Abstract
Background
Lactoferrin, a normal component of human colostrum and milk, can enhance host defenses and may be effective for prevention of sepsis and necrotizing enterocolitis (NEC) in preterm neonates.
Objectives
To assess the safety and effectiveness of lactoferrin supplementation to enteral feeds for prevention of sepsis and NEC in preterm neonates. Secondarily, we assessed the effects of lactoferrin supplementation to enteral feeds on the duration of positive‐pressure ventilation, development of chronic lung disease (CLD) or periventricular leukomalacia (PVL), length of hospital stay to discharge among survivors, and adverse neurological outcomes at two years of age or later.
Search methods
We used the standard search strategy of Cochrane Neonatal to update our search. We searched the Cochrane Central Register of Controlled Trials (CENTRAL 2019, Issue 9), MEDLINE via PubMed (1966 to 20 January 2020), PREMEDLINE (1996 to 20 January 2020), Embase (1980 to 20 January 2020), and CINAHL (1982 to 20 January 2020). We also searched clinical trials databases, conference proceedings, and the reference lists of retrieved articles for randomized controlled trials and quasi‐randomized trials.
Selection criteria
In our search, we included randomized controlled trials (RCTs) evaluating enteral lactoferrin supplementation at any dose or duration to prevent sepsis or NEC in preterm neonates.
Data collection and analysis
We used the standard methods of Cochrane Neonatal and the GRADE approach to assess the certainty of evidence.
Main results
Meta‐analysis of data from twelve randomized controlled trials showed that lactoferrin supplementation to enteral feeds decreased suspected or confirmed late‐onset sepsis (typical RR 0.80, 95% CI 0.72 to 0.89; typical RD ‐0.05, 95% CI, ‐0.07 to ‐0.02; NNTB 20, 95% CI 14 to 50; 12 studies, 5425 participants, low‐certainty evidence) and decreased length of hospital stay (MD ‐2.38 to 95% CI, ‐4.67 to ‐0.09; 3 studies, 1079 participants, low‐certainty evidence). A subgroup analysis including data of infants with confirmed sepsis demonstrates a decrease in confirmed late‐onset sepsis (typical RR 0.83, 95% CI 0.73 to 0.94; typical RD ‐0.03, 95% CI, ‐0.04 to ‐0.01; NNTB 33, 95% CI 25 to 100; 12 studies, 5425 participants, low‐certainty evidence).
Sensitivity analysis including only good methodological certainty studies suggested a decrease in late‐onset sepsis (both suspected and confirmed) with enteral lactoferrin supplementation (typical RR 0.82, 95% CI, 0.74 to 0.91; typical RD ‐0.04, 95% CI, ‐0.06 to ‐0.02; NNTB 20, 95% CI 14 to 50; 9 studies, 4702 participants, low‐certainty evidence).
There were no differences in NEC stage II or III (typical RR 1.10, 95% CI, 0.86 to 1.41; typical RD ‐0.00, 95% CI, ‐0.02 to 0.01; 7 studies, 4874 participants; low‐certainty evidence) or 'all‐cause mortality' (typical RR 0.90, 95% CI 0.69 to 1.17; typical RD ‐0.00, 95% CI, ‐0.01 to 0.01; 11 studies, 5510 participants; moderate‐certainty evidence). One study reported no differences in neurodevelopmental testing by Mullen's or Bayley III at 24 months of age after enteral lactoferrin supplementation (one study, 292 participants, low‐certainty evidence).
Lactoferrin supplementation to enteral feeds with probiotics decreased late‐onset sepsis (RR 0.25, 95% CI 0.14 to 0.46; RD ‐0.13, 95% CI ‐0.18 to ‐0.08; NNTB 8, 95% CI 6 to 13; 3 studies, 564 participants; low‐certainty evidence) and NEC stage II or III (RR 0.04, 95% CI 0.00 to 0.62; RD ‐0.05, 95% CI ‐0.08 to ‐0.03; NNTB 20, 95% CI 12.5 to 33.3; 1 study, 496 participants; very low‐certainty evidence), but not 'all‐cause mortality' (very low‐certainty evidence).
Lactoferrin supplementation to enteral feeds with or without probiotics had no effect on CLD, duration of mechanical ventilation or threshold retinopathy of prematurity (low‐certainty evidence). Investigators reported no adverse effects in the included studies.
Authors' conclusions
We found low‐certainty evidence from studies of good methodological quality that lactoferrin supplementation of enteral feeds decreases late‐onset sepsis (both suspected and confirmed, and confirmed only) but not NEC ≥ stage II or 'all cause mortality' or neurodevelopmental outcomes at 24 months of age in preterm infants without adverse effects. Low‐ to very low‐certainty evidence suggests that lactoferrin supplementation of enteral feeds in combination with probiotics decreases late‐onset sepsis (data from confirmed sepsis only) and NEC ≥ stage II in preterm infants without adverse effects, however, there were few included studies of poor methodological quality. The presence of publication bias and small studies of poor methodology that may inflate the effect size make recommendations for clinical practice difficult.
Keywords: Humans; Infant, Newborn; Administration, Oral; Bacterial Infections; Bacterial Infections/epidemiology; Bacterial Infections/prevention & control; Cause of Death; Chronic Disease; Enteral Nutrition; Enterocolitis, Necrotizing; Enterocolitis, Necrotizing/epidemiology; Enterocolitis, Necrotizing/prevention & control; Infant, Premature; Infant, Premature, Diseases; Infant, Premature, Diseases/prevention & control; Lacticaseibacillus rhamnosus; Lactoferrin; Lactoferrin/administration & dosage; Lung Diseases; Lung Diseases/epidemiology; Mycoses; Mycoses/epidemiology; Mycoses/prevention & control; Numbers Needed To Treat; Probiotics; Probiotics/administration & dosage; Randomized Controlled Trials as Topic; Retinopathy of Prematurity; Retinopathy of Prematurity/epidemiology; Sepsis; Sepsis/prevention & control
Plain language summary
Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants
Review question: Does administering lactoferrin with feeds decrease the risk of sepsis or necrotizing enterocolitis in preterm babies?
Background: Preterm babies are at risk for blood infection (sepsis) and/or gastrointestinal injury (necrotizing enterocolitis, or NEC). Many babies with sepsis or NEC die or develop long‐term brain and lung injury despite treatment with antibiotics. Lactoferrin, a protein that is present in human milk, has been shown to be effective against infection when tested in animals and in the laboratory. Lactoferrin also enhances the ability of babies to fight infection.
Study characteristics: Through literature searches updated to 20 January 2020, we found 12 studies that enrolled 5425 preterm babies and tested the effects of lactoferrin given with feeds. We also found ongoing studies that may increase the strength of our findings when their results become available.
Key results: Lactoferrin given with feeds with or without a probiotic decreases blood infection including fungal infection in preterm infants with no adverse effects. Lactoferrin with probiotics, but not lactoferrin alone, decreases gastrointestinal injury. Clarification regarding dosing, duration, type of lactoferrin (human or bovine), and development of preterm babies is still needed.
Certainty of evidence: Low to very low
Summary of findings
Summary of findings 1. Lactoferrin supplementation compared to control for very low birth weight infants.
| Lactoferrin supplementation compared to control for very low birth weight infants | ||||||
| Patient or population: prevention of sepsis and necrotizing enterocolitis in preterm infants Setting: Neonatal intensive care unit Intervention: lactoferrin supplementation with enteral feeds Comparison: placebo | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | What happens | ||
| Without lactoferrin supplementation with enteral feeds | With lactoferrin supplementation with enteral feeds | Difference | ||||
| All‐cause Mortality № of participants: 5510 (11 RCTs) | RR 0.97 (0.79 to 1.20) | Study population | ⊕⊝⊝⊝
VERY LOW1,2,3 |
Risk of bias, imprecision and funnel plot asymmetry | ||
| 5.9% | 5.7% (4.6 to 7) | 0.2% fewer (1.2 fewer to 1.2 more) | ||||
| necrotizing enterocolitis № of participants: 4874 (7 RCTs) | RR 0.90 (0.69 to 1.17) | Study population | ⊕⊕⊝⊝ LOW1,2 | Risk of bias in the included trials, and imprecision | ||
| 4.7% | 4.2% (3.2 to 5.5) | 0.5% fewer (1.4 fewer to 0.8 more) | ||||
| Late onset sepsis
№ of participants: 5425
(12
RCTs) [Data includes both suspected and confirmed sepsis] |
RR 0.80 (0.72 to 0.89) | Study population | ⊕⊕⊝⊝ LOW1,2 | Risk of bias in the included trials, and asymmetry of the funnel plot | ||
| 21.1% | 17.3% (15.6 to 19.2) | 3.8% fewer (5.5 fewer to 1.9 fewer) | ||||
| Bacterial sepsis № of participants: 3565 (8 RCTs) | RR 0.86 (0.74 to 1.00) | Study population | ⊕⊕⊝⊝ LOW1,2 | Risk of bias and. moderate heterogeneity | ||
| 16.1% | 13.9% (11.9 to 16.1) | 2.3% fewer (4.2 fewer to 0 fewer) | ||||
| Fungal infection № of participants: 3266 (6 RCTs) | RR 0.23 (0.10 to 0.54) | Study population | ⊕⊕⊝⊝ LOW1,2 | Risk of bias and moderate heterogeneity | ||
| 1.7% | 0.4% (0.2 to 0.9) | 1.3% fewer (1.5 fewer to 0.8 fewer) | ||||
| Chronic lung disease № of participants: 2984 (5 RCTs) | RR 1.00 (0.89 to 1.12) | Study population | ⊕⊕⊝⊝ LOW1,2 | Low risk of bias, moderate heterogeneity and imprecision | ||
| 27.2% | 27.2% (24.2 to 30.5) | 0.0% fewer (3 fewer to 3.3 more) | ||||
| Length of hospital stay № of participants: 1079 (3 RCTs) | ‐ | The mean length of hospital stay without lactoferrin supplementation with enteral feeds was 34.14 days | ‐ | MD 2.38 days lower (4.67 lower to 0.09 lower) | ⊕⊝⊝⊝ VERY LOW1,2,3 | Risk of bias and severe heterogeneity |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Risk of bias, 2imprecision, 3funnel plot asymmetry
Summary of findings 2. Lactoferrin supplementation with enteral feeds in combination with probiotics compared to placebo for prevention of sepsis and necrotizing enterocolitis in preterm infants.
| Lactoferrin supplementation with enteral feeds in combination with probiotics compared to placebo for prevention of sepsis and necrotizing enterocolitis in preterm infants | ||||||
| Patient or population: prevention of sepsis and necrotizing enterocolitis in preterm infants Setting: Neonatal Intensive care unit Intervention: Lactoferrin supplementation with enteral feeds in combination with probiotics Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with Lactoferrin supplementation with enteral feeds in combination with probiotics | |||||
| Any late‐onset sepsis ‐ All infants [Data on only confirmed sepsis available] |
Study population | RR 0.25 (0.14 to 0.46) | 564 (3 RCTs) | ⊕⊕⊝⊝ LOW1 2 | Risk of bias and imprecision | |
| 177 per 1,000 | 44 per 1,000 (25 to 82) | |||||
| NEC ≥ stage II | Study population | RR 0.04 (0.00, 0.62) |
496 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | Risk of bias and two levels for imprecision | |
| 54 per 1,000 | 0 per 1,000 (0 to 0) | |||||
| All‐cause mortality | Study population | RR 0.58 (0.30, 1.13) |
671 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 | Risk of bias and two levels for imprecision | |
| 69 per 1,000 | 0 per 1,000 (0 to 0) | |||||
| Bacterial sepsis | Study population | RR 0.28 (0.11 to 0.72) | 319 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | Risk of bias and imprecision | |
| 119 per 1,000 | 33 per 1,000 (13 to 86) | |||||
| Fungal Infection | Study population | RR 0.24 (0.08 to 0.71) | 494 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | Risk of bias and imprecision | |
| 70 per 1,000 | 17 per 1,000 (6 to 50) | |||||
| Chronic lung disease | Study population | RR 0.67 (0.25 to 1.79) | 319 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | Risk of bias and two levels for imprecision | |
| 60 per 1,000 | 40 per 1,000 (15 to 107) | |||||
| Length of stay among survivors | MD 2 higher (1.88 lower to 5.88 higher) | ‐ | 496 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | Risk of bias and two levels for imprecision | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Unclear blinding of intervention and outcome assessment, 2 Data from only one or few studies (imprecision)
Background
Description of the condition
Neonatal sepsis is the most common cause of neonatal death worldwide (Lawn 2006). The incidence of neonatal sepsis in the developed world is reported to be between one and four cases per 1000 live births (Stoll 2004b). In the developing world, the rate of neonatal sepsis is significantly higher (6.5 to 38 per 1000 live hospital births) (Zaidi 2005). Sepsis is a particular problem in very low birth weight (VLBW) infants (birth weight < 1500 g); early‐onset sepsis (sepsis in infants at < 72 hours of life) occurs in about 1.5% and late‐onset sepsis in about 21% of VLBW infants (Stoll 2002; Stoll 2005). Infections due to Staphylococcus and Candida species are among the common infections in the neonate. Mortality and morbidity (including patent ductus arteriosus, prolonged ventilation, prolonged need for intravascular access, bronchopulmonary dysplasia, necrotizing enterocolitis, and increased length of hospital stay) are significantly increased among infected infants. In a large cohort study of infants born weighing less than 1000 g, infected infants had a significantly higher incidence of adverse neurodevelopmental outcomes at follow‐up when compared with uninfected infants (Stoll 2004a).
Necrotizing enterocolitis (NEC) occurs in 1% to 5% of admissions to the neonatal intensive care unit (NICU) (Lin 2006). The most consistent risk factors are prematurity and low birth weight. Gastrointestinal immaturity, enteral feeding (especially formula feeding), presence of bacteria, and inflammation in the gastrointestinal (GI) tract may all contribute to the development of NEC (Lin 2006). Host‐pathogen interactions trigger inflammation in the gut, which may contribute to the pathogenesis of NEC and septic shock (Blackwell 1997; Neish 2004). NEC significantly increases mortality (attributable mortality of 15% to 30%) and morbidity (including surgery in 20% to 40% of infants and delayed neurodevelopment) (Bell 1978; Lin 2006; Stoll 2004a).
Mortality and morbidity due to sepsis and NEC remain high despite the use of potent anti‐microbial agents (Stoll 2002; Stoll 2005). Increased use of anti‐microbials has led to the emergence of antibiotic‐resistant strains of bacteria (Levy 1998). Adverse pulmonary and neurodevelopmental outcomes after sepsis or NEC may be due to inflammatory injury (Adams‐Chapman 2006; Speer 1999). Agents that modulate inflammation and enhance host defenses may improve the outcomes of infants with neonatal sepsis or NEC.
Description of the intervention
The glycoprotein lactoferrin is a component of the innate immune response and a potent immunomodulator (Legrand 2016). It is found in significant concentrations in human colostrum and in lower concentrations in human milk, tears, saliva, and seminal fluid, and in secondary granules of neutrophils. Lactoferrin has broad‐spectrum, anti‐microbial activity against bacteria, fungi, viruses, and protozoa, which may result from its ability to sequester iron, or may occur as a direct lytic effect on microbial cell membranes (Valenti 2005). Proteolysis of lactoferrin under acidic conditions (as would occur in the stomach or in the phagolysosomes of neutrophils) yields peptides called lactoferricins, which have enhanced anti‐microbial activity (Gifford 2005).
Current increased interest in lactoferrin stems not only from improved understanding of its functions, but also from its increased availability in various forms and sources. Lactoferrin processed from bovine and human milk is available commercially as a food supplement (Swedish Dairies Association, Tatua Co‐operative Dairy Company in New Zealand, Lacto Bretagne Associes' in Belgium, Milei in Germany, Morinaga Industries in Japan, DoMO Food Ingredients, a subsidiary of Friesland Dairy Foods, in the Netherlands, etc). In the United States, human recombinant lactoferrin (talactoferrin from Agennix, Inc., Houston, Texas, USA) has an investigational new drug status for clinical research purposes. Lactoferrin expression in transgenic rice (Ventrus Biosciences, New York City, New York, USA) and in transgenic maize (Meristem Therapeutics, Clermont‐Ferrand, France) is being researched. Bovine lactoferrin is less expensive than human lactoferrin and is affordable even in developing countries.
How the intervention might work
Lactoferrin inhibits the growth of Staphylococcus epidermidis and Candida albicans in vitro (Valenti 2005). It reduces the minimum inhibitory concentrations of vancomycin against S epidermidis and of antifungal agents such as azoles and amphotericin against Candida (Kuipers 1999; Leitch 1999). Lactoferrin and lactoferrin‐derived peptides are highly effective in vitro against antibiotic‐resistant Klebseilla and Staphylococcus aureus (Nibbering 2001).
