Abstract
This article summarizes the likely benefits of melatonin in the attenuation of COVID-19 based on its putative pathogenesis. The recent outbreak of COVID-19 has become a pandemic with tens of thousands of infected patients. Based on clinical features, pathology, the pathogenesis of acute respiratory disorder induced by either highly homogenous coronaviruses or other pathogens, the evidence suggests that excessive inflammation, oxidation, and an exaggerated immune response very likely contribute to COVID-19 pathology. This leads to a cytokine storm and subsequent progression to acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) and often death. Melatonin, a well-known anti-inflammatory and anti-oxidative molecule, is protective against ALI/ARDS caused by viral and other pathogens. Melatonin is effective in critical care patients by reducing vessel permeability, anxiety, sedation use, and improving sleeping quality, which might also be beneficial for better clinical outcomes for COVID-19 patients. Notably, melatonin has a high safety profile. There is significant data showing that melatonin limits virus-related diseases and would also likely be beneficial in COVID-19 patients. Additional experiments and clinical studies are required to confirm this speculation.
Keywords: COVID-19, SARS-CoV-2, Melatonin, Oxidation-reduction, Cytokines, Immunomodulation
Graphical abstract
Melatonin as a potential adjuvant treatment for COVID-19.
1. Introduction
Coronaviruses (CoVs) are RNA viruses infecting both human and animals; this infection involves the respiratory, gastrointestinal and central nervous system [1]. Severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) are infectious and lethal, and have caused thousands of deaths in the past two decades. The recent outbreak was discovered in Wuhan, China; this highly contagious disease has spread throughout China and other countries [2]. Although antiviral therapy, corticosteroid therapy and mechanical respiratory support have been applied, there is lack of a specific treatment for COVID-19 [2].
Melatonin (N-acetyl-5-methoxytryptamine) is a bioactive molecule with an array of health-promoting properties; melatonin has been successfully used to treat sleep disorders, delirium, atherosclerosis, respiratory disease and viral infections [3]. Previous research has documented the positive effects of melatonin in alleviating acute respiratory stress induced by virus, bacteria, radiation, etc. [[4], [5], [6]]. Herein, we review the evidence indicating that melatonin will have supportive adjuvant utility in treating COVID-19 induced pneumonia, acute lung injury (ALI) and acute respiratory distress syndrome (ARDS).
2. Pathogenesis of COVID-19 and the rationale for melatonin use
Patients with COVID-19 (who were infected by SARS-CoV-2) are reported to present with fever, dry cough, myalgia, fatigue, and diarrhea, etc. with symptoms varying somewhat with the patients' age. In some cases, the severe progression of the disease results in ALI/ARDS, respiratory failure, heart failure, sepsis, and sudden cardiac arrest within a few days [2,7]. The pathogenic examination of lung specimens from mild COVID-19 patients (who were retrospectively found to have COVID-19 at the time of lung cancer surgery) showed edema, proteinaceous exudate with globules, patchy inflammatory cellular infiltration and moderate formation of hyaline membranes [8]. In a postmortem assessment of a COVID-19 patient with severe ARDS, specimens of infected lungs demonstrated bilateral diffuse alveolar damage with edema, pneumocyte desquamation and hyaline membrane formation [9].
Though these pathological reports were reported in only a small number of cases, the findings do resemble the pathological features found in SARS- and MERS-induced pneumonia [10]. SARS-CoVs, MERS-CoVs and SARS-CoV-2 are classified in beta-coronavirus family members [11]. Recent published research suggests that SARS-CoV-2 shares 79.0% nucleotide identity to SARS-CoV and 51.8% identity to MERS-CoV [12], indicating a high genetic homology among SARS-CoV-2, MERS-CoV and SARS-CoV. In SARS-CoV and MERS-CoV infected animal model, marked inflammatory and immune responses may activate a “cytokine storm”, and apoptosis of epithelial cells and endothelial cells; subsequently, vascular leakage, abnormal T cell and macrophages responses ensue and induce ALI/ARDS or even death [13].
Based on genetic homology and pathologic features of the infected lung, we predicted that a cytokine storm also prevails in patients with COVID-19. In the blood of patients with COVID-19, there was a marked increase in interleukin 1β (IL-1β), interferon γ (IFN-γ), interferon-inducible protein 10 (IP-10), and monocyte chemoattractant protein 1 (MCP-1), as well as IL-4 and IL-10 when compared to that of SARS patients. This suggests some potential difference from SARS and MERS in the pathogenesis of coronavirus [2]. There is also a potential repressed immune function in COVID-19 patients with the hypo-albuminemia, lymphopenia, neutropenia, and decreased percentage of CD8+ T cell [2,7]. Recent reports suggest that in some COVID-19 patients, although being negative for the viral nucleic acid test, still sometimes present with a high level of inflammation. A clinical trial using certolizumab pegol (a TNF blocker) along with other anti-virus therapies may have beneficial effects in COVID-19 patients. Collectively, the finding indicates that inflammation is a major feature in COVID-19 patients. Thus, we hypothesize that excessive inflammation, depressed immune system, and an activate cytokine storm substantially contribute to the pathogenesis of COVID-19.
In the early stages of coronaviruses infection, dendritic cells and epithelial cells are activated and express a cluster of pro-inflammatory cytokines and chemokines including IL-1β, IL-2, IL-6, IL-8, both IFN-α/β, tumor necrosis factor (TNF), C—C motif chemokine 3 (CCL3), CCL5, CCL2, and IP-10, etc. These are under the control of immune system. Thus, the overproduction of these cytokines and chemokines contributes to the development in disease [[14], [15], [16]].
