skinner MP, Lucas CM, Burns GF, Chesterman CN, Berndt MC. GMP-140 binding to neutrophils is inhibited by sulfated glycans. J. Biol. Chem. 1991;266:5371–5374. [PubMed] [Google Scholar]
- 31.Kawashima H, et al. Binding of a large chondroitin sulfate/dermatan sulfate proteoglycan, versican, to L-selectin, P-selectin, and CD44. J. Biol. Chem. 2000;275:35448–35456. doi: 10.1074/jbc.M003387200. [DOI] [PubMed] [Google Scholar]
- 32.Kawashima H, et al. Oversulfated chondroitin/dermatan sulfates containing GlcAβ1/IdoAα1–3GalNAc(4,6-O-disulfate) interact with L- and P-selectin and chemokines. J. Biol. Chem. 2002;277:12921–12930. doi: 10.1074/jbc.M200396200. [DOI] [PubMed] [Google Scholar]
- 33.Wilkins PP, Moore KL, McEver RP, Cummings RD. Tyrosine sulfation of P-selectin glycoprotein ligand-1 is required for high affinity binding to P-selectin. J. Biol. Chem. 1995;270:22677–22680. doi: 10.1074/jbc.270.39.22677. [DOI] [PubMed] [Google Scholar]
- 34.Matsuda M, et al. Therapeutic effect of sulphated hyaluronic acid, a potential selectin-blocking agent, on experimental progressive mesangial proliferative glomerulonephritis. J. Pathol. 2002;198:407–414. doi: 10.1002/path.1209. [DOI] [PubMed] [Google Scholar]
- 35.Yoshida T, et al. Synthesis of a set of di- and tri-sulfated galabioses. Carbohydr. Res. 2001;335:167–180. doi: 10.1016/s0008-6215(01)00222-1. [DOI] [PubMed] [Google Scholar]
- 36.Kretzschmar G, Toepfer A, Huels C, Krause M. Pitfalls in the synthesis and biological evaluation of sialyl Lewisx mimetics as potential selectin antagonists. Tetrahedron. 1997;53:2485–2494. [Google Scholar]
- 37.Hidalgo A, et al. Heterotypic interactions enabled by polarized neutrophil microdomains mediate thromboinflammatory injury. Nature Med. 2009;15:384–391. doi: 10.1038/nm.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turhan A, Weiss LA, Mohandas N, Coller BS, Frenette PS. Primary role for adherent leukocytes in sickle cell vascular occlusion: a new paradigm. Proc. Natl Acad. Sci. USA. 2002;99:3047–3051. doi: 10.1073/pnas.052522799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanley WD, Burdick MM, Konstantopoulos K, Sackstein R. CD44 on LS174T colon carcinoma cells possesses E-selectin ligand activity. Cancer Res. 1997;65:5812–5817. doi: 10.1158/0008-5472.CAN-04-4557. [DOI] [PubMed] [Google Scholar]
- 40.Iwai K, et al. Importance of E-selectin (ELAM-1) and sialyl Lewisa in the adhesion of pancreatic carcinoma cells to activated endothelium. Int. J. Cancer. 1993;54:972–977. doi: 10.1002/ijc.2910540618. [DOI] [PubMed] [Google Scholar]
- 41.Jeschke U, et al. Expression of sialyl Lewisx, sialyl Lewisa, E-cadherin and cathepsin-D in human breast cancer: immunohistochemical analysis in mammary carcinoma in situ, invasive carcinoma and their lymph node metastasis. Anticancer Res. 2005;25:1615–1622. [PubMed] [Google Scholar]
- 42.Inata J, et al. Circulating KL-6/MUC1 mucin carrying sialyl Lewisa oligosaccharide is an independent prognostic factor in patients with lung adenocarcinoma. Int. J. Cancer. 2007;120:2643–2649. doi: 10.1002/ijc.22613. [DOI] [PubMed] [Google Scholar]
- 43.Dimitroff CJ, et al. Identification of leukocyte E-selectin ligands, P-selectin glycoprotein ligand-1 and E-selectin ligand-1, on human metastatic prostate tumor cells. Cancer Res. 2005;65:5750–5760. doi: 10.1158/0008-5472.CAN-04-4653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Magnani JL, et al. A monoclonal antibody-defined antigen associated with gastrointestinal cancer is a ganglioside containing sialylated lacto-N-fucopentaose. J. Biol. Chem. 1982;257:14365–14369. [PubMed] [Google Scholar]
- 45.Matsumoto S, et al. Cimetidine increases survival of colorectal cancer patients with high levels of sialyl Lewisx and sialyl Lewisa epitope expression on tumor cells. Brit. J. Cancer. 2002;86:161–167. doi: 10.1038/sj.bjc.6600048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Noguchi M, Sato N, Sugimori H, Mori K, Oshimi K. A minor E-selectin ligand, CD65, is critical for extravascular infiltration of acute myeloid leukemia cells. Leukemia Res. 2001;25:847–853. doi: 10.1016/s0145-2126(01)00036-4. [DOI] [PubMed] [Google Scholar]
- 47.Krause DS, Lazarides K, von Andrian UH, van Etten RA. Requirement for CD44 in homing and engraftment of BCR-ABL-expressing leukemic stem cells. Nature Med. 2006;12:1175–1180. doi: 10.1038/nm1489. [DOI] [PubMed] [Google Scholar]
- 48.Sackstein R. The bone marrow is akin to skin: HCELL and the biology of hematopoietic stem cell homing. J. Invest. Dermatol. 2004;122:1061–1069. doi: 10.1111/j.0022-202X.2004.09301.x. [DOI] [PubMed] [Google Scholar]
- 49.Ishikawa F, et al. Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nature Biotechnol. 2007;25:1315–1321. doi: 10.1038/nbt1350. [DOI] [PubMed] [Google Scholar]
- 50.Geijtenbeek TBH, et al. Identification of DC-SIGN, a novel dendritic cell-specific ICAM-3 receptor that supports primary immune responses. Cell. 2000;100:575–585. doi: 10.1016/s0092-8674(00)80693-5. [DOI] [PubMed] [Google Scholar]
