Abstract
Autophagy is an evolutionarily conserved process central to host metabolism. Among its major functions are conservation of energy during starvation, recycling organelles, and turnover of long-lived proteins. Besides, autophagy plays a critical role in removing intracellular pathogens and very likely represents a primordial intrinsic cellular defence mechanism. More recent findings indicate that it has not only retained its ability to degrade intracellular pathogens, but also functions to augment and fine tune antiviral immune responses. Interestingly, viruses have also co-evolved strategies to manipulate this pathway and use it to their advantage. Particularly intriguing is infection-dependent activation of autophagy with positive stranded (+)RNA virus infections, which benefit from the pathway without succumbing to lysosomal degradation. In this review we summarise recent data on viral manipulation of autophagy, with a particular emphasis on +RNA viruses and highlight key unanswered questions in the field that we believe merit further attention.
Keywords: Autophagy, Positive stranded RNA virus, Viral subversion strategies
1. Introduction
RNA viruses have evolutionarily constrained genome sizes. At the same time they have co-evolved efficient means to manipulate host cellular processes to acquire nutrients while evading immune detection. Multifunctional viral proteins, molecular mimicry of host components, and the intrinsically high mutagenicity of their RNA genome converge to dysregulate host cellular pathways, and exploit metabolic processes to their advantage. One such target is the autophagy machinery. While this cellular degradative process has been historically described to restrict intracellular pathogens including bacteria, parasites and viruses, many have evolved mechanisms to circumvent and even actively benefit from it.
Autophagy is initiated by sequestration of cytoplasmic proteins and damaged organelles into crescent-shaped double-membrane vesicles known as isolation membranes, long-debated on their membrane source [1]. The best understood trigger for induction of autophagy is amino acid deprivation, whereby autophagy related proteins (ATGs) are recruited to nucleate the isolation membrane, which forms a cup-shaped phagophore. Current consensus on the source of autophagosomal membranes is the endoplasmic reticulum [2]. Once contents are captured, the immature isolation membranes expand to forming autophagosomes, which subsequently fuse with lysosomes, thus forming autolysosomes. The contents undergo degradation within the autolysosomes to enable recycling during starvation. About 30 genes have been reported to participate in the process of autophagosomal degradation.
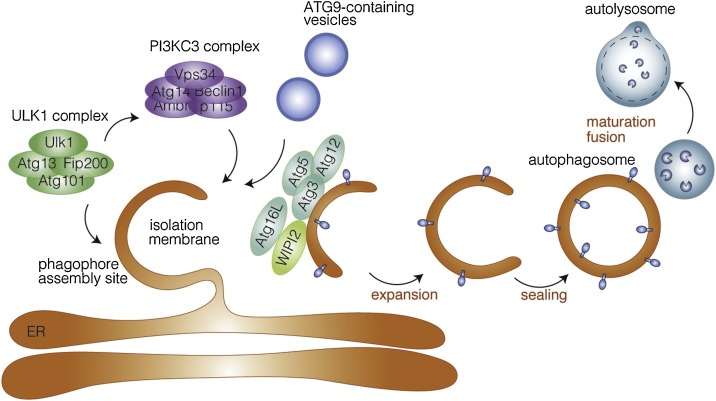
The core autophagy proteins are broadly categorised into five complexes: (i) the Unc-51 Like Kinase 1 (ULK1) complex, (ii) ATG9, (iii) the class III PI3K complex, (iv) WD repeat domain phosphoinositide-interacting proteins (WIPI), and (v) Ubiquitin-like ATG12 and ATG8 complexes. Although a mechanistic understanding of the process is currently incomplete, formation of phagophore is believed to involve a cooperative activity of the ULK1 and PI3K complexes, along with local phosphatidylinositol synthesis. These activities are followed by recruitment of ATG9-containing vesicles to phagophore assembly sites, which results in membrane expansion to form the autophagosomes (Fig. 1 ). Detailed analyses of the known regulatory mechanisms have been reviewed elsewhere [3,4].
Fig. 1.
Induction of the autophagy pathway.
Autophagy is initiated typically from cellular stress, such as starvation, whereby Unc-51-like kinase 1 (ULK1) complex (comprising ULK1, autophagy-related protein 13 (ATG13), FIP200 and ATG101 are activated. This complex triggers nucleation of the phagophore by phosphorylating components of the class III PI3K (PI3KC3) complex I (consisting of class III PI3K, vacuolar protein sorting 34 (VPS34), Beclin 1, ATG14, activating molecule in Beclin 1-regulated autophagy protein 1 (AMBRA1) and general vesicular transport factor (p115). This in turn activates local phosphatidylinositol-3-phosphate (PI3P) production at discrete ER sites often referred to as omegasomes. WD repeat domain phosphoinositide-interacting proteins (WIPIs) and zinc-finger FYVE domain-containing protein 1 (DFCP1) are then recruited to these phagosome assembly sites followed by recruitment of ATG12˜ATG5–ATG16L1 complex that enhances ATG3-mediated conjugation of ATG8 family proteins, including microtubule-associated protein light chain 3 (LC3) proteins to membrane-resident phosphatidylethanolamine (PE), thus forming the membrane-bound, lipidated form LC3-II — the characteristic signature of autophagic membranes. ATG8s are required for elongation and closure of the phagophore membrane, and in selective autophagy, are involved in sequestration of specific cargo into autophagosomes. Several cellular membranes, most likely the ER, contribute to elongation of the autophagosomal membrane by serving as membrane reservoir - delivered by ATG9-containing vesicles. Once sealed, autophagosomal membranes give rise to double-layered vesicles called autophagosomes, which mature and fuse with the lysosomes. Autophagic cargo is hydrolysed and recycled back to the cytoplasm.
Apart from turnover of organelles and primarily long-lived proteins, autophagy operates to defend host cells against intracellular pathogens – delivering trapped bacterial or viral products to lysosomes for degradation. Besides, it is equipped to clear invasive pathogens through induction of CD8+ T-cell responses, and also initiates a primordial innate immune response by cooperating with pattern recognition receptor signalling to induce interferon production. This was recently described in the context of DNA virus infections, where cyclic GMP-AMP (cGAMP) and STING-dependent activation of autophagy was necessary to remove viral DNA from the cytosol [5]. However, in an ongoing evolutionary arms race, most pathogens have acquired the ability to hijack and subvert autophagy to evade degradation through this pathway. More remarkably, +RNA viruses have adapted to not only protect themselves from autophagic elimination but even harness the machinery to their own benefit, as will be covered in more detail in the subsequent sections.
2. Subversion of autophagy by +RNA viruses
Among the +RNA viruses, data on favourable versus detrimental impact of autophagy is particularly confounding [4]. A link between autophagosomes and virus-induced vesicles was proposed by George Palade by EM imaging of poliovirus containing vesicles that resembled autophagosomal membranes [6]. Over the past few decades, a growing body of research has defined the critical role of this pathway in facilitating infection by numerous +RNA RNA viruses, including poliovirus (PV) [7,8], Coxsackievirus B3 (CVB3) [9,10], CVB4 [11], Enterovirus 71 (EV71) [12], Human rhinovirus (HRV) [13], Foot-and-mouth disease virus (FMDV) [14], encephalomyocarditis virus (EMCV) [15], Dengue virus (DENV) [16,17], Zika virus (ZIKV) [18,19], Hepatitis C virus (HCV) [20], Mouse hepatitic virus (MHV), Newcastle disease virus (NDV) [21], Severe and acute respiratory syndrome coronavirus (SARS-CoV) [22], Chikungunya virus (ChikV) [23], and Japanese encephalitis virus (JEV) [24]. In many of the above cases, pharmacological or genetic manipulation of autophagy in vitro confirmed an inhibition in replication and/or spread of these viruses, whereas induction of autophagy resulted in increased production of progeny virions [21,25].
Current evidence indicates that many, if not all +RNA RNA viruses depend on the initiation of the autophagic pathway for their optimal production. This is counterintuitive, since these viruses replicate in the cytosol, and autophagy serves to promote degradation of cytosolic contents. Therefore, it is evident that +RNA RNA viruses in particular have evolved sophisticated mechanisms to circumvent or exploit this pathway. Not surprisingly, most +RNA RNA viruses also trigger massive membrane remodelling within infected host cells to create membrane delineated structures, often referred to as replication organelles, vesicle packets, convoluted membranes or double membrane vesicles, depending on their morphology and ultrastructure [18,26]. Whether these replication organelles are pseudo-autophagosomes, has long been a point of contention.