IL-10, produced by T-helper-2 (Th2), is antiviral, with an infection of coronaviruses leading to a marked decrease in this agent [17,18]. Interestingly, COVID-19 patients sometimes have a significantly elevated level of IL-10 [2]. Whether this is a feature of the COVID-19 infection or the result of medical treatment is unknown. The amplification of the inflammatory response would promote cellular apoptosis or necrosis of the affected cells, which would further fuel inflammation, followed by increasing permeability of blood vessels and the aberrant accumulation of inflammatory monocytes, macrophages and neutrophils in the lung alveoli [19]. This vicious circle would intensify the situation as the regulation of immune response is lost and cytokine storm is further activated, resulting in dire consequences.
This putative “cytokine storm” pathology associated with coronaviruses is also supported by experimental SARS-CoV models, one of which showed that the severity of ALI was accompanied by an elevated expression of inflammation-related genes rather than increased viral titers. In another case, the ablation of IFN-α/β receptor or the depletion of inflammatory monocytes/macrophages caused a marked rise in the survival rate of coronaviruses host without a change in viral load [19,20]. Both situations suggest a potential amplifying mechanism involved in CoV-induced ALI/ARDS regardless of the viral load. If a similar pathology also exists in COVID-19, the attenuation of the cytokine storm by targeting several key steps in the process could bring about improved outcomes.
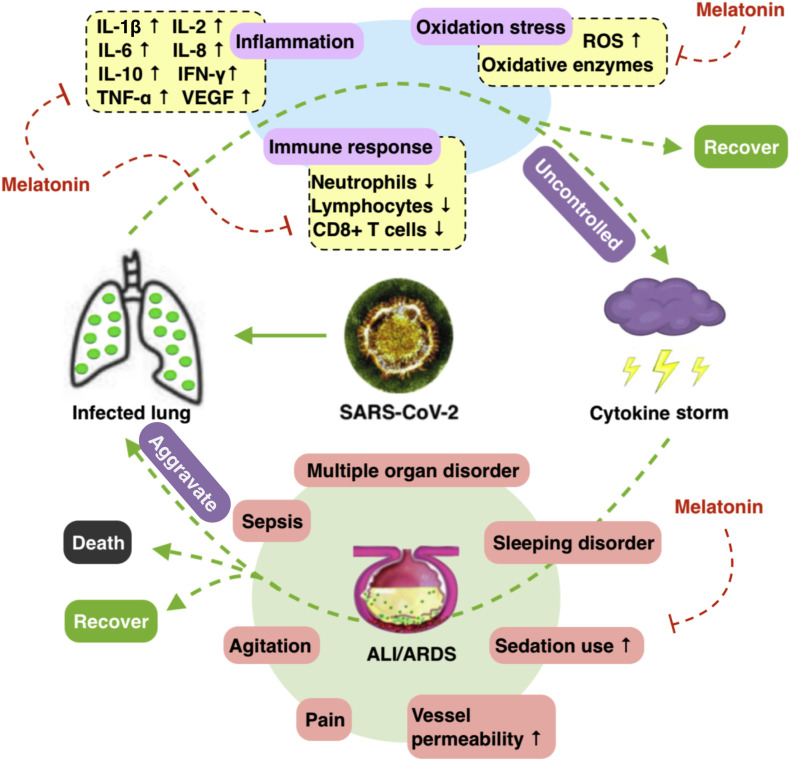
Melatonin is not viricidal but it has indirect anti-viral actions [3] due to its anti-inflammation, anti-oxidation and immune enhancing features [[21], [22], [23], [24]]. There are situations in which melatonin suppresses the features of viral infections. In mice whose central nervous system is infected by virus (e.g., encephalitis), the use of melatonin caused less viremia, reduced paralysis and death, and decreased virus load [25]. In previous respiratory syncytial virus models, melatonin caused down-regulation of acute lung oxidative injury, pro-inflammatory cytokine release and inflammatory cell recruitment. These findings, along with those recently summarized by Reiter et al. [3], support a rationale for melatonin use in viral diseases. Also, melatonin's anti-inflammation, anti-oxidation, immune enhancing actions supports its potential attenuation of COVID-19 infection (Fig. 1 ).
Fig. 1.
Pathogenesis of COVID-19 and potential adjuvant use of melatonin. We postulated that lungs infected by SARS-CoV-2, and a suppressed immune response, elevated inflammation and excessive oxidation stress proceed unabated, this results in the activation of the cytokine storm. ALI/ARDS may ensue, accompanied by a series of complications, the outcomes of which vary according to the severity of the disease. Melatonin may play a role of adjuvant medication in the regulation of immune system, inflammation and oxidation stress, and provide support for patients with ALI/ARDS and related complications. ALI: Acute lung injury; ARDS: Acute respiratory distress syndrome.
3. Melatonin & anti-inflammation
Melatonin exerts anti-inflammatory effects through various pathways. Sirtuin-1 (SIRT1) may mediate the anti-inflammatory actions of melatonin by inhibiting high mobility group boxechromosomal protein 1 (HMGB1), and thus down-regulating the polarization of macrophages towards the pro-inflammatory type [26]. In sepsis-induced ALI, the proper regulation of SIRT1 attenuates lung injury and inflammation, in which the application of melatonin might be beneficial [27]. Nuclear factor kappa-B (NF-κB) is closely associated with pro-inflammatory and pro-oxidative responses while being an inflammatory mediator in ALI. The anti-inflammatory effect of melatonin involves the suppression of NF-κB activation in ARDS [28,29]. Melatonin reportedly down-regulate NF-κB activation in T cells and lung tissue [30,31]. The stimulation of NF-E2-related factor 2 (Nrf2) is crucial in protecting lung from injury. In related studies, melatonin induces the up-regulation of Nrf2 with therapeutic effects in hepatoprotection, cardioprotection, etc. [32]. Whether Nrf2 is involved in the CoV-induced ALI remains unknown, but the close interaction of SIRT1, NF-κB and Nrf2 suggests their participation in the CoV-induced ALI/ARDS. As such, the data support the potential anti-inflammatory action of melatonin. Inflammation is commonly associated with an elevated production of cytokines and chemokines, while melatonin causes a reduction in the pro-inflammatory cytokines. TNF-α, IL-1β, IL-6, and IL-8, and an elevation in the level of anti-inflammatory cytokine IL-10 [33,34]. There may be, however, some concerns about the potential pro-inflammatory actions of melatonin when used in very high doses or under suppressed immune conditions where it may induce an increase production of pro-inflammatory cytokines, IL-1β, IL-2, IL-6, IL-12, TNF-α, and IFN-γ [35]. Conversely, in ALI infection models, melatonin presents with anti-inflammatory and protective action [6].
