Abstract
Background
Telemedicine is defined by three characteristics: (1) using information and communication technologies, (2) covering a geographical distance, and (3) involving professionals who deliver care directly to a patient or a group of patients. It is said to improve chronic care management and self-management in patients with chronic diseases. However, currently available guidelines for the care of patients with diabetes, hypertension, or dyslipidemia do not include evidence-based guidance on which components of telemedicine are most effective for which patient populations.
Objective
The primary aim of this study was to identify, synthesize, and critically appraise evidence on the effectiveness of telemedicine solutions and their components on clinical outcomes in patients with diabetes, hypertension, or dyslipidemia.
Methods
We conducted an umbrella review of high-level evidence, including systematic reviews and meta-analyses of randomized controlled trials. On the basis of predefined eligibility criteria, extensive automated and manual searches of the databases PubMed, EMBASE, and Cochrane Library were conducted. Two authors independently screened the studies, extracted data, and carried out the quality assessments. Extracted data were presented according to intervention components and patient characteristics using defined thresholds of clinical relevance. Overall certainty of outcomes was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) tool.
Results
Overall, 3564 references were identified, of which 46 records were included after applying eligibility criteria. The majority of included studies were published after 2015. Significant and clinically relevant reduction rates for glycated hemoglobin (HbA1c; ≤−0.5%) were found in patients with diabetes. Higher reduction rates were found for recently diagnosed patients and those with higher baseline HbA1c (>8%). Telemedicine was not found to have a significant and clinically meaningful impact on blood pressure. Only reviews or meta-analyses reporting lipid outcomes in patients with diabetes were found. GRADE assessment revealed that the overall quality of the evidence was low to very low.
Conclusions
The results of this umbrella review indicate that telemedicine has the potential to improve clinical outcomes in patients with diabetes. Although subgroup-specific effectiveness rates favoring certain intervention and population characteristics were found, the low GRADE ratings indicate that evidence can be considered as limited. Future updates of clinical care and practice guidelines should carefully assess the methodological quality of studies and the overall certainty of subgroup-specific outcomes before recommending telemedicine interventions for certain patient populations.
Keywords: telemedicine, diabetes mellitus, hypertension, dyslipidemia, review, GRADE approach, treatment outcome
Introduction
Background
Diabetes is affecting 463 million people worldwide (aged between 20 and 79 years) [1]. Hypertension and hyperlipidemia (or hypercholesterolemia) are common comorbidities in patients with type 2 diabetes (T2D), and also show an increasing coprevalence [2,3]. The risk of diabetes-associated complications can be reduced by continuous control of blood glucose [4], blood pressure (BP) lowering [5-8], and blood lipid profile [9,10]. Current guidelines of the American Diabetes Association (ADA) recommend that most adults with diabetes achieve glycated hemoglobin (HbA1c) <7.0%, BP<140/90 mmHg (<130/90 for patients with increased cardiovascular [CV] risk), and low-density lipoprotein cholesterol (LDL-c) <100 mg/dL [11]. Diabetes self-management education and support, defined as an interactive and continuous process intended to increase knowledge, skills, and abilities required for successful self-management of diabetes interventions [12], has proven to be effective [13,14]. Similarly, hypertensive patients may benefit from the combination of self-monitoring with education or counseling in terms of increased medication adherence and improved BP control [15].
The application of information and communication technologies (ICTs) in health care has been rapidly increasing worldwide. Telemedicine is defined by three characteristics: (1) using ICTs, (2) covering a geographical distance, and (3) involving professionals who deliver care directly to a patient or a group of patients [16,17]. Owing to the need for individualized and continuous monitoring and self-management support for patients, chronic diseases are considered the ideal target conditions for the development and implementation of telemedicine approaches [18,19].
However, detailed guidance is still lacking on how to choose and integrate tools for specific target groups in diabetes care [20,21]. Earlier systematic reviews of high-quality review articles already uncovered key elements for technology-enabled self-management, such as (1) communication between a health care provider and patient, (2) patient-generated health data, (3) education, and (4) feedback [22], or they simply underlined the promising nature of telemedicine [23]. However, the available overviews mainly focus on a specific target group, do not take into account the heterogeneity of telemedicine applications, or focus on a specific tool [24]. Heterogeneous applications of the term telemedicine [16] further limit the external validity of single studies. Owing to the differentiated phenotypes of applied telemedicine solutions, their components, and settings, as well as missing analyses of the quality of studies (and certainty of effects), evidence-based guidance on the best available digital intervention is challenging [25-27].
Objective
Therefore, the primary objective of this umbrella review is to identify, synthesize, and critically appraise the evidence on the effectiveness of telemedicine solutions and their components on clinical outcomes—HbA1c, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol (TC), triglycerides (TGC), systolic BP (SBP), diastolic BP (DBP)—in patients with diabetes (type 1 diabetes [T1D] and T2D), hypertension, or dyslipidemia. Owing to the increasing number of available reviews and meta-analysis as well as the potential of addressing three prevalent chronic conditions with multiple digital interventions, the analysis was conducted as an umbrella review [28,29].
The research question is based on the Population, Intervention, Control, Outcome, and Time (PICOT) criteria: In patients with diabetes, hypertension or dyslipidemia, what is the evidence for the effectiveness of telemedicine-supported chronic care on disease-specific clinical outcomes?
Methods
Search Strategy and Eligibility Criteria
We conducted an umbrella review using extensive automated and manual searches of the databases PubMed, EMBASE, and the Cochrane Library to identify relevant evidence on the effectiveness of telemedicine interventions on the three target diseases. Umbrella reviews summarize and contrast evidence from existing systematic reviews and meta-analyses by looking at specific outcomes across included records [28].
The search was carried out in October 2018. PICOT-criteria (Table 1) for “population,” “intervention,” and “study design” were combined to develop the search strings (Multimedia Appendix 1). No time limitation was applied.
Table 1.
Population, Intervention, Control, Outcome, and Time and eligibility criteria.
| Population, Intervention, Control, Outcome, and Time criteria | Eligibility | |
|
|
Inclusion | Exclusion |
| Population | Humans; only studies addressing at least one of the predetermined target diseases within their initial search | Studies addressing chronic diseases in general, other than the three diseases defined, or not addressing any disease at all; specific populations (pregnant women and ethnical minorities); and animals |
| Intervention | Primary studies applying telemedicine intervention specified as (1) using ICTsa, (2) covering distance, and (3) involving a health care provider for delivering care to the patient | Studies focusing solely on monitoring or data storage and exchange tools (such as electronic health records) |
| Control | Usual care | No control group available or not specified |
| Outcome | Effectiveness analyses allowing for quantitative comparisons between groups using clinical parameters (primary outcome HbA1cb, SBPc, DBPd, HDL-ce, LDL-cf, TCg, and TGCh) | Studies primarily investigating mortality, costs or cost-effectiveness, or feasibility; or efficacy |
| Time | Follow-up time of at least three months | No or shorter follow-up periods described |
| Study design | Study design being either a systematic review or meta-analysis of randomized controlled trials | Other, including a systematic review or meta-analysis of observational studies |
aICT: information and communication technology.
bHbA1c: glycated hemoglobin.
cSBP: systolic blood pressure.
dDBP: diastolic blood pressure.
eHDL-c: high-density lipoprotein cholesterol.
fLDL-c: low-density lipoprotein cholesterol.
gTC: total cholesterol.
hTGC: triglycerides.
Records that fulfilled the following eligibility criteria were included (Table 1): systematic reviews or meta-analyses of randomized controlled trials (RCTs; as this is regarded as highest level of evidence) [30] evaluating the effectiveness of telemedicine in at least one of the target diseases (diabetes, hypertension, and/or dyslipidemia) in adults. No restrictions were made with respect to the kind of participating medical providers. We included all eligible articles in English language and with full text available.
Relevant reviews or meta-analyses were excluded if their primary studies mainly assessed mortality, utilization of health services, the usability of the technology studied, or patients’ acceptance of or satisfaction with the telemedicine tools, or if no quantitative comparison based on clinical outcomes was reported. Studies evaluating interventions using automated feedback without involving a professional or those providing only monitoring of relevant parameters (without feedback) were excluded. In addition, studies evaluating telemedicine use of medical providers only or those in which the components of the intervention were not transparently described were excluded. Eligible records had to report a change in one of the specified clinical outcomes after a follow-up time of at least three months, as this period is in line with current treatment guidelines [15,31,32].
Conference abstracts or protocols were excluded as well. Research was excluded if it focused on specific countries or regions or targeted specified populations (eg, minorities and pregnant women with diabetes). We excluded those studies for which updates of the evidence—indicated by the same group of authors and/or application of identical search string—were available.
We further searched the reference lists of all relevant publications by hand, to identify any additional studies. After carrying out the title-abstract screening, we conducted a hand search in Google Scholar and the three most relevant journals in the field of digital health, as indicated by the highest number of potentially relevant publications (Multimedia Appendix 2).
Data Extraction and Quality Assessment
Two authors (PT and LH) independently screened the records, extracted data, and carried out the quality assessments. The quality assessment of records was done using the Oxford Quality Assessment Questionnaire (OQAQ) to eliminate records of low quality before data extraction [33]. Any disagreement over the suitability of certain records was discussed among the raters and resolved by consensus.
As the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) is the established tool for assessing the overall certainty of evidence by analyzing its risk of bias, imprecision, inconsistency, indirectness, and publication bias, it was used to assess the quality of included records [34]. This assessment was performed by three independent researchers (PT, SO, and LH), using independent pairwise ratings. Disagreements were again resolved by discussion or, where not possible, by consulting the independent third coder [35].
The results of the included records were extracted using a piloted, standardized data extraction form. According to the methodological considerations for conducting umbrella or meta-reviews, the results were reported descriptively and in tabular form [28,29].
Data Analysis
The presentation of data is descriptive; however, the results of meta-analyses and subgroup analyses were specifically analyzed to find effective components or modes of delivery (intensity and frequency) in subgroups or settings. In light of previous trials, a clinically relevant reduction of –0.5% in HbA1c is considered a suitable threshold (Table 2) [36,37]. The definition of clinically relevant reduction rates (direction of arrows) and the statistical significance (green) were used to compare interventions’ effectiveness (Tables 3-5).
Table 2.
Definition of clinically relevant differences in glycated hemoglobin.
| Reduction rate in glycated hemoglobin (%) | P value | Guidance |
| ≤−0.5 | >.05 |
 a
a
|
| >−0.5, <0 | >.05 |
 b
b
|
| >0 | >.05 |
 c
c
|
| >−0.5, <0 | <.05 |
 d
d
|
| ≤−0.5 | <.05 |
 e
e
|
anon-significant but clinically relevant change.
bnon-significant and not clinically relevant change.
cnon-significant and not clinically relevant change.
dsignificant but not clinically relevant change.
esignificant and clinically relevant change.
Table 3.
Effectiveness of telemedicine on glycated hemoglobin in patients with diabetes, according to intervention duration.
| Application category and type of diabetes | Intervention duration | Trials, n | Patients, n | Outcome | MDa (95% CI) of percent change in HbA1cb | P value | I2 (%) | Grading of Recommendations, Assessment, Development, and Evaluation | |
| Digital health education [56] | |||||||||
|
|
T1Dc/T2Dd | 3 months | 3 | 203 |
 e
e
|
−0.71 (−1.0 to −0.43) | .90 | 0 |