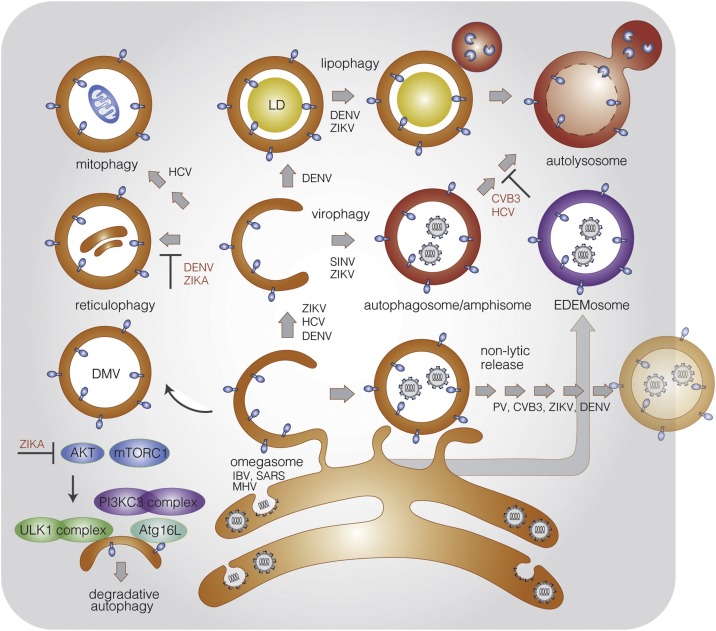
Several genome-wide screens, e.g with CRISPR/Cas9 libraries, haploid KBM7 cells, and shRNA depletions, as well as proteomic studies have universally indicated the involvement of the autophagy pathway in +RNA RNA virus infections [25,27,28]. However, among the 30 odd autophagy-related genes, the functional contribution of the individual components in virus infection is far from clear. A recent targeted CRISPR/Cas9 screen uncovered a fairly diverse range of involvement among autophagic components in three +RNA RNA virus infections – PV, DENV and ZIKV [29]. The authors reported that all three viruses employed multiple proteins of the autophagy pathway while bypassing others, and each virus used a unique set of initiation components. A common feature among the tested viruses underscored the requirement of the LC3 protein but not its canonical cellular lipidation process, where LC3 was recruited to virally induced membranes by alternative means. This study highlights the importance of assessing the pathway in its entirety when seeking to understand how pathogens co-opt it for purposes of genome replication and spread, as well as to identify universal drug targets. Many different mechanisms have been proposed on how autophagy is manipulated to facilitate infection while preventing degradation of +RNA RNA viruses (Fig. 2 ). While in no way exhaustive, the following sections cover the salient features that are recurrent among several viral genera:
Fig. 2.
Mechanisms of viral subversion of autophagy.
Schematic illustration of the different pathways of selective autophagy that are triggered upon +RNA RNA virus infections. Initiation of autophagosomes is through formation of an isolation membrane most likely derived from the ER. Depending on the molecular composition and function, they may form either omegasomes, EDEMosomes or amphisomes. Flaviviruses such as ZIKV non-structural protein 4A (NS4A) and NS4B activate autophagy by inhibiting AKT and mTORC1; autophagosomes generated are subverted to specialized functions to prevent viral degradation. Turnover of organelles occur through convergence of specialised autophagosomes with lysosomes for their selective degradation: ER via reticulophagy; mitochondria via mitophagy; lipid droplets via lipophagy and virions or viral proteins via virophagy. Viruses that are known to upregulation specific autophagosomal pathways are depicted in black, those that suppress specific types or steps of autophagy are depicted in red.
2.1. Partial/selective autophagy
The physical hallmark of the autophagy pathway is formation of LC3+ cytosolic double-membrane vesicles, also often observed in +RNA RNA virus infections. One of the long-running debates is whether these replication organelles are themselves immature autophagosomes or take advantage of the same machinery for their biogenesis. However, canonical autophagic vesicles are part of a degradative pathway, where they fuse with lysosomes for their contents to be hydrolysed by proteases and lipases. Viruses from different families appear to possess a diverse set of strategies to prevent this from happening. Flaviviruses, such as DENV and ZIKV have been reported to trigger autophagy on the one hand, while utilising the ER as a focal point for generating their replication organelles and assembly of progeny virions. Consequently, both viruses have evolved means to suppress ER-turnover via reticulophagy. The ER-localised reticulophagy receptor FAM134B was identified as a restriction factor for both DENV and ZIKV. RNAi-depletion of FAM134B significantly enhanced DENV and ZIKV replication at an early stage of the viral life cycle. The virus-encoded NS3 protease from several flaviviruses directly cleaved FAM134B at a single site within its reticulon homology domain to selectively suppress ER degradation [30], underscoring a sophisticated mechanism to differentially regulate specific arms of autophagy.
Coxsackievirus B3 (CVB3), an enterovirus belonging to the Picornaviridae family, is known to rely on autophagosome formation for optimal replication [31,32]; however, both in vitro and in vivo evidence suggest that during infection, amphisome maturation and autophagic protein degradation are inhibited. An increase in autophagosomal abundance concomitant with a decrease in autophagic flux was reported with CVB3, prompting the hypothesis that infection selectively triggers autophagosome formation while preventing the terminal stages in degradation [7,33]. The molecular determinants and mechanism by which CVB3 limits autophagic degradation is currently unknown. Interestingly, treatment of CVB3-infected cells with inhibitors of autophagosome maturation resulted in increased virus production, indicating that canonical autophagy was not completely blocked in virus-infected cells, and at least a population of the virus remained sensitive. A similar finding was reported more recently with rotavirus where virus replication benefited from induction of autophagy while blocking degradation [34]. As with CVB3, the mechanism by which rotaviruses specifically inhibit autolysosomal degradation has not been elucidated, emphasising the importance of identifying the specific virus or host components that prevent degradation to provide fundamental insights on autophagic regulation in general.
The case with HCV infection is more convoluted on account of contradictory data: whereas GFP-RFP-LC3 expressing cells infected with HCV displayed a complete maturation of autophagosomes followed by fusion with lysosomes [35,36], atleast one other study reported that HCV replication restricted autophagosomal fusion [37]. Yet another study reported that the autophagy pathway in its entirety was necessary during HCV-infection for optimal replication; however, the advantage derived from it was primarily due to suppression of innate immune responses [36]. Blocking fusion between autophagosomes and lysosomes has also been reported to increase DENV2 yield [38]. However, this effect may be viral serotype-specific, since inhibiting lysosome fusion reduced DENV3 production [39]. The mechanisms by which autophagy favors DENV production was recently described where rather than replication, assembly and release of progeny virions was affected by blocking autophagy mediated lipid droplet hydrolysis [16,40,41].
With Coronaviruses, initiation of autophagy appears to be through the ER-derived, Ptdlns3P-enriched omegasomes that normally operate during starvation. Infectious bronchitis virus (IBV) - an avian coronavirus responsible for major losses to the poultry industry, is one such example where a significant portion of the genome encodes nonstructural proteins (NSP) dedicated to virus replication. Expression of NSP6 proteins resulted in increased levels of Ptdlns3P on ER membranes, recruitment of Ptdlns3P effector protein WIPI2 and the generation of autophagosomes directly from the ER [42,43]. However, when compared to the properties of starvation-induced autophagosomes, those generated by Coronavirus infection or NSP6 proteins presented significant differences. NSP6-induced autophagosomes displayed limited ability to undergo expansion, preventing formation of large autolysosomes, and hence circumvented degradation of viral particles through the lysosomal pathway [43]. Results obtained with IBV, SARS and MHV nsp6 was recapitulated with Middle eastern respiratory syndrome coronavirus (MERS-CoV), where a similar phenomenon was observed for nsp6 [44].
