Highlights
-
•
Mammalian body temperature presents a constraint on virus binding.
-
•
Negligible changes in heat capacity promote virus transmission at low temperatures in the case of arboviruses.
-
•
Observed virus volume/host temperature relationship explained through entropy of virus binding.
-
•
Non-specific attachment of virus overcomes entropy issues in large viruses such as HIV binding at human body temperature
-
•
Antivirals such as zinc oxide should focus on the entropy of virus binding as a novel approach.
Keywords: Temperature, Virus size, Entropy, Antivirals, Heat capacity
Abbreviations: AIV, avian influenza virus; BBF, brush border fragments from midgut; BTV, bluetongue virus; Cp, heat capacity at constant pressure; ΔCp, change in heat capacity; Cr, host cell receptor; CD4, host cell receptor for HIV; Ctotal, number of host cells which can bind virus in a given volume of host fluid (midgut or blood); C.VT, number of host cells with bound virus at temperature T; DENV, Dengue virus; EA, activation energy; EBOV, Zaire ebolavirus; EM, electron microscopy; Env, HIV gp120 trimer envelope protein which binds to a single CD4 molecule; FcT, fraction of arthropod midgut cells with bound virus at temperature T; ΔGa_virus_T, change in Gibbs free energy on association of virus and host cell at temperature T; GP, viral (glyco)protein on virus surface that binds to Cr; HA, haemagglutinin; ΔHa_receptor_T, change in enthalpy for binding of virus GP to host Cr receptor at a temperature T; HIV, human immunodeficiency virus; HSV-2, herpes simplex virus type 2; ΔHa_virus_T, change in enthalpy for binding of virus to host cell at temperature T; Ka_virus_T, association constant for binding of virus to host cells at temperature T; Kd_receptor_T, dissociation constant for GP from Cr at temperature T; Kd_virus, dissociation constant for virus from host cell; M, molar (moles dm-3); n, number of GP/Cr contacts made on virus binding to cell; ptransmissionT, probability of successful infection of the arthropod salivary glands after oral exposure at temperature T; pcompleteT, probability given a virion has bound to the surface of a midgut cell that that midgut cell becomes infected and that its progeny viruses go on to infect the salivary gland so completing the arthropod infection process within the life time of the arthropod at temperature T; R, ideal gas constant; ΔSa_receptor_T, change in entropy for binding of virus GP to host Cr receptor; ΔSa_virus_T, change in entropy for binding of virus to host cell at temperature T; ΔSa_immob, change in entropy on immobilization of whole virus to cell surface; ΔSa_non_specific, change in entropy on immobilization of virus to cell surface through non-specific binding; ΔSa_specific, change in entropy on immobilization of virus to cell surface through specific GP/Cr-driven binding; SA, sialic acid; SIV, simian immunodeficiency virus; Vfree, virus not bound to cells; Vtotal, virus challenge dose in volume of host fluid; WEEV, Western equine encephalitis virus; WNV, West Nile virus; ZnOT, zinc oxide tetrapod
Abstract
Virus binding to host cells involves specific interactions between viral (glyco)proteins (GP) and host cell surface receptors (Cr) (protein or sialic acid (SA)). The magnitude of the enthalpy of association changes with temperature according to the change in heat capacity (ΔCp) on GP/Cr binding, being little affected for avian influenza virus (AIV) haemagglutinin (HA) binding to SA (ΔCp = 0 kJ/mol/K) but greatly affected for HIV gp120 binding to CD4 receptor (ΔCp = −5.0 kJ/mol/K). A thermodynamic model developed here predicts that values of ΔCp from 0 to ~−2.0 kJ/mol/K have relatively little impact on the temperature sensitivity of the number of mosquito midgut cells with bound arbovirus, while intermediate values of ΔCp of ~−3.0 kJ/mol/K give a peak binding at a temperature of ~20 °C as observed experimentally for Western equine encephalitis virus. More negative values of ΔCp greatly decrease arbovirus binding at temperatures below ~20 °C. Thus to promote transmission at low temperatures, arboviruses may benefit from ΔCp ~ 0 kJ/mol/K as for HA/SA and it is interesting that bluetongue virus binds to SA in midge midguts. Large negative values of ΔCp as for HIV gp120:CD4 diminish binding at 37 °C. Of greater importance, however, is the decrease in entropy of the whole virus (ΔSa_immob) on its immobilisation on the host cell surface. ΔSa_immob presents a repulsive force which the enthalpy-driven GP/Cr interactions weakened at higher temperatures struggle to overcome. ΔSa_immob is more negative (less favourable) for larger diameter viruses which therefore show diminished binding at higher temperatures than smaller viruses. It is proposed that small size phenotype through a less negative ΔSa_immob is selected for viruses infecting warmer hosts thus explaining the observation that virion volume decreases with increasing host temperature from 0 °C to 40 °C in the case of dsDNA viruses. Compared to arboviruses which also infect warm-blooded vertebrates, HIV is large at 134 nm diameter and thus would have a large negative ΔSa_immob which would diminish its binding at human body temperature. It is proposed that prior non-specific binding of HIV through attachment factors takes much of the entropy loss for ΔSa_immob so enhancing subsequent specific gp120:CD4 binding at 37 °C. This is consistent with the observation that HIV attachment factors are not essential but augment infection. Antiviral therapies should focus on increasing virion size, for example through binding of zinc oxide nanoparticles to herpes simplex virus, hence making ΔSa_immob more negative, and thus reducing binding affinity at 37 °C.
1. Introduction
Some viruses infect hosts over a range of temperatures depending on the host species. Most notable are the arboviruses which may infect the arthropod vector over a range of ambient temperatures from ~15 °C to >30 °C (Mullens et al., 2004), and then infect a vertebrate host at temperatures from 37 °C up to 44 °C in the case of West Nile virus (WNV) in infected American crows (Corvus brachyrhynchos) (Kinney et al., 2006). Birds generally have higher body temperatures than mammals (Brault 2009) and the avian influenza virus (AIV) when jumping from birds to humans has to adapt to a temperature drop of 8 °C since the temperature in the human upper respiratory tract is ~33 °C compared to ~41 °C in the avian intestinal tract which is the site of replication of avian viruses (De Graaf and Fouchier, 2014). Bats have higher core body temperatures than primates (up to 42.1 °C for Phyllostomus hastatus which is an omnivorous bat from South America) when flying (O'Shea et al., 2014). The core body temperature during flight of the insectivorous free-tailed bat (Mops condylurus) which may have been the origin of the 2013/15 severe Zaire ebolavirus (EBOV) outbreak in West Africa (Saez et al., 2015) is 40.5 °C ± 1 °C (O'Shea et al., 2014). Thus EBOV which infects a range of vertebrate species from bats to primates and deer may have to infect mammalian hosts over a range of temperatures. Similarly Nipah virus on jumping from fruit bats to pigs and humans (Daszak et al., 2013) may experience a small fall in temperature. Furthermore, cross-species transmission of viruses to bats (and other mammals) from invertebrates may occur with more regularity than has been appreciated (Bennett et al., 2018; Leendertz 2016), and Bennett et al. (2018) have suggested that arthropods may host many “bat-associated” viruses that have defied detection in bats themselves (e.g. EBOV). Depending on the ambient temperature, viruses in arthropods would experience a 9 °C to 15 °C temperature increase on being ingested by a bat at 41 °C (Gale 2017) and this could affect the binding affinity of the virus to its host cell depending on the thermodynamics of virus binding as is discussed here. In contrast other viruses only infect related host species, and in effect are maintained at similar temperatures. For example, simian immunodeficiency viruses (SIV) infect 36 different nonhuman primate species in sub-Saharan Africa and SIVs from chimpanzees (Pan troglodytes) have crossed species barriers on multiple occasions generating human immunodeficiency virus (HIV) types 1 and 2 (Sharp et al., 2005). Thus the main source of temperature variation experienced by SIV and HIV would be the effect of the circadian rhythm and the slight rise in temperature due to infection of the host which gives a range of 36 °C to 38 °C in the case of Rhesus monkeys (Huitron-Resendiz et al., 2007).
Viruses bind to host cells through interactions between a virus surface (glyco)protein (GP) and a host cell receptor (Cr). The Cr molecule on the cell surface may be a protein as in the case of HIV (Myszka et al., 2000), EBOV (Yuan et al., 2015), Hendra virus (Xu et al., 2012) and MERS-CoV (Lu et al., 2013) or alternatively is a sialic acid (SA) on a glycan as in the case of AIV (De Graaf and Fouchier, 2014; Fei et al., 2015) and arboviruses such as bluetongue virus (BTV) (Zhang et al., 2010). The thermodynamics of virus binding in terms of the changes in enthalpy (ΔHa_receptor_T) and entropy (ΔSa_receptor_T) on the specific interaction of the GP with the Cr receptor at temperature T during binding of virus to the host cell surface has been set out previously (Gale 2018, 2019). The interactions between the HIV GP and its CD4 cellular receptor (Myszka et al., 2000; Dey et al., 2007) and between the AIV haemagglutinin (HA) and its α2,3-SA or α2,6-SA receptors (Fei et al., 2015) are enthalpy driven, i.e. large negative values of ΔHa_receptor_T overcome unfavourable values of ΔSa_receptor_T. Also the binding of vesicular stomatitis virus to phospholipid bilayers is enthalpy driven (Carneio et al. 2002) with very large negative values of ΔHa_receptor_T.
Temperature may impose constraints on viruses’ jumping the species barrier through its effect on the binding affinity of GP to Cr. There may also be constraints on the activities of viral replication proteins such as the AIV polymerase which showed a significantly higher activity at 33 °C than 37 °C (Ngai et al., 2013). Only virus binding is considered here. Thus according to the Van't Hoff Isochore, the binding affinity for a virus to its host cell at temperature T as represented by the association constant Ka_virus_T would be greatly diminished for enthalpy-driven GP/Cr interactions at higher temperatures compared to lower temperatures depending on the magnitude of ΔHa_receptor_T (Gale 2019). Indeed, assuming ΔHa_receptor_T is constant over the temperature range, the more negative ΔHa_receptor_T is in magnitude, the weaker the binding at higher temperatures. This presents a paradox if the Ka_virus_T falls to less than ~1014 M− 1 in that higher temperatures would greatly diminish infectivity (Gale 2019).
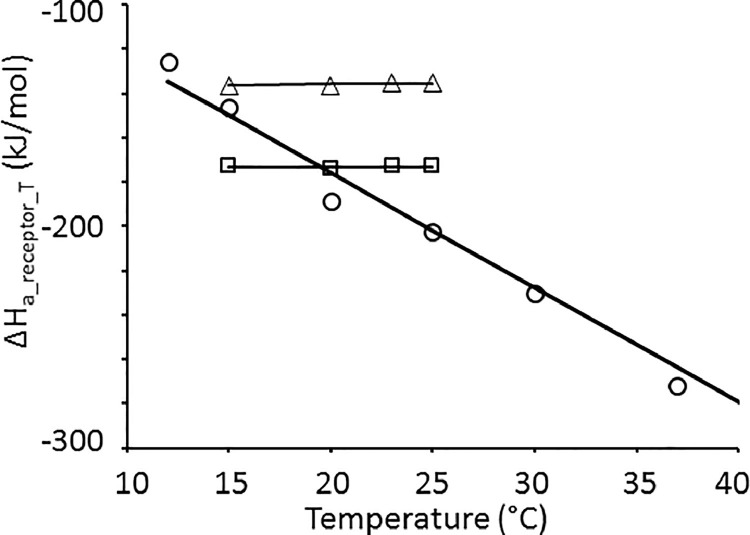
While the values of ΔHa_receptor_T and ΔSa_receptor_T may be constant over the biological temperature range for some GP/Cr systems, e.g. AIV haemagglutinin (HA) binding to sialic acid (SA) residues (Fei et al., 2015) they may change considerably in magnitude over the biologically relevant temperature range particularly for protein:protein systems as in the case of HIV gp120 binding to CD4 (Myszka et al., 2000) (Fig. 1 ). The effect of this on Ka_virus_T is considered in this work. The change in ΔHa_receptor_T with temperature is defined by the difference in heat capacities (Cp) of the GP/Cr “product” complex and the free GP/free host Cr “reactants” and is represented by ΔCp which is the slope of the lines in Fig. 1 and typically ranges from ~0 kJ/mol/K to −5.0 kJ/mol/K depending on the system.
Fig. 1.
Variation in ΔHa_receptor_T as a function of temperature as reported for HIV gp120 monomer binding to CD4 (○) (Myszka et al., 2000) and AIV HA monomer binding to soluble α2–6 sialyllactose (Δ) and α2–3 sialyllactose (□) (Fei et al., 2015). The slopes of the lines represent the ΔCp values which are summarised in Table 3.
