Abstract
Respiratory gene therapy has been considered for the treatment of a broad range of pulmonary disorders. However, respiratory secretions form an important barrier towards the pulmonary delivery of therapeutic nucleic acids. In this review we will start with a brief description of the biophysical properties of respiratory mucus and alveolar fluid. This must allow the reader to gain insights into the mechanisms by which respiratory secretions may impede the gene transfer efficiency of nucleic acid containing nanoparticles (NANs). Subsequently, we will summarize the efforts that have been done to understand the barrier properties of respiratory mucus and alveolar fluid towards the respiratory delivery of therapeutic nucleic acids. Finally, new and current strategies that can overcome the inhibitory effects of respiratory secretions are discussed.
Keywords: Respiratory gene therapy, NANs, Nucleic acid containing nanoparticles, Mucus Alveolar fluid
1. Introduction
Respiratory gene therapy is considered for the treatment of a variety of lung diseases like cystic fibrosis (CF), asthma, emphysema, lung cancer, α1-antitrypsin deficiency and surfactant protein-B (SP-B) deficiency [1], [2], [3], [4], [5]. Additionally, DNA vaccination via the respiratory tract may also be of interest for certain infectious diseases [6], [7]. Recently, the delivery of siRNA containing nanoparticles to the lungs has also gained much attention for the treatment of lung infections caused by e.g. SARS (severe acute respiratory syndrome) or (avian) influenza viruses [8]. However, it is known that lung infections may, as in CF patients, lead to the production of purulent respiratory secretions. These altered secretions may drastically lower the number of siRNA molecules that can reach their target cells in the lung.
Depending on the respiratory disease and the therapeutic goal the target cells in the lung can vary from epithelial cells, alveolar cells, macrophages, respiratory stem cells or endothelial cells. All these cell types, except the latter two, can be directly accessed via inhalation or instillation of nucleic acid containing nanoparticles (NANs). These delivery routes have as advantage that they exclusively target the lungs and thereby prevent that NANs end-up in non-target tissues. Additionally, by playing around with the diameter of the aerosol droplets it is possible to direct the disposition of the NANs to the tracheobronchial (4–7 µm droplet diameter) or alveolar region (1–3 droplet diameter µm) [9]. Nevertheless, systemic administration is still the best delivery route if the NANs need to transfect the endothelial cells of capillaries that supply blood to e.g. lung tumors. Respiratory stem cells are interesting targets for genetic diseases like CF [10]. However, NANs can only reach these respiratory stem cells after opening of the tight junctions between epithelial cells or alveolar cells.
The therapeutic efficiency of nucleic acid delivery to the lungs depends on the capacity of the NANs to overcome the different barriers towards respiratory gene therapy. To be effective, NANs have to (1) withstand the shear forces during nebulization, (2) overcome the mucus layer that covers the conducting airways, or the liquid layer in the alveoli, (3) overcome antibodies and macrophages (if they are not the target cells), (4) enter the target cells and (5) escape from the endosomes. Additionally, if the therapeutic nucleic acids are genes than the NANs or genes also have to enter the nucleus. In this review we will focus on the extracellular barriers encountered by pulmonary delivered NANs on their way to epithelial cells, pneumocytes and lung macrophages. It is not the goal of this review to discus the other barriers mentioned above or to summarize the outcome of all in vivo experiments or clinical trials in the field of respiratory gene therapy. The latter has been covered by some recent reviews [1], [3], [4]. To allow the reader to gain insights into the mechanism by which extracellular fluids in the lungs may affect the performance of NANs we will start the review with a brief introduction to the biochemical and physical properties of especially respiratory mucus and alveolar fluid. This part will be followed with an overview and discussion of the scientific papers that deal with the behavior of NANs in the different extracellular secretions present in the respiratory tract. Most of the efforts in respiratory gene therapy have focused on CF gene therapy. Therefore, special attention will be given to the extracellular barriers in CF gene therapy. CF is the most common lethal autosomal-recessive disorder in Caucasians, affecting approximately 1 in 2000 newborns, and is characterized by the presence of tenacious mucus in the lungs, intestines and vagina [11]. However, fifteen years of pre-clinical and clinical research, using both viral and non-viral NANs, has revealed that the delivery of the CFTR gene to the lung epithelium of CF patients is a very difficult task. Extracellular barriers play an important role in the failure of CF gene therapy. In the last part of this review we will discuss the strategies that have been evaluate to overcome the different extracellular barriers in respiratory gene therapy. Additionally, we will also suggest new strategies that may enhance the success of respiratory gene therapy.
2. Biochemical and physical aspects of respiratory secretions
2.1. Respiratory mucus
The air we daily inhale contains besides gas also dust, toxic substances and pathogens. Therefore, the lungs have developed ingenious mechanisms to remove and/or neutralize these alien materials. One of the most important defense mechanism against these inhaled materials is respiratory mucus, which lines the respiratory epithelium from the nose to the terminal bronchioles [12]. This mucus layer lays on the tips of the cilia which bath in a periciliary fluid layer. Inhaled materials are captured in this blanket of mucus and are together with the mucus continuously transported by the cilia to the esophagus. The physical properties of respiratory mucus determines the efficiency of this mucociliary clearance mechanism [13]. Indeed, in lung diseases characterized by very tenacious mucus the mucociliary clearance is impaired and elimination of mucus occurs via coughing [14], [15]. The thickness of the mucus layer depends on the location in the airways and the presence of a pathologic condition. Although very difficult to determine, it has been reported that in non-pathological conditions the thickness varies between 10 and 30 µm in the trachea and between 2 and 5 µm in the bronchi [16], [17]. However, other reports claim that the thickness of the mucus layer can vary between 5 and 260 µm [18]. In CF and other respiratory diseases the mucus layer is much thicker [19].
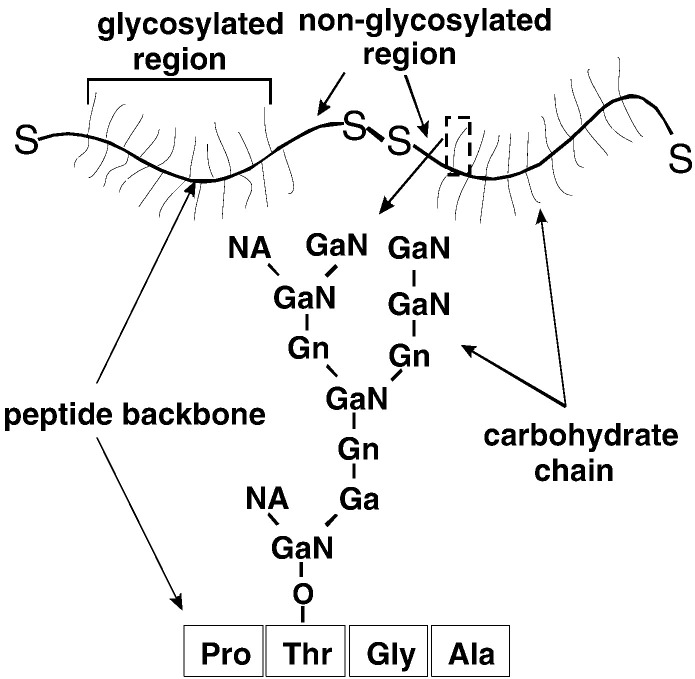
Respiratory mucus is mainly composed of a three-dimensional network of cross-linked mucin chains which gives the mucus viscoelastic properties [20], [21], [22]. The Globlet cells and submucosal glands are the producers of these mucins. Mucins are built up by 4 to 5 subunits which are bound together head-to-tail by intramolecular disulfide bridges (Fig. 1 ) [23]. The subunits, which have a length of about 500 nm, consist of a highly glycosylated protein backbone with non-glycosylated ends [24]. The molecular weight of mucins varies from 2 to 16 MDa. Mucins are negatively charged due to the presence of N-acetylneuramic acids (also called sialic acids) and sulphated monosaccharides in the sugars chains [23], [24]. The latter can contain 1 to 20 sugar monomers and they are covalently linked through O-glycosidic bounds between N-acetylgalactosamine and serine or threonine residues. It is important to realize that each epithelial layer secretes its own characteristic mucins. Therefore, the biophysical characteristics of mucus depend on the location in the body. In the respiratory tract two types of mucins are mainly expressed: MUC5AC and MUC5B [25]. Additionally, it has been found that the glycosylation pattern of these respiratory mucins is altered in CF patients [26].
Fig. 1.
Schematic representation of human respiratory mucins and their carbohydrate side chains. Mucins consist out of up to 5 subunits attached to each other by disulfide bonds. These subunits are highly glycosylated proteins with non-glycosylated ends. The depicted carbohydrate chain is only illustrative. Ala, Gly, Pro, Thr, Ga, GaN, Gn, and NA correspond respectively to alanine, glycine, proline, threonine, galactose, N-acetylgalactosamine, N-acetylglucosamine, and N-acetylneuraminic acid (adapted from Ref. [120]).
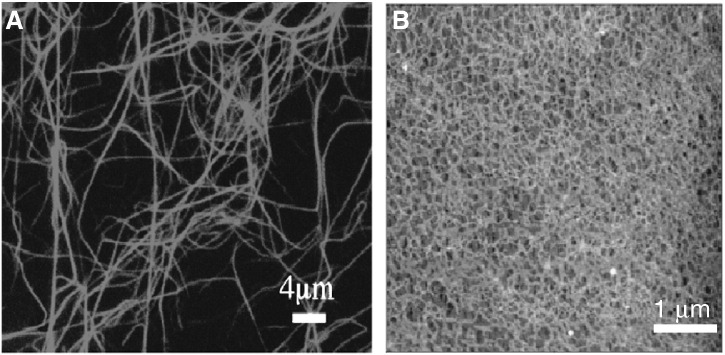
The concentration of the different constituents and the physical properties of normal respiratory mucus have not been studied in detail as it is very difficult to collect normal lung mucus. Therefore, many studies were performed on mucus obtained from patients having mucus hypersecretion (e.g. patients with CF and chronic obstructive pulmonary diseases (COPD)). Nevertheless, in non-pathological mucus the mucin concentration is about 20 g/l [27], [28]. In CF sputum (i.e. respiratory mucus expectorated by CF patients) slightly lower mucin concentrations have been found [29], [30] (Table 1 ). However, higher mucin concentrations (up to 47 g/l) were found in CF patients that produce very tenacious sputum [31]. Table 1 gives an overview of the concentration of the most abundant compounds in CF sputum. The water content in sputum from CF patients is about 90%, while mucus of healthy individuals contains about 95% water. Besides mucins and water, mucus also contains proteins, lipids, proteoglycans and electrolytes [20], [22], [32]. The major proteins in respiratory mucus are albumin, proteases, anti-proteases, immunoglobulins, lysozyme and lactoferrin [33]. The respiratory secretions of patients with cystic fibrosis or respiratory infections also contain huge amounts of DNA and actin (Table 1). These biopolymers are derived from neutrophils, epithelial cells and pathogens that died and subsequently released their intracellular content in the mucus. DNA and actin have like mucins a high molecular weight and can cross-link and thereby form a DNA or actin gel (Figs. 2 A and B) [34], [35]. These properties of DNA and actin drastically increase the viscoelasticity of CF mucus. Additionally, mucin, DNA and actin chains can also interact physically (by entanglements) and chemically (by hydrogen bonds, electrostatic and hydrophobic interactions) with each other [36], [37]. Interestingly, a tight binding between respiratory mucins and lipids has been reported [38]. Such interaction may make the mucin chains more hydrophobic. These interactions between mucus constituents make (CF) mucus one of the most complex biopolymer networks.
Table 1.
Biochemical composition and viscoelasticity of CF sputum
| Calcium (mM) | 3.0 ± 0.7 |
| Chloride (mM) | 81 ± 18 |
| Bicarbonate (mM) | 11 ± 6 |
| Inorganic phosphate (mM) | 13 ± 7 |
| Magnesium (mM) | 1.7 ± 0.6 |
| Potassium (mM) | 20 ± 3 |
| Proteins (mg/ml) | 26 ± 16 |
| Sodium (mM) | 92 ± 14 |
| Osmolality (mosmol/kg) | 256 ± 47 |
| DNA (mg/ml) | 3 ± 2 |
| Mucin (mg/ml) | 17 ± 7 |
| Total (G + F) actin (mg/ml) | 0.07 ± 0.03 |
| Elastic modulus (Pa) | 8 ± 6 |
| Viscous modulus (Pa) | 2 ± 1 |
The viscoelasticity was determined by a rotation rheometer (AR 1000, TA-Instruments) using a cone-plate geometry. Twenty two CF sputa were analyzed and the mean values (± standard deviations) are shown.
Fig. 2.
