Abstract
Background
The policy in a number of countries is to provide people with a terminal illness the choice of dying at home. This policy is supported by surveys indicating that the general public and people with a terminal illness would prefer to receive end‐of‐life care at home. This is the fourth update of the original review.
Objectives
To determine if providing home‐based end‐of‐life care reduces the likelihood of dying in hospital and what effect this has on patients' symptoms, quality of life, health service costs, and caregivers, compared with inpatient hospital or hospice care.
Search methods
We searched the following databases until April 2015: Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library), Ovid MEDLINE(R) (from 1950), EMBASE (from 1980), CINAHL (from 1982), and EconLit (from 1969). We checked the reference lists of potentially relevant articles identified and handsearched palliative care publications, clinical trials registries, and a database of systematic reviews for related trials (PDQ‐Evidence 2015).
Selection criteria
Randomised controlled trials, interrupted time series, or controlled before and after studies evaluating the effectiveness of home‐based end‐of‐life care with inpatient hospital or hospice care for people aged 18 years and older.
Data collection and analysis
Two review authors independently extracted data and assessed study quality. We combined the published data for dichotomous outcomes using fixed‐effect Mantel‐Haenszel meta‐analysis. When combining outcome data was not possible, we reported the results from individual studies.
Main results
We included four trials in this review and did not identify new studies from the search in April 2015. Home‐based end‐of‐life care increased the likelihood of dying at home compared with usual care (risk ratio (RR) 1.33, 95% confidence interval (CI) 1.14 to 1.55, P = 0.0002; Chi2 = 1.72, df = 2, P = 0.42, I2 = 0%; 3 trials; N = 652; high quality evidence). Admission to hospital while receiving home‐based end‐of‐life care varied between trials, and this was reflected by a high level of statistical heterogeneity in this analysis (range RR 0.62 to RR 2.61; 4 trials; N = 823; moderate quality evidence). Home‐based end‐of‐life care may slightly improve patient satisfaction at one‐month follow‐up and reduce it at six‐month follow‐up (2 trials; low quality evidence). The effect on caregivers is uncertain (2 trials; low quality evidence). The intervention may slightly reduce healthcare costs (2 trials, low quality evidence). No trial reported costs to patients and caregivers.
Authors' conclusions
The evidence included in this review supports the use of home‐based end‐of‐life care programmes for increasing the number of people who will die at home, although the numbers of people admitted to hospital while receiving end‐of‐life care should be monitored. Future research should systematically assess the impact of home‐based end‐of‐life care on caregivers.
Plain language summary
Home‐based end‐of‐life care
Background
A number of countries have invested in health services to provide care at home to people with a terminal illness who wish to die at home. The preferences of the general public and people with a terminal illness seem to support this, as most people indicate that they would prefer to receive end‐of‐life care at home.
Objectives
We systematically reviewed the literature to see if the provision of end‐of‐life home‐based care reduced the likelihood of dying in hospital and what effect this has on patients' and caregivers' satisfaction and health service costs, compared with being admitted to a hospital or hospice. This is the fourth update of the original review.
Study characteristics
We searched the literature until April 2015 and found no new trials for this update. We found four trials for the previous updates.
Main results
We included four trials in our review and report that people receiving end‐of‐life care at home are more likely to die at home. It is unclear whether home‐based end‐of‐life care increases or decreases the probability of being admitted to hospital. Admission to hospital while receiving home‐based end‐of‐life care varied between trials. People who receive end‐of‐life care at home may be slightly more satisfied after one month and less satisfied after six months. It is unclear whether home‐based end‐of‐life care reduces or increases caregiver burden. Healthcare costs are uncertain, and no data on costs to participants and their families were reported.
Authors' conclusions
People who receive end‐of‐life care at home are more likely to die at home. There were few data on the impact of home‐based end‐of‐life services on family members and lay caregivers.
Summary of findings
Summary of findings for the main comparison. Summary of findings table for main outcomes.
| Participant outcomes for home‐based end‐of‐life care | ||||||
|
Patient or population: terminally ill people
Settings: Norway, UK, USA
Intervention: home‐based end‐of‐life care Comparison: a combination of services that could include routine (not specialised) home care, acute inpatient care, primary care services, and hospice care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Home‐based end‐of‐life care | |||||
| Place of death (home) Follow‐up: 6 to 24 months | Study population | RR 1.33 (1.14 to 1.55) | 652 (3 studies) | ⊕⊕⊕⊕ high | In 1 trial, eligible participants were assigned treatment according to the district (cluster) in which they lived | |
| 444 per 1000 | 591 per 1000 (506 to 688) | |||||
|
Difference: 147 more (62 to 244 more) | ||||||
| Medium‐risk population | ||||||
| 510 per 1000 | 678 per 1000 (581 to 790) | |||||
|
Difference: 168 more (71 to 280 more) | ||||||
|
Admission to hospital Follow‐up: 6 to 24 months |
Estimates ranged from a relative increase in risk of admission to hospital of 2.61 to a relative reduction in risk of 0.62 | 823 (4 studies) |
⊕⊕⊕⊝ moderate1 |
Data were not pooled due to the high degree of statistical heterogeneity for this outcome | ||
|
Patient satisfaction Follow‐up: 1 to 6 months |
A small increase in satisfaction for those receiving end‐of‐life care at home reported at 1 month, and reduced at 6 months | 199 (2 studies) |
⊕⊕⊝⊝2 low |
Satisfaction measured using questions derived from the US National Hospice Study and the Reid‐Gundlach Satisfaction with Services instrument (minimum low score 1, high score 5) | ||
|
Caregiver burden Follow‐up 6 months |
One study demonstrated a reduction in psychological well‐being for caregivers of participants who had survived more than 30 days, and a second study reported little or no difference in caregiver response to bereavement | 155 (2 studies) |
⊕⊕⊝⊝2 low |
Measured by the Philadelphia Geriatric Center Morale Scale and the Texas Revised Inventory of Grief | ||
| Health service cost | A reduction in total health service cost was reported for those participants receiving end‐of‐life care at home (range from a 18% to 30% reduction) | 2 studies | ⊕⊕⊝⊝3 low |
|||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | ||||||
1We downgraded the certainty of the evidence due to inconsistency of findings among studies.
2We downgraded the certainty of the evidence as different measures were used, and only two out of the four included studies reported data for these outcomes.
3We downgraded the certainty of evidence due to inconsistency of findings among studies, studies reporting different healthcare resources, and only two out of four included studies reporting data for this outcome.
Background
Description of the condition
Surveys of the preferences of the general public and terminally ill people report a growing consensus that, given adequate support, most people would prefer to receive end‐of‐life care at home (Department of Health 2008; Gomes 2012; Higginson 2000). The preference of patients who do not have caregivers is less clear. While a policy supporting choice is broadly endorsed (Agelopoulos 2009; Department of Health 2008), it brings with it conceptual and methodological difficulties for those evaluating the effectiveness of these types of services, and further challenges to those responsible for implementing these interventions, due to patient and caregiver preference changing over time.
Description of the intervention
End‐of‐life care at home is the provision of a service that provides active treatment for continuous periods of time by healthcare professionals in the patient's home for patients who would otherwise require hospital or hospice inpatient end‐of‐life care.
How the intervention might work
The rationale for providing end‐of‐life care at home is complex as it reflects the policy objective of providing patients and their families with a choice of where and when they want care. One difficulty underpinning the concept of choice in this context is that while more people want to die at home, they also recognise the practical and emotional difficulties of exercising this choice. For example, terminally ill people express concern about being a 'burden' to family and friends and worry about their families seeing them in distress or having to get involved with intimate aspects of care (Gott 2004). Similarly, although caregivers of terminally ill people often prefer to care for their relatives at home (Woodman 2015), continuity of care may be difficult to achieve, and yet is essential to fulfil the choice of dying at home (Seamark 2014).
Why it is important to do this review
In some countries, namely the US and Canada, the number of people dying at home has increased (Decker 2006; Wilson 2009), whereas in others, for example Italy and Japan, it has decreased. A retrospective cohort study of Taiwanese patients who died of cancer reported a decrease in the proportion of patients dying at home from 36% to 32%, due to access to treatments that were only available in hospital palliative‐care settings (Tang 2010). Although recent data indicate a small increase in the number of people who have died at home in the UK, it was estimated that in 2008 18% of deaths were at home and 58% were in hospitals (Department of Health 2008), and in 2013 22% of people died at home, 22% died in care homes, 6% in hospices, and 48% in hospital (NEoLCIN 2014). The reduction in the proportion of people dying in hospital could be attributed, at least in part, to the improvements in care and services as a result of the 2008 National End of Life Care Strategy (Department of Health 2008). Explanations for the large proportion of people still dying in hospital include poorly co‐ordinated services with variable provision, making it difficult for people to be transferred between settings (National Audit Office 2008). Improved collaboration between health and social care, and acute and community services, could improve the quality of care, reduce emergency admissions, and allow more people to die in the place of their choosing (National Audit Office 2008). Importantly, although between 30% and 90% of people die in their preferred death place, the likelihood of doing so decreases if they had chosen home (Bell 2010). This is the fourth update of the original review.
Objectives
To determine if providing home‐based end‐of‐life care reduces the likelihood of dying in hospital and what effect this has on patients' symptoms, quality of life, health service costs, and caregivers compared with inpatient hospital or hospice care. We addressed the following questions:
Are people who receive end‐of‐life care at home more likely to die at home than those who are allocated to inpatient hospital or hospice care?
Do people receiving end‐of‐life care at home have an increased risk of unplanned or precipitous admission to hospital?
Do people who receive end‐of‐life care at home have better symptom control than those who are allocated to inpatient hospital or hospice care?
Does patient and caregiver satisfaction differ between end‐of‐life care at home and inpatient hospital care?
Does providing end‐of‐life care at home alter the costs to health services?
Methods
Criteria for considering studies for this review
Types of studies
We included the following types of studies:
Randomised controlled trials
Interrupted time series
Controlled before and after studies
The inclusion of study designs other than randomised controlled trials is supported by the small number of randomised trials conducted within this research topic, which in turn is explained by obstacles to recruitment and high attrition, amongst other factors (Higginson 2013). We excluded controlled before and after studies with fewer than two intervention sites and two control sites. We also excluded interrupted time series without a clearly defined point in time when the intervention occurred and at least three data points before and three after the intervention.
Types of participants
We included evaluations of end‐of‐life care at home for people, aged 18 years and over, who are at the end of life and require terminal care.
Types of interventions
We included studies comparing end‐of‐life care at home with inpatient hospital or hospice care. The end‐of‐life care at home (which may be referred to as terminal care at home, hospital at home, or hospice at home) studies could include people referred directly from the community who therefore have no physical contact with the hospital, or those referred from the emergency room or hospital inpatient services. We used the following definition to determine if studies should be included in the review: end‐of‐life care at home is a service that provides active treatment for continuous periods of time by healthcare professionals in the patient's home for patients who would otherwise require hospital or hospice inpatient end‐of‐life care.
Types of outcome measures
Main outcomes
Place of death
Unplanned/precipitous admission to or discharge from hospital
Other outcomes
Control of symptoms (pain, breathlessness, nausea and vomiting, constipation, terminal agitation)
Delay in care (medical, nursing, or domiciliary care) from point of referral to intervention (end‐of‐life home care/hospice at home or inpatient care)
Participant health outcomes, including patient‐reported outcomes such as functional status and patient satisfaction
Family‐ or caregiver‐reported symptoms, including stress and anxiety
Family or caregiver unable to continue caring
Participant's preferred place of death
Health service use, including system and caregiver costs
Search methods for identification of studies
Electronic searches
We searched the following databases until April 2015: the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library), Ovid MEDLINE(R) (from 1950), EMBASE (from 1980), CINAHL (from 1982), and EconLit (from 1969). We have provided full details of the search terms used in Appendix 1.