- 51.Geijtenbeek TBH, et al. DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances trans-infection of T cells. Cell. 2000;100:587–597. doi: 10.1016/s0092-8674(00)80694-7. [DOI] [PubMed] [Google Scholar]
- 52.Appelmelk BJ, et al. Cutting edge: carbohydrate profiling identifies new pathogens that interact with dendritic cell-specific ICAM-3-grabbing nonintegrin on dendritic cells. J. Immunol. 2003;170:1635–1639. doi: 10.4049/jimmunol.170.4.1635. [DOI] [PubMed] [Google Scholar]
- 53.van Liempt E, et al. Specificity of DC-SIGN for mannose- and fucose-containing glycans. FEBS Lett. 2006;580:6123–6131. doi: 10.1016/j.febslet.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 54.Lozach PY, et al. DC-SIGN and L-SIGN are high affinity binding receptors for hepatitis C virus glycoprotein E2. J. Biol. Chem. 2003;278:20358–20366. doi: 10.1074/jbc.M301284200. [DOI] [PubMed] [Google Scholar]
- 55.Tassaneetrithep B, et al. DC-SIGN (CD209) mediates dengue virus infection of human dendritic cells. J. Exp. Med. 2003;197:823–829. doi: 10.1084/jem.20021840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alvarez CP, et al. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J. Virol. 2002;76:6841–6844. doi: 10.1128/JVI.76.13.6841-6844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marzi A, et al. DC-SIGN and DC-SIGNR interact with the glycoprotein of Marburg virus and the S protein of severe acute respiratory syndrome coronavirus. J. Virol. 2004;78:12090–12095. doi: 10.1128/JVI.78.21.12090-12095.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Han DP, Lohani M, Cho MW. Specific asparagine-linked glycosylation sites are critical for DC-SIGN and L-SIGN-mediated severe acute respiratory syndrome coronavirus entry. J. Virol. 2007;81:12029–12039. doi: 10.1128/JVI.00315-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Halary F, et al. Human cytomegalovirus binding to DC-SIGN is required for dendritic cell infection and target cell trans-infection. Immunity. 2002;17:653–664. doi: 10.1016/s1074-7613(02)00447-8. [DOI] [PubMed] [Google Scholar]
- 60.Tailleux L, et al. DC-SIGN is the major Mycobacterium tuberculosis receptor on human dendritic cells. J. Exp. Med. 2003;197:121–127. doi: 10.1084/jem.20021468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Colmenares M, Puig-Kroeger A, Pello OM, Corbi AL, Rivas L. Dendritic cell (DC)-specific intercellular adhesion molecule 3 (ICAM-3)-grabbing nonintegrin (DC-SIGN, CD209), a C-type surface lectin in human DCs, is a receptor for Leishmania amastigotes. J. Biol. Chem. 2002;277:36766–36769. doi: 10.1074/jbc.M205270200. [DOI] [PubMed] [Google Scholar]
- 62.van Die I, et al. The dendritic cell-specific C-type lectin DC-SIGN is a receptor for Schistosoma mansoni egg antigens and recognizes the glycan antigen Lewisx. Glycobiology. 2003;13:471–478. doi: 10.1093/glycob/cwg052. [DOI] [PubMed] [Google Scholar]
- 63.Gurney KB, et al. Binding and transfer of human immunodeficiency virus by DC-SIGN+ cells in human rectal mucosa. J. Virol. 2005;79:5762–5773. doi: 10.1128/JVI.79.9.5762-5773.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Naarding MA, et al. Lewisx component in human milk binds DC-SIGN and inhibits HIV-1 transfer to CD4+ T lymphocytes. J. Clin. Invest. 2005;115:3256–3264. doi: 10.1172/JCI25105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lasala F, Arce E, Otero JR, Rojo J, Delgado R. Mannosyl glycodendritic structure inhibits DC-SIGN-mediated ebola virus infections in cis and in trans. Antimicrob. Agents Chemother. 2003;47:3970–3972. doi: 10.1128/AAC.47.12.3970-3972.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rappocciolo G, et al. DC-SIGN is a receptor for human herpesvirus 8 on dendritic cells and macrophages. J. Immunol. 2006;176:1741–1749. doi: 10.4049/jimmunol.176.3.1741. [DOI] [PubMed] [Google Scholar]
- 67.Guo Y, et al. Structural basis for distinct ligand-binding and targeting properties of the receptors DC-SIGN and DC-SIGNR. Nature Struct. Mol. Biol. 2004;11:591–598. doi: 10.1038/nsmb784. [DOI] [PubMed] [Google Scholar]
- 68.Adams EW, et al. Oligosaccharide and glycoprotein microarrays as tools in HIV glycobiology; glycan-dependent gp120/protein interactions. Chem. Biol. 2004;11:875–881. doi: 10.1016/j.chembiol.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 69.Reina JJ, et al. 1,2-Mannobioside mimic: synthesis, DC-SIGN interaction by NMR and docking, and antiviral activity. ChemMedChem. 2007;2:1030–1036. doi: 10.1002/cmdc.200700047. [DOI] [PubMed] [Google Scholar]
- 70.Tabarani G, et al. Mannose hyperbranched dendritic polymers interact with clustered organization of DC-SIGN and inhibit gp120 binding. FEBS Lett. 2006;580:2402–2408. doi: 10.1016/j.febslet.2006.03.061. [DOI] [PubMed] [Google Scholar]
- 71.Frison N, et al. Oligolysine-based oligosaccharide clusters: selective recognition and elective recognition and endocytosis by the mannose receptor and dendritic cell-specific intercellular adhesion molecule 3 (ICAM-3)-grabbing nonintegrin. J. Biol. Chem. 2003;278:23922–23929. doi: 10.1074/jbc.M302483200. [DOI] [PubMed] [Google Scholar]
