Abstract
Influenza A virus (IAV) is a pulmonary pathogen, responsible for significant yearly morbidity and mortality. Due to the absence of highly effective antiviral therapies and vaccine, as well as the constant threat of an emerging pandemic strain, there is considerable need to better understand the host–pathogen interactions and the factors that dictate a protective versus detrimental immune response to IAV. Even though evidence of IAV-induced cell death in human pulmonary epithelial and immune cells has been observed for almost a century, very little is known about the consequences of cell death on viral pathogenesis. Recent study indicates that both the type of cell death program and its kinetics have major implications on host defense and survival. In this review, we discuss advances in our understanding of cell death programs during influenza virus infection, in hopes of fostering new areas of investigation for targeted clinical intervention.
Keywords: Influenza A virus, Cell death program, Pulmonary macrophages, Alveolar epithelial cells, Apoptosis, Necroptosis
1. Introduction
Influenza viruses cause the most recurring respiratory disease in humans, with outbreaks likely occurring since at least the Middle Ages [1]. Present estimates indicate that each year, seasonal influenza affects 5–10% of the world's population, resulting in 3–5 million cases of severe illness and between 250 000 to 500 000 deaths [2]. In addition to seasonal outbreaks, influenza pandemics sporadically emerge, causing markedly higher mortality. In 1918, the worst pandemic in recorded history caused more than 50 million deaths worldwide [3]. Since then, three other pandemics have occurred: first in 1957, then again in 1968 and finally in 2009 [4]. Currently, there are major concerns surrounding the emergence of the new highly pathogenic avian influenza (HPAI) viruses of H5N1, H7N9, H10N8, or the more recent H5N8—the only HPAI strain to cross from Eurasia to America [5], [6], [7], [8], [9].
One of the key characteristics of highly infectious IAV and HPAI viruses is that they are poorly glycosylated and, thus, able to bypass the upper airway defense mechanisms to reach the lower respiratory tract, leading to pneumonia [10]. Histopathologic studies of influenza autopsies from 1918 outline the key changes characteristic of severe IAV viral pneumonia. These include “… varying degrees of acute intra-alveolar edema and/or hemorrhage, and diffuse alveolar damage in addition to necrotizing bronchitis and bronchiolitis” [11]. Similarly, in the recent 2009 H1N1 outbreak, viral antigen could be found in the alveolar space, suggesting pandemic strains of IAV have the capacity to infect distal areas of the lung and directly cause alveolar damage. These occurrences collectively predispose to a clinical condition termed acute respiratory distress syndrome (ARDS), which may occur as a complication of primary viral pneumonia [12]. ARDS is precipitated by cell death among the epithelial–endothelial barrier (EEB) of the distal lung, barrier rupture, fluid leakage into the alveolar lumen and respiratory insufficiency. Hence, understanding and disrupting the strategies employed by the virus to damage the lower airways is critical in preserving pulmonary architecture.
The most distal structure of the lung, the alveolus, is constantly patrolled by alveolar macrophages (AMφ) and is delimited by the EEB—a bi-cellular layer composed of type I and type II alveolar epithelial cells (AEC-I and AEC-II), facing the air space, and endothelial cells that form the pulmonary capillaries. The identification of the infective target cells of severe pulmonary viruses within the alveolus is critical in evaluating the potential effects of cell damage on lung function. For example, ex vivo infection of human lungs with Middle East respiratory syndrome coronavirus (MERS-CoV)—a recent zoonotic virus with a fatality rate of 35–50% in humans—showed that AEC-I, AEC-II and endothelial cells can all be infected and killed [13], [14], [15]. In addition, while MERS-CoV productively replicates in human macrophages and T lymphocytes, it is also cytotoxic in these cells [16], [17]. Interestingly, the tropism of the virus appears to have a significant impact on severity of disease. For instance, in comparison to MERS-CoV that infects both structural cells and leukocytes and causes high mortality, severe acute respiratory syndrome (SARS)-CoV only infects structural cells, causing less mortality [17]. In IAV infection, a number of reports identify AEC-II as the primary replicative niche in the human lung for highly pathogenic strains, while low-pathogenicity strains fail to penetrate the lower airways [18], [19], [20], [21], [22]. HPAI also infects human endothelial cells in vitro and some evidence suggests that infection of the endothelium may occur in vivo [23], [24]. In addition, IAV antigens are found in human AMφ and the virus can productively infect and kill human macrophages [18], [19], [10], [23], [21], [25], [26], [27]. Thus, similar to the highly pathogenic MERS-CoV, highly virulent IAV shows tropism for both human alveolar structural cells and leukocytes, highlighting the severity of pandemic strains.
AMφ within the airways are the first leukocytes to encounter the majority of pulmonary pathogens and their initial response to infection is critical in “setting the tone” and orchestrating an effective immune response. Studies examining how AMφ are altered following pulmonary viral infection suggest that the loss of EEB integrity, reduction in regulatory mediators and activation of multiple pattern-recognition receptors (PRR) lead to these cells becoming pro-inflammatory, rather than regulatory [28]. Upon infection with IAV, AMφ initiate the immune response by producing chemokines and cytokines, including type I interferons (IFN-I; primarily composed of IFN-α/β), as well as instructing adaptive immune responses [25], [29]. If adequately regulated, these responses lead to effective immunity, clearance of the virus with minimal immunopathology and return to pulmonary homeostasis. If dysregulated, however, these responses can have dramatically deleterious effects, marked by impaired viral clearance, increased immunopathology and enhanced susceptibility to infection. Thus, pulmonary immune responses must be tightly regulated to effectively eliminate viruses that reach the distal airways, while minimizing immunopathology in order to maintain optimal gas exchange [29].
The death of host cells as a result of infection has been recognized for over a century and it is now understood that pathogen-induced cell death may occur through a variety of complex mechanisms. Initially, cell death was discussed in dichotomy as either: (1) apoptosis, considered an active—or programmed—process that preserves the plasma membrane and leads to the deletion of cells with little tissue disruption and no inflammation; or (2) necrosis, a passive form of cell death leading to complete disruption of the plasma membrane and spillage of cellular contents, causing inflammation and tissue damage [30]. However, this simplification of the cell death program has altered considerably over the last couple of decades. There are now several distinct forms of programmed cell death that have been described in addition to apoptosis, including pyroptosis, paraptosis and necroptosis [31]. Interestingly, some of these cell death modalities have been observed in autopsies of IAV-infected humans, particularly HPAI cases [11], [32]; yet, the consequences of these cell death programs on host immunity and the pathogenesis of IAV are not fully understood. Therefore, a more complete characterization of the forms of cell death occurring in IAV infected lungs may define why certain cell types are more, or less, susceptible to IAV-induced cell death and how this impacts viral propagation. Furthermore, different forms of cell death may have distinct consequences on the virulence of IAV strains by differentially modulating the immune response. This suggests that regulated modulation of cell death programs during IAV infection may be an appealing target for anti-IAV therapies.
In this review, we focus on the current state of knowledge of cell death during influenza infection and explore research avenues that aim to dissect cell death programs, as well as their ensuing consequences in the pathogenesis of this threatening virus. Considering the mechanisms of cell death have been extensively reviewed elsewhere [33], [34], herein we focus on severe influenza infection and the immunological effects of influenza-induced cell death in the lung structural cells (e.g. epithelial cells) as well as immune cells (e.g. macrophages). Finally, we suggest that manipulation of specific cell death programs at different stages of infection may offer avenues for novel therapy to IAV by both sequestering viral replication and promoting host resistance mechanisms through immunomodulation.
2. Cell death in IAV-infected pulmonary epithelial cells
IAV utilizes epithelial cells as its primary replicative site and all pulmonary epithelial cells are permissive to infection and subsequent replication. However, proximity of the replication to distal portions of the lung is strongly associated with an increase in virulence capacity of IAV strains. For example, seasonal influenza strains, or those of low pathogenicity, replicate primarily in the upper airways and are rapidly killed in the pharynx and proximal lung by host resistance mechanisms, causing minor acute disease. On the contrary, HPAI and highly pathogenic H1N1 strains bypass immune mechanisms of the upper airways to replicate in the distal portions of the lung and this distal tropism is highly correlated with primary viral pneumonia and mortality [11]. Altered tropism of IAV to the lower airways is thought to be mediated by two mechanisms. First, IAV infects cells by its hemagglutinin (HA) binding to terminal sialic acids on the plasma membrane of cells, attached either via an α2,3 or α2,6 linkage. Both α2,3 and α2,6 linkages are present throughout the human lung; however, preferential binding of α2,3 linked residues by IAV hemagglutinin favors more distal and severe infections. Second, glycosylation of IAV hemagglutinin is inversely correlated with pathogenicity, as highly glycosylated hemagglutinins are more efficiently trapped and cleared from the upper airways by ciliary motion [35], while poorly glycosylated IAV bypass this host defense mechanism and access the lower airways [35]. For instance, the pandemic 1918 H1N1 strain exhibited only 1 glycosylation site on its hemagglutinin protein and HPAI strains are known to preferably bind α2,3 residues, due to their enhanced expression on avian epithelial cells.
In the lower airways, it was shown in a human lung explants model that approximately 90% of influenza positive cells are AEC-II cells, with a minor contribution of AMφ and other cell types [21]. Interestingly, IAV replication is enhanced in AEC-II compared to bronchial epithelial cells [36]. Therefore, highly pathogenic strains of IAV have mechanisms to reach their preferred replicative niche in AEC-II in the distal lung, suggesting that maintenance of pulmonary epithelial cells is beneficial to the virus in promoting its replication. However, considering that IAV is also lytic in epithelial cells of humans [37] and mice [38] hints that at certain time points after infection, cell death may be involved in preventing or facilitating viral propagation, escape and reinfection. Therefore, the consequences of cell death in structural cells, and in particular AEC-II, on host immunity to IAV must diverge depending on the kinetics of the infection.
2.1. Apoptosis in IAV-infected lung epithelial cells
Apoptosis comes from the ancient Greek word meaning “falling off” and is the most characterized form of programmed cell death. Proceeding in a non-inflammatory manner, apoptosis likely evolved to meet the growing demand to remove aging or damaged cells from the body as more complex and multicellular organisms appeared and, as a result, the apoptotic machinery remains evolutionarily conserved. Indeed, at homeostasis in an adult human, it is estimated that between 100 and 200 billion cells are being cleared daily via apoptosis [39]. This number can then augment dramatically in developmental stages and aging. Thus, the physiological demand for cellular turnover in a non-inflammatory manner is essential to maintain homeostasis.