4. Melatonin & anti-oxidation
The anti-oxidative effect of melatonin cooperates with its anti-inflammatory actions by up-regulating anti-oxidative enzymes (e.g. superoxide dismutase), down-regulating pro-oxidative enzymes (e.g. nitric oxide synthase), and it may also interact directly with free radicals, functioning as free radical scavenger [3,4]. Viral infections and their replication constantly generate oxidized products. In a SARS-induced ALI model, the production of oxidized low density lipoprotein activates innate immune response by the overproduction of IL-6 alveolar macrophages via Toll-like receptor 4 (TLR4)/NF-kB signaling, thereby leading to ALI [36]. TLR4 is a receptor for the innate immune system, and it is also a therapeutic target for melatonin. In brain ischemia, gastritis and periodontitis disease models, melatonin has documented anti-inflammation actions via TLR4 signaling [[37], [38], [39]]. The anti-oxidative effect of melatonin has also been confirmed in ALI caused by radiation, sepsis and ischemia-reperfusion [4,40,41]. In ALI/ARDS patients, especially when the disease is advanced and in patients treated in intense care units (ICUs), severe inflammation, hypoxemia and mechanical ventilation with high oxygen concentrations inevitably increases oxidant generation locally and systematically [42,43]. Accordingly, we speculate that excessive oxidation also is likely involved in COVID-19. The extensive studies of Gitto et al. [44,45], who used melatonin to treat newborn infants with respiratory distress, has documented the anti-oxidant and anti-inflammatory actions of melatonin in the lung. Thus, it is likely that the application of melatonin would be beneficial in controlling the inflammation and oxidation in coronavirus infected subjects.
5. Melatonin & immunomodulation
When virus is inhaled and infects respiratory epithelial cells, dendritic cells phagocytose the virus and present antigens to T cells. Effector T cell function by killing the infected epithelial cells, and cytotoxic CD8+ T cells produce and release pro-inflammatory cytokines which induce cell apoptosis [46]. Both the pathogen (CoV) and cell apoptosis trigger and amplify the immune response. The exacerbation of cytokine production, excessive recruitment of immune cells and the uncontrollable epithelial damage generates a vicious circle for infection related ALI/ARDS [47]. The clinical characteristics of COVID-19 suggest that a reduced level of neutrophils, lymphocytes and CD8+ T cells in peripheral blood [7,48]. Melatonin exerts regulatory actions on the immune system and directly enhances the immune response by improving proliferation and maturation of natural killing cells, T and B lymphocytes, granulocytes and monocytes in both bone marrow and other tissues [49]. In macrophages, antigen presentation is also augmented after the application of melatonin, where the up-regulation of complement receptor 3, MHC class I and class II, and CD4 antigens were detected [50].
NOD-like receptor 3 (NLRP3) inflammasome is part of the innate immune response during lung infection. The pathogen, including a virus (CoVs has not yet been tested), triggers NLRP3 activation to amplify the inflammation. There is probably a balance of the protective and damaging actions of NLRP3 in the lung. Thus, in a mouse experiment, inhibition of NLRP3 in the early phase of infection increased mortality, whereas suppression of NLRP3 at the peak of infection allowed for a protective effect [51]. This supports the use of melatonin in ALI/ARDS when inflammation is most severe. Inflammasome NLRP3 is correlated to lung diseases caused by infection, including influenza A virus, syncytial virus, and bacteria [[51], [52], [53]]. The efficacy of melatonin in regulating NLRP3 has been proven in radiation-induced lung injury, allergic airway inflammation and oxygen-induced ALI and LPS-induced ALI models, in which melatonin reduced the infiltration of macrophages and neutrophils into the lung in ALI due to the inhibition of NLRP3 inflammasome [4,28,54,55].
6. Melatonin effects in cytokine levels in human
Although there is obviously no report related to the use of melatonin in COVID-19 patients, in subjects with other diseases and an increased level of inflammation, the application of melatonin showed promising results regarding the attenuation of circulating cytokines levels. In a randomized controlled trial, 8-week oral intake of 6 mg/d melatonin caused a significant decrease in serum levels of IL-6, TNF-α and hs-C-reactive protein (hs-CRP) in patients with diabetes mellitus and periodontitis [56]. In another trial of patients suffering with severe multiple sclerosis, orally 25 mg/d of melatonin for 6 months also promoted a significant reduction in serum concentrations of TNF-α, IL-6, IL-1β and lipoperoxides [57]. In the acute phase of inflammation, including during surgical stress [58], brain reperfusion [59], and coronary artery reperfusion [60], melatonin intake of 10 mg/d, 6 mg/d and 5 mg/d of melatonin for less than 5 days induced a reduced level of pro-inflammatory cytokines. A recent meta-analysis of a total of 22 randomized controlled trials suggested that a supplementary use of melatonin is associated with a significant reduction of TNF-α and IL-6 level [61]. This clinical evidence suggests that the use of melatonin as a supplement may effectively reduce the levels of circulating cytokines, and may potentially also lower pro-inflammatory cytokine levels in COVID-19 patients.