2.2. Autophagosomes as viral replication sites
A distinctive feature shared by +RNA RNA viruses is to assemble and replicate on intracellular membranes, which have been proposed to offer a two-fold advantage: (a) scaffold for anchoring and concentrating the replication complexes and (b) to insulate dsRNA intermediates from innate sensing by cytosolic pattern recognition receptors [45]. The replication complexes are typically composed of the viral RNA-dependent RNA polymerase, accessory non-structural proteins, viral RNA, and host factors. Specialised autophagosomes, sometimes referred to as amphisomes (formed upon fusion with endosomes), omegasomes, and EDEMosomes (both ER-derived) have been hypothesised to function as replication organelles [43,46,47]. Given the resemblance of virus-triggered double membrane vesicles with that of autophagosomes, it is plausible that generation of replication organelles are a result of mechanisms similar to autophagy [[48], [49], [50], [51]]. Like autophagosomal membranes, many virus-induced vesicles are believed to be ER-derived. Recent data from several different studies have provided direct evidence of the association between viral replication complexes and autophagosome structures as summarized in Table 1 . Poliovirus (PV) vesicle clusters were found to contain LC3 and lysosomal markers, reminiscent of autolysosomes, and colocalised with the PV replication complex [7,52]. Furthermore, formation of infectious PV progeny virions was reported to depend on vesicular acidification, prompting the hypothesis that particle assembly, genome replication and virion maturation occurred in bona fide autophagosomal vesicles [46].
Table 1.
Viral protein interaction with components of the host autophagy machinery.
| Virus | Viral protein | Interaction with autophagy machinery | Reference |
|---|---|---|---|
| Flaviviridae | |||
| DENV | NS1 | Colocalises with dsRNA, autophagic vacuoles and cathepsin D | [38,39] |
| NS4A | Induces PI3K-dependent autophagy and protect cell death from stress; redistributes to LC3+ vesicles | [16,81] | |
| WNV | NS4A, NS4B | Single amino acid substitution in either protein is sufficient to upregulate autophagy | [97] |
| ZIKV | NS1 | Possible transport through autophagic secretion | [98] |
| NS4A, NS4B | Supresses Akt-mTOR signaling to induce autophagy | [53] | |
| JEV | NS1 | Colocalises with endogeneous LC3 | [99] |
| DENV, WNV, ZIKV | NS2B, NS3 | Cleaves FAM134B to interfere with reticulophagy | [30] |
| HCV | NS4B | Redistributes LC3 to punctuate structures | [100] |
| NS5A | Degraded in autophagosomes by SCOTIN | [95] | |
| Upregulates Beclin 1 and activates mTOR signaling pathway | [101] | ||
| NS5B | Interacts with autophagy elongation complex (ATG5-12/16L1) for proper membranous web formation at replication sites | [102] | |
| Coronaviridae | |||
| HCoV-NL63 | NSP3 | PLP2 domain interacts with LC3 and Beclin 1 to induce autopahgosomes while blocking lysosomal fusion | [103] |
| MHV | NSP2, NSP3 | Colocalises but does not interact with LC3-I | [104] |
| IBV, SARS, MHV | NSP6 | Induces Atg5 and LC3 dependent, starvation-independent autopahgosomes | [43,105] |
| Picornaviridae | |||
| CVB3 | 2A | Cleaves p62/SQSTM1 to disrupt selective autophagy and NFκB signaling | [106] |
| 2B | Autophagy-inducing motif at 36-83 amino aicds | [107] | |
| EV-D68 | 3C | Cleaves autophagosomal SNARE, SNAP29 | [108] |
| EV71 | VP1 | Colocalises with LC3 to form autophagosome-like vesicles | [59] |
| FMDV | VP1 | Colocalises with Atg5 and p62 | [14] |
| VP2 | Induces autophagy through HSPB1 and EIF2S1-ATF4 pathway | [109] | |
| 2B | Induces autophagy | [110] | |
| 2B, 2C, 3A | Colocalises with LC3 | [14] | |
| PV | VP1 | Colocalises with LC3, postulated to release virus through autophagosome-like vesicles | [7] |
| 2BC, 3A | Induces formation of LC3 coated double membrane vesicles | [111] | |
| 3AB | Induces formation of autophagosome-like double-membrane liposomes | [112] | |
Summary of Interactions between proteins from positive strand RNA viruses and host autophagy machinery.
Among the Flaviviridae family, several non-structural proteins have been observed in LC3+ vesicles. DENV non-structural protein NS1 and dsRNA were reported to co-localise with LC3 and ribosomal proteins [38,39]. Another study described the induction of LC3+ vesicles, which colocalised with NS4A in infected cells, or when transfected with a combination of DENV NS4A and NS4B [16]. This was independently corroborated by ZIKV infection in human fetal neural stem cells where expression of NS4A and NS4B were sufficient to block neurogenesis and promote autophagy, displaying partial colocalisation with LC3+ vesicles [53]. Ultrastructural analysis of ChikV virions also suggested their location in the lumen of autophagome-like vacuoles [23].
Similar to other members of this family, HCV infection induces massive intracellular membrane rearrangements. Competing hypotheses have been proposed as to whether autophagosomes themselves serve as sites for HCV replication. By sucrose gradient analysis, LC3-II was found to co-sediment with HCV RNA and non-structural proteins NS3 and NS5A [54]. However, in a separate study confocal microscopy showed little evidence of co-localisation of LC3 or Atg5 with HCV proteins [55,56]. Along the same lines, depletion of either LAMP2 or Rab7, which allowed accumulation of autophagosomes by preventing fusion with lysosomes inhibited HCV viral replication, also suggesting that they are not the major sites for HCV genome replication [36], while multiple reports indicate that lipid droplets are the more likely sites for replication and assembly, as reviewed elsewhere [40,57].
Conflicting evidence also exists for MHV-induced replication compartments. On the one hand, MHV replication complexes were found to be associated with LC3 and Atg12 in embryonic stem cell lines [22]. On the other hand in primary macrophages and murine embryonic fibroblasts MHV replication did not require the autophagy gene Atg5 [58]. Differences in permisiveness to infection often exists between primary cells and transformed cell lines, as does viral tropism towards distinct cell types, either of which can account for these experimental discrepancies. Among other +RNA RNA viruses, immunoelectron microscopy demonstrated co-localisation of EV71 capsid protein VP1 with autophagosomes in virus-infected mouse neurons [59]. Similarly, during EMCV infection, colocalisation of non-structural protein 3A and capsid protein VP1 was visualised by confocal and immunoelectron microscopy [60]. Colocalisation of non-structural proteins 2B, 2C, and 3A with LC3, and structural protein VP1 with Atg5 were also reported in FMDV-infected cells [14]. Although direct evidence of the association of viral replication complexes with autophogasomes is lacking for CVB3, impaired maturation of autolysosomes brought about through pharmacological or genetic inhibition increased the accumulation of autophagosomes in virus-infected cells resulting in enhanced viral replication [31,32]. These data implicated autophagosomes as virus anchoring and replication sites during CVB3 replication.
2.3. Autophagy as a mechanism to facilitate virus assembly
Delineating the process of viral assembly from replication is technically challenging, especially since both processes would very likely occur in concert at the same sites. Although utilisation of autophagosomes as assembly sites has been recorded for some DNA-viruses e.g., Hepatitis B virus (HBV) [61], experimental data with +RNA RNA viruses are scant. However, atleast for DENV, recent evidence indicates that autophagy might actually assist in assembly of progeny virions, without them serving as replication organelles. One of the initial studies describing the induction of autophagy in flavivirus infections was performed by Lee et al [62]. The authors demonstrated that DENV2 infection in hepatocytes induced autophagy; targeting with either the inhibitor 3-methyladenine (3MA) or siRNAs against autophagy genes compromised infection. DENV-induced autophagosomes colocalised with LAMP1, a marker of lysosomal fusion, which was independently validated by immunofluorescence assays and pharmacological inhibition. Following this initial characterisation, a more mechanistic study emerged describing the role of selective autophagy facilitating hydrolysis of lipid droplets in an infection-specific manner [17].
Apart from the relatively non-specific bulk macroautophagy, cellular organelles are turned over through several types of selective autophagy. This phenomenon occurs under normal physiological conditions and is hypothesised to initiate a physiological response to appropriately address a specific stress. In the context of DENV infection, a type of selective autophagy of lipid storage organelles (lipid droplets) referred to as lipophagy was described that hydrolyses neutral fat deposits to free fatty acids and cholesterol, and supplements cellular energy reservoirs [40,63,64]. Heaton et al performed a targeted siRNA screen to identify cellular cofactors of DENV2 replication in hepatocytes, which revealed, among others, genes involved in the induction of autophagy [65], and were further characterised to reveal that DENV induced autophagosomes not only acquired LAMP1, but underwent complete maturation to become autolysosomes [17]. These did not colocalise with markers of the viral replication complex, suggesting that they may play an indirect, non-structural role in DENV replication. A subsequent study described the involvement of AUP1, a type-III membrane protein, in the initiation of virus-induced autophagy. AUP1 was regulated by monoubiquitin modification, where infection or a combined expression of viral NS4A and NS4B were necessary and sufficient to generate the unmodified form of AUP1 – a step that was critical in induction of this pathway. Interestingly, loss of AUP1 did not affect viral replication; however, impaired autophagy was accompanied by degradation of viral proteins through the proteasomal pathway resulting in significantly reduced production of progeny virions, supporting a specific role of AUP1-dependent lipophagy in assembly of virus particles [16]. These results were in agreement with an independent report demonstrating expression of Dengue NS4A was sufficient to trigger autophagy and protect against cell death.