The signature of early apoptosis involves condensing of chromatin within the nucleus, compartmentalization of cellular organelles and the shrinking of the cell membrane. Ultimately, these compartments bleb off in the form of apoptotic bodies, which are phagocytosed and degraded by macrophages and other phagocytic cells in a process known as efferocytosis [39]. Importantly, the cell membrane of apoptotic cells remains intact throughout and the cell shrinks rather than ruptures, as appearing in necrotic forms of cell death. Thus in apoptotic cells, there is no leakage of cytosolic contents to initiate an inflammatory response [33]. There are two major pathways that lead to apoptosis: intrinsic and extrinsic, both of which primarily converge on a family of proteins called caspases that cleave cellular substrates and lead to the morphological signature of apoptosis [40]. Intrinsic apoptosis is initiated by the mitochondrion in response to internal cellular stress and involves activation of caspase 9 by cytochrome c. Extrinsic apoptosis, on the other hand, is dependent upon death ligands of the TNF superfamily like TRAIL or FasL binding their cognate cell surface receptors and the subsequent activation of caspase 8 [41], [42].
In addition to its physiological role, apoptosis is involved in promoting resistance or susceptibility to intracellular pathogens. For example, virulent Mycobacterium tuberculosis (Mtb) contains an anti-apoptotic gene (nuoG) that diminishes both innate and adaptive immunity to promote the bacterial growth [43]. In contrast to Mtb, apoptosis induced by Listeria monocytogenes is an immune evasion strategy, allowing the bacteria to disseminate [44]. Thus, it appears that apoptosis can be both protective and detrimental to the host depending on the pathogen. Interestingly, both extrinsic and intrinsic pathways of apoptosis were shown to be activated in influenza-infected cells [45]. This observation is well established, being described in human autopsies for almost a century, beginning with the 1918 pandemic, where pronounced epithelial desquamation, hyalination and sloughing were noted [37]. Experimentally, apoptosis of IAV-infected epithelial cells was shown to be dependent upon viral replication, as an inactivated virus failed to induce apoptosis in mice [46] and human cells [47]. Moreover, the magnitude of epithelial cell apoptosis was positively associated with IAV strain pathogenicity in vivo [32], [23], [48] and in vitro [38], [49] in both mice and humans. However, whether apoptosis promotes host resistance or IAV dissemination remains to be determined.
Logically, apoptosis of epithelial cells could represent a resistance strategy to IAV, as it eliminates the intracellular niche required for viral replication. Support for the protective capacity of apoptosis is that critical host antiviral factors actively induce epithelial cell apoptosis. Upon viral infection, IFN-I (IFN-β) is rapidly produced, following recognition of the viral genome by pattern-recognition receptors (PRR). In IAV infection, RNA sensing is predominantly mediated by the cytosolic retinoic acid-inducible gene (RIG-I), which interacts with the mitochondrial antiviral signaling protein (MAVS) at the mitochondrial outer-membrane to initiate IFN-I production mainly via the transcription factor interferon regulatory factor 3 (IRF3) (reviewed in Ref. [50]). IFN-I then signals through a heterodimeric receptor complex of IFNαR1 and 2, leading to sustained IFN-I (largely IFN-α) production and an upregulation of a large subset of genes, together termed interferon stimulated genes (ISGs). ISGs then serve to halt viral replication through both direct or indirect mechanisms. Interestingly, both IFN-I and ISGs have been shown to induce apoptosis. Following IAV infection, IFN-I signaling activates caspase-dependent apoptosis in AEC-II cells [51], and the pharmacological inhibition of these caspases blocks apoptosis and enhances viral replication. Additionally, several classical apoptosis proteins, including caspase 8 and TRAIL, are ISGS upregulated by IFN-I signaling. Thus, IAV sensing causes the release of IFN-I that induces epithelial cell apoptosis directly through caspase activation downstream of the IFNαR1/2 complex, and indirectly by promoting the transcription of pro-apoptotic ISGs.
Other ISGs have been equally implicated in promoting apoptosis in IAV-infected cells as an antiviral mechanism. For example, Protein Kinase R (PKR) is an ISG known to inhibit IAV replication through a variety of mechanisms. PKR can directly sense dsRNA generated during viral replication to induce Fas expression and FADD-dependent apoptosis [52], as well as inhibit host and viral protein translation through the phosphorylation of eIF2α [53] in IAV-infected cells [54]. Moreover, PKR has been shown to increase IFN-I production in fibroblasts directly in response to another RNA virus: Semliki Forest virus [55]. Thus, it appears PKR and other ISGs contribute to antiviral immunity by promoting IFN-I responses, restricting viral protein translation and inducing apoptosis.
In addition to being directly antiviral, apoptosis also protects against IAV infection through the resolution of the immune response. In response to HPAI, bronchiolar epithelial cell apoptosis limits excess pro-inflammatory cytokine (ie. TNF) release to dampen immunopathology and avoid the onset of ARDS [56]. Furthermore, a recent study has implicated club cells, a subset of bronchiolar epithelial cells, in augmenting immunopathology to an H1N1 IAV virus, by failing to undergo apoptosis following viral clearance [57]. Therefore, the protective capacity of apoptosis in structural cells is both antiviral and immunomodulatory.
Given the importance of apoptosis in antiviral immunity, it is not surprising that IAV has encoded factors to block its induction. The principal IAV virulence factor, non-structural protein 1 (NS1), is rapidly transcribed upon infection and is the first protein expressed in infected cells. NS1 blocks early apoptosis in epithelial cells and fibroblasts by inhibiting IFN-I induction [58] and activating the host pro-survival PI3K/Akt pathway to facilitate viral replication [59]. Importantly, these functions are critical in viral fitness, as strains lacking a functional NS1 are severely impaired in their virulence. Taken together, all the above studies highlight the importance of apoptosis of structural cells in promoting immunity to influenza, by limiting the intracellular niche necessary for viral replication.
However, the notion that apoptosis solely represents a host-driven antiviral strategy is confounded by the fact that IAV encodes both anti- and pro-apoptotic factors. For example, H5N1 NS1 facilitates airway epithelial apoptosis [60], [49], suggesting a strain- or expression level-specific role for this protein in IAV pathogenesis. Furthermore, recent study has characterized H1N1 IAV nucleoprotein (NP) as a pro-apoptotic viral protein in human airway epithelial cells [61] that targets the host's anti-apoptotic protein AP15 [62]. In fact, host apoptotic machinery has been shown to be essential in promoting new virion production in epithelial cells in vitro [63], [64], [65], in a caspase-3- [66] and -9-dependent manner [67], and in vivo by IAV-manipulation of annexin-A1 [68]. These findings outline IAV as an effective regulator of the host's apoptotic machinery in structural cells, capable of both inducing and blocking apoptosis to further its pathogenesis.
The paradoxical role of apoptosis in immunity to IAV, which appears to both prevent and permit viral dissemination, can perhaps be explained by the kinetics of the apoptotic response in epithelial cells (Fig. 1 ). Immediately upon infection, it is beneficial for IAV to block epithelial cell apoptosis to avoid destroying its replicative niche and this is primarily mediated by viral NS1. Early blockage of apoptosis by IAV is counteracted by host mechanisms, such as IFN-I signaling, to induce apoptosis and resist viral replication [69]. Yet, following initial replication cycles, at later time points, IAV must activate apoptotic pathways to generate new infectious virions, promote budding at the cell surface and facilitate subsequent rounds of infection in neighboring cells. Thus, pharmacological inhibition of apoptosis in humans during the later stages of infection may offer appealing therapeutic avenues, either by blocking pro-apoptotic pathways [65] or enhancing anti-apoptotic proteins [64]. Interestingly, neutralization of pro-apoptotic TRAIL or Fas signaling post-IAV infection in AEC-II cells decreased IAV load [70]. Similarly, mice treated with decoy Fas in vivo to block FasL signaling were protected from lethal IAV infection, when compared to untreated mice [71].
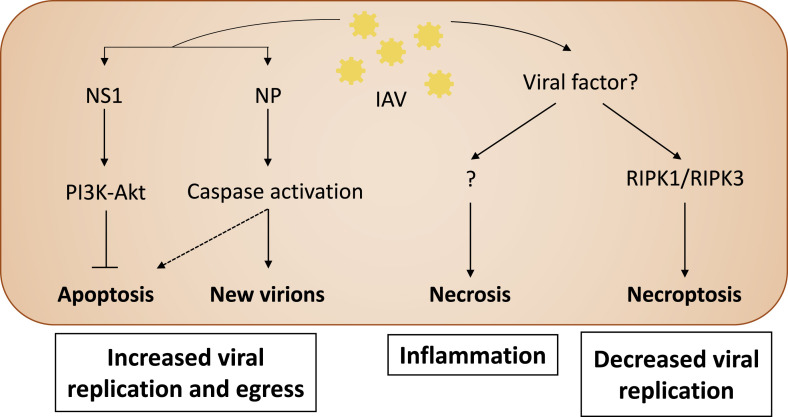
Fig. 1.
Activation of cell death pathways in IAV-infected epithelial cells. Following IAV infection, the viral protein NS1 inhibits apoptosis by activating the PI3K/Akt pro-survival pathway, therefore leading to increased viral replication. Later, viral proteins, predominantly NP, activate caspase signaling to facilitate viral protein packaging and virion production, leading to viral egress and consequentially apoptosis. Unknown viral factors induce necrosis through unelucidated mechanisms, causing enhanced inflammation. Finally, IAV-infected epithelial cells undergo necroptosis, a programmed form of necrosis involving the proteins RIPK3 and MLKL. By eliminating the natural replicative niche of the virus, necroptosis helps limit viral replication. Solid arrows indicate both direct viral and host effects, while dashed arrows indicate indirect by-products.
Our understanding of the interplay between influenza, host apoptotic machinery and resistance mechanisms has increased exponentially recently. However, much of our knowledge still derives from study in vitro using human or mouse cells and, thus, the exact effects of these pathways on disease outcome remain to be determined.
2.2. Necrosis in IAV-infected epithelial cells
Like apoptosis, the observation that IAV causes necrosis in epithelial cells has long been established. Yet, the impact of IAV-induced epithelial cell necrosis on the host immune response, and the factors—viral or host-derived—involved in this process are just beginning to become known. Canonically, necrosis was considered a passive form of cell death associated with increased injury or disease severity. However, it is now well established that many forms of necrosis are, in fact, programmed. Necrotic cell death is delineated from apoptosis by a disruption of the cell membrane and spilling out of cytosolic contents that act as danger-associated molecular patterns (DAMPs). These DAMPs are sensed by neighboring cells, resulting in a robust inflammatory response [72], [73], thus, generating a potential positive feedback loop of tissue damage and immunopathology. The observation that HPAI [11] and pandemic H1N1 often induce necrosis in epithelial cells, while seasonal H3N2 appears only to cause it in immune compromised hosts [48], may at least partly explain the association between severity of disease and necrosis of the epithelium. Moreover, other strains of highly pathogenic viruses such as dengue virus [74] or MERS-CoV [75] appear to induce considerable necrosis in epithelial cells to promote viral replication and propagation, while less virulent viruses like rhinovirus, or SARS-CoV induce limited or no necrosis [75], [76]. In vitro, H1N1 IAV induces necrosis in human lung bronchiolar epithelial cells, coupled with massive release of proinflammatory cytokines and neutrophil chemoattractant CXCL8, which is highly suggestive of a link between necrosis of the epithelium and ARDS [77]. Collectively, these observations promote the notion that epithelial cell necrosis is detrimental to the host and is consequential of severe infection.
