Abstract
Purpose
Blastomyces dermatitidis is a dimorphic fungus endemic to North America capable of causing fatal respiratory failure. Acute respiratory distress syndrome (ARDS) complicates up to 10% of pulmonary blastomycosis in hospitalized patients and carries a mortality of 50-90%. This report describes the clinical course of four consecutive patients with blastomycosis-related ARDS treated with venovenous extracorporeal membrane oxygenation (ECMO) during 2009-2014.
Clinical features
Four adults were referred from northwestern Ontario, Canada with progressive respiratory illnesses. All patients developed diffuse bilateral opacities on chest radiography and required mechanical ventilation within 6-72 hr. Patients satisfied Berlin criteria for severe ARDS with trough PaO2/FiO2 ratios of 44-61 on positive end-expiratory pressure of 12-24 cm H2O. Wet mount microscopy from respiratory samples showed broad-based yeast consistent with B.dermatitidis. Despite lung protective ventilation strategies with maximal FiO2 (patients A-D), neuromuscular blockade (patients A-D), inhaled nitric oxide (patients A and D), and prone positioning (patient D), progressive hypoxemia resulted in initiation of venovenous ECMO by hours 24-90 of mechanical ventilation with subsequent de-escalation of ventilatory support. In all four cases, ECMO decannulation was performed (7-23 days), mechanical ventilation was withdrawn (18-52 days), and the patients survived to hospital discharge (31-87 days).
Conclusion
This report describes the successful application of ECMO as rescue therapy in aid of four patients with refractory blastomycosis-associated ARDS. In addition to early appropriate antimicrobial therapy, transfer to an institution experienced with ECMO should be considered when caring for patients from endemic areas with rapidly progressive respiratory failure.
Keywords: Acute Respiratory Distress Syndrome, Extracorporeal Membrane Oxygenation, Blastomycosis, Target Temperature Management, ECMO Support
Résumé
Objectif
Blastomyces dermatitidis est un champignon dimorphique endémique en Amérique du Nord, susceptible de provoquer une défaillance respiratoire fatale. Le syndrome de détresse respiratoire aiguë (SDRA) complique jusqu’à 10 % des cas de blastomycose pulmonaire chez les patients hospitalisés avec un taux de mortalité de 50 % à 90 %. Ce compte rendu décrit l’évolution clinique de quatre patients consécutifs atteints de SDRA lié à une blastomycose et traités par oxygénation par membrane extracorporelle (ECMO) par voie veinoveineuse entre 2009 et 2014.
Caractéristiques cliniques
Quatre adultes en provenance du nord-ouest de l’Ontario (Canada) ont été transférés pour des maladies respiratoires évolutives. Tous les patients ont développé des opacités diffuses bilatérales sur les radiographies de thorax et une ventilation mécanique a été nécessaire dans un délai de 6 à 72 heures. Les patients répondaient aux critères de Berlin pour un SDRA sévère avec des rapports minimums PaO2/CiO2 de 44 à 61 sur une pression positive de fin d’expiration de 12 à 24 cm H2O. Un examen microscopique sur lame humide des échantillons respiratoires a montré une levure à base large compatible avec B. dermatitidis. En dépit de stratégies ventilatoires protégeant le poumon avec une FiO2 maximum (patients A à D), un bloc neuromusculaire (patients A à D), du monoxyde d’azote inhalé (patients A et D), et une position en procubitus (patient D), la progression de l’hypoxémie a nécessité l’instauration d’une ECMO veinoveineuse dans un délai de 24 à 90 heures après l’instauration de la ventilation mécanique, suivie d’une désescalade progressive du soutien ventilatoire. Dans ces quatre cas, la décanulation de l’ECMO a pu avoir lieu (entre 7 et 23 jours), la ventilation mécanique a été retirée (entre 18 et 52 jours) et les patients ont survécu après leur congé de l’hôpital (31 à 87 jours).
Conclusion
Ce compte rendu décrit la réussite de l’utilisation de l’ECMO comme traitement de secours visant à aider quatre patients atteints d’un SDRA réfractaire associé à une blastomycose. En plus du traitement antimicrobien adapté, le transfert des patients vers un établissement ayant l’habitude de l’ECMO doit être envisagé au cours de la prise en charge de patients vivant en zone d’endémie et présentant une défaillance respiratoire rapidement évolutive.