2.4. Dysregulation of mitochondria by selective mitophagy
A growing body of evidence indicates that mitochondrial function is altered during flavivirus infections. Although the mechanistic underpinnings are currently not well understood, atleast for HCV, Parkin-dependent mitophagy has a significant effect on virus propagation. This was verified by silencing Parkin and PINK1, which inhibited HCV-triggered mitophagy and in turn blocked virus replication. Ultrastuctural analyses by electron microscopy and immunoelectron microscopy also confirmed the presence of damaged mitochondria in double-membrane vesicles in HCV-infected cells [66]. Whether this pathway is activated during infection by other flaviviruses is currently not known.
2.5. Non-lytic viral transmission by secretory autophagy
Several reports on mechanisms of secretion and cell-to-cell transfer of intracellular pathogens indicate non-degradative autophagic vesicles as an efficient mode of transport. An recent study with Mycobacterium demonstrated that autophagosomes chaperone an organelle referred to as the “ejectosome”, facilitating cell-to-cell spread of cytosolic bacteria [67]. Secretory autophagy is a newly discovered pathway in which autophagosomes fuse with the plasma membrane instead of lysosomes and release single membrane vesicles containing cytosolic content into the extracellular milieu [68].
Non-degradative autophagy has been suggested to facilitate non-lytic egress of some +RNA RNA viruses. The initial characterisation was with enteroviruses, which appear to exploit this pathway to exit cells, and are released into the extracellular environment as particle populations contained within vesicles [69]. Clusters of enteroviral particles were packaged with phosphatidyl serine into autophagic vesicles, which enabled efficient transfer to primary macrophages, significantly enhancing viral infectivity. This revealed a novel mode of transport where viral genomes were transferred en bloc to recipient cells, facilitating genetic cooperativity and enhancing infection. This mode of transfer had previously also been noted for CVB3, where a recombinant fluorescent virus was released into the extracellular medium in microvesicles containing autophagic markers [70].
Poliovirus is often considered a lytic virus; however, non-lytic release of poliovirus has also been reported [8]. Reduced levels of viral particles in extracellular medium in autophagy-deficient cells correlated with inhibition of non-lytic release of autophagic vesicles. More recently, an important role of the secretory autophagy pathway was implicated in ZIKV vertical transmission as well as cell-to-cell spread of DENV. ZIKV-induced autophagic activity in human trophoblasts restricted by pharmacological inhibition, or by deficiency in an essential autophagy gene, Atg16L1, limited ZIKV vertical transmission and improved placental and fetal outcomes, which supported a role for autophagic secretion in the process [71]. Along the same lines, it was hypothesised that DENV might evade neutralising antibodies and increase viral spread by exploiting autophagic vesicles for delivery to the extracellular medium [72]. Double staining of DENV E antigen and LC3 in a close-contact co-culture experimental set-up verified secretion of DENV-containing autophagic vesicles from donor cells, which were subsequently taken up by recipient cells. In a parallel study, maturation of infectious DENV virus particles was attributed to this process, when cleavage of Pr peptide from PrM by the furin protease was prevented upon blocking autophagy [73]. Further investigation is needed to provide more direct evidence on the mechanism, regulation and molecular determinants of secretory autophagy in facilitating viral release.
2.6. Suppression of innate antiviral responses through activation of autophagy
Activation of autophagy represents a fairly ubiquitous response to eliminate intracellular pathogens. Several studies have described mechanisms where pathogen recognition receptors trigger this response upon detection of microbe-specific pathogen associated molecular patterns. A diverse set of pathogens including bacteria, viruses and parasites have provided corroborating evidence supporting this phenomenon. Whether this process occurs in parallel to non-degradative autophagy, or the cross-talk that might exist between the two flavours of autophagy during +RNA RNA viral infection merits further investigation.
Recent studies have shed light on how autophagy offers an advantage to HCV infection by suppressing innate immune responses [36,74]. This contrasts with previous data on HCV-induced incomplete autophagy and defined a pathway where the entire process from initiation through lysosomal degradation is necessary for HCV replication largely to suppress anti-viral innate immune response. In HCV-infected cells, interferon-β (IFN-β) production could be modulated by UPR-mediated autophagy; activation of this pathway reduced IFN-β production and vice-versa [75]. Inhibition of autophagy by suppressing Beclin-1 or Atg7 reduced HCV replication, which was accompanied by the activation of IFN signaling. A similar phenomenon was also proposed for DENV where activation of autophagy not only facilitated viral replication, but also suppressed IFN-I production, suggesting that both viruses may share the same mechanism to evade innate immune responses. Interestingly, in West Nile virus infections, perturbation of intracellular cholesterol levels dictated IFN-I responses [76,77]. Although the role of autophagy in WNV infection has been contested, replication was reported to occur independent of autophagy by mutiple groups – a clear difference from other flaviviruses; however, whether it plays a role in regulating free cholesterol and fatty acid levels is yet to be determined. Together, these studies indicate a critical mechanism by which flaviviruses may avoid innate immune responses through activating the host autophagy pathway.
2.7. Induction of autophagy to facilitate cell survival
The link between autophagy and apoptosis has been defined extensively in various contexts including cancer, neurodegenerative disorders, and infectious diseases [78]. A more comprehensive understanding on circumventing cell death has been recorded for bacterial rather than viral infections, amongst which most are DNA viruses. Premature cell death can function as an anti-viral host mechanism by providing an unfavorable environment and shorter timeframes for viral propagation. Induction of autophagy has often been linked to inhibition of apoptosis [79,80]. Both DENV2 and a murine flavivirus-induced autophagy was reported to prevent apoptosis mediated via the viral NS4A protein [81]. Knockdown of autophagy-related gene expression abolished the protective role of autophagy against cell death and resulted in reduced viral replication. Apart from DENV, cross-talk between autophagy and apoptosis was also reported in CVB4 infection, where suppression of autophagy by 3MA triggered caspase activation and vice-versa [82].
3. Impact of virus-triggered autophagy on antigen presentation
An interesting question that arises from virus-triggered induction of autophagy in the context of flavivirus infections is the process of antigen presentation. Particularly in Major histocompatibility complex (MHC)-II positive cells, autophagosomes are constitutively generated to deliver viral antigens on MHC-II molecules for adaptive immune responses. Virus infections therefore frequently impede maturation of antigen presenting cells and subsequent adaptive immunity as reviewed in detail elsewhere [4]. Monocytes and monocyte-derived cells are a major target of flaviviruses, where antigen presentation is facilitated by autophagy. This implies that while autophagy favours production of viral progeny, it should simultaneously increase viral antigen presentation and T-cell responses, thus generating neutralising antibodies and promoting cytotoxic T-cell killing. Information on these seemingly contradictory processes is currently limited. However, DENV-infected human monocyte-derived DCs fail to upregulate MHC and co-stimulatory molecules and have an impaired ability to polarize CD4 + Th type 1 (Th1) effector properties [83], contributing to inefficient adaptive immune responses observed in patients. In bulk cultures of dendritic cells, exposure to DENV augments MHC-I and MHC-II expression in non-infected bystander cells; however, infected monocyte-derived dendritic cells display an inhibition in this process within the same cultures [84]. In clinical studies gene expression analyses of DENV patients revealed that severe cases expressed lower levels of genes linked to antigen processing, presentation and T-cell activation compared to mild cases. Another related flavivirus, Japanese Encephalitis virus, inhibits expression of MHC-I and induces functional impairment of DCs, resulting in poor CD8 + T cell responses [85]. Thus impaired antigen presentation and functionality of virus-infected DCs may reflect a viral immune escape strategy to dampen T-cell responses and impact disease severity. One study reported that DENV activated autophagy only during the early infection stage, suggesting a biphasic response of autophagy to DENV infection, where it shifted from a supporting to an antiviral role at later time points [86]. These results might enable us to reconcile how flaviviruses have evolved strategies to manipulate this pathway while subverting T-cell based immune responses. A quantitative and time resolved analyses of this process in virus-infected cells might shed light on its utilisation in the benefit versus detriment towards virus production.