The most characterized form of programmed necrosis is RIPK3-dependent programmed necrosis (termed necroptosis). Necroptosis is dependent upon the formation of the necrosome, which consists of RIPK1 and RIPK3, interacting through their RIP homotypic interaction motifs (RHIM). Typically, RIPK1 and RIPK3 are cleaved by caspase-8, causing their inactivation and leading to extrinsic apoptosis. However, when caspase-8 activity is compromised, the necrosome is activated to induce necroptosis. Known mediators downstream of the necrosome include mixed lineage kinase domain like pseudokinase (MLKL). MLKL is a substrate for RIPK3 and induces necroptosis by a combination of the assembly of a pore-forming complex at the plasma membrane, or as a platform for Ca2+-mediated necrosis [78]. Although the exact executioner mechanisms of necroptosis remain unknown, recent study has implicated the plasma membrane repair machinery ESCRT III as a potential mediator [79].
Necroptosis regulates a variety of inflammatory processes, including ischemic heart disease, bacterial infection and embryogenesis [80]. Interestingly, there is accumulating evidence for a role of necroptosis in promoting immunity to viral infection. Seminal work showed necroptosis to be essential in antiviral defense, as Ripk3 −/− mice succumbed to vaccinia virus infection [81]. Moreover, herpes simplex viruses (HSV-1/2) and murine cytomegalovirus (MCMV) encode inhibitors of necroptosis, UL39 and M45 respectively, suggesting that viruses may block necroptosis as part of their pathogenesis [82], [83]. Although no IAV inhibitors of necroptosis have yet been identified; most recently, RIPK3-dependent necroptosis of murine fibroblasts and alveolar epithelial cells was demonstrated to be critical in promoting IAV clearance from the lungs and, as a result, RIPK3-deficient mice were highly susceptible to IAV infection coupled with enhanced viral loads [84]. Thus, this study hints at a protective role for necroptosis in immunity to IAV. However, human studies are required to investigate the potential clinical targeting of the necroptotic pathway in protection against IAV infection.
2.3. Other forms of cell death in IAV-infected lungstructural cells
Certainly, apoptosis and, more recently, necrosis have dominated study of IAV-mediated cell death. However, the role of other forms of cell death in immunity to infectious diseases, such as IAV, is beginning to be recognized. Pyroptosis is a form of rapid inflammatory cell death with cell membrane rupture and DNA damage, which is dependent upon caspase-1 and certain NOD-like receptors. Pyroptosis is coupled with proinflammatory IL-1β and IL-18 release from pyroptotic cells, which contributes in part to its inflammatory nature [85]. Caspase-1 activation and subsequent cytokine release induced by IAV in murine lung fibroblasts has been shown to inhibit viral pathogenesis [86], [87]. Yet, whether caspase-1 activation in these models led to pyroptosis, or rather defined a pyroptosis-independent role for caspase-1 was not carefully elucidated. Thus, more study of the role of caspase-1 activation and pyroptosis in immunity to IAV is needed.
Although epithelial cells constitute the major replicative niche for IAV, the lung is a complex organ and thus other structural cells can be infected with IAV. Pulmonary fibroblasts are the most substantial subset of structural cells in the lung interstitium, playing a significant role in the repair process to injurious exposure and pulmonary inflammatory disorders, such as asthma and COPD [88]. Fibroblasts are used extensively in IAV studies as a model of lung structural cells. As in epithelial cells, fibroblasts are sensitive to both IAV-induced apoptosis [58] and necroptosis [84] in vitro. However, the contribution of fibroblasts in immunity to IAV infection is not well understood. Whether fibroblasts are a target for IAV infection in vivo and/or whether their response is analogous to, or completely independent of, epithelial cells, requires further investigation. Understanding the role of fibroblasts in the pathogenesis of IAV may provide additional targeted therapy against IAV infection.
Similarly, endothelial cells represent a substantial compartment of the lung and in vitro infection of human endothelial cells led to productive IAV replication and increased vascular leak, mediated by apoptosis [89], particularly upon infection with HPAI (e.g. H5N1) [90]. HPAI has been shown to disseminate from the lung systemically upon infection in mice [91]. This has equally been observed in humans, where viral RNA was found in multiple organs, including the brain and placenta, of fatal cases of H5N1 [92], [93]. The ability of HPAI viruses to disseminate to other tissues is predominately mediated by changes to the cleavage sites of the viral HA protein, which is essential for viral entry into cells. In the case of low virulence seasonal strains of IAV, HA cleavage occurs at a single basic arginine by trypsin-like proteases found exclusively in cells of the respiratory tree and gastrointestinal tract. On the other hand, HPAI HA proteins contain polybasic cleavage sites that permit cleavage by furin proteases that are ubiquitously expressed. Thus, this allows HPAI strains to disseminate and cause systemic infection [94]. Additionally, pandemic and highly virulent strains of the virus, including HPAI and the 1918 H1N1 strain, are known to completely exhaust the replicative niche of epithelial cells of the lung over the course of infection as a by-product of overly exuberant replication and failure of immune response to control viral propagation. Thus, it is appealing to associate the infection of endothelial cells by HPAI viruses with subsequent systemic dissemination, made possible by the polybasic cleavage sites. However, this is complicated by the fact that no virus was found in endothelial cells of fatal cases of H5N1 infection [93], yet virus was found in hyaline membranes and endothelial cells of fatal cases of the 2009 H1N1 pandemic, where dissemination to other organs was not noted [23]. As there is no known evolutionary advantage for IAV to disseminate to other organs, a greater level of study is required to confirm what role infection of endothelial cells in humans plays and whether endothelial cell death is a pro-host or pro-pathogen strategy.
3. Cell death in pulmonary macrophages
During influenza virus infection, the pulmonary inflammatory response is characterized by early infiltration of leukocytes, including neutrophils and mononuclear cells and later by adaptive immune lymphocytes [95], [96]. Autopsy reports of humans infected with HPAI and pathogenic strains of H1N1 exhibited severe pulmonary leukopenia, which together constituted important clinical features of severe infection and fatal cases [97], [32]. Importantly, this leukopenia was mainly contributed to IAV-induced death of these cells at the site of infection, rather than failed recruitment or effector function in the lung [98], [99], [100]. Interestingly, pulmonary IAV infection has also been shown to have profound effects on bone marrow hematopoiesis in an IFN-I-dependent manner [101]. Thus, the observed leukopenia could alternatively be explained by other mechanisms, such as exhaustion of the bone marrow hematopoietic stem cells due to severe infection. Hematopoietic stem cell exhaustion is a phenomenon often observed during chronic bacterial or viral infections [102], [103], but remains poorly characterized in IAV infections. Nevertheless, these findings illustrate the importance of preserved leukocyte viability and function in host defense to highly pathogenic strains of IAV and activation of the cell death program in these cells may represent a strategy of immune evasion by IAV. Although IAV has been shown to contribute to cell death in the majority of leukocytes—including neutrophils, dendritic cells and lymphocytes—this review will focus on cell death in pulmonary monocyte/macrophages, given their critical role in the initial response to the infection.
Pulmonary macrophage populations change considerably during IAV infection. At homeostasis, tissue resident AMφ constitute the vast majority of cells in the airways and are the first leukocytes to encounter the virus, following replication in epithelial cells [29]. AMφ can then be readily infected [104], [105] and activated to secrete a spectrum of cytokines and chemokines that orchestrate both innate and adaptive immune responses to IAV and other pulmonary viral infections [106], [25], [107]. Over the course of infection, AMφ populations are diminished, while inflammatory monocyte-derived macrophages (MD-Mφ, also called exudate macrophages) expand and then contract during the resolution phase [108]. Both AMφ and MD-Mφ have been linked to host protection and disease pathogenesis depending on the magnitude of activation of the immune response, which is directly associated with disease tolerance [108]. Invariably, loss of AMφ causes increased susceptibility to infection, due to reduced production of antiviral IFN-I (mainly IFN-β) leading to uncontrolled viral replication and increased immunopathology [106], [25], [107], [109]. Thus, AMφ represent a logical target for IAV to induce cell death and, indeed, several studies have reported early apoptosis post-infection in AMφ [110], [111], [112]. Similarly, recruited Mφ are highly permissive to IAV infection and susceptible to IAV-induced cell death [26], [113]. Collectively, these findings suggest that in contrast to the biphasic role of epithelial cell apoptosis in preventing or promoting pathogenesis, highly virulent IAV rapidly infects and induces early death in pulmonary Mφ to suppress antiviral responses.
3.1. Apoptosis in IAV-infected macrophages
Apoptosis occurs in Mφ during IAV infection and can be either triggered intrinsically by viral proteins or activated extrinsically by host factors in the pulmonary microenvironment. While the induction of apoptosis by viral proteins has been studied extensively in structural cells, fewer studies have investigated it in Mφ [114], [115], [112], [116], [117]. Interestingly, influenza virus contains an essential gene, polymerase basic protein 1-frame 2 (PB1-F2, a product of an alternate reading frame of the PB1 gene), which increases apoptosis-mediated pathogenicity in IAV [118]. Functionally, PB1-F2 has been shown to be the main inducer of apoptosis in monocytes/Mφ, but not epithelial cells [116], [112]. The pro-apoptotic effect of PB1-F2 is elicited by its translocation to the mitochondrion [119]. In mitochondria, PB1-F2 interacts with components of the permeability transition pore complex (PTPC) ANT3 and VDAC1 [120] to disrupt the mitochondrial inner membrane potential, followed by cytochrome c release and the induction of apoptosis, which subdues the Mφ antiviral capacity and promotes host susceptibility [116].
IAV-induced apoptosis in Mφ is not solely caused by viral protein expression and may result from the activation of the extrinsic pathway by host factors [110], [115], [121]. Interestingly, IAV-infected Mφ are the main source of the key antiviral cytokine: IFN-I [25], [122], [116] and can induce Mφ cell death via the upregulation of ISGs. Moreover, infection of human Mφ with HPAI strains induces TRAIL release to trigger the apoptotic cascade [123], [27]. Equally, upregulation of Fas and secretion of FasL at later time points post-infection have been shown to induce apoptosis selectively in recruited Mφ [115], [121], a process which is thought to contribute to immune contraction and the return to homeostasis. Of note, although TNF has been reported to induce apoptosis in IAV-infected epithelial cells, it does not appear to mediate Mφ apoptosis [45]. Thus, during IAV infection, activation or inhibition of apoptotic pathways are cell-type specific and can either promote or prevent IAV pathogenesis. Therefore, this complex network certainly needs to be interrogated more intensely.