The previous thermodynamic treatment of virus binding (Gale 2019) identified the entropy change (ΔSa_immob) on immobilisation of the whole virus particle on the host cell surface as a key parameter for which there are currently no data. ΔSa_immob would be expected to be large and negative in magnitude due to the decrease in the absolute entropy on immobilisation of a large molecular entity such as a virion. A recent analysis has shown that virion volume (and genome length) for dsDNA viruses decreases by about 55-fold as the temperature of occurrence (i.e. host) increases from 0 to 40 °C (Nifong and Gillooly 2016). The temperature of occurrence in these dsDNA viruses ranges from near zero for those inhabiting polar environments to over 40 °C for those inhabiting endothermic vertebrates. Nifong and Gillooly (2016) suggest that this could reflect smaller viruses being able to replicate more quickly (due to more compact genomes) perhaps together with energetic constraints imposed by their hosts. However from the thermodynamic perspective, the decrease in volume and hence mass and radius of the virus will make ΔSa_immob less negative for a smaller virus than for a larger virus. It is shown here how a less negative ΔSa_immob increases binding of the virus at the relatively high mammalian body temperatures and it is proposed that thermodynamic binding constraints may give smaller viruses a selective advantage for infecting hosts at the higher body temperatures of mammals and birds. In this respect, the large size of the HIV virion may present a constraint to binding at human body temperatures compared to the much smaller arboviruses for example.
In the case of HIV, the GP component of the GP/Cr interaction is the envelope protein (Env) which is a trimer of gp120 monomers. Each HIV Env trimer interacts with one CD4 molecule (Chuang et al., 2017; Liu et al., 2017a). This is different from the AIV HA trimer in which each monomer in the trimer interacts with one glycan Cr (De Graaf and Fouchier, 2014; Fei et al., 2015). Initial attachment of the HIV virion to the host CD4+ T cell surface is relatively nonspecific (Wilen et al., 2012) with HIV Env interacting with negatively charged host cell surface heparan sulphate proteoglycans, or with pattern recognition receptors. According to Wilen et al. (2012), non-specific HIV attachment to the host cell via any of these factors likely brings HIV Env into close proximity with the viral receptor CD4 and the CRR5 coreceptor, so increasing the efficiency of infection, although the physiologic role of non-specific attachment in vivo remains unclear. Here it is suggested that non-specific binding helps to overcome the thermodynamic entropy constraint of immobilisation of a large virus on binding at human body temperature by taking some of the entropy loss in ΔSa_immob prior to specific HIV Env:CD4 binding. This would be consistent with the fact that non-specific attachment factors differ from receptors in that they are not essential, although they augment infection in vitro (Wilen et al., 2012).
A review of the literature has not found any results for the effect of temperature on the binding of HIV to CD4+ T cells with which to test or validate the HIV thermodynamic binding model developed here. However, Frey et al. (1995) reported the binding of cells expressing HIV GP on their surface to CD4+ T cells over the temperature range of 0 °C to 42 °C. It is known that increasing host membrane fluidity at higher temperature allows effective recruitment of more Cr molecules to bind the HIV virion (Harada et al., 2004) such that the number, n, of GP/Cr contacts increases with temperature (Frey et al., 1995), and that increasing n can overcome both the effect of temperature on decreasing the GP/Cr binding affinity and the effect of a large negative ΔSa_immob (Gale 2019). The thermodynamic HIV binding model here is therefore modified to accommodate increasing n with temperature and so attempt to reproduce the results of Frey et al. (1995). The success of the model here is in predicting the subsequent decrease in binding reported by Frey et al. (1995) at higher temperatures due to ΔSa_immob.
Here six case studies are presented to illustrate the effects of the magnitude of n, ΔCp and ΔSa_immob on the temperature sensitivity of virus binding. These are:-
-
1
The predicted effect of the magnitude of ΔCp on the temperature dependence of Dengue virus (DENV) transmission by Aedes albopictus;
-
2
The predicted effect of the magnitude of ΔCp on the temperature peak observed for the specific binding of Western equine encephalitis virus (WEEV) to susceptible Culex tarsalis brush border fragments (BBFs);
-
3
A large negative ΔCp for a protein:protein GP/Cr system as represented by HIV gp120:CD4 diminishes host cell binding at human body temperature;
-
4
A large virus diameter as for the HIV virion diminishes host cell binding at the higher temperature of the human body through the large negative ΔSa_immob;
-
5
Non-specific attachment factors may partially overcome the unfavourable ΔSa_immob and hence enhance specific HIV binding through Env:CD4 interactions at human body temperature; and
-
6
Increasing the number, n, of GP/Cr contacts with temperature to reproduce the data of Frey et al. (1995) for binding of HIV Env-expressing cells to cells expressing CD4.
It may be thought there is little point in modelling HIV binding with temperature because HIV only infects human hosts at ~37 °C. However, the model here suggests mammalian temperature may be a constraint on HIV binding (due to the large negative ΔCp and ΔSa_immob) in effect exposing a potential weakness in the HIV infection process which could be exploited for antiviral therapy. The implications of making ΔSa_immob more negative are considered here as a novel approach to developing antiviral therapies with reference to Antoine et al. (2012) using zinc oxide nanoparticles for preventing infection by herpes simplex virus type 2 (HSV-2).
2. Methods
2.1. The change in heat capacity (ΔCp) on binding of virus GP to Cr receptors on the host cell
The change in enthalpy (H) with temperature (T) at constant pressure is the heat capacity, Cp.
Integrating with respect to temperature relates the absolute enthalpy (HT) at temperature T to that (HT0) at a given reference temperature T0 through Cp according to Eq. (1) (see Table 1 ). The attachment of a virus to its host cell is driven by the n individual interactions between GP and Cr made on binding as represented by the dynamic equilibrium in Eq. (2). The change in enthalpy for GP binding to Cr at temperature T, ΔHa_receptor_T, is given by Eq. (3).
Table 1.
Equations used. See methods for derivation.
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
| ||
|
Substituting Eq. (1) into Eq. (3) for the enthalpies for the GP.Cr complex (HT(GP.Cr)), the free GP (HT(GP)) and the free Cr (HT(Cr)) relates the enthalpy change for GP binding to Cr at temperature T, ΔHa_receptor_T, to that (ΔHa_receptor_T0) measured experimentally at temperature T0 (Du et al., 2016) according to Eq. (4) where ΔCp is the change in heat capacity defined as the difference between the heat capacities of the GP.Cr complex and the sum of the heat capacities of the free GP and Cr molecules as given by Eq. (5). Similarly the entropy change (ΔSa_receptor_T) for GP binding to Cr at temperature T is related to that (ΔSa_receptor_T0) measured experimentally at temperature T0 (Du et al., 2016) according to Eq. (6).
2.2. Modelling the effect of temperature on ΔHa_virus_T and ΔSa_virus_T and hence Ka_virus_T
ΔHa_virus_T and ΔSa_virus_T are the changes in enthalpy and entropy respectively on binding of virus to host cell at temperature T. Substituting the terms for ΔHa_virus_T (Eq. (7)) and ΔSa_virus_T (Eq. (8)) into Eq. (9) expresses ΔGa_virus_T in terms of n, ΔSa_immob, ΔHa_receptor_T and ΔSa_receptor_T (Eq. (10)) where ΔGa_virus_T is the change in Gibbs free energy on association of virus with a host cell at temperature T and ΔSa_immob is the change in entropy on immobilisation of the whole virus on the cell surface (Gale 2018; 2019).
2.2.1. The change in heat capacity on virus binding to its host cell
For this work it is assumed that the change in heat capacity on binding of a virus to a host cell is determined by the change in heat capacity on interaction of GP with Cr according to Eq. (5) and that ΔSa_immob in Eq. (10) is unaffected. In effect therefore the heat capacity of the “bulk” (i.e. non-GP/Cr) of the bound virus/host cell is the same as the sum of the heat capacities for the free virus and free host cell. This is acceptable because a change in heat capacity is related to a change in conformation of the molecular components (Myszka et al., 2000) and the conformation of the bulk of the host cell and the virus would be unaffected by attachment. Indeed, ΔSa_immob is mainly related to changes in rotational and translational mobility of the virus particle as a whole (see below) and does not involve the conformational changes in GP and Cr which are accommodated in the ΔSa_receptor_T term (Gale 2019). Since the heat capacity of the “bulk” of the bound virus/host cell is the same as the sum of the heat capacities for the free virus and free host cell, ΔCp for the bulk equals zero, and according to Eq. (6) therefore, ΔSa_immob itself at temperature T (calculated as ΔSa_immob_T = ΔSa_immob_T0 + ΔCp.ln(T/T0)) would be unaffected by temperature and hence constant as assumed in the models here.
2.2.2. The effect of the magnitude of ΔCp on virus binding affinity at temperature T
Substituting ΔHa_receptor_T and ΔSa_receptor_T from Eqs. (4) and (6) respectively into Eq. (10) gives Eq. (11) from which Ka_virus_T is calculated according to Eq. (12) where R is the ideal gas constant.
2.2.3. The choice of reference temperature, T0
Comparing the predicted effect on Ka_virus_T of the magnitude of ΔCp in Case studies 1, 2 and 3 requires a reference temperature, T0, to be defined at which the plots of Ka_virus_T intercept. Values of Ka_virus_T intercept at T = T0 because the n.ΔCp (T – T0 + T.ln(T/T0)) term in Eq. (11) equals zero. Therefore for the purpose of demonstrating the effect of ΔCp on the temperature sensitivity of Ka_virus_T, T0 needs to be chosen to be well above or below the temperature range of interest. It should be noted that the choice of reference temperature is artificial and is only used here out of necessity to demonstrate the effect of different ΔCp values while fixing the Ka_virus_T intercept temperature. Indeed a given GP/Cr system has its own natural ΔCp value which cannot be altered and is measured experimentally (Myszka et al., 2000; Fei et al., 2015). The T0 temperature of 37 °C is appropriate to study arthropod vector competence for arbovirus transmission over the 10 to 35 °C temperature range in Case studies 1 and 2 as used previously for the arthropod vector competence model (Gale 2019). However, since 37 °C is the human body temperature at which HIV binds to host cells, 37 °C is not a good choice for T0 in case study 3 for which T0 is therefore set to 4 °C. The reference temperature is 37 °C in Case studies 4, 5 and 6 because the experimentally measured value of ΔCp for HIV gp120:CD4 binding (Fig. 1) is used together with ΔHa_receptor_T0 and ΔSa_receptor_T0 values measured experimentally at a temperature T0 of 37 °C (Myszka et al., 2000), i.e. real data are used.
2.3. Case study 1: The predicted effect of the magnitude of ΔCp on the temperature dependence of DENV transmission by Aedes albopictus
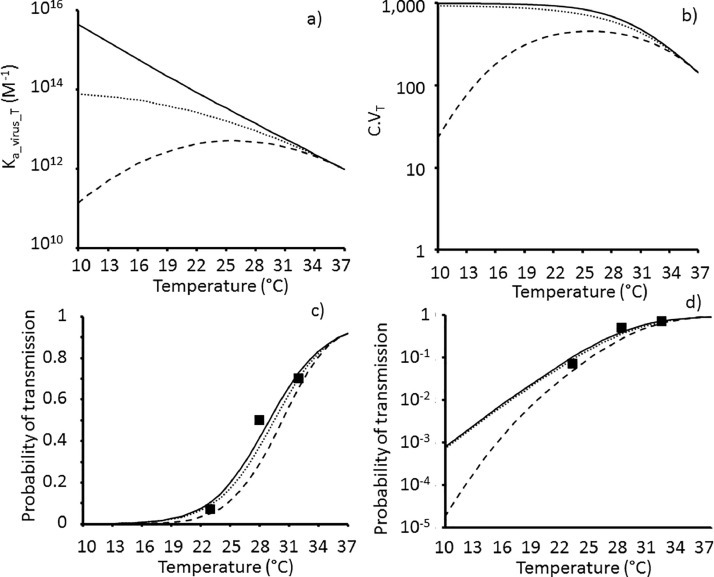
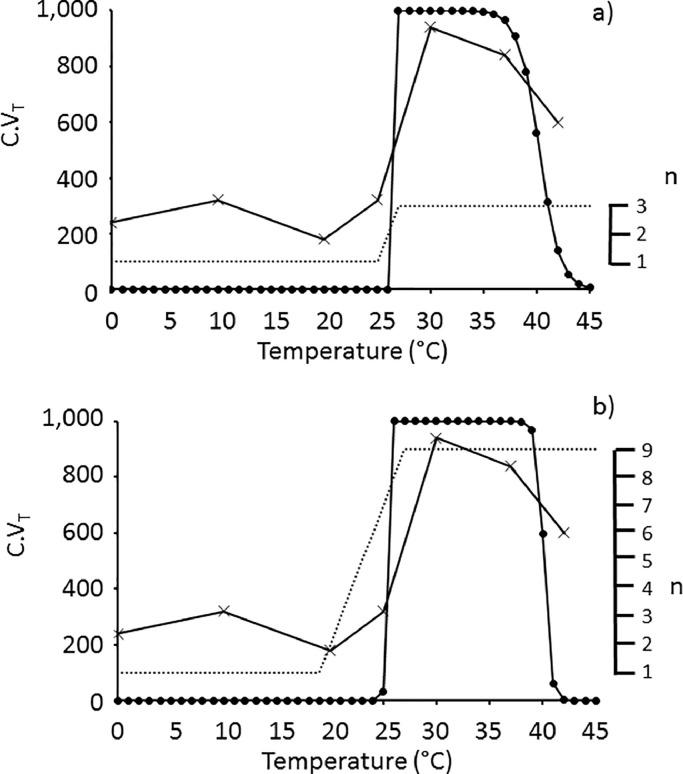
The approach for modelling arbovirus transmission efficiency by the arthropod vector has been fully described previously (Gale 2019) and is summarised here for the purpose of the models in Figs. 2 and 3 .
Fig. 2.