Lactoferrin prophylaxis is effective in animal models of systemic and intestinal infection. In mice infected with Escherichia coli, pretreatment with lactoferrin improved survival from 4% to 70% (Zagulski 1989). In neonatal rats, lactoferrin reduced the severity of blood and liver infection after enteral infection with E coli (Edde 2001). Parenteral prophylaxis with lactoferrin enhanced survival in a neonatal rat model of polymicrobial infection with C albicans and S epidermidis (Venkatesh 2007). In a germ‐free, colostrum‐deprived piglet model challenged with E coli lipopolysaccharide, oral pretreatment with lactoferrin reduced mortality from 74 % to 17% after a challenge with E coli lipopolysaccharide (Lee 1998). In animal colitis, lactoferrin reduced intestinal injury and inflammation (Togawa 2002). The systemic effects of oral lactoferrin generally are thought to be indirect and probably are initiated by contact with intestinal epithelial cells and gut‐associated lymphoid tissue (GALT). Lactoferrin modulates cytokine and/or chemokine production by GALT cells, which then enter the systemic circulation and influence circulating leukocytes (Bellamy 1992; Tomita 2002). Lactoferrin and other similar products in milk (probiotics) create an environment for growth of beneficial bacteria within the gut, reducing colonization with pathogenic bacteria. Demonstrated intestinal receptors for lactoferrin and its ability to modulate intestinal cell differentiation and proliferation (Buccigrossi 2007) make lactoferrin a promising agent for prevention or treatment of NEC.
In adult humans, oral recombinant human lactoferrin has been found to be safe and well tolerated. Oral lactoferrin has shown promise as an anti‐tumour agent (Hayes 2006) and has been shown to reduce viremia in chronic hepatitis C infection (Iwasa 2002; Tanaka 1999). In patients with acute myeloid leukanemia and neutropenia, lactoferrin reduced the incidence, duration, and severity of bacteremia due to enteric pathogens (Trumpler 1989). To date, animal and human studies have reported no significant adverse effects.
Lactoferrin provides significant potential benefit for preterm infants including anti‐microbial and immunomodulatory effects and promotion of neurodevelopment (Manzoni 2016; Ochoa 2017). Systematic reviews on probiotics in preterm infants have reported decreased NEC and mortality (Alfaleh 2014; Dermyshi 2017). Lactoferrin has been reported to act synergistically with probiotic strains of bacteria, enhancing their growth and inhibiting intestinal pathogens (Chen 2017; Tian 2010).
Why it is important to do this review
The potential beneficial effects of lactoferrin make it a promising agent for prevention of neonatal sepsis and NEC. This review evaluated the role of lactoferrin supplementation to enteral feeds in the prevention of neonatal sepsis and NEC in preterm neonates.
Objectives
To assess the safety and effectiveness of lactoferrin supplementation to enteral feeds for prevention of sepsis and NEC in preterm neonates. Secondarily, we assessed the effects of lactoferrin supplementation to enteral feeds on the duration of positive‐pressure ventilation, development of chronic lung disease (CLD) or periventricular leukomalacia (PVL), length of hospital stay to discharge among survivors, and adverse neurological outcomes at two years of age or later.
Methods
Criteria for considering studies for this review
Types of studies
Randomized or quasi‐randomized controlled trials that have been completed (published or unpublished).
Types of participants
Preterm (< 37 completed weeks of gestation) neonates (< 28 days).
Types of interventions
Lactoferrin supplementation of enteral feeds at any dosage or duration used to prevent neonatal sepsis or NEC compared with placebo or no intervention. Separate analyses were performed for oral lactoferrin given with or without additional probiotics.
Types of outcome measures
Primary outcomes
-
Confirmed or suspected sepsis during hospital stay:
Confirmed sepsis is defined as clinical signs and symptoms consistent with infection and microbiologically proven with a positive blood culture, cerebrospinal fluid (CSF) culture, urine culture (obtained by a suprapubic tap), or culture from a normally sterile site (e.g., pleural fluid, peritoneal fluid, autopsy specimens) for bacteria or fungi;
Suspected sepsis is defined as clinical signs and symptoms consistent with sepsis without isolation of a causative organism.
-
NEC Bell's stage II or III during hospital stay:
necrotizing enterocolitis (NEC) (definitive NEC and perforated NEC, Bell's stage II or III) (Bell 1978) during hospital stay.
'All‐cause mortality' during hospital stay.
Secondary outcomes
Neurological outcome at two years of age or later (neurodevelopmental outcome as assessed by a validated test);
Chronic lung disease (CLD) in survivors (CLD defined as oxygen requirement at 36 weeks' postmenstrual age (PMA));
Adverse outcomes directly attributable to oral lactoferrin: increased gastric residuals (gastric aspirate > 10% of oral feed), vomiting, and other GI disturbances during hospital stay;
Periventricular leukomalacia (PVL) (defined as necrosis of brain white matter in a characteristic distribution, i.e. in the white matter dorsal and lateral to the external angles of lateral ventricles involving particularly the centrum semi‐ovale and optic and acoustic radiations and diagnosed by magnetic resonance imaging (MRI), or as periventricular cystic lesions seen on cranial ultrasonography (Volpe 1995) at discharge or at neurodevelopmental follow‐up);
Duration of assisted ventilation through an endotracheal tube measured in days during hospital stay;
Length of hospital stay measured in days to discharge for survivors; and
Post hoc analyses of bacterial infection, fungal infection, threshold retinopathy of prematurity, and urinary tract infection.
Search methods for identification of studies
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal search strategy for specialized register).
Electronic searches
We conducted a comprehensive search including: Cochrane Central Register of Controlled Trials (CENTRAL 2019, Issue 9) in the Cochrane Library; MEDLINE via PubMed (1966 to 20 January 2020); Embase (1980 to 20 January 2020); and CINAHL (1982 to 20 January 2020); using the following search terms: (sepsis, septicemia, septic, necroti(s)ing enterocolitis, lactoferrin, talactoferrin), plus database‐specific limiters for randomized controlled trials and neonates (see Appendix 1 for the full search strategies for each database). We did not apply language restrictions.
We searched clinical trials registries for ongoing or recently completed trials (clinicaltrials.gov; the World Health Organization’s International Trials Registry and Platform, Australian and New Zealand Clinical Trials Registry (anzctr.org.au) and the ISRCTN).
Searching other resources
We also searched the reference lists of any articles selected for inclusion in this review in order to identify additional relevant articles. We contacted study authors who published in this field to ask about unpublished articles. We searched the abstracts of conferences from proceedings of Pediatric Academic Societies (American Pediatric Society, Society for Pediatric Research, and European Society for Pediatric Research) from 1990 to 20 January 2020 in the journal Pediatric Research and in Abstracts Online.
Data collection and analysis
We used the standard methods of Cochrane Neonatal for conducting a systematic review (neonatal.cochrane.org/en/index.html).
Selection of studies
Two review authors assessed the titles and abstracts of studies identified by the search strategy to determine eligibility for inclusion in this review. If this could not be done reliably by title and abstract review, we obtained full‐text versions for assessment. We resolved differences by mutual discussion and obtained full‐text versions of all eligible studies for certainty assessment.
Data extraction and management
We designed forms for documenting trial inclusion/exclusion, for extracting data, and for requesting additional published information from authors of the original reports. We independently extracted data using specially designed paper forms.
Assessment of risk of bias in included studies
Two review authors (MP, GS) independently assessed risk of bias (low, high, or unclear) of all included trials using the Cochrane 'Risk of bias' tool (Higgins 2011) for the following domains.
Sequence generation (selection bias);
Allocation concealment (selection bias);
Blinding of participants and personnel (performance bias);
Blinding of outcome assessment (detection bias);
Incomplete outcome data (attrition bias);
Selective reporting (reporting bias); or
Any other bias.
We resolved disagreements by discussion. See Appendix 2 for a detailed description of risk of bias for each domain.
Measures of treatment effect
We performed statistical analyses according to recommendations of Cochrane Neonatal. We analyzed all randomly assigned infants on an 'intention‐to‐treat basis,' irrespective of whether they received their allocated treatment. We analyzed treatment effects in individual trials. We used the statistical package (RevMan 5.3) provided by the Cochrane Collaboration. We reported risk ratios (RRs) and risk differences (RDs) with 95% confidence intervals (CIs) for dichotomous outcomes, and weighted mean differences for continuous outcomes. We calculated and reported the number needed to treat for an additional beneficial outcome (NNTB) or the number needed to treat for an additional harmful outcome (NNTH) for statistically significant reductions in RD.
Unit of analysis issues
We included randomized and quasi‐randomized trials and used each participant as the unit of analysis. We did not encounter repeated measurements, and we excluded cluster‐randomized and cross‐over trials.
Dealing with missing data
We contacted trial investigators to obtain missing data.
Assessment of heterogeneity
We assessed heterogeneity of treatment effects between trials using the I2 statistic to check the appropriateness of pooling data and performing meta‐analyses. We deferred meta‐analysis if heterogeneity was high (≥ 75%). We used the following cut‐offs to report the degree of heterogeneity: < 25% no heterogeneity; 25% to 49% low heterogeneity; 50% to 74% moderate heterogeneity; and ≥ 75% high heterogeneity. If we detected statistical heterogeneity, we explored possible causes (e.g. differences in study certainty, participants, intervention regimens, or outcome assessments) by performing post hoc subgroup analyses.
Assessment of reporting biases
We assessed publication bias by visually analyzing the funnel plot for the outcome of late‐onset neonatal sepsis and 'all‐cause mortality' in the included trials (Figure 1; Figure 2). The visual analysis showed asymmetry of the funnel plot, with more trials with a positive outcome than trials with no effect or a negative outcome. The asymmetry may be due to publication bias but also by many small studies (Akin 2014; Barrington 2016; Dai 2015; Kaur 2015; Liu 2016; Ochoa 2015; Sherman 2016; and Tang 2017), some with poor methodological certainty inflating the effects of enteral lactoferrin supplementation. We have downgraded the evidence based on publication bias, small studies with poor methodological certainty for the outcome of late‐onset sepsis and 'all‐cause mortality' for comparison 1.
1.

Funnel plot of comparison: 1 Lactoferrin supplementation with enteral feeds versus placebo, outcome: 1.1 Any late‐onset sepsis.
2.

Funnel plot of comparison: 1 Lactoferrin supplementation with enteral feeds versus placebo, outcome: 1.3 All‐cause mortality.
Data synthesis
We used a fixed‐effect model for meta‐analysis when appropriate, with Review Manager software (RevMan 2014) as recommended by Cochrane Neonatal. For estimates of typical relative risk and risk difference, we used the Mantel‐Haenszel method.
Certainty of evidence
We used the GRADE approach, as outlined in the GRADE Handbook and Schünemann 2013, to assess the certainty of evidence for the following (clinically relevant) outcomes: any late‐onset sepsis, bacterial sepsis, fungal sepsis, all‐cause mortality, NEC ≥ stage II, chronic lung disease, threshold retinopathy of prematurity, length of hospital stay among survivors and duration of mechanical ventilation.
Two review authors (MP, GS) independently assessed the certainty of evidence for each of the outcomes above. We considered evidence from RCTs as high certainty but downgraded the evidence one level for serious (or two levels for serious) limitations based on the following: design (risk of bias), consistency across studies, directness of the evidence, precision of estimates, and presence of asymmetry of the funnel plot (publication bias). We used the GRADEpro GDT Guideline Development Tool to create a 'Summary of findings' table to report the certainty of the evidence.
The GRADE approach yields an assessment of the certainty of a body of evidence according to one of four grades.
High: We are very confident that the true effect lies close to the estimate of effect.
Moderate: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of effect but may be substantially different.
Low: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of effect.
Very low: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Subgroup analysis and investigation of heterogeneity
Key subgroups were based on the following.
-
Gestational age:
Preterm infants (32 to 36 weeks' gestational age)
Preterm infants (< 32 weeks' gestational age)
-
Birth weight:
VLBW infants (birth weight < 1500 g)
ELBW infants (birth weight < 1000 g)
-
Feedings:
Breast milk feeding
Formula feeding
Sensitivity analysis
We performed a post hoc sensitivity analysis by excluding studies of poor methodological certainty from the meta‐analysis for the outcome of late‐onset sepsis.
Results
Description of studies
Results of the search
Our search strategy yielded twelve randomized controlled trials (published in fourteen reports) that were eligible for inclusion (Figure 3). Three published reports described one multicenter trial of enteral lactoferrin prophylaxis in preterm neonates (Manzoni 2014), and the other included studies enrolled preterm neonates from the United States (Sherman 2016), Turkey (Akin 2014), Canada (Barrington 2016), India (Kaur 2015), Peru (Ochoa 2015, Ochoa 2020), United Kingdom (ELFIN 2018), Australia and New Zealand (LIFT 2020) and China (Dai 2015; Liu 2016; Tang 2017). Refer to the Characteristics of included studies table for details.
3.
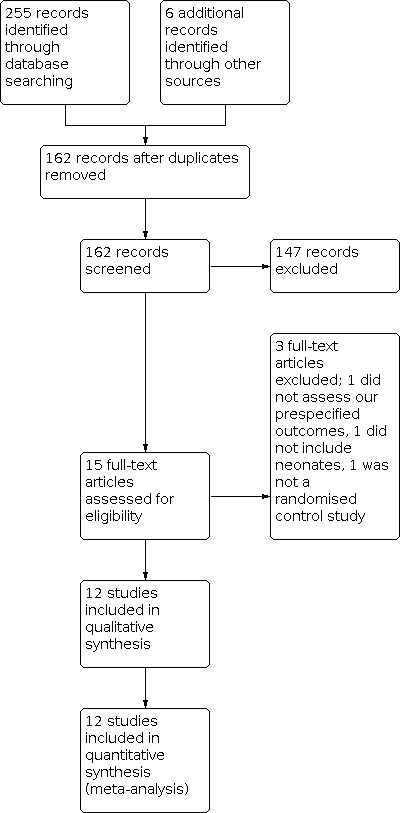
Study flow diagram for the updated search in January 20, 2020
Included studies
This study consisted of 3 separate reports published by the investigators in 2009, 2012 and 2014.
Manzoni 2009: Manzoni and coworkers randomly assigned VLBW infants (birth weight < 1500 g) in 11 Italian NICUs to enteral bovine lactoferrin alone or in combination with a probiotic (Lactobacillus rhamnosus GG) or to placebo. The study enrolled neonates from Oct 1, 2007 to July 31, 2008. Late‐onset sepsis, defined as isolation of a pathogen in the blood, peritoneal fluid, or CSF after three days of life, was the primary outcome of interest. Secondary outcomes assessed included gram‐positive, gram‐negative, or fungal sepsis; mortality before hospital discharge; urinary tract infection; fungal colonization; progression from fungal colonization to invasive fungal infection; bronchopulmonary dysplasia (BPD); severe intraventricular hemorrhage (grade III or IV); threshold retinopathy of prematurity (ROP); NEC ≥ stage II; alteration of liver functions; and adverse effects.
Manzoni 2012: This report presented the secondary analysis of data from the Manzoni 2009 report pertaining to fungal colonization and invasive fungal infections. Interventions and patient populations were similar to those in the Manzoni 2009 study. Prophylaxis with antifungal drugs was an exclusion criterion which was not permitted by the study protocol. Primary outcomes assessed were incidence rates of fungal colonization and invasive fungal infection. Secondary outcomes included intensity of fungal colonization, rate of progression to infection in colonized infants, frequencies of single fungal species in all groups, and mortality related to invasive fungal infections.
Report published in 2014: This continuation of a randomized trial (Manzoni 2009) was conducted to enhance power for assessing effects of enteral bovine lactoferrin in prevention of NEC. Thirteen neonatal intensive care units (NICUs) in Italy and New Zealand participated and enrolled neonates from October 1, 2007 through July 31, 2010. Interventions and patient populations and outcomes were similar to those included in the Manzoni 2009 study.
This prospective, single‐centre, double‐blind, randomized controlled trial was performed at Ankara University, Turkey, between December 2009 and January 2011. Investigators randomly assigned inborn neonates born at < 1500 g or at gestational age < 32 weeks to bovine lactoferrin (200 mg/d) or placebo (2 mL of saline), once a day until discharge. Exclusion criteria were lack of parental consent, severe congenital malformations, severe hypoxic‐ischemic encephalopathy (HIE), and death before 72 hours of life. Primary outcomes assessed were nosocomial sepsis as defined by criteria of the Centers for Disease Control and Prevention and NEC stage II. Secondary outcomes included safety (feeding tolerance, abdominal distention, emesis, and gastric residuals), length of hospital stay, and maturation of regulatory T‐cell (Treg) levels.