3.2. Apoptosis in IAV-infected macrophages: friend or foe?
The outcome of IAV-induced Mφ apoptosis is still controversial, as it may favor both the host and the virus. Nonetheless, much of the literature suggests a host-detrimental effect of Mφ apoptosis. For instance, HPAI and pandemic H1N1 influenza viruses hijack innate antiviral responses by inducing apoptosis in Mφ to decrease Mφ-antiviral cytokines (primarily IFN-I) and promote viral replication [27], [123], [124]. Considering residential AMφ are the first immune cells encountered by the influenza virus and are critical in mounting an immune response, it is not surprising that IAV efficiently infects and kills AMφ to suppress their antiviral responses. Thus, shortly after severe IAV infection, the original pool of resident AMφ decreases, resulting in enhanced viral replication [110], [105]. Similarly, limiting AMφ cell death through the exogenous administration or overexpression of GM-CSF—the critical growth and maintenance factor for AMφ—is protective, leading to lowered pulmonary viral load, decreased immunopathology and increased survival of mice after IAV infection [125], [109]. In addition to inhibiting the early antiviral responses, IAV-induced Mφ apoptosis might skew the balance from a protective to pathological immune response. During IAV infection, it has been shown that mice lacking type I IFN signaling die from an uncontrolled inflammatory response, as IFN-I signaling was essential to induce anti-inflammatory IL-10 production by “regulatory” Mφ [126]—a subset of Mφ known to be more susceptible to IAV-induced apoptosis [113].
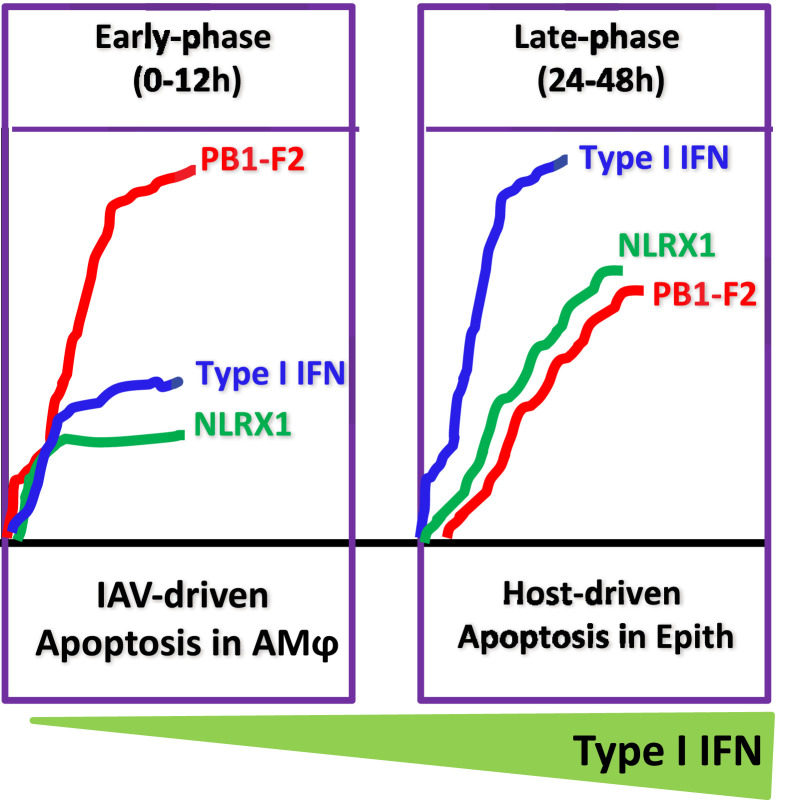
Mechanistically, IAV-induced Mφ apoptosis is mainly mediated by the viral protein PB1-F2 and its expression has been linked to delayed viral clearance [120]. Expression of the 1918 PB1-F2 protein in a mouse-adapted H1N1 strain resulted in early increased viral titers and death of infected Mφ [127]. To prevent PB1-F2-induced early Mφ apoptosis, we have recently shown that the host mitochondrial NLR-member NLRX1 directly interacts with PB1-F2 within mitochondria to disarm its apoptotic function. In IAV-infected Nlrx1 −/− mice, or Mφ in vitro, higher levels of apoptosis were observed compared to WT Mφ. This was associated with reduced production of IFN-I and increased viral loads in vitro and in vivo [116]. Thus, by inducing Mφ cell death, IAV hijacks the host's key antiviral responses, resulting in both enhanced IAV replication/dissemination and impairment of the anti-inflammatory response, which drives immunopathology and potentially ARDS (Fig. 2 ).
Fig. 2.
The impact of early versus late apoptosis of pulmonary macrophages on immunity to IAV infection. IAV induces early apoptosis in alveolar macrophages via the pro-apoptotic PB1-F2-IAV protein. We envision that the low levels of mitochondrial NLRX1 protein upon infection leads to early apoptosis and reduced production of type I IFN in alveolar macrophages. However, during the late phase of infection, high levels of mitochondrial NLRX1 protein disarm the pro-apoptotic function of PB1-F2 that leads to increased macrophage survival as well as IFN-I production. The increased levels of IFN-I in the alveolar space induce apoptosis in IAV-infected epithelial cells (Epith) and, thus, disrupt the niche for viral replication.
However, recent findings indicate that in some cases, apoptosis of pulmonary Mφ may be beneficial for the host. Indeed, early apoptosis of HPAI-infected porcine AMφ correlated to decreased viral replication and magnitude of the inflammatory response [112]. Aside from viral proteins, our laboratory recently demonstrated that IAV induces production of the host eicosanoid prostaglandin E2 (PGE2) to directly inhibit early production of IFN-I, which increased viral loads through reduced Mφ apoptosis. Thus, whether apoptosis is protective or pathological seems, again, to be connected to the kinetics of its induction. Early post-infection, Mφ viability is essential to promote antiviral immunity and this is countered by IAV proteins such as PB1-F2. Later, however, Mφ apoptosis becomes protective, as the apoptotic vesicles stimulate adaptive immunity by promoting cross-presentation [25].
To conclude, apoptotic cell death of macrophages appears to be a double-edged sword—both beneficial and detrimental to the host, depending on IAV virulence factors and host mediators. Further work is needed with closer inspection of the kinetics of expression of viral proteins (e.g. PB1-F2, NS1) as well as host factors (eg. NLRX1, IFN-I, eicosanoids) and their link with kinetics of Mφ cell death (early versus late induction) to fully understand whether timing or, rather, specific pathways or types of apoptosis dictate this complex phenomenon.
3.3. Other cell death programs in IAV-infected macrophages
Despite apoptosis being the main Mφ death modality observed in IAV infections, there is also evidence of necrosis [128], [32] and, specifically, of the more recently characterized RIPK3-mediated necroptosis. However, IAV-induced macrophage necrosis has been poorly studied in vivo and most of our knowledge is confined to in vitro observation. At low multiplicities of infection (MOI), necrosis is not substantially induced in Mφ [116], [26], [129]. In addition, we and others have recently shown that IAV does not induce RIPK3-mediated necroptosis in Mφ, both in vivo and in vitro, but, rather, RIPK3 plays a crucial role in the production of IL-1β [129] and IFN-I [130] and, as a result, mice deficient in RIPK3 are extremely susceptible to IAV infection. However, following severe infection with a high viral titer, IAV induces necroptosis through the RIPK1–RIPK3–Caspase 8 complex in vitro [86], suggesting a potential role for RIPK3-mediated necroptosis in depletion of Mφ during infection with highly virulent strains. Synergy between these two observations may come from the pleiotropic function of IFN-I, which has been also shown to induce Mφ necroptosis in vitro or in vivo during bacterial infections [131], [132], [133]. Thus, it can be envisioned that dysregulated RIPK3-mediated IFN-I production in severe infection may, in fact, become detrimental to the host by inducing necroptosis of pulmonary Mφ, suggesting a threshold for protective IFN-I production and deleterious immunopathology induced by Mφ necroptosis. Of note, pathways known to induce IFN-I in response to IAV and other viruses, such as TLR3 [134], PKR [132] and DNA-dependent activator of IFN-regulatory factors (DAI) [135] have also been shown to trigger necroptosis, advocating a potential link between type I IFN production and necroptosis induction.
Finally, IAV-infected macrophages produce IL-1β through inflammasome activation and caspase-1 cleavage, which are characteristics of pyroptotic cell death [136], [129]. However, there was no difference in cell death in IAV-infected Nlrp3 −/− (lacking the NLRP3 inflammasome) and WT Mφ, in vitro [86], suggesting that pyroptosis does not occur in Mφ during IAV infection. Certainly, further investigation is required to fully understand the precise mechanisms involved in this process.
4. Cross-talk between macrophages and epithelial cells
The lung represents a diverse microenvironment filled with numerous cell–cell interactions with high turnover under homeostatic and pathological conditions. In particular, epithelial cells of the EBB and AMφ exist in close proximity and are known to regulate each other's functions at homeostasis and upon infection. Over the last ten years, we have gained appreciable knowledge of how pulmonary macrophages induce apoptosis in infected epithelial cells. In 2008, Herold et al. showed for the first time that secretion of TRAIL by Mφ induced apoptosis of AEC and contributed to lung injury during IAV infection [137]. Further investigation also revealed that secretion of IFN-I, and specifically IFN-β, by infected AMφ was responsible for autocrine TRAIL expression and epithelium injury [138]. Most importantly, an upregulation of TRAIL expression and secretion was observed in AMφ from pandemic H1N1-infected individuals [138]. In addition to potentiating lung injury, this could potentially lead to viral dissemination by promoting efferocytosis. Efferocytosis is the phagocytosis of apoptotic bodies released from dying cells by neighboring Mφ [139]. Recently, annexin A1, a key protein involved in efferocytosis [140], [141], [148], was shown to facilitate IAV replication and dissemination in vivo [68]. Interestingly, Tcherniuk et al. showed that newly formed viral particles contained annexin A1 on their membranes, increasing their infectivity and viral replication through enhanced uptake [142]. In addition, activation of formyl peptide receptor 2/lipoxin A4 receptor (FPR2/ALX) via annexin A1, increased pulmonary viral load and susceptibility to infection [142]. Hence, one can envision a model wherein the induction of epithelial cell apoptosis by AMφ-derived IFN-I leads to the presence of annexin A1-expressing viral particles on the surface of infected cells. These new viral particles are, in turn, recognized and taken up by bystander Mφ, infecting them and preventing their antiviral responses. This leads to increased viral replication that subsequently enhances the magnitude of the immune response—thus, continuing this vicious cycle of lung injury/reinfection. This may potentially explain how HPAI and pandemic H1N1 viruses strip the pulmonary epithelium and leave the host leukopenic, as seen in fatal cases. Therefore, discovery of factors that can mitigate this pathological cycle would be of clinical significance in combatting highly pathogenic strains of IAV.
5. Targeting cell death programs as a potential therapy?
Despite influenza virus infections likely dating back to the Middle Ages and considerable burden on global health, there is no effective therapy against IAV. To prevent infection, vaccination strategies are deployed worldwide. However, the protection conferred by vaccination is highly variable, due to the ability of the virus to shift antigens, leading to vaccine mismatch and a decrease in efficacy. Antiviral therapies, like neuraminidase inhibitors (i.e. Oseltamivir) that block viral egress to potentially ameliorate disease are currently in use. Despite considerable efficacy in murine models in lowering viral titers and improving disease outcome [143], [144], its protective effect in humans is controversial and limited benefit has been shown in the majority of patients [145], [146]. Additionally, highly resistant strains of IAV to Oseltamivir have recently emerged that raises growing concern [147]. Thus, these factors collectively suggest that the dogma of only targeting the virus and not the host’s immune response in the generation of anti-IAV drugs needs to be revisited.