- 72.Timpano G, et al. Synthesis of novel DC-SIGN ligands with an alpha-fucosylamide anchor. Chembiochem. 2008;9:1921–1930. doi: 10.1002/cbic.200800139. [DOI] [PubMed] [Google Scholar]
- 73.Borrok MJ, Kiessling LL. Non-carbohydrate inhibitors of the lectin DC-SIGN. J. Am. Chem. Soc. 2007;129:12780–12785. doi: 10.1021/ja072944v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Crocker PR, Paulson JC, Varki A. Siglecs and their role in the immune system. Nature Rev. Immunol. 2007;7:255–266. doi: 10.1038/nri2056. [DOI] [PubMed] [Google Scholar]
- 75.Kelm S, et al. Sialoadhesin, myelin-associated glycoprotein and CD22 define a new family of sialic acid-dependent adhesion molecules of the immunoglobulin superfamily. Curr. Biol. 1994;4:965–972. doi: 10.1016/s0960-9822(00)00220-7. [DOI] [PubMed] [Google Scholar]
- 76.Chen MS, et al. Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature. 2000;403:434–439. doi: 10.1038/35000219. [DOI] [PubMed] [Google Scholar]
- 77.Wang KC, et al. Oligodendrocyte-myelin glycoprotein is a Nogo receptor ligand that inhibits neurite outgrowth. Nature. 2002;417:941–944. doi: 10.1038/nature00867. [DOI] [PubMed] [Google Scholar]
- 78.Mukhopadhyay G, Doherty P, Walsh FS, Crocker PR, Filbin MT. A novel role for myelin-associated glycoprotein as an inhibitor of axonal regeneration. Neuron. 1994;13:757–767. doi: 10.1016/0896-6273(94)90042-6. [DOI] [PubMed] [Google Scholar]
- 79.Filbin MT. Myelin-associated inhibitors of axonal regeneration in the adult mammalian CNS. Nature Rev. Neurosci. 2003;4:703–713. doi: 10.1038/nrn1195. [DOI] [PubMed] [Google Scholar]
- 80.Yang LJ-S, et al. Gangliosides are neuronal ligands for myelin-associated glycoprotein. Proc. Natl Acad. Sci. USA. 1996;93:814–818. doi: 10.1073/pnas.93.2.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yamashita T, Higuchi H, Tohyama M. The p75 receptor transduces the signal from myelin-associated glycoprotein to Rho. J. Cell. Biol. 2002;157:565–570. doi: 10.1083/jcb.200202010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yang LJS, et al. Sialidase enhances spinal axon outgrowth in vivo. Proc. Natl Acad. Sci. USA. 2006;103:11057–11062. doi: 10.1073/pnas.0604613103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hotta K, Ishida H, Kiso M, Hasegawa A. Synthetic studies on sialoglycoconjugates 66: first total synthesis of a cholinergic neuron-specific ganglioside GQ1bα. J. Carbohydr. Chem. 1995;14:491–506. [Google Scholar]
- 84.Ito H, Ishida H, Waki H, Ando S, Kiso M. Total synthesis of a cholinergic neuron-specific ganglioside GT1aα: A high affinity ligand for myelin-associated glycoprotein (MAG) Glycoconjugate J. 1999;16:585–598. doi: 10.1023/a:1007020815583. [DOI] [PubMed] [Google Scholar]
- 85.Ito H, Ishida H, Kiso M. A highly efficient total synthetic route to α-series gangliosides: GM1α, GD1α, and GT1α. J. Carbohydr. Chem. 2001;20:207–225. [Google Scholar]
- 86.Collins BE, et al. Enhanced binding of the neural siglecs, myelin-associated glycoprotein and Schwann cell myelin protein, to Chol-1 (α-series) gangliosides and novel sulfated Chol-1 analogs. J. Biol. Chem. 1999;274:37637–37643. doi: 10.1074/jbc.274.53.37637. [DOI] [PubMed] [Google Scholar]
- 87.Shin S-Y, et al. Binding epitope of gangliosides to their neuronal receptor, myelin-associated glycoprotein, from saturation transfer difference NMR. ChemBioChem. 2008;9:2946–2949. doi: 10.1002/cbic.200800485. [DOI] [PubMed] [Google Scholar]
- 88.Vyas AA, Blixt O, Paulson JC, Schnaar RL. Potent glycan inhibitors of myelin-associated glycoprotein enhance axon outgrowth in vitro. J. Biol. Chem. 2005;280:16305–16310. doi: 10.1074/jbc.M500250200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ofek I, Hasty DL, Sharon N. Anti-adhesion therapy of bacterial diseases: prospects and problems. FEMS Immunol. Med. Microbiol. 2003;38:181–190. doi: 10.1016/S0928-8244(03)00228-1. [DOI] [PubMed] [Google Scholar]
- 90.Levy SB. Antibiotic resistance – the problem intensifies. Adv. Drug. Deliv. Rev. 2005;57:1446–1450. doi: 10.1016/j.addr.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 91.Winzer K, et al. The Pseudomonas aeruginosa lectins PA-IL and PA-IIL are controlled by quorum sensing and by RpoS. J. Bacteriol. 2000;182:6401–6411. doi: 10.1128/jb.182.22.6401-6411.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bajolet-Laudinat O, et al. Cytotoxicity of Pseudomonas aeruginosa internal lectin PA-I to respiratory epithelial cells in primary culture. Infect. Immun. 1994;62:4481–4487. doi: 10.1128/iai.62.10.4481-4487.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mewe M, et al. Pseudomonas aeruginosa lectins I and II and their interaction with human airway cilia. J. Laryngol. Otol. 2005;119:595–599. doi: 10.1258/0022215054516313. [DOI] [PubMed] [Google Scholar]