7. Melatonin & other supportive adjuvant effects
The integrity of the vascular endothelial barrier is crucial in the immunoregulation within alveoli. Severe inflammation and immune responses induce epithelial and endothelial cell apoptosis, as well as increasing the production of VEGF, which aggravates edema and the extravasation of the immune cells from blood vessels. Experimental evidence suggests that melatonin mediates the suppression of VEGF in vascular endothelial cells [62]. Based on clinical reports of COVID-19, patients with severe ALI/ARDS may also have an increased risk of sepsis and cardiac arrest [2]. Published reports indicate that the application of melatonin may ameliorate the septic shock via the NLRP3 pathway [63]. Specifically, melatonin may a have preventive effect against sepsis-induced renal injury, septic cardiomyopathy and liver injury [[64], [65], [66]]. It was also reported that melatonin had benefits in patients with myocardial infarction, cardiomyopathy, hypertensive heart diseases and pulmonary hypertension, and probably functions via the TLR4/survivor activating factor enhancement pathway [67]. Moreover, melatonin exerts neurological protection by reducing the cerebral inflammatory response, cerebral edema and brain-blood barrier permeability under a number of experimental conditions [68]. In the ICU, deep sedation is associated with increased long-term mortality, and the application of melatonin reduces sedation use and the frequency of pain, agitation, anxiety [69,70]. Also, a recent meta-analysis showed that melatonin improves sleep quality in patients in the ICU [71]. Thus, the rationale for the use of melatonin in COVID-19 patients not only focuses on the attenuation of the infection-induced respiratory disorders, but also on an overall improvement and prevention of patients' wellbeing and potential complications.
8. Melatonin & safety
When considering the use of melatonin to treat COVID-19, the safety of the melatonin is of utmost significance to consider. As reviewed previously, short-term use of melatonin is safe, even in those given high doses, and the reported adverse effects are limited to occasional dizziness, headache, nausea and sleepiness; in general melatonin's safety in humans is very high [72]. In clinical trials, doses of 3 mg, 6 mg and 10 mg of melatonin oral intake by patients in ICU showed satisfactory safety when compared to placebo [70,73,74]. Also, even when melatonin was given to humans at dose of 1 g/d for a month, there were no adverse reports of the treatment [75]. Finally, there were no adverse effects recorded after the use of melatonin in ALI/ARDS animal studies [3,4,28]. While the safety of melatonin has been verified in many human studies, its effect when given to COVID-19 patients should be carefully monitored despite the very high safety profile of melatonin.
9. Conclusion
The possible beneficial effects of melatonin as adjuvant use in COVID-19 in anti-inflammation, anti-oxidation, immune response regulation has been repeatedly demonstrated in respiratory disorder models induced by infections and associated complications. Melatonin has a high safety profile. Although the direct evidence of melatonin application in COVID-19 is unclear, both its use in experimental animal models and in studies on humans has continuously documented its efficacy and safety and its use by COVID-19 patients predictably would be highly beneficial.
CRediT authorship contribution statement
Rui Zhang:Resources, Writing - original draft.Xuebin Wang:Writing - original draft.Leng Ni:Writing - review & editing, Supervision.Xiao Di:Visualization.Baitao Ma:Writing - review & editing.Shuai Niu:Resources.Changwei Liu:Conceptualization, Supervision.Russel J. Reiter:Writing - review & editing.
Acknowledgments
Acknowledgement
We thank all the doctors, nurses, and researchers who have fought against the virus on the frontline of 2019-nCoV epidemic. We thank everyone who has given great and selfless support to the fight against this deadly infection. This research did not receive a specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
References
- 1.Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reiter R.J., Ma Q., Sharma R. Treatment of Ebola and other infectious diseases: melatonin “goes viral”. Melatonin Res. 2020;3:43–57. doi: 10.32794/mr11250047. [DOI] [Google Scholar]
- 4.Wu X., Ji H., Wang Y., Gu C., Gu W., Hu L., Zhu L. Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 axis. Oxidative Med. Cell. Longev. 2019;2019:4087298. doi: 10.1155/2019/4087298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yip H.-K., Chang Y.-C., Wallace C.G., Chang L.-T., Tsai T.-H., Chen Y.-L., Chang H.-W., Leu S., Zhen Y.-Y., Tsai C.-Y., Yeh K.-H., Sun C.-K., Yen C.-H. Melatonin treatment improves adipose-derived mesenchymal stem cell therapy for acute lung ischemia-reperfusion injury. J. Pineal Res. 2013;54:207–221. doi: 10.1111/jpi.12020. [DOI] [PubMed] [Google Scholar]