Searching other resources
We checked the reference lists of articles identified electronically for evaluations of end‐of‐life home‐based care and obtained potentially relevant articles. We searched clinical trials registries ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform (http://www.who.int/ictrp/en/) for potentially relevant ongoing trials under the headings 'palliative care' and 'hospital at home', respectively. We searched the online database PDQ‐Evidence to identify other systematic reviews and their primary studies. We handsearched palliative care journals indexed by ISI Web of Science for online first references and current issues (American Journal of Hospice and Palliative Medicine; BMC Palliative Care; BMJ Supportive & Palliative Care; Journal of Palliative Medicine; Palliative Medicine; Palliative & Supportive Care). We sought unpublished studies by contacting providers and researchers known to be involved in this field. We developed a list of contacts using the existing literature and following discussion with researchers in the area.
Data collection and analysis
Selection of studies
One review author (DCGB or SS) read all the abstracts in the records retrieved by the electronic searches in order to identify publications that appeared to be eligible for this review, screened the relevant trials retrieved by the clinical trials registry as well as the identified systematic review, and handsearched relevant publications in palliative care. Two review authors (DCGB and SS) independently read the publications that appeared to be eligible and selected studies for the review according to the prespecified inclusion criteria. We resolved any disagreements by discussion.
Data extraction and management
For the previous updates, two review authors (SS and BW or SS and SES) completed data extraction independently using a checklist developed by Effective Practice and Organisation of Care (EPOC), modified and amended for the purposes of this review (EPOC 2010). The current update did not identify any new trials.
Assessment of risk of bias in included studies
Two review authors (SS and BW or SS and SES) independently assessed risk of bias in included studies using the Cochrane 'Risk of bias' criteria (Higgins 2011).
Unit of analysis issues
The study by Jordhøy 2000 was a cluster‐randomised trial; this was taken into account in the published analysis for some of the outcomes by testing the significance of differences between treatment groups using bootstrap estimation to fit regression models, allowing for clustering (Jordhøy 2000). For the outcomes place of death and admission to hospital, Jordhøy 2000 reported no confidence intervals, therefore we adjusted the data entered into the meta‐analysis using an estimate of the intra‐correlation coefficient (ICC) of 0.02; we obtained this from the Aberdeen database of ICCs (http://www.abdn.ac.uk/hsru/research/research‐tools/study‐design). This was a post‐hoc decision. We contacted the authors of this study for an estimate of the ICC but have not received the data.
Assessment of heterogeneity
We quantified heterogeneity using Cochrane's Q and the I2 statistic, the latter quantifying the percentage of the total variation across studies that is due to heterogeneity rather than chance (Cochrane 1954; Higgins 2003); smaller percentages suggest less observed heterogeneity. Statistical significance throughout was taken at the two‐sided 5% level (P < 0.05) and data were presented as the estimated effect with 95% confidence intervals. When combining outcome data was not possible because of differences in the reporting of outcomes, we reported the findings of the individual studies.
Data synthesis
We combined the published data for dichotomous outcomes using fixed‐effect Mantel‐Haenszel meta‐analysis (Bradburn 2007). The pooled effect is expressed as a risk ratio for end‐of‐life home‐based care compared with usual hospital care; values greater than 1 indicate outcomes favouring end‐of‐life care at home, and less than 1 for other outcomes.
We created a summary of findings table using the following outcomes: place of death; hospital admission; patient satisfaction; and caregivers outcomes. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and risk of bias) to assess the certainty of the evidence as it relates to the main outcomes (Guyatt 2008). We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We justified all decisions to down‐ or up‐grade the certainty of evidence using footnotes to aid readers' understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
We did not plan a priori subgroup analysis and did not perform post hoc subgroup analysis.
Sensitivity analysis
We did not plan a priori sensitivity analysis and did not perform post hoc sensitivity analysis.
Results
Description of studies
Results of the search
For this update, we retrieved 2344 references, from which we identified 11 potentially relevant references. Full‐text assessment indicated that nine studies did not fulfil the inclusion criteria, and we excluded those references. The main reason for exclusion was that the intervention was not home‐based end‐of‐life care. The other two references are one ongoing trial (NCT01885637), and one trial that is currently awaiting classification (NTR2817). We did not identify any new studies (Figure 1).
1.
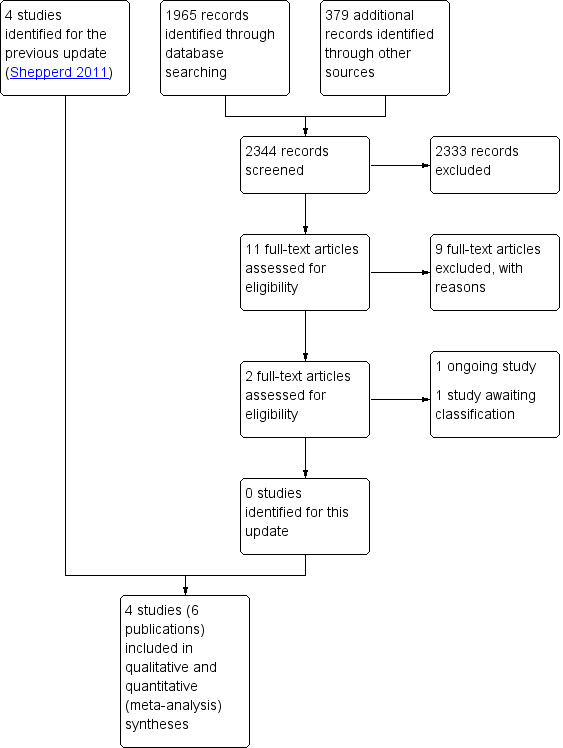
Study flow diagram.
Included studies
We identified four published trials (six publications), three trials where the participant was randomised and one cluster‐randomised trial, for inclusion in this review (Brumley 2007; Grande 2000; Hughes 1992; Jordhøy 2000). Two of the randomised controlled trials were conducted in the US (Brumley 2007; Hughes 1992), one in Norway (Jordhøy 2000), and one in the UK (Grande 2000).
The mean age of participants ranged from 63 years to 74 years, with similar proportions of male and female participants. Between 17% and 36% of participants lived alone (Brumley 2007; Grande 2000; Jordhøy 2000). The diagnosis of trial participants varied. In one trial, conducted in the US, 21% of participants had a diagnosis of late‐stage chronic obstructive pulmonary disease, 33% of heart failure, and 47% of cancer, with an estimated life expectancy of 12 months or less (Brumley 2007). The most common diagnosis in the second trial conducted in the US was cancer, with 73% in the intervention group and 80% in the control group having this diagnosis (Hughes 1992). In Grande 2000, conducted in the UK, 86% of participants had a diagnosis of cancer, and the survival from referral was a median of 11 days. The Jordhøy 2000 trial, conducted in Norway, recruited participants with incurable malignant diseases, excluding those with haematological malignant disease other than lymphoma.
The intervention in three trials was multidisciplinary care, which included specialist palliative‐care nurses, family physicians, palliative‐care consultants, physiotherapists, occupational therapists, nutritionists, and social care workers (Brumley 2007; Hughes 1992; Jordhøy 2000). In one trial the focus of the intervention was on nursing care, which was only available for the last two weeks of life (Grande 2000). In three trials, nursing care was available for 24 hours if required; in the trial conducted in Norway the smallest urban district did not have access to 24‐hour care. The intervention evaluated by Jordhøy 2000 was hospital‐based at the Palliative Medicine Unit, which provided community outreach. The intervention had four components:
all inpatient and outpatient hospital services were provided at the Palliative Medicine Unit unless care was required elsewhere for medical reasons;
the Palliative Medicine Unit served as a link to the community services, and the palliative‐care physician and community nurse were defined as the main caregivers;
predefined guidelines were used to keep optimal interaction between services; and
community professionals were offered an educational programme that included bedside training and six to 12 hours of lectures every six months. The lectures addressed the most frequent symptoms and difficulties in palliative care.
Follow‐up consultations were with the community staff. In one trial, the intervention group had access to input available to the control group (that is care was supplemented by general practitioner and other community care when less than 24‐hour hospital at home input was provided) (Grande 2000).
Participants received end‐of‐life care at home for a maximum of 14 days in the trial by Grande 2000 and for an average of 68 days in the trial by Hughes 1992. The other two trials did not report duration of care (Brumley 2007; Jordhøy 2000); although survival time was reported, it was not possible to link survival time to duration of the intervention as participants moved between care settings.
Two trials described an educational component. In one, this was for the participants and their families and included identifying goals of care and the expected course of the disease and outcomes, as well as the likelihood of success of various treatments (Brumley 2007). In the other trial, an educational programme was provided for community staff (Jordhøy 2000). In two trials, the service was co‐ordinated by a nurse (Grande 2000; Jordhøy 2000); one was physician‐led (Hughes 1992), and in one a core team of physician, specialist nurse, and social worker managed care across settings and provided assessment, evaluation, planning, care delivery, follow‐up, monitoring, and continuous reassessment of care (Brumley 2007).
The care that the control group received varied across trials and thus reflected differences in health systems and the way that standard care is delivered. In two trials, this was described as including home care (though not specialised end‐of‐life care), acute inpatient care, primary care services, and inpatient hospice care (Brumley 2007; Grande 2000). In one trial, the control group received inpatient care at a Veterans Administration (VA) hospital (Hughes 1992), and in another trial conventional care was shared among the hospital departments and the community, with no well‐defined practice (Jordhøy 2000) (see Characteristics of included studies).
Excluded studies
We excluded nine trials, five of which reported an intervention that did not provide home‐based end‐of‐life care or was not an alternative to inpatient hospital or hospice care (Brännström 2014; Brumley 2003; Holdsworth 2015; Hughes 1990; Hughes 2000), and three that did not fulfil the criterion for study design (Enguidanos 2005; McCusker 1987; McWhinney 1994). For one of the trials, we could not locate outcome data or details of the control group, as this information was only reported as an abstract; we contacted the authors for these details but did not receive a reply (Stern 2006) (see Characteristics of excluded studies).
Risk of bias in included studies
Allocation
Two trials clearly described the method of randomisation and allocation (Brumley 2007; Grande 2000).
Blinding
Blinding was not possible in any of the trials.
Incomplete outcome data
No trials reported loss of follow‐up data for place of death; there was up to 25% loss to follow‐up in trials assessing patient satisfaction.
Selective reporting
There was no evidence of selective reporting of outcome data in three of the trials (Grande 2000; Hughes 1992; Jordhøy 2000).
Other potential sources of bias
All four trials collected baseline data (Figure 2 and Figure 3).
2.