|
|
|
T1D/T2D | 6 months | 2 | 562 |
 e
e
|
−0.52 (−0.75 to −0.29) | .65 | 0 |

|
|
|
T1D/T2D | 12 months | 6 | 1153 |
 e,f
e,f
|
−0.55 (−0.7 to −0.39) | <.001 | 78 |

|
| Telemedicine [70,85] | |||||||||
|
|
T1D | <6 months | 7 | NSg |
 e
e
|
0.07 (−0.16 to 0.31) | NS | NS |

|
|
|
T1D | ≥6 months | 21 | NS |
 e
e
|
−0.24 (−0.41 to −0.07) | NS | NS |

|
|
|
T2D | ≤3 months | 17 | 1377 |
 e
e
|
−0.67 (−0.93 to −0.41) | NS | NS |

|
|
|
T2D | 4-6 months | 36 | 4538 |
 e
e
|
−0.41 (−0.84 to 0.02) | NS | NS |

|
|
|
T2D | 7-11 months | 4 | 659 |
 e
e
|
−0.66 (−1.18 to −0.15) | NS | NS |

|
|
|
T2D | ≥12 months | 36 | 10,237 |
 e
e
|
−0.26 (−0.40 to −0.12) | NS | NS |

|
| Digital self-management [59,60,72,83] | |||||||||
|
|
T2D | ≤3 months | 10 | NS |
 e,f
e,f
|
−0.51 (−0.71 to −0.31) | <.001 | 41.8 |

|
|
|
T2D | >3 and ≤6 months | 10 | NS |
 e,f
e,f
|
−0.48 (−0.68 to −0.28) | <.001 | 34.5 |

|
|
|
T2D | 3-4 months | 11 | 1613 |
 e,f
e,f
|
−0.30 (−0.50 to −0.11) | <.001 | 89.1 |

|
|
|
T2D | >6 months | 15 | NS |
 e,f
e,f
|
−0.35 (−0.53 to −0.18) | <.001 | 70.5 |

|
|
|
T2D | 6-8 months | 14 | 2389 |
 e,f
e,f
|
−0.59 (−0.78 to −0.39) | <.001 | 84.8 |

|
|
|
T2D | 9-12 months | 7 | 1272 |
 e
e
|
−0.21 (−0.35 to −0.075) | .131 | 39.1 |

|
|
|
T1D/T2D | ≤ 6 months | 30 | NS |
 e,f
e,f
|
−0.56 (NS) | <.001 | 30 |

|
|
|
T1D/T2D | 6 months | 6 | 741 |
 e
e
|
−0.57 (−0.85 to −0.30) | .099 | NS |

|
|
|
T1D/T2D | >6 months | 25 | NS |
 e,f
e,f
|
−0.40 (NS) | <.001 | 25 |

|
|
|
T1D/T2D | 12 months | 7 | 3466 |
 e
e
|
−0.30 (−0.48 to −0.11) | .099 | NS |

|
| Digital self-management (SMS) [75] | |||||||||
|
|
T2D | <6 months | 6 | NS |
 e,f
e,f
|
−0.60 (−0.80 to −0.40) | <.001 | NS |

|
|
|
T2D | ≥6 months | 4 | NS |
 e,f
e,f
|
−0.40 (−0.56 to −0.24) | <.001 | NS |

|
| Digital self-management (social network service) [78] | |||||||||
|
|
T1D/T2D | ≤3 months | 13 | 799 |
 e,f
e,f
|
−0.54 (−0.80 to −0.28) | <.001 | 23 |

|
|
|
T1D/T2D | 3-12 months | 11 | 1465 |
 e,f
e,f
|
−0.41 (−0.63 to −0.19) | <.001 | 25 |

|
|
|
T1D/T2D | >12 months | 10 | 2713 |
 e,f
e,f
|
−0.36 (−0.59 to −0.14) | <.002 | 90 |

|
aMD: mean difference.
bHbA1c: glycated haemoglobin
cT1D: type 1 diabetes.
dT2D: type 2 diabetes.
eThe direction of the arrows indicates potential clinically relevant reduction rates (see Table 2).
fGreen arrows show statistical significance.
gNS: not specified—cases in which no data were provided. Missing data on statistical significance were handled as nonsignificant.
Table 5.
Effectiveness of telemedicine on glycated hemoglobin in patients with diabetes, according to population characteristics.
| Category of application and type of diabetes | Population characteristics | Trials, n | Patients, n | Outcome | MDa (95% CI) of percent change in HbA1cb | P value | I2 (%) | Grading of Recommendations, Assessment, Development, and Evaluation | |
| Telemedicine [70,85] | |||||||||
|
|
T1Dc | Adults | 15 | 1256 |
 d,e
d,e
|
−0.26 (−0.47 to −0.05) | <.01 | 79.7 |

|
|
|
T1D | Children and adolescents | 11 | 796 |

|
−0.12 (−0.30 to 0.05) | .70 | 0 |

|
|
|
T1D | Baseline HbA1c <9.0% | 16 | NS |

|
−0.06 (−0.02 to 0.09) | NSf | NS |

|
|
|
T1D | Baseline HbA1c ≥9.0% | 12 | NS |

|
−0.34 (−0.57 to −0.11) | NS | NS |

|
|
|
T2Dg | Baseline HbA1c <8.0% | 48 | 5720 |

|
−0.22 (−0.25 to −0.19) | NS | NS |

|
|
|
T2D | Baseline HbA1c ≥8.0% | 45 | 8100 |

|
−0.60 (−0.61 to −0.60) | NS | NS |

|
| Digital self-management [60-62,68,72,79,83] | |||||||||
|
|
T2D | Age <55 years | 7 | 701 |

|
−0.67 (−1.15 to −0.20) | .52 | 75 |

|
|
|
T2D | Age ≥55 years | 8 | 541 |

|
−0.41 (−0.62 to −0.21) | .52 | 0 |

|
|
|
T2D | Age undetermined | 2 | 289 |

|
−0.72 (−1.60 to 0.16) | .52 | 47 |

|
|
|
T2D | Diagnosish <8.5 years ago | 7 | 549 |

|
−0.83 (−1.10 to 0.56) | .007 | 0 |

|
|
|
T2D | Diagnosish ≥8.5 years ago | 4 | 394 |

|
−0.22 (−0.44 to 0.01) | .007 | 0 |

|
|
|
T2D | Diagnosis timeh undetermined | 6 | 588 |

|
−0.43 (−0.71 to −0.30) | .007 | 55 |

|
|
|
T2D | Baseline HbA1c ≤8.0% | 6 | 590 |

|
−0.49 (−0.71 to −0.27) | .69 | 0 |

|
|
|
T2D | Baseline HbA1c ≤8.0% | 7 | NS |

|
−0.33 (−0.53 to −0.13) | <.05 | 46 |

|
|
|
T2D | Baseline HbA1c >7.0% | 11 | 1707 |

|
−0.33 (−0.48 to −0.18) | <.001 | 77.8 |

|
|
|
T2D | Baseline HbA1c >7.5% | 10 | 1921 |

|
−0.45 (−0.70 to −0.21) | <.001 | 80.4 |

|
|
|
T2D | Baseline HbA1c >8.0% | 11 | 941 |

|
−0.57 (−0.93 to −0.22) | .69 | 65 |

|
|
|
T2D | Baseline HbA1c >8.0% | 11 | NS |

|
−0.70 (−1.03 to −0.36) | <.05 | 81 |

|
|
|
T2D | Baseline BMI <30 kg/m2 | 5 | 359 |

|
−0.64 (−0.91 to −0.36) | .49 | 0 |

|
|
|
T2D | Baseline BMI ≥30 kg/m2 | 10 | 966 |

|
−0.43 (−0.68 to −0.17) | .49 | 35 |

|
|
|
T2D | Baseline BMI undetermined | 2 | 206 |

|
−0.96 (−2.76 to 0.85) | .49 | 91 |

|
|
|
T1D/T2D | Age <40 years | 14 | NS |

|
−0.32 | .02 | NS |

|
|
|
T1D/T2D | Age <40 years | 11 | NS |

|
−0.85 (−1.79 to 0.10) | .07 | 98 |

|
|
|
T1D/T2D | Age ≥40 years | 40 | NS |

|
−0.53 | <.001 | NS |

|
|
|
T1D/T2D | Age 41-50 years | 8 | NS |

|
−1.83 (−3.17 to −0.48) | <.001 | 96.2 |

|
|
|
T1D/T2D | Age >50 years | 17 | NS |

|
−1.05 (−1.50 to −0.60) | <.001 | 97 |

|
|
|
T1D/T2D | Baseline HbA1c <8.0% | 6 | NS |

|
−0.26 (−0.43 to −0.10) | .03 | NS |

|
|
|
T1D/T2D | Baseline HbA1c ≥ 8.0% | 8 | NS |

|
−0.64 (−0.93 to −0.35) | .03 | NS |

|
|
|
T1D/T2D | Baseline HbA1c <9.0% | NS | NS |

|
−0.35 | NS | NS |

|
|
|
T1D/T2D | Baseline HbA1c ≥9.0% | NS | NS |

|
−1.22 | NS | NS |

|
| Digital self-management (mobile health) [66,84] | |||||||||
|
|
T2D | Baseline HbA1c <8.0% | 4 | 696 |

|
−0.33 (−0.59 to −0.06) | .02 | 70 |

|
|
|
T1D/T2D | Average age <25 years | 5 | NS |

|
−0.5 (−0.8 to −0.1) | .54 | NS |

|
|
|
T1D/T2D | Average age ≥25 years | 17 | NS |

|
−0.5 (−0.7 to −0.3) | .54 | NS |

|
|
|
T1D/T2D | BMI ≥25 kg/m2 | 7 | NS |

|
−0.8 (−1.1 to −0.5) | .93 | NS |

|
|
|
T1D/T2D | 24 kg/m2≤ BMI <25 kg/m2 | 3 | NS |

|
−0.8 (−1.7 to 0.1) | .93 | NS |

|
|
|
T1D/T2D | BMI unspecified | 12 | NS |

|
−0.3 (−0.5 to −0.1) | .93 | NS |

|
| Digital self-management (SMS) [75] | |||||||||
|
|
T2D | Age <55 years | 5 | NS |