Confocal image of a network of polymerized actin filaments (0.01 mg/ml) in the presence of MgCl2 (80 mM) (A) and atomic force microscopy image of a DNA network (100 µg/ml) (B) (reproduced from Refs. [34] and [35]).
2.2. Alveolar fluid
The alveolar epithelium is covered with a thin continuous layer of pulmonary surfactant which comprises phospholipids and specific surfactant-associated proteins and which are synthesized and secreted by type II alveolar cells. The aqueous alveolar subphase lying between the pulmonary surfactant film and the alveolar epithelium has an average thickness ranging from 0.18 µm above flat alveolar walls to 0.89 µm in the alveolar corners. The major function of pulmonary surfactant is to reduce surface tension at the air–water interface of the terminal airways, thereby reducing the tendency of alveoli to collapse [39].
The detailed composition of the pulmonary surfactant was characterized from biochemical analysis of bronchoalveolar lavage fluid (BALF) and is composed of lipids (90%) and proteins (10%) [39]. Although the lipids are ultimately responsible for the reduction of the surface tension during inhalation and expiration, surfactant-associated proteins are suggested to assist within this process. About 80% of the lipids are phophatidylcholins (PC). The most abundant PC (50%) is the zwitterionic dipalmitoylphospatidylcholin (DPPC). This PC substantially contributes to the unique properties of pulmonary surfactant [40]. The residual PC in surfactant primarily consists of molecular derivatives containing monoenoic and dienoic fatty acids and minor amounts of short chains or polyunsaturated acyl groups. The acidic and thus negatively charged phospholipids, phosphatidylglycerol (PG) and phosphatidylinositol (PI), account for 8–15% of the total surfactant phospholipids. Low levels of phophatidylserine (PS) are also present in BALF. The positively charged phosphatidylethanolamine (PE) accounts for 3–5% of the total surfactant phospholipids. In addition, neutral lipids such as cholesterol are found at varying levels in pulmonary surfactant [40].
The protein fraction in BALF contains a highly variable amount of serum proteins (50–90% of the total amount of proteins) and proteins specifically expressed from the lungs, among which four surfactant proteins [41]. The surfactant proteins (SPs) have been termed SP-A, -B, -C, and -D. Whereas the hydrophilic surfactant proteins SP-A and SP-D play essential roles in pulmonary immune defense, SP-B and SP-C lower the surface tension, facilitate formation and stabilization of the surfactant film. The major proteins found in BALF are albumin (50%), transferrin (5–6%), α1-antitrypsin and immuglobulin A and G (together 30%) [42]. These proteins originate either from plasma or are expressed from the lung tissue. In some cases proteins may be both derived from plasma and secreted from the lung tissue, e.g. α1-antitrypsin [43]. The total protein concentration can only be roughly estimated from the dilution of ALF and is approximately 54 mg/ml [44]. The concentration of albumin which is the predominant protein in the ALF is approximately 19 mg/ml. Finally, nucleic acids, mucins and glycoproteins and massive amounts of white blood cells are found in BALF [44].
BALF also protects the alveoli against pathogens. Indeed, inhaled pathogens can become opsonized by SP-A, SP-D, and immunoglobulins and subsequently eliminated via alveolar macrophages [45]. Therefore, alveolar fluid represents a critical immunological barrier which has to be overcome by NANs before they can bind to the apical membrane of pneumocytes. Additionally, the charged compounds in (B)ALF may also interact with NANs and thereby change their surface properties or even disrupt the NANs. These fatal interactions will be discussed in Section 4.
3. Respiratory mucus as a barrier towards pulmonary gene therapy
Three phenomena may prevent that inhaled or intratracheal instillated NANs reach the lung epithelium. First, the biopolymer network that builds up the mucus may hinder the diffusion of NANs by sterical obstruction or by binding the NANs. Second, non-cross-linked (i.e. free moving) (macro)molecules may also bind to the surface of the NANs. The latter can lead to aggregation of the NANs which will further impede their capacity to move through the meshes of the biopolymer network in mucus. Additionally, even when no aggregation occurs, it has been reported that the binding of extracellular compounds to the surface of NANs may drastically decrease their gene transfer capacity [46]. Third, as mentioned above, the mucus blanket is continuously removed via mucociliary transport or coughing. Therefore, the NANs should be able to cross the mucus layer before they are cleared from the respiratory tract. The respiratory cilia transport mucus at a rate of 3.6 mm/min [47]. However, this speed of mucus clearance may drastically change in pathological situations like cystic fibrosis [48]. Therefore, both the diffusion coefficient of the NANs in the mucus, the thickness of the mucus layer and the rate of mucus clearance will determine whether the NANs will reach the epithelial cells. In this section we will first focus on the transport of NANs, or nanoparticles that are often used as simple models for NANs, through respiratory mucus. Subsequently, the interactions of NANs in respiratory mucus will be discussed. In this review we only considered respiratory mucus, as we expect that the transport and interaction of NANs in other types of mucus is not completely representative for respiratory mucus. For example, the mobility of nanospheres is much lower in cervical mucus than in CF or COPD mucus [49], [50], [51]. Additionally, cervical mucus has another biochemical composition than respiratory mucus and a much lower viscosity than COPD or CF mucus.
3.1. Mobility of NANs in respiratory mucus
Information on the mobility of NANs in respiratory mucus is very scarce. However, polystyrene nanoparticles have been used in several papers to gain insights into the mobility of nanosized drug carriers in respiratory mucus. To our knowledge three groups have so far studied the mobility of nanosized particles in respiratory mucus. The findings of these three groups are reviewed in this section.
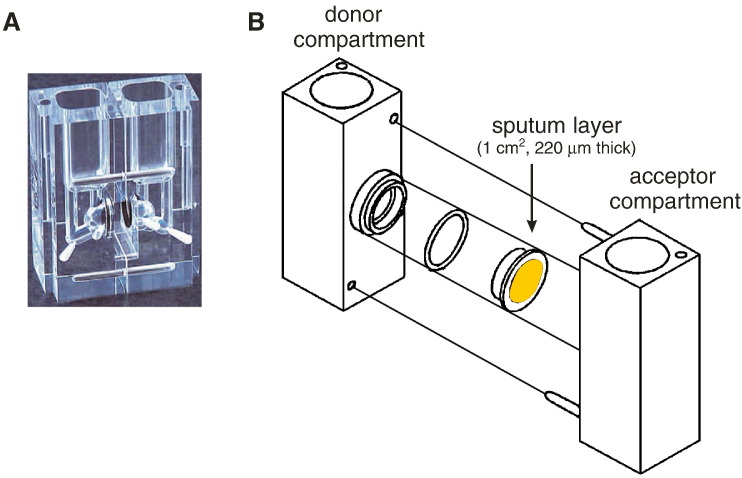
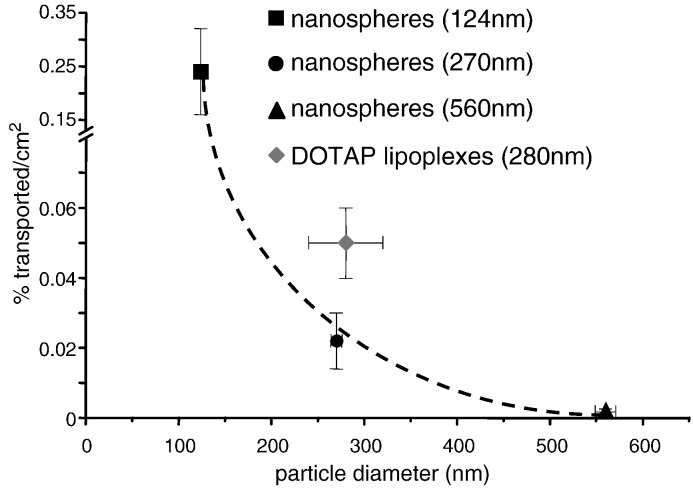
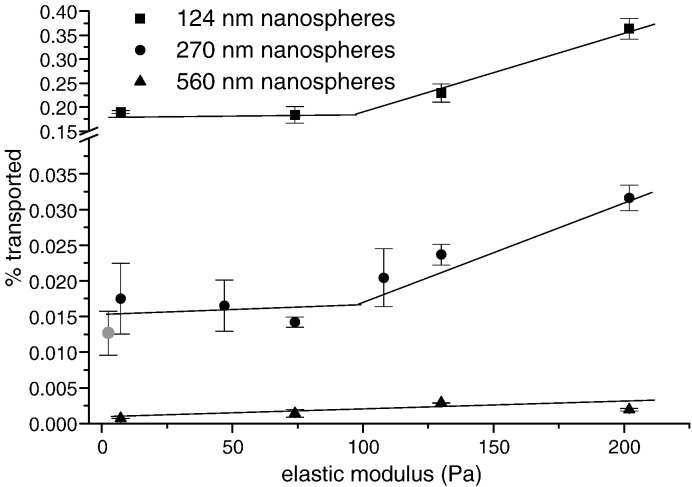
Our group evaluated as first the transport of negatively charged (polystyrene) nanospheres and cationic lipoplexes (i.e. complexes of nucleic acids with cationic liposomes) through sputa from CF patients [49], [52], [53]. In these experiments we sandwiched a 220 µm thick layer of CF sputum between the donor and acceptor side of vertical diffusion chambers (Fig. 3 ) [49]. The number of nanospheres and lipoplexes transported after 150 min through this CF sputum layer was very low (< 0.5% of total number of particles present at the donor side) and strongly depending on the size of the particles (Fig. 4 ) [49], [52]. The transport of 120 nm, 270 nm and 560 nm nanospheres through an equal sized buffer layer was respectively 1.3-fold, 6.8-fold and 42-fold higher than through CF sputum. As the smallest nanospheres were retarded by CF sputum only by a factor of 1.3, we hypothesized that the meshes in CF sputum must be large enough to allow a more or less free passage of these nanospheres. These data also indicate that for small particles (~ 120 nm) the low transport through the CF sputum is primarily due to the distance (i.e. the thickness of the sputum layer) the particles have to travel. For larger particles (~ 270 nm) the low transport through CF sputum is due to both the latter phenomenon as well as steric obstruction of the particles by the biopolymer network in CF sputum. The fact that the largest nanospheres (~ 560 nm) almost do not move through the CF sputum may indicate that most of the meshes between the biopolymers in CF sputum are too small to allow free passage of these nanospheres. Indeed, via scanning electron microscopy we found that CF sputum contains many small meshes (~ 100 nm), a few meshes 100 and 300 nm, and almost no meshes > 500 nm (Fig. 5 ) [49]. Similar mesh sizes have recently been detected in CF sputa via atomic force microscopy (AFM) [37]. The mean mesh sizes (± standard deviation) determined by AFM in 3 CF sputa were 300 ± 106 nm, 578 ± 191 nm and 711 ± 328 nm [37]. Although, these mesh sizes are larger than the ones derived from the electron microscopy pictures of CF sputum, they are still not large enough to allow completely unhindered passage of 560 nm nanospheres. Finally, we unexpectedly observed that the nanospheres diffused more easily through the most viscoelastic sputa (Fig. 6 ) [49]. To explain this we hypothesized that in highly viscoelastic sputa the higher amount of entangling biopolymers enables the formation of a more heterogeneous macroporous network with meshes that contain a limited number of free biopolymers. The viscosity in these meshes, i.e. the microviscosity, will determine the mobility of nanospheres in CF sputa. Of course the latter only holds true if the nanospheres are small enough to enter the meshes in the sputa. In CF sputa with a low viscoelasticity a more homogeneous microporous network with many free biopolymers in the meshes is probably present. Therefore, the microviscosity in low viscoelastic sputa is probably higher than the microviscosity in high viscoelastic sputa. Hence, nanoparticles in such low viscoelastic sputum will experience a higher viscous drag than in a more viscoelastic sputum. Based on this hypothesis degradation of the biopolymer network in CF sputum by mucolytic drugs may not be the most ideal strategy to enhance transport of nanoparticles through mucus. Indeed, cleave of the biopolymer network will not only increase the mesh size, but also the viscous drag in the meshes between the biopolymers. The latter effect is expected as the cleaved polymer fragments will be released in the meshes of the network. From the perspective of a diffusion particle these two effects are counteracting. The increase in mesh size gives the nanoparticles more ‘space’ to move through the sputum, but the increasing number of free polymers in the meshes will slow them down. The effects of mucolytic agents on the transport of nanoparticles and on the gene transfer capacity of NANs are discussed in more detail in Section 5.1.1.
Fig. 3.
Photo (A) and schematic drawing (B) of the vertical diffusion chambers. A thin CF sputum layer was placed between the donor and acceptor sides using modified snapwells. Snapwells containing a polycarbonate membrane (pore size 3 µm) were modified by gluing a 220 µm thick ring on their borders. This ring was filled with CF sputum and sealed with a second polycarbonate membrane. Finally, the modified snapwell was placed between the donor and acceptor side. The diffusion experiments were started by filling the donor side with nanoparticles or NANs and the acceptor side with buffer. Subsequently the transport of nanoparticles or NANs through the sputum layer was followed by measuring, at the desired time points, their concentration at the acceptor side.