Ochoa and coworkers enrolled 190 preterm infants < 2500 g in five neonatal intermediate and intensive care units in Lima, Peru, who were admitted to the NICU during the first 72 hours of life. Researchers randomly assigned neonates to oral bovine lactoferrin (200 mg/kg/d divided into three doses) or to oral maltodextrin (200 mg/kg/d in three divided doses) for four weeks; they dissolved both in human milk or formula or in 5% glucose solution. The primary outcome assessed was the number of confirmed episodes of late‐onset sepsis in the first month of life; secondary outcomes assessed were incidence of gram‐positive and gram‐negative bacterial sepsis, fungal sepsis, pneumonia, diarrhea, and mortality in the first month of life.
This randomized clinical trial of human recombinant lactoferrin (talactoferrin (TLF)) conducted in the United States enrolled a total of 120 neonates (60 in each group). Investigators randomly assigned preterm infants with birth weight of 750 to 1500 g to enteral TLF or to placebo from 1 to 29 days of life at a dose of 150 mg/kg every 12 hours (TLF was provided by Agennix, Inc.). Primary outcomes assessed were bacteremia, meningitis, pneumonia, urinary tract infection, and necrotizing enterocolitis; secondary outcomes were sepsis syndrome and suspected NEC.
This randomized controlled trial of oral bovine lactoferrin in Montreal, Canada enrolled 79 neonates between January 2011 and April 2013. Investigators randomly assigned preterm infants in the NICU at CHU Sainte Justine, with a gestational age at birth between 23 0/7 and 30 6/7 weeks, who were less than 48 hours of age, to oral lactoferrin or placebo. The exclusion criterion was the presence of intestinal abnormalities that would prevent enteral feeding, such as gastroschisis. The intervention group received 100 mg per day of bovine lactoferrin, divided into two doses per day, starting on the first day of enteral feeding (day of enrollment) or at the latest at 48 hours of age and until 36 weeks' PMA or discharge home. The control group received milk without lactoferrin. The primary outcome assessed was feeding tolerance, defined as the length of time required to achieve 140 mL/kg/d; secondary outcomes were death, late‐onset sepsis, combined variable of death or late‐onset sepsis, NEC stage II or III, duration of total parenteral nutrition (TPN), number of times made nil by mouth, growth variables at discharge, ROP, and BPD.
This trial randomized inborn neonates with birth weight less than 2000 g, who had no maternal risk factors for sepsis, to bovine lactoferrin or to placebo from day 1 to day 28 of life. The dose of lactoferrin ranged from 100 to 250 mg and was based on birth weight. Criteria for exclusion were congenital anomalies, severe birth asphyxia, history of maternal chorioamnionitis, suspected congenital infection, and family history of cow's milk allergy. Neonates with culture‐proven early‐onset sepsis were also excluded. The primary outcome was culture‐proven late‐onset sepsis. Secondary outcome measures were probable late‐onset sepsis, any late‐onset sepsis, and sepsis‐attributed mortality.
This randomized trial in Puning, China, enrolled 105 very low birth weight infants between October 2010 and May 2014. The average gestational age was 30 weeks. The study investigated the effects of lactoferrin (100 mg/d) or lactoferrin plus probiotic LGG, comparing with control group (placebo). The primary outcome assessed was late‐onset sepsis and the secondary outcomes were the infection markers C‐reactive protein (CRP) and procalcitonin (PCT).
This randomized controlled trial, of oral bovine lactoferrin in Guangzhou, China, enrolled 257 infants between January 2013 and December 2015. Investigators randomly assigned preterm infants who were less than 72 hours of age into a control group, lactoferrin group, and lactoferrin plus probiotic LGG group. The exclusion criteria were congenital anomaly of digestive tract, respiratory distress more than three days, and discharge without medical advice. The intervention group received 125 mg/dose, 2 doses per day of bovine lactoferrin. The control group received the same volume of water with glucose (placebo). The primary outcomes assessed were late‐onset sepsis, NEC, mortality during hospitalization, and length of hospital stay.
This randomized controlled trial of oral bovine lactoferrin in Zhengzhou, China, enrolled 160 infants between March 2013 and June 2014. Investigators randomly assigned low birth weight infants (26‐36 weeks' gestational age) to lactoferrin or control groups at less than 72 hours of age. The exclusion criteria were infants receiving antifungal medications, early‐onset sepsis (within three days), and hepatic failure. The lactoferrin intervention group received 100 mg/d of bovine lactoferrin. The control group received the same volume of water with 5% glucose (placebo). The primary outcomes assessed were late‐onset sepsis, all‐cause mortality, and sepsis‐related mortality during hospitalization.
This multicenter, randomized, placebo‐controlled trial conducted in the United Kingdom examined prophylactic enteral lactoferrin supplementation to prevent late‐onset invasive infection in very preterm infants. The investigators enrolled 2203 participants between May 2014 to September 2017. Infants are eligible to participate if gestational age at birth was < 32 weeks', if they were < 72 hours old, and if written informed parental consent was obtained. Researchers randomly assigned infants to receive lactoferrin (150 mg/kg/d to a maximum of 300 mg) or placebo once daily until 34 completed weeks' post‐menstrual age. Primary outcomes assessed included the incidence of microbiologically confirmed or clinically suspected late‐onset infection from trial entry until hospital discharge. Secondary outcomes included 'all‐cause mortality' before hospital discharge; necrotizing enterocolitis (NEC) Bell’s stage II or III; severe ROP treated medically or surgically; BPD; a composite of invasive infection, major morbidity (NEC, ROP, or BPD), and mortality; number of days of administration of antibiotics per infant from 72 hours until death or discharge from hospital; number of days of administration of antifungal agents per infant; and length of hospital stay. This study was coordinated by the National Perinatal Epidemiology Unit Clinical Trials Unit, at the University of Oxford, UK. We thank Dr. William McGuire from the trial investigator group for providing data for inclusion in this systematic review.
The Lactoferrin Infant Feeding Trial (LIFT) to prevent sepsis and death in preterm infants was a double‐blind, randomized, controlled trial conducted in Australia and New Zealand. Eligibility for inclusion was based on the following: (1) doctor and parents are substantially uncertain whether bovine lactoferrin (BLF) is indicated or contraindicated, (2) < 1500 g birth weight, (3) < 7 days old, and (4) written informed consent from the parent. Researchers randomly assigned neonates to BLF at 200 mg/kg/d dissolved in breast milk or formula until 34 weeks' corrected gestational age or hospital discharge or to placebo (breast milk or formula (without BLF)). The primary outcome was mortality or major morbidity before hospital discharge. Morbidity was defined as the diagnosis of sepsis, brain injury, chronic lung disease, necrotizing enterocolitis, or severe retinopathy. Secondary outcomes assessed included mortality related to sepsis (as assessed by positive blood culture). The trial was registered as ACTRN12611000247976.
This was a phase 3 randomized controlled trial of oral lactoferrin for prevention of sepsis in infants (NEOLACTO study) conducted in Lima, Peru. Neonates with birth weight between 500 g and 2000 g and born in or referred to the neonatal unit of one of the participating hospitals during the first 72 hours of life were eligible. Investigators randomly assigned preterm neonates to oral bovine lactoferrin (200 mg/kg/d divided in three doses) or oral maltodextrin (200 mg/kg/d in three divided doses) for eight weeks. The primary outcome assessed was a composite outcome of first episode of late‐onset sepsis or sepsis‐associated death. The secondary outcome was neurodevelopment at 24 months' corrected age assessed by the Mullen Scale for Early Learning and Bayley III. The trial was registered as NCT01525316.
Excluded studies
Investigators enrolled healthy, formula‐fed infants at 34 weeks' gestation or later and at four weeks of age or younger from a pediatric clinic. Infants received formula supplemented with lactoferrin (850 mg/L) or commercial cow's milk‐based formula (102 mg/L) for 12 months. Researchers collected growth parameters and information on gastrointestinal, respiratory, and colic illnesses for the infants' first year. Review authors excluded this study, as most enrolled infants were beyond the neonatal period and trial authors did not assess our prespecified neonatal outcomes.
This community‐based, randomized, double‐blind, placebo‐controlled trial compared supplementation with bovine lactoferrin versus placebo. Investigators randomly assigned 577 weaned children at 12 to 18 months and followed them for six months with daily home visits. Treatment was given to prevent diarrhea, and outcomes assessed included number of diarrheal episodes, longitudinal prevalence of diarrhea, and severity of diarrhea and dehydration. Review authors excluded this study, as participants were not neonates.
This nonrandomized, retrospective, observational study compared the lactoferrin prophylaxis cohort (during the years 2004‐2011) with an historical cohort without lactoferrin prophylaxis (during the years 2001‐2004). The prophylaxis cohort received 100 mg of bovine lactoferrin and a probiotic. This conference abstract reported rates of NEC, late‐onset sepsis, and ROP treatment. Review authors excluded this study because it was a nonrandomized study.
Studies awaiting classification
This randomized controlled trial of lactoferrin supplementation included preterm infants with birth weight ≤ 1500 g and/or gestational age ≤ 32 weeks. The study excluded neonates if fetal‐onset disorders were recognizable at birth, and if milk intolerance, family history of allergy, and use of infant formula supplemented with lactoferrin were reported. The intervention group (n = 650) received a daily dose of 100 mg of lactoferrin, and the control group (n = 650) received only standard therapy. Primary outcomes to be assessed were antioxidant effects of lactoferrin and its ability to reduce free radical‐related diseases in the newborn; these were assessed through neurodevelopmental follow‐up. The secondary outcome was identification of a panel of markers for assessment of oxidative stress and for correlation with the lactoferrin antioxidant effect. This study planned to enroll 1300 neonates starting January 2011. We have re‐requested details of the study from the principal investigator.
This was a prospective, double‐blind, randomized, placebo‐controlled study of preterm infants (n = 60) with gestational age 26 ± 0 to 35 ± 6 weeks. Researchers excluded neonates if born weighing < 600 g, or if they had life‐threatening congenital malformations, non‐Dutch or non‐English‐speaking parents, or a history of allergy among parents or siblings. Trial investigators randomly assigned infants to standard preterm formula, standard preterm formula with probiotics (galacto‐oligosaccharides 28.5%, lactose 9.5%, galactose 0.5%, minerals 3.5%, fat 1.5%, and water 3%), or standard preterm formula with dairy lactoferrin 1 mg/100 mL (n = 20 in each group). The primary outcome assessed was composition of the gut flora at six weeks of full enteral feeds, incidence of infection, oxidative stress, and iron status. Secondary outcomes assessed were growth (weight, length, and head circumference), feeding intolerance, and psychomotor development at one year of age. This unpublished study was completed in 2009. We have re‐requested details of the study from the principal investigator.
This completed randomized controlled study enrolled 180 preterm neonates (< 37 weeks' gestation counting from the first day of the last menstrual period and confirmed by Ballard score) admitted to the NICUs of Ain Shams University Hospitals during the period from August 2014 to December 2015. Researchers further randomly subdivided enrolled participants into three groups according to the dose regimen of lactoferrin supplementation: Group A (60 preterm neonates) received oral lactoferrin supplementation at a dose of 100 mg/d starting on day 1 and continuing for four to six weeks; Group B (60 preterm neonates) received oral lactoferrin supplementation at a dose of 100 mg/d starting on day 3 (48 to 72 hours) of life and continuing for four to six weeks; and Group C (60 preterm neonates) who received placebo in the form of distilled water. Primary outcomes included evaluation of the effectiveness of oral lactoferrin in preventing neonatal sepsis according to Tollner score, haematological scoring system (HSS), and positive blood culture.over four to six weeks of life. Secondary outcomes included evaluation of the effects of lactoferrin supplementation on long‐term complications of BPD (defined by clinical symptoms and signs and chest X‐ray findings), ROP (as defined by the International Classification of Retinopathy of Prematurity (ICROP)), NEC (defined by Modified Bell's criteria), and any reported side effects for bovine lactoferrin. The trial was completed in October 2016. We have re‐requested details of the study from the principal investigator without response.
Ongoing studies
This double‐blind, randomized, controlled trial included neonates weighing between 500 g and 2500 g and at ≤ 36 weeks' gestation, who were born in or were referred to the NICU of one of the participating hospitals during the first 48 hours of life. Investigators randomly assigned preterm neonates to one of three groups: low‐dose lactoferrin (100 mg/d), high‐dose lactoferrin (150 mg/kg/twice daily), or placebo (distilled water). The primary outcome assessed was blood culture positivity; secondary outcomes were complete blood count with differential leukocyte count and C‐reactive protein quantitative assay. This study was scheduled to start in June 2013 and planned to enroll 180 preterm neonates through January 2016. We have re‐requested details of the study from the principal investigator without response.
Risk of bias in included studies
A 'Risk of bias' summary and graph are reported in Figure 4; and Figure 5.
4.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
5.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
In the multicenter trial of Manzoni 2014, investigators stratified randomization by centre and generated randomization sequences by using computer software. The pharmacy at each centre prepared the interventions and diluted them in milk feeds on the basis of randomization sequence. Akin 2014; Dai 2015; Liu 2016; and Tang 2017 did not report random sequence generation nor allocation concealment. Sherman 2016 randomly assigned enrolled neonates centrally using a permuted block method. Barrington 2016; ELFIN 2018; Kaur 2015; LIFT 2020; Ochoa 2015 and Ochoa 2020 had low risk of selection bias, as researchers reported adequate randomization and allocation concealment methods.
Blinding
Manzoni 2014 investigators diluted interventions in feeds and blinded clinical and research staff to the intervention. Blinding of clinicians was not adequately reported in Dai 2015; Liu 2016; or Tang 2017. Other included studies reported blinding of caregivers and were at low risk for performance bias.
None of the included studies except Akin 2014, ELFIN 2018 and LIFT 2020 explicitly reported blinding of outcome assessment.
Incomplete outcome data
Researchers in included studies assessed outcomes at hospital discharge and adequately accounted for incomplete data. In the study of Ochoa 2020, 25% of infants did not have a neurodevelopmental exam at 24 months either due to death or dropout.
Selective reporting
None of the included studies revealed selective outcome reporting or other biases.
Effects of interventions
Lactoferrin supplementation of enteral feeds versus placebo (comparison 1)
All twelve included trials provided outcome data for this comparison (Akin 2014; Barrington 2016; Dai 2015; ELFIN 2018; Kaur 2015; LIFT 2020; Liu 2016; Manzoni 2014; Ochoa 2015; Ochoa 2020; Sherman 2016; Tang 2017).
Late‐onset sepsis (outcome 1.1)
All infants with either suspected or culture proven sepsis (outcome 1.1.1)
This outcome includes data on suspected (when reported) and confirmed late‐onset sepsis. Only 4 of 12 included studies (ELFIN 2018; Kaur 2015; Ochoa 2015; Ochoa 2020) reported data on suspected sepsis and the rest reported culture‐proven sepsis. Lactoferrin supplementation of enteral feeds in preterm infants decreased suspected or culture proven late‐onset sepsis (typical RR 0.80, 95% CI 0.72 to 0.89; typical RD ‐0.05, 95% CI, ‐0.07 to ‐0.02; NNTB 20, 95% CI 14 to 50; 12 studies, 5425 participants) (Analysis 1.1)(Figure 6). Results showed moderate heterogeneity (I2 = 59%) among the twelve trials for this outcome. We downgraded evidence to low certainty because of risk of bias in the included trials, and asymmetry of the funnel plot.
1.1. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 1: Any late‐onset sepsis
6.

Forest plot of comparison: 1 Lactoferrin supplementation with enteral feeds versus placebo, outcome: 1.1 Any late‐onset sepsis.
Sensitivity analysis of good methodological studies (excluding studies of poor methodology: Dai 2015; Liu 2016; Tang 2017) showed that lactoferrin supplementation of enteral feeds in preterm infants decreased suspected or culture proven late‐onset sepsis (typical RR 0.82, 95% CI, 0.74 to 0.91; typical RD ‐0.04, 95% CI, ‐0.06 to ‐0.02; NNTB 20, 95% CI 14 to 50; 9 studies, 4702 participants, (low‐certainty evidence). Results showed moderate heterogeneity (I2 = 61%) among the nine trials for this outcome. (Analysis 1.11)
1.11. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 11: Late onset sepsis ‐ good methodology studies
Subgroup analyses for the outcome of late‐onset sepsis
Culture proven sepsis (outcome 1.1.2)
All 12 included studies reported on culture proven sepsis.The estimated risk ratio for the outcome of culture proven sepsis was (typical RR 0.83, 95% CI 0.73 to 0.94; typical RD ‐0.03, 95% CI, ‐0.040 to ‐0.01; NNTB 33, 95% CI 25 to 100; 12 studies, 5425 participants, low‐certainty evidence). Results showed moderate heterogeneity (I2 = 54%) among the twelve trials for this outcome. (Analysis 1.1)
Birth weight < 1000 g (outcome 1.1.3)
The estimated risk ratio for the outcome of late‐onset sepsis in ELBW infants was 0.31 (95% CI 0.14 to 0.70; RD ‐0.25, 95% CI ‐0.40 to ‐0.10; NNTB 4, 95% CI 2.5 to 25; 1 study, 113 participants) (Figure 6).