Indeed, there are several “proof-of-concept” studies highlighting the promising therapeutic potential of targeting host cell death programs during IAV-infection. First, anti-TRAIL treatments selectively attenuated epithelial cells apoptosis, lung injury and increased survival of mice after IAV infection. Secondly, we recently demonstrated that targeted inhibition of mPGES-1, the key enzyme in PGE2 production, selectively regulated pulmonary Mφ apoptosis to boost antiviral and immunoregulatory properties. Importantly, mPGES-1 inhibition was effective even after three days of IAV-infection, coinciding with the onset of symptoms in humans. In line with this, a recent study by Hung et al. showed a reduction in viral titers, hospital stay and mortality when individuals infected with H3N2 IAV were given a combinatory therapy of Clarithromycin (antibiotic) –Naproxen (COX inhibitor) – Oseltamivir (neuraminidase inhibitor) [147], compared to Oseltamivir treatment alone, highlighting the importance of combining immunomodulatory therapies and those directly targeting the pathogen.
Additionally, we suggest RIPK3 as an attractive target for immunomodulatory therapy. Recently, the antiviral capabilities of RIPK3 have been shown to be at least twofold, by both inducing epithelial cell necroptosis and promoting IFN-I responses from pulmonary Mφ to potentiate survival to lethal IAV infection. Therefore, agonists of RIPK3 may promote viral clearance via both epithelial cells and macrophages and ultimately confer survival to severe disease. This shows that combining treatments that differentially target structural cell and pulmonary Mφ can significantly improve the outcome of influenza virus infection.
6. Conclusion
The constant exposure of humans to potentially life-threatening respiratory pathogens presents ongoing challenges to clinicians. The knowledge gained from the studies of cell death programs in epithelial cells and macrophages during IAV infection provide significantly better understanding of host mechanisms involved in protective or pathological immunity to IAV infection. However, further investigation is still required to identify the kinetics of cell death during influenza infection, which appears to be critical in regulating antiviral and anti-inflammatory responses. In addition, most of our knowledge comes from in vitro experiments and thus a need for greater tools to investigate cell death in vivo and discovery of new cellular markers of the various cell death programs will be required for developing a novel therapy in influenza virus infection. .
Conflict of interest
All authors declare that no conflicts of interest exist.
Acknowledgments
This work was supported by the Canadian Institute of Health Research (CIHR) Foundation Grant (FDN-143273) to M.D. M.D. holds the Fonds de recherche du Québec–Santé (FRQS). J.D. is supported by Research Institute of McGill University Health Centre (RI-MUHC) Studentship. E.P. is supported by FRQS Postdoctoral Fellowship.
References
- 1.Hirsh A. New Sydenham Soc; London: 1883. Handbook of geographical and historical pathology. [Google Scholar]
- 2.WHO . WHO; 2016. Influenza (seasonal) fact sheet. [Google Scholar]
- 3.Taubenberger J.K., Morens D.M. 1918 influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saunders-Hastings P.R., Krewski D. Reviewing the history of pandemic influenza: understanding patterns of emergence and transmission. Pathogens. 2016;5 doi: 10.3390/pathogens5040066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen H., Yuan H., Gao R., Zhang J., Wang D., Xiong Y. Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: a descriptive study. Lancet. 2014;383:714–721. doi: 10.1016/S0140-6736(14)60111-2. [DOI] [PubMed] [Google Scholar]
- 6.Claas E.C., Osterhaus A.D., van Beek R., De Jong J.C., Rimmelzwaan G.F., Senne D.A. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet. 1998;351:472–477. doi: 10.1016/S0140-6736(97)11212-0. [DOI] [PubMed] [Google Scholar]
- 7.Ip H.S., Torchetti M.K., Crespo R., Kohrs P., DeBruyn P., Mansfield K.G. Novel Eurasian highly pathogenic avian influenza A H5 viruses in wild birds, Washington, USA, 2014. Emerg Infect Dis. 2015;21:886–890. doi: 10.3201/eid2105.142020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saito T., Tanikawa T., Uchida Y., Takemae N., Kanehira K., Tsunekuni R. Intracontinental and intercontinental dissemination of Asian H5 highly pathogenic avian influenza virus (clade 2.3.4.4) in the winter of 2014–2015. Rev Med Virol. 2015;25:388–405. doi: 10.1002/rmv.1857. [DOI] [PubMed] [Google Scholar]
- 9.Yu H., Cowling B.J., Feng L., Lau E.H., Liao Q., Tsang T.K. Human infection with avian influenza A H7N9 virus: an assessment of clinical severity. Lancet. 2013;382:138–145. doi: 10.1016/S0140-6736(13)61207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuiken T., Taubenberger J.K. Pathology of human influenza revisited. Vaccine. 2008;26(Suppl. 4):D59–D66. doi: 10.1016/j.vaccine.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taubenberger J.K., Morens D.M. The pathology of influenza virus infections. Annu Rev Pathol. 2008;3:499–522. doi: 10.1146/annurev.pathmechdis.3.121806.154316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Short K.R., Kroeze E.J., Fouchier R.A., Kuiken T. Pathogenesis of influenza-induced acute respiratory distress syndrome. Lancet Infect Dis. 2014;14:57–69. doi: 10.1016/S1473-3099(13)70286-X. [DOI] [PubMed] [Google Scholar]
- 13.WHO . 2016. MERS-CoV global summary and risk assessment. [Google Scholar]
- 14.Chan R.W., Hemida M.G., Kayali G., Chu D.K., Poon L.L., Alnaeem A. Tropism and replication of Middle East respiratory syndrome coronavirus from dromedary camels in the human respiratory tract: an in-vitro and ex-vivo study. Lancet Respir Med. 2014;2:813–822. doi: 10.1016/S2213-2600(14)70158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hocke A.C., Becher A., Knepper J., Peter A., Holland G., Tonnies M. Emerging human middle East respiratory syndrome coronavirus causes widespread infection and alveolar damage in human lungs. Am J Respir Crit Care Med. 2013;188:882–886. doi: 10.1164/rccm.201305-0954LE. [DOI] [PubMed] [Google Scholar]
- 16.Chu H., Zhou J., Wong B.H., Li C., Chan J.F., Cheng Z.S. Middle East respiratory syndrome coronavirus efficiently infects human primary T lymphocytes and activates the extrinsic and intrinsic apoptosis pathways. J Infect Dis. 2016;213:904–914. doi: 10.1093/infdis/jiv380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou J., Chu H., Li C., Wong B.H., Cheng Z.S., Poon V.K. Active replication of Middle East respiratory syndrome coronavirus and aberrant induction of inflammatory cytokines and chemokines in human macrophages: implications for pathogenesis. J Infect Dis. 2014;209:1331–1342. doi: 10.1093/infdis/jit504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan M.C., Chan R.W., Chan L.L., Mok C.K., Hui K.P., Fong J.H. Tropism and innate host responses of a novel avian influenza A H7N9 virus: an analysis of ex-vivo and in-vitro cultures of the human respiratory tract. Lancet Respir Med. 2013;1:534–542. doi: 10.1016/S2213-2600(13)70138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan M.C., Chan R.W., Yu W.C., Ho C.C., Yuen K.M., Fong J.H. Tropism and innate host responses of the 2009 pandemic H1N1 influenza virus in ex vivo and in vitro cultures of human conjunctiva and respiratory tract. Am J Pathol. 2010;176:1828–1840. doi: 10.2353/ajpath.2010.091087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knepper J., Schierhorn K.L., Becher A., Budt M., Tonnies M., Bauer T.T. The novel human influenza A (H7N9) virus is naturally adapted to efficient growth in human lung tissue. mBio. 2013;4:e00601–e00613. doi: 10.1128/mBio.00601-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinheimer V.K., Becher A., Tonnies M., Holland G., Knepper J., Bauer T.T. Influenza A viruses target type II pneumocytes in the human lung. J Infect Dis. 2012;206:1685–1694. doi: 10.1093/infdis/jis455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang J., Zhang Z., Fan X., Liu Y., Wang J., Zheng Z. 2009 pandemic H1N1 influenza virus replicates in human lung tissues. J Infect Dis. 2010;201:1522–1526. doi: 10.1086/650544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shieh W.J., Blau D.M., Denison A.M., Deleon-Carnes M., Adem P., Bhatnagar J. 2009 pandemic influenza A (H1N1): pathology and pathogenesis of 100 fatal cases in the United States. Am J Pathol. 2010;177:166–175. doi: 10.2353/ajpath.2010.100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang W., Mu X., Zhao L., Wang J., Chu Y., Feng X. Transcriptional response of human umbilical vein endothelial cell to H9N2 influenza virus infection. Virology. 2015;482:117–127. doi: 10.1016/j.virol.2015.03.037. [DOI] [PubMed] [Google Scholar]
- 25.Coulombe F., Jaworska J., Verway M., Tzelepis F., Massoud A., Gillard J. Targeted prostaglandin E2 inhibition enhances antiviral immunity through induction of type I interferon and apoptosis in macrophages. Immunity. 2014;40:554–568. doi: 10.1016/j.immuni.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Hoeve M.A., Nash A.A., Jackson D., Randall R.E., Dransfield I. Influenza virus A infection of human monocyte and macrophage subpopulations reveals increased susceptibility associated with cell differentiation. PLoS ONE. 2012;7:e29443. doi: 10.1371/journal.pone.0029443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mok C.K., Lee D.C., Cheung C.Y., Peiris M., Lau A.S. Differential onset of apoptosis in influenza A virus H5N1- and H1N1-infected human blood macrophages. J Gen Virol. 2007;88:1275–1280. doi: 10.1099/vir.0.82423-0. [DOI] [PubMed] [Google Scholar]
- 28.Hussell T., Bell T.J. Alveolar macrophages: plasticity in a tissue-specific context. Nat Rev Immunol. 2014;14:81–93. doi: 10.1038/nri3600. [DOI] [PubMed] [Google Scholar]