|
−0.65 (−0.88 to −0.41) | <.001 | NS |

|
|
|
T2D | Age ≥55 years | 5 | NS |

|
−0.42 (−0.56 to −0.27) | .006 | NS |

|
|
|
T2D | Diagnosish <7 years ago | 4 | NS |

|
−0.61 (−0.79 to −0.42) | .001 | NS |

|
|
|
T2D | Diagnosish ≥7 years ago | 3 | NS |

|
−0.37 (−0.62 to −0.13) | .031 | NS |

|
|
|
T2D | Baseline HbA1c <8.0% | 5 | NS |

|
−0.71 (−0.93 to −0.48) | <.001 | NS |

|
|
|
T2D | Baseline HbA1c ≥8.0% | 5 | NS |

|
−0.38 (−0.53 to −0.24) | <.001 | NS |

|
aMD: mean difference.
bHbA1c: glycated hemoglobin.
cT1D: type 1 diabetes.
dThe direction of the arrows indicates potential clinically relevant reduction rates (see Table 2).
eGreen arrows show statistical significance.
fNS: not specified—cases in which no data were provided. Missing data on statistical significance were handled as nonsignificant.
gT2D: type 2 diabetes.
hDiagnosis time: time since first diagnosis of diabetes.
In terms of BP control, a −10 mmHg reduction in SBP or a −5 mmHg reduction in DBP is considered as clinically relevant [38]. No exact clinical relevance margins for lipid profiles could be prespecified, as European guidelines recommend a risk-based approach with regard to the presence of CV risk or established CV disease [32].
To compare overall treatment effects between baseline and follow-up, meta-analyses reporting treatment effects as mean differences (MD), standardized mean difference (SMD), Cohen d, and Hedge g were included. For heterogeneity testing, results of I2 statistics (indicating variation across studies that is not due to chance) were used. A value of <40% indicates a low, 30%-60% a moderate, and >75% a substantial-to-high level of heterogeneity [39].
Results
Review Characteristics
Overall, 3564 references were identified. After title-abstract screening, 119 records remained for further full-text analysis. Details of the extracted evidence are provided in the Multimedia Appendices 3-9. The most important reasons for exclusion were low quality (n=15) and applied interventions not matching the prespecified telemedicine definition (n=14; annex section V). Overall, 46 studies were included in this umbrella review (Figure 1). In Figure 1, the Preferred Reporting Items for Systematic Reviews and Meta-analyses flowchart shows the study selection process, covering the single steps of identification via a 2-step screening (title and abstract and full-text base) for eligibility and inclusion into the qualitative synthesis of this review.
Figure 1.
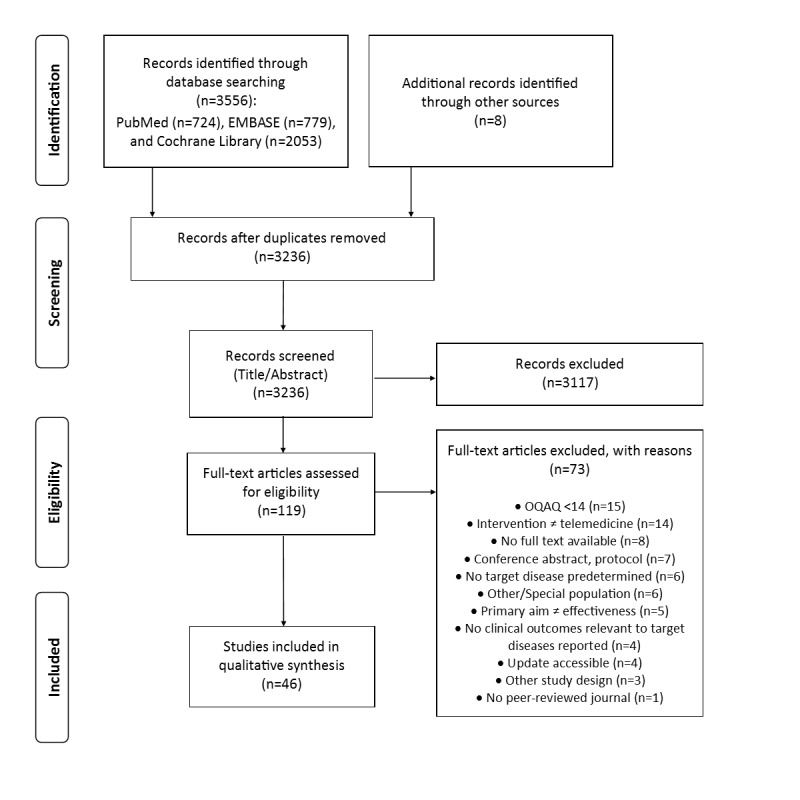
Preferred Reporting Items for Systematic Reviews and Meta-analyses flowchart of the study selection process. OQAQ: Overview Quality Assessment Questionnaire.
Study Characteristics
Study designs included 16 systematic reviews [40-55], 7 meta-analyses [56-62], 19 records conducting both a systematic review and meta-analysis [63-81], three systematic reviews and meta-analyses with meta-regression [82-84], and one systematic review and network meta-analysis [85]. The included meta-studies were published between 2009 and 2018, the majority was published after 2015 (Multimedia Appendix 5) and focused on diabetes. No high-quality reviews or meta-analyses were found targeting patients with dyslipidemia.
An analysis of primary studies revealed significant overlaps among the 26 meta-analyses (Multimedia Appendix 5). The majority of primary studies were published after 2010 (Multimedia Appendix 5).
On a scale of 0 to 18, the median OQAQ score of the 46 included studies was 16 (IQR 1), indicating that they were good quality systematic reviews and meta-analyses.
Results of Included Systematic Reviews
Data from 16 systematic reviews were extracted (Multimedia Appendix 6) [40-54]. Diabetes was the chronic disease covered most often by the included reviews. A total of 5 systematic reviews dealt with T2D [41,43,46,49]; however, only one systematic review dealt with T1D [53]. Both types were studied together for a total of 4 times [42,45,48,51], four other systematic reviews did not specify which type of diabetes they focused on [44,50,52,54]. Among the other diseases studied, hypertension was the most common [40,44,50,55]. The results of the included systematic reviews were mixed, presenting a tendency for positive effects of telemedicine, in general, and digitally supported self-management using phones or apps on HbA1c [42,44,54] and SBP/DBP [40,55]. In contrast, the majority of studies evaluating telemonitoring and self-monitoring interventions found no significant improvements in HbA1c, fasting plasma glucose, or BP [49-51].
Results of Meta-Analyses
Effectiveness of Telemedicine in Patients With Diabetes
Digital self-management in diabetes (T1D and T2D) was analyzed by 13 meta-analyses, of which 4 meta-analyses evaluated the effectiveness of mobile health (mHealth) [63,65,84] and one meta-analysis evaluated the use of social network services (SNS) [78]. In digital self-management interventions, those including prescription (−0.75%, 95% CI −1.05 to −0.43; P=.013), teleconsultation (−0.62%; P<.001), and health information technologies on top of usual care (mostly based on tele-education; −0.57%, 95% CI −0.71 to −0.43; P<.005) showed significant clinically relevant mean reductions in HbA1c [60,72,80]. Digital self-management interventions using mHealth showed significant clinically relevant reductions in HbA1c if they provided remote access to usual care (−0.55%, 95% CI −0.72 to −0.38; P<.001), used one or two features (−0.52%, 95% CI −0.76 to −0.28; P<.001), used SMS-based feedback (−0.64%, 95% CI −1.09 to −0.19; P=.005), included a potential risk intervention (−0.61%, 95% CI −0.95 to −0.27; P<.001), included a structured display (−0.69%, 95% CI −0.32 to −1.06; P=.008), provided medication management (−0.56%, 95% CI −0.99 to −0.13; P<.001), and provided lifestyle modification management (−0.52%, 95% CI −0.84 to −0.20; P<.001) [63,65,80]. SNS applied in diabetes self-management interventions proved to be effective if they were Web-based (−0.51%, 95% CI −0.68 to −0.34; P<.001) or combined Web-based SNS with mobile technologies (−0.54%, 95% CI −0.72 to −0.37; P<.001) [78].
Overall mean reductions in HbA1c of telemedicine interventions in patients with T1D ranged between −0.12% and −0.86% [60,61,63,70,72,78,82,84]. Overall mean reductions were mostly not significant. Highest mean reductions were observed for the combination of tele-education with teleconsultation (−0.91%, 95% CI −1.21 to −0.61), although data on statistical significance were not provided [70]. No significant clinically relevant reductions for population characteristics such as baseline HbA1c or age were identified in patients with T1D.
Although varying in range (−0.01% to −1.13%), telemedicine significantly reduced HbA1c in patients with T2D [59,60,64,66,68,72,73,75,76,78,79,81,85].
Effectiveness According to Intervention Duration
Table 3 summarizes the effectiveness of telemedicine in patients with diabetes by comparing intervention durations.
Significant and clinically relevant reductions were found for short (≤3 months), middle (4-8 months), and long (>12 months) intervention durations. Digital health education, analyzed in the meta-analysis by Angeles et al [56], on average, reduced HbA1c above the predefined clinical relevance margin (HbA1c ≤−0.5%; Table 2). However, only the effects of interventions with a long-term study duration (12 months) were statistically significant (−0.55%, 95% CI −0.7 to −0.39; P<.001). Although three meta-analyses observed a tendency for higher reduction rates in shorter intervention durations [59,75,85], no general significant differences in reduction rates among intervention durations were found.
Short-term intervention durations (≤6 months) of digital self-management showed greater mean reductions (−0.56%; P<.001) [60] compared with mid- and long-term durations (>6 months) [60,72]. Clinically relevant mean reductions in SNS were significant for short-term intervention durations (≤3 months) as well [78]. Using Web-based SNS for digital self-management proved to be significantly effective in the three pooled follow-up measurements. Again, the greatest mean reductions were apparent during the short-term (≤3 months) follow-up (−0.54%, 95% CI −0.80 to −0.28; P<.001) [78].
Effectiveness According to Feedback Mode, Frequency, and Intensity
Although telemedicine interventions using feedback functions significantly reduced HbA1c in several studies [56,60-63,66,67,72,80], the highest reduction rates were found when no personalized feedback was provided (−0.61%, 95% CI −1.40 to 0.19; P=.001) [63]. No difference in HbA1c change was found for the type of health care professionals providing the feedback (eg, nurses or physicians) [72].
In addition, feedback, provided either via human telephone calls (−1.13%, 95% CI −1.51 to −0.75; P<.05) or via the internet (−0.62%, 95% CI −0.82 to −0.42; P<.001), significantly reduced HbA1c to a clinically relevant extent (≤−0.5 change) [68,81]. Higher frequency of provider feedback also showed greater reductions in HbA1c (−1.12%, 95% CI −1.32 to −0-91; P<.001) when compared with mean reduction rates of interventions utilizing low frequency rates (−0.33%, 95% CI −0.59 to −0.07; P<.01) [82] (Table 4).
Table 4.
Effectiveness of telemedicine on glycated hemoglobin in patients with diabetes, according to feedback mode, frequency, and intensity.
| Application category and type of diabetes | Feedback characteristics | Trials, n | Patients, n | Outcome | MDa (95% CI) of percent change in HbA1c | P value | I2 (%) | Grading of Recommendations, Assessment, Development, and Evaluation | |
| Telemedicine [70,82] | |||||||||
|
|
T1Db | App based | 5 | 336 |
 c
c
|
−0.37 (−0.94 to 0.20) | .20 | 81.74 |

|
|
|
T1D | High intensityd | 13 | NS |
 c
c
|
−0.24 (−0.49 to 0.01) | NSe | NS |

|
|
|
T1D | ≠ High intensity | 14 | NS |
 c
c
|
−0.09 (−0.23 to 0.06) | NS | NS |

|
|
|
T1D | Audit + feedback | 24 | NS |
 c
c
|
−0.22 (−0.38 to −0.06) | NS | NS |

|
|
|
T1D | No audit + feedback | 4 | NS |
 c
c
|
0.01 (−0.27 to −0.30) | NS | NS |

|
| Digital self-management [59,68,72,81,83] | |||||||||
|
|
T2Df | Human call/telephone | 5 | NS |
 c,g
c,g
|
−1.13 (−1.51 to −0.75) | <.05 | 38 |

|
|
|
T2D | Human call/telephone | 12 | NS |
 c,g
c,g
|
−0.53 (−0.81 to −0.26) | <.001 | 76.35 |