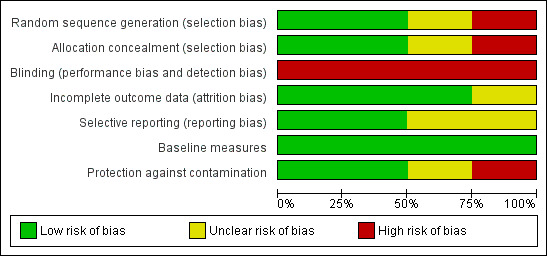
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
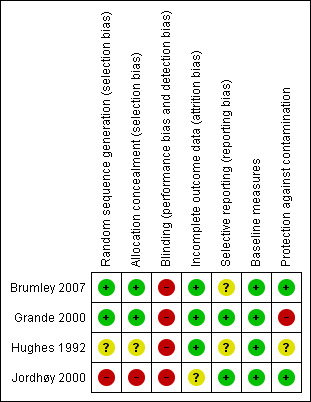
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Table 1
Place of death
We were able to combine data from three trials to assess the effectiveness of end‐of‐life home‐based care on dying at home. We found that home‐based end‐of‐life care increased the likelihood of dying at home compared with usual care, which included hospice care, inpatient care, and routinely available primary healthcare (risk ratio (RR) 1.33, 95% confidence interval (CI) 1.14 to 1.55, P = 0.0002; Chi2 = 1.72, df = 2, P = 0.42, I2 = 0%; 3 trials; N = 652; high quality evidence; Analysis 1.1). In one of the trials, 61% (n = 113/186) of participants allocated to end‐of‐life home‐based care actually received this form of care (Grande 2000); and 152/186 (82%) in the end‐of‐life home care group spent time at home in the last two weeks of life, compared with 34/44 (77%) in the usual care group (Analysis 1.2). One trial reported data on numbers dying in hospital (RR 1.12, 95% CI 0.82 to 1.52, P = 0.49; Analysis 1.3) and in a nursing home (RR 0.47, 95% CI 0.17 to 1.32, P = 0.15; Analysis 1.4; Analysis 1.5) (Jordhøy 2000).
1.1. Analysis.
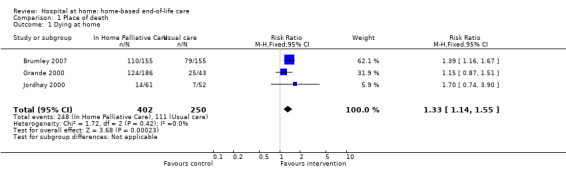
Comparison 1 Place of death, Outcome 1 Dying at home.
1.2. Analysis.
Comparison 1 Place of death, Outcome 2 Time spent at home in the last 2 weeks of life.
| Time spent at home in the last 2 weeks of life | |
|---|---|
| Study | |
| Grande 2000 | T= 152/186 (82%), C= 34/44 (77%), P = 0.46 |
1.3. Analysis.
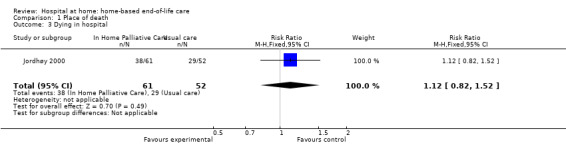
Comparison 1 Place of death, Outcome 3 Dying in hospital.
1.4. Analysis.
Comparison 1 Place of death, Outcome 4 Dying in a nursing home.
| Dying in a nursing home | |
|---|---|
| Study | |
| Jordhøy 2000 | T= 19/235 (9%), C= 36/199 (21%), P = 0.01 |
1.5. Analysis.
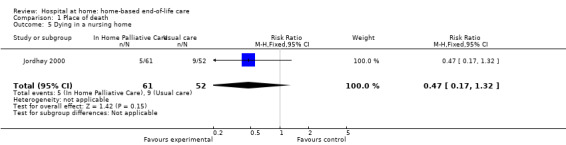
Comparison 1 Place of death, Outcome 5 Dying in a nursing home.
Unplanned/precipitous admission to or discharge from hospital
Four trials assessed the effectiveness of end‐of‐life home‐based care on this outcome. We initially combined data from all four trials for this outcome (RR 0.93, 95% CI 0.82 to 1.05; Analysis 2.1); however, due to a high level of statistical heterogeneity (Chi2 = 25.63, df = 3, P < 0.0001, I2 = 88%), we have not retained this analysis. The RR ranged from RR 0.62 to RR 2.61 (4 trials; N = 823; moderate quality evidence).
2.1. Analysis.
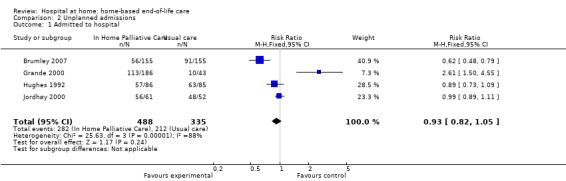
Comparison 2 Unplanned admissions, Outcome 1 Admitted to hospital.
Control of symptoms
One trial reported on control of symptoms. Grande 2000 obtained participant outcome data from general practitioners, district nurses, and informal caregivers, as previous attempts to obtain data directly from participants proved unsuccessful (Analysis 3.1; Analysis 3.2). Outcomes focused on the need for additional support with care and symptoms (pain, nausea/vomiting, constipation, diarrhoea, breathlessness, anxiety and depression), and assessments varied by assessor. For example, there was a small difference in caregivers' assessment of pain control (mean difference (MD) ‐0.48 points on a 4‐point scale, 95% CI ‐0.93 to ‐0.03), whereas general practitioners reported little or no difference (MD ‐0.32, 95% CI ‐0.68 to 0.04) (low quality evidence). The assessments of depression and anxiety also differed between general practitioners (depression MD on a 4‐point scale ‐0.6, 95% CI ‐0.90 to ‐0.20; anxiety MD on a 4‐point scale ‐0.40, 95% CI ‐0.80 to ‐0.02) and caregivers (depression MD 0.15, 95% CI ‐0.41 to 0.71; anxiety MD ‐0.05, 95% CI ‐0.62 to 0.52) (low quality evidence) (Grande 2000).
3.1. Analysis.
Comparison 3 Control of symptoms, Outcome 1 Caregivers' ratings of symptoms.
| Caregivers' ratings of symptoms | ||
|---|---|---|
| Study | Outcomes | Notes |
| Grande 2000 |
Pain, mean SD T= 2.49 (0.92), C= 3.12 (1.05), P = 0.02 Nausea/vomiting, mean SD T= 1.91 (0.87), C= 2.47 (1.07), P = 0.06 Constipation, mean SD T= 2.32 (1.09), C= 2.50 (0.97), P = 0.51 Diarrhoea, mean SD T= 1.49 (0.88), C= 1.60 (0.98), P = 0.69 Breathlessness, mean SD T= 2.39 (1.17), C= 2.21 (1.19), P = 0.70 Anxiety, mean SD T= 2.45 (1.05), C= 2.50 (1.10), P = 0.10 Depression, mean SD T= 2.08 (0.97), C= 1.93 (1.14), P = 0.65 |
4‐point scale completed by the care giver. Lower score indicates less of a problem. |
3.2. Analysis.
Comparison 3 Control of symptoms, Outcome 2 GPs' ratings of symptoms.
| GPs' ratings of symptoms | ||
|---|---|---|
| Study | Outcomes | Notes |
| Grande 2000 |
Pain, mean SD T= 2.03 (0.73), C= 2.35 (0.95), P = 0.09 Nausea/vomiting, mean SD T= 1.78 (0.82), C= 2.00 (1.02), P = 0.28 Constipation, mean SD T= 1.81 (0.78), C= 1.97 (0.94), P = 0.45 Diarrhoea, mean SD T= 1.17 (0.49), C= 1.36 (0.73), P = 0.20 Breathlessness, mean SD T= 1.82 (1.01), C= 1.66 (0.93), P = 0.42 Anxiety, mean SD T= 2.10 (0.95), C= 2.50 (0.97), P = 0.05 Depression, mean SD T= 1.62 (0.76), C= 2.19 (1.08), P = 0.01 |
Intention to treat 4‐point scale completed by the GP Lower score indicates less of a problem. No difference was detected for the ratings reported by district nurses and informal care givers |
Delay in care
None of the studies reported on delay in care.
Participant health outcomes
Participant health outcomes included patient‐reported outcomes, such as functional status and well‐being; patient satisfaction; and mortality. Home‐based end‐of‐life care may make little difference to functional status (measured by the Barthel Index), psychological well‐being, or cognitive status (1 trial; N = 168; low quality evidence; Analysis 4.1, Analysis 4.2, Analysis 4.3) (Hughes 1992). Home‐based end‐of‐life care may slightly increase patient satisfaction (2 trials; low quality evidence; Analysis 4.4). Participants receiving end‐of‐life home‐based care reported greater satisfaction than those in the hospital group at one‐month follow‐up (Hughes 1992). This difference disappeared at six‐months follow‐up, which may reflect a reduced sample size due to the death of a number of these participants. Brumley 2007 reports similar findings, with greater satisfaction reported by those receiving end‐of‐life home‐based care at 30 days (odds ratio (OR) 3.37, 95% CI 1.42 to 8.10) and greater uncertainty at 60 days (OR 1.79, 95% CI 0.65 to 4.96) (Brumley 2007). It is unclear whether end‐of‐life home‐based care has an effect on six‐month mortality (MD 1.4, 95% CI ‐10.9 to 13.7; Analysis 4.5) (Hughes 1992). Home‐based end‐of‐life care may make little to no difference for survival time from referral (Analysis 4.6) (Brumley 2007; Grande 2000; Jordhøy 2000).
4.1. Analysis.
Comparison 4 Participant health outcomes, Outcome 1 Functional status.
| Functional status | ||
|---|---|---|
| Study | Outcomes | Notes |
| Hughes 1992 | At 6 months, mean T= 72 (n=18) C= 69.31 (n=16) | High attrition in both groups due to death. The Barthel Self‐Care Index with modified scoring system was used. No P value given, insufficient data to calculate CI |
4.2. Analysis.
Comparison 4 Participant health outcomes, Outcome 2 Psychological well‐being.
| Psychological well‐being | ||
|---|---|---|
| Study | Outcomes | Notes |
| Hughes 1992 | At 6 months, mean T= 1.54 (n=17) C= 1.57 (n=14) | High attrition in both groups due to death. Philadelphia Geriatric Morale Scale used (shortened version). No P value given, insufficient data to calculate CI |
4.3. Analysis.
Comparison 4 Participant health outcomes, Outcome 3 Cognitive status.
| Cognitive status | ||
|---|---|---|
| Study | Outcomes | Notes |
| Hughes 1992 | At 6 months, mean T= 8.33 (n=18) C= 8.86 (n=14) | High attrition in both groups due to death. Short Portable Mental Status Questionnaire used (10 items). No P value given, insufficient data to calculate CI |
4.4. Analysis.
Comparison 4 Participant health outcomes, Outcome 4 Patient satisfaction.
| Patient satisfaction | ||
|---|---|---|
| Study | Outcomes | Notes |
| Brumley 2007 | At 30 days OR = 3.37, 95% CI = 1.42‐8.10 (n=216) At 60 days OR= 1.79, 95% CI 0.65 to 4.96 (n=168) |
Satisfaction measured by the Reid‐Gundlack Satisfaction with Service instrument |
| Hughes 1992 | At one month: P = .02 At 6 months, mean T= 2.72 (n=17), C= 2.45 (n=14) | 17 item questionnaire derived from the National Hospice Study No P value reported, insufficient data to calculate CI. |
4.5. Analysis.
Comparison 4 Participant health outcomes, Outcome 5 Mortality.
| Mortality | |
|---|---|
| Study | |
| Hughes 1992 | At 6 month, proportion (percentage) T= 68/86 (79.1%), C= 66/85 (77.6%), difference 1.4, 95% CI ‐10.9 to 13.7 |
4.6. Analysis.
Comparison 4 Participant health outcomes, Outcome 6 Survival time from referral to death.
| Survival time from referral to death | |
|---|---|
| Study | |
| Brumley 2007 | Days, mean (SD) T= 196 (164), C= 242 (200), P = 0.03 |
| Grande 2000 | Treatment group (allocated and admitted to hospital at home): median 16 days Allocated and not admitted to hospital at home: median 8 days Z = 3.005, P = 0.003 |
| Jordhøy 2000 | Days, median (95% CI) T= 99 (79 to 119), C= 127 (88 to 166) |
Caregiver‐reported outcomes
Two trials reported on caregiver outcomes (Grande 2004; Hughes 1992). In one trial caregivers of participants receiving end‐of‐life home‐based care reported higher satisfaction compared with caregivers in the control group at one‐month follow‐up (Analysis 5.1) (Hughes 1992). This difference disappeared at six months, which may reflect a reduced sample size. At six‐months follow‐up, caregivers of participants in the end‐of‐life home‐based care group who had survived more than 30 days reported a decrease in psychological well‐being compared with caregivers looking after participants in the control group (measured by the Philadelphia Geriatric Center Morale Scale). Grande 2004 found end‐of‐life care at home may make little or no difference for caregiver bereavement response six months following death (low quality evidence) (measured by the Texas Revised Inventory of Grief) (end‐of‐life care at home: mean 46.5 (standard deviation (SD) 12.9), control mean 46.8 (SD 11.8)). We are uncertain whether home‐based end‐of‐life care improves caregiver outcomes (2 trials; low quality evidence).