Fig. 4.
Percentages of nanospheres and DOTAP/DOPE lipoplexes that crossed a 220 µm thick layer of CF sputum after 150 min as a function of the average size of the particles (n = 4) (reproduced from Ref. [53]).
Fig. 5.
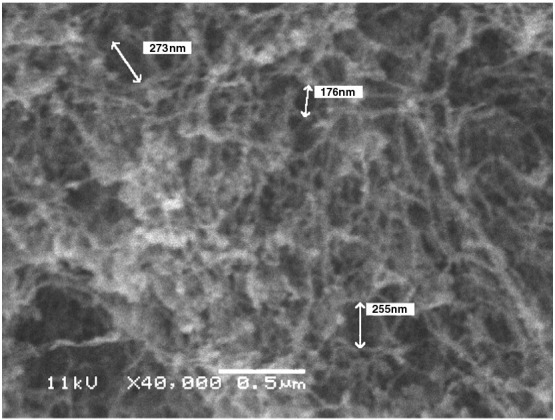
Scanning electron microscopic image of CF sputum showing the meshes in the biopolymer network. The CF sputum samples were processed as previously described [49] (reproduced from Ref. [49]). Bar = 0.5 µm.
Fig. 6.
Percentages of nanospheres (per cm2) that crossed a 220 µm thick layer of CF or COPD (gray circle) sputum after 150 min as a function of the elastic moduli of the sputum samples (n = 4) (reproduced from Ref. [49]).
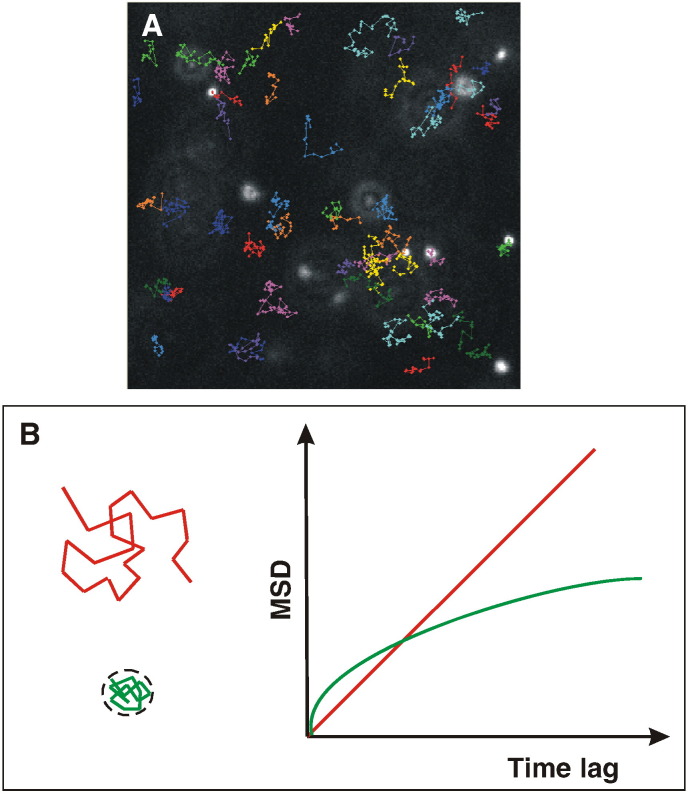
The group of Justin Hanes used multiple particle tracking (MPT), also sometimes indicated as single particles tracking (SPT), to gain more insights into the diffusion characteristics of individual nanospheres in CF sputum [50], [54]. In MPT the trajectories of about ten nanospheres, that are fluorescent labeled, are simultaneously followed by collecting sequential images with an epi-fluorescence microscope equipped with a fast and sensitive CCD camera [55], [56] (Fig. 7 ). After analysis of the images and localization of the nanospheres, it is possible to reconstitute the trajectory of each nanosphere. From this trajectory it is possible to calculate the distance (mean square displacement, MSD) the nanospheres traveled during a certain timeframe. This MSD can be related to the diffusion coefficient through different models, depending on the type of motion. In the work of Dawson et al. the trajectories of negatively charged polystyrene nanospheres of varies diameters (100, 200 and 500 nm as defined by the supplier) was monitored in CF sputum [50]. The average diffusion coefficient of the 100, 200 and 500 nm nanospheres in CF sputum as measured with MPT was 300-fold, 500-fold and 2400-fold lower than in buffer. In the work of Sanders et al. CF sputum caused a much lower retardation of nanospheres [49]. However, it is important to stress that MPT revealed that the transport rates of individual nanospheres in one CF sputum sample showed a very broad distribution. Indeed, a small fraction of the 100 and 200 nm nanospheres showed transport rates that were up to 40-fold higher than the average transport rate of the whole population [50]. Such a fast-moving fraction was not observed with the 500 nm nanospheres [50]. This fraction of highly mobile nanospheres was probably measured in the work of Sanders et al. [49]. The existence of a fraction of nanospheres that can rapidly move through CF sputum may indicate that there are a limited number of consecutive large meshes that form ‘transport highways’ for the 100 and 200 nm nanospheres. Therefore, it will be crucial that NANs find these channels and do not get lost in too narrow or/and twisting side roads [51]. Additionally, MPT also detected fluctuations in the speed of an individual nanosphere [50]. This has been attributed to the temporal ‘caging’ of the nanospheres in region of the sputum where the mesh sizes are too small to allow free diffusion. By studying the trajectories of individual nanospheres in CF sputum the group of Hanes et al. was also able to probe the microviscosity that these nanospheres encountered in the CF sputum [50]. Interestingly, the encountered microviscosity by the 100- and 200 nm nanospheres was respectively 15- and 7-fold lower than the sputum macroviscosity measured with a rheometer. The fact that the 200 nm nanosphere sense a higher apparent viscosity is probably due to a partial steric hinder of these nanospheres by the biopolymer network in CF sputum, as suggested by Sanders et al. [49]. Finally, Dawson et al. also found that negatively charged polystyrene nanospheres bound, probably via hydrophobic interactions; more strongly to the biopolymers in CF sputum than neutral polystyrene nanospheres [50]. Via fluorescence recovery after photobleaching (FRAP) we also found that small polystyrene nanospheres (89 nm as measured via dynamic light scattering) become immobilized in certain regions within CF sputum [57]. Furthermore, coating of these polystyrene nanospheres with polyethylene glycol strongly decreased their binding to biopolymers present in cervical mucus [51]. The binding or interaction of mucus compounds with NANs will be discussed in more detail in Section 3.2.
Fig. 7.
Principle of multiple particle tracking. In a MPT experiment a high-speed film is recorded of particles. If the particle size is below the microscope's resolution limit, they are seen as dots of light with a Gaussian intensity distribution. However, with suitable image processing software, one can determine the centre of the particles with very high accuracy, typically in the order of tens of nanometers. By determining the position of the particles in all frames of the MPT film, trajectories can be calculated for each individual particle as shown in A (colored lines). The mean square displacements (MSD) of the trajectories can be used for further quantitative analysis in terms of the mode of motion (free diffusion, directed transport, etc.) and the corresponding quantitative parameters (diffusion coefficient, velocity). In B the trajectories of free-diffusing (red) and confined (green) particles are shown. The graph on the right depicts the corresponding MSD of a particle as a function of lag time. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Finally, the group of Janis Shute et al. used micro-Boyden chambers to study the diffusion of 200 nm negatively charged polystyrene nanospheres in CF sputum [35], [37]. In their experiments they mixed the nanospheres with CF sputum. Subsequently, the sputum with the nanospheres (10 µl) was transferred to the upper chamber of the diffusion chamber that was separated from the lower chamber (that was filled with 50 µl of buffer) by a membrane with a pore size of 8 µm. After 1 h they measured the amount of nanospheres in the lower compartment. Compared to nanospheres mixed with buffer (control), CF sputum caused a 10- to 20-fold decrease in transport [35], [37].
3.2. Fatal interactions of NANs with respiratory mucus
Non-viral NANs are built up by cationic lipids or polymers, which bind the therapeutic DNA or RNA by electrostatic interactions [58]. The first generation of non-viral NANs also had a positively charged surface. Additionally, it is important to realize that also certain viruses like herpes simplex virus and certain retroviruses have a positive surface charge [59], [60]. Consequently, one can expect that viral NANs based on these viruses will bind via charge interactions to negatively charged components present in mucus. Additionally, other components in mucus like antibodies may interact with NANs [61], [62]. These interaction of NANs with mucus compounds may cause (1) entrapment of the NANs in the mucus, (2) aggregation of the NANs due to neutralization of their surface charges, (3) release of therapeutic DNA/RNA from non-viral NANs, (4) an inefficient cell binding of the NANs due to shielding of their positive charges or their receptor binding ligands, and (5) endosomal entrapment of NANs. All these effects will strongly impede the gene transfer efficiency of NANs in the presence of mucus. Information on the interactions of NANs with respiratory mucus is scarce. Nevertheless, different researchers reported that negatively charged as well as neutral polystyrene nanospheres bind to filaments present in CF sputum and cervical mucus [51], [57]. This indicates that these negatively nanospheres can adhere to polymer filaments via hydrophobic interactions as these filaments are also negatively charged. Additionally, is has been shown that cationic herpes simplex viruses stick to the mucin filaments present in cervical mucus [63]. All these data indicate that NANs may be prone to interactions with respiratory (CF) mucus. Due to the lack of other reports on this topic we will in this section mainly focus on our data.
We examined the influence of individual CF sputum components and diluted CF sputum on the physicochemical stability and gene transfection activity of cationic DOTAP/DOPE lipoplexes [31]. Incubation of these lipoplexes with increasing amounts of albumin, linear DNA and mucin decreased and reversed the surface charge of these NANs. This clearly indicates that these negatively charged CF mucus components bind to cationic NANs. Moreover, at the cross-over point from positive to negatively charged lipoplexes we observed a massive aggregation of the lipoplexes and a strong reduction of their gene transfer efficiency. The latter was probably due to a decreased internalization of these large aggregates. Interestingly, higher amounts of albumin and linear DNA created an anionic shield around the lipoplexes that protected them against aggregation. Remarkably, these albumin or linear DNA covered lipoplexes did not have significant decreased gene transfer efficiencies in vitro, although linear DNA, but not albumin, released small amounts of pDNA from the lipoplexes. In contrast, binding of mucins strongly decreased the gene transfer of the DOTAP/DOPE lipoplexes without causing large aggregates or dissociation of the lipoplexes. This indicates that mucins alter (intra)cellular steps in the transfection process of these lipoplexes. Finally, cationic DOTAP/DOPE lipoplexes did not or very slightly release pDNA after incubating them with diluted CF sputa obtained from patients with respectively moderated or severe lung infections. In contrast, a massive dissociation of cationic DOTAP/DOPE lipoplexes was observed when they were incubated with diluted synthetic sputum (i.e. a mixture of albumin, linear DNA, mucin and lung surfactants). It is known that the network structure in CF sputum cannot be simulated by simply mixing of CF sputum constituents. In synthetic sputum the CF sputum components are not well cross-linked and thus more available for fatal interactions with NANs. Similarly, dilution of our CF sputa may have liberated CF sputum components from the polymer network that would otherwise not been able to bind on the surface of the lipoplexes. Consequently, the observed dissociation of NANs in the presence of CF sputum compounds or diluted CF sputum may have generated data that overestimate the potential disintegration of NANs in undiluted CF sputum.
3.3. Effect of respiratory mucus on the gene transfer efficiency of NANs
The group of Alton et al. studied the effect of normal respiratory mucus and CF sputum on the gene transfer capacity of lipoplexes, polyplexes and adenoviral vectors [64], [65], [66], [67]. In their first paper they covered cell cultures with a 2 mm thick layer of diluted CF sputum [64]. The least diluted sputa (i.e. 1:1 diluted with culture medium) caused a 20-fold reduction of the gene transfer efficiency of both DC-Chol/DOPE based lipoplexes and adenoviral vectors. Strikingly, highly diluted sputa (i.e. 100-fold) also caused a drastic reduction in gene transfer of adenoviral vectors and especially lipoplexes. This indicates that CF sputum is not only a diffusion barrier for NANs, as at such high dilutions the polymer network and sputum viscosity is expected to be disrupted and drastically reduced, respectively. The fact that CF sputum is not only a diffusion barrier was further supported by the observation that removal of the diluted CF sputum, by washing with phosphate buffered saline (PBS), before addition of the lipoplexes did not restore the gene transfer capacity of the lipoplexes. Furthermore, incubation of cells with a DNA solution containing > 100 µg/ml genomic DNA and removal of this DNA solution before lipoplex mediated transfection still caused a 10-fold decrease in gene transfer. Additionally, the capacity of lipoplexes and adenoviral vectors to transfect cells that had been exposed to CF sputum or a DNA solution was respectively partly and completely restored when the cells were incubated with rhDNase before transfection. Consequently, all these observations indicate (1) that DNA present in CF sputum strongly binds to epithelial cell surfaces, (2) that this cell associated DNA drastically limits the gene transfer of both lipoplexes and adenoviral vectors and (3) that rhDNase increases the gene transfer in cells that have been exposed to CF sputum by removing the DNA that became bound to the cell surface.