Blastomyces dermatitidis, a dimorphic fungus endemic to well-described regions in North America, is capable of causing life-threatening disease in young immunocompetent adults.1,2 Blastomycosis remains a rare disease, but incidence reaches seven cases per 100,000 annually in northwestern Ontario.1 Although 90% of affected patients have primarily pulmonary involvement, clinical manifestations vary widely.1-3 Up to 10% of hospitalized patients with pulmonary blastomycosis develop acute respiratory distress syndrome (ARDS).3,4 In contrast to ARDS of other etiologies, patients with blastomycosis-related ARDS have disproportionately high reported mortality (50-90%) and may be more likely to die from early refractory respiratory failure.2,5,6 Expert consensus supports early aggressive treatment; however, a specific strategy has yet to be developed.3
Venovenous extracorporeal membrane oxygenation (ECMO) has been utilized for the management of severe ARDS to facilitate gas exchange, allow lung rest by de-escalation of ventilatory support, and provide time for resolution of the underlying disease.7 Extracorporeal membrane oxygenation is generally considered in ARDS patients with refractory hypoxemia or hypercapnia despite a lung protective ventilation strategy or in those where the maintenance of adequate gas exchange requires potentially injurious applied volumes or pressures.8 Selective application of ECMO may have resulted in a reduction in mortality among patients with severe ARDS secondary to H1N1 infection.9-11 Nevertheless, uncertainty exists regarding the appropriateness of ECMO during disseminated fungal infection or septic shock in adults.12 We describe a case series of four critically ill patients with blastomycosis-related ARDS treated with venovenous ECMO.
Clinical features
Ethics approval was provided by the University of Manitoba Health Research Ethics Board (Registration number: University of Manitoba H2014:215, June, 2014), and informed consent was obtained in three of four cases in which contact information was available. A retrospective cohort study was performed on all patients with blastomycosis-related ARDS treated with ECMO at a single Canadian site during 2009-2014. The ECMO referral centre is a regional tertiary care 550-bed academic facility that performs approximately ten venovenous ECMO cannulations for respiratory failure annually. Patient demographics, ECMO-related variables, and clinical data were obtained from the medical record. Descriptive statistical analysis was performed with GraphPad Prism V6.0c (GraphPad Software Inc., La Jolla, CA, USA).
Four adults aged 21-39 were referred from northwestern Ontario, Canada with progressive respiratory symptoms, including coughing, sputum production, fever, and dyspnea. Three of four patients were previously healthy and immunocompetent. One patient had complex comorbidities, including hemochromatosis, type 1 diabetes mellitus, stiff person syndrome (a rare autoimmune disorder of progressive muscle rigidity), and Addison’s disease. All patients required tracheal intubation and mechanical lung ventilation for hypoxemic (patient C) or mixed hypoxemic/hypercapneic (patients A, B, D) respiratory failure. On admission to the intensive care unit, the patients were hemodynamically unstable requiring vasopressor support, with APACHE II scores ranging from 18-26. The patients initially received antimicrobial therapy for community-acquired bacterial pneumonia at local emergency departments or nursing stations. Upon arrival at the tertiary facility, bronchoscopy with bronchoalveolar lavage was performed. Wet mount microscopy of respiratory samples showed yeast morphology consistent with B. dermatitidis, subsequently confirmed by culture. Accordingly, in patients A-C, liposomal intravenous amphotericin B 5 mg·kg−1·day−1 was initiated within the first 48 hr of hospital care. Patient D was given conventional amphotericin B infusion 1 mg·kg−1·day−1 commencing at hour 78. Three of four patients received systemic corticosteroids (Methylprednisone 40-60 mg every six hours) within the first 48 hr of mechanical ventilation. Additional baseline characteristics are summarized in Table 1.
Table 1.