5.1. Analysis.
Comparison 5 Caregiver‐reported outcomes, Outcome 1 Caregiver satisfaction.
| Caregiver satisfaction | ||
|---|---|---|
| Study | Outcomes | Notes |
| Hughes 1992 | At 1 month: Carers in the treatment group reported a greater level of satisfaction At 6 months: NS | |
Family or caregiver unable to continue caring
No study reported on the caregiver's inability to continue caring.
Participant’s preferred place of death
No study reported on participant's preferred place of death.
Cost and use of other health services
Trials reported data for healthcare costs (Brumley 2007; Hughes 1992), health service use (Grande 2000; Hughes 1992), inpatient days (Hughes 1992; Jordhøy 2000), and number of inpatient days (Jordhøy 2000). Home‐based end‐of‐life care may slightly reduce healthcare cost (2 trials; low quality evidence; Analysis 6.1). One study reported total costs including VA hospital, private hospital, nursing home, outpatient clinic, home care, and community nursing (Hughes 1992); a second study reported costs including emergency department visits, physician office visits, hospital days, skilled nursing days, home health and palliative visits (including physician visits), and days in hospice (Brumley 2007). Hughes 1992 reported lower healthcare costs for those receiving end‐of‐life home care (mean cost USD 3479 versus mean cost USD 4248, P > 0.05); Brumley 2007 reported that the average cost per day incurred by those receiving end‐of‐life home‐based care was lower than for those receiving standard care (MD ‐117.50, P = 0.02), and that the overall mean cost (adjusted for survival, age, and severity of illness) to the health service was USD 12,670 (SD USD 12,523) compared with USD 20,222 (SD USD 30,026) for usual care. None of the studies reported costs incurred by the participants or the caregivers.
6.1. Analysis.
Comparison 6 Resource use and cost, Outcome 1 Cost.
| Cost | ||
|---|---|---|
| Study | Outcomes | Notes |
| Brumley 2007 | Controlling for survival, age, severity of illness and primary disease, adjusted mean cost (SD) T= $12,670 ($12,523) C= $20,222 ($30,026) Average cost per day incurred by those on intervention arm ($95.30) was significantly lower than that of comparator group ($212.80) (t = ‐2.417; P = 0.02) |
Service costs were calculated using actual costs for contracted medical services in Colorado and proxy cost estimates for all services provided within the HMO as services within the HMO are not billed separately. Costs were based on figures from 2002 Hospitalisation and emergency department cost estimates were calculated using aggregated data from more than 500,000 HMO patient records and include ancillary services such as laboratory and radiology. Costs of physician office visits included nurse and clerk expenses. Home health and palliative care visits were calculated using average time spent on each visit and multiplying that by the cost for each discipline’s reimbursement rate. Proxy costs generated for hospital days and emergency department visits were significantly lower than the actual costs received from contracted providers. Total cost variable was constructed by aggregating costs for physician visits, emergency department visits, hospital days, skilled nursing facility days and home health or palliative days accumulated from the point of study enrolment until the end of the study period or death |
| Hughes 1992 | 1986 prices (average costs) Home care T= $1,001, C=, P = 0.001 VA hospital T= $1,795, C= $3,434, P = 0.02 Cost of all institutional care T= 2341.79, C= $3757.37, P = 0.05 Total costs (VA hospital, private hospital, nursing home, outpatient clinic, home care, community nursing) T= $3,479.36, C= $4,248.68 | |
Hughes 1992 reported data on the use of healthcare services. Those receiving end‐of‐life home‐based care made fewer visits to outpatient clinics (difference 1.86, 95% CI ‐3.2 to ‐0.53, P = 0.01; Analysis 6.2), and the use of VA hospital beds was lower for participants allocated to end‐of‐life home‐based care compared with those allocated to hospital care (MD ‐5.9 days, 95% CI 0.78 to 11.00) (Hughes 1992). Jordhøy 2000 reported a small reduction in the number of inpatient days for participants receiving end‐of‐life home‐based care (MD ‐4.30, 95% CI ‐13.88 to 5.28) (Analysis 6.3; Analysis 6.4).
6.2. Analysis.
Comparison 6 Resource use and cost, Outcome 2 Health service use.
| Health service use | ||
|---|---|---|
| Study | Outcomes | Notes |
| Grande 2000 |
GP workload in penultimate week of life Evening home visits, mean (SD) T= 0.17 (0.46), C= 0.61 (1.42), Z = 2.295, P = 0.022 Night visits, mean (SD) T= 0.04 (0.20), C= 0.26 (0.55), Z = 3.61, P = 0.0003 GP workload in last week of life Evening home visits, mean (SD) T= 0.17 (0.46), C= 0.61 (1.42) Night time visits, mean (SD) T= 0.04 (0.2), C= 0.26 (0.55) Primary and secondary care services in last 2 weeks of life: failed to detect a difference |
|
| Hughes 1992 | VA services at 6 months Outpatient visits mean (SD) T= 0.73 (1.9), C= 2.59 (6.1), difference: 1.86, P = 0.01 | 95% CI not calculated as equal variances can not be assumed Comparisons were made with 13 other types of service, not reported. |
6.3. Analysis.
Comparison 6 Resource use and cost, Outcome 3 Inpatient days.
| Inpatient days | |
|---|---|
| Study | |
| Hughes 1992 | At 6 months
General bed days, mean (SD) T= 5.63 (10), C= 12.06 (15.2), mean difference 6.43 days (95% CI 2.55 to 10.3), P = 0.002 All VA hospital days, mean (SD) T= 9.94 (13.3), C= 15.86 (20.1), mean difference 5.92 (95% CI 0.78 to 11), P = 0.03 |
| Jordhøy 2000 | Nmber of inpatient days, mean (SD) T= 5.0 (17.3), C= 9.3 (31.4) |
6.4. Analysis.
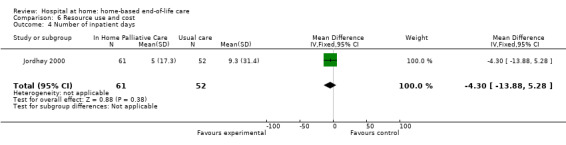
Comparison 6 Resource use and cost, Outcome 4 Number of inpatient days.
Staff views on the provision of services
Grande 2000 reported the views of general practitioners, district nurses, and informal caregivers in terms of the provision of services. District nurses reported that there should have been additional help for the caregivers looking after the participants (difference 0.45 on a 3‐point scale with lower scores indicating less of a problem, 95% CI 0.12 to 0.77), and that there should have been additional help with night nursing (difference ‐0.60 on a 3‐point scale with lower scores indicating less of a problem, 95% CI ‐0.86 to ‐0.34); this was an on‐treatment analysis (Analysis 7.1).
7.1. Analysis.
Comparison 7 Staff views, Outcome 1 District nurse views.
| District nurse views | ||
|---|---|---|
| Study | Outcomes | Notes |
| Grande 2000 | District nurse thought there should be additional help for the care giver, mean (SD) T= 1.81 (0.87) (n = 141), C= 1.36 (0.60) (n = 31), P = 0.005 District nurse thought there should be more help with night nursing T= 1.43 (0.64) (n = 143), C= 2.03 (0.84) (n = 33); P < 0.0001 |
3 point scale with lower scores indicating less of a problem
No difference was detected for the ratings reported by GPs and informal care givers. A 3 point scale with lower scores indicating less of a problem No difference was detected for the ratings reported by GPs and informal care givers. |
Discussion
Despite the widespread support for models of care that better serve the needs of patients at the end of their life, there is limited evidence supporting the effectiveness of home‐based end‐of‐life care. This is not surprising given the difficulties in conducting research in this area.
Summary of main results
Those participants receiving home‐based end‐of‐life care were more likely to die at home compared with those receiving usual care (high quality evidence); there was substantial variability among studies in admission to hospital during follow‐up (moderate quality evidence). The point in a participant's illness that end‐of‐life care at home was provided also varied between trials, as did the duration of care. For example, in one trial, median survival from recruitment was 11 days (Grande 2000), and in another it was 196 days (Brumley 2007). There was also considerable heterogeneity between trials regarding hospital admission while receiving home‐based end‐of‐life care. Home‐based end‐of‐life care may slightly increase patient satisfaction at one‐month follow‐up (low quality evidence). We are uncertain whether home‐based end‐of‐life care improves caregiver outcomes. Two of the four trials reported data on caregiver outcomes, with one of these trials reporting that caregivers of terminally ill people receiving home‐based end‐of‐life care experienced greater satisfaction than those receiving hospital care (low quality evidence) (Hughes 1992). However, caregivers experienced lower morale if the participant survived more than 30 days.
One trial (Hughes 1992), conducted in the US, examined cost in some detail and did not report differences in overall net health costs between end‐of‐life home‐based care and hospital care, although the use of VA hospital beds was lower for those receiving home‐based end‐of‐life care. A second trial (Brumley 2007), also conducted in the US, reported that the average cost per day incurred by those participants receiving home‐based care was lower than for those receiving standard care (low quality evidence). None of the studies reported on costs incurred by the participant or the caregiver.
Overall completeness and applicability of evidence
The included trials were conducted between 1992 and 2007; all were conducted in a high‐income country, with two in the US, one in the UK, and one in Norway. A total of 694 participants were recruited by three trials, and in one trial, three clusters were randomised (N = 434 participants). Around a quarter of participants lived alone. Participant survival times varied, indicating that they were recruited at different stages of their illness. In Grande 2000, participants had a median survival of 11 days from referral; participants recruited to the cluster trial in Norway had an estimated life expectancy of between two and nine months (Jordhøy 2000); and participants in the trial conducted in the US had a life expectancy of 12 months or less (Brumley 2007). Admissions to hospital also varied, which may be explained by the different healthcare systems, the configuration of existing community‐based services, and support provided to caregivers. Despite these differences, the evidence does support the implementation of home‐based end‐of‐life care programmes with access to 24‐hour care to support more people dying at home.