Temperature variation of a) Ka_virus_T; b) C.VT, c) and d) ptransmissionT for ΔCp = 0 (solid line), −1.97 (dotted line) and −5.02 (dashed line) kJ/mol/K (Table 3) with model parameters for arbovirus binding to mosquito midgut cells in Table 2 and ΔSa_immob = 0 J/mol/K. Experimental data (■) in c) and d) for DENV transmission efficiency by Aedes albopictus mosquitoes from Liu et al. (2017b).
Fig. 3.
Temperature variation of a) Ka_virus_T and b) C.VT for ΔCp = 0 (solid line), −3.0 (dotted line) and −5.02 (dashed line) kJ/mol/K (Table 3) with model parameters for arbovirus binding to mosquito midgut cells in Table 2 and ΔSa_immob = 0 J/mol/K. Experimental data (■) in b) show specific binding (as the percentage of total virus bound) of Western equine encephalitis virus (WEEV) to brush border fragments from susceptible Culex tarsalis mosquitoes as determined by Houk et al. (1990).
2.3.1. Modelling Ka_virus_T as a function of temperature
The strength of GP/Cr binding at temperature T is often expressed as the dissociation constant, Kd_receptor_T, for which smaller values indicate stronger binding (Xiong et al., 2013). The thermodynamic model is based on an enthalpy-driven GP/Cr interaction with a Kd_receptor_T0 of 10−3 M at 37 °C (T0) as used previously (Gale 2019) to represent the interaction between an arbovirus GP and a SA glycan (Cr) on the brush border surface of the epithelial cells lining the arthropod midgut. The parameters ΔHa_receptor_T0 and ΔSa_receptor_T0 at T0 = 37 °C for DENV transmission by Aedes albopictus together with n and ΔSa_immob are set out in Table 2 and values of Ka_virus_T over the temperature range 10–37 °C are calculated for the ΔCp values in Table 3 using ΔGa_virus_T from Eq. (11) in Eq. (12).
Table 2.
Summary of the parameters for the enthalpy-driven GP/Cr binding model for DENV transmission by Aedes albopictus developed previously (Gale 2019).
| Parameter | Value |
|---|---|
| Replication kinetic parameters for Eq. (15) | |
| pcomplete283 (10 °C) | 8.0 × 10−7 |
| EA (kJ/mol) | 270.0 |
| GP/Cr binding parameters | |
| ΔHa_receptor_T0 at 37 °C (kJ/mol) | −56.545 |
| ΔSa_receptor_T0 at 37 °C (J/mol/K) | −125 |
| Kd_receptor_T0 at 37 °C | 10−3 M |
| Whole virus binding parameters | |
| ΔSa_immob (J/mol/K) | 0 |
| Number of GP/Cr contacts (n) | 4 |
| ΔHa_virus_T0 (kJ/mol) from Eq. (7) | −226.2 |
| ΔSa_virus_T0 (J/mol/K) from Eq. (8) | −500 |
Table 3.
Summary of some published ΔCp values for protein/protein and protein/sialic acid (SA) interactions.
| System | Kd_receptor_T (Temperature) | ΔCp kJ/mol/K (95% c.i.) | Temperature range of experiment | References |
|---|---|---|---|---|
| HIV gp120 monomer: CD4 | 5 × 10−9 M (37 °C) | −5.02 (± 0.84) | 12 to 44 °C | Myszka et al. (2000) |
| E3 in pyruvate dehydrogenase multienzyme complex | 6 × 10−10 M (25 °C) | −1.32 (±0.06) | 10 to 37 °C | Jung et al. (2002) |
| E1 in pyruvate dehydrogenase multienzyme complex | 3 × 10−10 M (25 °C) | −1.97 (±0.06) | 10 to 37 °C | Jung et al. (2002) |
| AIV HA monomer: SAα−2,6 | 4.8 × 10−2 M (25 °C) | +0.125* | 15 to 25 °C | Fei et al. (2015) |
| AIV HA monomer: SAα−2,3 | 2.6 × 10−2 M (25 °C) | −0.0074* | 15 to 25 °C | Fei et al. (2015) |
Analysis of the data of Fei et al. (2015) by using their reported ΔG/TΔS values and Kd_receptor_T values confirms that ΔHa_receptor_T does not change with temperature with regression coefficients not being significantly different to zero (P >0.19) for binding of α2–3 and α2–6 sialyllactose to AIV HA monomer.
2.3.2. Modelling the effect of temperature on the number of cells in the arthropod midgut with bound arbovirus
The arbovirus challenge dose is 105 virions and the midgut volume is 10−6 dm3 giving a virus concentration [Vtotal] = 1.7 × 10−13 M. The fraction (FcT) of arthropod midgut cells with bound arbovirus at temperature T is calculated from Ka_virus_T using Eq. (13) assuming the concentration of free virus ([Vfree]) ~ [Vtotal]. The number, C.VT, of midgut cells with bound arbovirus at temperature T is calculated by multiplying FcT by the total number of midgut cells (Ctotal = 1000) (Eq. (14)) as described previously (Gale 2019).
2.3.3. Modelling the effect of temperature on the arbovirus transmission efficiency
The probability, pcompleteT, of an arthropod midgut cell with bound virus successfully leading to infection of the arthropod salivary glands and completion of virogenesis within in the lifetime of the arthropod at temperature T is calculated using the Arrhenius equation (Eq. (15)) where pcomplete283 is the probability of this happening at 10 °C (283 K) and EA is the activation energy of the rate-limiting step in virogenesis (Table 2). The probability, ptransmissionT, of arbovirus transmission by the arthropod (i.e. successful infection of the arthropod salivary glands after oral exposure) at temperature T given C.VT midgut cells have bound virus is given by Eq. (16).
2.4. Case study 2: The magnitude of ΔCp could explain the temperature peak observed in the specific binding of WEEV to susceptible Culex tarsalis BBFs
The value of ΔCp in Eq. (11) with the GP/Cr binding parameters for DENV in Table 2 was optimised so that C.VT as a function of temperature best approximated the specific binding affinity of WEEV to BBFs from susceptible Culex tarsalis mosquitoes as determined by Houk et al. (1990) and shown in Fig. 3.
2.5. Case study 3: A large negative ΔCp for a protein:protein GP/Cr system as represented by HIV gp120:CD4 diminishes host cell binding at higher temperatures
2.5.1. Estimation of n for HIV
Yang et al. (2005) using defective HIV gp120 monomers concluded that a single Env trimer is sufficient to mediate the entry of one virion, but that all three gp120 monomers in that trimer must be active. Klasse (2012) has proposed that a realistic model allows both a minimum requirement of two gp120 monomers with an increment in function by the third. This is consistent with the cryo-electron microscopy (EM) structure of the Env glycoprotein trimer (Liu et al., 2017a) showing that in each trimer, one gp120 monomer makes a primary contact with the bound CD4 Cr molecule while a second makes a partial contact (called the quaternary contact reflecting protein structure nomenclature) and the third gp120 monomer makes no direct contact with the CD4 at all. For the purpose of the model here, n represents the number of Env trimers on each HIV virion that interact with a CD4 Cr during binding. Brandenberg et al. (2015) demonstrate that divergent HIV strains differ in their stoichiometry of entry and require between 1 and 7 Env trimers, with most strains depending on 2 to 3 Env trimers to complete infection. Here it is assumed that n = 3 Env:CD4 interactions for HIV binding although the results of Brandenberg et al. (2015) do not separate cell surface binding itself from the subsequent HIV/cell fusion in the entry process. If it is later found that cell surface binding only requires one Env:CD4 interaction for example, while more are required for the membrane fusion, then the model here for C.VT should be re-parameterised with n = 1 although the number of Env:CCR5 and non-specific Env interactions with attachment factors (see below) should also be built into the model. It should be noted that as for the arbovirus model, it is assumed that the n = 3 Env:CD4 interactions act independently and not co-operatively in binding. This is reflected in Eqs. (7) and (8) where ΔHa_receptor_T and ΔSa_receptor_T act additively.
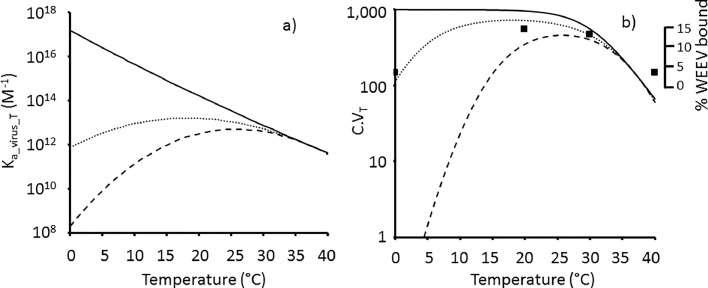
2.5.2. Thermodynamic parameters for HIV Env:CD4 binding at T0 of 37 °C
The Env trimer binds a single soluble CD4 with a Kd_receptor_T (25 °C) of 1.4 × 10−9 M (Chuang et al., 2017) which is 15-fold higher than that for the gp120 monomer:CD4 interaction estimated at 25 °C from the data of Myszka et al. (2000) in Table 4 . To the author's knowledge there are no data for ΔHa_receptor_T and ΔSa_receptor_T for Env trimer binding to CD4. Therefore the values for ΔHa_receptor_T0 and ΔSa_receptor_T0 for HIV gp120 monomer:CD4 binding at 37 °C from Myszka et al. (2000) are used for Env trimer binding to a single CD4 in the HIV model in Fig. 4 a and b as set out in Table 4. Dey et al. (2007) reported values at 37 °C of −287.9 kJ/mol and –786.9 J/mol/K for ΔHa_receptor_T and ΔSa_receptor_T respectively for the wildtype HIV-1 YU2 gp120 monomer binding to soluble CD4. The more negative ΔSa_receptor_T value for gp120 monomer:CD4 binding from Dey et al. (2007) reduces the binding affinity for gp120:CD4 by nine-fold (Kd_receptor_ T = 4.2 × 10−8 M) at 37 °C compared to that of 4.75 × 10−9 M from Myszka et al. (2000) (Table 4). This difference may simply reflect the different strains of HIV-1 used, namely YU2 by Dey et al. (2007) and WD61 by Myszka et al. (2000). The HIV gp120 monomer:CD4 binding data of Myszka et al. (2000) are chosen here over those of Dey et al. (2007) because Myszka et al. (2000) present the variation in ΔHa_receptor_T with temperature as shown in Fig. 1 together with information on ΔCp which Dey et al. (2007) do not consider. It is therefore assumed here that ΔCp = −5.02 kJ/mol/K for the Env trimer:CD4 interaction as reported by Myszka et al. (2000) for the gp120 monomer:CD4 interaction (Table 3).
Table 4.
Thermodynamic parameters for HIV Env binding to CD4 receptor at different temperatures. In the absence of data, the binding parameters for HIV Env trimer to CD4 as used in the models here are based on those from Myszka et al. (2000) for the full-length gp120 monomer binding to CD4.
| 37 °C | 4 °C | 25 °C | |
|---|---|---|---|
| ΔHa_receptor_T (kJ/mol) | −263.59a | −97.9c | −198.2e |
| ΔSa_receptor_T (J/mol/K) | −691.04b | −126.01d | −472.9e,f |
| Kd_receptor_T (M) | 4.75 × 10−9 | 1.28 × 10−12 | e0.91 × 10−10 |
From Myszka et al. (2000) for full length gp120 (reported as −63 kcal/mol) at 37 °C.
Calculated from –TΔS = +214.22 kJ/mol for full length gp120 (reported as +51.2 kcal/mol by Myszka et al. (2000)) at 37°C.
Estimated from values for ΔHa_receptor_T and -TΔSa_receptor_T presented in Fig. 4 of Myszka et al. (2000) for gp120 binding to CD4 at 25 °C.
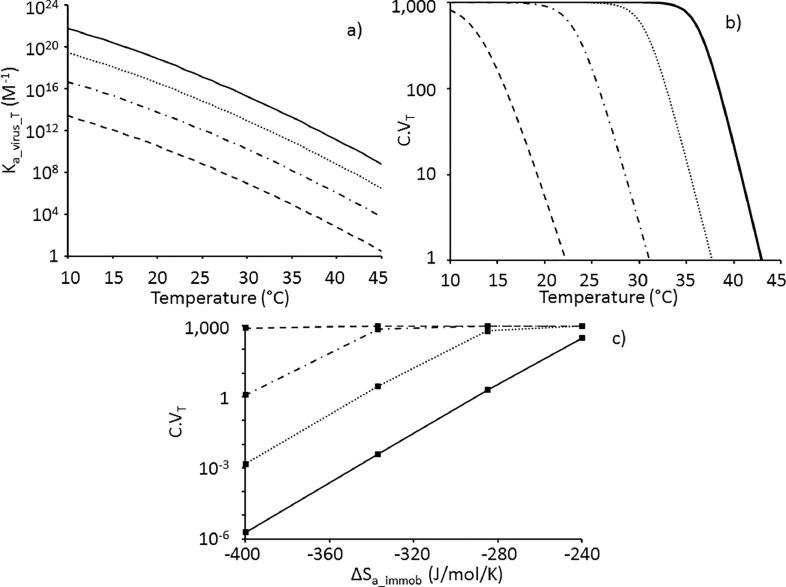
Fig. 4.
Temperature variation of a) and c) Ka_virus_T and b) and d) number, C.VT, of CD4+T cells per mm3 blood with bound HIV virions in HIV model for ΔCp = 0 (solid line), −1.97 (dotted line) and −5.02 (dashed line) kJ/mol/K (Table 3) and thermodynamic parameters for n = 3 HIV Env:CD4 interactions in Table 4 at reference temperature a) and b) T0 = 37 °C; c) and d) T0 = 4 °C. ΔSa_immob = −400 J/mol/K.