|
|
|
T2D | Manual | 6 | 1180 |
 c,g
c,g
|
−0.44 (−0.74 to −0.15) | .04 | NS |

|
|
|
T2D | Manual | 22 | NS |
 c,g
c,g
|
−0.50 (−0.65 to −0.34) | <.001 | 67.2 |

|
|
|
T2D | Automated | 5 | NS |
 c,g
c,g
|
−0.50 (−0.69 to −0.32) | <.001 | 0 |

|
|
|
T2D | Automated calls | 2 | NS |
 c
c
|
−0.01 (−0.32 to 0.29) | .94 | 0 |

|
|
|
T2D | Automated text | 9 | NS |
 c
c
|
−0.36 (−0.47 to −0.24) | NS | 0 |

|
|
|
T2D | Text message | 3 | 380 |
 c,g
c,g
|
−0.52 (−1.04 to 0.00) | <.05 | 73.5 |

|
|
|
T2D | Web-based | 13 | 2405 |
 c,g
c,g
|
−0.41 (−0.55 to −0.27) | <.05 | 79.6 |

|
|
|
T2D | Web-based | 19 | NS |
 c,g
c,g
|
−0.62 (−0.82 to −0.42) | <.001 | 77.57 |

|
| Digital self-management (mobile health) [63,82,84] | |||||||||
|
|
T2D | Low frequency | 7 | 440 |
 c,g
c,g
|
−0.33 (−0.59 to −0.07) | .01 | 47.35 |

|
|
|
T2D | High frequency | 5 | 326 |
 c,g
c,g
|
−1.12 (−1.32 to −0.91) | <.001 | 0 |

|
|
|
T1D/T2D | Personalized feedback | 8 | NS |
 c,g
c,g
|
−0.43 (−0.74 to −0.12) | <.001 | 75 |

|
|
|
T1D/T2D | ≠ Personalized feedback | 4 | NS |
 c,g
c,g
|
−0.61 (−1.40 to 0.19) | .001 | 81 |

|
|
|
T1D/T2D | Frequency (daily) | 15 | NS |
 c
c
|
−0.6 (−0.9 to −0.4) | .27 | NS |

|
|
|
T1D/T2D | Frequency (weekly) | 3 | NS |
 c
c
|
−0.2 (−0.6 to 0.2) | .27 | NS |

|
|
|
T1D/T2D | Frequency (not specified) | 4 | NS |
 c
c
|
−0.4 (−0.5 to −0.2) | .27 | NS |

|
aMD: mean difference.
bT1D: type 1 diabetes.
cThe direction of the arrows indicates potential clinically relevant reduction rates (see Table 2).
dDirect contact at least once a week.
eNS: not specified—cases in which no data were provided. Missing data on statistical significance were handled as nonsignificant.
fT2D: type 2 diabetes.
gGreen arrows show statistical significance.
The meta-regression carried out by Huang et al [68] also revealed that factors we previously disregarded, such as study location, sample size, and feedback methods, were associated significantly with changes in HbA1c. Their combination in multivariate meta-regression analyses explained almost 100% of the variance among studies.
Effectiveness According to Population Characteristics
Subgroup analyses on the effectiveness of telemedicine in certain patient populations (Table 5) were carried out by 12 meta-analyses [60-62,66,68,70,72,75,79,83-85].
Although differences were not always significant, those subgroups with higher baseline HbA1c (>7.5% or >8.0%) showed increased reductions rates [62,68,70,72,79,83,85]. Only for interventions categorized as digital self-management using SMS, the reduction rates were higher (−0.71%, 95% CI −0.93 to −0.48; P<.001) in patients with lower baseline HbA1c (<8%) when compared with those with higher (≥8%) baseline HbA1c (−0.38%, 95% CI −0.53 to −0.24; P<.001) [75]. Using meta-regression methods, Kebede et al [83] found significant reduction rates in HbA1c for baseline HbA1c >7.5% (beta=−.44, 95% CI −0.81 to −0.06; P=.031), self-monitoring of behavioral outcomes, such as diets and physical activity (beta=−1.21, 95% CI −1.95 to −0.46; P=.009), and for support in problem solving (beta=−1.30, 95% CI −2.05 to −0.54; P=.007).
Significant differences for age groups were sparse, as only three meta-analysis found significant reduction rates in patients with T2D [75] and both types combined [60,61]. The meta-analysis by Saffari et al [75] on SMS-based digital self-management found significantly greater mean reductions (P=.006) in HbA1c for patients younger than 55 years (−0.65%, 95% CI −0.88 to −0.41; P<.001) when compared with the older age group (−0.42%, 95% CI −0.56 to −0.27; P<.001) [75]. The greatest significant mean reductions were observed for patients with diabetes aged 41 to 50 years (−1.83%, 95% CI −3.17 to −0.48; P<.001) and those over 50 years (−1.05%, 95% CI −1.50 to −0.60; P<.001) [60,61].
For digital self-management, a shorter time since diagnosis (<8.5 years) was associated with significantly greater mean reduction in HbA1c (−0.83%, 95% CI −1.10 to −0.56; P=.007) when compared with patients being diagnosed more than 8.5 years ago (−0.22%, 95% CI −0.44 to 0.01; P=.007) [79]. Similarly, patients diagnosed less than 7 years ago showed higher mean reductions (−0.61%, 95% CI −0.79 to −0.42) compared with their counterparts (−0.37%, 95% CI −0.61 to −0.13; P=.03) after using SMS-based digital self-management [75].
Effect of Telemedicine on Blood Pressure in Patients With Diabetes
Mean reductions of both SBP and DBP were also found in T2D patients. Toma et al [78] found highly significant mean reductions in patients with both T1D and T2D for SBP (−3.47 mmHg, 95% CI −5.01 to −1.94; P<.001) and DBP (−1.84 mmHg, 95% CI −2.98 to −0.70; P=.002) because of Web- and mobile-based SNS interventions. Evaluating the effect of digitally supported dietary interventions in patients with chronic diseases, Kelly et al [69] also reported significant mean reductions in SBP (−5.91 mmHg, 95% CI −11.14 to −0.68; P=.003) in the diabetes subgroup (although showing high heterogeneity between the two studies; I²=69%). Although no information on statistical significance was provided, Lee et al [85] showed greatest mean reductions in SBP for the telemedicine subgroups focusing on tele-education (−4.05 mmHg, 95% CI −5.64 to −1.10), as well as those combining tele-education and telemonitoring (−3.91 mmHg, 95% CI −10.07 to 2.25). Analyzing the data of four studies, Cui et al [66] found nonsignificant reductions for both DBP (−1.76 mmHg, 95% CI −3.6 to 0.07; P=.06) and SBP (−2.62 mmHg, 95% CI −5.6 to 0.36; P=.08). Digitally supported dietary interventions in patients with diabetes resulted in significant mean reductions in SBP (−5.91 mmHg, 95% CI −11.14 to −0.68; P=.003) [69]. However, none of the presented reduction rates reached the predefined clinical relevance margin.
Effect of Telemedicine on Lipid Profiles in Patients With Diabetes
Only 8 of the included studies reported on lipid profiles; 4 in T1D/T2D patients [56,65,72,78], 2 in T2D patients [73,85], 1 in T1D patients [70], and 1 in several chronic diseases [69]. On the basis of these studies, evidence on the effectiveness of telemedicine in lowering LDL-c or TGC or increasing high-density lipoprotein cholesterol (HDL-c) in patients with diabetes is scarce and heterogeneous. Marcolino et al [72] found evidence that digital self-management applications for both diabetes types can reduce LDL-c levels; however, although significant, the effect was small (−6.6 mg/dL, 95% CI −8.3 to −4.9; P<.001; I²=24%) [72]. In addition, for both types of diabetes, Toma et al [78] found evidence for a significant improvement in TC (−5.74 mg/dL, 95% CI −9.71 to −1.78; P<.005; I²=53%), HDL (1.90 mg/dL, 95% CI 0.24 to 3.57; P=.02; I²=19%), and TGC (−11.05 mg/dL, 95% CI −20.92 to −1.18; P<.03; I²=0%). Reductions in LDL (−1.15 mg/dL, 95% CI −5.19 to 2.88; P=.58; I2=47%) were not significant. Again, for patients with T2D, the pooled analysis of Lee et al [85] found little and rather inconsistent effects, be it for LDL-c, HDL-c, TC, and TGC.
Effects of Telemedicine in Patients With Hypertension
A total of 3 of the included meta-analyses focused on patients with hypertension [57,71]. Although the two analyses of Omboni et al [57,58] focused on home BP monitoring, Liu et al [71] examined the effect of internet-based interventions. Liu et al [71] reported a significant overall mean reduction in SBP (−3.8 mmHg, 95% CI −5.63 to −2.06; P=.001) and DBP (−2.1 mmHg, 95% CI −3.51 to −0.65; P<.05). Owing to the identified heterogeneity for SBP (I²=61%), the authors carried out a subgroup analysis, revealing that mean change in SBP was greater in long-term interventions (6-12 months; −5.8 mmHg, 95% CI −4.3 to −4.1) when compared with short-term interventions (<6 months; −3.47 mmHg, 95% CI −5.2 to −1.7). However, data on statistical significance were not provided [71]. The results of Omboni et al [57] show significant mean reductions in SBP when using ambulatory measurement (−2.28 mmHg, 95% CI −4.32 to −0.24; P<.05). In their more recent analysis, they included studies evaluating additional features such as combined data transmission to physician, feedback, advice, and medication regulation. This time, they observed significant mean reductions (−3.48 mmHg, 95% CI −5.31 to −1.64; P<.001) [58].
Grading of Evidence
The quality assessment of outcomes using the GRADE framework revealed the following levels of certainty (Multimedia Appendix 8). Of the 219 HbA1c outcomes assessed overall, 170 (77.63%) outcomes were rated as very low evidence and 42 (19.18%) outcomes were rated as low evidence. All of the 42 outcomes measuring SBP or DBP resulted in very low ratings of overall certainty (Table 6).
Table 6.
Grading of Recommendations, Assessment, Development, and Evaluation assessment of certainty of glycated hemoglobin and systolic blood pressure/diastolic blood pressure outcomes.
| GRADEa | HbA1cb, n (%) | SBPc/DBPd, n (%) |