Birth weight 1000 to 1500 g (outcome 1.1.4)
The estimated risk ratio for the outcome of late‐onset sepsis in this subgroup was 0.46 (95% CI 0.12 to 1.74; RD ‐0.03, 95% CI ‐0.09 to 0.020; 1 study, 208 participants) (Figure 6).
Exclusively maternal milk‐fed infants (outcome 1.1.5)
The estimated risk ratio for the outcome of late‐onset sepsis in exclusively maternal milk fed infants was 1.02 (95% CI 0.81 to 1.30; RD 0.01, 95% CI ‐0.06 to 0.07; 2 studies, 685 participants) (Figure 6). This suggests no differences in late‐onset sepsis among preterm infants exclusively receiving maternal milk supplemented with lactoferrin.
Formula‐fed infants (outcome 1.1.6)
The estimated risk ratio for the outcome of late‐onset sepsis in formula‐fed infants was 0.75 (95% CI 0.38 to 1.50; RD ‐0.05, 95% CI ‐0.16 to 0.07; 2 studies, 159 participants) (Figure 6).
NEC ≥ stage II (outcome 1.2)
Enteral lactoferrin supplementation in preterm infants had no effect on NEC ≥ stage II (typical RR 1.10, 95% CI, 0.86 to 1.41; typical RD ‐0.00, 95% CI, ‐0.02 to 0.01; 7 studies, 4874 participants) (Figure 7). We observed mild heterogeneity (I2 = 37%) among the seven trials for this outcome. We downgraded the certainty of evidence to low because of risk of bias in the included trials and imprecision.
7.

Forest plot of comparison: 1 Lactoferrin supplementation with enteral feeds versus placebo, outcome: 1.2 NEC ≥ stage II.
All‐cause mortality (outcome 1.3)
Lactoferrin supplementation of enteral feeds in preterm infants did not affect 'all‐cause mortality' (typical RR 0.90, 95% CI 0.69 to 1.17; typical RD ‐0.00, 95% CI, ‐0.01 to 0.01; 11 studies, 5510 participants) (Figure 8). We noted mild heterogeneity (I2 = 26%) among the 11 included trials for this outcome. We downgraded the certainty of evidence to very low because of risk of bias in the included studies, imprecision and asymmetry of the funnel plot (publication bias and small poor‐certainty studies).
8.

Forest plot of comparison: 1 Lactoferrin supplementation with enteral feeds versus placebo, outcome: 1.3 All‐cause mortality.
Bacterial sepsis (outcome 1.4)
The estimated risk ratio for the outcome of bacterial sepsis in preterm infants was 0.86 (95% CI, 0.74 to 1.00; RD ‐0.02, 95% CI, ‐0.05 to 0.00; 8 studies, 3575 participants). We downgraded the certainty of evidence to moderate because of unclear risk of detection bias in the included trials and unclear risk of selection bias in one trial.
Fungal sepsis (outcome 1.5)
The estimated risk ratio for the outcome of fungal sepsis in preterm infants was 0.23 (95% CI, 0.10 to 0.54; RD ‐0.01, 95% CI, ‐0.02 to ‐0.01; NNTB 100, 95% CI 50 to 100; 6 studies, 3266 participants). This suggests a decrease in fungal sepsis among preterm infants whose feedings were supplemented with lactoferrin. We downgraded the certainty of evidence to moderate because of risk of bias.
Chronic lung disease (outcome 1.6)
The estimated typical risk ratio for the outcome of chronic lung disease was 1.00 (95% CI 0.89 to 1.12 and typical RD was 0.00, 95% CI ‐0.03 to 0.03; 5 studies, 2984 participants) (Figure 10). We observed no heterogeneity (I2 = 0%) among the four trials for this outcome. We downgraded the certainty of evidence to moderate because of unclear risk of bias in the included studies.
Duration of mechanical ventilation (outcome 1.7)
The estimated mean difference for the outcome of duration of mechanical ventilation in preterm infants was ‐0.45 (95% CI, ‐1.30 to 0.39; 3 studies, 925 participants). We downgraded the certainty of evidence to low because of unclear risk of bias, and because data were derived from only two studies (imprecision).
Length of hospital stay among survivors (outcome 1.8)
The estimated mean difference for the outcome of length of hospital stay among survivors in preterm infants was ‐2.38 (95% CI, ‐4.67 to ‐0.09; 3 studies, 1079 participants). We downgraded the certainty of evidence to low because of unclear risk of bias and severe heterogeneity (I2 = 85%).
Threshold retinopathy of prematurity (outcome 1.9)
The estimated risk ratio for the outcome of threshold ROP in preterm infants was 0.88 (95% CI, 0.69 to 1.13; RD ‐0.01, 95% CI, ‐0.02 to 0.01; 5 studies, 4515 participants). We downgraded the certainty of evidence to low because of unclear risk of bias, and moderate heterogeneity (I2 = 46%).
Urinary tract infection (outcome 1.10)
The estimated risk ratio for the outcome of urinary tract infection in preterm infants was 0.33 (95% CI, 0.13 to 0.86; RD ‐0.03, 95% CI, ‐0.05 to ‐0.01; NNTB 33, 95% CI 20 to 100; 3 studies, 854 participants). We downgraded the certainty of evidence to low because of unclear risk of bias, and because data were derived from only two studies (imprecision).
Neurodevelopmental outcome assessment at 24 months of age by Mullen testing (outcome 1.12)
There were no differences in the estimated mean difference for neurodevelopmental assessment at the age of 24 months by Mullen test after enteral lactoferrin supplementation. The estimated mean differences for subcomponents of the Mullen testing were: composite MD 0.70 (95% CI ‐2.36 to 3.76), gross motor ‐1.00 (95% CI ‐2.71 to 0.71), visual reception 0.60 (95% CI ‐1.53 to 2.73), fine motor ‐0.60 (95% CI ‐2.92 to 1.72), receptive language 0.30 (95% CI ‐2.42 to 3.02) and expressive language 0.90 (95% CI ‐0.83 to 2.63)(1 study, 292 participants). We downgraded the certainty of evidence to low because of unclear risk of bias, and because data were derived from only one study (Ochoa 2020)(imprecision).
Neurodevelopmental outcome assessment at 24 months of age by Bayley III testing (outcome 1.13)
There were no differences in the estimated mean difference for neurodevelopmental assessment at the age of 24 months by Bayley III testing after enteral lactoferrin supplementation. The estimated mean differences for subcomponents of the Bayley III testing were: cognitive MD ‐0.70 (95% CI ‐2.70 to 1.30), language 1.20 (95% CI ‐1.24 to 3.64), motor ‐0.90 (95% CI ‐3.73 to 1.93) and social emotional score ‐1.00 (95% CI ‐5.98 to 3.98)(1 study, 292 participants). We downgraded the certainty of evidence to low because of unclear risk of bias, and because data were derived from only one study (Ochoa 2020) (imprecision).
Other outcomes
No study reported adverse effects for this comparison.
Lactoferrin supplementation of enteral feeds in combination with probiotics versus placebo (comparison 2)
We derived outcome data for analyses for this comparison from three trials (Dai 2015; Manzoni 2014; Tang 2017), in which investigators randomly assigned preterm infants to enteral bovine lactoferrin or enteral bovine lactoferrin in combination with the probiotic Lactobacillus rhamnosus GG or placebo. All three studies included in this comparison used the same probiotic organism at the same dosage (6 x 109 colony forming units/day) but for different duration. We conducted subgroup analyses using birth weight and types of milk subgroups for late‐onset sepsis for the outcome of 'late‐onset sepsis.' Data for subgroup analyses for other outcomes were not available.
Late‐onset sepsis (outcome 2.1)
All infants with both suspected and confirmed sepsis (outcome 2.1.1)
The studies eligible for inclusion for this outcome reported only confirmed sepsis (Dai 2015; Manzoni 2014; Tang 2017). Lactoferrin supplementation of enteral feeds in combination with probiotics in preterm infants decreased confirmed late‐onset sepsis (typical RR 0.25, 95% CI 0.14 to 0.46; typical RD ‐0.13, 95% CI ‐0.18 to ‐0.08; NNTB 8, 95% CI 6 to 13; 3 studies, 564 participants). Results showed no heterogeneity (I2 = 0%) among the three trials for this outcome. We downgraded the certainty of evidence to low because of risk of bias in the included studies and the data from only three studies. There were no data for suspected sepsis from the included 3 studies.
Birth weight < 1000 g (outcome 2.1.2)
The estimated risk ratio for the outcome of late‐onset sepsis in ELBW infants was 0.30 (95% CI 0.13 to 0.69; RD ‐0.26, 95% CI ‐0.40 to ‐0.11; NNTB 5, 95% CI 2 to 9; 1 study, 114 participants). This suggests a decrease in late‐onset sepsis among ELBW infants who were supplemented with lactoferrin in combination with probiotics. We downgraded the certainty of evidence to low because data were obtained from only one study (Manzoni 2014) (imprecision) and risk of bias.
Birth weight 1000 to 1500 g (outcome 2.1.3)
The estimated risk ratio for the outcome of late‐onset sepsis in preterm infants with birth weight from 1000 to 1500 g was 0.16 (95% CI 0.02 to 1.27; RD ‐0.05, 95% CI ‐0.11 to 0.0; 1 study, 205 participants). We downgraded the certainty of evidence to low because data were obtained from only one study (Manzoni 2014)(imprecision) and risk of bias.
Exclusively maternal milk‐fed infants (outcome 2.1.4)
The estimated risk ratio for the outcome of late‐onset sepsis in preterm infants fed exclusively on maternal milk was 0.33 (95% CI 0.07 to 1.48; RD ‐0.13, 95% CI ‐0.28 to 0.02; 1 study, 69 participants). We downgraded the certainty of evidence to low because data were obtained from only one study (Manzoni 2014) (imprecision) and risk of bias.
Exclusively formula‐fed infants (outcome 2.1.5)
The estimated risk ratio for the outcome of late‐onset sepsis in preterm infants fed formula milk was 0.09 (95% CI 0.01 to 1.67; RD ‐0.18, 95% CI ‐0.35 to ‐0.01; 1 study, 48 participants). We downgraded the certainty of evidence to low because data were obtained from only one study (Manzoni 2014) (imprecision) and risk of bias.
NEC ≥ stage II (outcome 2.2)
Lactoferrin supplementation of enteral feeds in combination with probiotics in preterm infants decreased NEC ≥ stage II in preterm infants (RR 0.04, 95% CI 0.00 to 0.62; RD ‐0.05, 95% CI ‐0.08 to ‐0.03; NNTB 20, 95% CI 12.5 to 33.3; 1 study, 496 participants). We downgraded the certainty of evidence to very low because data were obtained from only one study (Manzoni 2014) (serious imprecision) and risk of bias.
All‐cause mortality (outcome 2.3)
The estimated risk ratio for the outcome of 'all‐cause mortality' in preterm infants was 0.58, 95% CI 0.30 to 1.13; RD ‐0.03, 95% CI ‐0.06 to 0.01; two studies, 671 participants). We downgraded the certainty of evidence to very low because data were obtained from only two studies (Manzoni 2014; Tang 2017) (serious imprecision) and risk of bias.
Bacterial sepsis (outcome 2.4)
The estimated risk ratio for the outcome of bacterial sepsis in preterm infants was 0.28 (95% CI 0.11 to 0.72; RD ‐0.09, 95% CI ‐0.14 to ‐0.03; NNTB 11, 95% CI 7 to 33; 1 study, 319 participants). We downgraded the certainty of evidence to low because data were obtained from only one study (Manzoni 2014) and unclear risk of bias.
Fungal sepsis (outcome 2.5)
The estimated risk ratio for the outcome of fungal sepsis in preterm infants was 0.24 (95% CI 0.08 to 0.71; RD ‐0.05, 95% CI ‐0.09 to ‐0.02; NNTB 20, 95% CI 11 to 50; 2 studies, 494 participants). This suggests a decrease in fungal sepsis among preterm infants whose feedings were supplemented with lactoferrin in combination with probiotics. We downgraded the certainty of evidence to low because of unclear risk of bias, and because data were obtained from only two studies (Manzoni 2014, Tang 2017) (imprecision).
Chronic lung disease (outcome 2.6)
The study definition of chronic lung disease was oxygen requirement greater than 30% for 28 days, positive‐pressure ventilation at 36 weeks, or both. We have requested data from the study authors on infants who required oxygen at 36 weeks' corrected age.
The estimated risk ratio for the outcome of chronic lung disease in preterm infants was 0.67 (95% CI 0.25 to 1.79; RD ‐0.02, 95% CI ‐0.07 to 0.03; 1 study, 319 participants). We downgraded the certainty of evidence to very low because data were obtained from only one study (Manzoni 2014) (serious imprecision) and unclear risk of bias.
Duration of mechanical ventilation (outcome 2.7)
The estimated mean difference for the outcome of 'duration of mechanical ventilation' in preterm infants was ‐1.10 (95% CI ‐3.04 to 0.84; 1 study, 321 participants). We downgraded the certainty of evidence to very low because data were obtained from only one study (Manzoni 2014) (serious imprecision) and unclear risk of bias.
Length of hospital stay among survivors (outcome 2.8)
The estimated mean difference for the outcome of 'length of hospital stay among survivors' in preterm infants was 2.00 (95% CI ‐1.88 to 5.88; 1 study, 496 participants). We downgraded the certainty of evidence to very low because data were obtained from only one study (Manzoni 2014) (serious imprecision) and unclear risk of bias.
Threshold retinopathy of prematurity (outcome 2.9)
The estimated risk ratio for the outcome of threshold ROP in preterm infants was 0.76 (95% CI 0.39 to 1.49; RD ‐0.03, 95% CI ‐0.09 to 0.04; 1 study, 319 participants). We downgraded the certainty of evidence to very low because data were obtained from only one study (Manzoni 2014) (serious imprecision) and unclear risk of bias.
Urinary tract infection (outcome 2.10)
The estimated risk ratio for the outcome of urinary tract infection in preterm infants was 0.67 (95% CI 0.25 to 1.79; RD ‐0.02, 95% CI ‐0.07 to 0.03; 1 study, 319 participants). We downgraded the certainty of evidence to very low because data were obtained from only one study (Manzoni 2014) (serious imprecision) and unclear risk of bias.
Other outcomes
The studies included in this comparison reported no adverse effects due to lactoferrin supplementation of enteral feeds in combination with probiotics. Included studies did not assess neurological outcome at two years of age or older or PVL.
Discussion
Summary of main results
We identified 12 randomized controlled trials that enrolled 5425 preterm infants and evaluated lactoferrin supplementation of enteral feeds with or without probiotics (Lactobacillus rhamnosus GG) compared with placebo.
I. Lactoferrin supplementation of enteral feeds without probiotics compared with placebo
Decreased late‐onset sepsis (both suspected and confirmed sepsis) (typical RR 0.80, 95% CI 0.72 to 0.89; typical RD ‐0.05, 95% CI, ‐0.07 to ‐0.02; NNTB 20, 95% CI 14 to 50; 12 studies, 5425 participants, low‐certainty evidence)
Subgroup analysis of data on confirmed late‐onset sepsis suggests decrease in late‐onset sepsis with enteral lactoferrin supplementation (typical RR 0.83, 95% CI 0.73 to 0.94; typical RD ‐0.03, 95% CI, ‐0.04 to ‐0.01; NNTB 33, 95% CI 25 to 100; 12 studies, 5425 participants, low‐certainty evidence)
Sensitivity analysis including only good methodological certainty studies suggested a decrease in late‐onset sepsis (both suspected and confirmed) with enteral lactoferrin supplementation (typical RR 0.82, 95% CI, 0.74 to 0.91; typical RD ‐0.04, 95% CI, ‐0.06 to ‐0.02; NNTB 20, 95% CI 14 to 50; 9 studies, 4702 participants).
Decreased fungal sepsis (typical RR 0.23, 95% CI, 0.10 to 0.54; RD ‐0.01, 95% CI, ‐0.02 to ‐0.01; NNTB 100, 95% CI 50 to 100; 6 studies, 3266 participants; moderate‐certainty evidence).
Decreased length of hospital stay (MD ‐2.38, 95% CI, ‐4.67 to ‐0.09; 3 studies, 1079 participants, low‐certainty evidence).
Decreased urinary tract infection (typical RR 0.33, 95% CI, 0.13 to 0.86; RD ‐0.03, 95% CI, ‐0.05 to ‐0.01; NNTB 33, 95% CI 20 to 100; 3 studies, 854 participants, low‐certainty evidence).
There were no differences in:
NEC stage II or III (typical RR 1.10, 95% CI, 0.86 to 1.41; typical RD ‐0.00, 95% CI, ‐0.02 to 0.01; 7 studies, 4874 participants; low‐certainty evidence).