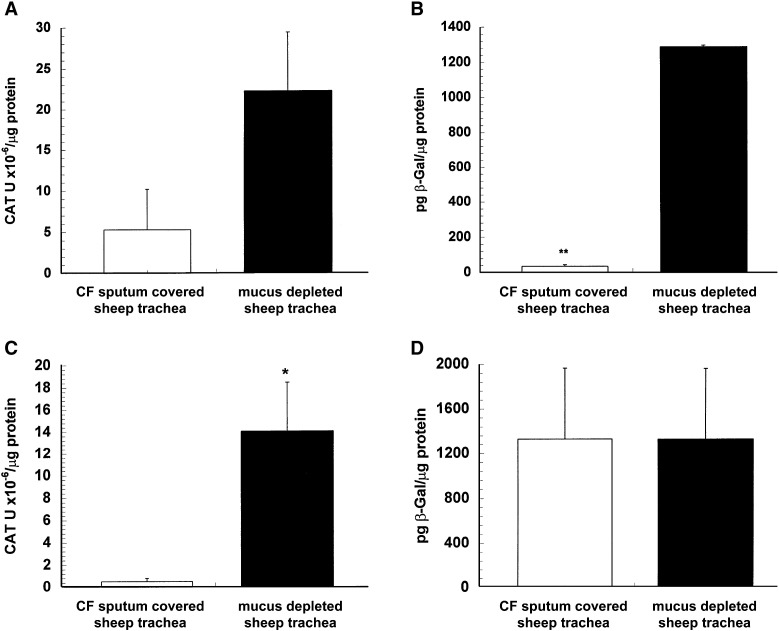
Later on the group of Alton et al. also evaluated the effect of undiluted CF sputum on the transfection efficiency of NANs [65]. In this study sheep tracheae were covered with a 1.5 mm thick layer of CF sputum and the ability of GL67/DOPE based lipoplexes and adenoviral vectors to transfect the underlying epithelium was determined and compared to the transfection efficiency in the absence of CF sputum. The efficiency of both NANs was significantly decreased by CF sputum. Surprisingly, adenoviral vectors were much more affected by the CF sputum layer than the lipoplexes. In the presence of CF sputum the gene transfer of lipoplexes and adenoviruses was respectively 5- and 35-times lower (Figs. 8 A and B) [66].
Fig. 8.
Effect of CF sputum (upper panels) and normal respiratory mucus (lower panels) on the in vitro gene expression of cationic GL67/DOPE based lipoplexes (A and C) and adenoviral vectors (B and D) in sheep tracheae. Error bars indicate standard error of the mean. (n = 6, ⁎p < 0.05, ⁎⁎ p < 0.01) (reproduced from Ref. [65]).
The ex vivo sheep trachea model has also been used to evaluate the effect of normal (sheep) respiratory mucus on the gene transfer capacity of lipoplexes, polyplexes, sendai and adenoviral vectors [66], [67]. Interestingly, these experiments demonstrated that normal respiratory mucus did not represent a barrier to adenovirus and sendai mediated gene transfer, while the gene transfer of both lipoplexes and polyplexes was ~ 30-fold lower in the presence of normal respiratory mucus (Figs. 8C and D) [66], [67]. They hypothesized that this result is related to the differences in surface charges between the non-viral and viral NANs. Indeed, lipoplexes and polyplexes are positively charged and hence more prone to electrostatic binding with mucins than the negatively charged viral vectors. Adenoviruses and sendai viruses seem to possess natural strategies to overcome normal respiratory mucus. This is not surprising as adenoviruses are causing the common cold. Hydrophobic interactions play a role in the formation of a mucin gel [68]. Therefore, it is possible that viruses like adenoviruses have hydrophobic moieties on their surface that can disrupt the hydrophobic cross links between mucins. However, it has been reported that transmembrane mucins, such as MUC1, strongly impedes adenoviral gene transfer [69].
Finally, we want to remark that in CF patients the amount of inhaled NANs that come in contact with 1 cm2 of CF sputum will be much lower than the amount of NANs used in vitro by Alton's group and by Sanders et al. [53], [70]. Therefore, one has to realize that the chance that NANs can overcome the CF sputum barrier in vivo is most likely highly underestimate by these in vitro experiments and also by in vivo experiments in mice. Indeed, in the latter experiments the ratio between the administered pDNA dose and lung surface is much higher than can be achieved in CF patients.
4. Alveolar fluid as a barrier towards pulmonary gene therapy
Upon topical delivery of NANs to the lung periphery they will encounter the lipids of the pulmonary surfactant layer as the very first endogenous interface in the alveolar region. Therefore, the influence of the pulmonary surfactant lipids on the particle characteristics and their transfection efficiency has been intensively investigated [71], [72], [73]. A general finding of these studies is that the presence of both synthetic and especially naturally derived surfactant preparations results in a dose-dependent transfection inhibition of cationic lipid based NANs. In contrast to naturally derived surfactant preparations, such as the commonly used product Alveofact®, synthetic surfactant preparations (e.g. Exosurf®) do not contain surfactant proteins and anionic lipids. It has been reported that especially these negatively charged lipids inhibit gene transfer mediated by cationic lipoplexes [73]. It has been suggested that this inhibitory effect results from disintegration of the lipoplexes by the negatively charged lipids leading to accessibility of the pDNA to nucleases and thus its degradation and loss of function [73]. Therefore, pulmonary surfactant represents a critical barrier which leads to fatal interaction with lipoplexes. Interestingly, NANs derived from cationic polymers such as polyethylenimine (PEI) and dendrimers (PAMAM) have been demonstrated to be more resistant to detrimental effects by pulmonary surfactant. Neither PEI–pDNA nor PAMAM–pDNA complexes were inhibited by naturally derived and synthetic surfactant preparations in vitro [73], [74] and in vivo [75]. However, isolated negatively charged lipids from pulmonary surfactant resulted in comparable transfection inhibition as observed for lipoplexes. Therefore, it has been suggested that this inhibitory effect is compensated by other constituents of naturally derived surfactant, presumably the surfactant proteins, although this requires further detailed investigation [73]. A clear advantage of NANs derived from cationic polymers seems to be their increased complex stability which avoids complex disintegration by the surfactant lipids. Synthetic surfactants such as Exosurf® have been reported even to increase transfection efficiency of PAMAM–pDNA complexes [74]. These results illustrate that NANs derived from cationic polymers are not subject to fatal interactions with pulmonary surfactant lipids and may therefore be more suitable for gene delivery to the alveolar epithelium in vivo. However, commercial available lung surfactant preparations do not completely represent the liquid layer present in the alveoli. Therefore, Rosenecker et al. studied, via 2-D-gel electrophoresis, the interaction of NANs with the protein fraction present in human BALF. BALF proteins were absorbed more intensively to lipoplexes than to polyplexes [76]. In addition, glycosylated components of the BALF strongly bound to lipoplexes but only weakly to polyplexes. These interactions resulted in a 10-fold increase of the lipoplex diameter and a slight decrease of their surface charge, while the size of polyplexes was not affected but their surface charge changed from positive to negative. In both cases the interaction with the BALF did not lead to NANs disintegration as assessed by quenching assays, which reflects true binding of the BALF components to the NAN's surface. Interestingly transfection inhibition was stronger for polyplexes than for lipoplexes, although the latter were more prone to adsorption of BALF components [76]. A possible reason for this at first view opposing observation could be the loss of the positively charged polyplex surface, which has been suggested to be the precondition to initialize binding to the negatively charged cell surface and subsequent cellular uptake [77]. In summary, these observations demonstrate that both lipids and proteins present in BALF interact with NANs and are responsible for transfection inhibition. Although lipoplexes were generally more susceptible to interactions with BALF components than polyplexes, their transfection efficiency remained, in contrast to polyplexes, relatively unaffected in the presence of BALF.
5. Overcoming the mucus and alveolar fluid layer in pulmonary gene therapy
5.1. Increasing the mobility of NANs in respiratory mucus
5.1.1. Mucolytic agents
To facilitate their mobility in protective mucus layers certain bacteria, fungi and viruses secrete enzymes that hydrolyze mucins [78], [79], [80]. Therefore, many research groups evaluated the effect of different mucolytic agents, which either degrade actin, DNA or mucin, on the mobility of NANs and nanospheres in (CF) mucus [37], [49], [50], [67], [81]. However, as discussed above mucolytic agents that degraded the biopolymers that build up the three-dimensional polymer network in CF sputum will not only increase the mesh size, but also the viscous drag in the meshes between the cross-linked biopolymers. Therefore, we can expect that the effect of mucolytic agents on the transport of NANs and nanoparticles through especially CF sputum will be limited. However, this does not exclude that mucolytics have a positive effect on the transport of NANs or nanospheres through normal respiratory mucus, which has other biophysical properties than CF sputum. An overview of the reported effects of different mucolytics on the transport of nanospheres and on the gene transfer efficiency of NANs is given below.
5.1.1.1. rhDNase
Recombinant human DNase (rhDNase) is a clinically used enzyme that liquefies CF mucus by cleaving the DNA chains in CF mucus [82]. RhDNase is administered to CF patients via inhalation. The effect of rhDNase on the mobility of nanoparticles through CF sputum has been studied in only three reports. We showed that the transport of 270 nm polystyrene nanospheres and DOTAP/DOPE based lipoplexes was respectively 2.5- and 1.4-fold higher through sputa that were liquefied by rhDNase (6 µg rhDNase/ml) [49], [52]. Via MPT Dawson et al. showed that the average mobility of 200 nm polystyrene nanospheres was not altered in CF sputum that was liquefied by rhDNase (7 µg/ml) [50]. However, rhDNase decreased the spreading of the diffusion coefficients of the nanoparticles [50]. Finally, the group of Shute et al. also found no effect of rhDNase on the transport of the same nanospheres through ‘synthetic CF sputum’, i.e. a mixture of DNA, mucin and actin [37]. However, in additional experiments they demonstrated that the lack of any effect of rhDNase on the transport of nanospheres was due to an inhibition of rhDNase by actin [37]. Indeed, the magnesium concentration in their ‘synthetic sputum’ (1.2 mM) was to low to keep actin fully polymerized [30]. Therefore, significant amounts of actin monomers, which strongly inhibit rhDNase [30], are expected to present in their synthetic sputum. It has been proposed that gelsolin can also, besides depolymerizing actin, dissociate DNase–actin complexes [83]. However, the simultaneous addition of gelsolin and rhDNase did not restore the rhDNase activity nor increased the transport of nanospheres through ‘synthetic sputum’ [37].
5.1.1.2. N-acetylcysteine
N-acetylcysteine (NAC) and its derivatives lower the viscosity and elasticity of mucus by reducing the disulfide bonds between the subunits in mucins [13]. These mucin degrading agents can be administered orally or via inhalation. They are clinically used by e.g. asthma, COPD and CF patients to enhance the clearance of their respiratory secretions [84]. Interestingly, it has been reported that nacystelyn, a lysine salt of NAC, inhibits the maturation of dendritic cells and possess anti-inflammatory properties [85], [86]. These properties of nacystelyn may reduce the immune response against especially viral NANs. The effect of N-acetylcysteine based mucolytics on the efficacy of NANs or on the transport of nanospheres through mucus has been exclusive evaluate with normal respiratory mucus. This is probably due to the limited effects of these mucolytics agents on the viscosity and elasticity of CF sputum. Using the ex vivo sheep trachea model Ferrari et al. [67] demonstrated that the gene transfer of both ethyldimyristoylphosphatidyl choline/cholesterol (EDMPC/Chol) based lipoplexes and linear PEI based polyplexes was respectively ~ 20 and ~ 10-fold higher when the mucus covered epithelium was treated with nacystelyn or NAC before application of the NANs. Interestingly, intranasal administration of nacystelyn (150 µl; 100 mM) 30 min before intranasal application of the EDMPC/Chol based lipoplexes resulted in a 100-fold increase in gene expression in the nasal turbinates of mice [67]. Strikingly, nasal delivery of nacystelyn together with the lipoplexes did not enhance and even slightly decreased the gene transfer efficiency of the lipoplexes [67]. Also Kushwah et al. found that intranasal administration of nacystelyn (50 µl, 100 mM) together with diethylaminoethyl-dextran (DEAE-dextran) coated adenoviruses did not enhance the gene transfer efficiency in the lungs of mice [81]. However, intranasal administration of nacystelyn 30 min before the application of the DEAE-dextran coated adenoviruses significantly increased the distribution and the level of gene expression in the lungs of mice [81]. Therefore, the benefits of mucolytics on the gene transfer of NANs are probably compensated by an enhanced clearance of the NANs out the respiratory tract when NANs and mucolytic agents are administered together to the airways. Importantly, nacystelyn pretreatment did not enhance the gene transfer of uncoated adenoviruses in the lungs of mice [81]. This is in line with the observation that normal respiratory mucus did not represent a barrier to negatively charged adenoviral vectors in the ex vivo sheep trachea model of the group of Alton et al. [67]. Finally, nacystelyn did also not increase the transport of negatively charged polystyrene nanospheres (200 nm) through ‘synthetic CF sputum’ [37].