Baseline characteristics of study patients
| Characteristic | Patient A | Patient B | Patient C | Patient D |
|---|---|---|---|---|
| Age | 22 | 39 | 21 | 39 |
| Sex (female) | Yes | No | Yes | No |
| BMI (kg·m−2) | 25.5 | 33.2 | 28.6 | 24.3 |
| Aboriginal descent | Yes | Yes | Yes | No |
| Comorbidities | ||||
| Obesity | No | Yes | Yes | No |
| Smoking | No | No | Yes | No |
| Ethanol use | No | Yes | No | No |
| Vital signs on presentation | ||||
| Mean arterial pressure (mmHg) | 45 | 98 | 74 | 65 |
| Respiratory Rate (breaths·min−1) | 30 | 48 | 38 | 23 |
| Heart rate (beats·min−1) | 102 | 129 | 134 | 113 |
| Temperature (°C) | 38 | 38.9 | 39.6 | 39.2 |
| Organ dysfunction (ICU admission) | ||||
| Creatinine (µmol·L−1) | 68 | 473 | 77 | 86 |
| AST (U·L−1) | 15 | 60 | 62 | 20 |
| Bilirubin (µmol·L−1) | 11 | 8 | 11 | 7 |
| WBC (cell count ×10−9·L−1) | 27.9 | 15.5 | 38.6 | 7 |
| Lactate (mmol·L−1) | - | 2.3 | 4.1 | 1.8 |
| APACHE II score | 19 | 26 | 20 | 18 |
| Duration of illness | ||||
| Symptoms to hospital admission (days) | 9 | 3 | 14 | 7 |
| Admission to tracheal intubation (hr) | 6 | 3 | 48 | 70 |
| Time until appropriate antimicrobials administered (hr) | 24 | 12 | 48 | 78 |
| Systemic corticosteroids within 48 hr of mechanical ventilation | Yes | Yes | No | Yes |
| Norepinephrine use during hospital admission (days) | 13 | 1 | 9 | 3 |
| Vasopressin use during hospital admission (days) | 12 | 1 | 13 | 1 |
| ECMO configuration (I-inflow, R-return) | I:19Fr LCFV + 17Fr RIJ, R:19Fr RCFV | I/R: 31Fr RIJ bicaval dual lumen | I/R: 31 Fr RIJ bicaval dual lumen + I: 21Fr RCFV | I: 24 Fr RIJ + 22 Fr LCFV, R: 23 Fr RCFV |
APACHE II = acute physiology and chronic health evaluation II; AST = aspartate aminotransferase; BMI = body mass index; ECMO = extracorporeal membrane oxygenation; Fr = French; ICU = intensive care unit; LCFV = left common femoral vein; RCFV = right common femoral vein; RIJ = right internal jugular vein; WBC = white blood cell
Patients developed four-quadrant airspace opacification on chest radiography (Fig. 1) with Murray lung injury scores of 2.75-4. Berlin criteria for severe ARDS were satisfied with trough PaO2/FiO2 ratios of 44-61 on positive end-expiratory pressure (PEEP) levels of 12-24 cm H2O. Positive end-expiratory pressure was titrated based on observation of gas exchange during bedside PEEP trials. A low tidal volume ventilation strategy (5-8 mL·kg−1 of predicted body weight) with permissive hypercapnia was used. Life-threatening hypoxemia, acidosis, and injurious airway pressures developed despite 100% FiO2 (patients A-D), neuromuscular blockade (patients A-D), inhaled nitric oxide at 20 ppm (patients A and D), and prone positioning (patient D) (Table 2). In two cases, these conditions prompted dispatch of an aeromedical ECMO transport team, consisting of a cardiothoracic surgeon, perfusionist, critical care nurse, and critical care fellow, to facilitate ECMO cannulation in the peripheral hospital. In the remaining cases, the cannulation procedure was performed on-site at the ECMO facility.
Fig. 1.
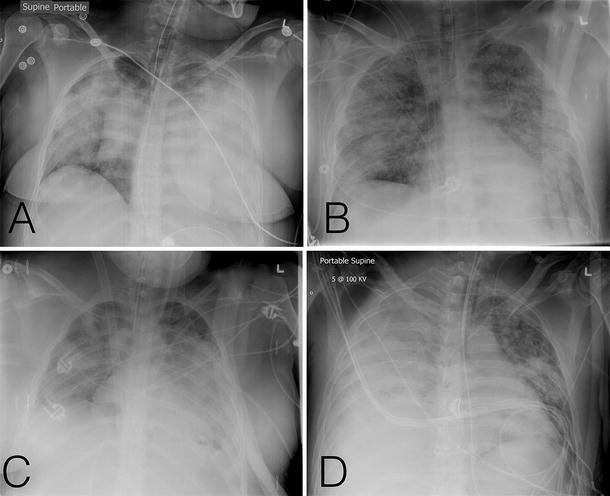
Chest radiography. Anterior-posterior chest radiographs obtained following mechanical ventilation in patients A, B, C, and D, respectively
Table 2.