'All‐cause mortality' (typical RR 0.90, 95% CI 0.69 to 1.17; typical RD ‐0.00, 95% CI, ‐0.01 to 0.01; 11 studies, 5510 participants; very low‐certainty evidence).
Chronic lung disease (typical RR 1.00, 95% CI 0.89 to 1.12; typical RD 0.00, 95% CI ‐0.03 to 0.03; 5 studies, 2984 participants; moderate‐certainty evidence).
Duration of mechanical ventilation (MD ‐0.45, 95% CI, ‐1.30 to 0.39; 3 studies, 925 participants; low‐certainty evidence).
Threshold retinopathy of prematurity (typical RR 0.88, 95% CI, 0.69 to 1.13; RD ‐0.01, 95% CI, ‐0.02 to 0.01; 5 studies, 4515 participants; low‐certainty evidence).
Neurodevelopmental outcomes at 24 months of age by Mullen and Bayley III developmental tests:
Mullen: The estimated mean differences for subcomponents of the Mullen testing were: composite MD 0.70 [‐2.36, 3.76], gross motor ‐1.00 [‐2.71, 0.71], visual reception 0.60 [‐1.53, 2.73], fine motor ‐0.60 [‐2.92, 1.72], receptive language 0.30 [‐2.42, 3.02] and expressive language 0.90 [‐0.83, 2.63], 1 study, 292 participants, low‐certainty evidence.
Bayley III: The estimated mean differences for subcomponents of the Bayley III testing were: cognitive MD ‐0.70 [‐2.70, 1.30], language 1.20 [‐1.24, 3.64], motor ‐0.90 [‐3.73, 1.93] and social emotional score ‐1.00 [‐5.98, 3.98], 1 study, 292 participants, low‐certainty evidence.
In subgroup analyses, extremely low birth weight (ELBW) infants and those fed exclusively maternal milk showed a reduction in late‐onset sepsis after oral lactoferrin supplementation (1 study; low‐certainty evidence). Investigators reported no differences in chronic lung disease or duration of mechanical ventilation.
II. Lactoferrin supplementation to enteral feeds with probiotics
Decreasedlate‐onset sepsis (typical RR 0.25, 95% CI 0.14 to 0.46; RD ‐0.13, 95% CI ‐0.18 to ‐0.08; NNTB 8, 95% CI 6 to 13; 3 studies, 564 participants; low‐certainty evidence). All 3 included studies reported data on confirmed sepsis only.
Decreased fungal sepsis (typical RR 0.24, 95% CI 0.08 to 0.71; RD ‐0.05, 95% CI ‐0.09 to ‐0.02; NNTB 20, 95% CI 11 to 50; 2 studies, 494 participants; low‐certainty evidence).
Decreased NEC stage II or III (typical RR 0.04, 95% CI 0.00 to 0.62; RD ‐0.05, 95% CI ‐0.08 to ‐0.03; NNTB 20, 95% CI 12.5 to 33.3; 1 study, 496 participants; very low‐certainty evidence).
No differences on 'all‐cause mortality' (typical RR 0.58, 95% CI 0.30 to 1.13; RD ‐0.03, 95% CI ‐0.06 to 0.01; 2 studies, 671 participants; very low‐certainty evidence).
No differences in chronic lung disease, urinary tract infection, duration of mechanical ventilation, or length of hospital stay.
Investigators did not report any adverse effects related to lactoferrin supplementation nor to the probiotic. None of the included studies assessed long‐term neurological outcomes or periventricular leukomalacia (PVL).
Overall completeness and applicability of evidence
The 12 randomized controlled trials were performed in neonatal intensive care units in Italy, New Zealand, the United States, Peru, Turkey, Canada, India, the United Kingdom, Australia & New Zealand, and China. Trials are currently ongoing in Egypt and the Netherlands. Studies have evaluated enteral lactoferrin in both the developing and the developed world.
We assessed visual asymmetry of the funnel plot for the outcome of 'late‐onset sepsis' and 'all‐cause mortality' where more than 10 trials provided data for inclusion (Figure 1; Figure 2). The visual analysis showed asymmetry of the funnel plot, with more trials with a positive outcome and few trials with no effect or negative outcomes. The asymmetry can be explained by publication bias but also by many small studies (Akin 2014; Barrington 2016; Dai 2015; Kaur 2015; Liu 2016; Ochoa 2015; Sherman 2016; and Tang 2017), some with poor methodological quality inflating the effects of enteral lactoferrin supplementation. We have downgraded the evidence based on publication bias, small studies with poor methodological certainty for the outcomes of late‐onset sepsis and 'all‐cause mortality'.
A major concern of investigators in the initial trials was safety of enteral lactoferrin in preterm neonates, especially ELBW infants, who are at high risk of developing sepsis and NEC. In this review involving more than 5200 preterm neonates, researchers observed no adverse effects due to enteral lactoferrin. One trial evaluated human recombinant lactoferrin; all other trials used bovine lactoferrin. Bovine lactoferrin has a 69% DNA sequence homology to human lactoferrin (Pierce 1991). Differences in glycosylation patterns of human recombinant and bovine lactoferrins may be responsible for differences in susceptibility to proteolysis and pathogen adhesion (Barboza 2012; Bellamy 1992). Whether human lactoferrin is as effective in vivo as bovine lactoferrin, or whether higher doses of human lactoferrin can be tolerated, needs to be confirmed in future trials.
The optimal timing of prophylaxis is unclear but supplementation as early as possible after birth appeals to reason. Three trials recruited subjects within the first three days of life ELFIN 2018; Manzoni 2014 and Ochoa 2020 and one recent trial in the first seven days of life (LIFT 2020). The duration of prophylaxis with enteral lactoferrin that provides optimal benefit without adverse effects for preterm neonates remains unclear but two recent large trials (ELFIN 2018; LIFT 2020) continued lactoferrin till 34 weeks corrected gestational age and the latest study (Ochoa 2020) for eight weeks after birth. It is not clear whether prophylaxis of increased duration is more effective in preventing late‐onset sepsis or NEC. Dosing based on birth weight (150‐300 mg/kg/day) was considered optimal and was used in the most recent trials (ELFIN 2018; LIFT 2020; Ochoa 2020).
Quality of the evidence
We assessed the certainty of evidence using the GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) method (Guyatt 2008); we downgraded the certainty of evidence to low or very low on the basis of potential risk of bias, availability of data from only one or two studies (imprecision), the presence of moderate to severe heterogeneity (inconsistency) and asymmetry of the funnel plot. Eight out of twelve included studies reported explicit randomization and allocation concealment without risk of bias. In the Akin 2014; Dai 2015; Liu 2016; and Tang 2017 studies, investigators could not assess generation of randomization sequences and allocation concealment, and the risk of selection bias was unclear. We noted that all included studies except Dai 2015; Liu 2016; and Tang 2017, were at low or unclear risk for performance bias. In Manzoni 2014, researchers diluted interventions in feeds, and clinical and research staff were blinded to the intervention. Other included studies did not show risk of performance bias. None of the included studies explicitly reported blinding of outcome assessors (to minimize detection bias) except Akin 2014; ELFIN 2018, LIFT 2020; and Ochoa 2020. Investigators in included studies, except Ochoa 2020, noted no attrition bias, performed all outcome assessments before hospital discharge, and adequately accounted for incomplete data.
Potential biases in the review process
We strove to decrease bias in the review process. Both review authors performed the literature search using an inclusive search strategy and combined search results. Our search strategy revealed fourteen reports on prespecified neonatal outcomes from 12 randomized clinical trials. Our post hoc analysis of evaluation of fungal sepsis, bacterial sepsis, threshold retinopathy of prematurity, or urinary tract infection did not change the conclusions of the review. We contacted investigators of published randomized controlled trials and searched conference proceedings for data and missing information with limited success.
Agreements and disagreements with other studies or reviews
We identified one review that synthesized data from trials of lactoferrin supplementation of enteral feeds in preterm neonates by meta‐analysis using a random‐effects model (He 2018). This review included nine RCTs with 1834 participants and reported that lactoferrin enteral supplementation decreased late‐onset sepsis, NEC stage II or III, hospital‐acquired infection, infection‐related mortality, decreased time to full enteral feeds but no decrease in 'all cause mortality.' Our review found decreased late‐onset sepsis and fungal sepsis but decrease in NEC stage II or III only when lactoferrin was combined with probiotics. Our review also did not find any effect on 'all‐cause mortality.' Ochoa 2017 and Turin 2014 reviewed the details of published and ongoing clinical trials on oral lactoferrin prophylaxis in preterm neonates. Lingappan 2013 reviewed and expanded on the biology, anti‐microbial effects, and immunomodulatory effects of lactoferrin and commented on efficacy and safety related to its use in the newborn.
Authors' conclusions
Implications for practice.
We found low‐certainty evidence that lactoferrin supplementation of enteral feeds decreases late‐onset sepsis (both suspected and confirmed, and confirmed only) but not NEC ≥ stage II, 'all cause mortality', or neurodevelopmental outcomes at 24 months of age in preterm infants without adverse effects. Low to very low‐certainty evidence suggests that lactoferrin supplementation of enteral feeds in combination with probiotics decreases late‐onset sepsis (data from confirmed sepsis only) and NEC ≥ stage II in preterm infants without adverse effects, however, there are very few studies and included studies are of poor methodological quality. Due to the presence of publication bias and small studies of poor methodology inflating the effect size, recommendations for clinical practice remain difficult.
Implications for research.
Addition of data from ongoing trials to the meta‐analysis may or may not enhance the certainty and applicability of evidence for enteral lactoferrin prophylaxis in preterm infants. Study findings should also clarify effects of exclusive maternal milk feeding and addition of probiotics to lactoferrin supplementation. An individual patient data meta‐analysis is underway and may provide useful data including dosing and whether infants fed on human milk or formula will benefit the most from enteral supplementation with lactoferrin.
What's new
| Date | Event | Description |
|---|---|---|
| 2 February 2021 | Amended | Added the full publication reference for the LIFT 2020 trial. Amedned author name to Kanekal S Gautham. |
History
Protocol first published: Issue 2, 2008 Review first published: Issue 5, 2010
| Date | Event | Description |
|---|---|---|
| 5 May 2020 | Amended | Amended to correct the outcome data for late onset sepsis, which did not change the direction or appreciably change the magnitude of the outcome. |
| 24 March 2020 | New citation required and conclusions have changed | Conclusions and summary of findings table have been revised with the inclusion of 6 new studies. |
| 24 March 2020 | New search has been performed | We updated the search on Jan 20th, 2020 and new trials were included in the meta‐analysis. |
| 18 December 2018 | Feedback has been incorporated | Editorial feedback incorporated |
| 13 October 2018 | New search has been performed | We updated the literature search in September 2018 and the review was updated with four new studies. We updated the data on late‐onset sepsis from Sherman 2016 based on author feedback. Conclusions and summary of findings table revised. |
| 3 May 2017 | New citation required but conclusions have not changed | Conclusions are unchanged |
| 11 February 2017 | New search has been performed | We updated the literature search in December 2016, added 2 new studies, updated data for previously included studies, and added 1 excluded study and 1 ongoing study. This review updates the review, "Oral lactoferrin for the prevention of sepsis and necrotizing enterocolitis in preterm infants" (Pammi 2015) |
| 9 September 2014 | New citation required but conclusions have not changed | We updated the search in July 2014. We revised the review by adding 4 new included studies, 4 new ongoing studies, and 2 "studies awaiting classification." We revised the text and conclusions of the review. Additionally, we used the GRADE method to rate the quality of evidence |
| 22 August 2014 | New search has been performed | This review updates the review, "Oral lactoferrin for the prevention of sepsis and necrotizing enterocolitis in preterm infants" (Pammi 2011) |
| 9 November 2011 | Amended | Abstract, Results: We corrected Manzoni reference from Manzoni 2008 to Manzoni 2009 |
| 11 July 2011 | New search has been performed | This review updates the review, "Oral lactoferrin for the
prevention of sepsis and necrotizing enterocolitis in
preterm infants," which was published in the Cochrane
Database of Systematic Reviews (Pammi 2010) We performed an updated search in July 2011 and identified 2 additional ongoing studies (Akin 2009 and Ochoa 2011a) |
| 11 July 2011 | New citation required but conclusions have not changed | We made no changes to the conclusions |
| 7 December 2010 | Amended | We updated review author contact details |
| 11 May 2010 | Amended | Copyeditor made minor text edits |
| 7 July 2008 | Amended | We were able to review the study protocol |
Acknowledgements
We sincerely acknowledge the help of Yolanda Montagne Brosseau in performing a literature search in Embase.
We acknowledge the help of Dr.Tao Xiong for translation and extraction of data from 3 studies published in Chinese.
We acknowledge the contributions of Dr Steve Abrams, previous co‐author of this review.
The methods section of this protocol is based on a standard template used by Cochrane Neonatal.
Appendices
Appendix 1. Cochrane Neonatal standard search strategy
PubMed: ((infant, newborn[MeSH] OR newborn OR neonate OR neonatal OR premature OR low birth weight OR VLBW OR LBW or infan* or neonat*) AND (randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized [tiab] OR placebo [tiab] OR drug therapy [sh] OR randomly [tiab] OR trial [tiab] OR groups [tiab]) NOT (animals [mh] NOT humans [mh]))
Embase: (infant, newborn or newborn or neonate or neonatal or premature or very low birth weight or low birth weight or VLBW or LBW or Newborn or infant* or neonat*) AND (human not animal) AND (randomized controlled trial or controlled clinical trial or randomized or placebo or clinical trials as topic or randomly or trial or clinical trial)
CINAHL: (infant, newborn OR newborn OR neonate OR neonatal OR premature OR low birth weight OR VLBW OR LBW or Newborn or infant* or neonat*) AND (randomized controlled trial OR controlled clinical trial OR randomized OR placebo OR clinical trials as topic OR randomly OR trial OR PT clinical trial)
Cochrane Library: (infant or newborn or neonate or neonatal or premature or preterm or very low birth weight or low birth weight or VLBW or LBW)
We used this search strategy for MEDLINE and PREMEDLINE (adapted strategy as needed to suit Embase, CINAHL, and CENTRAL).
explode "sepsis" [all subheadings in MIME, MJME].
sepsis or septicemia.
septic.
NEC.
"necrotizing enterocolitis".
# 1 or # 2 or # 3 or # 4 or # 5.
explode "infant ‐ newborn" [all subheadings in MIME, MJME].
Neonat*.
Newborn*.
# 7 or # 8 or # 9.
# 6 and # 10.
"lactoferrin" [all subheadings on MIME, MJME].
talactoferrin.
# 10 or # 11.
# 9 and # 12.
Appendix 2. Risk of bias tool
We used the standard methods of the Cochrane Collaboration and the Cochrane Neonatal Review Group to assess the methodological certainty (to meet the validity criteria) of the trials. For each trial, we sought information regarding the method of randomization and blinding and reporting of all outcomes of all infants enrolled in the trial. We assessed each criterion as low, high, or unclear risk. Two review authors separately assessed each study. We resolved disagreements by discussion. We added this information to the Characteristics of included studies table. We evaluated the following issues and entered the findings into the 'Risk of bias' table.
1. Sequence generation (checking for possible selection bias). Was the allocation sequence adequately generated?
For each included study, we categorised the method used to generate the allocation sequence as:
a. Low risk (any truly random process, e.g. random number table; computer random number generator);
b. High risk (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number); or
c. Unclear risk.
2. Allocation concealment (checking for possible selection bias). Was allocation adequately concealed?
For each included study, we categorised the method used to conceal the allocation sequence as:
a. Low risk (e.g. telephone or central randomization; consecutively numbered sealed opaque envelopes);
b. High risk (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
c. Unclear risk.
3. Blinding of participants and personnel (checking for possible performance bias). Was knowledge of the allocated intervention adequately prevented during the study?
For each included study, we categorised the methods used to blind study participants and personnel from knowledge of which intervention a participant received. Blinding was assessed separately for different outcomes or classes of outcomes. We categorized the methods as:
a. Low risk, high risk, or unclear risk for participants; or
b. Low risk, high risk, or unclear risk for personnel.
4. Blinding of outcome assessment (checking for possible detection bias). Was knowledge of the allocated intervention adequately prevented at the time of outcome assessment?
For each included study, we categorized the methods used to blind outcome assessment. Blinding was assessed separately for different outcomes or classes of outcomes. We categorized the methods as:
a. Low risk for outcome assessors;
b. High risk for outcome assessors; or
c. Unclear risk for outcome assessors.
5. Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations). Were incomplete outcome data adequately addressed?