5.1.2. Magnetic forces
Magnetofection is a novel method to enhance the efficiency of NANs [87]. In this approach NANs are associated with magnetic particles and magnetic forces are used to pull the magnetic NANs towards the target cells and possibly also inside the target cells [87]. Magnetofection has been shown to increase transfection efficiency of NANs in cell cultures and in vivo [88], [89], [90]. Furthermore, Dames et al. demonstrated that aerosol droplets comprising superparamagnetic nanoparticles (SPIONs), so called nanomagnetosols, could be efficiently targeted to desired regions in the lungs of mice by application of external magnetic gradient fields during inhalation [91]. This is important progress towards deposition of higher dosages of NANs in the desired lung regions. We speculate that magnetic gradient fields may also pull magnetic NANs through the mucus or alveolar fluid barrier. Additionally, the usage of pulsed magnetic fields in addition to a target magnetic field [92] may further facilitate the uptake of magnetic NANs in respiratory cells.
5.1.3. Future approaches
5.1.3.1. Motorized NANs with mucolytic properties
Addition of mucolytic agents to mucus mainly results in a reduction of the macroviscosity. However, as discussed earlier, the mobility of small nanospheres (≤ 200 nm) in CF sputum is determined by the microviscosity (i.e. the viscosity in the meshes of the network) and not by the macroviscosity [50]. Therefore, to enhance the mobility of these nanoparticles in CF sputum, mucolytic agents should specifically lower the microviscosity by degrading the polymers present in the meshes. The latter will reduce the viscous drag that the diffusing nanoparticles encounter, without releasing extra polymers from the three-dimensional network into the meshes. On the other hand larger nanoparticles are often ‘caged’ in the meshes or even cannot enter the meshes present in the mucus gel. For these larger (> 200 nm) nanoparticles mucolytic agents should in the first place cut the filaments that build up the three-dimensional network. Therefore taking into account these considerations, we should give to NANs the capacity to specifically cleave these biopolymers that they encounter on their way through the mucus. This can be done by linking mucolytic enzymes to the surface of NANs and nanoparticles in general. Enzymes that can degrade mucin, DNA, actin, collagen or protein filaments are interesting candidates. Such functionalized NANs are expected to cut a way through the mucus. The observation that linkage of collagenase to nanoparticles enhanced their transport through the extracellular matrix proves that this idea may indeed work [93], [94]. Finally, we can also give extra speed to the NANs by attaching a ‘motor’ to their surface. This proposed strategy may sound quite futuristic. However, autonomous movement of nanosized objects has been obtained by putting chemical nanomotors to their surface [94], [95].
5.1.3.2. Ultrasound
Low-frequency (20 to 100 kHz) ultrasound has been used to enhance the transport of drugs and drug carriers through the skin via a mechanism described as sonophoresis [96]. Sonophoresis is mainly caused by acoustic cavitation, i.e. the formation, oscillation and collapse of gaseous microbubbles in a fluid exposed to ultrasound waves [97]. These bubbles are spontaneously formed by ultrasound when dissolved air is present in the fluid. Cavitation can either be stable or inertial. Stable cavitation corresponds to the periodic growth/shrinking of microbubbles. Inertial cavitation is defined as the violent growth and collapse of microbubbles. Due to the collapse of these bubbles shock waves and microjets are generated [97]. These effects may increase the velocity of NANs and the mesh sizes in mucus. In a recent study we observed that the transport of polystyrene nanospheres (500 nm; negatively charged) through CF sputum was 10-fold higher in the presence of low-frequency ultrasound (Sanders et al., unpublished data). In these experiments we used our vertical diffusion chamber setup (Fig. 3) [49] and exposed the CF sputum discontinuously (to prevent heating) to ultrasound. Taking into account that we used pulsed ultrasound the total exposure time to ultrasound was 2.3% of the duration of the transport experiment. Therefore, application of ultrasound for longer periods will probably cause more drastic increases. Although, these data are promising we want to remark that the application of ultrasound to the lungs is not simple. Indeed, ultrasound that enters the lungs from a source outside the body will be highly reflected by the air in the lungs. Therefore, to prevent this reflection of ultrasound by the air in the lungs one may also directly insert the ultrasound probe in the lungs, via a bronchoscope, as is done in bronchoscopic ultrasound examination of the tracheobronchial tree [98]. High-frequency ultrasound together with diagnostic microbubbles can increase the gene transfer efficacy of naked pDNA or NANs by temporarily perforating cell membranes [99]. Xenariou et al. recently found that an external high-frequency ultrasound source (1 MHz) combined with diagnostic microbubbles increased the gene transfer of naked pDNA in the lungs of mice [100]. These data may indicate that high-frequency ultrasound can reach the lung epithelial cells in mice. It is not know whether high-frequency ultrasound can also increase the transport of NANs through mucus.
5.2. Avoiding interactions of NANs with respiratory secretions
One of the most successful strategies to avoid interaction of NANs with components of biological fluids has been their modification with biocompatible hydrophilic but biologically inert polymers [58]. It is obvious that this concept may be applicable to pulmonary gene delivery, where reduction of interaction with mucus and alveolar fluid components is highly desirable. Shielding of NANs may not only be important to reduce interaction with mucus and alveolar fluid components but may also diminish clearance by alveolar macrophages which is considerably observed after aerosol delivery of non-shielded PEI polyplexes [101]. In this section we will first give an overview of the different strategies that can be used to avoid interaction of NANs with respiratory secretions. Subsequently we will discuss the behavior of shielded NANs in respiratory (CF) secretions. We will close this section with some critical remarks on PEGylation. Although the effect of mucolytic enzymes on the interaction of NANs with mucus components has not been studied in detail, one can expect that degraded mucus components will show less fatal interaction with NANs. Therefore, besides improving the mobility of NANs in (CF) mucus, mucolytic enzymes may also decrease the interactions of NANs with (CF) mucus components.
5.2.1. Strategies for shielding NANs
Extracellular components most often interact with NANs via charge and hydrophobic interactions. Therefore, the aggregation and the interaction of NANs with extracellular components can be prevented by shielding the positive surface charges of NANs with neutral hydrophilic polymers (e.g. polyethylene glycol (PEG)). NANs that bear such inert polymers at their surface can be obtained via two strategies. In the first strategy, which can only be used for non-viral NANs that are made via self-assembly, the cationic carrier is covalently coupled to the shielding polymer and subsequently mixed with the nucleic acids [102]. During the self-assembly the cationic carrier and the nucleic acids interact with each other and create a slightly hydrophobic core that is surrounded by a shield of hydrophilic polymers. This method has as disadvantage that the shielding polymers can, especially when high amounts of shielding polymer are used, hinder the self-assembling process between the cationic carrier and the nucleic acids. Therefore, post-shielding has been considered and involved the covalent attachment of the shielding polymer to pre-formed non-viral NANs [103], [104]. However, PEGylation also has back draws. Indeed, it is well known that PEG chains at the surface of NANs prevent endosomal escape, which has a negative effect on the biological efficiency of such shielded NANs. Therefore, different groups are currently making NANs that lose their PEG-chains at the cell surface or in acidifying endosomes [105].
Finally, the surface of charged NANs can also be modified by absorption of opposite charged polymers. For example, Cheung et al. [106] coated cationic non-viral NANs with poly(propylacrylic acid) (PPAA), an anionic polymer that can disrupt endosomal membranes, while Finsinger et al. [107] coated the cationic surface of NANs by using a PEG that was linked to negatively charged peptides. A drawback of this strategy is, however, that the stability of the ionic coating in blood or mucus is questionable and has not yet been demonstrated. This post-shielding strategy has also been applied to prevent recognition of viral NANs by the immune system and to enable retargeting of these viral NANs to a desired tissue [108], [109].
5.2.2. Behavior of shielded NANs in respiratory secretions
Lipoplexes based on the GL67 (genzyme lipid 67) lipid are one of the most successful NANs for gene delivery to the lungs [110]. In their optimized formulation these lipoplexes contain PEGylated lipids. Sanders et al. has comprehensively demonstrated the benefits of the presence of these PEG-lipids in these lipoplexes [111]. In contrast to the cationic DOTAP/DOPE lipoplexes, exposure of these PEGylated GL67/DOPE lipoplexes to CF mucus compounds (linear DNA, albumin, phospholipids and mucin), at concentrations expected to occur in vivo, did not affect their gene transfection activity [111]. Additionally, these PEG chains prevented that these GL67/DOPE lipoplexes became aggregated by the CF mucus compounds. Similar observations were made for PEG copolymer-protected PEI polyplexes which adsorbed only low amounts of serum-derived proteins and were virtually inert against mucin binding from BALF [112]. However, copolymer protection resulted in a strong decrease of transfection efficiency in the mouse lungs, which could be partially restored by coupling of transferrin as a targeting ligand [112]. An increase of the colloidal stability in the presence of BALF has also been observed for PEGylated and TAT peptide-modified PEI polyplexes [113]. Another approach which has been successfully performed to achieve high transfection efficiency of PEI polyplexes in the presence of CF sputum sol phase makes use of polyplex pre-incubation with serum albumin [114]. Although the underlying mechanism has not been entirely elucidated up till now, pre-incubation of PEI polyplexes with human serum albumin resulted in up to 80-fold higher transfection rates in the presence of CF sputum than without human serum albumin [114]. The authors speculate that the albumin-coated PEI polyplexes may have been targeted to albumin receptors which are expressed on the apical surface. In context with this observation coupling of targeting ligands to the NANs may represent a suitable approach to augment their transfection efficiency. An increase in gene transfer efficiency has been obtained in lung epithelial cells with various targeting ligands, like SP-B [115], UTP [116], mannuronic acid [117], and lactoferrin [118]. Coupling of targeting ligands to NANs may be of particular interest to increase their internalization kinetics by the targeted lung cells in terms of the fast clearance kinetics by the alveolar macrophages. Indeed, one has to consider that one microliter (1 mm3) of BALF contains roughly 19.000 alveolar macrophages [44].
In summary, these results allow us to conclude that shielding of NANs by e.g. polyethylene glycol favors their physicochemical stability and their gene transfer capacity in the presence of respiratory (CF) secretions.
5.2.3. Some critical remarks on PEGylation of NANs
The presence of e.g. PEG polymers on the surface of NANs prevents aggregation by avoiding that NANs can come in close proximity to each other during collision. However, the surface of NANs is often not completely covered with the shielding polymer. Therefore, between the shielding polymers gaps may be present that allow small charged molecules to reach the surface of the NANs. Indeed, we have for example observed that albumin (at concentrations found in blood) is able to penetrate between the PEG of siRNA–liposome complexes containing 5 mol% PEG–lipids and to cause the release of all the siRNAs [119]. Similarly, high amounts of albumin could release one third of the pDNA from PEGylated GL67/DOPE lipoplexes [111]. This indicates that albumin is on one hand small enough to penetrate between the PEG chains, and on the other hand large enough to allow a ‘thermodynamical’ competition with pDNA for binding to the cationic lipids. The anionic phospholipids present in lung surfactant were also able to dissociate these PEGylated GL67/DOPE lipoplexes [111]. However, the dissociation was very limited and only occurred when the lipoplexes were incubated with extreme high concentrations of lung surfactant. This indicates that the ‘thermodynamic power’ of these negatively charged phospholipids to push off the much larger pDNA molecules from the cationic liposomes is low. To prevent that small molecules, like albumin, can penetrate between the PEG-chains of PEGylated NANs one can either increase the degree of shielding or the chain length of the polymers. However, one should realize that for example long PEG chains (~ > 10 kDa) may entangle in the biopolymer network of biogels [51]. Therefore, particles containing such long PEG chains may become immobilized in mucus.