4. Autophagy-mediated restriction of +RNA virus infections
Activation of autophagy in the presence of intracellular pathogens is a fairly universal cellular response. Xenophagy as an intrinsic defence mechanism was first described through electron microscopy studies upon visualising HSV-1 and cytomegalovirus inside autophagosomes [87].
Among viruses, autophagic protection has been recorded in a wide-ranging species and genera [[88], [89], [90]]. The mechanism of autophagy-mediated restriction of +RNA RNA viruses is less well-documented on account of its proviral influence in most cases. However, there are instances where autophagic degradation of virions (virophagy) or viral proteins has been observed, especially in neurons where it is a critical form of antiviral defence. During Sindbis virus (SINV) infection, Beclin 1 and p62-dependent degradation of the capsid protein protects against SINV-mediated encephalitis [91,92]. Moreover, ATG5 deficiency results in delayed SINV clearance and accumulation of the autophagy receptor p62. More recently, Fanconi anaemia group C protein (FANCC) was found to interact with the SINV capsid protein and facilitate virophagy [28]. Picornaviruses, such as PV and HRV permeabilise endosomes to release their genome into the cytosol. This step is detected by galectin 8, which restricts viral infection by initiating degradation of the viral RNA genome [93]. As counterstrategy, the host protein HRAS-like suppressor 3 (PLA2G16) is exploited by the virus to enable genome delivery. CVB3, also belonging to the same family, undergoes p62-dependent degradation and uses the viral protease 2A to cleave p62 and inhibit virophagy [94]. Interestingly, although HCV has been demonstrated to induce autophagy to its own advantage by multiple groups, one study demonstrated that an ER transmembrane protein, SCOTIN, interacted with the viral protein NS5A, resulting in its autophagic degradation to suppress viral replication [95]. Among flaviviruses, autophagosomal degradation of neurotropic viruses has been recorded. In the drosophila brain, ZIKV infection triggered NFκB-dependent inflammatory signaling, inducing expression of dSTING which subsequently restricted infection by upregulating autophagy. Defective or absence of autophagy resulted in increased infection in the fly brain and death [96]. STING-dependent induction of protective autophagy was independently reported for DNA viruses and sea anemone, supporting an evolutionarily conserved role for STING in microbial autophagy [5].
5. Future perspectives
Despite major advances in elucidating molecular determinants of the autophagy pathway, the rules that govern its utilisation during infections are far from obvious. A complex interplay between viral manipulation and host innate immunity dictates disease outcomes. Autophagy is expected to restrict viral infections at multiple levels by eliminating viruses, regulating inflammatory responses and promoting antigen presentation. However, +RNA viruses have co-evolved to manipulate autophagy for immune evasion, replication, assembly and release from infected cells. The repertoire of universal and distinct mechanisms that these viruses draw on to interfere with autophagy are striking, often targeting the same pathway in unique ways with different functional implications. Distinct viral strategies fine-tune the process to simultaneously escape destruction while capitalising on the structural and nutrient benefits that autophagy provides. Several gaps remain in our understanding within the remit of viral manipulation of autophagy. First and foremost, more advanced strategies of isolating autophagic vesicles will be imperative for better characterisation of this process. Emerging data indicate that many LC3-positive vesicles that are induced upon virus infections are not autophagosomes. A combination of ultracentrifugation, density gradient separations and enrichment techniques will be necessary to characterise these vesicle populations. Furthermore, in the context of virus infection, the equilibrium between degradative and secretory autophagy versus biogenesis of exosomal vesicles will need to be quantitated to arrive at firm conclusions regarding the functional outcome of autophagy. Along the same lines, differences between infected host cells and neighbouring cells will become important to develop a more complete picture of its impact in viral pathogenesis versus immune responses. Further understanding of the contribution of autophagy to the different stages in the viral life-cycle, subversion of its antigen presentation function and innate immune responses is therefore necessary to delineate the diverse functions of autophagy in virus pathogenesis.
Acknowledgements
This work was supported by Health and Medical Research Funds (16150592 and 17161202 and 17161032), and partially by Research Grants Council-General research funds (17112617). SS is supported by the Croucher Foundation.
References
- 1.Shibutani S.T., Yoshimori T. Vol. 24. Nature Publishing Group; 2014. pp. 58–68. (A Current Perspective of Autophagosome Biogenesis). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mijaljica D., Prescott M., Devenish R.J. Endoplasmic reticulum and Golgi complex: contributions to, and turnover by, autophagy. Traffic. 2006;7:1590–1595. doi: 10.1111/j.1600-0854.2006.00495.x. [DOI] [PubMed] [Google Scholar]
- 3.Dikic I., Elazar Z. Mechanism and medical implications of mammalian autophagy. Nat. Rev. Mol. Cell Biol. 2018;19:349–364. doi: 10.1038/s41580-018-0003-4. [DOI] [PubMed] [Google Scholar]
- 4.Choi Y., Bowman J.W., Jung J.U. Autophagy during viral infection - a double-edged sword. Nat. Rev. Microbiol. 2018;16:341–354. doi: 10.1038/s41579-018-0003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gui X., Yang H., Li T., Tan X., Shi P., Li M. Autophagy induction via STING trafficking is a primordial function of the cGAS pathway. Nature. 2019;567:262–266. doi: 10.1038/s41586-019-1006-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dales S., Eggers H.J., Tamm I., Palade G.E. Electron microscopic study of the formation of poliovirus. Virology. 1965;26:379–389. doi: 10.1016/0042-6822(65)90001-2. [DOI] [PubMed] [Google Scholar]
- 7.Jackson W.T., Giddings T.H., Taylor M.P., Mulinyawe S., Rabinovitch M., Kopito R.R. Subversion of cellular autophagosomal machinery by RNA viruses. PLoS Biol. 2005;3:e156. doi: 10.1371/journal.pbio.0030156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bird S.W., Maynard N.D., Covert M.W., Kirkegaard K. Nonlytic viral spread enhanced by autophagy components. Proc. Natl. Acad. Sci. 2014;111:13081–13086. doi: 10.1073/pnas.1401437111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alirezaei M., Flynn C.T., Wood M.R., Harkins S., Whitton J.L. Coxsackievirus can exploit LC3 in both autophagy-dependent and -independent manners in vivo. Autophagy. 2015;11:1389–1407. doi: 10.1080/15548627.2015.1063769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohamud Y., Shi J., Qu J., Poon T., Xue Y.C., Deng H. Enteroviral infection inhibits autophagic flux via disruption of the SNARE complex to enhance viral replication. CellReports. 2018;22:3292–3303. doi: 10.1016/j.celrep.2018.02.090. [DOI] [PubMed] [Google Scholar]
- 11.Yoon S.Y., Ha Y.E., Choi J.E., Ahn J., Lee H., Kweon H.-S. Coxsackievirus B4 uses autophagy for replication after calpain activation in rat primary neurons. J. Virol. 2008;82:11976–11978. doi: 10.1128/JVI.01028-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee Y.-R., Wang P.-S., Wang J.-R., Liu H.-S. Enterovirus 71-induced autophagy increases viral replication and pathogenesis in a suckling mouse model. J. Biomed. Sci. 2014;21:80. doi: 10.1186/s12929-014-0080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klein K.A., Jackson W.T. Human rhinovirus 2 induces the autophagic pathway and replicates more efficiently in autophagic cells. J. Virol. 2011;85:9651–9654. doi: 10.1128/JVI.00316-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Donnell V., Pacheco J.M., LaRocco M., Burrage T., Jackson W., Rodriguez L.L. Foot-and-mouth disease virus utilizes an autophagic pathway during viral replication. Virology. 2011;410:142–150. doi: 10.1016/j.virol.2010.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hou L., Ge X., Xin L., Zhou L., Guo X., Yang H. Nonstructural proteins 2C and 3D are involved in autophagy as induced by the encephalomyocarditis virus. Virol. J. 2014;11:156. doi: 10.1186/1743-422X-11-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang J., Lan Y., Li M.Y., Lamers M.M., Fusade-Boyer M., Klemm E. Flaviviruses exploit the lipid droplet protein AUP1 to trigger lipophagy and drive virus production. Cell Host Microbe. 2018;23:819–831. doi: 10.1016/j.chom.2018.05.005. e5. [DOI] [PubMed] [Google Scholar]