- 6.Huang S.-H., Cao X.-J., Liu W., Shi X.-Y., Wei W. Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice. J. Pineal Res. 2010;48:109–116. doi: 10.1111/j.1600-079X.2009.00733.x. [DOI] [PubMed] [Google Scholar]
- 7.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (London, England) 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tian S., Hu W., Niu L., Liu H., Xu H., Xiao S. Preprints (Www.Preprints.Org); 2020. Pulmonary Pathology of Early Phase SARSCoV-2 Pneumonia. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.-S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30076-X. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu J., Zheng X., Tong Q., Li W., Wang B., Sutter K., Trilling M., Lu M., Dittmer U., Yang D. Overlapping and discrete aspects of the pathology and pathogenesis of the emerging human pathogenic coronaviruses SARS-CoV, MERS-CoV, and 2019-nCoV. J. Med. Virol. 2020 doi: 10.1002/jmv.25709. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 2020 doi: 10.1016/j.micinf.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ren L.-L., Wang Y.-M., Wu Z.-Q., Xiang Z.-C., Guo L., Xu T., Jiang Y.-Z., Xiong Y., Li Y.-J., Li X.-W., Li H., Fan G.-H., Gu X.-Y., Xiao Y., Gao H., Xu J.-Y., Yang F., Wang X.-M., Wu C., Chen L., Liu Y.-W., Liu B., Yang J., Wang X.-R., Dong J., Li L., Huang C.-L., Zhao J.-P., Hu Y., Cheng Z.-S., Liu L.-L., Qian Z.-H., Qin C., Jin Q., Cao B., Wang J.-W. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin. Med. J. 2020 doi: 10.1097/CM9.0000000000000722. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Channappanavar R., Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin. Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheung C.Y., Poon L.L.M., Ng I.H.Y., Luk W., Sia S.-F., Wu M.H.S., Chan K.-H., Yuen K.-Y., Gordon S., Guan Y., Peiris J.S.M. Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: possible relevance to pathogenesis. J. Virol. 2005;79:7819–7826. doi: 10.1128/JVI.79.12.7819-7826.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Law H.K.W., Cheung C.Y., Ng H.Y., Sia S.F., Chan Y.O., Luk W., Nicholls J.M., Peiris J.S.M., Lau Y.L. Chemokine up-regulation in SARS-coronavirus-infected, monocyte-derived human dendritic cells. Blood. 2005;106:2366–2374. doi: 10.1182/blood-2004-10-4166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu H., Zhou J., Wong B.H.-Y., Li C.C., Chan J.F.-W., Cheng Z.-S., Yang D., Wang D., Lee A.C.-Y., Li C.C., Yeung M.-L., Cai J.-P., Chan I.H.-Y., Ho W.-K., To K.K.-W., Zheng B.-J., Yao Y., Qin C., Yuen K.-Y. Middle east respiratory syndrome coronavirus efficiently infects human primary T lymphocytes and activates the extrinsic and intrinsic apoptosis pathways. J. Infect. Dis. 2016;213:904–914. doi: 10.1093/infdis/jiv380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fehr A.R., Channappanavar R., Jankevicius G., Fett C., Zhao J., Athmer J., Meyerholz D.K., Ahel I., Perlman S. The conserved coronavirus macrodomain promotes virulence and suppresses the innate immune response during severe acute respiratory syndrome coronavirus infection. MBio. 2016;7 doi: 10.1128/mBio.01721-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chien J.-Y., Hsueh P.-R., Cheng W.-C., Yu C.-J., Yang P.-C. Temporal changes in cytokine/chemokine profiles and pulmonary involvement in severe acute respiratory syndrome. Respirology (Carlton, Vic.) 2006;11:715–722. doi: 10.1111/j.1440-1843.2006.00942.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Channappanavar R., Fehr A.R., Vijay R., Mack M., Zhao J., Meyerholz D.K., Perlman S. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smits S.L., de Lang A., van den Brand J.M.A., Leijten L.M., van IJcken W.F., Eijkemans M.J.C., van Amerongen G., Kuiken T., Andeweg A.C., Osterhaus A.D.M.E., Haagmans B.L. Exacerbated innate host response to SARS-CoV in aged non-human primates. PLoS Pathog. 2010;6 doi: 10.1371/journal.ppat.1000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Junaid A., Tang H., van Reeuwijk A., Abouleila Y., Wuelfroth P., van Duinen V., Stam W., van Zonneveld A.J., Hankemeier T., Mashaghi A. Ebola hemorrhagic shock syndrome-on-a-chip. IScience. 2020;23 doi: 10.1016/j.isci.2019.100765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boga J.A., Coto-Montes A., Rosales-Corral S.A., Tan D.-X., Reiter R.J. Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”? Rev. Med. Virol. 2012;22:323–338. doi: 10.1002/rmv.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson G., Maes M., Markus R.P., Rodriguez M. Ebola virus: melatonin as a readily available treatment option. J. Med. Virol. 2015;87:537–543. doi: 10.1002/jmv.24130. [DOI] [PubMed] [Google Scholar]
- 24.Reiter R.J., Ma Q., Sharma R. Melatonin in mitochondria: mitigating clear and present dangers. Physiology (Bethesda) 2020;35:86–95. doi: 10.1152/physiol.00034.2019. [DOI] [PubMed] [Google Scholar]
- 25.Ben-Nathan D., Maestroni G.J., Lustig S., Conti A. Protective effects of melatonin in mice infected with encephalitis viruses. Arch. Virol. 1995;140:223–230. doi: 10.1007/bf01309858. [DOI] [PubMed] [Google Scholar]