- 29.Divangahi M., King I.L., Pernet E. Alveolar macrophages and type I IFN in airway homeostasis and immunity. Trends Immunol. 2015;36:307–314. doi: 10.1016/j.it.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Kerr J.F., Wyllie A.H., Currie A.R. Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer. 1972;26:239–257. doi: 10.1038/bjc.1972.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kroemer G., Galluzzi L., Vandenabeele P., Abrams J., Alnemri E.S., Baehrecke E.H. Classification of cell death: recommendations of the nomenclature committee on cell death 2009. Cell Death Differ. 2009;16:3–11. doi: 10.1038/cdd.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uiprasertkul M., Kitphati R., Puthavathana P., Kriwong R., Kongchanagul A., Ungchusak K. Apoptosis and pathogenesis of avian influenza A (H5N1) virus in humans. Emerg Infect Dis. 2007;13:708–712. doi: 10.3201/eid1305.060572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35:495–516. doi: 10.1080/01926230701320337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vandenabeele P., Galluzzi L., Vanden Berghe T., Kroemer G. Molecular mechanisms of necroptosis: an ordered cellular explosion. Nat Rev Mol Cell Biol. 2010;11:700–714. doi: 10.1038/nrm2970. [DOI] [PubMed] [Google Scholar]
- 35.McCullers J.A. The co-pathogenesis of influenza viruses with bacteria in the lung. Nat Rev Microbiol. 2014;12:252–262. doi: 10.1038/nrmicro3231. [DOI] [PubMed] [Google Scholar]
- 36.Kroeker A.L., Ezzati P., Halayko A.J., Coombs K.M. Response of primary human airway epithelial cells to influenza infection: a quantitative proteomic study. J Proteome Res. 2012;11:4132–4146. doi: 10.1021/pr300239r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Winternitz M.C., Lambert R.A. Edema of the lungs as a cause of death. J Exp Med. 1919;29:537–545. doi: 10.1084/jem.29.6.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tate M.D., Schilter H.C., Brooks A.G., Reading P.C. Responses of mouse airway epithelial cells and alveolar macrophages to virulent and avirulent strains of influenza A virus. Viral Immunol. 2011;24:77–88. doi: 10.1089/vim.2010.0118. [DOI] [PubMed] [Google Scholar]
- 39.Martin C.J., Peters K.N., Behar S.M. Macrophages clean up: efferocytosis and microbial control. Curr Opin Microbiol. 2014;17:17–23. doi: 10.1016/j.mib.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salvesen G.S. Caspases and apoptosis. Essays Biochem. 2002;38:9–19. doi: 10.1042/bse0380009. [DOI] [PubMed] [Google Scholar]
- 41.Igney F.H., Krammer P.H. Death and anti-death: tumour resistance to apoptosis. Nat Rev Cancer. 2002;2:277–288. doi: 10.1038/nrc776. [DOI] [PubMed] [Google Scholar]
- 42.Schmitz I., Kirchhoff S., Krammer P.H. Regulation of death receptor-mediated apoptosis pathways. Int J Biochem Cell Biol. 2000;32:1123–1136. doi: 10.1016/s1357-2725(00)00048-0. [DOI] [PubMed] [Google Scholar]
- 43.Divangahi M., Behar S.M., Remold H. Dying to live: how the death modality of the infected macrophage affects immunity to tuberculosis. Adv Exp Med Biol. 2013;783:103–120. doi: 10.1007/978-1-4614-6111-1_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Czuczman M.A., Fattouh R., van Rijn J.M., Canadien V., Osborne S., Muise A.M. Listeria monocytogenes exploits efferocytosis to promote cell-to-cell spread. Nature. 2014;509:230–234. doi: 10.1038/nature13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McKinney L.C., Galliger S.J., Lowy R.J. Active and inactive influenza virus induction of tumor necrosis factor-alpha and nitric oxide in J774.1 murine macrophages: modulation by interferon-gamma and failure to induce apoptosis. Virus Res. 2003;97:117–126. doi: 10.1016/j.virusres.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 46.Mori I., Komatsu T., Takeuchi K., Nakakuki K., Sudo M., Kimura Y. In vivo induction of apoptosis by influenza virus. J Gen Virol. 1995;76:2869–2873. doi: 10.1099/0022-1317-76-11-2869. [DOI] [PubMed] [Google Scholar]
- 47.Takizawa T., Matsukawa S., Higuchi Y., Nakamura S., Nakanishi Y., Fukuda R. Induction of programmed cell death (apoptosis) by influenza virus infection in tissue culture cells. J Gen Virol. 1993;74:2347–2355. doi: 10.1099/0022-1317-74-11-2347. [DOI] [PubMed] [Google Scholar]
- 48.Guarner J., Falcon-Escobedo R. Comparison of the pathology caused by H1N1, H5N1, and H3N2 influenza viruses. Arch Med Res. 2009;40:655–661. doi: 10.1016/j.arcmed.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 49.Daidoji T., Koma T., Du A., Yang C.S., Ueda M., Ikuta K. H5N1 avian influenza virus induces apoptotic cell death in mammalian airway epithelial cells. J Virol. 2008;82:11294–11307. doi: 10.1128/JVI.01192-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kawai T., Akira S. Innate immune recognition of viral infection. Nat Immunol. 2006;7:131–137. doi: 10.1038/ni1303. [DOI] [PubMed] [Google Scholar]
- 51.El-Sayed I., Bassiouny K., Nokaly A., Abdelghani A.S., Roshdy W. Influenza A virus and influenza B virus can induce apoptosis via intrinsic or extrinsic pathways and also via NF-kappaB in a time and dose dependent manner. Biochem Res Int. 2016;2016:1738237. doi: 10.1155/2016/1738237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Balachandran S., Kim C.N., Yeh W.C., Mak T.W., Bhalla K., Barber G.N. Activation of the dsRNA-dependent protein kinase, PKR, induces apoptosis through FADD-mediated death signaling. EMBO J. 1998;17:6888–6902. doi: 10.1093/emboj/17.23.6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meurs E., Chong K., Galabru J., Thomas N.S., Kerr I.M., Williams B.R. Molecular cloning and characterization of the human double-stranded RNA-activated protein kinase induced by interferon. Cell. 1990;62:379–390. doi: 10.1016/0092-8674(90)90374-n. [DOI] [PubMed] [Google Scholar]
- 54.Balachandran S., Roberts P.C., Brown L.E., Truong H., Pattnaik A.K., Archer D.R. Essential role for the dsRNA-dependent protein kinase PKR in innate immunity to viral infection. Immunity. 2000;13:129–141. doi: 10.1016/s1074-7613(00)00014-5. [DOI] [PubMed] [Google Scholar]
- 55.Barry G., Fragkoudis R., Ferguson M.C., Lulla A., Merits A., Kohl A. Semliki forest virus-induced endoplasmic reticulum stress accelerates apoptotic death of mammalian cells. J Virol. 2010;84:7369–7377. doi: 10.1128/JVI.02310-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brydon E.W., Smith H., Sweet C. Influenza A virus-induced apoptosis in bronchiolar epithelial (NCI-H292) cells limits pro-inflammatory cytokine release. J Gen Virol. 2003;84:2389–2400. doi: 10.1099/vir.0.18913-0. [DOI] [PubMed] [Google Scholar]
- 57.Heaton N.S., Langlois R.A., Sachs D., Lim J.K., Palese P., tenOever B.R. Long-term survival of influenza virus infected club cells drives immunopathology. J Exp Med. 2014;211:1707–1714. doi: 10.1084/jem.20140488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhirnov O.P., Konakova T.E., Wolff T., Klenk H.D. NS1 protein of influenza A virus down-regulates apoptosis. J Virol. 2002;76:1617–1625. doi: 10.1128/JVI.76.4.1617-1625.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ehrhardt C., Wolff T., Pleschka S., Planz O., Beermann W., Bode J.G. Influenza A virus NS1 protein activates the PI3K/Akt pathway to mediate antiapoptotic signaling responses. J Virol. 2007;81:3058–3067. doi: 10.1128/JVI.02082-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lam W.Y., Tang J.W., Yeung A.C., Chiu L.C., Sung J.J., Chan P.K. Avian influenza virus A/HK/483/97(H5N1) NS1 protein induces apoptosis in human airway epithelial cells. J Virol. 2008;82:2741–2751. doi: 10.1128/JVI.01712-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tripathi S., Batra J., Cao W., Sharma K., Patel J.R., Ranjan P. Influenza A virus nucleoprotein induces apoptosis in human airway epithelial cells: implications of a novel interaction between nucleoprotein and host protein Clusterin. Cell Death Dis. 2013;4:e562. doi: 10.1038/cddis.2013.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mayank A.K., Sharma S., Nailwal H., Lal S.K. Nucleoprotein of influenza A virus negatively impacts antiapoptotic protein API5 to enhance E2F1-dependent apoptosis and virus replication. Cell Death Dis. 2015;6:e2018. doi: 10.1038/cddis.2015.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tran A.T., Cortens J.P., Du Q., Wilkins J.A., Coombs K.M. Influenza virus induces apoptosis via BAD-mediated mitochondrial dysregulation. J Virol. 2013;87:1049–1060. doi: 10.1128/JVI.02017-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nencioni L., De Chiara G., Sgarbanti R., Amatore D., Aquilano K., Marcocci M.E. Bcl-2 expression and p38MAPK activity in cells infected with influenza A virus: impact on virally induced apoptosis and viral replication. J Biol Chem. 2009;284:16004–16015. doi: 10.1074/jbc.M900146200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McLean J.E., Datan E., Matassov D., Zakeri Z.F. Lack of Bax prevents influenza A virus-induced apoptosis and causes diminished viral replication. J Virol. 2009;83:8233–8246. doi: 10.1128/JVI.02672-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wurzer W.J., Planz O., Ehrhardt C., Giner M., Silberzahn T., Pleschka S. Caspase 3 activation is essential for efficient influenza virus propagation. EMBO J. 2003;22:2717–2728. doi: 10.1093/emboj/cdg279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gannage M., Dormann D., Albrecht R., Dengjel J., Torossi T., Ramer P.C. Matrix protein 2 of influenza A virus blocks autophagosome fusion with lysosomes. Cell Host Microbe. 2009;6:367–380. doi: 10.1016/j.chom.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Arora S., Lim W., Bist P., Perumalsamy R., Lukman H.M., Li F. Influenza A virus enhances its propagation through the modulation of Annexin-A1 dependent endosomal trafficking and apoptosis. Cell Death Differ. 2016;23:1243–1256. doi: 10.1038/cdd.2016.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Othumpangat S., Noti J.D., Beezhold D.H. Lung epithelial cells resist influenza A infection by inducing the expression of cytochrome c oxidase VIc which is modulated by miRNA 4276. Virology. 2014;468–470:256–264. doi: 10.1016/j.virol.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wurzer W.J., Ehrhardt C., Pleschka S., Berberich-Siebelt F., Wolff T., Walczak H. NF-kappaB-dependent induction of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) and Fas/FasL is crucial for efficient influenza virus propagation. J Biol Chem. 2004;279:30931–30937. doi: 10.1074/jbc.M403258200. [DOI] [PubMed] [Google Scholar]
- 71.Fujikura D., Chiba S., Muramatsu D., Kazumata M., Nakayama Y., Kawai T. Type-I interferon is critical for FasL expression on lung cells to determine the severity of influenza. PLoS One. 2013;8:e55321. doi: 10.1371/journal.pone.0055321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Iyer S.S., Pulskens W.P., Sadler J.J., Butter L.M., Teske G.J., Ulland T.K. Necrotic cells trigger a sterile inflammatory response through the Nlrp3 inflammasome. Proc Natl Acad Sci U S A. 2009;106:20388–20393. doi: 10.1073/pnas.0908698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Scaffidi P., Misteli T., Bianchi M.E. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature. 2002;418:191–195. doi: 10.1038/nature00858. [DOI] [PubMed] [Google Scholar]