- 94.Adam EC, Mitchell BS, Schumacher DU, Grant G, Schumacher U. Pseudomonas aeruginosa II lectin stops human ciliary beating: therapeutic implications of fucose. Am. J. Respir. Crit. Care Med. 1997;155:2102–2104. doi: 10.1164/ajrccm.155.6.9196121. [DOI] [PubMed] [Google Scholar]
- 95.Mitchell E, et al. Structural basis for oligosaccharide-mediated adhesion of Pseudomonas aeruginosa in the lungs of cystic fibrosis patients. Nature Struct. Biol. 2002;9:918–921. doi: 10.1038/nsb865. [DOI] [PubMed] [Google Scholar]
- 96.Sabin C, et al. Binding of different monosaccharides by lectin PA-IIL from Pseudomonas aeruginosa: thermodynamics data correlated with X-ray structures. FEBS Letters. 2006;580:982–987. doi: 10.1016/j.febslet.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 97.Wentworth JS, et al. Cytoplasmic lectins contribute to the adhesion of Pseudomonas aeruginosa. Biofouling. 1991;4:99–104. [Google Scholar]
- 98.von Bismarck P, Schneppenheim R, Schumacher U. Successful treatment of Pseudomonas aeruginosa respiratory tract infection with a sugar solution — a case report on a lectin based therapeutic principle. Klin. Padiatr. 2001;213:285–287. doi: 10.1055/s-2001-17220. [DOI] [PubMed] [Google Scholar]
- 99.Imberty A, Chabre YM, Roy R. Glycomimetics and glycodendrimers as high affinity microbial anti-adhesins. Chem. Eur. J. 2008;14:7490–7499. doi: 10.1002/chem.200800700. [DOI] [PubMed] [Google Scholar]
- 100.Perret S. et. al. Structural basis for the interaction between human milk oligosaccharides and the bacterial lectin PA-IIL of Pseudomonas aeruginosa. Biochem. J. 2005;389:325–332. doi: 10.1042/BJ20050079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Marotte K, et al. X-ray structures and thermodynamics of the interaction of PA-IIL from Pseudomonas aeruginosa with disaccharide derivatives. ChemMedChem. 2007;2:1328–1338. doi: 10.1002/cmdc.200700100. [DOI] [PubMed] [Google Scholar]
- 102.Marotte K, et al. Synthesis and binding properties of divalent and trivalent clusters of the Lewis a disaccharide moiety to Pseudomonas aeruginosa lectin PA-IIL. Org. Biomol. Chem. 2007;5:2953–2961. doi: 10.1039/b708227d. [DOI] [PubMed] [Google Scholar]
- 103.Johansson EM, et al. Combinatorial variation of branching length and multivalency in a large (390 625 member) glycopeptide dendrimer library: ligands for fucose-specific lectins. New J. Chem. 2007;31:1291–1299. [Google Scholar]
- 104.Deguise I, Lagnoux D, Roy R. Synthesis of glycodendrimers containing both fucoside and galactoside residues and their binding properties to PA-IL and PA-IIL lectins from Pseudomonas aeruginosa. New J. Chem. 2007;31:1321–1331. [Google Scholar]
- 105.Magnani, J. L., Patton, J. T. & Sarkar, A. K. Glycomimetic inhibitors of the PA-IL lectin, PA-IIL lectin or both of the lectins from pseudomonas. US Patent 7 517 980 B2.
- 106.Fihn SD. Acute uncomplicated urinary tract infection in women. N. Engl. J. Med. 2003;349:259–266. doi: 10.1056/NEJMcp030027. [DOI] [PubMed] [Google Scholar]
- 107.Mak RH, Kuo H-J. Pathogenesis of urinary tract infection: an update. Curr. Opin. Pediatr. 2006;18:148–152. doi: 10.1097/01.mop.0000193276.39495.0d. [DOI] [PubMed] [Google Scholar]
- 108.Palmer LM, Reilly TJ, Utsalo SJ, Donnenberg MS. Internalization of Escherichia coli by human renal epithelial cells is associated with tyrosine phosphorylation of specific host cell proteins. Infect. Immun. 1997;65:2570–2575. doi: 10.1128/iai.65.7.2570-2575.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sharon N. Carbohydrates as future anti-adhesion drugs for infectious diseases. Biochim. Biophys. Acta. 2006;1760:527–537. doi: 10.1016/j.bbagen.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 110.Hung C-S, et al. Structural basis of tropism of Escherichia coli to the bladder during urinary tract infection. Mol. Microbiol. 2002;44:903–915. doi: 10.1046/j.1365-2958.2002.02915.x. [DOI] [PubMed] [Google Scholar]
- 111.Firon N, Ofek I, Sharon N. Interaction of mannose-containing oligosaccharides with the fimbrial lectin of Escherichia coli. Biochem. Biophys. Res. Commun. 1982;105:1426–1432. doi: 10.1016/0006-291x(82)90947-0. [DOI] [PubMed] [Google Scholar]
- 112.Firon N, Ashkenazi S, Mirelman D, Ofek I, Sharon N. Aromatic alpha-glycosides of mannose are powerful inhibitors of the adherence of type 1 fimbriated Escherichia coli to yeast and intestinal epithelial cells. Infect. Immun. 1987;55:472–476. doi: 10.1128/iai.55.2.472-476.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Choudhury D, et al. X-ray structure of the FimC–FimH chaperone–adhesin complex from uropathogenic Escherichia coli. Science. 1999;285:1061–1066. doi: 10.1126/science.285.5430.1061. [DOI] [PubMed] [Google Scholar]
- 114.Wellens A, et al. Intervening with urinary tract infections using anti-adhesives based on the crystal structure of the FimH-oligomannose-3 complex. PLOS ONE. 2008;3:4. doi: 10.1371/journal.pone.0002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Berglund, J., Bouckaert, J., De Greve, H. & Knight, S. Anti-adhesive compounds to prevent and treat bacterial infections. Patent application PCT WO 2005/089733 A2 (2005).