Severity of ARDS prior to initiation of ECMO
| Patient A | Patient B | Patient C | Patient D | |
|---|---|---|---|---|
| Ventilation and gas exchange | ||||
| Highest FiO2 | 1.0 | 1.0 | 1.0 | 1.0 |
| Trough PaO2/FiO2 ratio | 58 | 61 | 55 | 44 |
| Highest PEEP administered (cm H2O) | 16 | 24 | 12 | 14 |
| Lowest pH | 7.13 | 7.06 | 7.17 | 6.99 |
| Highest PaCO2, (mmHg) | 73 | 78 | 46 | 102 |
| Tidal volume mL·kg−1 PBW | 5.1 | 7.6 | 6.3 | 7.1 |
| Highest peak/plateau airway pressure (cm H2O) | 50/- | 40/- | -/33 | 46/35 |
| Quadrants of chest radiograph affected (number) | 4 | 4 | 4 | 4 |
| Murray lung injury score | 4 | 2.75 | 3.5 | 3.5 |
| Adjunctive/Rescue therapy | ||||
| Neuromuscular blockade within 48 hr of mechanical ventilation | Yes | Yes | Yes | Yes |
| Recruitment maneuvers | No | Yes | No | Yes |
| Inhaled nitric oxide | Yes | No | No | Yes |
| Prone positioning | No | No | No | Yes |
| Airway pressure release ventilation | No | Yes | No | No |
| Sodium bicarbonate intravenous infusion | Yes | Yes | No | Yes |
| Hours of mechanical ventilation prior to starting ECMO | 42 | 58 | 24 | 90 |
| ECMO retrieval | No | Yes | Yes | No |
ARDS = acute respiratory distress syndrome; ECMO = extracorporeal membrane oxygenation; FiO2 = fraction of inspired oxygen; PaO2 = partial pressure of oxygen; PaCO2 = partial pressure of carbon dioxide; PBW = predicted body weight; PEEP = positive end-expiratory pressure
Patients were considered for ECMO support if they had ARDS and satisfied one of the following three conditions: (i) a PaO2/FiO2 ratio < 80 on a PEEP of at least 15 cm H2O, (ii) a pH < 7.15 or PaCO2 > 80 mmHg despite an optimal lung protective ventilation strategy, or (iii) plateau pressures > 35 cm H2O despite optimal ventilatory management; and if they were within seven days of the onset of ARDS. If strict inclusion criteria were not met but rapid clinical deterioration was apparent, patients could be considered for aeromedical ECMO retrieval from distant sites within the centre’s catchment region at the discretion of the receiving intensivist and cardiothoracic surgeon.
Following informed consent by the substitute decision maker, venovenous peripheral ECMO cannulation was performed at the patient’s bedside under sterile conditions. One of two circuit configurations was selected at the cardiothoracic surgeon’s discretion (Table 1). The bi-femoral configuration consisted of drainage via the left common femoral vein (LCFV) with return via a long single-stage right common femoral vein cannula directed to the atrial-caval junction. The right internal jugular configuration consisted of a single 31Fr bicaval dual-lumen catheter (Avalon Laboratories, Rancho Dominguez, CA, USA) capable of drainage via the superior and inferior venae cavae and return via the right atrial inlet. In either configuration, an additional venous drainage catheter could be added at an available site to achieve adequate flows and oxygenation, if required. The circuit was connected to a BioMedicus® 540 centrifugal pump (Medtronic, Minneapolis, MN, USA) and a Maquet QUADROX-iD oxygenator/heat exchanger (MAQUET Cardiovascular, San Jose, CA, USA). The circuits were heparin coated and primed with Lactated Ringer’s solution 600 mL at room temperature. The cannula position was confirmed via transthoracic or transesophageal echocardiography and chest radiography. Following confirmation of adequate flow and favourable gas exchange on ECMO, inspired FiO2 was weaned and lung rest settings were applied to facilitate peak inspiratory pressures < 30 cm H2O, PEEP 10-15 cm H2O, and respiratory rate ~10 breaths·min−1, as described in the CESAR trial.9 Weaning from extracorporeal support was considered after a global assessment of disease resolution based on chest radiography, respiratory mechanics and work of breathing, and adequacy of gas exchange while delivering a lung protective ventilation strategy. At this point, a weaning trial of extracorporeal FiO2 and/or ECMO blood flow was initiated prior to release from ECMO.
Use of ECMO resulted in rapid improvements in oxygenation, ventilation, and acid-base status (Table 3). This facilitated reductions in tidal volume and PEEP which resulted in significantly lower airway pressures. Vasopressor requirements, hemodynamic parameters, and serum lactate levels also improved within 24 hr of ECMO support. In three cases, continuous venovenous hemodiafiltration was incorporated into the ECMO circuit due to acute kidney injury and volume overload. This facilitated achievement of a negative fluid balance and recruitment of the native lung. A timeline of in-hospital events is presented in Fig. 2. The duration of ECMO ranged from seven to 23 days (Table 4). Patients A, B, and D were relieved of mechanical ventilation at 18-25 days and were subsequently discharged with a Cerebral Performance Category 1 score obtained via chart review. Patient C sustained a 15-min cardiac arrest due to tension pneumothorax seven days after ECMO decannulation. Despite targeted temperature management, the patient experienced an anoxic cerebral injury that required prolonged rehabilitation. Three months later, the patient returned home and was independent with several activities of daily living. Patient outcomes, adverse events, and transfusion requirements are summarized in Table 4.