- 17.Heaton N.S., Randall G. Dengue virus-induced autophagy regulates lipid metabolism. Cell Host Microbe. 2010;8:422–432. doi: 10.1016/j.chom.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cortese M., Goellner S., Acosta E.G., Neufeldt C.J., Oleksiuk O., Lampe M. Ultrastructural characterization of zika virus replication factories. CellReports. 2017;18:2113–2123. doi: 10.1016/j.celrep.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Offerdahl D.K., Dorward D.W., Hansen B.T., Bloom M.E. Cytoarchitecture of Zika virus infection in human neuroblastoma and Aedes albopictus cell lines. Virology. 2017;501:54–62. doi: 10.1016/j.virol.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hansen M.D., Johnsen I.B., Stiberg K.A., Sherstova T., Wakita T., Richard G.M. Hepatitis C virus triggers Golgi fragmentation and autophagy through the immunity-related GTPase M. Proc. Natl. Acad. Sci. 2017;114:E3462–E3471. doi: 10.1073/pnas.1616683114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun Y., Yu S., Ding N., Meng C., Meng S., Zhang S. Autophagy benefits the replication of Newcastle disease virus in chicken cells and tissues. J. Virol. 2014;88:525–537. doi: 10.1128/JVI.01849-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prentice E., Jerome W.G., Yoshimori T., Mizushima N., Denison M.R. Coronavirus replication complex formation utilizes components of cellular autophagy. J. Biol. Chem. 2004;279:10136–10141. doi: 10.1074/jbc.M306124200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krejbich-Trotot P., Gay B., Li-Pat-Yuen G., Hoarau J.-J., Jaffar-Bandjee M.-C., Briant L. Chikungunya triggers an autophagic process which promotes viral replication. Virol. J. 2011;8:432. doi: 10.1186/1743-422X-8-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharma M., Bhattacharyya S., Sharma K.B., Chauhan S., Asthana S., Abdin M.Z. Japanese encephalitis virus activates autophagy through XBP1 and ATF6 ER stress sensors in neuronal cells. J. Gen. Virol. 2017;98:1027–1039. doi: 10.1099/jgv.0.000792. [DOI] [PubMed] [Google Scholar]
- 25.Orvedahl A., Sumpter R., Xiao G., Ng A., Zou Z., Tang Y. Image-based genome-wide siRNA screen identifies selective autophagy factors. Nature. 2011;480:113–117. doi: 10.1038/nature10546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paul D., Bartenschlager R. Flaviviridae replication organelles: oh, what a tangled web we weave. Annu. Rev. Virol. 2015;2:289–310. doi: 10.1146/annurev-virology-100114-055007. [DOI] [PubMed] [Google Scholar]
- 27.Savidis G., McDougall W.M., Meraner P., Perreira J.M., Portmann J.M., Trincucci G. Identification of Zika virus and dengue virus dependency factors using functional genomics. CellReports. 2016;16:232–246. doi: 10.1016/j.celrep.2016.06.028. [DOI] [PubMed] [Google Scholar]
- 28.Sumpter R., Sirasanagandla S., Fernández Á., Wei Y., Dong X., Franco L. Fanconi anemia proteins function in mitophagy and immunity. Cell. 2016;165:867–881. doi: 10.1016/j.cell.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abernathy E., Mateo R., Majzoub K., van Buuren N., Bird S.W., Carette J.E. Differential and convergent utilization of autophagy components by positive-strand RNA viruses. PLoS Biol. 2019;17 doi: 10.1371/journal.pbio.2006926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lennemann N.J., Coyne C.B. Dengue and Zika viruses subvert reticulophagy by NS2B3-mediated cleavage of FAM134B. Autophagy. 2017;13:322–332. doi: 10.1080/15548627.2016.1265192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kemball C.C., Alirezaei M., Flynn C.T., Wood M.R., Harkins S., Kiosses W.B. Coxsackievirus infection induces autophagy-like vesicles and megaphagosomes in pancreatic acinar cells in vivo. J. Virol. 2010;84:12110–12124. doi: 10.1128/JVI.01417-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wong J., Zhang J., Si X., Gao G., Mao I., McManus B.M. Autophagosome supports coxsackievirus B3 replication in host cells. J. Virol. 2008;82:9143–9153. doi: 10.1128/JVI.00641-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kemball C.C., Alirezaei M., Flynn C.T., Wood M.R., Harkins S., Kiosses W.B. Coxsackievirus infection induces autophagy-like vesicles and megaphagosomes in pancreatic acinar cells in vivo. J. Virol. 2010;84:12110–12124. doi: 10.1128/JVI.01417-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crawford S.E., Hyser J.M., Utama B., Estes M.K. Autophagy hijacked through viroporin-activated calcium/calmodulin-dependent kinase kinase-β signaling is required for rotavirus replication. Proc. Natl. Acad. Sci. 2012;109:E3405–13. doi: 10.1073/pnas.1216539109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kimura S., Noda T., Yoshimori T. Dissection of the autophagosome maturation process by a novel reporter protein, tandem fluorescent-tagged LC3. Autophagy. 2007;3:452–460. doi: 10.4161/auto.4451. [DOI] [PubMed] [Google Scholar]
- 36.Ke P.-Y., Chen S.S.L. Activation of the unfolded protein response and autophagy after hepatitis C virus infection suppresses innate antiviral immunity in vitro. J. Clin. Invest. 2011;121:37–56. doi: 10.1172/JCI41474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sir D., Chen W.-L., Choi J., Wakita T., Yen T.S.B., Ou J.-H.J. Induction of incomplete autophagic response by hepatitis C virus via the unfolded protein response. Hepatology. 2008;48:1054–1061. doi: 10.1002/hep.22464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Panyasrivanit M., Khakpoor A., Wikan N., Smith D.R. Co-localization of constituents of the dengue virus translation and replication machinery with amphisomes. J. Gen. Virol. 2009;90:448–456. doi: 10.1099/vir.0.005355-0. [DOI] [PubMed] [Google Scholar]
- 39.Khakpoor A., Panyasrivanit M., Wikan N., Smith D.R. A role for autophagolysosomes in dengue virus 3 production in HepG2 cells. J. Gen. Virol. 2009;90:1093–1103. doi: 10.1099/vir.0.007914-0. [DOI] [PubMed] [Google Scholar]
- 40.Zhang J., Lan Y., Sanyal S. Modulation of lipid droplet metabolism – a potential target for therapeutic intervention in flaviviridae infections. Front. Microbiol. 2017;8:2286. doi: 10.3389/fmicb.2017.02286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heaton N.S., Randall G. Dengue virus and autophagy. Viruses. 2011;3:1332–1341. doi: 10.3390/v3081332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Angelini M.M., Akhlaghpour M., Neuman B.W., Buchmeier M.J. Severe acute respiratory syndrome coronavirus nonstructural proteins 3, 4, and 6 induce double-membrane vesicles. mBio. 2013;4:1967. doi: 10.1128/mBio.00524-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cottam E.M., Whelband M.C., Wileman T. Coronavirus NSP6 restricts autophagosome expansion. Autophagy. 2014;10:1426–1441. doi: 10.4161/auto.29309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lundin A., Dijkman R., Bergström T., Kann N., Adamiak B., Hannoun C. Targeting membrane-bound viral RNA synthesis reveals potent inhibition of diverse coronaviruses including the middle East respiratory syndrome virus. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1004166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miller S., Krijnse-Locker J. Modification of intracellular membrane structures for virus replication. Nat. Rev. Microbiol. 2008;6:363–374. doi: 10.1038/nrmicro1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richards A.L., Jackson W.T. Intracellular vesicle acidification promotes maturation of infectious poliovirus particles. PLoS Pathog. 2012;8 doi: 10.1371/journal.ppat.1003046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richards A.L., Soares-Martins J.A.P., Riddell G.T., Jackson W.T. Generation of unique poliovirus RNA replication organelles. mBio. 2014;5 doi: 10.1128/mBio.00833-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Paul D., Bartenschlager R. Architecture and biogenesis of plus-strand RNA virus replication factories. World J. Virol. 2013;2:32–48. doi: 10.5501/wjv.v2.i2.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gosert R., Kanjanahaluethai A., Egger D., Bienz K., Baker S.C. RNA replication of mouse hepatitis virus takes place at double-membrane vesicles. J. Virol. 2002;76:3697–3708. doi: 10.1128/JVI.76.8.3697-3708.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Snijder E.J., van Tol H., Roos N., Pedersen K.W. Non-structural proteins 2 and 3 interact to modify host cell membranes during the formation of the arterivirus replication complex. J. Gen. Virol. 2001;82:985–994. doi: 10.1099/0022-1317-82-5-985. [DOI] [PubMed] [Google Scholar]