|
—e | — |

|
2 (0.92) | — |

|
42 (19.8) | — |

|
170 (77.63) | 42 (100) |
aGRADE: Grading of Recommendations, Assessment, Development, and Evaluation.
bHbA1c: glycated hemoglobin.
cSBP: systolic blood pressure.
dDBP: diastolic blood pressure.
eNot applicable.
The main reasons for low-quality assessment results in both outcome categories were as follows:
Unclear or high-risk of bias: Missing allocation concealment, missing blinding of patients, study personnel and outcome assessors, high risk of selection bias and reporting bias (intention-to-treat analysis), and high or unclear losses to follow-up.
Inconsistency: High heterogeneity in subgroup analysis, inconsistent confidence intervals crossing the mark for no effect.
Indirectness: Differences in populations (type of diabetes, baseline HbA1c, age, duration of diabetes, and gender), differences in interventions (devices used, components combined, feedback intensity and frequency, and professional or professionals involved), and differences in settings (community, hospital, and primary care) in the pooled subgroups.
Imprecision: Large confidence intervals and small effect sizes mostly because of small sample sizes.
Publication bias: Visual and statistical or missing publication bias assessment; the reasons for the increased risk of publication bias mostly referred to the overrepresentation of smaller studies with higher effect sizes (favoring telemedicine). Furthermore, one reason is the paucity of data on mid- and long-term effects (6-12 months).
Underreporting of relevant information: Reporting of study duration, dropouts/missing data, and follow-up time. Guidance on this matter was further complicated as some authors did not make a clear distinction between study duration and follow-up [61].
Only for two outcomes (0.92%) measuring HbA1c, overall certainty was judged as moderate (Tables 5 and 6). In 6 (5 in HbA1c and 1 in DBP) cases, the outcomes of subgroup analyses were not assessed using GRADE, as results of only one trial were used by the authors of meta-analyses to pool data.
As the initial search did not identify records primarily targeting patients with dyslipidemia and subgroup analyses on HDL, LDL, TC, and TGC were sparse, no grading of lipid outcomes was performed.
Discussion
Principal Findings
High-level evidence from the 46 included meta-analyses and systematic reviews suggests that telemedicine interventions can be effective in improving clinical outcomes in patients with diabetes. Observed reduction rates are comparable with those of nonpharmacological eg, nutrition intervention [86] or increased physical activity [87]) and some pharmacological interventions (−0.5% to −1.25%) [88]. The observed reduction rates are encouraging, bearing in mind that the United Kingdom Prospective Diabetes Study (UKPDS) revealed that a 0.9% decrease in HbA1c was associated with a 25% reduction in microvascular complications, a 10% decrease in diabetes-related mortality, and a 6% reduction in all-cause mortality [89].
In patients with diabetes, significant differences between telemedicine interventions and for certain population characteristics were identified. Telemedicine interventions embedded in frequent and intense patient-provider interactions and interventions with short durations (≤6 months) showed greater benefits. In addition, higher reduction rates were found for recently diagnosed patients and those with higher baseline HbA1c. However, quality assessment using GRADE revealed that overall and subgroup-specific certainty of evidence is low to very low. Therefore, the identified reduction rates have to be dealt with caution when translating them into evidence-based recommendations for treatment guidelines.
Telemedicine was not found to have a significant and clinically meaningful impact on BP. Assessing the certainty of SBP and DBP outcomes, GRADE only revealed very low ratings. No records primarily targeting patients with dyslipidemia were found.
According to the recent consensus report of the ADA and European Association for the Study of Diabetes, the application of telemedicine in diabetes is associated with a modest improvement in glycemic control [31]. The European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines for the management of arterial hypertension also report that telemonitoring and mobile phone apps may lead to improved outcomes for patients with hypertension [15]. Our umbrella review updates this assessment of the effectiveness of telemedicine with special regard to intervention components, population characteristics, and it provides an in-depth assessment of the certainty of evidence. A brief summary of the study results can be found in Textbox 1.
Brief summary of the study results. HbA1c: glycated hemoglobin; GRADE: Grading of Recommendations, Assessment, Development, and Evaluation.
Telemedicine has the potential to improve clinical outcomes in patients with diabetes. Mixed results were found for patients with hypertension, none for those with dyslipidemia.
Specific characteristics of the intervention (eg, high frequency and intensity of feedback/interaction and short treatment duration) and the patient (age <55 years, high baseline HbA1c, and recent diagnosis) seem to be associated with increased benefits in patients with diabetes.
An assessment of the overall certainty using GRADE resulted in low and very low ratings, indicating that effects have to be dealt with caution.
Intervention Components
Looking at the characteristics of the telemedicine applications analyzed by the included meta-analyses, those encompassing frequent and intense patient-provider communication interactions showed greater benefit in HbA1c reduction. This was especially true for the combination of tele-case management with either teleconsultation (−1.20%, 95% CI −2.30 to −0.10; P<.001) or telemonitoring (−0.54%, 95% CI −2.44 to −0.06) in patients with T2D [85]. Similarly, analogue disease self-management education interventions are known to be more effective in terms of HbA1c reduction when they offer additional support (eg, structured dietary or exercise interventions) [37,90]. On the basis of the analysis by Kastner et al [91], the combination of case management and self-management in addition to education provides potential for reduced HbA1c levels when compared with education and plain care coordination. Therefore, continuous and frequent communication, either via intensive feedback [68,81] or psychological support [92], seems most promising.
With a longer duration of follow-ups, the quality of evidence steadily declines because of considerable risk of bias and heterogeneity of study populations and interventions included. As for digital self-management, the evidence base is larger yet more diverse, as SMS (1 meta-analysis), social networks (1 meta-analysis), and mHealth apps (4 meta-analysis) can be used. However, the quality of evidence for digital self-management is low to very low, irrespective of the basal technology or the type of diabetes.
In our analysis, some application types were found to reduce BP, for example, in SBP after tele-education (−4.05 mmHg, 95% CI −5.64 to −1.10), as well as strategies combining tele-education and telemonitoring (−3.91 mmHg) [85]. In patients with diabetes, Web- and mobile-based SNS interventions significantly reduced DBP (−3.47 mmHg) [78], and digitally supported dietary interventions led to significant mean reductions in SBP (−5.91 mmHg) [69]. Although these reduction rates did not reach clinical relevance of ≥10 mmHg in SBP or ≥5 mmHg in DBP, they are similar to the expected reduction rates of nonpharmacologic interventions in patients with hypertension. Our results support the identified potential of telemonitoring and mobile phone apps in home BP self-monitoring, articulated in the current ESC/ESH guideline [15] because of the additional advantages in memorizing, reviewing, and transmitting BP measurements [58,93].
On the basis of the identified potential of telemedicine to provide individual self-management support, it is likely that embedded or additional components may have an additive and/or sustained impact on clinical outcomes. As such, recent evidence identified social media [94,95], gamification [96], and machine learning models [97,98] as successful strategies to improve clinical outcomes and prevent disease-related complications.
Population Characteristics
According to the included meta-analyses, telemedicine interventions are more effective for patients with T2D, higher baseline HbA1c, and a more recent diagnosis of diabetes. The increased potential for newly diagnosed patients was also identified by systematic reviews [99,100] and landmark trials such as the UKPDS [5]. As for hypertension, the results did not allow for population-specific analyses, which might be because of the rather passive interventions studies, such as telemonitoring.
With the exception of a baseline BMI <30 kg/m2 (considered in one meta-analysis), all population-specific subgroup analyses were of low or very low evidence, the latter being more prevalent. This is also true for differences among age groups, for which no significant evidence was found. However, there was a tendency for higher reduction rates of HbA1c in younger patient cohorts with diabetes [60,75]. Owing to the increased risk of elevated BP levels (> 130/80) and long-term risk of CV events, the current ESC/ESH guideline suggests treatment in younger adults (<50 years) [15]. In terms of age-specific BP control, ADA suggests focusing on DBP in patients under 50 years [101].
Overall, as the results concerning population characteristics are diverse and of low to very low quality, our analysis did not find enough high-level evidence to recommend telemedicine for the treatment of patients with both hypertension and diabetes.
Only reviews or meta-analyses reporting lipid outcomes in patients with diabetes were found. The extracted results on lipid outcomes are sparse and too heterogeneous to draw a conclusion on the effectiveness of telemedicine on these outcomes [41,44,46,49,53,55]. With special regard to the effects of statins, as the first-line agents used to decrease cholesterol in the management of dyslipidemia and hypertension, the extracted effects of telemedicine on lipid profiles can be considered as minor [15,32]. However, recent evidence underlines the promising potential of mobile phone-based self-monitoring interventions in patients with lipid metabolism disorders [102], because of the combination of therapy and lifestyle behavior changes.
Limitations
Robust systematic reviewing methods were used to generate an overview of high-quality evidence on the effects of telemedicine in three prevalent chronic conditions. The protocol of this umbrella review was presented to the research community [103]. However, this study has several limitations, starting with the initial search and inclusion process. Although a comprehensive and piloted search strategy has been used, it is possible that some relevant studies were missed, if the exact search terms were used neither by the authors nor by the databases examined (Multimedia Appendix 10). The search within three different databases, complemented by a comprehensive hand search within the most important journals in the field of telemedicine, the use of MeSH terms, and a broad set of keywords, may have limited this risk of selection bias.
In addition, some full-text articles were excluded because of their definition and application of the term “telemedicine,” which did not comply with standardized definitions, such as the one provided by Sood et al [17]. Although the technology applied to deliver telemedicine has made tremendous advances during the past 10 years, our thorough application of the telemedicine definition and subgroup analyses using the GRADE assessment ensures comparability of intervention types. Intensive full-text assessment was applied to limit the bias of falsely including/excluding systematic reviews and meta-analyses because of mislabeling and inadequate delimitations of efficacy and effectiveness, as studies focusing on efficacy were excluded. As telemedicine is mostly embedded in low-risk interventions, mortality as an outcome was not considered. Although internationally recommended to be reported in addition to changes in HbA1c [104], parameters such as the time below, in, or above range, the number of hypoglycemic episodes, and quality of life were only reported by a few study authors and therefore did not allow for evidence-based guidance on this matter. A reason may be the publication date (median=2011) of the primary studies (Multimedia Appendix 6), which is before these recommendations were made.