Values of ΔSa_receptor_T are not documented by Myszka et al. (2000) other than that at 37 °C (Table 4) and values at lower temperatures are therefore calculated from that at T0 = 37 °C according to Eq. (6) using ΔCp = −5.02 kJ/mol/K for HIV gp120:CD4 (Table 3). Some reassurance that Eq. (6) is appropriate is that the value of ΔSa_receptor_T of −493 J/mol/K predicted at T = 25 °C by Eq. (6) is very close to that of −473 J/mol/K calculated from the –T. ΔSa_receptor_T value reported by Myszka et al. (2000) at 25 °C (Table 4).
2.5.3. Thermodynamic parameters for HIV Env:CD4 binding at T0 of 4 °C
Predicted values for ΔHa_receptor_T and ΔSa_receptor_T for HIV Env:CD4 binding at 4 °C are set out in Table 4 and are used as ΔHa_receptor_T0 and ΔSa_receptor_T0 respectively for the HIV model in Fig. 4c and d with the reference temperature, T0, set to 4 °C to assess the effect of varying ΔCp on the temperature sensitivity of Ka_virus_T and C.VT up to and above human body temperature.
2.5.4. Model for HIV binding to CD4+T cells in blood
The 2.5 to 97.5 percentile range for the number of CD4+ T cells in humans is 448 to 1611 cells per mm3 (10−6 dm3) of blood with a mean of 919 cells per mm3 (Thakar et al., 2011). The model here takes 1 mm3 of blood with Ctotal = 103 CD4+ T cells and introduces Vtotal = 105 HIV virions. Dividing 105 HIV virions in 10−6 dm3 by the Avogadro number gives [Vtotal] = 1.7 × 10−13 M. The advantage of using a high Vtotal that greatly exceeds Ctotal is that as previously demonstrated by Gale (2018) not only may the fraction, FcT, of CD4+ T cells with bound HIV be calculated from Eq. (13) with [Vfree] ~ [Vtotal] but also any complications of handling stochastic effects at low virus doses are avoided. It is recognised that the HIV concentration at 105 HIV virions per mm3 used in this model is 10-fold to 100-fold higher than that expected in a recipient person's blood present in the capillaries lining the skin at the wound site where semen or blood from an infected source were introduced since maximum human plasma and human semen HIV loadings are in the region of 13,000 copies per mm3 and 1800 copies per mm3 respectively (Gupta et al., 1997). This is not important, however, because the purpose of the models here in Figs. 4 –6 is not to produce a realistic dose-response but to explore the effect of changing ΔCp, ΔSa_immob, n and temperature on the trend in the predicted number, C.VT, of host CD4+ T cells with bound virus. Indeed, the overall conclusions of the model in terms of the effect of temperature on the number of CD4+ T cells with bound virus will still be representative and the interpretation applicable to all doses of viruses as there is no cooperation between viruses in this model (Gale 2018). Furthermore, the levels of SIV in Rhesus monkey blood plasma were in the region of 2.1 × 108 virions per ml (Huitron-Resendiz et al., 2007) which is 2.1 × 105 virions per mm3 and representative of the 105 used for [Vtotal] in the model here. C.VT is calculated by multiplying FcT by Ctotal (Eq. (14)).
Fig. 6.
Experimental binding of HIV Env-expressing cells to cells expressing CD4 as reported by Frey et al. (1995) increases three to four fold at 25 °C (cross). The number, C.VT, of CD4+T cells with bound HIV virions per mm3 blood predicted by the thermodynamic model (circle) using Eq. (11) with the number, n, of GP/Cr contacts increasing according to the dotted line with temperature in a) from 1 to 3 between 25 and 27 °C; and in b) from 1 to 9 between 19 °C and 27 °C. The values of ΔHa_receptor_T0 and ΔSa_receptor_T0 at T0 = 37 °C for non-specific attachment factor binding and for HIV Env:CCR5 co-receptor binding are as those for specific HIV Env:CD4 binding in Table 4 with ΔCp = −5.02 kJ/mol/K (Table 3). ΔSa_immob = a) −206 J/mol/K to represent prior elimination of ΔSa_non_specific through binding of virus through non-specific attachment; and b) −1,110 J/mol/K to represent free virus binding.
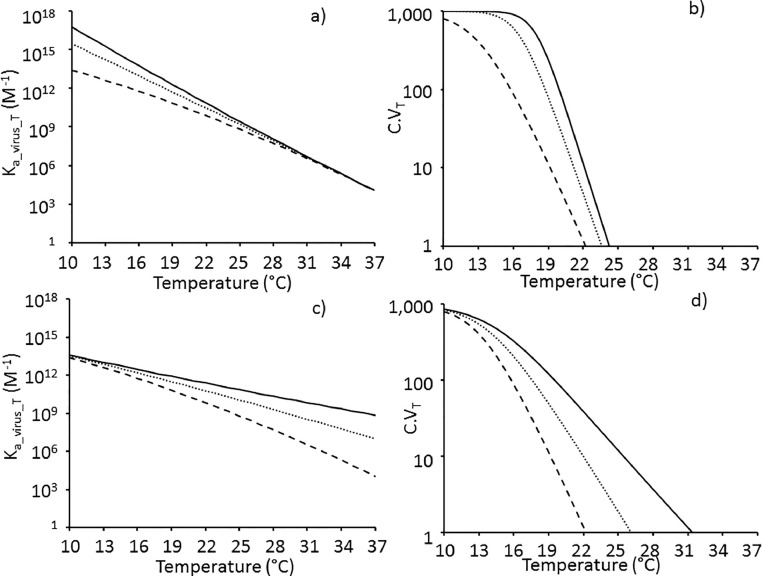
2.6. Case study 4: A large virus diameter such as for the HIV virion diminishes host cell binding at the higher temperatures of the human body through the large negative ΔSa_immob
2.6.1. Estimation of ΔSa_immob for a virus
There are currently no data available on the magnitude of ΔSa_immob which was first defined through development of a thermodynamic model (Gale 2019). Xiong et al. (2013) reported a Kd_virus of 10−15 M for AIV where Kd_virus is the dissociation constant for virus from the host cell and is the inverse of Ka_virus_T. According to Yang et al. (2005) HIV virions bearing influenza A virus HA required 8 or 9 HA trimers for virus entry. This is equivalent to n = 24 to 27 HA monomers each of Kd_receptor = 10−3 M (Xiong et al., 2013). It is not clear whether the 8 or 9 AIV HA trimers are required for cell binding or membrane fusion in Yang et al. (2005). However, if n = 24 HA monomers are required for AIV binding to the host cell to give a Ka_virus_T of 1015 M− 1 then ΔSa_immob equals −1091 J/mol/K from Eq. (17) (derived in Gale 2019). This is in the same order of magnitude as assumed for ΔSa_immob on the basis of virus molecular weight (Gale 2019). It must be emphasized that the estimate of 8 or 9 HA trimers in Yang et al. (2005) is based on a number of assumptions that may not hold, for example whereas each infection of a cell is a quantal, all-or-nothing event, the infectivity of a virion could span a wide spectrum of propensities and each mathematical model could have different virological interpretations (see Klasse 2012). However, in the absence of any data for ΔSa_immob the value of n from Yang et al. (2005) at least provides a theoretical approach to estimate it from Eq. (17) for this “proof of concept” model.
2.6.2. Effect of virus size on the magnitude of ΔSa_immob
It was shown previously (Gale 2019) that ΔSa_immob is the sum of the changes in translational entropy (ΔStrans) and rotational entropy (ΔSrot) of the whole virus on binding. According to Mammen et al. (1998) ΔStrans ∝ ln(Mass) and ΔSrot ∝ ln(Ix x Iy x Iz) where Ix, Iy and Iz are the moments of inertia about the three principle axes of rotation. Since mass, M, is proportional to the volume and I = Mr2 where r is the radius of the virus, it may be shown that the decrease in entropy on immobilisation (ΔSa_immob) of a spherical virus can be expressed as Eq. (18).
Examples of diameters for arboviruses are ~50 nm for WNV (Mukhopadhyay et al., 2003) and DENV, 66 nm for Eastern equine encephalitis virus (Hasan et al., 2018) with BTV being slightly larger at 85 nm (Nason et al., 2004). In contrast, HIV is much larger with a mean diameter of 134 nm in the case of mature HIV virions containing a single core (Briggs et al., 2003). The problem with Eq. (18) is that proportionality constants in units of J/mol/K are needed probably based on R as in the Sackur-Tetrode equation and the natural logarithm terms should be dimensionless such that the units of radius cancel out. However for the purpose of representing the effect of increasing the radius of the virus on ΔSa_immob Eq. (18) is used with the virus radius in units of nm. Thus from Eq. (18), the magnitude of ΔSa_immob for a virus of diameter 134 nm is 18.6% more negative than that for a virus of diameter 66 nm. To illustrate the effect of increasing virus size on the number of CD4+ T cells in 1 mm3 of blood with bound virus, C.VT is calculated for the HIV model using values of ΔSa_immob which decrease in steps of 18.6% from −240 J/mol/K (i.e. to −285 J/mol/K, −337 J/mol/K and −400 J/mol/K).
2.7. Case study 5: HIV attachment factors may partially overcome the unfavourable ΔSa_immob and enhance specific virus binding through Env/CD4 interactions at human body temperature
2.7.1. Modelling the effect of non-specific binding of HIV to host CD4+ T cells prior to specific Env:CD4 interaction
The term ΔSa_immob represents the decrease in entropy of the virus on going from a freely rotating entity to being immobilised in a specific orientation on the host cell surface through n = 3 specific Env:CD4 interactions. Thermodynamically this could be accomplished in two consecutive steps whereby the virus first binds non-specifically to attachment proteins on the host cell surface with an entropy change of ΔSa_non_specific, and then rolls into place driven by n = 3 specific Env:CD4 interactions resulting in a further entropy loss (ΔSa_specific) as the virus particle takes up a specific orientation ready for viral entry. In effect ΔSa_immob is the sum of two components, namely ΔSa_non_specific and ΔSa_specific according to Eq. (19). It should be noted that non-specific binding to HIV attachment factors would not increase ΔSa_immob to zero because there are multiple ways a virus could bind non-specifically compared to the one way in which it binds to the CD4 receptors through a specific interaction between Env and CD4, that is the ΔSa_specific term is always negative i.e. <0 J/mol/K and ΔSa_non_specific is always less negative than ΔSa_immob.
Prior attachment through non-specific binding would realise the ΔSa_non_specific loss before specific Env:CD4 binding so that specific binding involves the ΔSa_specific term alone. The value of ΔSa_immob is estimated to be −1091 J/mol/K (see above) and for the purpose of demonstration here ΔSa_immob is replaced by ΔSa_specific in Eq. (11) which is set to values of −400, −337, −285 and −240 J/mol/K in effect representing the effect of prior non-specific binding eliminating ΔSa_non_specific values of −691, −754, −806 and −851 J/mol/K respectively according to Eq. (19).
2.8. Case study 6: Increasing the number, n, of GP/Cr contacts with temperature to reproduce the data of Frey et al. (1995) for binding of HIV Env-expressing cells to cells expressing CD4
Two outputs of the model are demonstrated. The first output builds on the model in Case study 5 with a ΔSa_specific of −206 J/mol/K to accommodate prior non-specific binding to attachment factors having eliminated the ΔSa_non_specific of ~−900 J/mol/K. The model assumes n = 3 Env:CD4 interactions where n in Eq. (11) is increased from n = 1 to n = 3 with temperature between 25 °C and 27 °C (Fig. 6a) to represent the increase in contacts reported by Frey et al. (1995).
The second output attempts to include non-specific binding and also CCR5 co-receptor binding and a ΔSa_immob of −1110 J/mol/K is used to represent the free virus binding (i.e. prior to non-specific binding). Kuhmann et al. (2000) demonstrated that approximately four to six CCR5 molecules assemble around the HIV virion to form a complex needed for infection. The model here assumes n = 2 non-specific Env interactions with attachment factors followed by n = 4 Env:CCR5 interactions according to Kuhmann et al. (2000) and finally n = 3 Env:CD4 interactions based on Brandenberg et al. (2015) to form a complex for binding with n = 9 contacts in total which increase from 1 to 9 with temperature as shown in Fig. 6b. Doranz et al. (1999) estimated the Kd_receptor_T of interaction between CCR5 and HIV gp120 to be 4 × 10−9 M. This is remarkably similar to the Kd_receptor_T for the interaction between CD4 and HIV Env of 4.75 × 10−9 M at 37 °C (Table 4) and the same values for ΔHa_receptor_T0 and ΔSa_receptor_T0 not only for the four HIV Env:CCR5 interactions but also for the two non-specific interactions are therefore used as for the three HIV Env:CD4 interactions in Table 4 with the reference temperature, T0 at 37 °C.