For each included study and for each outcome, we described the completeness of data including attrition and exclusions from the analysis. We noted whether attrition and exclusions were reported, numbers included in the analysis at each stage (compared with total randomized participants), reasons for attrition or exclusion when reported, and whether missing data were balanced across groups or were related to outcomes. When sufficient information was reported or supplied by trial authors, we re‐included missing data in the analyses. We categorized the methods as:
a. Low risk (< 20% missing data);
b. High risk (≥ 20% missing data); or
c. Unclear risk.
6. Selective reporting bias. Were reports of the study free of the suggestion of selective outcome reporting?
For each included study, we described how we investigated the possibility of selective outcome reporting bias and what we found. We assessed methods as:
a. Low risk (when it is clear that all of the study's prespecified outcomes and all expected outcomes of interest to the review have been reported);
b. High risk (when not all the study's prespecified outcomes have been reported; when one or more reported primary outcomes were not prespecified outcomes of interest and are reported incompletely and so cannot be used; when study fails to include results of a key outcome that would have been expected to have been reported); or
c. Unclear risk.
7. Other sources of bias. Was the study apparently free of other problems that could put it at high risk of bias?
For each included study, we described any important concerns that we had about other possible sources of bias (e.g. whether a potential source of bias was related to the specific study design, whether the trial was stopped early owing to some data‐dependent process). We assessed whether each study was free of other problems that could put it at risk of bias as:
a. Low risk;
b. High risk; or
c. Unclear risk.
If needed, we explored the impact of the level of bias by undertaking sensitivity analyses.
Data and analyses
Comparison 1. Lactoferrin supplementation with enteral feeds versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Any late‐onset sepsis | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1.1 All infants with both suspected and culture proven sepsis | 12 | 5425 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.72, 0.89] |
| 1.1.2 Culture‐proven sepsis | 12 | 5425 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.72, 0.94] |
| 1.1.3 Birth weight < 1000 g | 1 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.14, 0.70] |
| 1.1.4 Birth weight 1000‐1500 g | 1 | 208 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.12, 1.74] |
| 1.1.5 Maternal milk‐fed infants | 2 | 685 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.81, 1.30] |
| 1.1.6 Formula‐fed infants | 2 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.38, 1.50] |
| 1.2 NEC ≥ stage II | 7 | 4874 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.69, 1.17] |
| 1.3 All‐cause mortality | 11 | 5510 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.70, 1.30] |
| 1.4 Bacterial sepsis | 8 | 3575 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.74, 1.00] |
| 1.5 Fungal infection | 6 | 3266 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.10, 0.54] |
| 1.6 Chronic lung disease | 5 | 2984 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.89, 1.12] |
| 1.7 Duration of mechanical ventilation | 3 | 925 | Mean Difference (IV, Fixed, 95% CI) | ‐0.45 [‐1.30, 0.39] |
| 1.8 Length of stay among survivors | 3 | 1079 | Mean Difference (IV, Fixed, 95% CI) | ‐2.38 [‐4.67, ‐0.09] |
| 1.9 Threshold retinopathy of prematurity | 5 | 4515 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.69, 1.13] |
| 1.10 Urinary tract Infection | 3 | 854 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.13, 0.86] |
| 1.11 Late onset sepsis ‐ good methodology studies | 9 | 5023 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.74, 0.91] |
| 1.12 Neurodevelopemental outcome by Mullen at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.12.1 Composite | 1 | 292 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐2.36, 3.76] |
| 1.12.2 Gross motor | 1 | 292 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐2.71, 0.71] |
| 1.12.3 Visual reception | 1 | 292 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐1.53, 2.73] |
| 1.12.4 Fine motor | 1 | 292 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐2.92, 1.72] |
| 1.12.5 Receptive language | 1 | 292 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐2.42, 3.02] |
| 1.12.6 Expressive language | 1 | 292 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.83, 2.63] |
| 1.13 Neurodevelopmental outcome by Bayley III at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.13.1 Cognitive | 1 | 224 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐2.70, 1.30] |
| 1.13.2 Language | 1 | 224 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐1.24, 3.64] |
| 1.13.3 Motor | 1 | 224 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐3.73, 1.93] |
| 1.13.4 Social emotional score | 1 | 224 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐5.98, 3.98] |
1.2. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 2: NEC ≥ stage II
1.3. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 3: All‐cause mortality
1.4. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 4: Bacterial sepsis
1.5. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 5: Fungal infection
1.6. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 6: Chronic lung disease
1.7. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 7: Duration of mechanical ventilation
1.8. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 8: Length of stay among survivors
1.9. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 9: Threshold retinopathy of prematurity
1.10. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 10: Urinary tract Infection
1.12. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 12: Neurodevelopemental outcome by Mullen at 24 months
1.13. Analysis.

Comparison 1: Lactoferrin supplementation with enteral feeds versus placebo, Outcome 13: Neurodevelopmental outcome by Bayley III at 24 months
Comparison 2. Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Any late‐onset sepsis | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 All infants | 3 | 564 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.14, 0.46] |
| 2.1.2 Birth weight < 1000 g | 1 | 114 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.13, 0.69] |
| 2.1.3 Birth weight 1000‐1500 g | 1 | 205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.27] |
| 2.1.4 Maternal milk‐fed infants | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.07, 1.48] |
| 2.1.5 Formula milk‐fed infants | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.67] |
| 2.2 NEC ≥ stage II | 1 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.04 [0.00, 0.62] |
| 2.3 All‐cause mortality | 2 | 671 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.30, 1.13] |
| 2.4 Bacterial sepsis | 1 | 319 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.11, 0.72] |
| 2.5 Fungal Infection | 2 | 494 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.08, 0.71] |
| 2.6 Chronic lung disease | 1 | 319 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.25, 1.79] |
| 2.7 Duration of mechanical ventilation | 1 | 319 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐3.04, 0.84] |
| 2.8 Length of stay among survivors | 1 | 496 | Mean Difference (IV, Fixed, 95% CI) | 2.00 [‐1.88, 5.88] |
| 2.9 Threshold retinopathy of prematurity | 1 | 319 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.39, 1.49] |
| 2.10 Urinary tract infection | 1 | 319 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.25, 1.79] |
2.1. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 1: Any late‐onset sepsis
2.2. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 2: NEC ≥ stage II
2.3. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 3: All‐cause mortality
2.4. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 4: Bacterial sepsis
2.5. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 5: Fungal Infection
2.6. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 6: Chronic lung disease
2.7. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 7: Duration of mechanical ventilation
2.8. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 8: Length of stay among survivors
2.9. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 9: Threshold retinopathy of prematurity
2.10. Analysis.

Comparison 2: Lactoferrin supplementation with enteral feeds in combination with probiotics versus placebo, Outcome 10: Urinary tract infection
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Akin 2014.
| Study characteristics | ||
| Methods | Prospective, single‐centre, double‐blind, randomized controlled trial | |
| Participants | Inborn neonates, birth weight < 1500 g or gestational age < 32 weeks. Exclusion criteria were lack of parental consent, severe congenital malformations, and severe HIE or death before 72 hours of life. | |
| Interventions | Bovine lactoferrin (200 mg/d) or placebo (2 mL of saline) once a day until discharge | |
| Outcomes | Primary outcomes: nosocomial sepsis as defined by CDC criteria, NEC stage II. Secondary outcomes: safety (feeding tolerance, abdominal distention, emesis, and gastric residuals), length of hospital stay, maturation of Treg levels | |
| Notes | Ankara University, Turkey; conducted between December 2009 and January 2011 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Clinicians and outcome assessors were unaware of study groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analysed data from 47/50 enrolled neonates |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | Followed up 47/50 enrolled neonates |
| Blinding of outcome assessment | Low risk | Coordinator who was blinded to the study group assessed outcomes. |
Barrington 2016.
| Study characteristics | ||
| Methods | Single‐centre, blinded, randomized trial | |
| Participants | Inborn infants at < 31 weeks' gestation were enrolled in the first 48 hours of life. Exclusion criteria were proven or suspected gastrointestinal anomalies, serious cardiac anomalies, moribund and not expected to survive. | |
| Interventions | Milk supplemented with 100 mg of bovine lactoferrin OR milk with no lactoferrin supplementation. All infants received probiotics as per unit policy. | |
| Outcomes | Primary outcome: feed tolerance defined as time taken to achieve feeds to 140 mL/kg/d. Secondary outcomes: late‐onset sepsis, death, NEC, duration of TPN, growth variables, BPD, ROP | |
| Notes | Study conducted in Montreal, Canada, from December 2012 to September 2013 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomization |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Only the technician in the kitchen who prepared the milk knew the allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None noted |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | No attrition noted |
| Blinding of outcome assessment | Unclear risk | Blinding of outcome assessors was not explicit. |
Dai 2015.
| Study characteristics | ||
| Methods | Single centre, randomized, placebo‐controlled trial | |
| Participants | VLBW infants, average GA 30 weeks (range 26‐33 weeks) | |
| Interventions | 3 groups: first group placebo, second group lactoferrin, third group lactoferrin with probiotics | |
| Outcomes | Primary outcome: culture‐proven late‐onset sepsis. Secondary outcomes: CRP and procalcitonin | |
| Notes | Puning People's Hospital, China, Oct 2010 to May 2014 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The exact method of random generation not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not known |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not known |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts noted in the short‐term outcomes that were evaluated |
| Selective reporting (reporting bias) | Unclear risk | No details |
| Other bias | Unclear risk | None noted |
| Completeness of follow‐up | Unclear risk | NK |
| Blinding of outcome assessment | Unclear risk | Not explicit |
ELFIN 2018.
| Study characteristics | ||
| Methods | Phase 3, multicenter, placebo‐controlled, randomized controlled trial in the United Kingdom | |
| Participants | Infants eligible to participate if:
1.
gestational age at birth < 32 weeks;
2.
< 72 hours old; and
3. written informed
parental consent was obtained. If infants were receiving antibiotic treatment for suspected or confirmed infection, they were still eligible for recruitment. Exclusion criteria included: 1. infants with severe congenital anomalies; 2. anticipated enteral fasting longer than 14 days; and 3. infants who, in the opinion of the treating clinician, had no realistic prospect of survival. |
|
| Interventions | Infants were randomly allocated to receive lactoferrin (150 mg/kg/d to a maximum of 300 mg) or placebo. Until discharge, they were monitored for late‐onset invasive infection, necrotizing enterocolitis, bronchopulmonary dysplasia, retinopathy of prematurity, length of hospital stay, and length of time in intensive care. | |
| Outcomes | Primary outcome: incidence of microbiologically
confirmed or clinically suspected late‐onset
infection from trial entry until hospital
discharge Secondary outcomes: 1. All‐cause mortality before hospital discharge; 2. necrotizing enterocolitis (NEC): Bell’s stage II or III; 3. Severe retinopathy of prematurity (ROP) treated medically or surgically; 4. Bronchopulmonary dysplasia (BPD): Infant was still receiving mechanical ventilator support or supplemental oxygen at 36 weeks' postmenstrual age; 5. A composite outcome of invasive infection, major morbidity (NEC, ROP, or BPD as defined above), and mortality; 6. Total number of days of administration of antibiotics per infant from 72 hours until death or discharge from hospital; 7. Total number of days of administration of antifungal agents per infant; 8. Total length of stay until discharge home; 9. Length of stay in (1) intensive care, (2) high dependency care, (3) special care. |
|
| Notes | This study was coordinated by the National Perinatal Epidemiology Unit Clinical Trials Unit, at the University of Oxford, UK: ISRCTN88261002. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Secure web‐based randomization facility at the National Perinatal Epidemiology Unit, University of Oxford |
| Allocation concealment (selection bias) | Low risk | No bias noted. Secure web‐based randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of parents, clinicians, investigators and outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome status not known for 45 infants of 2203 recruited (2%) |
| Selective reporting (reporting bias) | Low risk | No selective reporting noted |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | Outcome status not known for 45 infants of 2203 recruited (2%) |
| Blinding of outcome assessment | Low risk | Outcome assessors blinded to intervention assignment |
Kaur 2015.
| Study characteristics | ||
| Methods | Single‐centre, randomized, placebo‐controlled trial | |
| Participants | Inborn neonates admitted in the first 12 hours of birth with no maternal risk factors for sepsis were enrolled. Exclusion criteria were congenital anomalies, severe birth asphyxia, history of maternal chorioamnionitis, suspected congenital infection, family history of cow's milk allergy. Neonates with culture‐proven early‐onset sepsis were also excluded. | |
| Interventions | Infants were randomized to bovine lactoferrin (100‐250 mg/d based on birth weight) or placebo once daily for the first 28 days of life. | |
| Outcomes | Primary outcome: culture‐proven late‐onset sepsis. Secondary outcomes: probable late‐onset sepsis, any late‐onset sepsis, sepsis‐attributed mortality | |
| Notes | Conducted in northern India between May 2012 and June 2013 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomization by a computer‐generated random table |
| Allocation concealment (selection bias) | Low risk | Sealed envelope method |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Physician and parents were blinded. Study drug and placebo sachets with lactoferrin were similar in appearance and were prepared by the hospital pharmacy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: < 10% accounted for in the analysis |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | Loss to follow‐up < 10% |
| Blinding of outcome assessment | Unclear risk | Blinding of outcome assessors was not explicit. |
LIFT 2020.
| Study characteristics | ||
| Methods | A multicenter, double‐blind, randomized trial conducted at 16 Australian and New Zealand sites | |
| Participants | Infants with birth weight below 1,500 g and younger than eight days were randomly assigned 200 mg/kg lactoferrin as daily supplements or no lactoferrin supplement. Web‐based randomization was minimized by site, sex, birth weight < 1000 versus ≥ 1000‐1499 g and single versus multi‐fetal pregnancy. Parents, caregivers and investigators were unaware of group assignment. | |
| Interventions | 200 mg/kg lactoferrin as daily supplements or no lactoferrin supplement | |
| Outcomes | The primary outcome was death‐before‐hospital discharge or major morbidity, defined as brain injury, necrotizing enterocolitis, late‐onset sepsis, or retinopathy treated before hospital discharge. | |
| Notes | This trial was registered with the Australian and New Zealand Clinical Trials Registry, number ACTRN12611000247976. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were allocated to treatment or control by central, web‐based randomization in a 1:1 ratio using minimization with a random component, stratifying by site, gender, birth weight (< 1000 vs ≥ 1000‐1499 g) and multiple birth (yes or no). |
| Allocation concealment (selection bias) | Low risk | Central randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Lactoferrin was mixed with milk by designated staff. Clinical team unaware |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None noted |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as per prespecified protocol |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | All participants assessed for outcomes before or at hospital discharge |
| Blinding of outcome assessment | Low risk | Outcome assessors unaware of intervention assignment |
Liu 2016.
| Study characteristics | ||
| Methods | Single centre, quasi‐randomized trial. not clear how admission sequence affected randomization | |
| Participants | Bwt < 2500 g, GA 26‐36 weeks | |
| Interventions | Two groups of 80 each, one group randomized to lactoferrin and other to placebo | |
| Outcomes | The primary outcome was late‐onset sepsis and secondary outcomes were NEC, 'in hospital mortality', pneumonia and length of hospitalization. | |
| Notes | North China‐ ZhengZhou Peoples hospital, March 2012‐ June 2014 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Possibly a quasi‐randomized trial due to sequence of participant admission |
| Allocation concealment (selection bias) | Unclear risk | No details available |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details available |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None noted |
| Selective reporting (reporting bias) | Unclear risk | Difficult to assess |
| Other bias | Unclear risk | None noted |
| Completeness of follow‐up | Low risk | Yes |
| Blinding of outcome assessment | Unclear risk | Not explicitly stated |
Manzoni 2014.
| Study characteristics | ||
| Methods | Prospective, multicenter, double‐blind, placebo‐controlled, randomized trial, reported in 3 published reports in 2009, 2012 and 2014 | |
| Participants | Preterm neonates with birth weight < 1500 g within the first 3 days of life, enrolled from 13 neonatal intensive care units in Italy and New Zealand, from October 1, 2007, through July 31, 2010 | |
| Interventions | Infants randomized to 3 groups: Bovine lactoferrin
(100 mg/d) alone or bovine lactoferrin (100 mg/d)
with Lactobacillus rhamnosus LGG (6 ×
109 CFU/mL) or placebo Interventions were diluted in milk feeds. If infants were not being fed, interventions were administered through an orogastric tube. |
|
| Outcomes |
Report 2009:The primary outcome was first
episode of late‐onset sepsis of bacterial or fungal
origin. Secondary outcomes were
gram‐positive/gram‐negative bacterial and fungal
sepsis, mortality prior
to discharge (overall
and sepsis attributable), incidence of urinary tract
infections, fungal colonization, progression from
fungal colonization to invasive fungal infection
(IFI), stage 2 or greater necrotizing enterocolitis,
threshold retinopathy of prematurity, severe (grade
3‐4) intraventricular
hemorrhage,
bronchopulmonary dysplasia,
alteration of liver function, and adverse effects or
intolerance. Report 2012: Primary outcome‐ fungal colonization and infection. Secondary outcomes were intensity of fungal colonization; rate of progression to infection in colonized infants; frequencies of single fungal species in all groups; and IFI‐related deaths. Report published in 2014: Primary outcomes: NEC ≥ stage II, death and/or ≥ stage II NEC before discharge Secondary outcomes: mortality attributable to NEC, mortality not associated with NEC before discharge |
|
| Notes | The study protocol and methods were the same for all the 3 reports (same RCT). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly allocated to 1 of 3 groups by computer‐generated allocation sequences |
| Allocation concealment (selection bias) | Low risk | The random allocation sequence was generated using a computer program which the pharmacy at each centre used to prepare drug doses. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study authors reported that clinical and research staff were unaware of study group, as interventions and placebo were diluted in milk. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9/485 in the intervention arm and 5/258 in the placebo arm had missing or incomplete data. Intention‐to‐treat analyses were performed. |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Unclear risk | Continuation of study from the first report and change in primary outcomes from the first and the last reports of the RCT |
| Completeness of follow‐up | Low risk | Assessed in the hospital before discharge |
| Blinding of outcome assessment | Unclear risk | Blinding of outcome assessors not explicit (for NEC stage II or III) |
Ochoa 2015.