We also included different types of statistical analyses, including meta-analysis, network-meta-analysis, and meta-regression. Although the majority reported MD, there was a considerable methodological heterogeneity. This was because of the application of fixed- and random-effects models, as well as the reporting of SMD, Hedge g, or Cohen d instead of MD. Comparing the aggregated results of those statistical values without considering their weight (on the basis of the number of studies or number of patients per subgroup analysis) may have biased our analysis. However, this process was impeded by inconsistent reporting of baseline data such as the number of trials and participants in subgroup analysis. In addition, it is likely that reporting bias within the included systematic reviews and meta-analysis also affected our analysis. When studying the funnel plots, we also observed a tendency toward overrepresented smaller studies with higher effect sizes (favoring telemedicine), thereby increasing the risk of publication bias within some of the included analyses.
Further Methodological Considerations
Owing to the multimodal and individualized nature of digital interventions, the low GRADE results, especially the increase I2, are not surprising. In addition, we found significant overlaps among the primary studies of the included records (Multimedia Appendix 6). The results of the subgroup analysis therefore need to be considered with exceptional care before recommending certain intervention components for certain populations. However, as GRADE is the established procedure to evaluate the certainty of evidence when developing or updating guidelines, new quality assessment tools appropriate for the tailored and hybrid design of digital interventions should be developed [105]. Along with the need for rather adaptive study designs, there is growing criticism on the suitability of RCTs for evaluating the effectiveness of digital interventions. In light of current efforts to support the clinical effectiveness, quality, and economic value of new technologies by using new assessment frameworks [106-110], our analysis underlines the challenges in this endeavor. In addition, future assessments on the clinical effectiveness should also include consolidated core outcome sets and patient-reported outcomes [111,112]. However, as stated by the included records, longer study durations and more rigorously designed studies are needed for these future research needs.
Conclusions
The results of this umbrella review indicate that telemedicine has the potential to improve clinical outcomes in patients with diabetes. Evidence extracted from systematic reviews and meta-analyses of RCTs showed subgroup-specific effectiveness rates favoring certain intervention and population characteristics. However, as indicated by the low GRADE ratings, evidence on the effectiveness of telemedicine in the three chronic conditions can be considered as limited.
Future updates of clinical care and practice guidelines should carefully assess the methodological quality of studies and assess the overall certainty of subgroup-specific outcomes before recommending telemedicine interventions for certain patient populations.
Acknowledgments
The authors wish to thank Jochen Schmitt, Hendrikje Lantzsch, and Kristin Kemple for their valuable input to the conduct of the umbrella review and the design of the manuscript. The work on this review was partly funded by the European Social Fund and the Free State of Saxony (Grant number: 100310385).
Parts of this manuscript were presented on a poster during a German Conference (Diabetes Kongress 2019) on May 30, 2019 and during a talk on October 10, 2019, (18 Deutscher Kongress für Versorgungsforschung) in Berlin.
Abbreviations
- ADA
American Diabetes Association
- BP
blood pressure
- CV
cardiovascular
- DBP
diastolic blood pressure
- ESC/ESH
European Society of Cardiology/European Society of Hypertension
- GRADE
Grading of Recommendations, Assessment, Development, and Evaluation
- HbA1c
glycated hemoglobin
- HDL
high-density lipoprotein
- HDL-c
high-density lipoprotein cholesterol
- ICT
information and communication technology
- LDL
low-density lipoprotein
- LDL-c
low-density lipoprotein cholesterol
- MD
mean difference
- mHealth
mobile health
- OQAQ
Oxford Quality Assessment Questionnaire
- PICOT
Population, Intervention, Control, Outcome, and Time
- RCT
randomized controlled trial
- SBP
systolic blood pressure
- SMD
standardized mean difference
- SNS
social network services
- T1D
type 1 diabetes
- T2D
type 2 diabetes
- TC
total cholesterol
- TGC
triglycerides
- UKPDS
United Kingdom Prospective Diabetes Study
Appendix
Population, Intervention, Control, Outcome, and Time criteria and principles of data extraction.
Number of manuscripts per journal after title/abstract screening.
Quality assessment for study inclusion.
List of excluded studies with reasons.
Characteristics of included records.
Results of included systematic reviews.
Results of included meta-analyses.
Grading of Recommendations Assessment, Development and Evaluation of glycated haemoglobin and diastolic blood pressure/systolic blood pressure outcomes.
References of multimedia appendices.
Electronic database search strategy.
Footnotes
Authors' Contributions: PT and LH designed the study and also conducted the search. PT and LH were responsible for critical evaluation, analysis, and presentation of the results. PT, LH, and SO conducted the GRADE Assessment. PT and LH drafted the manuscript. PT, LH, SO, and PS critically evaluated the article and gave their final approval before submission.
Conflicts of Interest: None declared.
References
- 1.Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R, IDF Diabetes Atlas Committee Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9 edition. Diabetes Res Clin Pract. 2019 Nov;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- 2.Iglay K, Hannachi H, Joseph Howie P, Xu J, Li X, Engel SS, Moore LM, Rajpathak S. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016 Jul;32(7):1243–52. doi: 10.1185/03007995.2016.1168291. [DOI] [PubMed] [Google Scholar]
- 3.Song Y, Liu X, Zhu X, Zhao B, Hu B, Sheng X, Chen L, Yu M, Yang T, Zhao J. Increasing trend of diabetes combined with hypertension or hypercholesterolemia: NHANES data analysis 1999-2012. Sci Rep. 2016 Nov 2;6:36093. doi: 10.1038/srep36093. doi: 10.1038/srep36093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwarz PE, Timpel P, Harst L, Greaves CJ, Ali MK, Lambert J, Weber MB, Almedawar MM, Morawietz H. Blood sugar regulation for cardiovascular health promotion and disease prevention: JACC health promotion series. J Am Coll Cardiol. 2018 Oct 9;72(15):1829–44. doi: 10.1016/j.jacc.2018.07.081. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(18)36953-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352(9131):837–53. [PubMed] [Google Scholar]
- 6.- Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. Br Med J. 1998 Sep 12;317(7160):703–13. http://europepmc.org/abstract/MED/9732337. [PMC free article] [PubMed] [Google Scholar]
- 7.Turnbull F, Neal B, Algert C, Chalmers J, Chapman N, Cutler J, Woodward M, MacMahon S, Blood Pressure Lowering Treatment Trialists' Collaboration Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005 Jun 27;165(12):1410–9. doi: 10.1001/archinte.165.12.1410. [DOI] [PubMed] [Google Scholar]
- 8.Thomopoulos C, Parati G, Zanchetti A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10 - Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J Hypertens. 2017 May;35(5):922–44. doi: 10.1097/HJH.0000000000001276. [DOI] [PubMed] [Google Scholar]
- 9.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R, Cholesterol Treatment Trialists' (CTT) Collaborators Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005 Oct 8;366(9493):1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 10.ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association 9. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S86–104. doi: 10.2337/dc18-S009. [DOI] [PubMed] [Google Scholar]
- 12.Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, Cypress M, Faulkner P, Fischl AH, Francis T, Kolb LE, Lavin-Tompkins JM, MacLeod J, Maryniuk M, Mensing C, Orzeck EA, Pope DD, Pulizzi JL, Reed AA, Rhinehart AS, Siminerio L, Wang J, 2017 Standards Revision Task Force 2017 National Standards for Diabetes Self-Management Education and Support. Diabetes Care. 2017 Oct;40(10):1409–19. doi: 10.2337/dci17-0025. [DOI] [PubMed] [Google Scholar]
- 13.He X, Li J, Wang B, Yao Q, Li L, Song R, Shi X, Zhang J. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine. 2017 Mar;55(3):712–31. doi: 10.1007/s12020-016-1168-2. [DOI] [PubMed] [Google Scholar]
- 14.Sherifali D, Bai J, Kenny M, Warren R, Ali MU. Diabetes self-management programmes in older adults: a systematic review and meta-analysis. Diabet Med. 2015 Nov;32(11):1404–14. doi: 10.1111/dme.12780. [DOI] [PubMed] [Google Scholar]
- 15.Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GY, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, ESC Scientific Document Group 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1;39(33):3021–104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 16.Otto L, Harst L, Schlieter H, Wollschlaeger B, Richter P, Timpel P. Towards a Unified Understanding of eHealth and Related Terms – Proposal of a Consolidated Terminological Basis. Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies; BIOSTEC'18; Jan 19-21, 2018; Funchal, Madeira, Portugal. Health Informatics Europe; 2018; Madeira: HEALTHINF; 2018. pp. 533–9. http://www.scitepress.org/DigitalLibrary/Link.aspx? [DOI] [Google Scholar]
- 17.Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, Merrell RC. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health. 2007 Oct;13(5):573–90. doi: 10.1089/tmj.2006.0073. [DOI] [PubMed] [Google Scholar]
- 18.Kruse CS, Soma M, Pulluri D, Nemali NT, Brooks M. The effectiveness of telemedicine in the management of chronic heart disease - a systematic review. JRSM Open. 2017 Mar;8(3):2054270416681747. doi: 10.1177/2054270416681747. http://europepmc.org/abstract/MED/28321319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanlon P, Daines L, Campbell C, McKinstry B, Weller D, Pinnock H. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. 2017 May 17;19(5):e172. doi: 10.2196/jmir.6688. https://www.jmir.org/2017/5/e172/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Diabetes Association 5. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S51–4. doi: 10.2337/dc18-S005. [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association 6. Glycemic Targets: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S55–64. doi: 10.2337/dc18-S006. [DOI] [PubMed] [Google Scholar]
- 22.Greenwood DA, Gee PM, Fatkin KJ, Peeples M. A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. J Diabetes Sci Technol. 2017 Sep;11(5):1015–27. doi: 10.1177/1932296817713506. http://europepmc.org/abstract/MED/28560898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010 Nov;79(11):736–71. doi: 10.1016/j.ijmedinf.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 24.Kitsiou S, Paré G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: An overview of systematic reviews. PLoS One. 2017;12(3):e0173160. doi: 10.1371/journal.pone.0173160. http://dx.plos.org/10.1371/journal.pone.0173160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ekeland AG, Bowes A, Flottorp S. Methodologies for assessing telemedicine: a systematic review of reviews. Int J Med Inform. 2012 Jan;81(1):1–11. doi: 10.1016/j.ijmedinf.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 26.Dinesen B, Nonnecke B, Lindeman D, Toft E, Kidholm K, Jethwani K, Young HM, Spindler H, Oestergaard CU, Southard JA, Gutierrez M, Anderson N, Albert NM, Han JJ, Nesbitt T. Personalized Telehealth in the future: a global research agenda. J Med Internet Res. 2016 Mar 1;18(3):e53. doi: 10.2196/jmir.5257. https://www.jmir.org/2016/3/e53/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kirley K, Sachdev N. Digital health-supported lifestyle change programs to prevent Type 2 Diabetes. Diabetes Spectr. 2018 Nov;31(4):303–9. doi: 10.2337/ds18-0019. http://europepmc.org/abstract/MED/30510384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015 Sep;13(3):132–40. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 29.Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018 Mar 1;7(1):39. doi: 10.1186/s13643-018-0695-8. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-018-0695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, GRADE Working Group What is 'quality of evidence' and why is it important to clinicians? Br Med J. 2008 May 3;336(7651):995–8. doi: 10.1136/bmj.39490.551019.BE. http://europepmc.org/abstract/MED/18456631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2018 Dec;41(12):2669–701. doi: 10.2337/dci18-0033. http://europepmc.org/abstract/MED/30291106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Catapano AL, Graham I, de Backer G, Wiklund O, Chapman MJ, Drexel H, Hoes AW, Jennings CS, Landmesser U, Pedersen TR, Reiner Ž, Riccardi G, Taskinen M, Tokgozoglu L, Verschuren WM, Vlachopoulos C, Wood DA, Zamorano JL, Cooney MT, ESC Scientific Document Group 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J. 2016 Oct 14;37(39):2999–3058. doi: 10.1093/eurheartj/ehw272. [DOI] [PubMed] [Google Scholar]