- 116.Imberty A, Chabre YM, Roy R. Glycomimetics and glycodendrimers as high affinity microbial anti-adhesins. Chem. Eur. J. 2008;14:7490–7499. doi: 10.1002/chem.200800700. [DOI] [PubMed] [Google Scholar]
- 117.Sperling O, Fuchs A, Lindhorst TK. Evaluation of the carbohydrate recognition domain of the bacterial adhesin FimH: design, synthesis and binding properties of mannoside ligands. Org. Biomol. Chem. 2006;4:3913–3922. doi: 10.1039/b610745a. [DOI] [PubMed] [Google Scholar]
- 118.Bouckaert J, et al. Receptor binding studies disclose a novel class of high-affinity inhibitors of Escherichia coli FimH adhesin. Mol. Microbiol. 2005;55:441–455. doi: 10.1111/j.1365-2958.2004.04415.x. [DOI] [PubMed] [Google Scholar]
- 119.Nilsson LM, Thomas WE, Sokurenko EV, Vogel V. Elevated shear stress protects Escherichia coli cells adhering to surfaces via catch bonds from detachment by soluble inhibitors. Appl. Environ. Microbiol. 2006;72:3005–3010. doi: 10.1128/AEM.72.4.3005-3010.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pak J, Pu Y, Zhang Z-T, Hasty DL, Wu X-R. Tamm-Horsfall protein binds to type 1 fimbriated Escherichia coli and prevents E. coli from binding to uroplakin Ia and Ib receptors. J. Biol. Chem. 2001;276:9924–9930. doi: 10.1074/jbc.M008610200. [DOI] [PubMed] [Google Scholar]
- 121.Nilsson LM, Thomas WE, Sokurenko EV, Vogel V. Beyond induced-fit receptor-ligand interactions: structural changes that can significantly extend bond lifetimes. Structure. 2008;16:1047–1058. doi: 10.1016/j.str.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 122.Merritt EA, et al. Characterization and crystal structure of a high-affinity pentavalent receptor-binding inhibitor for cholera toxin and E. coli heat-labile enterotoxin. J. Am. Chem. Soc. 2002;124:8818–8824. doi: 10.1021/ja0202560. [DOI] [PubMed] [Google Scholar]
- 123.Spiess M. The asialoglycoprotein receptor: a model for endocytic transport receptors. Biochemistry. 1990;29:10009–10018. doi: 10.1021/bi00495a001. [DOI] [PubMed] [Google Scholar]
- 124.Ernst B, Hart G, Sinay P. Carbohydrates in Chemistry and Biology: A Handbook in 4 Volumes. 2000. [Google Scholar]
- 125.Seeberger PH, Werz DB. Automated synthesis of oligosaccharides as a basis for drug discovery. Nature Rev. Drug Discov. 2005;4:751–763. doi: 10.1038/nrd1823. [DOI] [PubMed] [Google Scholar]
- 126.Somers WS, Tang J, Shaw GD, Camphausen RT. Insights into the molecular basis of leukocyte tethering and rolling revealed by structures of P- and E-selectin bound to SLeX and PSGL-1. Cell. 2000;103:467–479. doi: 10.1016/s0092-8674(00)00138-0. [DOI] [PubMed] [Google Scholar]
- 127.May AP, Robinson RC, Vinson M, Crocker PR, Jones EY. Crystal structure of the N-terminal domain of sialoadhesin in complex with 3′ sialyllactose at 1.85 Å resolution. Mol. Cell. 1998;1:719–728. doi: 10.1016/s1097-2765(00)80071-4. [DOI] [PubMed] [Google Scholar]
- 128.Feinberg H, Mitchell DA, Drickamer K, Weis WI. Structural basis for selective recognition of oligosaccharides by DC-SIGN and DC-SIGNR. Science. 2001;294:2163–2166. doi: 10.1126/science.1066371. [DOI] [PubMed] [Google Scholar]
- 129.Bhunia A, et al. Consistent bioactive conformation of the Neu5Acα(2→3)Gal epitope upon lectin binding. ChemBioChem. 2008;9:2941–2945. doi: 10.1002/cbic.200800458. [DOI] [PubMed] [Google Scholar]
- 130.Thoma G, Magnani JL, Patton JT, Ernst B, Jahnke W. Preorganization of the bioactive conformation of sialyl Lewisx analogues correlates with their affinity to E-selectin. Angew. Chem. Int. Ed. Engl. 2001;40:1941–1945. [PubMed] [Google Scholar]
- 131.Mayer M, Meyer B. Characterization of ligand binding by saturation transfer difference spectroscopy. Angew. Chem. Int. Ed. Engl. 1999;38:1784–1788. doi: 10.1002/(SICI)1521-3773(19990614)38:12<1784::AID-ANIE1784>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 132.Haselhorst T, et al. STD NMR spectroscopy and molecular modeling investigation of the binding of N-acetylneuraminic acid derivatives to rhesus rotavirus VP8* core. Glycobiology. 2007;17:68–81. doi: 10.1093/glycob/cwl051. [DOI] [PubMed] [Google Scholar]
- 133.Herfurth L, et al. Comparative epitope mapping with saturation transfer difference NMR of sialyl Lewisa compounds and derivatives bound to a monoclonal antibody. J. Med. Chem. 2005;48:6879–6886. doi: 10.1021/jm0502687. [DOI] [PubMed] [Google Scholar]
- 134.Rinnbauer M, et al. Epitope mapping of sialyl LewisX bound to E-selectin using saturation transfer difference NMR experiments. Glycobiology. 2003;13:435–443. doi: 10.1093/glycob/cwg043. [DOI] [PubMed] [Google Scholar]
- 135.Schwardt O, et al. Examination of the biological role of the α(2–6)-linked sialic acid in gangliosides binding to the myelin-associated glycoprotein. J. Med. Chem. 2009;52:989–1004. doi: 10.1021/jm801058n. [DOI] [PubMed] [Google Scholar]
- 136.Schwardt O, Kolb HC, Ernst B. The Organic Chemistry of Sugars. 2005. p. 803. [Google Scholar]