- 51.Goldsmith C.S., Tatti K.M., Ksiazek T.G., Rollin P.E., Comer J.A., Lee W.W. Ultrastructural characterization of SARS coronavirus. Emerging Infect. Dis. 2004;10:320–326. doi: 10.3201/eid1002.030913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Suhy D.A., Giddings T.H., Kirkegaard K. Remodeling the endoplasmic reticulum by poliovirus infection and by individual viral proteins: an autophagy-like origin for virus-induced vesicles. J. Virol. 2000;74:8953–8965. doi: 10.1128/jvi.74.19.8953-8965.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liang Q., Luo Z., Zeng J., Chen W., Foo S.-S., Lee S.-A. Zika virus NS4A and NS4B proteins deregulate Akt-mTOR signaling in human fetal neural stem cells to inhibit neurogenesis and induce autophagy. Cell Stem Cell. 2016;19:663–671. doi: 10.1016/j.stem.2016.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ferraris P., Blanchard E., Roingeard P. Ultrastructural and biochemical analyses of hepatitis C virus-associated host cell membranes. J. Gen. Virol. 2010;91:2230–2237. doi: 10.1099/vir.0.022186-0. [DOI] [PubMed] [Google Scholar]
- 55.Dreux M., Gastaminza P., Wieland S.F., Chisari F.V. The autophagy machinery is required to initiate hepatitis C virus replication. Proc. Natl. Acad. Sci. 2009;106:14046–14051. doi: 10.1073/pnas.0907344106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tanida I., Fukasawa M., Ueno T., Kominami E., Wakita T., Hanada K. Knockdown of autophagy-related gene decreases the production of infectious hepatitis C virus particles. Autophagy. 2009;5:937–945. doi: 10.4161/auto.5.7.9243. [DOI] [PubMed] [Google Scholar]
- 57.Filipe A., McLauchlan J. Hepatitis C virus and lipid droplets:finding a niche. Trends Mol. Med. 2015;21:34–42. doi: 10.1016/j.molmed.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 58.Zhao Z., Thackray L.B., Miller B.C., Lynn T.M., Becker M.M., Ward E. Coronavirus replication does not require the autophagy gene ATG5. Autophagy. 2007;3:581–585. doi: 10.4161/auto.4782. [DOI] [PubMed] [Google Scholar]
- 59.Huang S.-C., Chang C.-L., Wang P.-S., Tsai Y., Liu H.-S. Enterovirus 71-induced autophagy detected in vitro and in vivo promotes viral replication. J. Med. Virol. 2009;81:1241–1252. doi: 10.1002/jmv.21502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang Y., Li Z., Ge X., Guo X., Yang H. Autophagy promotes the replication of encephalomyocarditis virus in host cells. Autophagy. 2011;7:613–628. doi: 10.4161/auto.7.6.15267. [DOI] [PubMed] [Google Scholar]
- 61.Döring T., Zeyen L., Bartusch C., Prange R. Hepatitis B virus subverts the autophagy elongation complex Atg5-12/16L1 and does not require Atg8/LC3 lipidation for viral maturation. J. Virol. 2018;92:101. doi: 10.1128/JVI.01513-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee Y.-R., Lei H.-Y., Liu M.-T., Wang J.-R., Chen S.-H., Jiang-Shieh Y.-F. Autophagic machinery activated by dengue virus enhances virus replication. Virology. 2008;374:240–248. doi: 10.1016/j.virol.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu K., Czaja M.J. Regulation of lipid stores and metabolism by lipophagy. Cell Death Differ. 2013;20:3–11. doi: 10.1038/cdd.2012.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Singh R., Kaushik S., Wang Y., Xiang Y., Novak I., Komatsu M. Autophagy regulates lipid metabolism. Nature. 2009;458:1131–1135. doi: 10.1038/nature07976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Heaton N.S., Perera R., Berger K.L., Khadka S., Lacount D.J., Kuhn R.J. Dengue virus nonstructural protein 3 redistributes fatty acid synthase to sites of viral replication and increases cellular fatty acid synthesis. Proc. Natl. Acad. Sci. 2010;107:17345–17350. doi: 10.1073/pnas.1010811107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim S.-J., Syed G.H., Siddiqui A. Hepatitis C virus induces the mitochondrial translocation of Parkin and subsequent mitophagy. PLoS Pathog. 2013;9 doi: 10.1371/journal.ppat.1003285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gerstenmaier L., Pilla R., Herrmann L., Herrmann H., Prado M., Villafano G.J. The autophagic machinery ensures nonlytic transmission of mycobacteria. Proc. Natl. Acad. Sci. 2015;112:E687–E692. doi: 10.1073/pnas.1423318112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ponpuak M., Mandell M.A., Kimura T., Chauhan S., Cleyrat C., Deretic V. Secretory autophagy. Curr. Opin. Cell Biol. 2015;35:106–116. doi: 10.1016/j.ceb.2015.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen Y.-H., Du W., Hagemeijer M.C., Takvorian P.M., Pau C., Cali A. Phosphatidylserine vesicles enable efficient en bloc transmission of enteroviruses. Cell. 2015;160:619–630. doi: 10.1016/j.cell.2015.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Robinson S.M., Tsueng G., Sin J., Mangale V., Rahawi S., McIntyre L.L. Coxsackievirus B exits the host cell in shed microvesicles displaying autophagosomal markers. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1004045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cao B., Parnell L.A., Diamond M.S., Mysorekar I.U. Inhibition of autophagy limits vertical transmission of Zika virus in pregnant mice. J. Exp. Med. 2017;214:2303–2313. doi: 10.1084/jem.20170957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wu Y.-W., Mettling C., Wu S.-R., Yu C.-Y., Perng G.C., Lin Y.-S. Autophagy-associated dengue vesicles promote viral transmission avoiding antibody neutralization. Sci. Rep. 2016;6:32243. doi: 10.1038/srep32243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mateo R., Nagamine C.M., Spagnolo J., Méndez E., Rahe M., Gale M. Inhibition of cellular autophagy deranges dengue virion maturation. J. Virol. 2013;87:1312–1321. doi: 10.1128/JVI.02177-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shrivastava S., Raychoudhuri A., Steele R., Ray R., Ray R.B. Knockdown of autophagy enhances the innate immune response in hepatitis C virus-infected hepatocytes. Hepatology. 2011;53:406–414. doi: 10.1002/hep.24073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ke P.-Y., Chen S.S.L. Activation of the unfolded protein response and autophagy after hepatitis C virus infection suppresses innate antiviral immunity in vitro. J. Clin. Invest. 2011;121:37–56. doi: 10.1172/JCI41474DS1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mackenzie J.M., Khromykh A.A., Parton R.G. Cholesterol manipulation by West Nile virus perturbs the cellular immune response. Cell Host Microbe. 2007;2:229–239. doi: 10.1016/j.chom.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 77.Pombo J.P., Sanyal S. Perturbation of intracellular cholesterol and fatty acid homeostasis during flavivirus infections. Front. Immunol. 2018;9:1276. doi: 10.3389/fimmu.2018.01276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Levine B., Yuan J. Autophagy in cell death: an innocent convict? J. Clin. Invest. 2005;115:2679–2688. doi: 10.1172/JCI26390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jäättelä M. Lysosomes and autophagy in cell death control. Nat. Rev. Cancer. 2005;5:886–897. doi: 10.1038/nrc1738. [DOI] [PubMed] [Google Scholar]
- 80.Levine B., Sinha S.C., Kroemer G. Bcl-2 family members: dual regulators of apoptosis and autophagy. Autophagy. 2008;4:600–606. doi: 10.4161/auto.6260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McLean J.E., Wudzinska A., Datan E., Quaglino D., Zakeri Z. Flavivirus NS4A-induced autophagy protects cells against death and enhances virus replication. J. Biol. Chem. 2011;286:22147–22159. doi: 10.1074/jbc.M110.192500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yoon S.Y., Choi J.E., Ahn J., Lee H. Autophagy in coxsackievirus-infected neurons. Autophagy. 2009;5:388–389. doi: 10.4161/auto.5.3.7723. [DOI] [PubMed] [Google Scholar]