We do not anticipate the effects of the intervention to differ for disadvantaged populations (Dans 2007). Although all trials were conducted in high‐income countries, more than one‐third of the participants included in one trial, Brumley 2007, and about 10% of those recruited to another trial, Hughes 1992, belonged to an ethnic minority group. No subgroup analyses were reported for those participants.
Quality of the evidence
The quality, or certainty, of the evidence included in this review reflects the difficulties in conducting research in this area. Trials were unblinded, and participants crossed over between intervention and control groups. In addition, measuring symptoms and quality of life is difficult, and may have to be done by a proxy (for example a nurse, doctor, or caregiver). Each of these groups can form different impressions, which are then reflected in their assessments of the participant (Grande 2000). There is a risk that some of the results may have occurred by chance, as several of the studies conducted a large number of statistical tests. Finally, and most importantly, there are ethical concerns with randomising people at the end of their life rather than letting them exercise their choice of where they want to be cared for.
Potential biases in the review process
Only one review author reviewed the abstracts and applied the inclusion criteria to produce a long list of potentially eligible studies. Two review authors independently applied eligibility criteria and assessed these studies for inclusion, extracted data, and evaluated the scientific quality. We identified only one abstract of an ongoing trial (Stern 2006), and did not identify subsequent publication of these trial results. We did not identify any unpublished randomised data to include in this review, therefore there is a risk that we have excluded studies that could contribute to this review.
Agreements and disagreements with other studies or reviews
Previous systematic reviews include one published by Smeenk 1998, which compared home‐care programmes for people with incurable cancer to routinely available home care. This review excluded studies in which the control group received hospital care. In addition to noting the poor descriptions of the intervention and control groups' care, Smeenk 1998 reported that the evidence supporting home‐care programmes is inconclusive. Zimmermann 2008 published a systematic review of specialised palliative care across a range of settings. They also concluded that methodological limitations contribute to a weak evidence base. Luckett 2013 assessed to what extent home nursing increased the likelihood of dying at home, similarly concluding that the existing evidence precluded definitive recommendations.
Authors' conclusions
Implications for practice.
Unless major changes are made to the way services are provided, a growing ageing population will have an impact on the number of people dying in hospital (Gomes 2008). The evidence included in this review supports the use of home‐based end‐of‐life care programmes for increasing the number of people who will die at home, although the numbers of people being admitted to hospital and the time spent at home while receiving end‐of‐life care should be monitored, to ensure that the required support is available. The organisation of home‐based end‐of‐life care will depend on the configuration of existing services, as caring for more patients at home will place additional demands on primary care. For example, the trial in Norway concluded that a service with restrictive night services and staff with no specific training in palliative care limited the number of patients who could be admitted. The authors suggest that a more advanced and extensive home‐based end‐of‐life care service may be necessary to substantially increase the proportion of days in home care (Jordhøy 2000). The model of end‐of‐life care evaluated by Grande 2000 restricted end‐of‐life care to two weeks; this could have led to difficulties in withdrawing a service if a patient had not died within the two‐week time frame. All of the trials included in this review highlighted the need for access to 24‐hour care. There are examples of innovative models of care, several of which use a whole‐systems approach. In the UK there are the Midhurst Macmillan Specialist Palliative Care Service and the Marie Curie Delivering Choice Programme (Noble 2015). The latter programme includes community service models that provide 24‐hour care and aim to strengthen co‐ordination between services (Agelopoulos 2009). In Italy, a hospital‐based home palliative‐care programme implemented between 2009 and 2011 provided care to more than 11,000 patients, with 75% of deaths occurring at home by its final year (Masella 2015). The authors also noted that the involvement of primary healthcare workers was essential for the success of their programme.
Implications for research.
Given that the average age at death is predicted to increase and that those dying are likely to have increasingly complex comorbidities (Gomes 2008), attention should be given to testing different models of end‐of‐life home‐based care. A patient preference design comparing different models could be considered, but may limit patient numbers and further reduce the generalisability of the results (Grande 2000). Prospective audit with robust methods of data collection to document patients' transfer between care settings also has a place. The Methods Of Researching End of life Care (MORECare) statement provides evidence‐based guidance on how to design and conduct research on end‐of‐life care, suggesting how observational data and natural experimental methods can be integrated within more traditional randomised controlled trial designs (Higginson 2013). Key research outcomes should include facilitating patient choice, place of death, the control of patients' symptoms, transfer to other care settings, impact on healthcare resources, and caregiver burden. The burden on caregivers can be substantial, as they provide assistance with a complex range of care needs (Kleinman 2009). This burden can contribute to psychological and physical morbidity. The lack of precision around estimates of admission, or readmission, to hospital could have a major bearing on cost. This needs to be addressed, given the high costs of care at the end of life in high‐income countries.
Feedback
Feedback on review, 5 December 2012
Summary
I would like to draw attention to some fundamental errors in this review.
The review states that "Studies comparing end of life care at home with inpatient hospital or hospice care are included". Surely, this means that in an included controlled trial, one arm is allocated to home care, and one arm to in‐hospital or in‐hospice care, at the point of admission or for early discharge during an admission. As the authors state "We used the following definition to determine if studies should be included in the review: end of life care at home is a service that provides active treatment for continuous periods of time by healthcare professionals in the patient's home for patients who would otherwise require hospital or hospice inpatient end of life care."
However, in none of the included studies is this the case. All studies are comparing different intensities of home care services, sometimes specialist inpatient units are also part of the intervention, with both intervention and control groups able to use hospital or hospice services.
This is what the articles say:
1. Grande GE:
Intervention (BMJ article):
Hospital at home provides practical home nursing care for up to 24 hours a day for up to two weeks. The service was used mainly for terminal care during the last two weeks of life. The hospital at home team consisted of six qualified nurses, two nursing auxiliaries, and a nurse coordinator.
Agency nurses were also used as required.
Both patients allocated to hospital at home and control patients could receive the standard care services provided in the district. The intervention group, however, could also receive hospital at home. Thus the trial compared hospital at home and standard care versus standard care only.
Standard care comprised care in hospital or hospice or care at home with input from general practice, district nursing, Marie Curie nursing, Macmillan nursing, evening district nursing, social services, a flexible care nursing service, or private care.
Or in their Palliative Medicine article: Both CHAH and control patients could receive the standard care provided locally. This included care in hospital or hospice, or care at home with input from GP, district nursing, Marie Curie nursing, Macmillan nursing, evening district nursing, Social Services, private care and a Flexible Care nursing service. The latter was a home nursing service, similar to Marie Curie nursing, but funded by the community NHS Trust and available to all diagnostic groups. Thus the trial compared CHAH and standard care with standard care only.
2. Hughes
"The Edward Hines, Jr. VA Hospital has had a Hospital‐Based Home Care (HBHC) program since 1971....(the primary aim of the study was about cost but) we also sought to compare the attributes of the Hines model of care with traditional community home care services to which control group patients could be referred."
3. Jordhoy
Conventional care is shared among the hospital departments and the community, according to diagnosis and medical needs. No well‐defined routines exist.
Palliative‐care intervention: The Palliative Medicine Unit has 12 inpatient beds, an outpatient clinic, and a consultant team that works in and out of the hospital.... We compared the palliative‐care intervention with conventional care (control).
4. Brumley
This was a randomized, controlled trial conducted at two separate managed care sites to test the replicability and the effectiveness of an In‐home Palliative Care (IHPC) program.... Each patient enrolled in the intervention arm received customary and usual standard care within individual health benefit limits in addition to the IHPC program.... Usual care consisted of standard care to meet the needs of the patients and followed Medicare guidelines for home healthcare criteria.
There would seem to me to be a major lack of understanding of what Hospital at Home means.
Could you please inform me of how the Cochrane Collaboration will address these major flaws?
Submitter agrees with default conflict of interest statement:
I work in a public hospital and in a public hospital in the home unit. I am also President of the Hospital in the Home Society of Australasia, which is a not for profit organisation.
Gideon Caplan
Occupation Director, Post Acute Care Services
Reply
Response: As we mention in the discussion of our systematic review, conducting research in the area of end of life care is complex. One of the difficulties is that the care needs and preferences for place of death 1 of people approaching the end of their life can change rapidly; as a result they may require care from different groups of healthcare professionals and in different settings. In the trials included in our systematic review this resulted in a cross over between intervention and control groups (mentioned in the discussion of this systematic review). Finally, and most importantly, there are ethical concerns with not allowing people approaching the end of their life to choose where they want to be cared for. An added challenge for a systematic review in this area is that the evidence cuts across different health systems, again something we mention in the discussion: ‘the care that the control group received varied across trials and thus reflected differences in health systems and the way standard care is delivered.’
1Munday D, Petrova M, Dale J. Exploring preferences for place of death with terminally ill patients: qualitative study of experiences of general practitioners and community nurses in England. BMJ 2009; 338: b2391 doi:10.1136/bmj.b2391
Our response to the points you make for each of the included studies is below.
Feedback: 1. Grande GE:
Intervention (BMJ article):
Hospital at home provides practical home nursing care for up to 24 hours a day for up to two weeks. The service was used mainly for terminal care during the last two weeks of life. The hospital at home team consisted of six qualified nurses, two nursing auxiliaries, and a nurse coordinator. Agency nurses were also used as required.
Both patients allocated to hospital at home and control patients could receive the standard care services provided in the district. The intervention group, however, could also receive hospital at home. Thus the trial compared hospital at home and standard care versus standard care only. Standard care comprised care in hospital or hospice or care at home with input from general practice, district nursing, Marie Curie nursing, Macmillan nursing, evening district nursing, social services, a flexible care nursing service, or private care.
Or in their Palliative Medicine article:
Both CHAH and control patients could receive the standard care provided locally. This included care in hospital or hospice, or care at home with input from GP, district nursing, Marie Curie nursing, Macmillan nursing, evening district nursing, Social Services, private care and a Flexible Care nursing service. The latter was a home nursing service, similar to Marie Curie nursing, but funded by the community NHS Trust and available to all diagnostic groups. Thus the trial compared CHAH and standard care with standard care only.
Response: People receiving specialist end of life home care could also be admitted to inpatient care, hospice care and access primary care services (SS, SS, BW).
Feedback: 2. Hughes
"The Edward Hines, Jr. VA Hospital has had a Hospital‐Based Home Care (HBHC) program since 1971....(the primary aim of the study was about cost but) we also sought to compare the attributes of the Hines model of care with traditional community home care services to which control group patients could be referred."
Response: The control group also received inpatient care (SS, SS, BW).
Feedback: 3. Jordhoy
Conventional care is shared among the hospital departments and the community, according to diagnosis and medical needs. No well‐defined routines exist.
Palliative‐care intervention: The Palliative Medicine Unit has 12 inpatient beds, an outpatient clinic, and a consultant team that works in and out of the hospital.... We compared the palliative‐care intervention with conventional care (control).
Response: We gave additional detail in the included studies table: A hospital‐based intervention co‐ordinated by the Palliative Medicine Unit with community outreach. The intervention had been working for 2 years and 8 months. The Palliative Medicine Unit provided supervision and advice and joined visits at home. The community nursing office determined the type and amount of home care and home nursing offered. The care was multidisciplinary, involving a palliative care team, community team, patients and families. Specialist palliative care nurses provided care in the home with a family physician and palliative care consultants (n = 3). Physiotherapy, nutrition and social care were available as was access to a priest. 24‐hour care was limited; the smallest urban district had no access to 24‐hour care.