- 74.Chen L.C., Yeh T.M., Wu H.N., Lin Y.Y., Shyu H.W. Dengue virus infection induces passive release of high mobility group box 1 protein by epithelial cells. J Infect. 2008;56:143–150. doi: 10.1016/j.jinf.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 75.Tao X., Hill T.E., Morimoto C., Peters C.J., Ksiazek T.G., Tseng C.T. Bilateral entry and release of Middle East respiratory syndrome coronavirus induces profound apoptosis of human bronchial epithelial cells. J Virol. 2013;87:9953–9958. doi: 10.1128/JVI.01562-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bossios A., Psarras S., Gourgiotis D., Skevaki C.L., Constantopoulos A.G., Saxoni-Papageorgiou P. Rhinovirus infection induces cytotoxicity and delays wound healing in bronchial epithelial cells. Respir Res. 2005;6:114. doi: 10.1186/1465-9921-6-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Arndt U., Wennemuth G., Barth P., Nain M., Al-Abed Y., Meinhardt A. Release of macrophage migration inhibitory factor and CXCL8/interleukin-8 from lung epithelial cells rendered necrotic by influenza A virus infection. J Virol. 2002;76:9298–9306. doi: 10.1128/JVI.76.18.9298-9306.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pasparakis M., Vandenabeele P. Necroptosis and its role in inflammation. Nature. 2015;517:311–320. doi: 10.1038/nature14191. [DOI] [PubMed] [Google Scholar]
- 79.Gong Y.N., Guy C., Olauson H., Becker J.U., Yang M., Fitzgerald P. ESCRT-III acts downstream of MLKL to regulate necroptotic cell death and its consequences. Cell. 2017;169:286–300. doi: 10.1016/j.cell.2017.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kaczmarek A., Vandenabeele P., Krysko D.V. Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity. 2013;38:209–223. doi: 10.1016/j.immuni.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 81.Cho Y.S., Challa S., Moquin D., Genga R., Ray T.D., Guildford M. Phosphorylation-driven assembly of the RIP1–RIP3 complex regulates programmed necrosis and virus-induced inflammation. Cell. 2009;137:1112–1123. doi: 10.1016/j.cell.2009.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Guo H., Omoto S., Harris P.A., Finger J.N., Bertin J., Gough P.J. Herpes simplex virus suppresses necroptosis in human cells. Cell Host Microbe. 2015;17:243–251. doi: 10.1016/j.chom.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Upton J.W., Kaiser W.J., Mocarski E.S. Cytomegalovirus m45 cell death suppression requires receptor-interacting protein (RIP) homotypic interaction motif (RHIM)-dependent interaction with RIP1. J Biol Chem. 2008;283:16966–16970. doi: 10.1074/jbc.C800051200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nogusa S., Thapa R.J., Dillon C.P., Liedmann S., Oguin T.H., 3rd, Ingram J.P. RIPK3 activates parallel pathways of MLKL-driven necroptosis and FADD-mediated apoptosis to protect against influenza A virus. Cell Host Microbe. 2016;20:13–24. doi: 10.1016/j.chom.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bergsbaken T., Fink S.L., Cookson B.T. Pyroptosis: host cell death and inflammation. Nat Rev Microbiol. 2009;7:99–109. doi: 10.1038/nrmicro2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kuriakose T., Man S.M., Malireddi R.K., Karki R., Kesavardhana S., Place D.E. ZBP1/DAI is an innate sensor of influenza virus triggering the NLRP3 inflammasome and programmed cell death pathways. Sci Immunol. 2016;1 doi: 10.1126/sciimmunol.aag2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ichinohe T., Lee H.K., Ogura Y., Flavell R., Iwasaki A. Inflammasome recognition of influenza virus is essential for adaptive immune responses. J Exp Med. 2009;206:79–87. doi: 10.1084/jem.20081667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Postma D.S., Timens W. Remodeling in asthma and chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2006;3:434–439. doi: 10.1513/pats.200601-006AW. [DOI] [PubMed] [Google Scholar]
- 89.Armstrong S.M., Wang C., Tigdi J., Si X., Dumpit C., Charles S. Influenza infects lung microvascular endothelium leading to microvascular leak: role of apoptosis and claudin-5. PLoS One. 2012;7:e47323. doi: 10.1371/journal.pone.0047323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zeng H., Pappas C., Belser J.A., Houser K.V., Zhong W., Wadford D.A. Human pulmonary microvascular endothelial cells support productive replication of highly pathogenic avian influenza viruses: possible involvement in the pathogenesis of human H5N1 virus infection. J Virol. 2012;86:667–678. doi: 10.1128/JVI.06348-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cilloniz C., Pantin-Jackwood M.J., Ni C., Goodman A.G., Peng X., Proll S.C. Lethal dissemination of H5N1 influenza virus is associated with dysregulation of inflammation and lipoxin signaling in a mouse model of infection. J Virol. 2010;84:7613–7624. doi: 10.1128/JVI.00553-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Uyeki T.M. Human infection with highly pathogenic avian influenza A (H5N1) virus: review of clinical issues. Clin Infect Dis. 2009;49:279–290. doi: 10.1086/600035. [DOI] [PubMed] [Google Scholar]
- 93.Gu J., Xie Z., Gao Z., Liu J., Korteweg C., Ye J. H5N1 infection of the respiratory tract and beyond: a molecular pathology study. Lancet. 2007;370:1137–1145. doi: 10.1016/S0140-6736(07)61515-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fukuyama S., Kawaoka Y. The pathogenesis of influenza virus infections: the contributions of virus and host factors. Curr Opin Immunol. 2011;23:481–486. doi: 10.1016/j.coi.2011.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Perrone L.A., Plowden J.K., Garcia-Sastre A., Katz J.M., Tumpey T.M. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 2008;4:e1000115. doi: 10.1371/journal.ppat.1000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tumpey T.M., Basler C.F., Aguilar P.V., Zeng H., Solorzano A., Swayne D.E. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 97.Chen Y., Liang W., Yang S., Wu N., Gao H., Sheng J. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet. 2013;381:1916–1925. doi: 10.1016/S0140-6736(13)60903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boonnak K., Vogel L., Feldmann F., Feldmann H., Legge K.L., Subbarao K. Lymphopenia associated with highly virulent H5N1 virus infection due to plasmacytoid dendritic cell-mediated apoptosis of T cells. J Immunol. 2014;192:5906–5912. doi: 10.4049/jimmunol.1302992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Colamussi M.L., White M.R., Crouch E., Hartshorn K.L. Influenza A virus accelerates neutrophil apoptosis and markedly potentiates apoptotic effects of bacteria. Blood. 1999;93:2395–2403. [PubMed] [Google Scholar]
- 100.Thitithanyanont A., Engering A., Ekchariyawat P., Wiboon-ut S., Limsalakpetch A., Yongvanitchit K. High susceptibility of human dendritic cells to avian influenza H5N1 virus infection and protection by IFN-alpha and TLR ligands. J Immunol. 2007;179:5220–5227. doi: 10.4049/jimmunol.179.8.5220. [DOI] [PubMed] [Google Scholar]
- 101.Seo S.U., Kwon H.J., Ko H.J., Byun Y.H., Seong B.L., Uematsu S. Type I interferon signaling regulates Ly6C(hi) monocytes and neutrophils during acute viral pneumonia in mice. PLoS Pathog. 2011;7:e1001304. doi: 10.1371/journal.ppat.1001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ramos-Casals M., Garcia-Carrasco M., Lopez-Medrano F., Trejo O., Forns X., Lopez-Guillermo A. Severe autoimmune cytopenias in treatment-naive hepatitis C virus infection: clinical description of 35 cases. Medicine (Baltim) 2003;82:87–96. doi: 10.1097/00005792-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 103.Matatall K.A., Jeong M., Chen S., Sun D., Chen F., Mo Q. Chronic infection depletes hematopoietic stem cells through stress-induced terminal differentiation. Cell Rep. 2016;17:2584–2595. doi: 10.1016/j.celrep.2016.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.van Riel D., Leijten L.M., van der Eerden M., Hoogsteden H.C., Boven L.A., Lambrecht B.N. Highly pathogenic avian influenza virus H5N1 infects alveolar macrophages without virus production or excessive TNF-alpha induction. PLoS Pathog. 2011;7:e1002099. doi: 10.1371/journal.ppat.1002099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tate M.D., Pickett D.L., van Rooijen N., Brooks A.G., Reading P.C. Critical role of airway macrophages in modulating disease severity during influenza virus infection of mice. J Virol. 2010;84:7569–7580. doi: 10.1128/JVI.00291-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schneider C., Nobs S.P., Heer A.K., Kurrer M., Klinke G., van Rooijen N. Alveolar macrophages are essential for protection from respiratory failure and associated morbidity following influenza virus infection. PLoS Pathog. 2014;10:e1004053. doi: 10.1371/journal.ppat.1004053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Snelgrove R.J., Goulding J., Didierlaurent A.M., Lyonga D., Vekaria S., Edwards L. A critical function for CD200 in lung immune homeostasis and the severity of influenza infection. Nat Immunol. 2008;9:1074–1083. doi: 10.1038/ni.1637. [DOI] [PubMed] [Google Scholar]
- 108.Duan M., Hibbs M.L., Chen W. The contributions of lung macrophage and monocyte heterogeneity to influenza pathogenesis. Immunol Cell Biol. 2017;95:225–235. doi: 10.1038/icb.2016.97. [DOI] [PubMed] [Google Scholar]
- 109.Sever-Chroneos Z., Murthy A., Davis J., Florence J.M., Kurdowska A., Krupa A. GM-CSF modulates pulmonary resistance to influenza A infection. Antiviral Res. 2011;92:319–328. doi: 10.1016/j.antiviral.2011.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ghoneim H.E., Thomas P.G., McCullers J.A. Depletion of alveolar macrophages during influenza infection facilitates bacterial superinfections. J Immunol. 2013;191:1250–1259. doi: 10.4049/jimmunol.1300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hashimoto D., Chow A., Noizat C., Teo P., Beasley M.B., Leboeuf M. Tissue-resident macrophages self-maintain locally throughout adult life with minimal contribution from circulating monocytes. Immunity. 2013;38:792–804. doi: 10.1016/j.immuni.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chang P., Kuchipudi S.V., Mellits K.H., Sebastian S., James J., Liu J. Early apoptosis of porcine alveolar macrophages limits avian influenza virus replication and pro-inflammatory dysregulation. Sci Rep. 2015;5:17999. doi: 10.1038/srep17999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Campbell G.M., Nicol M.Q., Dransfield I., Shaw D.J., Nash A.A., Dutia B.M. Susceptibility of bone marrow-derived macrophages to influenza virus infection is dependent on macrophage phenotype. J Gen Virol. 2015;96:2951–2960. doi: 10.1099/jgv.0.000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen W., Calvo P.A., Malide D., Gibbs J., Schubert U., Bacik I. A novel influenza A virus mitochondrial protein that induces cell death. Nat Med. 2001;7:1306–1312. doi: 10.1038/nm1201-1306. [DOI] [PubMed] [Google Scholar]