Table 3.
Therapeutic response to ECMO for patients A-D
| 1 hr prior to ECMO start | 24 hr following ECMO start | 48 hr following ECMO start | 24 hr prior to ECMO stop | 24 hr after ECMO stop | |
|---|---|---|---|---|---|
| ECMO flow (L·min−1) | - | 4.5 (4.2-5) | 4.3 (4.1-4.6) | 3 (2.9-3.1) | - |
| PaCO2 (mmHg) | 71 (52-77) | 42 (36-45) | 42 (35-52) | 40 (36-43) | 40 (34-55) |
| pH | 7.12 (7.1-7.2) | 7.40 (7.36-7.46) | 7.37 (7.32-7.44) | 7.37 (7.34-7.41) | 7.38 (7.22-7.41) |
| Sweep flow (L·min−1) | - | 5.5 (3.5-6.9) | 6.5 (3.5-8.8) | 2.8 (0.5-7.2) | - |
| Inspired FiO2 | 1.0 (1.0-1.0) | 0.70 (0.55-0.7) | 0.43 (0.4-0.56) | 0.55 (0.43-0.6) | 0.5 (0.42-0.65) |
| ECMO FiO2 | - | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) | 0.61 (0.21-1.0) | - |
| PaO2 (mmHg) | 60 (56-62) | 87 (70-116) | 74 (66-99) | 70 (60-103) | 87 (74-98) |
| PaO2/FiO2 | 60 (56-62) | 149 (100-180) | 176 (120-248) | 138 (111-205) | 169 (142-194) |
| Tidal volume (mL·kg−1 PBW) | 6.3 (5.1-7.5) | 5.2 (4.2-7) | 5.2 (3.4-7) | 7.4 (5.4-7.7) | 9.4 (7.4-11.1) |
| PEEP (cm H2O) | 15 (13-21) | 10 (10-12) | 10 (10-12) | 11(10-12) | 11(10-12) |
| PIP or Pplateau (cm H2O) | 43 (35-49) | 31 (27-35) | 25 (21-29) | 22 (18-27) | 23 (22-29) |
| Cumulative fluid balance (L) | 2.9 (−2.2-11.3) | 5 (−2.3-11) | −4.5 (−12.5-7.3) | −5.7 (−15-10.2) | |
| Norepinephrine dose (µg·kg−1·min−1) | 0.33 (0.1-0.6) | 0.01 (0-0.05) | 0.02 (0-0.08) | 0 (0-0.04) | 0 (0-0.02) |
| Vasopressin dose (U·hr−1) | 2.4 (2.4-2.9) | 0.6 (0-2.1) | 0 (0-1.8) | 0 (0-1.8) | 0 (0-1.8) |
| Mean arterial pressure (mmHg) | 68 (55-70) | 75 (70-82) | 76 (67-82) | 89 (83-94) | 78 (68-80) |
| Heart rate (beats·min−1) | 138 (102-146) | 91 (81-106) | 90 (74-116) | 95 (83-115) | 114 (99-127) |
| Patients receiving continuous venovenous hemodiafiltration (n) | 0 | 1 | 3 | 2 | 2 |
| Lactate (mmol·L−1) | 3.4 (3-4) | 2.5 (2-7.4) | 2.7 (2.2-6.2) | 1.6 (1.3-2.3) | 1.5 (1.3-1.9) |
| Platelets (number ×10−9·L−1) | 355 (201-505) | 246 (145-481) | 182 (143-303) | 66 (46-271) | 88 (75-181) |
AST = aspartate aminotransferase; ECMO = extracorporeal membrane oxygenation; FiO2 = fraction of inspired oxygen; PaCO2 = partial pressure of carbon dioxide; PaO2 = partial pressure of oxygen; PBW = predicted body weight; PEEP = positive end-expiratory pressure; PIP = peak inspiratory pressure; Pplateau = plateau pressure; SvO2 = central venous oxygen saturation
Fig. 2.
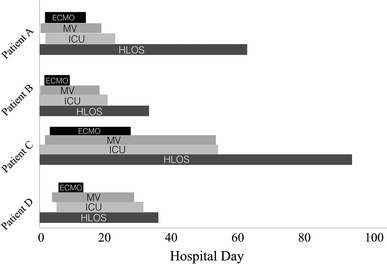
Timeline of events in hospital. ECMO = duration of extracorporeal membrane oxygenation; MV = duration of mechanical ventilation; ICU = intensive care unit length of stay; HLOS = hospital length of stay
Table 4.