In addition we asked the authors for additional data and to clarify that their trial was eligible for the review (SS, SS, BW).
Feedback: 4. Brumley
This was a randomized, controlled trial conducted at two separate managed care sites to test the replicability and the effectiveness of an In‐home Palliative Care (IHPC) program.... Each patient enrolled in the intervention arm received customary and usual standard care within individual health benefit limits in addition to the IHPC program.... Usual care consisted of standard care to meet the needs of the patients and followed Medicare guidelines for home healthcare criteria.
Response: The difference between the intervention and the control group was that the control group did not receive specialised 24 hour ‘in home palliative care’ while those allocated to the intervention had access to it until death or transfer to a hospice (see included studies table) (SS, SS, BW).
Feedback: Could you please inform me of how the Cochrane Collaboration will address these major flaws?
Response: The feedback was submitted to the EPOC feedback editor, who then passed it on to the authors and the EPOC managing editor. The authors drafted a response, which was approved by the feedback editor and an additional EPOC editor.
Contributors
Sasha Shepperd
Bee Wee
Sharon E Straus
What's new
| Date | Event | Description |
|---|---|---|
| 23 October 2015 | New citation required but conclusions have not changed | We included no new studies in this update |
| 22 April 2015 | New search has been performed | We have updated searches. We have updated Methods to align with current Cochrane guidance |
History
Review first published: Issue 7, 2011
| Date | Event | Description |
|---|---|---|
| 18 January 2012 | Feedback has been incorporated | Feedback submitted; feedback and responses included in "Feedback section". |
Acknowledgements
Professor Steve Iliffe assisted with data extraction for one of the trials (Hughes 1992). We would like to acknowledge the peer review contribution from Mike Bennett, Luciana Ballini, Camilla Zimmermann, Álvaro Sanz, Andy Oxman, and Craig Ramsay; and Nia Roberts for conducting the electronic searches.
Appendices
Appendix 1. Search strategy
April 2015
MEDLINE search terms
1. (hospital adj2 home).tw.
2. home based versus hospital based.tw.
3. home hospitalization.tw.
4. exp Home Care Services/
5. exp Hospitalization/
6. 4 and 5
7. 1 or 2 or 3 or 6
8. randomized controlled trial.pt.
9. controlled clinical trial.pt.
10. randomized.ab.
11. placebo.ab.
12. drug therapy.fs.
13. randomly.ab.
14. trial.ab.
15. groups.ab.
16. 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp animals/ not humans.sh.
18. 16 not 17
19. 7 and 18
20. (2011* or 2012* or 2013* or 2014* or 2015*).ed,dp,yr.
21. 19 and 20
EMBASE search terms
1. (hospital adj2 home).tw.
2. home hospitalization.tw.
3. home based versus hospital based.tw.
4. exp home care/
5. hospitalization/
6. 4 and 5
7. 1 or 2 or 3 or 6
8. clinical trial/
9. RANDOMIZATION/
10. randomized controlled trial/
11. crossover procedure/
12. double blind procedure/
13. single blind procedure/
14. (randomised or randomized).tw.
15. PLACEBO/
16. (controlled adj study).tw.
17. 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
18. 7 and 17
19. nonhuman/
20. 18 not 19
21. (2011* or 2012* or 2013* or 2014* or 2015*).em,dp,yr.
22. 20 and 21
CINAHL search terms
1. TI hospital N2 home OR AB hospital N2 home
2. TI Home‐based versus hospital‐based OR AB Home‐based versus hospital‐based
3. TI Home hospitalization OR AB Home hospitalization
4. (MH "Home Health Care")
5. (MH "Hospitalization")
6. 4 AND 5
7. 1 OR 2 OR 3 OR 6
8. (MH "Clinical Trials+")
9. PT clinical trial
10. TI ( controlled trial or controlled study ) OR AB ( controlled trial or controlled study )
11. TI ( randomised or randomized ) OR AB ( randomised or randomized )
12. TI ( (random* N1 (allocat* or assign*)) ) OR AB ( (random* N1 (allocat* or assign*)) )
13. 8 OR 9 OR 10 OR 11 OR 12
14. 6 AND 13
15. 6 AND 13 Limiters ‐ Published Date: 20110101‐20151231
CENTRAL search terms
#1 hospital near/2 home:ti,ab,kw (Word variations have been searched)
#2 home hospitalization:ti,ab,kw (Word variations have been searched)
#3 Home‐based versus hospital‐based :ti,ab,kw (Word variations have been searched)
#4 #1 or #2 or #3
Econlit search terms
S5 (hospital NEAR/2 home) OR "home hospitalization" OR "home based versus hospital based"Limits applied
S4 (hospital NEAR/2 home) OR "home hospitalization" OR "home based versus hospital based"
S3 "home based versus hospital based"
S2 "home hospitalization"
S1 hospital NEAR/2 home
Data and analyses
Comparison 1. Place of death.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Dying at home | 3 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [1.14, 1.55] |
| 2 Time spent at home in the last 2 weeks of life | Other data | No numeric data | ||
| 3 Dying in hospital | 1 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.82, 1.52] |
| 4 Dying in a nursing home | Other data | No numeric data | ||
| 5 Dying in a nursing home | 1 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.32] |
Comparison 2. Unplanned admissions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Admitted to hospital | 4 | 823 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.82, 1.05] |
Comparison 3. Control of symptoms.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caregivers' ratings of symptoms | Other data | No numeric data | ||
| 2 GPs' ratings of symptoms | Other data | No numeric data |
Comparison 4. Participant health outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Functional status | Other data | No numeric data | ||
| 2 Psychological well‐being | Other data | No numeric data | ||
| 3 Cognitive status | Other data | No numeric data | ||
| 4 Patient satisfaction | Other data | No numeric data | ||
| 5 Mortality | Other data | No numeric data | ||
| 6 Survival time from referral to death | Other data | No numeric data |
Comparison 5. Caregiver‐reported outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caregiver satisfaction | Other data | No numeric data |
Comparison 6. Resource use and cost.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cost | Other data | No numeric data | ||
| 2 Health service use | Other data | No numeric data | ||
| 3 Inpatient days | Other data | No numeric data | ||
| 4 Number of inpatient days | 1 | 113 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐13.88, 5.28] |
Comparison 7. Staff views.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 District nurse views | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Brumley 2007.
| Methods | RCT | |
| Participants | Age: Mean 74 years, SD 12.0 Sex: 51% men (n = 151), 49% women (n = 146) Ethnicity: 37% belonged to an ethnic minority group; 18% were Asian/Pacific Islanders, 13% Hawaiian, 4% Latino, 2% other Place of residence: 66% lived in their own home or apartment; 8% lived in the home of a family member; 74% resided with a family member, primarily a spouse or a child; 26% lived alone Condition: Late‐stage COPD (21%), CHF (33%), or cancer (47%) and a life expectancy of 12 months or less; participants visited the emergency department or hospital at least once within the previous year; and scored 70% or less on the Palliative Performance Scale. The primary care physician assessed life expectancy, responding to the question 'Would you be surprised if this patient died in the next year?' Number recruited: 718 referred to the study, 408/718 excluded: 196 did not meet eligibility criteria, 67 were eligible for and admitted to hospice care, 59 refused, 38 died before enrolment, 26 were part of another research project, and 22 moved out of the area or could not be contacted. 310 terminally ill participants were randomly allocated: T = 155, C = 155. 8/155 in the intervention group died before receiving palliative care, while in the control group 5/155 withdrew from the study. This left 297 available for analysis |
|
| Interventions | Multidisciplinary team including a physiotherapist, occupational therapist, speech therapist, dietitian, social worker, bereavement co‐ordinator, counsellor, chaplain, pharmacist, palliative‐care physician, and a specialist nurse trained in symptom control and biopsychosocial interventions. The specialist nurse provided education, discussed goals of care and the expected course of the disease and expected outcomes, as well as the likelihood of success of various treatment and interventions. 24‐hour care was available if required The service was co‐ordinated by a core team of physician, specialist nurse, and social worker who managed care across settings and provided assessment, evaluation, planning, care delivery, follow‐up, monitoring, and continuous reassessment of care. The service was not time‐limited and was provided until death or transfer to a hospice Control care: followed Medicare guidelines, services included home health services, acute care services, primary care services, and hospice care |
|
| Outcomes | Reid‐Gundlach Satisfaction with Services instrument was used to measure overall satisfaction with services, perception of service providers, and likelihood of positive recommendations of services to others. Palliative Performance Scale was used to measure severity of illness Data were also collected retrospectively from HMO service utilisation databases at each site, from time participant enrolled in study until time of death or end of study period. Medical service use data: costs for all standard medical care and costs associated with the palliative‐care programme. Service data: number of emergency department visits, physician office visits, hospital days, skilled nursing facility days, home health and palliative visits, palliative physician home visits, and days in hospice. Service costs calculated using actual costs for contracted medical services (Colorado) and proxy cost estimates for all services provided within the HMO |
|
| Notes | Healthcare system: US healthcare system, not‐for‐profit HMOs. 2‐group model, closed panel, non‐profit HMOs providing integrated healthcare services in Hawaii and Colorado. The Colorado site has more than 500 physicians representing all medical specialities and subspecialities in 16 separate ambulatory medical offices spread across a greater metropolitan area. The HMO contracts with outside providers for emergency department, hospital, home health, and hospice care to serve its 477,000‐person membership, which spans the 6‐county Denver metropolitan area. The Hawaii site is located in Oahu and serves approximately 224,000 members, with 12 medical offices in Oahu, 3 in Maui, and 3 on the Big Island. A medical group of 317 physicians provide care. In contrast to Colorado, the HMO provides all outpatient and most inpatient care, and it also has an internal home health agency | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group assignment was determined by blocked randomisation using a computer‐generated random number chart, stratified according to study site |
| Allocation concealment (selection bias) | Low risk | Once eligibility was determined, the intake clerk contacted the evaluators, who randomly assigned participants to the palliative‐care intervention or to usual care |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and clinical staff were aware of the intervention; the researchers employed research assistants who were blinded to the group assignments and collected data by telephone |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8/155 died in the intervention group before the intervention was delivered; 5/155 withdrew from the control group During the course of the study (maximum follow‐up time at 120 days), 75% (n = 225) participants died |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Baseline measures | Low risk | Palliative Performance Scale, demographic data similar between groups |
| Protection against contamination | Low risk | Both groups had access to hospice care; the control group did not have access to the intervention (an interdisciplinary home‐based healthcare programme) |
Grande 2000.
| Methods | RCT | |
| Participants | Requiring terminal care: treatment = 186 (87% with a diagnosis of cancer); control = 43 (86% with a diagnosis of cancer) Living alone: treatment 21%, control 17% Mean age: treatment 72 (SD 11); control 73 (SD 14) Male 50%, female 54% Survival from referral for both groups: a median of 11 days |
|
| Interventions | Referred from primary or secondary care 6 qualified nurses, 2 nursing aides, a co‐ordinator (RGN level), agency staff providing 24‐hour care if required for a maximum of 2 weeks, most had Marie Curie experience Intervention participants could also access standard care Control group received standard care: hospital care or hospice care, with input from the GP and district nurses, Marie Curie nursing, Macmillan nursing, social services, and private nursing |
|
| Outcomes | Symptoms and support, GP visits, place of death, and admission to hospital | |
| Notes | UK study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 4:1 randomisation ratio (HAH:control) to ensure sufficient admissions to hospital at home. Random numbers from a random number table were used |
| Allocation concealment (selection bias) | Low risk | Allocation for each referral was assigned by the researcher using a random number table and concealed in sequentially numbered, opaque, sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | It was not possible for participants to be blinded to the intervention, hence there is a risk that intervention status may have biased place of death decisions. Low risk for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Response rates: 144/198 (73%) for caregivers, 225/228 (99%) district nurses, 194/228 (85%) primary care physicians |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported |
| Baseline measures | Low risk | Demographic data |
| Protection against contamination | High risk | Intervention was contaminated by other input available to the control group (e.g. supplemented by GP and other community care when less than 24‐hour hospital‐at‐home input was provided) |
Hughes 1992.