3. Results
3.1. Published data on ΔCp for GP/Cr binding and other protein-protein interactions
Published values of ΔCp for protein/protein binding and for AIV HA binding to SA glycans vary in magnitude (Table 3). For the binding of HIV gp120 to CD4 which is a protein-protein interaction, the magnitude of ΔHa_receptor_T becomes more negative as the temperature increases i.e. ΔCp is negative (Fig. 1). Similarly, negative values of ΔCp were reported for other protein-protein systems, namely the binding of E3 and E1 proteins, respectively, in the assembly of the enzyme pyruvate dehydrogenase (Jung et al., 2002), although with ΔCp values less negative than that for HIV gp120:CD4 (Table 3). In contrast for AIV HA binding to the SA glycan the magnitude of ΔCp is not significantly different from zero with ΔHa_receptor_T constant over the temperature range 15 °C to 25 °C at least for binding of both α2–3 and α2–6 sialyllactose (Fig. 1).
3.2. Case study 1: The predicted effect of the magnitude of ΔCp on the temperature dependence of DENV transmission by Aedes albopictus
Values of Ka_virus_T predicted over the temperature range of 10 °C to 37 °C using different values of ΔCp intercept at the reference temperature (T0) of 37 °C (Fig. 2a) with Ka_virus_ T = 1012 M− 1 as expected for n = 4 GP/Cr interactions each of Kd_receptor_T0 of 10−3 M (Eq. (17)). With ΔCp = 0 kJ/mol/K as for AIV HA/SA, Ka_virus_T increases with decreasing temperature according to the Van't Hoff Isochore. In contrast with ΔCp = −5.02 kJ/mol/K as for HIV gp120:CD4, Ka_virus_T peaks at 26 °C and decreases rapidly at lower temperatures.
For the simulated DENV/Ae. albopictus model used here, small negative values of ΔCp (−2.0 kJ/mol/K to 0 kJ/mol/K) have little effect on the probability of transmission at low temperatures (Fig. 2c,d). This is because in the model here with ΔCp in the range of-2.0 kJ/mol/K to 0 kJ/mol/K, Ka_virus_T is high at >1014 M− 1 at low temperatures (Fig. 2a) and thus C.VT is little affected until higher temperatures (Fig. 2b) at which Ka_virus_T falls below 1014 M− 1 (Fig. 2a). Large negative values of ΔCp (−5.0 kJ/mol/K) cause C.VT to peak rapidly falling at lower temperatures (Fig. 2b). This has a large effect on the predicted probability of transmission at lower temperatures with ptransmissionT 44-fold lower at 10 °C (Fig. 2d). It is interesting to note that ΔCp has little effect on ptransmissionT over the range of temperature (23 °C to 32 °C) at which laboratory vector competence experiments (Liu et al., 2017b) are typically conducted (Fig. 2c).
3.3. Case study 2: The magnitude of ΔCp could explain the temperature peak observed in the specific binding of WEEV to susceptible Culex tarsalis BBFs
With a ΔCp = −3.0 kJ/mol/K the magnitude of Ka_virus_T between 0 and 40 °C is relatively constant compared to those with ΔCp = 0 kJ/mol/K and −5.02 kJ/mol/K (Fig. 3a) varying by only 40-fold and peaking at 1.62 × 1313 M− 1 at 18 °C. However, this variation in Ka_virus_T between 1012 and 1013 M − 1 is optimal for affecting the number of midgut cells with bound virus (Fig. 3b). This is because Ka_virus_T is high enough such that a significant proportion of midgut cells have bound virus over the 0 °C to 40 °C temperature range but not high enough to exceed the 1014 M− 1 above which all the midgut cells are saturated with virus. The variation in C.VT with temperature with ΔCp = −3.0 kJ/mol/K shows some similarity to the percentage variation in the amount of WEEV bound to BBFs from susceptible Culex tarsalis mosquitoes as measured experimentally by Houk et al. (1990) as represented by the symbols in Fig. 3b. According to Houk et al. (1990) the Ka_virus_T at 20 °C for WEEV binding to BBFs from susceptible Culex tarsalis mosquitoes is 2.2 × 1011 M− 1. This is within two orders of magnitude of the value of 1.57 × 1013 M− 1 predicted by the model here with ΔCp = −3.0 kJ/mol/K (Fig. 3a).
3.4. Case study 3: A large negative ΔCp for a protein:protein GP/Cr system as represented by HIV gp120:CD4 diminishes host cell binding at higher temperature
3.4.1. Reference temperature, T0, equals 37 °C
Ka_virus_T values for HIV binding and C.VT values for the number of CD4+ T cells in 1 mm3 of blood with bound HIV as a function of temperature are shown in Fig. 4a and b respectively for different ΔCp values with T0 = 37 °C. The Ka_virus_T and C.VT values in Fig. 4a and b respectively assume n = 3 Env:CD4 contacts with thermodynamic parameters in Table 4 and ΔSa_immob = −400 J/mol/K. The large negative value of ΔCp of −5.02 kJ/mol/K reported for gp120:CD4 (Table 3) diminishes binding at higher temperatures compared to ΔCp of 0 kJ/mol/K. Thus from Fig. 4b, only half of the 1000 cells have bound virus at 12 °C with ΔCp = −5.02 kJ/mol/K while with ΔCp = 0 kJ/mol/K half the cells still have bound virus at a temperature of 6 °C higher (18 °C). With ΔCp = −5.02 kJ/mol/K, C.VT is <1 cell (i.e. no virus bound) at 22 °C while with ΔCp = 0 kJ/mol/K the slightly higher temperature of 24 °C is required to decrease C.VT to <1 cell (Fig. 4b).
3.4.2. Effect of changing the reference temperature, T0, from 37 °C to 4 °C
The three lines representing Ka_virus_T for different values of ΔCp in Fig. 4a intercept at 37 °C (T0) and would do for C.VT in Fig. 4b if extrapolated to 37 °C. To demonstrate how the magnitude of ΔCp affects Ka_virus_T at temperatures of 37 °C representing mammalian body temperature, the reference temperature is set to 4 °C such that the three plots for Ka_virus_T intercept at 4 °C in Fig. 4c with much lower Ka_virus_T values predicted at 37 °C with a large negative ΔCp than for a system with ΔCp = 0 kJ/mol/K. The effect of ΔCp on the number of cells with bound virus at higher temperatures is considerable with C.VT reduced to 1 cell at 22 °C with ΔCp = −5.02 kJ/mol/K compared to 31 °C with ΔCp = 0 kJ/mol/K (Fig. 4d).
It should be noted that the dashed lines in Fig. 4c and d are the same as those in Fig. 4a and b respectively being based on experimental data for HIV gp120:CD4 (Fig. 1). The purpose of the dotted and solid lines is merely to illustrate the effect of less negative ΔCp increasing the binding at higher temperatures for the purpose of understanding.
3.5. Case study 4: A large virus diameter as for the HIV virion diminishes host cell binding at the higher temperature of the human body through the large negative ΔSa_immob
From Eq. (18), ΔSa_immob becomes more negative as the diameter of the virus increases. The value of Ka_virus_T decreases with increasing temperature in Fig. 5 a while more negative values of ΔSa_immob merely shift each parallel curve to lower Ka_virus_T values as expected from Eq. (17) such that Ka_virus_T falls below 1014 M− 1 at progressively lower temperatures. Values of C.VT with ΔSa_immob decreasing from −240 J/mol/K to −400 J/mol/K in steps of 18.6% are plotted in Fig. 5b and show that the number of cells with bound virus falls to <1 at progressively lower temperature as ΔSa_immob becomes more negative through increasing the virus diameter. The temperature at which C.VT falls to <1 is predicted to increase from 22 °C to 43 °C as ΔSa_immob increases in magnitude from −400 J/mol/K to −240 J/mol/K. The conclusion from Fig. 5a and b is that smaller viruses with less negative ΔSa_immob bind more strongly at higher temperatures than larger viruses. Only with ΔSa_immob as high as −240 J/mol/K representing smaller viruses do more than 30% of the 1000 cells have bound virus at the human body temperature of 37 °C according to the model in Fig. 5b. This is shown in Fig. 5c where nearly all the cells have bound virus at 10 °C irrespective of ΔSa_immob while at higher temperatures fewer cells have bound virus as ΔSa_immob becomes more negative.
Fig. 5.
Predicted effect of ΔSa_immob on the temperature sensitivity of a) Ka_virus_T and b) the number of host CD4+T cells, C.VT, with bound HIV virions in a system comprising Ctotal = 103 CD4+ host T cells in a 1 mm3 vol of blood with a challenge dose of 105 HIV virions. The values of ΔHa_receptor_T0 and ΔSa_receptor_T0 at T0 = 37 °C for specific HIV Env:CD4 binding are given in Table 4 with n = 3 Env:CD4 specific interactions and ΔCp = −5.02 kJ/mol/K (Table 3) for ΔSa_immob = −400 J/mol/K (dashed line), −337 J/mol/K (dash-dotted line), −285 J/mol/K (dotted line) and −240 J/mol/K (solid line). c) Effect of ΔSa_immob on C.VT predicted at temperatures of 10 °C (dashed line), 22 °C (dash-dotted line), 30 °C (dotted line) and 37 °C (solid line) with symbols representing outputs from model. For case study 4, more negative values of ΔSa_immob represent virions of increasing diameter. For case study 5, non-specific HIV attachment factor interactions prior to the specific HIV Env:CD4 interactions make ΔSa_immob less negative through realising entropy loss of ΔSa_non_specific in Eq. (19) (see text).
3.6. Case study 5: HIV attachment factors may partially overcome the unfavourable ΔSa_immob and enhance specific virus binding through Env/CD4 interactions at human body temperature
Fig. 5 can also be interpreted in terms of the effect of prior non-specific binding of HIV to attachment factors eliminating ΔSa_non_specific values of −691, −754, −806 and −851 J/mol/K according to Eq. (19) thus increasing ΔSa_specific for specific Env:CD4 binding (as ΔSa_immob in Eq. (11)) from −400 J/mol/K to −240 J/mol/K. Fig. 5b shows that the number of CD4+ T cells in a 1 mm3 vol of blood with bound HIV falls from 1000 to <1 over a temperature range of ~10 °C. The temperature at which fewer than half the T cells in the 1 mm3 vol of blood have bound HIV virus increases with increasing ΔSa_specific from 12.5 °C for ΔSa_specific = −400 J/mol/K to 36.5 °C for ΔSa_specific = −240 J/mol/K (Fig. 5b). Indeed once the ΔSa_specific is >−200 J/mol/K, 98% of the 1000 T cells have bound HIV at 37 °C (not shown). With ΔSa_specific <−285 J/mol/K virus is not specifically bound to any of the 1000 T cells at temperatures above 37 °C. It is concluded that the effect of making ΔSa_immob less unfavourable through prior non-specific binding taking some of the entropy loss enhances subsequent specific binding of HIV through Env:CD4 interactions at higher temperatures. Fig. 5c shows that at 37 °C increasing ΔSa_specific from −400 to −240 J/mol/K increases the number of CD4+ T cells with HIV bound through specific Env/CD4 interactions in a 1 mm3 vol of blood from 2 × 10−6 to 307. It should be noted that 2 × 10−6 cells in 1 mm3 is equivalent to 1 cell in 500 cm3 of blood.
3.7. Case study 6: Increasing the number, n, of GP/Cr contacts with temperature to reproduce the data of Frey et al. (1995) for binding of HIV Env-expressing cells to cells expressing CD4
Cells expressing HIV Env on their surface can bind and fuse with cells expressing CD4 Cr (Frey et al., 1995). Frey et al. (1995) reported a three to four fold increase in cell binding at temperatures above 25 °C with a substantial decrease in binding at temperatures above 37 °C (Fig. 6 ), the latter being predicted by the thermodynamic model in Fig. 5b. Frey et al. (1995) attribute the increase at 25 °C to the additional adhesion molecules which are brought into contact to increase the avidity of binding at higher temperatures. The thermodynamic model for HIV binding with ΔSa_immob of −206 J/mol/K reproduces the increase in predicted C.VT in Fig. 6a by increasing n from 1 to 3 over the temperature range 25 °C and 27 °C to reflect the effect of temperature facilitating multiple HIV adhesion/binding sites due to increased membrane fluidity (Frey et al., 1995; Harada et al., 2004). Increasing n from 1 to 9 over the temperature range 19 °C and 27 °C gives a sharp increase in C.VT at 26 °C (Fig. 6b) with ΔSa_immob of −1110 J/mol/K. The subsequent sharp fall in C.VT at temperatures above 37 °C is due to the large negative magnitude of ΔSa_immob (−206 J/mol/K in Fig. 6a and -1110 J/mol/K in Fig. 6b) relative to n such that the diminished GP/Cr affinity at higher temperatures is not sufficient to maintain binding even with n = 9 GP/Cr interactions in Fig. 6b. The decrease in GP/Cr binding affinity with temperature for HIV Env:CD4 is apparent from the Ka_virus_T values in Fig. 5a and the increase in the values of Kd_receptor_T for the temperatures 4 °C, 25 °C and 37 °C in Table 4.
4. Discussion
Previously a thermodynamic model for the effect of temperature on arthropod vector competence was developed (Gale 2019) based on the parameters ΔHa_receptor_T, ΔSa_receptor_T, ΔSa_immob and n, together with the kinetic parameters, pcomplete283 and EA (Table 2). This paper furthers that model by allowing the change in heat capacity, ΔCp, on GP/Cr binding to be included. This is important because it defines the effect of temperature on ΔHa_receptor_T (Eq. (4)) and ΔSa_receptor_T (Eq. (6)) and hence Ka_virus_T. Of potentially greater importance, however, is the parameter ΔSa_immob first formally identified in the thermodynamic analysis of virus binding (Gale 2019). Thus it is proposed here that the value of ΔSa_immob is not only important in explaining the observation that dsDNA viruses infecting warmer hosts are generally smaller in volume than those infecting colder hosts (Nifong and Gillooly 2016) but also may contribute to explaining the need for attachment factors to allow binding of a large virus such as HIV at the relatively high human body temperature of 37 °C. This has implications for the design of novel antiviral therapies. The mechanistic model developed here for HIV goes as far as cell binding and viral membrane fusion (Harrison 2015) could be added as the next stage to complete the cell entry process.