- 137.Mehta P, Cummings RD, McEver RP. Affinity and kinetic analysis of P-selectin binding to P-selectin glycoprotein ligand-1. J. Biol. Chem. 1998;273:32506–32513. doi: 10.1074/jbc.273.49.32506. [DOI] [PubMed] [Google Scholar]
- 138.Wild MK, Huang M-C, Schulze-Horsel U, van der Merwe PA, Vestweber D. Affinity, kinetics and thermodynamics of E-selectin binding to E-selectin ligand-1. J. Biol. Chem. 2001;276:31602–31612. doi: 10.1074/jbc.M104844200. [DOI] [PubMed] [Google Scholar]
- 139.Nicholson MW, Barclay AN, Singer MS, Rosen SD, van der Merwe PA. Affinity and kinetic analysis of L-selectin (CD62L) binding to glycosylation-dependent cell-adhesion molecule-1. J. Biol. Chem. 1998;273:763–770. doi: 10.1074/jbc.273.2.763. [DOI] [PubMed] [Google Scholar]
- 140.Copeland RA, Pompliano DL, Meek TD. Drug-target residence time and its implications for lead optimization. Nature Rev. Drug Discov. 2006;5:730–739. doi: 10.1038/nrd2082. [DOI] [PubMed] [Google Scholar]
- 141.Kolb HC, Ernst B. Development of tools for the design of selectin antagonists. Chem. Eur. J. 1997;3:1571–1578. [Google Scholar]
- 142.Kolb, H. C. Diglycosylated 1,2-diols as mimetics of sialyl Lewisx and sialy Lewisa. Patent application PCT WO 1997/01569 (1997).
- 143.Lee RT, Lee YC. Affinity enhancement by multivalent lectin-carbohydrate interaction. Glycoconj. J. 2000;17:543–551. doi: 10.1023/a:1011070425430. [DOI] [PubMed] [Google Scholar]
- 144.Lundquist JL, Toone EJ. The cluster glycoside effect. Chem. Rev. 2002;102:555–578. doi: 10.1021/cr000418f. [DOI] [PubMed] [Google Scholar]
- 145.Mammen M, Choi S-K, Whitesides GM. Polyvalent interactions in biological systems: implications for the design and use of multivalent ligands and inhibitors. Angew. Chem. Int. Ed. 1998;37:2754–2794. doi: 10.1002/(SICI)1521-3773(19981102)37:20<2754::AID-ANIE2754>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 146.Kitov PI, et al. Shiga-like toxins neutralized by tailored multivalent carbohydrate ligands. Nature. 2000;403:669–672. doi: 10.1038/35001095. [DOI] [PubMed] [Google Scholar]
- 147.Kitov PI, Bundle DR. On the nature of the multivalency effect: a thermodynamic model. J. Am. Chem. Soc. 2003;125:16271–16284. doi: 10.1021/ja038223n. [DOI] [PubMed] [Google Scholar]
- 148.Martinez MN, Amidon GL. A mechanistic approach to understanding the factors affecting drug absorption: a review of fundamentals. J. Clin. Pharmacol. 2002;42:620–643. doi: 10.1177/00970002042006005. [DOI] [PubMed] [Google Scholar]
- 149.Lipinski CA, Lombardo F, Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Del. Rev. 1997;23:3–25. doi: 10.1016/s0169-409x(00)00129-0. [DOI] [PubMed] [Google Scholar]
- 150.Lima LM, Barreiro EJ. Bioisosterism: a useful strategy for molecular modification and drug design. Curr. Med. Chem. 2005;12:23–49. doi: 10.2174/0929867053363540. [DOI] [PubMed] [Google Scholar]
- 151.Rautio J, et al. Prodrugs: design and clinical applications. Nature Rev. Drug Discov. 2008;7:255–270. doi: 10.1038/nrd2468. [DOI] [PubMed] [Google Scholar]
- 152.Taylor NR, von Itzstein M. Molecular modeling studies on ligand binding to sialidase from influenza virus and the mechanism of catalysis. J. Med. Chem. 1994;37:616–624. doi: 10.1021/jm00031a011. [DOI] [PubMed] [Google Scholar]
- 153.He G, Massarella J, Ward P. Clinical pharmacokinetics of the prodrug oseltamivir and its active metabolite Ro 64-0802. Clin. Pharmacokinet. 1999;37:471–484. doi: 10.2165/00003088-199937060-00003. [DOI] [PubMed] [Google Scholar]
- 154.You G, Morris ME. Drug transporters: molecular characterization and role in drug disposition. 2007. [Google Scholar]
- 155.Inui K-I, Terada T, Masuda S, Saito H. Physiological and pharmacological implications of peptide transporters, PEPT1 and PEPT2. Nephrol. Dial. Transplant. 2000;15:11–13. doi: 10.1093/ndt/15.suppl_6.11. [DOI] [PubMed] [Google Scholar]
- 156.Bailey, P. D. et al. Affinity prediction for substrates of the peptide transporter PepT1. Chem. Commun. 323–325 (2006). [DOI] [PubMed]
- 157.Riley RJ, Grime K. Metabolic screening in vitro: metabolic stability, CYP inhibition and induction. Drug Discov. Today Technol. 2004;1:365–372. doi: 10.1016/j.ddtec.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 158.Mizuno N, Niwa T, Yotsumoto Y, Sugiyama Y. Impact of drug transporter studies on drug discovery and development. Pharmacol. Rev. 2003;55:425–461. doi: 10.1124/pr.55.3.1. [DOI] [PubMed] [Google Scholar]
- 159.Shitara Y, Horie T, Sugiyama Y. Transporters as a determinant of drug clearance and tissue distribution. Eur. J. Pharm. Sci. 2006;27:425–446. doi: 10.1016/j.ejps.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 160.Holodniy M, et al. Pharmacokinetics and tolerability of oseltamivir combined with probenecid. Antimicrob. Agents Chemother. 2008;52:3013–3021. doi: 10.1128/AAC.00047-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Weitz JI. Low-molecular-weight heparins. N. Engl. J. Med. 1997;337:688–699. doi: 10.1056/NEJM199709043371007. [DOI] [PubMed] [Google Scholar]