6. Conclusions and perspectives
During the design of new NANs for respiratory gene therapy one should take into account that respiratory secretions are present above the target cells. In this review we demonstrated that the size and the surface properties of especially non-viral NANs determine their behavior in respiratory secretions. A first key message is that the cationic surface of (non-viral) NANs should be shielded by neutral and hydrophilic polymers to prevent that these NANs stick to the three-dimensional polymer network in respiratory mucus and/or become covered or dissociated by macromolecules that are not embedded in the mucus network. Additionally, NANs with a too hydrophobic surface are also expected to stick to the mucus network. Does the size of NANs matter? Two independent reports clearly found that smaller nanoparticles are less retarded by CF sputum [49], [50]. Based on these reports we can conclude that NANs should be 100 nm or smaller to allow free passive through the mesh network in CF sputum. However, one should realize that this size is not necessarily the optimal size for free diffusion of NANs in normal respiratory mucus or other type of mucus. Indeed, it has been recently demonstrated that large (surface shielded) polystyrene nanospheres move faster through cervical mucus than their smaller (also surface shielded) counterparts [51]. It is important to realize that the thickness of the mucus layer is also an important barrier. Indeed, only a small fraction of nanoparticles can cross a 150 µm thick mucus blanket within 150 min, i.e. the estimated renewal time of respiratory mucus. Therefore, to drastically enhance the number of NANs that can reach the cells beneath the mucus layer one should give ‘motility’ to the NANs. Possible approaches are for example the attachment of nanomotors to the NANs or the use of ultrasound or magnetic forces.
Besides optimizing the design of the NANs one can also try to reduce the barrier properties of respiratory secretions. All the data in the literature consistently confirm that treatment of the respiratory tract with mucolytic agents like NAC or rhDNase (at least 30 min) before the administration of NANs significantly favor respiratory gene transfer [67], [81]. Via this pre-treatment with mucolytics a significant amount of the mucus is probably removed.
Acknowledgements
Niek Sanders is a postdoctoral fellow of FWO (Fund for Scientific Research-Flanders). The financial support of this institute is acknowledged with gratitude. This work was supported by grants from Ghent University and the fund for scientific research-Flanders (grants G.0310.02 and G.0320.04).
Footnotes
This review is part of the Advanced Drug Delivery Reviews theme issue on "Drug and Gene Delivery to Mucosal Tissues: The Mucus Barrier.
References
- 1.Factor P. Gene therapy for asthma. Mol. Ther. 2003;7:148–152. doi: 10.1016/s1525-0016(03)00003-0. [DOI] [PubMed] [Google Scholar]
- 2.Aneja M.K., Rudolph C. Gene therapy of surfactant protein B deficiency. Curr. Opin. Mol. Ther. 2006;8:432–438. [PubMed] [Google Scholar]
- 3.Griesenbach U., Geddes D.M., Alton E.W.F.W. Gene therapy progress and prospects: cystic fibrosis. Gene Ther. 2006;13:1061–1067. doi: 10.1038/sj.gt.3302809. [DOI] [PubMed] [Google Scholar]
- 4.Densmore C.L. Advances in noninvasive pulmonary gene therapy. Curr. Drug Deliv. 2006;3:55–63. doi: 10.2174/156720106775197547. [DOI] [PubMed] [Google Scholar]
- 5.Birchall J. Pulmonary delivery of nucleic acids. Expert. Opin. Drug Deliv. 2007;4:575–578. doi: 10.1517/17425247.4.6.575. [DOI] [PubMed] [Google Scholar]
- 6.Alpar H.O., Somavarapu S., Atuah K.N., Bramwell V. Biodegradable mucoadhesive particulates for nasal and pulmonary antigen and DNA delivery. Adv. Drug Deliv. Rev. 2005;57:411–430. doi: 10.1016/j.addr.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Bivas-Benita M., Ottenhoff T.H.M., Junginger H.E., Borchard G. Pulmonary DNA vaccination: concepts, possibilities and perspectives. J. Control. Release. 2005;107:1–29. doi: 10.1016/j.jconrel.2005.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas M., Lu J.J., Chen J.Z., Klibanov A.M. Non-viral siRNA delivery to the lung. Adv. Drug Deliv. Rev. 2007;59:124–133. doi: 10.1016/j.addr.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newman S.P. Aerosol deposition considerations in inhalation therapy. Chest. 1985;88:S152–S160. doi: 10.1378/chest.88.2_supplement.152s. [DOI] [PubMed] [Google Scholar]
- 10.Conese M., Rejman J. Stem cells and cystic fibrosis. J. Cyst. Fibros. 2006;5:141–143. doi: 10.1016/j.jcf.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Davis P.B. Cystic fibrosis since 1938. Am. J. Respir. Crit. Care Med. 2006;173:475–482. doi: 10.1164/rccm.200505-840OE. [DOI] [PubMed] [Google Scholar]
- 12.Knowles M.R., Boucher R.C. Mucus clearance as a primary innate defense mechanism for mammalian airways. J. Clin. Invest. 2002;109:571–577. doi: 10.1172/JCI15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King M., Rubin B.K. Pharmacological approaches to discovery and development of new mucolytic agents. Adv. Drug Deliv. Rev. 2002;54:1475–1490. doi: 10.1016/s0169-409x(02)00156-4. [DOI] [PubMed] [Google Scholar]
- 14.King M. The role of mucus viscoelasticity in cough clearance. Biorheology. 1987;24:589–597. doi: 10.3233/bir-1987-24611. [DOI] [PubMed] [Google Scholar]
- 15.Deneuville E., Perrot-Minot C., Pennaforte F., Roussey M., Zahm J.M., Clavel C., Puchelle E., de Bentzmann S. Revisited physicochemical and transport properties of respiratory mucus in genotyped cystic fibrosis patients. Am. J. Respir. Crit. Care Med. 1997;156:166–172. doi: 10.1164/ajrccm.156.1.9606123. [DOI] [PubMed] [Google Scholar]
- 16.Wine J.J. The genesis of cystic fibrosis lung disease. J. Clin. Invest. 1999;103:309–312. doi: 10.1172/JCI6222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patton J.S. Mechanisms of macromolecule absorption by the lungs. Adv. Drug Deliv. Rev. 1996;19:3–36. [Google Scholar]
- 18.Widdicombe J.G. Airway liquid: a barrier to drug diffusion? Eur. Respir. J. 1997;10:2194–2197. doi: 10.1183/09031936.97.10102194. [DOI] [PubMed] [Google Scholar]
- 19.Lopez-Vidriero M.-T., Reid L. Bronchial mucus in health and disease. Br. Med. Bull. 1978;34:63–74. doi: 10.1093/oxfordjournals.bmb.a071461. [DOI] [PubMed] [Google Scholar]
- 20.Creeth J.M. Constituents of mucus and their separation. Br. Med. Bull. 1978;34:17–24. doi: 10.1093/oxfordjournals.bmb.a071454. [DOI] [PubMed] [Google Scholar]
- 21.Robinson N.P., Kyle H., Webber S.E., Widdicombe J.G. Electrolyte and other chemical concentrations in tracheal airway surface liquid and mucus. J. Appl. Physiol. 1989;66:2129–2135. doi: 10.1152/jappl.1989.66.5.2129. [DOI] [PubMed] [Google Scholar]
- 22.Lethem M.I. The role of tracheobronchial mucus in drug administration to the airways. Adv. Drug Deliv. Rev. 1993;11:271–298. [Google Scholar]
- 23.Lamblim G., Aubert J.P., Perini J.M., Klein A., Porchet N., Degand P., Roussel P. Human respiratory mucins. Eur. Respir. J. 1992;5:247–256. [PubMed] [Google Scholar]
- 24.Carlstedt I., Sheehan J.K., Corfield A.P., Gallagher J.T. Mucous glycoproteins: a gel of a problem. Essays Biochem. 1985;20:40–76. [PubMed] [Google Scholar]
- 25.Groneberg D.A., Eynott P.R., Oates T., Lim S., Wu R., Carlstedt I., Nicholson A.G., Chung K.F. Expression of MUC5AC and MUC5B mucins in normal and cystic fibrosis lung. Respir. Med. 2002;96:81–86. doi: 10.1053/rmed.2001.1221. [DOI] [PubMed] [Google Scholar]
- 26.Schulz B.L., Sloane A.J., Robinson L.J., Prasad S.S., Lindner R.A., Robinson M., Bye P.T., Nielson D.W., Harry J.L., Packer N.H., Karlsson N.G. Glycosylation of sputum mucins is altered in cystic brosis patients. Glycobiology. 2007;17:698–712. doi: 10.1093/glycob/cwm036. [DOI] [PubMed] [Google Scholar]
- 27.Lopez-Vidriero M.-T. Lung secretions. In: Clarke S.W., Pavia D., editors. Aerosols and the Lung: Clinical and Experimental Aspects. Butterworths; London: 1984. pp. 19–48. [Google Scholar]
- 28.Bansil R., Stanley E., LaMont J.T. Mucin biophysics. Annu. Rev. Physiol. 1995;57:635–657. doi: 10.1146/annurev.ph.57.030195.003223. [DOI] [PubMed] [Google Scholar]
- 29.Henke M.O., Renner A., Huber R.M., Seeds M.C., Rubin B.K. MUC5AC and MUC5B mucins are decreased in cystic fibrosis airway secretions. Am. J. Respir. cell Mol. Biol. 2004;31:86–91. doi: 10.1165/rcmb.2003-0345OC. [DOI] [PubMed] [Google Scholar]
- 30.Sanders N.N., Franckx H., De Boeck K., Haustraete J., De Smedt S.C., Demeester J. Role of magnesium in the failure of rhDNase therapy in patients with cystic fibrosis. Thorax. 2006;61:962–968. doi: 10.1136/thx.2006.060814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanders N.N., Van Rompaey E., De Smedt S.C., Demeester J. Structural alterations of gene complexes by cystic fibrosis sputum. Am. J. Respir. Crit. Care Med. 2001;164:486–493. doi: 10.1164/ajrccm.164.3.2011041. [DOI] [PubMed] [Google Scholar]
- 32.Mrsny R.J., Daugherty A.L., Short S.M., Widmer R., Siegel M.W., Keller G.A. Distribution of DNA and alginate in purulent cystic fibrosis sputum: implications to pulmonary targeting strategies. J. Drug Target. 1996;4:233–243. doi: 10.3109/10611869608995625. [DOI] [PubMed] [Google Scholar]
- 33.Jacquot J., Hayem A., Galabert C. Functions of proteins and lipids in airway secretions. Eur. Respir. J. 1992;5:343–358. [PubMed] [Google Scholar]
- 34.Pelletier O., Pokidysheva E., Hirst L.S., Bouxsein N., Li Y., Safinya C.R. Structure of actin cross-linked with alpha-actinin: a network of bundles. Phys. Rev. Lett. 2003;91 doi: 10.1103/PhysRevLett.91.148102. (Art. No 148102) [DOI] [PubMed] [Google Scholar]
- 35.Broughton-Head V.J., Shur J., Carroll M.P., Smith J.R., Shute J.K. Unfractionated heparin reduces the elasticity of sputum from patients with cystic fibrosis. Am. J. Physiol.-Lung Cell Mol. Physiol. 2007;293:L1240–L1249. doi: 10.1152/ajplung.00206.2007. [DOI] [PubMed] [Google Scholar]
- 36.Sheils C.A., Kas J., Travassos W., Allen P.G., Janmey P.A., Wohl M.E., Stossel T.P. Actin filaments mediate DNA fiber formation in chronic inflammatory airway disease. Am. J. Pathol. 1996;148:919–927. [PMC free article] [PubMed] [Google Scholar]
- 37.Broughton-Head V.J., Smith J.R., Shur J., Shute J.K. Actin limits enhancement of nanoparticle diffusion through cystic fibrosis sputum by mucolytics. Pulm. Pharmacol. Ther. 2007;20:708–717. doi: 10.1016/j.pupt.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 38.Houdret N., Perini J.M., Galabert C., Scharfman A., Humbert P., Lamblin G., Roussel P. The high lipid-content of respiratory mucins in cystic-fibrosis is related to infection. Biochim. Biophys. Acta. 1986;880:54–61. doi: 10.1016/0304-4165(86)90119-4. [DOI] [PubMed] [Google Scholar]