- 115.Xing Z., Cardona C.J., Adams S., Yang Z., Li J., Perez D. Differential regulation of antiviral and proinflammatory cytokines and suppression of Fas-mediated apoptosis by NS1 of H9N2 avian influenza virus in chicken macrophages. J Gen Virol. 2009;90:1109–1118. doi: 10.1099/vir.0.007518-0. [DOI] [PubMed] [Google Scholar]
- 116.Jaworska J., Coulombe F., Downey J., Tzelepis F., Shalaby K., Tattoli I. NLRX1 prevents mitochondrial induced apoptosis and enhances macrophage antiviral immunity by interacting with influenza virus PB1-F2 protein. Proc Natl Acad Sci U S A. 2014;111:E2110–E2119. doi: 10.1073/pnas.1322118111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.McAuley J.L., Hornung F., Boyd K.L., Smith A.M., McKeon R., Bennink J. Expression of the 1918 influenza A virus PB1-F2 enhances the pathogenesis of viral and secondary bacterial pneumonia. Cell Host Microbe. 2007;2:240–249. doi: 10.1016/j.chom.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Conenello G.M., Tisoncik J.R., Rosenzweig E., Varga Z.T., Palese P., Katze M.G. A single N66S mutation in the PB1-F2 protein of influenza A virus increases virulence by inhibiting the early interferon response in vivo. J Virol. 2011;85:652–662. doi: 10.1128/JVI.01987-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chanturiya A.N., Basanez G., Schubert U., Henklein P., Yewdell J.W., Zimmerberg J. PB1-F2, an influenza A virus-encoded proapoptotic mitochondrial protein, creates variably sized pores in planar lipid membranes. J Virol. 2004;78:6304–6312. doi: 10.1128/JVI.78.12.6304-6312.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zamarin D., Garcia-Sastre A., Xiao X., Wang R., Palese P. Influenza virus PB1-F2 protein induces cell death through mitochondrial ANT3 and VDAC1. PLoS Pathog. 2005;1:e4. doi: 10.1371/journal.ppat.0010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.William JJ, Lea B, Alaina M, Rebecca EO-D, Mark TK, Claudia J, et al. Fas determines differential fates of resident and recruited macrophages during resolution of acute lung injury. [DOI] [PMC free article] [PubMed]
- 122.Goritzka M., Makris S., Kausar F., Durant L.R., Pereira C., Kumagai Y. Alveolar macrophage-derived type I interferons orchestrate innate immunity to RSV through recruitment of antiviral monocytes. J Exp Med. 2015;212:699–714. doi: 10.1084/jem.20140825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Geiler J., Michaelis M., Sithisarn P., Cinatl J., Jr. Comparison of pro-inflammatory cytokine expression and cellular signal transduction in human macrophages infected with different influenza A viruses. Med Microbiol Immunol. 2011;200:53–60. doi: 10.1007/s00430-010-0173-y. [DOI] [PubMed] [Google Scholar]
- 124.Ekchariyawat P., Thitithanyanont A., Sirisinha S., Utaisincharoen P. Apoptosis induced by avian H5N1 virus in human monocyte-derived macrophages involves TRAIL-inducing caspase-10 activation. Innate Immun. 2012;18:390–397. doi: 10.1177/1753425911410998. [DOI] [PubMed] [Google Scholar]
- 125.Huang F.F., Barnes P.F., Feng Y., Donis R., Chroneos Z.C., Idell S. GM-CSF in the lung protects against lethal influenza infection. Am J Respir Crit Care Med. 2011;184:259–268. doi: 10.1164/rccm.201012-2036OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Arimori Y., Nakamura R., Yamada H., Shibata K., Maeda N., Kase T. Type I interferon limits influenza virus-induced acute lung injury by regulation of excessive inflammation in mice. Antiviral Res. 2013;99:230–237. doi: 10.1016/j.antiviral.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 127.Smith A.M., Adler F.R., McAuley J.L., Gutenkunst R.N., Ribeiro R.M., McCullers J.A. Effect of 1918 PB1-F2 expression on influenza A virus infection kinetics. PLoS Comput Biol. 2011;7:e1001081. doi: 10.1371/journal.pcbi.1001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rodrigue-Gervais I.G., Labbe K., Dagenais M., Dupaul-Chicoine J., Champagne C., Morizot A. Cellular inhibitor of apoptosis protein cIAP2 protects against pulmonary tissue necrosis during influenza virus infection to promote host survival. Cell Host Microbe. 2014;15:23–35. doi: 10.1016/j.chom.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 129.Wang X., Jiang W., Yan Y., Gong T., Han J., Tian Z. RNA viruses promote activation of the NLRP3 inflammasome through a RIP1–RIP3–DRP1 signaling pathway. Nat Immunol. 2014;15:1126–1133. doi: 10.1038/ni.3015. [DOI] [PubMed] [Google Scholar]
- 130.Downey J., Pernet E., Coulombe F., Allard B., Meunier I., Jaworska J. RIPK3 interacts with MAVS to regulate type I IFN-mediated immunity to Influenza A virus infection. PLoS Pathog. 2017;13:e1006326. doi: 10.1371/journal.ppat.1006326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.McComb S., Cessford E., Alturki N.A., Joseph J., Shutinoski B., Startek J.B. Type-I interferon signaling through ISGF3 complex is required for sustained Rip3 activation and necroptosis in macrophages. Proc Natl Acad Sci U S A. 2014;111:E3206–E3213. doi: 10.1073/pnas.1407068111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Thapa R.J., Nogusa S., Chen P., Maki J.L., Lerro A., Andrake M. Interferon-induced RIP1/RIP3-mediated necrosis requires PKR and is licensed by FADD and caspases. Proc Natl Acad Sci U S A. 2013;110:E3109–E3118. doi: 10.1073/pnas.1301218110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Robinson N., McComb S., Mulligan R., Dudani R., Krishnan L., Sad S. Type I interferon induces necroptosis in macrophages during infection with Salmonella enterica serovar Typhimurium. Nat Immunol. 2012;13:954–962. doi: 10.1038/ni.2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kaiser W.J., Sridharan H., Huang C., Mandal P., Upton J.W., Gough P.J. Toll-like receptor 3-mediated necrosis via TRIF, RIP3, and MLKL. J Biol Chem. 2013;288:31268–31279. doi: 10.1074/jbc.M113.462341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Takaoka A., Wang Z., Choi M.K., Yanai H., Negishi H., Ban T. DAI (DLM-1/ZBP1) is a cytosolic DNA sensor and an activator of innate immune response. Nature. 2007;448:501–505. doi: 10.1038/nature06013. [DOI] [PubMed] [Google Scholar]
- 136.Pang I.K., Iwasaki A. Inflammasomes as mediators of immunity against influenza virus. Trends Immunol. 2011;32:34–41. doi: 10.1016/j.it.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Herold S., von Wulffen W., Steinmueller M., Pleschka S., Kuziel W.A., Mack M. Alveolar epithelial cells direct monocyte transepithelial migration upon influenza virus infection: impact of chemokines and adhesion molecules. J Immunol. 2006;177:1817–1824. doi: 10.4049/jimmunol.177.3.1817. [DOI] [PubMed] [Google Scholar]
- 138.Hogner K., Wolff T., Pleschka S., Plog S., Gruber A.D., Kalinke U. Macrophage-expressed IFN-beta contributes to apoptotic alveolar epithelial cell injury in severe influenza virus pneumonia. PLoS Pathog. 2013;9:e1003188. doi: 10.1371/journal.ppat.1003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hashimoto Y., Moki T., Takizawa T., Shiratsuchi A., Nakanishi Y. Evidence for phagocytosis of influenza virus-infected, apoptotic cells by neutrophils and macrophages in mice. J Immunol. 2007;178:2448–2457. doi: 10.4049/jimmunol.178.4.2448. [DOI] [PubMed] [Google Scholar]
- 140.Arur S., Uche U.E., Rezaul K., Fong M., Scranton V., Cowan A.E. Annexin I is an endogenous ligand that mediates apoptotic cell engulfment. Dev Cell. 2003;4:587–598. doi: 10.1016/s1534-5807(03)00090-x. [DOI] [PubMed] [Google Scholar]
- 141.Yona S., Heinsbroek S.E., Peiser L., Gordon S., Perretti M., Flower R.J. Impaired phagocytic mechanism in annexin 1 null macrophages. Br J Pharmacol. 2006;148:469–477. doi: 10.1038/sj.bjp.0706730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tcherniuk S., Cenac N., Comte M., Frouard J., Errazuriz-Cerda E., Galabov A. Formyl peptide receptor 2 plays a deleterious role during influenza A virus infections. J Infect Dis. 2016;214:237–247. doi: 10.1093/infdis/jiw127. [DOI] [PubMed] [Google Scholar]
- 143.Yen H.L., Monto A.S., Webster R.G., Govorkova E.A. Virulence may determine the necessary duration and dosage of oseltamivir treatment for highly pathogenic A/Vietnam/1203/04 influenza virus in mice. J Infect Dis. 2005;192:665–672. doi: 10.1086/432008. [DOI] [PubMed] [Google Scholar]
- 144.Leyva-Grado V.H., Palese P. Aerosol administration increases the efficacy of oseltamivir for the treatment of mice infected with influenza viruses. Antiviral Res. 2017;142:12–15. doi: 10.1016/j.antiviral.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jefferson T., Jones M.A., Doshi P., Del Mar C.B., Hama R., Thompson M.J. Neuraminidase inhibitors for preventing and treating influenza in healthy adults and children. Cochrane Database Syst Rev. 2014:CD008965. doi: 10.1002/14651858.CD008965.pub3. [DOI] [PubMed] [Google Scholar]
- 146.Dobson J., Whitley R.J., Pocock S., Monto A.S. Oseltamivir treatment for influenza in adults: a meta-analysis of randomised controlled trials. Lancet. 2015;385:1729–1737. doi: 10.1016/S0140-6736(14)62449-1. [DOI] [PubMed] [Google Scholar]
- 147.Hung I.F.N., To K.K.W., Chan J.F.W., Cheng V.C.C., Liu K.S.H., Tam A. Efficacy of clarithromycin–naproxen–oseltamivir combination in the treatment of patients hospitalized for influenza A (H3N2) infection: an open-label randomized, controlled, phase IIb/III trial. Chest. 2017;151:1069–1080. doi: 10.1016/j.chest.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 148.Tzelepis F., Verway M., Daoud J., Gillard J., Hassani-Ardakani K., Dunn J. Annexin1 regulates DC efferocytosis and cross-presentation during Mycobacterium tuberculosis infection. J Clin Invest. 2015 Feb;125(2):752–768. doi: 10.1172/JCI77014. [DOI] [PMC free article] [PubMed] [Google Scholar]