| Methods | RCT | |
| Participants | People who had an estimated life expectancy of < 6 months were recruited People requiring terminal care (73% in the intervention group and 80% in the control group had a diagnosis of cancer) Number of participants in 3 years: T = 83, C = 85 Average age: T = 65.7 years, C = 63.3 years | |
| Interventions | Hospital at home Type of service: physician‐led Skill mix and size of team: nurses; 1 physiotherapist; 1 dietitian; 1 social worker; health technicians Control group: inpatient hospital care | |
| Outcomes | Mortality, functional status, psychological well‐being, cognitive status, patient satisfaction, readmission, cost, inpatient hospital days, use of other health services, caregiver satisfaction, caregiver morale Follow‐up: 1 month, 6 months |
|
| Notes | US study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | It was not possible for participants to be blinded to the intervention, hence there is a risk that intervention status may have biased assessments of participant functioning |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Hospital databases used for healthcare utilisation data |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Baseline measures | Low risk | No differences in key baseline characteristics |
| Protection against contamination | Unclear risk | No information |
Jordhøy 2000.
| Methods | Cluster‐RCT (3 pairs of clusters stratified into pairs according to the number of inhabitants older than 60 years, and if area was urban or rural) Originally 8 clusters, 2 urban districts with the smallest number of inhabitants > 60 years were merged with larger ones |
|
| Participants | People with incurable malignant disease, life expectancy of 2 to 9 months (estimated at referral) and age older than 18 years. People with haematological malignant disorders other than lymphomas were excluded from the trial Median age (range): T = 70 years (38 to 90), C = 69 years (37 to 93) Sex (percentage male): T = 132/235 (56%), C = 98/199 (49%) Living alone: T = 70/235 (30%), C = 71/199 (36%) Relatives in the same neighbourhood: T = 214/235 (91%), C = 179/199 (90%) Receiving home help at the time of recruitment: T = 26/235 (11%), C = 45/199 (23%) Number recruited from March 1995 to November 1997: 434/707 referred patients were included; T = 235, C = 199 Numbers of participants per cluster: cluster 1: T = 134, C = 116; cluster 2: T = 77, C = 65; cluster 3: T = 24, C = 18 |
|
| Interventions | A hospital‐based intervention co‐ordinated by the Palliative Medicine Unit with community outreach. The intervention had been operational for 2 years and 8 months. The Palliative Medicine Unit provided supervision and advice and joined visits at home. The community nursing office determined the type and amount of home care and nursing home care offered. Multidisciplinary, involving palliative‐care team, community team, participants, and families Specialist palliative‐care nurses provided care in the home with a family physician and palliative‐care consultants (n = 3). Physiotherapy, nutrition and social care available. Access to a priest. 24‐hour care was limited, with the smallest urban district not having access to 24‐hour care Educational programme for community staff including bedside teaching and 6 to 12 hours of lectures every 6 months Access to informal help (T = 187/235 (80%), C = 140/199 (70%); Control group: conventional care is shared among the hospital departments and the community) |
|
| Outcomes | Time at home, place of death, admissions to hospital, health‐related quality of life, admission to nursing home, survival Follow‐up of maximum 2 years |
|
| Notes | Healthcare system: the Norwegian Public Health Service, which provides hospital and community care. The intervention was linked to the Trondheim University Hospital. The Norwegian Public Health Service provides hospital and community care. 8 community healthcare districts participated: 6 districts of Trondheim city (population 141,000) and 2 neighbouring rural communities (Malvik: population 10,000, and Melhus: population 13,000) Community services in all the districts are similar, including family physicians, home care nursing, and nursing homes. 1 family physician manpower‐year serves around 1500 inhabitants. A mean of 30 manpower‐years of home care nurses’ or nurse assistants’ time are available per 1000 inhabitants older than 67 years. All except the smallest urban district provides 24‐hour home care service. However, night service is limited to short visits or telephone consultations. Number of nursing home beds (short and long term) is restricted to 20 beds per 100 inhabitants older than 80 years. In each district, home care and nursing home services are co‐ordinated at a common community nursing office, which decides the type and amount of service that a referred patient will be offered Hospital services for all 8 districts are provided by Trondheim University Hospital. Palliative Medicine Unit has 12 inpatient beds, an outpatient clinic, and a consultant team that works in and out of the hospital, including 2 palliative‐care nurses, a social worker, a priest, a nutritionist, and a part‐time physiotherapist. 3 full‐time physicians were employed during the study. The team only worked daytime hours |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Eligible patients were assigned treatment according to the district (cluster) in which they lived |
| Allocation concealment (selection bias) | High risk | Cluster‐RCT of 8 local community healthcare districts stratified into pairs according to the number of inhabitants older than 60 years and whether the areas were rural or urban. 2 small urban districts were merged with larger ones, for a total of 3 clusters |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding not possible, reliable measures of outcome used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Alive at follow‐up: 10/229 in the intervention group and 13/189 in the control group |
| Selective reporting (reporting bias) | Low risk | Wide range of outcomes reported |
| Baseline measures | Low risk | No differences in key baseline characteristics |
| Protection against contamination | Low risk | Intervention was not available to control groups |
C = control CHF = congestive heart failure COPD = chronic obstructive pulmonary disease GP = general practitioner HAH = hospital at home HMO = health maintenance organisation RCT = randomised controlled trial RGN = registered general nurse SD = standard deviation T = treatment
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Brumley 2003 | A non‐randomised study (it is described as a "non‐equivalent comparison group") and compares a palliative‐care programme with home care |
| Brännström 2014 | Intervention is not an alternative to inpatient hospital or hospice care |
| Enguidanos 2005 | Non‐equivalent study design |
| Holdsworth 2015 | Intervention is not an alternative to inpatient hospital or hospice care |
| Hughes 1990 | Intervention does not provide end‐of‐life home‐based care |
| Hughes 2000 | Intervention is not an alternative to inpatient hospital or hospice care |
| McCusker 1987 | Non‐randomised study using routinely collected data |
| McWhinney 1994 | No outcome data reported; authors describe the challenges of conducting a trial in this area |
| Stern 2006 | Abstract only, no outcome data reported. Full article not identified |
Characteristics of studies awaiting assessment [ordered by study ID]
NTR2817.
| Methods | Cluster randomised controlled trial (general practitioner as unit of randomisation) |
| Participants | Participants aged >= 18 years old, with progressive oncological disease, life expectancy <= 3 months; excluded if unable to provide informed consent |
| Interventions | Weekly teleconsultation with a research nurse, using a telemedicine computer installed at the participant's home; any ongoing needs identified are then transmitted to the general practitioner. More frequent appointments are possible if requested by the participant |
| Outcomes | Main outcome: symptom burden experienced by the participant Other outcomes: hospital admission; number of problems and needs for palliative care; patient and caregiver satisfaction; experienced continuity of medical care in the last phase of life; caregiver's burden |
| Notes | Care received by control group is not described; awaiting further information. The Netherlands National Trial Register NTR2817 |
Characteristics of ongoing studies [ordered by study ID]
NCT01885637.
| Trial name or title | Danish Palliative Care Trial (DOMUS) |
| Methods | Controlled randomised clinical trial with a balanced parallel‐group randomisation (1:1) |
| Participants | 340 in‐ and outpatients treated at the Department of Oncology at Copenhagen University Hospital |
| Interventions | Treatment group: standard care plus specialised palliative care and a standardised psychological intervention, home‐delivered for participants and caregiversComparison: standard care alone |
| Outcomes | Main outcome: residence in preferred place of care Other outcomes: symptoms, quality of life, psychosocial problems, survival (participants); quality of life, psychosocial problems, bereavement (caregivers); co‐operation (professionals); and cost |
| Starting date | June 2013 |
| Contact information | |
| Notes | ClinicalTrials.gov identifier: NCT01885637 |
Differences between protocol and review
This review was originally part of a broader review evaluating the effectiveness of hospital at home services, first published in Issue 1, 1998 of the Cochrane Library (Shepperd 2005). As more data have become available, this broader review has been split into three: Hospital at home admission avoidance, Hospital at home early discharge, and Hospital at home: home‐based end‐of‐life care. The titles have been changed for consistency. Hospital at home admission avoidance, Shepperd 2008, and Hospital at home early discharge, Shepperd 2009, are published in the Cochrane Library.
We made a post‐hoc decision to adjust the data entered into the meta‐analysis using an estimate of the intracorrelation coefficient of 0.02, as the authors reported no confidence intervals (Jordhøy 2000). We included a new outcome (staff views on the provision of services). We updated the methods in this update to align with current Cochrane guidance, including the Methodological standards for the reporting of Cochrane Intervention Reviews (MECIR 2012).
Contributions of authors
DCGB screened the results from the search strategy for this update, handsearched PDQ‐Evidence, ClinicalTrials.gov, and relevant palliative‐care publications, and updated the Background and Discussion sections. SS, BW, and SES extracted data; SS conducted the analysis and led on writing the systematic review. BW and SES provided advice on the selection criteria and commented on the draft manuscripts.
Sources of support
Internal sources
-
Department of Public Health, University of Oxford, UK.
Part‐funded SS
External sources
-
NIHR Cochrane Programme Grant, UK.
Part‐funded SS
-
Canada Research Chair in Knowledge Translation, Canada.
Funded SES
Declarations of interest
BW is a full‐time salaried employee of the National Health Service in the UK. Her responsibilities include the provision of specialist palliative care services (in the hospice, community, and hospital), service development, education, and research in palliative care. Neither she, nor her organisation, stands to gain or lose from the conclusions of this review, but like other services within the National Health Service, the conclusions of this review may inform future service development or commissioning, or both.