4.1. Justification of assumptions for ΔSa_immob
Calculations using Eq. (17) on the basis of limited available data suggest ΔSa_immob ~ −1100 J/mol/K for HIV although it is acknowledged above that there is considerable uncertainty in the absence of definitive experimental data. It is possible that statistical thermodynamics approaches analogous to the Sackur-Tetrode equation for the entropy of a gas may be developed to estimate ΔSa_immob theoretically. The large size of the HIV virion (134 nm mean diameter) compared to a typical arbovirus (50 to 70 nm diameter) is consistent with a more negative value of ΔSa_immob providing justification for the more negative ΔSa_immob values used here for the HIV models in Fig. 4, Fig. 5, Fig. 6 compared to that used for the arbovirus models in Figs. 2 and 3.
4.2. Interpretation of figures
Fig. 2, Fig. 3, Fig. 4, Fig. 5 show the variation of Ka_virus_T and C.VT with temperature as predicted by models assuming Ctotal = 103 host cells in a 10−6 dm3 volume (i.e. mosquito midgut or human blood sample) challenged with Vtotal = 105 virions. Previously it was shown that if Ka_virus_ T > ~1014 M− 1 then nearly all the host cells have bound virus at such a high virus dose (Gale 2018; 2019). Thus the Ka_virus_T plots and corresponding C.VT plots are best interpreted in terms of the temperature ranges over which Ka_virus_ T < ~1014 M− 1.
4.3. The importance of negligible ΔCp for low temperature arbovirus transmission
For the arbovirus models in Figs. 2 and 3, the main conclusion regarding the change in heat capacity on GP/Cr binding is that as ΔCp becomes more negative so a peak temperature for Ka_virus_T becomes apparent such that binding affinity falls at lower and higher temperatures, directly affecting C.VT when Ka_virus_T falls below 1014 M− 1. Values of ΔCp from 0 to ~−2.0 kJ/mol/K have relatively little impact on the temperature sensitivity of the number, C.VT, of mosquito midgut cells with bound virus (Fig. 2b), while intermediate values of ΔCp of ~−3.0 kJ/mol/K give a peak binding at a temperature of ~20 °C as observed experimentally for WEEV binding to BBFs from susceptible mosquito midguts in Fig. 3b. More negative values of ΔCp at −5.0 kJ/mol/K greatly diminish arbovirus binding affinity at temperatures below ~20 °C (Fig. 2b) which in turn diminishes the transmission efficiency of the arbovirus at temperatures below 20 °C compared to GP/Cr systems with ΔCp in the range of −2.0 to 0 kJ/mol/K (Fig. 2d). In evolutionary terms, to optimise arbovirus infectivity with n = 4 GP/Cr interactions over a range of temperatures, GP/Cr interactions with small ΔCp would be selected as for AIV HA/SA binding (Table 3). It is proposed here that to maintain some transmission efficiency at lower temperatures, arboviruses may use SA binding interactions as shown for BTV coat protein VP2 (Zhang et al., 2010) for which ΔCp may approximate 0 kJ/mol/K as in the case of AIV HA/SA (Table 3). This would facilitate arboviruses’ expanding their range into temperate regions of the world with climate change.
4.3.1. The value of ΔCp does not affect arbovirus binding to arthropod midguts at higher temperatures
With the reference temperature of T0 = 37 °C, C.VT falls rapidly at temperatures above 20 °C in the arbovirus model here with n = 4 GP/Cr interactions irrespective of the magnitude of ΔCp (Fig. 2b) as the Ka_virus_T values fall below 1014 M − 1 and converge at 1012 M − 1 at 37 °C (Fig. 2a). This fall is observed experimentally as the temperature is increased from 20 °C to 40 °C (Fig. 3b) for WEEV binding to BBFs from susceptible mosquito midguts as reported by Houk et al. (1990).
4.4. The large negative ΔCp for HIV gp120:CD4 diminishes binding at human body temperature in the HIV model
The ΔCp for HIV gp120:CD4 binding is well documented unlike that for arbovirus binding and the values of ΔHa_receptor_T have been reported over the temperature range of 12 °C to 44 °C (Fig. 1). The results with varying ΔCp in Fig. 4 are therefore hypothetical but illustrate how the large negative ΔCp for the HIV Env:CD4 interaction diminishes binding at the higher temperatures of mammals and birds compared to a system such as HA/SA for which ΔCp = 0 kJ/mol/K. Thus, a less negative ΔCp increases the number of cells with bound virus at higher temperatures, albeit more markedly for the reference temperature T0 = 4 °C (Fig. 4d) than for T0 = 37 °C (Fig. 4b). In the absence of data for ΔCp for HIV Env:CD4 binding, the value for the gp120 monomer:CD4 interaction is used for the HIV models in Fig. 4, Fig. 5, Fig. 6. Evidence for a large negative ΔCp for HIV Env:CD4 binding is that cryo-EM demonstrates considerable conformational shifts (Liu et al., 2017a).
4.5. ΔSa_immob as a repulsive force in virus binding
A negative value of ΔSa_immob presents a repulsive force between the virus and the host cell in effect preventing virus binding and with n = 0 GP/Cr contacts, Ka_virus_T is < 1 M− 1 according to Eq. (17) (Gale 2019). Increasing the value of n is one way for the virus to overcome a large negative value of ΔSa_immob (Gale 2019). Thus 15 to 18 GP/Cr contacts of Kd_receptor_T0 = 10−3 M (37 °C) were sufficient to overcome a ΔSa_immob of −750 J/mol/K such that Ka_virus_ T > 1014 M− 1 (Fig. 3 of Gale (2019)). This is apparent from Fig. 6a where n = 3 GP/Cr contacts can overcome a ΔSa_immob of −206 J/mol/K while n = 9 GP/Cr contacts are required to overcome the more negative ΔSa_immob of −1110 J/mol/K in Fig. 6b.
4.6. A less negative ΔSa_immob maintains virus binding at higher temperatures
Even for ΔSa_immob = 0 J/mol/K as in Figs. 2a and 3a, the magnitude of Ka_virus_T decreases with increasing temperature (albeit after a peak in the case of ΔCp < −2.0 kJ/mol/K). This is due to the reduced affinity of the enthalpy-driven GP/Cr interactions at higher temperatures. Making ΔSa_immob more negative shifts the Ka_virus_T curve to lower values (Fig. 5a) thus exacerbating the effect of higher temperature on reducing binding. As Ka_virus_T falls below 1014 M − 1 at higher temperatures, so C.VT falls (Fig. 5b). The magnitude of ΔSa_immob merely positions the C.VT curve relative to the temperature scale with less negative values of ΔSa_immob shifting the curve to higher temperatures (Fig. 5b) such that high C.VT values are maintained at progressively higher temperatures as ΔSa_immob becomes less negative (Fig. 5c).
4.7. Balancing opposing constraints at mammalian host temperatures
The thermodynamic model here suggests that a large negative ΔCp for HIV Env:CD4 diminishes binding at higher temperatures. However, there may be molecular constraints such that a large negative ΔCp value is a direct consequence of a molecular mechanism involving a large conformational change that serves a purpose for cell entry/fusion (Harrison 2015) such that a negligible ΔCp value may not be achievable. Furthermore, a large negative ΔSa_immob imposes additional constraints on virus binding at higher temperatures exacerbating the reduced strength of the enthalpy-driven GP/Cr interactions at higher temperatures. Therefore other mechanisms may be needed by the virus to achieve binding at 37 °C. These could include more GP/Cr contacts at higher temperature (Frey et al., 1995; Harada et al., 2004). An alternative strategy evolved by viruses could be to make ΔSa_immob itself less negative such that virus binding is maintained at the higher body temperatures of mammals and birds. Two possible evolutionary strategies are suggested here which could make ΔSa_immob less negative. The first is decreasing the size of the virus and the second is the use of non-specific attachment factors to randomly trap the virus on the cell surface prior to specific GP/Cr binding.
4.8. Small virus size makes ΔSa_immob less negative thus maintaining binding at higher temperatures
Decreasing the size of a virus makes ΔSa_immob less negative (Eq. (18)) such that smaller viruses bind more strongly at the higher temperatures of mammals and birds (Fig. 5). It is suggested that binding to cells at the higher temperatures of avian and mammalian hosts selects for viruses of smaller diameter through a less negative ΔSa_immob. This could explain the decrease in volume of viruses with increasing host/environment temperature as reported by Nifong and Gillooly (2016) for dsDNA viruses. Thus the average diameters of dsDNA viruses decreased from 182 nm at a host/environment temperature of 10 °C down to 74 nm at 37 °C according to the best fit line of Nifong and Gillooly (2016) suggesting the HIV virion at 134 nm mean diameter is almost double the size for a virus infecting at avian/mammalian host temperature. It is interesting to note that thermophilic bacteria adapted to high temperature may be subject to selection favouring smaller cell size. This may aid attachment to biofilms which provide some protection against temperature stress.
4.9. The importance of prior non-specific binding in taking some of the entropy loss in ΔSa_immob
It is proposed here that by taking the entropy loss ΔSa_non_specific in ΔSa_immob that non-specific binding to attachment factors facilitates subsequent specific HIV Env binding to CD4 receptors on the host CD4+ T cell at human body temperature. Thus the shift in the Ka_virus_T curve to higher values with a less negative ΔSa_immob in Fig. 5a is consistent with HIV attachment factors augmenting infection (Wilen et al., 2012). Indeed with n = 3 Env:CD4 contacts, significant binding of HIV to host cells is only achieved at 37 °C if ΔSa_immob is increased to > −280 J/mol/K (Fig. 5c). ΔSa_immob is estimated here to be −1091 J/mol/K for HIV. Thus the prior non-specific binding of HIV would need to realise a ΔSa_non_specific of −810 J/mol/K for subsequent effective Env:CD4 binding at human body temperature according to the model such that ΔSa_non_specific in Eq. (19) takes ~75% of the entropy loss in ΔSa_immob. Wilen et al. (2012) also report that HIV attachment factors are not essential. Again this is consistent with the model here when it is noted that the C.VT value of <1 CD4+ T cell with bound virus in Fig. 5b is not a threshold and merely represents 1 mm3 of blood. Thus with ΔSa_immob = −348 J/mol/K, C.VT = 1 × 10−3 at 37 °C (Fig. 5c). This represents one CD4+ T cell with bound HIV in 1000 × 1 mm3 vol of blood, i.e. in 1 cm3 of blood. Decreasing ΔSa_immob further to −405 J/mol/K gives C.VT = 1 × 10−6 at 37 °C representing one CD4+ T cell with bound HIV in 1 litre of blood.
4.10. Making ΔSa_immob more negative as a strategy for development of antiviral therapeutics
The model here suggests human body temperature may be a constraint on HIV binding (due to the large negative values of both ΔCp and ΔSa_immob) in effect exposing a potential weakness in the HIV infection strategy which could be exploited for antiviral therapy. Figure 9 of Antoine et al. (2012) shows a herpes simplex virus type 2 (HSV-2) bound to a tetrahedral nanoparticle of zinc oxide (ZnO) called a zinc oxide tetrapod (ZnOT). The mechanism behind the ability of ZnOTs to prevent, neutralize or reduce HSV-2 infection relies on their ability to bind the HSV-2 virions (Antoine et al., 2012). The ZnOT being some 40 µm in size is much larger than the attached virion which could still attach to a host cell surface in terms of spatial considerations. However, the magnitude of ΔSa_immob for an HSV-2 virion bound to a ZnOT nanoparticle would be very large and negative, indeed much more negative than for ΔSa_immob for a free HSV-2 virion. Thus according to Fig. 5c, binding of HSV-2/ZnOT to host cells would be greatly diminished particularly at the human body temperature due to the very large negative ΔSa_immob. Although ΔSa_immob changes logarithmically (i.e. slowly) with virus size according to Eq. (18), the number, C.VT, of cells with bound virus is very sensitive to changes in ΔSa_immob at 37 °C (Fig. 5c). It is proposed that antiviral research should take into account and even focus on making the magnitude of ΔSa_immob more negative in addition to looking at conventional approaches to block the GP/Cr interaction. The advantage of focusing on ΔSa_immob is that only one ZnOT nanoparticle has to bind to a virus to markedly affect ΔSa_immob, while a large proportion of the GP molecules on the virus have to be bound with inhibitors, including neutralising antibodies, to block virus binding (Klasse 2012) and hence eliminate ΔHa_receptor_T0 in Eq. (11). The temperature dependence of virus diffusion in mucus (Erickson et al., 2015) could also be considered not only in mechanistic dose-response models for viral infection at mucosal epithelial membranes in the intestine (Gale 2018) but also in terms of therapeutics when combined with the thermodynamic approach developed here. Normal, acidic cervicovaginal mucus greatly hinders the movement of virions of HSV and HIV, whereas mucus that is neutralized by semen provides a much less effective barrier against the same virions (Erickson et al., 2015). Thus binding of the HSV or HIV virion to a ZnOT particle may not only decrease its diffusion coefficient in mucus but also make the magnitude of ΔSa_immob more negative hence reducing the binding affinity of those virions which do make it through the mucus to the epithelial cell surface at human body temperature.