Outcomes, adverse events, and transfusion requirements
| Patient A | Patient B | Patient C | Patient D | |
|---|---|---|---|---|
| Outcomes | ||||
| Hospital length of stay (days) | 58 | 31 | 87 | 33 |
| Duration of mechanical ventilation (days) | 19 | 18 | 52 | 25 |
| ECMO duration (days) | 12 | 8 | 23 | 7 |
| ICU length of stay (days) | 22 | 22 | 55 | 27 |
| Survival to hospital discharge | Yes | Yes | Yes | Yes |
| CPC status at hospital discharge | 1 | 1 | 2 | 1 |
| Adverse events | ||||
| Neurologic | - | Mycotic cerebral vasculitis | Anoxic cerebral injury | - |
| Respiratory | - | - | Tension pneumothorax | Re-intubation |
| Cardiovascular | Atrial dysrhythmias | - | - | Right ventricular dysfunction |
| Gastrointestinal | - | - | Upper gastro-intestinal bleeding | Upper gastro-intestinal bleeding |
| Transfusion requirements | ||||
| PRBC, units/ICU days | 0.05 | - | 0.29 | 0.48 |
| FFP (500 mL doses)/ICU days | 0.27 | - | - | - |
| Platelets, total* | - | - | - | 3 doses |
CPC = cerebral performance category (1 = good cerebral performance, 2 = moderate cerebral disability, 3 = severe cerebral disability, 4 = coma/vegetative state, 5 = brain death);22 ECMO = extracorporeal membrane oxygenation; FFP = fresh frozen plasma; ICU = intensive care unit; PRBC = packed red blood cells. *One adult dose is a pool of six whole blood-derived platelets
Discussion
Two reports have previously described attempts to rescue patients with refractory blastomycosis- related ARDS with ECMO.13,14 Resch et al. reported a case of a 33-yr-old previously healthy male with blastomycosis-related ARDS in Germany.13 Venovenous ECMO was initiated on the fourth day of illness; however, bilateral pneumothoraces and multi-system organ failure resulted in death on ECMO at day 14.13 Due to a delay in diagnosis, antifungal therapy was initiated only on the final days in the course of the illness. Dalton et al. reported a case of a 15-yr-old male with blastomycosis-related ARDS in which veno-arterial ECMO was initiated at day five of mechanical ventilation.14 Although amphotericin B was initiated after approximately seven days of hospital contact, the patient developed progressive pulmonary necrosis and sustained a cardiac arrest due to bilateral tension pneumothoraces on ECMO day 18.14 A single reported case of central veno-arterial ECMO for blastomycosis-related septic shock in a 12-yr-old was similarly unsuccessful.15
Post-mortem specimens from affected patients have shown the classic pathologic features of ARDS,2 but they have also shown severe necrosis, abscess formation, hemorrhagic cysts, and invasive parenchymal destruction.13,14 This raises the possibility that blastomycosis-related ARDS may be a uniquely severe disease entity due to virulence factors of an organism, pronounced host inflammatory response, or late recognition and treatment of the disease. It is possible that previous applications of ECMO in refractory blastomycosis-related ARDS failed due to delays in diagnosis and antimicrobial therapy or late initiation of extracorporeal support.13,14
In contrast to previous reports, this case series describes the successful application of ECMO as a rescue therapy in blastomycosis-related ARDS. All patients in this series had severely impaired gas exchange, reduced pulmonary compliance, and rapid deterioration despite respiratory support consistent with the standard of care. Extracorporeal membrane oxygenation facilitated improved gas exchange, as evidenced by increased PaO2/FiO2 ratios and normalization of pH and PaCO2, and allowed lung rest as shown by reductions in potentially injurious airway pressures. Although the therapy was resource intensive and necessitated prolonged admissions to hospital and the intensive care unit, in all four cases, ECMO decannulation was performed, mechanical ventilation was withdrawn, and the patients were discharged home with acceptable quality of life. These outcomes are exceptional given the uniquely high mortality of blastomycosis-related ARDS.