DCGB: none. SS: none. SES: none.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Brumley 2007 {published data only}
- Brumley R, Enguidanot S, Jamison P, Seitz R, Morgenstern N, Saito S, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in‐home palliative care. Journal of the American Geriatrics Society 2007;S5:993‐1000. [DOI] [PubMed] [Google Scholar]
Grande 2000 {published data only}
- Grande G, Farquhar MC, Barclay SIG. Caregiver bereavement outcome: relationship with hospital at home, satisfaction with care and home death. Journal of Palliative Care 2004;20(2):69‐77. [PubMed] [Google Scholar]
- Grande GE, Todd CJ, Barclay SI, Farquhar MC. A randomised controlled trial of a hospital at home service for the terminally ill. Palliative Medicine 2000;14:375‐85. [DOI] [PubMed] [Google Scholar]
- Grande GE, Todd CJ, Barclay SI, Farquhar MC. Does hospital at home for palliative care facilitate death at home? Randomised controlled trial. BMJ 1999;319:1472‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hughes 1992 {published data only}
- Hughes SL, Cummings J, Weaver F, Manheim L, Braun B, Conrad K. A randomized trial of the cost effectiveness of VA hospital‐based home care for the terminally ill. Health Services Research 1992;26:801‐17. [PMC free article] [PubMed] [Google Scholar]
Jordhøy 2000 {published data only}
- Jordhøy MS, Fayers P, Saltnes T, Ahlner‐Elmqvist M, Jannert M, Kaasa S. A palliative care intervention and death at home: a cluster randomized trial. The Lancet 2000;356:888‐93. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Brännström 2014 {published data only}
- Brännström M, Boman K. Effects of person‐centred and integrated chronic heart failure and palliative home care. PREFER: A randomized controlled study. European Journal of Heart Failure 2014;16(10):1142‐51. [DOI] [PubMed] [Google Scholar]
Brumley 2003 {published data only}
- Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a home‐based palliative care program for end‐of‐life. Journal of Palliative Medicine 2003;6(5):715‐24. [DOI] [PubMed] [Google Scholar]
Enguidanos 2005 {published data only}
- Enguidanos SM, Cherin D, Brumley R. Home‐based palliative care study: site of death, and costs of medical care for patients with congestive heart failure, chronic obstructive pulmonary disease, and cancer. Journal of Social Work in End‐of‐Life & Palliative Care 2005;1(3):37‐56. [DOI] [PubMed] [Google Scholar]
Holdsworth 2015 {published data only}
- Holdsworth LM, Gage H, Coulton S, King A, Butler C. A quasi‐experimental controlled evaluation of the impact of a hospice rapid response community service for end‐of‐life care on achievement of preferred place of death. Palliative Medicine 2015;29(9):817‐25. [DOI: 10.1177/0269216315582124] [DOI] [PubMed] [Google Scholar]
Hughes 1990 {published data only}
- Hughes SL, Cummings J, Weaver F, Manheim LM, Conrad KJ, Nash K. A randomized trial of Veterans Administration home care for severely disabled veterans. Medical Care 1990;28(2):135‐45. [DOI] [PubMed] [Google Scholar]
Hughes 2000 {published data only}
- Hughes SL, Weaver FM, Giobbie‐Hurder A, Manheim L, Henderson W, Kubal JD, et al. Department of Veterans Affairs Cooperative Study Group on Home‐Based Primary Care. Effectiveness of team‐managed home‐based primary care: a randomized multicenter trial. JAMA 2000;284(22):2877‐85. [DOI] [PubMed] [Google Scholar]
McCusker 1987 {published data only}
- McCusker J, Stoddard AM. Effects of an expanding home care program for the terminally ill. Medical Care 1987;25:373‐85. [DOI] [PubMed] [Google Scholar]
McWhinney 1994 {published data only}
- McWhinney IR, Bass MJ, Donner A. Evaluation of a palliative care service: problems and pitfalls. BMJ 1994;309:1340‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stern 2006 {published data only}
- Stern A, Goldsmith C, Thabane L, Abernathy T, Cohen R, Jadad A, et al. The efficacy of home telehealth in palliative care for oncology patients and their caregivers. Journal of Palliative Care 2006;22:208‐9. [Google Scholar]
References to studies awaiting assessment
NTR2817 {published data only}
- Duursma F, Schers HJ, Vissers KCP, Hasselaar J. Study protocol: optimization of complex palliative care at home via telemedicine. A cluster randomized controlled trial. BMC Palliative Care 2011;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NTR2817. Optimization of complex palliative care at home by means of expert consultation via telemedicine. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=2817 (accessed 14 August 2015).
References to ongoing studies
NCT01885637 {published data only}
- NCT01885637. DOMUS: A Trial of Accelerated Transition From Oncological Treatment to Continuing Palliative Care at Home. https://clinicaltrials.gov/ct2/show/NCT01885637 (accessed 14 August 2015).
- Nordly M, Benthien KS, Maase H, Johansen C, Kruse M, Timm H, et al. The DOMUS study protocol: A randomized clinical trial of accelerated transition from oncological treatment to specialized palliative care at home. BMC Palliative Care 2014;13:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Agelopoulos 2009
- Agelopoulos N, Tate T. The Marie Curie Delivering Choice Programme. European Journal of Palliative Care 2009;16:290‐4. [Google Scholar]
Bell 2010
- Bell CL, Somogyi‐Zalud E, Masaki KH. Factors associated with congruence between preferred and actual place of death. Journal of Pain and Symptom Management 2010;39(3):591‐604. [DOI: 10.1016/j.jpainsymman.2009.07.007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bradburn 2007
- Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A. Much ado about nothing: A comparison of the performance of meta‐analytical methods with rare events. Statistics in Medicine 2007;26(1):53‐77. [DOI] [PubMed] [Google Scholar]
Cochrane 1954
- Cochrane WG. The combination of estimates from different experiments. Biometrics 1954;10:101‐29. [Google Scholar]
Dans 2007
- Dans AM, Dans LF, Oxman AD, Robinson V, Acuin J, Tugwell P, et al. Addressing inequities in clinical practice guidelines. Clinical Epidemiology 2007;60:540‐6. [DOI] [PubMed] [Google Scholar]
Decker 2006
- Decker SL, Higginson IJ. A tale of two cities: Factors affecting place of cancer death in London and New York. European Journal of Public Health 2006;17(3):285‐90. [DOI] [PubMed] [Google Scholar]
Department of Health 2008
- Department of Health. End of life care strategy ‐ promoting high quality care for all adults at the end of life. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_086345.pdf (accessed 05/02/2016).
EPOC 2010
- Cochrane Effective Practice and Organisation of Care Review Group. Data abstraction form. http://www.epoc.uottawa.ca/tools.htm (accessed June 2010).
Gomes 2008
- Gomes B, Higginson IJ. Where people die (1974 to 2030): past trends, future projections and implications for care. Palliative Medicine 2008;22:33‐41. [DOI] [PubMed] [Google Scholar]
Gomes 2012
- Gomes B, Higginson IJ, Calanzani N, Cohen J, Deliens L, Daveson BA, et al. PRISMA. Preferences for place of death if faced with advanced cancer: A population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Annals of Oncology 2012;238(8):2006‐15. [DOI] [PubMed] [Google Scholar]
Gott 2004
- Gott M, Seymour J, Bellamy G, Clark D, Ahmedzai S. Older people's views about home as a place of care at the end of life. Palliative Medicine 2004;18:460‐7. [DOI] [PubMed] [Google Scholar]
Grande 2004
- Grande G, Farquhar MC, Barclay SIG. Caregiver bereavement outcome: relationship with hospital at home, satisfaction with care and home death. Journal of Palliative Care 2004;20(2):69‐77. [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI: 10.1136/bmj.39489.470347.AD] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analysis. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons, Ltd, 2011. [DOI: 10.1002/9780470712184.ch8] [DOI] [Google Scholar]
Higginson 2000
- Higginson IJ, Sen‐Gupta GJA. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. Journal of Palliative Medicine 2000;3(3):287‐300. [DOI] [PubMed] [Google Scholar]
Higginson 2013
- Higginson IJ, Evans CJ, Grande G, Preston N, Morgan M, McCrone P, et al. on behalf of MORECare. Evaluating complex interventions in End of Life Care: The MORECare Statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Medicine 2013;11:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kleinman 2009
- Kleinman A. Caregiving: the odyssey of becoming more human. The Lancet 2009;373:292‐3. [DOI] [PubMed] [Google Scholar]
Luckett 2013
- Luckett T, Davidson PM, Lam L, Phillips J, Currow DC, Agar M. Do community specialist palliative care services that provide home nursing increase rates of home death for people with life‐limiting illnesses? A systematic review and meta‐analysis of comparative studies. Journal of Pain and Symptom Management 2013;45(2):279‐97. [DOI] [PubMed] [Google Scholar]
Masella 2015
- Masella C, Garavaglia G, Borghi G, Castelli A, Radaelli G, Peruselli C. Implementation of a Hospital‐Based Home Palliative Care at regional level: A quantitative study of the Ospedalizzazione Domiciliare Cure Palliative Oncologiche program in Lombardy. Palliative Medicine 2015;29(3):241‐8. [DOI] [PubMed] [Google Scholar]
MECIR 2012
- Methodological Expectations of Cochrane Intervention Reviews (MECIR). Standards for the reporting of new Cochrane Intervention Reviews Version 1.1. http://editorial‐unit.cochrane.org/sites/editorial‐unit.cochrane.org/files/uploads/MECIR%20Reporting%20standards%201.1_17122012_2.pdf Accessed 05/02/16.
National Audit Office 2008
- National Audit Office. End of Life Care. https://www.nao.org.uk/wp‐content/uploads/2008/11/07081043.pdf (accessed 05/02/2016).
NEoLCIN 2014
- National End of Life Care Intelligence Network. What We Know Now 2014. Public Health England, 2014. [Google Scholar]
Noble 2015
- Noble B, King N, Woolmore A, Hughes P, Winslow M, Melvin J, et al. Can comprehensive specialised end‐of‐life care be provided at home? Lessons from a study of an innovative consultant‐led community service in the UK. European Journal of Cancer Care 2015;24(2):253‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seamark 2014
- Seamark D, Blake S, Brearley SG, Milligan C, Thomas C2, Turner M, et al. Dying at home: A qualitative study of family carers' views of support provided by GPs community staff. BJGP 2014;64(629):e‐796‐803. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepperd 2008
- Shepperd S, Doll H, Angus R, Clarke M, Iliffe S, Kalra L, et al. Hospital at home admission avoidance. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007491] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepperd 2009
- Shepperd S, Doll H, Broad J, Gladman J, Iliffe S, Langhorne P, et al. Hospital at home early discharge. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD000356.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smeenk 1998
- Smeenk FWJM, va Haastregt JCM, Witte LP, Crebolder HFJM. Effectiveness of home care programmes for patients with incurable cancer on their quality of life and time spent in hospital: a systematic review. BMJ 1998;316:1939‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tang 2010
- Tang ST, Huang EW, Liu TW, Rau KM, Hung YN, Wu SC. Propensity for home death among Taiwanese cancer decedents in 2001‐2006, determined by services received at end of life. Journal of Pain and Symptom Management 2010;40(4):566‐74. [DOI: 10.1016/j.jpainsymman.2010.01.020] [DOI] [PubMed] [Google Scholar]
Wilson 2009
- Wilson DM, Truman CD, Thomas R, Fainsinger R, Kovacs‐Burns K, Froggatt K, et al. The rapidly changing location of death in Canada, 1994‐2004. Social Science & Medicine 2009;68(10):1752‐8. [DOI] [PubMed] [Google Scholar]
Woodman 2015
- Woodman C, Baillie J, Sivvel S. The preferences and perspectives of family caregivers towards place of care for their relatives at the end‐of‐life. A systematic review and thematic synthesis of the qualitative evidence. BMJ Supportive & Palliative Care 2014. [DOI: 10.1136/bmjspcare-2014-000794] [DOI] [PMC free article] [PubMed]
Zimmermann 2008
- Zimmermann C, Riechelmann R, Kryzanowska M, Rodin G, Tannock I. Effectiveness of specialised palliative care ‐ a systematic review. JAMA 2008;299(14):1698‐709. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Shepperd 2005
- Shepperd S, Iliffe S. Hospital at home versus in‐patient hospital care. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD000356.pub2] [DOI] [PubMed] [Google Scholar]
Shepperd 2011
- Shepperd S, Wee B, Straus SE. Hospital at home: home‐based end of life care. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009231] [DOI] [PMC free article] [PubMed] [Google Scholar]