- 162.Weinreb NJ, et al. Guidance on the use of miglustat for treating patients with type 1 Gaucher disease. Am. J. Hematol. 2005;80:223–239. doi: 10.1002/ajh.20504. [DOI] [PubMed] [Google Scholar]
- 163.Maryanoff BE, Nortey SO, Gardocki JF, Shank RP, Dodgson SP. Anticonvulsant O-alkyl sulfamates. 2,3:4,5-bis-O-(1-methylethylidene)-beta-D-fructopyranose sulfamate and related compounds. J. Med. Chem. 1987;30:880–887. doi: 10.1021/jm00388a023. [DOI] [PubMed] [Google Scholar]
- 164.Li X, et al. Arthroscopic debridement of the osteoarthritic knee combined with hyaluronic acid (Orthovisc®) treatment: a case series and review of the literature. J. Orthopaedic Surg. Res. 2008;3:43–50. doi: 10.1186/1749-799X-3-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ito H, et al. Systematic synthesis and MAG-binding activity of novel sulfated GM1b analogues as mimics of Chol-1 (α-series) gangliosides: highly active ligands for neural siglecs. Carbohydr. Res. 2003;338:1621–1639. doi: 10.1016/s0008-6215(03)00245-3. [DOI] [PubMed] [Google Scholar]
- 166.Schwizer D, et al. Antagonists of the myelin-associated glycoprotein: a new class of tetrasaccharide mimics. Bioorg. Med. Chem. 2006;14:4944–4957. doi: 10.1016/j.bmc.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 167.Kelm S, et al. Functional groups of sialic acids involved in binding to Siglecs (Sialoadhesins) deduced from interactions with synthetic analogues. Eur. J. Biochem. 1998;255:663–672. doi: 10.1046/j.1432-1327.1998.2550663.x. [DOI] [PubMed] [Google Scholar]
- 168.Shelke SV, et al. Synthesis of sialic acid derivatives as ligands for the myelin-associated glycoprotein (MAG) Bioorg. Med. Chem. 2007;15:4951–4965. doi: 10.1016/j.bmc.2007.04.038. [DOI] [PubMed] [Google Scholar]
- 169.Gao G-P, et al. Mimetics of the tri- and tetrasaccharide epitope of GQ1bα as myelin-associated glycoprotein (MAG) ligands. Bioorg. Med. Chem. 2007;15:7459–7469. doi: 10.1016/j.bmc.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 170.Kötter S, Krallmann-Wenzel U, Ehlers S, Lindhorst TK. Multivalent ligands for the mannose-specific lectin on type 1 fimbriae of Escherichia coli: syntheses and testing of trivalent α-D-mannoside clusters. J. Chem. Soc. Perkin Trans. 1998;1:2193–2200. [Google Scholar]
- 171.Dubber M, Sperling O, Lindhorst TK. Oligomannoside mimetics by glycosylation of 'octopus glycosides' and their investigation as inhibitors of type 1 fimbriae-mediated adhesion of Escherichia coli. Org. Biomol. Chem. 2006;4:3901–3912. doi: 10.1039/b610741a. [DOI] [PubMed] [Google Scholar]
- 172.König B, Fricke T, Wassmann A, Krallmann-Wenzel U, Lindhorst TK. α-Mannosyl clusters scaffolded on azamacrocycles: synthesis and inhibitory properties in the adhesion of type 1 fimbriated Escherichia coli to guinea pig erythrocytes. Tetrahedron Lett. 1998;39:2307–2310. [Google Scholar]
- 173.Touaibia M, et al. Mannosylated G0 dendrimers with nanomolar affinities to Escherichia coli FimH. ChemMedChem. 2007;2:1190–1201. doi: 10.1002/cmdc.200700063. [DOI] [PubMed] [Google Scholar]
- 174.Appeldoorn CCM, et al. Novel multivalent mannose compounds and their inhibition of the adhesion of type 1 fimbriated uropathogenic E. coli. Tetrahedron Asym. 2005;16:361–372. [Google Scholar]
- 175.Scheffler K, et al. Determiation of the bioactive conformation of the carbohydrate ligand in the E-Selectin/sialyl Lewisx complex. Angew. Chem. Int. Ed. Engl. 1995;34:1841–1844. [Google Scholar]
- 176.Poppe L, Brown GS, Philo JS, Nikrad PV, Shah BH. Conformation of sLex tetrasaccharide, free in solution and bound to E-, P-, and L-selectin. J. Am. Chem. Soc. 1997;119:1727–1736. [Google Scholar]
- 177.Harris R, et al. Stable-isotope-assisted NMR studies on13C-enriched sialyl Lewisx in solution and bound to E-selectin. J. Am. Chem. Soc. 1999;121:2546–2551. [Google Scholar]
- 178.Norman KE, Anderson GP, Kolb HC, Ley K, Ernst B. Sialyl Lewisx (sLex) and a sLex mimetic, CGP69669A, disrupt E-selectin-dependent leukocyte rolling in vivo. Blood. 1998;91:475–483. [PubMed] [Google Scholar]
- 179.Kerr KM, et al. The use of Cylexin (CY-1503) in prevention of reperfusion lung injury in patients undergoing pulmonary thromboendarterectomy. Am. J. Respir. Crit. Care Med. 2000;162:14–20. doi: 10.1164/ajrccm.162.1.9712142. [DOI] [PubMed] [Google Scholar]
- 180.Kogan TP, et al. Novel synthetic inhibitors of selectin-mediated cell adhesion: synthesis of 1,6-Bis[3-(3-carboxymethylphenyl)-4-(2-D-mannopyranosyloxy)phenyl]hexane (TBC1269) J. Med. Chem. 1998;41:1099–1111. doi: 10.1021/jm9704917. [DOI] [PubMed] [Google Scholar]
- 181.Ikegami-Kuzuhara A, Yoshinaka T, Ohmoto H, Inoue Y, Saito T. Therapeutic potential of a novel synthetic selectin blocker, OJ-R9188, in allergic dermatitis. Br. J. Pharmacol. 2001;134:1498–1504. doi: 10.1038/sj.bjp.0704397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Magnani, J. L., Patton, J. T., Sarkar, A. K., Svarovsky, S. A. & Ernst, B. Heterobifunctional pan-selectin inhibitors. International patent application PCT/US 2006/034274 (2006).