Indications for ECMO among patients with ARDS are evolving.7,8,16 In addition to providing rescue therapy for patients with refractory hypoxemia, hypercapnia, or acidosis, when instituted early, ECMO may prevent ventilator-induced lung injury by allowing de-escalation of mechanical ventilatory support.7,8 Observational trials of ECMO among patients with ARDS due to H1N1 virus have shown survival rates as high as 75%,10 though data from high-quality randomized controlled trials are lacking.16 With its inherently severe clinical course, blastomycosis-related ARDS has thus been considered a therapeutic target for ECMO. Maintaining a lung protective ventilation strategy may have greater clinical importance in this setting due to the pathologic severity of blastomycosis-related ARDS.2
Several factors may have contributed to the favourable outcomes in our cohort. First, diagnoses were made relatively early due to high clinical suspicion and experienced laboratory personnel. Accordingly, appropriate antimicrobial agents were instituted early in the clinical course. It is well established that the administration of early appropriate antimicrobials reduces mortality in septic shock.17 Second, ECMO support was initiated within 72 hr in all patients. Extracorporeal membrane oxygenation may confer greater therapeutic benefit in ARDS when initiated within seven days.8,18 In addition, three patients in this series received early systemic corticosteroids, a therapy which may limit the inflammatory response and possibly reduce mortality in blastomycosis-related ARDS,4 although controlled studies are lacking. Finally, all patients in our cohort were cannulated with venovenous ECMO configurations. Previous attempts at veno-arterial ECMO in blastomycosis-related ARDS may have been less efficacious due to reduced pulmonary blood flow in this configuration.14
The paucity of published attempts at ECMO rescue in this setting may reflect clinicians’ reluctance to apply ECMO in the context of septic shock and possible fungemia, both of which are considered relative contraindications to the use of ECMO.12,14 We observed a decline in vasopressor requirement within the first 24-48 hr of ECMO support. Although ECMO flows upon peripheral cannulation were 4-5 L·min−1, this would not have matched patients’ cardiac output prior to cannulation in the setting of septic shock,19 nor would ECMO be expected to deliver direct improvement in hemodynamics in a venovenous configuration. Thus, we speculate that ECMO indirectly improved hemodynamics by improving oxygen delivery to vital organs and restoring physiologic acid-base balance. Accordingly, ECMO may still have a therapeutic role in the setting of primary pulmonary disease with concomitant septic shock.
Our findings should be interpreted with several considerations. The previously reported mortality of blastomycosis-related ARDS largely reflects case series predating the ARMA study, representing an era in which lung protective ventilation was not standard practice.20 Thus, with modern ventilatory strategies and possibly prone positioning, it is possible that more patients with blastomycosis-related ARDS may be salvageable and not require ECMO rescue.20,21 Our case series was small, retrospective, and lacked a control group; however, no patients referred for ECMO for pulmonary blastomycosis were refused during the study period. Last, our aeromedical transport team provided several patients with early aggressive care and extracorporeal support. We acknowledge that our findings may lack generalizability because many centres lack such a service.
Conclusions
Extracorporeal membrane oxygenation may be an effective treatment modality for patients with blastomycosis-related ARDS and refractory hypoxemia despite optimal mechanical ventilation. Early application of ECMO and timely appropriate antimicrobial therapy may contribute to favourable patient outcomes. When blastomycosis-related ARDS is identified or suspected, transport to an ECMO-capable centre should be considered.
Acknowledgement
The authors gratefully acknowledge the contributions of Louise Dyck who provided quality assurance regarding the reporting of technical aspects of ECMO conduct and equipment.
Conflicts of interest
None declared.
Disclosures
No funding sources, commercial or non-commercial affiliations, associations, or consultancies apply to the corresponding author or author group.
Footnotes
This article is accompanied by an editorial. Please see Can J Anesth 2015; 62: this issue.
Author contributions
Joseph M. Bednarczyk, Anand Kumar, Shravan Kethireddy, Christopher W. White, Darren H. Freed, Rohit K. Singal, Dean Bell, and Syed Zaki Ahmed contributed to the conception and design of the study as well as data acquisition, analysis and interpretation. As the first author, Joseph M. Bednarczyk contributed to primary article drafting and project synthesis. Shravan Kethireddy, Christopher W. White, Darren H. Freed, Rohit K. Singal, Dean Bell, and Syed Zaki Ahmed contributed to drafting the article. Joseph M. Bednarczyk, Shravan Kethireddy, and Christopher W. White contributed to critical revisions. Darren H. Freed, Rohit K. Singal, Dean Bell, Syed Zaki Ahmed, and Anand Kumar contributed to substantial critical revisions as medical experts for intellectual content. Anand Kumar contributed to the overall project leadership. Bruce Light acted as senior project leader and supervisor, made significant contributions to project conception, design, and data interpretation, and revised and drafted the original manuscript for intellectual content.