| Study characteristics | ||
| Methods | randomized, placebo‐controlled, double‐blind study of 190 preterm infants < 2500 g in 5 neonatal Intermediate and intensive care units in Lima, Peru | |
| Participants | Birth weight between 500 and 2500 g; admitted to NICU in the first 72 hours of life | |
| Interventions | Oral bovine lactoferrin (200 mg/kg/d divided into 3
doses) for 4 weeks OR oral maltodextrin (200 mg/kg/d
in 3 divided doses) for 4 weeks Both dissolved in human milk or formula or 5% glucose solution |
|
| Outcomes | Primary outcome: number of confirmed episodes of
late‐onset sepsis in the first month of life Secondary outcomes: incidence of gram‐positive and gram‐negative bacterial sepsis, fungal sepsis, pneumonia, diarrhea, mortality in the first month of life |
|
| Notes | Trial ID: www.clinicaltrials.gov: NCT01264536 Peruvian study in 5 neonatal units in Lima, enrolled between January 31 and August 6, 2011 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block‐randomized, stratified by weight by a third party |
| Allocation concealment (selection bias) | Low risk | randomization performed before enrollment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinded trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and included in the analysis |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | Loss to follow‐up < 10% |
| Blinding of outcome assessment | Unclear risk | Not explicit |
Ochoa 2020.
| Study characteristics | ||
| Methods | Double‐blind randomized controlled trial in 3 units in Lima, Peru | |
| Participants | Infants weighing 500‐2000 g at birth enrolled in the first 72 hrs after birth | |
| Interventions | Bovine lactoferrin dissolved in mother's milk or formula at 200 mg/kg/day in 3 divided doses for 8 weeks | |
| Outcomes | Aim 1:Primary study outcome was a composite outcome of the first culture‐proven LOS or sepsis‐associated death (deaths associated with probable sepsis). Secondary outcomes were the composite outcome in very low birth weight infants (< 1500 g), pathogen‐specific LOS, necrotizing enterocolitis (Bell stage ≥ 2), retinopathy of prematurity requiring surgery, intraventricular hemorrhage (grade III‐IV), bronchopulmonary dysplasia (oxygen requirement for > 28 days), serious infections before discharge, hospitalization duration, re‐hospitalisation, overall mortality, infection‐related mortality, and frequency of adverse events or intolerance. Aim 2:Primary outcome was the mean age‐adjusted normalized Mullen composite score at 24 months. Secondary outcomes were neurodevelopmental delay (Mullen composite score of ≤ 70, Bayley‐III scores < 85), delayed adaptive skills (ABAS‐II) general adaptive composite score of < 70), neurodevelopmental impairment (Mullen composite score of ≤ 70, moderate‐to‐severe cerebral palsy, bilateral hearing impairment requiring amplification or bilateral blindness), and growth delay (height‐for‐age and weight‐for height Z‐scores of <− 2). All study outcomes were prespecified in the protocol. | |
| Notes | Only study to have assessed and reported developmental outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central randomization, stratified by birth weight |
| Allocation concealment (selection bias) | Low risk | Central randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Only the research nurse knew the intervention. Caregivers were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Short‐term outcomes were reported for all 414 infants enrolled. 25% of infants were not followed due to death or dropout for the neurodevelopmental assessment at 24 months. |
| Selective reporting (reporting bias) | Low risk | Reporting according to prespecified protocol |
| Other bias | Low risk | None other noted |
| Completeness of follow‐up | Low risk | Dropout rate of 9.2% (38/414) in survivors |
| Blinding of outcome assessment | Unclear risk | Not clear if outcome assessors were blinded to the intervention |
Sherman 2016.
| Study characteristics | ||
| Methods | Phase 1 and Phase 2 randomized clinical trial | |
| Participants | Preterm infants with birth weight of 750 to 1500 g in participating units in the United States, enrolled within 24 hours of birth | |
| Interventions | Infants were given enteral human recombinant lactoferrin (talactoferrin, TLF) or placebo from day 1 to 29 days of life at a dose of 300 mg/kg/d. | |
| Outcomes | Primary outcomes: reduction in hospital‐acquired
infection; bacteremia, meningitis, pneumonia,
urinary tract infection, necrotizing
enterocolitis Secondary outcomes: mortality, duration of hospitalization, time to regain birth weight, time to reach full enteral feeds |
|
| Notes | Trial ID: ClinicalTrials.gov Identifier:
NCT00854633 Trial was conducted in participating units in the United States, between July 1, 2009, and March 17, 2012. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned by a central computer system |
| Allocation concealment (selection bias) | Low risk | Centrally randomized |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blinded study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Low risk | None noted |
| Completeness of follow‐up | Low risk | All primary and secondary outcomes assessed during hospital stay |
| Blinding of outcome assessment | Unclear risk | Not explicit |
Tang 2017.
| Study characteristics | ||
| Methods | Single centre, randomized controlled trial | |
| Participants | GA < 37 weeks, preterm infants | |
| Interventions | 3 groups: 90 infants in the control group (placebo), 82 infants in the lactoferrin group, 85 infants lactoferrin + LGG probiotic | |
| Outcomes | Primary outcome was culture‐proven late‐onset sepsis. Secondary outcomes were infection‐related mortality and all‐cause mortality. | |
| Notes | Guangzhou Zengchun district, Maternal and Childcare Service Ccentre, Jan 2013‐ Dec 2015 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details available |
| Allocation concealment (selection bias) | Unclear risk | No details available |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | NK |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data reported for all infants |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Unclear risk | No details available |
| Completeness of follow‐up | Low risk | All infants were accounted for. |
| Blinding of outcome assessment | Unclear risk | Not explicit |
ABAS‐II: Adaptive behaviour assessment system, second edition BPD: bronchopulmonary dysplasia Bwt: Birth weight CDC: Centers for Disease Control and Prevention CFU: colony‐forming units CRP: C‐reactive protein CSF: cerebrospinal fluid GA: gestational age HIE: hypoxic‐ischaemic encephalopathy IFI: Invasive fungal infection LGG: Lactobacillus rhamnosus GG (GG derives from the first letter of last names of scientists who isolated the bacteria, Sherwood Gorbach and Barry Goldin) LOS:Late‐onset sepsis NEC:necrotizing enterocolitis NICU: neonatal intensive care unit NK: Natural Killer RCT: Randomized controlled trial ROP: retinopathy of prematurity TLF: talactoferrin TPN: total parenteral nutrition Treg: regulator T‐cells VLBW: Very low birth weight
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| King 2007 | We excluded this study, as participants were not neonates. Enrolled healthy, formula‐fed infants at 34 weeks' gestation or later and at 4 weeks of age or younger. Infants received formula supplemented with lactoferrin (850 mg/L) or commercial cow's milk‐based formula (102 mg/L) for 12 months. Investigators collected growth parameters and information on gastrointestinal, respiratory, and colic illnesses for the infants' first year. |
| Meyer 2016 | This was not a randomized study. It was a retrospective, observational study comparing the lactoferrin prophylaxis cohort (2004‐2011) with an historical cohort without lactoferrin prophylaxis (2001‐2004). The prophylaxis cohort received 100 mg of bovine lactoferrin and a probiotic. |
| Ochoa 2013 | We excluded this study, as participants were not neonates. This community‐based, randomized, double‐blind, placebo‐controlled trial compared supplementation with bovine lactoferrin versus placebo. Researchers randomly assigned 577 weaned children at 12 to 18 months and followed them for 6 months with daily home visits. The aim was prevention of diarrhea; outcomes assessed were number of diarrhea episodes, longitudinal prevalence of diarrhea, severity of diarrhea, and dehydration. |
Characteristics of studies awaiting classification [ordered by study ID]
ISRCTN71737811.
| Methods | Prospective, double‐blind, randomized, placebo‐controlled study |
| Participants | Preterm infants with gestational age 26 to 36 weeks |
| Interventions | Infants were randomly assigned to: 1. standard preterm formula; 2. standard preterm formula with probiotics (galacto‐oligosaccharides 28.5%, lactose 9.5%, galactose 0.5%, minerals 3.5%, fat 1.5%, water 3%); or 3. standard preterm formula with dairy lactoferrin 1 mg/100 mL. |
| Outcomes | Primary outcomes: composition of gut flora at 6 weeks
of full enteral feeds, incidence of infection,
oxidative stress, iron status Secondary outcomes: growth (weight, length, and head circumference), feeding intolerance, psychomotor development at 1 year of age |
| Notes | Unpublished study completed in 2009. Study author
contacted for data Trial ID: ISRCTN71737811 |
NCT01172236.
| Methods | Controlled phase 4 trial of lactoferrin supplementation in preterm infants |
| Participants | Newborn infants with birth weight ≤ 1500 g and/or
gestational age ≤ 32 weeks Exclusion criteria: fetal‐onset disorders and/or recognizable at birth, milk intolerance, family history of allergy, use of infant formula supplemented with lactoferrin |
| Interventions | Intervention group (n = 650) received a daily dose of 100 mg of lactoferrin + standard therapy; control group (n = 650) received only standard therapy. |
| Outcomes | Primary outcome: evaluation of the antioxidant effect
of lactoferrin and its ability to reduce free
radical‐related disease in the newborn through
assessment of neurodevelopmental follow‐up Secondary outcome: identification of a panel of markers for assessing oxidative stress and for correlating with the lactoferrin antioxidant effect |
| Notes | We have requested details of the study from the
principal investigator. Trial ID: ClinicalTrials.gov identifier: NCT01172236 |
NCT02959229.
| Methods | Prospective randomized controlled study |
| Participants | Preterm infants (< 37 weeks' gestation) |
| Interventions | Enteral lactoferrin supplementation at 100 mg/d starting on day 1 or day 3 (early vs late) |
| Outcomes | Neonatal sepsis by Tollner score, haematological scoring system, and positive blood culture |
| Notes | Study completed enrollment of 180 preterm neonates admitted to NICU at Ain Shams University Hospitals, from August 2014 to December 2015; clinicaltrials.gov NCT02959229. |
NICU: neonatal intensive care unit
Characteristics of ongoing studies [ordered by study ID]
NCT01821989.
| Study name | Oral lactoferrin supplementation for prevention of sepsis in preterm neonates |
| Methods | Double‐blind, randomized, controlled trial |
| Participants | Preterm neonates with birth weight between 500 g and
2500 g and ≤ 36 weeks' gestation, born in or
referred to the neonatal intensive care unit of one
of the participating hospitals in the first 48 hours
of life Exclusion criteria: neonates with underlying gastrointestinal problems that prevent oral intake, neonates with predisposing conditions that profoundly affect growth and development (chromosomal abnormalities, structural brain anomalies, severe congenital abnormalities), neonates with a family background of cow's milk allergy, neonates who will not have the chance to complete the study time (who will be referred to another hospital), neonates whose parents decline to participate, neonates with early‐onset sepsis |
| Interventions | Preterm neonates will be randomly assigned to 1 of 3 groups: low‐dose lactoferrin (100 mg/d), high‐dose lactoferrin (150 mg/kg/twice daily), or placebo (distilled water). |
| Outcomes | Primary outcome: blood culture positivity Secondary outcome: complete blood count with differential leukocyte count and C‐reactive protein quantitative assay |
| Starting date | June 2013 and plans to enroll 180 neonates |
| Contact information | Mostafa AM Elmokadem: drmooselmokadem@hotmail.com; Egypt: Ain Shams University |
| Notes | Trial ID: ClinicalTrials.gov identifier: NCT01821989 |
BLF: bovine lactoferrin BPD: bronchopulmonary dysplasia NEC: necrotizing enterocolitis ROP: retinopathy of prematurity
Differences between protocol and review
Differences between the protocol and the review include post hoc decisions regarding
1. adding the certainty of evidence using GRADE (Grades of Recommendation, Assessment, Development and Evaluation) methods.
2. including trials with probiotics as a co‐intervention post in the comparison of enteral lactoferrin versus placebo (comparison 1).
3. including the outcomes of threshold retinopathy of prematurity and urinary tract infection as well as subgroup analyses of confirmed bacterial sepsis and fungal sepsis.
Contributions of authors
Mohan Pammi wrote the text of the protocol and the review, formulated the search strategy, performed the literature search, wrote the review and is the corresponding author.
Gautham Suresh assisted in checking the accuracy of the data, assessing risk of bias of included studies, and assisted in writing the final version of this review.
Sources of support
Internal sources
None, Other
External sources
-
National Institute for Health Research, UK
UK editorial support for Cochrane Neonatal has been funded by funds from a UK National Institute of Health Research Grant (NIHR) Cochrane Programme Grant (13/89/12). The views expressed in this publication are those of the review authors and are not necessarily those of the NHS, the NIHR, or the UK Department of Health
-
Vermont Oxford Network, USA
Vermont Oxford Network is a not‐for‐profit voluntary collaboration of Neonatal Intensive Care Units dedicated to improving newborn care throughout the world. Vermont Oxford Network supports administrative needs of Cochrane Neonatal.
Declarations of interest
Agennix, Inc. donated human recombinant lactoferrin for Dr Pammi's laboratory research from 2006 through 2009.