- 39.Goerke J. Pulmonary surfactant: functions and molecular composition. Biochim. Biophys. Acta-Mol. Basis Dis. 1998;1408:79–89. doi: 10.1016/s0925-4439(98)00060-x. [DOI] [PubMed] [Google Scholar]
- 40.Veldhuizen R., Nag K., Orgeig S., Possmayer F. The role of lipids in pulmonary surfactant. Biochim. Biophys. Acta-Mol. Basis Dis. 1998;1408:90–108. doi: 10.1016/s0925-4439(98)00061-1. [DOI] [PubMed] [Google Scholar]
- 41.Wattiez R., Falmagne P. Proteomics of bronchoalveolar lavage fluid. J. Chromatogr. B. 2005;815:169–178. doi: 10.1016/j.jchromb.2004.10.029. [DOI] [PubMed] [Google Scholar]
- 42.Noel-Georis I., Bernard A., Falmagne P., Wattiez R. Database of bronchoalveolar lavage fluid proteins. J. Chromatogr. B. 2002;771:221–236. doi: 10.1016/s1570-0232(02)00114-9. [DOI] [PubMed] [Google Scholar]
- 43.Magi B., Bargagli E., Bini L., Rottoli P. Proteome analysis of bronchoalveolar lavage in lung diseases. Proteomics. 2006;6:6354–6369. doi: 10.1002/pmic.200600303. [DOI] [PubMed] [Google Scholar]
- 44.Sutinen S., Riska H., Backman R., Sutinen S.H., Froseth B. Alveolar lavage fluid (Alf) of normal volunteer subjects: cytologic, immunocytochemical, and biochemical reference values. Respir. Med. 1995;89:85–92. doi: 10.1016/0954-6111(95)90189-2. [DOI] [PubMed] [Google Scholar]
- 45.Fehrenbach H. Alveolar epithelial type II cell: defender of the alveolus revisited. Respir. Res. 2001;2:33–52. doi: 10.1186/rr36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ruponen M., Yla H.S., Urtti A. Interactions of polymeric and liposomal gene delivery systems with extracellular glycosaminoglycans: physicochemical and transfection studies. Biochim. Biophys. Acta-Biomembr. 1999;1415:331–341. doi: 10.1016/s0005-2736(98)00199-0. [DOI] [PubMed] [Google Scholar]
- 47.Yeates D.B., Aspin N., Levison H., Jones M.T., Bryan A.C. Mucociliary tracheal transport rates in man. J. Appl. Physiol. 1975;39:487–495. doi: 10.1152/jappl.1975.39.3.487. [DOI] [PubMed] [Google Scholar]
- 48.Yeates D.B., Sturgess J.M., Kahn S.R., Levison H., Aspin N. Mucociliary transport in trachea of patients with cystic fibrosis. Arch. Dis. Child. 1976;51:28–33. doi: 10.1136/adc.51.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sanders N.N., De Smedt S.C., Van Rompaey E., Simoens P., De Baets F., Demeester J. Cystic fibrosis sputum — a barrier to the transport of nanospheres. Am. J. Respir. Crit. Care Med. 2000;162:1905–1911. doi: 10.1164/ajrccm.162.5.9909009. [DOI] [PubMed] [Google Scholar]
- 50.Dawson M., Wirtz D., Hanes J. Enhanced viscoelasticity of human cystic fibrotic sputum correlates with increasing microheterogeneity in particle transport. J. Biol. Chem. 2003;278:50393–50401. doi: 10.1074/jbc.M309026200. [DOI] [PubMed] [Google Scholar]
- 51.Lai S.K., O'Hanlon D.E., Harrold S., Man S.T., Wang Y.Y., Cone R., Hanes J. Rapid transport of large polymeric nanoparticles in fresh undiluted human mucus. Proc. Natl. Acad. Sci. U.S.A. 2007;104:1482–1487. doi: 10.1073/pnas.0608611104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sanders N.N., Van Rompaey E., De Smedt S.C., Demeester J. On the transport of lipoplexes through cystic fibrosis sputum. Pharm. Res. 2002;19 doi: 10.1023/a:1015139527747. [DOI] [PubMed] [Google Scholar]
- 53.Sanders N.N., De Smedt S.C., Demeester J. Mobility and stability of gene complexes in biogels. J. Control. Release. 2003;87:117–129. doi: 10.1016/s0168-3659(02)00355-3. [DOI] [PubMed] [Google Scholar]
- 54.Suh J., Dawson M., Hanes J. Real-time multiple-particle tracking: applications to drug and gene delivery. Adv. Drug Deliv. Rev. 2005;57:63–78. doi: 10.1016/j.addr.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 55.Garcia-Saez A.J., Schwille P. Single molecule techniques for the study of membrane proteins. Appl. Microbiol. Biotechnol. 2007;76:257–266. doi: 10.1007/s00253-007-1007-8. [DOI] [PubMed] [Google Scholar]
- 56.Levi V., Gratton E. Exploring dynamics in living cells by tracking single particles. Cell Biochem. Biophys. 2007;48:1–15. doi: 10.1007/s12013-007-0010-0. [DOI] [PubMed] [Google Scholar]
- 57.Braeckmans K., Peeters L., Sanders N.N., De Smedt S.C., Demeester J. Three-dimensional fluorescence recovery after photobleaching with the confocal scanning laser microscope. Biophys. J. 2003;85:2240–2252. doi: 10.1016/s0006-3495(03)74649-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Remaut K., Sanders N.N., De Geest B.G., Braeckmans K., Demeester J., De Smedt S.C. Nucleic acid delivery: Where material sciences and bio-sciences meet. Mater. Sci. Eng. R-Rep. 2007;58:117–161. [Google Scholar]
- 59.Callahan L.N., Phelan M., Mallinson M., Norcross M.A. Dextran sulfate blocks antibody binding to the principal neutralizing domain of human immunodeficiency virus type 1 without interfering with gp120–CD4 interactions. J. Virol. 1991;65:1543–1550. doi: 10.1128/jvi.65.3.1543-1550.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Le Doux J.M., Morgan J.R., Snow R.G., Yarmush M.L. Proteoglycans secreted by packaging cell lines inhibit retrovirus infection. J. Virol. 1996;70:6468–6473. doi: 10.1128/jvi.70.9.6468-6473.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Perricone M.A., Rees D.D., Sacks C.R., Smith K.A., Kaplan J.M., St-George J.A. Inhibitory effect of cystic fibrosis sputum on adenovirus-mediated gene transfer in cultured epithelial cells. Hum. Gene Ther. 2000;11:1997–2008. doi: 10.1089/10430340050143426. [DOI] [PubMed] [Google Scholar]
- 62.Croyle M.A., Chirmule N., Zhang Y., Wilson J.M. “Stealth” adenoviruses blunt cell-mediated and humoral immune responses against the virus and allow for significant gene expression upon readministration in the lung. J. Virol. 2001;75:4792–4801. doi: 10.1128/JVI.75.10.4792-4801.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Olmsted S.S., Padgett J.L., Yudin A.I., Whaley K.J., Moench T.R., Cone R.A. Diffusion of macromolecules and virus-like particles in human cervical mucus. Biophys. J. 2001;81:1930–1937. doi: 10.1016/S0006-3495(01)75844-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stern M., Caplen N.J., Browning J.E., Griesenbach U., Sorgi F., Huang L., Gruenert D.C., Marriot C., Crystal R.G., Geddes D.M., Alton E.W.F.W. The effect of mucolytic agents on gene transfer across a CF sputum barrier in vitro. Gene Ther. 1998;5:91–98. doi: 10.1038/sj.gt.3300556. [DOI] [PubMed] [Google Scholar]
- 65.Kitson C., Angel B., Judd D., Rothery S., Severs N.J., Dewar A., Huang L., Wadsworth S.C., Cheng S.H., Geddes D.M., Alton E.W.F.W. The extra- and intracellular barriers to lipid and adenovirus-mediated pulmonary gene transfer in native sheep airway epithelium. Gene Ther. 1999;6:534–546. doi: 10.1038/sj.gt.3300840. [DOI] [PubMed] [Google Scholar]
- 66.Yonemitsu Y., Kitson C., Ferrari S., Farley R., Griesenbach U., Judd D., Steel R., Scheid P., Zhu J., Jeffery P.K., Kato A., Hasan M.K., Nagai Y., Masaki I., Fukumura M., Hasegawa M., Geddes D.M., Alton E.W.F.W. Efficient gene transfer to airway epithelium using recombinant Sendai virus. Nat. Biotechnol. 2000;18:970–973. doi: 10.1038/79463. [DOI] [PubMed] [Google Scholar]
- 67.Ferrari S., Kitson C., Farley R., Steel R., Marriott C., Parkins D.A., Scarpa M., Wainwright B., Evans M.J., Colledge W.H., Geddes D.M., Alton E.W. Mucus altering agents as adjuncts for nonviral gene transfer to airway epithelium. Gene Ther. 2001;8:1380–1386. doi: 10.1038/sj.gt.3301525. [DOI] [PubMed] [Google Scholar]
- 68.Bansil R., Turner B.S. Mucin structure, aggregation, physiological functions and biomedical applications. Curr. Opin. Colloid Interface Sci. 2006;11:164–170. [Google Scholar]
- 69.Stonebraker J.R., Wagner D., Lefensty R.W., Burns K., Gendler S.J., Bergelson J.A., Boucher R.C., O'Neal W.K., Pickles R.J. Glycocalyx restricts adenoviral vector access to apical receptors expressed on respiratory epithelium in vitro and in vivo: role for tethered mucins as barriers to lumenal infection. J. Virol. 2004;78:13755–13768. doi: 10.1128/JVI.78.24.13755-13768.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ferrari S., Geddes D.M., Alton E.W.F.W. Barriers to and new approaches for gene therapy and gene delivery in cystic fibrosis. Adv. Drug Deliv. Rev. 2002;54:1373–1393. doi: 10.1016/S0169-409X(02)00145-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Duncan J.E., Whitsett J.A., Horowitz A.D. Pulmonary surfactant inhibits cationic liposome-mediated gene delivery to respiratory epithelial cells in vitro. Hum. Gene Ther. 1997;8:431–438. doi: 10.1089/hum.1997.8.4-431. [DOI] [PubMed] [Google Scholar]
- 72.Tsan M.F., Tsan G.L., White J.E. Surfactant inhibits cationic liposome-mediated gene transfer. Hum. Gene Ther. 1997;8:817–825. doi: 10.1089/hum.1997.8.7-817. [DOI] [PubMed] [Google Scholar]
- 73.Ernst N., Ulrichskotter S., Schmalix W.A., Radler J., Galneder R., Mayer E., Gersting S., Plank C., Reinhardt D., Rosenecker J. Interaction of liposomal and polycationic transfection complexes with pulmonary surfactant. J. Gene Med. 1999;1:331–340. doi: 10.1002/(SICI)1521-2254(199909/10)1:5<331::AID-JGM60>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 74.Kukowska-Latallo J.F., Chen C., Eichman J., Bielinska A.U., Baker J.R. Enhancement of dendrimer-mediated transfection using synthetic lung surfactant exosurf neonatal in vitro. Biochem. Biophys. Res. Commun. 1999;264:253–261. doi: 10.1006/bbrc.1999.1458. [DOI] [PubMed] [Google Scholar]
- 75.Rudolph C., Lausier J., Naundorf S., Muller R.H., Rosenecker J. In vivo gene delivery to the lung using polyethylenimine and fractured polyamidoamine dendrimers. J. Gene Med. 2000;2:269–278. doi: 10.1002/1521-2254(200007/08)2:4<269::AID-JGM112>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 76.Roesnecker J., Naundorf S., Gersting S.W., Hauck R.W., Gessner A., Nicklaus P., Muller R.H., Rudolph C. Interaction of bronchoalveolar lavage fluid with polyplexes and lipoplexes: analysing the role of proteins and glycoproteins. J. Gene Med. 2003;5:49–60. doi: 10.1002/jgm.291. [DOI] [PubMed] [Google Scholar]
- 77.Kopatz I., Remy J.S., Behr J.P. A model for non-viral gene delivery: through syndecan adhesion molecules and powered by actin. J. Gene Med. 2004;6:769–776. doi: 10.1002/jgm.558. [DOI] [PubMed] [Google Scholar]
- 78.Colina A.R., Aumont F., Deslauriers N., Belhumeur P., de Repentigny L. Evidence for degradation of gastrointestinal mucin by Candida albicans secretory aspartyl proteinase. Infect. Immun. 1996;64:4514–4519. doi: 10.1128/iai.64.11.4514-4519.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Connaris S., Greenwell P. Glycosidases in mucin-dwelling protozoans. Glycoconj. J. 1997;14:879–882. doi: 10.1023/a:1018554408558. [DOI] [PubMed] [Google Scholar]