- 33.Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44(11):1271–8. doi: 10.1016/0895-4356(91)90160-b. [DOI] [PubMed] [Google Scholar]
- 34.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ, GRADE Working Group GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J. 2008 Apr 26;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. http://europepmc.org/abstract/MED/18436948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, New Jersey, United States: Wiley; 2019. [Google Scholar]
- 36.Little RR, Rohlfing CL, Sacks DB, National Glycohemoglobin Standardization Program (NGSP) Steering Committee Status of hemoglobin A1c measurement and goals for improvement: from chaos to order for improving diabetes care. Clin Chem. 2011 Feb;57(2):205–14. doi: 10.1373/clinchem.2010.148841. http://www.clinchem.org/cgi/pmidlookup?view=long&pmid=21148304. [DOI] [PubMed] [Google Scholar]
- 37.Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns. 2016 Jun;99(6):926–43. doi: 10.1016/j.pec.2015.11.003. https://linkinghub.elsevier.com/retrieve/pii/S0738-3991(15)30116-6. [DOI] [PubMed] [Google Scholar]
- 38.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. Br Med J. 2009 May 19;338:b1665. doi: 10.1136/bmj.b1665. http://europepmc.org/abstract/MED/19454737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schünemann H, Brożek J, Guyatt G, Oxman A. GRADEpro GDT. 2013. [2020-01-16]. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations https://gdt.gradepro.org/app/handbook/handbook.html.
- 40.Alessa T, Abdi S, Hawley MS, de Witte L. Mobile apps to support the self-management of hypertension: systematic review of effectiveness, usability, and user satisfaction. JMIR Mhealth Uhealth. 2018 Jul 23;6(7):e10723. doi: 10.2196/10723. https://mhealth.jmir.org/2018/7/e10723/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aspry KE, Furman R, Karalis DG, Jacobson TA, Zhang AM, Liptak GS, Cohen JD. Effect of health information technology interventions on lipid management in clinical practice: a systematic review of randomized controlled trials. J Clin Lipidol. 2013;7(6):546–60. doi: 10.1016/j.jacl.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 42.Baron J, McBain H, Newman S. The impact of mobile monitoring technologies on glycosylated hemoglobin in diabetes: a systematic review. J Diabetes Sci Technol. 2012 Sep 1;6(5):1185–96. doi: 10.1177/193229681200600524. http://europepmc.org/abstract/MED/23063046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Connelly J, Kirk A, Masthoff J, MacRury S. The use of technology to promote physical activity in Type 2 diabetes management: a systematic review. Diabet Med. 2013 Dec;30(12):1420–32. doi: 10.1111/dme.12289. [DOI] [PubMed] [Google Scholar]
- 44.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev. 2012 Dec 12;12:CD007459. doi: 10.1002/14651858.CD007459.pub2. http://europepmc.org/abstract/MED/23235644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.El-Gayar O, Timsina P, Nawar N, Eid W. A systematic review of IT for diabetes self-management: are we there yet? Int J Med Inform. 2013 Aug;82(8):637–52. doi: 10.1016/j.ijmedinf.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Farmer AJ, McSharry J, Rowbotham S, McGowan L, Ricci-Cabello I, French DP. Effects of interventions promoting monitoring of medication use and brief messaging on medication adherence for people with Type 2 diabetes: a systematic review of randomized trials. Diabet Med. 2016 May;33(5):565–79. doi: 10.1111/dme.12987. [DOI] [PubMed] [Google Scholar]
- 47.Fu H, McMahon SK, Gross CR, Adam TJ, Wyman JF. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2017 Sep;131:70–81. doi: 10.1016/j.diabres.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 48.Holmen H, Wahl AK, Småstuen MC, Ribu L. Tailored communication within mobile apps for diabetes self-management: a systematic review. J Med Internet Res. 2017 Jun 23;19(6):e227. doi: 10.2196/jmir.7045. https://www.jmir.org/2017/6/e227/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mushcab H, Kernohan WG, Wallace J, Martin S. Web-based remote monitoring systems for self-managing Type 2 Diabetes: a systematic review. Diabetes Technol Ther. 2015 Jul;17(7):498–509. doi: 10.1089/dia.2014.0296. [DOI] [PubMed] [Google Scholar]
- 50.Paré G, Moqadem K, Pineau G, St-Hilaire C. Clinical effects of home telemonitoring in the context of diabetes, asthma, heart failure and hypertension: a systematic review. J Med Internet Res. 2010 Jun 16;12(2):e21. doi: 10.2196/jmir.1357. https://www.jmir.org/2010/2/e21/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Porter J, Huggins CE, Truby H, Collins J. The effect of using mobile technology-based methods that record food or nutrient intake on diabetes control and nutrition outcomes: a systematic review. Nutrients. 2016 Dec 17;8(12):pii: E815. doi: 10.3390/nu8120815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rush KL, Hatt L, Janke R, Burton L, Ferrier M, Tetrault M. The efficacy of telehealth delivered educational approaches for patients with chronic diseases: A systematic review. Patient Educ Couns. 2018 Aug;101(8):1310–21. doi: 10.1016/j.pec.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 53.Russell-Minda E, Jutai J, Speechley M, Bradley K, Chudyk A, Petrella R. Health technologies for monitoring and managing diabetes: a systematic review. J Diabetes Sci Technol. 2009 Nov 1;3(6):1460–71. doi: 10.1177/193229680900300628. http://europepmc.org/abstract/MED/20144402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sun C, Malcolm JC, Wong B, Shorr R, Doyle M. Improving glycemic control in adults and children with Type 1 Diabetes with the use of smartphone-based mobile applications: a systematic review. Can J Diabetes. 2019 Feb;43(1):51–8.e3. doi: 10.1016/j.jcjd.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 55.Vargas G, Cajita MI, Whitehouse E, Han H. Use of short messaging service for hypertension management: a systematic review. J Cardiovasc Nurs. 2017;32(3):260–70. doi: 10.1097/JCN.0000000000000336. http://europepmc.org/abstract/MED/27111819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Angeles RN, Howard MI, Dolovich L. The effectiveness of web-based tools for improving blood glucose control in patients with diabetes Mellitus: a meta-analysis. Can J Diabetes. 2011;35(4):344–52. doi: 10.1016/S1499-2671(11)54011-0. [DOI] [Google Scholar]
- 57.Omboni S, Guarda A. Impact of home blood pressure telemonitoring and blood pressure control: a meta-analysis of randomized controlled studies. Am J Hypertens. 2011 Sep;24(9):989–98. doi: 10.1038/ajh.2011.100. [DOI] [PubMed] [Google Scholar]
- 58.Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens. 2013 Mar;31(3):455–67; discussion 467. doi: 10.1097/HJH.0b013e32835ca8dd. [DOI] [PubMed] [Google Scholar]
- 59.Shen Y, Wang F, Zhang X, Zhu X, Sun Q, Fisher E, Sun X. Effectiveness of internet-based interventions on glycemic control in patients with Type 2 Diabetes: meta-analysis of randomized controlled trials. J Med Internet Res. 2018 May 7;20(5):e172. doi: 10.2196/jmir.9133. https://www.jmir.org/2018/5/e172/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Su D, Zhou J, Kelley MS, Michaud TL, Siahpush M, Kim J, Wilson F, Stimpson JP, Pagán JA. Does telemedicine improve treatment outcomes for diabetes? A meta-analysis of results from 55 randomized controlled trials. Diabetes Res Clin Pract. 2016 Jun;116:136–48. doi: 10.1016/j.diabres.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 61.Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali G, Rusch E. Clinical effectiveness of Telemedicine in Diabetes Mellitus: a meta-analysis of 42 randomized controlled trials. Telemed J E Health. 2019 Jul;25(7):569–83. doi: 10.1089/tmj.2018.0128. [DOI] [PubMed] [Google Scholar]
- 62.Wu C, Wu Z, Yang L, Zhu W, Zhang M, Zhu Q, Chen X, Pan Y. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 2018 Oct;97(43):e12962. doi: 10.1097/MD.0000000000012962. doi: 10.1097/MD.0000000000012962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu Y, Yao X, Vespasiani G, Nicolucci A, Dong Y, Kwong J, Li L, Sun X, Tian H, Li S. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth. 2017 Mar 14;5(3):e35. doi: 10.2196/mhealth.6522. https://mhealth.jmir.org/2017/3/e35/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alharbi NS, Alsubki N, Jones S, Khunti K, Munro N, de Lusignan S. Impact of Information Technology-based interventions for Type 2 Diabetes Mellitus on glycemic control: a systematic review and meta-analysis. J Med Internet Res. 2016 Nov 25;18(11):e310. doi: 10.2196/jmir.5778. https://www.jmir.org/2016/11/e310/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bonoto BC, de Araújo VE, Godói IP, de Lemos LL, Godman B, Bennie M, Diniz LM, Junior AA. Efficacy of mobile apps to support the care of patients with Diabetes Mellitus: a systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2017 Mar 1;5(3):e4. doi: 10.2196/mhealth.6309. https://mhealth.jmir.org/2017/3/e4/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cui M, Wu X, Mao J, Wang X, Nie M. T2DM self-management via smartphone applications: a systematic review and meta-analysis. PLoS One. 2016;11(11):e0166718. doi: 10.1371/journal.pone.0166718. http://dx.plos.org/10.1371/journal.pone.0166718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Faruque LI, Wiebe N, Ehteshami-Afshar A, Liu Y, Dianati-Maleki N, Hemmelgarn BR, Manns BJ, Tonelli M, Alberta Kidney Disease Network Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. Can Med Assoc J. 2017 Mar 6;189(9):E341–64. doi: 10.1503/cmaj.150885. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=27799615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Huang Z, Tao H, Meng Q, Jing L. Management of endocrine disease. Effects of telecare intervention on glycemic control in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Eur J Endocrinol. 2015 Mar;172(3):R93–101. doi: 10.1530/EJE-14-0441. [DOI] [PubMed] [Google Scholar]
- 69.Kelly JT, Reidlinger DP, Hoffmann TC, Campbell KL. Telehealth methods to deliver dietary interventions in adults with chronic disease: a systematic review and meta-analysis. Am J Clin Nutr. 2016 Dec;104(6):1693–702. doi: 10.3945/ajcn.116.136333. [DOI] [PubMed] [Google Scholar]
- 70.Lee SW, Ooi L, Lai YK. Telemedicine for the management of glycemic control and clinical outcomes of Type 1 Diabetes Mellitus: a systematic review and meta-analysis of randomized controlled studies. Front Pharmacol. 2017;8:330. doi: 10.3389/fphar.2017.00330. doi: 10.3389/fphar.2017.00330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu S, Dunford SD, Leung YW, Brooks D, Thomas SG, Eysenbach G, Nolan RP. Reducing blood pressure with internet-based interventions: a meta-analysis. Can J Cardiol. 2013 May;29(5):613–21. doi: 10.1016/j.cjca.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 72.Marcolino MS, Maia JX, Alkmim MB, Boersma E, Ribeiro AL. Telemedicine application in the care of diabetes patients: systematic review and meta-analysis. PLoS One. 2013;8(11):e79246. doi: 10.1371/journal.pone.0079246. http://dx.plos.org/10.1371/journal.pone.0079246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pal K, Eastwood SV, Michie S, Farmer A, Barnard ML, Peacock R, Wood B, Edwards P, Murray E. Computer-based interventions to improve self-management in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2014 Jun;37(6):1759–66. doi: 10.2337/dc13-1386. [DOI] [PubMed] [Google Scholar]