Edited (no change to conclusions)
References
References to studies included in this review
Akin 2014 {published data only}
- Akin IM, Atasay B, Dogu F, Okulu E, Arsan S, Karatas HD, et al. Oral lactoferrin to prevent nosocomial sepsis and necrotizing enterocolitis of premature neonates and effect on T-regulatory cells. American Journal of Perinatology 2014;31(12):1111-20. [DOI: 10.1055/s-0034-1371704] [PMID: ] [DOI] [PubMed] [Google Scholar]
Barrington 2016 {published data only}
- Barrington KJ, Assaad MA, Janvier A. The Lacuna Trial: a double-blind randomized controlled pilot trial of lactoferrin supplementation in the very preterm infant. Journal of Perinatology 2016;36(8):666-9. [DOI: 10.1038/jp.2016.24] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dai 2015 {published data only}
- *.Dai JZ, Xie C. The effect of lactoferrin supplementation combining Lactobacillus rhamnosus for prevention of late onset sepsis in premature neonates. China Practical Medicine 2015;10:98-100. [Google Scholar]
ELFIN 2018 {unpublished data only}88261002
- ISRCTN88261002. Enteral lactoferrin supplementation for very preterm infants: a randomised controlled trial. isrctn.com/ISRCTN88261002 (first received 5 June 2013). [DOI: 10.1186/ISRCTN88261002] [DOI]
Kaur 2015 {published data only}
- Kaur G, Gathwala G. Efficacy of bovine lactoferrin supplementation in preventing late-onset sepsis in low birth weight neonates: a randomized placebo-controlled clinical trial. Journal of Tropical Pediatrics 2015;61(5):370-6. [DOI: 10.1093/tropej/fmv044] [PMID: ] [DOI] [PubMed] [Google Scholar]
LIFT 2020 {published data only}
- Tarnow-Mordi WO, Abdel-Latif ME, Martin A, Pammi M, Robledo K, Manzoni P, et al, LIFT collaborators. The Lactoferrin Infant Feeding Trial (LIFT): a pragmatic, randomised, multicentre study in very low birth weight infants. Lancet. Child and Adolescent Health. 2020;4(6):444-54 (with online Supplementary Appendix pp S1-44). [DOI: 10.1016/S2352-4642(20)30093-6] [DOI] [PubMed] [Google Scholar]
Liu 2016 {published data only}
- *.Liu YH, Guan HS, Liang GJ, Li YZ, Zuo A. The effect of lactoferrin on low birth weight neonates during hospitalization. Maternal and Child Health Care of China 2016;31(21):4464-5. [Google Scholar]
Manzoni 2014 {published data only}
- *.Manzoni P, Meyer M, Stolfi I, Rinaldi M, Cattani S, Pugni L, et al. Bovine lactoferrin supplementation for prevention of necrotizing enterocolitis in very-low-birth-weight neonates: a randomized clinical trial. Early Human Development 2014;90 Suppl 1:S60-5. [DOI: 10.1016/S0378-3782(14)70020-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Manzoni P, Rinaldi M, Cattani S, Pugni L, Romeo MG, Messner H, et al. Bovine lactoferrin supplementation for prevention of late-onset sepsis in very low-birth-weight neonates: a randomized trial. JAMA 2009;302(13):1421-8. [DOI: 10.1001/jama.2009.1403] [PMID: DOI: 10.1001/jama.2009.1403; PubMed: 19809023]] [DOI] [PubMed] [Google Scholar]
- Manzoni P, Stolfi I, Messner H, Cattani S, Laforgia N, Romeo MG, et al. Bovine lactoferrin prevents invasive fungal infections in very low birth weight infants: a randomized controlled trial. Pediatrics 2012;129(1):116-23. [PMID: 10.1542/peds.2011-0279; PubMed: 22184648]] [DOI] [PubMed] [Google Scholar]
Ochoa 2015 {published and unpublished data}
- Ochoa TJ, Zegarra J, Cam L, Llanos R, Pezo A, Cruz K, et al. Randomized controlled trial of lactoferrin for prevention of sepsis in Peruvian neonates less than 2500 g. Pediatric Infectious Disease Journal 2015;34(6):571-6. [DOI: 10.1097/INF.0000000000000593] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ochoa 2020 {unpublished data only}
- *.Ochoa T, Zegarra J, Bellomo S, Carcamo C, Cam L, Castaneda A, et al, Neolacto Research Group. Randomized controlled trial of bovine lactoferrin for prevention of sepsis and neurodevelopmental impairment in infants weighing less than 2000 grams. Journal of Pediatrics (in press) 2020. [DOI] [PMC free article] [PubMed]
Sherman 2016 {published data only}
- Sherman MP, Adamkin DH, Niklas V, Radmacher P, Sherman J, Wertheimer F, et al. Randomized controlled trial of talactoferrin oral solution in preterm infants. Journal of Pediatrics 2016;175:68-73. [DOI: 10.1016/j.jpeds.2016.04.084] [PMID: 27260839] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tang 2017 {published data only}
- *.Tang JP, Sun HQ, Zheng YH, Lu GH. Randomized control trial of lactoferrin for the prevention of late onset sepsis in premature neonates. Maternal and Child Health Care of China 2017;32(6):1223-5. [Google Scholar]
References to studies excluded from this review
King 2007 {published data only}
- King JC Jr, Cummings GE, Guo N, Trivedi L, Readmond BX, Keane V, et al. A double-blind, placebo-controlled, pilot study of bovine lactoferrin supplementation in bottle-fed infants. Journal of Pediatric Gastroenterology and Nutrition 2007;44(2):245-51. [DOI: 10.1097/01.mpg.0000243435.54958.68] [PMID: ] [DOI] [PubMed] [Google Scholar]
Meyer 2016 {published data only}
- Meyer MP, Alexander T. Reduction in necrotizing enterocolitis and improved outcomes in preterm infants following routine supplementation with lactobacillus GG in combination with bovine lactoferrin. Journal of Neonatal-Perinatal Medicine 2016;10(3):249-55. [DOI: 10.3233/NPM-16130] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ochoa 2013 {published data only}
- Ochoa T, Chea-Woo E, Baiocchi N, Pecho I, Campos M, Prada A, et al. Randomized double-blind controlled trial of bovine lactoferrin for prevention of diarrhea in children. Journal of Pediatrics 2013;162(2):349–56. [DOI: 10.1016/j.jpeds.2012.07.043] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
ISRCTN71737811 {published data only}
- ISRCTN71737811. Effect of prebiotic or lactoferrin supplementation in formula on the gut flora of preterm infants. isrctn.com/ISRCTN71737811 (first received 5 September 2008).
NCT01172236 {published data only}
- NCT01172236. Supplementation with lactoferrin in preterm newborns (lactoprenew). clinicaltrials.gov/show/NCT01172236 (first received 29 July 2010).
NCT02959229 {published data only}
- NCT02959229. Early versus late lactoferrin in prevention of neonatal sepsis [Systematic randomized, single blinded, placebo-controlled trial of early versus late lactoferrin in prevention of neonatal sepsis]. clinicaltrials.gov/show/NCT02959229 (first received 27 October 2016).
References to ongoing studies
NCT01821989 {published data only}
- NCT01821989. Oral lactoferrin supplementation for prevention of sepsis in preterm neonate. clinicaltrials.gov/show/NCT01821989 (first received 27 March 2013).
Additional references
Adams‐Chapman 2006
- Adams-Chapman I, Stoll BJ. Neonatal infection and long-term neurodevelopmental outcome in the preterm infant. Current Opinion in Infectious Diseases 2006;19(3):290-7. [DOI: 10.1097/01.qco.0000224825.57976.87] [PMID: ] [DOI] [PubMed] [Google Scholar]
Alfaleh 2014
- AlFaleh K, Anabrees J. Probiotics for prevention of necrotizing enterocolitis in preterm infants. Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No: CD005496. [DOI: 10.1002/14651858.CD005496.pub4] [DOI] [PubMed] [Google Scholar]
Barboza 2012
- Barboza M, Pinzon J, Wickramasinghe S, Froehlich J, Moeller I, Smilowitz J, et al. Glycosylation of human milk lactoferrin exhibits dynamic changes during early lactation enhancing its role in pathogenic bacteria-host interactions. Molecular Cell Proteomics 2012;11(6):M111.015248. [DOI: 10.1074/mcp.M111.015248] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bell 1978
- Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Annals of Surgery 1978;187(1):1-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bellamy 1992
- Bellamy W, Takase M, Wakabayashi H, Kawase K, Tomita M. Antibacterial spectrum of lactoferricin B, a potent bactericidal peptide derived from the N-terminal region of bovine lactoferrin. Journal of Applied Bacteriology 1992;73(6):472-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Blackwell 1997
- Blackwell TS, Christman JW. The role of nuclear factor-kappa B in cytokine gene regulation. American Journal of Respiratory Cell and Molecular Biology 1997;17(1):3-9. [DOI: 10.1165/ajrcmb.17.1.f132] [PMID: ] [DOI] [PubMed] [Google Scholar]
Buccigrossi 2007
- Buccigrossi V, De Marco G, Bruzzese E, Ombrato L, Bracale I, Polito G, et al. Lactoferrin induces concentration-dependent functional modulation of intestinal proliferation and differentiation. Pediatric Research 2007;61(4):410-4. [DOI: 10.1203/pdr.0b013e3180332c8d] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chen 2017
- Chen PW, Liu ZS, Kuo TC, Hsieh MC, Li ZW. Prebiotic effects of bovine lactoferrin on specific probiotic bacteria. Biometals 2017;30(2):237-48. [DOI: 10.1007/s10534-017-9999-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dermyshi 2017
- Dermyshi E, Wang Y, Yan C, Hong W, Qiu G, Gong X, et al. The "golden age" of probiotics: a systematic review and meta-analysis of randomized and observational studies in preterm infants. Neonatology 2017;112(1):9-23. [DOI: 10.1159/000454668] [PMID: ] [DOI] [PubMed] [Google Scholar]
Edde 2001
- Edde L, Hipolito RB, Hwang FF, Headon DR, Shalwitz RA, Sherman MP. Lactoferrin protects neonatal rats from gut-related systemic infection. American Journal of Physiology. Gastrointestinal and Liver Physiology 2001;281(5):G1140-50. [DOI: 10.1152/ajpgi.2001.281.5.G1140] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gifford 2005
- Gifford JL, Hunter HN, Vogel HJ. Lactoferricin: a lactoferrin-derived peptide with antimicrobial, antiviral, antitumor and immunological properties. Cellular and Molecular Life Sciences 2005;62(22):2588-98. [DOI: 10.1007/s00018-005-5373-z] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 9 March 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [DOI: 10.1136/bmj.39489.470347.AD] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2006
- Hayes TG, Falchook GF, Varadhachary GR, Smith DP, Davis LD, Dhingra HM, et al. Phase I trial of oral talactoferrin alfa in refractory solid tumors. Investigational New Drugs 2006;24(3):233-40. [DOI: 10.1007/s10637-005-3690-6] [PMID: ] [DOI] [PubMed] [Google Scholar]
He 2018
- He Y, Cao L, Yu J. Prophylactic lactoferrin for preventing late-onset sepsis and necrotizing enterocolitis in preterm infants. Medicine 2018;97(35):e11976. [DOI: 10.1097/MD.0000000000011976] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Iwasa 2002
- Iwasa M, Kaito M, Ikoma J, Takeo M, Imoto I, Yamauchi K, et al. Lactoferrin inhibits hepatitis C virus viremia in chronic hepatitis C patients with high viral loads and HCV genotype 1b. American Journal of Gastroenterology 2002;97(3):766-7. [DOI: 10.1111/j.1572-0241.2002.05573.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kuipers 1999
- Kuipers ME, De Vries HG, Eikelboom MC, Meijer DK, Swart PJ. Synergistic fungistatic effects of lactoferrin in combination with antifungal drugs against clinical Candida isolates. Antimicrobial Agents and Chemotherapy 1999;43(11):2635-41. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawn 2006
- Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. International Journal of Epidemiology 2006;35(3):706-18. [DOI: 10.1093/ije/dyl043] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lee 1998
- Lee WJ, Farmer JL, Hilty M, Kim YB. The protective effects of lactoferrin feeding against endotoxin lethal shock in germfree piglets. Infect Immun 1998;66:1421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Legrand 2016
- Legrand D. Overview of lactoferrin as a natural immune modulator. Journal of Pediatrics 2016;173 Suppl:S10-5. [DOI: 10.1016/j.jpeds.2016.02.071] [PMID: ] [DOI] [PubMed] [Google Scholar]
Leitch 1999
- Leitch EC, Willcox MD. Lactoferrin increases the susceptibility of S. epidermidis biofilms to lysozyme and vancomycin. Current Eye Research 1999;19(1):12-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Levy 1998
- Levy SB. Antimicrobial resistance: bacteria on the defence. Resistance stems from misguided efforts to try to sterilize our environment. BMJ 1998;317(7159):612-3. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lin 2006
- Lin PW, Stoll BJ. Necrotizing enterocolitis. Lancet 2006;368(9543):1271-83. [DOI: 10.1016/S0140-6736(06)69525-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lingappan 2013
- Lingappan K, Arunachalam A, Pammi M. Lactoferrin and the newborn: current perspectives. Expert Reviews of Anti-Infective Therapy 2013;11(7):695-707. [DOI: 10.1586/14787210.2013.811927] [PMID: ] [DOI] [PubMed] [Google Scholar]
Manzoni 2016
- Manzoni P. Clinical benefits of lactoferrin for infants and children. Journal of Pediatrics 2016;173 Suppl:S43-52. [DOI: 10.1016/j.jpeds.2016.02.075] [PMID: ] [DOI] [PubMed] [Google Scholar]
Neish 2004
- Neish AS. Molecular aspects of intestinal epithelial cell-bacterial interactions that determine the development of intestinal inflammation. Inflammatory Bowel Diseases 2004;10(2):159-68. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nibbering 2001
- Nibbering PH, Ravensbergen E, Welling MM, Van Berkel LA, Van Berkel PH, Pauwels EK, et al. Human lactoferrin and peptides derived from its N terminus are highly effective against infections with antibiotic-resistant bacteria. Infection and Immunity 2001;69(3):1469-76. [DOI: 10.1128/IAI.69.3.1469-1476.2001] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ochoa 2017
- Ochoa TJ, Sizonenko SV. Lactoferrin and prematurity: a promising milk protein? Biochemistry and Cell Biology 2017;95(1):22-30. [DOI: 10.1139/bcb-2016-0066] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pierce 1991
- Pierce A, Colavizza D, Benaissa M, Maes P, Tartar A, Montreuil J, et al. Molecular cloning and sequence analysis of bovine lactotransferrin. European Journal of Biochemistry 1991;196(1):177-84. [PMID: ] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s), GRADE Working Group. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). gdt.gradepro.org/app/handbook/handbook.html (accessed prior to 16 March 2020).
Speer 1999
- Speer CP. Inflammatory mechanisms in neonatal chronic lung disease. European Journal of Pediatrics 1999;158 Suppl 1:S18-22. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stoll 2002
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002;110(2 Pt 1):285-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stoll 2004a
- Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292(19):2357-65. [DOI: 10.1001/jama.292.19.2357] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stoll 2004b
- Stoll BJ. Infections of the neonatal infant. In: Behrman RE, Kliegman R, Jenson HB, editors(s). Nelson's Textbook of Pediatrics. 17th edition. Philadelphia (PA): Saunders, 2004:623-40. [Google Scholar]
Stoll 2005
- Stoll BJ, Hansen NI, Higgins RD, Fanaroff AA, Duara S, Goldberg R, et al. Very low birth weight preterm infants with early onset neonatal sepsis: the predominance of gram-negative infections continues in the National Institute of Child Health and Human Development Neonatal Research Network, 2002-2003. Pediatric Infectious Disease Journal 2005;24(7):635-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tanaka 1999
- Tanaka K, Ikeda M, Nozaki A, Kato N, Tsuda H, Saito S, et al. Lactoferrin inhibits hepatitis C virus viremia in patients with chronic hepatitis C: a pilot study. Japanese Journal of Cancer Research 1999;90(4):367-71. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tian 2010
- Tian H, Maddox IS, Ferguson LR, Shu Q. Influence of bovine lactoferrin on selected probiotic bacteria and intestinal pathogens. Biometals 2010;23(3):593-6. [DOI: 10.1007/s10534-010-9318-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Togawa 2002
- Togawa J, Nagase H, Tanaka K, Inamori M, Umezawa T, Nakajima A, et al. Lactoferrin reduces colitis in rats via modulation of the immune system and correction of cytokine imbalance. American Journal of Physiology. Gastrointestinal and Liver Physiology 2002;283(1):G187-95. [DOI: 10.1152/ajpgi.00331.2001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tomita 2002
- Tomita M, Wakabayashi H, Yamauchi K, Teraguchi S, Hayasawa H. Bovine lactoferrin and lactoferricin derived from milk: production and applications. Biochemistry and Cell Biology 2002;80(1):109-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Trumpler 1989
- Trumpler U, Straub PW, Rosenmund A. Antibacterial prophylaxis with lactoferrin in neutropenic patients. European Journal of Clinical Microbiology and Infectious Diseases 1989;8(4):310-3. [PMID: ] [DOI] [PubMed] [Google Scholar]
Turin 2014
- Turin CG, Zea-Vera A, Pezo A, Cruz K, Zegarra J, Bellomo S, et al. Lactoferrin for prevention of neonatal sepsis. Biometals 2014;27(5):1007-16. [DOI: 10.1007/s10534-014-9754-3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Valenti 2005
- Valenti P, Antonini G. Lactoferrin: an important host defence against microbial and viral attack. Cellular and Molecular Life Sciences 2005;62(22):2576-87. [DOI: 10.1007/s00018-005-5372-0] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venkatesh 2007
- Venkatesh M, Pham D, Kong L, Weisman L. Prophylaxis with lactoferrin, a novel antimicrobial agent, enhances survival in a neonatal rat model of co-infection. Advances in Therapy 2007;24(5):941-54. [PMID: ] [DOI] [PubMed] [Google Scholar]
Volpe 1995
- Volpe JJ. Neurology of the Newborn. 3rd edition. Philadelphia: WB Saunders, 1995. [Google Scholar]
Zagulski 1989
- Zagulski T, Lipinski P, Zagulska A, Broniek S, Jarzabek Z. Lactoferrin can protect mice against a lethal dose of Escherichia coli in experimental infection in vivo. British Journal of Experimental Pathology 1989;70(6):697-704. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Zaidi 2005
- Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet 2005;365(9465):1175-88. [DOI: 10.1016/S0140-6736(05)71881-X] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Pammi 2010
- Pammi M, Abrams SA. Oral lactoferrin for the prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database of Systematic Reviews 2010, Issue 5. Art. No: CD007137. [DOI: 10.1002/14651858.CD007137.pub2] [DOI] [PubMed] [Google Scholar]
Pammi 2011
- Pammi M, Abrams SA. Oral lactoferrin for the prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD007137. [DOI: 10.1002/14651858.CD007137.pub3] [DOI] [PubMed] [Google Scholar]
Pammi 2015
- Pammi M, Abrams SA. Oral lactoferrin for the prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No: CD007137. [DOI: 10.1002/14651858.CD007137.pub4] [DOI] [PubMed] [Google Scholar]