- 83.Chase A.J. Impairment of CD4+ T cell polarization by dengue virus–infected dendritic cells. J. Infect. Dis. 2011;203:1763–1774. doi: 10.1093/infdis/jir197. [DOI] [PubMed] [Google Scholar]
- 84.Celluzzi C., Bisbing J., Marovich M.A., Burgess T. Differential effects of dengue virus on infected and bystander dendritic cells. J. Virol. 2005;79:2432–2439. doi: 10.1128/JVI.79.4.2432-2439.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aleyas A.G., Han Y.W., George J.A., Kim B., Kim K., Lee C.-K. Multifront assault on antigen presentation by Japanese encephalitis virus subverts CD8+ T cell responses. J. Immunol. 2010;185:1429–1441. doi: 10.4049/jimmunol.0902536. [DOI] [PubMed] [Google Scholar]
- 86.Metz P., Chiramel A., Chatel-Chaix L., Alvisi G., Bankhead P., Mora-Rodríguez R. Dengue virus inhibition of autophagic flux and dependency of viral replication on proteasomal degradation of the autophagy receptor p62. J. Virol. 2015;89:8026–8041. doi: 10.1128/JVI.00787-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Smith J.D., de Harven E. Herpes simplex virus and human cytomegalovirus replication in WI-38 cells. III. Cytochemical localization of lysosomal enzymes in infected cells. J. Virol. 1978;26:102–109. doi: 10.1128/jvi.26.1.102-109.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shelly S., Lukinova N., Bambina S., Berman A., Cherry S. Autophagy is an essential component of Drosophila immunity against vesicular stomatitis virus. Immunity. 2009;30:588–598. doi: 10.1016/j.immuni.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Orvedahl A., Alexander D., Tallóczy Z., Sun Q., Wei Y., Zhang W. HSV-1 ICP34.5 confers neurovirulence by targeting the Beclin 1 autophagy protein. Cell Host Microbe. 2007;1:23–35. doi: 10.1016/j.chom.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 90.Kyei G.B., Dinkins C., Davis A.S., Roberts E., Singh S.B., Dong C. Autophagy pathway intersects with HIV-1 biosynthesis and regulates viral yields in macrophages. J. Cell Biol. 2009;186:255–268. doi: 10.1083/jcb.200903070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liang X.H., Kleeman L.K., Jiang H.H., Gordon G., Goldman J.E., Berry G. Protection against fatal Sindbis virus encephalitis by beclin, a novel Bcl-2-interacting protein. J. Virol. 1998;72:8586–8596. doi: 10.1128/jvi.72.11.8586-8596.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Orvedahl A., MacPherson S., Sumpter R., Tallóczy Z., Zou Z., Levine B. Autophagy protects against Sindbis virus infection of the central nervous system. Cell Host Microbe. 2010;7:115–127. doi: 10.1016/j.chom.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Staring J., von Castelmur E., Blomen V.A., van den Hengel L.G., Brockmann M., Baggen J. PLA2G16 represents a switch between entry and clearance of Picornaviridae. Nature. 2017;541:412–416. doi: 10.1038/nature21032. [DOI] [PubMed] [Google Scholar]
- 94.Mohamud Y., Qu J., Xue Y.C., Liu H., Deng H., Luo H. CALCOCO2/NDP52 and SQSTM1/p62 differentially regulate coxsackievirus B3 propagation. Cell Death Differ. 2019;26:1062–1076. doi: 10.1038/s41418-018-0185-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kim N., Kim M.-J., Sung P.S., Bae Y.C., Shin E.-C., Yoo J.-Y. Interferon-inducible protein SCOTIN interferes with HCV replication through the autolysosomal degradation of NS5A. Nat. Commun. 2016;7:10631. doi: 10.1038/ncomms10631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Liu Y., Gordesky-Gold B., Leney-Greene M., Weinbren N.L., Tudor M., Cherry S. Inflammation-induced, STING-dependent autophagy restricts Zika virus infection in the drosophila brain. Cell Host Microbe. 2018;24:57–68. doi: 10.1016/j.chom.2018.05.022. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Blázquez A.-B., Saiz J.-C. Amino acid substitutions in the non-structural proteins 4A or 4B modulate the induction of autophagy in West Nile virus infected cells independently of the activation of the unfolded protein response. Front. Microbiol. 2014;5:797. doi: 10.3389/fmicb.2014.00797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang Z.-W., Li Z.-L., Yuan S. The role of secretory autophagy in Zika virus transfer through the placental barrier. Front. Cell. Infect. Microbiol. 2016;6:206. doi: 10.3389/fcimb.2016.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gupta V., Abdin M.Z. Japanese encephalitis virus replication is negatively regulated by autophagy and occurs on LC3-I- and EDEM1-containing membranes. Autophagy. 2014;10:1637–1651. doi: 10.4161/auto.29455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Su W.-C., Chao T.-C., Huang Y.-L., Weng S.-C., Jeng K.-S., Lai M.M.C. Rab5 and class III phosphoinositide 3-kinase Vps34 are involved in hepatitis C virus NS4B-induced autophagy. J. Virol. 2011;85:10561–10571. doi: 10.1128/JVI.00173-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shrivastava S., Bhanja Chowdhury J., Steele R., Ray R., Ray R.B. Hepatitis C virus upregulates Beclin1 for induction of autophagy and activates mTOR signaling. J. Virol. 2012;86:8705–8712. doi: 10.1128/JVI.00616-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fahmy A.M., Labonté P. The autophagy elongation complex (ATG5-12/16L1) positively regulates HCV replication and is required for wild-type membranous web formation. Sci. Rep. 2017;7:40351. doi: 10.1038/srep40351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chen X., Wang K., Xing Y., Tu J., Yang X., Zhao Q. Coronavirus membrane-associated papain-like proteases induce autophagy through interacting with Beclin1 to negatively regulate antiviral innate immunity. Protein Cell. 2014;5:912–927. doi: 10.1007/s13238-014-0104-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Reggiori F., Monastyrska I., Verheije M.H., Calì T., Ulasli M., Bianchi S. Coronaviruses hijack the LC3-I-positive EDEMosomes, ER-derived vesicles exporting short-lived ERAD regulators, for replication. Cell Host Microbe. 2010;7:500–508. doi: 10.1016/j.chom.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cottam E.M., Maier H.J., Manifava M., Vaux L.C., Chandra-Schoenfelder P., Gerner W. Coronavirus nsp6 proteins generate autophagosomes from the endoplasmic reticulum via an omegasome intermediate. Autophagy. 2011;7:1335–1347. doi: 10.4161/auto.7.11.16642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shi J., Wong J., Piesik P., Fung G., Zhang J., Jagdeo J. Cleavage of sequestosome 1/p62 by an enteroviral protease results in disrupted selective autophagy and impaired NFKB signaling. Autophagy. 2013;9:1591–1603. doi: 10.4161/auto.26059. [DOI] [PubMed] [Google Scholar]
- 107.Wu H., Zhai X., Chen Y., Wang R., Lin L., Chen S. Protein 2B of coxsackievirus B3 induces autophagy relying on its transmembrane hydrophobic sequences. Viruses. 2016;8 doi: 10.3390/v8050131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Corona A.K., Saulsbery H.M., Corona Velazquez A.F., Jackson W.T. Enteroviruses remodel autophagic trafficking through regulation of host SNARE proteins to promote virus replication and cell exit. CellReports. 2018;22:3304–3314. doi: 10.1016/j.celrep.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sun P., Zhang S., Qin X., Chang X., Cui X., Li H. Foot-and-mouth disease virus capsid protein VP2 activates the cellular EIF2S1-ATF4 pathway and induces autophagy via HSPB1. Autophagy. 2018;14:336–346. doi: 10.1080/15548627.2017.1405187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ao D., Guo H.-C., Sun S.-Q., Sun D.-H., Fung T.S., Wei Y.-Q. Viroporin activity of the foot-and-mouth disease virus non-structural 2B protein. PLoS One. 2015;10 doi: 10.1371/journal.pone.0125828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Taylor M.P., Kirkegaard K. Modification of cellular autophagy protein LC3 by poliovirus. J. Virol. 2007;81:12543–12553. doi: 10.1128/JVI.00755-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang J., Ptacek J.B., Kirkegaard K., Bullitt E. Double-membraned liposomes sculpted by poliovirus 3AB protein. J. Biol. Chem. 2013;288:27287–27298. doi: 10.1074/jbc.M113.498899. [DOI] [PMC free article] [PubMed] [Google Scholar]