References
- 1.Crampton TL, Light RB, Berg GM, et al. Epidemiology and clinical spectrum of blastomycosis diagnosed at Manitoba hospitals. Clin Infect Dis. 2002;34:1310–1316. doi: 10.1086/340049. [DOI] [PubMed] [Google Scholar]
- 2.Lemos LB, Baliga M, Guo M. Acute respiratory distress syndrome and blastomycosis: Presentation of nine cases and review of the literature. Ann Diagn Pathol. 2001;5:1–9. doi: 10.1053/adpa.2001.21473. [DOI] [PubMed] [Google Scholar]
- 3.Chapman SW, Lin AC, Hendricks KA, et al. Endemic blastomycosis in Mississippi: epidemiological and clinical studies. Semin Respir Infect. 1997;12:219–228. [PubMed] [Google Scholar]
- 4.Lahm T, Neese S, Thronburg AT, Ober MD, Sarosi G, Hage CA. Corticosteroids for blastomycosis-induced ARDS: a report of two cases and review of the literature. Chest. 2008;133:1478–1480. doi: 10.1378/chest.07-2778. [DOI] [PubMed] [Google Scholar]
- 5.Meyer KC, McManus EJ, Maki DG. Overwhelming pulmonary blastomycosis associated with the adult respiratory distress syndrome. N Engl J Med. 1993;329:1231–1236. doi: 10.1056/NEJM199310213291704. [DOI] [PubMed] [Google Scholar]
- 6.Vasquez JE, Mehta JB, Agrawal R, Sarubbi FA. Blastomycosis in northeast Tennessee. Chest. 1998;114:436–443. doi: 10.1378/chest.114.2.436. [DOI] [PubMed] [Google Scholar]
- 7.Del Sorbo L, Cypel M, Fan E. Extracorporeal life support for adults with severe acute respiratory failure. Lancet Respir Med. 2014;2:154–164. doi: 10.1016/S2213-2600(13)70197-8. [DOI] [PubMed] [Google Scholar]
- 8.Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med. 2011;365:1905–1914. doi: 10.1056/NEJMct1103720. [DOI] [PubMed] [Google Scholar]
- 9.Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 10.Australia and New-Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Davies A, Jones D, Bailey M, et al. Extracorporeal membrane oxygenation for, influenza A(H1N1) acute respiratory distress syndrome. JAMA. 2009;2009(302):1888–1895. doi: 10.1001/jama.2009.1535. [DOI] [PubMed] [Google Scholar]
- 11.Freed DH, Henzler D, White CW, et al. Extracorporeal lung support for patients who had severe respiratory failure secondary to influenza A (H1N1) 2009 infection in Canada. Can J Anesth. 2010;57:240–247. doi: 10.1007/s12630-009-9253-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang CT, Tsai YJ, Tsai PR, Ko WJ. Extracorporeal membrane oxygenation resuscitation in adult patients with refractory septic shock. J Thorac Cardiovasc Surg. 2012;146:1041–1046. doi: 10.1016/j.jtcvs.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Resch M, Kurz K, Schneider-Brachert W, et al. Extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS) in fulminant blastomycosis in Germany: BMJ Case Rep 2009; DOI: 10.1136/bcr.07.2008.0392. [DOI] [PMC free article] [PubMed]
- 14.Dalton HJ, Hertzog JH, Hannan RL, Vezza P, Hauser GJ. Extracorporeal membrane oxygenation for overwhelming Blastomyces dermatitidis pneumonia. Crit Care. 1999;3:91–94. doi: 10.1186/cc349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watson J, McDonald M. Central extracorporeal membrane oxygenation support for disseminated blastomycosis septic shock. Crit Care Med 2013; 41: 1298 (abstract).
- 16.Mitchell MD, Mikkelsen ME, Umscheid CA, Lee I, Fuchs BD, Halpern SD. A systematic review to inform institutional decisions about the use of extracorporeal membrane oxygenation during the H1N1 influenza pandemic. Crit Care Med. 2010;38:1398–1404. doi: 10.1097/CCM.0b013e3181de45db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 18.Patroniti N, Zangrillo A, Pappalardo F, et al. The Italian ECMO network experience during the 2009 influenza A(H1N1) pandemic: preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011;37:1447–1457. doi: 10.1007/s00134-011-2301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jellema WT, Wesseling KH, Groeneveld AB, Stoutenbeek CP, Thijs LG, van Lieshout JJ. Continuous cardiac output in septic shock by simulating a model of the aortic input impedance: a comparison with bolus injection thermodilution. Anesthesiology. 1999;90:1317–1328. doi: 10.1097/00000542-199905000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Anonymous. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000; 342: 1301-8. [DOI] [PubMed]
- 21.Guerin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 22.Ajam K, Gold LS, Beck SS, Damon S, Phelps R, Rea TD. Reliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resusc Emerg Med. 2011;19:38. doi: 10.1186/1757-7241-19-38. [DOI] [PMC free article] [PubMed] [Google Scholar]