- 26.Hardeland R. Melatonin and inflammation-story of a double-edged blade. J. Pineal Res. 2018;65:e12525. doi: 10.1111/jpi.12525. [DOI] [PubMed] [Google Scholar]
- 27.Wang Q.-L., Yang L., Peng Y., Gao M., Yang M.-S., Xing W., Xiao X.-Z. Ginsenoside Rg1 regulates SIRT1 to ameliorate sepsis-induced lung inflammation and injury via inhibiting endoplasmic reticulum stress and inflammation. Mediat. Inflamm. 2019;2019:6453296. doi: 10.1155/2019/6453296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun C.-K., Lee F.-Y., Kao Y.-H., Chiang H.-J., Sung P.-H., Tsai T.-H., Lin Y.-C., Leu S., Wu Y.-C., Lu H.-I., Chen Y.-L., Chung S.-Y., Su H.-L., Yip H.-K. Systemic combined melatonin-mitochondria treatment improves acute respiratory distress syndrome in the rat. J. Pineal Res. 2015;58:137–150. doi: 10.1111/jpi.12199. [DOI] [PubMed] [Google Scholar]
- 29.Ling Y., Li Z.-Z., Zhang J.-F., Zheng X.-W., Lei Z.-Q., Chen R.-Y., Feng J.-H. MicroRNA-494 inhibition alleviates acute lung injury through Nrf2 signaling pathway via NQO1 in sepsis-associated acute respiratory distress syndrome. Life Sci. 2018;210:1–8. doi: 10.1016/j.lfs.2018.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Pedrosa A.M. da C., Weinlich R., Mognol G.P., Robbs B.K., Viola J.P. de B., Campa A., Amarante-Mendes G.P. Melatonin protects CD4+ T cells from activation-induced cell death by blocking NFAT-mediated CD95 ligand upregulation. J. Immunol (Baltimore, Md.: 1950) 2010;184:3487–3494. doi: 10.4049/jimmunol.0902961. [DOI] [PubMed] [Google Scholar]
- 31.Shang Y., Xu S.-P., Wu Y., Jiang Y.-X., Wu Z.-Y., Yuan S.-Y., Yao S.-L. Melatonin reduces acute lung injury in endotoxemic rats. Chin. Med. J. 2009;122:1388–1393. [PubMed] [Google Scholar]
- 32.Ahmadi Z., Ashrafizadeh M. Melatonin as a potential modulator of Nrf2. Fund. Clin. Pharmacol. 2020;34:11–19. doi: 10.1111/fcp.12498. [DOI] [PubMed] [Google Scholar]
- 33.Habtemariam S., Daglia M., Sureda A., Selamoglu Z., Gulhan M.F., Nabavi S.M. Melatonin and respiratory diseases: a review. Curr. Top. Med. Chem. 2017;17:467–488. doi: 10.2174/1568026616666160824120338. [DOI] [PubMed] [Google Scholar]
- 34.Hardeland R. Aging, melatonin, and the pro- and anti-inflammatory networks. Int. J. Mol. Sci. 2019;20 doi: 10.3390/ijms20051223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carrascal L., Nunez-Abades P., Ayala A., Cano M. Role of melatonin in the inflammatory process and its therapeutic potential. Curr. Pharm. Design. 2018;24:1563–1588. doi: 10.2174/1381612824666180426112832. [DOI] [PubMed] [Google Scholar]
- 36.Imai Y., Kuba K., Neely G.G., Yaghubian-Malhami R., Perkmann T., van Loo G., Ermolaeva M., Veldhuizen R., Leung Y.H.C., Wang H., Liu H., Sun Y., Pasparakis M., Kopf M., Mech C., Bavari S., Peiris J.S.M., Slutsky A.S., Akira S., Hultqvist M., Holmdahl R., Nicholls J., Jiang C., Binder C.J., Penninger J.M. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133:235–249. doi: 10.1016/j.cell.2008.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao Y., Wang H., Chen W., Chen L., Liu D., Wang X., Wang X. Melatonin attenuates white matter damage after focal brain ischemia in rats by regulating the TLR4/NF-kappaB pathway. Brain Res. Bull. 2019;150:168–178. doi: 10.1016/j.brainresbull.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 38.Luo J., Song J., Zhang H., Zhang F., Liu H., Li L., Zhang Z., Chen L., Zhang M., Lin D., Lin M., Zhou R. Melatonin mediated Foxp3-downregulation decreases cytokines production via the TLR2 and TLR4 pathways in H. pylori infected mice. Int. Immunopharmacol. 2018;64:116–122. doi: 10.1016/j.intimp.2018.08.034. [DOI] [PubMed] [Google Scholar]
- 39.Renn T.-Y., Huang Y.-K., Feng S.-W., Wang H.-W., Lee W.-F., Lin C.-T., Burnouf T., Chen L.-Y., Kao P.-F., Chang H.-M. Prophylactic supplement with melatonin successfully suppresses the pathogenesis of periodontitis through normalizing RANKL/OPG ratio and depressing the TLR4/MyD88 signaling pathway. J. Pineal Res. 2018;64 doi: 10.1111/jpi.12464. [DOI] [PubMed] [Google Scholar]
- 40.Chen H.-H., Chang C.-L., Lin K.-C., Sung P.-H., Chai H.-T., Zhen Y.-Y., Chen Y.-C., Wu Y.-C., Leu S., Tsai T.-H., Chen C.-H., Chang H.-W., Yip H.-K. Melatonin augments apoptotic adipose-derived mesenchymal stem cell treatment against sepsis-induced acute lung injury. Am. J. Transl. Res. 2014;6:439–458. [PMC free article] [PubMed] [Google Scholar]
- 41.Wang M.-L., Wei C.-H., Wang W.-D., Wang J.-S., Zhang J., Wang J.-J. Melatonin attenuates lung ischaemia-reperfusion injury via inhibition of oxidative stress and inflammation. Interact. Cardiov. Th. 2018;26:761–767. doi: 10.1093/icvts/ivx440. [DOI] [PubMed] [Google Scholar]
- 42.Tamura D.Y., Moore E.E., Partrick D.A., Johnson J.L., Offner P.J., Silliman C.C. Acute hypoxemia in humans enhances the neutrophil inflammatory response. Shock (Augusta, Ga.) 2002;17:269–273. doi: 10.1097/00024382-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Sarma J.V., Ward P.A. Oxidants and redox signaling in acute lung injury. Compr. Physiol. 2011;1:1365–1381. doi: 10.1002/cphy.c100068. [DOI] [PubMed] [Google Scholar]