4.11. Validation of the HIV model
It is assumed for the purpose of the “proof of concept” model here that the thermodynamic parameters for the HIV gp120 monomer:CD4 interaction in Myszka et al. (2000) can be used for HIV Env trimer binding to a single CD4 in the absence of data. Although the Kd_receptor_T value for the Env trimer:CD4 interaction (1.4 × 10−9 M, Chuang et al., 2017) is 15-fold higher than that for the gp120 monomer:CD4 interaction (0.9 × 10−10 M, Table 4) at 25 °C, this is close enough to support using the gp120 monomer:CD4 data, particularly as Kd_receptor_T values for the gp120 monomer:CD4 interaction vary nine-fold between two HIV strains (see above).
The predicted values of Ka_virus_T increase with decreasing temperature according the HIV model in Fig. 5a. This is unexpected on the basis of the ΔHa_receptor_T values reported by Myszka et al. (2000) for gp120:CD4 which become less negative with decreasing temperature (Fig. 1). However, according to Eq. (6) the predicted ΔSa_receptor_T term becomes more favourable (less negative) with decreasing temperature and it is therefore the entropy term that facilitates the tighter binding of gp120 to CD4 at lower temperatures. Unfortunately Myszka et al. (2000) only give the full range of values for ΔHa_receptor_T (Fig. 1) with no data for ΔSa_receptor_T over the range of temperature. However, Myszka et al. (2000) do give some graphical data from which ΔSa_receptor_T at 25 °C can be estimated and it is reassuring this ΔSa_receptor_T is much less negative at −473 J/mol/K than that of −691 J/mol/K measured at 37 °C and furthermore is actually less negative than the value of −492.8 J/mol/K predicted for 25 °C by Eq. (6) (Table 4) and used in the model in Fig. 5. This is strong experimental evidence that warming to 37 °C and above does indeed give a significant reduction in the binding affinity of Env to CD4 as borne out by the 52-fold increase in the Kd_receptor_T value for gp120:CD4 on warming from 25 °C to 37 °C as calculated from the actual data of Myszka et al. (2000) (Table 4). Furthermore it suggests that the actual increase in Ka_virus_T on cooling from 37 °C down to 25 °C may be greater than that predicted by the model in Fig. 5a. The decrease in binding affinity with increasing temperature for HIV Env:CD4 is also supported by experimental data of Moore and Klasse (1992) which showed that soluble CD4 dissociated from HIV virions at temperatures above 35 °C. Similarly Doranz et al. (1999) demonstrated that gp120 bound to CD4+ T cells began to dissociate at temperatures above 45 °C. The data of Frey et al. (1995) in Fig. 6 offer further validation of the model in that the binding of HIV Env-expressing cells to cells expressing CD4 decreases substantially at 37 °C as predicted by the model. The Env trimer is stable up to at least 60 °C (Chuang et al., 2017) suggesting it is not denaturation of the Env trimer itself that is responsible for the decreased binding at higher temperatures. However, care has to be taken in using Eqs. (4) and (6) to predict ΔHa_receptor_T and ΔSa_receptor_T respectively down to very low temperatures. Thus although the predicted value of Kd_receptor_T for gp120:CD4 at 4 °C is 3700-fold lower than that at 37 °C (Table 4), Frey et al. (1995) cite some studies which suggested weaker binding of soluble CD4 to HIV virions at 4 °C compared to 37 °C. Without actual binding data for HIV over the full temperature range, it cannot be ruled out that Ka_virus_T does not exhibit a peak with temperature as for the WEEV binding in Fig. 3b. Indeed, binding of 125I-labelled gp120 to T cells peaked at 16 °C with binding at 4 °C much lower than that at 37 °C (Frey et al., 1995). The observed increase between 4 °C and 16 °C is unlikely to be due to increased fluidity of the membrane allowing recruitment of more CD4 molecules because unlike the virus, each gp120 only binds a single Cr molecule. Dimitrov et al. (1992) showed that the activation energy for binding of soluble CD4 to cells expressing HIV Env changed at 18 °C suggesting 18 °C is a transition temperature. This could explain the peak in binding of gp120 at 16 °C reported by Frey et al. (1995). Thus extrapolation of ΔHa_receptor_T and ΔSa_receptor_T through Eqs. (4) and (6), respectively to temperatures below 18 °C may not be justified in the case of HIV binding.
It should be remembered that HIV only infects humans at 37 °C and therefore the lower temperature predictions are more of academic interest, although temperature trends may give an insight into weaknesses in the HIV infection strategy as suggested here. It is only the 37 °C line in Fig. 5c which is important for HIV and it is reassuring to note that this is based on actual experimental data for gp120 monomer:CD4 binding measured at that temperature. The lower temperature lines in Fig. 5c are of more general interest, for example in explaining the observed relationship (Nifong and Gillooly 2016) between larger virus volume and lower host temperature.
4.12. Variation between virions in an exposure dose
Individual virions of the same virus may vary both in size (Briggs et al., 2003) and in the case of some RNA viruses in the actual base sequence of the genome giving a spectrum of mutants. The infection process may represent a bottleneck such that only one or two viral variants in the exposure dose successfully establish infection (Bull et al., 2011). Thus in the case of norovirus, only minor variants at frequencies as low as 0.01% were successfully transmitted to establish a new infection (Bull et al., 2012). The work here suggests that the actual size of the virion itself may present an additional constraint particularly at mammalian body temperatures. Thus although the average diameter for HIV virions with a single core is 134 nm, individual virions display a broad range of diameters extending from 120 to 200 nm with a skewed distribution (Briggs et al., 2003). Furthermore while the majority of HIV virions contained a single core, almost a third contained two or more cores. The mean diameter of the HIV virions containing a single core (134 ± 11 nm, n = 89) was significantly smaller than the mean diameter of virions containing two cores (158 ± 16 nm, n = 43) (Briggs et al., 2003). Thus the magnitude of ΔSa_immob may vary between individual HIV virions within the same exposure dose. The key conclusion from Fig. 5c is that the number of CD4+ T cells with bound virus is highly sensitive to the magnitude of ΔSa_immob with just a 4.5% increase in the magnitude of ΔSa_immob from –290 to –277 J/mol/K for example increasing C.VT by five-fold from 1 to 5 CD4+ T cells per mm3 of blood at 37 °C. Thus smaller diameter viruses in a challenge does may have an advantage in binding and hence initiating infection at mammalian body temperatures. This also raises the question of the magnitude of ΔSa_immob for an aggregate containing several virions of the same virus and in the case of EBOV, for the long filaments linking multiple genome copies (Beniac et al., 2012). It has previously been proposed that fusing multiple genome copies into the same filament in the case of EBOV takes some of the entropy loss for ΔSa_immob prior to binding to the cell surface (Gale 2017) such that aggregation can be viewed as a cooperative effect in the infection process. The effect of aggregation and virus size on the magnitude of ΔSa_immob according to Eq. (18) needs to be investigated and understood to further the work here.
5. Conclusion
From a thermodynamic perspective, the affinity of virus binding to a host cell is greatly decreased at the higher body temperatures of mammals and birds such that temperature can be considered a constraint to be overcome. The relationship between binding affinity and temperature can be markedly affected by the change in heat capacity (ΔCp) on virus binding through its effect on the enthalpy and entropy of the GP/Cr interaction. Specifically large negative values of ΔCp reduce binding at both low and high temperatures giving a peak binding at a medium temperature as has been observed experimentally in binding of WEEV to mosquito midguts. Very large negative values of ΔCp for protein/protein GP/Cr interactions are predicted to diminish arbovirus transmission at low temperatures compared to the HA/SA glycan interaction for which ΔCp is negligible. Thus selecting for SA glycan interactions as reported for BTV binding may be a mechanism to allow transmission at the lower temperatures experienced by arboviruses infecting arthropods in temperate regions of the world.
The magnitude of ΔSa_immob is currently unknown but is predicted to be large and negative and to be more negative for larger viruses such as HIV (mean diameter 134 nm) compared to the smaller arboviruses (diameter 50 to 70 nm). Small virion diameter through a less negative ΔSa_immob, favours virus binding at higher temperatures giving smaller viruses a selective advantage for infecting hosts at the higher body temperatures of mammals and birds. This is in agreement with the published observational findings that virus volume decreases with increasing host temperature in the case of dsDNA viruses.
In the case of HIV, the unfavourable effect at human body temperature of the large negative ΔSa_immob value due to the large size of the virus may be overcome by non-specific binding. It is proposed here that non-specific binding of HIV as the virus first randomly attaches to a host CD4+ T cell surface takes a large proportion (represented by ΔSa_non_specific) of the entropy loss of ΔSa_immob such that HIV can then bind specifically through Env:CD4 interactions at the relatively high temperature of the human body. The randomly attached virus “rolls into place” driven by n = 3 specific Env:CD4 interactions resulting in a further entropy loss (ΔSa_specific) as the virus particle takes up a specific orientation ready for viral entry. Non-specific attachment factors are all the more important for a GP/Cr system such as the HIV Env:CD4 interaction for which ΔCp is large and negative and diminishes binding at higher temperatures.
It is concluded that experimental data on ΔSa_immob should be obtained and antiviral therapeutic strategies, for example using zinc oxide nanoparticles for herpes simplex virus or neutralising antibodies to block virus binding, should focus not only on blocking the Cr-binding sites on the GP molecules themselves but also on targeting ΔSa_immob by increasing the size of the virus itself and so minimising host cell binding affinity at human body temperatures according to the model here. Bacterial cells are larger than viruses and ΔSa_immob would be expected to be more negative. Targeting ΔSa_immob may also have application as an alternative approach to antibiotics for bacterial pathogens when bacterial pathogenesis depends on attachment to cells. However, it should be noted that ΔSa_immob decreases logarithmically (i.e. slowly) with increasing size which may limit the practicability to bacteria.
Declaration of Competing Interest
None declared.
Acknowledgments
Acknowledgements
I thank the anonymous reviewer who helped me with the HIV binding data and greatly improved this manuscript.
Author Statement
I wrote the whole of this paper, did all the work and developed all the ideas. I have done this work in my spare time at home with no funding. I greatly enjoy doing this sort of paper.
Disclaimer
The views expressed in this paper are those of the author and not necessarily those of any organisations.