- 183.Kaila N, et al. 2-(4-Chlorobenzyl)-3-hydroxy-7,8,9,10-tetrahydrobenzo[H]quinoline-4-carboxylic acid (PSI-697): identification of a clinical candidate from the quinoline salicylic acid series of P-selectin antagonists. J. Med. Chem. 2007;50:40–64. doi: 10.1021/jm060631p. [DOI] [PubMed] [Google Scholar]
- 184.Wada Y, et al. Studies on selectin blockers. 2. Novel selectin blocker as potential therapeutics for inflammatory disorders. J. Med. Chem. 1996;39:2055–2059. doi: 10.1021/jm950877m. [DOI] [PubMed] [Google Scholar]
- 185.Schon MP, et al. Efomycine M, a new specific inhibitor of selectin, impairs leukocyte adhesion and alleviates cutaneous inflammation. Nature Med. 2002;8:366–372. doi: 10.1038/nm0402-366. [DOI] [PubMed] [Google Scholar]
- 186.von Itzstein M. The war against influenza: discovery and development of sialidase inhibitors. Nature Rev. Drug Discov. 2007;6:967–974. doi: 10.1038/nrd2400. [DOI] [PubMed] [Google Scholar]
- 187.Amonsen M, Smith DF, Cummings RD, Air GM. Human parainfluenza viruses hPIV1 and hPIV3 bind oligosaccharides with α2–3 linked sialic acids that are distinct from those bound by H5 avian influenza virus hemagglutinin. J. Virol. 2007;81:8341–8345. doi: 10.1128/JVI.00718-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Choi J-M, Hutson AM, Estes MK, Prasad VV. Atomic resolution structural characterization of recognition of histo-blood group antigens by Norwalk virus. Proc. Natl Acad. Sci. USA. 2008;105:9175–9180. doi: 10.1073/pnas.0803275105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Isa P, Arias CF, Lopez S. Role of sialic acids in rotavirus infection. Glycoconj. J. 2006;23:27–37. doi: 10.1007/s10719-006-5435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Copeland R, et al. Using a 3-O-sulfated heparin octasaccharide to inhibit the entry of herpes simplex virus type I. Biochem. 2008;47:5774–5783. doi: 10.1021/bi800205t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Rademacher C, Krishna NR, Palcic M, Parra F, Peters T. NMR experiments reveal the molecular basis of receptor recognition by a calicvirus. J. Am. Chem. Soc. 2008;130:3669–3675. doi: 10.1021/ja710854r. [DOI] [PubMed] [Google Scholar]
- 192.Schwegmann-Wessels C, Herrier G. Sialic acids as receptor determinants for coronaviruses. Glycoconj. J. 2006;23:51–58. doi: 10.1007/s10719-006-5437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Gillet L, Colaco S, Stevenson PG. The murid herpesvirus-4 gH/gL binds to glycosaminoglycans. PLoS ONE. 2008;3:1–9. doi: 10.1371/journal.pone.0001669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Nilsson EC, Jamshidi F, Johansson SMC, Oberste MS, Arnberg N. Sialic acid is a cellular receptor for Coxsackievirus A24 variant, an emerging virus with pandemic potential. J. Virol. 2008;82:3061–3068. doi: 10.1128/JVI.02470-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.de Witte L, et al. Binding of human papilloma virus L1 virus-like particles to dendritic cells is mediated through heparan sulfates and induces immune activation. Immunobiology. 2007;212:679–691. doi: 10.1016/j.imbio.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 196.Dugan AS, Gasparovic ML, Atwood WJ. Direct correlation between sialic acid binding and infection of cells by two human polyomaviruses (JC virus and BK virus) J. Virol. 2008;82:2560–2564. doi: 10.1128/JVI.02123-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Neu U, Woellner K, Gauglitz G, Stehle T. Structural basis of GM1 ganglioside recognition by simian virus 40. Proc. Natl Acad. Sci. USA. 2008;105:5219–5224. doi: 10.1073/pnas.0710301105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Suzuki Y, Suzuki T, Matsunaga M, Matsumoto M. Gangliosides as paramyxovirus receptor. Structural requirement of sialo-oligosaccharides in receptors for hemagglutinating virus of Japan (Sendai virus) and Newcastle disease virus. J. Biochem. 1985;97:1189–1199. doi: 10.1093/oxfordjournals.jbchem.a135164. [DOI] [PubMed] [Google Scholar]