- 44.Gitto E., Reiter R.J., Sabatino G., Buonocore G., Romeo C., Gitto P., Buggé C., Trimarchi G., Barberi I. Correlation among cytokines, bronchopulmonary dysplasia and modality of ventilation in preterm newborns: improvement with melatonin treatment. J. Pineal Res. 2005;39:287–293. doi: 10.1111/j.1600-079X.2005.00251.x. [DOI] [PubMed] [Google Scholar]
- 45.Gitto E., Reiter R.J., Cordaro S.P., La R.M., Chiurazzi P., Trimarchi G., Gitto P., Calabrò M.P., Barberi I. Oxidative and inflammatory parameters in respiratory distress syndrome of preterm newborns: beneficial effects of melatonin. Am. J. Perinatol. 2004;21:209–216. doi: 10.1055/s-2004-828610. [DOI] [PubMed] [Google Scholar]
- 46.Rogers M.C., Williams J.V. Quis Custodiet Ipsos Custodes? Regulation of cell-mediated immune responses following viral lung infections. Annu. Rev. Virol. 2018;5:363–383. doi: 10.1146/annurev-virology-092917-043515. [DOI] [PubMed] [Google Scholar]
- 47.Yang C.-Y., Chen C.-S., Yiang G.-T., Cheng Y.-L., Yong S.-B., Wu M.-Y., Li C.-J. New insights into the immune molecular regulation of the pathogenesis of acute respiratory distress syndrome. Int. J. Mol. Sci. 2018;19 doi: 10.3390/ijms19020588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J., Wang Z., Li J., Li J., Feng C., Zhang Z., Wang L., Peng L., Chen L., Qin Y., Zhao D., Tan S., Yin L., Xu J., Zhou C., Jiang C., Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 2020 doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller S.C., Pandi-Perumal S.R., Esquifino A.I., Cardinali D.P., Maestroni G.J.M. The role of melatonin in immuno-enhancement: potential application in cancer. Int. J. Exp. Pathol. 2006;87:81–87. doi: 10.1111/j.0959-9673.2006.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaur C., Ling E.A. Effects of melatonin on macrophages/microglia in postnatal rat brain. J. Pineal Res. 1999;26:158–168. doi: 10.1111/j.1600-079x.1999.tb00578.x. [DOI] [PubMed] [Google Scholar]
- 51.Tate M.D., Ong J.D.H., Dowling J.K., McAuley J.L., Robertson A.B., Latz E., Drummond G.R., Cooper M.A., Hertzog P.J., Mansell A. Reassessing the role of the NLRP3 inflammasome during pathogenic influenza a virus infection via temporal inhibition. Sci. Rep. 2016;6:27912. doi: 10.1038/srep27912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shen C., Zhang Z., Xie T., Ji J., Xu J., Lin L., Yan J., Kang A., Dai Q., Dong Y., Shan J., Wang S., Zhao X. Rhein suppresses lung inflammatory injury induced by human respiratory syncytial virus through inhibiting NLRP3 inflammasome activation via NF-kappaB pathway in mice. Front. Pharmacol. 2019;10:1600. doi: 10.3389/fphar.2019.01600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mei S.H.J., McCarter S.D., Deng Y., Parker C.H., Liles W.C., Stewart D.J. Prevention of LPS-induced acute lung injury in mice by mesenchymal stem cells overexpressing angiopoietin 1. PLoS Med. 2007;4:e269. doi: 10.1371/journal.pmed.0040269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu H.-M., Xie Q.-M., Zhao C.-C., Xu J., Fan X.-Y., Fei G.-H. Melatonin biosynthesis restored by CpG oligodeoxynucleotides attenuates allergic airway inflammation via regulating NLRP3 inflammasome. Life Sci. 2019;239:117067. doi: 10.1016/j.lfs.2019.117067. [DOI] [PubMed] [Google Scholar]
- 55.Zhang Y., Li X.X., Grailer J.J., Wang N., Wang M., Yao J., Zhong R., Gao G.F., Ward P.A., Tan D.-X., Li X.X. Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J. Pineal Res. 2016;60:405–414. doi: 10.1111/jpi.12322. [DOI] [PubMed] [Google Scholar]
- 56.Bazyar H., Gholinezhad H., Moradi L., Salehi P., Abadi F., Ravanbakhsh M., Zare Javid A. The effects of melatonin supplementation in adjunct with non-surgical periodontal therapy on periodontal status, serum melatonin and inflammatory markers in type 2 diabetes mellitus patients with chronic periodontitis: a double-blind, placebo-controlled trial. Inflammopharmacology. 2019;27:67–76. doi: 10.1007/s10787-018-0539-0. [DOI] [PubMed] [Google Scholar]
- 57.Sanchez-Lopez A.L., Ortiz G.G., Pacheco-Moises F.P., Mireles-Ramirez M.A., Bitzer-Quintero O.K., Delgado-Lara D.L.C., Ramirez-Jirano L.J., Velazquez-Brizuela I.E. Efficacy of melatonin on serum pro-inflammatory cytokines and oxidative stress markers in relapsing remitting multiple sclerosis. Arch. Med. Res. 2018;49:391–398. doi: 10.1016/j.arcmed.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 58.Kucukakin B., Lykkesfeldt J., Nielsen H.J., Reiter R.J., Rosenberg J., Gogenur I. Utility of melatonin to treat surgical stress after major vascular surgery–a safety study. J. Pineal Res. 2008;44:426–431. doi: 10.1111/j.1600-079X.2007.00545.x. [DOI] [PubMed] [Google Scholar]
- 59.Zhao Z., Lu C., Li T., Wang W., Ye W., Zeng R., Ni L., Lai Z., Wang X., Liu C. The protective effect of melatonin on brain ischemia and reperfusion in rats and humans: in vivo assessment and a randomized controlled trial. J. Pineal Res. 2018;65:e12521. doi: 10.1111/jpi.12521. [DOI] [PubMed] [Google Scholar]