References
- Antoine T., Mishra Y.K., Trigilio J., Tiwari V., Adelung R., Shukla D. Prophylactic, therapeutic and neutralizing effects of zinc oxide tetrapod structures against herpes simplex virus type-2 infection. Antiviral. Res. 2012;96:363–375. doi: 10.1016/j.antiviral.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beniac D.R., Melito P.L., deVarennes S.L., Hiebert S., Rabb M.J., Lamboo L.L., Jones S.M., Booth T.F. The organisation of Ebola virus reveals a capacity for extensive modular polyploidy. PLoS ONE. 2012;7(1):e29608. doi: 10.1371/journal.pone.0029608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett A.J., Bushmaker T., Cameron K., Ondzie A., Niama F.R., Parra H.J., Mombouli J.-.V., Olson S.H., Munster V.J., Goldberg T.L. Diverse rna viruses of arthropod origin in the blood of fruit bats suggest a link between bat and arthropod viromes. Virology. 2018;1:64–72. doi: 10.1016/j.virol.2018.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandenberg O.F., Magnus C., Rusert P., Regoes R.R., Trkola A. Different infectivity of HIV-1 strains is linked to number of envelope trimers required for entry. PLoS Pathog. 2015;11(1) doi: 10.1371/journal.ppat.1004595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault A.C. Changing patterns of west Nile virus transmission: altered vector competence and host susceptibility. Vet. Res. 2009;40:43. doi: 10.1051/vetres/2009026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs J.A.G., Wilk T., Welker R., Krausslich H.G., D.Fuller Stephen. Structural organization of authentic, mature HIV-1 virions and cores. EMBO J. 2003;22:1707–1715. doi: 10.1093/emboj/cdg143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull R.A., Luciani F., McElroy K., Gaudieri S., Pham S.T., Chopra A., Cameron B., Maher L., Dore G.J., White P.A., Lloyd A.R. Sequential bottlenecks drive viral evolution in early acute hepatitis c virus infection. PLoS Pathog. 2011;7 doi: 10.1371/journal.ppat.1002243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull R.A., Eden J.-.S., Luciani F., McElroy K., Rawlinson W.D., White P.A. Contribution of intra- and interhost dynamics to norovirus evolution. J. Virol. 2012;86:3219–3229. doi: 10.1128/JVI.06712-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carneiro F.A., Bianconi M.L., Weissmuller G., Stauffer F., Da Poian A. Membrane recognition by vesicular stomatitis virus involves enthalphy-driven protein-lipid interactions. J. Virol. 2002;76:3756–3764. doi: 10.1128/JVI.76.8.3756-3764.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang G.-.Y., Geng H., Pancera M., Xu K., Cheng C., Acharya P., Chambers M., Druz A., Tsybovsky Y., Wanninger T.G., Yang Y., Doria-Rose N.A., Georgiev I.S., Gorman J., Joyce M.G., O'Dell S., Zhou T., McDermott A.B., Mascola J.R., Kwong P.D. Structure-based design of a soluble prefusion-closed HIV-1 env trimer with reduced CD4 affinity and improved immunogenicity. J. Virol. 2017;91 doi: 10.1128/JVI.02268-16. e02268-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daszak P., Zambrana-Torrelio C., Bogicha T.L., Fernandez M., Epstein J.H., Murray K.A., Hamilton H. Interdisciplinary approaches to understanding disease emergence: the past, present, and future drivers of Nipah virus emergence. Proc. Natl. Acad. Sci. USA. 2013;110(Supplement 1):3681–3688. doi: 10.1073/pnas.1201243109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Graaf M., Fouchier R.A.M. Role of receptor binding specificity in influenza a virus transmission and pathogenesis. EMBO J. 2014;33:823–841. doi: 10.1002/embj.201387442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey B., Pancera M., Svehla K., Shu Y., Xiang S.-.H., Vainshtein J., Li Y., Sodroski J., Kwong P.D., Mascola J.R., Wyatt R. Characterization of human immunodeficiency virus type 1 monomeric and trimeric gp120 glycoproteins stabilized in the CD4-bound state: antigenicity, biophysics, and immunogenicity. J. Virol. 2007;81:5579–5593. doi: 10.1128/JVI.02500-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitrov D.S., Hillman K., Manischewitz J., Blumenthal R., Golding H. Kinetics of soluble CD4 binding to cells expressing human immunodeficiency virus type 1 envelope glycoprotein. J. Virol. 1992;66:132–138. doi: 10.1128/jvi.66.1.132-138.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doranz B.J., Baik S.S., Doms R.W. Use of a gp120 binding assay to dissect the requirements and kinetics of human immunodeficiency virus fusion events. J. Virol. 1999;73:10346–10358. doi: 10.1128/jvi.73.12.10346-10358.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du X., Li Y., Xia Y.-.L., Ai S.-.M., Liang J., Sang P., Ji X.-.L., Liu S.-.Q. Insights into protein–ligand interactions: mechanisms, models, and methods. Int. J. Mol. Sci. 2016;17:144. doi: 10.3390/ijms17020144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson A.M., Henry B.I., Murray J.M., Klasse P.J., Angstmann C.N. Predicting first traversal times for virions and nanoparticles in mucus with slowed diffusion. Biophys. J. 2015;109:164–172. doi: 10.1016/j.bpj.2015.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fei Y., Sun Y.-.S., Li Y., Yu H., Lau K., Landry J.P., Luo Z., Baumgarth N., Chen X., Zhu X. Characterization of receptor binding profiles of influenza a viruses using an ellipsometry-based label-free glycan microarray assay platform. Biomolecules. 2015;5(1):480–481. doi: 10.3390/biom5031480. 498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey S., Marsh M., Günther S., Pelchen-Matthews A., Stephens P., Ortlepp S., Stegmann T. Temperature dependence of cell-cell fusion induced by the envelope glycoprotein of human immunodeficiency virus type 1. J. Virol. 1995;69:1462–1472. doi: 10.1128/jvi.69.3.1462-1472.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale P. Could bat cell temperature and filovirus filament length explain the emergence of ebola virus in mammals? predictions of a thermodynamic model. Transbound. Emerg. Dis. 2017;64:1676–1693. doi: 10.1111/tbed.12580. [DOI] [PubMed] [Google Scholar]
- Gale P. Using thermodynamic parameters to calibrate a mechanistic dose-response for infection of a host by a virus. Microbial Risk Anal. 2018;8:1–13. doi: 10.1016/j.mran.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale P. Towards a thermodynamic mechanistic model for the effect of temperature on arthropod vector competence for transmission of arbovirus. Microbial Risk Anal. 2019;12:27–43. doi: 10.1016/j.mran.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P., Mellors J., Kingsley L., Riddler S., Singh M.K., Schreiber S., Cronin M., Rinaldo C.R. High viral load in semen of human immunodeficiency virus type 1-infected men at all stages of disease and its reduction by therapy with protease and nonnucleoside reverse transcriptase inhibitors. J. Virol. 1997;71:6271–6275. doi: 10.1128/jvi.71.8.6271-6275.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada S., Akaike T., Yusa K., Maeda Y. Adsorption and infectivity of human immunodeficiency virus type 1 are modified by the fluidity of the plasma membrane for multiple-site binding. Microbiol. Immunol. 2004;48(4):347–355. doi: 10.1111/j.1348-0421.2004.tb03516.x. [DOI] [PubMed] [Google Scholar]
- Harrison S.C. Viral membrane fusion. Virology. 2015;479-480:498–507. doi: 10.1016/j.virol.2015.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan S.S., Sun C., Kim A.S., Watanabe Y., Chen C.-.L., Klose T., Buda G., Crispin M., Diamond M.S., Klimstra W.B., Rossmann M.G. Cryo-EM structures of eastern equine encephalitis virus reveal mechanisms of virus disassembly and antibody neutralization. Cell Rep. 2018;25:3136–3147. doi: 10.1016/j.celrep.2018.11.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houk E.J., Arcus Y.M., Hardy J.L., Kramer L.D. Binding of western equine encephalomyelitis virus to brush border fragments isolated from mesenteronal epithelial cells of mosquitoes. Virus Res. 1990;17:105–117. doi: 10.1016/0168-1702(90)90072-j. [DOI] [PubMed] [Google Scholar]
- Huitron-Resendiz S., Marcondes M.C.G., Flynn C.T., Lanigan C.M.S., Fox H.S. Effects of simian immunodeficiency virus on the circadian rhythms of body temperature and gross locomotor activity. Proc. Natl. Acad. Sci. USA. 2007;104:15138–15143. doi: 10.1073/pnas.0707171104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung H.-.I., Bowden S.J., Cooper A., Perham R.N. Thermodynamic analysis of the binding of component enzymes in the assembly of the pyruvate dehydrogenase multienzyme complex of Bacillus stearothermophilus. Protein Sci. 2002;11:1091–1100. doi: 10.1110/ps.4970102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney R.M., Huang C.Y.H., Whiteman M.C., Bowen R.A., Langevin S.A., Miller B.R., Brault A.C. Avian virulence and thermostable replication of the North American strain of west Nile virus. J. Gen. Virol. 2006;87:3611–3622. doi: 10.1099/vir.0.82299-0. [DOI] [PubMed] [Google Scholar]
- Klasse P.J. The molecular basis of HIV entry. Cell Microbiol. 2012;14:1183–1192. doi: 10.1111/j.1462-5822.2012.01812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhmann S.E., Platt E.J., Kozak S.L., Kabat D. Cooperation of multiple CCR5 coreceptors is required for infections by human immunodeficiency virus type 1. J. Virol. 2000;74:7005–7015. doi: 10.1128/jvi.74.15.7005-7015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leendertz S.A.J. Testing new hypotheses regarding ebolavirus reservoirs. Viruses. 2016;8:30. [Google Scholar]
- Liu Q., Acharya P., Dolan M.A., Zhang P., Guzzo C., Lu J., Kwon A., Gururani D., Miao H., Bylund T., Chuang G.-.Y., Druz A., Zhou T., Rice W.J., Wigge C., Carragher B., Potter C.S., Kwong P.D., Lusso P. Quaternary contact in the initial interaction of CD4 with the HIV-1 envelope trimer. Nat. Struct. Mol. Biol. 2017;24:370–378. doi: 10.1038/nsmb.3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Zhang Z., Lai Z., Zhou T., Jia Z., Gu J., Wu K., Chen X.-.G. Temperature increase enhances Aedes albopictus competence to transmit Dengue virus. Front. Microbiol. 2017;8:2337. doi: 10.3389/fmicb.2017.02337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu G., Hu Y., Wang Q., Qi J., Gao F., Li Y., Zhang Y., Zhang W., Yuan Y., Bao J., Zhang B., Shi Y., Yan Y., Gao G.F. Molecular basis of binding between novel human coronavirus MERS-COV and its cellular receptor CD26. Nature. 2013;500:227–231. doi: 10.1038/nature12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mammen M., Choi S.-.K., Whitesides G.M. Polyvalent interactions in biological systems: implications for design and use of multivalent ligands and inhibitors. Angew. Chem. Int. Ed. 1998;37:2754–2794. doi: 10.1002/(SICI)1521-3773(19981102)37:20<2754::AID-ANIE2754>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Moore J.P., Klasse P.J. Thermodynamic and kinetic analysis of sCD4 binding to HIV-1 virions and of gp120 dissociation. AIDS Res. Hum. Retroviruses. 1992;8:443–450. doi: 10.1089/aid.1992.8.443. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay S., Kim B.S., Chipman P.R., Rossmann M.G., Kuhn R.J. Structure of west Nile virus. Science. 2003;302:248. doi: 10.1126/science.1089316. [DOI] [PubMed] [Google Scholar]
- Mullens B.A., Gerry A.C., Lysyk T.J., Schmidtmann E.T. Environmental effects on vector competence and virogenesis of bluetongue virus in Culicoides interpreting laboratory data in a field context. Vet. Ital. 2004;40:160–166. [PubMed] [Google Scholar]
- Myszka D.G., Sweet R.W., Hensley P., Brigham-Burke M., Kwong P.D., Hendricksoni W.A., Wyatt R., Sodroski J., Doyle M.L. Energetics of the HIV gp120-CD4 binding reaction. Proc. Natl. Acad. Sci. USA. 2000;97:9026–9031. doi: 10.1073/pnas.97.16.9026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nason E.L., Rothagel R., Mukherjee S.K., Kar A.K., Forzan M., Prasad B.V.V., Polly Roy P. Interactions between the inner and outer capsids of bluetongue virus. J. Virol. 2004;78:8059–8067. doi: 10.1128/JVI.78.15.8059-8067.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngai K.L.K., Chan M.C.W., Chan P.K.S. Replication and transcription activities of ribonucleoprotein complexes reconstituted from avian H5N1, H1N1pdm09 and H3N2 influenza A viruses. PLoS ONE. 2013;8(6):e65038. doi: 10.1371/journal.pone.0065038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nifong R.L., Gillooly J.F. Temperature effects on virion volume and genome length in dsDNA viruses. Biol. Lett. 2016;12 doi: 10.1098/rsbl.2016.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Shea T.J., Ctyan P.M., Cunnignham A.A., Fooks A.R., Hayman D.T.S., Luis A.D., Peel A.J., Plowright R.K, Wood J.L.N. Bat flight and zoonotic viruses. Emerg. Infect. Dis. 2014;20:741–745. doi: 10.3201/eid2005.130539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saez A.M., Weiss S., Nowak K., Lapeyre V., Zimmermann F., Dux A., Kuhl H.S., Kaba M. Investigating the zoonotic origin of the west African Ebola epidemic. EMBO Mol. Med. 2015;7:17–23. doi: 10.15252/emmm.201404792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp P.M., Shaw G.M., Hahn B.H. Simian immunodeficiency virus infection of Chimpanzees. J. Virol. 2005;79:3891–3902. doi: 10.1128/JVI.79.7.3891-3902.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakar M.R., Abraham P.R., Arora S., Balakrishnan P., Bandyopadhyay B., Joshi A.A., Devi K.R., Vasanthapuram R., Vajpayee M., Desai A., Mohanakrishnan J., Narain K., Ray K., Patil S.S., Singh R., Singla A., Paranjape R.S. Establishment of reference CD4+ t cell values for adult Indian population. AIDS Res. Ther. 2011;8:35. doi: 10.1186/1742-6405-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilen C.B., Tilton J.C., Doms R.W. HIV: cell binding and entry. in additional perspectives on HIV. In: Bushman Frederic D., Nabel Gary J., Swanstrom Ronald., editors. Vol. 2012. 2012. (Cold Spring Harbor Perspectives in Medicine). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong X., Coombs P.J., Martin S.R., Liu J., Xiao H., McCauley J.W., Locher K., Walker P.A., Collins P.J., Kawaoka Y., Skehel J.J., Gamblin S.J. Receptor binding by a ferret-transmissible H5 avian influenza. Nature. 2013;497:392–396. doi: 10.1038/nature12144. [DOI] [PubMed] [Google Scholar]
- Xu K., Chan Y.-.P., Rajashankar K.R., Khetawat D., Yan L., Momchil V., Kolev M.V., Broder C.C., Nikolov D.B. New insights into the Hendra virus attachment and entry process from structures of the virus G glycoprotein and its complex with ephrin-B2. PLoS ONE. 2012;7:e48742. doi: 10.1371/journal.pone.0048742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X., Kurteva S., Ren X., Lee S., Sodroski J. Stoichiometry of envelope glycoprotein trimers in the entry of human immunodeficiency virus type 1. J. Virol. 2005;79:12132–12147. doi: 10.1128/JVI.79.19.12132-12147.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Cao L., Ling H., Dang M., Sun Y., Zhang X., Chen Y., Zhang L., Su D., Wang X., Rao Z. TIM-1 acts a dual-attachment receptor for Ebolavirus by interacting directly with viral GP and the PS on the viral envelope. Protein Cell. 2015;6(11):814–824. doi: 10.1007/s13238-015-0220-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Boyce M., Bhattacharya B., Zhang X., Schein S., Roy P., Zhou Z.H. Bluetongue virus coat protein VP2 contains sialic acid-binding domains, and VP5 resembles enveloped virus fusion proteins. PNAS. 2010;107:6292–6297. doi: 10.1073/pnas.0913403107. [DOI] [PMC free article] [PubMed] [Google Scholar]