- 74.Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K. Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obes Metab. 2009 Oct;11(10):913–30. doi: 10.1111/j.1463-1326.2009.01057.x. [DOI] [PubMed] [Google Scholar]
- 75.Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes. 2014 Dec;8(4):275–85. doi: 10.1016/j.pcd.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 76.Spencer-Bonilla G, Ponce OJ, Rodriguez-Gutierrez R, Alvarez-Villalobos N, Erwin PJ, Larrea-Mantilla L, Rogers A, Montori VM. A systematic review and meta-analysis of trials of social network interventions in type 2 diabetes. BMJ Open. 2017 Aug 21;7(8):e016506. doi: 10.1136/bmjopen-2017-016506. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28827256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Suksomboon N, Poolsup N, Nge YL. Impact of phone call intervention on glycemic control in diabetes patients: a systematic review and meta-analysis of randomized, controlled trials. PLoS One. 2014;9(2):e89207. doi: 10.1371/journal.pone.0089207. http://dx.plos.org/10.1371/journal.pone.0089207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toma T, Athanasiou T, Harling L, Darzi A, Ashrafian H. Online social networking services in the management of patients with diabetes mellitus: systematic review and meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2014 Nov;106(2):200–11. doi: 10.1016/j.diabres.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 79.Wu IX, Kee JC, Threapleton DE, Ma RC, Lam VC, Lee EK, Wong SY, Chung VC. Effectiveness of smartphone technologies on glycaemic control in patients with type 2 diabetes: systematic review with meta-analysis of 17 trials. Obes Rev. 2018 Jun;19(6):825–38. doi: 10.1111/obr.12669. [DOI] [PubMed] [Google Scholar]
- 80.Yoshida Y, Boren SA, Soares J, Popescu M, Nielson SD, Simoes EJ. Effect of health information technologies on glycemic control among patients with type 2 diabetes. Curr Diab Rep. 2018 Oct 18;18(12):130. doi: 10.1007/s11892-018-1105-2. http://europepmc.org/abstract/MED/30338403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhai Y, Zhu W, Cai Y, Sun D, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore) 2014 Dec;93(28):e312. doi: 10.1097/MD.0000000000000312. doi: 10.1097/MD.0000000000000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hou C, Xu Q, Diao S, Hewitt J, Li J, Carter B. Mobile phone applications and self-management of diabetes: a systematic review with meta-analysis, meta-regression of 21 randomized trials and GRADE. Diabetes Obes Metab. 2018 Aug;20(8):2009–13. doi: 10.1111/dom.13307. [DOI] [PubMed] [Google Scholar]
- 83.Kebede MM, Zeeb H, Peters M, Heise TL, Pischke CR. Effectiveness of digital interventions for improving glycemic control in persons with poorly controlled type 2 diabetes: a systematic review, meta-analysis, and meta-regression analysis. Diabetes Technol Ther. 2018 Nov;20(11):767–82. doi: 10.1089/dia.2018.0216. [DOI] [PubMed] [Google Scholar]
- 84.Liang X, Wang Q, Yang X, Cao J, Chen J, Mo X, Huang J, Wang L, Gu D. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med. 2011 Apr;28(4):455–63. doi: 10.1111/j.1464-5491.2010.03180.x. [DOI] [PubMed] [Google Scholar]
- 85.Lee SW, Chan CK, Chua SS, Chaiyakunapruk N. Comparative effectiveness of telemedicine strategies on type 2 diabetes management: a systematic review and network meta-analysis. Sci Rep. 2017 Oct 4;7(1):12680. doi: 10.1038/s41598-017-12987-z. doi: 10.1038/s41598-017-12987-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Snorgaard O, Poulsen GM, Andersen HK, Astrup A. Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2017;5(1):e000354. doi: 10.1136/bmjdrc-2016-000354. http://europepmc.org/abstract/MED/28316796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pai L, Li T, Hwu Y, Chang S, Chen L, Chang P. The effectiveness of regular leisure-time physical activities on long-term glycemic control in people with type 2 diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2016 Mar;113:77–85. doi: 10.1016/j.diabres.2016.01.011. https://linkinghub.elsevier.com/retrieve/pii/S0168-8227(16)00060-7. [DOI] [PubMed] [Google Scholar]
- 88.Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC. The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care. 2010 Aug;33(8):1859–64. doi: 10.2337/dc09-1727. http://europepmc.org/abstract/MED/20484130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.- Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352(9131):854–65. [PubMed] [Google Scholar]
- 90.Pillay J, Armstrong MJ, Butalia S, Donovan LE, Sigal RJ, Vandermeer B, Chordiya P, Dhakal S, Hartling L, Nuspl M, Featherstone R, Dryden DM. Behavioral programs for type 2 diabetes mellitus: a systematic review and network meta-analysis. Ann Intern Med. 2015 Dec 1;163(11):848–60. doi: 10.7326/M15-1400. [DOI] [PubMed] [Google Scholar]
- 91.Kastner M, Cardoso R, Lai Y, Treister V, Hamid JS, Hayden L, Wong G, Ivers NM, Liu B, Marr S, Holroyd-Leduc J, Straus SE. Effectiveness of interventions for managing multiple high-burden chronic diseases in older adults: a systematic review and meta-analysis. Can Med Assoc J. 2018 Aug 27;190(34):E1004–12. doi: 10.1503/cmaj.171391. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=30150242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Viana LV, Gomes MB, Zajdenverg L, Pavin EJ, Azevedo MJ, Brazilian Type 1 Diabetes Study Group Interventions to improve patients' compliance with therapies aimed at lowering glycated hemoglobin (HbA1c) in type 1 diabetes: systematic review and meta-analyses of randomized controlled clinical trials of psychological, telecare, and educational interventions. Trials. 2016 Feb 17;17:94. doi: 10.1186/s13063-016-1207-6. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-016-1207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Parati G, Omboni S. Role of home blood pressure telemonitoring in hypertension management: an update. Blood Press Monit. 2010 Dec;15(6):285–95. doi: 10.1097/MBP.0b013e328340c5e4. [DOI] [PubMed] [Google Scholar]
- 94.Gabarron E, Årsand E, Wynn R. Social media use in interventions for diabetes: rapid evidence-based review. J Med Internet Res. 2018 Aug 10;20(8):e10303. doi: 10.2196/10303. https://www.jmir.org/2018/8/e10303/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Litchman ML, Edelman LS, Donaldson GW. Effect of diabetes online community engagement on health indicators: cross-sectional study. JMIR Diabetes. 2018 Apr 24;3(2):e8. doi: 10.2196/diabetes.8603. https://diabetes.jmir.org/2018/2/e8/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Theng Y, Lee JW, Patinadan PV, Foo SS. The use of videogames, gamification, and virtual environments in the self-management of diabetes: a systematic review of evidence. Games Health J. 2015 Oct;4(5):352–61. doi: 10.1089/g4h.2014.0114. [DOI] [PubMed] [Google Scholar]
- 97.Faruqui SH, Du Y, Meka R, Alaeddini A, Li C, Shirinkam S, Wang J. Development of a deep learning model for dynamic forecasting of blood glucose level for type 2 diabetes mellitus: secondary analysis of a randomized controlled trial. JMIR Mhealth Uhealth. 2019 Nov 1;7(11):e14452. doi: 10.2196/14452. https://mhealth.jmir.org/2019/11/e14452/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jahmunah V, Oh SL, Wei JK, Ciaccio EJ, Chua K, San TR, Acharya UR. Computer-aided diagnosis of congestive heart failure using ECG signals - a review. Phys Med. 2019 Jun;62:95–104. doi: 10.1016/j.ejmp.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 99.Weaver RG, Hemmelgarn BR, Rabi DM, Sargious PM, Edwards AL, Manns BJ, Tonelli M, James MT. Association between participation in a brief diabetes education programme and glycaemic control in adults with newly diagnosed diabetes. Diabet Med. 2014 Dec;31(12):1610–4. doi: 10.1111/dme.12513. [DOI] [PubMed] [Google Scholar]
- 100.Bongaerts BW, Müssig K, Wens J, Lang C, Schwarz P, Roden M, Rathmann W. Effectiveness of chronic care models for the management of type 2 diabetes mellitus in Europe: a systematic review and meta-analysis. BMJ Open. 2017 Mar 20;7(3):e013076. doi: 10.1136/bmjopen-2016-013076. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28320788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.de Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, Rossing P, Zoungas S, Bakris G. Diabetes and hypertension: a position statement by The American Diabetes Association. Diabetes Care. 2017 Sep;40(9):1273–84. doi: 10.2337/dci17-0026. [DOI] [PubMed] [Google Scholar]
- 102.Steinert A, Eicher C, Haesner M, Steinhagen-Thiessen E. Effects of a long-term smartphone-based self-monitoring intervention in patients with lipid metabolism disorders. Assist Technol. 2018 Jun 26;:1–8. doi: 10.1080/10400435.2018.1493710. [DOI] [PubMed] [Google Scholar]
- 103.Timpel P, Harst L. German Medical Science. GMS Publishing House; 2018. Oct 12, [2020-01-16]. Effectiveness of Telemedicine Interventions for the Most Prevalent Chronic Diseases in German Primary Care – A Protocol for an Umbrella Review https://www.egms.de/static/en/meetings/dkvf2018/18dkvf200.shtml. [Google Scholar]
- 104.Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, Bosi E, Buckingham BA, Cefalu WT, Close KL, Cobelli C, Dassau E, DeVries JH, Donaghue KC, Dovc K, Doyle FJ, Garg S, Grunberger G, Heller S, Heinemann L, Hirsch IB, Hovorka R, Jia W, Kordonouri O, Kovatchev B, Kowalski A, Laffel L, Levine B, Mayorov A, Mathieu C, Murphy HR, Nimri R, Nørgaard K, Parkin CG, Renard E, Rodbard D, Saboo B, Schatz D, Stoner K, Urakami T, Weinzimer SA, Phillip M. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019 Aug;42(8):1593–603. doi: 10.2337/dci19-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Law LM, Wason JM. Design of telehealth trials--introducing adaptive approaches. Int J Med Inform. 2014 Dec;83(12):870–80. doi: 10.1016/j.ijmedinf.2014.09.002. https://linkinghub.elsevier.com/retrieve/pii/S1386-5056(14)00167-1. [DOI] [PubMed] [Google Scholar]
- 106.Agarwal S, LeFevre AE, Lee J, L'Engle K, Mehl G, Sinha C, Labrique A, WHO mHealth Technical Evidence Review Group Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. Br Med J. 2016 Mar 17;352:i1174. doi: 10.1136/bmj.i1174. [DOI] [PubMed] [Google Scholar]
- 107.Kidholm K, Clemensen J, Caffery LJ, Smith AC. The Model for Assessment of Telemedicine (MAST): A scoping review of empirical studies. J Telemed Telecare. 2017 Oct;23(9):803–13. doi: 10.1177/1357633X17721815. [DOI] [PubMed] [Google Scholar]
- 108.Enam A, Torres-Bonilla J, Eriksson H. Evidence-based evaluation of eHealth interventions: systematic literature review. J Med Internet Res. 2018 Nov 23;20(11):e10971. doi: 10.2196/10971. https://www.jmir.org/2018/11/e10971/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.National Institute for Health and Care Excellence National Institute for Health and Care Excellence. 2019. [2020-01-16]. Evidence Standards Framework for Digital Health Technologies (March 2019) https://www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf.
- 110.Eysenbach G, CONSORT-EHEALTH Group CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011 Dec 31;13(4):e126. doi: 10.2196/jmir.1923. https://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Clarke M, Williamson PR. Core outcome sets and systematic reviews. Syst Rev. 2016 Jan 20;5:11. doi: 10.1186/s13643-016-0188-6. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Anker SD, Agewall S, Borggrefe M, Calvert M, Caro JJ, Cowie MR, Ford I, Paty JA, Riley JP, Swedberg K, Tavazzi L, Wiklund I, Kirchhof P. The importance of patient-reported outcomes: a call for their comprehensive integration in cardiovascular clinical trials. Eur Heart J. 2014 Aug 7;35(30):2001–9. doi: 10.1093/eurheartj/ehu205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Population, Intervention, Control, Outcome, and Time criteria and principles of data extraction.
Number of manuscripts per journal after title/abstract screening.
Quality assessment for study inclusion.
List of excluded studies with reasons.
Characteristics of included records.
Results of included systematic reviews.
Results of included meta-analyses.
Grading of Recommendations Assessment, Development and Evaluation of glycated haemoglobin and diastolic blood pressure/systolic blood pressure outcomes.
References of multimedia appendices.
Electronic database search strategy.