- 60.Shafiei E., Bahtoei M., Raj P., Ostovar A., Iranpour D., Akbarzadeh S., Shahryari H., Anvaripour A., Tahmasebi R., Netticadan T., Movahed A. Effects of N-acetyl cysteine and melatonin on early reperfusion injury in patients undergoing coronary artery bypass grafting: a randomized, open-labeled, placebo-controlled trial. Medicine. 2018;97:e11383. doi: 10.1097/MD.0000000000011383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zarezadeh M., Khorshidi M., Emami M., Janmohammadi P., Kord-Varkaneh H., Mousavi S.M., Mohammed S.H., Saedisomeolia A., Alizadeh S. Melatonin supplementation and pro-inflammatory mediators: a systematic review and meta-analysis of clinical trials. Eur. J. Nutr. 2019 doi: 10.1007/s00394-019-02123-0. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 62.Cheng J., Yang H.-L., Gu C.-J., Liu Y.-K., Shao J., Zhu R., He Y.-Y., Zhu X.-Y., Li M.-Q. Melatonin restricts the viability and angiogenesis of vascular endothelial cells by suppressing HIF-1alpha/ROS/VEGF. Int. J. Mol. Med. 2019;43:945–955. doi: 10.3892/ijmm.2018.4021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Volt H., Garcia J.A., Doerrier C., Diaz-Casado M.E., Guerra-Librero A., Lopez L.C., Escames G., Tresguerres J.A., Acuna-Castroviejo D. Same molecule but different expression: aging and sepsis trigger NLRP3 inflammasome activation, a target of melatonin. J. Pineal Res. 2016;60:193–205. doi: 10.1111/jpi.12303. [DOI] [PubMed] [Google Scholar]
- 64.Dai W., Huang H., Si L., Hu S., Zhou L., Xu L., Deng Y. Melatonin prevents sepsis-induced renal injury via the PINK1/Parkin1 signaling pathway. Int. J. Mol. Med. 2019;44:1197–1204. doi: 10.3892/ijmm.2019.4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang J., Wang L., Xie W., Hu S., Zhou H., Zhu P., Zhu H. Melatonin attenuates ER stress and mitochondrial damage in septic cardiomyopathy: a new mechanism involving BAP31 upregulation and MAPK-ERK pathway. J. Cell. Physiol. 2020;235:2847–2856. doi: 10.1002/jcp.29190. [DOI] [PubMed] [Google Scholar]
- 66.Chen J., Xia H., Zhang L., Zhang H., Wang D., Tao X. Protective effects of melatonin on sepsis-induced liver injury and dysregulation of gluconeogenesis in rats through activating SIRT1/STAT3 pathway. Biomed. Pharmacother. 2019;117:109150. doi: 10.1016/j.biopha.2019.109150. [DOI] [PubMed] [Google Scholar]
- 67.Nduhirabandi F., Lamont K., Albertyn Z., Opie L.H., Lecour S. Role of toll-like receptor 4 in melatonin-induced cardioprotection. J. Pineal Res. 2016;60:39–47. doi: 10.1111/jpi.12286. [DOI] [PubMed] [Google Scholar]
- 68.Tordjman S., Chokron S., Delorme R., Charrier A., Bellissant E., Jaafari N., Fougerou C. Melatonin: pharmacology, functions and therapeutic benefits. Curr. Neuropharmacol. 2017;15:434–443. doi: 10.2174/1570159X14666161228122115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lewandowska K., Malkiewicz M.A., Sieminski M., Cubala W.J., Winklewski P.J., Medrzycka-Dabrowska W.A. The role of melatonin and melatonin receptor agonist in the prevention of sleep disturbances and delirium in intensive care unit - a clinical review. Sleep Med. 2020;69:127–134. doi: 10.1016/j.sleep.2020.01.019. [DOI] [PubMed] [Google Scholar]
- 70.Mistraletti G., Umbrello M., Sabbatini G., Miori S., Taverna M., Cerri B., Mantovani E.S., Formenti P., Spanu P., D’Agostino A., Salini S., Morabito A., Fraschini F., Reiter R.J., Iapichino G. Melatonin reduces the need for sedation in ICU patients: a randomized controlled trial. Minerva Anestesiol. 2015;81:1298–1310. [PubMed] [Google Scholar]
- 71.Lewis S.R., Pritchard M.W., Schofield-Robinson O.J., Alderson P., Smith A.F. Melatonin for the promotion of sleep in adults in the intensive care unit. The Cochrane Database of Syst. Rev. 2018;5:CD012455. doi: 10.1002/14651858.CD012455.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Andersen L.P.H., Gogenur I., Rosenberg J., Reiter R.J. The safety of melatonin in humans. Clin. Drug Investig. 2016;36:169–175. doi: 10.1007/s40261-015-0368-5. [DOI] [PubMed] [Google Scholar]
- 73.Bourne R.S., Mills G.H., Minelli C. Melatonin therapy to improve nocturnal sleep in critically ill patients: encouraging results from a small randomised controlled trial. Crit. Care (London, England). 2008;12:R52. doi: 10.1186/cc6871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mistraletti G., Sabbatini G., Taverna M., Figini M.A., Umbrello M., Magni P., Ruscica M., Dozio E., Esposti R., DeMartini G., Fraschini F., Rezzani R., Reiter R.J., Iapichino G. Pharmacokinetics of orally administered melatonin in critically ill patients. J. Pineal Res. 2010;48:142–147. doi: 10.1111/j.1600-079X.2009.00737.x. [DOI] [PubMed] [Google Scholar]
- 75.Nordlund J.J., Lerner A.B. The effects of oral melatonin on skin color and on the release of pituitary hormones. J. Clin. Endocrinol. Metab. 1977;45:768–774. doi: 10.1210/jcem-45-4-768. [DOI] [PubMed] [Google Scholar]