- 80.Bisaillon M., Senechal S., Bernier L., Lemay G. A glycosyl hydrolase activity of mammalian reovirus sigma1 protein can contribute to viral infection through a mucus layer. J. Mol. Biol. 1999;286:759–773. doi: 10.1006/jmbi.1998.2495. [DOI] [PubMed] [Google Scholar]
- 81.Kushwah R., Oliver J.R., Cao H., Hu J. Nacystelyn enhances adenoviral vector-mediated gene delivery to mouse airways. Gene Ther. 2007;14:1243–1248. doi: 10.1038/sj.gt.3302968. [DOI] [PubMed] [Google Scholar]
- 82.Sanders N.N., De Smedt S.C., Demeester J. Deoxyribonuclease I. In: McGrath B.M., Walsh G., editors. Directory of Therapeutic Enzymes. Taylor & Francis; Boca Raton: 2005. pp. 97–116. [Google Scholar]
- 83.Davoodian K., Ritchings B.W., Ramphal R., Bubb M.R. Gelsolin activates DNase I in vitro and in cystic fibrosis sputum. Biochemistry. 1997;36:9637–9641. doi: 10.1021/bi9711487. [DOI] [PubMed] [Google Scholar]
- 84.Rubin B.K. Mucolytics, expectorants, and mucokinetic medications. Respir. Care. 2007;52:859–865. [PubMed] [Google Scholar]
- 85.Vosters O., Neve J., De Wit D., Willems F., Goldman M., Verhasselt V. Dendritic cells exposed to nacystelyn are refractory to maturation and promote the emergence of alloreactive regulatory T cells. Transplantation. 2003;75:383–389. doi: 10.1097/01.TP.0000043924.09647.61. [DOI] [PubMed] [Google Scholar]
- 86.Antonicelli F., Brown D., Parmentier M., Drost E.M., Hirani N., Rahman I., Donaldson K., MacNee W. Regulation of LPS-mediated inflammation in vivo and in vitro by the thiol antioxidant nacystelyn. Am. J. Physiol.-Lung Cell Mol. Physiol. 2004;286:L1319–L1327. doi: 10.1152/ajplung.00329.2003. [DOI] [PubMed] [Google Scholar]
- 87.Plank C., Schillinger U., Scherer F., Bergemann C., Remy J.S., Krotz F., Anton M., Lausier J., Rosenecker J. The magnetofection method: using magnetic force to enhance gene delivery. Biol. Chem. 2003;384:737–747. doi: 10.1515/BC.2003.082. [DOI] [PubMed] [Google Scholar]
- 88.Scherer F., Anton M., Schillinger U., Henkel J., Bergemann C., Kruger A., Gansbacher B., Plank C. Magnetofection: enhancing and targeting gene delivery by magnetic force in vitro and in vivo. Gene Ther. 2002;9:102–109. doi: 10.1038/sj.gt.3301624. [DOI] [PubMed] [Google Scholar]
- 89.Gersting S.W., Schillinger U., Lausier J., Nicklaus P., Rudolph C., Plank C., Reinhardt D., Rosenecker J. Gene delivery to respiratory epithelial cells by magnetofection. J. Gene Med. 2004;6:913–922. doi: 10.1002/jgm.569. [DOI] [PubMed] [Google Scholar]
- 90.Xenariou S., Griesenbach U., Ferrari S., Dean P., Scheule R.K., Cheng S.H., Geddes D.M., Plank C., Alton E.W.F.W. Using magnetic forces to enhance non-viral gene transfer to airway epithelium in vivo. Gene Ther. 2006;13:1545–1552. doi: 10.1038/sj.gt.3302803. [DOI] [PubMed] [Google Scholar]
- 91.Dames P., Gleich B., Flemmer A., Hajek K., Seidl N., Wiekhorst F., Eberbeck D., Bittmann I., Bergemann C., Weyh T., Trahms L., Rosenecker J., Rudolph C. Targeted delivery of magnetic aerosol droplets to the lung. Nat. Nanotechnol. 2007;2:495–499. doi: 10.1038/nnano.2007.217. [DOI] [PubMed] [Google Scholar]
- 92.Kamau S.W., Hassa P.O., Steitz B., Petri-Fink A., Hofmann H., Hofmann-Amtenbrink M., von Rechenberg B., Hottiger M.O. Enhancement of the efficiency of non-viral gene delivery by application of pulsed magnetic field. Nucleic Acids Res. 2006;34:e40. doi: 10.1093/nar/gkl035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kuhn S.J., Finch S.K., Hallahan D.E., Giorgio T.D. Proteolytic surface functionalization enhances in vitro magnetic nanoparticle mobility through extracellular matrix. Nano Lett. 2006;6:306–312. doi: 10.1021/nl052241g. [DOI] [PubMed] [Google Scholar]
- 94.Dhar P., Fischer T.M., Wang Y., Mallouk T.E., Paxton W.F., Sen A. Autonomously moving nanorods at a viscous interface. Nano Lett. 2006;6:66–72. doi: 10.1021/nl052027s. [DOI] [PubMed] [Google Scholar]
- 95.Ozin G.A., Manners I., Fournier-Bidoz S., Arsenault A. Dream nanomachines. Adv. Mater. 2005;17:3011–3018. [Google Scholar]
- 96.Mitragotri S., Kost J. Low-frequency sonophoresis — a review. Adv. Drug Deliv. Rev. 2004;56:589–601. doi: 10.1016/j.addr.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 97.Joshi A., Raje J. Sonicated transdermal drug transport. J. Control. Release. 2002;83:13–22. doi: 10.1016/s0168-3659(02)00200-6. [DOI] [PubMed] [Google Scholar]
- 98.Shulman L., Ost D. Advances in bronchoscopic diagnosis of lung cancer. Curr. Opin. Pulm. Med. 2007;13:271–277. doi: 10.1097/MCP.0b013e3281c9b0ee. [DOI] [PubMed] [Google Scholar]
- 99.Newman C.M.H., Bettinger T. Gene therapy progress and prospects: ultrasound for gene transfer. Gene Ther. 2007;14:465–475. doi: 10.1038/sj.gt.3302925. [DOI] [PubMed] [Google Scholar]
- 100.Xenariou S., Griesenbach U., Liang H.D., Zhu J., Farley R., Somerton L., Singh C., Jeffery P.K., Ferrari S., Scheule R.K., Cheng S.H., Geddes D.M., Blomley M., Alton E.W.F.W. Use of ultrasound to enhance nonviral lung gene transfer in vivo. Gene Ther. 2007;14:768–774. doi: 10.1038/sj.gt.3302922. [DOI] [PubMed] [Google Scholar]
- 101.Rudolph C., Schillinger U., Ortiz A., Plank C., Golas M.M., Sander B., Stark H., Rosenecker J. Aerosolized nanogram quantities of plasmid DNA mediate highly efficient gene delivery to mouse airway epithelium. Mol. Ther. 2005;12:493–501. doi: 10.1016/j.ymthe.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 102.Lee M., Kim S.W. Polyethylene glycol-conjugated copolymers for plasmid DNA delivery. Pharm. Res. 2005;22:1–10. doi: 10.1007/s11095-004-9003-5. [DOI] [PubMed] [Google Scholar]
- 103.Wheeler J.J., Palmer L., Ossanlou M., MacLachlan I., Graham R.W., Zhang Y.P., Hope M.J., Scherrer P., Cullis P.R. Stabilized plasmid–lipid particles: construction and characterization. Gene Ther. 1999;6:271–281. doi: 10.1038/sj.gt.3300821. [DOI] [PubMed] [Google Scholar]
- 104.Thompson B., Mignet N., Hofland H., Lamons D., Seguin J., Nicolazzi C., de la Figuera N., Kuen R.L., Meng X.Y., Scherman D., Bessodes M. Neutral postgrafted colloidal particles for gene delivery. Bioconjug. Chem. 2005;16:608–614. doi: 10.1021/bc040244z. [DOI] [PubMed] [Google Scholar]
- 105.Meyer M., Wagner E. pH-responsive shielding of non-viral gene vectors. Expert Opin. Drug Deliv. 2006;3:563–571. doi: 10.1517/17425247.3.5.563. [DOI] [PubMed] [Google Scholar]
- 106.Cheung C.Y., Murthy N., Stayton P.S., Hoffman A.S. A pH-sensitive polymer that enhances cationic lipid-mediated gene transfer. Bioconju. Chem. 2001;12:906–910. doi: 10.1021/bc0100408. [DOI] [PubMed] [Google Scholar]
- 107.Finsinger D., Remy J.S., Erbacher P., Koch C., Plank C. Protective copolymers for nonviral gene vectors: synthesis, vector characterization and application in gene delivery. Gene Ther. 2000;7:1183–1192. doi: 10.1038/sj.gt.3301227. [DOI] [PubMed] [Google Scholar]
- 108.Fisher K.D., Stallwood Y., Green N.K., Ulbrich K., Mautner V., Seymour L.W. Polymer-coated adenovirus permits efficient retargeting and evades neutralising antibodies. Gene Ther. 2001;8:341–348. doi: 10.1038/sj.gt.3301389. [DOI] [PubMed] [Google Scholar]
- 109.Fisher K.D., Green N.K., Hale A., Subr V., Ulbrich K., Seymour L.W. Passive tumour targeting of polymer-coated adenovirus for cancer gene therapy. J. Drug Target. 2007;15:546–551. doi: 10.1080/10611860701501014. [DOI] [PubMed] [Google Scholar]
- 110.Cheng S.H., Marshall J., Scheule R.K., Smith A.E. Cationic lipid formulations for the intracellular gene delivery of cystic fibrosis transmembrane conductance regulator to airway epithelia. Methods Enzymol. 1998;292:697–717. doi: 10.1016/s0076-6879(98)92054-7. [DOI] [PubMed] [Google Scholar]
- 111.Sanders N.N., De Smedt S.C., Cheng S.H., Demeester J. Pegylated GL67 lipoplexes retain their gene transfection activity after exposure to components of CF mucus. Gene Therap. 2002;9:363–371. doi: 10.1038/sj.gt.3301663. [DOI] [PubMed] [Google Scholar]
- 112.Rudolph C., Schillinger U., Plank C., Gessner A., Nicklaus P., Muller R.H., Rosenecker J. Nonviral gene delivery to the lung with copolymer-protected and transferrin-modified polyethylenimine. Biochim. Biophys. Acta-Gen. Subj. 2002;1573:75–83. doi: 10.1016/s0304-4165(02)00334-3. [DOI] [PubMed] [Google Scholar]
- 113.Kleemann E., Neu M., Jekel N., Fink L., Schmehl T., Gessler T., Seeger W., Kissel T. Nano-carriers for DNA delivery to the lung based upon a TAT-derived peptide covalently coupled to PEG–PEI. J. Control. Release. 2005;109:299–316. doi: 10.1016/j.jconrel.2005.09.036. [DOI] [PubMed] [Google Scholar]
- 114.Carrabino S., Di Gioia S., Copreni E., Conese M. Serum albumin enhances polyethylenimine-mediated gene delivery to human respiratory epithelial cells. J. Gene Med. 2005;7:1555–1564. doi: 10.1002/jgm.799. [DOI] [PubMed] [Google Scholar]
- 115.Baatz J.E., Bruno M.D., Ciraolo P.J., Glasser S.W., Stripp B.R., Smyth K.L., Korfhagen T.R. Utilization of modified surfactant-associated protein-b for delivery of DNA to airway cells in culture. Proc. Natl. Acad. Sci. U.S.A. 1994;91:2547–2551. doi: 10.1073/pnas.91.7.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kreda S.M., Pickles R.J., Lazarowski E.R., Boucher R.C. G-protein-coupled receptors as targets for gene transfer vectors using natural small-molecule ligands. Nat. Biotechnol. 2000;18:635–640. doi: 10.1038/76479. [DOI] [PubMed] [Google Scholar]
- 117.Weiss S.I., Sieverling N., Niclasen M., Maucksch C., Thunemann A.F., Mohwald H., Reinhardt D., Rosenecker J., Rudolph C. Uronic acids functionalized polyethyleneimine (PEI)–polyethyleneglycol (PEG)–graft-copolymers as novel synthetic gene carriers. Biomaterials. 2006;27:2302–2312. doi: 10.1016/j.biomaterials.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 118.Elfinger M., Maucksch C., Rudolph C. Characterization of lactoferrin as a targeting ligand for nonviral gene delivery to airway epithelial cells. Biomaterials. 2007;28:3448–3455. doi: 10.1016/j.biomaterials.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 119.K. Buyens, B. Lucas, K. Raemdonck, K. Braeckmans, J. Vercammen, J. Hendrix, Y. Engelborghs, S.C. De Smedt, N.N. Sanders, A fast and sensitive method for measuring the integrity of siRNA–carrier complexes in full human serum, J. Control. Release 126 (2008) 67–76. [DOI] [PubMed]
- 120.Sanders N.N., Eijslnk V.G.H., van den Pangaart P.S., van Neerven R.J.J., Simons P.J., De Smedt S.C., Demeester J. Mucolytic activity of bacterial and human chitinases. Biochim. Biophys. Acta-Gen. Subj. 2007;1770:839–846. doi: 10.1016/j.bbagen.2007.01.011. [DOI] [PubMed] [Google Scholar]